SOUTHWEST UTAH PUBLIC HEALTH FOUNDATION SPRING 2025
BLOOD PRESSURE
POSTPARTUM DEPRESSION PG. 18 MORTALITY INSIGHTS PG. 16 PG. 10



SOUTHWEST UTAH PUBLIC HEALTH FOUNDATION SPRING 2025
BLOOD PRESSURE
POSTPARTUM DEPRESSION PG. 18 MORTALITY INSIGHTS PG. 16 PG. 10


It is incredibly rewarding to continue sharing insights through this magazine that we hope will help improve your life. Today, information is available on almost any topic at the click of a button. Yet, with so much out there, it can be difficult to determine what is truly reliable. That’s why we value trusted sources—those that carefully vet the information for accuracy. We hope this magazine serves as one of those trusted resources for you— offering clear, practical, and dependable health information.
With so much information out there, it can be difficult to determine what is truly reliable. We hope this magazine serves as a trusted resource for you.
In this issue, we begin an ongoing discussion about the leading causes of death in our communities. We focus on what can be done to address them in both our personal lives as well as in our communities. We also address a broad range of topics that can impact your health and those around you. We invite you to take a closer look at any of the topics that speak to you. We have an extensive library of resources on our website (swuhealth.gov) and in past issues of HEALTH Magazine (issuu. com/swuhealth) that allow you to dive deeper and learn more.
The effort that goes into these magazine issues is astounding. These remarkable people care about bringing a quality message to you that can make a difference in your life. Bridging the gap between what we know and what we do isn’t always easy, but small steps toward better health add up. Thank you for reading our magazine and supporting our efforts as your health department.
Here’s to your good health!


Sincerely,

David W. Blodgett, MD, MPH Southwest Utah Public Health Department (SWUPHD) Director & Health Officer

ASSISTING




By Peter Jones, SWUPHD Epidemiologist
For many of us, disease outbreaks that make international headlines often seem like something out of a movie. We read about severe symptoms, rapid spread, and strict containment measures in far-off places.
One disease recently in the news is the Marburg virus—a rare but dangerous hemorrhagic fever in the same family as Ebola. Outbreaks in parts of Africa have sparked intense media coverage because of Marburg’s high fatality rate and rapid spread through direct contact with bodily fluids. The symptoms can be dramatic: high fevers, intense headaches, and—in seri-
ous cases—uncontrolled bleeding. However, it’s important to keep the threat of Marburg virus in context:
• No cases have been reported in the United States.
• Outbreaks remain confined to certain regions where health experts are collaborating to limit further spread.
• If you do not travel to or have direct contact with someone from an affected region, your personal risk is extremely low.
The bottom line? While Marburg virus is undeniably scary, it’s very unlikely to pose an immediate threat to those of us in Southwest Utah. The reality is that the illnesses that most impact our health aren’t exotic—they're the ones already circulating in our community.
Sometimes, it’s the less dramatic diseases that end up causing the most disruption. Data from the Southwest Utah Public Health Department consistently show that a few communicable diseases remain our top concerns year after year:
• The flu can lead to severe complications—particularly for older adults, young children, and those with underlying health conditions.
• Annual vaccination, frequent handwashing, and staying home when you’re ill significantly reduce the spread.
• RSV primarily affects young children and older adults, but anyone can catch it.
• The virus often spreads in close-contact settings like daycares, schools, and nursing homes.
• Vigilance and consistent hygiene are key to prevention.


• Commonly known as the “stomach flu,” norovirus can strike quickly and cause vomiting and diarrhea.
• Outbreaks often occur in schools, longterm care facilities, and other crowded settings.
• Proper handwashing and frequent disinfection of surfaces are essential for control.
• These arise from consuming contaminated foods or beverages—often due to improper handling, cooking, or storage.
• Common culprits include Salmonella, E. coli, and Campylobacter.
• Preventive measures include thorough cooking of meats, avoiding cross-contamination in the kitchen, and washing produce properly.
While these illnesses may not command headlines like Marburg virus, we tend to underestimate their impact because they seem familiar or routine. Fortunately, the spread of these infections can be decreased through consistent practices of hygiene, safe handling, and social considerations.
The Southwest Utah Public Health Department will keep area residents informed of any significant outbreaks, whether the pathogen is common or unusual. Local health alerts are shared with local news agencies and posted online at swuhealth.gov and social media platforms (search for swuhealth on Facebook and Instagram).

Learn More: For local disease trends, see our Annual Report on page 24.
Walking is one of the easiest ways to improve your health, but getting started may not be so easy if you’ve been sedentary for a while. It's common to face barriers when starting an exercise routine, whether it's battling fatigue, struggling with stress or depression, or simply feeling too busy. Walking, however, doesn't have to be complicated—it’s one simple action that can set the foundation for a healthier, more active life.
It’s important to acknowledge that taking

that first step can feel like a challenge. Here are a few barriers many people face and some tips to help overcome them: Mental Blocks and Depression: Depression and anxiety can make even small tasks feel like mountains (like taking a walk). But even a short 5-minute walk can help alleviate symptoms over time. Start small, focus on the act of moving, and know that any step forward is a win. Don’t be surprised if you end up walking farther than you though you would.


