The pulse of community health, Leasowes, Rowley Regis, City Hospital, Sandwell General and the Midland Metropolitan University Hospital Issue 158 October 2022 Sandwell and West Birmingham NHS Trust Newly opened discharge lounges Page 12 Breast cancer awareness month - Cathy's story Page 18 Vaccination calendar from now until the New Year Pages 4-5 Harvest View keys handed to officials Page 22 Star Awards 2022: Celebrating and showcasing outstanding achievements Pages 14-15 Clockwise from top: District Nursing Blue Team: Quality of Care Award winners, District Nursing Matron Andrew Churm: Employee of the Year, Vaccination Team: Clinical Team of the Year, Portering Team: Non-clinical Team of the Year S AWArRDS
This month, we celebrate our stars by recognising the achievements of colleagues at the annual Star Awards. We've included a summary of the night, as well as all winning colleagues and teams, on pages 14-15. With the weather getting colder, we're all aware of a potential rise in viral infection rates. If you're yet to get your COVID-19 and flu vaccinations, you can see a full calendar of staff clinics on page 5, as well as further information on the programme on page 4. Once you're done with the magazine, cut out the timetable and add it to a noticeboard.
Contact us
Communications Team
Ext 5303
swbh.comms@nhs.net
Communications Department Ground Floor, Trinity House Sandwell Hospital
Published by Communications Team
Sandwell and West Birmingham Hospitals NHS Trust
Designed by Medical Illustration, Graphics Team Sandwell and West Birmingham Hospitals NHS Trust
Submit an idea
If you’d like to submit an idea for an article, contact the communications team
Ext 5303
swbh.comms@nhs.net
Stay updated
We send out a Communications Bulletin via email every day and you can now read Heartbeat articles throughout the month on Connect. Don't forget you can follow us on:
FROM THE CHAIR
Sir David talks about…Celebrating our stars
It was fantastic to join in with the celebrations of the Trust’s Star Awards earlier this month.

During the night, Villa Park was packed full of our very best shortlisted teams and individuals, all of whom have been nominated by a colleague or patient. What a privilege to be among such hard working and committed people, who have made a significant contribution to either improve patient care, provide innovative services or support one another during times of challenge.
We heard loud and clear on the night that everyone who was in the room was a winner, whether or not they managed to come away with a trophy. The sheer number of nominations this year (over 400) just goes to show how appreciated staff at SWB are from every part of our Trust.
As well as the opportunity to recognise all that is best about our Trust, people enjoyed simply getting together to have a good time. There are too few occasions in the NHS to do this and, the buzz (and volume!) coming from every table was heart-warming. This was our first awards event in three years that hasn’t been hampered by COVID-19 restrictions so the party was in full force.
This would not have been possible without the generous support from our sponsors, all
of whom have worked closely with the Trust over the past year and were only too happy to help fund our event.
We know that working in the NHS is often very tough and the challenges appear, at times, to be insurmountable. The way in which we recognise, reward and support each other through these times is what will help us to continue to do our best for our patients. I saw great camaraderie at the awards night, with everyone rooting for each other and being delighted to share in the combined success.
Many more of you, no doubt, deserve some additional recognition, so don’t just wait for next year’s Star Awards nominations to open. Right now you can show your appreciation by nominating someone for a Star of the Week award or a simple shoutout – find the details on our intranet site, Connect. Telling someone you appreciate them can and should be something we do day in, day out. It makes a real difference when we feel valued – helping us through difficult times, and reminding us why we chose to work in public service.
Sir David Nicholson KCB CBE, Chair
Welcome to the October edition of Heartbeat.
Enjoy
HELLO
SWB help shape the future of PPE
During October, our Trust played host to an NHS Supply Chain national event focussed on PPE.

The special event was hosted at our Sandwell Education Centre and invited clinical and nonclinical colleagues, both in the hospital and the community, to drop in and give their feedback. Manufacturers, suppliers, and technical decontamination and cleaning experts were all in attendance at the event which gave anyone an opportunity to provide opinions and help improve PPE quality going forward.
Paul Chivers, Head of PPE Innovation & Sustainability at NHS Supply Chain, was at the event at Sandwell and said: “We wanted to hear the good, bad and the ugly of staff experiences of wearing masks, visors and other PPE as this feedback would allow everyone to improve their products and services.”
“PPE has never been more prevalent part of the NHS and society as a whole since
the COVID-19 pandemic so it is vital that staff across the spectrum have the highest quality PPE especially if they have to wear it for long periods of time during work.
Clare Nash, Nurse and Head of Clinical Products Management was also in attendance at the national PPE event and believes it was a success.
She said: “Staff gave their honest views of wearing PPE, which ultimately will go to help shape the future designs for the better.”
She added: “If just some of the feedback can be taken on board by the suppliers, PPE will be more sustainable, comfortable, fit better, and protect our NHS staff, patients and the planet well into the future. I must say a huge thanks to all those staff at the Trust who gave up their time to discuss their experiences of wearing PPE and how it could be improved.”
Did you miss the event and still want to have your say on anything PPE? Please email any feedback you may have around PPE to england.pperis@nhs.net.
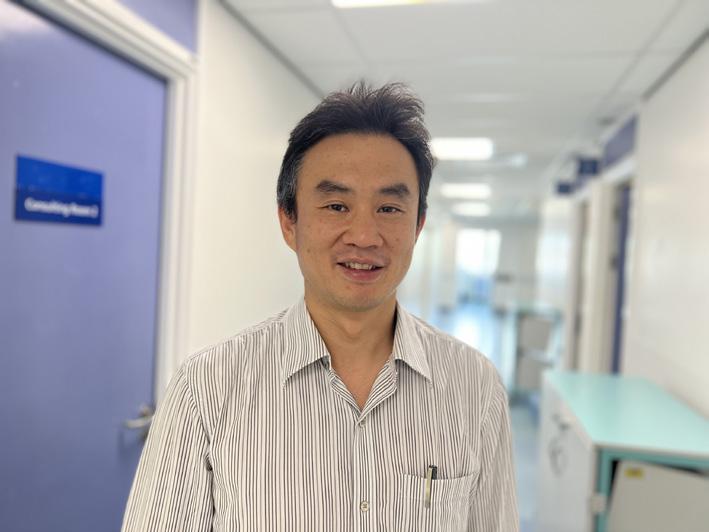
Celebrating our allied health professionals
Earlier this month we recognised Allied Health Professions (AHPs) Day! It's the annual opportunity for AHPs and support workers to come together and celebrate being part of the AHP family.

AHP Day also serves as a platform to showcase some of the amazing work carried out by Allied Health Professions within the Trust and further afield.
Allied Health Professions are a group of healthcare professionals from 14 different professions, making up the third largest healthcare workforce.
Here at the Trust we employ 10 of the 14 professions which include diagnostic radiographers, speech and language therapists, operating department practitioners, dietitians, physiotherapists, orthotists, orthoptists, paramedics, podiatrists and occupational therapists. We do not currently employ osteopaths, music therapists, drama therapists or art therapists.
James Severs, Chief Allied Health Professional said: “I’m so proud of our AHP family and the impact that they have on our everyday patient care. I’d like to say thank you to all our AHP colleagues and healthcare support workers for all they do.”
Some our AHP colleagues shared selfies to celebrate their profession





