OCTOBER 6–7, 2025
HILTON COSTA MESA

OCTOBER 6–7, 2025
HILTON COSTA MESA
TIME
SUNDAY, OCTOBER 5
4:00 pm–6:00 pm EARLY REGISTRATION Catalina Foyer
MONDAY, OCTOBER 6
7:30 am–4:30 pm REGISTRATION DESK OPEN Catalina Foyer
7:30 am–8:30 am CONTINENTAL BREAKFAST Fountain Terrace
7:30 am–4:30 pm EXHIBIT TABLES OPEN (setup 6:30 am)
8:30 am–9:00 am
9:00 am–10:15 am
Catalina Foyer
GENERAL SESSION: Summit Welcome
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California Catalina Ballroom
KEYNOTE: Leading With Love: Tackling Hard Problems and Breathing New Life Into Hospice
Ira Byock, MD, FAAHPM, Principal, Clinical Transformation Specialists
10:15 am–10:45 am BREAK WITH EXHIBITORS
BREAKOUT SESSIONS I (choose one)
Navigating Perils and Protecting the Potential of Hospice Care (Catalina Ballroom)
10:45 am–11:45 am
Utilizing Patient & Caregiver Voices to Promote Palliative Care (Newport Beach 2)
Can AI Scribes Improve Clinician Efficiency & Work–Life Balance in Supportive Care? (Laguna Beach 1-2)
Catalina Ballroom
Engaging Emotions to Strengthen the Therapeutic Relationship During Serious Illness (Laguna Beach 3)
Stronger Together: Integrating NeuroOncology and Pediatric Palliative Care at Diagnosis (Huntington Beach)
11:45 am–1:00 pm NETWORKING LUNCH Fountain Terrace
POLST eREGISTRY UPDATE AND BRIEFING
1:00 pm–1:45 pm
Kevin Chan, Branch Chief, State of California-Emergency Medical Services Authority, Health Information and Data Technologies Catalina Ballroom
1:45 pm–2:00 pm BREAK WITH EXHIBITORS
TIME
BREAKOUT SESSIONS II (choose one)
Navigating Conversations: Aid in Dying in Palliative Care Practice (Bristol 3)
2:00 pm–3:00 pm
Text-Based Support Throughout the Caregiver Journey: Bridging the Care Continuum From Diagnosis to Bereavement (Newport Beach 2)
Good to Go? How Do We Get Our Community to Care About and Attend End-of-Life Care Education? (Laguna Beach 1-2)
3:00 pm–3:30 pm BREAK WITH EXHIBITORS
GENERAL SESSION: ACP Innovation Award
UCLA Health Advance Care Planning Program
3:30 pm–4:45 pm
LOCATION
Innovative Training for Chaplains and Social Workers in Hospice and Palliative Care: A One-Year Residential Fellowship (Laguna Beach 3)
Pediatric Hospice: More Than the Sum of the Parts (Huntington Beach)
Neil Wenger, MD, MPH, Director, UCLA Health Advance Care Planning Program/ Professor, University of California, Los Angeles
Shirley Otis-Green, MSW, MA, ACSW, LCSW, OSW-C, Founder and Consultant, Collaborative Caring
5:00 pm–6:00 pm MOVIE NIGHT: “Going Your Way”
TUESDAY, OCTOBER 7
Catalina Ballroom
Catalina Ballroom
7:00 am–4:30 pm REGISTRATION DESK OPEN Catalina Foyer
7:00 am–8:30 am CONTINENTAL BREAKFAST Fountain Terrace
SPECIAL BREAKFAST SESSION: Results and Implications of the Statewide POLST Knowledge Survey
7:15 am–8:15 am
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
Catalina Ballroom
7:30 am–2:00 pm EXHIBIT TABLES OPEN Catalina Foyer
WELCOME BACK / HOUSEKEEPING
8:30 am–8:45 am
8:45 am–9:45 am
9:45 am–10:00 am
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
OPENING GENERAL SESSION: Reconstructing Palliative Care: A Beginning
Terry Altilio, LCSW, APHSW-C, ACSW, Consultant
Vickie Leff, LCSW, APHSW-C, Palliative Care Consultant
CCCC UPDATE
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
Catalina Ballroom
Catalina Ballroom
Catalina Ballroom
TUESDAY, OCTOBER 7 (continued)
10:00 am–10:30 am BREAK WITH EXHIBITORS
BREAKOUT SESSIONS III (choose one)
10:30 am–11:30 am
Rounding With Chaplains: Interprofessional Training Program for Whole Person Care (Newport Beach 2)
Integrating a Reconstruction Lens: Pain Management, Language, Culture, & Sustainability (Laguna Beach 1-2)
Humanity in Action: How Innovations in Prison Hospice Can Improve Care for All (Laguna Beach 3)
Bridging the Gap: A Hospital-Based Framework for Perinatal Loss Support (Huntington Beach)
11:30 am–12:30 pm NETWORKING LUNCH Fountain Terrace
12:30 pm–1:45 pm POSTER SESSION (See page 13 for poster descriptions and presenters) Bristol 3
1:45 pm–2:00 pm BREAK WITH EXHIBITORS
BREAKOUT SESSIONS IV (choose one)
Caring for Seriously Ill Patients in a Changing Climate (Newport Beach 2)
2:00 pm–3:00 pm
Improving Compassionate Communication Through an Arts and Humanities–Based Curriculum (Laguna Beach 1-2)
3:00 pm–3:15 pm BREAK
3:15 pm–4:30 pm
Leveraging Hybrid Palliative Care Models for Access in Rural Communities (Laguna Beach 3)
Reimagining Spiritual Care for Children on Hospice (Huntington Beach)
CLOSING PLENARY SESSION: Leading Through Change (And Out the Other Side): A Fireside Chat with Sachin Jain, MD, MBA, and Panel Discussion
Sachin Jain, MD, MBA, CEO, SCAN Group & Health Plan
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
Susan Wang, MD, FAAHPM, HDMC, National Director for Palliative Care, Kaiser Permanente
Lori Dangberg, Executive Vice President, Alliance of Catholic Health Care
Skelly Wingard, RN, MSN, PHN, CEO, By the Bay Health
Justin Baker, MD, FAAP, FAAHPM, Division Chief, Pediatric Palliative Care, Stanford Health Catalina Ballroom
Pediatric Palliative Care Look for the purple lettering throughout this program to easily find all sessions featuring highly relevant topics for those who work with children, adolescents, and young adults.