Time Constraints: In our busy lives, finding time for exercise can be difficult. If you feel like you don’t have 30 minutes, start with 5 or 10. Breaking up your walks into smaller sessions throughout the day can still provide benefits without overwhelming your schedule.
Physical Limitations: If you have health issues or pain, walking might feel intimidating. It’s okay to take it slow and listen to your body. Begin with shorter walks on flat ground and gradually increase your distance as your body adjusts.
Lack of Motivation: Getting started can be hard if you don’t feel motivated. Try to make walking more enjoyable—invite a friend, listen to your favorite podcast, or explore a new route to keep things interesting. If you’re ready to take that first step, here’s how to make it feel more manageable:
Start Small and Set Your Intention. Begin with just 5-10 minutes. Even a short walk is a step toward better health. Set a goal to walk every day, starting with a small commitment and working your way up.
Choose a Comfortable Pace. Don’t worry about speed. Walk at a pace that feels right for you. The goal is to get moving, not to run a marathon. A brisk walk that makes you breathe slightly heavier is enough to feel the benefits.
Create a Routine. Pick a time of day that works for you—whether in the morning, at lunch, or after work. Building it into your daily routine helps establish consistency and makes it easier to keep going.
Celebrate Your Progress. Tracking your steps or milestones—like walk-

ing for 10 minutes or hitting 5,000 steps—helps build motivation. Celebrate each achievement, no matter how small, and be proud of your consistency.
Walk with Someone. Walking doesn’t have to be a solitary activity. Invite a friend, family member, or even a pet to join you. Social support can make walking feel less like a chore and more like a fun activity.
Start with a Focus on Mental Health. If depression or anxiety is holding you back, try to focus on the mental health benefits of walking. Getting outside and moving your body can help boost endorphins, improve mood, and reduce feelings of sadness or stress. Think of your walk as an act of self-care.
If you're ready to get moving, Southwest Utah offers many beautiful areas throughout the five counties, whether you prefer an easy stroll or a more scenic adventure. Start in your neighborhood or get online to find out what trails are near you:
St. George: maps.sgcity.org/sgcitytrails
Washington City: washingtoncity.org/recreation/trails
Washington County: trails.greaterzion.com
Kanab/Kane County: visitsouthernutah.com/trail-maps
Cedar City: cedarcityut.gov/246/Trails
You can also look for walking/hiking routes in Bryce and Zion National Parks, Cedar Breaks and Grand Staircase-Escalante National Monuments, and Snow Canyon State Park. The possibilities are endless, but more important than where is when: start your walking journey today!



Motherhood is beautiful, but it can also be challenging. The changes that come with pregnancy, childbirth, and parenting can affect physical and mental health. The signs of anxiety or depression can sometimes be brushed aside, misunderstood, or never talked about at all. Here are the stories of two local moms who share their postpartum experiences so that other moms can feel seen and supported and know they’re not alone.
It could have been a combination of things, but I was pregnant with our fourth child as we moved to a different town on the weekend that COVID-19 shut-downs started. Two weeks later, I had my baby.
I remember having a nurse call a couple of times to check in on me and ask if I was ex-
periencing any postpartum depression, which seemed like such an odd question because why would I be depressed? I wanted this baby, and now he’s here, and everything’s great! Recovery from my first three kids had gone well, and I don’t think I understood what depression felt like.
And so, when it hit me, I didn't recognize it right away. I kept thinking, “What’s wrong with me?” I felt numb. I didn’t feel like smiling or laughing; I just cried all the time. I wondered if I would ever be happy again. I had never experienced feelings like this in my life,


