Quality Improvement Priorities
2:1 Model for Quality Improvement
As a hospice we strive to deliver outstanding care, by embedding continuous quality improvement methodology and implementing best practice.
To enable the hospice to provide a consistent approach to achieving Quality Improvement Priorities we have reviewed various quality improvement methodologies. The hospice has agreed to adopt the Plan, Do, Study, Act (PDSA) cycle as its recommended Quality Improvement (QI) methodology.
A Quality Improvement “Plan, Do, Study, Act (PDSA) template for staff to use when completing quality improvement projects has been created. Thisallows the template to be applicable to a wide range of clinical and non-clinical quality improvement projects and also allows for continuous improvement.
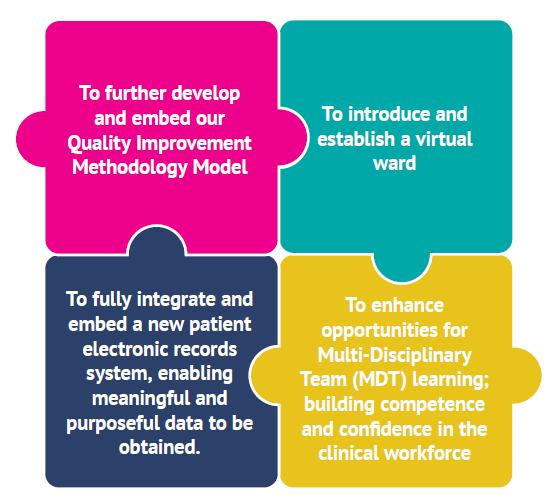
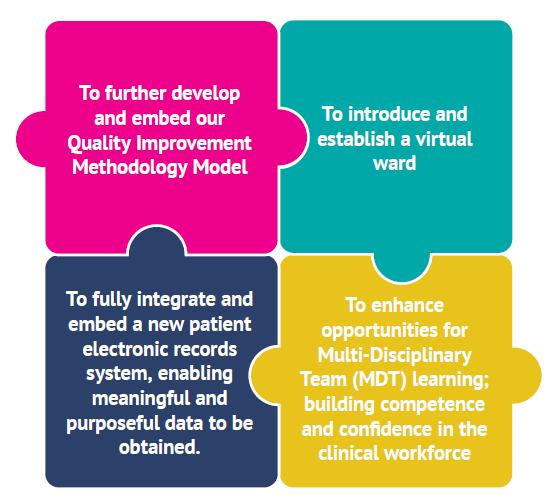
2:2 Quality Improvement Priorities for 2023-2024
8 / Quality Accounts 2022-2023 / Part Two
‘It’s like we have a big blanket around us. They have been amazing. They are like the hub arranging all the care.’ Relative of a patient
1. To further develop and embed our Quality Improvement Methodology Model
Why?
• To ensure there is a constant focus across the organisation on enhancing the quality and safety of care.
• We recognise the need for a hospice-wide approach to quality improvement and a clear methodology applied across the board.
• The Model for Improvement methodology, using the “Plan, Do, Study, Act” (PDSA) process was approved in 2022-23. This now needs to be implemented.
• As an organisation we are committed to a culture of quality improvement to deliver outstanding care.
How?
• Complete, as a minimum, two Quality Improvement Projects using the Quality Improvement “Plan, Do, Study Act” (PDSA) template during the 2023-24 financial year.
• Develop a Quality Improvement Methodology group, where Quality Improvement Projects will be discussed openly, monitored and evaluated.
• Working as a multi-disciplinary team, we will promote awareness of quality improvement methodology.
• Quality Improvement Projects will have an identified lead who will be facilitated to support them with the completion of the template and the project.
• Deliver a Quality Improvement event where staff can share experiences of being involved in a Quality Improvement Project to promote learning.
• Evaluate the Quality Improvement “Plan, Do, Study, Act” (PDSA) template following feedback from staff using the tool.

9 / Quality Accounts 2022-2023 / Part Two
2. To introduce and establish a virtual ward
Why?
• We have seen longer hospice Inpatient Unit (IPU) admissions, which reduces capacity and responsiveness for urgent admission.
• To enable an enhanced level of support for patients.
• To enhance care delivery through meeting individualised care and patient choice.
• The hospice is committed to reach more people at the end of life and improving access.

• There is a national drive to create the virtual wards model of care.
• To create suitable step-down options for patients, which may increase availability of specialist palliative care beds for patients.
How?
Use of the Quality Improvement (Plan, Do, Study, Act) template to enable outcomes to be monitored and the QIP to be evaluated.
• Establish a virtual ward steering group to provide governance, planning, monitor and scrutiny.
• Develop a plan of implementation.
• Use a culture of reflective learning with staff and service users to evaluate the project.
10 / Quality Accounts 2022-2023 / Part Two
‘My association with the hospice has given me confidence, social contact and some wonderful friendships.’ Patient
3. To fully integrate and embed a new patient electronic records system, enabling meaningful and purposeful data to be obtained.
Why?
The hospice implemented a new electronic patient record (EPR) database (SystmOne) on 13th March 2023, this needs to be embedded.
• To provide assurance to the board and external partners that agreed Key Performance Indicators (KPIs) and business objectives are being met.
• To ensure optimum use of the new electronic patient records (EPR) database.
• To maximise the potential of the IPU handheld devices, which have not been fully integrated but can provide a direct link with patient records using risk assessment, outcome measures, observations and the patient voice feedback.
• We need to be able to respond to patient and user feedback.
How?
• Produce data that is meaningful, timely and accurate.
• Continue a series of training sessions on the use of the modules within the SystmOne database.
• Develop resources and guides on the use of the different modules within the SystmOne database. Use SystmOne to share patient care information with system partners.
• Identify and agree a suite of reports which allow accurate activity reporting.
• Evaluate the implementation of SystmOne.
• Explore options for Electronic Prescribing and agree next steps.
4. To enhance opportunities for Multi-Disciplinary Team (MDT) learning; building competence and confidence in the clinical workforce.
Why?
• We have had feedback from carers to suggest that we could have adopted a more problemsolving approach when we have responded to complex patient issues. (Highlighted by Freedom to Speak Up Guardian incident and highlighted in patient documentation).
• We need to enhance skills in addressing complex patient scenarios where a variety of factors coincide, including manual handling challenges, behavioural and emotional issues, communication challenges, pain management and (often co-morbid) disease-related factors.
• With the correct knowledge and skills, clinical staff will be able to respond in a timely way rather than relying on a single discipline to identify solutions to changing patient situations.
How?
• Completion of the Quality Improvement (Plan, Do, Study, Act) template so that outcomes of an identified QI project can be monitored and evaluated.
• Adopting the four main principles of the Patient Safety Incident Response Framework (PSIRF):
1. compassionate engagement and involvement of those affected;
2. a system-based approach to learning;
3. considered and proportionate responses;
4. supportive oversight focused on strengthening response systems and improvement.
• Introducing new, responsive forums where clinical scenarios and / or incidents are proactively discussed.
11 / Quality Accounts 2022-2023 / Part Two
2:3 Feedback on Quality Improvement Priorities (QIPs) for 2022-2023
The following section describes the activity which has taken place through the reporting year to address the QIPs.
1. To review and improve our current offer and practice in regard to Advance Care Planning (ACP)
Through a user involvement group of patient and carers the ACP section of the hospice website is being configurated to include four downloadable nationally recognised ACP tools for people to use.
In the reporting year there has been 404 patients who have had a Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) form created within the patient electronic records, this is 20 more patients compared to 2021-2022. A culture of reflective learning has been created through Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) Quality Assurance Forums (QAF). Extending membership has demonstrated more shared learning in collaboration with our external partners.
Staff identified there was a training need required through self-reflections and practice. From April 2023, as part of the Registered Nurse (RN) mandatory clinical skills days, sessions will focus on having difficult conversations and introducing ACP to patients and carers.
The hospice now has a corneal donation leaflet available for patients and carers. Teaching sessions have been delivered to increase confidence in introducing donation with patients. Between January 23 and March 23 there has been at least one corneal donation at the hospice.
2. To amplify the patient/family voice in planning and delivery
Following the first quarterly VOICES (Views of Informal Carers Evaluation of Services) feedback session it was acknowledged that the format did not achieve good engagement with clinical teams. As a response, further review of how to demonstrate learning and changes in practice following feedback is being led by the Associate Director for Clinical Services.
An additional Social Worker has joined the patient and family support team, with a focus to identify and address carer needs.
A Patient and Family Engagement Officer role was put on hold within the reporting year. The hospice aims to recruit to this role in 2023-2024 if grant funding can be sourced.