Welcome to CCCC’s Annual Summit!
Way back last fall, when we selected our theme for this year’s gathering, no one could have anticipated just how hard the problems facing us would be! On top of the usual pressures – an expanding aging population, a shrinking and burned-out workforce, ever-tighter reimbursement models, and pernicious bad actors scamming vulnerable patients – we now have catastrophic cuts to Medi-Cal and, by extension, Medicare, undermined community supports, and a state budget in the basement. Yikes.
But enough of hard problems – we’re here for the solutions! And the next two days will be full of exciting innovations, fresh approaches, and inspiring calls to action!

Our 18 breakout sessions and the Poster Presentations are rich with new information and actionable models for improving care. Our plenary sessions feature world-renowned clinicians and leaders with hopeful messages for how every one of us can make our work and our worlds better.
This year’s ACP Innovation Award will give you a blueprint for improving advance care planning across a large health system. For fun, and to offer you a useful community education tool, we’re hosting a Movie Night –complete with popcorn and soda and a book giveaway to top off the day.
One of the most anticipated new solutions is the POLST eRegistry! We are thrilled to have Kevin Chan from EMSA here to give us a walk-through of the interface and answer your questions.
And our exhibitors, whose support and presence really truly no kidding make this event possible, have great stories to tell and products and services to showcase. Be sure to give them a visit!
Jennifer Moore Ballentine, MA CEO, Coalition for Compassionate Care of California
• Articulate the dual clinical and cultural mission of hospice and palliative care.
• Dispel the myth that palliative care services cost health systems more than they contribute to the systems’ financial bottom lines.
• Overcome the prevalent reticence within our field to call ourselves by our real names – hospice and palliative care.
• Name three or more components of our field’s response to the current threats to hospice care.
• Describe two barriers to ACP addressed by UCLA’s ACP Program.
• Discuss how ACP document integration into the electronic health record helped increase document completion rates.
• Critique the historical influence of medical structures in palliative care with respect to unintended consequences.
• Apply foundational concepts from nonmedical scholars to the history of palliative care to mitigate unintended consequences and promote positive change in practice.
• Identify and define social science constructs that expand the medical viewpoint to address inequities, enrich practice, and contribute to sustainability in the work.
• Evaluate at least two impacts of changes in the healthcare landscape on your professional setting and practice.
• Demonstrate three qualities of conscious leadership.
• Apply at least one tangible action step to improve care for seriously ill patients in California.
Sunday, October 5
4:00–6:00 pm | EARLY REGISTRATION
Monday, October 6
7:30 am–4:30 pm | REGISTRATION DESK & EXHIBITS OPEN
7:30–8:30 am | CONTINENTAL BREAKFAST
8:30–9:00 am | GENERAL SESSION Summit Welcome
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
9:00–10:15 am | KEYNOTE
Leading With Love: Tackling Hard Problems and Breathing New Life Into Hospice
Ira Byock, MD, FAAHPM, Principal, Clinical Transformation Specialists
Despite demonstrating that much better care for seriously ill and dying people is both feasible and affordable, the transformative potential of hospice and palliative care remains unfulfilled. People living with life-threatening conditions and their families are still at risk of suffering from poorly managed symptoms, feeling bewildered and overwhelmed, and depending on over-stretched healthcare providers. Both access to and quality of hospice care are highly variable and inequitable. Multiple media exposés and government reports of fraud and abuse by hospice companies have damaged public confidence. Palliative care programs have proliferated unevenly and insufficiently to meet the needs of seriously ill Americans. Outdated accounting and faulty assumptions about the financial impact of palliative care continue to constrain our clinical capacity, workforce development, and program growth. Our field’s founding purpose and core values – and our successes – suggest a way forward. Dr. Byock offers a practical strategy with 5 key elements for addressing the hard problems we face and realizing our field’s dual mission of providing the best care for ill and dying people, and helping society integrate illness, caregiving, dying, and grieving within a continuum of living fully.
10:15–10:45 am | BREAK WITH EXHIBITORS
10:45–11:45 am | BREAKOUT SESSION I (Choose 1)
Perils and Protecting the Potential of Hospice Care
Ira Byock, MD, FAAHPM, Principal, Clinical Transformation Specialists (Moderator); Charles von Gunten, MD, Chief Medical Officer, The Elizabeth Hospice; Suzi Johnson, Board President, California Hospice and Palliative Care Association;
Craig Dresang, CEO, YoloCares; and Joycelyn Smart-Sanchez, MBA, PPSC, LCSW, Clinical Director, Medicare Advantage, UCLA Health
Our panel of clinical and administrative experts will address key challenges that California hospices face and discuss practical solutions. Topics will include: What more can our industry do to better protect vulnerable patients from unscrupulous hospice providers? What are reasonable caseloads for hospice nurses that ensure safe and effective care, while supporting nurses’ professional satisfaction? How can the public distinguish good hospices from bad ones, and excellent hospices from those that are mediocre? Can organizations develop preferred provider lists for discharge planners, referring physicians, as well as patients and families? Trends of diminishing hospice physician roles result in unmet patient needs, complaints about being unable to see a doctor, and hospice case managers feeling inadequately supported. Advance practice providers can fill most, but not all of the gap. What are ways to assure that hospice physicians can fully participate in IDT meetings, make patient visits when necessary, and be available in emergencies? For-profit hospice companies, including those that are publicly traded and private equity owned, are currently associated with higher margins, but lower quality. To what extent could clear clinical and programmatic standards, meaningful quality metrics, and quality-based competition diminish the importance of ownership?
