








Welcome to the April edition of Heartbeat.
This month, we're celebrating innovation. Head to page three to read more about Rhea Conn's work as Clinical Sustainability Lead alongside Fran Silcocks, Head of Sustainability, and what they've achieved so far this year at SWB.
We're marking the opening of our new SDEC unit on page 18, and on page 20 you can read about maternity's new 'interpreters on wheels', for women who need on-the-spot support to communicate. You can also read about our advanced new defibrillators on page 19.
Enjoy J
If you’d like to submit an idea for an article, contact the communications team Ext 5303
swbh.comms@nhs.net
We send out a Communications Bulletin via email every day and you can now read Heartbeat articles throughout the month on Connect. Don't forget you can follow us on:
The provision of primary care is essential to our vision to become the most integrated healthcare provider. Your Health Partnership (YHP), the Primary Care Network that runs the Lyndon Primary Care Centre at Sandwell Hospital joined our Trust in 2020 and brings valuable expertise and in many cases, helpful challenge as we aim to further integrate services, based around our population’s needs.

And I saw first-hand how they are adapting services to enhance patient experience when I visited them recently. I’d like to call out three things in particular:
Medicines management: A number of clinical pharmacists and a pharmacy technician are integrated into the practice to deal with matters such as:
• Medication reviews for those on repeat prescriptions. They are available to speak to patients about their medication and help them to understand their conditions better
• Actioning changes to medication made whilst patients are in hospital (typically within 48 hours)
• They are also involved in long term condition management with plans in place for each pharmacist to eventually manage their own speciality, e.g. hypertension.
The presence of these pharmaceutical colleagues means the practice is able to prescribe safely by running regular safety audits, particularly for high-risk drugs. They are also able to identify compliance issues.
As a result, patients are not having to wait for GP appointments and queries are dealt with quickly. The team are available every weekday, often offering extended hours access on a Saturday too.
Cloud based telephone system: In 2018, YHP introduced an operating system for their central contact centre which handles
all incoming calls for 53,000 patients, approximately 2,800 – 3,000 calls per week. In November 2021 they invested in enhanced functionality which gave access to better data gathering, a reporting suite and a live dashboard.
The functionality improves the quality of incoming calls as there is an ability for colleagues to listen to their own calls, which is great for learning. Through the live dashboard it is possible to see exactly what our patients are experiencing in the moment – the number of people in the queue and the current wait time. This enables colleagues to be deployed quickly to assist if required.
The next phase is to introduce a software called CallConnect GP which links directly with our GP patient record system and will bring further benefits such as the ability to see who is calling, saving an average of 12 seconds per call. It will have the capability to place a telephone call to a patient directly from their record, saving an average of six seconds per outbound call.
Primary Care Networks have been set the task of introducing cloud-based systems during this financial year so it’s incredibly positive that YHP are ahead of the curve and leading the way.

GP recruitment: YHP work with the medical staffing team to proactively recruit GPs and it is expected that the next round of interviews will take them to full establishment. A number of the applicants are those who undertook placement training at YHP and have chosen to return and work for the practice full time as a salaried employee – a clear indication of the quality of training delivered.
The work taking place at YHP is a great illustration of our purpose which is - to improve the life chances and health outcomes of our population. It also delivers on our five-year strategic objectives of Patients – People - Population
reach an 80 per cent reduction by 2028 to 2032;
2. For the NHS carbon footprint plus, or the emissions we can influence, to reach net zero by 2045, with an ambition to reach an 80 per cent reduction by 2036 to 2039.
SWB is driving sustainability into how we deliver care. We have implemented many projects, including solar PV, replacing inefficient boilers, installed LED lighting, rolling out our Green Impact staff engagement programme and much more. To further our engagement with clinicians, we recently became the first trust in the country to pilot a scheme behind a newly created clinical sustainability lead post. This role is carried out by Rhea Conn, who also works as a senior sister on the critical care ward. She dedicates 30 hours a week to her nursing role and spends 7.5 hours working as clinical sustainability lead.

The 75th anniversary of the NHS occurs this year, and it’s a fantastic time to look back at the history of the organisation and everything it has achieved in the last 75 years. However, it’s crucial that as we mark this momentous birthday, we also look forward to the next 75 years, discussing how we move forward and continue to provide first-class care for our patients.
Some example projects include:
• Conducting walk-arounds, asking staff about sustainability, as well as raising awareness of green impact and the Trust’s green plan.
• Drafting CQC sustainability standards following their introduction to CQC criteria.
• Supporting other teams, including cardiac cath lab and endoscopy, to reduce waste and move towards reusables
• Working to reduce theatre waste –engaging the team to move towards reusable hats
• Establishing a sustainability team within ITU, as well as an information board at both Sandwell and City. Rhea has also implemented a gloves off campaign in ITU with an audit and teaching package.
One key aspect of the NHS Long Term Plan is sustainability. Having a healthy planet and a healthy population go hand-in-hand. The NHS has two targets here:
1. For the NHS carbon footprint, or the emissions we directly control, to reach net zero by 2040, with an ambition to
What is climate change, and how does healthcare contribute to it?
• The phrase climate change refers to the long-term shifts in temperatures and weather patterns. The planet has been coping with climate changes for centuries resulting in significant ecological, evolutionary and socioeconomic change. Since the industrial revolution the average global temperature has continued to rise and is now around one degree warmer than average surface temperatures in 1880.
• The carbon emissions produced by the healthcare system contribute significantly to climate change, which affects the health of the people it is caring for. If healthcare was a country, it would be the fifth largest carbon emitter on the planet.
• Air pollution is one of the largest risks to health causing seven million
The role focuses on identifying routes to sustainability in the clinical environment, and Rhea works with colleagues across the organisation to explore their ideas. Since starting in January, Rhea has worked alongside Head of Sustainability, Fran Silcocks to deliver a number of projects, focussed on reducing environmental impact, reducing waste, saving costs and improving patient care.
preventable deaths per year worldwide and more than half of the world's population is exposed to unsafely managed water.
• Around 1.8 million people in the UK are living in areas that are at significant risk of flooding – a number which could increase by over 40 per cent, to 2.6 million, in as little as 17 years.
• Public Health England research found that over a third of people who were flooded in 2014 suffered with depression, anxiety or PTSD (Post Traumatic Stress Disorder) and nearly a quarter of people were still experiencing these negative mental health impacts two years later.
If you’d be interested in pursuing any sustainability ideas or having some teaching sessions, please contact Fran Silcocks on Francesca.silcocks@nhs.net or Rhea Conn on rhea.conn@nhs.net.
A survey conducted by the Women’s Clinician Network (WCN) at
The Women’s Clinicians Network (WCN), led by Dr Sarb Clare, is a network of colleagues within the Trust aiming to empower people with knowledge and skills. They have delivered events including a national conference, and recently the group presented the findings of their research, “Say Her Name: Abuse Within the NHS” at the Medical Women’s Federation in March 2023.
The Medical Women's Federation is the largest UK body of women doctors. The organisation is dedicated to the advancement of the personal and professional development of women in medicine and to improving the health of women and their families in society.
It has been recognised that violence against NHS staff has increased since the coronavirus pandemic. The survey, conducted by the WCN prior to a workshop on 13 May 2022, discovered that a large proportion, 82 per cent, of staff had suffered abuse (verbal, physical or sexual) at work. Female staff suffer disproportionately high levels of this, making up 80 per cent of those who had suffered abuse.
Whilst there was no significant difference in rates of verbal and physical abuse
experienced by men and women, women were statistically more likely to experience sexual abuse in the workplace, and a greater proportion of women felt unsafe out of hours. Common barriers to reporting included feeling ‘nothing will be done’, abuse being ‘part of the job’ and ‘fear of consequences’; the latter was described only for reporting sexual abuse.
The data was collected from attendees at a workshop held by the WCN, which aimed to address fears held by the workforce and to empower staff to begin reporting abuse they suffer or witness. Data was collected from attendees prior to the course. The same questionnaire was later shared with colleagues working at various trusts across the UK. A total of 50 responses were collected, with no respondents identifying as anything other than male or female.
Post course feedback was collected, with findings as follows:
• 94 per cent of attendees felt courses such as this were helpful for staff to deal with verbal abuse and physical violence at work.
• 94 per cent of attendees stated they would report incidents where they may have been a witness to abuse as opposed to having been the victim.
• 89 per cent of staff felt more empowered to report incidents to the police.
The workshop was open to all members of staff working within SWB, of all genders and disciplines.
• Feedback included the desire to have quarterly refresher training in reporting and selfdefence.
BMA: ‘Preventing and reducing violence towards staff’ Nov 2021: Unison, It’s Never OK: A report on sexual harassment against healthcare staff, accessed via: https://www.unison.org.uk/conte
The WCN are holding workshops this year, on the following dates:
The initial talks focussed on the disproportionate levels of violence against women in society, and how this is mirrored in the workplace. The talk also highlighted the role of men as allies, with examples of practical measures which can be taken. In addition, a panel discussion was led by representatives from West Midlands Police, including ways in which trust in authority can be developed and fostered.
• 9 June - Learning to Fail
Common barriers to reporting included feeling ‘nothing will be done’, abuse being ‘part of the job’ and ‘fear of consequences’; the latter was described only for reporting BMA:
• 12 July - Navigating the NHS whilst having a family - Top Tips
For more information and to attend, please contact swbh. acutemedicalsecretariesamu1@nhs.net.
to do; firstly, acknowledge that there is a problem and that you have a duty to do something about it. Secondly, do not try to implement any knee jerk interventions, take a systematic approach, carry out needs assessments and understand the issue before implementing a solution.
“We know the data we’re presented with is often retrospective, and when you’re proactive about engaging you often only get 30 per cent engagement, which whilst it may seem wonderful, leaves you with 70 per cent as the silent majority.
“Quite often we find the reasons we’re presented with for sickness absence are not really the root cause. 70 per cent of absences can be attributed to mental health, though initially they’ll be reported as musculoskeletal, when you drill down, the driver is mental health, feelings of not being supported and anxiety around returning.
Masood Aga, Clinical Director for Occupational Medicine and Specialty Lead for Health and Wellbeing recently took part in a HSJ webinar on the subject of staff absence in the NHS.
With NHS staff absence rates already higher than those in the rest of the economy, the pandemic has made the situation even more challenging. Anxiety, stress, depression, and other mental health issues are the most reported reasons for absence. But how can we reduce avoidable absence and provide the right support to staff?
Masood had some fantastic insights into this issue. He stressed the importance of addressing
staff concerns in a timely and effective manner, as well as being proactive in managing staff health and wellbeing. The webinar was a valuable platform for experts in the field to come together and discuss practical solutions to this critical issue facing the NHS.
Sharing his thoughts Masood said: “At SWB we straddle two Integrated Care Systems which nationally sit first and second position for deprivation, which means we have a mammoth task at hand as we find that our staff reflect the same demographic.