3. To improve reach of, and access to, hospice care ensuring equity in relation to diagnosis, location and demographics
GP surgeries were invited to feed back on specific end of life activity for bespoke reporting. Only 50% replied but this has been superseded by an Integrated Care Board (ICB) wide commissioned report. The population report was received at end of the reporting year and will be reviewed at the beginning of 2023-24.
The hospice took part in the National Equitable Care for all Ethnicities at the end-of-life audit led by Kings College Hospital, London. The findings of the audit were published at the end of the reporting year but will be shared with the wider team at the beginning of 2023-24.
Spot audits to capture compliance of recording demographics were undertaken and a training presentation created with the EDI (equality, diversity and inclusion) lead for the hospice. The process was reviewed as part of moving to a new electronic patient records (EPR) system in March 2023. A plan is in place to reintroduce spot audits in the next reporting year.
The hospice contributes to local oversight of enhanced health in care homes development. Referrals are accepted for all kinds of care and nursing homes based on need.
A task and finish multi-disciplinary meeting was set up to review non-accepted admissions. This led to a new ‘Nurseline (the hospice’s telephone support service) only’ mini assessment to increase the hospice reach with a proportionate and effective response.
4. To improve use of digital health approaches
IT Competencies were created by the Digital Health Lead in their first year in the role. At the end of the reporting year over 50% of the clinical workforce had completed their IT competencies since the roll out in August 2022.
The hospice migrated over to a new electronic patient record (EPR) system in mid-March. Staff across all clinical areas were trained prior to the go live date.
NHS digital Smartcards were issued to relevant clinical staff prior to migrating over to the new EPR system.
All patient rooms on the Inpatient Unit (IPU) now have access to a handheld digital device, ensuring risk assessments, evaluations and reviews are now carried out within close proximity of the patient.
Staff have embraced the use of digital platforms to continue to enhance the care the hospice provides to our patients and carers.
The hospice now has a direct email for community patients and carers. The purpose of the email is for non-urgent advice and requests to the community team.
Funding has been secured to purchase visual reality (VR) headsets. A task and finish working group will be created in reporting year 23-24 where the new Quality Improvement methodology template will be used to ensure patient safety and appropriateness for VR headset use.
The hospice has started to look at a digital patient app to monitor patient outcomes within the new EPR.
13 / Quality Accounts 2022-2023 / Part Two
Quality Performance Overview for 2022-2023
3.1 Review of Services Inpatient Services
Our Inpatient Unit (IPU) continued to provide end of life care to the patients with the most complex needs. We had 206 admissions within the reporting year, compared to 267 in the previous year.
Activity has been disrupted due to the challenge of recruiting to Registered Nurse (RN) roles on the IPU. We have responded by flexing the number of beds available to ensure we maintain safe staffing levels. We have held two external recruitment days and we received a positive response. As we go into the new reporting year we have seen an increase in recruiting.
The average length of stay has been 21 days, compared to 22 days in the previous year. We have maintained our medical consultant-led specialist palliative care beds, as well as our NHS continuing care healthcare-supported nurse-led beds. The hospice has seen an 83% bed occupancy across the IPU. 82% of the IPU admission ended with the death of the patient on the IPU, this is an increase compared to previous year.
For a three-month period up until 29th March 2023 some of the beds on IPU were used under the NHS Winter Pressure Scheme, which was a result of NHS England asking hospices across England to assist with severe bed capacity issues. This was co-ordinated by the Sussex Integrated Care System (NHS Sussex). A total of 61 bed days were provided to East Sussex patients. The care provided was of a level appropriate for nurse-led care. The hospice received excellent feedback from both patients and families.
The hospice multi-disciplinary team was flexible in the mix of use of beds, always ensuring adequate provision for admission of community patients with complex needs.
Community Services
Our community services have had a year of increased activity, with some new developments to the hospice’s service provision.
The hospice has supported 1,201 patients in community settings, including own home, care homes, outpatients, and virtual consultations, compared to 1,075 in the previous year. There were 6,319 face-to-face contacts in total over the reporting year.
The community team structure involves small teams established in clinical hubs which support primary care neighbourhood areas. Staff within the hubs have the responsibility to manage and review their caseloads. There has been a re-organisation of the hubs to improve effectiveness, A duty Register Nurse (RN) and Healthcare Assistant (HCA) are available from 7am-7pm seven days a week, this provides the team with the ability to respond to urgent patient need in a timely manner.
The hospice continues to show a strong response to urgent referrals achieving 93% within 24 hours of the referral received.
The hospice 24/7 Nurseline has continued to provide support to patients, families health and social care professionals. The hospice has handled 17,713 calls, compared to 19,027 in the previous year. Feedback demonstrated this remained a highly valued hospice support service.
‘The staff are wonderful, kind and compassionate. They are just great. They are very dedicated and never seem rushed. It is great to be able to phone Nurseline and get the advice we need. I can think of no improvement needed’.
14 / Quality Accounts 2022-2023 / Part Three
The hospice is taking part in a Hospice Line project. Working in collaboration with three other local hospices, this aims to integrate telephone advice and support services. A single integrated service would ensure that patients have the same level of access to advice and support regardless of where they live. This would give us the opportunity to improve the patient experience across all four hospices.
The hospice has seen the implementation of the Living Well Hub in October 2022. This is a service for patients and carers known to the hospice to access discussion with a Clinical Nurse Specialist (CNS), community links access and palliative rehabilitation, without the need for a referral or appointment. There has been a steady growth in attendance, and the hospice has received some positive feedback including:-

‘Meet people in similar situations’.
‘It’s helpful to myself and my husband to go out and meet others’.
The hospice has also seen the development of a ‘Nurseline only’ service prior to quarter four. Patients on this caseload are patients who have been referred to the hospice and triaged to receive telephone support only. At the end of the reporting year there were 62 patients on the caseload.
The hospice maintained a high level of attendance at primary care meetings in GP Surgeries. Our Community Support Volunteers (CSVs) continue to provide valuable befriending support to people in their own homes, an important component of the hospice’s range of services. In addition, we have now expanded our befriending services to our IPU. With our new IPU Companion role volunteers provide social support to our IPU patients. We have also launched several Bereavement Help Points across our catchment area, where CSVs are available to provide a listening ear and emotional support to anyone who has been affected by bereavement. Within the reporting year there have been 18 new CSVs. In total at the end of March 2023 there were 55 CSVs and 34 telephone befrienders.
Living Well
The Therapies Team has continued to support the development of our Living Well concept. Established groups, such as the Fatigue and Breathless Clinic, continue to have strong attendance and the hospice has developed extra physiotherapy-led gym groups as well as re-establishing Living Well Matters. This is an 8-week programme aimed at supporting new patients to orientate to hospice services. Each session is facilitated by a different member of the MDT each week. Over the course of the next year, the Therapies Team aims to continue their work on referral and assessment pathways for community patients as well as embed new groups (such as an Occupational Therapy clinics) and continue to support patients on IPU to access Living Well activities.
As part of the hospice community service the Therapies Team continue to work with patients in their own home. They support people to remain safe at home as their needs increase, assess for equipment and mobility needs and offer goal-orientated rehabilitation programmes. The hospice is also working more effectively with our partners in statutory services, ensuring that the right team is working with our patients at the right time. We are also collaborating with therapists from other services closely, including joint working in some cases, which is leading to timely therapies being made.
Community Links Network
Our Community Links Network has been running since 2019. It is a network of organisations across the hospice’s catchment areas who we share information about our services with and learn about groups and activities which may be beneficial to those we support.

During the reporting year our Community Links Network continued to grow to encompass over 90 local organisations. The network includes a diversity of organisations and groups serving particular populations such as ethnically diverse communities and refugees.
During the year we continued to run regular networking sessions for groups to share knowledge. We began to develop new initiatives in partnership with Community Links such as a monthly craft group at the hospice in collaboration with Hampden Park Shed. We also used the expertise of links to run training sessions for staff and volunteers, for example Vision Awareness Training.
In addition to the network, our Community Engagement team developed close links with our Equality, Diversity and Inclusion Lead to begin more focused work sharing our services with different groups and reaching out to the community through community engagement tours in different parts of our catchment area. The links network is now being proactively used as a resource to signpost patients to activities and support which may benefit them in their own community.
Patient & Family Support Services
This has been another good year for Patient and Family Support Services.
We continue to support almost 30% of all those under our care with counselling, including adults and children, pre- and post-bereavement. The Community Bereavement Service for those where their loved one died not under the care of the hospice, first established in response to the Covid19 crisis, is now firmly established. We continue to support those bereaved by sudden death such as suicide or road traffic accidents alongside those bereaved by anticipated death, including those bereaved under the hospice.
Likewise, the Seahorse Project continues to cater for children and young people both linked to the hospice and those from our local community. Our first ‘Seahorse Stroll’ has been particularly successful. This was an event run in parallel to a whole hospice fundraising event, the ‘Starlight Stroll’. It provided an opportunity for bereaved children and young people to come together, normalising their shared experience of grief.
