
Department




Department


Faculty:
Full Members: William E. Evans, PharmD (Emeritus); James M. Hoffman, PharmD, MS; Mark Leggas, PhD; Mary V. Relling, PharmD (Emerita); P. David Rogers, PharmD, PhD, (Chair); John D. Schuetz, PhD; Clinton F. Stewart, PharmD; Jun J. Yang, PhD (Division Director, Pharmaceutical Sciences)
Associate Members: Brooke Bernhardt, PharmD (Division Director, Pharmaceutical Services); Kelly Caudle, PhD, PharmD; Cyrine Haidar, PharmD; Daniel Savic, PhD
Assistant Members: Samuel Brady, PhD; Peijun Ma, PhD; Jeffrey Rybak, PharmD, PhD; Liqin Zhu, PhD
Department Leadership Team: David Aguero, PharmD, MSTL; Kristine R. Crews, PharmD; William Humphrey, MS, MBA, BS Pharm; John McCormick, PharmD; Alejandro Molinelli, PhD; Steve Pate, DPh
Pharmaceutical Sciences Staff: Mohammad Aslam Khan, PhD; Kathy Barker, PhD; Kelly Barnett, PhD; Tony Brown, PhD; LaChelle Buckley; Kami Chauncy; Divyabharathi Chepyala, PhD; Landon Choi; Carla Cook; Guoqing Du, PhD; Dawn Fisher; Yu Fukuda, PhD; Amanda Gilbert; Wenbo Ge; Sadakatali Gori, PhD; Tomoka Gose, PhD; Murad Hasan; Yu- Jamie Horn, PhD; Chih Hsiao, MS; Sarah Jones; Elaine King; Zhenhua Li, PhD; Xiaoli Liu, PhD; John Lynch, PhD; Andrey Matlin; Pamela McGill; Ben McKinley; Claire Mills; Robert Mobley, PhD; Chris Moon; Sreenath Nair, PhD; Thandra Owens; Carl Panetta, PhD; Andrew Pappas, MA;Tracy Peters, MS; Nick Selvo; Hanfu Shi, MS; Ana Oliveira Souza, PhD; Abi Stolarski; Tina Thornton; Megan Walker, PhD; Yao Wang, MD; Kazuto Yasuda, PhD; Qing Zhang; Wenjian Yang, PhD
Pharmaceutical Services Staff: Tekoa Akins; Eric Andrews, MS; Chris Askins, PharmD; Dina Bachor; PJ Barker, PharmD; Amy Bass,
PharmD; Alysa Baumann, PharmD, MBA; Debra Black; Hui Black, PhD; Ellie Boldreghini, RN; Kymira Boone; Melissa Bourque, PharmD; Toya Bowman; Becky Boyd; Allison Bragg, PharmD; Cindy Brasher, PharmD, MS; Sharon Brittman; Felicia Brooks; Mike Brown; Thomas Bryant; Derrick Calhoun; Delia Carias, PharmD; Liz Carlton; Susan Carr, PharmD; Andy Christensen, PharmD; Misti Clark, PharmD; Rochelle Connors; Madison Cole, PharmD; Jennifer Cooper; Nicole Cox; Shane Cross, PharmD; Maria Darby; Paula Davies; LaChaka Davis; Regenia Davis; Nousheen DeRenzo, PharmD; Roseann Donnelly, PharmD; Katie Duncan; Ryan Duncan, PharmD; Nicole Edwards-Durden, PharmD; Krystal Effinger; Maureen Esposito, PharmD; Debra Ethridge, PharmD; Joseph Evans, PharmD; Tamra Filkins; Liz Gallimore, PharmD; Emma Gant, PharmD; Randy Garrett; Amanda Gillispie, PharmD; Bruce Girdler; Elbony Gray; Catina Greer; Danaka Hancock, PharmD; Torrery Hardin; Charlisa Harris; Nekia Harris; Jaclyn Hopp, PharmD; Timothy Howze, PharmD; Carlton Hughes; Kristen Hughes, PharmD; Kipp Hunter; Pat Hunter; Million Irvin; Servin Izadian, PharmD; Nevonda Jackson, PharmD; Tim Jacobs, PharmD; Sherree Johns; Clara Johnson, MS; Jennifer Kemper, PharmD; Melissa Key; Jenny Knych, PharmD; Kristen Kuehn; Terri Kuehner; Trevor Lannom, PharmD; Subrena Lesure-Johnson; David Lewis; Nichole Lewis, RN; Lie Li, PhD; Alvertis London Sr.; Maira Lopez; Natiya Lundy; William Mabry; Bertha Macklin; Shane Marshall, PharmD; Ashley Martin; Elvis Martinez; Astrid Mathis, MS; Kim McClelland, MBA; Anne McCormick, BS Pharm; Kristy McRae; Shevette Milan; Camille Miller; Thomas Mills, PharmD; Ben Moore, PharmD; Heather Morgan; PharmD; Ted Morton, PharmD; Heather Mullins, PharmD; Tiffany Nason, PharmD; Geannie Navarro; Tam Nguyen; Christina Owens; Monica Patel, PharmD; Jennifer Pauley, PharmD; Trina Peery, PharmD; Jackie Quackenbush, BS Pharm; Julie Richardson, PharmD; Sheri Ring, RN; Jennifer Robertson, PharmD; Charles Rose;

Margaret Russell; Robert Rutschman, PharmD; Kaley Salamon; Courtney Sartain; Linda Schiff, PharmD; Joe Sciasci, PharmD; Chris Scobey, PharmD; Nicole Sims; Camille Smith, PharmD; Kelsey Finnell Smith, PharmD; Kevin Smith, PharmD, HMBA; Terrilyn Smith; Hope Swanson, PharmD; Kelly Tartera, PharmD; Paula Taylor; Willie Taylor III; Nick Thomas, MS; Laura Todd; Tabetha Todd, PharmD; Deni Trone, PharmD; Dagny Ulrich, PharmD, PhD; Liz Velazquez; Huy Vi, PharmD; Madison Wade; Lynlie Wallach, RN; Deborah Ward, PharmD; Angela Watson; Yvette White; Courtney Wilburn Lee; Cheri Wilkerson, PharmD; Barry Williams, BS Pharm; Diana Wu, PharmD; Paula Yates; Curtis Yeh, PharmD; Keith Young, BS Pharm
Postdoctoral Fellows: Srijan Acharya, PhD; Stefanie Baril, PhD; Akash Bhaskar, PhD; Kashi Raj Bhattarai, PhD; Laura Doorley, PhD; Carolin Escherich, PhD; Luisa Gomez Londono, PhD; Keito Hoshitsuki, PharmD; Ruida Hou, MD, PhD; Priyanka Karmokar, PhD; Ke Liu, PhD; Maud Maillard, PhD; Sabina Ranjit, PhD; Gustavo Santiago-Collazo, PhD; Cheng Tian, PhD; Bailey Tibben, PhD; Rajesh Yetirajam, PhD; Satoshi Yoshimura, MD, PhD; Huanbin Zhao, PhD
Pharmacy Residents: Nicholas Jantrakul, PharmD; Milre Matherne, PharmD; Thanh Pham, PharmD; Kayla Thibodaux, PharmD; Megan Wright, PharmD
Graduate Students: Savanna Brinkman; Joanne Canedo, PharmD; Gabrielle Carreon; Sowjanya Cherukuri; Ashley Gray; Uzal Gurung; Jeremy Hunt; Kyle Kauler; Ani Mikoyan; Joey Miller; Kumar Niloy; Jingwen Zhu, PhD
Pharmacy Interns: Jylexus Burks, Jennifer Hampton, Cameron Harrison, Brandy Hernandez, Diana Makram, Abigail Mason, Madeline Matheson, Matthew Middleton, PhD, Maryam Moradi, Neil Patel, Braxton Snuffer, Kayla Tolbert
Visiting Student: David Wilcox




Post-doctoral
Graduate
Pharmacists BPS


The mission of the Department of Pharmacy & Pharmaceutical Sciences is to generate new knowledge to advance pharmacotherapy and provide the best patient care for children with catastrophic diseases. With a focus on patient care, discovery and implementation, and training and advocacy, the department comprises the Division of Pharmaceutical Sciences and the Division of Pharmaceutical Services. Both research and treatment are highly integrated at St. Jude Children’s Research Hospital, and many of our departmental faculty and staff members are extensively involved in both domains. Indeed, the synergies and efficiencies of having the research and patient care components in a single academic department have been hallmarks of St. Jude since its establishment in 1962, and they facilitate the success of our institution.
Our vision is to transform pharmacotherapy for patients with catastrophic childhood diseases. Survival rates for children with cancer, rare neurological diseases, hematologic disorders and infectious diseases continue to increase, largely through improvements and advances of drug therapy. Failure of current therapies and unacceptable adverse effects are partly due to suboptimal use of medications. We aim to elucidate the biological basis of inter-individual differences in pharmacologic response, translate our findings into more precise therapies and improve patient care.
Heterogeneity in many drugs’ metabolism, transport, elimination, targets, and consequent variability in therapeutic or adverse effects may result from genetic variation in normal and malignant cells. Nongenetic factors, such as drug interactions, host organ function and maturity, disease severity and adherence to therapy, also
Many aspects comprise the Department of Pharmacy and Pharmaceutical Sciences vision.
• Translate research findings into better treatments
• Optimize treatments for individual patients
• Improve overall care
Discovery and Implementation
• Clarify biological basis of drug response differences
• Identify genetic determinants of drug effects
• Develop preclinical models and integrate them into translational clinical studies
Training and Advocacy
• Faculty-led interdisciplinary St. Jude programs
• Lead and participate in national and international research collaborations and consortia
• Regular workshops, journal clubs and seminars
influence drug response. Genetic variability in the infecting pathogen can further impact anti-infective therapy, resulting in anti-infective tolerance or resistance.
We develop preclinical models to systematically characterize the biological determinants of drug response and integrate our work into translational clinical studies. Laboratory work informs clinical studies, and clinical problems drive much of our laboratory work.
Faculty members lead and participate in interdisciplinary St. Jude programs and national cooperative research collaborations. Our research integrates genome-wide analyses, functional genomics, pharmacokinetics and pharmacodynamics to identify genetic determinants of drug effects, with the long-term goal of optimizing therapy for individual patients. The Department comprises faculty members, post-doctoral fellows, residents, undergraduate and graduate students, over 33 board-certified pharmacists, and full-time staff members working as computing experts, research nurses, technical, laboratory, administrative and clinical staff.
The department is led by David Rogers, PharmD, PhD, who serves as chair, and Jun J. Yang, PhD, and Brooke Bernhardt, PharmD, MS, Division Directors of the Divisions of Pharmaceutical Sciences and Pharmaceutical Services, respectively.



Chair: David Rogers, PharmD, PhD
Division Director of Pharmaceutical Sciences: Jun J. Yang, PhD
Research and clinical implementation often inform each other in a continuous cycle.
Division Director of Pharmaceutical Services: Brooke Bernhardt, PharmD, MS
The department is supported in part by grants from industry, foundations and the National Institutes of Health. The research in the department includes clinical and fundamental pharmacology, pharmacokinetics, pharmacodynamics and pharmacogenomics. The Division of Pharmaceutical Sciences occupies over 15,000 sq. ft. of contiguous, state-of-the-art laboratory and office space, and the Division of Pharmaceutical Services occupies over 18,000 square feet of space in the clinical areas of St. Jude. The department hosts weekly research workshops and journal clubs, as well as monthly seminars that are open to the entire institution. Additionally, we host multiple laboratory-andservices–specific meetings, webinars with national and international colleagues.
Learn more about our department and the work we do:

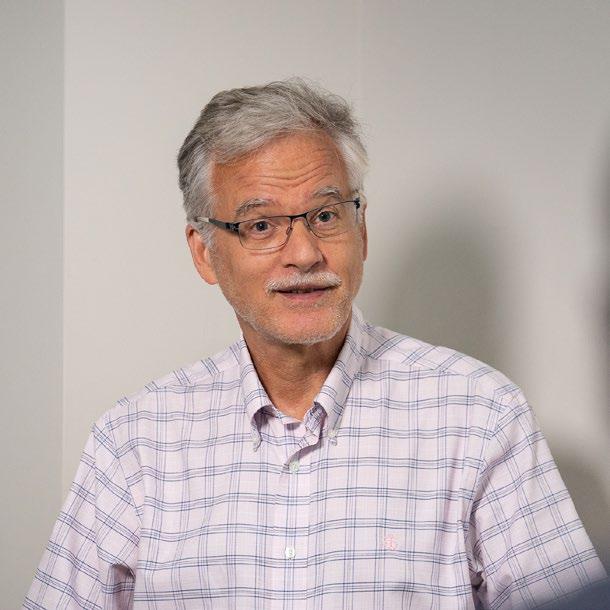
David Rogers, PharmD, PhD, serves as Chair of the Department of Pharmacy and Pharmaceutical Sciences at St. Jude and holds the St. Jude Endowed Chair in Pharmaceutical Sciences. He received his Doctor of Pharmacy degree from the University of Tennessee and his Master of Science and Doctor of Philosophy in Microbiology and Immunology from the University of Mississippi. Rogers completed his residency in pharmacy practice (PGY1) at the Regional Medical Center, Memphis, and residency (PGY2) and clinical fellowship in infectious diseases pharmacy practice at the University of Mississippi Medical Center.
Before joining the faculty at St. Jude, he was a Professor of Clinical Pharmacy and Translational Science at the University of Tennessee College of Pharmacy. There, he also held the First Tennessee Endowed Chair of Excellence in Clinical Pharmacy, served at various times as Vice Chair of the Department of Clinical Pharmacy and Translational Science, Associate Dean for Clinical and Translational Research, and Director of the UTHSC Center of Excellence for Pediatric Experimental Therapeutics. He is an elected Fellow of the American College of Clinical Pharmacy (ACCP) and the American Academy of Microbiology. He has served on the Board of Trustees for the ACCP Research Institute and on the Board of Directors for the Society of Infectious Diseases Pharmacists. He recently completed a six-year term as a member of the NIH Drug Discovery and Mechanisms of Antimicrobial Resistance (DDR) Study Section, and he currently serves on the Board of Trustees of the ACCP Foundation and has been appointed as an Ex Officio Member of the National Academies Forum on Antimicrobial Threats.

For over two decades, his research program has focused on improving antifungal pharmacotherapy by studying how pathogenic fungi develop resistance to antifungal agents. He has authored over 330 publications and scientific abstracts, has received funding from foundations, industry, and the NIH, and currently serves as PI for several NIH R01 grants. In 2021, he received the ACCP Russell R. Miller Award and the ACCP Therapeutic Frontiers Lecture Award.
The overarching goal of the Rogers lab is to improve the safety and efficacy of antifungal pharmacotherapy. Treatment of invasive fungal infections is limited to only a handful of antifungal classes, each with significant shortcomings. Moreover, resistance to these antifungals has become a significant clinical concern that threatens the utility of many front-line therapies. Few new antifungal drug classes are on the horizon; therefore, novel strategies are urgently needed to preserve, improve and expand the current antifungal armamentarium.
For over two decades, our primary focus has been understanding the molecular and cellular basis of resistance to the triazole class of antifungal agents in pathogenic fungi. Our work exploring the transcriptional and proteomic profiles of the response to antifungals in Candida albicans led to
the discovery of general and specific responses, some of which aligned with the antifungal mechanism of action and gave insight into factors influencing antifungal susceptibility. We used similar approaches for the analysis of azole antifungal resistance in clinical isolates of Candida species, which led to our discovery that activating mutations in genes encoding the transcription factors Mrr1 and Upc2 in C. albicans and Pdr1 in C. glabrata lead to overexpression of efflux pumps and the triazole target enzyme (Erg11) in clinical isolates.
More recently, we have found that the transcription factor Upc2A in C. glabrata plays a central role in fluconazole susceptibility and are exploring the Upc2A pathway for opportunities to enhance the activity of this antifungal agent against this otherwise fluconazole-resistant pathogen. We have begun to map the genomes of triazole-resistant clinical isolates of Aspergillus fumigatus and have discovered that mutations in the region encoding the sterol sensing domain of HMG-CoA reductase
are a novel driver of triazole resistance in this mold and that the mechanism of action of the triazole antifungal is partially driven through this enzyme. By mapping the genomes of antifungal-resistant isolates of C. auris, we have recently found that activating mutations in the gene encoding the transcription factor Tac1b is a major driver of fluconazole resistance. In contrast, mutations in ERG6, encoding sterol methyltransferase, represent the first identified mechanism of clinical resistance to amphotericin B in this emerging fungal pathogen. Recently, we have expanded our efforts to understand the basis of fluconazole resistance in Candida parapsilosis, a fungal pathogen of growing clinical concern. Through this work, we have demonstrated the significance of activating mutations in the Mrr1 and Tac1 transcription factors and specific drug transporters under their control.
Scan the QR code to view all of Dr. Roger’s publications:

David Rogers
Departmentof
Pharmacy and Pharmaceutical Sciences ChairJun J. Yang
Division of Pharmaceutical Sciences Division Director
Division of Pharmaceutical Sciences Faculty
Pharmacotyping
Graduate Students
Administrative Staff Center for Translational Pharmacology
Laboratory Staff
Pharmacogenomics
Postdoctoral Fellows
Brooke Bernhardt Division of Pharmaceutical Services Division Director
Pharmacy Operations
Inpatient Pharmacy
Outpatient & Specialty Pharmacy
Home Infusion
Pharmacy Informatics & Analytics
Clinical Research Pharmacy
Pharmacy Academic and Clinical Programs
Clinical Pharmacy Services
Clinical Pharmacogenomics
Clinical Pharmacokinetics Lab
Education & Training Programs
Medication Safety & Policy
The core mission of the Division of Pharmaceutical Sciences is to generate new and fundamental knowledge about how to individualize drug therapy for children with catastrophic diseases. Basic science has always been represented in our research portfolio, with faculty exploring fundamental biology of drug transport, metabolism, toxicity and resistance. We continue to build on our groundbreaking efforts in pharmacogenomics and lead the world in the discovery and clinical implementation of pharmacogenomicsguided precision medicine. Our faculty study genomic and epigenomic architecture of drug phenotypes, develop more accurate models of pediatric cancers for preclinical evaluation, and elucidate the molecular basis of resistance to anticancer and anti-infective agents. The Division integrates expertise in pharmacokinetics, pharmacodynamics, and pharmacogenomics with state-of-the-art technologies to drive discovery research in therapeutic science across disease specialties. Importantly, our unique strength also lies in the ability to translate our laboratory discoveries into patient care, in some cases shifting the paradigm of how pharmacotherapy is practiced. Housed on the 5th floor of the Chili’s Care Center, the laboratories of the division faculty provide superb infrastructure for translational research and an outstanding training environment for graduate students, postdoctoral fellows, and clinician-scientist trainees.
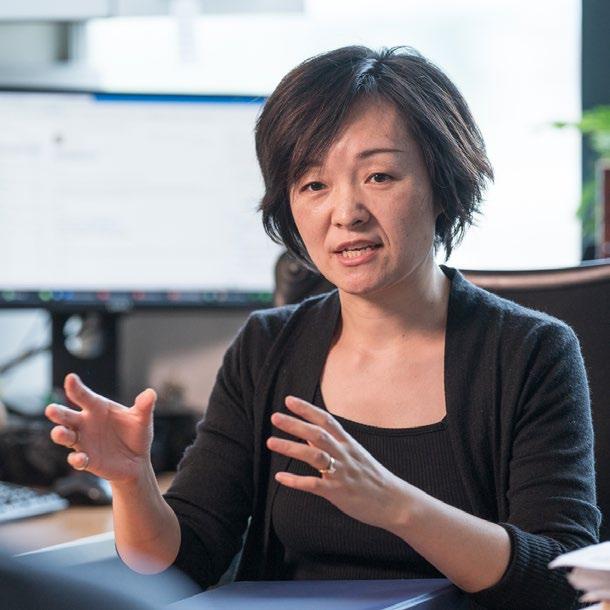
Jun J. Yang Member, Division Director Division of Pharmaceutical SciencesSt. Jude Endowed Chair in
PharmacogenomicsDr. Jun J. Yang is Member and holds the St. Jude Endowed Chair in Pharmacogenomics in Pharmacogenomics and serves as the Director for the Division of Pharmaceutical Sciences.
Dr. Yang’s research focuses on pharmacogenomics of anti-cancer drugs in children with a particular interest in childhood acute lymphoblastic leukemia (ALL). Leveraging a wide range of genomic profiling and functional genomics approaches, his work aims to elucidate biological factors and processes governing efficacy and toxicity of anticancer drugs. The goal is to ultimately develop pharmacogenomics-guided treatment individualization for children with catastrophic diseases.
Because genetic factors in both host and tumor genome can affect drug response, the Yang Lab examines inherited (germline) and acquired (somatic) genetic factors for their association with treatment response in ALL.
In 2023, Dr. Yang and team published a landmark study comprehensively describing the variations in drug sensitivity in 23 genetic subtypes of ALL, the results of which provide a blueprint to advance individualized therapy. Dr. Yang also led research efforts that advance treatment opportunities by leveraging combination therapy to harness genetic susceptibilities and overcome inhibitor resistance

in KMT2A rearranged leukemia. In collaboration with Dr. Ching-hon Pui in the Department of Oncology, he defined pharmacological basis of differential prognosis within hyperdiploid ALL, the largest subtype of this cancer. Most notably in 2023, Dr. Yang received the prestigious Waun Ki Hong Award for Outstanding Achievement in Translational and Clinical Cancer Research from the American Association of Cancer Research (AACR) honoring his work on pharmacogenomics of cancer drugs in minority and diverse populations.
Scan the QR code to view all of Dr. Yang’s publications:
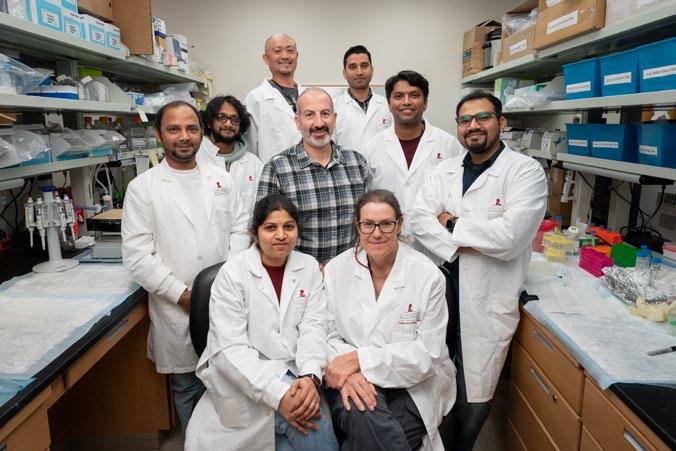
Samuel Brady, PhD, joined the Department of Pharmacy and Pharmaceutical Sciences in 2023. Since joining, he has established his lab and hired staff to support their research endeavors.
The overarching objective within the Brady lab is to use cancer genomics and pharmacology to identify improved pediatric cancer treatment approaches. Patients with cancer will often respond to their initial treatment, but sometimes, a small subset of cancer cells evade treatment and develop drug resistance; the Brady lab aims to understand why and how that occurs. One method the team employs is identifying mutational signatures; preliminary research indicates that the sources of DNA mutations leading to acquired drug resistance within cancer cells can be identified using mutational signature analysis. For example, neuroblastoma has a mutational signature indicative of reactive oxygen species (ROS) DNA damage. These mutations may lead to drug resistance while conferring vulnerabilities to other therapies; discerning how to prevent or exploit these mutations is the next step towards developing better therapies and preventing relapses.
The team also uses mutational signatures to understand how existing therapies may induce secondary cancers in survivors later in life. Many pediatric cancer survivors will undergo treatment and be cured of their initial cancer but then develop a second cancer due to their prior therapy. The Brady lab uses mutational signatures and other genomic techniques to understand how therapy can induce specific mutations that initiate second cancers. The results of this work could help inform which therapies should be reduced to a lower dosage and which should be avoided entirely in certain patient populations.

Finally, the Brady lab aims to tackle new therapeutic targets. Many existing cancer therapies are toxic, which is a significant problem for pediatric patients because their bodies are still developing. In order to develop treatments that will have the maximum impact on cancer cells with minimal impact on healthy tissue, the team is working to identify the genes that are unnecessary for human survival but vital to a cancer cell’s survival. This research will allow new therapies to target specific proteins and minimize the toxicity of treatment.
Scan the QR code to view all of Dr. Brady’s publications:
Evans joined St. Jude in 1976 and chaired the department from 1983 to 2002, served as Deputy Director of St. Jude from 1998 to 2004, and as St. Jude fifth President and CEO from 2004 to 2014. The Evans lab examined the pharmacogenomics of anticancer agents, specializing in childhood acute lymphoblastic leukemia (ALL). Evans and his team aimed to elucidate genomic determinants of toxicity and efficacy of anticancer agents and translate this knowledge into new diagnostics and treatment strategies to optimize ALL therapy. They achieved their aims by evaluating patient cohorts’ leukemia cells for drug sensitivity and clinical response in prospective clinical trials. They used comprehensive DNA and RNA sequencing to identify genes and genome variations that are important determinants of antileukemic agents’ disposition and effects.
The Evans lab closed in 2021 and no longer accepts students or post-doctoral trainees. As an emeritus faculty member, he and his collaborators continue to analyze and report data generated over the last several years to improve the safety and efficacy of medications used to treat children with cancer.

Scan the QR code to view all of Dr. Evans’ publications:
Dr. Mark Leggas is a Member of the Department of Pharmacy and Pharmaceutical Sciences and the Director of the Center for Translational Pharmacology. The Leggas Lab has a longstanding effort in translational pharmacology to optimize the clinical use of existing drugs or new drug candidates. The lab has two major projects to develop a new targeted therapy for Ewing Sarcoma and to assess the utility of a nonopioid medication to treat neonates physically dependent on opioids.
The Ewing Sarcoma project is centered around semi-synthetically modified mithramycin analogs, which have been shown to interfere with the oncogenic transcription factor responsible for Ewing Sarcoma growth. This is significant because this oncogenic transcription factor (i.e., EWS-FLI1) is recognized as the Achilles heel of Ewing Sarcoma, but efforts to develop treatments that interfere with its function have not succeeded. Currently, several analogs are progressing through preclinical evaluation and, if successful, will transition to the NCI Experimental Therapeutics program to complete all the preclinical evaluations required for entry into the clinic.
The neonate project is centered around a randomized controlled clinical trial that evaluated the use of clonidine, an alpha-2 adrenoceptor agonist, in comparison to morphine for the treatment of neonates who are born physically dependent on opioids due to prenatal exposure. The lab is using population PK/PD to describe the exposure and response of each treatment in the neonates but also attempts to understand the sources of variability in drug exposure and response to treatment through population covariate

modeling that includes pharmacogenetics of genes responsible for the transport, metabolism and pharmacological action of each drug. In 2023, the Leggas Lab further contributed to the study of neonatal opioid exposure by publishing works that analyzed the clinical utility of the Finnegan neonatal abstinence scoring tools and examined the behavioral and transcriptome alterations that occur because of opioid exposure. These efforts contribute to early diagnosis and treatment of neonatal opioid withdrawal syndrome (NOWS).
Scan the QR code to view all of Dr. Leggas’ publications:
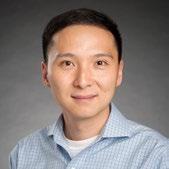
Dr. Peijun Ma joined the Department of Pharmacy and Pharmaceutical Sciences as an Assistant Member in 2023. Her previous research focused on developing bacterial single-cell RNA sequencing technology and understanding the evolution of antibiotic resistance in gram-negative bacterial pathogens. At St. Jude, Dr. Ma’s research group aims to investigate bacterial heterogeneity and its impact on the evolution of antibiotic resistance and persistence using bacterial single-cell transcriptomics.
The emergence of antibiotic resistance and persistence can directly lead to treatment failure, posing a significant threat to human health. A major issue in our current efforts to combat antibiotic resistance and persistence is the predominant characterization of bacteria as whole populations. However, resistant and persistent clones typically arise from single-cell events. The heterogeneity in bacterial populations has not been well-characterized, and the mechanisms leading to this heterogeneity remain unclear. To address this problem, the Ma Lab will apply the innovative bacterial single-cell transcriptomics to characterize bacterial drug-induced heterogeneity at the single-cell level. Additionally, Dr. Ma’s team will characterize the microbiome using bacterial single-cell transcriptomics to understand the evolution of antibiotic resistance and persistence in the context of the host microenvironment, particularly in pediatric patients with recurrent bacterial infections. This work will provide novel and exciting insight into bacterial heterogeneity and lead to the identification of drug targets for treating bacterial infections associated with antibiotic resistance and persistence.
Scan the QR code to view all of Dr. Ma’s’ publications:
Mary Relling, PharmD, became a faculty member in the Department of Pharmaceutical Sciences at St. Jude in 1988 and served as department chair from 2003 to 2020. Her primary research efforts focused on translational research in childhood acute lymphoblastic leukemia (ALL), aiming to identify the host- and treatment-related risk factors for adverse treatment outcomes. The Relling lab’s use of precision medicine approaches to tailor therapeutic dosages enabled them to incorporate pharmacogentically-based dosage adjustments in ALL trials and for all other St. Jude patients via the clinical protocol PG4KDS.
Relling co-founded the Clinical Pharmacogenetics Implementation Consortium (CPIC), an NIHsupported genomics resource focused on facilitating the clinical implementation of germline pharmacogenetic testing. After stepping down as department chair and moving to parttime status in 2021, Relling retired in June of 2023, but her collaborators continue to build on her tireless work.
Scan the QR code to view all of Dr. Relling’s publications:
Jeffrey M. Rybak, PharmD, PhD, joined the Department of Pharmacy and Pharmaceutical Sciences faculty at St. Jude Children’s Research Hospital in September 2020. Previously, his research focused on discovering the molecular mechanisms underpinning antifungal resistance among challenging fungal pathogens such as Aspergillus fumigatus and Candida auris. Employing whole genome and transcriptome sequencing, in vitro evolution studies and targeted allelic replacement, Rybak and his colleagues revealed mutations in the A. fumigatus HMG-CoA reductase gene, hmg1, and the C. auris zinc-cluster transcription factor gene, TAC1B, as widespread genetic determinants of clinical triazole antifungal resistance.
Rybak’s current research focuses on advancing the treatment of invasive fungal infections by developing new therapeutic strategies to overcome difficult-to-treat fungal pathogens. In pursuit of this objective, the Rybak lab has developed the C. auris-optimized Episomal Plasmid Induced Cas9 (EPIC) system, capable of single nucleotide-editing, and used this system to interrogate the role of the fungal-specific zinc-cluster transcription factors (ZCF) in regulating the response to antifungalinduced stress in C. auris. They have demonstrated that targeted disruption of one of these ZCF genes, UPC2, results in decreased resistance to triazole antifungals and increased resistance to amphotericin B. Furthermore, the Rybak lab has observed that while triazoles are conventionally limited to fungistatic activity against species of Candida, disruption of C. auris UPC2 conferred rapid fungicidal activity to the triazole agents at pharmacologically achievable concentrations. Their ongoing studies seek to characterize the C. auris UPC2 regulatory network and to reveal molecular weak points that can be targeted

to restore and enhance the activity of the triazoles and amphotericin B.
The Rybak lab also seeks to advance the treatment of invasive mold infections. Recently, they demonstrated that a specific group of commonly observed mutations in the cyp51A gene, which alter the glycine-54 residue (G54), confer increased resistance to long-lipophilic triazoles such as posaconazole while creating a previously unknown collateral sensitivity to compact triazoles. They then demonstrated that this vulnerability could be therapeutically exploited to treat even pantriazole-resistant A. fumigatus clinical isolates with G54 altering mutations by utilizing targeted combinations of clinically available triazoles in a murine model of pulmonary aspergillosis. In a study published in 2023, they demonstrated that hapE and hmg1 mutations additively contribute to pan-triazole resistance in an A. fumigatus clinical isolate, which can lead to treatment failure and high mortality rates.
In addition to his benchtop research, Rybak is a member of the Antimicrobial Utilization and Improvement Committee (AUIC) and co-authored the updated St. Jude Antifungal Utilization Guidelines.
Scan the QR code to view all of Dr. Rybak’s publications:
Dr. Daniel Savic leads a research program that focuses on the noncoding regulatory genome to identify and functionally characterize cis-regulatory disruptions impacting chemotherapeutic drug resistance, treatment response and relapse in childhood acute lymphoblastic leukemia (ALL). For this research, the Savic Laboratory utilizes diverse functional genomic and related high-throughput screening approaches, including massively parallel reporter assays and epigenomic CRISPR-based screening of the noncoding genome.
The Savic Lab has three areas of research: evaluating cis-regulatory element function and gene regulation in ALL, functionally characterizing inherited noncoding genetic variation that impacts chemotherapeutic drug resistance, treatment response and relapse in patients with ALL and mapping gene regulatory responses to chemotherapeutic drugs that impact drug resistance. In 2022, the Savic Lab identified numerous cis-regulatory disruptions at glucocorticoid receptor binding sites that impact glucocorticoid resistance in ALL, including two cisregulatory disruptions at the TLE1 gene locus that codes for a canonical Wnt signaling antagonist. A follow-up of this work identified extensive crosstalk and mutual antagonism between glucocorticoids and canonical Wnt signaling pathways in B-ALL cells, which offers evidence for treatment with canonical Wnt antagonists in patients with glucocorticoid resistant disease.
The long-term goal of Dr. Savic’s research effort is to improve precision medicine in childhood ALL by gaining a better understanding of genome function and the underlying gene regulatory

factors that contribute to chemotherapeutic failure in patients. In addition to the research work he leads in the Department of Pharmacy and Pharmaceutical Sciences, Dr. Savic is also a member of the Hematological Malignancies Program at St. Jude and the Pharmacogenomics Research Network (PGRN).
Scan the QR code to view all of Dr. Savic’s’ publications:
Investigations in the John Schuetz Lab determine how transporters and metabolic pathways impact disease, cancer and therapeutics.
Recent work published by the Schuetz Lab details how the therapeutically important ABC transporter, ABCG2, discriminates among its over 300 substrates. The polar residue, N436, in the binding pocket of ABCG2, has an important role as a substrate discriminator. The lab also used molecular dynamic simulations to show that the N436 residue is vital to determining how inhibitors interact with ABCG2. Other work published by the lab assessed the molecular basis of ABCC4 in both protecting megakaryocytes and regulating megakaryoppoiesis, the process leading to platelet formation.
With respect to medulloblastoma, the lab conducted collaborative work with the Roussel Lab to investigate the role of a novel ABCC4 interacting protein, scribble, in regulating the activity of the sonic hedgehog pathway. Scribble appears to have a key role in regulating optimal transcriptional activity of the hedgehog pathway. In identifying metabolic liabilities in cancer cells, the Schuetz lab determined that PPIX contributes to ferroptotic death by interacting with a protein. PPIX is prominent in the heme biosynthetic pathway, which provides a key to understanding how PPIX-interacting proteins affect leukemias. Understanding PPIX interacting proteins may reveal a potential strategy in leukemic therapies.
The findings of the Schuetz Lab reveal insights into key transporters and pathways that can help guide the development of novel therapeutic approaches
in the future. These efforts and discoveries led to Dr. Schuetz’s election to the American Society of Pharmacology and Experimental Therapeutics (ASPET) and International Transmembrane Transporter Society (ITTS) presidencies.
Scan the QR code to view all of Dr. Schuetz’s publications:
Dr. Clinton Stewart joined St. Jude in 1991, and during his tenure his work has focused on translational research of anticancer drugs in children with solid and brain tumors. The Stewart Lab has addressed clinically relevant problems encountered in the therapy of children with brain tumors, primarily the central nervous system (CNS) penetration of novel compounds used to treat pediatric brain tumors. The process used includes tumor subgroup-specific models of pediatric CNS tumors grown in mice, cerebral microdialysis sampling of tumor extracellular fluid and ventricular CSF, drug measurement using mass spectrometry, and pharmacokinetic modeling and simulation of the derived data to directly assess the unbound partition coefficient for the drug under study.
As little is known about the disposition of most anti-cancer agents in children with cancer, the Stewart Lab has collaborated with clinical investigators to conduct comprehensive pharmacology studies in clinical trials. These studies include pharmacokinetic, pharmacogenetic, and pharmacodynamic studies of novel drugs to gain a better understanding of the variability in drug disposition in children with cancer. The lab has contributed to studies that advance the understanding of pharmacologic therapies across diseases states such as medulloblastoma, glioma, AT/RT, neuroblastoma, retinoblastoma and sarcoma.
Beyond these contributions, the Stewart Lab has translated findings from the lab to clinic for several drugs to enhance the care for children with cancer. A study from the lab showed mice treated with topotecan had better antitumor responses, which

led to a series of studies where Bayesian analysis of pharmacokinetic data determined the patient’s system clearance, allowing for individualized topotecan dosage.
Further delving into dosing, the lab characterized brain penetration of methotrexate (MTX) and its metabolite 7-hydroxymethotrexate (7OHMTX) in murine models with Group 3 medulloblastoma. Characterizations showed penetration similarities between MTX and 7OHMTX and the validated model offers the opportunity to further study MTX dosing in children with brain tumors. Finally, in a collaborative effort with Dr. John Schuetz, the Stewart Lab developed a murine cerebral microdialysis model to examine IWR-1-endo, an inhibitor of the Wnt/β-catenin pathway at the blood-brain barrier. The collaborative study established stability measures for IWR-1-endo in murine plasma and microdialysate samples, which allows for further development and application of this inhibitor.
Scan the QR code to view all of Dr. Stewart’s’ publications:
Dr. Liqin Zhu, Assistant Member in the Department of Pharmacy and Pharmaceutical Sciences, studies the molecular and cellular mechanisms driving the metastasis and drug resistance of pediatric and adult liver cancer. Her research aims to determine the role of the host liver microenvironment in liver cancer metastasis and investigate the newly acquired vulnerability of liver tumor cells induced by standard treatment to identify new drug targets for adjuvant therapies.
Using multiple metastatic models of pediatric and adult liver cancer, the Zhu Lab found that there is a developmentally prometastatic niche to pediatric hepatoblastoma in the neonatal liver mediated by the Cxcl1/Cxcr2 axis. Further analysis showed it as an ongoing competitive process between the attempt of the activated myofibroblasts as part of the host liver defense to block local growth of the tumor, and that of tumor cells to break through the suppression and metastasize in a Vcam1-dependent manner. In work that advances therapeutic knowledge, Zhu demonstrated there is a dynamic, reversible switching between the two ribonucleotide reductase M2 subunits, RRM2 and RRM2B, that supports the transition of hepatoblastoma cells between a growing state and a surviving state under standard chemotherapy. In 2023, Dr. Zhu also published work showcasing differences in hepatocellular iron metabolism between male and females with hepatocyte ferroptosis, accounting for sexual dimorphism in liver diseases.
Through these studies, it has become evident that the molecular and cellular networks supporting liver tumor metastasis and drug response are highly plastic and dependent on changes in both intra- and extra-tumoral microenvironment.
Scan the QR code to view all of Dr. Zhu’s’ publications:

Director:
Mark Leggas, PhD
Associate
Director: Kristine Crews, PharmD
Associate Director: Clinton
Stewart, PharmDThe Center for Translational Pharmacology advances the implementation of pharmacokinetic and pharmacodynamic translational research at St. Jude. The aim of our work is to centralize high-quality, competitively funded peer-reviewed clinical pharmacology research in the context of clinical trials.
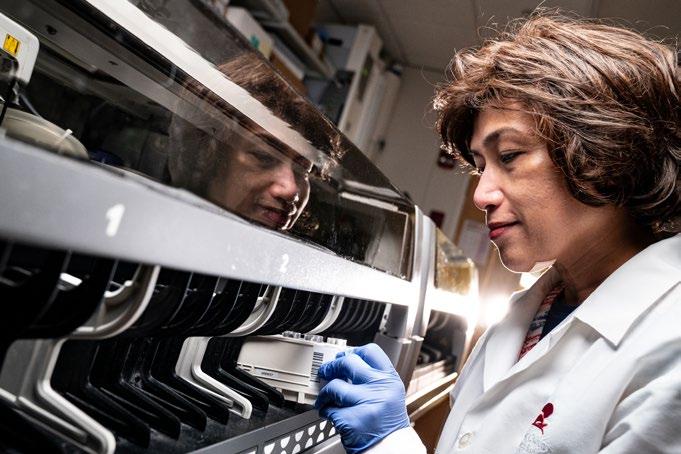
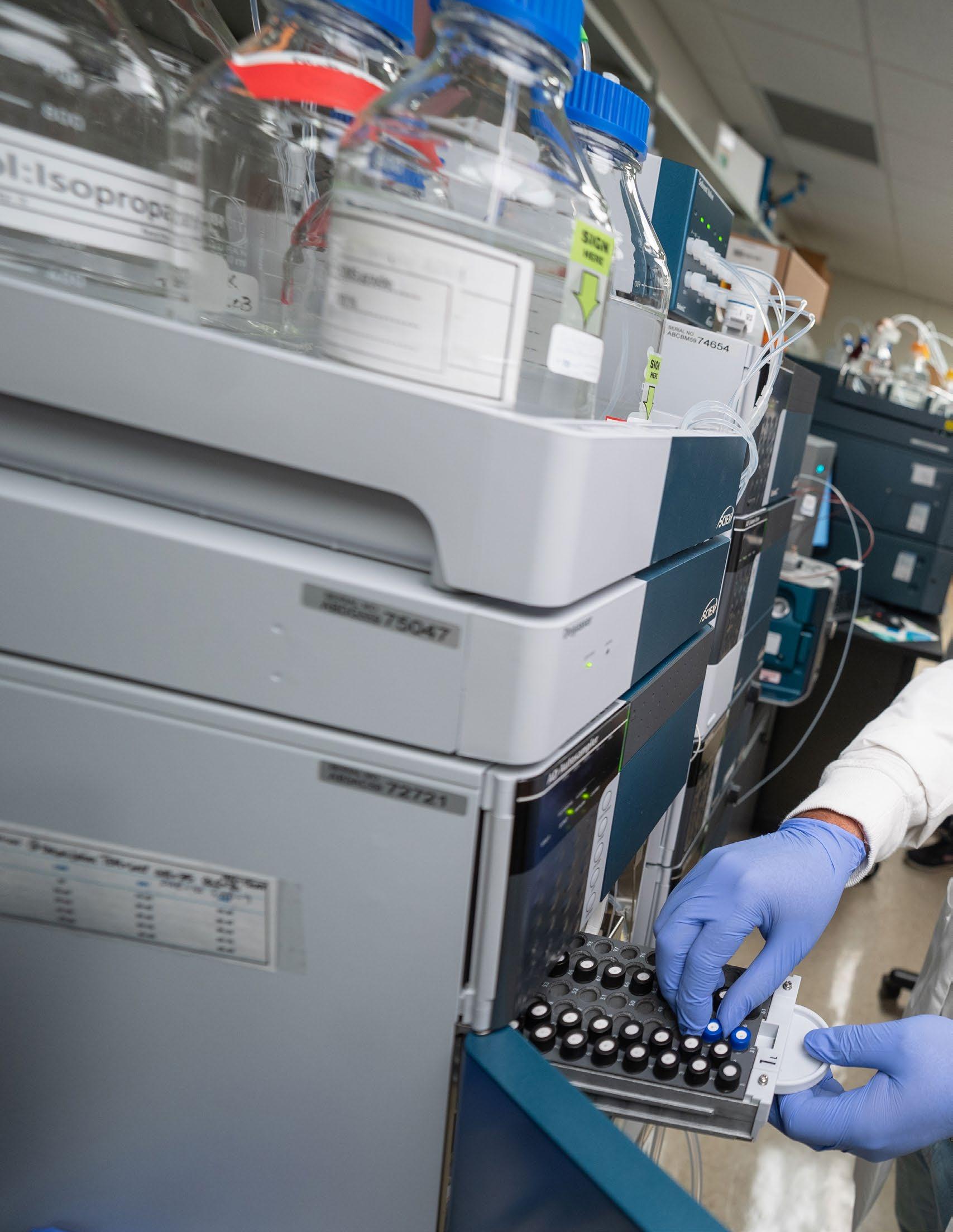
Situated on the fifth floor of the Chili’s Care Center and equipped with state-of-the-art equipment and experienced personnel, the Center is positioned to increase the impact and value of clinical trials at St. Jude by providing expertise in pharmacokinetic and pharmacodynamic study design, developing and applying novel mathematical models and providing high-quality data. The Center staff assists with building electronic sample orders, laboratory test procedures and educating clinical staff on protocolspecific procedures. Dedicated research nurses facilitate proper sample collection and logistical support to ensure efficient sample handling, processing, storage and distribution. The Center offers bioanalytical assay development and validation under FDA guidelines and sample analysis for accurate measurement of drug and metabolite concentrations in plasma, blood and other relevant biological matrices. The Center also offers state-of-the-art mathematical modeling and simulation, providing quantitative input toward rational study design and interpretation. Services are available to all faculty who initiate St. Jude trials as well as to those participating in externally collaborative projects, industry-sponsored studies, and consortium-led clinical initiatives.
To access these services, faculty and staff may request a consultation through the SRM2 portal.

Director: Jun J. Yang, PhD

Over the past 40 years, pharmacogenomics has been a central research endeavor for the Department of Pharmacy and Pharmaceutical Sciences at St. Jude. Our discoveries of the genetic determinants of drug toxicity and response have fundamentally improved pediatric cancer therapy and made St. Jude a leader in pharmacogenomics-driven precision medicine. Pharmacotyping — defining interpatient variability in drug sensitivity — is the starting point for correlating drug phenotype to patient genomic profiles.
Associate Director: Kristine Crews, PharmD

The Pharmacotyping Resource, located within the Division of Pharmaceutical Sciences, supports the opportunity to “embrace the challenge to create a new tomorrow.” The mission of the Pharmacotyping Resource is to leverage new drug screening technology to enable collaborative pharmacogenomics research that improves cancer treatment outcomes.
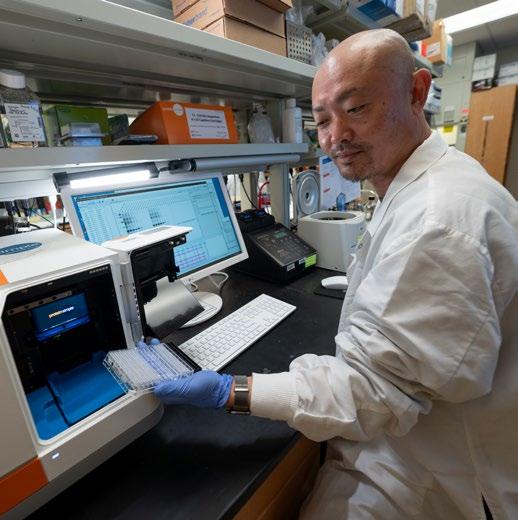
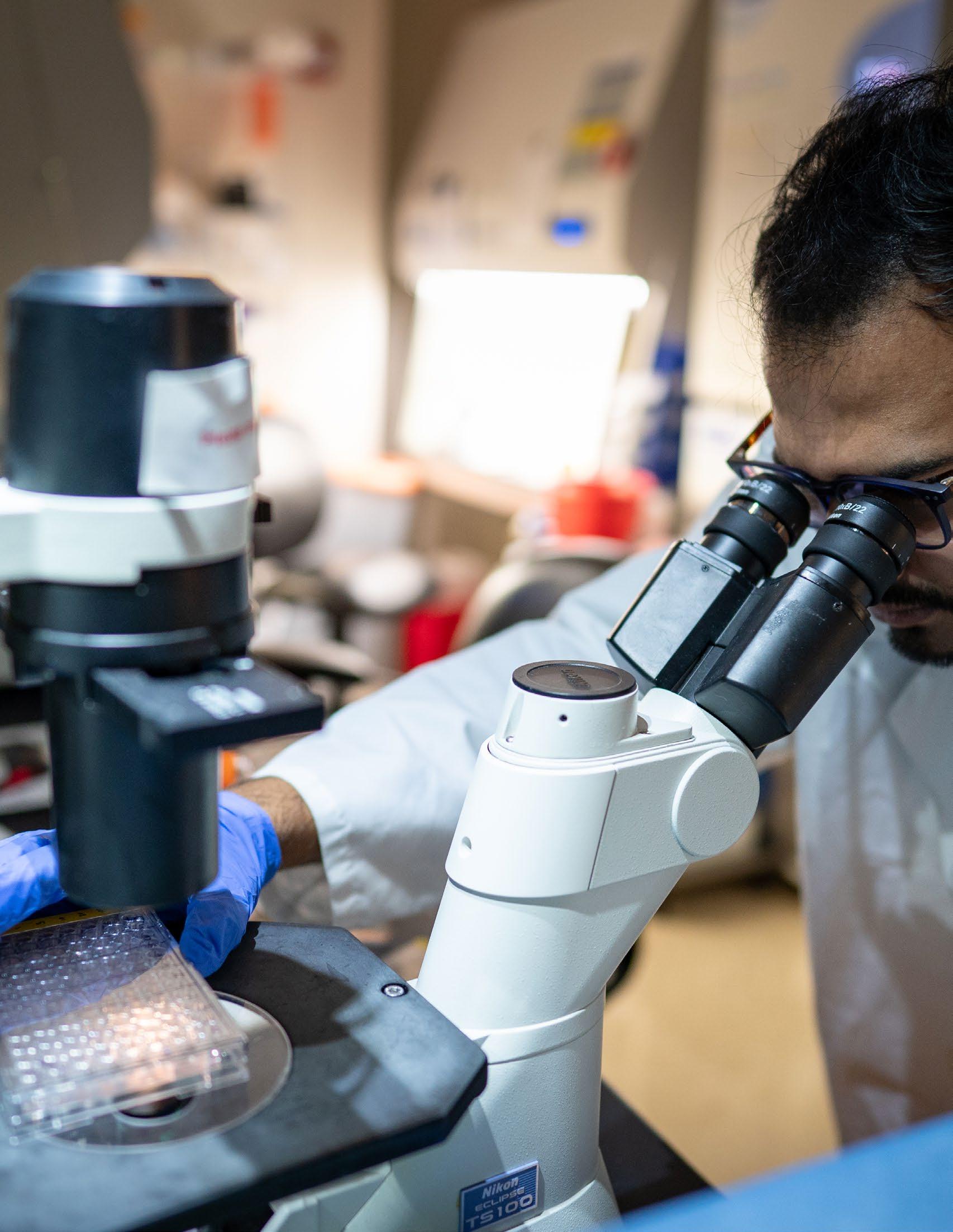
The resource offers a state-of-the-art imaging platform to test drug sensitivity profiles (pharmacotyping) of primary patient tumor cells as a functional precision medicine method. A team of research technologists, led by Jun J. Yang, PhD and Kristine Crews, PharmD, operates the Resource with expertise in high-content imaging, deep machine learning, drug assay development, preclinical drug evaluation and research informatics. Building upon our strength in this field, we use a modern pharmacotyping platform to discover new therapeutic opportunities for leukemia.
To this end, the Pharmacotyping Resource is equipped with a PerkinElmer Operetta CLS high-content analysis system for imaging- based drug sensitivity testing. The Operetta CLS is an automated confocal spinning disk fluorescence microscope. It is capable of imaging in 96 or 384 well plate formats. This imager is combined with the PerkinElmer Harmony data analysis software that allows for quantitative image analysis with image analysis capabilities powered by machine learning.
The team validated the pharmacotyping assay in tumor cells collected from patients treated for leukemia in clinical trials run by the Hematological Malignancies Program. Leukemia cells obtained from patients are tested for ex vivo sensitivity to 40 anti-leukemia drugs, and genomic profiling is done in parallel by whole genome sequencing and other assays. Our published data shows wide variability among patients in drug sensitivity and an association between sensitivity profiles and event free survival. These findings point to therapeutic implications of genomic alterations in acute lymphoblastic leukemia (ALL). The integration of tumor cell sensitivity measures with genomic data advances pharmacogenomics discovery research at St. Jude and guides the next generation of pediatric cancer therapy.

The Division of Pharmaceutical Services is led by Brooke Bernhardt, PharmD, and is staffed by pharmacists, pharmacy technicians, laboratory and nursing professionals, research and administrative staff, and faculty, all dedicated providing patients the best pharmaceutical care possible at St. Jude while supporting a collective research endeavor. Working with other clinicians in a cutting-edge and highly collaborative environment, our personnel ensure the best possible drug therapy outcomes. Nearly 180 pharmacy staff are involved in these care efforts. Their work emphasizes integrating optimal conduct of St. Jude medicationrelated clinical research, helping to fulfill our organizational mission to “advance cures and means of prevention for pediatric catastrophic diseases through research and treatment.” Over 30 pharmacists are certified as specialists by the Board of Pharmacy Specialties, and four other pharmacists carry at least one credential from other certifying organizations, testifying to the staff’s commitment to a deep understanding and high level of clinical practice of pharmacotherapy and research.
The Pharmaceutical Services team underwent significant growth and progress in 2023. The team successfully recruited Bernhardt as the new Chief Pharmaceutical Officer (CPO), promoted Steve Pate, PharmD, to the role of Senior Director and Deputy CPO and appointed two new faculty members (Cyrine Haidar, PharmD, and Kelly Caudle, PharmD, PhD). Under the guidance of Alejandro Molinelli, PhD, the Clinical Pharmacokinetics Lab achieved successful CAP reaccreditation, while Pate and his team successfully obtained ACHC accreditation for the Home Infusion Pharmacy and Specialty Pharmacy. The team also expanded their services, successfully opening the Medication Kiosk in Domino’s Village — the first approved in the state.
Brooke Bernhardt, PharmD, MS joined St. Jude in 2023 as Associate Member, Division Director, and Chief Pharmaceutical Officer for the Division of Pharmaceutical Services. As a board-certified pediatric and oncology pharmacist, Dr. Bernhardt brings a wealth of experience to her leadership roles within the department. Prior to joining St. Jude, Bernhardt was a faculty member at Baylor College of Medicine (BCM) and clinical pharmacy leader at Texas Children’s Hospital (TCH).
While at BCM/TCH, Bernhardt was a member of the Center for Epidemiology and Population Science where she led and contributed to research in molecular epidemiology with a focus on improving our understanding of treatment-related toxicities, pharmacogenomics, and health disparities in the pediatric Latino population with cancer. Her interests encompass pharmacogenomic factors that influence drug disposition, metabolomics, toxicity, and survival in children with cancer. She will continue this work in close collaboration with Jun J. Yang, PhD, as they continue to research the role of pharmacogenomics and examine disparate outcomes across different populations of children with cancer.
Dr. Bernhardt has also served as a pharmacist leader in cooperative group clinical trials as an NCI-funded pharmacist for the Children’s Oncology Group (COG) and as the Vice-Chair of the Pharmacy Discipline within COG. In this capacity, she has also contributed to over 50 cooperative group clinical trials through COG and the NCI’s Pediatric Early Phase Clinical Trials Network (PEPCTN). She continues to lead in this space and is actively designing new studies leveraging COG data through a collaboration between the COG Pharmacy Discipline and COG Epidemiology Domain Committee.