“Tackling this issue head on at our Trust, we understood there were two things we needed
“Our biggest barrier we have been challenged with is access to treatment. Whilst you may be able to fast track initial assessments, ongoing referrals can take their toll. We have focussed on ensuring we have a coordinated approach to HR, learning and development and the wider people functions so that we have one single coordinated way of thinking for sickness absence.”
The conclusions drawn from the webinar are essential reading for anyone involved in managing staff health and wellbeing, from frontline workers to senior leaders. With Masood Aga's insights and other expert opinions, we can start to develop a better understanding of the root causes of staff absence and put measures in place to tackle it head-on.
If you missed the webinar, you can watch it back at https://www.hsj.co.uk/ hsj-webinar-on-understanding-staffabsence-in-the-nhs/7034083.article
Since late last year, we have been celebrating winners of the 2022 Star Awards, recognising them for their hard work and the positive impact this has had on our people, patients and population.

We’re speaking directly with the winners to get their views and hear what winning meant to them.
For this month’s Our Winners feature, we spoke with the winners of the Quality of Care Award and the Clinical Team of the Year.
The winner of 2022’s Quality of Care Award was the district nursing blue team. Based in the community, the team contains 22 people in total, from band 3 to band 7. The roles are varied, including nurses, HCAs and a phlebotomist, overseen by team leader, Helen Benwell. We met with Helen and Matron Simon Lines to discuss the work of the team and their Star Award win.
The day of a team member on the district nursing blue team is varied; around 11 community nurses will be on shift on a given day and will visit an average of 10 to 12 patients throughout their shifts. They see a wide range of patients, with their nursing needs varying accordingly: a nurse could be administering insulin, changing dressings, carrying out palliative care for end-of-life patients, or any number of other duties. Helen notes this is a key aspect of the role. She said: “District nurses have to have a wide range of skills, as they will deal with a number of different conditions in the average day.
“It’s not just about skillset, attitude and persona are crucial. Our patients aren’t visiting hospitals and therefore on our territory, we are going into their homes. These are private spaces, and in many cases we could be the only person they see that day or that week. The way we approach the situation and patient is paramount.”
The Quality of Care Award is nominated by patients, visitors and carers who call out colleagues or teams they think provide excellent quality care, in line with our quality plan, producing improved outcomes for patients and their loved ones. In this instance, SWB received an email from the family of Barbara, a patient who received palliative care from the district nursing blue team. Barbara’s family, namely her daughter Jayne, called the team “angels in blue”, praising their compassion, patience and calmness throughout the process. It’s clear that the team made a very painful time more tolerable for Barbara and her family, and it’s this work that was recognised by the Star Award win.
The care they provided was person-centred, prioritising the wellbeing of Barbara and her family. This included ensuring the environment was calm and peaceful, that Barbara was free from pain, and that everyone understood what was happening. Helen stated: “Things such as the right music playing, the lights
being dimmed and fewer people being in the room make a big difference with end-of-life patients. In this instance, everything just aligned and we were able to make things easier for Barbara and her family.”
The win itself has really impacted the team. Simon stated: “The blue team is one of the highest performing teams, so it’s crucial that they are recognised for their commitment. This is a first for us really, as we haven’t had the team recognised at Trust level for a while.”
Helen added “Community isn’t always acknowledged as much as acute departments, so this win was huge for the team. Working away from the acute setting can sometimes result in colleagues feeling somewhat more distant from the organisation, as we don’t have that touchpoint.
“This win boosted everyone’s morale and energy; we revamped our office recently and have our award and certificate displayed on a shelf, which serves as a clear reminder of what we have achieved and continue to accomplish every day.”
Since the win, the district nursing blue team have received lots more positive feedback from patients and families, as well as having some money donated to do something positive for the team. Helen and Simon are looking to use this soon to thank the team for their dedication, commitment and care.

The recipient of the 2022 Star Award for Clinical Team of the Year was the vaccination team. Established in response to the COVID-19 pandemic, the team were formed of colleagues from a number of different areas and led by Louise Brown, Digital Transformation Manager. We met with Louise, alongside Lead Pharmacist for the programme Faraz Ahmed, retired ED Sister, Pamela Bradley-Lake and retired Ward Manage, Joy Haywood to discuss their experiences in the team and what the win meant to them.
Louise said: “We were asked to mobilise in late 2020, just before Christmas. Many of us received phone calls from the deputy chief nurse and came in during annual leave to help out.
“We began carrying out an awful lot of activity that week, starting on Boxing Day. The conference room in the education centre at Sandwell Hospital was transformed into a clinical environment. We were given some vaccine with a five-day expiry and asked to vaccinate around 1,200 people during the week between Christmas and New Year’s Eve.”
The team responded to this immense task with gusto, utilising a number of techniques to incentivise people. “There was a lot a lot of blitz spirit, the chaos was intense, but the camaraderie was high” said Louise.
Shortly after this initial period, the team were mobilised again and built a temporary team, made up of full-time secondees, bank and agency, and retired colleagues. Everyone in the team came together to help the effort. The expectation was that the programme would last around 12 weeks in total, but it simply grew and grew. Faraz said,:“We started in the education centre, opening the clinic at Tipton Sports Centre on 22 February 2021, followed by the hospital hubs at City and Sandwell.”
The vaccination programme was huge, and the team are quick to note that it was largely defined by continued variability, with Faraz stating: “The guidance and eligibility kept changing, as well as supplier routes, and we were mobilising to vaccinate as many people as possible. We were walking into something unknown.” Louise echoed these thoughts, noting that the team would hear updated government guidance on the news on a Sunday night and begin implementing changes when they went into work on Monday morning. This uncertainty was unprecedented, and it’s clear that the experience was a once-in-a-lifetime occurrence for the team. “The programme was constantly evolving, constantly expanding, and we were asked to do more and more,” says Louise. “This was great, as it was clear we were doing things well.”In total, the team estimate that they vaccinated around 200,000 people.
Joy notes that the breadth of knowledge onsite meant many colleagues were able to assist people with health issues. “What was nice from the team point of view was that we were so varied, and the majority of us were bank, agency or retired. This meant that we did lots of health education based on our experiences.” Pamela agreed, stating: “We also extended our skills, because we
didn’t have pharmacy team colleagues onsite all day. This meant the nurses were learning new skills. We also signed off medical and dental students with competencies.”
The Star Award win meant a great deal to the team, with Joy stating it served as a: “Rubber stamp that we had the backing of the organisation for what we had done.” Faraz felt that it recognised their work, noting: “The shifts weren’t easy, with long days which sometimes extended until 10:30pm. We didn’t go in expecting a pat on the back, we did it to get the Trust and country back on track, but it feels amazing to be acknowledged.”
They were also aware of the competition, and that Clinical Team of the Year is one of the most sought after accolades in the Trust, with the winner being voted for by SWB colleagues. Pamela stated: “I didn’t think we’d win, I thought it would be one of the exceptional teams we were nominated alongside. I still miss the programme to this day, and it’s given me a wealth of knowledge for my current role in paediatrics.”
Louise emphasised what it meant to the team: “A huge sense of pride, to be part of the team, to do our bit, and to be recognised. For that moment in time we stood out, which gives us all a huge sense of achievement.”
Many of the team still stay in touch, meeting up every few months and staying in contact through messaging groups. There’s no doubt that the experience will be one that they will never forget, and will stand out in their careers for years to come. This was summarised by Louise, who stated: “When the programme closed, and wound down, it felt like a loss. Most of us had never experienced that camaraderie before, and we may never again. I’m so proud of the team and what we were able to achieve.”
Provided excellent end of life care to a patient on D27. The family provided feedback that their loved one felt comfortable and safe on the ward, while the relatives themselves felt listened to and supported. Dr Rai was highlighted amongst the rest of the team's great work. Thank you!
Thank you all for welcoming me to your team. I have learnt something from each and every one of you. It's a shame it had to end. Stay strong and stay you, you are all amazing in your own unique ways.
Shout out has been a regular feature in Heartbeat and it is fantastic to see colleagues regularly taking the time to give positive feedback to each other.
To nominate a colleague, visit connect2. swbh.nhs.uk/communications/shout-out/, or search 'shout out' on Connect and fill in the form.