3 CORPORATE AND GENERAL NEWS
PPE event
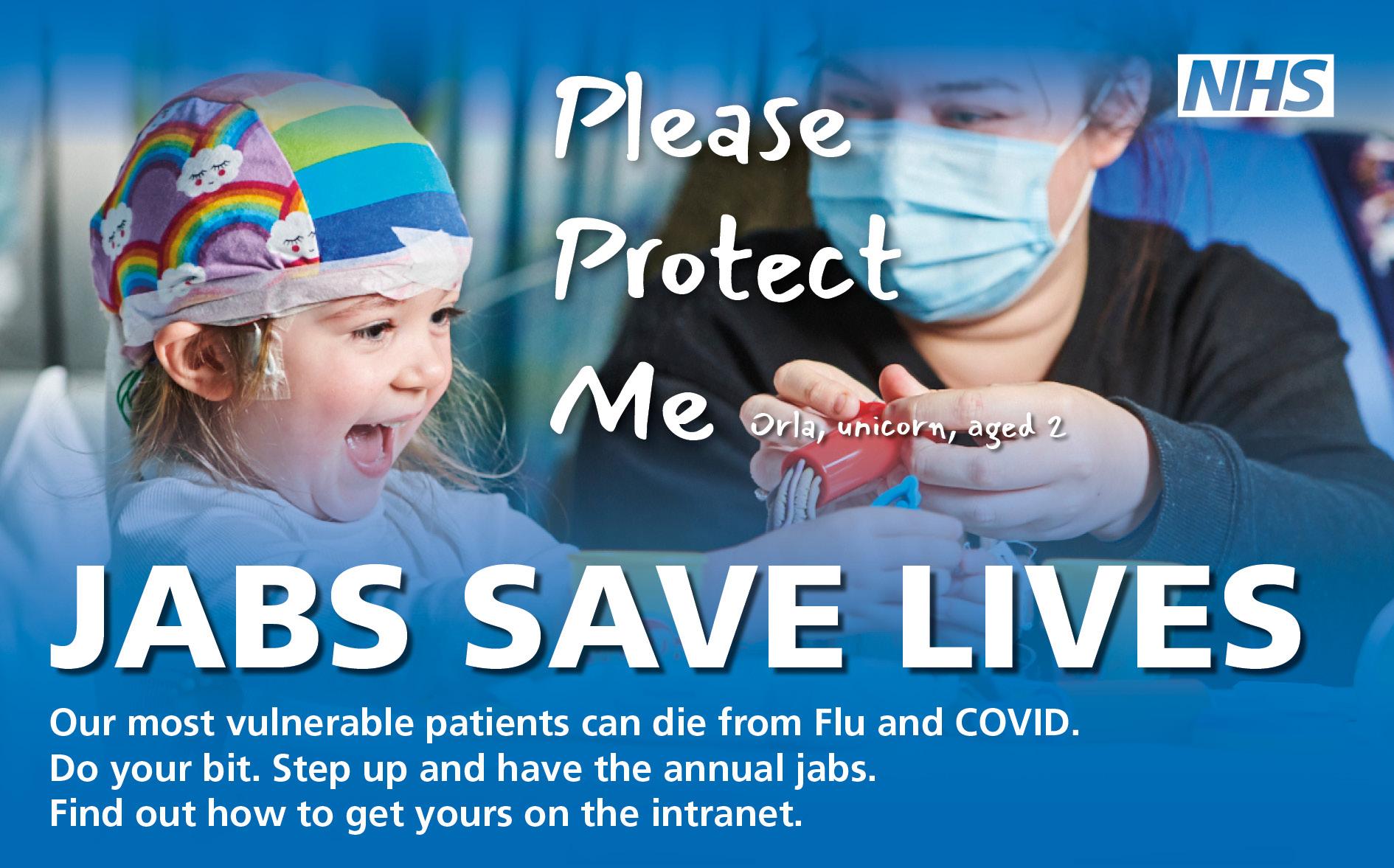
Boost your immunity this winter by getting your COVID and flu vaccinations
The occupational health and wellbeing team continue to offer vaccinations to colleagues across the Trust.
We’re now at the time of year when respiratory infection figures start to increase, with the possibility for a surge of COVID and seasonal flu. As in the previous year, all colleagues at our Trust will be able to protect themselves with a COVID-19 booster jab and an additional flu vaccination, ensuring they are fully protected.
Stocks of vaccines for colleagues arrived in late September, and clinics have been running every week since this point. Many colleagues have already received their vaccinations, but for those that are yet to do so, the Trust is providing ample opportunities to get these with ease.
We now have a stock of Pfizer Bivalent covid booster for staff. You must have
had two primary doses of either Pfizer, AstraZeneca or Moderna. Your last vaccine must have been more than 91 days ago and you must be 18 years or over to meet the criteria. Flu vaccine is cell-based quadrivalent influenza (QIVc).
Points to remember:
• You can have the flu and show no symptoms meaning you can be unknowingly spreading the virus to your family, friends and our patients.
• It’s important to have vaccinations as soon as possible, it can take up to 2 weeks for your body to build up good level of immunity.
• Our flu vaccines do not contain any porcine or egg content.
You will be able to have either or both of the vaccines, administered in two separate injections, on the same day.
If possible, please have your NHS number to hand upon attending, as this will help speed up the process.
Clinics are based at the following locations:
• Sandwell General Hospital: The Berridge room, Courtyard Gardens
• Birmingham City Hospital: first floor corridor towards link to Birmingham Treatment Centre
• Rowley Regis: Westwood Ward
For any departments that are struggling to leave their areas due to workload, the team are able to work with you to arrange a vaccinator to attend the department. To discuss this, managers should contact Cara Shelton on 07507 523924.
A schedule from 31 October until the new year is available overleaf: once you and your colleagues are finished with the magazine, please do cut the page out and pin the timetable to a noticeboard.
Monday Tuesday Wednesday Thursday Friday Saturday Sunday 31 October City 08:30-16:00 1 November City 08:30-16:00 2 November City 08:30-16:00 3 November City 08:30-20:00 4 November City 08:30-16:00 5 November No clinics 6 November No clinics 7 November Sandwell 08:30-16:00 8 November Sandwell 08:30-16:00 9 November Rowley 08:30-16:00 10 November Sandwell 08:30-20:00 11 November Sandwell 08:30-16:00 12 November Sandwell 08:30-16:00 13 November No clinics 14 November City 08:30-16:00 15 November City 08:30-16:00 16 November City 08:30-16:00 17 November City 08:30-20:00 18 November City 08:30-16:00 19 November No clinics 20 November No clinics 21 November Sandwell 08:30-16:00 22 November Sandwell 08:30-16:00 23 November Sandwell 08:30-16:00 24 November Sandwell 08:30-20:00 25 November Sandwell 08:30-16:00 26 November No clinics 27 November No clinics 28 November City 08:30-16:00 29 November City 08:30-16:00 30 November City 08:30-16:00 1 December City 08:30-20:00 2 December City 08:30-16:00 3 December No clinics 4 December No clinics 5 December Sandwell 08:30-16:00 6 December Sandwell 08:30-16:00 7 December Sandwell 08:30-16:00 8 December Sandwell 08:30-16:00 9 December Sandwell 08:30-16:00 10 December No clinics 11 December No clinics 12 December City 08:30-16:00 13 December City 08:30-16:00 14 December City 08:30-16:00 15 December City 08:30-16:00 16 December City 08:30-16:00 17 December City 08:30-16:00 18 December No clinics 19 December Sandwell 08:30-16:00 20 December Sandwell 08:30-16:00 21 December Sandwell 08:30-16:00 22 December Sandwell 08:30-16:00 23 December Sandwell 08:30-16:00 24 December No clinics 25 December No clinics 26 December No clinics 27 December No clinics 28 December City 08:30-16:00 29 December City 08:30-16:00 30 December City 08:30-16:00 31 December No clinics COVID-19 and flu vaccination clinics # If you have any questions, please contact Occupational Health on 0121 507 3306.
Segregate for safety - laundry service need your help
The Trust’s dedicated in-house laundry team are requesting colleague support to segregate linen properly to safeguard against cross infection risks and to limit the amount of linen being mislaid and mishandled.


Aner Marcelo, Head of Support Services, told Heartbeat: “In-house, we launder pyjamas, curtains, nightwear, scrubs, oven gloves, mops, tea cloths and lab coats, amongst other things.
“The operation requires a very particular set of skills which are easy to overlook. However, there is lot more to laundering than meets the eye.
“My day-to-day job involves handling chemicals, operating machines, good coordination, and impeccable timing to ensure that linens leave the laundry room clean, crisp, and on time.
“If not segregated properly there is a high possibility of cross infection. Furthermore, we get charged by an external contractor if the above items get mixed with theirs and as a result, the items end up in waste bins.”
Aner added: “It’s important for colleagues to be mindful on how to prevent cross contamination and reduce cost pressures.
“Linen can be made safe by washing it to remove any contaminating body fluids, but it is often not practical to wash domestic linen at high temperatures because of the heat lability of fabrics.
“And so, we encourage all colleagues, clinician and non-clinical alike to follow proper linen segregation.”
All PJs, curtains, nightwear, scrubs, oven gloves, mops, tea cloths, and lab coats need to be segregated and sent to internal laundry. PJs need
to be put in the green bags, whilst scrubs are to be put in the blue bins. All other items are to be sent to external providers.
Trust raises living wage in line with Living Wage Foundation
Our Trust is a long-standing member of the Living Wage Foundation where employers commit to paying their staff the real living wage. The real living wage is based on real living costs and is higher than national government minimum wages set for adults.
New real living wage rates were announced on Thursday 22 September: as part of our membership, we are required to introduce the new rate as soon as possible and by May 2023 at the latest. The new real living
wage rate applicable to all areas outside London is now £10.90 per hour – more than the national minimum of £9.50 per hour. Our Trust has agreed to introduce this new rate of £10.90 per hour for our lowest paid workers during the month of October so staff should expect to see this increase reflected in your October pay.
We are among a minority of NHS organisations who are committed to the real living wage that reflects cost of living increases and are proud to be able to
honour this commitment as soon as the new rates were announced.
For more information on the Living Wage Foundation and how the rate is calculated please visit livingwage.org.uk.
6 CORPORATE AND GENERAL NEWS
Stacey, Laundry Assistant in the laundry department
Staff Nurses collecting their uniforms from laundry. (Doreen, Aderonke, Stacey, Lisa and Aner)
Learning from our experiences to improve end of life care
Over the past year the palliative care team have been leading a Trustwide quality improvement project to enhance the care delivered to patients approaching the end of life. This is relevant to colleagues in all specialties and an opportunity to see excellence in care become the consistent norm for our patients, whoever they are and wherever they are looked after.
In this issue of Heartbeat, we feature the story of Dr Paul Turner, a local GP who tells us of his experiences with our teams when his father was in his last days of his life.
Paul said: “Dad was 87 and had been working as a doctor in Africa until a year before he died. His death was a real shock to all of us as he was doing press ups every day until two months before he was admitted to hospital. He was full of life and had just re-married, so he had a lot to live for.