Ann Cao-Nasalga, MBA, Program Coordinator, Stanford Health Care; Olivia Tigre Nerimora, MHA, Project Manager, Stanford School of Medicine; Grant Smith, MD, Palliative Care Physician, Stanford School of Medicine; Sheralin Samuels, Stanford Health Care
For over five years, the Stanford Palliative Care Community Partnerships Team has been dedicated to raising awareness and understanding of palliative care, particularly among underserved communities. Throughout our outreach, one message has remained constant: patient stories resonate deeply and meaningfully with audiences. In response, our team launched a storytelling project to highlight the value of palliative care through the voices of those who have lived it. We partnered with four individuals—patients and caregivers—who generously shared their personal journeys working with a palliative care team. Their stories were captured in a series of short, heartfelt videos designed to demystify palliative care, highlight its benefits, and foster trust and connection within the community. This session will showcase these four powerful videos and reflect on key lessons learned throughout the process. We will also hear directly from one of the participating caregivers, offering an intimate perspective on the impact of sharing her story and the support received through palliative care.
Finly Zachariah, MD, FAAFP, FAAHPM, FAMIA, Medical Director, Value-Based Supportive Care/Associate CMIO, City of Hope
This session will provide an overview of an AI scribe solution, how it works, some of the benefits and challenges for supportive care clinicians, and the impact the solution has had on efficiency and well-being for many clinicians at City of Hope. A demonstration utilizing the Microsoft Dragon Ambient eXperience (DAX Copilot) AI Scribe solution will be done live, with the output shown for a supportive care mock case. Opportunity to ask questions and have an open discussion will be provided.
Judy Thomas, JD, Consultant
Serious illness is not just a physical experience; it’s an emotional one as well. Science has started to reveal that emotional processing can be a therapeutic modality that increases patients’ sense of wellness. This session will delve into decoding emotions, accumulated emotional pain, multiple techniques for processing emotions, and more.
Kimberly Bower, MD, FAAHPM, HMDC, Attending Physician, Rady Children’s Hospital; JoAnne Auger, RN, CHPPN, Oncology Supportive Care Nurse Coordinator, Rady Children’s Hospital; Jennifer Elster, MD, Pediatric Neuro-Oncologist, Rady Children’s Hospital
In this session, we will review the progress that has been made in pediatric brain tumor diagnosis and treatment over the last decade. Neuro-oncology specialists will review new therapies and how these therapies have changed the prognosis in children with brain tumors. We will review the outcomes achieved in a joint palliative care and neurooncology program and discuss the key factors in creating effective collaboration between the palliative care and the oncology team.
11:45 am–1:00 pm | NETWORKING LUNCH
1:00–1:45 pm | GENERAL SESSION POLST eRegistry Update and Briefing
Kevin Chan, Branch Chief, State of California-Emergency Medical Services Authority, Health Information and Data Technologies
Since 2022, CCCC has been working closely with the California Emergency Medical Services Authority on the development and implementation of the California POLST eRegistry. We are thrilled to share that the Registry is currently undergoing internal testing and limited pilot review. This presentation will give our community a first-hand preview of the draft interface and description of how the Registry will facilitate creation, upload, and retrieval of POLST information for rapid, secure, and current access from any healthcare setting or in the field. This is also a unique opportunity to ask questions and provide valuable prime-user input to EMSA ahead of the official launch of the eRegistry.
1:45–2:00 pm | BREAK WITH EXHIBITORS
2:00–3:00 pm | BREAKOUT SESSION II (Choose 1)
Thalia
DeWolf, RN, BSN, CHPN, PHN, Hospice Outreach Coordinator and Nurse Education Coordinator, The Academy of Aid-in-Dying Medicine
We will explore techniques for facilitating nonjudgmental conversations about end-of-life wishes, including a patient’s desire for a hastened death. We will cover the legal criteria for aid in dying and delve deeper into the essential practical requirements that patients
need to understand to set realistic expectations. We will examine common barriers to accessing aid-in-dying care and discuss potential strategies to address them.
Text-Based Support Throughout the Caregiver Journey: Bridging the Care Continuum From Diagnosis to Bereavement
Melissa Lunardini, PhD, MA, MBA, FT, Chief Clinical Officer, Help Texts
This presentation addresses the critical gap in caregiver support during the transition from active caregiving to bereavement. A new text-based intervention offers an innovative SMS solution that provides seamless, continuous support across both phases, eliminating the typical service disruption that occurs after a loved one’s death. The program delivers personalized support messages twice weekly, beginning during active caregiving and continuing through bereavement without interruption. This approach reduces access barriers, prevents caregiver isolation, and supports better bereavement outcomes while providing healthcare organizations with a sustainable model for extended family engagement.
Patty Barnett Mouton, MSG, Vice President, Alzheimer’s Orange County; Vincent Nguyen, DO, CMD, Program Medical Officer, Palliative Care, Hoag Palliative Services
Since 2010, the OC POLST Coalition leadership has endeavored to educate and normalize conversations about serious illness and end-oflife decisions with community members and encourage appropriate use of the POLST document among clinical providers. Over the most recent years, special creative considerations to reach the community continued, and informed the evolving process of enticing people to attend programs discussing advance care planning and end-of-life issues. This session will detail innovative strategies to make education programs interesting and compelling for all audiences. We will use didactic, “show and tell” of promotional materials and marketing plans, as well as group discussions to explore how Orange County has consistently attracted attendance, particularly among clinicians, leveraged service providers as partners, and shared the unique and particularly successful collaborations with faith communities.
Glen Komatsu, MD, Chief Medical Officer, Providence Hospice Los Angeles; Matthew Bradley, MDiv, Chaplain, Providence Kids Care
Workforce shortages for well-trained clinicians in every discipline exist in hospice and palliative care. These fellowships, modeled after physician fellowships, were developed to address the shortage and offer fellowship training that is uncommon for chaplains and social workers. The presentation will describe the development and actualization of these fellowships, including the vision, pedagogy, and day-to-day experience of the fellows. Funding and maintenance of the fellowships also will be addressed.
Pediatric Hospice: More Than the Sum of the Parts
David Steinhorn, MD, FAAP, Pediatric Hospice Medical Director, Hinds Kids (Hinds Hospice); Rebecca Simonitsch, MSGH, MAEd, Quality Initiatives Program Manager & Partner for Kids Lead, Cottage Health; Kieran Shah, CHPCA, President/CEO, VNA Health; Michael Cruse, MSW, LCSW, Manager, Children’s and Family Services, Hospice of Santa Barbara
The presentation will describe the process utilized by multiple existing agencies in Santa Barbara County to create a cohesive pediatric home hospice and palliative care program where none previously existed. The process of assessing needs, identifying existing resources, developing a collaborative partnership, educating providers, and creating referral mechanisms will be discussed. This process demonstrates the result is more than simply the sum of individual parts. Lessons learned will be presented.
3:00–3:30 pm | BREAK WITH
3:30–4:45 pm | GENERAL SESSION ACP Innovation Award
UCLA Health Advance Care Planning Program
Neil Wenger, MD, MPH, Director, UCLA Health Advance Care Planning Program/Professor, University of California, Los Angeles; Shirley Otis-Green, MSW, MA, ACSW, LCSW, OSW-C, Founder and Consultant, Collaborative Caring
Implementing an advance care planning (ACP) program within a health system is complex. This presentation will outline how UCLA Health used an implementation science approach to target barriers to ACP by developing innovative approaches to advance directive accessibility and understandability, specification of unofficial surrogates, ACP document integration into the electronic health record, consultation to facilitate the ACP process, and continuity of ACP decisions. Presenters will also discuss how innovations implemented by the ACP Program are incrementally changing the culture of the health system to promote ACP throughout the trajectory of illness, aiming to increase ACP until the measured outcome is goal-concordant care.
5:00–6:00 pm | MOVIE NIGHT
Going Your Way
Top off the day with popcorn, soda, and a movie! By special arrangement with 9 PBS, St. Louis, we are pleased to present “Going Your Way,” a new PBS documentary that explores the personal, medical, and spiritual aspects of end-of-life care. This 55-minute film, an homage to Bill Moyers’ landmark “On Our Own Terms,” is a valuable public education resource, which can be licensed for screenings to foster conversation, provoke discussion, and introduce hospice and palliative care services to your community. Attendees will have an opportunity to participate in a giveaway of books authored by our plenary speakers.
Tuesday, October 7
7:00 am–4:30 pm | REGISTRATION DESK OPEN
7:00–8:30 am | CONTINENTAL BREAKFAST
7:15–8:15 am | SPECIAL BREAKFAST SESSION
Results and Implications of the Statewide POLST Knowledge Survey
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
In anticipation of the launch of the POLST eRegistry, CCCC undertook to assess the current state of understanding of POLST to focus educational and operational efforts to support the registry. The survey comprised 4 demographic questions and 19 multiple-choice knowledge questions testing respondents’ knowledge of the POLST form and process across 4 competencies. CCCC engaged numerous associations and healthcare partners to deploy the survey and encourage completion: 3,247 surveys were completed by clinicians and administrators representing a broad array of disciplines and settings and confirming concerns that gaps in knowledge and practice persist, risking real patient harm. This session will present top-level results and selected details, their implications for success of the POLST eRegistry, and recommendations for process improvement across all settings of healthcare in California.
7:30 am–2:00 pm | EXHIBITS OPEN
8:30–8:45 am | GENERAL SESSION Welcome Back / Housekeeping
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
8:45–9:45 am | OPENING GENERAL SESSION Reconstructing Palliative Care: A Beginning
Terry Altilio, LCSW, APHSW-C, ACSW, Consultant; Vickie Leff, LCSW, APHSW-C, Palliative Care Consultant
Palliative practice has prioritized a medical model over the contributions of social science and the humanities. Social work and other disciplines, too, have tended to mirror traditional medical constructs without actively challenging inequities. This plenary will propose expanding this viewpoint to create new strategies and accentuate new connections in policy and practice. We will examine educational and professional practice with discussions around teams, power relationships, environmental contexts, and social determinants of health. The goal is to provide equitable care to patients, families, and the community while remaining true to ourselves. Our discussion engages many nonmedical thinkers to push us past traditional models, challenge assumptions, and invite advocacy to strengthen our perspective and reconstruct the practice of palliative and end-of-life care.
9:45–10:00 am | GENERAL SESSION CCCC Update
Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California
10:00–10:30 am | BREAK WITH EXHIBITORS
10:30–11:30 am | BREAKOUT SESSION III (Choose 1)
Rounding With Chaplains: Interprofessional Training Program for Whole Person Care
Nadya Dimitrov, DPM, PA-C, DFAAPA, Clinical Associate Professor, Stony Brook University, NY/Physician Associates in Hospice and Palliative Medicine (PAHPM); Rebekah Halpern, PA-C, MPAS, DFAAPA, Physician Assistant, Children’s Hospital Los Angeles; Rev. Joshua Morris, PhD, BCC, Assistant Professor, Practical Theology, Union Presbyterian Seminary Palliative care guidelines for training in spirituality include an assessment of spiritual distress. There are few tools that incorporate an interprofessional reciprocal learning approach. This curricular innovation demonstrates an enhanced training experience using evaluations, debriefing, narrative medicine, and reflection. A pediatric chaplain, pediatric palliative care clinician, and a faculty preceptor who have been involved in this type of work will incorporate a didactic presentation and role playing in this unique, interactive breakout session.