and it lasted for months, far longer than it should have.
I had always been into exercise and would gradually get back into working out after my previous pregnancies, but the pandemic had closed the gyms down. Finally, amidst my loneliness, it finally dawned on me, “I don’t have to be in the house this whole time - why am I not going outside to at least take a walk?” So I started going on walks to get some exercise and fresh air. As I got my body moving, the world felt much better, and my mood improved as the depression faded away, but I don’t know that I quite made the correlation at the time.
Fast forward to baby number five…who was a surprise. Thinking we were done, I had moved on with other plans and had settled into a routine that included fun fitness classes with music and people. But being pregnant and giving birth slowed me down, and it was hard to adjust. I loved this baby more than anything, but I felt like I’d lost my identity.
Loneliness and sadness crept back in, but by now I’d learned that exercise wasn’t just about staying fit—it was about my mental health. I truly believe it increases my energy and happiness and makes me a better mom. That’s what I was missing the last time. So, after four weeks, I jumped back into the classes, and the depression got significantly better.
Looking back, I probably would have paced myself a little more, maybe started with some walks, knowing that things were going to get better. I think moms should know that there’s no specific time frame to recover from postpartum depression, but it does get better. Talk to a husband, a friend, maybe a therapist; getting help is not a bad thing.
Before my pregnancy, I felt healthy—I was a dance student and instructor, physically active for about four hours a day. I loved walking, rock climbing, and canyoneering. Mental healthwise, I had some anxiety and was on medication, and I felt like I had a good handle on it.
Around six weeks into my pregnancy, I started dealing with severe morning sickness that turned into hyperemesis gravidarum (HG). It was much worse than I expected—I couldn't keep food or water down for over 24 hours at a time. I needed IVs to stay hydrated and was on modified bed rest for most of my pregnancy. It was draining mentally and physically—I had lost a lot of weight and strength and developed fears about food and public spaces. The anxiety
from HG made it feel like a never-ending cycle.
I was nervous about taking medication during pregnancy, but after consulting with my doctor, I started a mood stabilizer and felt much more balanced. I was concerned about the effects on my baby, but I felt reassured by the doctors' guidance.
Shortly after delivery, the anxiety hit hard, especially with worries about my baby’s feeding and sleep. Sleep deprivation made everything worse. I started having thoughts that were troubling, like my son being better off with someone else. But when I realized these thoughts weren’t normal, I reached out to my support system—my husband, my mom, and others—to talk about it. Their feedback was invaluable and helped me understand I wasn’t alone.
I also went to the women’s clinic for a mental health screening. The staff were supportive and didn’t judge me for how I was feeling. They assured me that postpartum depression and anxiety were common, and they helped me find the right medication. Within a week of starting the medication, I felt like a different person—more like myself.
Physically, recovery was tough due to a pelvic floor injury, which made it difficult to get back into activity. I felt discouraged watching others recover faster, but physical therapy helped a lot.
The whole experience taught me a lot about managing mental health, and I now feel more prepared to handle challenges. My son is doing great—he’s healthy, very intelligent, and right on track developmentally.
If I could go back and give advice to new moms, I would say don’t hesitate to reach out for help if you think you're struggling with postpartum depression or anxiety. Be honest in your screenings, and don’t feel guilty about taking medication if it’s what you need. For me, it was a game-changer, allowing me to truly enjoy motherhood.
Most new moms experience "baby blues" after childbirth, which include mood swings, crying, anxiety, and sleeping problems. Baby blues start in the first 2 to 3 days after delivery and can last up to two weeks. But some women (about 15% in Utah) experience a more severe, long-lasting condition known as postpartum depression (also called perinatal depression because it can start during pregnancy and continue after childbirth). Moms and their loved ones should talk about any concerns with healthcare providers. Almost all postpartum depression can be resolved, especially with treatment. Visit swuhealth.gov/maternal for more information.





By Shallen Sterner, SWUPHD Environmental Health Scientist
On a trip to the Oregon Coast last year, I snapped a picture of a sign posted at a food establishment I visited, which said: WE HATE to inform you, but unless YOUR DOG is a service animal, it is not allowed within this establishment. Now that we have your attention…we really love all animals. Unfortunately, Oregon law prohibits all animals except service animals in grocery stores, restaurants, and other food establishments.
As a health inspector, I’m always looking at how other health districts are handling sensitive issues, and I thought this was a humorous way to let the public know about the requirements of the FDA Food Code, which does not allow any animal in a food establishment - unless it is a service animal.
The FDA Food Code aligns with the ADA (Americans With Disabilities Act) in how it defines a Service Animal:
• A service animal is typically a dog that has been individually trained to perform tasks directly related to a person's disability (tasks include guiding or alerting individuals with visual or hearing impairments, detecting medical conditions, or assisting during psychiatric episodes).
• Emotional support, comfort, or therapy animals are NOT considered as service animals, even with a doctor’s note.
• A service animal is not considered to be a pet.
Service animals are allowed in restaurants wherever the public is normally allowed, including dining rooms, outdoor seating areas, and waiting areas. They are not permitted in food preparation or storage areas.
There are additional guidelines all food service establishments should know:
• Staff may only ask two specific questions to determine if a dog qualifies as a service animal: 1: "Is the dog required because of a disability?" and 2. "What work or task(s) is the dog trained to perform?"
• Staff cannot request documentation or ask for details about the customer's disability.
• The customer must keep their dog under control with a harness or

tether, unless those would impede its ability to perform tasks. The animal should not be disruptive, aggressive, or exhibit unsafe behavior (like barking excessively or jumping on people), otherwise the restaurant has the right to ask that the animal be removed.
• Service animals must not pose a hygiene or food safety risk. If the dog has an accident or causes a mess, it must be promptly cleaned in compliance with sanitation standards.
• Staff members are not required to provide care, food, or water for the service animal.
• Restaurants may not refuse entry, segregate, or charge additional fees to individuals with service animals, as long as the animal complies with behavior standards and hygiene guidelines.
Restaurant owners should train their staff on ADA and FDA rules and plan how to handle animal-related cleanups, conflict de-escalation, and customer complaints. Signage should be posted specifying that service animals are welcome but pets and non-service animals are not permitted (find a printable sign at swuhealth.gov/food and click the “No Pets Allowed” link or request a sticker by calling 435-9862584).
Utah restaurants may (but are not required to) allow non-service dogs in outdoor patio areas as long as they meet certain standards. These include separate entrances, proper signage, proper restraints, and cleanliness. Search online for Utah Rule R392-100 for more details.
Restaurants must strike a balance between accommodating service animals and maintaining high standards of food safety and customer satisfaction. By understanding these regulations, we can help restaurants maintain a safe and welcoming environment for everyone.