“We first started to notice something was wrong when he suddenly started to fall over and also had trouble breathing. One night dad couldn’t breathe well and fell which led him being admitted to Sandwell Hospital.”
Paul said doctors found that his father (William) had metastatic spread from an undiagnosed cancerous tumour. This was complicated by large pleural effusions, for which chest drains were inserted and William was admitted onto a ward.
“At the time of dad’s admission, the team looking after him kept telling him that once the chest drains are done he could go home,” added Paul. “No one actually explained how serious the situation was and that there was little that could be done to change it. Instead, they kept giving him hope for a recovery and trying different treatments that were not making a difference. Dad, being a doctor, was also desperate to get well and wanted to try everything in order to get better.
“It was during the COVID restrictions and communication was difficult as we were not able to visit dad. In the meantime, numerous teams were visiting and assessing dad and going away without really telling him what was going on.
“It soon became clear that the team looking after him really did not know what to do – dad was dying and no one was acknowledging it.
“Things changed for the better when senior doctors realised dad was dying and made the decision to put him on the supportive care plan.
“Once dad was on the correct plan we were allowed to visit him and we could see a huge change in the way the team was treating him. They showed compassion and kindness to our entire family and did everything they could to ensure dad was able to be comfortable in his last days.
“From our point of view as a family whilst learning that dad was dying was extremely shocking, it helped take away the fear and angst that we had. As a doctor, when you avoid the conversation about death you take away the opportunity for people to say goodbye and prepare for what’s to come. As healthcare teams we must be brave enough to have these conversations with patients and their families as it’s part of our role.”
“While dad’s care was not always appropriate when he was first admitted to Sandwell, we were lucky that things changed for the better and we were allowed to say goodbye to him.”
Paul Turner concluded: “We miss dad dearly. He was an extraordinary man and had a chuckle that would send his grandchildren into streams of laughter. He loved people and was one of a kind. He was very special to me.”
Dr Turner’s top tips for caring for end of life patients
• Don’t be afraid to recognise dying
• Communicate clearly, compassionately and as early as possible.
• Be brave and kind
• Focus on the kind of care that can make the biggest difference to patients.
Please visit the palliative care Connect page for a whole range of resources that will equip you to play your part.
7 CORPORATE AND GENERAL NEWS
Dr Paul Turner with his father Dr William Turner (left)
Gotta have faith!
would be building upon what services and facilities we already have in place in our hospital settings and creating a sense of continuity whilst we develop our new area at Midland Met. Plus, there is a desire to explore the philosophy and purpose that underpins our spiritual faith centre, and we will fully engage with as many different faiths and leaders to gather feedback.
“We will continue to reach out to faith groups to seek their support and involvement. Members of our existing staff groups are welcome to attend. If anyone is part of any religious groups outside of work, please spread the word and encourage others to join us.”

Earlier this month, SWB welcomed community faith-based leaders to discuss plans for our spiritual faith centre at Midland Met.
It will be our purpose-built, multi-faith centre open to all staff, patients, visitors and our local communities.

The role of faith leaders is an important one. Their ability to guide, inspire and lead on changes that will impact those who use this new space is integral to our plans for Midland Met.
Often when in a hospital setting, those of both religious and non-religious backgrounds turn to our existing facilities and the support of our chaplaincy team. Having that support system and connection to faith and an awareness of cultural and spiritual needs brings comfort for those in our care and their families.
As we make plans for opening, we’re seeking the views of a broad cross-section of religious leaders and groups to ensure our space meets the needs of those that will use it. That is not an easy task as it will mean different things to different
people, and so, along with our communities, we have committed to working together to create a sacred space that promotes a sense of togetherness.
Jayne Salter-Scott, Head of Public and Community Engagement, told us: “Our initial faith meeting saw several faith-based community organisations and leaders attend and proved positive in helping us to begin to realise the potential of our new spiritual faith centre.
“Beginning this conversation was a constructive first step. It was also a valuable opportunity to listen and learn to our community faith leaders, after all, they know their communities best.
“We heard how several religions wash before prayer so the facilities we have need to be accessible to all, there was a consensus that the space should be versatile enough that anyone can worship there irrespective of which religion they observe. Plus, there was an engaging conversation around what language we use so that the space we create is welcoming.”
Jayne added: “There were also some good learnings from the session. One such example
Reverend Mary Causer, Lead Chaplain, led part of the discussions at the meeting. She told us: “The importance of faith and spirituality is something we closely examined at our initial meeting. There was a general agreement around the vital role religious groups and customs play in the healing process and the support and comfort having this service and our facilities bring to patients and families in their time of need.
“There were some lively conversations and one of the most valuable things I took away from the session was our shared goal of working together to create a truly unique space. I also enjoyed listening to the different perspectives and needs of those who will use the area, and it cemented my belief in the vital role our community faith leaders have in this project.
“While the hospital will provide the medical care patients need, we will provide the spiritual care and support to those who call on us. We have a diverse chaplaincy team, and we look forward to building on our existing ways of working to create a space we can all be proud of.”
The next meeting will be during Inter Faith week between 13-20 November. To find out more, email swbh.engagement@nhs.net and check out the daily bulletin for updates.
8 If you have heard any rumours about the Midland Met and you want to know if there is any truth to them, however far-fetched, intriguing or interesting, email the communications team at swbh.comms@nhs.net for an answer.
Sandwell and West Birmingham NHS Trust
Thank you to community faith-based leaders and groups joined us to discuss plans for our spiritual faith centre.
From now until when we move into Midland Met, we will be sharing updates with you about the many people involved in the project and the role they each play.
Getting us to Midland Met is a team effort. We all have a part to play in making it #morethanahospital!
My part in Midland Met
We caught up with Rev Mary Causer, Lead Chaplain to discuss all things Midland Met.

How long have you been at SWB and what is your current role?

I have worked for the Trust since June 2016 and my current role is lead chaplain.
What part does your role contribute to the Midland Met project?
I have spiritual oversight for the Trust, which means I have responsibility for the chapels and spiritual faith centre at Midland Met.
Faith is important for many people, not only in the Trust but for our patients, visitors and communities, so using the space well is really important.
How are you preparing for the opening of Midland Met in your team/department?
Some of the team have already been on the new site, which was so exciting; it helped us to see where we will be based and consider how we will use the space.
We are also working with other faith groups to help build relationships in the community that Midland Met is situated in.
In what ways will our new hospital help to shape your role or service for the better?


We will have a bigger brief – five hospitals to look after. My role will become more community focused. We hope more volunteers will come on board and help us to make the spiritual faith centre a success.
The biggest benefit that Midland Met will bring in your opinion is...
For us, the opportunity to work from a more meaningful perspective, exploring inter-faith/multi-faith perspectives with our communities.
Have you been on a site tour?
Yes, I have been on site. Seeing the sheer size of the building puts our task into perspective. We will have more people to care for and would like to integrate our spiritual faith centre firmly into the heart of the communities we serve.
9 NEWS
Sandwell and West Birmingham NHS Trust
Rev Mary Causer
EQUANS has the mission to connect, power & protect - empowering businesses and communities to not only fully embrace the energy transition, but also the digital & industrial transitions that are redesigning the way we move, work and live. Acting on our commitment to Net Zero by helping our clients to reduce the amount of carbon that is produced across the NHS Estate. equans.co.uk
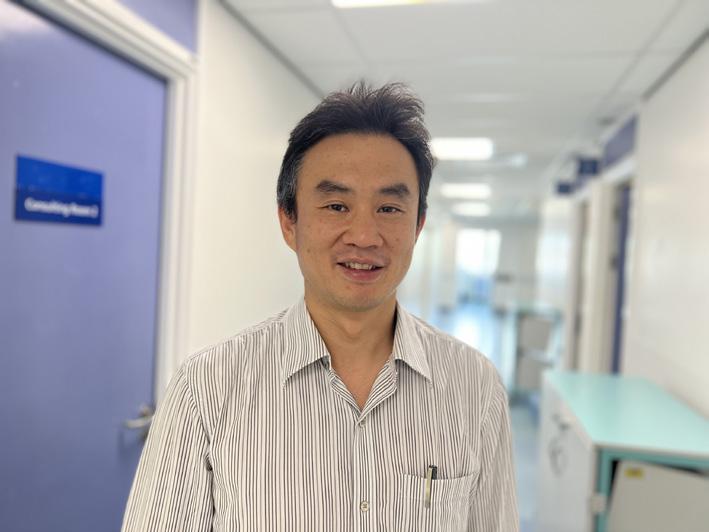
How to be a chief medical officer –007 need not apply
Choosing to step down as chief medical officer was a complex decision for Rheumatologist
Professor David Carruthers for he has devoted his career to the wellbeing of people, both his patients and the many hundreds of doctors who have been benefited from his teaching.

