BCMSScript.
Newsletter of the Bucks County Medical Society Winter 2026
OUR MISSION
The Bucks County Medical Society strives to advance the professional and personal development of its physician members by providing educational and practice related resources as well as legislative advocacy. Moreover, the Bucks County Medical Society seeks to promote optimal outcomes for our patients as well as the public health of the Bucks County community.
EDITORIAL BOARD
Marilyn
Heine,
MD, Editor-in-Chief
J. Matthew Bohning, MD
Hannah Do, MD
John Gallagher, MD
John Pagan, MD, MBA
President’s Message
President’s Message

The more things change . . .
Like most years in medicine, 2025 has been eventful for doctors and patients. Our PAMED and Bucks County Medical Society (CMS) physician leaders continue to advocate for common sense in prior authorizations, non-compete agreements, and fair reimbursement for medical services. We inform legislators and the public on the implications of rapidly advancing AI in medicine and potential downsides of increasing private equity ownership of physician groups. Physician-led, team-based care remains a cornerstone of our profession along with a healthy environment to provide care be it in private practice or an employed setting.
Our Bucks County Medical Society annual meeting and brunch with decades of medical service to our Bucks community and new and old friends. The lively discussions around the room and challenges we mutually face in patient care remind us how our stronger than our differences.
Following a lengthy budget stalemate, some legislative highlights of the year include proposals to strengthen the current requirements for certificate of merit and medical experts (SB 340 and HB 2088) and a constitutional amendment on medical liability venues (SB 125); definitive action by the General Assembly is pending. Potential pitfalls of private equity in medicine were emphasized by our PAMED President, Dr. Lucas-Fehm MD JD, in her presentation at our Annual Bucks CMS Brunch and legislative testimony resulting in the introduction of a private equity in medicine bill (HB 1460). Relationships to advance these initiatives were fostered at our Bucks CMS legislative reception in Doylestown in October.
Bucks CMS remains a vibrant part of PAMED in leadership and in our House of Delegates. Bucks CMS collaborated with our neighboring county medical societies in District II and other delegations. We worked to assure that the voice of independent practice remains in policy decisions, to discuss healthcare worker safety, and advance policy to strengthen the physician workforce, and enhance our public health infrastructure. Although medical perspectives may vary, our common interests across geographies and specialties far outweigh any differences. We are certainly stronger together. The 100% PAMPAC membership of our Bucks CMS delegation at the House of Delegates echoes that unity. We thank all from Bucks CMS who are PAMPAC members.
I am honored to join the esteemed line of presidents of this great roots tracing back to 1848—the same year our Pennsylvania Medical Some of the numerous challenges facing our profession and the navigate have returned over the past 25 years when I first start in Sellersville. I’ve dedicated my career to amplifying our collective Society, advocating for both our profession and our patients in Pennsylvania Medical Society, proudly advancing our shared causes.
As a new year begins, Bucks CMS extends warmest wishes for health, happiness, and prosperity to you and your family, staff, and patients. Your commitment to your profession and patients is not only admirable, but essential to our profession.
John J. Pagan, MD, MBA, FACS President, Bucks County Medical Society
Medicine and my career have changed a lot in that time, but common solutions persist. Fair valuation and payment for physician services, of lesser trained medical professions, the corporatization of medicine, medical legal challenges we face in caring for patients are issues our careers to varying degrees. While our combined multipronged substantial tort reforms decades ago, liability venue shopping
Savvy Snoozing: Hot Topics in Sleep Medicine
Savvy Snoozing: Hot Topics in Sleep Medicine