By Jeremy Roberts, SWUPHD Environmental Health Director
There is a lot of work that goes on behind the scenes in our communities to help protect our health. For example, water operators work to provide safe, clean water through our taps for drinking and washing. Wastewater operators handle the “re-cleaning” of that water before it goes back into the environment. Homes and businesses not connected to a sewer system are able to safely treat wastewater using septic systems on their property.


Protection of our water, food, and air are key principles of environmental health, which is one component of public health. The Southwest Utah Public Health Department safeguards our community by inspecting and permitting septic systems, public pools, tanning facilities, schools, food establishments, and body art studios.
Besides our established programs, we often get calls and inquiries about environmental issues that are outside our authority or responsibility. The following are some of the most common examples of these questions and possible agencies that might be able to help.
Housing & private property consultations and complaints
While renters and landlords should ideally work together to resolve problems, a renter sometimes feels the landlord is not correcting problems that may affect health and safety.
Health departments are typically unable to become involved in private property issues, but both the renter and landlord have rights and responsibilities that can be found in the Utah Fit Premises Act. Some cities and counties also have ordinances in regards to housing and may have code enforcement officers that can look into complaints.
What about household mold growth and concerns that it might affect the health of the occupants? The Centers for Disease Control and Prevention (CDC) website is a good source for finding out how to prevent and clean mold in your home (cdc.gov/ mold).

We are sometimes asked about possible methamphetamine contamination inside a dwelling where production or use is suspected. For testing and cleanup, contact a Certified Decontamination Specialist Contractor. A list of contractors is available through the Utah Department of Environmental Quality (deq.utah.gov, search 'CERCLA').
Complaints about solid or animal waste nuisances on neighboring properties should be directed to city or county waste and code enforcement officers.
Environment consultations & complaints
Concerns about drinking water can often be addressed by contacting the Public Water System that provides your water. If a complaint is not being resolved at that level, the Drinking Water Division of the Utah Department of Environmental Quality (DEQ) can be contacted (deq.utah.gov/division-drinking-water).
Harmful Algal Blooms (HABs) have been discovered in some lakes and rivers that we enjoy using for recreation. The DEQ’s Water Quality Division receives calls and monitors some of the bodies of water in our area for HABs. Recreational water conditions can be checked at deq.utah.gov/water-quality/recreational.
For immediate threats to life or property, call 911. For environmental concerns like hazardous waste spills or smoking vehicles, report incidents at deq.utah.gov (click 'Report an Incident').
By Jamie Anderson, SWUPHD Health Educator


One of the simplest yet most effective ways to combat heart disease is by monitoring our blood pressure. High blood pressure, also known as hypertension, is a leading cause of death and is often called the "silent killer" because it usually has no symptoms. If left unchecked, it can lead to serious health issues, including heart disease, stroke, and kidney problems.

For adults over 50, taking the time to regularly check your blood pressure is a small but impactful step in protecting your heart. By following the right techniques and using the proper equipment, you can manage your health more effectively and catch potential issues before they become serious problems. Your heart is your lifeline—keeping track of its health is one of the best ways to ensure it stays strong for years to come.
“Measuring your blood pressure at home provides a clearer picture of your health than relying solely on occasional readings at the doctor’s office,” - Dr. Stephen K. Williams, Cardiologist
Getting an accurate reading is key to understanding your heart health. Here are some tips for the best possible results to avoid “white coat syndrome” (elevated blood pressure in the clinicians office, but normal blood pressure at home).
Take your blood pressure in a quiet place where you can relax for a few minutes. Sit comfortably with your back supported and feet flat on the floor. Rest your arm on a table or flat

surface so your elbow is at the same level as your heart.
For at least 30 minutes before measuring, avoid caffeine, nicotine, or vigorous activity, as these can temporarily raise your blood pressure.
Home blood pressure monitors are available for purchase at department stores or online. Look for one that is approved by the FDA or American Heart Association. You can also check out a monitor kit for free at many local libraries in Southwest Utah. Use a blood pressure cuff that fits your arm correctly. An ill-fitting cuff can lead to inaccurate readings.
Follow the instructions on your blood pressure monitor. Keep still and quiet while the reading is taken.
Start a blood pressure log by writing down your systolic (top number) and diastolic (bottom number) readings, along with the date and time. Take multiple readings- If your first reading is very high or low, wait a few minutes and take another measurement to ensure accuracy. Do this twice a day for a week to get an accurate average reading.
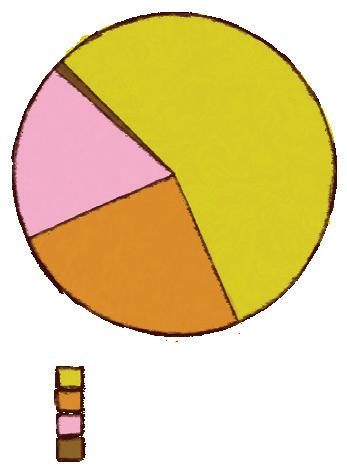
In prior issues of HEALTH Magazine, we’ve examined the root causes of disease, both locally and nationwide. It’s helpful to know what drives unhealthy conditions in order to improve health and wellness.
This article introduces the leading causes of death in our communities, and upcoming issues will include articles helping us to understand what is contributing to these deaths and ways that we can reduce the risk of the conditions behind them. Some of these causes of death are linked with chronic illnesses, while others, such as accidents and suicides, are sudden but still preventable.