Shortlisted for in the prestigious ‘Excellence in Education’ category by Birmingham Awards 2022, David will hear next month if he has been awarded the top prize, as he has devoted his career to medicine and the teaching of medical students and junior doctors primarily in the field of rheumatology. As both clinician and academic he has taught over 1000 medical students and junior doctors and inspired a generation of medics to undertake life enhancing research, benefiting patients both across Birmingham and further afield through publication of an impressive list of research and academic articles.
Talking to Heartbeat he recalled his early career decision when he was faced with a choice of mathematics or medicine.
At 17 and a half years old it was by no means a foregone conclusion, for there is little he loves more than a challenge requiring strategy and analysis and the attraction of maths was a genuine pull. To this day he loves board games which require a strategic plan, with one of his favourites being Risk - a strategy board game of diplomacy, conflict, and conquest. Understanding that leads to an insight of the man and understanding of his choice of speciality. Rheumatology offers him the opportunity to plan treatment for patients long into the future as he oversees the care of patients with lifelong conditions.
He explained: “Even if I went back to that time, I would still make the same choice. I love my career; it gives me a buzz and real pleasure. I have done stuff I have really enjoyed.”
On taking on the post of chief medical officer in January 2018 he characteristically thought about what he could achieve for doctors across the organisation and how medical education and research could be served with his focus on them. He questioned himself on whether he could make a difference and on deciding he could he made the move.
“I recognised the value of research early
in my career and my academic training has allowed me to continue an active research role especially in the field of rheumatology. I have been involved in several research areas including systemic vasculitis, vascular disease, and inflammatory arthritis. I was awarded my PhD in 1999 (The role of intracellular Ca2+ in T-cell signalling in rheumatoid arthritis) and have maintained my acute interest in research to this day,” he added.
As a hands-on clinician David’s focus in teaching was more on how to learn and apply medicine, rather than the study of facts in textbooks. A natural born innovator he was keen to seek out new ways to train medical students, engaging them in technology with the development of virtual reality apps in identifying sepsis and conducting eye examinations.
More recently he steered the organisation through the early months of COVID as acting chief executive and recalls the laser focus that served the Trust well: “I did it because it was the right option for the organisation at that time. It was a relatively easy decision because it was not about running a busy acute Trust in normal times. We had clarity of thought and direction to doing the right thing. All focus was on the safety of our colleagues, our patients, and our communities. It was not on the myriad of other competing priorities that we have today. Now we are back into a very complex system, a chief executive needs a
political skill set.”
Possessed of an exciting back story with adventures James Bond would be proud of David recalled the occasion when he was stung by a scorpion in Malawi, Africa: “I fell off the back of a lorry while I was sleeping and woke up the next morning with an obvious bite on my hand. The locals identified it as a green scorpion sting. I remember it was incredibly painful, and the only pain relief I had was whisky – I hate the taste. I suffered for two weeks as it swelled badly then decided to cut the blister – when I did, I could see down to the bone. Consulting a local doctor, I discovered I had gangrene which had eaten through my tendons, leaving me with a permanent injury. This was on New Year’s Eve in 1991.”
His adventures culminated in a tobogganing accident on Boxing Day seven years ago. He recalled: “I came off my sledge and hurt my back so had an x-ray but was told there wasn’t anything seriously wrong. I came to work the next day despite the severe back pain and in clinic I saw a patient who was clearly unwell, and who subsequently had a heart attack. I wonder at which point fate intervened to ensure I was there and able to get immediate help for him. For I was taking my clinic without knowledge of the two broken bones in my back that would surely have cancelled my clinic that morning.”
10 CORPORATE AND GENERAL NEWS
Professor David Carruthers
We really appreciate how hard you work to ensure all the mums you see have an antenatal conversation about getting off to a good start with feeding and developing a close and loving relationship with their baby and for documenting it on Badgernet. Antenatal conversations improve the postnatal experience for parents and babies and help reduce readmissions and it is great to see them documented.
Shout out has been a regular feature in Heartbeat and it is fantastic to see colleagues regularly taking the time to give positive feedback to each other.

We regularly receive positive feedback from our patients too, and this month we wanted to share some of those heartwarming messages which have been sent via our website and social media platforms.
Thank you all for your support during my first year at Uni for my NAA course. Especially Liz for being my assessor, advising and supporting me and Fran for all your help and advice on my assignments. I could not have gone through it without all your support. THANK YOU xxx
From – Minara Khatun
To – Bob Singh
To – Balbinder Aujla
Bal has been extremely helpful and welcoming, she is always ready to teach. As a third year student Bal has ensured to construct a plan with me to help meet my learning needs every time I've worked alongside her. She has supported my medicine management, time management and helped me understand how best to plan and coordinate care. She has ensured to answer all my questions appropriately to help with my transition from student to registered nurse. Thankyou Bal for all your support
From – Savera Ahmed
To – Paul Heath from IT
Whenever Sandwell A&E reception needs IT support, Paul will go above and beyond to get the job done. Today Paul had to search the hospital for the correct screws to secure a computer monitor. He always has a smile on his face.
I'm new to SWBH and my role involves travelling to both sites via the shuttle bus. I just wanted to say that Bob is exceptionally jolly and welcoming and a credit to the SWBH Team.
Ezinne has recently taken on the link nurse position on D30 and has approached it with refreshing enthusiasm meaning D30 has a exciting approach to infection control. Thank you for making a difference for our patients!!!
From – Claire Obiakor
To – Joanne Wright
I would like to put a shout out for Jo on behalf of her staff upon lyndon one. She goes above and beyond in her role as a manager and works past her time to ensure staff are supported. She helps and supports the staff. She helps in many ways with staff along with patients and families.
To – Felix Sagoe Felix always goes above and beyond for his patients. He is calm, well mannered, polite and always delivers excellent patient care. he has slotted into the team so well and the AMU cluster are lucky to have you Felix!
From – AMU, City
To –The Medical Ward's Discharge Coordinators
The team work tirelessly on a daily basis supporting their ward team and the capacity team. The have fantastic working relation with the MDT which helps provide well organised, speedy discharges to our patients. They are an amazing team who's skills are second to none. Lets give them all a shout out because they are truly AMAZING!!!
From – Sherry Craig
To – Janet Hanson
Going over and above following a home visit where the patient was enduring unacceptable living conditions and at significant risk of poor mental health and post-surgical wound infection. Janet has taken the time to ensure the patient has a safety net in place escalated her concerns with the landlord, social services, the police and the patient's GP. Janet has given exceptional care and shown real humanity in her support of this patient. She's a credit to the Trust.
From – Chloe Travers
To – Lisa Hall from Delivery Suite
Positive feedback from one of our birthing families, who as a refugee felt overwhelmed about birthing in a new country. She expressed how positive her experience was with Lisa's care. Thank you
From – Afrah Muflihi
Thank you all for your part in the extraordinary MDT effort last night on labour ward. You have taken the families concerns into account and kept a clear and thorough record of the whole process.
From – Chloe Travers
To – Emmie Cliff
A couple have expressed what a lovely experience they had whilst visiting maternity triage and how Emmie was professional and so kind to them. Emmie is an example of how to model our Trust values. Thank you Emmie.
From – Afrah Muflihi
11 CORPORATE AND GENERAL NEWS
To – Cherelle Goodall, Nazmeen Bibi, Emily Fidoe, Haja Anifa Sanusi, Narinder Kaur, Micheala Fellows, Gemma Gates, Samina Chaudary, Roisin Bailey, Angela Barlow, Riya Jerry, Clementine Jack and Sarah Harrison
From – Infant Feeding Team
From – Lucy Keates
To – Elizabeth Crisp, Julie Hopkins-Budd, Helen Bateman, Lisa Stewart and Frances Edwards
To – Ezinne Otiba
From – Kayleigh Beaumont
To – Katie Lamb, Emmanuel Emovon, Rose Chaudhuri, Elaine Leung, Faisal Baig
From – Lisa Joiner
Discharge lounges – relaxing spaces for those ready to return home
Patients who no longer meet the criteria to reside can now relax in comfort in newly opened discharge lounges based in Newton 1 ward at Sandwell Hospital and AMU 1 (old AMAA) at City Hospital as they prepare to return home or move in to a community bed.

Whilst acute hospital beds are often in high demand there are many patients who are ready to return home and are simply waiting for family members to collect them, transport to arrive, letters to be completed or medication to arrive. However, with the opening of the new discharge lounges, patients can move from their wards to the discharge lounge and relax whilst they wait.
Sharing the news of the new discharge lounges opening, Heartbeat spoke to Sister Louisa Lowe, she said, “The new discharge lounges have the potential to be incredibly beneficial to the Trust as well as improving patient experience. Acute beds are in high demand and there’s always a push improve patient flow and to try and ensure that patients are discharged as early as possible so that the bed can be made available for another patient, on occasion this is problematic due to logistics, when family can collect a patient and when transport
can make time. The new lounges take some of the worry away, offering patients a relaxing environment they can move to, which is quieter than a standard ward, where their needs can continue to be met and they can prepare to return home.”
The new discharge lounges are open 7 days a week, from 7am through to 7pm. Please include the discharge lounge in your patient discharge discussions so they are aware of
the journey. The lounges have eight chair spaces and four bed spaces on each site to support our patients comfort whilst awaiting discharge/transfer.
For more information on the new discharge lounges, contact Karenjit Birring on karenjit.birring@nhs.net or 07976075498. To call the lounges directly, call ext. 2752 or 2757 for Sandwell, or ext. 4990 or 5131 for City.
Colleagues at the newly opened Sandwell discharge lounge ready to welcome their patients
MEDICINE AND EMERGENCY CARE
Heart expert focuses on prevention
MEDICINE AND
CARE
Coronary angioplasty, carried out in the cath lab, involves successful balloon stretching and stenting of the coronary arteries.
It’s now the most popular method of revascularisation with 100,000 procedures performed annually in the UK and means most patients don’t need to have bypass surgery.
Derek’s passion for secondary prevention within the population has been further propelled with his appointment as the cardiac lead for the Black Country Integrated Care Board and the Integrated Care Partnership.
After performing more than 5,000 lifesaving operations in the cardiac catheter (cath) labs at our Trust, consultant cardiologist Professor Derek Connolly is hanging up his scrubs to focus on prevention across our population.
For more than 34 years the clinician has devoted himself to coronary intervention setting up the primary angioplasty service after arriving from Papworth, Cambridge in 2000.

