l e t t e r
e d i t o r
f r o m
t h e
i n c h i e f


l e t t e r
e d i t o r
f r o m
t h e
i n c h i e f

WRITER: AVANEESH TISGAONKAR | EDITOR:JAMES LEE
Abstract
Psychedelics are notable for their hallucination-inducing properties, and have been associated with an abusive party culture. However, recent research suggests thatpsychedelicspromoteneuroplasticity have therapeutic value. Psychedelics have been found to promote the growth of dendriticspikes,whichisduetotheirability enhance brain-derived neurotrophic factor (BDNF) levels. Due to their relative nonpolarity,psychedelicsareabletobindto intracellular 5-hydroxytryptamine 2A (5-HT2A) receptors, causing hallucinations. The ability of psychedelics to enhance neuroplasticity and induce subjective hallucinationexperienceslikelyisthebasis thetherapeuticbenefits,suchastheirability tocuredepressionoranxiety.Whilethereis cleartherapeuticvalueinpsychedelics,there ismuchthatstillneedstobeknown,before psychedelics can be used widely as therapeutictreatment.


KEYWORDS: Psychedelic, Neuroplasticity

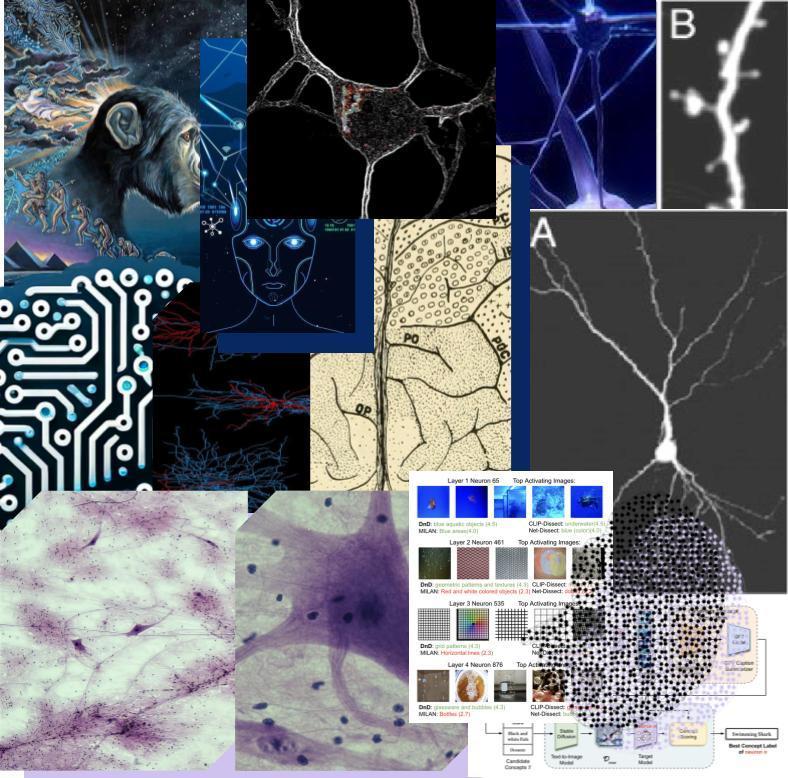
Psychedelicsareaclassofdrugsnotable for their ability to induce hallucinations and apparent expansions of consciousness [1]. The Stoned Ape Hypothesis, proposed by Terence McKenna in the 1970s, states that the consumption of psychedelic mushrooms byearlyhominidsinAfrica,over2million years ago, caused the doubling of the human brain’s size [2]. While the hypothesis may be far-fetched, recent research supports that psychedelics are indeed capable of promoting neuroplasticity, and have therapeutic value.
A study at the University of Southern Florida in 2013 found that low doses of psilocybin erased conditioned fear in mice [3]. To create this conditioned fear, the mice were shocked each time a certain audible tone was played [3]. Soon, whenever the mice would hear suchasound,theywouldsuddenlyfreeze — a fear response, because they had associated the sound with the correspondingshock[3].
Two groups of mice were in this experiment: one was given psilocybin, a psychedelic, and the other group was givenketanserin,acontrol[3].Whilethere was no difference in the time taken for either group to develop the conditioned fear, the psilocybin group took a significantly shorter time to forget the fear [3]. A similar study done in Beijing, also in 2013, also found that psilocybin facilitated the extinction of conditioned fears[4].
Such a result is thought to be due to psychedelics’ ability to promote the growthofdendriticspines,akeyagentin neuroplasticity,whichistheabilityofthe braintochangeitsactivityinresponseto intrinsic or extrinsic stimuli [5]. In 2021, Yaleresearchersfoundthatasinglesmall dose of psilocybin given to mice immediately caused a lasting increase in connections between neurons [6]. Alex Kwan, Associate Professor in the DepartmentofPsychiatryatYaleSchool of Medicine, reported a 10% increase in the number of neuronal connections, as wellasa10%increaseinthesizeofeach connection[6,7].Morespecifically,Yale’s researchers found that psychedelics like psilocybin increased the density of dendritic spines, which are small protrusions on neurons that are constantly changing in response to received stimuli [6]. In the Beijing study mentioned in the previous paragraph, researchers similarly found that psilocybin reversed the “decrease in hippocampal dendritic complexity and spine density” induced by the conditioned fear [4]. The increase in dendritic density translates to increased neuralconnectionandneuroplasticity.