By David Blodgett, MD, MPH

We’ll also compare our communities with the rest of Utah and the nation to help us understand risks that are unique to this area. We often find that we are doing well with preventable diseases that are prevalent elsewhere but much less common here. However, there are some diseases that are

more common here than they should be, and any cause of death should give us pause to consider how we can do better.
As part of our annual report (see page 28), we identify the top 13 causes of death in our area. If you were to look at a similar ranking from the year 1900, you would notice that individual infectious diseases would account for about 75% of the leading causes of death. Pneumonia, tuberculosis, and diarrhea were the top three, accounting for about one-third of deaths annually. Diphtheria, pertussis, and measles were very common causes of mortality, particularly in the young. Life expectancy at the time was averaged at 45 years old, primarily because so many children died from childhood illness.
Today, the top causes of death are largely related to chronic diseases. Heart disease, cancer, stroke, and chronic respiratory illness account for a large portion of those. Fortunately, deaths from some of
these conditions have decreased steadily over the past several decades. Fatalities from cardiovascular disease, for example, have declined by about thirty percent. Still, two-thirds of men and half of all women will develop heart disease in their lifetime. In most of the country, heart disease is the leading cause of death. In our area, we have lower risks of both heart disease and cancer than the rest of the nation, but cancer has overtaken heart disease as the number one cause of death overall.
Liver diseases and conditions related to alcohol consumption are much more common in the rest of the country, but they barely make it onto our list. Accidental deaths and suicides occur at higher rates in our area compared to the national average.
The official top causes of death in Southwest Utah (Washington, Iron, Kane, Beaver, and Garfield counties), in descending order, are:
Malignant Neoplasms (Cancer): Cancer includes many diseases that affect nearly every part of the body. We have made dramatic improvements against some cancers while others remain difficult to treat.
Cardiovascular Disease (Heart Disease): This includes a range of conditions from hypertension (high blood pressure) to myocardial infarction (heart attacks). While deaths from these conditions have decreased recently, rates of heart disease remain high.
Alzheimer’s Disease: Southwest Utah has a higher proportion of older adults than the rest of the state. Mild winter weather attracts many seniors to make their home here, which means we will see more age-related health conditions. Alzheimer’s and other forms of dementia are higher on our list than other parts of the state, and, unfortunately, overall rates of Alzheimer’s continue to increase nationwide.
Unintentional injuries (accidents): Deaths from unintentional injury are the leading cause of death in younger age groups. Whether it is a motor vehicle accident, fall, or work-related injury, there is much that can be done to help prevent these deaths.


Cerebrovascular Diseases (such as strokes or brain aneurysms): This is another area where higher rates due to increasing age are expected.
Chronic Lower Respiratory Diseases: This class of disease includes Chronic Obstructive Pulmonary Disease (COPD), where smoking is a primary culprit.
Diabetes Mellitus: Rates of diabetes continue to increase and is a cause for concern, which is why we address type 2 diabetes and prediabetes frequently in HEALTH Magazine (see page 30). Thankfully, it is largely preventable.
Intentional Self Harm (Suicide): It is unfortunate that this category appears on this list. Rates of suicide remain higher in Utah and our area than the US average.
Septicemia: These are infections that make it into the bloodstream, making them difficult to treat. For most of the country this is not among the top causes of death.
Kidney Diseases (Nephritis, Nephrosis, Nephrotic syndrome): Kidney diseases can have many causes and are more common than many realize. It is the tenth most common cause of death in our area.
Influenza and Pneumonia: Influenza (flu) lost its title as the deadliest infectious disease killer to COVID-19 for a year or two, but it re-took the title in 2023. Most vulnerable are the elderly and the very young.
Chronic Liver Disease and Cirrhosis: Alcohol related illnesses such as cirrhosis are much more common in the rest of the country, often representing the fourth most common cause of death. Gratefully, it is much less common here.
COVID-19: COVID will continue to circulate as part of the upper-respiratory tract infections we see during cold and flu season.
As we explore each of these leading causes of death in future articles, we hope to enlighten and educate you on what actions can be taken to reduce your risks and live a longer, healthier life.