Before the primary angioplasty service one in seven patients died of their heart attack despite being admitted to
Hospital. Overnight, with the start of primary angioplasty it went to one in 30 saving many lives over the last two decades.
Derek, who is also the Trust’s Director of Research and Development, said: “For 34 years I have dedicated myself to coronary intervention. Five years after starting up the service at SWB it went 24/7 for heart attacks and we were one of very first Trusts in the country to do this. There were cath labs at both Sandwell and City Hospitals then.
“It was pioneering, and we were leading the way.”
He’s been also busy building our already successful relationship with Aston University and as such he’s been given an honorary professorship.
He added: “I am giving up treating patients presenting with heart attacks and instead preventing heart attacks happening. Prevention is definitely better than cure but I am grateful for my younger colleagues continuing the phenomenal primary angioplasty programme."
Medical SDEC – formerly known as AMAA
The Acute Medical Assessment Area (AMAA) is now known as Medical SDEC (Same Day Emergency Care) following a rebranding exercise.
The service is for patients who need to see a hospital doctor but don’t require an overnight stay. They are referred via the emergency departments (ED) and also via SPA.
Staff should also be aware that Medical SDEC at City Hospital has moved to the former Medical Infusion Suite, opposite AMU2, first floor.
At Sandwell, it is currently situated at the former Chest Clinic, ground floor near to ED, but is due to be moved over the coming months. Colleagues will be updated when this takes place.
Chris Mason, Service Manager, said of the change: “We have done this to improve the flow through the organisation with an aim to decongest our emergency departments, to ensure that patients are seen within the most clinically appropriate environment for their needs.
“The teams at both sites have worked incredibly hard to support the move and are fully behind the ongoing plans for the development of Medical SDEC. We have already seen a marked improvement in our figures following the move at City and hope within the coming months to replicate this at Sandwell.”
The service has also been changed to Medical SDEC on the IT systems.

13
Professor Derek Connolly who will now be focusing on prevention
EMERGENCY
Dr Sarb Clare, Andy Wilkinson, Sajan Sathyan visit Midland Met to inspect the SDEC facilities being constructed
Team of the
S AWArRDS
The tables were laid, the drinks were poured and the scene was set; we were just waiting on the most important element, our guests.
On the evening of Friday 7 October, we celebrated teams and colleagues from across the Trust at the Star Awards 2022.


With 14 awards up for grabs, colleagues from departments across the Trust arrived eager to find out who had won the coveted prizes and enjoy the carnival. Around 350 people from SWB, as well as our community and partners, attended on Friday.



We're grateful to all sponsors, without whom we would not have been able to celebrate as we did. Our congratulations go to this years' winners, who demonstrated how they go above and beyond in living our values every day.

Vaccination Team, Clinical
Year
Siten Roy
Afrah Muhlifli
Equality, Diversity and Inclusion Award Andrew Churm, Employee of the Year Portering Team Integrated Discharge Hub Partnerships with the Community Award Distinguished Service Award Non-Clinical Team of the Year
2022 Winners:







15
Grace Hughes, Learner of the Year District Nursing Blue Team
Rhea Conn, Sustainability Award
Michael Reay
Emergency Department, Special Recognition
Award
Jason Yap Justine Irish
Shivan Pancham
Prize for Transformation and Research Quality
of
Care
Award
Patient Safety Award RisingStarAward Volunteer of the Year
S AWArRDS






16
to our sponsorsThank you Congratulations to everyone #SWBAwards22 16
Raising awareness of sickle cell wonder drug
MEDICINE AND EMERGENCY CARE
about to have a crisis. This lasts for five minutes then disappears. There’s definitely an improvement and I feel I have come on leaps and bounds.
“I’ve suffered for years and years thanks to this disease and as a result have a number of health issues. I definitely feel had I had this drug when I was younger, I wouldn’t be suffering as much with the various ailments I have. It’s important that people with the disease are aware of this treatment and the film that will be produced will go across social media so that sufferers can see first-hand how it is helping me.”
As many as 5,000 people will be treated over the next three years with the new drug.
Loury said previously about the disease: “It’s been part of my entire life. People look at you and think you look fine, but they don’t understand the pain and the trauma along with the many trips to A&E.
“When I have a sickle cell crisis, it’s like someone has a knife and they are ripping it through my joints – particularly my hips and legs.
“Whenever I thought about having this new drug it brought tears to my eyes. I am so excited and over the moon because it is literally lifechanging for me and my family. I really want to encourage other eligible people with this disease to come forward and get this drug”.
Crizanlizumab, delivered by a transfusion drip, works by binding to a protein in the blood cells to prevent the restriction of blood and oxygen supply that leads to a sickle cell crisis.
Patients with sickle cell suffer from monthly episodes, making it difficult for people to continue in their jobs or other everyday activities.
In February we became the first Trust in the region to administer the crizanlizumab drug to sickle cell patients.
The new treatment reduces chronic pain which leads to trips to A&E and dramatically improves the quality of life for patients.
Now seven months on, Loury Mooruth, who was one of the first to receive it, is pleased with the results the drug is having
so far and her journey has been documented by a filmmaker so that she is able to raise awareness of the treatment.
She said: “Since I started on crizanlizumab, I have had one crisis which was in March. It lasted five days – normally they last 10 and I will have a major one every two months.

“One thing I’ve noticed is that I will have a feeling every two days or so that I am
The drug is expected to reduce the number of times a sickle cell patient needs to go to A&E by two fifths.
The Trust is one of the 10 dedicated centres to treat sickle cell disease across the country. Patients will be able to access the new treatment through their consultant at one of these clinics regardless of where they live in the country.
17
Loury Mooruth is highlighting how crizanlizumab is helping her condition by featuring in a film about the drug
Breast cancer awareness month –Cathy's story
Following a devastating diagnosis of breast cancer, colleague Cathy Brown chose to deal with it head on and treat each day as an opportunity to continue living her life.

She explained: “Throughout my treatment I was determined to keep a positive mental attitude - I couldn’t change my diagnosis or treatment regime and dwelling on it was not going to change anything – and my family, friends and colleagues were so supportive and were there (sometimes virtually) to ‘pick’ me up when I was having an off day – I couldn’t have got through this without them.
“My story starts when I found a lump around the end of last year and then following a visit to my GP, was referred to a ‘one stop’ appointment at my local hospital. I underwent a mammogram and ultrasound and they took a small biopsy of the lump at that visit - I was given my diagnosis a week later, and embarked on what seems like a whirlwind of treatment. So far, I have had eight cycles of IV chemotherapy and initial surgery, where the lump and some of the lymph nodes in my armpit were removed. I am currently undergoing a further six cycles of oral chemotherapy, prior to further surgery next year. Throughout this my team and managers have been hugely supportive – I was able to work from home as much as I felt able to whilst I was having my chemotherapy and it gave me something to distract me from what I was going though. It was lovely to be able to see colleagues on Teams and would have felt very isolated had this not been possible.
“However this last year has been a real rollercoaster with various side effects of the treatment to contend with. I lost my hair very quickly, with it coming out after my first round of chemo – I had been prepared by the oncology team that this would happen and had my hair cut short prior to starting the treatment so it wasn’t such a shock to me or others! I used hats or headscarves initially as I was very self-conscious, but quickly became more confident with my ‘new look’ and stopped wearing them. Other side effects were acute, but quite short lived after each chemo infusion, however my general level of physical fitness and stamina were greatly reduced. Another side effect was insomnia, which compounded the overall lack of energy and tiredness.
“I managed to keep active, by walking my dog at least once a day – even if that was for only ten minutes. By the end of my chemotherapy, I could only walk about 100 yds before getting breathless, but within two weeks of finishing my chemo, I was back to walking about 3-4 miles a day, which was not only good for my physical fitness, but a huge boost to my mental wellbeing as I felt that I was getting back to ‘normal’. Additionally, I had to limit the number of people I saw face to face, as I was immunocompromised from the treatment, particularly in enclosed environments – so getting out and about allowed me to interact with friends and family – thank goodness we had good weather this summer!
“Following my recent surgery, I was off work for about six weeks and am now phasing myself back to fulltime hours. I am currently having to work from home again, as I have just started more chemotherapy. Although the cancer has never made me feel unwell and if I’m honest, apart from a couple of occasions, I didn’t feel unwell whilst I was having chemo (even though it was unpleasant), it nevertheless affected my day to day living, in terms of not being able to do things that
previously I’d been able to do – I found this really frustrating and quite demoralising. As I result, I had to adapt my lifestyle, doing things when I felt able and listening to my body – resting when I needed to and having naps during the day, particularly if I hadn’t slept well. The chemo also affected my sense of taste and meant I didn’t enjoy certain foods, so I changed my diet and just ate what I fancied!
“Receiving a cancer diagnosis is devastating, but as long as it is caught early enough, its normally treatable. I would urge everyone to ensure they take up offers of screening and look out for signs and symptoms of cancer. For breast cancer, colleagues should ensure that they check themselves regularly and act on anything unusual – my tumour was very fact growing and was about five cm by the time I found it, about six weeks after I’d previously checked myself. I would also advocate trying to keep positive and talking to friends, family and colleagues – a problem shared is a problem halved. Whilst no-one can change what you are going through – you’re not going through it alone and that makes all the difference.”
18
Cathy Brown
WOMENS AND CHILD HEALTH
Menopause: Continuing the conversation
on the topic with the title of Menopause and Hormone Replacement Therapy – Evidence based Update and added it to the electronic platforms of both Aston University and University of Birmingham for year 4 and 5 medical students.
World Menopause Day is held every year on 18 October and was designated by the International Menopause Society to raise awareness of the menopause and to support options to improve health and wellbeing for women in mid-life and beyond.
One of our colleagues Consultant Gynaecologist, Professor Shagaf Bakour is helping transform doctor teaching by ensuring students receive education on the menopause.