The social workers continue to play a strong role in the areas of safeguarding and mental capacity alongside their core role. The year’s focus on how best to support carers lead to the decision to recruit a third full time social worker, in post from end of March 23. We look forward to this additional resource making a significant difference with regards to carer support going forward.
Counselling Services
Total number of individuals supported through counselling services, across all strands (pre- and post-bereavement, children and adults, community and hospice) increased from 656 to 680.
Pre-bereavement referrals for adults (IPU and community) have increased, from 311 to 476. Post-bereavement referrals (hospice bereavement service and community bereavement service combined) have also increased, from 313 to 357. Seahorse has seen slightly fewer referrals this year, 96 compared to 110 previously.
In summary, across all strands of Counselling Services, we have delivered fewer counselling sessions, 2,886 compared to 3,009, but supported more people in this reporting year. This is in line with our increasing focus on time-limited, targeted rather than long-term counselling support (the right support at the right time). Overall, Counselling Services have continued to support 29% of those under the hospice’s care.
Social work
Social workers have provided a total of 1,098 sessions for patients and their families, including phone calls and face-to-face sessions. Unlike counselling sessions these may have been contacts of a few minutes’ length or visits over two hours or more. Those 1,098 sessions were equivalent to 345 one-hour sessions. 133 referrals came from the Community Team, 38 from IPU.
17 / Quality Accounts 2022-2023 / Part Three
Learning & Development
It has been a busy and productive year for Learning & Development. During COVID we delivered a reduced programme of training, and this reporting year we have been able to deliver a full suite of courses, refreshers, and workshops for staff, and in particular a welcome return to face-to-face sessions.
We have delivered a new programme of Clinical Skills Days that enabled us to offer new learning, and specialised education and training to Clinical Nurse Specialists (CNS), Registered Nurses (RNs), Healthcare Assistants (HCAs) and Care Assistants. Alongside these days we have delivered practical Manual Handling workshops and Resuscitation sessions. Further training days have been delivered on Lone Working and Conflict Resolution. Safeguarding training has involved face-to-face reflective sessions for both the community and the inpatient staff. There has been a rollout of a Digital Competency training framework, and this has proved valuable in light of training staff in the use of a new EPR system.
Statutory and Mandatory training modules have been delivered online, and through our Learning Management system (LMS) we have enhanced provision with the addition of training in the use of medical gases. Space has been made available to set up a simulation room for the clinical staff to train and practise their practical skills, and this has become a valuable resource. Our library has been re-purposed as a Learning Resource Hub. Therefore, as well as books, it is now able to deliver small group learning and engagement, complementing our online Learning Hub where training materials and resources are available for staff use.
The ECHO (Extension for Community Healthcare Outcomes) programme delivered with the Sussex Hospice Collaborative provided an external training programme for care homes, delivered via tele mentoring and video, and the pilot has now ended. It has been delivered to seven cohorts of staff (knowledge networks) throughout the programme. These are now communities of practice.
Several staff have completed university modules in the past year, including Advanced Physical Assessment and Non-Medical Prescribing. Internally, staff continue to work on competency frameworks; for our Care Assistants we have delivered The Care Certificate. We have hosted students from universities, and these have included pre-registration nurses, therapy students, paramedics and a social worker. We have also provided placements for Foundation year Doctors and trainee GPs.
3:2 Clinical Governance
During the reporting year the established clinical governance structure continued to ensure safety, effectiveness and evidence-based practice across clinical services.
The Deputy Director for Quality and Infection Prevention from the Integrated Care Board (ICB) joined the Clinical Governance Committee (CGC) as a co-optee. The Assistant Director of Nursing for the community NHS trust continued in her role as co-optee. The Associate Director for Clinical Services and a new trustee with a governance background has also joined the committee.
Safety metrics were scrutinised at the quarterly CGC meetings, which are chaired by a trustee, and report to the Board of Trustees.
A key focus at one meeting was the potential risks of workforce vacancies on the quality and safety of care. Included was potential impact of the ability of staff to comply with mandatory training due to staff shortages and absences. There was no identified correlation to suggest that the staffing shortages negatively impacted patient care.
Another focus was the positive impact of attending a leadership development programme for two clinical roles. Staff found the course to be extremely beneficial and influential in the way they now work, including having grown in confidence.
18 / Quality
Accounts 2022-2023 / Part Three
3:3 Risk Management
The hospice has a web-based accident, incident and near miss reporting system (Sentinel).
The Sentinel Reporting System is the sole reporting platform for all staff across the hospice, including retail.
A root cause analysis (RCA) template is built into the incident reporting database. The template is based on the ‘Yorkshire Contributory Framework’ and identifies key information and actions to prevent further incidents. Additional training on the completion of an RCA has taken place.
All patient risk assessments are accessible through the new EPR system. Notifications are set up within the EPR system to alert staff to complete and review risk assessments.
The majority of risk registers are held within the Sentinel reporting system. The reporting system enables the CEO and all members of the Leadership Team to have oversight of all currently active risks as well as their departmental risks. All active risks on the Quality and Safety risk register are discussed and reviewed at the Quality and Safety meetings as a standard agenda item.
The CEO and Registered Manager are automatically notified of any risk added to a risk register which has a high rating.
3:4 Care Quality Commission
St Wilfrid’s Hospice is registered with the Care Quality Commission (CQC) and is currently registered for the following regulated activity:
Treatment of disease, disorder or injury.
• The Associate Director for Quality and Governance has taken on the responsibility of the Registered Manager for the hospice following the promotion of the existing Registered Manager to CEO.
• The hospice has updated its Statement of Purpose describing:
- What we do
- Where we provide the service
- Who we provide the service to
• St Wilfrid’s Hospice’s current rating is outstanding. There have been no conditions attached to registration, or any special reviews or investigations that have impacted on our registration status during 2022-2023.
3:5 Data Protection and Security
The hospice places great importance on data protection and security and strives to be open, honest and transparent about how we process personal data in compliance with the Data Protection Act.
We submitted our annual NHS Digital Data Protection and Security Toolkit at the end of June 2022 with ‘standards exceeded.’ We also engaged an external auditor in January 2023 to undertake an initial toolkit ‘healthcheck’ of mandatory items against the 10 NHS data security standards. Work continues towards our 2023 submission with auditors due to complete the follow-up audit in May, ahead of the June deadline.
For any new initiatives involving the processing of personal data our staff complete a privacy impact assessment so that key elements of data security are taken into account and approved before proceeding.
This is the second year that data protection incidents have been logged on the online accident, incident and near miss reporting system. There were 49 data protection incidents logged in this
19 / Quality
Accounts 2022-2023 / Part Three
reporting year, slightly up on the previous year (44). The largest incident category (34%) were external scam/phishing attempts via email, phone or text. We continue to raise awareness of these through training and communications to staff.
The hospice has seen a range of human error incidents, another potential cause of data breaches, and there have been a number of low-risk incidents such as emails sent to the wrong person/group, items left on photocopiers, items posted to the wrong address. We continue to raise awareness of these through training, communications to staff and visible signage in rooms and on copiers to try and prevent/mitigate these risks.

With the retirement of the hospice’s CEO in December 2022 the new CEO has taken up the role of designated Senior Information Risk Owner (SIRO) responsible for information risk across the organisation. Their role is to ensure that systems, policies and procedures are in place to identify, control and manage risks associated with information.
In March 2023 we moved onto our new EPR system (SystmOne), enabling greater integration and data sharing capabilities across the wider healthcare community. Whilst all user access can be authenticated by a standard username/password combination, many clinicians also now have NHS smartcards having been through a thorough ID verification process. This smartcard access enables searches for information held against national NHS databases such as the SPINE/Summary Care Record (SCR). Patient demographics can be uploaded automatically to facilitate faster patient registration.
Patient data sharing with other healthcare organisations is welcomed to ensure that all those involved in a patient’s care can access up to date accurate information in the best interests of patient care and support. We gain patient consent for the sharing of data and, if patients do not wish to do so, their SystmOne record can be flagged to prevent sharing. In addition, we will also make patients aware that they can opt-out of their data being used for any secondary purposes using the National Data Opt-Out scheme offered by GP practices and the NHS.
‘The standard of care at the hospice is second to none,’ he told us.
‘All of the staff and the volunteers are amazing, even the cleaners. They’re like a big family and I love spending time chatting to them all.’ Patient
3:6 Participation in Clinical Audits Summary of Clinical Audits
To ensure the hospice is consistently providing a high-quality service and continually meeting standards, we have an audit timetable. The audit timetable is reviewed at the Clinical Effectiveness and People with Personal Experience (PPE) Group, this allows us to monitor the quality of service in a systematic way, identifying areas for Quality Improvement within our service.
Completed audits are presented to staff and volunteers at our Audit and PPE feedback presentations. Sessions are a hybrid of face-to-face and virtual to encourage more engagement from staff and volunteers. They provide opportunities for participants to have a greater awareness of the clinical audit process and to reflect on clinical practice. Also, the process supports identification of areas for further development and the evidence to support change in practice. This further demonstrates the hospice’s strong commitment to the QIPs, in particular ‘To further develop and embed our Quality Improvement Methodology Model’. Audits have been completed by a variety of patient facing and non-patient facing staff as illustrated below:-
Hospice UK General Medicines Audit
Annual Audit assessing the quality of medicines management.
Aim
The management of non-controlled medicines will meet the requirement of the Medicines Act (1968), Misuse of Drugs Regulations (2006) and the Health Act (2006).
Outcomes
• Overall compliance over 98%.
• Limited documentation of medications received on admission.
• Limited evidence of recording drug suitability.
• No clear documentation of patients being informed when medications are used ‘beyond licence’.
Changes in practice / next steps
• Post-migration to new EPR system, identify the most effective way of reconciling medicines to improve compliance.
• At safety huddles, MDTs and team meetings, reintroduce the completion of drug suitability documentation.
• Introduced a designated leaflet on ‘beyond license’ medicines for patients and carers.
• To continue to audit this area of practice annually.
Hospice UK Controlled Drugs Audit
Aim
The management of controlled drugs will meet the requirements of the Misuse of Drugs Regulations (2021) as amended on 16th August 2007, The Health Act (2006) and the Controlled Drugs (Supervision of Management and Use) Regulations (2006).
Outcomes
• Overall compliance over 95%
Changes in practice / next steps
• Documentation errors with CD register to be amended in line with policy guidance.
21 / Quality Accounts 2022-2023 /
Part Three
Medication Charts Audit
Aim
To look at all aspects of the medication charts and ensure we are compliant with the national guidance and St Wilfrid’s Hospice Medicines Management policy and procedure.
Outcomes
• Compliance over 95%.
• Duration times for steroids and antibiotics not always recorded.
• Allergies not always documented.
• Limited evidence of the completion of ‘effect box’.
Changes in practice / next steps
• Revised inductions with new staff across the MDT.
• Reported documentation errors and the outcomes fed back at team meetings, resulting in downward trend three months post audit.
• Clinical pharmacist provides training for new members of staff and meets with staff after significant errors.
• Re-audit six monthly.
Opioid Benchmarking Audit
Aim
To audit doses of opiates and sedatives administered to patients in the last 24 hours of life. Demonstrate appropriate opioid and sedative prescribing, as well as clear documentation and discussion with families and carers.
Outcomes
• Sample size x33 patients notes were reviewed.
• Data from four hospices were benchmarked.
• Reviewed medication charts to see the amount of medication given – opioids, midazolam, levomepromazine and haloperidol.
• The median doses of opioids, midazolam, and haloperidol were in keeping with other hospices, suggesting appropriate prescribing.
• Clear documentation explaining patients were dying (92%) and regarding use of syringe drivers (77%). These have been identified as areas that can be improved.
Changes in practice / next steps
• Look at how we can capture with more accurate documentation within the EPR system.
• Re-audit every 2 years.
CD Administration times against prescribed times
Aim
To ensure all CD medications are administered within one hour of the actual prescribed time.
Outcomes
• Sample size x7.
• Limitations of the audit: small sample size.
• Overall compliance: 100%.
Changes in practice / next steps
• Frequency of audit changed to six-monthly from bi-monthly due to increased compliance.
22 / Quality Accounts 2022-2023 / Part Three
Patients discharged from IPU on Steroids Audit
Aim
To ensure appropriate use and management of steroids in palliative care patients.
Outcomes
• Compliance increased with the number of patients being prescribed Proton Pump Inhibitors (PPI) when on steroids.
• Documented evidence that patients who were discharged on steroids had received the correct follow-on instructions communicated to the GP and care providers.
• Lack of evidence of which patients should receive an emergency adrenal crisis card on discharge.
Changes in practice / next steps
• Created an IPU checklist to ensure the correct procedure is followed on discharge.
• Patients discharged with a management plan for ongoing management.
• Process agreed for patients who are established on steroids to be given an emergency adrenal crisis card on discharge.
Review of Diabetes management on the IPU
Aim
• Retrospective audit looking at how patients with diabetes were managed on the IPU.
Outcome
• 19 patients were audited in total.
• All patients had diabetic medications prescribed appropriately on admission.
• Medications were adjusted depending on Capillary Blood Glucose (CBG), however target ranges were slightly different to the Diabetes UK algorithm.
• CBG readings were documented daily on CBG charts for 68.4% of patients (13/19). Of those who did not have readings documented five were not on diabetic medications on admission and one of the patients had insulin stopped on day one of admission.
• The pattern of glucose monitoring required was only documented for 2/19 patients in the designated space on their CBG chart.
• The instruction to check daily CBGs were documented in notes for 12 of 19 (63%) on initial assessment and an additional four did have CBG checked on admission on their CBG charts but not documented in notes.
• Two patients were found to be self-monitoring.
• Documentation of who performed the monitoring was not always clear.
• It was only documented that one of the two patients was self-adjusting insulin.
Changes in practice / next steps
• To document pattern of CBG monitoring e.g. BD, OD, QDS.
• Adjust CBG ranges and monitoring frequency based on the patient’s current condition.
• Standard to be set by the hospice for the CBG range once patient in terminal stage.
• Nursing and HCA staff should be mindful of the coding protocols for self-monitored vs nurse/ HCA monitored results.
• All staff to be aware that patients on hypoglycemic medication should have PRN treatment for hypoglycemia pre-charted.
23 / Quality Accounts 2022-2023 / Part Three
Completion of Risk Assessments
Aim
Baseline audit to identify the completion rate of risk assessments pre-implementation of handheld devices.
Outcomes
• Sample size x7.
• Documented evidence of over 90% of risk assessment completed on admission.
• Slighty reduced in the number of completed reviews of risk assessment during a patient admission despite change in patient need.
Changes in practice / next steps
• Re-audit, post mitigation to a new EPR system (March 2023), to identify if the compliance in the completion review on the handheld device has improved.
Hospice Criteria Referrals Audit
Aim
To identify if information on the referral form is fully completed and appropriately referred to the service to enable effective triaging of patients.
Outcomes
• Data gathered over a four-week period.
• Sample size x24 referrals for IPU or community services.
• Over 50% of the referrals received were incomplete.
• Identified referrals were not using the most up to date version of the hospice’s referral.
Changes in practice / next steps
• Only accept referrals with mandatory info boxes completed.
• Resend the current referral document to practice managers at GP surgeries.
• Inform external partners that referral form can be accessed from the website.
• To go back to referrers when referral is incomplete and request for uncompleted section to be completed.
Mental Capacity Audit
Aim
To review the quality and consistency of Mental Capacity Care Plan completion.
Outcomes
• x10 patients in the IPU and x10 patients in the community notes were reviewed to look for evidence of documentation of mental capacity concerns, evidence of the two-stage assessment and a relevant management plan.
• Care plans not updated when patients’ capacity is restored.
• No documented two stage assessment.
• However, staff and patient concerns were regularly documented.
Changes in practice / next steps
• Create a Functional Analysis of Care Environment (FACE) form at the end on the task window on the EPR system.
24 / Quality Accounts 2022-2023 / Part Three
Use of PPE and Infection Prevention Measures Audit (3 monthly rolling audit)
Aim
To identify any continued or additional learning, training or policy-related needs and to ascertain if IPC measures are embedded in day-to-day practice.
Outcomes
• Overall compliance 89%.
• Widespread lack of clarity around CPR / first aid practice.
• Good, widespread knowledge of covid symptoms and own responsibilities as employees e.g. for self-isolation etc.
• Pool cars not clean and tidy.
• Evidence of widespread good practice in relation to hand washing.
• Inconsistency with the donning and doffing of PPE.
Change in practice / next steps
• Pool cars cleaned weekly
• Designated boxes for the storage of PPE provided to all community staff.
• New cleaning schedule introduced on the IPU. Cleaning schedule was created using The National Standards of Healthcare Cleanliness (2021) as a reference point.
• IPC designated resource page on the hospice’s intranet for all staff to access.
• IPC support role created a film on the donning and doffing of PPE.
• Quarterly IPC Newsletter.
External Audit
The Infection Prevention Society (IPS), Process Improvement Tool (PIT) 2016
Aim
To ensure Infection Prevention and Control practices are compliant with current legislation and national guidelines, good practice of Infection Prevention.
Outcomes
• 21 sections, 440 standards / questions were used.
• 14 standards / questions were non-compliant.
• Overall compliance 96.8%, demonstrating an increase in compliance against the same audit carried out in January 2020.
Changes in practice / next steps
• Clostridium Difficle policy updated to reflect the new name Clostridioides Difficle.
• Alcohol based hand rubs in trigger bottles replaced with pump dispensers.
• Felt boards in medication room replaced with a magnetic board to enable more effective cleaning.
• Water Safety Plan has been reviewed and updated.
• Refer to Infection Prevention and Control section 3:13 for further analysis of the outcome of the audit.
25 / Quality Accounts 2022-2023 / Part Three
National Audit
Equitable care of all ethnicities at end of life audit (led by Kings College Hospital, London)
Aim
To investigate the validity and consistency of recorded ethnicity groups across palliative care relevant UK health databases using patient self-definition.
Outcomes
• One day audit completed comparing patients self-reported ethnicity against their ethnicity held in healthcare databases.
• The findings of the audit were published by Kings College Hospital, London at the end of the reporting year and will be shared with the wider team at the beginning of 2023/2024.
Nurse-led improvement Projects in Digital Health
We have successfully established a Nurse led Digital Health project at the hospice following a grant through the Burdett Trust for Nursing. The Digital Health Lead has expertly driven the project, with support from our Associate Director for Clinical Services, to explore new technologies for patient benefit which are crucial in bringing about lasting improvements in our care. Most importantly, this initiative has empowered nurses and healthcare staff to be involved in technological processes, build their confidence, and ensure their voices are heard in the design and delivery of these offerings. We are also pleased to be continuing this work beyond the grant period which will contribute to a landscape whereby Digital Health Nursing is part of a new normal in hospice care.
Case study
Helen Fothergill – Inpatient Team Leader

‘I’ve been nursing for thirty years now. It used to be handwritten records, but things constantly change and no-one tells you how to do it, you just had to figure it out on your own. It’s great to have someone there supporting us. I feel like my voice is heard and I feel more confident asking for help. I’ve given feedback on digital things like the IPU tablets and changes have been made which shows people are listening. I’m also a Digital Champion, which means I’m a point of contact for people who have questions. If you’re a bit older like me, you can be more nervous about asking for help. I enjoy helping people and highlighting that technology isn’t as complicated and scary as it may seem!’

3.7 Research
St Wilfrid’s Hospice is committed to research into palliative and end of life care. The hospice recognises the contribution research makes to the development and the quality of care delivery within specialist palliative care and end of life care services. This a subject within the terms of reference of the Clinical Effectiveness & People with Personal Experience (PPE) Group, a sub-committee of the CGC, with an aim of working towards being a ‘research active’ organisation. The Clinical Research Policy and Procedure provides guidance for the conduct of research at or by St Wilfrid’s Hospice. A Research Group has been set up this year to oversee participation in the CHELSea II Trial and monitor opportunities for involvement in other research activity.
The hospice has introduced a quarterly journal club for staff and volunteers. The aim of the sessions is to inform participants on up to date clinical practices through critical analysis of research and how it can be applied in our setting.
Research Activity
CHELSea II Trial
This is a cluster randomised trial of clinically assisted hydration in patients in the last days of life. It is run by the University of Surrey and recognised by the National Institute for Health Research.
St Wilfrid’s opened as a site in March 2023 and we started recruiting patients to the trial in May 2023.
Upcoming Research Studies
Exercise and Nutrition based Rehabilitation (ENeRgise)
This study is still seeking funding but is an international, open label, randomised trial of an Exercise and Nutrition based Rehabilitation programme (ENeRgise) delivered by health professionals, versus standard care.
We have been accepted into the research study as a locality team involving both hospices in East Sussex – St Wilfrid’s Hospice (Eastbourne) and St Michael’s Hospice, Hastings – along with East Sussex Healthcare NHS Trust. By joining together as a research site, we will increase opportunities for recruitment and ensure access to the components of the intervention with physiotherapy coming from the hospices and dietetic support from the NHS Trust.
3:8 Medical Revalidation
Doctors who work at the hospice have all undertaken Appraisal and Medical Revalidation as set out in General Medical Council (GMC) guidance in the reporting year.
Doctors employed directly by the hospice (the designated body they have a prescribed connection with) all undertake appraisals through the support of East Sussex Healthcare NHS Trust (ESHT) with the Responsible Officer being the ESHT Medical Director. A Service Level Agreement and Policies support this process.
Some of our consultants are employed directly by ESHT and hence this is their designated body. Doctors in training have a prescribed connection with the Deanery. All consultants contributing to the second medic on call have prescribed connections with their host organisations.
In the reporting year the process of monitoring all non-training doctors was transferred to Human Resources - preparing Transfer of Information forms for individual doctors then obtaining completed Appraisal Output Statements from them. Doctors in training are supported through their respective online training portfolios (HORUS for foundation doctors, Fourteen Fish for GP Trainees).
27 / Quality
Accounts 2022-2023 / Part Three
3:9 Income Generated
While some of our funding comes from the NHS, over 70% of the £18,000 a day we need to provide our care is generated through fundraising, legacies and trading activities.
With restrictions lifted after the Covid pandemic we were able to run a range of mass participation events like the Rainbow Run, sporting and overseas challenge events, and social events including the Winter Gala, which ran for the first time this year.

Grant funding for specific projects included ongoing funding from Children in Need for the Seahorse Children’s Bereavement Project, from the Good News Foundation for Spiritual Support and the Burdett Trust for Digital Health.
We were grateful to the many individuals, businesses and community groups who continued to support the hospice despite the uncertain economic climate and increases in the cost of living. Retail activity included a new shop in Herstmonceux and a new furniture store in Eastbourne.
‘I have nothing but love and respect for St Wilfrid’s. I will always be grateful for the excellent care they gave my partner.’ Relative of a patient
3:10 Medicines Management
The Medicines Optimisation Group (MOG) comprises a multi-disciplinary membership and has terms of reference which are reviewed annually to oversee practice across the hospice.
The MOG provides scrutiny of the budget for medicines, which is delegated from the Integrated Care Board (ICS).
The hospice has also held a joint MOG meeting with a neighbouring hospice. Future areas of work to include:
• Joined up training.
• Themes from incidents and changes in practice.
• Auditing across sites.
• Reviewing Medication Charts and Syringe Pumps Charts.
• Preceptorship – Medicines Optimisation.
The hospice has gone through a joint tender process with a neighbouring hospice to secure service provision for the supply of medicines and pharmaceutical services for at least the next three years from a local community pharmacy.
The hospice has introduced a mini-MOG. The aim of the group is to ensure standardisation and scrutiny of medication related incidents. The process of scrutiny ensures investigations are consistent, with relevant patient and environmental factors taken into consideration. The introduction of mini-MOG allows debate about why and how an incident had been graded which deepens understanding and will generate consistency over time.
Following a medication incident, staff complete a medication reflection tool. Registered Nurses and Doctors have found the process beneficial, especially when completing their reflective discussion evidence for their ongoing professional development and revalidation.
The Care at Home service now accepts patients requiring medication support. This service has enabled Continuing Health Care (CHC) funded patients to have their medication needs met safely within the domiciliary care setting. The staff have ongoing support from the Community Team Leaders.
The hospice continues to be part of Hospice UK’s national benchmarking for medication incidents. There has been an increase in our medication incidents compared to previous years. Over 90% of the reported incidents resulted in no adverse effect to the patient.
Accountable Officer for Controlled Drugs
The Associate Director for Quality and Governance is the Controlled Drugs Accountable Officer (CDAO). The individual has undertaken formal training on the CDAO role. There is no specific guidance on requirements for refresher training. The Quality Lead, a newly established role in the year, will be attending formal training on the CDAO role in May 2023 and will take on the role of the deputy CDAO once the training has been completed.
The CDAO ensures they are kept up to date with current legislation and guidelines around Controlled Drugs (CDs), including attendance at the Local Intelligence Network (LIN) meetings and CD LIN learning events. The CDAO undertook a CQC Self Assessment for Controlled Drugs Accountable Officer to provide assurance with national protocols.
There has been quarterly virtual attendance at the NHS England South East Controlled Drug Local Intelligence Network Meeting by the CDAO and the quarterly reports of CD incidents have been submitted.
The CDAO completed the annual Hospice UK CD audit and has undertaken quarterly stock level checks with Associate Director for Clinical Services. Authorised witnesses have been trained to observe the destruction of CDs on the premises. Destruction of controlled drugs which are
29 / Quality Accounts 2022-2023 /
Part Three
no longer required is carried out by a competent representative from the pharmacy provider with an authorised witness from the hospice overseeing the process of destruction. The hospice holds a valid T28 certificate to permit the denaturing of controlled drugs on the hospice premises.
3:11 Falls
The falls risk assessment was reviewed prior to migrating over to a new EPR system. When patients are admitted to the IPU a falls risk assessment is completed. Staff are encouraged to identify why an individual person is a falls risk so that more effective and individualised action plans can be created to reduce risk and harm.
The IPU holds twice daily ‘safety huddles’ (see glossary). Patients who are at a high risk of falls are highlighted, enhancing communication among the MDT.
The safety huddles have provided protected time at least once a shift for staff to focus on specific questions. Overall they aim to reduce errors, minimise harm, eliminate preventable harm, improve communication in teams and create a culture of safety. There have been four fewer falls reported this year compared to the previous year. Fall incidents are reported and analysed at the Quality and Safety Group.
Potential contributing factors in the reduction in falls could be:
• More patients being admitted for complex symptom management who are less mobile with a reduced Australian Karnofsky Performance Status (AKPS).
• Good use of one-to-one supervision.
• Safety huddles being routine practice seven days a week on the IPU.
• Reduced overall bed occupancy resulting in fewer fall incidents.
3:12 Pressure Ulcers
All pressure ulcers, including Category 1, are reported. Some pressure ulcers deteriorate further, exacerbated by the dying process as the organs slow down and fail, and skin changes take place.
Of the patients that acquired pressure damage while on the IPU, their phase of illness was predominately dying or deteriorating, and many of these patients were either bedbound or had very poor mobility potential. It is important to note that these patients were low in weight, and had problems maintaining adequate levels of nutrition and fluids.
All patients admitted onto the IPU have a PURPOSE T risk assessment and skin assessment completed on admission via the EPR system. The PURPOSE T is reviewed and updated at least weekly. All beds on the IPU are profiling beds and have an alternating pressure mattress.
The hospice was involved in the National STOP Pressure Ulcer Day. There were various resources available for staff including a quiz on pressure ulcer care and categorisation of pressure damage. Members across all the clinical teams attended, with constructive feedback being received for future events.
The management and care of pressure ulcers has been part of the RNs and HCAs mandatory clinical skills study days for 2022/2023. The session incorporated an interactive quiz for participants to engage with pressure ulcer care before and after the session. The session was well evaluated.
30 / Quality Accounts 2022-2023 / Part Three
During the reporting year, staff identified that there may be a correlation with the use of wendylett systems and the deterioration of patients’ skin.
‘Wendylett systems are based on a satin finsh woven textile that can be left in place as bed linen under patients. The system is intended to be used for people who have difficulties turning and positioning independently in bed.’
In conjunction with training, a risk assessment for the use of wendylett systems was introduced. In the later part of the year the hospice has seen a reduction in the use of wendylett system and new pressure ulcers being reported. The hospice has recognised that prior to any new equipment being rolled out training needs for users need to be identified.
3:13 Infection Prevention and Control
St Wilfrid’s Hospice is committed to ensuring that effective prevention and control of healthcare associated infections (HCAIs) is embedded into everyday practice. The hospice’s Board of Trustees recognises and agrees its collective responsibility for minimising the risks of infection and has agreed the general means by which it prevents and controls these risks. The responsibility for Infection Prevention (IP) is designated to the Associate Director for Quality and Governance.
The NHS National Infection Prevention and Control Manual now forms the hospice’s Infection Prevention and Control Procedure. Implementing this document has provided a consistent and up to date approach to Infection Prevention and Control.
At St Wilfrid’s Hospice there have been no cases of patients with a new diagnosis of Clostridium Difficile infection or a blood stream MRSA infection (see glossary). No vomiting and diarrhoea outbreaks took place at the hospice from April 2022 to March 2023.
The hospice introduced a designated Infection Prevention and Control Support Role in September 2022. Since the introduction of the new role the importance of IPC has been recognised more within the organisation. Some achievements in the first six months include:-
• Introduction of a cleaning rota on the IPU.
• Reduction in the wearing of lanyards in the clinical areas.
• Cleaning of the medication trollies.
• Filming of a video of the donning and doffing of Personal Protective Equipment.
• Building a good network of IPC resources.
• Involvement in the reviewing of IPC polices and procedures.
• Annual subscription to the IPC Society.
• Co-authoring the quarterly IPC Newsletter.
The Infection Prevention Society (IPS) Process Improvement Tool (PIT) (2016), was completed by an external auditor on 28th June 2022. The tool reflects current legislation, national guidelines, and good practice of infection prevention within a healthcare environment.
21 sections were audited, and 440 standards/questions were used, some of these were repeated. 14 standard/questions were non-complaint, providing the hospice with an overall compliance score of 96.8%.
31 / Quality Accounts 2022-2023 / Part Three
Below is a table of the results with a comparison with the compliance of the same audit in January 2020.
32 / Quality Accounts 2022-2023 / Part Three Score Score 2020 2022 1 Infection prevention and control is integral to safety in this hospice 70% 100% 2 The staff are afforded health and safety protection from potential infection risks 100% 100% 3 There is a competent and confident workforce trained to minimise infection risks 90% 100% 4 There is evidence of compliance with policies, procedures and guidance 66% 100% 5 Personal Protective Equipment is used to minimise infection risks 93% 100% 6 Environment: general environment safety and cleanliness (including lobby / reception and entrance) 96% 100% 7 Environment: the patient’s bedroom 88% 100% 8 Environment: hand hygiene facilities 84% 100% 9 Environment: relatives lounge / Garden Room 78% 100% 10 Environment: the bathroom(s) / showers 96% 100% 11 Environment: the toilet(s) 95% 100% 12 Environment: clean utility 81% 93% 13 Environment: dirty utility / sluice area 95% 97% 14 Environment: pets and Pets Therapy is safely managed 60% N/A 15 Environment: maintenance and use of chilled water / ice making facilities 50% 83% 16 Environment: safety, in use and not in a store 92% 92% 17 Environment: storage room and stored equipment N/A N/A 18 Waste, safe discarding and disposal including the safe use of sharps 86% 82% 19 Linen, safe storage, segregation and usage 100% 100% 20 Water, safety management 64% 85%
Since the audit, work has taken place to address the areas of improvement to ensure a high compliance in specific sections.
33 / Quality Accounts 2022-2023 / Part Three 21 Ventilation 33% 100% 22 Aromatherapy, beauty and hair salon 58% N/A 23 Mortuary N/A N/A 24 Laundry management 97% 95% 25 Housekeeping room 100% 92% Overall average 86% 96.8% Score Score 2020 2022
‘I have so much respect and gratitude for St Wilfrid’s Hospice. The care they have given my family is second to none.’ Relative of a patient
3:14 Data Quality
Good data quality underpins the effective delivery of patient care and is essential if improvements in quality of care are to be made. A key aim to meet this is to identify and agree a suite of reports which allow accurate activity reporting.
As the hospice has moved to a new EPR system we need to ensure the data which is being produced is meaningful, timely and accurate.
During 2022-2023 we have continued to monitor and scrutinise data quality through our Clinical Governance structure. St Wilfrid’s Hospice reports its own clinical activity dashboard which provides an overview of all clinical activity and supports service development and QIPs. In the next reporting year the hospice is planning on introducing the use of Statistical Process Control (SPC) charts (see glossary) for reporting patient safety metrics to the Clinical Governance Committee.
The hospice continues to provide data on reported falls, medication and pressure ulcer incidents to Hospice UK for national benchmarking.
As a specialist palliative and end of life care provider, the hospice does not submit data information to the Hospital Episodes Statistics (HES) database because hospices are not eligible to participate in the data collection.

34 / Quality Accounts 2022-2023 / Part Three
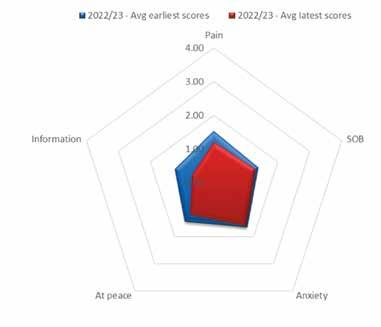
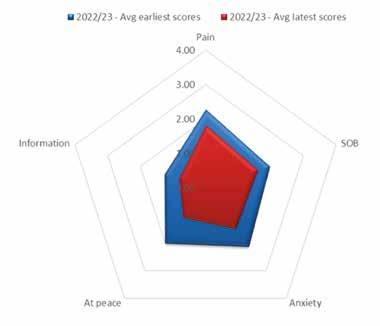
Integrated Palliative Outcome Scale (IPOS) Average Score Comparisons
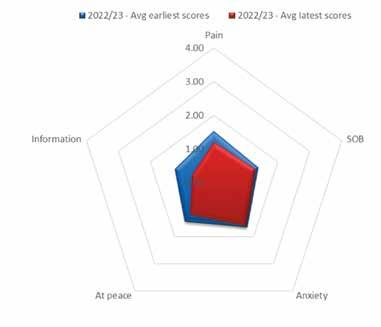
The Integrated Palliative Care Outcome Score (IPOS) is one of a suite of outcome measures used at the hospice to measure changes over time, in relation to what patients are thinking and feeling. This holistic assessment covers many areas including physical issues, their main concerns, psychosocial issues, wellbeing, other symptoms and whether they have any unmet needs such as practical issues or wanting more information. Scores are taken from 0 to 4 and reassessed at a later date, with the hope that the scores have reduced, indicating an improvement. The five elements shown in the charts below show average scores taken in IPU or Community settings for pain, shortness of breath, anxiety, feeling at peace and information needs.
2022/23 – IPOS 5 Average Score
Comparison – IPU
Comparison based on between 49 to 60 records in 2022-23 where an initial assessment element score existed followed by at least one later score for the same element.
2022/23 – IPOS 5 Average Score
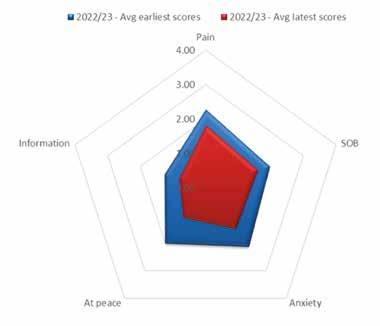
Comparison – Community
Comparison based on between 159 to 183 records in 2022-23 where an initial assessment element score existed followed by at least one later score for the same element.
35 / Quality Accounts 2022-2023 / Part Three
3:15 Safeguarding
This year the focus on safeguarding as an organisation-wide priority has continued.
The numbers for safeguarding referrals from the hospice to Adult Social Care/Children’s Services, as well as concerns identified internally and monitored closely but with no referral, have hovered at a similar level for the last three years. Previously numbers were significantly lower. This indicates a maturing level of engagement with safeguarding amongst clinical staff.
Ongoing training for clinical and non-clinical staff, volunteers and trustees, in line with national guidance, has of course played a key part in ensuring increased confidence in dealing with safeguarding matters.
The latest available completion rates for training (Jan 23) are satisfactory, including 95% for Safeguarding Adults level 2, 81% for Safeguarding Adults level 3, 80% for Safeguarding Children level 2 and 89% for Safeguarding level 3. Different staff groups are required to undertake different levels of e-learning and the above are just examples. In April 23 the hospice switched to a new learning platform. It is expected that going forward this will impact very positively on completion rates and related reporting.
Participatory safeguarding learning to complement e-learning, for clinical staff, is now firmly embedded. This is a key achievement. One of the hospice social workers delivers face to face safeguarding learning sessions to IPU staff, based on case scenarios. The expectation is that all IPU staff attend one of these sessions per year. Community staff have the opportunity to attend 6 weekly safeguarding reflective practice sessions, with the expectation that they submit two written reflections on these sessions each year. The latter sessions in particular have proved popular, with good attendance and lively discussion. Retail staff have again undertaken one day bespoke safeguarding training tailored to their specific circumstances.
Learning from SARs (Safeguarding Adult Reviews) has been a focus, with a dedicated interactive teaching session on SARs delivered to trustees in December 22. This year, for the first time, the hospice has been involved with a SAR enquiry regarding an ex-patient. Currently this is on hold whilst other proceedings are under way.
The focus on continuous improvement of the hospice’s safeguarding culture continues with regular safeguarding awareness emails to all staff on a range of topics. In November 22 the hospice took part in the Ann Craft Trust Safeguarding Adults Week, again an awareness raising exercise, with daily emails and a blog. Trustees visit staff regularly and each time include some questions regarding safeguarding awareness and practice.
Completion of a safeguarding adults peer audit developed by the Sussex Hospices Collaborative (see glossary) is under way, with a peer review visit by safeguarding trustees from neighbouring hospices planned. This has already proved to be a useful tool for ongoing quality improvement in this area.
36 / Quality Accounts
2022-2023 / Part Three
‘St Wilfrids is amazing. Since we have been under the care of St Wilfrid’s we have both had so much support. The care they give is amazing.’ Patient

Part Four Feedback About Our Organisation
4:1 Duty of Candour
St Wilfrid’s Hospice recognises that the effects of harming a patient can have devastating emotional and physical consequences for patients, their families, and carers. It can also be distressing for the professionals involved.
The hospice’s Duty of Candour Policy and Procedure provides guidance to staff and volunteers around being open and honest with patients and their families following an incident which has resulted in harm.
All incidents are discussed at the Quality and Safety Group and summarised to the CGC. A root cause analysis (RCA) is completed for serious incidents to ensure the reporting manager has detailed understanding of the cause of the event and promotes organisational learning.
All serious incidents are reported to the CQC as well as other statutory bodies as required. No clinical serious incidents took place during 2022-2023.
4:2 Freedom to Speak Up
The hospice is committed to proactively enabling any employee or volunteer to raise reasonable concerns about any aspect of our service. All staff and volunteers are encouraged to raise any matter that is or has the potential to be detrimental to their work or to the quality of the services that we provide including:
• Actions that may cause or present a risk to the provision of safe patient care.
• Unsafe working conditions.
• Unethical behaviour.
• A bullying culture.
Staff are supported in doing this without fear for their future role in the organisation or of any form of retribution. They can raise their concerns through their line manager, the Human Resources (HR) Team or the trained Freedom to Speak Up Guardians (FSUG). The FSUGs are based in a variety of different clinical and non-clinical areas. They may be approached in person, by phone, email or in writing and the supporting policy makes it clear that individuals can raise their concern anonymously and in confidence. The FSUG have direct access to the CEO, to external mentors and to the National Guardian’s Office for advice. The FSUGs submit anonymised data in relation to the concerns they receive to the NGO on a quarterly basis and provide a six-monthly review to the CEO. They also analyse their data, looking for recurring themes, and continuously review their service with a view to maximizing accessibility.
4:3 Service User Feedback and Engagement – VOICES and Views on Care
St Wilfrid’s Hospice uses VOICES as one of its tools for gaining user feedback. The survey is adapted from a validated service evaluation and quality assurance tool for use in hospices, developed jointly between the Southampton University School of Health Sciences and St Christopher’s Hospice, London. It is based on the National Bereavement Survey – VOICES –conducted by the National Office of Statistics.
38 / Quality Accounts
2022-2023 / Part Four
In the most recent reporting period (2021-22) a response rate overall of 28% was achieved. This was a dip compared to the previous year (38% in 2020-21) but still higher than 22% in 2019-20.
Key findings included: -
• 94% of respondents felt that the care they received from the Inpatient Team was above ‘good’ (compared to 83% the previous year).
• 83% of respondents felt that they and their family got as much help and support from the Community team as they needed (compared to 80% the previous year).
• 92% of respondents (86% the previous year) said they were extremely likely to recommend St Wilfrid’s Hospice to friends and family.
The hospice used the recognised Views on Care (VoC) tool to assess patients’ own rating of their quality of life, their views of the impact of the service on their main problem(s) and their wellbeing.

In the reporting year there have been 156 assessments completed (81 IPU, 75 community) with 82 patients declining or not clinically appropriate at the time. The largest increase was seen in the community where the process for collecting VoC was reviewed and there is now a designated Quality and Feedback volunteer collecting this information on a regular basis.
Key findings were:
• 103/156 (66%) feel things are a little or much better.
• 138/156 (88%) are getting some or a lot of benefit from us.
Word cloud below taken from VoC responses for the year:
39 / Quality Accounts 2022-2023 / Part Four
Some comments taken from this year:
• The level of care is amazing and the support given is outstanding!
• 100% quality of service!
• Was reluctant to come into the hospice, but now realises it is a safe and caring place. Their daughter is getting some rest now.
• Psychologically much better since the hospice involvement. The hospice involvement is extremely beneficial.
• The care is excellent. Loves being in a single room. Feels very safe.
• Family has felt very well supported by the community team.
• The hospice has been a very good experience - has felt supported by the whole team and will continue to feel this when at home.

• Care is simply phenomenal!
• Everyone at St Wilfrid’s has been incredibly kind to me. I am so lucky to have their support. Thank you.
• Excellent communication from Nurseline. Received counselling that has helped. Reflexology has helped with relaxation and muscle release. Overall service amazing.
4:4 People/Patient with Personal Experience (PPE)
There continues to be a commitment from staff to obtaining and acting on feedback from PPE. There have been nine People with Personal Experience initiatives completed. Feedback from the work that has been completed is presented at the Quality and Audit Forums.
The forums are open to all staff and volunteers to attend.
4:5 Trustee Visits
At least two trustees have visited the hospice each quarter to meet front line staff. The visits provide an opportunity for staff to give feedback on working at the hospice. Throughout the year staff from all clinical areas, including patient and family support services and care@home have spoken to trustees. Areas that have been explored were:
• Migration to a new Electronic Patient Record system.
• Equality and Diversity Awareness.
• Community Nursing and Lone Working.
• Counselling and Seahorse Project.
• Safeguarding.
In the coming year an annual timetable has been created with themes to look at each visit which include:-
• Secure and safe management of medicines.
• Safeguarding.
• Patient feedback.
• Safe care and closing the loop on incidents.
• Quality improvement.
Highlights of good practice
• Staff are proud to work at the hospice. They value the positive working environment and feel well supported. Several staff said team working was excellent, and that they felt there was no unnecessary hierarchy, and everyone was approachable.
• There were examples of how staff had gone the extra mile to meet patients’ needs.
• Staff felt the hospice culture was open and accepting of differences. One person said St Wilfrid’s Hospice being involved in Eastbourne Pride had been a great opportunity to engage with the public and break down barriers.
• Staff felt training about the new Electronic Patient Record system was good and that it could offer benefits, especially access to district nursing records, and avoidance of duplication, thereby saving time.
• Reports are discussed at the Clinical Governance Committee and an annual report of the feedback themes and actions taken following the trustees’ visits have been shared with the board.
4:6 Complaints and Compliance
The hospice has a policy to welcome comments, suggestions and complaints, because they can be invaluable in achieving improvements in service delivery. During the reporting year we received three formal complaints related to clinical support. There were no themes identified through these complaints, all were investigated and an outcome provided to the complainant within the hospice’s stated timeframe.
During the year, we have continually taken time to reflect on our approach to complaints. We continue to look at improving our ability to respond in an open way, and to ensure learning from investigations contributes to positive changes in practice.
41 / Quality Accounts 2022-2023
/ Part Four
4:7 Hospice UK National Benchmarking Programme
St Wilfrid’s Hospice submits data to the Hospice UK (HUK) national benchmarking programme quarterly.
Data which is correlated includes:
• Inpatient bed occupancy.
• Patient throughput.
• Patient falls.
• Level of harm following a patient’s fall.
• Medication incidents.
• Level of harm following a medication incident.
• Pressure ulcers on admission.
• Pressure ulcers acquired during admission.
• Categories of pressure ulcers damage.
Outcomes of the data received are reported to the Quality and Safety Group, Medicines Optimisation Group and the CGC for further analysis and scrutiny.
Over the reporting year the hospice has reported fewer falls than other hospices with similar bed capacity.
The number of medication incidents is slightly higher compared to other hospices of similar bed capacity. A large proportion on the number of medication incidents were level one: no harm incident not prevented.
The number of patients admitted and who have developed pressure damage is slightly higher compared to other hospices of similar bed capacity.
4:8 Staff – Pulse Survey
The hospice has a schedule of surveys to be sent to staff throughout the year. Each survey is based on a different subject with two standard questions asked in each to help determine our net promoter score.
Our recent staff surveys have covered topics such as employee retention and speaking up. Our usual response rate to staff surveys is around 40% with feedback being gathered from clinical, non-clinical and retail staff. Feedback and input collected from staff within these surveys allows us to identity gaps, make changes and introduce new initiatives in line with our workforce wants and needs.
Some examples of actions that have been implemented from survey feedback include:
• Learning and Development strategic review to ensure consistent and equitable access to development.
• Introduction of a learning management system to streamline training and access to records.
• Job evaluation review underway to support transparent and fair pay across the hospice.
• Additional training for managers such as up and coming course IOSH managing safely to upskill in H&S and risk management.
42 / Quality Accounts 2022-2023
Part
/
Four
4.9. Feedback from Integrated Care Board
‘Thank you for giving NHS Sussex Integrated Care Board (ICB) the opportunity to comment on St Wilfrid’s Hospice’s Quality Account for 2022/23. We appreciate the collaboration and open communication with St Wilfrid’s during 2022/23. We would like to thank the organisation for its ongoing commitment to quality improvement through achievement of its objectives for 2022/23 for Sussex residents. We are pleased to see that the Hospice Board has agreed some of the objectives for 2023/24, building on the progress made from previous objectives, and, notably, St Wilfrid’s continuing to reach ever more people who could benefit from your services. It was good to read how you are learning from and adapting your services using feedback from patients, family members and users accessing your wider services. Your commitment to removing perceived or actual barriers to services and seeking new ways to improve access is commended.
The hospice has achieved many successes in 2022/23, most notably:
• Reviewing and improving your offer and practice regarding Advance Care Planning (ACP), involving patients and carers reconfiguring the ACP section of the hospice website to include four downloadable nationally recognised ACP tools for people to use.
• Amplifying the patient/family voice in planning and delivery through an additional Social Worker joining the patient and family support team, with a focus to identify and address carer needs.
• Improving the reach of, and access to, hospice care, ensuring equity in relation to diagnosis, location, and demographics with a new ‘Nurseline (the hospice’s telephone support service) only’ mini assessment to increase the hospice reach with a proportionate and effective response.
• Improving the use of digital health approaches. For example, ensuring all patient rooms on the Inpatient Unit (IPU) having access to a handheld digital device; and the introduction of the hospice direct email for community patients and carers for non-urgent advice and requests to the community team.
St Wilfrid’s Hospice Quality Account outlines the priorities for improvement in 2023/24 as well, and how these will be achieved and measured, using the Plan, Do, Study, Act (PDSA) cycle as the hospice recommended Quality Improvement methodology.
NHS Sussex ICB acknowledges some of your key priorities:
• To further develop and embed your Quality Improvement Methodology Model.
• Introducing and establishing a virtual ward.
• Fully integrating and embedding a new patient electronic records system, enabling meaningful and purposeful data to be obtained.
• Enhancing opportunities for Multi-Disciplinary Team (MDT) learning; building competence and confidence in the clinical workforce.
The ICB supports these priorities and the detailed work that underpins them and will continue to seek assurance regarding progress of implementation throughout the year via our established processes.
My colleagues and I look forward to the continued collaborative working with St Wilfrid’s and the wider system partners.’
Allison Cannon Chief Nursing Officer NHS Sussex
43 / Quality Accounts 2022-2023 / Part Four
Glossary
Care Quality Commission (CQC) Independent regulator of all health and social care services in England.
Clinical Nurse Specialist (CNS) Registered Nurses with a specialist knowledge and qualifications in cancer and palliative care.
Continuing Health Care (CHC) A package of care for people who are not in hospital and have been assessed as having a primary healthcare need. Paid by the NHS.
Integrated Palliative Care Outcome Score (IPOS) A tool for global measurement of palliative care concerns, suitable completion by patients and healthcare staff in various care settings.
General Data Protection Regulation (GDPR) A European Union law which governs the way we can use, process and store personal data.
Multi Disciplinary Team (MDT) A group of healthcare workers who are members of different disciplines each providing a specific service to the patient.
Methicillin-resistant Staphylococcus Aureus (MRSA) A group of gram-positive bacteria.
Phase of Illness (POI) Describes stages of advanced illness according to care needs of the individual, family and suitability of care plan.
PLACE System A set of health and care providers in a town or district.
Safety huddles Brief, focused and structured exchanges of information about potential or existing safety risks which may affect patients, staff and any person accessing the healthcare environment.
Safety huddles are held at points in the day to allow teams to:
• Develop on the spot action plans to address safety concerns.
• Provide an update on the action taken on risk previously identified.
• Celebrate success and compliments.
Sussex Hospices Collaborative Network of seven adult hospices in Sussex working collaboratively to combine resources, share knowledge and speak effectively with one voice. Schwartz Rounds Conversations with staff about the emotional impact of their work. Schwartz Rounds provide an opportunity for staff from all disciplinary across a healthcare organisation to reflect on the emotional aspects of their work.
VOICES survey St Wilfrid’s VOICES survey is adapted from a validated service evaluation and quality assurance tool for use in hospices, developed jointly between the Southampton University School of Health Sciences and St Christopher’s Hospice, London. It is based on the National Bereavement Survey VOICES conducted by the National Office of Statistics. It is common for hospices to have adapted the national tool to local circumstances and services.
Wendylett systems A satin finsh woven textile that can be left in place as bed linen under patients. The system is intended to be used for people who have difficulties turning and positioning independently in bed.
44 / Quality Accounts 2022-2023
45 / Quality Accounts 2022-2023
46 / Quality Accounts 2022-2023
47 / Quality Accounts 2022-2023
Registered as a company limited by guarantee in England and Wales No: 1594410 / Registered Charity No: 283686 St Wilfrid’s Hospice, 1 Broadwater Way, Eastbourne, East Sussex BN22 9PZ 01323 434200 / www.stwhospice.org stwilfridshospice @stwilfridstweet @stwhospice @peopleofstwilfrids