Theabilityofpsychedelicstoenhance neuroplasticitycanbetracedtotheir abilitytoenhancebrain-derived neurotrophicfactor(BDNF)levels,which areknownfortheirfunctionin neuritogenesisandspinogenesis[8].A studyattheUniversityofCalifornia, Davisfoundthatpsychedelicscancause a100%increaseinBDNFproteinlevels[8]. WhenBDNF’sreceptor,Tropomyosin receptorkinaseB(TrkB),wasinhibited, psychedelicswerenotabletostimulate neurogenesisorspinogenesis[8].The abilityofpsychedelicstoenhance spinogenesis(whichisthegrowthof dendriticspikes)andneuritogenesis(the developmentofsmallprocessesor protrusionsthatformcomplexneural circuits)providethebasefor psychedelicstopromoteneurogenesis[9, 10].
Theabilityofpsychedelicstoinduce hallucinationsisduetotheiractivationof the5-hydroxytryptamine2A(5-HT2A) receptor.Serotoninalsobindsto5-HT2A, butdoesn’tinducehallucinationslike psychedelicsdo,becauseserotoninonly bindstothe5-HT2Areceptorsonthecell
surface(Serotoninishighlypolar,and thereforecannotpassthroughthe nonpolarcellmembrane)[11].Mostofthe 5-HT2Areceptorsinneuronsaremore insidethecell{seefigure3},unlikemost G-proteincoupledreceptors(GPCRs), whichareatthesurface[11].5-HT2A receptorsmoreontheinsideofthecell leadtodifferentcellularresponses. Psychedelics,whicharelesspolarthan serotonin,cancrossthemembraneand reach5-HT2Areceptorsontheinside, inducingtheprocessesthatcreate hallucinations[11,12].

Theabilityofpsychedelicstoinduce hallucinationsmaybethebasisfortheir therapeuticvalue.JohnsHopkins University(JHU)iscurrentlytakingin patientsintoaprogramthatinvolves psychedelictreatmenttoaddressmental healthissues.OnesuchpatientisTony Head,whohadbeenstrugglingwith anxiety,afterbeingdiagnosedwith prostatecancer.Afterapsychedelic, “mystical”experience,Headreports feeling“suchimmensepower”thatmade him“morecomfortablewithliving”and “Notafraidofdying”[13].Alasting, long-termdecreaseinanxietyand depression,forpeoplelikeHead, diagnosedwithcancer,cameonlyaftera significantsubjectiveexperience[14].
JHU’sresultsproposethattheabilityof psychedelicstoinducesubjective, “mystical”hallucinationsarewhatmake themsotherapeuticallybeneficial.
Mentaldisordersreducethebrain’s neuroplasticity;forexample,depression reducesthedensityofdendriticspineson nervouscells.Theabilityofpsychedelics, suchaspsilocybin,toenhancedendritic spines(asmentionedearlyoninthis article)andthereforeneuralconnections, maybewhatreversestheeffectsof mentalissuessuchassevereanxietyor depression.Therefore,psychedelic enhancingofneuroplasticitytranslatesto theirtherapeuticbenefit.Whilethereis cleartherapeuticvalueinpsychedelics, thereismuchthatstillneedstobe known,beforepsychedelicscanbeused widelyastherapeutictreatment.
[1]
https://www.merriam-webster.com/dictionary/psyc hedelic#:~:text=adjective-,1,the%20use%20of%20ps ychedelic%20drugs
[2]
https://www.zmescience.com/feature-post/historyand-humanities/anthropology-articles/stoned-ape-t heory-feature/
[3]
https://hscweb3.hsc.usf.edu/blog/2013/07/15/low-do ses-of-psychedelic-drug-erases-conditioned-fear-in -mice/
[4]
https://journals.lww.com/cmj/fulltext/2023/12200/psi locybin_facilitates_fear_extinction_in_mice_by.11.as px
[5]
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC640 0842/#:~:text=Neural%20plasticity%2C%20also%20k nown%20as,structure%2C%20functions%2C%20or%2 0connections.
[6]
https://news.yale.edu/2021/07/05/psychedelic-spurs -growth-neural-connections-lost-depression
[7]
https://medicine.yale.edu/psychiatry/profile/alex-k wan/
[8]
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC608 2376/
[9] https://en.wiktionary.org/wiki/spinogenesis
[10]
https://www.sciencedirect.com/topics/neu roscience/neurite#:~:text=Neurites%20are %20small%20processes%20on,the%20tip% 20of%20the%20neurite
[11]
https://cen.acs.org/biological-chemistry/n euroscience/psychedelic-compounds-stim ulate-neuronal-growth/101/web/2023/02
[12]
https://health.ucdavis.edu/health-magazi ne/issues/spring2023/features/psychedeli c-research-snapshots.html#:~:text=Serot onin%20itself%20is%20polar%2C%20mean ing,the%20interior%20of%20a%20cell.
[13] Fantastic Fungi
[14]
https://www.ncbi.nlm.nih.gov/pmc/article s/PMC8033615/