Shagaf who is also a director of medical education at Aston Medical School said: “Forty-one per cent of UK universities do not have mandatory menopause education on the curriculum. Realising this gap and acknowledging the significance of medical students understanding the menopause, the hormones and the menopausal hormone therapy, I developed e-resources
“The Academy and I also organised tutorials where the clinical teaching fellows learn the topic using these e-resources and teach the medical students at our Trust. The tutorial sessions have been truly interactive and have intrigued good discussions which would further enhance students’ understanding and applying the knowledge on case discussion.”
We asked Shagaf what inspired her to focus on the menopause as a special interest.
“It’s important that women who are going through the menopause recognise what it is and how to get help and support,” said Shagaf. “It is also equally important that when women seek help, those professionals are able to advise and put them on a bespoke best treatment plan.
“Educating medical students, our tomorrow’s doctors, about this subject as a core condition would enhance their understanding of the menopausal transition, recognise the symptoms and be confident when encountering such a patient, to diagnose the condition early and move readily to the correct management. When appropriate, HRT should be the first line treatment for vasomotor symptoms (hot flushes) not anti-depressants
From imaging to acting
Elizabeth Kirk, Cancer Services Patient Administration Manager, is making an impact both at SWB and as part of Walsall Operatic Society.
Elizabeth started working at SWB in April 2002, joining straight from college. Previously a medical secretary, she recently began working in her current role: it’s newly created, and Elizabeth is beginning with a 12 month period to prove the concept. It’s different to her previous role: where she she used to spend a good amount of time focused on interaction across a number of patient groups, she now focuses more on patient care and ensuring cancer patients are able to get their scans in a timely manner. Elizabeth stated, “After 20 years in the trust as a secretary I decided it was time to embark on a new adventure whilst still being able to play an active part in patient care.”
In her spare time, Elizabeth focuses on something very different from her career –she has, for around 18 years, been heavily involved in amateur dramatics as part of
Walsall Operatic Society. Performing one show and one concert a year, the group performed most recently in October, and are currently preparing for the auditioning and casting process for their upcoming show, The Full Monty, due to be performed at the Prince of Wales theatre in Cannock in March 2023.

This show is a change for the group, who are used to more traditional productions. Elizabeth said it’s “unusual, but we are looking forward to making it work!”.
Elizabeth has always been musical, having performed in Sandwell Youth Music from the age of 7. When she started working at the Trust, she left the group and joined an operatic society instead – and she’s had the bug ever since, only
Shagaf told us many women are turned away by their doctor, denied treatment for debilitating symptoms when they are not recognised as being connected to menopause and are incorrectly offered antidepressants.
She added: “Uncertainty in medicine comes from either lack of personal knowledge or limitation of the current medical knowledge or a combination of both. As the medical knowledge on the topic of menopause has been refined by the NICE guideline that is evidencebased, and regularly updated, we need to educate the learners to ensure their knowledge is up to the expectations.”
“We need education on the menopause standardised across universities and we need to ensure there is mandatory catchup CPD courses for GPs and general gynaecologists. The curriculum and menopause training for GPs currently in practice needs to be urgently addressed. Otherwise, the inconsistent quality, quantity, depth and breadth of the information available to trainees and students will continue to result in a postcode lottery for women which is unacceptable.”
IMAGING
taking breaks when she had her children. Rehearsing two to three times a week, she also takes part in a local church drama group in Willenhall with her daughter.
Elizabeth recalls that over the years, a number of Trust colleagues were also part of the society, and emphasises that it helps her to switch off from work. She encourages anyone with an interest to get involved; “We welcome anybody over the age of 14 years, it’s a great hobby for socialising and making new friends.
“It helps me to deal with stresses of everyday life when I am on stage its just about being that moment and being someone different!”
If you’d like to get learn more and get involved, please get in touch with Elizabeth on Elizabeth.kirk@nhs.net, or visit the website at www.walsalloperatic.com.
19 WOMENS AND CHILD HEALTH
(NICE, NG 23 last update March 2022).”
Professor Shagaf Bakour
Walsall Operatic Society
Simba's sniff saves life - dog detects cancer in colleague
IMAGING
When colleague Theresa Field’s dog started pawing at her chest, she thought he was just being affectionate.

But for two weeks puppy Simba, a cross boxer breed, wouldn’t leave her alone.

Eventually she felt around her breast area where the dog was snuggling into and discovered a lump. Knowing it could be serious Theresa, who works as an admin in occupational health and wellbeing, contacted her GP and was quickly diagnosed with breast cancer.
The mum-of-one, aged 50 said: “Simba is my superhero – I believe he’s saved my life.
“I had him for 10 months when he just began behaving differently around my body. He would jump up onto the sofa and start nudging my breast. I kept pushing him away but he was really insistent.
“He wouldn’t leave me alone. It was really out of the blue, so I did think it was strange. Simba had been trying to tell me something was really wrong for two weeks but initially I just thought he was after a bit of attention.”
She added: “Eventually I thought I’d better check as you hear these stories about dogs having a sixth sense, and as I felt around the area I discovered the lump.
“I’m so glad that he persevered – as if I had left it any longer my condition would have worsened.”
After finding the lump on 5 August, Theresa didn’t hesitate in booking an appointment with her GP and she was immediately referred to City Hospital’s rapid access clinic within the breast unit.

“I went along and had all the testing done with the results coming back really quickly,” she explained. “The clinic was amazing and the staff working there have been so supportive.”
Theresa will now undergo an operation to remove the lump and her left breast.
She added: “I never really thought about checking my breasts for lumps, but this shows you how important it is. I want to raise awareness around this so that women check themselves regularly. If you’ve got an animal and it starts acting strangely around your body, then please get checked out and don’t ignore it. I’d also urge women to attend their routine breast screening appointments as well.
“These last few weeks have been extremely difficult but imagine how much worse it could have been had I not been alerted to the lump so early on.”
Theresa will undergo a course of radiotherapy after her operation.
She added: “I’ll have Simba with me at home supporting me throughout which I’m so thankful for.”
Claire Murphy, Health Promotions Specialist, said: “We would urge everyone to regularly check their breasts for any changes and report any symptoms to your GP.
“Women registered with a GP will be invited for NHS breast screening every three years between the ages of 50 and 71. Women aged over 71 can also attend breast screenings every three years, but they must self-refer by calling the screening office to book an appointment.
“Mammograms are performed by female mammographers who are trained to help you feel more comfortable and provide support with any questions or concerns you may have.
“As well as attending routine breast screening when ladies receive an invite, it is important to be breast aware and report any changes to their GP.”
20
Theresa Field with her dog Simba
Theresa Field
Kindness gets kids on the road to recovery
In September 2020, children in BMEC were delighted as the department was gifted a mini-Tesla. The donation was from Tesla Owners UK to Your Trust Charity for paediatric patients to make their way to theatres for surgery.

Unfortunately, the steering wheel was damaged on site, and after many attempts to repair it or find a replacement part, the car became unusable.
James Morrissey, Theatre Manager, told us: “Our youngest patients enjoyed using the toy car to drive themselves to surgery. Surgery can be daunting, but somehow the car made it a more fun process, and they enjoyed driving it down to us. Seeing their little faces light up as they got into the car was a joy which is why we were all saddened when we could not organise a repair.
from America and got the car repaired.
“This act of kindness means that our youngest patients can now drive themselves down to us to have their surgery. It helps to change what might be a negative experience into a joyous experience for the children in our care. The team and I are all grateful for Kelly’s support. She is, in our opinion, the best example of someone that lives our values and goes above and beyond to enhance the patient experience.”
Ava made her way to surgery in the toy Tesla along with members of the theatres team
“Not long after joining the department, Kelly Papavarnava, Deputy Group Director of Nursing (Surgical Services), heard about our toy car and set about finding a replacement part with the help of her dad. Much to our amazement, Kelly was able to source a replacement steering wheel
Kelly told us: “My inspiration was to support the team as they had worked hard to resolve this for the benefit of our paediatric patients. The use of the car is extremely positive and brings some laughter and joy to children at what can be a scary time for them and their parents.”
Heart-felt donations make a huge impact to mortuary service
PRIMARY CARE, COMMUNITY AND THERAPIES
can do to support; simply making sure we have a supply of clothes for some of our smallest patients so they can be dressed before their parents see them can have a huge impact.
“Alongside the baby grows, the Wednesbury Craft Group have knitted some incredible intricate moses baskets and blankets for babies that we will be distributing across the Trust to the emergency department and neonatal department, ensuring that any newborns have a warm blanket and comfortable basket when they’re delivered.”
Members of Wednesbury Craft Group show off their touching creations for tiny babies
Members of the community have made an incredible impact with their recent round of heart-felt donations to the Trust’s mortuary service – helping care for deceased babies.
Sharing the touching news of the donations, Mortuary Service Manager Lauren Wood spoke to Heartbeat. She
said, “Recently, kind members of the community have been donating baby grows to our department, so that when a baby is transferred into the care of the mortuary department, we have some suitable clothing and grows to dress them in.

“Losing a child is an incredibly traumatic experience, so we’re keen to do anything we
“I am absolutely amazed by the kindness and support of our local community. It has been heart-warming to see their generosity, their kind donations will have an impact on many lives for months to come.”
For more information on how you can support the mortuary service, contact mortuary services Manager Lauren Wood on email: lauren.wood19@nhs.net
21 SURGICAL SERVICES
Keys handed over to region’s first reablement centre
A new £14 million integrated reablement centre has been officially handed over to officials from Sandwell Council.
Richard Beeken, Chief Executive alongside Rashpal Bishop, Director of Adult Social Care for Sandwell Council and Councillor Suzanne Hartwell, cabinet member for adults, social care and health were at Harvest View, in Rowley Regis, which is the first of its kind in the region, for the event.