By Stephanie Ward, SWUPHD Environmental Health Educator
Breathing in fresh, clean air—free from smoke or vapor—is one of the best things you can do for your health. Quitting smoking or vaping can feel overwhelming, especially if you've been using tobacco products for years, but it's never too late to quit, no matter how long you've had the habit.
Cigarette smoking remains the leading cause of preventable disease and death in the United States. Over 16 million
Americans live with at least one illness caused by smoking. The financial cost is staggering, with smoking-related illnesses estimated to cost $170 billion in medical expenses each year.
Utah has one of the lowest smoking rates in the country, but tobacco and vaping still pose significant health risks. These affect not only those who smoke, but also those around them. Smokers face serious health risks as they age, including an increased likelihood of stroke, lung cancer, and coronary heart disease. Smoking also con-


tributes to nasal irritation and reproductive issues in women, such as low birth weight during pregnancy.
The longer someone smokes, the greater the risks become. The American Cancer Society found that smoking is responsible for an estimated 75% of cancer deaths among individuals who began smoking before age 10 and 59% among those who started at age 21, but also found that "Smokers who quit before age 40 can avoid 90% of the excess risk of cancer death associated with continued smoking." Even for older smokers, quitting can still substantially reduce the risk of cancer death.
Secondhand smoke is a danger to those who spend time or live around smokers. The risks for children are especially concerning, with exposure linked to serious conditions such as Sudden Infant Death Syndrome (SIDS), middle ear disease, respiratory symptoms, and impaired lung function. These health hazards highlight the need to protect non-smokers, especially vulnerable populations, from the harmful effects of tobacco smoke.
Commercial tobacco smoke contains hundreds of harmful chemicals that are toxic or cancer-causing. Some of these include benzene (found in gasoline), butane (used in lighter fluid), ammonia (used in household cleaners), toluene (used in paint thinners), cadmium (used in making batteries), and hydrogen cyanide (used in chemical weapons).
Quitting is more than willpower—it’s about planning and support:
1. Set a Quit Date
Pick a specific day within the next two weeks. Commit to it and mark it on your calendar.
2. Identify Triggers
Notice what makes you reach for a cigarette or vape. Is it stress, certain places, or routines? Plan ways to avoid or manage these triggers.
3. Healthier Alternatives
Instead of smoking or vaping, try sug-
ar-free gum, water, deep breathing, exercise, or other activities to cope with cravings.
4. Use Quit Aids
Nicotine replacement therapy (gum, patches, lozenges) and medications (Chantix, Zyban) help reduce cravings. Replacement aids are available over the counter, while medications are prescribed by a healthcare provider.
5. Lean on Support
Include your family, friends, or a support group. There are free smartphone and virtual options ready to help you as well:
• 1-800-QUIT-NOW (Utah’s tobacco quit line)
• waytoquit.org (connect with resources like free coaching, nicotine replacement aids, and medications)
• ut.mylifemyquit.org (resources for teens)
• Text "DITCHVAPE" to 88709 (text support for youth and young adults)
6. Prepare for Withdrawal
Expect irritability, cravings, and difficulty concentrating. These symptoms are temporary—stay busy and hydrated to make it through.
7. Stay Committed
You may not succeed on the first try. If you slip up, don’t give up—keep refining your quit plan and try again.
After 20 minutes of not smoking, your heart rate and blood pressure drop. Your carbon monoxide levels normalize after just 12 hours without smoking. In a few weeks, your circulation and lung function significantly improves and after several months your risk of heart disease begins to drop. Most people report less anxiety, depression, and stress after giving up smoking and vaping.
Once you are smoke-free for a few years, your risk of having a stroke, lung disease, and several types of cancer is reduced, making it possible to recover your health and increase your life span. Ready to give it a try? It may not be easy, but it will be worth it!
By RuthAnne Watt – SWUPHD Administrative Liaison & Anna Fajardo, RN – Travel Nurse
Traveling to other countries can be an exciting endeavor. Most travelers enjoy their time abroad without any issues, but there are places in the world where sanitary and environmental conditions are quite different from what you may be used to. Whether it’s water and food safety or disease risk, it’s good to be informed and prepared before you start your journey. Setting up a consultation with a travel nurse at the Southwest Utah Public Health Department is a great way to help you navigate the unknowns of any country you may be visiting. We recommend that you schedule the appointment for 4 - 6 weeks prior to your travel date.
What can I expect at my travel consultation appointment?
You will meet with one of our nurses who are trained in travel medicine. They will review your medical history, discuss food and water safety, personal safety, and recommend vaccines and medications. Plan enough time (about an hour) for your visit, which may take longer if more people are attending.