The orange DN Team led by Leanne Skelding have been providing care at home to several palliative care patients with complex needs and symptom management. They have shown empathy and professionalism to enable these patients to remain at home to die in their preferred place of care. We just wanted to take the time to recognise that this may have been challenging at times but your care and compassion has shone through.
From – Laura Melough
Went above and beyond to get a frail elderly patient to their loved ones funeral, going out their way to get their clothes and transport so they could say their last goodbyes to their loved one. This is what the NHS is. WELL DONE GUYS
Fiza is a newly qualified radiographer who has handled a potential radiation incident with control and great professionalism. It was a difficult situation and she made the correct decision under difficult circumstances and extreme pressure. We are very proud of her and are grateful to have her as part of Team Imaging.
From
Sonia is always going above and beyond to support our staff and families on the Neonatal Unit. Thank you Sonia for your continued hard work and dedication in making positive changes to improve our families experience and for all the work you are doing with family integrated care.
To – All the support staff in Sandwell maternity community and antenatal clinic
I would like to thank you all for your continued hard work in what is a very challenging time. For all the hard work to tidy and sort the clinic over the last few weeks. Thank you for staying and helping to rearrange the clinics I would not have been able to do it without your help. We just have to keep smiling.
Since mangol has joined the team on waste collection the cardboard on link areas has been kept to a minimum. He works extremely hard and very pleasant.
From – Donna Merson
Kerry went out of her way to help a patient who needed hoist assistance in another area of the department which meant the scan could be completed and avoided a rebook. The patient was delighted. Thank you. Absolute Superstar!
For exceptional antenatal care with a recent patient that needed further DS support for eclampsia. On reviewing the medical notes I have observed continuity, compassion and excellent clinical judgment in transferring a patient in via ambulance saving potentially Mum and baby from an adverse outcome.
Over the last three years Emma has been absolute pleasure to work with when resolving any patient related Unity queries. She always provides prompt answers to the hundreds of questions that I have asked her over the years so that I can assist her and the department resolve their queries quickly and efficiently.
I would like to thank them both for being extremely patient and caring when an adolescent patient with complex needs came to theatre. This patient had come to theatre previously but failed to have the surgery. This particular admission the theatre staff were able to give this patient the time and some control that they needed, which helped this patient's anxiety and surgery was successful.
Andy has been a superstar in IT. I am fairly new to the organisation and he has helped me set up new email addresses, sorted IT equipment and phones and helped me update IT equipment. He has been really approachable, friendly, supportive and extremely knowledgeable and gone above and beyond - thanks Andy :)
Nikki is a star for sorting out a work experience placement and continuing to support the development of our future workforce. Thanks Nikki, much appreciated.
Sam always goes above and beyond to keep products on shelves and keep theatres running, despite the many stock challenges thrown at her. She also supports product evaluations and her knowledge of the processes keeps our patients and staff safe.
We all know that taking breaks and having a space to relax and unwind during a busy workday is crucial for our mental health and wellbeing. That's why we're excited to announce that staff rest areas are being redeveloped around the Trust, and this month we present to you the revamped physiotherapy department's rest area.
We understand the need for colleagues to have a space to enjoy their lunch and breaks in peace and quiet away from their jobs. That's why we're working hard with colleagues in estates to provide you with tranquil and relaxing environments that you can enjoy during your downtime.
The physiotherapy department at Sandwell Hospital is the first to showcase their revamped rest area, having taken a huge step in creating a beautiful and calming space for colleagues. Poppy Bhachu, a member of the department, took it upon herself to transform a staff area that had become a bit of a dumping ground for

broken equipment and supplies, into a haven for colleagues to enjoy during their breaks.
Poppy has worked tirelessly to tidy and clear out the space, and her hard work has paid off. The revamped area now boasts plenty of seating, including comfortable massage chairs, a coffee machine, refreshments, and even a TV for staff to catch up on their favourite shows during their breaks.
We caught up with Poppy to hear more about her efforts and how colleagues are enjoying the new space. "It was really important to me that we had a space where staff could come and relax, away from their busy schedules," she said. "I wanted to create a tranquil environment where staff could unwind and de-stress during their breaks."
Poppy's efforts have been widely praised by colleagues and managers who have enjoyed the revamped rest area. "It's such a lovely space to come and unwind during a busy day," said one staff member. "I feel so much more refreshed after taking a break here," said another.
We're thrilled to see the positive impact that the newly revamped rest area has had on our colleagues in the physiotherapy department, and we're excited to roll out similar projects across the Trust.
Remember, taking breaks and having a space to relax during a busy working day is essential for our mental health and wellbeing. We encourage all colleagues to take advantage of the rest areas around the Trust and enjoy some muchneeded downtime.
If you have a rest area that could do with a revamp to make it more useable and comfortable for colleagues, contact the Estates team on 0121 507 4444.
Bill Thomson, the former head of physics and nuclear medicine at SWB, was recently awarded the Innovation Gold Medal by the Institute of Physics and Engineering in Medicine for a lifetime of contributions to the field. This isn’t Bill’s first award, in 2014, he was given a similar honour by the British Nuclear Medicine Society.
Bill studied physics at Edinburgh University and during his studies he did a summer job in nuclear medicine at a local hospital. Fascinated by the work of the department, the experience steered him towards the NHS when he graduated in 1971. Armed with his degree, he moved to University Hospital of Wales in Cardiff to work and complete his PHD. After 12 years in Cardiff, he was appointed as the head of physics and nuclear medicine at City Hospital, then called Dudley Road Hospital.
Bill remained as head of department at SWB for 38 years, retiring in 2021 after 50 years NHS service. Bill states: “My main focus was on running the department smoothly, and ensuring it had a strong ethos of research and development, which all staff could contribute to. I worked on many areas
of image analysis to improve nuclear medicine studies. I was also involved in radiation protection aspects for both patients and staff.”
Despite retiring, Bill hasn’t ended his relationship with the Trust, he continues to be the radioactive waste advisor for the department and works on two sessions a week, as well as helping to provide cover and help train new members of staff.
In his spare time, Bill carries out his own research; recently, he’s been focused on radiation dose to the skin, which can occur through accidents. These mainly affect staff within the nuclear medicine department, and Bill notes: “These incidents have previously been difficult to estimate. It’s been hard to measure and model incidents of this nature.
“My work is mainly to do with improved modelling and dose estimates, and increasing knowledge of this area. The health and safety executive has been taking an increased interest in this aspect, so there’s lots of awareness in that at the moment.”
This interest has led to Bill sharing his work with colleagues across the wider NHS. He has given around eight invited talks on this over the previous two years, with three so far in 2023. Bill also has a mailing list of over 100 people who are interested in the topic, and sends information of interest to this group on a regular basis.
Bill’s award, presented to him by IPEM president Dr Robert Farley, was given to recognise his numerous achievements

to nuclear medicine over his 50-year career, with the certificate stating it is: "In recognition of his substantial and sustained track record at an outstanding level of contribution to the advancement of healthcare innovation resulting in translation into clinical practice, related to physics and engineering applied to medicine and biology".
He considers this to be akin to a lifetime achievement award, Bill said: “It’s a great honour. I’m really grateful to IPEM for their recognition of my career and input to the field. I’ve covered a lot of different areas over 50 years and it’s been a big effort, so I’m really appreciative.”
Bill has taken some time to enjoy his retirement, spending his free time climbing and mountaineering, he enjoys cross country skiing and trekking in Norway and goes indoor climbing twice a week. He’s also been able to spend more time visiting his daughter, who works as a radiologist, and his two grandchildren.
Bill says he’s satisfied with how his time is split: “Work still takes up a good amount of my time, but I enjoy it. Nuclear medicine has been a lifetime interest, so it’s hard to let it go completely!”
Congratulations go to Bill on this fantastic achievement and for his lifetime contributions to nuclear medicine.