The centre, opening in November, has
80 bedrooms with state-of-the-art facilities providing nursing, care, and therapy to support people for up to six weeks, to get back on their feet after a hospital stay or prevent an avoidable admission to hospital. The unit will have a strong focus on ‘homefirst’ reablement and supporting individuals to live as independently as possible following a social care or health crisis and avoiding unnecessary placements for people in long term care facilities.
There are also facilities such as a physiotherapy facility, large communal areas and treatment rooms and the centre is designed to ensure accessibility throughout the building for people with limited mobility.
This integrated social care and health centre facility will provide much needed support
to residents and will support the council’s wider regeneration vision to ensure that people live and age well within the borough.
Daren Fradgley, Chief Integration Officer added: “Harvest View represents another exciting opportunity to deliver integrated health and social care services across our system for the people of Sandwell, building on the positive work we have already started with Discharge To Assess (D2A). This is a very real example of how the health and care partners across the borough are working together for the benefit of the patient in a truly integrated way. We look forward to welcoming patients through the doors later this year.”
22
Harvest View keys are handed over to Sandwell Council
PRIMARY CARE, COMMUNITIES AND THERAPIES
Letters, of less than 200 words please, can be sent to the Communications Department, Trust Headquarters, Sandwell Hospital or by email to swb–tr.SWBH–GM–Heartbeat@nhs.net
Do our senior team just enjoy a day out?
Dear Heartbeat,
So recently I’ve seen that all sorts of teams have been off on days out, and attended some sort of improvement events. I get why these happen, but why haven’t my team had the same? We had one during covid but haven’t had one since and I think it would be really good for everyone to get together and enjoy a day out. We work really hard with our patients and I think it’s only fair that we get the same chance to go out as any other team. How can I ask my manager to organise one of these days out?
Kind regards Anonymous
Dear colleague
I agree – time together as a team is really precious and I’m pleased you were able to make use of the centrally funded time-outs that were part of our commitment to staff to support restoration and recovery. The first round was publicised and open to all; all applications were considered and those which represented value for money were approved. Many teams already have regular time out or time together scheduled and the additional support was to ensure that funding was not an object in allowing people to spend time reflecting on experiences and building back relationships.
We have had a lot of interest and requests for further support for funded team time-outs. We are currently in a very different (and difficult) financial position and the ready money available to the NHS during the COVID-19 pandemic has now stopped. Nevertheless, we recognise the importance of teams spending time together so are committed to bringing back the opportunity to request central funding. Our criteria will be slightly more stringent than before as we will want to be able to demonstrate the learning outcomes so that it stands up to public scrutiny. The application process will be published shortly.
Best wishes
Dinah McLannahan, Chief Finance Officer
Is the shuttle bus running as it should be?
Dear Heartbeat,
So it seems time after time whether that be at the actual shuttle stop or in staff comms I see the shuttle service is operating a reduced service. I understood during peak COVID but this seems to be an ongoing issue. It seems we have a reduced service more than full capacity these days. The Trust encourages us to use the shuttle to save lots of people driving back and forth but at the moment the service is inadequate and unreliable. I can’t depend on it if I need to get across site as I don’t know when the shuttle will be turning up because there is a reduced service o if it does turn up, due to the lower amount of buses there won’t enough seats. The odd meeting I can do by Teams but majority of the time me and my team need to be able to get cross site. Is it a staffing issue and we need to employ more drivers or is it a servicing issue where we do not have enough vehicles? I hope this gets sorted soon otherwise the Trust might as well scrap the whole service and just reimburse better rates for petrol as it seems like that may be the only suitable option as things stand. I can only hope we don’t just get a generic response from this letter and instead issues are actually addressed. PS: It would be nice if the shuttle service actually let us put small parcels on again within reason. It seems the service has gone backwards since I joined the hospital and care more about enforcing this rule than sorting themselves out which only frustrates more staff and when things go wrong it naturally only makes us feel less inclined to have any empathy for them…
Kind regards Anonymous
Dear Anonymous, I am sorry your day was disrupted. Due to unforeseen staffing circumstances, we were forced to reduce the shuttle bus service for a period of 7 days. During this period the service was running hourly between sites. The details were sent out in daily comms bulletins.
With the approval of the CE and COO, and the amazing support of the Trust Bank, we were able to fast track a driver with the required licence and the service returned to normal (half hourly between sites) on Wednesday 19th Oct. We are again out to advert for a substantive member of staff.
In regards to parcels/packages there are several reasons we do not allow parcels/packages on the shuttle: they take up a valuable seat that a staff member could utilise, we are unable to secure them in the vehicle so they are a health and safety concern, and at the end of each week the transport department is left with dozens of uncollected parcels/ packages, often not labelled. These include items such as IT and medical equipment, patient property, confidential patient documentation and various other items. Transport is then left trying to sort these out or taking numerous calls from depts looking for lost parcels/packages. Transport do offer a safe and secure service for transporting parcels/ packages across site: to book, please contact 3869 option 4.
Kind regards, Patricia Kehoe
23
DGM OPD Services YOUR RIGHT TO BE HEARD
This month we say hello to Darren Smith, Group Director of Operations (Imaging and Pathology). We spoke to Darren to learn about his career and plans since joining SWB.

Reflecting on his early career, Darren explained: “I started working for the NHS after graduating with my law degree. I got my first job in October 2009, intending to go back into law, but I have been in the NHS ever since. I have worked in several organisations, which has given me valuable experiences and learnings.
“My first role was during the swine flu pandemic as a site manager for the anti-viral drop off. My first substantive role was as a crisis coordinator in Nottingham within an MDT setting to prevent hospital admissions.
“To gain acute experience, I worked at Nottingham University Hospitals as a bed manager for critical care and major trauma before I moved to the West Midlands and took a role up as an epilepsy surgery coordinator. My first step into a leadership role was as a senior operational services manager looking after bariatric and vascular services. From
Darren Smith
Group Director of Operations (Imaging and Pathology)
there, I worked in various roles, including as a directorate manager, and director of operations in surgery, before taking up my current role. Working in these positions and different areas of the NHS gives me a well-rounded view of the care we provide and the challenges we face as healthcare professionals.”
Since joining SWB, Darren has wasted no time getting to grips with his new role. He explained: “There are several exciting projects underway within our Group. Projects include enhancing diagnostic delivery through community diagnostic hubs, reviewing additional scanning capability within Midland Met and retained estate, pathology work with Black Country Pathology Services, and increasing our work with AI that we've shared globally.
“At a time when demand exceeds capacity, we are reviewing all pathways working collaboratively with clinical groups. It will support patients in getting the right diagnostics, at the right time, at the first time asking. We ask for the continued support of our colleagues to help us achieve this goal, and we will share more information with teams shortly.”
Darren added: “Our teams, like others across SWB, are working extremely hard to ensure we provide the best care by bringing down the backlog where possible. At times of pressure, we ask colleagues to remember that kindness, care and compassion are at the heart of our new strategic values and to keep treating each other well and with civility. Should anyone wish to speak to me about anything directly, I am a phone call, email, or Teams message away.”
Looking to the future, Darren recognises the significance of Midland Met and the many opportunities it provides for colleagues, patients and our communities. He said: “I recently enjoyed a tour of Midland Met, and this was my first time on site. My first impressions were positive – our move will allow us to work with the latest technology to support the delivery of patient care and allow continued collaboration between clinical groups.
“The move to Midland Met will enable us to focus on the inpatient work while the retained estate at Sandwell and BTC and the work we are considering for community diagnostic hubs will support the demand on diagnostic services.”
24
Darren Smith, Group Director of Operations (Imaging and Pathology)
24
News in brief from around our organisation
If you have a story you would like to appear on the Pulse page, please email a photo and a short explanation to swbh.comms@nhs.net
Stephanie Coates, Nurse Lead for Sepsis and Vascular Access, is travelling to New York to run the New York City marathon on the 6 November in memory of Donna Coates, her sisterin-law. She is raising money for the Polycystic Kidney Disease Charity, founded in 2000.
Donna, who worked at SWB as lead nurse for advanced clinical practice, suffered with polycystic kidney disease and had received liver and kidney transplants, but still suffered with some underlying symptoms. She passed away in 2019 after collapsing at home. Other members of Stephanie’s family also suffer from PKD, which affects around 70,000 people in the UK.
Stephanie has previously run the London Marathon a number of times, raising

money for a number of other charities. She originally registered for NYC marathon in 2020, but COVID-19 restricted her from attending until this year. She is now training for the marathon regularly, and despite struggling with a knee injury is well
prepared, running with several friends who provide support.
Stephanie stated: “Donna was the life and soul of the party, with the most infectious laugh – she was very strong, and you’d never have known what she was going through. She always had a positive mental attitude in the face of whatever she was going through. Her loss has left a huge hole in the lives of those who knew and loved her.
“I want to raise money for a cause that means a lot to me, and the PKD charity aims to discover therapies to improve the quality of life of those who suffer with PKD. I’ll be in New York for five days: I want to do some good, take home my medal, do some sightseeing, and most importantly raise a lot of money for such an important cause.”
To learn more about the organisation and sponsor Stephanie’s efforts, visit her Go Fund Me page on https://gofund. me/a4509cd6
Wave goodbye to…
After four decades at SWB, we will be saying goodbye to Geraldine Sheridan, Macmillan Breast Care Nurse.