As the senior leader of the Division of Pharmaceutical Services, Bernhardt strives to ensure that the Division provides the highest level of pharmaceutical care to the patients of St. Jude. To achieve this, the Division collaborates closely with the Division of Pharmaceutical Sciences to optimize opportunities for translational care. The Division also collaborates with other clinical departments, including Oncology, Hematology, and Epidemiology and Cancer Control. The Division of Pharmaceutical Services is also committed to training the next generation of pharmacists, with a significant focus on training pharmacy students and pharmacy residents. Bernhardt has created a new Clinical Pharmacy Fellowship in Pharmacoepidemiology and Pharmacogenomics to allow for additional sub-specialty research training and has recruited the first fellow to start in FY25. Finally, in the upcoming year Bernhardt will lead the launch of two new initiatives for the Division, specifically clinical and research programs in Clinical Pharmaceutics and Pharmacoeconomics.
Scan the QR code to view all of Dr. Bernhardt’s publications:
Dr. Kelly Caudle has served as the Clinical Pharmacogenetics Implementation Consortium (CPIC) Director and Senior Program Manager for Pharmacogenomics at St. Jude since 2015 and was recently promoted to Associate Member in the Department of Pharmacy and Pharmaceutical Sciences. Dr. Caudle’s research interests and clinical experience focuses on efforts to facilitate the proper use of pharmacogenomic tests in clinical settings.
As Principal Investigator (PI) and Director of CPIC, an NIH funded consortium of over 700 members from around the world, Dr. Caudle works to develop and disseminate freely available, peer-reviewed, updatable, and detailed gene/drug clinical practice guidelines. Beyond the development of pharmacogenomic guidelines, Dr. Caudle’s other areas of research include implementation science. As a clinical pharmacist and scientist, she is wellpositioned to identify and provide solutions to the barriers clinicians face as they try to implement guidelines for pharmacogenomic testing. Part of this work extends to the standardization of pharmacogenomics to ensure successful implementation, and she actively works with the Pharmacogenomics Program to apply these guidelines in the integration of pharmacogenomic testing at St. Jude.

Scan the QR code to view all of Dr. Caudle’s publications:
Cyrine Haidar, PharmD, joined St. Jude Children’s Research Hospital in 2004 and was promoted to an associated faculty member at the end of 2023. Her work within the Department of Pharmacy and Pharmaceutical Sciences revolves around implementing preemptive pharmacogenomic testing into clinical practice, which helps clinicians tailor the pharmacotherapy of patients based on their pharmacogenomic profile. This involves developing ways to best integrate pharmacogenomics testing into the electronic health record. For clinicians, this creates easy access and utilization of the pharmacogenomic test results during their dayto-day patient treatment. In addition, patients are taught about the lifelong implications of their pharmacogenomic test results, which hopefully empowers them to share these results with their non-St. Jude health care providers when they return to their home environments.
In 2023, Haidar has focused on starting the Pharmacogenomics Clinic at St. Jude. This clinic saw its first patient in November of 2023 and will focus on the return of pharmacogenomic test results to patients and their families. Additionally, she has worked closely with Epic in establishing and co-leading the Pharmacogenomics Brain Trust, Epic’s first genomic-based brain trust. Drawing from the St. Jude pharmacogenomic implementation expertise and Epic’s experience, the Brain Trust’s goal is to create robust and standardized support for pharmacogenomics within Epic and across organizations. This would enable a more seamless integration of pharmacogenomics within the electronic health record frameworks.

Haidar’s clinical research explores the impact of patients’ genetics combined with certain medications or dosage levels on treatment outcomes. Notably, her collaboration with Jun J. Yang, “Additive effects of TPMT and NUDT15 on thiopurine toxicity in children with acute lymphoblastic leukemia across multiethnic populations,” which was accepted for publication in late 2023 and will be published in early 2024 in the Journal of the National Cancer Institute, investigates how dosages of thiopurines, such as mercaptopurine (MP), need to be reduced in acute lymphoblastic leukemia (ALL) treatment to minimize and mitigate toxicity in patients with reduced abilities to metabolize Thiopurine-Smethyltransferase (TPMT) and Nudix hydrolase 15 (NUDT15).
Scan the QR code to view all of Dr. Haidar’s publications:
James Hoffman, PharmD, MS, joined the Department of Pharmaceutical Sciences in 2004 and has made evaluating and improving complex medication use systems his priority. He took on a hospital-wide leadership role for patient safety when he became Chief Patient Safety Officer in 2015. In 2022, he took on additional responsibilities as Senior Vice President – Quality and Safety.
Hoffman has focused on identifying and evaluating risk for patient harm and improving patient safety. He concentrates on refining existing tools and identifying new means of patient safety event detection, improving patient safety culture, and developing and improving informatics and clinical decision support. At St. Jude, he has participated in efforts related to all these areas and has extensive experience leading change across the institution. After leadership selected DNV as the institution’s accreditation partner in 2022, he was the senior leader directing the transition, resulting in a successful first DNV survey in October 2023. The transition to DNV aligns with ongoing efforts to enhance quality systems, including improving institutional quality indicators and the annual quality planning process.
Hoffman emphasizes building the reputation of St. Jude as an academic leader in quality, patient safety and improvement science for children with catastrophic diseases. In 2023, his work explored whether the stress associated with electronic health record implementation led to increased hospitalacquired conditions in pediatric patients. He led novel uses of Epic for patient safety data, including presenting how St. Jude was the first to collect hand hygiene observations directly in Epic at a national meeting. He was also part of a panel at the Institute for Healthcare Improvement Forum on Demystifying the Chief Quality Officer Role.

Through his collaboration with Cyrine Haidar, PharmD, and Kelly Caudle, PharmD, PhD, he focuses on implementing pharmacogenomics as a patient safety strategy. Through these efforts, he implements research discoveries in pharmacogenomics into the clinic by developing and disseminating model practices and clinical practice guidelines. This work includes PG4KDS: Clinical Implementation of Pharmacogenetics at St. Jude and nationally through the NIH-funded Clinical Pharmacogenetic Implementation Consortium (CPIC).
Hoffman remains a leader in various topics relevant to pharmacy practice. He has engaged in the ASHP Pharmacy Forecast for over a decade, which provides strategic advice for health system pharmacy leaders. He contributes as an author of an annual paper forecasting drug expenditures in health systems, and he serves as a contributing editor for the American Journal of Health System Pharmacy.
Scan the QR code to view all of Dr. Hoffman’s publications:
 Director: Alejandro Molinelli, PhD
Director: Alejandro Molinelli, PhD
The Clinical Pharmacokinetics (CPK) Laboratory, located in the Division of Pharmaceutical Sciences, supports the St. Jude mission by providing state-of-the-art therapeutic drug monitoring and pharmacogenetic testing that clinical pharmacists interpret to ensure optimal drug dosing. It is directed by Alejandro Molinelli, PhD, with translational support from Kristine Crews, PharmD.
The CPK lab is certified as a high-complexity laboratory by CLIA (Clinical Laboratory Improvement Amendments) and is accredited by the College of American Pathologists. Our staff consists of licensed medical laboratory scientists. Every year, the laboratory processes and analyzes approximately 8000 clinical specimens and sends out another 550 to reference laboratories. The laboratory’s in-house test menu includes multiple high-complexity assays ranging from therapeutic drug determinations (e.g., immunosuppressant, antifungal drugs) to glomerular filtration rate estimation using 99mTc-DTPA. Some of our resources include random access immunochemistry analyzers (e.g., Abbott Architect) and analytical instrumentation (e.g., LC-MS/MS, HPLC).
Most of our instruments have bidirectional interfaces with the Epic electronic health record. The laboratory also handles pharmacogenetic testing for the hospital, offering genotyping results that accompany consults prepared by clinical pharmacists or pharmacy specialty residents.
The laboratory staff and pharmacists at St. Jude work closely to provide prompt results. Once a test result is obtained, the laboratory scientists alert the pharmacist, who then prepares a clinical consult. This close integration of care ensures that our patients receive the best treatment while minimizing adverse drug effects. The laboratory staff is also involved in clinical translational science projects, for which tests developed in the research laboratories are validated and incorporated into the CPK lab test menu to bring cutting-edge care to our patients.
In addition to the samples for clinical testing, the CPK laboratory staff members also process thousands of patient research specimens yearly in support of St. Jude clinical trials for the Center for Translational Pharmacology.
Leadership:





The Clinical Pharmacogenomics Program aims to integrate preemptive pharmacogenomic testing into patient care to improve the safety and efficacy of medication use.
In November 2023, a pharmacist-led Pharmacogenomics Clinic, one of the first nationwide, was launched to provide in-person counseling to patients and families about their pharmacogenomic test results and emphasize the importance of sharing these results with healthcare providers. Integration with clinical informatics remains critical to preemptive pharmacogenomic testing.
We recently published an analysis of 4,783 clinical decision support alerts guided by pharmacogenomics presented to St. Jude clinicians for 12 genes and 60 drugs. We found clinicians adhered to the therapeutic recommendations provided in 4392 alerts (92%). The Clinical Pharmacogenomics Program advances the ability for other organizations to build similar pharmacogenomics capabilities in their electronic health record. Notably, Dr. Haidar serves as one of the founding Chairs of the Epic Pharmacogenomics Brain Trust. She was also elected to the Epic Genetics Specialty Steering Board to represent the pharmacogenomics perspective of genomic implementation.
To facilitate evidence-based clinical pharmacogenomic testing worldwide, the Clinical Pharmacogenetics Implementation Consortium (CPIC®) was created in 2011. Kelly Caudle, PharmD, PhD, leads CPIC as coPI and Director with James Hoffman, PharmD, as co- leader of CPIC informatics. The Department is well represented in CPIC with additional involvement as co-authors and other roles from Cyrine Haidar, PharmD; Kristine Crews, PharmD; Alejandro Molinelli, PhD; Jun Yang, PhD; and others. CPIC membership has grown to over 700 members of international clinicians and scientists and continues to provide education and valuable resources to guide the implementation of pharmacogenomics into clinical practice. A significant 2023 accomplishment was successful renewal of NIH funding in collaboration with colleagues at Stanford University and the University of Pennsylvania and continued planning for how CPIC will connect with other established genomic resources. CPIC guidelines are indexed in PubMed as clinical guidelines, endorsed by ASHP and ASCPT and referenced in ClinGen and PharmGKB.
The goal at St. Jude is to implement all genes and drugs encompassed by CPIC guidelines. As of 2023, the Clinical Pharmacogenomics Program has implemented 16 genes and 75 drugs at St. Jude. Over 7,300 patients have consented for pre-emptive pharmacogenomic testing through the multidisciplinary PG4KDS protocol.
To continually advance clinical implementation, the Clinical Pharmacogenomics Program personnel train the next generation of pharmacogenomics professionals through the PGY2 residency in Clinical Pharmacogenomics and educate health care professionals and patients. Through the Department’s Clinical Pharmacogenomics Program, pharmacogenomic testing benefits St. Jude patients and actively disseminates resources to advance pharmacogenomics implementation for patients worldwide.
 Director: John McCormick, PharmD
Director: John McCormick, PharmD
By providing clinical pharmacy services to the institution, Clinical Pharmacy Specialists extend the reach of Pharmaceutical Services to direct patient care. Our clinicians provide support to the Leukemia/ Lymphoma, Solid Tumor, Neuro-Oncology, Bone Marrow Transplant & Cellular Therapy, Intensive Care, Surgery, (non-malignant) Hematology and HIV care teams. Our board-certified Clinical Pharmacy Specialists are credentialed members of the medical staff with collaborative authority to perform direct patient assessment and prescribe medication therapy and associated laboratory tests.
These pharmacists provide pharmacokinetic assessments, which include individualized targeted therapy for antineoplastics and other medications. Further individualization incorporates the use of clinical pharmacogenomics in medication selection and dosing approaches. Our pharmacists work closely with clinicians to provide oversight and development of care plans (non-protocol treatment plan) for patients who are not managed on an approved research protocol. We also provide departmental and institutional support for research protocol development and implementation.
Our pharmacists offer expertise for services including intra- and inter-departmental education as well as post graduate training in pediatric hematology/oncology medication management and disease states. Team members continue involvement in multiple collaborative efforts. We provide leadership and direction for the antimicrobial stewardship program which helps maintain the institution’s status as an Antimicrobial Stewardship Center of Excellence as designated by the Infectious Diseases Society of America. This is an ongoing collaboration between our department and the Department of Infectious Diseases. We continue to assist with the implementation of the new electronic health record (EPIC). Expanding our reach beyond St. Jude and Memphis, we provide support for the role of a Clinical Pharmacy Specialist in our Global Pediatric Medicine program to ensure the efforts and impact of Clinical Pharmacy Services have a global reach.


 Director: Jennifer Robertson, PharmD
Director: Jennifer Robertson, PharmD
The Pharmaceutical Services Medication Safety and Policy Team, led by Jennifer Robertson, PharmD, ensures safe medication systems throughout St. Jude. Discrete functions include setting and revising policies related to medication use within the institution; routine and ongoing efforts to improve the safety of medication use systems, based on both reactive and proactive review of events and risk; establishing and maintaining high-quality drug information resources and drug therapy guidelines; maintaining the drug formulary; implementing cost savings efforts, when relevant; and supporting ongoing performance improvement related to medication use. Many system refinements are accomplished each year, impacting physicians, advanced practice providers, nurses and pharmacists as they provide patient care.
The team leads and works with the institution’s Medication Use Safety Team (MUST) to complete actions outlined in the latest Medication Safety Strategic Plan. The plan continues to focus on a culture of safety, improving medication use systems, high-alert medications and using technology to enhance the safety of medications. The 2023 plan’s major emphasis was continuing performance improvement (PI) projects for IV infusion pump drug library compliance and opioid consent adherence, as well as assisting with electronic health record improvements.
Significant contributions from Robertson’s team in 2023 include successfully coordinating the launch of new IV infusion pumps and meeting the PI project’s goal to increase the safety parameters of infusion pumps to 85% compliance. Additionally, the team participated in a first successful DNV accreditation.

 Director: David Aguero, PharmD
Director: David Aguero, PharmD
The Pharmacy Informatics Community aims to implement, maintain and optimize best-in-class medication technology solutions and analytics that support exceptional pharmaceutical care. Through collaboration with clinical staff, Quality and Patient Care and Information Services, Pharmacy Informatics strives to facilitate practical solutions that achieve optimal patient outcomes, workflow efficiency and resource stewardship within the medication use process at St. Jude.
The informatics ecosystem at St. Jude is quite complex, and the work of this team helps assure that this complex system is functional and results in excellent patient care. In addition to this ecosystem, our team maintains a host of different solutions, which range from inventory control tools, infusion pumps, financial systems, drug information systems and important trial randomization software.

Data created during medication management guides the functions of the department and serves as benchmarks for pharmaceutical data stewardship within the institution and externally. Our team, through Pharmacy Analytics Services, uses this data to create and maintain a business intelligence portfolio as part of the departmental data strategy. Following our Epic implementation, electronic health record (EHR) dashboards continue to be built and optimized. Where Epic can’t meet department needs, data is migrated to Microsoft Azure and projected through dashboards to support data-driven decisions throughout the organization.
Managing the pharmaceutical supply chain landscape is a difficult task. Our Pharmacy Supply Chain Services is an operational coalition that manages a service line focused in two areas:
• Strategic sourcing: responsible for managing pharmaceutical vendor relationships, accounts payable, contracts, and drug shortage monitoring. The team collaborates with our Group Purchasing Organization (Vizient) and leverages our strategic partnerships with wholesaler McKesson to reinforce consistent supply while being good stewards of St. Jude resources.
• Pharmacy supply chain operations: responsible for managing inventory movement to and from stakeholders, ensuring consistency of customer service, supervising vendor purchasing decisions, inventory optimizations, aligning inventory systems and compliance and assisting with communication and coordination of drug shortages.
 Director: William Humphrey, DPh, MS, MBA
Director: William Humphrey, DPh, MS, MBA

Senior Director and Deputy Chief Pharmaceutical Officer: Steve
Pate, DPhThe Division of Pharmaceutical Services comprehensively addresses the needs of St. Jude patients, providing services across the care continuum. Within the Division is a team dedicated to daily operations in the acute care and ambulatory setting.
The Acute Care Pharmacy team is responsible for the entire medication use process, including order verification; preparation and dispensing, including sterile and non-sterile compounding of medications and the safe handling of hazardous agents; and compliance with extensive number of regulatory requirements. An extension of this service includes the Infusion Center Pharmacy, which provides sterile products for patients treated in the clinics, procedure areas, diagnostic areas and the infusion center.
The Ambulatory Pharmacy team includes the Ambulatory Care Unit (ACU) Pharmacy, specialty pharmacy, prescription mail service, and the home infusion pharmacy. Outpatient pharmacy programs are accredited Accreditation Commission for Health Care (ACHC) and Utilization Review Accreditation Commission (URAC). In November 2023, the Outpatient Pharmacy program installed the first medication dispensing kiosk at The Domino’s Village to support its efforts to improve the patient experience and decentralize the medication dispensing process closer to the point of care. The Outpatient team also serve patients residing beyond the greater Memphis area, ensuring medications are dispensed through the prescription mail order service or through other local contracted or affiliate pharmacies.
The Acute Care and Ambulatory Pharmacy staff is a team comprised of Clinical Staff Pharmacists and Certified Pharmacy Technicians who provide a wide variety of services that deliver high-quality care consistent with the defined research protocol or non-protocol treatment plan. Clinical Staff Pharmacists collaborate with Clinical Pharmacy Specialists to ensure patients and their caregivers are well-educated on their medication regimen through discharge medication teaching, medication adherence counseling and tracking, and comprehensive medication reconciliation across transitions of care. Clinical Research Pharmacists and Certified Pharmacy Technicians on the Investigational Pharmacy Services team help execute the therapeutic clinical trials conducted at St. Jude. This team assists with protocol development; investigational agent accountability and handling; and the creation of information for pharmacy staff about each protocol and study agent. Staff across the Division collaborate closely with St. Jude Affiliates to help ensure that the medication-related needs of patients managed at these locations are addressed. Lastly, all staff are involved in the education and training of future pharmacists and pharmacy technicians through formal student training programs and area institutions and universities.
The Department of Pharmacy and Pharmaceutical Sciences hosts PGY2 Residencies in Oncology Pharmacy, Medication Use Safety and Policy, Clinical Pharmacogenomics, Infectious Diseases, and Informatics. All programs are accredited by the American Society of Health System Pharmacists (ASHP). Trainees at St. Jude are supported by an institutional Clinical Education and Training Office, whose goal is to assist our investigators and professional staff to improve the quality of experiences, training, benefits, and support for our undergraduate, graduate, professional, and postdoctoral trainees. Over 300 postdoctoral trainees (post-PhD, MD, and PharmD) are at St. Jude.
FY23 PGY2 Pharmacy Residents:



Milre Matherne, PharmD Pharmacy Oncology

Megan Wright, PharmD Pharmacy Oncology

Thanh Pham, PharmD Pharmacy Infectious Diseases
Nicholas Jantrakul, PharmD Pharmacy Informatics
Kayla Thibodaux, PharmD Pharmacogenomics

Tiffany Nason, PharmD, was honored in the 2023 St. Jude Values Book for value 6, “always be respectful of your coworkers, our patients and their families, and visitors to campus.”
As a pharmacist, Tiffany Nason, PharmD, knows the importance of the right medications to help sick children get well. But she also understands the power of resilience to help colleagues—vulnerable to stress from undertaking this crucial task—to heal. Nason has long backed this intuition with action. She’s a member of the St. Jude RISE (Resilience in Stress Events) steering committee and among the original group of RISE responders, who offer timely psychological first aid to peers experiencing traumatic patientrelated events, such as caring for children who are rapidly declining or have died. She added to those efforts this year by founding and chairing the Community Culture Committee within Pharmaceutical Sciences, aimed at promoting a positive culture within the department with a specific focus on resilience. The group has created a model approach to achieving this while caring for children with catastrophic diseases, devising plans to support colleagues and implement resiliencefocused initiatives. There’s no arguing that the lifegiving work of St. Jude can sometimes tax the soul. But Nason’s respect for that fact is proving life-altering for her comrades in arms.
Nominated by:
EllisNeufeld, MD, PhD Administration
Jun J. Yang, PhD, received the American Association of Cancer Research (AACR) Waun Ki Hong Award for Outstanding Achievement in Translational and Clinical Cancer Research.
The AACR established this Award in recognition of the extraordinary contributions of Waun Ki Hong, MD, FAACR, to advance cancer research, cancer care and cancer prevention during his longstanding and remarkable career as a physician-scientist.
This Award recognizes a cancer researcher who has conducted highly meritorious translational and clinical cancer research.
Jun J. Yang, PhD, was selected as the 2023 St Jude Postdoctoral Association Mentor of the Year.
Kelly Caudle, PharmD, received the Precision medicine World Conference 2023 Luminary Award which recognizes the recent contributions of prominent figures who have accelerated Precision Medicine into the clinic.
Kelly Caudle, PharmD, PhD, Kristine Crews, PharmD, and Mary Relling, PharmD (Emerita), were St. Jude scientists listed on the 2023 Highly Cited Researchers list.
Kelly Caudle, PharmD, was elected to Board of Trustees for the American College of Clinical Pharmacy Foundation
David Aguero, PharmD, Director for Medication Systems & Informatics, has been appointed to the GS1 US Healthcare Executive Leadership Committee (ELC) as a Pharmacy Committee member.