AUTHORS: Nicholas Bai*, Rahul Ajay Iyer*, Tuomas Oikarinen, and Tsui-Wei Weng *equal contributions
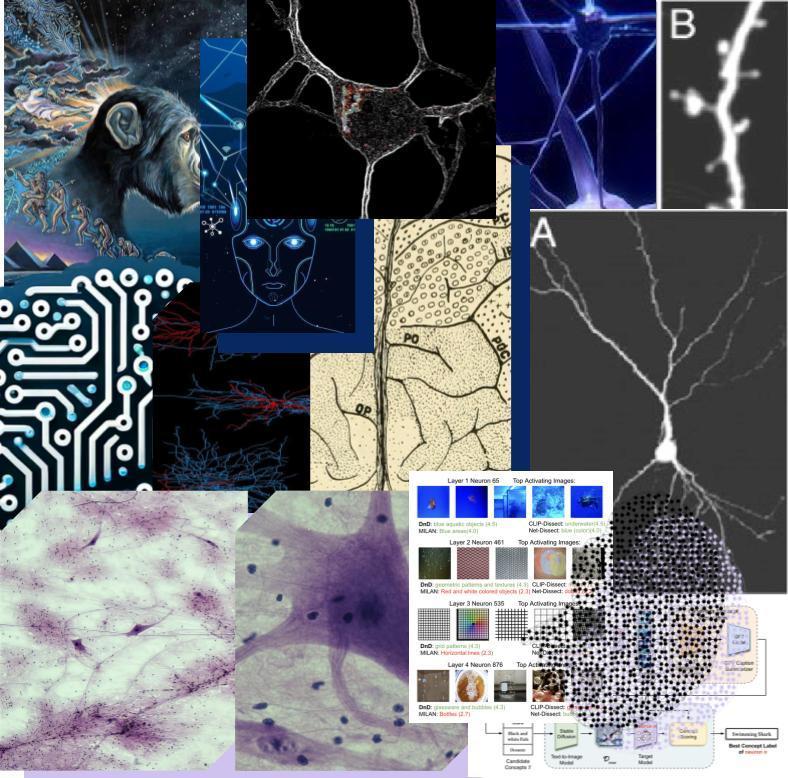
In this paper, we propose Describe-and-Dissect (DnD), a novel method to describe the roles of hidden neurons in vision networks. DnD utilizes recent advancements in multimodal deep learning to produce complex natural languagedescriptions,withouttheneedfor labeledtrainingdataorapredefinedsetof conceptstochoosefrom.Additionally,DnDis training-free, meaning we don’t train any newmodelsandcaneasilyleveragemore capable general purpose models in the future. We have conducted extensive qualitativeandquantitativeanalysistoshow that DnD outperforms prior work by providinghigherqualityneurondescriptions. Specifically, our method on average provides the highest quality labels and is morethan2×aslikelytobeselectedasthe bestexplanationforaneuronthanthebest baseline.
Recent advancements in Deep Neural Networks (DNNs) within machine learning have enabled unparalleled development in multimodal artificial intelligence. While thesemodelshaverevolutionizeddomains across image recognition and natural language processing, they haven’t seen much use in various safety-critical applications,suchashealthcareorethical decision-making. This is in part due to theircryptic“blackbox”nature,wherethe internal workings of complex neural networks have remained beyond human comprehension. This makes it hard to placeappropriatetrustinthemodelsand additional insight in their workings is neededtoreachwideradoption.
Previous methods have gained a deeper understanding of DNNs by examining the functionality (also known as concepts) of individual neurons1. This includes works based on manual inspection [3, 4, 9, 13], whichcanprovidehighqualitydescription at the cost of being very labor intensive. Alternatively, Network Dissection [1] automatedthislabelingprocessbycreat-
ing thepixelwiselabeleddataset,Broden, where fixed concept labels serve as ground truth binary masks for corresponding image pixels. While earlier works, such as Network Dissection, were restricted to an annotated dataset, CLIP-Dissect [8] offered a solution by no longerrequiringlabeledconceptdata,but stillrequiringapredeterminedconceptset asinput.MILAN[6]soughttoenhancethe quality of neuron labels by providing generative descriptions, but their method requirestraininganewdescriptionsmodel from scratch to match human explanationsonadatasetofneurons.


1We conform to prior works’ notation and use ”neuron” to describe a channel in CNNs.

Figure1.Neurondescriptionsprovidedby our method (DnD) and baselines CLIP-Dissect[8],MILAN[6],andNetwork Dissection [1] for random neurons from ResNet-50 trained on ImageNet. We includetheaveragequalityratingfrom our Amazon Mechanical Turk experiment next to each label and color-codedthedescriptionsbywhether we believed they are accurate, somewhatcorrectorvague/imprecise.
Figure 2. Overview of Describe-and-Dissect (DnD) algorithm. Given a Target model, it consiststhreeimportantstepstoidentifythe neuron concepts (e.g. ʻSwimming Sharkʻ for neuronn).