I’m not 18 yet… can I attend my consultation appointment alone?
We are unable to provide services to individuals under 18 without the presence of a parent or legal guardian (proof of guardianship required) with current and valid photo ID. They will need to sign the required paperwork.
What do I need to bring to my appointment?
Come prepared to avoid rescheduling for a later date by bringing the following: current insurance card that covers vaccines (if you have one), immunization records, itinerary (including layovers), list of medications you are currently taking, and a valid photo ID. To optimize your time with the travel nurse, we suggest submitting your completed and signed travel form (download and print from swuhealth.gov/travel, “Intake Form”), insurance information, immunization records, and travel itinerary to our office at least three days prior to your scheduled appointment.
What immunizations and prescriptions do you offer?
Written prescriptions: malaria, traveler’s diarrhea, motion sickness, and other travel-related illnesses.
Immunizations: Tetanus, Diphtheria & Pertussis (TDAP) or Tetanus & Diphtheria (TD), Measles, Mumps & Rubella (MMR), Hepatitis A, Hepatitis B, Influenza, Meningococcal Meningitis, Pneumococcal, and Polio.
Travel Vaccines: Chikungunya, Japanese Encephalitis, Rabies, Cholera, Typhoid, and Yellow Fever (most of these must be special ordered). Will the travel vaccines be covered by insurance?
How can I schedule my travel consultation appointment?
Call the office closest to you in Southwest Utah:
Washington County: 620 S 400 E, St. George 435-986-2557
Iron County: 260 E DL Sargent Dr, Cedar City 435-586-2437
Kane County: 445 North Main, Kanab 435-296-5477
I am traveling in a large group or have a large family… is there a discount?
Travel consultation appointments are currently $70 per individual. Groups of 4 cost $260 with $25 for each additional individual up to a total of 8 people. If there are more than 8 people in your group multiple appointments will need to be scheduled.
Visit our website (swuhealth.gov/ immunizations) to get the most up to date information about the insurances we accept. Most insurances DO NOT cover the cost of travel vaccines. It is always good to check with your insurance company to see if they will reimburse the costs.
I just need vaccines, why do I need to have a travel consultation?
Our travel clinics are overseen by medical doctors at the University of Utah, who specialize in travel medicine and are infectious disease experts. A travel consultation must be scheduled to receive travel vaccines and prescriptions. If you are traveling to a developed country, you may not need a travel visit and can receive vaccines through our regular immunization clinic.
Are you or a son or daughter preparing to serve a mission for The Church of Jesus Christ of Latter-Day Saints?
It’s best to get your consultation at least 2-4 months prior to leaving for the Missionary Training Center (MTC) or home MTC, early enough to make sure you have all the immunizations and prescriptions needed for your assigned country. Some vaccinations require a series of shots separated by a period of time before completion.
If you’re up-to-date on your childhood immunizations, you’ll have those needed to serve out-of-country, which include Tetanus, Diphtheria & Pertussis (TDAP) or Tetanus & Diphtheria (TD), Measles, Mumps & Rubella (MMR), Hepatitis A, Hepatitis B, and Polio. Some boosters may still be required.
Country-specific vaccines may include those for Rabies, Japanese Encephalitis, Chikunguyna, Cholera, Yellow Fever, and Typhoid. Also recommended are vaccinations for Influenza, Meningitis, Pneumonia, and Chicken Pox. If you don’t have all your childhood immunizations, make an appointment as soon as possible, especially if you are willing to serve outside the United States. It can take six months to a year to get you caught up on the required immunizations.

The Southwest Utah Public Health Department (SWUPHD) serves the approximately 295,000 residents of Washington, Iron, Kane, Beaver, and Garfield counties.
HAS 4 DIVISIONS: Clinical Services, Community Health, Emergency Preparedness & Environmental Health
• Immunizations administered: 11,979
• International travel consultations: 1,044
• TB (tuberculosis) tests: 1,070
• Prediabetes screenings: 227
• Total death certificates issued: 2,834
• Total birth certificates issued: 6,394
• Other certificates issued (marriage, etc.): 16,911
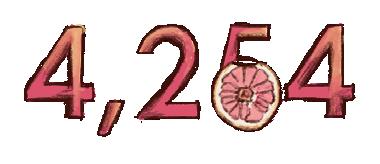
• Clients enrolled in WIC: 4,254
• Breastfeeding coaching contacts: 2,077
• Community events: 83
• Community coalitions: 21
• Mobile dental clinic patient visits: 155
• Certified car seat installation checks: 268
• Vaping and tobacco education reach: 356
• Quit-line referrals: 280
• Children served by TOP Star (obesity prevention): 1,108
• Safe Route Youth Education reach: 10,512
• MRC (Medical Reserve Corps) registered volunteers: 210 (1,302 hours volunteered, est. value $44k)
• Sponsored emergency preparedness trainings & events: 229 (4,985 participants)
• Full-Scale Strategic National Stockpile / Medical Countermeasure Exercises (Flu “Shootouts”): 7 Locations (968 Flu Shots Administered)
• Health Care Preparedness Coalition Members: 120
• Local and state partnerships: 18
• Reportable disease cases investigated (57 different diseases): 7,338
• Total food service inspections and consultations: 4,855
• Food Handler Cards issued: 10,213
• Water samples analyzed (for swimming pools and drinking water facilities): 8,966
• Public pools & spas in district: 873
• Restaurants/food establishments in district: 1,385
• Total septic inspections and consultations: 6,585
| SPRING 2025