By Kathy Tran-Gast, D.O.
Kathy Tran-Gast, DO, is a pulmonary, critical care, and sleep medicine physician in Doylestown.
Dr. Tran-Gast is a pulmonary, critical care, and sleep medicine physician in Doylestown.
Sleep medicine is broadly encompassing
Sleep medicine is broadly encompassing
7 hours for adults (age >18) and between 8-10 hours for children (age <18). We do know that sleep requirements differ based on whether we self-describe as ”short sleepers” or ”long sleepers” with some individuals requiring more sleep than others. It is important to rule out any underlying sleep disordered breathing in patients with hypertension, coronary artery disease, or other cardiac risk factors for stroke. There is still much to be learned regarding predisposing factors towards dementia or underlying cognitive disorders.
A link between sleep quality and heart health
Sleep medicine is a very dynamic specialty that encompasses an array of sleep conditions which with fields such as pulmonary, neurology, psychiatry, cardiology and pediatrics. The wide range syndromes may include sleep-related breathing disorders such as obstructive sleep apnea; but will include complex sleep-behavioral disorders such as insomnias, parasomnias, or narcolepsy. Each syndrome may be managed very differently depending on type and may incorporate multidisciplinary subspecialties including clinical psychology, dentistry and/or otolaryngology.
Latest advancements in sleep medicine
Sleep medicine is a very dynamic specialty that encompasses an array of sleep conditions which overlap with fields such as pulmonary, neurology, psychiatry, cardiology and pediatrics. The wide range of sleep syndromes may include sleeprelated breathing disorders such as obstructive sleep apnea; but will also include complex sleep-behavioral disorders such as insomnias, parasomnias, or narcolepsy. Each clinical syndrome may be managed very differently depending on type and may incorporate multidisciplinary subspecialties including clinical psychology, dentistry and/or otolaryngology.
Latest advancements in sleep medicine
In general, maintaining a regular sleep schedule is important for our overall physical and mental health. In patients with pre-existing heart disease, coronary artery disease, or heart failure disorders, it is important to rule out sleep disordered breathing as these heart conditions and sleep disorders may overlap significantly. Studies have shown a significant link between sleep apnea and increased cardiovascular risk, including hypertension, heart failure, and atrial fibrillation; with some studies showing up to a 45% increased risk for heart events.
In recent years, the majority of sleep studies are obtained at home which has facilitated diagnoses patient comfort. The studies are highly accurate with the added benefit of being remote. Surgical advancements in treatments for obstructive sleep apnea, such as the Inspire device, have increased interest in sleep technology. Medical treatments for insomnia and narcolepsy have improved sleep quality and quality of life for patients with these disorders.
Sleep duration and brain health
In recent years, the majority of sleep studies are obtained at home which has facilitated diagnoses and patient comfort. The studies are highly accurate with the added benefit of being remote. Surgical advancements in treatments for obstructive sleep apnea, such as the Inspire device, have increased interest in sleep technology. Medical treatments for insomnia and narcolepsy have improved sleep quality and quality of life for patients with these disorders.
Sleep duration and brain health
While there is interest in sleep duration and brain health there are no specific American Academy of Sleep Medicine guidelines. The general consensus recommendation has been to obtain greater than
Another hot topic in sleep medicine
One subject in which does not receive as much focus is how sleep is impacted in women of child-bearing age or older. Historically sleep disorders are underdiagnosed and not well recognized in women compared to men. Women are not screened as often for underlying sleep disordered breathing, partly due to lack of recognition but also likely due to fewer complaints by women compared to men. Women have increased risk of insomnia and other behavioral sleep disorders particularly through stages of hormone fluctuations such as pregnancy and/ or menopause. Recognition of this is crucial to improve understanding, diagnosis, and care in women’s health.
While there is interest in sleep duration and brain health there are no specific American Academy Sleep Medicine guidelines. The general consensus recommendation has been to obtain greater hours for adults (age >18) and between 8-10 hours for children (age <18). We do know that sleep requirements differ based on whether we self-describe as ”short sleepers” or ”long sleepers” with individuals requiring more sleep than others. It is important to rule out any underlying sleep disordered breathing in patients with hypertension, coronary artery disease, or other cardiac risk factors for There is still much to be learned regarding predisposing factors towards dementia or underlying cognitive disorders.
A link between sleep quality and heart health

In general, maintaining a regular sleep schedule is important for our overall physical and mental In patients with pre-existing heart disease, coronary artery disease, heart failure disorders, it is important to rule out sleep disordered breathing as these heart conditions and sleep disorders
Precision Healthcare with an AI Twist
Strengthening the Focus on Precision Healthcare with an AI Twist
Marilyn Heine, MD, FACEP, FACP, FCPP, is an Emergency Physician and Hematologist Oncologist in Bucks County.
By Marilyn Heine, MD, FACEP, FACP, FCPP
such as stress, aging, microbiome, inflammation, and gene expression.
Dr. Heine is an emergency physician and hematologist oncologist in Bucks County.
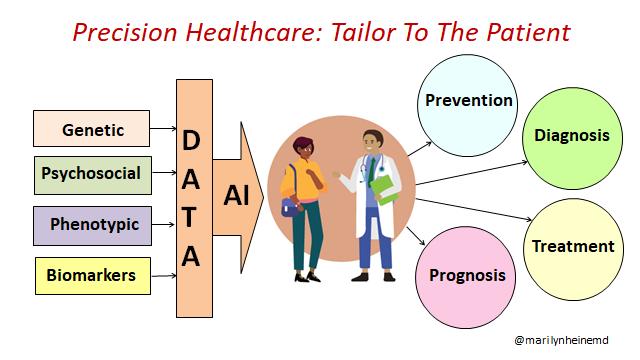
Patient’s Unique Factors in Precision Healthcare
•
Genetic: DNA analysis that impacts risk of disease and response to treatment (e.g. BRCA mutations in breast or ovarian cancer)
•
Precision healthcare aims to get “the right treatment to the right person at the right time.” Statement attributed to former Health and Human Services Secretary Michael O. Leavitt.
Benefits and components of precision healthcare
Precision healthcare: The aim is to get “the right treatment to the right person at the right time.” Statement attributed to former Health and Human Services Secretary Michael Leavitt. Goals are to improve effectiveness, target treatment to specific conditions and individuals, understand individual characteristics to lessen potential risks or side effects and enhance patient safety, ensure better outcomes, and improve quality of life. It emphasizes that healthcare is not one-size-fits-all.
•
•
Psychosocial: Mental health, social support, socioeconomics, lifestyle, and environment
Phenotypic: Clinical and physical presentation
Biomarkers: Blood tests and imaging to define disease characteristics and treatment response (e.g., hemoglobin A1c and tumor markers)
Goals of precision healthcare are to improve effectiveness, target treatment to specific conditions and individuals; enhance patient safety, understand individual characteristics to lessen potential risks or side effects; ensure better outcomes, and improve quality of life. It emphasizes that healthcare is not onesize-fits-all.
4 Ps of Precision Healthcare
• Predictive: Data to predict disease presence of progression, allow early intervention
Components of precision healthcare can be grouped into 4 Ps:
• Prevention: Steps to reduce disease risk, promote wellness, target interventions
• Personalized: Tailor treatment, address social drivers of health
• Predictive – use data and analytics to predict disease and progression and allow early intervention such as lung cancer screening;
By Marilyn Heine, MD, FACEP,
• Participatory: Engage patients in their healthcare with wearables and self-monitoring
• Prevention – take steps to reduce disease risk, promote overall wellness, and target interventions, as in diabetes, heart disease, and cancer;
Now let’s consider the role of biomarkers in a patient whom we will call “AB” who has been diagnosed with colon cancer. “AB”’s CEA level, a diagnostic biomarker, was high prior to surgery and decreased with resection of the tumor. The side of “AB”’s colon cancer has prognostic significance. “AB”’s tumor mutations are predictive as they correlate with risk of cancer recurrence. Since 5-FU is to be part of “AB”’s cancer chemotherapy, a gene test for a pharmacogenomic biomarker is performed to assess if the usual dose can be safely given. “AB” will have monitoring of circulating tumor cells to assess the clinical course.
5 Categories of Biomarkers
• Personalized – tailor treatment, address lifestyle and environmental interventions, such as with familial hypercholesterolemia and mutation-targeted cancer care; and
Transformative impact of genome
sequencing: Over the last 70 years, the study of a person’s DNA has evolved dramatically from the first chromosomal analysis to the development of vast genetic databanks and sophisticated DNA sequencing of the whole genome or targeted gene panels to identify genes that cause or increase risk for disease; aid diagnosis, and guide treatment.
Precision healthcare: The aim is to get the right treatment to the right person at the right time ” Statement attributed to former Health and Human Services Secretary Michael Leavitt. Goals are to improve effectiveness, target treatment to specific conditions and individuals understand individual characteristics to lessen potential risks or side effects and enhance patient safety, ensure better outcomes, and improve quality of life. It emphasizes that healthcare is not one-size-fits-all.
• Participatory – patients are engaged and empowered in their own healthcare decisions using wearables and self-monitoring.
4 Ps of Precision Healthcare
• Diagnostic: Confirms a disease or condition, and identifies persons with a disease subtype (e.g., hemoglobin S in sickle cell disease)
• Predictive: Data to predict disease presence of progression, allow early intervention
• Prevention: Steps to reduce disease risk, promote wellness, target interventions
• Personalized: Tailor treatment, address social drivers of health
• Participatory: Engage patients in their healthcare with wearables and self-monitoring
• Prognostic: Identifies likelihood of disease, recurrence, or progression (e.g., PSA in prostate cancer)
Precision healthcare recognizes a patient’s unique factors. Genetic aspects include DNA analysis that impact risk of disease and response to medication, such as BRCA gene mutations that increase risk of breast and ovarian cancer. Psychosocial factors can involve mental health, social support, socioeconomics, lifestyle, and environment such as residing in an older home with lead paint. Phenotypic traits are the patient’s clinical and physical presentation. Biomarkers such as blood tests and imaging help define disease characteristics and treatment response; examples are hemoglobin A1c and tumor markers.
Transformative impact of genome sequencing: Over the last 70 years, the study of a person’s DNA has evolved dramatically from the first chromosomal analysis to the development of vast genetic databanks and sophisticated DNA sequencing of the whole genome or targeted gene panels to identify genes that cause or increase risk for disease; aid diagnosis, and guide treatment.
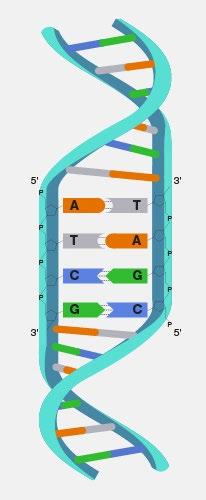
DNA does not equal destiny: The transition from a patient’s genome to their phenotype – the medical history, physical examination findings, disease severity, and response to treatment – is influenced by what epidemiologists call the “exposome.” The exposome is where personal factors such as exercise, substance use, diet, sleep, income, education, work, and access to healthcare; combine with external factors including exposure to pollution, high traffic and noise, or green space; leading to biological responses
• Predictive: Identifies the most effective treatment for a patient (e.g., presence of an abnormal BCR-ABL fusion gene of chronic myelogenous leukemia)
• Pharmacogenomic: Predicts a drug’s efficacy or toxicity based on genetic makeup (e.g., G6PD deficiency)
Genome sequencing: The study of an organism's entire genome or complete set of DNA has evolved dramatically from the first chromosomal analysis 70 years ago, to development of vast genetic databanks, and sophisticated DNA analysis essential in cancer care and other conditions. Sequencing of the whole genome or targeted gene panels identifies genes that cause or increase risk for disease; helps diagnose rare, unexplained, or atypical diseases; and guides treatment.
• Monitoring: Detects early signs of disease progression or recurrence (e.g, BNP in congestive heart failure or circulating tumor cells in certain types of cancer)
DNA does not equal destiny: The transition from a patient’s genome to their phenotype – the medical history, physical examination findings, disease severity and response to treatment – is influenced by
Psychosocial and phenotype: DNA does not equal destiny. A patient’s genome is their entire DNA. It is an “operating manual.” However, there is not an inevitable transition from a patient’s genome to their
Precision Healthcare with an AI Twist
FACP, FCPP
Dr. Heine is an emergency physician and hematologist oncologist in Bucks County
Since January 2025, Pennsylvania state law mandates that state-regulated health plans, including Medicaid, cover biomarker testing when used for diagnosis, treatment, management, or monitoring of a disease, aligning with clinical guidelines and evidence.
AI drives precision healthcare
With this abundance of data, there is a role for AI. AI is preferably called “augmented intelligence” that highlights the importance of having a “human in the loop.” Clinicians rely heavily on pattern recognition. AI augments the human ability to analyze and interpret vast, complex data, and identify patterns. In precision healthcare, individual genetic, psychosocial, phenotypic, and biomarker factors can be synthesized using AI to efficiently tailor disease prevention, diagnosis, treatment, and prognosis.
5 Clinical Capabilities of Healthcare AI
5 Clinical Capabilities of Healthcare AI
• Identification: Detecting patterns within data, often images (e.g., an early lung mass)
• Prediction: Forecasting events based on data and patterns (e.g., early recognition of sepsis)
• Summarization: Reviewing a large volume of records and efficiently summarizing key information necessary for clinical care
• Translation: Translating data into a another language or format to enhance communication
• Identification: Detecting patterns within data, often images (e.g., an early lung mass)

• Suggestion: Providing recommendations, guidance, or advice for action (e.g., based on continuous glucose monitoring patterns)
5 Clinical Capabilities
• Prediction: Forecasting events based on data and patterns (e.g., early recognition of sepsis)
• Identification:
• Summarization: Reviewing a large volume of records and efficiently summarizing key information necessary for clinical care
A word of caution
• Suggestion: Providing recommendations, guidance, or advice for action (e.g., based on continuous glucose monitoring patterns)
• Prediction:
• Translation: Translating data into a another language or format to enhance communication
• Summarization: information
• Translation:
With this abundance of data, there is a role for AI. AI is preferably called “augmented highlights the importance of having a “human in the loop.” Clinicians rely heavily AI augments the human ability to analyze and interpret vast, complex data, and precision healthcare, individual genetic, psychosocial, phenotypic, and biomarker synthesized using AI to efficiently tailor disease prevention, diagnosis, treatment,
Precision Healthcare: Tailor To The Patient
A word of caution

There is enthusiasm around the potential for ChatGPT and other large language models to decrease the administrative burden of generating office notes. Chatbots have potential to respond to patient inquiries. Which of these are among current limitations of using ChatGPT or other large language model tools in a clinical setting or for direct patient care?
A. Risk of incorrect and falsified responses
• Suggestion: continuous
A word of caution
There is enthusiasm around the potential for ChatGPT and other large language models to decrease the administrative burden of generating office notes. Chatbots have potential to respond to patient inquiries. Which of these are among current limitations of using ChatGPT or other large language model tools in a clinical setting or for direct patient care?
A. Risk of incorrect and falsified responses
B. Risk of bias, discrimination, promoting stereotypes, inequities
C. Risk of flawed training data
D. Impacts on data privacy
E. Liability
F. Absence of current regulation
G. All of the above
B. Risk of bias, discrimination, promoting stereotypes, inequities
C. Risk of flawed training data
D. Impacts on data privacy
see here
There is enthusiasm administrative burden inquiries. Which of tools in a clinical setting
A. Risk of incorrect
A survey by the American Medical Association (AMA) underscores that physicians’ priorities for AI adoption are to know if it will work, will it work in “my practice for my patients,” will insurance cover its use, and who is accountable if something goes wrong. In addition to its potential to assist on the administrative side of a practice, current clinical use cases of AI include its ability to identify high risk cardiology patients, recognize melanoma, assess blood pressure patterns on remote patient monitoring, detect stroke risk, improve detection of fetal abnormalities, analyze for diabetic retinopathy, enhance review of pathology specimens, detect critical illness earlier, auto-triage imaging exams, and more. Please see here.
E. Liability
F. Absence of current regulation
G. All of the above

B. Risk of bias, discrimination,
C. Risk of flawed
To learn more, please see here
D. Impacts on data
E. Liability
Correct answer: G
AMA policy is that “As the number of Augmented Intelligence (AI)-enabled health care tools and systems continue to grow, these technologies must be designed, developed, and deployed in a manner that is ethical, equitable, responsible, and transparent.”
F. Absence of current G. All of the above
AMA policy is that “As the number of Augmented Intelligence (AI)-enabled health care tools and systems continue to grow, these technologies must be designed, developed, and deployed in a manner that is ethical, equitable, responsible, and transparent.”

AMA policy is that continue to grow, ethical, equitable,
Precision healthcare, driven by AI, has the potential to improve effectiveness of patient care, enhance patient safety, and optimize patient outcomes. Central to patient-centered care are the patient’s values, personal goals, and level of function and support
A survey by the American Medical Association (AMA) underscores that physicians’ adoption are to know if it will work, will it work in “my practice for my patients,” use, and who is accountable if something goes wrong. In addition to its potential administrative side of a practice, current clinical use cases of AI include its ability cardiology patients, recognize melanoma, assess blood pressure patterns on remote detect stroke risk, improve detection of fetal abnormalities, analyze for diabetic review of pathology specimens, detect critical illness earlier, auto-triage imaging Please see here.


Precision healthcare, driven by AI, has the potential to improve effectiveness of patient care, enhance patient safety, and optimize patient outcomes. Central to patient-centered care are the patient’s values, personal goals, and level of function and support.
Precision healthcare patient safety, and personal goals, and
To watch a video of Dr. Heine’s related keynote for the Wilcoxon Innovation in Health Sciences Summit, please see here.
To watch a video of Dr. Heine’s related keynote for the Wilcoxon Innovation in Health Sciences Summit, please see here.
To watch a video of please see here.

In the Winter 2025 issue, there were montages of photos. Is that preferable? If space is limited, it may be preferable to include the scholarship donation request rather than the BCHIP engagement image.


The
Physicians’ Voice in Politics
JOIN PAMPAC HERE: www.PAMPAC.org

Thank you to the Bucks County Medical Society Members who were PAMPAC Members in 2025
Commonwealth Club
Marion Mass, MD | John Pagan, MD, FACS, MBA
Capitol Club
Judith Gallagher-Braun, MD | Marilyn Heine, MD, FACEP, FACP
Richard Leshner, DO | Mark Pappadakis, DO
Keystone Club
Robert Mirsky, MD | Rachael Sampson, MD
Mary Toporcer, MD
Sustainer Level
Arvind Cavale, MD, FACE, FCPP | Daniel Latta, MD
Steven Orland, MD
Other Contributors
John Gallagher, MD | Daniel Haimowitz, MD, CMP, FACP
Karl Helmond, MD, FACS | Bindukumar Kansupada, MD, MBA
David Levin, DO | David Pao, MD | Peter Schwartz, MD
Ann Showan, MD | Kathy Tran-Gast, DO | Joseph Werner, MD
Here are a couple of the many photos from the Bucks CMS Legislative Reception. If you think these will work, great; if not, I can send others. Between this and the next, all of the legislators are included. A simple caption could be: Bucks CMS members and state legislators enjoyed an evening of conversation to discuss issues important to physicians and patients.

Bucks County Medical Society celebrates unity with our community partners.

Bucks County Medical Society is proud to be a founding member of the Bucks County Health Improvement Partnership.
Bucks CMS delegation at the PAMED House of Delegates
With Senator Farry, at the Bucks CMS legislative reception
With Rep. Prokopiak and Rep. Hogan, at the Bucks CMS legislative reception
This Patient is Confused: Are They Having a Stroke?
“I’m Confused:” Is This Patient Having a Stroke?

Mark Pappadakis, DO, is an emergency physician from Bucks County.
By Mark Pappadakis, DO
Dr. Pappadakis is an emergency physician from Bucks County.
Emergency Medicine (EM) is often likened to “walking a minefield in clown shoes.” Undifferentiated patients with vague complaints present a high risk for misdiagnosis, a challenge amplified when metrics threaten to supersede clinical judgment. This is starkly evident is the patient with altered mental status (AMS), forcing the immediate question: Is this a stroke?
So while true ischemic stroke may not make up a large bulk of patients with AMS, it’s a diagnosis that needs to be respected. It’s also a diagnosis not to be made lightly, as deciding that a patient is having an ischemic event and giving thrombolytics can potentially cause harm. With Tenecteplase specifically, 20% of patients develop asymptomatic intracranial hemorrhage (ICH), with data showing anywhere from 1% to 6% of patients developing symptomatic ICH4 .
Emergency Medicine (EM) is often likened to “walking a minefield in clown shoes.” Undifferentiated patients with vague complaints present a high risk for misdiagnosis, a challenge amplified when metrics threaten to supersede clinical judgment. This is starkly evident is the patient with altered mental status (AMS), forcing the immediate question: Is this a stroke?
Consider two scenarios based on real cases. A nursing home patient, who presented to the emergency department (ED) with AMS, dysarthria, and ataxia, was last known to be “normal” within the 4-hour window for thrombolytics. The noncontrast CT is negative, vital signs are normal, and they are not on anticoagulants. With the door-toneedle clock ticking, do you push Tenecteplase?
These cases highlight the immense cognitive pressure on the EM physician. Anchoring, stereotyping, and confirmation biases loom before the patient is even fully examined. With metric-driven pressures mounting, the decision to treat can have lasting ramifications. The solution, however, is deceptively simple: step back and reexamine the patient without the noise.
Consider two scenarios based on real cases. A nursing home patient, who presented to the emergency department (ED) with AMS, dysarthria, and ataxia, was last known to be “normal” within the 4-hour window for thrombolytics. The non-contrast CT is negative, vital signs are normal, and they are not anticoagulants. With the door-to-needle clock ticking, do you push Tenecteplase?
A second patient, found by EMS in their apartment lobby, is reported as “intoxicated.” On arrival in ED, they appear to speak only Mandarin, but an interpreter reports their speech is incomprehensible. Given the initial report, is he simply placed in a hallway to sober up?
A second patient, found by EMS in their apartment lobby, is reported as “intoxicated.” On arrival in the ED, they appear to speak only Mandarin, but an interpreter reports their speech is incomprehensible. Given the initial report, is he simply placed in a hallway to sober up?
On examination, Patient 1 has jaundice and an abdominal fluid shift. Thrombolytics are held. Labs soon reveal coagulopathy and elevated ammonia — hepatic encephalopathy, not a stroke. In contrast, Patient 2 is found to have left-sided paralysis. A high suspicion for stroke prompts CT perfusion imaging, revealing a large vessel occlusion. After successful clot retrieval, his first words—in perfect English— were, “What happened?”
In 2002, it was estimated roughly 10% of all ER visits occurred due to AMS1. The number has increased, and the cause can be challenging to diagnose rapidly. Etiologies include trauma, hypoxia, infection, viral encephalopathy, nutritional deficiencies; psychosis has varied presentations. Depending on the region of the brain, stroke can account for 25% of patients presenting with AMS.2 A key driver of that diagnosis is lateralizing signs on neurologic exam3. Patients who present with nonlateralizing signs were found to have stroke mimics, including 23% vestibular dysfunction, 13% toxic/ metabolic, 13% seizure, 9% functional disorder, and 7% complex migraine3 .
These cases are potent reminders that cognitive biases remain a significant risk to both patient and physician. Clinical instinct shouldn’t be replaced by metrics and protocols, and patients never read the textbooks. These cases are potent reminders that cognitive biases remain a significant physician. Clinical instinct shouldn’t be replaced by metrics and protocols textbooks.
References:
References:




In 2002, it was estimated roughly 10% of all ER visits occurred due to AMS1. The number has increased and the cause can be challenging to diagnose rapidly. Etiologies include trauma, hypoxia, infection, encephalopathy, nutritional deficiencies; psychosis has varied presentations. Depending on the region the brain, stroke can account for 25% of patients presenting with AMS. 2 A key driver of that diagnosis lateralizing signs on neurologic exam3. Patients who present with non-lateralizing signs were found have stroke mimics, including 23% vestibular dysfunction, 13% toxic/metabolic, 13% seizure, 9% functional disorder, and 7% complex migraine3 .
So while true ischemic stroke may not make up a large bulk of patients with AMS, it’s a diagnosis that needs to be respected. It’s also a diagnosis not to be made lightly, as deciding that a patient is having ischemic event and giving thrombolytics can potentially cause harm. With Tenecteplase specifically, of patients develop asymptomatic intracranial hemorrhage (ICH), with data showing anywhere from to 6% of patients developing symptomatic ICH4 .
These cases highlight the immense cognitive pressure on the EM physician. Anchoring, stereotyping, confirmation biases loom before the patient is even fully examined. With metric-driven pressures mounting, the decision to treat can have lasting ramifications. The solution, however, is deceptively simple: step back and re-examine the patient without the noise.
BCHIP: The Power of Collaboration

BCMS Script sat down with Kimberly M. Permar, BS, MA, Executive Director of The Bucks County Health Improvement Partnership (BCHIP).
information and support. This was a partnership with Bucks County, local health systems, and community organizations.
Image change. Should be same size as original image, headshot.
BCMS Script: What is the mission of BCHIP?
Our mission at BCHIP is to provide leadership in Bucks County through collaboration, address gaps in health services, and improve the health of the community. When determining which programs to offer, we consider Board direction, partnership opportunities, available resources, and—most importantly—unmet needs within Bucks County.
BCMS Script: Bucks CMS is a founding member of BCHIP and a representative continues to serve on the BCHIP board. Who are the other BCHIP Board members?
Dr. David Damsker, Director of the Bucks County Department of Health, serves as chair of our Board. Our Board also includes the CEOs of all six Bucks County hospitals, along with leaders from the Bucks County Intermediate Unit, Bucks County Community College, Christ’s Home, Woods Services, Lenape Valley, and community members such as Vail Garvin and Charles Field. Their collective experience and guidance are essential to BCHIP’s work.
BCMS Script: What are some of BCHIP’s most successful initiatives?
Over the past 30 years, BCHIP has implemented numerous successful programs. Health and dental services program in Lower Bucks County met a significant need, but served only a small portion of the county, and changes in the healthcare environment ultimately led the Board to transition the program to St. Mary Medical Center.
In BCHIP’s countywide domestic violence awareness campaign, educational signage and resource cards were placed in restrooms across Bucks County, providing discreet access to
BCHIP’s greatest success has been expanding access to immunizations. We complement the Bucks County Department of Health by offering mobile vaccination services for homebound residents. We partner with local pharmacies to bring vaccines to vulnerable populations, including senior living facilities, shelters, senior centers, and school districts with high rates of unimmunized children. These services are provided at no cost; private funding is used to support underinsured and uninsured individuals.
BCMS Script: What are BCHIP’s priority endeavors for the near future?
Looking ahead, our priorities include sustaining existing services and identifying opportunities to address emerging healthcare gaps such as mental health advocacy. We support the Bucks-Mont Collaborative Advocacy Network to help address mental health and substance use disorder. BCHIP is committed to helping healthcare systems implement best practices in collaborative care and strengthening connections with community partners.
BCHIP has convened key stakeholders to address violence in healthcare settings. In partnership with the Bucks County District Attorney’s Office, local police departments, and hospital leaders, we are identifying resources and solutions to minimize violence to providers.
BCHIP provides several no-cost resources to support Bucks CMS members and their patients, including programs for Advance Care Planning, smoking cessation, and vaccinations. We continue to seek opportunities to collaborate with physician practices and connect patients to needed services.
The entire community benefits when healthcare organizations across the county work together. To learn more, please see: https://www.bchip.org/.

400 Winding Creek Blvd.
Mechanicsburg, PA 17050-1885
• The Bucks County Medical Society Board meets bimonthly. Bucks CMS members are welcome to attend Board meetings. For details, please contact buckscms@ pamedsoc.org
• SAVE THE DATE April 19, 2026 Annual Membership Meeting Location TBD

We thank you for your membership and welcome you to contact us anytime at buckscms@pamedsoc.org