We present Describe-and-Dissect (DnD), a comprehensive method to produce generative neuron descriptions in deep vision networks. Our method is training-free,model-agnostic,andcanbe easilyadaptedtoutilizeadvancementsin multimodaldeeplearning.DnDconsistsof threestepsshowninFig.2:
• Step 1. Probing Set Augmentation: Augment the prob ing dataset with attention cropping to include both global andlocalconcepts;
• Step 2. Candidate Concept Generation: Generate initial concepts by describing highly activating images [7] and subsequently summarize them into candidateconceptsusingGPT3.5[2];
•Step3.BestConceptSelection:Generate newimagesbasedoncandidateconcepts and select the best concept based on neuron activations on these synthetic images[11]withascoringfunction.
Scoring Function. For a given neuron, we use a scoring function to rate candidate conceptaccuracy.Simplemetricssuchas mean are heavily prone to outliers that result in skewed predictions so we proposeascoringfunctionthatweights
the average rank of top activating images mapping to a candidate concept. Here,theaveragerankofimagesfor candidate concept j, ∀j ∈ {1,...,N}, is denoted Rj and Rank(Rj) sorts Rj in increasing order. E(I,Dt j) computes the average cosine similarity between image embeddings of Dt j andIusingCLIP-ViT-B/16[10],withDt j ⊂ Dj for t highest activating images.Inpractice,Rjiscomputedas the square of the ranks in top β ranking images for better differentiation between scores, Rj = {(Rij)2;i≤ β}.


Table 1. Averaged AMT results across layers in ResNet-50. Our descriptions are consistently rated the highest and chosen as the best more thantwiceasoftenasthebestbaseline.

Ourcrowdsourcingexperimentcompares the quality of labels produced by DnD against 3 baselines: CLIP-Dissect [8], MILAN [6], and Network Dissection [1]. We evaluate 800 randomly chosen neurons across 4 intermediate layers of ResNet50 on ImageNet [12]. Each neurons description is evaluated by 3 different workers. Shown in Table 1, DnD performs over 2× better than all baseline methods whendissectingResNet-50[5].Resultsfor an identical experiment using 200 randomlychosenneuronsforResNet18[5] trained on ImageNet and Places365 [14] yieldedsimilarresults,withameanrating of4.16andselected63.21%ofthetime.
We also follow CLIP-Dissect [8] to quantitatively analyze description quality on last layer neurons, which have known ground truth labels. Results show DnD outperformsMILANwithagreater
average CLIP cosine similarity by 0.0518, average mpnet cosine similarityby0.18.
Additional qualitative figures, ablation studies, use case examples, and evaluation on MILANNOTATIONS will be publicly available at our website after publication.
ThisworkissupportedinpartbyNationalScience Foundation (NSF) awards CNS-1730158, ACI-1540112, ACI 1541349, OAC-1826967, OAC-2112167, CNS-2100237, CNS-2120019, the UniversityofCaliforniaOfficeofthePresident,and the University of California San Diego’s California Institute for Telecommunications and Information Technology/Qualcomm Institute. Thanks to CENIC forthe100Gbpsnetworks.ThisworkusedExpanse CPU,GPUandStorageatSDSCthroughallocation CIS230152fromtheAdvancedCyberinfrastructure Coordination Ecosystem: Services & Support program, which is supported by National Science Foundation grants 2138259, 2138286, 2138307, 2137603, and 2138296. The authors thank REHS program (Research Experience for High School students)inSanDiegoSupercomputerCenter.This workisalsopartiallysupportedbyNationalScience Foundation under Grant No. 2107189 and 2313105, andHellmanFellowship.
[1]DavidBau,BoleiZhou,AdityaKhosla,AudeOliva, and Antonio Torralba. Network dissection: Quanti fying interpretability of deep visual representations. ComputerVisionandPatternRecognition,2017.1,2
[2] Tom B. Brown, Benjamin Mann, Nick Ryder, Melanie Subbiah, Jared Kaplan, Prafulla Dhariwal, Arvind Nee lakantan, Pranav Shyam, Girish Sastry, Amanda Askell, Sandhini Agarwal, Ariel Herbert-Voss, Gretchen Krueger, Tom Henighan, RewonChild, Aditya Ramesh, Daniel M. Ziegler, JeffreyWu,ClemensWinter,ChristopherHesse,Mark Chen, Eric Sigler, Mateusz Litwin, Scott Gray, BenjaminChess,JackClark,ChristopherBerner,Sam McCandlish,AlecRadford,IlyaSutskever,andDario Amodei. Language models are few-shot learners. CoRR,abs/2005.14165,2020.2
[3] Dumitru Erhan, Yoshua Bengio, Aaron Courville, andPascalVincent.Visualizinghigher-layerfeatures ofadeepnetwork.2009.1
[4] Gabriel Goh, Nick Cammarata, Chelsea Voss, ShanCarter,MichaelPetrov,LudwigSchubert,Alec Rad ford, and Chris Olah. Multimodal neurons in artificialneuralnetworks.Distill,6(3):e30,2021.1
[5] Kaiming He, Xiangyu Zhang, Shaoqing Ren, and Jian Sun. Deep residual learning for image recognition.InProceedingsoftheIEEEconferenceon computer vision and pattern recognition, pages 770–778,2016.2
[6]EvanHernandez,SarahSchwettmann,DavidBau, Teona Bagashvili, Antonio Torralba, and Jacob An dreas. Natural language descriptions of deep visual features. International Conference on Learning Representations,2022.1,2
[7]JunnanLi,DongxuLi,CaimingXiong,andSteven Hoi.Blip:Bootstrappinglanguage-imagepre-training for unified vision-language understanding and generation,2022.2
[8] Tuomas Oikarinen and Tsui-Wei Weng. Clip-dissect: Automatic description of neuron representations in deep vision networks. International Conference on Learning Representations,2023.1,2
[9]ChrisOlah,NickCammarata,LudwigSchubert, GabrielGoh,MichaelPetrov,andShanCarter.Zoom in:Anintroductiontocircuits.Distill,5(3):e00024001,2020.1
[10] Alec Radford, Jong Wook Kim, Chris Hallacy, Aditya Ramesh, Gabriel Goh, Sandhini Agarwal, GirishSastry,AmandaAskell,PamelaMishkin,Jack Clark, Gretchen Krueger, and Ilya Sutskever. Learning transferable visual models from natural languagesupervision,2021.2
[11] Robin Rombach, Andreas Blattmann, Dominik Lorenz, Patrick Esser, and Björn Ommer. High-resolutionimagesynthesiswithlatentdiffusion models,2022.2
[12] Olga Russakovsky, Jia Deng, Hao Su, Jonathan Krause,SanjeevSatheesh,SeanMa,ZhihengHuang, AndrejKarpathy,AdityaKhosla,MichaelBernstein,et al.Imagenetlargescalevisualrecognitionchallenge. Internationaljournalofcomputervision,115:211-252, 2015.2
[13]BoleiZhou,AdityaKhosla,AgataLapedriza,Aude Oliva, and Antonio Torralba. Object detectors emerge in deep scene cnns. arXiv preprint arXiv:1412.6856,2014.1
[14] Bolei Zhou, Aditya Khosla, Agata Lapedriza, AntonioTorralba,andAudeOliva.Places:Animage databasefordeepsceneunderstanding,2016.2
WRITER: HARRY JANG | EDITOR: RYAN MIN
Abstract
Integration of AI in the field of medicine has and is bringing tremendous improvement concerning patient treatment strategies, accuracy in diagnosis, and general efficiency within a health institution. For example, AI-powered tools such as learning algorithms and neural networks have improved the accuracy of diagnostics like cancer, and cardiovascular diseases, among many more. As far as patient treatment plans are concerned, these AI systems, by analyzing data and coming up with optimum pathways of treatment for specific, individual genetic profiles, will give better results for the patients. In addition, AI is making administrative processes easier, thus reducing the workload for healthcare professionals and minimizing human error in such processes.


KEYWORDS: AI, medicine, patient treatment strategies, accuracy in diagnosis, efficiency, AI-powered tools, machine learning algorithms, neural networks, diagnostics, cancer, cardiovascular diseases, patient treatment plans, big data, genetic profiles, administrative, processes, healthcare professionals, human error
Artificial intelligence in medicine has comealongwaysinceitsinceptioninthe 1950s. Some of the more notable early forerunners include the development of theMYCINsystematStanfordUniversity in 1972—a system that was a trailblazer regardingtheuseofartificialintelligence for the diagnosis of bacterial infections, andtheprescriptionofeffectivetherapy.
The 2000s marked development in the application of machine learning techniques and usage of large-scale datasets. AI systems gained a greater ability to analyze complex medical information, which gave better predictive analytics and personalized medicinaL approaches. During this period, there were noticeable early AI-drivendiagnostictoolsandsystemsas well. The decade paved the way for much more sophisticated applications in
Medical imaging and diagnostic capabilities have been highly modernizedatanexponentialrateinthe 2010'sduetorapidprogressexperienced in deep learning and neural networks. Convolutional neural networks, being a branchofneuralnetworks,sawparticular advancementinadvancedimage-based diagnosis capabilities when FDA-cleared equipment such as AI-based medical devices like Arterys Cardio DL and IDx-DR became available in 2017 for cardiac picture analysis and detecting diabeticretinopathy,respectively.