Commissioner Victor Iverson
» Washington County

Kenneth Snow
» Washington County

Commissioner Paul Cozzens
» Iron County
Kent Peterson
» Iron County


Commissioner Celeste Meyeres
» Kane County

Jerica Bauer
» Kane County

Commissioner Wade
Hollingshead
» Beaver County
Scott
Symond
» Beaver County


Commissioner Jerry Taylor
» Garfield County

Nick Reynolds
» Garfield County

Disease Surveillance & Control
Epidemiology
Tuberculosis Program
Access & Functional Needs
Bioterrorism Prep/Planning
Community Training & Outreach
Free Emergency Resources
Hospital Surge Planning
Mass Flu Vaccination Events
Medical Reserve Corps
Pandemic Prep/Planning
Preparedness
Buddy
Strategic National Stockpile (SNS)
Air & Water Quality
Body Art Regulation
Child Care Inspections
Food Handler Permits
Hotel Sanitation Inspections
Pool Inspections
Restaurant Inspections
School Inspections
Septic System Inspections
Tanning Bed Sanitation Inspection/Enforcement
Temporary Mass Gathering Permits
Utah Indoor Clean Air Act Inspection/Enforcement
Water Lab
Alcohol Education (retailers)
Bicycle Safety
Car Seat Classes
Certified Car Seat Inspection Points
Community Training and Outreach
Diabetes Education
Healthy Dixie Liaison
Injury Prevention Safety Resources
Physical Activity & Nutrition Resources
Resources to Quit Tobacco
Tobacco Compliance Checks
Tobacco Education (retailers)
Tobacco-Free Housing Data
Baby Your Baby
Breastfeeding Consultation
Case Management
Child Care Resources/Referrals
Health Screenings
Immunizations
International Travel Clinic
Maternal Child Health
Mobile Clinic (rural counties)
Prenatal Resource Referrals
School Exemptions Education & Tracking
School Health/Nursing
WIC
Birth Certificates
Death Certificates
Disinterment Certificates
Divorce Certificates
Marriage Certificates
BY THE NUMBERS FOR 2024
Totals include Washington, Iron, Kane, Beaver, & Garfield Counties

REVENUE

IMMUNIZATIONS ADMINISTERED


DEATH CERTIFICATES


RESTAURANTS
EATING ESTABLISHMENTS

PUBLIC POOLS & SPAS

BIRTH CERTIFICATES

MEDICAL RESERVE CORPS VOLUNTEERS

CLIENTS ENROLLED IN WIC
Every year, the SWUPHD selects members of the community who have demonstrated exceptional support and service to the field of public health.
Utah State Senator, District 28
For his outstanding leadership and dedication to public health. His commitment to impactful legislation has made the communities he serves healthier and safer.

ST. GEORGE POLICE DEPARTMENT
#IamSGPD
For making a lasting impact through the Summer S.P.E.A.R. Academy, helping 6th8th graders build communication, resilien cy, and safety skills. We’re proud to collabo rate with them to promote My Life, My Quit for teens and WaytoQuit for families.

SEAN AMODT
Administrator for the Southwest Mosquito Abatement District

Sean and his team do a lot of work behind the scenes to protect us from diseases like West Nile virus that spread through certain species of mosquitoes.

BIRTHS BY COUNTY
Beaver Garfield Iron Kane
Washington

This graph shows provisional counts for the leading causes of death in the Southwest Utah Public Health Department (SWUPHD) district for 2024. Tracking and understanding mortality trends helps guide public health interventions and healthcare planning in our region:
Malignant neoplasm (Cancer)
Heart disease
Alzheimer's
Unintentional injuries
Cerebrovascular (Stroke)
Chronic lower respiratory disease
Diabetes mellitus
Intentional self-harm (Suicide)
Septicemia
Nephritis
Influenza & Pneumonia
Chronic liver disease & cirrhosis
COVID-19

This table summarizes the most common confirmed and probable communicable (can be passed from one person to another) disease cases in the SWUPHD district for the past two years (2023 & 2024):



Coronavirus,
Influenza
Respiratory Syncytial Virus (RSV)
Chlamudia trachomatis infection
Norovirus
Hepatitis C virus infection, chronic
Coccidioidomycosis
Influenza-associated hospitalization
Campylobacteriosis
Salmonellosis
Gonorrhea
Pertussis (Wooping Cough)
Lead poisoning
Giardiasis
Shiga toxin-producing Escherichia
Streptococcal disease, invasive
Syphilis, unknown duration or late
Shigellosis
Cryptosporidiosis
HIV



FIND US ON SOCIAL MEDIA
Search for swuhealth on Facebook, Instagram, X, and YouTube to find alerts, posts, and videos about all thing public health!





TUNE IN: WE'RE ON THE RADIO!
890 KDXU AM: Every Thursday @ 7:55am: Health Update
590 KSUB AM: Every Wednesday @ 6:30am: Ounce of Prevention
100.3 FM (St. George Radio): Every Thursday @ 4pm: Health Update

READ PAST ISSUES HERE
Find all past issues of HEALTH magazine here. Enjoy!
890 KDXU AM: Every first Wednesday@ 9am: The Andy Griffin Show hosts Dr. David Blodgett
Have you been screened for prediabetes? 1 out of 3 adults have it, but 80% of them don’t realize it.
We’re offering FREE A1C prediabetes tests during the month of May 2025! Just go online to swuhealth.gov/diabetes and take the screening. If you score a 5 or above (and you’re not already diagnosed with diabetes or prediabetes), you’re eligible! Then, call our nearest office (phone numbers are on the screening form) to make an appointment for your free A1C test. You’ll get results a few minutes after the finger-prick blood test. Resources will be provided if you test positive for prediabetes or diabetes (type 2).

“Wellness

C O L O R M E !
encompasses a healthy body, a sound mind, and a tranquil spirit. Enjoy the journey as you strive for wellness.”
“THE FIRST WEALTH IS HEALTH” -Ralph Waldo Emerson