The community heart failure team at the Trust have received a generous donation as a sign of gratitude for the care they delivered to a family’s late mother.
The community heart failure team endeavour to improve heart failure patients' quality of life, reduce their hospital admissions and support each patient throughout their journey living with heart failure from diagnosis to end of life.
They provide a seven-day service with home assessments, intravenous medication within the home and 12 clinics across Sandwell and West Birmingham, this also includes a Saturday morning clinic for younger working patients.
Isobel Blake, Community Heart Failure Specialist Nurse, said: “Valerie Haywood was a well-known patient to the heart failure team since 2014, before she sadly passed away in October 2022.
“At Valerie’s funeral, her friends and family requested that that any donations were to be
made to the Sandwell community heart failure team, to enable us to purchase equipment that would enhance the delivery of patient care and be useful for the staff.
“We are extremely grateful for the very generous donation of KardiaMobile devices - they can record a heart tracing to determine the heart rhythm. Every team member had one a few years ago, they proved very useful in determining heart rhythms and aiding quick treatment plans. Unfortunately, they were not replaced after damage through wear and tear.
“Currently we’ve been using a portable ECG machine or send patients into hospital to get an ECG. However, the new devices will be used in patients’ homes to help determine treatment options, avoid hospital admissions, and offer peace of mind.
“The devices will help over 1,500 patients a year and give staff the ability to make quicker, more informed decisions about treatment and find cause for deterioration – saving time.
“We are so touched by the Haywood family’s appreciation for the care that Valerie received from our team.”
Valerie’s daughter Joy Haywood has worked for the Trust for 42 years and continues to work as a bank nurse despite retiring five years ago. She said: “We decided to not have flowers at my mum’s funeral, and instead request donations to be made for the heart failure team.
“The family wanted to do something in her memory that would benefit patients and staff. We managed to buy three KardiaMobile six-lead devices and carrying cases. The whole family are thankful to the heart failure team who made Val’s life easier. She wouldn’t have lived as long without them, and some of them have become like family.”
The Care Navigation Centre (CNC) provides a single point of access for care professionals, carers and patients to arrange the right care for urgent and non-urgent referrals.

The CNC is based on the “no wrong door” ethos to facilitate and provide access to same day emergency care (medical and surgical), hots clinics, ambulatory care pathways, urgent community response, admission avoidance, community pathways, neighbourhood teams, virtual wards and third sector support.
It ensures that patients with scheduled and unscheduled care needs are streamed and navigated to the most appropriate pathway without delay.
Patients are assessed to access care that meets their needs in the first instance, by the appropriate team.
The team work together to provide the
appropriate assessment and care in collaboration with partners involved with the patient across the pathway.
As a multidisciplinary hub, the CNC ensure that urgent referrals and calls are dealt with by a triaging clinician - direct professional to professional contact.
Non-urgent referrals and calls are taken by an administrator who follows the correct triage
algorithms. They can transfer to a triaging clinician for further input and advice.
The CNC is a key resource for patients and professionals to co-ordinate the care for our population and ensure they receive the right care at the right time, in the right place, with the right professional; this is supported by a comprehensive model of community care which proactively supports patients in the community.
GP colleagues will only need to ring one number to refer to the Urgent Community Response (UCR), Connected Palliative Care Hub, Virtual Ward and Care Homes Team. The CNC also covers community services such as foot health, MSK physiotherapy, iCares, district nurse message taking, wheelchairs, continence, community respiratory and the heart failure service.
If a patient does not require 999 call but is in need of urgent care call, our CNC will support to get the patient seen by the right team.
The CNC can be contacted on 0121 507 2664, seven days a week, between 8am and 8pm.
Dr Pete Davies and Nadine Monk, from the department of diabetes and endocrinology, have published a book to mark 100 years since the discovery of insulin. The book highlights the lives of local people with type 1 diabetes, whose lived experiences span over 70 years.
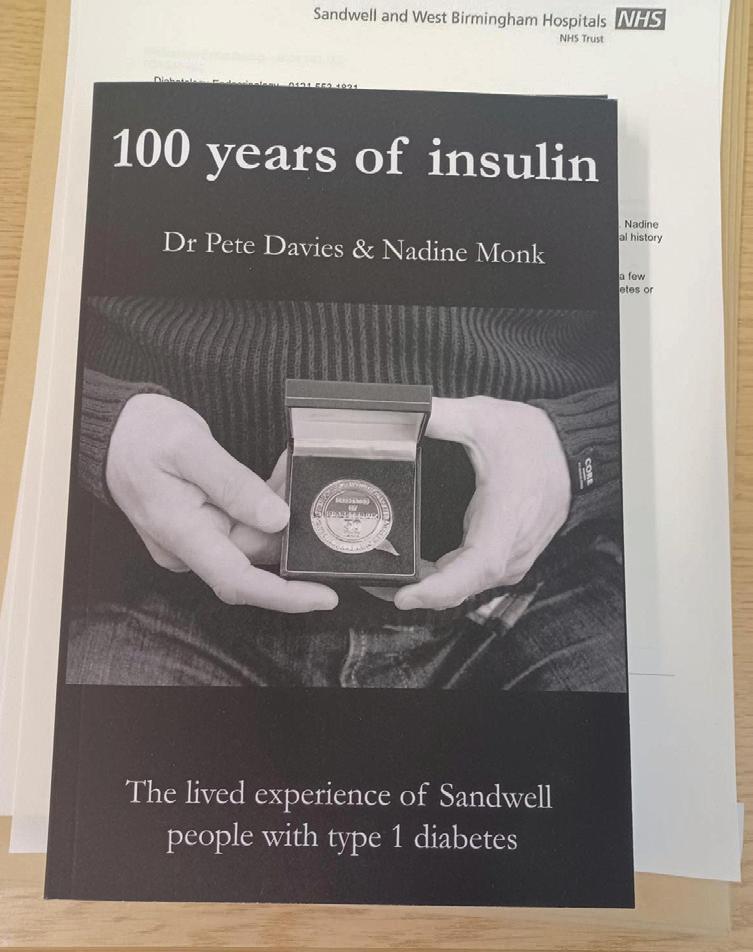
Before the discovery of insulin, people with type 1 diabetes had a very poor outlook. They could stay alive on a restricted diet for just a few uncomfortable months, at best a couple of years, before an inevitable death. Back then, there was little hope for those diagnosed with the condition.
The discovery of insulin changed everything. It meant that people with type 1 diabetes would be able to live long and fulfilling lives. The first patient was treated with insulin in Canada in 1922.
The book tells the stories of five local people who have lived with type 1 diabetes for between 38 to 74 years. Pete and Nadine collaborated with the West Bromwich History Society, who recorded participants' life stories, which will now form an oral history archive hosted by the Sandwell Library Service.
One of the patients featured is Annie, who was diagnosed with type 1 diabetes in
1948 when she was 16 years old. She recalled memories of her mother, who also lived with type 1 diabetes, and her family’s struggles to be able to pay for insulin at a time before the NHS. Annie told how a kind-hearted neighbour highlighted her unexplained weight loss and began her journey to diagnosis, treatment and better health. David, a retired teacher, shared memories of his
childhood growing up on a Shropshire farm, living a very healthy life before developing type 1 diabetes when he was aged seven. At the time, he recalled being asked to manage the diabetes with diet, with a significant delay before he finally met a specialist who recognised that insulin was required, firstly being injected by a nurse and eventually being asked to do it himself after practicing on an orange.
A theme emerges from the patient stories: that modern use of simple glucose-monitoring technology has been revolutionary, making it safer and easier to live with type 1 diabetes in the last few years. This became universally available via NHS funding in spring 2022.
These stories highlight the incredible resilience of people with type 1 diabetes and the progress that has been made in diabetes care over the last 100 years. Thanks to the discovery of insulin, people with type 1 diabetes can now live long and healthy lives. 100 Years of Insulin is available via Amazon.
Pete said: “The outlook of the Trust’s Diabetes Care team is to support people with diabetes and to help them access all available treatments, based on their individual needs and preferences. Most of all we strive that everyone can live well with diabetes and we look to learn from their experiences.”
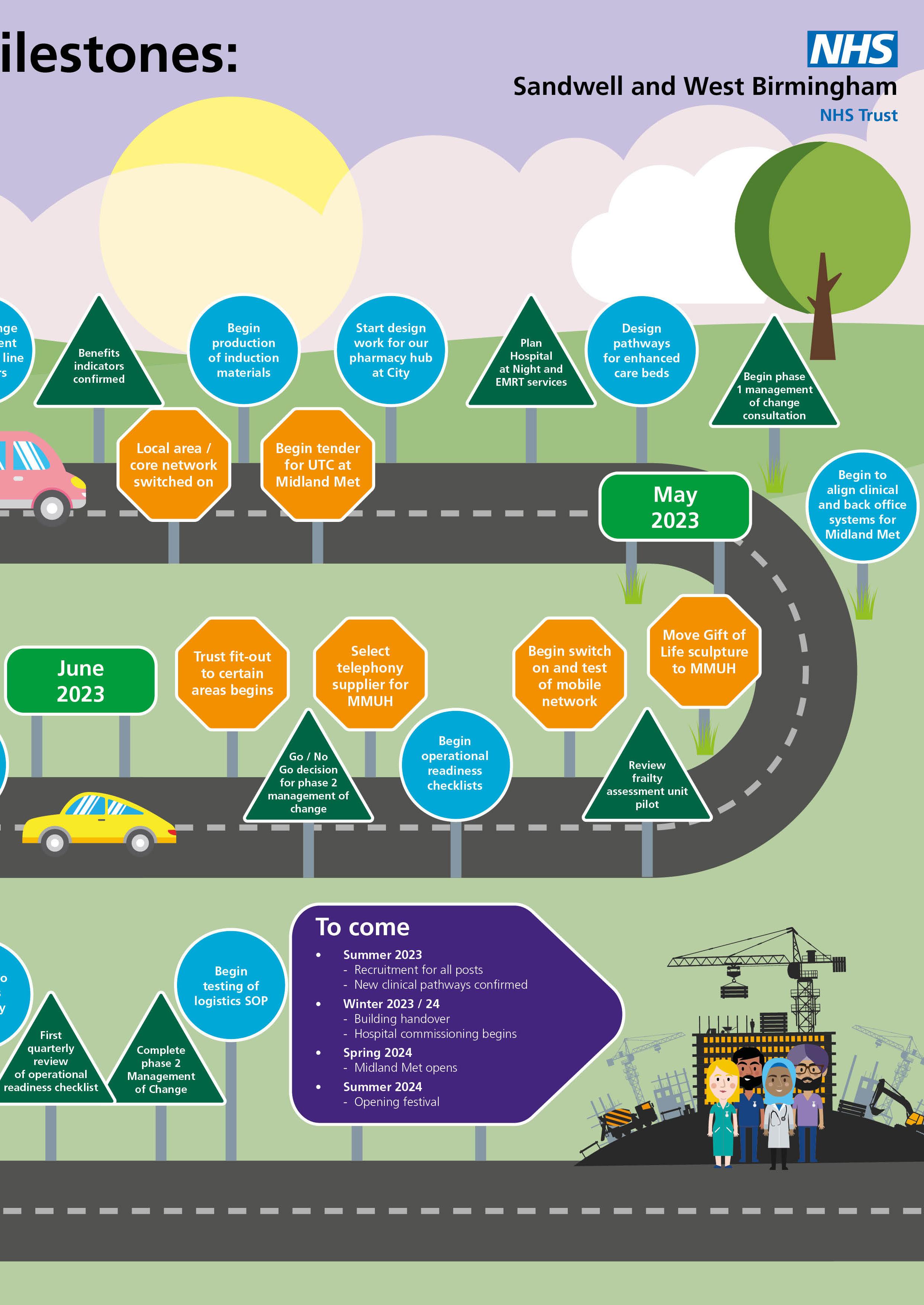
Do you have a clinical question about Midland Met? Well, now you can put it to the experts thanks to the launch of the Midland Met Clinical Reference Group (CRG).
Chaired by Dr Sarb Clare, Consultant and Deputy Medical Director, the group includes senior clinicians and experts who will provide recommendations on topics including, but not limited to, service specification, clinical pathways, policies, innovation and quality.
The forum meets twice a month and includes members such as our clinical safety officer, deputy chief nurse and a community clinician. These colleagues bring their knowledge and expertise to the group and will help us shape the clinical decisions we need to make before moving into Midland Met.
So, how does it work? If you have an issue, escalate it via your Midland Met workstream leadership team. In your request, you will need to outline these key areas:
• What issue/s needs resolving and why?
• Which internal experts/stakeholders and external bodies have been approached and their responses?
• Options appraisal, risk assessment and preferred option.
Importantly all requests should be evidencebased and provide as much detail as possible to support the submission. Once reviewed, a final decision is shared. The CRG will not review any requests again unless there is a significant change in clinical evidence.
All completed forms should be returned to sclare@nhs.net