Artificial intelligence cuts across many areas of medicine, transforming diagnosis, personalizing the regimen of treatments,anddiscoveringnewdrugs.It also changes the way patients are administered, and receive care while makinghealthmanagementeffective.
TheeffectofAIonthefieldofmedicineis stronglywitnessedintheinterpretationof diagnostic imaging. AI algorithms study indetailthemedicalimagesproducedby X-rays, MRIs, and CT scanners. Quite obviously, these systems are optimal at picking up subtle abnormalities, thus helping the radiologist make diagnoses about anything from tumors to fractures muchquickerandwithgreateraccuracy; not only improving diagnostic accuracy viathiscapabilitybutalsoquickeningthe treatment pathways provided for patients, which in many disciplines, such as emergency medicine and oncology, is crucial.
AI has been incorporated in this field of pathology and histopathology to enable machines to complement pathologists in a way that the machines by screening the tissue samples for cancerous cells and other diseases. By learning from every pattern, whether small or big, to find minute patterns and deviations, AI manufactures uniformity in diagnoses which would otherwise be prone to humanbiasandhence,willeventuallybe uniformineveryrespect.
Moreover, AI-based personalized medicine is at the cutting edge of medical development. Leveraging data about patients, their genetic profiles, biomarkers, past medical cases, and even lifestyle factors, makes treatments more personalized. Employing such complex data sets, AI algorithms can predict how a patient will respond to a particular treatment applied, optimize therapeutic strategies, and even predict adverse reactions—if any—thereby making the treatment as effective as possible, while minimizing the risks involved.
In drug discovery and development, for instance, AI is making the typically cumbersome process of finding new therapies much easier. Large databases of molecular structures, genetic data, and clinical trial outcomes are being trawled using sophisticated computational techniques to identify potential new drug candidates. Machine learning models are used to model compound-biological target interactions thatleadtofastidentificationofpossible treatments for anything from cancer to infectious diseases. This possibility not onlymakesthediscoveryprocessfaster, but, more importantly, enhances success rates in clinical stages and brings new treatments to patients much more

Moving beyond the strictly clinical applications, AI expands patient access and engagement through virtual health assistants and chatbots. With almost unlimited access to the needed information and advice, such AI-powered assistance is available 24/7, answering questions about medications, scheduling appointments, and sending personalized health information, thus engaging patients and making healthcaremoreaccessible.
AI has made its way into the management of healthcare systems and revolutionized it. Because AI also allows for predictions of admission rates, optimization of staff schedules, and efficient resource allocation, hospital operations can also be optimized. This predictive capability is not only operational in efficiency but also allows time-effective and efficient healthcare provision to patients by healthcare experts.

Massivechallengesandethicalissuesare apparent in the integration of AI into healthcare.Firstofall,AIalgorithmsused in clinical decision-making need to be accurate and reliable. Biases found in many datasets result in skewed outcomes and are widening healthcare disparities, so addressing those biases is goingtobecriticalintreatingallpatients fairly. Another ethical question is the transparency of AI algorithms. They operate through very complicated procedures that may not be clear when such decisions are made. Such transparency brings into question accountability and understanding of the decisions made by AI’s, particularly in various life-or-death decisions involving medicineandhealth.
The use of AI in medicine brings about other critical questions involving the privacy of their information and the security of patients' data. AI technology depends on a vast amount of sensitive patient data, including medical records andevengeneticinformation.Thisshould not be violated, or excessively accessed and abused. Given the fast evolution of AI,regulatorsarefacinganewchallenge in that the current framework might not keep pace with technological improvements. Thereisaneedforearmarkedguidelines that will subject the applications of AI to a stringent assessment process for safety, efficacy, and ethics before eventual large-scale clinical practice. Such navigation will only be possible through collaborative efforts of healthcare professionals, policy framers, implementers,technologists,andethicists so that, ultimately, AI works to enhance healthcare while protecting the welfare ofpatientsandethicalintegrity.
AUTHOR: ARJUN DASGUPTA
Abstract
Asachronicandrelapsingdisorder, sharescertainneurobiologicalsubstrates the mesolimbic pathway, prefrontal cortex, etc.)withotherformsofrepetitivebehavior, yet also alters the brain circuit regarding reward, stress, and self-control. “Addictive” substances utilize certain transcription factors,likedeltaFosB,toinducechangesin the brain that reinforce such addiction throughanelevatedassociationbetweenthe craving of the substance and certain environmental cues in addition to triggering relapse. Drugs of abuse also modulate the homeostasis between glutamate and GABA toestablishphysicaldependenceonthe tolerance to the drug, and withdrawal symptoms.Theaforementionedneuroplastic changes comprise the neurobiology of addiction.


KEYWORDS: Addiction, Neurobiology
Bothanimalsandhumansrepeatactions that reward them, often in the form of pleasure. Addictive drugs are characterized by their enhancement of the brain’s “series” reward circuit (only onecurrentinthewholecircuit)thatruns throughthemedialforebrainbundleand, as a result, the ventral tegmental area (VTA), nucleus accumbens (NAc), and ventral pallidum. One of the salient functions of the circuitry is the regulation ofhedonictone(arepresentationofone’s capacity to experience pleasure), and hedonicdysregulationwithinthecircuitry oftenengendersaddiction.
The aforementioned reward circuit enhancement is the result of the drugs’ direct, indirect, and transsynaptic enhancement of the dopaminergic rewardsynapticfunctionintheNAc.The self-administrationofdrugstranspiresso thatdopamineintheNAcremainswithin acertainrangeandsothattheelevated hedonic level is maintained. The motives for the self-administration of drugs progresses away from the notion of “gettinghigh”andfeelingeuphoricto


seeking normalcy, and the addiction becomes a habit-driven behavior rather than reward-seeking. This change is reflected in the neuroanatomy of the brain through the shift from the NAc to the dorsal striatum as the addiction controlcenter.

Neuroplasticity,theabilityofthebrainto formandalterexistingsynaptic connections,asaresultofaddictioncan becategorizedintotwoformsbasedon thedrugusage:tolerancewithphysical dependence(presentwhenacertain drugistakenrepeatedly)andthe alterationstotherewardsystem (repercussionsofcompulsive drug-seekingbehavior).Toleranceisthe reducedefficacyofadrugdueto repeateduse,andphysicaldependence isdisplayedviawithdrawalsymptoms. However,neuroplasticitydueto compulsivedrug-seekingissignificantly morestableandpermanentthanits repetitioninducedcounterpart.
Inthisform,thebrainassociatesthe addictive(drug)experienceandthe dopaminewithenvironmentalcues, increasingtheprominenceofthedrug andthepotentialforfuturerelapseinthe process.Inadditiontoreportingcraving, brainimagingstudiesdisplayedan increasedbloodflowtoreward
pathways in (at least) one month sober addicts upon triggering drug-related cues for less than 30 milliseconds, which exemplifies the neuroplasticity engendered by compulsive drug-seeking. Repeated exposure to addictive drugs foments the accumulation of delta Fos B, a transcription factor (proteins that aid in transcribing DNA into RNA) involved in the development of motivated behaviors, throughout dopamine tunnels in the prefrontal cortex and NAc. Delta Fos B facilitates the development of short-term drug-induced neuroplasticity and motor response to repeated doses of a stimulant, yet delta Fos B levels subside once the drug is removed from the system.
Furthermore, animals exposed to addictive substances experience changes in their dendritic spine density. Stimulants (e.g. cocaine) increase such spine density in neural regions involving dopamine, such as the nucleus accumbens, which enhances the connectivity and communication between neurons in the region. Enhanced neural communication strengthens the neural circuits involved in drug-seeking behavior and reinforces addiction. On the other hand, depressants (e.g. morphine) conversely reduce dendritic spine density, especially in the VTA, which impairs synaptic connectivity while reducing general cognitive and emotional function.
Astheprimaryexcitatory neurotransmitterinthebrain,glutamate isintegralintheregulationofaddiction throughitsinvolvementinthemesolimbic dopaminepathway,whichincludesthe VTA,NAc,andprefrontalcortex.Uponits bindingtoglutamatereceptorson dopaminergicneurons,glutamate inducesthereleaseofdopamineintothe NAc.Glutamatereceptors,namelyNMDA (N-methyl-D-aspartate)andAMPA (��-amino-3-hydroxy-5-methyl-4-isoxaz olepropionicacid)receptorsalsoaffect synapticplasticity.NMDAreceptorsare bothligand-gatedand voltage-dependent,whichmakesboth glutamatebindingandpostsynaptic depolarizationrequisitefortheopening oftheirionchannels.
Thepostsynapticdepolarizationremoves themagnesiumionblockadeandenables theentranceofcalciumionsintothe channel.Avastinfluxofcalciumions (duetohigh-frequencystimulationof synapses)resultsinLTP(long-term potentiation),whichischaracterizedbya sustainedincreaseinsynapticstrength, whileasmallerinfluxofcalciumions(due tolow-frequencystimulation)induces LTD(long-termdepression),which weakenssynapticstrength.


Calciumionsbindtocalmodulin,and together,theyformacomplexthat activatesCaMKII(calmodulin-dependent proteinkinaseII).CaMKIIphosphorylates certainserineandthreonineresidueson thecytoplasmictailsofAMPAreceptor subunits,mostnotablyGluA1,which amelioratestheconductanceofthe AMPAreceptorandhencethereceptor’s synaptictransmission(byallowingmore sodiumionstoenterthepostsynaptic neuron).Furthermore,phosphorylated AMPAreceptorsaresignificantlymore likely(thantheirunphosphorylated counterparts)tobeinsertedintothe postsynapticmembraneviaexocytosis. AnincreasednumberofAMPAreceptors inthesynapticmembraneimproves synapticstrengthandcontributestoLTP. Conversely,thecalciumionand calmodulincomplexactivatescalcineurin (alsoknownasproteinphosphatase2B), whichcounteractsCaMKIIby dephosphorylatingtheserineand threonineresiduesonAMPAreceptor
subunits.Thisdephosphorylation decreasesthenumberofAMPA receptorsinthesynapticmembrane, weakenssynapticstrength,and contributestoLTD.Inadditionto activatingCaMKIIandcalcineurin,the calciumionandcalmodulincomplexalso activatesCaMKIV,whichdirectly phosphorylatesCREB(cAMPresponse elementbindingprotein),anuclear transcriptionfactorthatregulatesthe transcriptionofdownstreamgenes.


Additionally,thelargecascadeof calciumionsalsoactivatesadenylate cyclase,whichincreasescAMP(cyclic adenosinemonophosphate)levelsand activatesPKA,aproteinthatthen phosphorylatesCREB.Once phosphorylated,CREBbindstocAMP responseelementsinthepromoter regionsoftargetgenes,onebeingthe immediateearlygenes(suchasc-fos andArc)thatareinvolvedinsynaptic plasticityandneuronalactivity.CREBalso facilitatestheexpressionofgenesthat encodeproteinsinvolvedinsynaptic growth(e.g.brain-derivedneurotrophic factor)thatsupportthesurvivaland differentiationofneuronsandsynapse formation.TheactivationofCREBand subsequentgenetranscriptionassiststhe strengtheningofsynapsesandgrowth andrestructuringofdendriticspines, bothofwhichenhancesynaptic connectivityandcontributetoLTP. Regardingaddiction,addictivedrugs oftenenhanceglutamatergicsignalingin ordertoinduceLTPinrewardpathways (suchasthemesolimbicdopamine
pathway)viathephosphorylationof AMPAandCREBandreinforcethe motivationalsalienceofdrug-related cuesandbehaviors.
Whileglutamateistheprimary excitatoryneurotransmitter,GABA (gamma-aminobutyricacid)isthe primaryinhibitoryneurotransmitter throughitsactivationofbothGABA_A andGABA_Breceptors,which hyperpolarizeneuronsanddecrease overallneuronalactivity.GABAactsas thefeedbackmechanismforglutamate, asGABAergicneuronshave glutaminergicreceptorsandcan consequentlyhyperpolarizeneuronsin responsetoaninfluxofglutamate. Depressants(suchasalcohol)utilize GABAergicsignalingtoproducecalming andanxiolyticeffects.However,to compensate,non-depressantinduced GABAergicsignalingisreduced, engenderingahyperexcitablestateafter suddencessationofthedepressantalong withotherwithdrawalsymptoms (includingseizures,hypertension,and tremors).
Chronicexposuretodepressantsreduces thesensitivityandnumberofGABA_A receptorsinadditiontoanupregulationin NMDAreceptors,whichhinders GABAergicinhibitionwhilefortifying glutaminergicdopaminerelease.Asa result,addictionfrequentlyinvolvesa dysregulationoftheglutamate-GABA balance(e.g.anincreasein glutamatergicneuronfunctionanda decreaseinGABAergicneuronfunction


Drugsofabuseinducelong-lasting alterationstobrainfunctionand anatomythatreinforcethecycleof addictionandchallengeprolonged addictionsuppressionthroughchangesin dendriticspinedensity,the phosphorylationofAMPAandCREB,and dysregulationofthebalancebetween glutamateandGABA.Currently,drug addictionaffectsover46.8millionpeople intheU.S.A.(2022UnitedStatesNational SurveyonDrugUseandHealth),a numberthatwillonlygrow.An amelioratedcognizanceofthecausesof andneurobiologicalchangesrelatedto addictionfostersthedevelopmentof moreeffectivetreatmentsandthe proliferationofaddictionawareness, bothofwhicharerequisitetocombat widespreadaddiction.
[1] D’Souza, Manoranjan S.
“Glutamatergic Transmission in Drug Reward: Implications for Drug Addiction.” Frontiers in Neuroscience, vol. 9, 5 Nov. 2015, https://doi.org/10.3389/fnins.2015.00404.
[2] Gardner, Eliot L. “Addiction and Brain Reward and Antireward Pathways.” Chronic Pain and Addiction, vol. 30, 2011, pp. 22–60, www.ncbi.nlm.nih.gov/pmc/articles/PMC 4549070/, https://doi.org/10.1159/000324065.
[3] Kim, Bohye, et al. “Dopamine Depletion Alters Neuroplasticity-Related Signaling in the Rat Hippocampus.” Animal Cells and Systems, vol. 27, no. 1, 11 Dec. 2023, pp. 436–446, https://doi.org/10.1080/19768354.2023.229 4308. Accessed 13 June 2024.
[4] Nutt, David J, and Liam J Nestor. The GABA System and Addiction. 1 Oct. 2013, pp. 52–65, https://doi.org/10.1093/med/97801996857 07.003.0008.
[5] O’Brien, Charles P. “Neuroplasticity in Addictive Disorders.” Dialogues in Clinical Neuroscience, vol. 11, no. 3, 1 Sept. 2009, pp. 350–353, www.ncbi.nlm.nih.gov/pmc/article s/PMC3181920/.
[6] Rivière, Priscille. “Glutamate, a New Player in Addiction.” Inserm Newsroom, 4 Aug. 2015, presse.inserm.fr/en/glutamate-a-n ew-player-in-addiction/56109/. Accessed 13 June 2024.
[7] Shyu, Claire, et al. “Quantifying GABA in Addiction: A Review of Proton Magnetic Resonance Spectroscopy Studies.” Brain Sciences, vol. 12, no. 7, 13 July 2022, p. 918, https://doi.org/10.3390/brainsci120 70918.