Geraldine started her registered adults nurse training at Dudley Road Hospital School of Nursing back in 1981. When qualified she would go on to work on our surgical wards on night duty for over 14 years.
“My real enthusiasm for nursing started in 1996 when I worked on what was then St Chads Unit and this is where my passion for oncology began,” said Geraldine.
“After developing this particular passion, I worked on the breast gynae oncology ward for around five years and then in 2004 moved to my present role as Macmillan Breast Care Nurse.”
Though Geraldine has wanted to nurse since she can remember, her most testing times came during the COVID-19 pandemic.
“My biggest challenge was when I was redeployed to work in critical care at City for around five months during the pandemic.
However, what started out as a frightening thought soon changed into a really positive experience thanks to the fantastic critical care team who helped and supported me through my time on the unit.”
Geraldine has been a real credit to SWB and supported many of our patients through difficult times. Don’t just take our word for it –her colleagues also have the same beliefs.
Helen Taylor, Macmillan Breast Care Nurse said: “You are truly an outstanding nurse who has
Geraldine Sheridan Macmillan Breast Care Nurse
touched and made a difference to so many patients’ lives.”
Dr David Spooner, Oncologist echoed these thoughts and said: You are and always will be a legend! Thousands of patients and relatives are grateful for your immense professional skill, but above all for your unique kindness, listening, personal touch, faithfulness, integrity and understanding.”
Mr Mehboob Mirza, Consultant Breast and General Surgeon Clinical Lead Breast Surgery, has also worked closely with Geraldine over the years and said: “Gez (Geraldine) has been an essential part of the breast unit for many years. She has worked with many colleagues including surgeons, radiologist and oncologists over these years and provided a first-class service to all her patients.”
As part of her retirement Geraldine plans to spend more time with her grandchildren.
Happy retirement Geraldine – good luck in the future!
25
Geraldine Sheridan and her team
Stephanie runs NYC marathon in memory of SWB matron and sister-in-law Donna
Stephanie Coates
Pulse
Wave goodbye to…
Brian Stubbs will be retiring after 38 years with the Trust
After well over three and a half decades at SWB, Brian Stubbs, Sterile Services Team Leader will be retiring from SWB.
His journey at the Trust began back in 1984 where he was one of 17 people to join the sterile services team based in Sandwell.
“When I joined the Sandwell based sterile services team back in the 80s the role entailed the collection and reprocessing of used operating trays and equipment for clinics and theatres, and returning after reprocessing,” said Brian.

“This involved washing and sterilisation as it was done in house at the time.”
When the role was in its infancy, it also involved the production and processing of soft packs, jugs, bowls, drapes, gowns as well as the supply of sterile syringes, needles for all wards, clinics and theatres at Sandwell and various clinics and hospitals in the Sandwell area on a daily basis.
As the years passed the role evolved and progressed but Brian always stayed relevant and also took up a few different roles at SWB.
“I was a van driver as well for a while before our transport department took over and pre sterile equipment replaced the items we had to produce before so the sterile services itself involved more purchasing and storing of goods.”
During his illustrious career at the Trust Brian would also meet his wife.
“I met my wife in sterile services when I first started around 38 years ago, she was one of the first people I actually met in the Trust and department. We eventually tied the knot and got married eight years ago which was a very special moment for us both and I may not have met her if I didn’t join SWB.”
When asked about advice he would give to others starting out their career in the NHS, Brian said: “I feel that with hindsight, my main advice would be to persevere and enjoy everything as much as you can as you go along. But most, try to enjoy the satisfaction of actually helping and making a difference to all of the staff and patients you meet and always keep in mind how you are making a positive difference to them.
Brian will be hugely missed by the Trust, especially his colleagues in sterile services.
Brian Stubbs
Sterile Services Team Leader
Geeta Rani, Storekeeper Clerk said: “Brian was an excellent team leader who was always supportive and helpful. His dedicated 38 years of service in the NHS shaped him into the kind and calm person that he is today. He will be missed.”
Sarnjit Kaur, Ward Services Officer said: “Brian was a great team leader who was always supportive and very helpful and understanding of any situation always spoke very kindly to all around him.”
Andrew Gilbert and William Caulfield, storekeepers have worked with Brian for many years and echo these thoughts.
They said: “Brian was methodical in his approach to work and always sought a good outcome for the theatres problems which he encountered daily. He had exemplary timekeeping and always was available to assist staff in his care.
“He was a true gentleman and always courteous and even tempered even under pressure.”
As part of his retirement Brain plans to go travelling as much as possible and see as much of the world as he can.
Happy retirement Brian!
26
Brian Stubbs
26
Richard talks about: Midland Metropolitan Programme Company
Richard Beeken, Chief Executive

RICHARD'S
In just 12 months’ time we are expecting Balfour Beatty to hand over a completed new hospital to the Trust. What will follow is a period of commissioning and equipping of the new building before we are ready to move in and treat our first patients.

Many of you have been patiently waiting for this new arrival for many years and as another date looms on the horizon you may be sceptical about whether it will actually happen. But I can confirm, along with many of your colleagues who have visited the site recently, that the pace of delivery on the hospital site is impressive. Many of the rooms have been completed to allow us to quality check the standards that the rest of the building will be built to and it really feels like we are in the final phase of construction.
It is easy for us to focus on the progress of the building when we think about Midland Met but of course that is only one part of a very large and complex programme of change. MMUH is “more than a hospital” as its strapline suggests. There is no part of our Trust that will be untouched by change when Midland Met opens, whether you work in acute services, in the community, in primary care, in a leadership role or in a support service. All of us need to spend the next period until we open getting ready.
And we are doing this amidst the context of a challenging time post COVID-19, delivering restoration and recovery and being one of the few NHS Trusts working across two integrated care systems and in two place based partnerships, one of which we host. Very few organisations have quite as much going on as we do.
The MMUH changes require new ways of working, different clinical pathways and new systems and processes. We also need to bring our partner organisations along with us so that our care plans work the same for patients who live in Birmingham as well as those who live in Sandwell.
Over the next few weeks, we are organising ourselves differently to ensure that the move to Midland Met is a success. Success doesn’t just mean that we have “moved house” without losing anything along the way! It means that we deliver the multiple benefits that this new hospital model has promised against the significant investment that we have received. These benefits are many and varied but ultimately must mean that patients are treated more safely and have better outcomes and experiences.
So that we give ourselves the best chance of success, we have reviewed national best practice in delivery of major projects and
are setting up an enhanced temporary organisation programme structure. This structure will be called the Midland Metropolitan University Programme Company. It exists within our Trust and will enable us to focus on delivering the remainder of the MMUH programme, the work of which becomes significantly more intense over the next 18 months. Moreover, it will allow us to devote more leadership time to the “core organisation”, our core day to day business, and deliver service and quality improvement in ways the public and our regulators expect of us.
The new critical path will be agreed in November, that aligns all the workstreams to the revised construction programme.
In coming weeks, the new structure will become visible along with detail on its own leadership team, the new or changed job roles and how those roles will be appointed to, bringing much needed capacity and expertise to the programme.
I am confident that by doing this, we are giving our Trust the tools to deliver better on its day to day agenda, whilst delivering a really fantastic new hospital with the accompanying transformed clinical services that will make big improvements to patient care.
27
LAST WORD
Connor takes on charity zip wire challenge
Marie, explained: “Connor is a massive AVFC fan; we all are in our family. Sadly, last year Connor’s nan passed away after battling lung cancer. It was a difficult time for us as a family, so Connor decided to do something to say thank you to the NHS. They were there for us as a family, and that is something we appreciated, the kindness and consideration at a time we found challenging.”
taking on a new challenge, Marie told us: “Connor is a natural daredevil. He has previously done zip-line challenges and abseils from the Holte End to raise funds for the Aston Villa Ability Counts programme. He's also raised funds for the Dementia Cafe - charity is close to Connor’s heart. He loves giving and supporting his local community.
It is not every day that you descend 220 metres on a zip line in the name of charity, but for one young man, it is soon to become a reality as he bravely steps up to raise funds for Your Trust Charity and Aston Villa FC Foundation.
Connor Sherry is an avid Aston Villa FC fan (AVFC) and will be taking the plunge off our zip line to raise funds for two causes close to his heart.

Speaking to Heartbeat, Connor’s mum,
Marie revealed that Connor is supporting AVFC for personal reasons too. She explained: “Aston Villa FC Foundation act as a force for good. They address social issues and drive positive change in Birmingham and beyond.
“The work the foundation does touches upon education, health, sports participation, and social cohesion. The club has always supported Connor, and now he plays disability football. He is the captain of Ability Counts, Aston Villa’s disability football provision. They provide inclusive, accessible football sessions and teach young players the skills they need to succeed.”
Speaking of Connor’s passion for
“So far, Connor has raised £480, surpassing the fundraising target. He set up a dedicated fundraising page and shared news of his latest challenge on Twitter. He is a real inspiration, and we will all be there on the day to support him –his brother, Jaydon, and dad will be there cheering him along with me every step of the way.”
Marie added: “It will be an honour to have Connor’s name printed on the glass borders at the Midland Metropolitan University Hospital to commemorate the part he played in fundraising for Your Trust Charity.”
If you would like to support Connor, visit https://donate.giveasyoulive. com/fundraising/crane-zip-wireconnor-sherry
October 2022 staff lottery results
1st
Don’t forget that Your Trust Charity lottery costs just £1 a month and anyone who works for the Trust can join. Payment is deducted from your wages each month. To take part
johnny.shah@nhs.net
£158.50 Surrinder Chumber 2nd £95.10 Lavinia Hines 3rd £63.40 Poonam Sandal
email
.
@SWBHCharity To donate to the Your Trust Charity text “SWBH16 £5” to 70070 YOUR TRUST CHARITY
Connor Sherry is taking part in our charity challenge