Being a good neighbour is a priority for the Trust, as we work towards the opening of the new hospital in spring 2024. Over the past few weeks, our Head of Public and Community Engagement, Jayne Salter-Scott has been busy promoting a series of meetings for people who live within a mile of Midland Met.

Three events were held, with a total of over 120 attendees from the local community surrounding the new hospital. Chief Executive, Richard Beeken shared the
history and latest updates relating to the new hospital and Rachel Barlow, Managing Director for the Midland Met Programme Company, talked about the clinical model and how Midland Met is a catalyst for regeneration.

Many questions and comments were put to the Trust representatives during the meetings, ranging from concern over parking on nearby streets when Midland Met opens, to job opportunities and community access to the public spaces both in and outside of the building.
We have committed to continued engagement with local residents and business owners and our next engagement session will be themed around traffic, transport and parking, where we will invite partners including local transport providers to join us.
As well as concerns about the effect the building will have on nearby streets, it was clear that there was significant interest and enthusiasm from local neighbours who are looking forward to the hospital being open and operational.

Cancer services has been awarded funding for a new smartphone app for patients which will provide free tailored information at their fingertips.
The MySunrise app has been developed to support people from the moment of their diagnosis all the way through their treatment pathway, and is expected to support thousands of people across Sandwell and West Birmingham. The Trust sees 300 new patients a year diagnosed with cancer and this app will be accessible to those who wish to use it.

It’s expected to be launched this summer and content is currently being gathered for it by the cancer services team.

Jenny Donovan, Cancer Services Manager, said: “This app will be a fantastic support for our patients, allowing them to access information they need at the press of a button.
“Content will include information about the different cancers we treat here, what public transport to catch, where to go for appointments, videos explaining how pathways work in a patient-friendly way and patient stories, amongst other things.
“If there are any developments in the service, we will be able to share these, as well as information about Midland Met and what patients can expect if they are being treated at the new hospital site.”
Funding for the development of the app has been secured through the West Midlands Cancer Alliance.
“We’re hoping that it will make a big
difference to the journey of a cancer patient,” added Jenny. “It’s being used at other NHS trusts across the country and the feedback has been excellent.
“Traditionally, we have spent a lot of time, energy and money getting information to patients through leaflets.
"Now, we can keep all of that information up to date in one place, patients can access it at their own convenience and it directs them to reliable local advice and support."
The initial version of the app was first launched in Cornwall and has been used by thousands of cancer patients receiving treatment.

EQUANS has the mission to connect, power & protect - empowering businesses and communities to not only fully embrace the energy transition, but also the digital & industrial transitions that are redesigning the way we move, work and live.
Acting on our commitment to Net Zero by helping our clients to reduce the amount of carbon that is produced across the NHS Estate.
Cancer patients attended a beauty workshop to rebuild their confidence and meet other women facing similar battles.
People undergoing treatment for cancer at the Trust were pampered during the sessions and given make-up tips and tricks. They were also invited to sign up for free online workshops, which offer advice on self-care, including skincare, make-up and building body confidence.

Cancer patient, Sarah Brown, said: “It’s been a great afternoon meeting other people going through similar things to me.
“I picked up some really good tips from Sally whilst she taught us how to apply makeup, which has boosted my confidence and we also got a goodie bag filled with beauty products to take home with us.”
Cathy Zaidi-Crosse, Living with and Beyond
Cancer Nurse Facilitator, explained: “We are
always proactively finding ways to support our cancer patients in holistic ways.
“It’s a privilege to be working with Look Good Feel Better again since the face-to-face workshops stopped due to the COVID-19 pandemic. We have been up and running since autumn 2022 to offer patients a feelgood pamper day.
“We always get a fantastic response from everyone participating and I hope going forward, more patients will get involved and to experience the benefits of the sessions.”
Sally Basketfield, Lead Volunteer with Look Good Feel Better, added: “This is an amazing charity that supports ladies and gentlemen with any type of cancer. It is the only cancer support charity offering support to women, men and young adults to combat the visible and emotional side-effects of their treatment.
“I have led on a few skincare and make-up workshops at the Trust where I teach people all aspects of skincare and makeup. The goal
is to help people combat the visible side effects of their cancer treatment from hair and eyebrow loss to brittle nails, body confidence and dry skin.
“I love running these sessions as they are so beneficial for the patients in many ways – they get a couple of hours where they can really make time for themselves and play with make-up. We have lots of laughs and great fun."
Meanwhile cancer patients were also invited to a health and wellbeing event where they learned more about the services they can access to support them. The session, held in West Bromwich Community Centre, included talks from Sandwell Council’s public health team and Stephanie Morris, a social prescriber working for Your Health Partnership GP practices.
The new building housing the Same Day Emergency Care (SDEC) unit has opened at Sandwell Hospital ahead of schedule.
The modular facility is adjacent to the existing A&E department and includes six bays, two triage rooms and a treatment room. Part of the design includes a comfortable and bright waiting room for patients.
Feedback for the new building, which
opened on 3 April at the West Bromwich site, has been positive so far, as Kiran Jassal, Unit Manager, explained: “Patients have said how much brighter the space is and they have found it really comfortable.

“We want to ensure they receive the best care possible. No one likes coming into hospital, but this new facility helps to make the experience better as they are in nicer, newer surroundings.”
She added: “SDEC aims to provide the right care, in the right place and at the right time for our patients. This is a benefit to our patients as they are assessed, diagnosed and start treatment on the same day,
improving patient experience and reducing hospital admissions.
“Colleagues are also really pleased with the new space. It’s much larger than our previous base which was set within the chest clinic.”
SDEC was previously known as AMAA, and provides rapid assessment, diagnosis and treatment for patients without the need to stay on a hospital ward. And if clinically safe to do so, they will go home the same day their care is provided.
Access to the new single storey building is via an enclosed linkway from the A&E department and also from Little Lane.
Saving lives is at the heart of what we do at the NHS, and we're thrilled to introduce two exciting new projects from the deteriorating patient and resuscitation team that are set to revolutionise the way we tackle emergency situations.

First up is the Mindray D3 defibrillator, which is set to replace the Stryker LifePak 20 defibrillators commonly seen in use at our Trust. The Mindray D3 is a cutting-edge device that boasts the latest technology, ensuring patients receive the best possible care during a cardiac emergency. And the best part?
The Mindray D3 has a quick and easy user interface, making it easier than ever for our colleagues to respond to cardiac emergencies and ultimately save lives.
This means that Midland Metropolitan University Hospital will only have one type of defibrillator in all clinical areas. This is great news for our colleauges as it simplifies the process of using and maintaining the device,
which in turn saves valuable time and ensures that everyone can use the device confidently and efficiently.
The Mindray D3 defibrillator also has the ability to download case reports, which can be analysed and included in quality feedback of events. This allows us to continually improve our resuscitation efforts by identifying areas of success and areas for improvement. Additionally, the downloaded report can be added to the patient's notes, providing a comprehensive record of their care.
Our team is also introducing a system called ‘My Kit Check’ which provides peace of mind by monitoring the compliance of emergency equipment checks. My Kit Check ensures that all equipment is checked, maintained, and up-todate, allowing for a seamless workflow and the assurance that emergencies can be responded to quickly and effectively with the knowledge that lifesaving kit is ready and waiting nearby.
We're proud to say that these projects not only improve patient outcomes but also make life easier for our hardworking staff. Positive human factors have been taken into consideration, including the simplified user interface of the
We're excited to roll out these projects in phases, starting with the cardiac catheter laboratory and gradually moving to more acute areas and eventually all remaining clinical areas that will move into MMUH. And rest assured, training will be provided by Mindray, with key personnel trained within each area to further cascade train. Training will also be included during our extensive life support courses and induction programmes.
We encourage all of our staff to take the opportunity to familiarise themselves with these new systems as they are implemented throughout the hospital. With the Mindray D3 and My Kit Check on our side, the future of emergency response and resuscitation efforts is looking brighter than ever before.
When it comes to labour, we know babies don’t wait and so it’s important to be able to communicate with women quickly, no matter what language they speak.
As a result, we have now 10 “interpreters on wheels” – offering on the spot translations for women coming into our maternity department.
Statistics show that over the last 12 months, nearly a quarter of women who have
birthed at our Trust needed an interpreter. Afrah Muflihi, Equality, Diversity and Inclusion Midwife, explains: “The interpreters on wheels offer on the spot translations for women coming into our maternity department. Babies don’t wait and when a woman’s in labour we need to be able to have an interpreter on hand for her when she needs it.
“The devices feature the top 20 languages that are used in Sandwell and West Birmingham for our patients. We have 10 devices to be used within the whole of the inpatient and neonatal unit areas.

“And we hope that this will bring a good
experience, not only for our patients but also for our workforce in ensuring they’re able to communicate effectively and properly with our patients. Making sure they all have full choice and are partners in decision making.”
Maternity colleagues will continue to access the pre-booked interpreting services via the inhouse system that the Trust has.
Afrah added: “What this does is ensure we can communicate with women who we have not pre-booked the inhouse service for. We are the first in the Black Country to use the devices within our whole inpatient service and we will continue to monitor and evaluate the effectiveness of them.”
But the goodwill doesn’t stop there; Ellie and family have also made kind donations to the nurses who were a huge part of their journey. She continued: “We started creating packs including notebooks and stationery for the amazing staff to show our gratitude.
“The care given by the whole team, particularly Stacey Shaw, who gave Haris his first ever bottle on the neonatal unit, helped get us through such a challenging time. She has always supported us and is amazing at what she does.”

Stacey, Matron for the Neonatal Unit “I worked closely with Haris and his family as he was born premature, poorly and very tiny. But I always knew he was mighty.
“The family have always stayed in close contact with me. I have since moved hospitals and I’m elated that they have very kindly started supporting the staff, families and babies that I work with at City Hospital.
“We are very grateful for all the wonderful treats especially the premature specific colouring books for siblings, as we have never had anything like this before. Haris is a little boy on a big mission and has improved the neonatal journey for so many families every year."
A schoolboy who weighed less than a bag of sugar when he was born has designed colouring books for young patients and their siblings to use.
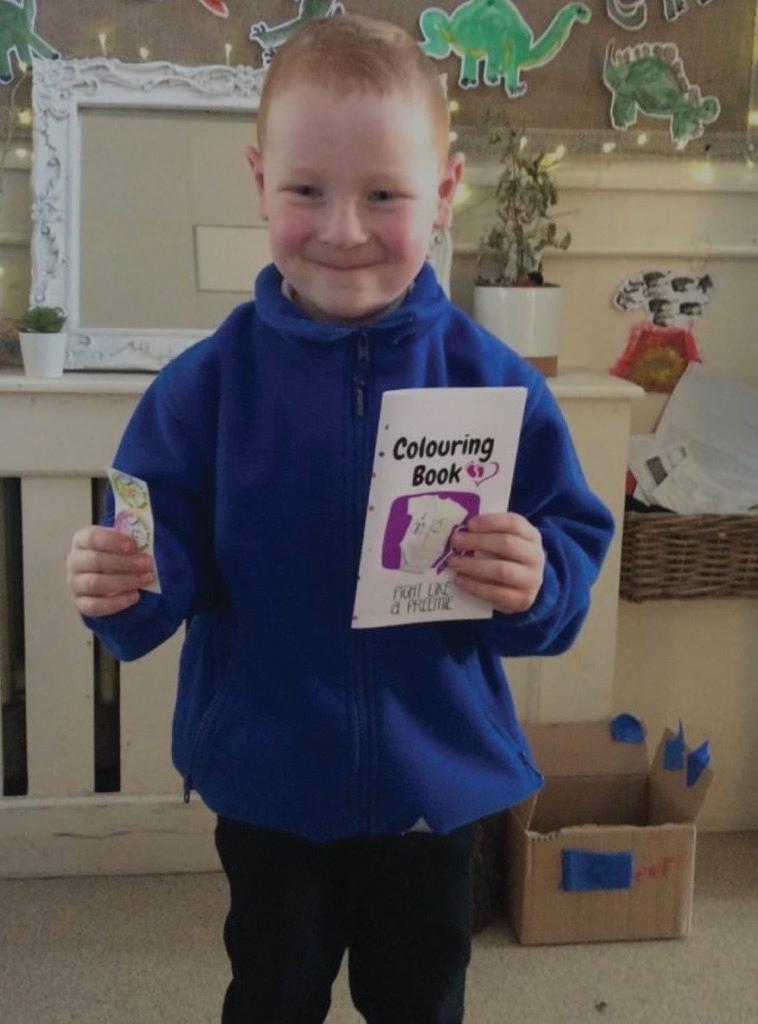
Haris Mockbill, who was delivered at 24 weeks and three days weighing 750g, has crafted the books with the help of his mum and donated them to the neonatal unit at City Hospital, where the nurse who cared for him now works.
The youngster, now aged four, spent 94 days on a neonatal unit. But he defied the odds and ever since his birth, mum Ellie Barr vowed to give back to the NHS.
She said: “It was such a difficult time for us as a family; we’d constantly be in and out of hospital. We experienced a very tough journey with lots of ups and downs.
“When Haris was discharged, we knew we wanted to give back to the NHS, which we have done every year since then. From raising money to creating new mummy bags and raffling prizes, we’ve made it our mission to help others.
“This year, I wanted to do something a little different, and now that Haris is older, I thought it would be a nice opportunity to involve him.
“He enjoys drawing, so we turned his illustrations into a colouring book for children – the idea being that it would give siblings of sick babies something to do in the hospital.
“Whilst we were visiting Haris in hospital, there wasn’t much to do for his older brother Elias, who was 19 months at the time.”
Dr Viresh Arora, ENT Consultant has recently been awarded a certificate of excellence for his outstanding work across the Sandwell borough.
Viresh has been recognised for this prestigious award by iWantGreatCare for achieving and maintaining 100 per cent positive feedback from his SWB patients. With over 60 reviews to date, Viresh is one of the leading consultants on the platform for SWB despite having only joined the organisation in November 2020 during the COVID-19 pandemic.
“I have always shown compassion and empathy to all of my patients, but I never anticipated getting such a recognition,” said Viresh.
“I prefer to see all of my patients after surgery, even on short notice, outside of my regular lists. In order to improve patient care and happiness, I always provide my patients my secretary's contact information in case they feel like they need assistance from me.”
Whilst some people review their hotels and holidays on Trip Advisor, millions of patients now give feedback and review their healthcare experiences. In fact, iWantGreatCare now shares over 6.1 million reviews making it one of the largest independent sources of patient feedback in the world.
Today, iWantGreatCare awards the certificate of excellence to those clinicians and practices who are most highly and consistently recommended by their patients with Viresh being one of those clinicians in the most recent cohort.
His hard work and dedication to his patients is unmatched by most.
“I work passionately, don't follow clock, even see patients at strange hours, when contacted through my secretary for their issues; I feel it’s my responsibility to give them with aftercare. I hold myself personally responsible for patient’s journey” said Viresh.
Viresh added: “I'm extremely grateful that my patients have expressed faith and trust in me, and I only hope that I can keep becoming better to help boost public confidence in the NHS, which continues providing all patients with the best possible service.”
Don’t just take our word for it – here is just a snippet of some of the fantastic feedback Viresh has received.
After the completion of a rhinoseptoplasty by Dr Arora, I must say I am over the moon with the results. The Dr made me feel so comfortable with the surgery and addressed clearly how the surgery is going to be. I can honestly say I am so pleased with the results I couldn’t recommend him enough. He has communicated with me throughout. Thank you for bringing a smile to my face, all my friends and family are thanking the doctor since he’s done such an amazing job. I feel like a totally new person, I can finally breathe and feel good about my nose. Once again, thank you Dr Arora you are the best!!!
I can't rate Mr Arora highly enough. I had a mastoid operation by him. The advice, support and professionalism I received from him both before the operation after care in my opinion was the highest quality. Mr Arora explained me detailed operative procedure thrice once in clinic, before the operation and during follow up and answered my queries with patience. He visited me 2-3 times after the operation. The procedure went better than I imagined, my recovery was quite smooth with well cared follow up. The hospital staff was very friendly.
I had surgery by Dr Arora, I would like to say Dr Arora was absolutely fantastic he explained everything step by step and that put my mind at ease, Dr Arora patient care and continuity of care was Excellent, I couldn't have asked for a better surgeon. Thank you so much for fixing my problem, and overall I'm very satisfied keep up the excellent work.
My 9yr old son had surgery in October 2022. Dr Arora was very patient and took time to explain the whole procedure, expectations and any possible difficulties that could arise during surgery. My son has multiple allergies which concerned me with the surgery but Mr Arora was diligent and showed great care. After the surgery on his rounds, he reassured my son who was upset due to pain and had a really nice tone when speaking to us both. He made me feel at ease and confident in his abilities. When we returned to post op appointment, again we were greeted warmly and discussed the outcome of surgery, which although more difficult than anticipated, went well and the expected result will be greatly improved. Thank you Mr Arora, you have a nice way with the children and their families. You are professional and caring and very talented.
Dear Heartbeat
Could you tell me why banks shifts that are worked on a weekend are not paid for two weeks? I have worked in other trusts and it has been paid the following week, with the way the economy is and the way people are struggling could you not look in to a way to speed up the process so people are not having to wait so long for payment.
Kind Regards
Yvonne Daly
Dear Yvonne,
Thanks for your question.
For bank shift payments, our week runs from Saturday to the following Friday at SWB, and as such we pay by a week ending on the Friday date.
If a colleague works a shift on a Saturday or Sunday, they are paid the following week. For example:

• Shifts worked Saturday 6 May or Sunday 7 May will be picked up on Monday 15 May and paid Friday 19 May.


• For bank payroll purposes, this would be week commencing 6 May and week ending 12 May.
This has been the case for a number of years. The main reason for this structure is that when going by Sunday as the end of the week, there were many bank workers who did not get weekend shifts verified. If payroll is run on a Monday morning, roster managers were not in over the weekend to verify the Saturday and Sunday hours and they would miss the deadline. The knock on effect of this is that it was then creating a lot of work for bank and rostering teams, as well as payroll, as advance payments were having to be raised. Therefore, an executive decision was made to change the week ending date to a Friday in order to give roster managers chance to ensure all bank shifts were signed off for Monday’s pay run.
Once again, thank you for the query and I hope this response clarifies the payment dates.
Kind regards,
Phil Andrew, HR Business Partner, and Veena Masih, Operations Manager
After 38 years at SWB, receptionist Indira Patel will be retiring from the Trust.


Many patients and colleagues alike know Indira as the face of the Birmingham Treatment Centre (BTC). She is often the first person you come into to contact with upon entering the treatment centre, however this wasn’t always the case.
Indira actually joined SWB in 1985 when City Hospital was known as Dudley Road Hospital. She started in the laundry; back in the 80s all laundry was done on site including the nurses uniforms. She would later progress to a supervisory role on the main reception desk in the BTC where she has been based for the last 17 years.
“One of my biggest challenges was moving on from supervising porters and domestic staff, to the role of a first point of contact receptionist on the BTC enquiries help desk, said Indira.
“Initially it was a big challenge having to meet and help people from all walks of life whether that be patients, visitors or staff. However, I soon became accustomed to it and really embraced my front of house role.”
She added: “Working at the BTC for over 15 years really allowed me to build my confidence and social skills as well as form some really special friendships which will last forever.”
Indira has had a positive influence on many of her colleagues both past and present at SWB, including Fay Williams, Senior Team Leader for
the outpatients department reception. She said: “Although Indira didn't work directly in my team, she was a great team player and helped out on a daily basis without being asked, which just goes to show what sort of a person she is. The team and myself will miss her greatly, along with many others.”
Jasbinder Poonia, one of Indira’s close work colleagues, has worked alongside her for the past 17 years and believes she will be missed.
She said: “Indira has been my best friend since
we have worked together and I, alongside many of our patients, will miss her so much.”
Balbir Kaur worked with Indira when she based in the laundry echoes these thoughts and said: “Indira was always a hard worker and good friend to everyone at the Trust and will be missed.”
As part of her retirement, Indira is planning on extended holidays abroad as well as spending quality time with her family, in particular her grandchildren.
Good look in the future Indira – happy retirement!
It's a welcome back this month as we say hello to Lydia Jones, the newest addition to our SWB family - yet a familiar face to many. As the Group Director of Operations for Primary Care, Community and Therapies (PCCT), Lydia brings with her extensive experience and a passion for quality and safety in healthcare.
Lydia is an allied health professional (AHP) by background with a proven track record of delivering excellent patient care. She returned to the Trust in January after 18 months away, and has been warmly welcomed back by her colleagues.
Since her return, Lydia has been working hard to meet as many teams as possible to understand their successes, challenges, and opportunities. This has enabled her to identify areas where she can offer support to improve both patient and staff experiences.

Lydia's immediate priorities are to develop and improve services for our patient population in outpatient, community and primary care settings. She is seeking to improve access, attendance and admission avoidance, early intervention and ease of navigation so patients get the right care first time, improved outcomes and patient experiences.
Lydia's expertise and knowledge will be invaluable to our Trust as we work together to deliver high-quality care to our patients. We are confident that she will make a real difference to our community.
In her previous role, Lydia was responsible for leading a diverse team of healthcare professionals as the director of therapies, ensuring good governance, supporting innovation and delivering best practice so that patients received the best possible care. She has a passion for listening to, coaching and developing colleagues to thrive in their roles delivering high quality services, which stems from her own career pathway having started out at SWB as a ‘cadet’ apprentice 21 years ago. With varied experience across healthcare settings, a good knowledge of the Trust and positive working relationships she has a strong foundation to make a difference.
One of the biggest changes since re-joining the trust is the emergence of the Integrated Care System and Place Based Partnerships, bringing even more opportunities to work collaboratively across organisation boundaries. Lydia recognises her role as a key contributor working alongside system colleagues in delivering the wider ‘place’ objectives and real
benefits to our SWB population under place leadership.
PCCT group is a diverse group with five directorates including ambulatory therapies, iCares (community services), iBeds (community bed & OPD and inpatient therapies), community medicine and primary care directorate. The group is ever growing as community settings develop and expand to ensure we provide as many services as possible, either in or close to our patients’ homes.
Lydia's return to the Trust is a great testament
to the positive working environment and the supportive culture that exists here. We are committed to creating an environment where our staff can thrive, and we are proud to welcome Lydia back.
Lydia is a keen gardener and enjoys the challenges of playing golf and learning to play the guitar in her free time.
If you see her around, please take a moment to introduce yourself and make her feel welcome. Welcome, Lydia!
Dr Anna Lock and Dr Santhana Kannan have both recently been appointed as deputy medical directors.
Anna joined the Trust over 13 years ago and she is well known across the Trust for her invaluable work within palliative care, as the first palliative medicine consultant at SWB.

“I am really pleased to be joining the medical director team as deputy director of integration and pathways. It is going to be a chance to collaborate with existing and new colleagues to improve models of care both within SWB and beyond, based on a compassionate organisational culture where we can be honest about our vulnerabilities and support others who are in less privileged positions” said Anna.
“I am eager to look further beyond classic health care models and at factors that influence health and its wider determinants more broadly, from birth through to death, to help us meet the challenges of our diverse aging population.”
She added: “I will be keeping my existing palliative care clinical role where I work with some amazing, motivated colleagues, both within connected palliative care and across specialties and disciplines as we work to improve the quality and consistency of palliative and end-of-life care for people wherever they are.”
Santhana joined the Trust in 2003 as a consultant in anaesthesia and intensive care.

“During my time at SWB, I have held various roles including divisional director in anaesthesia, intensive care and pain management, college tutor, medical appraisal lead, governance and mortality lead in intense care, and reviewer for anaesthesia clinical services accreditation” said Santhana.
“I am delighted to be appointed to this role
as I believe happy and proactive staff not only ensure patient safety and satisfaction, but also contribute to efficient working. This is what I hope to implement as a deputy medical director.”
He added: “In terms of other duties, my role will involve aiding staff to achieve their potential, support career development and Trust’s wellbeing agenda, as well as to aid the implementation of appraisal and revalidation processes.”

Last month I wrote about our progress so far since launching our five-year strategy and the work that has been taking place to agree our annual plan for this year.
This month I want to share what we will focus on in the annual plan which is expected to be signed off by the Board in May.
The annual plan is meant to be an outline of our commitments for the year that aligns with our strategic objectives and is easy to understand. We will face challenges within the organisation, whether that be responding to pressure on our services or externally when we have to meet national commitments. And we will deal with these challenges as they come but with the focus of staying on course on what we have agreed to deliver in the annual plan.
We have agreed 14 objectives that need to be delivered by April 2024. To achieve this, we have identified the key projects which will help us to achieve those 14 objectives and indeed, 6 of the 14 which we will in particular, prioritise and which will have the biggest impact.
Our key projects for 2023/24
Patients
• Harm free care and Patient Safety Incident Response Framework
• Communication
• Digital proficiency
• Elective activity (104 per cent of 2019/20) as per our production plan
• Financial plan including bank and agency reduction
• Patient journey including: integrated front door, care navigation centres and discharges before 1pm
• Improvement system development
People
• Leadership framework
• Population - management of change, recruitment and organisation development for MMUH
• Patients - support bank and agency reduction
Population
• Reduce bed occupancy: frailty same day emergency care (SDEC) and intervention team, medical SDEC, heart failure, frailty virtual wards, respiratory virtual wards, Walsall ED redirections, care homes admissions avoidance
• Urgent community response
• Health inequalities in type 1 diabetes and chronic respiratory conditions.
Patients 2023/24 Patient Annual Objectives
1 Increasing our reporting rate of incidents whilst decreasing the number with moderate harm or above.
2 Increase patients rating their experience as good or very good for all touchpoints including Friends & Family Test (FFT) by area
3 To reduce the maximum length of our waiting list in all specialities from 100 weeks to 65 weeks for Referral to Treatment standard
4 To increase patients who are seen and treated within the 4 hour emergency access standard from 73% to 76%
5 To increase cancer patients who are seen and treated within 62 days from 68% to 85%
6 To increase patients who have their diagnostic completed within 6 weeks of referral from 50% to 85%
7 To deliver our income and expenditure plan and improve our underlying deficit position from £46.9m to £40m
8 To increase elective activity from 94% to 104% of 2019/20 activity levels as per our production plan
9 To reduce our bank and agency spend from £64.4 million to £45.6 million
People
2023/24 People Annual Objectives
10 To improve staff experience from 60% to 70% (combined engagement score)
11 To develop 200 leaders in compassionate and inclusive leadership, restorative people management, and in safety and service innovation
Population
2023/24 Population Annual Objectives
12 To reduce the acute care occupied beds by 86 in line with our plans to fit into the new Midland Metropolitan Hospital.
13 To maintain that over 70% of patients are seen within the 2-hour urgent community response target, whilst increasing contacts per month from 1200 to 1500 per month.
14 To reduce health inequalities through targeted improvements for patients with type 1 diabetes and for patients with respiratory conditions. This will reduce type 1 attendances to Emergency Departments and unplanned admissions by 10% in identified early implementer primary care cohorts.
National Framework
Local target supporting Care Quality Commission
Local target supporting Care Quality Commission
NHS England operational planning guidance 2023/24
NHS England operational planning guidance 2023/24
NHS England operational planning guidance 2023/24
NHS England operational planning guidance 2023/24
NHS England operational planning guidance 2023/24 – ‘achieve a break even position’ locally agreed target
NHS England operational planning guidance 2023/24
NHS England operational planning guidance 2023/24 – locally agreed target
National Framework
Care Quality Commission, National NHS staff survey
Local target supporting Care Quality Commission, National NHS staff survey
National Framework
Local target
NHS England operational planning guidance 2023/24
Supports Core20plus5 in NHS England operational planning guidance 2023/24
For the first time, in setting these objectives for the year means we support you to prioritise the objectives that will have the biggest impact. However, as mentioned before we also need to be flexible when we have to work on new initiatives that are not necessarily part of the plan. We just need to consider whether any new initiatives are must dos or whether they help us to achieve our long term objectives faster or more easily. If they are either mandated or deemed as an accelerant, we will add them, deprioritising to create capacity where appropriate.
Our 14 objectives – our high impact objectives are in bold
“We want to do as much as we can to encourage our young patients, and any siblings they may have, to seek, find, and learn through play. These funded activities are also particularly beneficial for young patients with physical and sensory disabilities, where they can play and forget about their treatment.”
Mr Wallis added: “As a financial service mutual for teachers, doctors and dentists, it is very important for us to support the things that matter most to our customers and supporting the “We Are Metropolitan” campaign is a fantastic example.”
@SWBHCharity To donate to the Your Trust Charity text
“SWBH16 £5” to 70070
When Midland Met opens, our youngest patients are set to benefit thanks to a generous donation from the Wesleyan Foundation.
A generous donation of £35,000 will boost the children’s area in our new acute hospital currently under construction in Smethwick. The Wesleyan Foundation gifted the money to Your Trust Charity.

The money supports our “We Are Metropolitan” fundraising campaign which seeks to raise £2million towards added value activities for the new hospital. These include projects such as new community spaces and enhancing research and development. It will fund a play unit and interactive artwork in the children’s ward at the Midland Met.
Dr Nick Makwana, Consultant Paediatrician, said: “This fantastic generosity from the Wesleyan Foundation will help us provide an even greater level of care for our children and young people. The money will be used to create a home corner play unit and an interactive artwork display within our children’s ward.
Nathan Wallis, Chief of Staff at Wesleyan, said: “We are very pleased to be supporting Your Trust Charity in creating a welcoming and healing environment for young patients at their new hospital. This will help the lives of so many children and young people in Sandwell and West Birmingham. Not only will they receive world class care, but their experience in the hospital will be greatly enhanced.”
Johnny Shah, Head of Your Trust Charity, added: “As ever we are grateful to all who fundraise for the charity. We remain on track to achieve our target for our We Are Metropolitan fundraising campaign. However, we still need local businesses and our community to help us get to £2 million by the time our hospital opens. To make the Midland Met more than a hospital, we must continue raising these much-needed funds.”
Don’t forget that Your Trust Charity lottery costs just £1 a month and anyone who works for the Trust can join. Payment is deducted from your wages each month. To take part email johnny.shah@nhs.net.