Integrating a Reconstruction Lens: Pain Management, Language, Culture, & Sustainability
Terry Altilio, LCSW, APHSW-C, ACSW, Consultant; Vickie Leff, LCSW, APHSW-C, Palliative Care Consultant
This breakout session will focus on specific aspects of serious illness practice such as pain management, language, and word choice in conversation, documentation, and policy linking to inequities and unintended harms. The intention is to broaden the medical and palliative care perspective by moving from an individualized focus to one that disrupts assumptions, engages culture and community, and promotes the responsibility to create environments that are sustainable for staff and honor unique lives and values of patients and families. Using expanded perspectives to help us understand our professional strengths and opportunities will bring new energy to our day-to-day practice.
Laura Musselman, Director of Development and Communications, Humane Prison Hospice Project; Elena Tootell, MD, Physician, San Quentin Rehabilitation Center; Alison Pachynski, MD, Chief Medical Executive, San Quentin Rehabilitation Center
This session explores peer-led approaches to end-of-life care and planning in California prisons. Presenters will share a trauma-informed model that trains incarcerated individuals as palliative caregivers, and highlight efforts at San Quentin where Certified Peer Support Specialists guide advance directive conversations. Both approaches emphasize the power of peer connection to build trust, foster agency, and improve health outcomes for incarcerated individuals facing aging, serious illness, or end-of-life concerns. In addition to detailing these innovative programs, speakers will share what their experience has to tell us about improving advance care planning and caregiving in any setting.
Lisa Westrich, LCSW, Social Work Clinician – Bereavement, Stanford Medicine Children’s Health; Ana Stafford, LCSW, Manager, Family Guidance and Bereavement Program, Stanford Medicine Children’s Health
Perinatal loss is often met with silence and stigma, leaving many families to navigate disenfranchised grief alone. This session presents an innovative, hospital-based approach to addressing gaps in perinatal bereavement care after discharge. Drawing on clinical best practices and case studies, it explores early identification, coordinated followup, and family-centered interventions by trained clinicians. Attendees will explore real-world examples and learn how proactive, culturally responsive support can validate grief, promote healing, and close gaps in care for families who are too often overlooked.
11:30 am–12:30 pm | NETWORKING LUNCH
12:30–1:45 pm | POSTER SESSION
(See page 13 for poster descriptions and presenters)
1:45–2:00 pm | BREAK WITH EXHIBITORS
(Exhibits close at 2:00 pm)
2:00–3:00 pm | BREAKOUT SESSION IV (Choose 1)
Caring for Seriously Ill Patients in a Changing Climate
Aldebra Schroll, MD, Associate Director, Healthy Rural California Family Medicine Residency
Climate change exacerbates negative health outcomes, particularly for people with complex medical issues. This session will delve into the profound impacts of extreme weather events and climate-related disasters. Real-world narratives will highlight key challenges. We will also discuss actions HPC organizations can take to prepare for climaterelated disasters. As HPC professionals, we are accustomed to building interdisciplinary care teams, working with uncertainty, complex problem solving, and advocating on behalf of our patients.
Gary Buckholz, MD, HMDC, FAAHPM, Director, UC San Diego Institute for Empathy & Compassion; Kimberly Bower, MD, FAAHPM, HMDC, Attending Physician, Rady Children’s Hospital Participants will (1) Learn the difference between empathy and compassion, hear some key compassion statistics, and how education has been developed and administered to shift culture at UC San Diego Health through the Sanford Institute of Empathy and Compassion. (2) Experience one arts and humanities–based exercise to improve perspective-taking and narrative humility while avoiding the ladder of inference. (3) Complete a private written reflection. (4) Gain access to a free 150-page facilitation guide.
Michelle Ward, MSN, ANP-BC, ACHPN, Chief Operations Officer, Vynca
Delivering palliative care in rural communities poses challenges—from provider shortages to geographic and cultural barriers. This session explores a hybrid model combining in-person care with technologyenabled solutions to improve access and patient experience. Learn how AI-driven insights, remote monitoring, predictive analytics, and asynchronous data collection—such as symptom tracking and caregiver input—enable earlier complication detection, faster intervention, and better care coordination. The result: fewer hospitalizations, timely symptom management, and more consistent, compassionate support for patients and families in rural settings.
Glen Komatsu, MD, Chief Medical Officer, Providence Hospice Los Angeles; Matthew Bradley, MDiv, Chaplain Providence Kids Care
Spiritual care guidelines for children in hospice and palliative care tend to reflect an adult perspective of spiritual care. This session will explore what could constitute spirituality and spiritual care for readying children in the context of their lives and families. The presentation will be reflections of what constitutes spiritual care for children in terms of focus, methodologies, and overlap with other disciplines. Case studies and examples of spiritual care interventions will be presented for discussion.
3:00–3:15 pm | BREAK
3:15–4:30 pm | CLOSING PLENARY SESSION
Leading Through Change (And Out the Other Side): A Fireside Chat with Sachin Jain, MD, MBA, and Panel Discussion
Sachin Jain, MD, MBA, CEO, SCAN Group & Health Plan; Jennifer Moore Ballentine, MA, CEO, Coalition for Compassionate Care of California (Moderator); Susan Wang, MD, FAAHPM, HDMC, National Director for Palliative Care, Kaiser Permanente; Lori Dangberg, Executive Vice President, Alliance of Catholic Health Care; Skelly Wingard, RN, MSN, PHN, CEO, By the Bay Health; Justin Baker, MD, FAAP, FAAHPM, Division Chief, Pediatric Palliative Care, Stanford Health 2025 has brought an extraordinary cascade of change to healthcare. From the decimation of the federal healthcare administration workforce, defunding and reshuffling priorities for health research, acceleration of technological transformations in business and clinical practice, aggressive immigration enforcement impacting patients and healthcare workers, to the immediate and expected massive reductions to Medicaid and community-based supports stemming from H.R. 1, we are all feeling whiplashed and disoriented. As leaders and frontline professionals, we must forge ahead, finding brain space and energy to craft new solutions to hard problems and provide encouragement to our colleagues and the patients and families we serve. To help us find our footing, our closing plenary will feature a fireside chat with Sachin Jain of SCAN Group & Health Plan and a panel of strong voices representing our cross-sector membership. Dr. Jain, among many professional accomplishments, writes frequently in trade publications and online about the challenges and rewards of conscious leadership and has a perspective forged by in-the-trenches work and high-level roles. Our panelists will help bring his insights into our community’s context and send us home inspired with renewed hope and action steps we can all take in positive directions until we meet again.
The Coalition for Compassionate Care of California promotes high-quality, compassionate care for all who are seriously ill or nearing the end of life.
We envision a future where people can live their best lives possible during serious illness.
Our mission is to make conversations about serious illness a part of everyday life and palliative care a part of everyday health care.
Creating this change is bigger than any one individual or organization can achieve on their own. It requires systems change.
Continuing education (CMEs/CEs) are provided for full-day attendance. Partial-day credit is not available, except for disciplines that are self-reporting. All attendees must sign in with their professional license numbers on the morning of each day of the Summit. In order to receive credit, participants also must complete an online survey within 14 days following the Summit. Continuing education certificates will be sent via email. Certificates of attendance can be requested by signing up at the CE/CME table. Note: A 50-minute minimum of uninterrupted time is required to qualify for 1 hour of CME/CE credit. Continuing education excludes lunch and break periods.
PHYSICIANS & PHYSICIAN ASSISTANTS
NURSES
SOCIAL WORKERS & COUNSELORS
CHAPLAINS
Application has been made to the AAFP for CME approval. CME credits are sponsored by Partnership HealthPlan of California.
This course meets the qualifications for 9.25 contact hours. This provider is approved by the California Board of Registered Nursing, Provider #CEP 15403.
This course meets the qualifications for 9.25 hours of continuing education credit for LMFTs, LCSWs, LPCCs, and/or LEPs as required by the California Board of Behavioral Sciences. CCCC is approved by the California Association of Marriage and Family Therapists to sponsor continuing education for LCSWs and LMFTs, Provider #91987.
This program may be used for continuing education credit for chaplains certified with the Board of Chaplaincy Certification, Inc.
We applaud the Coalition for Compassionate Care of California’s mission and are proud to be a sponsor of the Annual Summit.


Terry Altilio is a palliative social worker with over 30 years of direct practice in acute care settings. She is a recipient of a Mayday Pain and Society Fellowship Award 2006 and a Social Work Leadership Award from the Open Society Institute’s Project on Death in America to support a social work postgraduate fellowship, which continued through 2024, and a social work listserv which currently networks 975 social workers. In 2013, she was selected to receive the Project on Death in America, Career Achievement Award from the Social Work Hospice and Palliative Network. Ms. Altilio lectures nationally and internationally on topics such as pain management, ethics, palliative care, language and psychosocial issues in serious illness care, teaches in post-Master’s programs at NYU, Smith, and is guest faculty in an online course through the CSU Shiley Haynes Institute for Palliative Care. In addition to co-authored journal publications, she is co-editor of the second edition of the Oxford Textbook of Palliative Social Work, 2022, and co-editor of Palliative Care – A Guide for Health Social Workers published in 2019. Most recently she has co-edited Mirrors & Windows: Reflections on the Journey of Serious Illness Practice.
Ira Byock is a leading medical authority, author, and public advocate for improving care for people living with serious medical conditions. Dr. Byock is an active emeritus professor of Medicine and Community & Family Medicine at Dartmouth’s Geisel School of Medicine. During his clinical career, he earned specialty certifications in Family Medicine, Emergency Medicine, and Hospice & Palliative Medicine. Dr. Byock has been involved in hospice and palliative care since 1978, and is a past president of the American Academy of Hospice and Palliative Medicine. In 2014, he founded the Institute for Human Caring within the multistate Providence health system. The Institute drives transformation to make caring for whole persons the new normal. Since leaving his position with the Institute in 2022, Dr. Byock is the principal consultant for Clinical Transformation Specialists PLLC, which advances highly personalized care as a values strategy for American healthcare. Dr. Byock has authored numerous articles in academic journals and several highly acclaimed books, including Dying Well, The Four Things That Matter Most, and The Best Care Possible. His research has contributed to conceptual frameworks for the lived experience of illness, developed measures for subjective quality of life, and refined counseling methods for life completion and well-being. Dr. Byock is a national and internally recognized speaker.
Chief Executive Officer of SCAN Group and SCAN Health Plan

read by healthcare leaders. He has been recognized by Modern Healthcare as one of the “100 Most Influential People in US Healthcare” and by LinkedIn as its top voice for healthcare industry-related content.
Vickie Leff, LCSW, APHSW-C

Vickie Leff is a palliative care consultant and an adjunct instructor at Yeshiva University, Wurzweiler School of Social Work. With over 35 years of clinical practice experience in oncology, palliative care, and hospice, she presents on topics such as moral distress and sustainability to several national educational organizations and institutions. Recently she served as the executive director of Social Work Hospice and Palliative Care Network (SWHPN) and prior to that as the executive director of the Advanced Palliative Care & Hospice Social Work Certification (APHSW). Her work has been published in Health Affairs, the Journal of Pain and Symptom Management (JPSM), Journal of Palliative Medicine, and other journals. She is on the editorial board of Social Work in Health Care Journal and is a member of the Board of Directors for the Center for Practical Bioethics. She is co-editor of the book Mirrors & Windows: Reflections on the Journey in Serious Illness Practice and co-author of Helping Children Cope When Someone They Love Has a Serious Illness. She earned her Master of Social Work from Simmons School of Social Work.
Shirley Otis-Green, MSW, MA, ACSW, LCSW, OSW-CE, FNAP, FAOSW
Founder and Consultant, Collaborative Caring
Shirley Otis-Green’s career is dedicated to enhancing excellence in the delivery of contextualized care to address the symptoms and stress of serious illness. Her education, research, and consultation efforts focus on quality of life, palliative care, and transformational leadership. As principal investigator on studies with over $3.5 million in external funding, her work has been disseminated through more than 100 publications and 500 professional presentations. She is a California Health Care Foundation Leadership Fellow, a fellow of both the Association of Oncology Social Work and National Academies of Practice, and is a National Association of Social Workers Pioneer. Ms. Otis-Green was among the first to receive an international, interprofessional Master of Arts in Health Research/Palliative Care from Lancaster University in Great Britain and is co-editor of the Oxford Textbook of Palliative Social Work


Sachin H. Jain, MD, MBA, is CEO of SCAN Group and Health Plan. Under Dr. Jain’s leadership, SCAN was rated #1 in customer satisfaction among Medicare Advantage plans in California by J.D. Power; received 4.5 STAR ratings six years in a row; launched a range of new products; and expanded its operations into four states. From 2015–2020, Dr. Jain was president and CEO of CareMore Health and Aspire Health, and prior to joining CareMore, was Chief Medical Information & Innovation Officer at Merck & Co. He also served as an attending physician at the Boston VA–Boston Medical Center and as a faculty member of Harvard Medical School and Harvard Business School. From 2009–2011, Dr. Jain was senior advisor to the administrator of the Centers for Medicare & Medicaid Services (CMS), as the first acting deputy director for policy and programs at the Center for Medicare and Medicaid Innovation (CMMI), and as special assistant to the National Coordinator for Health Information Technology. Dr. Jain earned his MD from Harvard Medical School and MBA from Harvard Business School. He trained in medicine at the Brigham & Women’s Hospital and is board certified in Internal Medicine. He is an adjunct professor of Medicine at the Stanford University School of Medicine and a practicing academic hospitalist with the U.S. Department of Veterans Affairs. A respected thought leader in healthcare, Dr. Jain’s columns for Forbes are widely
Neil S. Wenger, MD, MPH
Director, UCLA Health Advance Care Planning Program and Professor, University of California, Los Angeles

Neil Wenger is a professor in the Division of General Internal Medicine and Health Services Research at the University of California, Los Angeles and a practicing general internist with an interest in patients with complex illness. He also leads the Advance Care Planning and Services initiative. At RAND, he is a senior scientist and directed the Assessing Care of Vulnerable Elders (ACOVE) project. Dr. Wenger’s current efforts focus on building health system-level advance care planning structures and on measuring and improving the quality of care for vulnerable older persons. Dr. Wenger’s educational efforts focus on training physician fellows in health services and primary care research, training resident physicians in primary care general internal medicine, and teaching clinical ethics. He directs the HRSA-funded National Research Service Award Primary Care Research Fellowship in the Division of General Internal Medicine at UCLA. Dr. Wenger received his MD from the UCLA School of Medicine and his MPH from the UCLA School of Public Health.
The Irreducible Complexity of Advance Care Planning:
Navigating the Path to Goal Concordant Care, Erin Schweppe, MSN, RN, CNML, ACM, Denise Morse, MBA, Amis Christian, Valerie Rhea, MPA, FACHE, Carmen Geurrera, Christina Cabanillas, LCSW, and Finly Zachariah, MD, FAAFP, FAAHPM, FAMIA, City of Hope
Bridging Gaps: A Population Health Approach to Palliative Care Coordination, Michelle Curioso, BSN, MPA, Kern Health Systems
Interventions to Enhance Symptom Management and Quality of Care in Hospitalized Patients at the End-of-Life: A Scoping Review, Andrea M. Yeung, BA, Max T. Hukill, AB, Scott Y. Johnson, EdD, MLIS, AHIP, Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena; Susan E. Wang, MD, Department of Geriatrics and Palliative Medicine, Kaiser Permanente Southern California; Andre Cipta, MD, Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, & Department of Geriatrics and Palliative Medicine, Kaiser Permanente Southern California
Creation of an Acute Supportive Care Clinic at City of Hope Comprehensive Cancer Center and Patient Outcomes, Joseph Vega, DO, Jennifer Baecker, NP, Kumkum Mehta, NP, Navneet Kaur, MD, Stefanie Mooney, MD, and Adeboye Ogunseitan, MD, Department of Supportive Care Medicine, City of Hope
Early Palliative Care in Congestive Heart Failure Patients, Beverly Balfe, RN, Jenifer Tantarelli, FNP, Meadow Stempek, ACNP, Providence, Santa Rosa Memorial Hospital
CNSs in Long-Term Care: An Innovative Use for a Diverse Role, Jeannette Meyer, BSN, MSN, UCLA Health; Nerina Girasol, DNP, MPH, MSN, Hilltop Health Group; and Jennifer Manning, DNS, ACNSBC, CNE, FCNS, LSUHSC School of Nursing
Assessing Distress in Patients with Developmental Delay: The DisDAT, Jeannette Meyer, BSN, MSN, UCLA Health
Investing in the Future of Medicine: Integrating Respecting Choices at Ochsner Health, Susan E. Nelson, MD, FACP, FAAHPM, Ochsner Health & Ochsner Health Network; Elisabeth Monies, RN, BSEd, Ochsner Health, New Orleans
A Descriptive Study of Immediate Jeopardy Citations: Skilled Nursing Facility Failures to Honor CPR-Related Resident Preferences, Mary Ellen Dellefield, PhD, RN, FAAN, UCSF School of Nursing and Caroline B. Madrigal, PhD, RN, VA Boston Healthcare System
Enhancing Advanced Practice Clinicians’ Knowledge and Comfort in Discussing the Physician Orders for Life-Sustaining Treatment Form: A Homecare Quality Improvement Initiative, Jeanette M. Ruiz, DNP, APRN, FNP-C, Alignment Health Care Anywhere APC Supervisor LA/OC/VTA; Yvonne Wu, DNP, FNP-C, Alignment Health; Kristen R. Choi, PhD, PMHNPBC, FAAN, UCLA School of Nursing, UCLA Fielding School of Public Health; Emily J. Martin, MD, MS, FAAHPM, UCLA Health Department of Internal Medicine; and Eden R. Brauer, PhD, MSN, RN, UCLA School of Nursing
POLST Knowledge Survey: Results From a Statewide Survey Across Disciplines & Settings, Jennifer Moore Ballentine, MA, Kristine Wallach, and Keeta Scholl, Coalition for Compassionate Care of California
The Impact of Video Education on Advance Care Planning (ACP) Amongst Hospitalized Oncology Patients, Raina Saxena, DO, Ochsner Medical Center, New Orleans
Improving Advance Care Planning Using Virtual Group Patient Seminars, Shirley Otis-Green, MSW, MA, ACSW, LCSW, OSW-CE, FNAP, FAOSW, Hussai Nuristani, MPH, PMP, Anne M. Walling, MD, PhD, and Neil Wenger, MD, MPH, UCLA Advance Care Planning Program
A Strategy for Early Identification of Serious Illness Patients: The AIM Program Experience Using Proactive Identification Tools and Processes, Rajwant Dhillon, RN, Advanced Illness Management, Sutter Health
Public Patient Representation in California’s Skilled Nursing and Intermediate Care Facilities, Yarin Ascencio, Office of the Long-Term Care Patient Representative, California Department of Aging
A HyFlex Clinical Course for Palliative Care Training in Serious Illness Patient (SIP) Populations, Nadya Dimitrov, DPM, PA-C, DFAAPA
Susan Elizabeth Wang, MD, FAAHPM, HMDC Board Chair
National Medical Director, Palliative Care Kaiser Permanente
Kimberly Bower, MD, FAAHPM, HMDC Immediate Past Board Chair Physician
Rady Children’s Hospital
Karl Steinberg, MD, CMD, HMDC, HEC-C Board Secretary President
Stone Mountain Medical Associates, Inc.
Craig Dresang Board Treasurer Chief Executive Officer YoloCares
Zeinab Dabbah, MD, JD, MPH Deputy Chief Medical Officer CalOptima
Praba Koomson, DNP Director, Advanced Illness Management (AIM) Sutter Health
Tao Le, MD Senior Healthcare Executive
Joycelyn Smart-Sanchez , LCSW, MBA, PPSC Director of Clinical Services, Medicare Advantage UCLA Health
Jennifer Moore Ballentine, MA Chief Executive Officer Coalition for Compassionate Care of California
Kristine Wallach Chief Operating Officer
Keeta Scholl POLST Program Director
Summit Volunteers
Stephanie Linka Michael Scholl Jim Shaw
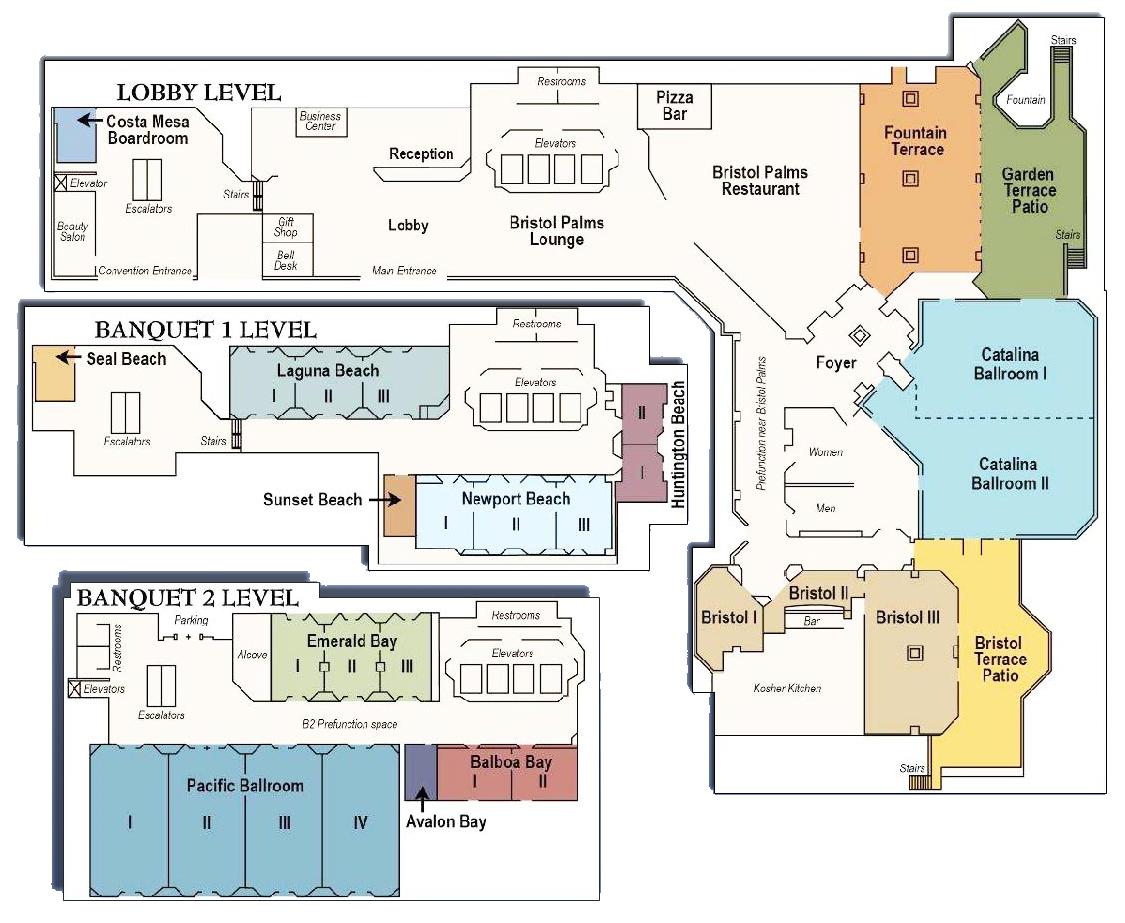
Hilton Costa Mesa Floor Plan

OCTOBER 6–7, 2025
HILTON COSTA MESA
THANK YOU TO OUR SUMMIT SPONSORS

