Kristen Hughes, PharmD, was honored in the 2023 St. Jude Values Book for value 5, “work collaboratively and help others to succeed.”
Medications can’t improve a child’s health without first passing a fundamental test: Are they safe? For Kristen Hughes, PharmD, this question drives her every effort. For example: IV infusions—a backbone of drug therapies—have the potential to harm patients when they’re linked with debilitating side effects or dangerous dosing errors. Hughes established “guardrails” around this process—literally—by initiating a program of the same name to boost the use of so-called “smart pumps” at St. Jude. Equipped with built-in error reduction software, these pumps represent a linchpin in safer care for St. Jude kids. With an incredible attention to detail, Hughes accomplished this goal by forming an interdisciplinary group of pharmacists, nurses and informatics experts to gather data to help clinicians understand the need for this software and tracking its use. Her leadership increased the use of these pumps’ safety features at St. Jude from 50% to 82%. Because of Guardrails’ success, the group recently set a loftier goal: 85% use. Working collaboratively, Hughes is guarding the mission of St. Jude to save the next child and find the next cure.
Nominatedby:
Jennifer Robertson, PharmD Pharmacy and Pharmaceutical SciencesP. Dave Rogers, PharmD, PhD, was elected Fellow of the American Academy of Microbiology
P. Dave Rogers, PharmD, PhD, was appointed to the National Academies of Sciences, Engineering, and Medicine Forum on Antimicrobial Threats.
Carolin Escherich, PhD in the Yang lab was selected for the prestigious Walter Benjamin Fellowship from the German Research Foundation. This program is similar to the K99 award in the US. The grant will support her work at St. Jude on inotuzumab pharmacogenomics.
Mark Leggas
Valent Technologies – $82,810
September 2022 to August 2023
Method Validation, Bioanalysis, and Pharmacokinetics of Oral Irinotecan in Pediatric Patients
Other Active Funding FY2023
Kelly Caudle
NHGRI U24 – $980,928
July 2022 to June 2023
Clinical Pharmacogenetics Implementation Consortium (CPIC)
James Hoffman
AHRQ R18 – $9,499
August 2022 to July 2023
Spread of Safety Interventions: Planning for Context
Mark Leggas
NCI P30 – $294,651
July 2022 to February 2023
CCSG - Pharmacokinetics Shared Resources
Mark Leggas
NIH R01 – $225,034
June 2023 to May 2024
Mechanistic and Pharmacologic Studies of Selective Mithramycin Analogues Targeting EWSFLI1 in Ewing Sarcoma
P. David Rogers
NIAID R01 – $147,567
March 2023 to February 2024
Non-cyp51A-mutation Mediated Triazole Resistance in Aspergillus fumigatus
Jun J. Yang
NIH R56 – $299,999
September 2022 to August 2023
Effects of Germline GATA3 Variants on ALL Somatic Genomics and Prognosis in Multi-ethnic Populations
P. David Rogers
NIAID R01 – $21,663
April 2023 to March 2024
Antifungal Antagonism as a Cause of Treatment Failure for Invasive Mycoses
Daniel Savic
NCI R01 – $472,116
August 2022 to July 2023
Characterizing Noncoding GWAS Variants in Acute Lymphoblastic Leukemia Treatment Outcome
John Schuetz
NCI R01 – $398,372
April 2023 to March 2024
Transporters and Medulloblastoma
Clinton Stewart
Pfizer ONITT – $18,316
February 2023 to February 2024
A Randomized Phase I/II Study of Onivyde in Combination with Talazoparib or Temozolomide in Children and Young Adults With Recurrent Solid Malignancies and Ewing Sarcoma
Jun J. Yang
LLS TRP – $192,180
July 2022 to June 2023
LCK-targeted Therapy in T cell Acute Lymphoblastic Leukemia
Clinton Stewart
Ipsen ONITT – $26,688
May 2023 to May 2024
A Randomized Phase I/II Study of Onivyde in Combination with Talazoparib or Temozolomide in Children and Young Adults with Recurrent Solid Malignancies and Ewing Sarcoma
Jun J. Yang
NCI R01 – $587,189
July 2022 to June 2023
Biomarkers of Dasatinib Response and Resistance in T-cell Acute Lymphoblastic Leukemia
Jun J. Yang
NIH R01 – $74,695
August 2022 to July 2023
Admixture Analysis of Acute Lymphoblastic Leukemia in African American Children: the ADMIRAL Study
Jun J. Yang
NCI R01 – $374,972
August 2022 to July 2023
Molecular Epidemiology of ALL in Children with Down Syndrome
P. David Rogers
NIAID R01 – $1,247,879
March 2023 to February 2024
Mapping the Genomic and Molecular Mechanisms of Antifungal Resistance in the Emerging Fungal Pathogen Candida auris
Jun J. Yang
NCI U01 – $212,165
September 2022 to August 2023
Clonal Therapy for Pediatric T-cell Acute Lymphoblastic Leukemia
Jun J. Yang
AstraZeneca – $161,070
October 2022 to October 2024
Combination Therapy with BH3 Mimetics for T-cell Acute Lymphoblastic Leukemia
Jun J. Yang
NIGMS R35 – $574,400
February 2023 to January 2024
Pharmacogenomics of Nucleobase and Nucleoside Analog Drugs
Jun J. Yang
NIH R01 – $136,591
March 2023 to February 2024
Predictors of Systemic Exposure to Oral 6MP
During Maintenance in Adolescents and Young Adults with Acute Lymphoblastic Leukemia (wolfson)
Jun J. Yang
NCI R01 – $31,849
May 2023 to April 2024
Understanding the Increased Risk of Childhood Acute Lymphoblastic Leukemia in Latinos
Leukemia
Epigenomic profiling of glucocorticoid responses identifies cis-regulatory disruptions impacting steroid resistance in childhood acute lymphoblastic leukemia.
Communications Biology
Ribonucleotide reductase subunit switching in hepatoblastoma drug response and relapse.
Bergeron BP, Diedrich JD, Zhang Y, Barnett KR, Dong Q, Ferguson DC, Autry RJ, Yang W, Hansen BS, Smith C, Crews KR, Fan Y, Pui CH, Pruett-Miller SM, Relling MV, Yang JJ, Li C, Evans WE, Savic D. Leukemia 36:2374-2383,2022. PMCID: PMC9522591 PUBMEDID: 36028659 NIHMSID: NIHMS1833642.
Pediatric Blood Cancer
Application to a pediatric high-risk neuroblastoma clinical trial.
Brown A, Pan Q, Fan L, Indersie E, Tian C, Timchenko N, Li L, Hansen BS, Tan H, Lu M, Peng J, Pruett-Miller SM, Yu J, Cairo S, Zhu L. Commun Biol. 2023 Mar 8;6(1):249. doi: 10.1038/ s42003-023-04630-7.PMID: 36882565.
Nature Communications
The net electrostatic potential and hydration of ABCG2 affect substrate transport.
Campagne O, Wu H, Wu J, Naranjo A, Daryani VM, Gajjar AJ, Park JR, Stewart CF. Topotecan clearance based on a single sample and a population pharmacokinetic model: Pediatr Blood Cancer. 2023 Nov;70(11):e30658. doi: 10.1002/ pbc.30658. Epub 2023 Sep 4. PMID: 37664968; PMCID: PMC10538374.
Clinical Oncology
Prognostic and pharmacotypic heterogeneity of hyperdiploidy in childhood ALL.
Gose T, Aitken HM, Wang Y, Lynch J, Rampersaud E, Fukuda Y, Wills M, Baril SA, Ford RC, Shelat A, Mara MLO, Schuetz JD. Nat Commun 14:5035-,2023. PMCID: PMC10439158 PUBMEDID: 37596258.
Nature Medicine
Pharmacotypes across the genomic landscape of pediatric acute lymphoblastic leukemia and impact on treatment response.
Lee SHR, Ashcraft E, Yang W, Roberts KG, Gocho Y, Rowland L, Inaba H, Karol SE, Jeha S, Crews KR, Mullighan CG, Relling MV, Evans WE, Cheng C, Yang JJ, Pui CH. J Clin Oncol :JCO2300880-,2023. PMCID: PUBMEDID: 37729596.
Lee SHR, Yang W, Gocho Y, John A, Rowland L, Smart B, Williams H, Maxwell D, Hunt J, Yang W, Crews KR, Roberts KG, Jeha S, Cheng C, Karol SE, Relling MV, Rosner GL, Inaba H, Mullighan CG, Pui CH, Evans WE, Yang JJ. Nat Med 29:170179,2023. PMCID: PMC9873558 PUBMEDID: 36604538.
Blood
Genomic landscape of Down syndrome-associated acute lymphoblastic leukemia.
Proceedings of the National Academy of Sciences
Interrogating bromodomain inhibitor resistance in KMT2A-rearranged leukemia through combinatorial CRISPR screens.
Li Z, Chang TC, Junco JJ, Devidas M, Li Y, Yang W, Huang X, Hedges DJ, Cheng Z, Shago M, Carroll AJ, Heerema NA, Gastier-Foster J, Wood BL, Borowitz MJ, Sanclemente L, Raetz EA, Hunger SP, Feingold E, Rosser TC, Sherman SL, Loh ML, Mullighan CG, Yu J, Wu G, Lupo PJ, Rabin KR, Yang JJ. Blood 142:172-184,2023. PMCID: PMC10352600 PUBMEDID: 37001051.
Pediatric Blood and Cancer
Outcomes following intolerance to calcineurin inhibitor-based graft-versus-host disease prophylaxis in children after allogeneic hematopoietic cell transplantation.
Wright S, Hu J, Hyle J, Zhang Y, Du G, Konopleva MY, Kornblau SM, Djekidel MN, Rosikiewicz W, Xu B, Lu R, Yang JJ, Li C. Proc Natl Acad Sci U S A 120:e2220134120-,2023. PMCID: PMC10120025 PUBMEDID: 37036970.
Wu D, Li Y, Bi Y, Lannom TM, Ward DA, Qudeimat A, Madden RM, Sharma A, Epperly R, Mamcarz E, Talleur A, Naik S, Selukar S, Triplett B, Srinivasan A. Pediatr Blood Cancer. 2023 Jun 20:e30517. doi: 10.1002/pbc.30517. Online ahead of print. PMID: 37338275.
Leukemia
Preclinical pharmacokinetic and pharmacodynamic evaluation of dasatinib and ponatinib for the treatment of T-cell acute lymphoblastic leukemia.
Clin Microbiol Infect
Mutations in TAC1 and ERG11 are major drivers of triazole antifungal resistance in clinical isolates of Candida parapsilosis
Yoshimura S, Panetta JC, Hu J, Li L, Gocho Y, Du G, Umezawa A, Karol SE, Pui CH, Mullighan CG, Konopleva M, Stock W, Teachey DT, Jain N, Yang JJ. Leukemia 37:1194-1203,2023. PMCID: PMC10347458 PUBMEDID: 37076694.
Doorley LA, Barker KS, Zhang Q, Rybak JM, Rogers PD. Mutations in TAC1 and ERG11 are major drivers of triazole antifungal resistance in clinical isolates of Candida parapsilosis. Clin Microbiol Infect. 2023 Dec;29(12):1602. e1-1602.e7. doi: 10.1016/j.cmi.2023.08.030. Epub 2023 Sep 4. PMID: 37666448.
Levinson AL, Tjoa K, Huang B, Meyer LK, Kim MO, Brady SW, Zhang J, Shannon K, Wandler AM. Opposing effects of KDM6A and JDP2 on glucocorticoid sensitivity in T-ALL. Blood Adv 7:3479-3484,2023. PMCID: PMC10362263 PUBMEDID: 36897249 NIHMSID:
Alcock LJ, Chang Y, Jarusiewicz JA, Actis M, Nithianantham S, Mayasundari A, Min J, Maxwell D, Hunt J, Smart B, Yang JJ, Nishiguchi G, Fischer M, Mullighan CG, Rankovic Z. Development of potent and selective Janus kinase 2/3 directing PG-PROTACs. ACS Med Chem Lett 13:475-482,2022. PMCID: PMC8919382 PUBMEDID: 35300081 NIHMSID:
Arunachalam S, Szlachta K, Brady SW, Ma X, Ju B, Shaner B, Mulder HL, Easton J, Raphael BJ, Myers M, Tinkle C, Allen SJ, Orr BA, Wetmore CJ, Baker SJ, Zhang J. Convergent evolution and multi-wave clonal invasion in H3 K27-altered diffuse midline gliomas treated with a PDGFR inhibitor. Acta Neuropathol Commun 10:80-,2022. PMCID: PMC9153212 PUBMEDID: 35642016 NIHMSID:
Baker SD, Bates SE, Brooks GA, Dahut WL, Diasio RB, El-Deiry WS, Evans WE, Figg WD, Hertz DL, Hicks JK, Kamath S, Kasi PM, Knepper TC, McLeod HL, O’Donnell PH, Relling MV, Rudek MA, Sissung TM, Smith DM, Sparreboom A, Swain SM, Walko CM. DPYD testing: Time to put patient safety first. J Clin Oncol 41:27012705,2023. PMCID: PMC10414691 PUBMEDID: 36821823 NIHMSID:
Baran N, Lodi A, Dhungana Y, Herbrich S, Collins M, Sweeney S, Pandey R, Skwarska A, Patel S, Tremblay M, Kuruvilla VM, Cavazos A, Kaplan M, Warmoes MO, Veiga DT, Furudate K, Rojas-Sutterin S, Haman A, Gareau Y, Marinier A, Ma H, Harutyunyan K, Daher M, Garcia LM, Al-Atrash G, Piya S, Ruvolo V, Yang W, Shanmugavelandy SS, Feng N, Gay J, Du D, Yang JJ, Hoff FW, Kaminski M, Tomczak K, Eric Davis R, Herranz D, Ferrando A, Jabbour EJ, Emilia Di Francesco M, Teachey DT, Horton TM, Kornblau S, Rezvani K, Sauvageau G, Gagea M, Andreeff M, Takahashi K, Marszalek JR, Lorenzi PL, Yu J, Tiziani S, Hoang T, Konopleva M. Inhibition of mitochondrial complex I reverses NOTCH1-driven metabolic reprogramming in T-cell acute lymphoblastic leukemia. Nat Commun 13:2801-,2022. PMCID: PMC9120040 PUBMEDID: 35589701 NIHMSID:
Baril SA, Gose T, Schuetz JD. How Cryo-EM has expanded our understanding of membrane transporters. Drug Metab Dispos 51:904-922,2023. PMCID: PMC10353158 PUBMEDID: 37438132 NIHMSID: Barsan V, Xia Y, Klein D, Gonzalez-Pena V, Youssef S, Inaba Y, Mahmud O, Natarajan S, Agarwal V, Pang Y, Autry R, Pui CH, Inaba H, Evans W, Gawad C. Simultaneous monitoring of disease and microbe dynamics through plasma DNA sequencing in pediatric patients with acute lymphoblastic leukemia. Sci Adv 8:eabj1360-,2022. PMCID: PMC9020671 PUBMEDID: 35442732 NIHMSID:
Bergeron BP, Barnett KR, Bhattarai KR, Mobley RJ, Hansen BS, Brown A, Kodali K, High AA, Jeha S, Pui CH, Peng J, Pruett-Miller SM, Savic D. Mutual antagonism between glucocorticoid and canonical Wnt signaling pathways in B-cell acute lymphoblastic leukemia. Blood Adv 7:4107-4111,2023. PMCID: PMC10388724 PUBMEDID: 37289547 NIHMSID:
Bergeron BP, Diedrich JD, Zhang Y, Barnett KR, Dong Q, Ferguson DC, Autry RJ, Yang W, Hansen BS, Smith C, Crews KR, Fan Y, Pui CH, Pruett-Miller SM, Relling MV, Yang JJ, Li C, Evans WE, Savic D. Epigenomic profiling
of glucocorticoid responses identifies cis-regulatory disruptions impacting steroid resistance in childhood acute lymphoblastic leukemia. Leukemia 36:2374-2383,2022. PMCID: PMC9522591 PUBMEDID: 36028659 NIHMSID: NIHMS1833642
Bisbee C, Campagne O, Gajjar A, Tinkle CL, Stewart CF. Population pharmacokinetics of crenolanib in children and young adults with brain tumors. Cancer Chemother Pharmacol 89:459-468,2022. PMCID: PMC8957602 PUBMEDID: 35212779 NIHMSID: NIHMS1786770
Bloom M, Oak N, Baskin-Doerfler R, Feng R, Iacobucci I, Baviskar P, Zhao X, Stroh AN, Li C, Ozark P, Tillman HS, Li Y, Verbist KC, Albeituni S, Scott DC, King MT, McKinney-Freeman SL, Weiss MJ, Yang JJ, Nichols KE. ETV6 represses inflammatory response genes and regulates HSPC function during stress hematopoiesis in mice. Blood Adv 7:5608-5623,2023. PMCID: PMC10514086 PUBMEDID: 37522715 NIHMSID:
Brady SW, Gout AM, Zhang J. Therapeutic and prognostic insights from the analysis of cancer mutational signatures. Trends Genet 38:194-208,2022. PMCID: PMC8752466 PUBMEDID: 34483003 NIHMSID: NIHMS1733775
Brady SW, Roberts KG, Gu Z, Shi L, Pounds S, Pei D, Cheng C, Dai Y, Devidas M, Qu C, Hill AN, Payne-Turner D, Ma X, Iacobucci I, Baviskar P, Wei L, Arunachalam S, Hagiwara K, Liu Y, Flasch DA, Liu Y, Parker M, Chen X, Elsayed AH, Pathak O, Li Y, Fan Y, Michael JR, Rusch M, Wilkinson MR, Foy S, Hedges DJ, Newman S, Zhou X, Wang J, Reilly C, Sioson E, Rice SV, Pastor Loyola V, Wu G, Rampersaud E, Reshmi SC, Gastier-Foster J, Guidry Auvil JM, Gesuwan P, Smith MA, Winick N, Carroll AJ, Heerema NA, Harvey RC, Willman CL, Larsen E, Raetz EA, Borowitz MJ, Wood BL, Carroll WL, Zweidler-McKay PA, Rabin KR, Mattano LA, Maloney KW, Winter SS, Burke MJ, Salzer W, Dunsmore KP, Angiolillo AL, Crews KR, Downing JR, Jeha S, Pui CH, Evans WE, Yang JJ, Relling MV, Gerhard DS, Loh ML, Hunger SP, Zhang J, Mullighan CG. The genomic landscape of pediatric acute lymphoblastic leukemia. Nat Genet 54:1376-1389,2022. PMCID: PMC9700506 PUBMEDID: 36050548 NIHMSID:
Brown A, Pan Q, Fan L, Indersie E, Tian C, Timchenko N, Li L, Hansen BS, Tan H, Lu M, Peng J, Pruett-Miller SM, Yu J, Cairo S, Zhu L. Ribonucleotide reductase subunit switching in hepatoblastoma drug response and relapse. Commun Biol 6:249-,2023. PMCID: PMC9992519 PUBMEDID: 36882565 NIHMSID:
Brown AL, Sok P, Raghubar KP, Lupo PJ, Richard MA, Morrison AC, Yang JJ, Stewart CF, Okcu MF, Chintagumpala MM, Gajjar A, Kahalley LS, Conklin H, Scheurer ME. Genetic susceptibility to cognitive decline following craniospinal irradiation for pediatric central nervous system tumors. Neuro Oncol 25:1698-1708,2023. PMCID: PMC10479777 PUBMEDID: 37038335 NIHMSID:
Cai J, Liu H, Chen Y, Yu J, Gao J, Jiang H, Zhai X, Ju X, Wu X, Wang N, Tian X, Liang C, Fang Y, Zhou F, Li H, Sun L, Yang L, Guo J, Liu A, Li CK, Zhu Y, Tang J, Yang JJ, Shen S, Cheng C, Pui CH. Effect of the tyrosine kinase inhibitors on the growth in children with Philadelphia chromosome-positive acute lymphoblastic leukemia: a case-control study. Lancet Reg Health West Pac 38:100818-,2023. PMCID: PMC10544282 PUBMEDID: 37790080 NIHMSID:
Campagne O, Wu H, Wu J, Naranjo A, Daryani VM, Gajjar AJ, Park JR, Stewart CF. Topotecan clearance based on a single sample and a population pharmacokinetic model: Application to a pediatric high-risk neuroblastoma clinical trial. Pediatr Blood Cancer 70:e30658-,2023. PMCID: PMC10538374 PUBMEDID: 37664968 NIHMSID:
Canté-Barrett K, Meijer MT, Cordo’ V, Hagelaar R, Yang W, Yu J, Smits WK, Nulle ME, Jansen JP, Pieters R, Yang JJ, Haigh JJ, Goossens S, Meijerink JP. MEF2C opposes Notch in lymphoid lineage decision and drives leukemia in the thymus. JCI Insight 7:-,2022. PMCID: PMC9310523 PUBMEDID: 35536646 NIHMSID:
Casado-García A, Isidro-Hernández M, Oak N, Mayado A, Mann-Ran C, Raboso-Gallego J, Alemán-Arteaga S, Buhles A, Sterker D, Sánchez EG, Martínez-Cano J, Blanco O, Orfao A, Alonso-López D, De Las Rivas J, Riesco S, Prieto-Matos P, González-Murillo Á, García Criado FJ, García Cenador MB, Radimerski T, Ramírez-Orellana M, Cobaleda C, Yang JJ, Vicente-Dueñas C, Weiss A, Nichols KE, Sánchez-García I. Transient inhibition of the JAK/STAT pathway prevents B-ALL development in genetically predisposed mice. Cancer Res 82:10981109,2022. PMCID: PMC9359729 PUBMEDID: 35131871 NIHMSID:
Caudle KE, Hoffman JM, Gammal RS. Pharmacogenomics implementation: “A little less conversation, a little more action, please”. Pharmacogenomics 24:183-186,2023. PMCID: PUBMEDID: 36946361 NIHMSID:
Chang Y, Keramatnia F, Ghate PS, Nishiguchi G, Gao Q, Iacobucci I, Yang L, Chepyala D, Mishra A, High AA, Goto H, Akahane K, Peng J, Yang JJ, Fischer M, Rankovic Z, Mullighan CG. The orally bioavailable GSPT1/2 degrader SJ6986 exhibits in vivo efficacy in acute lymphoblastic leukemia. Blood 142:629-642,2023. PMCID: PMC10447621 PUBMEDID: 37172201 NIHMSID:
Coffey M, Marino M, Lyren A, Purcell D, Hoffman JM, Brilli R, Muething S, Hyman D, Saysana M, Sharek PJ. Association between hospital-acquired harm outcomes and membership in a national patient safety collaborative. JAMA Pediatr 176:924-932,2022. PMCID: PMC9315995 PUBMEDID: 35877132 NIHMSID:
Crook JL, Lu Z, Wang X, Henderson N, Proctor KE, Maller VG, Prajapati HJ, Gold RE, Abdelhafeez AH, Talbot LJ, Pui CH, Davidoff AM, Hoffman JM, Murphy AJ. Why do subcutaneous ports get stuck? A case-control study. J Pediatr Surg 57:229-233,2022. PMCID: PUBMEDID: 34456040 NIHMSID:
DeWire M, Lazow M, Campagne O, Leach J, Fuller C, Senthil Kumar S, Stanek J, de Blank P, Hummel TR, Pillay-Smiley N, Salloum R, Stevenson CB, Baxter P, Gass D, Goldman S, Leary SES, Carle A, Mikael L, Crabtree D, Chaney B, Lane A, Drissi R, Stewart CF, Fouladi M. Phase I study of ribociclib and everolimus in children with newly diagnosed DIPG and high-grade glioma: A CONNECT pediatric neuro-oncology consortium report. Neurooncol Adv 4:vdac055-,2022. PMCID: PMC9122788 PUBMEDID: 35611273 NIHMSID:
Dickson AL, Daniel LL, Jackson E, Zanussi J, Yang W, Plummer WD, Dupont WD, Wei WQ, Nepal P, Hung AM, Cox NJ, Van Driest SL, Feng Q, Yang JJ, Stein CM, Mosley JD, Chung CP. Race, genotype, and azathioprine discontinuation : A cohort study. Ann Intern Med 175:1092-1099,2022. PMCID: PMC9378477 PUBMEDID: 35724382 NIHMSID: NIHMS1822059
Doorley LA, Barker KS, Zhang Q, Rybak JM, Rogers PD. Mutations in TAC1 and ERG11 are major drivers of triazole antifungal resistance in clinical isolates of Candida parapsilosis. Clin Microbiol Infect :-,2023. PMCID: PUBMEDID: 37666448 NIHMSID:
Doorley LA, Rybak JM, Berkow EL, Zhang Q, Morschhäuser J, Rogers PD. Candida parapsilosis Mdr1B and Cdr1B are drivers of Mrr1-mediated clinical fluconazole resistance. Antimicrob Agents Chemother 66:e0028922-,2022. PMCID: PMC9295576 PUBMEDID: 35699442 NIHMSID:
Dunn AD, Robinson SA, Nwokafor C, Estill M, Ferrante J, Shen L, Lemchi CO, Creus-Muncunill J, Ramirez A, Mengaziol J, Brynildsen JK, Leggas M, Horn J, Ehrlich ME, Blendy JA. Molecular and long-term behavioral consequences of neonatal opioid exposure and withdrawal in mice. Front Behav Neurosci 17:1202099,2023. PMCID: PMC10324024 PUBMEDID: 37424750 NIHMSID:
El-Boraie A, Tanner JA, Zhu AZX, Claw KG, Prasad B, Schuetz EG, Thummel KE, Fukunaga K, Mushiroda T, Kubo M, Benowitz NL, Lerman C, Tyndale RF. Functional characterization of novel rare CYP2A6 variants and potential implications for clinical outcomes. Clin Transl Sci 15:204-220,2022. PMCID: PMC8742641 PUBMEDID: 34476898 NIHMSID:
Escherich C, Chen W, Miyamoto S, Namikawa Y, Yang W, Teachey DT, Li Z, Raetz EA, Larsen E, Devidas M, Martin PL, Bowman WP, Wu G, Pui CH, Hunger SP, Loh ML, Takagi M, Yang JJ. Identification of TCF3 germline variants in pediatric B-cell acute lymphoblastic leukemia. Blood Adv 7:2177-2180,2022. PMCID: PMC10196986 PUBMEDID: 36576946 NIHMSID:
Evans WE, Pui CH. Remembering Donald Pinkel, MD: Acute lymphoblastic leukaemia pioneer September 7, 1927 -March 9, 2022. Leukemia :-,2022. PMCID: PUBMEDID: 35449233 NIHMSID:
Evans WI, Wilson MW, Bahrami A, Pappo AS, Hoehn ME. Uveal melanoma presenting as hepatic metastatis in a patient with culodermal melanocytosis. Retin Cases Brief Rep 17:403-405,2023. PMCID: PUBMEDID: 37364199 NIHMSID:
Fan L, Pan Q, Yang W, Koo SC, Tian C, Li L, Lu M, Brown A, Ju B, Easton J, Ranganathan S, Shin S, Bondoc A, Yang JJ, Yu J, Zhu L. A developmentally prometastatic niche to hepatoblastoma in neonatal liver mediated by the Cxcl1/Cxcr2 axis. Hepatology 76:1275-1290,2022. PMCID: PMC9385889 PUBMEDID: 35179799 NIHMSID: NIHMS1793851
Fan POL, Leung KT, Chan KYY, Leung AWK, Lam GKS, Chow TTW, Cheng FWT, Yuen LYP, Moriyama T, Yang JJ, Li CK. ABCC4, ITPA, NUDT15, TPMT and their interaction as genetic predictors of 6-mercaptopurine intolerance in chinese patients with acute lymphoblastic leukemia. Pediatr Hematol Oncol 39:254266,2022. PMCID: PUBMEDID: 34665987 NIHMSID:
Ferguson DC, McCorkle JR, Barnett KR, Bonten EJ, Bergeron BP, Bhattarai KR, Yang W, Smith C, Hansen BS, Bajpai R, Dong Q, Autry RJ, Gocho Y, Diedrich JD, Crews KR, Pruett-Miller SM, Roberts KG, Stock W, Mullighan CG, Inaba H, Jeha S, Pui CH, Yang JJ, Relling MV, Evans WE, Savic D. Amino acid stress response genes promote L-asparaginase resistance in pediatric acute lymphoblastic leukemia. Blood Adv 6:33863397,2022. PMCID: PMC9198938 PUBMEDID: 35671062 NIHMSID:
Finch ER, Janke LJ, Li L, Payton MA, Jenkins DA, Crews KR, Relling MV, Karol SE. Dasatinib does not exacerbate dexamethasone-induced osteonecrosis in murine models of acute lymphoblastic leukemia therapy. Pediatr Blood Cancer 69:e29490-,2022. PMCID: PMC8860849 PUBMEDID: 34866312 NIHMSID: NIHMS1766189
Flerlage JE, Myers JR, Maciaszek JL, Oak N, Rashkin SR, Hui Y, Wang YD, Chen W, Wu G, Chang TC, Hamilton K, Tithi SS, Goldin LR, Rotunno M, Caporaso N, Vogt A, Flamish D, Wyatt K, Liu J, Tucker M, Hahn CN, Brown AL, Scott HS, Mullighan C, Nichols KE, Metzger ML, McMaster ML, Yang JJ, Rampersaud E. Discovery of novel predisposing coding and noncoding variants in familial Hodgkin lymphoma. Blood 141:12931307,2023. PMCID: PMC10082357 PUBMEDID: 35977101 NIHMSID:
Gammal RS, Lee YM, Petry NJ, Iwuchukwu O, Hoffman JM, Kisor DF, Empey PE. Pharmacists leading the way to precision medicine: Updates to the Core Pharmacist Competencies in Genomics. Am J Pharm Educ 86:8634-,2022. PMCID: PMC10159420 PUBMEDID: 34301570 NIHMSID:
Gammal RS, Pirmohamed M, Somogyi AA, Morris SA, Formea CM, Elchynski AL, Oshikoya KA, McLeod HL, Haidar CE, Whirl-Carrillo M, Klein TE, Caudle KE, Relling MV. Expanded Clinical Pharmacogenetics Implementation Consortium guideline for medication use in the context of G6PD cenotype. Clin Pharmacol Ther 113:973-985,2023. PMCID: PMC10281211 PUBMEDID: 36049896 NIHMSID:
Gao Q, Ryan SL, Iacobucci I, Ghate PS, Cranston RE, Schwab C, Elsayed AH, Shi L, Pounds S, Lei S, Baviskar P, Pei D, Cheng C, Bashton M, Sinclair P, Bentley DR, Ross MT, Kingsbury Z, James T, Roberts KG, Devidas M, Fan Y, Chen W, Chang TC, Wu G, Carroll A, Heerema N, Valentine V, Valentine M, Yang W, Yang JJ, Moorman AV, Harrison CJ, Mullighan CG. The genomic landscape of acute lymphoblastic leukemia with intrachromosomal amplification of chromosome 21. Blood 142:711-723,2023. PMCID: PMC10460677
PUBMEDID: 37216686 NIHMSID:
Goodenough CG, Diouf B, Yang W, Sapkota Y, Finch ER, Lu L, Partin RE, Wogksch MD, Hudson MM, Robison LL, Wang Z, Jeha S, Evans WE, Ness KK. Association between CEP72 genotype and persistent neuropathy in survivors of childhood acute lymphoblastic leukemia. Leukemia 36:1160-1163,2022. PMCID: PMC8983435
PUBMEDID: 34980876 NIHMSID: NIHMS1757911
Goodings C, Zhao X, McKinney-Freeman S, Zhang H, Yang JJ. ARID5B influences B-cell development and function in mouse. Haematologica 108:502-512,2023. PMCID: PMC9890020 PUBMEDID: 35924577 NIHMSID:
Gose T, Aitken HM, Wang Y, Lynch J, Rampersaud E, Fukuda Y, Wills M, Baril SA, Ford RC, Shelat A, Mara MLO, Schuetz JD. The net electrostatic potential and hydration of ABCG2 affect substrate transport. Nat Commun 14:5035-,2023. PMCID: PMC10439158 PUBMEDID: 37596258 NIHMSID:
Haidar CE, Crews KR, Hoffman JM, Relling MV, Caudle KE. Advancing pharmacogenomics from single-gene to preemptive testing. Annu Rev Genomics Hum Genet 23:449-473,2022. PMCID: PMC9483991 PUBMEDID: 35537468 NIHMSID:
Haidar CE, Petry N, Oxencis C, Douglas JS, Hoffman JM. ASHP statement on the pharmacist’s role in clinical pharmacogenomics. Am J Health Syst Pharm 79:704-707,2022. PMCID: PUBMEDID: 34487145 NIHMSID:
Helmig SE, Hoffman JM. Building new standards to prevent harm from medication errors in children with cancer. Cancer 129:989-991,2023. PMCID: PUBMEDID: 36704992 NIHMSID:
Hijano DR, Ferrolino JA, Swift EG, Michaels CA, Max A, Hayden RT, Wolf J, Dallas RH, Greene WL, Richardson JL, Hakim H, Morton TH, Cross SJ. SARS-CoV-2 infection in high-risk children following tixagevimabcilgavimab (Evusheld) pre-exposure prophylaxis: A single-center observational study. Front Oncol 13:1229655-,2023. PMCID: PMC10436088 PUBMEDID: 37601666 NIHMSID:
Hijano DR, Hoffman JM, Tang L, Schultz-Cherry SL, Thomas PG, Hakim H, Webby RJ, Hayden RT, Gaur AH, St. Jude COVID-19 Employee Screening Program Team. An adaptive, asymptomatic SARS-CoV-2 workforce screening program providing real-time, actionable monitoring of the COVID-19 pandemic. PLoS One 17:e0268237-,2022. PMCID: PMC9075622 PUBMEDID: 35522615 NIHMSID:
Hijano DR, Hoffman JM, Webby RJ, Tang L, Hakim H, Hayden RT, Gaur AH. A nucleic acid amplification testbased strategy does not help inform return to work for healthcare workers with COVID-19. Influenza Other Respir Viruses 16:851-853,2022. PMCID: PMC9343333 PUBMEDID: 35615983 NIHMSID:
Hoffman JM, Cobaugh DJ. Pharmacy Forecast 2023: Balancing the urgency of now versus strategy for tomorrow. Am J Health Syst Pharm 80:1-2,2023. PMCID: PUBMEDID: 36314664 NIHMSID:
Hoffman JM, Thompson KK, Cobaugh DJ. Advancing pharmacogenomics into practice. Am J Health Syst Pharm 79:603-604,2022. PMCID: PMC8975574 PUBMEDID: 34999758 NIHMSID:
Hoshitsuki K, Zhou Y, Miller AM, Choi JK, Swanson HD, Bhakta NH, Jeha S, Karol SE, Ribeiro RC, Rubnitz JE, Mullighan CG, Cheng C, Yang JJ, Relling MV, Pui CH, Inaba H. Rituximab administration in pediatric patients with newly diagnosed acute lymphoblastic leukemia. Leukemia 37:1782-1791,2023. PMCID: PUBMEDID: 37543655 NIHMSID:
Hu J, Jarusiewicz J, Du G, Nishiguchi G, Yoshimura S, Panetta JC, Li Z, Min J, Yang L, Chepyala D, Actis M, Reyes N, Smart B, Pui CH, Teachey DT, Rankovic Z, Yang JJ. Preclinical evaluation of proteolytic targeting of LCK as a therapeutic approach in T cell acute lymphoblastic leukemia. Sci Transl Med 14:eabo5228-,2022. PMCID: PMC9730446 PUBMEDID: 36001679 NIHMSID:
Islam SMA, Díaz-Gay M, Wu Y, Barnes M, Vangara R, Bergstrom EN, He Y, Vella M, Wang J, Teague JW, Clapham P, Moody S, Senkin S, Li YR, Riva L, Zhang T, Gruber AJ, Steele CD, Otlu B, Khandekar A, Abbasi A, Humphreys L, Syulyukina N, Brady SW, Alexandrov BS, Pillay N, Zhang J, Adams DJ, Martincorena I, Wedge DC, Landi MT, Brennan P, Stratton MR, Rozen SG, Alexandrov LB. Uncovering novel mutational signatures by de novo extraction with SigProfilerExtractor. Cell Genom 2:None-,2022. PMCID: PMC9646490 PUBMEDID: 36388765 NIHMSID:
Jarusiewicz JA, Yoshimura S, Mayasundari A, Actis M, Aggarwal A, McGowan K, Yang L, Li Y, Fu X, Mishra V, Heath R, Narina S, Pruett-Miller SM, Nishiguchi G, Yang JJ, Rankovic Z. Phenyl dihydrouracil: An alternative cereblon binder for PROTAC design. ACS Med Chem Lett 14:141-145,2023. PMCID: PMC9923830 PUBMEDID: 36793425 NIHMSID:
Jiang C, Qian M, Gocho Y, Yang W, Du G, Shen S, Yang JJ, Zhang H. Genome-wide CRISPR/Cas9 screening identifies determinant of panobinostat sensitivity in acute lymphoblastic leukemia. Blood Adv 6:24962509,2022. PMCID: PMC9043932 PUBMEDID: 35192680 NIHMSID:
Karol SE, Pei D, Smith CA, Liu Y, Yang W, Kornegay NM, Panetta JC, Crews KR, Cheng C, Finch ER, Inaba H, Metzger ML, Rubnitz JE, Ribeiro RC, Gruber TA, Yang JJ, Evans WE, Jeha S, Pui CH, Relling MV. Comprehensive analysis of dose intensity of acute lymphoblastic leukemia chemotherapy. Haematologica 107:371-380,2022. PMCID: PMC8804576 PUBMEDID: 34196166 NIHMSID:
Kim JA, Crawford KA, Spada PA, Martin LR, Zhang J, Wong R, Reid JM, Stewart CF, Frank TM, Liu Q, Michalek JE, Keller C. Non-chemotherapy adjuvant agents in TP53 mutant Ewing sarcoma. Sci Rep 13:14360-,2023. PMCID: PMC10474113 PUBMEDID: 37658148 NIHMSID:
Kimura S, Montefiori L, Iacobucci I, Zhao Y, Gao Q, Paietta EM, Haferlach C, Laird AD, Mead PE, Gu Z, Stock W, Litzow M, Rowe JM, Luger SM, Hunger SP, Ryland GL, Schmidt B, Ekert PG, Oshlack A, Grimmond SM, Rehn J, Breen J, Yeung D, White DL, Aldoss I, Jabbour EJ, Pui CH, Meggendorfer M, Walter W, Kern W, Haferlach T, Brady S, Zhang J, Roberts KG, Blombery P, Mullighan CG. Enhancer retargeting of CDX2 and UBTF::ATXN7L3 define a subtype of high-risk B-progenitor acute lymphoblastic leukemia. Blood 139:35193531,2022. PMCID: PMC9203703 PUBMEDID: 35192684 NIHMSID:
Lee SHR, Antillon-Klussmann F, Pei D, Yang W, Roberts KG, Li Z, Devidas M, Yang W, Najera C, Lin HP, Tan AM, Ariffin H, Cheng C, Evans WE, Hunger SP, Jeha S, Mullighan CG, Loh ML, Yeoh AEJ, Pui CH, Yang JJ. Association of genetic ancestry with the molecular subtypes and prognosis of childhood acute lymphoblastic leukemia. JAMA Oncol 8:354-363,2022. PMCID: PMC8796058 PUBMEDID: 35084434
NIHMSID:
Lee SHR, Ashcraft E, Yang W, Roberts KG, Gocho Y, Rowland L, Inaba H, Karol SE, Jeha S, Crews KR, Mullighan CG, Relling MV, Evans WE, Cheng C, Yang JJ, Pui CH. Prognostic and pharmacotypic heterogeneity of hyperdiploidy in childhood ALL. J Clin Oncol :JCO2300880-,2023. PMCID: PUBMEDID: 37729596 NIHMSID:
Lee SHR, Li Z, Lim EHZ, Chin WHN, Jiang N, Chiew KH, Chen Z, Oh BLZ, Tan AM, Ariffin H, Yang JJ, Yeoh AEJ. Associations of T-cell receptor repertoire diversity with L-asparaginase allergy in childhood acute lymphoblastic leukemia. Cancers (Basel) 15:1829-,2023. PMCID: PMC10047007 PUBMEDID: 36980715
NIHMSID:
Lee SHR, Yang W, Gocho Y, John A, Rowland L, Smart B, Williams H, Maxwell D, Hunt J, Yang W, Crews KR, Roberts KG, Jeha S, Cheng C, Karol SE, Relling MV, Rosner GL, Inaba H, Mullighan CG, Pui CH, Evans WE, Yang JJ. Pharmacotypes across the genomic landscape of pediatric acute lymphoblastic leukemia and impact on treatment response. Nat Med 29:170-179,2023. PMCID: PMC9873558 PUBMEDID: 36604538
NIHMSID:
Li Y, Drabison T, Nepal M, Ho RH, Leblanc AF, Gibson AA, Jin Y, Yang W, Huang KM, Uddin ME, Chen M, DiGiacomo DF, Chen X, Razzaq S, Tonniges JR, McTigue DM, Mims AS, Lustberg MB, Wang Y, Hummon AB, Evans WE, Baker SD, Cavaletti G, Sparreboom A, Hu S. Targeting a xenobiotic transporter to ameliorate vincristine-induced sensory neuropathy. JCI Insight 8:e164646-,2023. PMCID: PMC10443802 PUBMEDID: 37347545 NIHMSID:
Li Y, Moriyama T, Yoshimura S, Zhao X, Li Z, Yang X, Paietta E, Litzow MR, Konopleva M, Yu J, Inaba H, Ribeiro RC, Pui CH, Yang JJ. PAX5 epigenetically orchestrates CD58 transcription and modulates blinatumomab response in acute lymphoblastic leukemia. Sci Adv 8:eadd6403-,2022. PMCID: PMC9750140 PUBMEDID: 36516256 NIHMSID:
Li Y, Yang X, Sun Y, Li Z, Yang W, Ju B, Easton J, Pei D, Cheng C, Lee S, Pui CH, Yu J, Chi H, Yang JJ. Impact of T-cell immunity on chemotherapy response in childhood acute lymphoblastic leukemia. Blood 140:15071521,2022. PMCID: PMC9523375 PUBMEDID: 35675514 NIHMSID:
Li Z, Chang TC, Junco JJ, Devidas M, Li Y, Yang W, Huang X, Hedges DJ, Cheng Z, Shago M, Carroll AJ, Heerema NA, Gastier-Foster J, Wood BL, Borowitz MJ, Sanclemente L, Raetz EA, Hunger SP, Feingold E, Rosser TC, Sherman SL, Loh ML, Mullighan CG, Yu J, Wu G, Lupo PJ, Rabin KR, Yang JJ. Genomic landscape of Down syndrome-associated acute lymphoblastic leukemia. Blood 142:172-184,2023. PMCID: PMC10352600 PUBMEDID: 37001051 NIHMSID:
Liu J, Vogel AK, Miao J, Carnahan JA, Lowes DJ, Rybak JM, Peters BM. Rapid hypothesis testing in Candida albicans clinical isolates using a cloning-free, modular, and recyclable system for CRISPR-Cas9 mediated mutant and revertant construction. Microbiol Spectr 10:e0263021-,2022. PMCID: PMC9241802 PUBMEDID: 35612314 NIHMSID:
Liu Y, Klein J, Bajpai R, Dong L, Tran Q, Kolekar P, Smith JL, Ries RE, Huang BJ, Wang YC, Alonzo TA, Tian L, Mulder HL, Shaw TI, Ma J, Walsh MP, Song G, Westover T, Autry RJ, Gout AM, Wheeler DA, Wan S, Wu G, Yang JJ, Evans WE, Loh M, Easton J, Zhang J, Klco JM, Meshinchi S, Brown PA, Pruett-Miller SM, Ma X. Etiology of oncogenic fusions in 5,190 childhood cancers and its clinical and therapeutic implication. Nat Commun 14:1739-,2023. PMCID: PMC10076316 PUBMEDID: 37019972 NIHMSID:
Lubas MM, Mandrell BN, Greene WL, Howell CR, Christensen R, Kimberg CI, Li C, Ness KK, Srivastava DK, Hudson MM, Robison LL, Krull KR, Brinkman TM. A randomized double-blind placebo-controlled trial of the effectiveness of melatonin on neurocognition and sleep in survivors of childhood cancer. Pediatr Blood Cancer 69:e29393-,2022. PMCID: PMC8859989 PUBMEDID: 34674368 NIHMSID: NIHMS1770872
Lynch J, Wang Y, Li Y, Kavdia K, Fukuda Y, Ranjit S, Robinson CG, Grace CR, Xia Y, Peng J, Schuetz JD. A PPIXbinding probe facilitates discovery of PPIX-induced cell death modulation by peroxiredoxin. Commun Biol 6:673-,2023. PMCID: PMC10290680 PUBMEDID: 37355765 NIHMSID:
Maillard M, Gong L, Nishii R, Yang JJ, Whirl-Carrillo M, Klein TE. PharmGKB summary: Acyclovir/ganciclovir pathway. Pharmacogenet Genomics 32:201-208,2022. PMCID: PMC9179945 PUBMEDID: 35665708 NIHMSID:
Mangum DS, Bishop JD, Zhou Y, Cheng C, Karol SE, Rubnitz JE, Ribeiro RC, Yang JJ, Mullighan CG, Jeha S, Pui CH, Inaba H. Characterisation of children and adolescents with acute lymphoblastic leukaemia who presented without peripheral blood blasts at diagnosis. Br J Haematol 200:338-343,2023. PMCID: PMC9852218 PUBMEDID: 36352514 NIHMSID:
Manolio TA, Narula J, Bult CJ, Chisholm RL, Deverka PA, Ginsburg GS, Goldrich M, Green ED, Jarvik GP, Mensah GA, Ramos EM, Relling MV, Roden DM, Rowley R, Williams MS. Genomic Medicine Year in Review: 2022. Am J Hum Genet 109:2101-2104,2022. PMCID: PMC9808495 PUBMEDID: 36459977 NIHMSID:
Miller JS, Bada HS, Leggas M, Westgate PM. Assessment of the relative clinical utility of shortened Finnegan neonatal abstinence scoring tools. J Perinatol 42:1051-1057,2022. PMCID: PUBMEDID: 35660789 NIHMSID:
Moriyama T, Yang W, Smith C, Pui CH, Evans WE, Relling MV, Bhatia S, Yang JJ. Comprehensive characterization of pharmacogenetic variants in TPMT and NUDT15 in children with acute lymphoblastic leukemia. Pharmacogenet Genomics 32:60-66,2022. PMCID: PMC8702453 PUBMEDID: 34412101 NIHMSID: NIHMS1726174
Morris SA, Crews KR, Hayden RT, Takemoto CM, Yang W, Baker DK, Broeckel U, Relling MV, Haidar CE. Incorporating G6PD genotyping to identify patients with G6PD deficiency. Pharmacogenet Genomics 32:87-93,2022. PMCID: PMC8976699 PUBMEDID: 34693927 NIHMSID:
Nair S, Davis A, Campagne O, Schuetz JD, Stewart CF. Development and validation of a sensitive and specific LC-MS/MS method for IWR-1-endo, a Wnt signaling inhibitor: Application to a cerebral microdialysis study. Molecules 27:-,2022. PMCID: PMC9457781 PUBMEDID: 36080214 NIHMSID:
Nguyen JQ, Crews KR, Moore BT, Kornegay NM, Baker DK, Hasan M, Campbell PK, Dean SM, Relling MV, Hoffman JM, Haidar CE. Clinician adherence to pharmacogenomics prescribing recommendations in clinical decision support alerts. J Am Med Inform Assoc 30:132-138,2022. PMCID: PMC9748527 PUBMEDID: 36228116 NIHMSID:
Perkins RS, Davis A, Campagne O, Owens TS, Stewart CF. CNS penetration of methotrexate and its metabolite 7-hydroxymethotrexate in mice bearing orthotopic Group 3 medulloblastoma tumors and model-based simulations for children. Drug Metab Pharmacokinet 48:100471-,2023. PMCID: PUBMEDID: 36669926 NIHMSID:
Pribnow A, Jonchere B, Liu J, Smith KS, Campagne O, Xu K, Robinson S, Patel Y, Onar-Thomas A, Wu G, Stewart CF, Northcott PA, Yu J, Robinson GW, Roussel MF. Combination of ribociclib and gemcitabine for the treatment of medulloblastoma. Mol Cancer Ther 21:1306-1317,2022. PMCID: PMC9578677 PUBMEDID: 35709750 NIHMSID:
Rabbani N, Pageler NM, Hoffman JM, Longhurst C, Sharek PJ. Association between electronic health record implementations and hospital-acquired conditions in pediatric hospitals. Appl Clin Inform 14:521-527,2023. PMCID: PMC10338103 PUBMEDID: 37075806 NIHMSID:
Rabin KR, Devidas M, Chen Z, Ji L, Kairalla J, Hitzler JK, Yang JJ, Carroll AJ, Heerema NA, Borowitz MJ, Wood BL, Roberts KG, Mullighan CG, Harvey RC, Chen IM, Willman CL, Reshmi SC, Gastier-Foster JM, Bhojwani D, Rheingold SR, Maloney KW, Mattano LA, Larsen EC, Schore RJ, Burke MJ, Salzer WL, Winick NJ, Carroll WL, Raetz EA, Loh ML, Hunger SP, Angiolillo AL. Outcomes in children, adolescents, and young adults with Down syndrome and ALL: A report From the Children’s Oncology Group. J Clin Oncol :JCO2300389-,2023. PMCID: PUBMEDID: 37890117 NIHMSID:
Rahrmann EP, Shorthouse D, Jassim A, Hu LP, Ortiz M, Mahler-Araujo B, Vogel P, Paez-Ribes M, Fatemi A, Hannon GJ, Iyer R, Blundon JA, Lourenço FC, Kay J, Nazarian RM, Hall BA, Zakharenko SS, Winton DJ, Zhu L, Gilbertson RJ. The NALCN channel regulates metastasis and nonmalignant cell dissemination. Nat Genet 54:1827-1838,2022. PMCID: PMC9729110 PUBMEDID: 36175792 NIHMSID:
Rogers PD, Lee RE. Editorial overview: Recent advances in antimicrobial drug discovery and resistance. Curr Opin Microbiol 71:102242-,2023. PMCID: PMC10364994 PUBMEDID: 36423503 NIHMSID:
Rogers PD. Sterol homeostasis in yeast. Nat Chem Biol 18:1170-1171,2022. PMCID: PUBMEDID: 36229682 NIHMSID:
Rowland L, Smart B, Brown A, Dettorre GM, Gocho Y, Hunt J, Yang W, Yoshimura S, Reyes N, Du G, John A, Maxwell D, Stock W, Kornblau S, Relling MV, Inaba H, Pui CH, Bourquin JP, Karol SE, Mullighan CG, Evans WE, Yang JJ, Crews KR. Ex vivo drug sensitivity imaging-based platform for primary acute lymphoblastic leukemia cells. Bio Protoc 13:e4731-,2023. PMCID: PMC10415213 PUBMEDID: 37575398 NIHMSID:
Rybak JM, Barker KS, Muñoz JF, Parker JE, Ahmad S, Mokaddas E, Abdullah A, Elhagracy RS, Kelly SL, Cuomo CA, Rogers PD. In vivo emergence of high-level resistance during treatment reveals the first identified mechanism of amphotericin B resistance in Candida auris. Clin Microbiol Infect 28:838-843,2022. PMCID: PMC9467277 PUBMEDID: 34915074 NIHMSID:
Rybak JM, Cuomo CA, David Rogers P. The molecular and genetic basis of antifungal resistance in the emerging fungal pathogen Candida auris. Curr Opin Microbiol 70:102208-,2022. PMCID: PMC10364995 PUBMEDID: 36242897 NIHMSID:
Saleh MAA, Gülave B, Campagne O, Stewart CF, Elassaiss-Schaap J, de Lange ECM. Using the LeiCNS-PK3.0 physiologically-based pharmacokinetic model to predict brain extracellular fluid pharmacokinetics in mice. Pharm Res :-,2023. PMCID: PUBMEDID: 37442882 NIHMSID:
Sapkota Y, Ehrhardt MJ, Qin N, Wang Z, Liu Q, Qiu W, Shelton K, Shao Y, Plyler E, Mulder HL, Easton J, Michael JR, Burridge PW, Wang X, Wilson CL, Jefferies JL, Chow EJ, Oeffinger KC, Morton LM, Li C, Yang JJ, Zhang J, Bhatia S, Mulrooney DA, Hudson MM, Robison LL, Armstrong GT, Yasui Y. A novel locus on 6p21.2 for cancer treatment-induced cardiac dysfunction among childhood cancer survivors. J Natl Cancer Inst 114:1109-1116,2022. PMCID: PMC9360468 PUBMEDID: 35698272 NIHMSID:
Schore RJ, Angiolillo AL, Kairalla JA, Devidas M, Rabin KR, Zweidler-McKay P, Borowitz MJ, Wood B, Carroll AJ, Heerema NA, Relling MV, Hitzler J, Kadan-Lottick NS, Maloney K, Wang C, Carroll WL, Winick NJ, Raetz EA, Loh ML, Hunger SP. Correction: Outstanding outcomes with two low intensity regimens in children with low-risk B-ALL: A report from COG AALL0932. Leukemia :-,2023. PMCID: PUBMEDID: 37157018 NIHMSID:
Schore RJ, Angiolillo AL, Kairalla JA, Devidas M, Rabin KR, Zweidler-McKay P, Borowitz MJ, Wood B, Carroll AJ, Heerema NA, Relling MV, Hitzler J, Kadan-Lottick NS, Maloney K, Wang C, Carroll WL, Winick NJ, Raetz EA, Loh ML, Hunger SP. Outstanding outcomes with two low intensity regimens in children with low-risk B-ALL: a report from COG AALL0932. Leukemia 37:1375-1378,2023. PMCID: PMC10503688 PUBMEDID: 36966262 NIHMSID:
Scott ER, Yang Y, Botton MR, Seki Y, Hoshitsuki K, Harting J, Baybayan P, Cody N, Nicoletti P, Moriyama T, Chakraborty S, Yang JJ, Edelmann L, Schadt EE, Korlach J, Scott SA. Long-read HiFi sequencing of NUDT15: Phased full-gene haplotyping and pharmacogenomic allele discovery. Hum Mutat 43:1557-1566,2022. PMCID: PMC9875722 PUBMEDID: 36057977 NIHMSID:
Smith J, Sun Y, Hijano DR, Hoffman JM, Hakim H, Webby RJ, Hayden RT, Gaur AH, Armstrong GT, Mori M, Tang L. covidscreen: A web app and R Package for assessing asymptomatic COVID-19 testing strategies. BMC Public Health 22:1361-,2022. PMCID: PMC9284969 PUBMEDID: 35840948 NIHMSID:
Souza ACO, Ge W, Wiederhold NP, Rybak JM, Fortwendel JR, Rogers PD. hapE and hmg1 mutations are drivers of cyp51A-independent pan-triazole resistance in an Aspergillus fumigatus clinical isolate. Microbiol Spectr 11:e0518822-,2023. PMCID: PMC10269825 PUBMEDID: 37140376 NIHMSID:
Tao H, Dar HY, Tian C, Banerjee S, Glazer ES, Srinivasan S, Zhu L, Pacifici R, He P. Differences in hepatocellular iron metabolism underlie sexual dimorphism in hepatocyte ferroptosis. Redox Biol 67:102892-,2023. PMCID: PMC10519854 PUBMEDID: 37741044 NIHMSID:
Terao M, Stokes CL, Sitthi-Amorn J, Vinitsky A, Burlison JD, Baker JN, Li C, Lu Z, McDonald M, Hoffman JM. Quality improvement knowledge in pediatric hematology/oncology physicians: A need for improved education. Pediatr Blood Cancer 69:e29794-,2022. PMCID: PUBMEDID: 35614566 NIHMSID:
Tian C, Li L, Fan L, Brown A, Norris EJ, Morrison M, Glazer ES, Zhu L. A hepatoprotective role of peritumoral non-parenchymal cells in early liver tumorigenesis. Dis Model Mech 16:dmm049750-,2023. PMCID: PMC10040241 PUBMEDID: 36728410 NIHMSID:
Tian C, Li L, Pan Q, Xu B, Li Y, Fan L, Brown A, Morrison M, Dey K, Yang JJ, Yu J, Glazer ES, Zhu L. Spatiotemporal regulation of cholangiocarcinoma growth and dissemination by peritumoral myofibroblasts in a Vcam1-dependent manner. Oncogene 42:1196-1208,2023. PMCID: PMC10079548 PUBMEDID: 36828890 NIHMSID:
Tichy EM, Hoffman JM, Suda KJ, Rim MH, Tadrous M, Cuellar S, Clark JS, Ward J, Schumock GT. National trends in prescription drug expenditures and projections for 2022. Am J Health Syst Pharm 79:11581172,2022. PMCID: PMC9383648 PUBMEDID: 35385103 NIHMSID:
Tichy EM, Hoffman JM, Tadrous M, Rim MH, Suda KJ, Cuellar S, Clark JS, Newell MK, Schumock GT. National trends in prescription drug expenditures and projections for 2023. Am J Health Syst Pharm 80:899913,2023. PMCID: PUBMEDID: 37094296 NIHMSID:
Toksvang LN, Lee SHR, Yang JJ, Schmiegelow K. Maintenance therapy for acute lymphoblastic leukemia: Basic science and clinical translations. Leukemia 36:1749-1758,2022. PMCID: PMC9252897 PUBMEDID: 35654820 NIHMSID:
Upadhyaya SA, Campagne O, Billups CA, Orr BA, Onar-Thomas A, Tatevossian RG, Mostafavi R, Myers JR, Vinitsky A, Moreira DC, Lindsay HB, Kilburn L, Baxter P, Smith A, Crawford JR, Partap S, Bendel AE, Aguilera DG, Nichols KE, Rampersaud E, Ellison DW, Klimo P, Patay Z, Robinson GW, Broniscer A, Stewart CF, Wetmore C, Gajjar A. Phase II study of alisertib as a single agent for treating recurrent or progressive atypical teratoid/rhabdoid tumor. Neuro Oncol 25:386-397,2023. PMCID: PMC9925713 PUBMEDID: 35652336 NIHMSID:
van de Velde ME, Uittenboogaard A, Yang W, Bonten E, Cheng C, Pei D, van den Berg MH, van der Sluis IM, van den Bos C, Abbink FCH, van den Heuvel-Eibrink MM, Segers H, Chantrain C, van der Werff Ten Bosch J, Willems L, Evans WE, Kaspers GJL. Genetic polymorphisms associated with vincristine pharmacokinetics and vincristine-induced peripheral neuropathy in pediatric oncology patients. Cancers (Basel) 14:3510,2022. PMCID: PMC9321338 PUBMEDID: 35884569 NIHMSID:
Wan Y, Zhang H, Zhang L, Cai J, Yu J, Hu S, Fang Y, Gao J, Jiang H, Yang M, Liang C, Jin R, Tian X, Ju X, Hu Q, Jiang H, Li H, Wang N, Sun L, Leung AWK, Wu X, Wang J, Li CK, Yang J, Tang J, Shen S, Zhai X, Pui CH, Zhu X. Extended vincristine and dexamethasone pulse therapy may not be necessary for children with TCF3PBX1 positive acute lymphoblastic leukaemia. Br J Haematol 199:587-596,2022. PMCID: PMC9649883 PUBMEDID: 36114009 NIHMSID: NIHMS1837119
Wang T, Tang Y, Cai J, Wan X, Hu S, Lu X, Xie Z, Qiao X, Jiang H, Shao J, Yang F, Ren H, Cao Q, Qian J, Zhang J, An K, Wang J, Luo C, Liang H, Miao Y, Ma Y, Wang X, Ding L, Song L, He H, Shi W, Xiao P, Yang X, Yang J, Li W, Zhu Y, Wang N, Gu L, Chen Q, Tang J, Yang JJ, Cheng C, Leung W, Chen J, Lu J, Li B, Pui CH. Coadministration of CD19- and CD22-directed chimeric antigen receptor T-cell therapy in childhood B-cell acute lymphoblastic leukemia: A single-arm, multicenter, phase II trial. J Clin Oncol 41:1670-1683,2023. PMCID: PMC10419349 PUBMEDID: 36346962 NIHMSID:
Wiley K, Findley L, Goldrich M, Rakhra-Burris TK, Stevens A, Williams P, Bult CJ, Chisholm R, Deverka P, Ginsburg GS, Green ED, Jarvik G, Mensah GA, Ramos E, Relling MV, Roden DM, Rowley R, Alterovitz G, Aronson S, Bastarache L, Cimino JJ, Crowgey EL, Del Fiol G, Freimuth RR, Hoffman MA, Jeff J, Johnson K, Kawamoto K, Madhavan S, Mendonca EA, Ohno-Machado L, Pratap S, Taylor CO, Ritchie MD, Walton
N, Weng C, Zayas-Cabán T, Manolio TA, Williams MS. A research agenda to support the development and implementation of genomics-based clinical informatics tools and resources. J Am Med Inform Assoc 29:1342-1349,2022. PMCID: PMC9277642 PUBMEDID: 35485600 NIHMSID:
Wright S, Hu J, Hyle J, Zhang Y, Du G, Konopleva MY, Kornblau SM, Djekidel MN, Rosikiewicz W, Xu B, Lu R, Yang JJ, Li C. Interrogating bromodomain inhibitor resistance in KMT2A-rearranged leukemia through combinatorial CRISPR screens. Proc Natl Acad Sci U S A 120:e2220134120-,2023. PMCID: PMC10120025
PUBMEDID: 37036970 NIHMSID:
Yang H, Zhang H, Luan Y, Liu T, Yang W, Roberts KG, Qian MX, Zhang B, Yang W, Perez-Andreu V, Xu J, Iyyanki S, Kuang D, Stasiak LA, Reshmi SC, Gastier-Foster J, Smith C, Pui CH, Evans WE, Hunger SP, Platanias LC, Relling MV, Mullighan CG, Loh ML, Yue F, Yang JJ. Noncoding genetic variation in GATA3 increases acute lymphoblastic leukemia risk through local and global changes in chromatin conformation. Nat Genet 54:170-179,2022. PMCID: PMC9794680 PUBMEDID: 35115686 NIHMSID:
Yang W, Karol SE, Hoshitsuki K, Lee S, Larsen EC, Winick N, Carroll WL, Loh ML, Raetz EA, Hunger SP, Winter SS, Dunsmore KP, Devidas M, Relling MV, Yang JJ. Association of inherited genetic factors with drug-induced hepatic damage among children with acute lymphoblastic leukemia. JAMA Netw Open 5:e2248803-,2022. PMCID: PMC9857512 PUBMEDID: 36580335 NIHMSID:
Yoshida M, Brown SA, Moriyama T, Nishii R, Tsujimoto SI, Yamada Y, Yoshida K, Shirai R, Osumi T, Utano T, Fukano R, Kudo K, Sakaguchi K, Arakawa Y, Koh K, Sekiguchi M, Sekimizu M, Miyamura T, Ishida H, Inukai T, Tomizawa D, Kiyokawa N, Kato M, Yang JJ. Low NUDT15 expression levels due to biallelic NUDT15 variants and 6-mercaptopurine intolerance. Br J Haematol 199:270-276,2022. PMCID: PMC9547862 PUBMEDID: 35905175 NIHMSID: NIHMS1824276
Yoshida M, Nakabayashi K, Yang W, Sato-Otsubo A, Tsujimoto SI, Ogata-Kawata H, Kawai T, Ishiwata K, Sakamoto M, Okamura K, Yoshida K, Shirai R, Osumi T, Kiyotani C, Shioda Y, Terashima K, Ishimaru S, Yuza Y, Takagi M, Arakawa Y, Imamura T, Hasegawa D, Inoue A, Yoshioka T, Ito S, Tomizawa D, Koh K, Matsumoto K, Kiyokawa N, Ogawa S, Manabe A, Niwa A, Hata K, Yang JJ, Kato M. Prevalence of pathogenic variants in cancer-predisposing genes in second cancer after childhood solid cancers. Cancer Med 12:1126411273,2023. PMCID: PMC10242325 PUBMEDID: 37021926 NIHMSID:
Yoshimura S, Panetta JC, Hu J, Li L, Gocho Y, Du G, Umezawa A, Karol SE, Pui CH, Mullighan CG, Konopleva M, Stock W, Teachey DT, Jain N, Yang JJ. Preclinical pharmacokinetic and pharmacodynamic evaluation of dasatinib and ponatinib for the treatment of T-cell acute lymphoblastic leukemia. Leukemia 37:11941203,2023. PMCID: PMC10347458 PUBMEDID: 37076694 NIHMSID:
Yu CH, Jou ST, Su YH, Coustan-Smith E, Wu G, Cheng CN, Lu MY, Lin KH, Wu KH, Chen SH, Huang FL, Chang HH, Wang JL, Yen HJ, Li MJ, Chou SW, Ho WL, Liu YL, Chang CC, Lin ZS, Lin CY, Chen HY, Ni YL, Lin DT, Lin SW, Yang JJ, Ni YH, Pui CH, Yu SL, Yang YL. Clinical impact of minimal residual disease and genetic subtypes on the prognosis of childhood acute lymphoblastic leukemia. Cancer 129:790-802,2023. PMCID: PUBMEDID: 36537587 NIHMSID:
Yu CH, Wu G, Chang CC, Jou ST, Lu MY, Lin KH, Chen SH, Wu KH, Huang FL, Cheng CN, Chang HH, Hedges D, Wang JL, Yen HJ, Li MJ, Chou SW, Hung CT, Lin ZS, Lin CY, Chen HY, Ni YL, Hsu YC, Lin DT, Lin SW, Yang JJ, Pui CH, Yu SL, Yang YL. Sequential approach to improve the molecular classification of childhood acute lymphoblastic leukemia. J Mol Diagn 24:1195-1206,2022. PMCID: PMC9667711 PUBMEDID: 35963521 NIHMSID:
Zhang H, Wan Y, Wang H, Cai J, Yu J, Hu S, Fang Y, Gao J, Jiang H, Yang M, Liang C, Jin R, Tian X, Ju X, Hu Q, Jiang H, Li Z, Wang N, Sun L, Leung AWK, Wu X, Qian X, Qian M, Li CK, Yang J, Tang J, Zhu X, Shen S, Zhang L, Pui CH, Zhai X. Prognostic factors of childhood acute lymphoblastic leukemia with TCF3::PBX1 in CCCGALL-2015: A multicenter study. Cancer 129:1691-1703,2023. PMCID: PUBMEDID: 36943767 NIHMSID:
Zhao X, Qian M, Goodings C, Zhang Y, Yang W, Wang P, Xu B, Tian C, Pui CH, Hunger SP, Raetz EA, Devidas M, Relling MV, Loh ML, Savic D, Li C, Yang JJ. Molecular mechanisms of ARID5B-mediated genetic susceptibility to acute lymphoblastic leukemia. J Natl Cancer Inst 114:1287-1295,2022. PMCID: PMC9468286 PUBMEDID: 35575404 NIHMSID:
Zhao X, Wang P, Diedrich JD, Smart B, Reyes N, Yoshimura S, Zhang J, Yang W, Barnett K, Xu B, Li Z, Huang X, Yu J, Crews K, Yeoh AEJ, Konopleva M, Wei CL, Pui CH, Savic D, Yang JJ. Epigenetic activation of the FLT3 gene by ZNF384 fusion confers a therapeutic susceptibility in acute lymphoblastic leukemia. Nat Commun 13:5401-,2022. PMCID: PMC9474531 PUBMEDID: 36104354 NIHMSID:
Zheng Y, Yang W, Estepp J, Pei D, Cheng C, Takemoto CM, Inaba H, Jeha S, Pui CH, Relling MV, Karol SE. Genomic analysis of venous thrombosis in children with acute lymphoblastic leukemia from diverse ancestries. Haematologica :-,2023. PMCID: PUBMEDID: 37408475 NIHMSID:
Zhu J, Miller JN, Schuetz JD. An ABC transporter as a potential target against SHH-Medulloblastoma: From benchtop to bedside. Oncotarget 13:1017-1019,2022. PMCID: PMC9457923 PUBMEDID: 36093294 NIHMSID:
Zou C, Beard JA, Yang G, Evans WE, Bonten EJ. CASPorter: A novel inducible human CASP1/NALP3/ASC inflammasome biosensor. J Inflamm Res 15:1183-1194,2022. PMCID: PMC8865862 PUBMEDID: 35221708 NIHMSID:
Zudeh G, Franca R, Lucafò M, Bonten EJ, Bramuzzo M, Sgarra R, Lagatolla C, Franzin M, Evans WE, Decorti G, Stocco G. PACSIN2 as a modulator of autophagy and mercaptopurine cytotoxicity: Mechanisms in lymphoid and intestinal cells. Life Sci Alliance 6:-,2023. PMCID: PMC9811133 PUBMEDID: 36596605 NIHMSID: