2024 ANNUAL REPORT
2024 ANNUAL REPORT



96%
MSN and Higher Degrees for Leadership
69%
Eligible Clinical Nurses with Specialty Certifications


95%
Clinical Nurses with Bachelor’s or Higher in Nursing
71%
Eligible Nurses with Specialty Certifications

Number of APRNs

Certification Rates for Leadership
100% 700
Number of Nurses


Nursing
Colleagues,
I am excited to celebrate our Nursing annual report with you. Woven throughout the stories are repeated examples of our care, dedication, and compassion. Ingenuity shines through as time after time nurses show up to solve challenges, work with urgency, and collaborate on improvement initiatives.
In the following pages, you’ll learn about enhancing care coordination and pressure injury prevention. You’ll gain insights into our leadership development and mentoring. Over the past year, we added needed infrastructure to our central staffing office and revised emergency response by integrating tiered intervention. The Center of Advanced Practice creatively developed the AWAKE project to reduce anesthesia and introduced their career ladder.
We had many occasions to celebrate this year, as our nurses and care teams were recognized for excellence within St. Jude, in the local community, in our health care field, and even internationally. Our influence reached around the world as we completed our first cohort of our global evidenced-based practice fellowship.
Our years-long preparation for Magnet redesignation culminated in submitting our evidence two weeks early, and we are optimistically waiting for the results of our site visit. I am confident the appraisers will confirm what we already know — our demonstrated and unwavering commitment to excellence.
The artwork you see decorating the report comes from our patients. Their colorful images are simple gifts to enjoy as you journey through the pages.
Let this report be a celebration — and a reminder — that your work matters and that together we can ensure the best possible care for our patients and families. Thank you to each and every one of our nurses for their individual contributions to our joint success.
Warmly,

Sarah Currie, MSN, RNC, NEA-BC Senior Vice President and Chief Nursing Executive

The year 2024 marked a period of significant growth and achievement for the Care Coordination team. Through strategic leadership enhancements, expanded patient support initiatives, and data-driven improvements in patient outcomes, the team has further reinforced its commitment to delivering high-quality, patient-centered care.
A key milestone was the promotion of two highly experienced care coordinators, Raechyl Moore, MSN, RN, and Tonita Robinson, MBA, BSN, RN, to supervisor roles. Their clinical expertise, leadership, and strategic vision brings added strength to the team, reinforcing efforts to enhance care across the continuum and ensure continued excellence in patient care.

Across service lines, the Care Coordination team has driven meaningful change by addressing complex care needs and implementing innovative strategies. Notably, Jess Abutu, MSN, RN, Jeri Thomas, MBTS, BSN, RN, and Nicole Pankey, MSPH, BSN, RN, spearheaded an initiative that significantly improved stroke prevention screening rates for sickle cell disease (SCD) patients, increasing screening rates from 71% in 2023 to 98% in 2024. Additionally, Sabrina Kelly, MSN, RN, led a cross-service effort to enhance discharge planning and patient choice documentation. Her collaboration with the Epic team optimized electronic health record tools and streamlined workflows, improving both efficiency and the overall patient experience. In addition, all Oncology service line coordinators have dedicated additional time to outpatient clinic support, helping to ensure continuity of care throughout the patient journey.
These achievements reflect the dedication, expertise, and teamwork that define the Care Coordination team. The team remains focused on advancing initiatives that elevate the quality of care and empower patients as they navigate their health care experience.

Clear role delineation is vital to maintaining seamless operations, quality patient care, and optimal team performance at St. Jude Children’s Research Hospital. In support of these goals, Sarah Currie, RNC, MSN, NEA-BC, senior vice president and chief nursing executive, championed the implementation of a RACI (Responsible, Accountable, Consulted, Informed) framework to define leadership roles more clearly across nursing services. This strategic initiative aims to eliminate role ambiguity, streamline workflows, and enhance accountability, aligning closely with St. Jude core values and strategic priorities.
The RACI project was thoughtfully structured into two distinct phases: RACI Development and RACI Implementation. The RACI Development phase was led by a select group of nursing leaders who laid the groundwork by identifying key leadership responsibilities, defining role expectations, and designing the initial RACI chart. This foundational work provided the blueprint for clarity and consistency in nursing leadership roles across the organization.
Currently, St. Jude is in the RACI Implementation phase, which has expanded the working group to include new members alongside some from the original development team. This intentional restructuring ensures diverse representation, bringing fresh perspectives and comprehensive insights from various practice areas, including inpatient, outpatient, Nursing Surgical Services and clinical support services. The broader participation helps tailor the RACI framework to meet the unique needs of all nursing leaders and fosters a more inclusive implementation process.
While the vision originated from Currie, the project’s progress is driven by the expert facilitation of Morgan Melancon, MSN, RN, CCRN, NE-BC, director of Nursing Education and Professional Development, and Nancy Ballinger, clinical program manager of Nursing Administration. Together, they continue to orchestrate the ongoing implementation activities, ensuring that all efforts remain aligned with the overarching goals of clarity, consistency, and accountability.
The RACI Implementation phase requires navigating complexities related to data access, role ambiguity, and workflow inconsistencies across units. To address these issues, the team has employed tools such as force field analyses to identify barriers and enablers. For example, data visibility issues have prompted collaborations with Epic specialists and internal stakeholders to improve how leaders make informed decisions.
Understanding that change management is often met with resistance, the implementation team adopted a phased rollout strategy, giving leaders time to adapt to new expectations. Additionally, tools such as “Permission Slip” were introduced to encourage participants to acknowledge the challenges of change and commit to the process. This approach supports a positive environment where leaders feel empowered to engage with the transformation and grow in their roles.
Although the RACI framework is still in the implementation phase, early progress shows promising outcomes. Improved role clarity is already reducing duplicative efforts, streamlining decision-making, and strengthening accountability among nursing leaders. Processes such as clinical practice trend reviews, event action planning, and staffing management are being standardized to improve workflows aimed at enhancing operational consistency and efficiency. The ongoing work includes further refining data accessibility, providing continuous leadership training, and evaluating the RACI framework’s long-term impact on operational performance and nursing outcomes. The lessons learned so far will inform subsequent phases, ensuring that the framework remains dynamic and responsive to the evolving needs of the nursing leaders at St. Jude.
The continued progress of the RACI framework underscores the power of visionary leadership, thoughtful planning, and collaborative execution. Currie’s vision, brought to life by a dedicated team of nursing leaders from both the development and implementation phases, is creating a robust foundation for role clarity and operational excellence. As the RACI project progresses and stakeholders learn more about each other’s current roles and challenges silos across front line nursing leadership begin to break down. The outcomes of this project will serve as a cornerstone for leadership effectiveness, ensuring that every leader understands their role, embraces accountability, and contributes meaningfully to the St. Jude mission of delivering worldclass care.
At St. Jude Children’s Research Hospital, leadership development is more than a goal—it’s a journey defined by intentional growth, collaboration, and innovation. The Learning Out Loud Together (LOLT) initiative embodies this philosophy, providing a vibrant and engaging environment where nursing leaders learn, reflect, and grow together. With its signature use of emojis, interactive activities, and a focus on psychological safety, LOLT has quickly become a beloved cornerstone of the St. Jude nursing leadership culture.

The LOLT program was created under the visionary leadership of Sarah Currie, RNC, MSN, NEA-BC, St. Jude senior vice president and chief nursing executive. Morgan Melancon, MSN, RN, CCRN, NE-BC, director of Nursing Education and Professional Development, and Nancy Ballinger, clinical program manager of Nursing Administration, lead the program’s development and facilitation. The LOLT program also has benefited from the contributions of Aimee Montgomery, administrative director for Nursing Administration, and Miranda Allen, senior administrative specialist for Inpatient Nursing. Together, this dedicated team ensures the LOLT program is thoughtfully designed and seamlessly executed. Melancon and Ballinger focus on crafting meaningful content and strategic leadership development experiences, while Montgomery and Allen manage the administrative and operational aspects of the program, ensuring its smooth delivery and success.
Currie’s vision for LOLT centers on fostering a fearless nursing leadership culture where vulnerability is seen as a strength, feedback is received as a gift, and curiosity is celebrated. Her leadership has provided the guiding principles that shape every element of the program, aligning perfectly with the broader St. Jude mission and values.
The LOLT program features a robust structure designed to build on critical leadership concepts in a way that strategically links them to one another, allowing nursing leaders to develop their skills progressively and cohesively. The program includes biannual Nursing Leadership Team (NLT) retreats held each fall and spring. These immersive retreats offer nursing leaders the opportunity to engage in experiential learning activities, explore leadership theories, and participate in reflective discussions. Themes such as shifting from a fear-based to a fearless organization inspire participants to embrace trust and resilience, equipping them to lead their teams through challenges. The retreats are complemented by monthly development sessions, which occur during the second hour of the monthly NLT meetings. This dedicated time ensures that leadership development remains a continuous focus throughout the year, with each session thoughtfully building upon the previous one. St. Jude has been partnering with Chapman & Co. Leadership Institute to bring fresh perspectives and expert insights into the program, exposing nursing leaders to cutting-edge leadership strategies and industry best practices. Incorporation of external voices enriches the learning experience and ensures St. Jude leadership development efforts remain dynamic and relevant.
Central to the LOLT philosophy is the creation of a psychologically safe environment where leaders feel empowered to challenge assumptions, explore new ideas, and engage in open dialogue. Through a combination of simulated exercises, group discussions, and real-time feedback sessions, participants practice building trust, navigating difficult conversations, and leading through change. The Emergenetics tool further enhances this experience by helping leaders understand their own behavioral tendencies and thinking styles. By gaining this selfawareness, leaders are better equipped to flex their communication styles and build stronger, more cohesive teams.
The impact of LOLT is evident in the growth and engagement of St. Jude nursing leaders. Participant feedback consistently highlights increased self-awareness, enhanced coaching skills, and the ability to develop actionable plans aligned with LOLT principles. Leaders have reported feeling more connected, confident, and prepared to guide their teams through complex challenges. The program has inspired ideas such as “Failure Fridays,” where leaders share lessons learned from challenges, reinforcing the idea that failure is an opportunity for growth.
As LOLT continues to evolve, the focus remains on sustaining a fearless, inclusive, and curious leadership culture at St. Jude. With Currie’s visionary guidance, Melancon and Ballinger’s expert content development, and Montgomery and Allen’s invaluable administrative and operational support, LOLT exemplifies how St. Jude is investing in its leaders—one emoji, one conversation, and one courageous step at a time.

In April 2023, work began in earnest to create the St. Jude Nursing Magnet Submission Document for October 2024. A project plan was developed by the clinical excellence department to manage the development of the document and to ensure timely submission. To ensure integrity, subject matters experts (SMEs) and leadership would review facts and data in every narrative prior to submission. Margie Kjellin, MSN, RN, NE-BC, senior director of Nursing Clinical Excellence, appointed Robin Mobley, MSN, RN, NE-BC, as the new Magnet program manager. Mobley collaborated with many leaders involved in the previous Magnet redesignation and also engaged new leaders in a focused role as contributors to the narratives. Mobley scheduled seminars to prepare leaders for the document writing process and to assign narrative ideas for each standard. Structure included the following:
1. Four groups with specific objectives:
a. Magnet Champions Committee – Magnet Champions consist of staff nurses and clinical leaders. Members are responsible for enculturating Magnet concepts in each nursing department, posting data in their area, and generating excitement about the document and site visit.
b. Steering Committee – Nurse Executive Team members are responsible for reviewing all final documents to ensure transparency for leadership.
c. Magnet Narrative Workgroup – Clinical Excellence Team, Nursing leaders, and Magnet Champions are responsible for submitting narrative ideas.
d. Writing Team – Clinical Excellence Team, two Nursing directors, two Nursing managers/ clinical nurse leaders, and two Magnet Champions are responsible for gathering information from subject matter experts, writing narratives, confirming consultants’ edits, and submitting the final documents.
2. A development and review process for writers to ensure integrity:
a. Request details from SMEs using the consultant template
b. Write the narrative
c. Return to SME expert for accuracy confirmation
d. Submit to consultant for review
e. Review revisions from consultant
f. Complete revisions and resend to SME for accuracy
g. Resubmit to consultant
h. Repeat steps e-g as necessary
i. Submit to Nurse Executive Team for final review
j. Incorporate narrative into the final document
k. Highlight narratives on the Nursing Hub
Ninety narratives were included in the submission. Five of these included benchmarked data with a national nursing benchmark company. There is a requirement that the applicant outperforms the benchmark in most areas in the majority of eight quarters. The areas include patient satisfaction, nurse satisfaction, and three nursing-sensitive indicators. Twenty-seven of the remaining 85 narratives required the submission of empirical outcome data. Empirical outcomes are those that directly affect patient care. For example, a reduction in patient infections would be an empirical outcome whereas an improvement in documentation would be a process outcome. It’s important to improve compliance on processes, but ultimately, it’s most important to show that the patients are improving. Demographic data of the nurses at St. Jude, including degrees, certifications, and turnover, also must be submitted in a separate document.
On September 23, 2024, the St. Jude Magnet document was uploaded to the American Nurse’s Credentialing Corporation (ANCC) to undergo a review by three Magnet appraisers. St. Jude submitted additional documents at the request of the Magnet appraisers, and the appraisers’ site visit was scheduled.
As part of a broader initiative to enhance health careacquired condition (HAC) prevention efforts, St. Jude implemented a new structure for the Pressure Injury Prevention HAC team in March 2024. While a strong multidisciplinary team was already in place, there was an identified need for greater clinical nurse involvement in preventing hospital-acquired pressure injuries. In collaboration with the Office of Quality and Patient Safety, a revised leadership model was established, incorporating a clinical nurse leader, an Advanced Practice Provider (APP), and a Clinical Excellence team member.
Following the selection of the new HAC team leaders, clinical nurses from each inpatient unit were designated as skin champions for their respective areas. These skin champions actively participate in monthly HAC meetings, contribute to the development of action plans for improvement, recommend documentation enhancements, evaluate new equipment, and propose practice changes related to pressure injury prevention. Additionally, they serve as key liaisons, sharing action items and educational updates with their units and leadership teams.
The revised leadership structure and the inclusion of skin champions have significantly increased clinical nurse engagement in pressure injury prevention efforts. As a result, the new HAC framework has contributed to a measurable decrease in hospital-acquired pressure injuries, reinforcing the effectiveness of a nurse-led, interdisciplinary approach to patient safety and quality improvement.



The Administrative Support Team in Nursing coordinates and supports many departmental and institutional initiatives. The team of 11 senior administrative specialists, administrative coordinators, and one executive coordinator, supports key initiatives across departments.
Miranda Allen, senior administrative specialist, and Aimee Montgomery, administrative director, have now successfully co-planned and coordinated three Nursing Leadership Team (NLT) retreats. Allen and Montgomery begin planning these retreats months in advance, meeting with fellow members of the NLT retreat planning committee, including Morgan Melancon, Nursing Education Professional Development (NEPD) director, and Nancy Ballinger, clinical program manager. This committee meets regularly to plan out every detail to ensure a fun and engaging environment for nurse leaders.
Bonnie Burgette, administrative specialist, and Carist Neal, program coordinator in the Center of Advanced Practice, work tirelessly to support more than 160 Advanced Practice Providers (APPs) at St. Jude. Each year, Burgette and Neal coordinate APP Week, a celebration honoring our nurse practitioners, physician assistants, and certified nurse registered anesthetists. Burgette and Neal organize a variety of activities, including breakfast, luncheons, gift giveaways, wellness events, and a “make your own snack bag” event. Coordination of this week requires multiple planning meetings, long hours, and an all-hands-on deck approach, culminating in something special for a special group of people.
The Nurse Residency Program has grown and flourished with the diligent support of Jessica Read, NEPD administrative coordinator. Under the leadership of NEPD Manager Annabeth Davis, Read helped implement meaningful changes to the program in 2024. Refining the process of the twoday interview retreat and creating color-coded folders for candidate cover letters and reference letters helped nurse leader interviewers feel better prepared and informed as they interviewed approximately 75 nursing students. This change was a significant success, with leaders commenting on how much more informed and confident they felt when interviewing candidates. Read also created a comprehensive run of show packet that included Webex links for the four virtual sessions, contact information for candidates (to quickly resolve no-shows or technical issues), leader assignments, and catering details, all organized to facilitate a smooth and seamless interview event. She also created a tracking tool that all interviewers can view in real time to see how candidates are performing across all sessions. In doing so, the tracking tool fostered collaboration and informed decision-making.
Lorena Monge, administrative coordinator in the Outpatient department, has taken over the organization and facilitation of monthly NLT meetings with skill and competency. When it was suggested that the NLT meetings could have better attendance and participation if they were conducted in person or hybrid, Monge organized a survey with thought-provoking questions to gauge nurse leaders’ thoughts on changes they would like to see in the monthly meetings. Monge used the survey results to create a compelling presentation for the Nursing Executive Team. She presented the data and made thoughtful recommendations for moving forward. Monge’s hard work resulted in a well-attended, highly participative two-hour monthly meeting at a new date and time. Her support has helped elevate the NLT meetings into lively group discussions.
Olivia Waggoner never stops planning fun and meaningful events for the Nursing Care Team. As administrative coordinator for Nursing Clinical Excellence, she sits on planning committees for some of the most highly attended and appreciated annual events in Nursing, such as the Nursing Gala, Shared Governance Retreat and Fair, and Nursing Care Team Week. Waggoner works closely with the Clinical Excellence team to ensure every detail of these special projects is thoughtfully curated and planned to create the best experience for St. Jude nurses, nurse leaders, and APPs. In 2024, Waggoner participated in the St. Jude Leading through Influence (LTI) program, a leadership development intensive designed for individual contributors (those without direct reports) to develop leadership skills that can be applied at any level of the organization.
In spring 2024, St. Jude celebrated the opening of the Hospital Operations & Patient Enterprise (HOPE) Center, a centralized command center to enhance clinical and operational efficiency. Senior Administrative Specialist Jenny Harp worked with the Clinical Logistics director and managers to arrange travel to tour clinical command centers at children’s hospitals across the country and coordinated planning meetings where the initial vision for the HOPE Center was further developed. Once the office was built, Harp organized the move of the House Supervisor office and five Clinical Logistics managers. She made the house feel like a home by stocking the new breakroom with all the necessities and brought the managers’ vision for a sitting area to life with the help of Facilities Operations and Maintenance. The HOPE Center celebrated its spring milestone in June with an open house event, welcoming those involved in the various planning phases and new building neighbors to come see the space built out and operating. Harp has been instrumental throughout the process of opening the HOPE Center and looks forward to supporting the team and office as it continues to grow for years to come.
Tanya Hendricks, executive coordinator in Nursing Administration, supports Sarah Currie, senior vice president and chief nursing executive. Hendricks helps Currie coordinate her busy daily schedule. In addition to serving as a behind-the-scenes superhero, Hendricks works with the Nursing Administration team on other departmental projects.
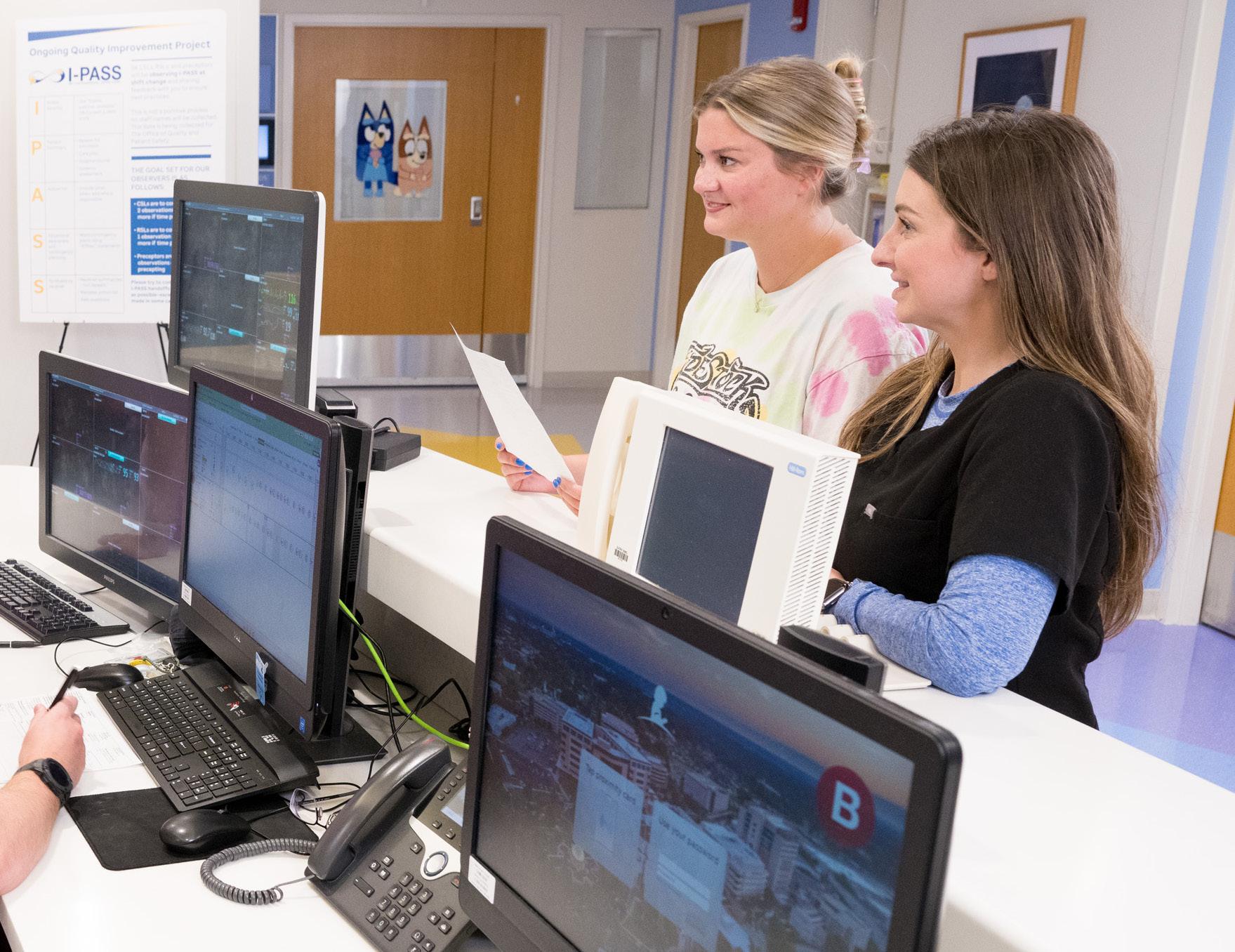
In addition to providing exemplary support to Andrea Orman and the Inpatient department, Kanetris Manning, senior administrative specialist, has been a significant contributor to the institutional Patient Handoff Project (IPASS). She has worked closely with Clinical Excellence and the Office of Quality and Patient Safety to improve the handoff transition between the Inpatient and Outpatient departments. Manning has coordinated with each department in Inpatient, so the IPASS team can listen to the department’s needs and develop a standardized IPASS form to align with the Epic EHR system that both departments can use. She also has conducted IPASS classes to serve as a refresher for nurses on how to properly use the system.
DaMaris Pullium Heidelberg, NEPD program coordinator, has played a significant role in contract negotiations with nursing schools, coordinating rotation schedules, and onboarding nursing students and externs. The student clinical rotation program would not be able to run as efficiently as it does without her.
The Nursing Administrative Team is a team in the true sense of the word. Team members cross train to ensure there is adequate support in Nursing when someone is out, and they work together to coordinate events, share knowledge, and find solutions to the challenges that come with supporting the daily needs of a large department. They also have fun together, participating in various team retreats and teambuilding activities, such as bowling, baking classes, and volunteering. These team members contribute significantly to the success and growth of nursing operations at St. Jude.

Quality planning is a critical process that enables organizations to identify patient and stakeholder needs, set clear quality goals, and develop strategies to ensure consistent, high-quality care. In 2023, St. Jude enhanced its annual quality planning process to foster a more inclusive approach in identifying priorities. By incorporating objective criteria—such as insights from existing quality measures—and leveraging new resources, the institution has strengthened its ability to execute impactful quality improvement (QI) initiatives.
Four key institutional QI projects were launched in July 2024 from this refined approach:
This initiative focuses on improving patient and caregiver education during the initial transition from inpatient care. The primary objective is to enhance knowledge retention and build confidence in managing critical aspects of care, including medication management, central line care, fever protocols, and infection prevention. To assess progress, the team has established two measurement points—at discharge and at the first follow-up clinic visit. Additionally, knowledge and comprehension assessments are being developed to establish baseline data and track improvements over time.
To mitigate CLABSI cases unrelated to mucosal barrier injury (MBI), this project employs a datadriven strategy across inpatient and ambulatory care settings. Each area is assessed independently, with ambulatory CLABSI cases identified within 48 hours of admission. A theory of change has been developed, and a Plan-Do-Study-Act cycle launched in February 2024 to enhance compliance with CHG bathing protocols. This will be achieved through targeted education and tracking measures, ensuring a sustained reduction in infection rates.
This initiative aims to boost flu vaccination uptake among eligible patients by standardizing a scalable process across inpatient and ambulatory settings. The project has yielded significant success, raising vaccine rates to 53%. Key interventions include implementing standardized scripting for staff to improve communication, administering vaccines during sedation when appropriate, and sending timely vaccination reminders. Continuous monitoring and refinement of strategies, along with improved metrics and dashboards, will drive further progress.
Effective communication during patient handoffs is essential for maintaining continuity of care and reducing errors. This project focuses on strengthening the use of the IPASS framework for shiftto-shift inpatient nursing handoffs and transitions from outpatient to inpatient care. To enhance compliance, clinical staff leaders, relief staff leaders, and preceptors from the Solid Tumor/NeuroOncology Unit received specialized training in the five IPASS elements:
• Illness severity
• Patient Summary
• Action List
• Situational awareness and contingency planning
• Synthesis by receiver
Following training, these leaders conducted peer observations, tracking compliance with IPASS standards. Results indicate a steady improvement in adherence. Additional efforts, such as awareness campaigns and updates to the IPASS tool within the Epic system, are underway. The team plans to expand this initiative to all inpatient and outpatient units in the future.
Through these four quality improvement projects, nursing continues to play a pivotal role in advancing patient safety and enhancing care delivery. By embracing evidence-based strategies and fostering a culture of continuous improvement, St. Jude remains committed to achieving excellence in patient outcomes.
Recognizing the need for stronger leadership development and peer support among relief staff leaders (RSLs), Inpatient Council Chair Katie Tomaszczuk, BSN, RN, CPHON, BMTCN, and CoChair Grace Davis, MSN, RN, CPHON, CNML, took the initiative to address these concerns. After hearing feedback from their teams, they consulted Director Andrea Orman, MSN, RN, CCRN, CNML, to determine how to best support inpatient RSLs across all units. Realizing there were limited resources, the inpatient council embraced the challenge to create a structured program tailored to the needs of these essential frontline leaders.

the needs of relief staff leaders
To gain deeper insights into the challenges RSLs face, Tomaszczuk and Davis designed and distributed an online questionnaire to all inpatient RSLs. The responses—collected from 22 participants—helped identify areas where additional support and training were most needed.
Four core themes emerged:
• Strengthening leadership skills
• Navigating difficult conversations
• RSL’s role in emergency events and end-of-life care
• Enhancing overall role support and professional development
With these findings in mind, Tomaszczuk and Davis partnered with the Inpatient Council’s Nursing Professional Development Specialists to design an innovative learning experience that would equip RSLs with the tools to lead effectively.
Jennifer Street, BSN, BS-Ed, RN, CPN, NPD-BC, and Lindy Finch, BSN, RN, CPHON, NPD-BC, played pivotal roles in shaping the program, partnering with Tomaszczuk and Davis to craft a structured retreat that would deliver impactful education. As part of the curriculum, simulation expert Amar Patel contributed an emergency response training, adding an immersive, hands-on component to the experience.
By October 2024, the team successfully launched the “RSL Retreat,” with four sessions held to date, reaching 48 inpatient RSLs.
The retreat followed a well-designed agenda:
• Breakfast and Leadership Foundations: Participants began the day exploring Enneagram personality types and their influence on leadership styles.
• Interactive Breakout Activity: Small groups collaborated to create and present their vision of an ideal RSL, fostering discussion and team building.
• Reality-Based Leadership & Panel Discussion: A panel of nursing professionals—including bedside nurses, preceptors, and nurse leaders—offered insights into common leadership challenges and strategies.
• Communication & Relationship Management: Interactive discussions explored strategies for effective team communication and conflict resolution.
• Hands-On Simulations and Role-Playing: Participants engaged in real-world scenario training, covering emergency response, rapid response leadership, end-of-life care management, and handling difficult conversations.
Effective communication during patient handoffs is essential for maintaining continuity of care and reducing errors. This project focuses on strengthening the use of the IPASS framework for shiftto-shift inpatient nursing handoffs and transitions from outpatient to inpatient care. To enhance compliance, clinical staff leaders, relief staff leaders, and preceptors from the Solid Tumor/NeuroOncology unit received specialized training in the five IPASS elements.
Following each retreat, participants completed a retrospective learning assessment to evaluate changes in their confidence and leadership abilities. The results were overwhelmingly positive—100% of attendees reported increased confidence in their role as RSLs.
The most significant areas of growth included:
• Ability to manage processes during critical patient events
• Confidence in providing staff support during emergencies
• Greater recognition and respect as a leader in the RSL role
• Heightened self-awareness of personal leadership strengths and areas for improvement
Encouraged by these successes, the team has incorporated RSL training into the “RSL Fundamentals Course,” which now serves both inpatient and outpatient RSLs. The first session successfully trained two outpatient RSLs, marking a significant step toward broader leadership development across all care settings.
Based on participant feedback, plans are underway to develop “RSL 2.0,” an advanced retreat that builds on the foundational course and provides tiered leadership development opportunities.
Through these initiatives, the Inpatient Council has not only strengthened the role of relief staff leaders but also established lasting leadership development. By fostering a culture of continuous learning, collaboration, and professional growth, this program is poised to make a meaningful and lasting impact on the nursing community. With ongoing support and innovation, the commitment to excellence in nursing leadership is stronger than ever.
Nursing professionals are the backbone for compassionate and safe patient care. The complex nature of health care has contributed to the alarming trend of high nurse burnout. The effects of burnout extend beyond individual nurses, impacting staffing, team dynamics, organizational efficiency, and ultimately, patient outcomes. It is crucial to address both organizational and individual nurse’s needs for access to tools and strategies to prevent burnout. The first step is to assess and prevent job stress in support of a healthy lifestyle, work environment, and safe, quality patient care.
With a continuous improvement approach, St. Jude Nursing conducted an initial survey in 2023 to establish the burnout baseline and identify and address contributing factors. The survey was repeated in fall of 2024 for comparison.
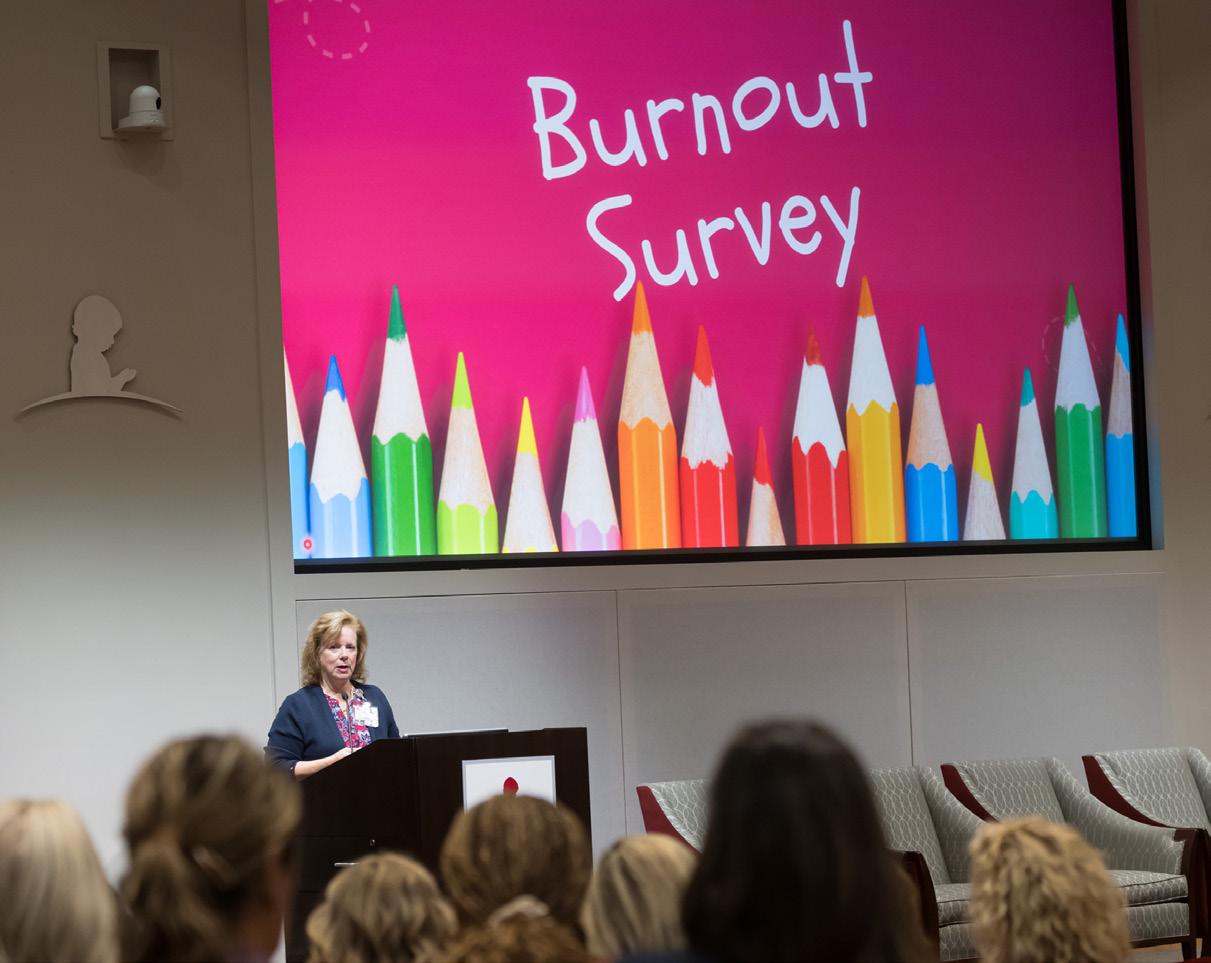
Nursing conducted the fourquestion burnout survey to identify the overall presence of burnout and major stressors for St. Jude nurses and advanced practice providers. The survey asked respondents to identify their overall presence of burnout on a sliding scale with level 1 being no symptoms of burnout to level 5 being completely burned out. Respondents were also asked to identify their top three stressors in the workday.
The results showed that 56.4% of respondents reported an overall presence of burnout between levels 3 to 5, which was comparable to benchmark data and national trends. Top stressors included staffing, teamwork/community, and patient load/clinical task volume. The results were shared with the nursing leaders and the shared governance councils who collaborated in providing resources and developing immediate and long-term actions to impact burnout.
Actions and resources taken to impact the top stressors included:
Focusing on recruitment:
• Narrowing time from initial screening to time of interview
• Adjustment of the external job site to more effectively recruit experienced nurses
• Hiring nurse residents in the float pool
Focusing on the retention of experienced staff, resource allocation, and flexible staffing:
• Adjustments to the weekender program based on staff feedback
• Trialing an admission, discharge, and transfer nurse position
• Implementation of the HOPE Center and the Central Staffing Office
• Maintaining low nurse-patient ratios
• Expansion of the nurse mentor program
• Launch of the Nursing Career Path
Focusing on meaningful recognition, team building, and inclusive leadership:
• Recognition of nurses with longevity with the Senior Nurse spotlight
• Shared governance councils hosting team-building events and community service projects
• Providing peer support and stress management programs:
• Quarterly contests promoting nursing burnout prevention videos on meaningful topics related to top stressors
• Focus on psychological safety by Learning Out Loud Together for intentional leadership development
• Epic Nursing Efficiency Training to address specific nursing documentation needs
• Promotion of the Resilience in Stressful Events (RISE) peer support program, Code Lavender, Living Well Resources, and Nursing Burnout Prevention resources.
The September 2024 comparison results showed 42.7% of respondents reported an overall presence of burnout (at levels 3-5) which demonstrated a 24% reduction in nursing burnout organization wide and significantly less burnout than the benchmark data. Level 5 burnout was reduced by 28%. Other key findings included nurses ages 45-54 reporting 41% less burnout. All nursing areas reported a reduction in burnout. The results showed significant improvement in the previous year’s top stressors. The top stressor reported in 2024 was related to the care of patients and their families.
The survey comparison data was discussed with the nursing team in the Nursing Open Forum with Sarah Currie, MSN, RNC, NEA-BC, and in various shared governance and organizational councils. Nursing has reason to celebrate the success of this past year, and to align resources and new initiatives for addressing the most relevant stressors to support nurses as they care for patients with catastrophic diseases and their families.
It has been well documented that professional advancement models for Advanced Practice Providers (APPs) influence job satisfaction, retention, engagement, and innovation. Over the past year, the Center of Advanced Practice launched a new professional advancement model at St. Jude Children’s Research Hospital.
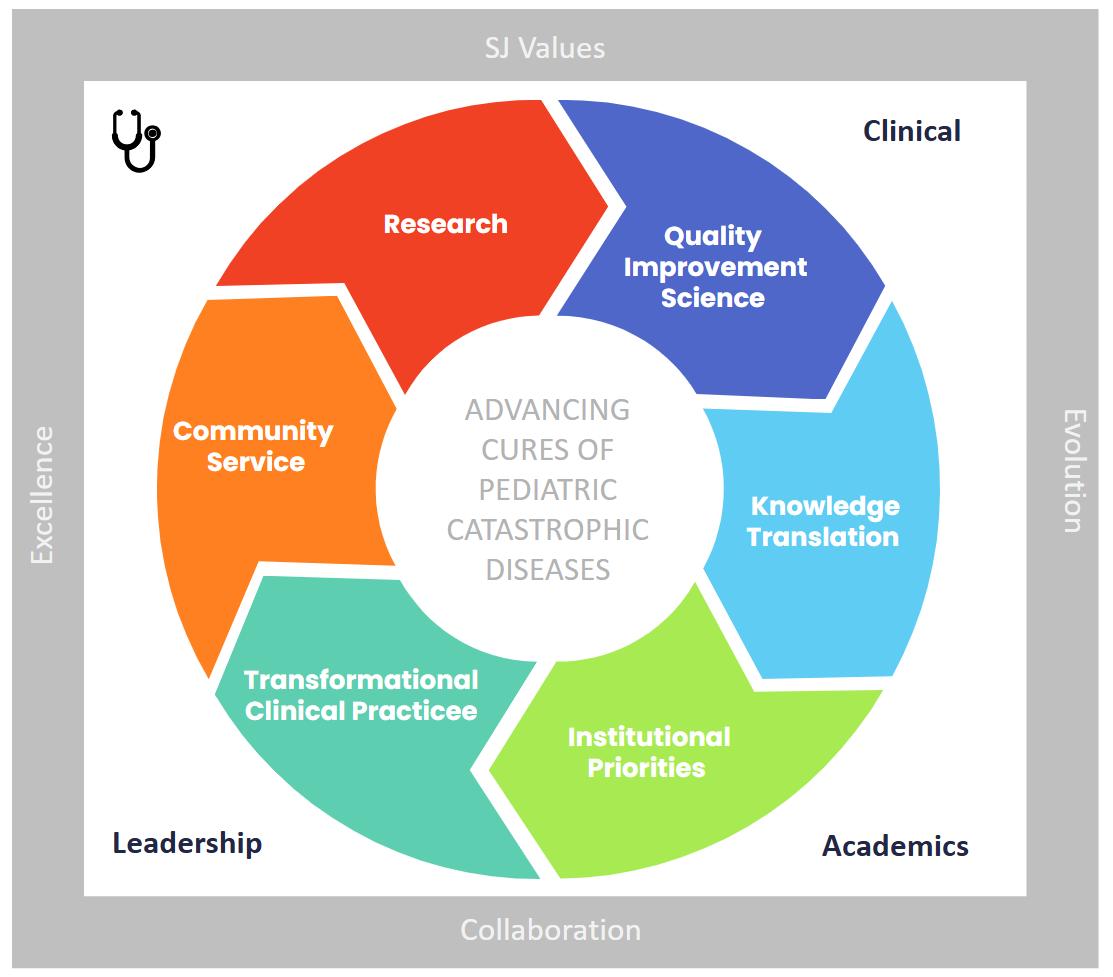
APPs have been active in clinical and professional activities throughout the institution’s history. The new professional advancement model was designed to reward these contributions through formal recognition, giving APPs a pathway to be promoted and mature in their role.
The new advancement model has four levels for nurse practitioners, physician assistants/associates, and certified registered nurse anesthetists. In addition to excelling clinically, the APPs have an opportunity to earn credit for scholarly and civic activities. They can choose one or multiple tracks to excel in, including research, quality improvement, institutional priorities, community service, knowledge translation, and clinical transformation. APPs are required to demonstrate impact and measurable outcomes to advance.
APPs undergo a rigorous review to be promoted. This process requires two letters of support, three peer references, a St. Jude-style Curriculum Vitae, time tracker of professional effort, and a seminar talk. Three peers from the Advanced Practice Council, Human Resources, and Compensation reviewed the applications. The seminar talk is where the candidate shares personal and professional achievements in an open forum. St. Jude employees in all disciplines are welcome to attend as these talks serve as valuable opportunities to learn from and celebrate colleagues’ accomplishments. Attendees often express awe in learning how APPs are engaged in clinical work and beyond.
Through this new model, APPs are rewarded at each level with a new title, increased professional development fund, and changes in compensation. In this fiscal year 2024, 10 APPs were promoted. Seven individuals went from APP level I to APP level II, and three individuals went from APP level II to APP level III. With their promotion, these APPs commit to fulfilling goals crafted during their promotion application. We look forward to seeing what tomorrow holds for these individuals and the next round of candidates!

At St. Jude Children’s Research Hospital, the commitment to developing nursing is central to delivering exceptional patient care. Building on the successful creation of the Clinical Staff Leader (CSL) Competency Assessment Tool (CAT), the next step was focusing on the Relief Staff Leader (RSL) Competency Assessment Tool. Recognizing gaps in the existing assessment and the evolving RSL role, a task force was formed to create a standardized, comprehensive tool designed to prepare RSLs for leadership success.

The RSL CAT revision arose from insights gained during the CSL CAT development. While working on CSL competencies, it became evident that the RSL competencies did not fully reflect the current expectations. The original competencies were created before the RSL role was fully implemented, leading to gaps and inconsistencies in knowledge, skills, and practice requirements.
Leadership and staff identified the need for a standardized competency assessment tool that would ensure all RSLs exit orientation with the competencies required to fulfill their roles effectively. The goal was an assessment tool that covered the complete RSL role and outlined clear expectations and qualifications for the first year.
The Nursing Education and Professional Development Department (NEPD), led by Natalie Yarmowich, MSN, RN, CPN, NPD-BC, Jennifer Street, BSN, BS-Ed, RN, CPN, NPD-BC, and Emily Smith, BSN, RN, facilitated the project. A diverse task force included:
• RSLs, CSLs, and managers representing inpatient, outpatient, and NSS (Procedures/ Surgery/DI/RO) service lines.
• Leadership oversight provided by leaders such as Scarlet Poley, MSA, BSN, RN, NE-BC, Lindsey Reap, DNP, MSN, RN, NE-BC, Melody Burchett, MSN, RN, CNML, Susan Bock, MSN, RN, NE-BC, Amanda Bowling, MSN, RN, CNML, and Brittany Bedard, BSN, RN.
The task force met monthly, conducting SWOT analyses to evaluate the previous RSL CAT and identify areas for improvement. The process included splitting into specialized groups to create area-specific inserts tailored to the unique needs of inpatient, outpatient, and NSS practice areas.
The RSL CAT was designed to:
• Provide protected training time tailored to the orientee’s experience.
• Outline role expectations and qualifications.
• Incorporate American Organization for Nursing Leadership standards to align with national leadership competency expectations.
The general RSL CAT includes competencies in:
• Leader Within: Reflective practice, foundational thinking, and career development.
• Professionalism: Professional accountability, advocacy, and health equity.
• Communication and Relationship Management: Effective communication and relationship-building strategies.
• Knowledge of the Healthcare Environment: Policy understanding, regulatory readiness, and patient safety.
• Business Skills and Principles: Financial management and strategic decision-making.
To ensure applicability across diverse practice settings, specialized area-specific inserts were created:
• Inpatient Insert: Focuses on critical inpatient leadership competencies like safety and sepsis huddles, facilitating staff assignments, participating in interdisciplinary rounds, managing daily operational tasks like crash cart checks, medication counts, and ensuring compliance with hospital-acquired conditions (HAC) documentation.
• Outpatient Insert: Covers essential outpatient leadership competencies, including staffing logistics, patient flow coordination, and medication management.
• NSS Insert: Addresses specialized areas like Radiology Oncology Clinic and perioperative environments, including anesthesia schedule assessments, interdepartmental coordination, and emergency preparedness.
The RSL Competency Assessment Tool is a key step forward in leadership development at St. Jude. By ensuring consistent orientation and aligning competencies with the evolving responsibilities of the RSL role, the tool prepares future leaders to meet role demands confidently.
This collaborative effort highlights the dedication of St. Jude Nursing leadership to continuous improvement and excellence. As the RSL CAT evolves, it will remain vital in developing competent, confident, and capable RSLs who are ready to support the mission of providing exceptional care to patients and families.
In 2024, St. Jude honored the dedication, expertise, and compassion of its nursing professionals through a year of meaningful recognition and celebration. From individual excellence to team achievements, St. Jude nurses continue to exemplify excellence in patient care and leadership in the field of nursing.
The DAISY Award for Extraordinary Nurses is a prestigious international recognition celebrating nurses who provide compassionate and outstanding care. A grateful St. Jude parent shared:
“DAISY Award honorees personify the remarkable patient care experience at St. Jude. These nurses consistently demonstrate excellence through their clinical expertise and extraordinary, compassionate care. They are recognized as outstanding role models in our nursing community.”
2024 DAISY Award Recipients:



Championing nursing heroes: The Nightingala Hero Awards
In collaboration with the University of Tennessee Health Science Center College of Nursing, St. Jude proudly sponsored the 2024 Nightingala Hero Awards, celebrating exceptional nurses across the community.
St. Jude Nightingala Award Honorees:
• Jasmin Elizarraras, MSN, RN, CNML – Executive Leader Nurse Hero
• Emily Nichols, BSN, RN, CPHON, CPN – Bedside Nurse Hero
• Erin Harper, MSN, CPNP-BC – Advanced Practice Nurse Hero
In December, the St. Jude Nursing Gala was held at the historic Peabody Hotel in Memphis. This annual event celebrated outstanding contributions across nursing disciplines.





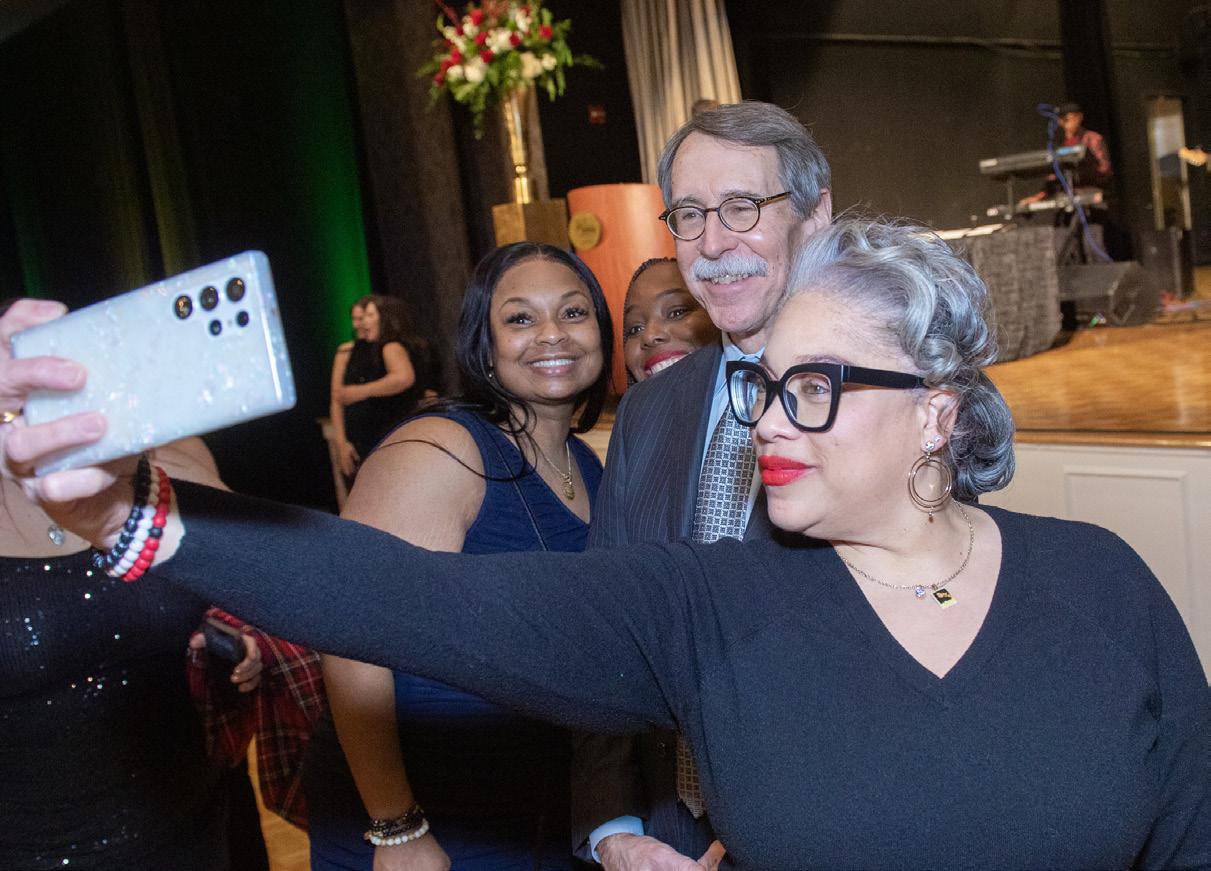

2024 Nursing Gala Honorees: , BSN, RN – Diversity, Equity, & Inclusion Nurse of the Year

• 4K Nursing Team, Inpatient Services – Nursing Team Award
• Noah Quinton, MDiv, BCC – Friend of Nursing
• Fanny Williams, surgical technician – BEE Award Recipient
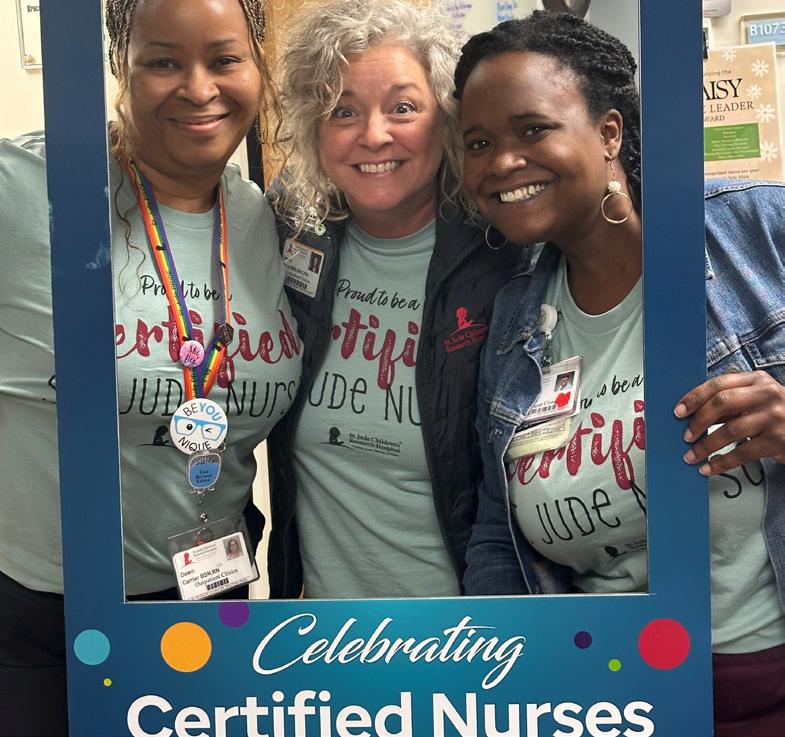

In March, St. Jude celebrated Certified Nurses Day, recognizing specialty-certified nurses for their professionalism, dedication, and commitment to improving patient outcomes. St. Jude supports these efforts by reimbursing exam fees, study materials, and review courses. The celebrations included social media spotlights, newsletter features, and a vibrant display on the Nursing Recognition Wall.
During Nursing Care Team Week, St. Jude honored the extraordinary impact of its nurses through engaging activities, including a Blessing of the Hands ceremony, specialty treats, and fun themed dressup days. The inaugural “Vulnerable Voices” event provided a powerful platform for patients and families to share heartfelt testimonies about the lasting impact of St. Jude nurses.
Additional 2024 recognitions and achievements
• Melody Burchett, MSN, RN, CNML – Jim Mobley Partner in Excellence Award
• St. Jude Nursing – Center of Excellence in Pediatric Sedation Award
• Katie Tomaszczuk, BSN, RN, CPHON, BMTCN – APHON Nurse of the Year 2024
• Kristen Campbell, MSN, RN, BMTCN – Preceptor of the Year
• Nursing Residency Program – Accredited Practice Transition Program with Distinction
• Nursing DEI Committee – Outstanding DEI Champion Award
Living Our Values honorees
• Kierra McCallum, BSN, RN – Infectious Diseases Clinic
• Patti Pease, MSN, FNP-BC, NPD-BC – Center of Advanced Practice
• Troy Wallach, MPA, BSN, RN, CPHON – Clinical Logistics
• Megan Bolling, BSN, RN, BMTCN, CPHON – BMT Inpatient
St. Jude Children’s Research Hospital remains dedicated to developing and training outstanding advanced practitioners to join the mission–advancing cures for pediatric catastrophic diseases. In alignment with this goal, the Center of Advanced Practice (CAP) has prioritized cultivating expert Advanced Practice Providers (APPs) through a structured, high-quality fellowship program. In 2023, CAP earned Advanced Practice Provider Fellowship Accreditation (APPFA) with distinction from the American Nurses Credentialing Center (ANCC). This recognition highlights the program’s innovative approach to supporting new graduate physician assistants and nurse practitioners into new practice settings.

Since the program’s launch, 10 APPs have entered and successfully completed the program. Graduates are working in various practice settings within the institution, including the After Completion of Therapy Clinic, Bone Marrow Transplantation, Solid Tumor Clinic, Intensive Care, the Hospitalist Program, and Quality of Life and Palliative Care. There are two APPs currently enrolled in the program.
To maintain APPFA accreditation, programs must demonstrate outcomes in the following five key categories:
• Learner professional development
• Learner competency
• Self-reported measures
• Key stakeholder evaluation
• Financial performance
To date, the fellowship program has exceeded all benchmarks across these areas. Fellows consistently demonstrate professional growth by leading clinical projects focused on education and knowledge dissemination. Learner competency is objectively measured through learner evaluation tools that emphasize patient safety and excellence. All fellows have demonstrated the ability to practice independently by the end of the program. Self-assessment results show that fellows meet expectations for clinical competency, professionalism, clinical scholarship, quality improvement, and health care advocacy within their first six months. Key stakeholder engagement is measured by evaluating the preceptor’s ability to lead fellows through professional and clinical growth. All preceptors meet program expectations as demonstrated by evaluations from program leadership and learners. The financial goal focuses on retention of staff as this is linked to cost savings, higher productivity, and higher job satisfaction. To date, all fellows remain employed at the institution one year after their start date.
The competency-based fellowship program is designed to develop autonomous, proficient APPs who provide safe, high-quality care to patients with catastrophic diseases. To support this goal, the program includes a variety of elements that support high-quality training. The program includes professional mentors, trained preceptors, didactic education, self-directed learning, peer support, and diverse clinical experiences.
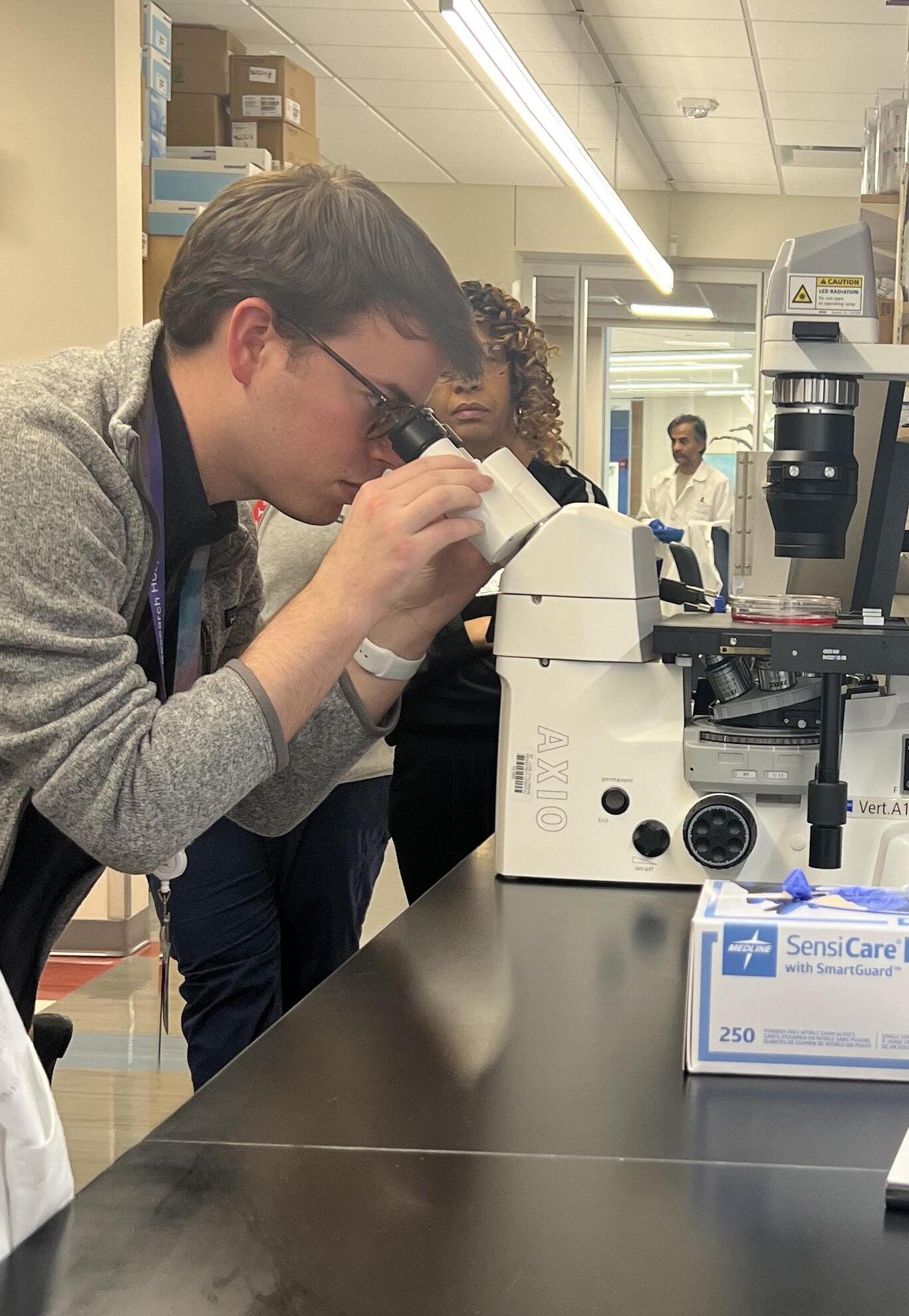
The CAP education team continues to enhance the fellowship experience. Recent improvements include the integration of simulation into didactic education days. Learners have participated in a virtual reality experience aimed at increasing knowledge about social determinants of health. Emergency management preparedness is prioritized through various simulation strategies including escape rooms, mock codes, and clinical scenarios with a mannequin. Another enhancement of the program is the addition of a new employee orientation dedicated to APPs. This orientation introduces APPs to the institution, CAP, their role, state and institution regulatory requirements, and pertinent policies and processes.
The DAISY Award was established in 1999 by the family of Patrick Barnes, who passed away from complications of an autoimmune disorder. The DAISY Award is given to extraordinary nurses who go above and beyond the call of duty. The mission of the DAISY Foundation is to meaningfully celebrate extraordinary, compassionate nurses, capturing those moments unique to nursing that make a profound difference in the lives of people around the world.
The Professional Achievements and Advancements Council proposed the idea to launch the DAISY Nurse Leader Award at St. Jude. The Daisy Nurse Leader Award recognizes and honors nurses in leadership roles who consistently create a compassionate and supportive work environment for their team, fostering high-quality patient care by demonstrating exemplary leadership. Award recipients are recognized for being accessible, responsive, and strong advocates for their staff, going beyond typical managerial responsibilities to positively impact the overall patient experience and promote a culture of compassion. With an abundance of exceptional nurse leaders at St. Jude, the Nurse Executive Team approved the proposal to begin the DAISY Nurse Leader Award in 2024.
The DAISY Nurse Leader Award is granted biannually to a nurse leader who was nominated by a staff member, peer, patient, or family. The Professional Achievements and Advancements Council votes on the blinded nominations and presents the prestigious award. In the inaugural year, Jasmin Elizarraras, MSN, RN, CNML, manager of 5k inpatient unit, received the first DAISY Nurse Leader Award in 2024. Elizarraras was described as a great leader who inspires others to lead, while going above and beyond to celebrate her employee’s successes. She fosters a healthy work environment which leads to a safe place for both employees and patients. Elizarraras works tirelessly to better the patient, family, and employee experience.
During the first DAISY Nurse Leader Award presentation, Tena Barnes Carraher, founder of the DAISY Foundation, was visiting St. Jude. She presented the DAISY Nurse Leader Award and spoke to attendees about her role in the foundation and the impact of extraordinary nurses and nurse leaders on the patient experience.

St. Jude made a significant upgrade by replacing all existing infusion pumps with the latest model from BD Alaris. This transition marked a step forward in enhancing patient care and ensuring optimal functionality of infusion devices.
Following the purchase of the BD Alaris infusion pumps, it became apparent that the cleaning and disinfection protocols were more complex than initially anticipated. The pumps’ intricate components and sensitive electronics necessitated a comprehensive, meticulous cleaning process to ensure they were free of contaminants and functioning properly.
To address this challenge, Nursing Leadership partnered with various departments across the institution, including Environmental Health and Safety, Facilities, Environmental Services, and Infection Prevention. They worked together to identify safe, accessible spaces for deep cleaning and disinfection and to ensure the process would meet St. Jude standards for patient safety.
Recognizing the need for clear and concise instructions, Nursing Professional Development Practitioners created specialized educational materials for both the staff responsible for cleaning the pumps and nursing teams across all departments. These resources ensured that everyone involved in the cleaning and maintenance process had a thorough understanding of the correct techniques, timelines, and safety protocols.
In October 2024, St. Jude hired temporary employees to help deep clean the infusion pumps. The team worked diligently to follow the newly developed cleaning protocols. During this time, a “soft go-live” was conducted to ensure the process was effective and adhered to the manufacturer’s recommendations.

By November 2024, staff in all clinical areas was successfully implementing the new cleaning process. The comprehensive approach to cleaning the BD Alaris pumps was met with positive feedback and showed early signs of improving both the safety and functionality of the equipment.
A new Standard Operating Procedure (SOP) outlined the precise cleaning and disinfection protocols required for the BD Alaris infusion pumps, ensuring that all devices are consistently cleaned according to the manufacturer’s recommendations.
As a result of this successful initiative, St. Jude has ensured that all infusion pumps are maintained at the highest standards of safety, quality, and performance, supporting our ongoing commitment to patient care excellence.

Mentorship plays a pivotal role in shaping the professional journeys of nurses at St. Jude Children’s Research Hospital. Through thoughtfully designed programs, St. Jude continues to build a robust culture of mentorship, supporting nurses at every stage of their careers. Two standout initiatives—the expanded Nurse Mentor Program and the Resident Professional Advancement and Learning Support (rPALS) Program—have been instrumental in fostering meaningful connections, professional growth, and sustained retention.
Originally piloted exclusively with nurse residents, the Nurse Mentor Program has undergone a significant transformation. Recognizing the value of mentorship for all nursing professionals, St. Jude expanded the program to include experienced nurses and non-nursing care team members as mentees. Additionally, St. Jude introduced mentorship opportunities for nurse leaders, supporting transitions into leadership roles and fostering strategic thinking.
This expansion was driven by the program’s vision to promote the personal and professional growth of St. Jude nurses through supportive and nurturing relationships. The pairing process now includes a broader pool of mentors and mentees. Participants are thoughtfully matched through a standardized process that considers career aspirations, professional backgrounds, and personal interests, ensuring optimal mentor-mentee compatibility.
Mentors are equipped with comprehensive resources, including web-based training modules and a Mentor Guidebook. These resources provide guidance on setting goals, establishing professional boundaries, and facilitating discussions on career advancement. Mentees, in turn, are empowered to take ownership of their development, with expectations to set at least one professional goal and meet regularly with their mentors over a 12-month period.
Andrew Robinson, RN, pediatric oncology nurse, is one of many who have benefited from the Nurse Mentor Program, where mentorship extends beyond professional guidance. He and his mentor, Lindsay McElroy, MSN, RN, program manager in Nursing Clinical Excellence, have attended hospital events together and engaged in meaningful discussions about personal growth. With McElroy’s insights and encouragement, he successfully completed his Clinical Advancement Program (CAP) application, an accomplishment that underscores the transformative power of mentorship at St. Jude.
Complementing the formal mentorship structure is the rPALS Program, a peer mentorship initiative that pairs new nurse residents with graduates from previous cohorts working in the same unit. This near-peer support provides a relatable perspective, helping new nurses navigate clinical challenges and workplace dynamics during their critical transition period.
The success of the rPALS Program lies in its ability to create a supportive environment where learners feel connected and empowered. By facilitating routine interactions, rPALS fosters a sense of belonging and community among new nurses. This foundational support often paves the way for seamless progression into the formal Nurse Mentor Program, creating a continuum of mentorship that spans the early years of a nurse’s career at St. Jude.
The combined success of the Nurse Mentor Program and the rPALS initiative illustrates an institutional commitment to fostering a culture of mentorship that transcends career stages. By offering diverse mentorship opportunities—from near-peer relationships to formal mentor-mentee pairings—St. Jude ensures that nurses receive the support they need to thrive professionally and personally.
As the mentorship programs continue to expand, St. Jude remains focused on creating tailored experiences that meet the evolving needs of nurses. With this approach, St. Jude enhances job satisfaction and retention among its employees and strengthens its reputation as a leader in pediatric oncology nursing excellence.
Mentorship at St. Jude is a commitment—to lifelong learning, to professional growth, and to the unwavering support of nurses dedicated to the institution’s mission of advancing cures and means of prevention for pediatric catastrophic diseases.
Eight months after Epic was implemented as the new electronic health record (EHR) at St. Jude, Nursing conducted an institution-wide survey to gauge clinical end users’ level of satisfaction with the new system. This was the first EHR-related survey since 2019 and would serve as a benchmark for determining areas for improvement in addition to overall satisfaction. Nurses representing multiple clinical specialties comprised roughly 20% of the overall respondents. According to the survey, nurses were among the least satisfied groups, particularly in the ambulatory clinics, Acute Care Clinic, Infusion Center, and Intensive Care Unit, respectively. However, 69% of nurses were optimistic that their experience would improve over the next 18 months, giving credence to the robust EHR governance structure at St. Jude.
After compiling the survey results, the Clinical Applications Training and Support Team worked with nursing leadership to develop a plan to improve nurse satisfaction and proficiency with Epic, focusing on the clinical areas mentioned above. In January 2024, the Nurse Efficiency Training Project was established and implemented in full swing. Individual nurses from each of the focus areas were identified as “Superstars.” Seventeen Superstars, representing nine clinical specialties, were identified.

These nurses had already demonstrated system proficiency and were willing to assist their coworkers in identifying problem areas and providing input for the training. Clinical Applications team members spent several weeks conducting shadowing sessions with the area Superstars. These sessions provided an opportunity to observe clinical workflows as the nurses were performing them in Epic, helping the team identify and better understand any pain points and system limitations. For example, 11 “breaks/fixes” were discovered. A break/fix occurs when Epic isn’t functioning as expected or when a vital component of the workflow is missing. Additionally, the shadowing sessions yielded 21 optimization requests and helped the Clinical Applications team identify the top five training opportunities for each area. The top five opportunities would then become the focus for additional training and education.
To address the top five opportunities, the Clinical Applications team developed training materials, including web-based learning modules. Training also consisted of teach-back sessions, where staff would demonstrate successful comprehension and integration of the content covered. Nearly 200 nursing staff participated in the training. End-of-training feedback surveys yielded favorable responses, with most nurses indicating overall satisfaction with the training and improved proficiency in Epic as a result. The success of this project has prompted leaders in Nursing as well as Clinical Applications to extend the work to the remaining inpatient floors beginning in early 2025.
Career paths define the skills and knowledge needed to successfully master roles within the institution. It increases our efforts to build talent from within as well as improve our ability to attract external talent. St. Jude has embarked on a multi-year initiative to develop career paths that provide growth opportunities throughout the institution. The Career Paths for Nursing and Advanced Practice Providers were completed in June 2024 as part of phase 3.

The Nursing Executive Team partnered with the Human Resources (HR) Compensation team and an HR consultant to develop separate career paths due to the unique skill sets of the two groups. The goal was to align the paths with the institutional initiative, job descriptions, the current clinical advancement program for clinical nurses, and the professional development model for advanced practice. Roles within the career map were defined and included job responsibilities, core skills, functional skills, and qualifications for nursing leaders and individual nurse contributors. The paths were designed to support the Nursing Department by identifying training and development needs to be successful in current and future roles, providing consistent
and competitive alignment of salary ranges, aid in succession planning, and help in recruiting and onboarding top candidates for open positions. The new career path also gives nurses a “roadmap” based on their career interests with visibility to roles within their path as well as other paths of interest and allowing them to plan to build on skills and education needed for growth.
The nurse managers and directors in each department were instrumental in identifying opportunities within current roles to better define proficiency level descriptors and qualifications for advancement. Nursing jobs were mapped to corresponding roles in the new career path. Leaders identified gaps where additional roles were needed to provide transitions for career growth to support the advancement of the institution and Nursing strategic plan. As a result, new roles were added, creating more opportunities for professional growth and allowing Nursing to have a competitive compensation strategy to the internal and external labor market.


The Nursing Executive Team partnered with the HR Compensation team to host Career Path overview sessions to discuss the new career path framework, answer questions, and provide support for those seeking advancement opportunities.
The Nursing Recognition Wall launched in 2021 to provide a public space for St. Jude staff, patients, and families to see how nurses are honored for accomplishments, milestones, and awards. The Nursing Recognition Wall, located near the ABC Wall, underwent a quiet, yet transformative shift. For years, the wall had served as a symbolic centerpiece, celebrating the remarkable achievements and contributions of Nursing staff. In late 2024, Nursing Clinical Excellence took ownership of the wall.

The decision to transition control of the Nursing Recognition Wall to Nursing Clinical Excellence was made after a series of discussions between leadership and staff. Nurses wanted the wall to feel more personal, for content to be updated more regularly, and to represent the big milestones as well as the everyday moments of compassion, skill, and commitment that defined their work.
The Clinical Excellence team had a simple vision: the wall should celebrate the achievements of individual nurses and also reflect the culture of excellence that is cultivated in the daily interactions between staff and patients.

The wall began to be updated frequently with new content that reflected the ebb and flow of nursing life. Recognition became more of an ongoing celebration of the many small wins that define the nursing profession.
The results were immediate and profound. Nurses began to feel more valued, knowing their efforts were being recognized regularly and in a way that felt authentic to their work. There was a renewed sense of pride in the profession, as stories of compassion, skill, and teamwork were displayed prominently.
One of the most significant changes was increased engagement from staff. Nurses are eager to see who is featured next, and it has become a point of pride for teams when one of their own is celebrated. There is a palpable sense of camaraderie as staff members share the latest stories of excellence during shift changes.
The wall’s new design has had a ripple effect beyond the Nursing staff. Patients and families find themselves drawn to the wall. It is a place where they can see firsthand the dedication and expertise of their nurses.

The wall has become more than just a place of recognition; it is a symbol of the hospital’s commitment to clinical excellence.
The wall not only showcases individual achievements but also demonstrates the collective strength of the Nursing team. It reinforces the hospital’s mission of providing compassionate, high-quality care, and has become a cornerstone of the hospital’s overall culture of excellence.
As the wall continued to evolve, it became clear that its true value is not just in the recognition, but in the community it has built. Nurses, staff, patients, and families see it as a testament to the power of care, collaboration, and clinical excellence.
The Nursing Recognition Wall has truly come to life, and with Clinical Excellence at the helm, it is now more than just a wall—it is a celebration of the heart of the hospital: its nurses.
The theories of Nursing Shared Governance were established in the 1980s as a way for nurses to have the authority to make decisions and have autonomy in nursing practice. In the nearly five decades since its inception, shared governance has had many iterations. Likewise, St. Jude nursing shared governance has looked different over the years.
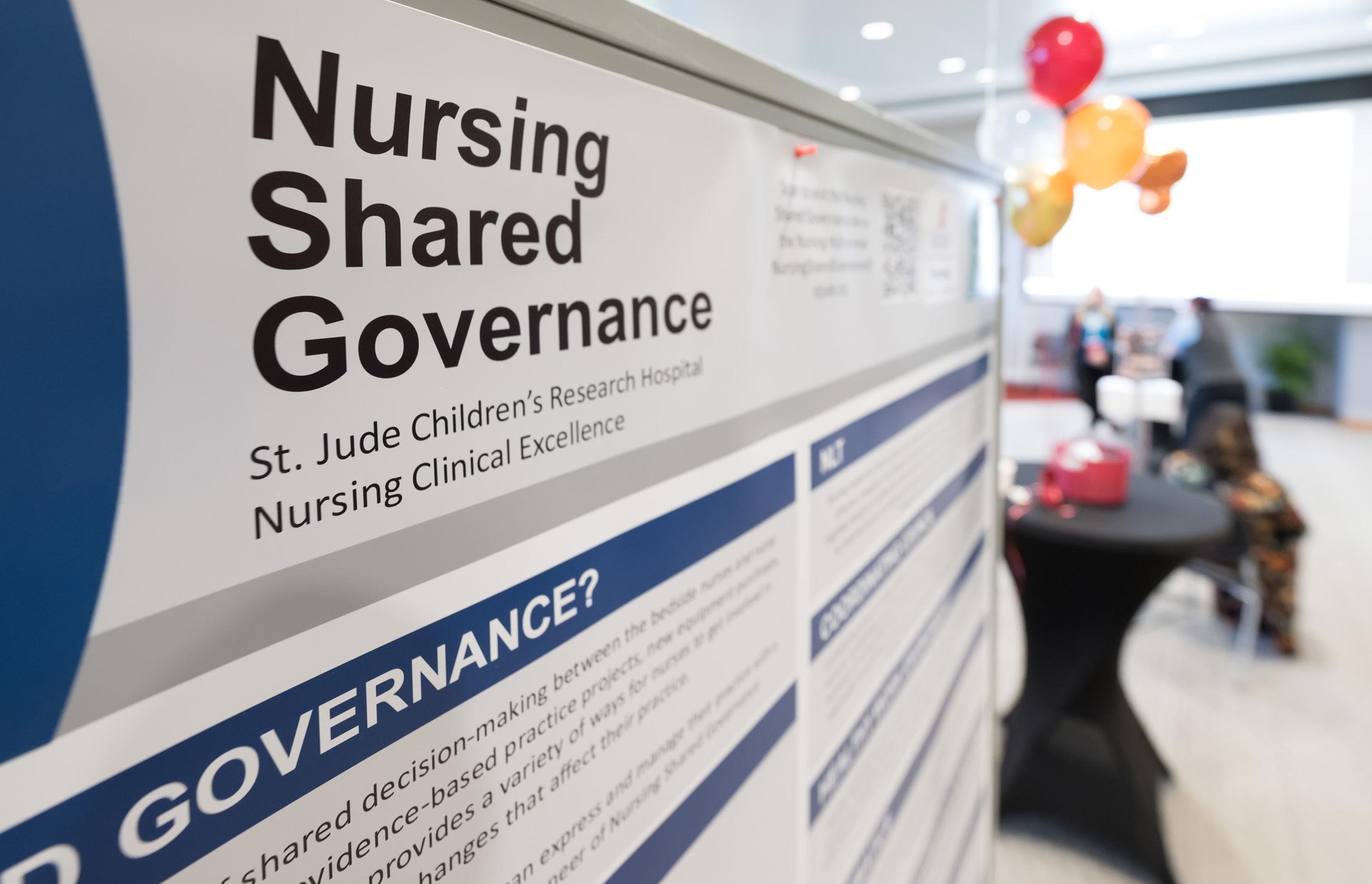
The current structure of Nursing Shared Governance at St. Jude is a councilor model of governance, with unit-based councils, central councils, and a Coordinating Council as the oversight body. St. Jude Nursing Shared Governance currently has 17 councils, five committees, and over 300 nurses as members of these groups.
The councils include the Nursing Leadership Team, Coordinating Council, Healthy Work Environment Council, Informatics Council, Research & Evidence Based Practice Council, Quality Council, Professional Achievements & Advancements Council, Advanced Practice Council, Nursing Surgical Services Service Line Council, Outpatient Clinics Unit-Based Council, Infusion Center & Acute Care Clinic Unit-Based Council, Inpatient Service Line Council, 5K Unit-Based Council, 4K Unit-Based Council, 3K Unit-Based Council, BMT Unit-Based Council, and ICU Unit-Based Council. The committees sanctioned by Coordinating Council are the Nurse Policy Committee, Magnet Champions Committee, Just Culture Committee, Clinical Advancement Program Committee, and Nursing Diversity Equity & Inclusion Committee.

Unique to St. Jude Nursing Shared Governance, parent advisers from the Patient and Family Centered Care (PFCC) office sit on most councils within the structure. The parent adviser’s input is vital to the council’s work for nurses to better understand the patient and family experience, especially when making practice changes in clinical areas. In 2024, the shared governance program manager partnered with PFCC to launch the Nursing Steering Council, consisting of all parent advisers on nursing councils, as well as nurses from each clinical area. Parents and nurses are able to share progress or barriers in their councils and form deeper connections during meetings. In the spring of 2024, leaders and advisors of shared governance councils met for the Annual Shared Governance Retreat, which consisted of team-building activities, leadership education, and council development work.

Nursing Shared Governance hosted the second annual Shared Governance Fair in the fall of 2024. All councils displayed posters depicting their goal achievements, plans for the next fiscal year, and other details about their work. All interdisciplinary stakeholders are invited to attend the Shared Governance Fair to see the projects that nurses are leading that are affecting patient outcomes as well as nursing satisfaction.

St. Jude nurse preceptors are essential to developing nursing expertise and guiding clinical practice. They play a vital role in supporting nurses—whether new graduates or experienced professionals—during critical transitions into new roles, specialties, or practice settings. Preceptorship extends beyond teaching skills; it ensures that nurses at every stage of their careers gain the confidence, knowledge, and critical thinking abilities necessary to provide exceptional patient care. By fostering clinical competence and professional growth, preceptors contribute directly to the continued excellence of nursing at St. Jude.

Preceptorship is a multifaceted role that demands dedication, professionalism, and a commitment to maintaining the highest standards of nursing practice. Preceptors serve as role models not only for their orientees but also for their peers. To fulfill this responsibility, preceptors are expected to stay up to date with mandatory training and education, maintain current licensure, and consistently demonstrate clinical competence. They must be in good standing within the organization and exhibit integrity, professionalism, and a commitment to personal and professional growth. This commitment ensures that preceptors provide a safe, structured learning environment where nurses thrive.
The role of a nurse preceptor also requires significant dedication to hands-on clinical teaching. Preceptors work closely with their orientees at the bedside, providing real-time guidance that demonstrates best practices in patient care, safety, and communication. In addition to their clinical duties, preceptors participate in bi-weekly meetings with orientees, Nursing Professional Development Practitioners (NPDPs), and Nursing leaders. These meetings provide opportunities to assess orientee progression, share successes and concerns, and collaboratively develop personalized plans to ensure each orientee’s success. Preceptors also handle extensive documentation and paperwork to track progress and competency achievements, further highlighting the complexity and commitment of the role.
Recognizing the hard work, dedication, and impact of these essential team members is a priority at St. Jude, aligning with the American Nurses Association (ANA) Scope and Standards of Practice. ANA emphasizes that all nurses have a responsibility to contribute to the future of nursing by promoting health and safety, preserving integrity, and maintaining competence. In 2024, St. Jude took a significant step in celebrating these contributions by establishing the Preceptor of the Year Award, presented annually by Nursing Education and Professional Development. This award honors a nurse preceptor who exemplifies excellence in clinical teaching, supports professional growth, and embodies the institution’s values. It serves as a reminder of the collective responsibility nurses share in fostering the development of future caregivers and leaders in health care.
The inaugural recipient of the Preceptor of the Year Award is Kristen Elkins Campbell, MSN, RN, BMTCN, a nurse whose dedication to preceptorship has left a profound impact on her colleagues and orientees. Kristen’s approach reflects the qualities St. Jude values most: compassion, expertise, and an unwavering commitment to professional growth.
Reflecting on the recognition, Campbell shared, “Receiving the first-ever Preceptor of the Year award has been one of the highlights of my career. Reading the nominations and being recognized by my orientees reminded me why I became a nurse and why I continue to work at the bedside today.”
Her words highlight the deeper meaning of preceptorship—being part of a process that shapes not only skilled clinicians but compassionate caregivers.
Campbell’s recognition came from a pool of 68 nominations, reflecting the deep appreciation nurses have for preceptors at St. Jude. Each nomination shared stories of preceptors who invest time and effort into shaping careers, building confidence, and ensuring nurses are equipped to handle the challenges of pediatric oncology care. These stories emphasize the critical role preceptors play in maintaining the high standards of nursing care at St. Jude.
Beyond the award itself, the institution’s focus on preceptor recognition reflects a broader commitment to professional development and excellence in nursing education. Preceptorship is more than a role; it is a responsibility that speaks to the heart of the nursing profession. According to the ANA Scope and Standards of Practice, contributing to the growth of future nurses is a professional obligation for all nurses. The institution’s emphasis on celebrating preceptors acknowledges this responsibility and highlights the dedication to fostering an environment where nurses are supported, valued, and inspired to lead.
The introduction of the Preceptor of the Year Award during Nursing Professional Development Week underscores the institution’s recognition of the essential role preceptors play in patient care and excellence. Campbell’s recognition as the inaugural recipient highlights the profound influence a dedicated preceptor can have on shaping the future of nursing. Her story, along with many other preceptors at St. Jude, serves as a testament to the power of preceptorship in cultivating confident, compassionate, and skilled nursing professionals.
As St. Jude continues to celebrate and support its preceptors, the award will serve as a symbol of gratitude for the hard work, dedication, and excellence that define nursing preceptorship. It is a reminder that every nurse who steps into the role of a preceptor is making an invaluable contribution—not only to individual careers but to the future of nursing and patient care at St. Jude and beyond.
St. Jude Children’s Research Hospital continues to set the standard for nursing excellence, proudly earning reaccreditation with distinction from the American Nurses Credentialing Center’s (ANCC) Practice Transition Accreditation Program® (PTAP). This prestigious recognition—the highest awarded by the ANCC—acknowledges the Nurse Residency Program as a robust, high-quality transition-to-practice program designed to develop competent, confident nurses dedicated to the St. Jude mission.

The reaccreditation reaffirms the program’s vital role in the St. Jude nursing workforce strategy. The program continues to attract top nursing graduates, boasting a remarkable 230% growth in applications and a 98% retention rate at one year—well above the national benchmark of 80%. The structured curriculum fosters clinical competence, professional confidence, and long-term retention, ensuring that St. Jude remains an employer of choice.
Despite its proven success, the journey to reaccreditation was challenging. Historically, gaining buyin from managers had been difficult, with some focusing more on perceived shortcomings to had been difficult” as the perceived shortcomings appeared to outweigh the program’s measurable achievements. However, the reaccreditation process provided an opportunity to showcase the program’s tangible benefits, highlighting its alignment with the hospital’s strategic goals and its contribution to a stable, skilled nursing workforce.
During the reaccreditation process, the program was recognized for displaying best practices in two key areas: the intentional development of goals and outcome measures, and its comprehensive succession planning process. These elements ensure that the program not only addresses immediate needs but also builds a sustainable pipeline of future nursing leaders who are equipped to support the St. Jude mission.
This significant achievement would not have been possible without the unwavering commitment of the Nursing Education and Professional Development (NEPD) team, led by Morgan Melancon, MSN, RN, CCRN-K, director of NEPD, and Annabeth Davis, MSN, RN, NPD-BC, program manager. The team meticulously prepared the self-study document, demonstrating how the program consistently meets the rigorous ANCC standards.
Equally commendable was the participation of various stakeholders during the virtual site visit. Managers, clinical staff leaders, residents, preceptors, and faculty played integral roles, sharing insights and experiences that showcased the program’s impact. Their engagement highlighted the collaborative spirit that drives the program’s continued success.
Receiving accreditation with distinction is more than an accolade—it’s a testament to the high standards of nursing excellence at St. Jude. This recognition validates the hard work invested in shaping a program that not only transitions new nurses into practice but also supports their growth as integral members of the care team. The program bridges the gap from student to professional nurse, ensuring that new nurses are confident, competent, and committed to delivering exceptional care.
As St. Jude looks to the future, sustaining and expanding the Nurse Residency Program remains a critical priority. By continuing to invest in the program, St. Jude ensures long-term workforce stability and maintains its reputation as a leader in pediatric health care and nursing excellence.
The reaccreditation with distinction serves as a reminder of the collective effort required to achieve such a milestone. It highlights the dedication of the NEPD team, the support of hospital leadership, and the contributions of every nurse who participates in and supports the program. Together, these efforts create a pathway for future nursing leaders and ensure that St. Jude remains a beacon of hope, healing, and excellence in nursing care.


At St. Jude, many patients—especially those under the age of 3— undergo multiple rounds of anesthesia during treatment and monitoring. While necessary in many cases, this raises significant concerns about potential neurodevelopmental risks. In 2017, the U.S. Food and Drug Administration (FDA) issued a warning about the possible risks of prolonged exposure to general anesthesia on brain development in young children. Despite these risks, many St. Jude patients receive multiple anesthetics, with some undergoing up to 30 administrations throughout their treatment. Addressing these concerns is critical to protecting the neurocognitive well-being of patients and ensuring that anesthesia use is guided by medical necessity and evidencebased practices.
To address this challenge, the AWAKE (Achieving Care With Less Anesthesia Keeps Everyone Safe) initiative was piloted in the magnetic resonance imaging (MRI) area in 2024. The pilot demonstrated that with proper preparation, education, and time, many patients who previously required general anesthesia could successfully complete their scans awake without compromising safety or image quality.
The AWAKE team established key goals, including:
• Use prescreening, patient preparation, and general anesthesia alternatives—such as sedation techniques—to achieve a 10% reduction in general anesthesia use for pediatric MRI patients ages 6 and older from August 2024 to August 2025.
• Offer anesthesia-reduction services—including mock scanner appointments, preparation, SmileyScope, and personalized coping plans—to an average of 71 patients per month during the same period.
Since the program’s official launch on July 29, 2024, the impact has been clear. Out of 155 patients identified so far:
• 39 completed their scans completely awake,
• 55 had reduced anesthesia and are working toward fully awake scans,
• 16 families requested to join the program—and successfully did scans with little or no anesthesia.
This initiative represents a significant win for both patient health and institutional cost savings. One example is cost savings for the institution. Just one element of this program has saved approximately $190,000 and significant other savings have been identified.
Looking ahead, the AWAKE team plans to expand this approach to other areas, including nuclear medicine and procedural interventions. This expansion will incorporate prescreening, screening calls, child life interventions, and dedicated AWAKE nursing/anesthesia teams. The projected cost savings per scan are significant, estimated at $3,049 for PET scans and $6,317 for MIBG scans.
These potential savings, coupled with the reduction in both short- and long-term patient risks, make the AWAKE initiative a promising step forward in pediatric care.
AWAKE is dedicated to supporting patients and families throughout their treatment, providing innovative and patient-centered opportunities for anesthesia reduction while prioritizing safety and quality care. The greatest success is always the experience of the patient.

In alignment with the institution’s commitment to a culture of excellence in patient care, the Nursing Quality Champions Program launched in the spring of 2024. Designed to support both institutional and nursing strategic priorities, this initiative aims to drive improvements in four key patient outcomes: skin integrity, infection prevention, patient safety, and overall patient experience. The program engages clinical nurses from all specialties, empowering frontline caregivers to standardize best practices and implement process improvements that enhance patient care.
A dedicated project workgroup was established in May 2024 to develop the program framework. Composed of clinical nurses, nurse leaders, and a representative from the Office of Quality and Patient Safety, the group included representation from Inpatient, Outpatient, and Surgical Services. The team worked collaboratively to define the program’s structure, outline key responsibilities for nurse quality champions, develop a reporting framework, and identify champions across all clinical areas.

By July, the workgroup finalized the program’s charter, mission, objectives, success metrics, and implementation strategies. With these elements in place, the next phase commenced to select and onboard quality champions from each clinical department. The program officially launched with a kickoff meeting in September 2024, followed by comprehensive education and training sessions in November and December. These sessions equipped champions with essential skills in process improvement and clarified their roles in driving quality initiatives.
The Nursing Quality Champions now meet regularly to lead and sustain quality improvement efforts. With the support of nursing leadership and subject matter experts, this program is positioned to create a lasting impact on patient outcomes, fostering a culture where excellence in care is not just a goal, but a shared commitment.
Sepsis is a major global health crisis and remains one of the leading causes of death in children. Each year, 75,000 children in the U. S. develop severe sepsis with 7,000 deaths. Weakened immune systems and treatments of hematology/oncology patients put them at a higher risk for developing and dying from sepsis. If they survive, they are less likely to return to their previous quality of life after sepsis.
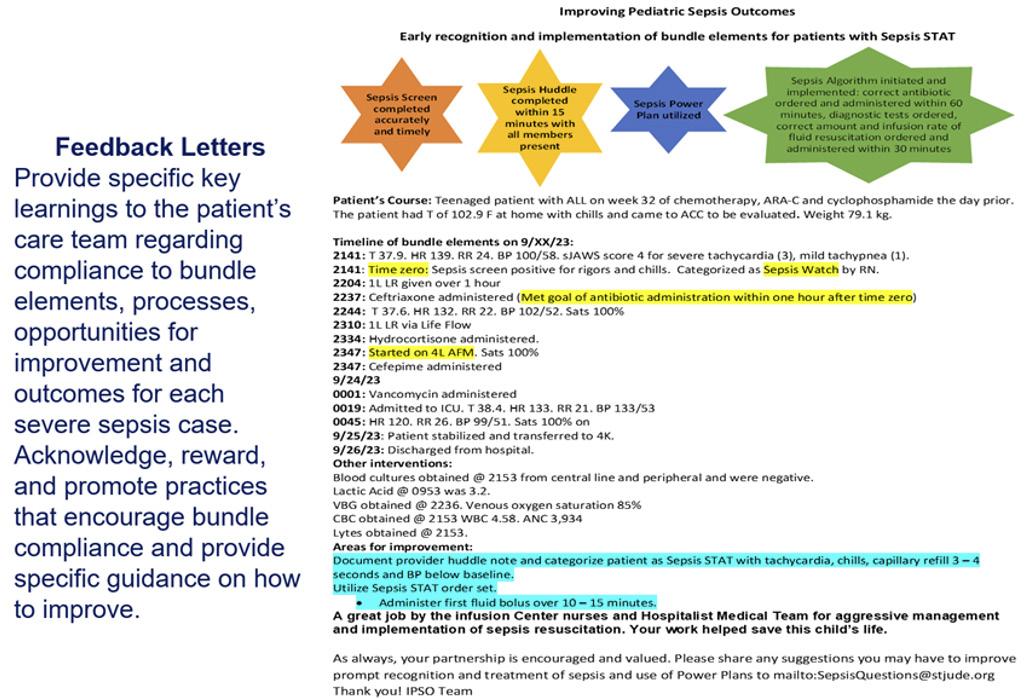
To reduce mortality of severe sepsis (Sepsis STAT) in our patients, St. Jude joined the Children’s Hospital Association Improving Pediatric Sepsis Outcomes (IPSO) multicenter quality improvement collaborative. A multiprofessional team including staff and family representatives developed evidence-based, hospital-specific Sepsis Recognition and Treatment Guidelines that included sepsis screening, team huddles, intervention algorithms, and order sets.
The St. Jude IPSO team used a data-driven approach to evaluate progress toward goals of compliance with the sepsis bundles of care. Based on baseline data in 2017-2018, several PDSA cycles were implemented to improve sepsis recognition and treatment in inpatient units first starting in 2019 followed by outpatient units in 2020.
The outcome measure for the IPSO team was 30-day sepsis-attributable mortality rate. Process measures from 2017–2023 included:
• Completion of a screening tool to identify potential sepsis (Time Zero)
• Classification of sepsis huddles after a team bedside assessment
• Use of order sets
• Minutes from Time Zero to antibiotic administration
• Minutes from Time Zero to fluid bolus administration
• Evaluation of diagnostic labs
• Administration of oxygen
• Transfer to the Intensive Care Unit (ICU)
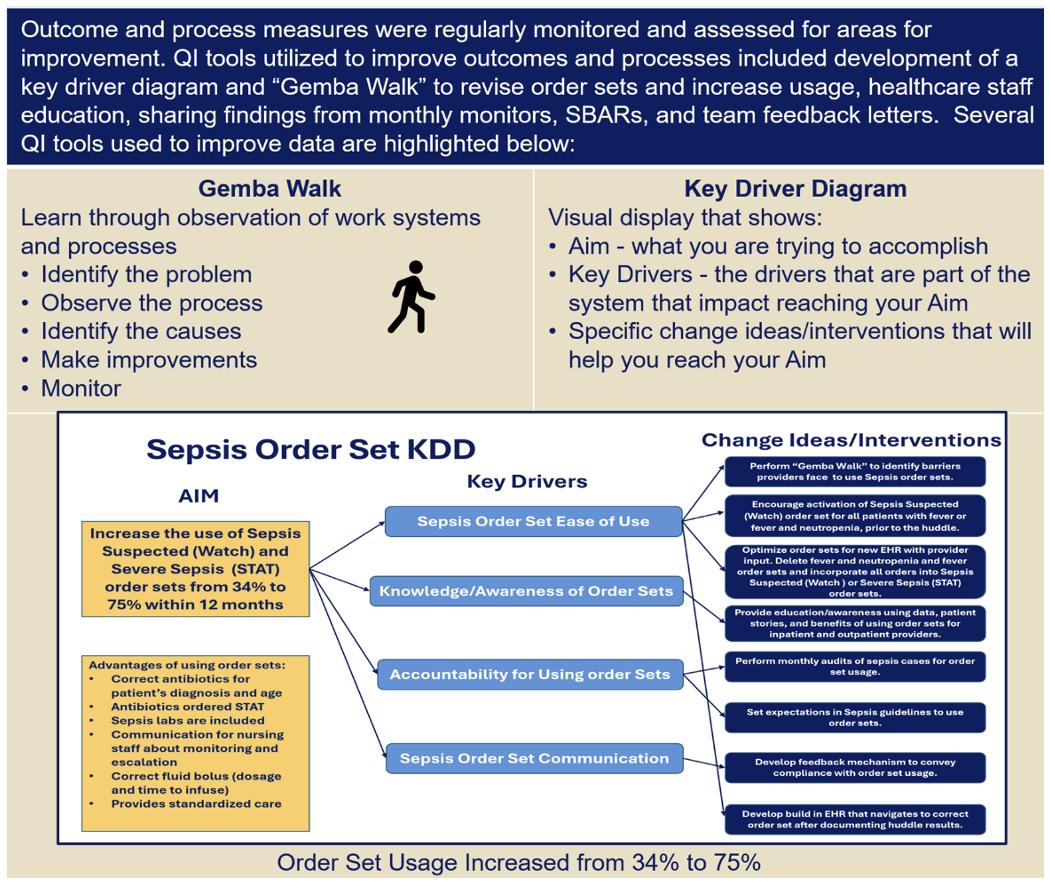
In 2024, the national IPSO collaborative disbanded, and a Sepsis Hospital Acquired Condition (HAC) team was created. This team consists of providers, clinical nurses, nursing leadership, and quality and patient safety team members. The team identified several initiatives to work on such as streamlining order sets and increasing sepsis huddle documentation for nurses and providers.
The centerline for the quarterly percent of 30-day sepsis-attributable mortality per severe sepsis episodes shifted from 0.18 at baseline in 2017-2018 to 0.02 in fourth quarter of 2023 with 16 of 20 quarters over the intervention period having no deaths attributed to sepsis.
Process measures for Sepsis STAT cases showed marked improvement from baseline:
• Screen activations increased from 0% to 100%
• Team huddle activations increased from 0% to 100%
• Time to first IV fluid bolus decreased from 125 to 8.6 minutes
• Time to first intravenous antibiotic decreased from 183 to 21.8 minutes
• Use of sepsis order sets increased from 34% to 72%
• The overall bundle compliance, defined by the collaborative as using sepsis recognition tool by either screening, huddle, or order set use, administration of IV antibiotics within 180 minutes, and administration of first IV fluid bolus within 60 minutes, increased from 0% to 100%
From the first quarter to the third quarter of 2024, St. Jude recorded no deaths attributed to sepsis. Implementation of quality improvement initiatives to standardize structures and processes in our hospital has helped improve and sustain early sepsis recognition and management which has proven to decrease morbidity and mortality and improve patient outcomes.
Based on a serious patient safety event involving patient device monitoring and management of abnormal vital signs, a root cause analysis was completed with a multidisciplinary team.
A key driver diagram was developed, and the following primary drivers were identified:
• Recognition and reporting of abnormal vital signs
• Clinical alarm management
• Documentation of concerns for patients
The Agency for Healthcare Research and Quality recognized alarm fatigue as a critical safety issue. Frequent, non-actionable alerts can desensitize staff, increase response times, and result in missed critical alarms.
The team wanted to address alarm fatigue and escalation of concerns as a root cause of the event. The team accomplished the following:
1. Reviewed, updated, and disseminated changes to staff for the following policies and procedures:
• Nursing Monitoring EKG, Pulse-Oximetry, and Non-invasive Blood Pressure
• Institutional Alarm Policy
• Vital Sign Policy
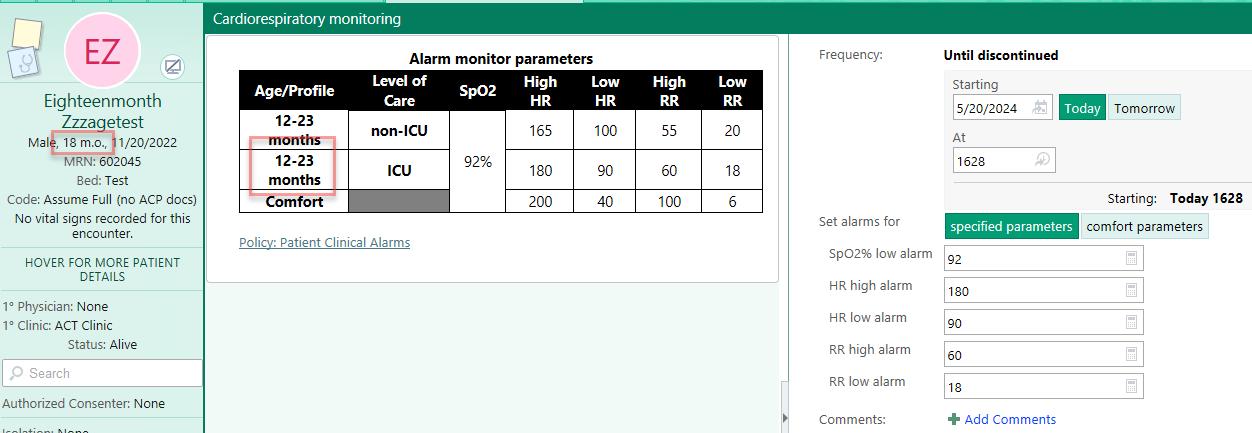
Example of vital sign order:
Example of cardiorespiratory monitoring order:
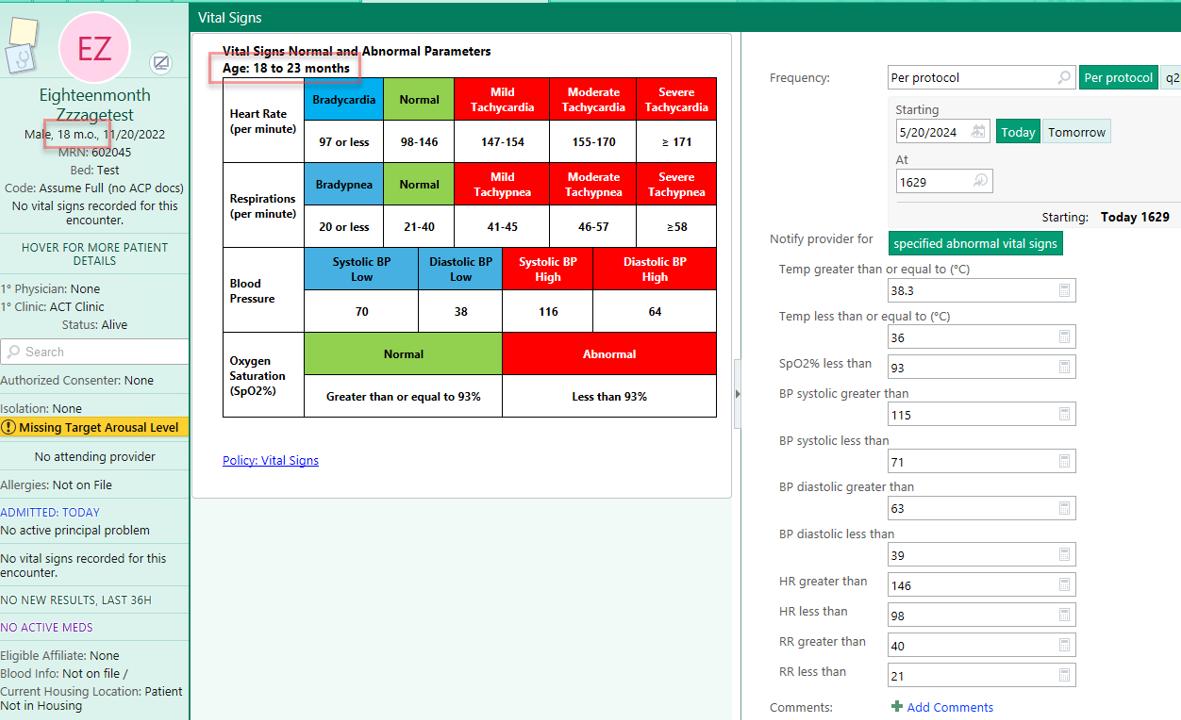
The team clarified and added language pertaining to setting alarm limits, responding to alarms, and communicating alarm alerts. The vital sign policy was updated to include concise steps to take when abnormal vital signs were obtained and subsequent communication with the providers.
2. Updated shift-to-shift and daily rounding reports to include review of vital sign ranges for the previous 24 hours for the patient.
3. Standardized inpatient messaging text from RN to provider using secure chat to set expectation of response timing.
4. Provided nursing documentation campaign that included expectations and instructions of what, when, and where to document.
5. Reviewed and updated nursing documentation for content, especially the definitions of Within Normal Limits (WNL) under each system review and removed irrelevant information in review of systems.
6. Collaborated with a multidisciplinary team including Information Services, Biomedical Engineering, and the Phillips Company to adjust default alarm parameters for inpatient units. In addition, age profiles were adjusted to be more like vital sign ranges, key alarm limits were adjusted to minimize unnecessary alarms, oxygen saturation-blood pressure profiles were added for patients not receiving cardiopulmonary monitoring, QT alarms were removed, and premature ventricular contractions (PVC) alarm alerts were changed from number of PVCs to runs of PVCs.
7. Ensured cardiopulmonary monitoring, continuous pulse oximeter monitoring, and inpatient orders were built with discrete parameters for notification of alarms with agespecific alarm parameters.
8. Revised vital sign monitoring inpatient orders to include parameters of when to notify provider outside of “normal” vital signs. These orders were built using the St. Jude Advanced Warning System (sJAWS) age limits and normal/abnormal values. A sidebar report was built to display the age specific vital signs.
Changes in the default alarm limit settings resulted in a significant reduction in inpatient alarm alerts. Over the course of one week, alerts decreased from 52,290 preintervention of changing alarm profiles and limits to 34,211 post intervention—a reduction of more than 35%. Ongoing audits are conducted in each inpatient unit to sustain these improvements for patients requiring clinical monitoring. Additionally, the updated documentation guidelines and new vital sign and alarm parameter orders have been positively received by clinical staff.
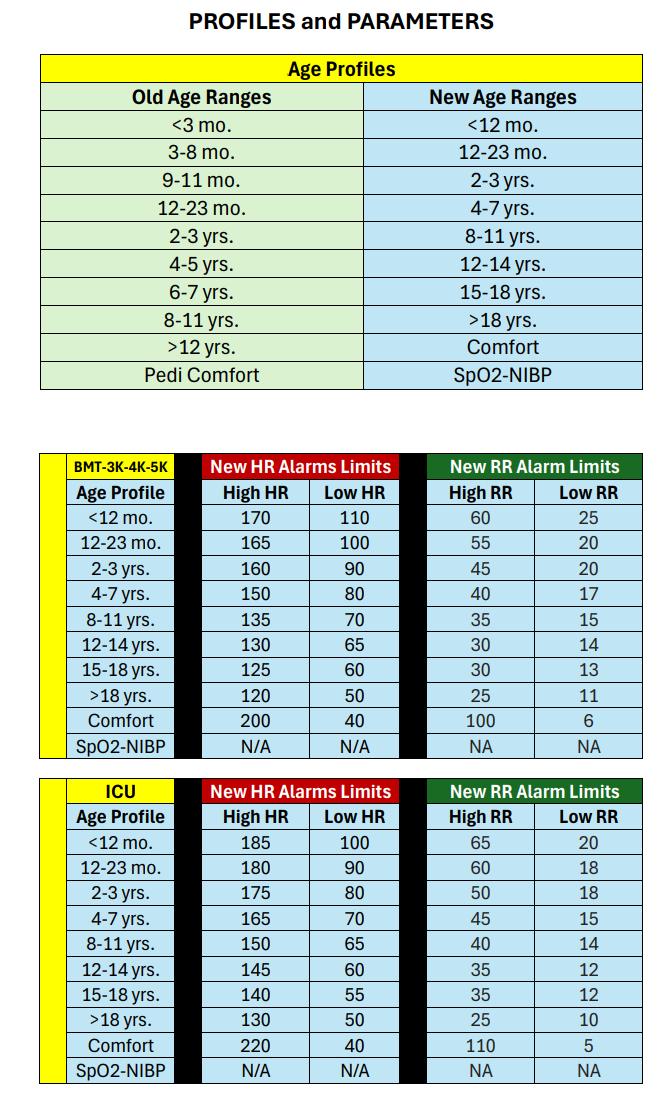
Enhancing campus-wide emergency response: A streamlined approach


The Nursing Clinical Logistics team and ICU medical staff at St. Jude recognized the need to refine the campus-wide emergency response process. Historically, emergencies occurring within designated patient care areas,–whether involving a patient, caregiver, visitor, or employee—were managed by the Harvey Team. This multidisciplinary team included an ICU attending physician, an Advanced Practice Provider, a clinical support leader, an ICU nurse, and additional personnel. However, emergencies occurring outside patient care areas were handled by the Campus Alert Team, which activated a response from the Occupational Health nurse, the Nursing house supervisor, and a Security officer.
Many incidents requiring the Harvey Team did not always need such specialized resources. This often diverted critical ICU staff away from patient care, creating inefficiencies. In response. Nolan Eason, MSN, RN, NEA-BC, director of Clinical Logistics, and Austin Hudson, MHA director of Inpatient Clinical Operations, led a task force to evaluate and optimize the campus emergency response process.
The task force, comprising two Clinical Logistics nurse managers, physicians, a legal representative, the nursing director of patient safety, and administrative support, developed a new response strategy. The proposed solution designated the Nursing house supervisors and Central Staffing supervisors as the primary responders to campus medical emergencies that did not require the Harvey Team.
Under the new protocol, emergency calls are triaged through Security dispatch communications, which then connects the Nursing house supervisor to assess the situation. This approach ensures a more efficient allocation of resources, allowing ICU staff to focus on patient care while enabling the Nursing house supervisors and Central Staffing supervisors to manage campus emergencies effectively. By streamlining response efforts, St. Jude enhances both patient safety and operational efficiency, ensuring that the right personnel are deployed where they are needed most.
Aromatherapy is the use of essential oils to create smells that target a part of the brain called the limbic system. Stimulating the limbic system can trigger emotions or memories, which causes the brain to release chemicals. The combination of essential oils and the release of natural chemicals in the body can help manage various symptoms. Aromatherapy is an integrative therapy used with other medical treatments to provide comfort in helping to manage symptoms, such as anxiety, stress, nausea, vomiting, pain, and sleep problems. Many patients admitted to the inpatient units typically receive some form of chemotherapy and biotherapy that frequently cause the patient to experience symptoms often managed with additional medications.

The Aromatherapy Workgroup is a multi-disciplinary team comprising clinical nurse experts from the bedside, Infection Control and Prevention, Nursing Education and Professional Development, the Office of Quality and Patient Safety, Regulatory Compliance, and Integrative Medicine. This team assembled in late 2023 and was led by Bridget Mans, BSN, RN, CPN, NE-BC. This team partnered with Materials Management, Environmental Health and Safety, and Strategic Communication, Education and Outreach (SCEO) to develop staff, patient, and family education. Essential oils was a new product that has now been ordered, stocked, or supplied to patients. Testing of the essential oils had to be completed to validate safety for patient storage as well as handling of the oils for regulatory compliance purposes. Based on symptom management, the workgroup identified five essential oils that would benefit St. Jude patients.
The group selected lavender, ginger, spearmint, orange, and lemon as essential oils for the inpatient units. These oils can help with the following:
• Lavender: Sleep problems, stress, anxiety, cough, and stomach cramps
• Spearmint: Nausea, upset stomach, cough, stress, and anxiety
• Orange: Sleep problems, upset stomach, stress, and anxiety
• Ginger: Nausea, loss of appetite, cough, and sore throat
• Lemon: Sleep problems, stress, and anxiety
Companies process essential oils using various methods, and the team worked diligently to identify the safest processing method to ensure patient safety was not compromised.
Staff training was also provided on how to dispense the oils and where to document the product in a patient’s chart. Education for patients and families was developed by Strategic Communication, Education, and Outreach (SCEO) and the information was shared on the Together by St. Jude website, which is an online resource. The essential oils were available on all inpatient floors in February 2024.
Integrated Medicine staff assisted with the institutional policy while Nursing created the standard operating procedure. SCEO developed patient education materials while Nursing Education and Professional Development created educational content and training for bedside nurses. After bedside nurses received education and training, the Inpatient Aromatherapy Program was implemented in all inpatient nursing units. There was great collaboration with Materials Management, whose team members were responsible for stocking the essential oils in a clean supply room on all units. Biomedical Engineering was a valuable partner in building a light-blocking container with a custom-built holder to house bottles of each essential oil and supporting supplies.
No two patients are alike and having more than one essential oil allows the patient the autonomy to choose what they feel might help. Patients select and use essential oils that help minimize side effects and anxiety—all in an environment that promotes healing. Complementary therapies and integrative health approaches such as aromatherapy contribute to the holistic approach of caring for the entire patient.
Nursing Clinical Logistics creates new Central Staffing supervisor role


In early 2024, the Clinical Logistics (CL) department created the Central Staffing supervisor position to provide oversight and coordination across Inpatient, Outpatient, and Surgical Services. This new role will ensure more efficient resource allocation and improve overall staffing consistency.
By April 2024, CL had successfully hired the first two Central Staffing supervisors. These hires played a critical role in shaping the Central Staffing office and began laying groundwork for upcoming changes.
CL launched the Central Staffing Office Task Force in July 2024. This task force brought together leaders from Inpatient services, Outpatient services, Surgical Services, and Clinical Logistics. With representatives from key departments, the task force thoroughly reviewed the scheduling process for each area, identified key differences and inefficiencies, and proposed solutions.
Through in-depth analysis and discussion, the task force found several critical issues within staffing processes, ranging from misaligned scheduling practices to resource allocation and communication challenges across departments. Based on these findings, the group developed a comprehensive business proposal for the Central Staffing office.
Once the proposal was complete, it was presented to the Nursing Executive Team (NET) for approval. After receiving NET’s support, the proposal was submitted for final approval to the Nursing Leadership Team.
Clinical Logistics planned a pilot run for the inpatient units beginning in April 2025.
Since 2021, St. Jude Home Care, LLC has been extending the care provided by St. Jude Children’s Research Hospital beyond the walls of the hospital. An important component of the St. Jude patient experience is to ensure patients thrive in their environments and enjoy their childhood as much as possible during treatment. Early patient experience surveys of discharged patients reflected patients and families greatly appreciated the convenience of receiving care by St. Judetrained clinicians in the comfort of their housing residence.
One parent said they “loved not having to go out for appointments.” Another patient lauded the convenience and accessibility of home-based care, saying her nurse “was amazing the whole way through. She checked on him in the hospital and responded timely, even at night. He was comfortable with her, and she made everything easier.”

Home Care’s nursing leaders are using the survey comments and feedback to enhance care delivery. For example, one patient in early 2023 expressed interest in additional services, such as physical and occupational therapy. By the end of the calendar year, both services were available to patients. Another parent noticed opportunities for improvement that the agency resolved through nursing re-education. Honest answers from patients and families provide valuable insights like these into patient safety, infection prevention, operations, and new services.
Feedback from patient experience surveys have been noted to boost morale and reignite the passion of frontline staff. Home Care leaders share specific comments from monthly surveys via their staff newsletter and bimonthly meetings. A great example of the connection established by providing care in the home environment is reflected by one parent: “He saw her at her worst and was the one she would call in a crisis. He was her backbone.” Another parent said, “She is like a big sister to me and helped me in the hard times.”
One unique advantage of home-based services that patient experience surveys highlight is the clinicians’ ability to identify and address patient needs in their natural, home environment. In one survey, a parent described how the nurse and rehabilitative therapists recognized her child’s decline and responded promptly when she became wheelchair bound. She said, “They talked to clinic and housing to get us into a more wheelchair-friendly apartment, which I didn’t even know was an option.” Another parent of a toddler expressed her desire for covers on outlets close to the ground. All feedback received is shared with the appropriate leaders so housing residences or care teams can respond and address the needs.
Home Care’s focus on patient and family-centered care is reflected in both the robust patient experience program and the responses it garners. In addition to the surveys, the agency prides itself on the recommendations and testimonials of repeat patients, who are readmitted for home care services numerous times as they come to St. Jude for extended periods of treatment. Ninetyeight percent of surveyed patients say they would recommend St. Jude Home Care to other families. One parent said they “wish we could transport the team” back to their hometown. Another young adult patient and his family appreciated the home-based care so much that they requested Home Care services before their return to St. Jude after several months away.
Despite the rapid expansion of services, a growing team, and increasing strategic priorities, Home Care consistently looks to its patients for purpose. Patient experience surveys are often the source of suggestions for improvement, morale-boosters for nurses, new patient safety considerations, and a last line of defense for service recovery or staff recognition. Home Care values the opportunity to be a part of the care journey for St. Jude patients and will continue to use feedback from the Patient Experience team to assess if the next innovations in care may be written in between the lines.
The Central Nervous System (CNS) is the processing center that manages the body’s thoughts and movements. The CNS collects, receives, and processes information and then responds with outputs like complex thinking, reasoning, planning, and making decisions.

In similar fashion, St. Jude Nursing has implemented a new role known as the Clinical Nurse Specialist (CNS). Serving as a processing center for the nursing team, the CNS collects and receives clinical information and helps expand outputs that drive improved outcomes across the St. Jude patient care continuum.
Sarah Currie, RNC, MSN, NEA-BC, St. Jude senior vice president and chief nursing executive, recognized the need for the CNS role and advanced the CNS position as a priority in the Nursing FY25 Strategic Plan as part of Goal No. 9 – “Reground nursing fundamentals and practice though leadership across clinical care teams to optimize patient care outcomes.”
Currie envisioned that the CNS would provide expertise and support to nurses caring for patients and help drive practice changes with a focus on three spheres of impact:
• Direct patient care
• Nurses/nursing personnel
• Organizations/systems
Mike Burgess, DNP, MBA, RN, BMTCN, and Pamela Renfrow, MSN, RN, are two newly appointed CNS leaders for Inpatient Units. Burgess and Renfrow each have many years of experience strengthening and fostering relationships as clinical role models at St. Jude. They are expertly equipped to serve as clinical subject matter experts to remove barriers to care, hardwire identification of nursing priorities, and nurture critical thinking. Their roles are strategically designed to support bedside nurses by identifying gaps in the delivery of care, helping to design and implement evidence-based interventions, and evaluating effectiveness of the changes.
There has been a resurgence of the CNS role, according to the World Health Organization (WHO). WHO also has reported that the effective deployment of CNS roles has strengthened quality of care, lowered health care costs, led system‐level nursing practice initiatives, and improved nurse recruitment and retention. The patient-centered mentorships and partnerships that Burgess and Renfrow build will help generate new knowledge and influence decisions that help shape nursing practice with best evidence and position nursing, which can produce outcomes that reach or surpass national benchmarks.


Evidence-Based Practice (EBP) has long been a recognized method to translate the best evidence into bedside patient care and improve patient outcomes. In 1998, the Division of Nursing Research initiated an EBP fellowship as a program to promote these knowledge and skills to nursing and other disciplines, and to create champions of the process. This long-standing program has joined with St. Jude Global Nursing in the design and implementation of an International EBP Fellowship. The goal of the fellowship is to support international nurses in the development and implementation of EBP projects as a practice change agent, thus impacting the care of children and adolescents with cancer in resource-limited countries.
In April 2023, seven nurses from the countries of Uganda, China, India, Pakistan, Poland, Jordan, and Brazil were selected with support from their supervisors to participate in the International EBP Fellowship. The fellowship entailed two weeklong site visits to St. Jude, the first four months after the initiation of the fellowship and the second at the 15-month conclusion. The curriculum included recorded sessions viewed via the Cure4Kids platform, the instructional framework for the fellowship. Bi-monthly Zoom meetings were held to discuss content and formulate EBP proposals. Each international nurse was paired with a St. Jude content expert nurse peer. The St. Jude nurse peer: Rima Saad, PhD, MSN, RN, CPHON; Jami Gattuso, APRN-CNP, CPON, FAPHON; Morgan Melancon, MSN, RN, CCRN, NE-BC; Sarah Currie, MSN, RNC, NEA-BC; Monnie Abraham, PhD, MSN, FISQua, CPHQ; and Belinda Mandrell, PhD, RN, FAAN, - collaborated with the international nurse via biweekly virtual meetings and during the on-site visits.

At the conclusion of the fellowship, the international nurses returned to St. Jude and presented their EBP project and outcome data. The EBP projects included:
• Uganda: Standardization of CPR guidelines
• China: Skin protection during transplant
• Poland: Patient reported pain assessment
• Jordan: Early ambulation post-surgery in the intensive care unit
• Brazil: Nurse initiated thrombolytic therapy for occluded central venous access devices
During the visit to St. Jude, each of the international nurses received the Daisy Foundation™ Nurse Leader Award for recognition of their EBP projects. Lastly, three of the nurses presented their work at International Society of Paediatric Oncology 2024, with an international nurse from China being awarded the highest scored abstract. Global Nursing sponsored the travel for the three international nurses and their St. Jude nursing peers to the SIOP meeting. Collectively, the EBP practice changes directly impacted 250 pediatric oncology patients in low- and middleincome countries.
The team found a virtual International EBP Fellowship can be successfully implemented with institutional nursing support, fostering international EBP initiatives and improving patient outcomes. The next International EBP Fellowship is slated to begin in spring 2025.
In the dynamic pediatric outpatient oncology setting, patient acuity varies significantly, directly impacting nurse workload and patient care quality. Historically, a fixed-staffing model has been employed, assigning nurses to patients based on the primary physician’s team rather than patient complexity or acuity. This approach often results in uneven workloads, leading to compassion fatigue, decreased job satisfaction, and inefficiencies in resource utilization.

Recognizing the need for a more balanced system, St. Jude Children’s Research Hospital implemented the Patient Acuity Tool (PAT) in 2024 to standardize nursing assignments based on patient needs. The PAT categorizes patient acuity into four levels:
• Low Acuity – Visits under 30 minutes
• Medium Acuity – Visits between 30 and 60 minutes
• High Acuity – Visits between 1 and 2 hours
• Extreme Acuity – Visits exceeding 2 hours
Nurses were responsible for tracking visit durations and assigning acuity levels, with data collected over a 90-day pilot period. The results revealed significant variability across clinical areas:
• Brain Tumor Clinic – 6.9% of patients had high or extreme acuity
• Solid Tumor Clinic – 24.03% of patients had high or extreme acuity
• Leukemia Clinic – 13.78% of patients had high or extreme acuity
• Transplant Clinic – 13.02% of patients had high or extreme acuity
These findings highlighted the limitations of a fixed-staffing model, reinforcing the need for a data-driven approach to workforce allocation. In response, the outpatient leadership teaminitiated phase 2 of the project, focusing on data verification and refinement. With support from Rachel Dhority, MBA, CPHQ, CSSGB, in Clinical Excellence, acuity data is now being compiled and analyzed in an improved electronic format. Angie Tidwell, MSN, RN, CAP V Advanced, is overseeing data validation, conducting retrospective chart reviews, and ensuring nurses complete reporting as required.
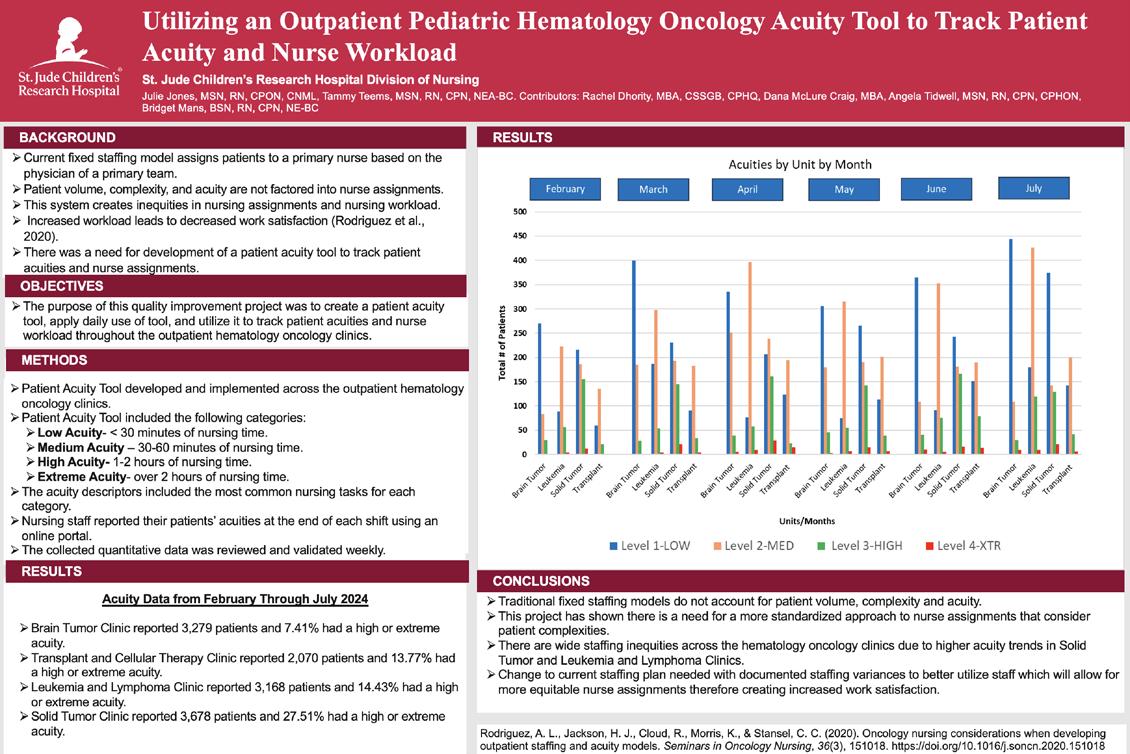
Looking ahead: Transforming staffing models for sustainability
The electronic acuity tracking system is now fully operational across all oncology clinics, with ongoing data collection over the coming months. The goal is to align nursing resources with patient acuity to optimize staff workload, enhance nurse satisfaction, and improve patient care delivery.
Leadership will use this comprehensive data to evaluate the current fixed staffing plan, ensuring it reflects the realities of patient complexity. Adjustments have already been made in the Solid Tumor Clinic, where nurse-to-patient ratios were adapted to accommodate consistently highacuity patients.
The success of this initiative hinges on the commitment of nursing leadership and staff to ongoing evaluation and refinement. By embracing data-driven decision-making, St. Jude is pioneering a sustainable, equitable staffing model that supports nurse well-being and patientcentered care.
Since Epic’s implementation at St. Jude in October 2022, optimization of the Epic user experience has been a major focus of St. Jude Nursing. In January 2024, Nursing initiated a project to improve the outpatient nurses’ rooming and screening process. When a nurse in one of the outpatient clinics opens a patient’s chart, the nurse is presented with a view of the rooming activity. The rooming activity is relatively a one-stop-shop where the nurse can review and enter pertinent patient information, such as medications, history, and vitals. Additionally, the nurse can complete required screenings for support services, including Clinical Nutrition, Child Life, and Social Work. Enhancements to the rooming activity required collaboration from Information Services analysts, outpatient nurses from multiple clinics, and nursing informatics representatives. The aim of the project was to provide a consistent, user-friendly experience across all outpatient departments by consolidating information, providing easier access to documentation and tools, and removing extraneous reports and questionnaires.
The first change involved moving the Developmental History and Performance Scores sections from the Rooming tab to the Plan tab. Doing so improves ease of access for the providers who typically perform these tasks.
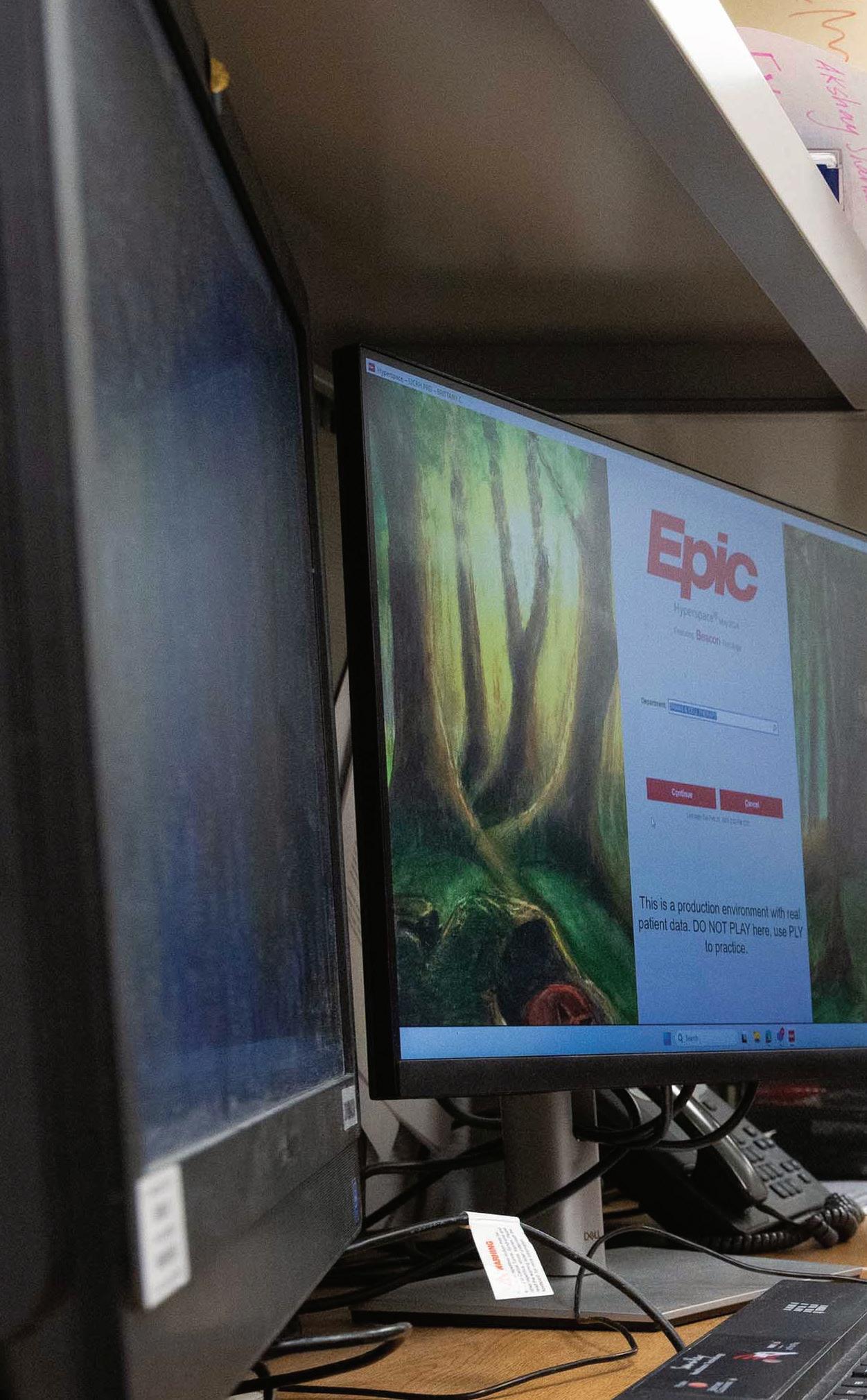
Next, the dual-pane activity view that Beacon users have used since go-live was extended to the Ambulatory and Specialty clinics. The left side of the activity features standard documentation for all clinics, while the right side contains both standard and specialty-specific documentation. The specialty-specific documentation is displayed based on the nurse’s log-in department to ensure each user can access the most relevant information for his or her area of expertise.
A third change involved the creation of a Nursing Documentation flowsheet designed to aggregate documentation, such as sJAWS, Sepsis, and Discharge Disposition. Nurses can access this flowsheet from the Rooming tab or Documentation Flowsheets activity.

Finally, the outpatient screenings, which previously contained three different assessment groupings and included many irrelevant questionnaires, were reduced to a single assessment containing only relevant information for our patients.
These changes were implemented in late June, bringing us closer to standardizing nursing documentation and improving our ability to provide outstanding patient care at St. Jude.

St. Jude has implemented a new document management framework through PolicyTech. PolicyTech hardwires workflows to ensure documents are not duplicative, are evaluated systematically, and updated timely. PolicyTech also enabled St. Jude to establish one repository for institutional and departmental documents. With over 200 policies and procedures, Nursing was one of the first departments that made the transition from paper to PolicyTech.
Margie Kjellin, MSN, RN, CPHON, NE-BC, senior director, Nursing Clinical Excellence, welcomed the opportunity to leverage technology that ensured the most current and relevant nursing information would be available to reduce potential for patient harm. This often arises from using outdated or incorrect versions of policies and procedures. Studies show that an efficient document management process can decrease variability in nursing practice which can reduce risk for adverse events by reducing errors and promoting clear communication.

Kjellin initiated discussions about the resources and preparation required for PolicyTech migration. She became aware that the file transfer into PolicyTech would temporarily suspend review activity as well as impact policy availability. St. Jude nurses routinely refer to policies and procedures to guide safe care and practice. Subsequently, PolicyTech became a high nursing priority and a planning process to support a go-live date of June 2024 was a key objective.
In January 2024, Felecia Warner, MHA, RHIA, CHC, CPHQ, CSSBB, senior program manager, Clinical Excellence, created an implementation plan to facilitate a phased
approach for migrating nursing documents from Sharepoint to PolicyTech by the go-live date. Jen Lamont, MSN, RN, program manager, Document Control and Management, was consulted to provide guidance. Lamont, the PolicyTech administrator, had gained valuable insight from the recent transfer of institutional policies. These lessons proved to be beneficial to help Nursing navigate bottlenecks and delays.
Kjellin, Lamont and Warner met weekly to discuss the progression of the project plan. It became evident that migration would be more than a move to a document control system. It was a movement to a robust software solution that required shifting of Nursing’s entire document landscape. Documents were assigned to specific categories. The title of the documents and the file name had to be aligned and reconciled with a master list. Documents were moved and saved to a Teams Workspaces site for non-searchable, secure download for historical reference. Members for Locked Committees designated to review the documents were identified. Approval groups were created for the workflow. Timeframes were outlined for system alerts and notifications to be generated. This information had to be managed timely, approved by nursing leaders, and submitted for upload into PolicyTech. The planning, consultation, collaboration, and communication along with guidance from Lamont and support of Nursing executive leadership resulted in a blueprint for success. Nursing document migration to PolicyTech was completed ahead of schedule – April 30, 2024. This implementation resulted in the identification of 20 policy duplications, six policy consolidations, and established a standardized platform for the review of nursing practice through the Nurse Policy Council within the shared governance structure.

Publications
Abramson, Z, Rabe, D, Persaud, Y. Pulmonary Microvascular Occlusion in Sickle Cell Disease. Journal of Pediatric Hematology/Oncology 46(3):p e212-e213, April 2024.
Chang KTE, et al., ALK-positive histiocytosis: An expanded clinicopathologic spectrum and frequent presence of KIF5B-ALK fusion. Mod Pathol. 2019 May;32(5):598-608.
Crom DB, Walters LA, Li Y, Liang J, Hijano DR, Mulrooney DA, Carmichael LA, Ford SL, Andrews SJ, Smith D, Hudson MM, Mandrell BN. Seroprevalence of measles (rubeola) antibodies in childhood cancer survivors. JOPON 2024 May 7: 27527530231221145. doi: 10.1177/27527530231221145.
Cuthbert, C., Zaghloul, T., Bhatia, S., Mothi, S. S., Davis, E., Havens, H.G., Bishop, M. W., Talbot, L. J., Neel, M. D., Abdelhafeez, A. H., (2024). Use of Vacuum-Assisted Closure to Reduce the Likelihood of Wound Complications after Limb-Sparing Resection of Pediatric Primary Bone Sarcomas of the Femur, Journal of Pediatric Surgery.
Gehle, D. B., Morrison, Z. D., Halepota, H. F., Kumar, A., Gwaltney, C., Krasin, M. J., Graetz, D. E., Santiago, T., Boston, U. S., Davidoff, A. M., & Murphy, A. J. (2024). Wilms Tumor with Vena Caval Intravascular Extension: A Surgical Perspective. Children (Basel, Switzerland), 11(8), 896.
Gray, N., Sims, K., Lewis, S., Lei, S., Bhatt, N., Gheorghe, G., Takemoto, C., & Wlodarski, M. W. (2024). The ghost of parvovirus past: Idiopathic pure red cell aplasia responding to IVIG following resolved perinatal parvovirus B19 infection. Pediatric blood & cancer, e31252. Advance online publication.
Harper, E.H., Woody, K., Ousley, M., Acharya, R., Davis, M., & Slone, J. (2024 ) Family centered round’s impact on communication and rounding efficiency for chemotherapy service. 2024 ASPHO Conference Papers and Posters. Pediatric Blood & Cancer, 71: e30977. http:// doi.org/10.1002/pbc.30977
Hines-Dowell S, McNamara E, Mostafavi R, Taylor L, Harrison L, McGee RB, Blake AK, Lewis S, Perrino M, Mandrell BN, Nichols KE. Genomes for nurses: Understanding and overcoming barriers to nurses utilizing genomics. Journal of Pediatric Hematology/Oncology Nursing 2024 Feb https://doi. org/10.1177/27527530231214540
Humphrey Y, Elliott A, Madni A, Mandrell BN. Early onset schizophrenia in a pediatric oncology setting: A case report. Issues of Mental Health Nursing 2024 Jul 16:1-5. doi: 10.1080/01612840.2024.2360588.
Johnson LM, Sharma A, Carroll Y, Goodson D, Mandrell BN, Gattuso JS, Young AJ, Boggs J, Wilfond B, Unguru Y. In Response to: Preferences for potential benefits and risks for gene therapy in the treatment of sickle cell disease. Blood Advances 2024 Jun 12: bloodadvances:2024012963. doi: 10.1182/bloodadvances.2024012963. PMID: 38865716.
Kemps PG, et al., ALK-positive histiocytosis: a new clinicopathologic spectrum highlighting neurologic involvement and responses to ALK inhibition. Blood. 2022 Jan 13;139 (2):256-280.
Lilley, M. M., Salek, M., Holland, A., Inaba, H., & Federico, S. M. (2024). Treatment of a pediatric patient with Concurrent Neuroblastoma and Acute Lymphoblastic Leukemia. Pediatric Blood & Cancer.
Mandrell BN, Boggs J, Gattuso J, Caples M, Sawyer K, Madni A, Johnson LM. Moral distress and moral stress among nurses facing challenges in a health care system under pressure. AJBO 24(12), 48-51. 2024. Doi: 10.1080/15265161.2024.2417992 PMID: 39565260.
Mandrell BN, Guo Y, Li Y, Hancock D, Caples M, Ashford JM, Merchant TE, Conklin HM, Crabtree VM. Internalizing symptoms and their impact on patient-reported heath related quality of life and fatigue among patients with craniopharyngioma during proton radiation therapy. Children 2024. doi.org/10.3390.
McGee, R. B., Oak, N., Harrison, L., Xu, K., Nuccio, R., Blake, A. K., Mostafavi, R., Lewis, S., Taylor, L. M., Kubal, M., Ouma, A., Hines-Dowell, S. J., Cheng, C., Furtado, L. V., & Nichols, K. E. (2023). Pathogenic Variants in Adult-Onset Cancer Predisposition Genes in Pediatric Cancer: Prevalence and Impact on Tumor Molecular Features and Clinical Management. Clinical cancer research : an official journal of the American Association for Cancer Research, 29(7), 1243–1251. https://doi.org/10.1158/1078-0432.CCR-22-2482.
Max, A., Glasgow, H. L., Santiago, T., Holland, A., Inaba, H., Cañete-Gibas, C. F....Adderson, E. E. (2024). Choanephora infundibulifera Rhinosinusitis in Man with Acute Lymphoblastic Leukemia, Tennessee, USA. Emerging Infectious Diseases, 30(6), 1245-1248.
Moody, J., Barker, P.J., Sciasci, J., Pauley, J. L., Bragg, A., McMillan, C., Triplett, B. M., & Swanson, H. D. (2024). Blinatumomab infusion interruptions in pediatric patients rarely lead to readmission. Pediatric Blood & Cancer, 71(10).
Pritchard M, Ogg S, Bosi J, Mandrell BN. Utilization of photobiomodulation for the prevention and treatment of oral mucositis. Journal of Pediatric Hematology Oncology Nurses, 2024 Mar-Apr; 41(2):107-113. doi: 10.1177/27527530231214525.
Purvis, K., Hiskey, L., Khanlari, M., Mead, P. E., Holland, A. C., Bag, A. K., Adderson, E., & Inaba, H. (2024). Simultaneous presentation of B-acute lymphoblastic leukemia and streptococcus agalactiae meningitis in a 3-year-old girl. Journal of Pediatric Hematology/Oncology.
Sanchez-Corzo A, Loschinskey Z, Navarrete M, Saini C, Ness KK, Hudson MM, Krull K, Mandrell BN, Siraram R. Correlation of sleep spindle structures and apnea/ hypopnea index in adult survivors of childhood Hodgkin lymphoma. Sleep Medicine 2024 Feb; 115 Sup 1 http://doi. org/10.1016/j.sleep.2023.11.919
Sharp KM, Clark ME, Jurbergs N, Ouma A, Harrison L, Taylor L, Hamilton K, McGee RB, Nuccio R, Hines-Dowell S, Gattuso JS, Pritchard M, Mandrell BN, Tercyak KP, Johnson LM, Nichols KE. A content analysis of parents’ reflections on pathogenic and uncertain pediatric oncology germline sequencing results. Familial Cancer 23, 551–561 (2024) https://doi.org/10.1007/s10689-024-00417-9.
Stone, S. Contributing Author of Hollier’s Clinical Guidelines in Primary Care: Fifth Edition (2024). Lung Cancer Screening. Lafayette, LA: Advanced Practice Education Association.
Presentations
Allen, H. & Burgess, R. Introduction to HIV. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. September 2024.
Andrews, S. & Poindexter, O. Introduction to survivorship. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN, United States. March 2024.
Attardi, E*., Gray, N.*, Lewis, S., Boals, M., Takemoto, C., Sharma, R., Christakopoulos, G., Bhoopalan, S., & Wlodarski, M. Benchmarking peripheral blood versus bone marrow for longitudinal monitoring of clonal hematopoiesis in predisposed individuals [Conference session]. Working Meeting EWOG MDS/SAA, Bologna, Italy. May 2024.
Baker, A. Introduction to critical care. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. June 2024.
Blazin LJ, Terao MA, Spraker-Perlman H, Baker JN, McLaughlin Crabtree V, Mandrell BN, Gattuso JS, Sellers J, Dunn TI, Lu Z, Hoffman JM, Burlison JD. An Organization Directed Approach to Improving Physician Burnout. MedStar Georgetown University Hospital Grand Rounds. August 2024.
Boggs JE, Caples M, Gattuso J, Levine D, Madni A, Shoulders L, Azzi Y, Ashcraft E, Li Y, Sawyer KE, Johnson LM, Mandrell BN. I’m trying to do the right thing! A mixed methods investigation of moral and ethical distress among pediatric hematology/oncology nurses. Association of Pediatric Hematology Oncology Nurses. Salt Lake City, UT. September 2024.
Brown, K. Introduction to anesthesia. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. March 2024.
Chittenden A. KIF5B-ALK Fusion Histiocytosis of the Central Nervous System in a 2- year-old: A Case Report. The American Society of Pediatric Hematology/Oncology. Seattle, WA. April 2024.
Clark, K. & Wheeler, C. Introduction to endocrine. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. September 2024.
Currie, S. From Bedside to Boardroom – Using Influence to Connect and Collaborate in High Stakes Communication. 2024 NICU Leadership Forum- Synova. Charlotte Harbor, Florida. April 2024; Nursing Research and Psychosocial Services Symposium. St. Jude Children’s Research Hospital. Memphis, TN. May 2024
Easterwood, C. & Max, A. Introduction to infectious disease. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. June 2024.
Ellis, Katherine. Hematology, St. Jude Children’s Research Hospital Affiliate Conference. March 2024.
Ellis, K. Hemophilia updates. Annual Affiliate Conference. St. Jude Children’s Research Hospital, Memphis, TN. March 2024.
Gibney K, Nisar S, Chakraborty K, Hanby P, Hudson MM, Ness KK, Mandrell BN, Krull K, Bagga P. Associations between neurometabolite levels and sleep quality in survivors of pediatric Hodgkin lymphoma. ISMRM & ISMRT Annual Meeting and Exhibition. Singapore, May 2024.
Gray, N. & Boals, M. Cases in bone marrow failure & myelodysplastic syndrome [Lecture]. St. Jude Children’s Research Hospital Pediatric Hematology Oncology Education Series. Memphis, TN, United States. March 2024.
Hoffman, J., Henderson, N., Currie, S., Lion, R., Stone, S., Havens, H., Orman, A. Taking care of skin is risky business [grand rounds]. St Jude Children’s Research Hospital. Memphis, TN. May 2024.
Humphrey, Y. Psychiatry in a pediatric oncology setting. Annual Affiliate Conference. St. Jude Children’s Research Hospital, Memphis, TN. March 2024.
Humphrey, Y. Introduction to psychiatry [Oral presentation]. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. June 2024.
Jiali, M., Davis, E. et al. Providing bundle education during bone marrow transplantation to decrease the incidence of incontinence associated dermatitis in children: an evidence-based practice project. International Society of Pediatric Oncology, Honolulu, HI. October 2024.
Johnson LM, Sharma A, Boggs J, Acharya R, Caples M, Gattuso J, Olufadi Y, Kang G, Mandrell BN. Attitudes toward medical research among adolescent patients and parents of children with sickle cell disease: It’s all about trust and human relationships. American Society of Bioethics and Humanities. St. Louis, MO. 2024.
Jones, S. Introduction to transition oncology program. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. March 2024.
Jones T, Williams CT. Advantages of Ultrasound Technology for Venous Access in a Blood Donor Center. American Society for Apheresis (ASFA). Las Vegas, NV. April 2024.
Kimble, A. Introduction to fertility. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. June 2024.
Lavoie, P. Introduction to hematology. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN September 2024.
London, C. Introduction to adolescent & young adult programs & support. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. June 2024.
Mandrell BN. Implementation of a photobiomodulation program within a pediatric oncology setting. International Conference of PBM. London. August 2024.
Mandrell, BN. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. September 2024.
McNeil, M. & Bobelis, A. Introduction to quality of life. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. March 2024.
Ogg S, Clug H, Bosi J, Prichard M, Mandrell BN. Developing a hospital-wide photobiomodulation program for a pediatric oncology hospital. SIOP. Honolulu, HI. October 2024.
Pease, P. Interprofessional teaming. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. June 2024.
Pease, P. & Dodson, M. Sepsis interactive simulation. Center of Advanced Practice Care of the Decompensating Patient. St. Jude Children’s Research Hospital, Memphis, TN. March 2024.
Pease, P. & Dodson, M. Advanced practice provider emergency management & escape room simulation. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. March 2024.
Pease, P. & Ureda, T. Working in wellness. ANCC Accreditation Transition to Practice Symposium. New Orleans, LA. April 2024.
Pease, P. & Walters, L. Compassionomics. Center of Advanced Practice Leadership Series. St. Jude Children’s Research Hospital, Memphis, TN. June 2024.
Proctor, K. Introduction to interventional radiology. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. March 2024.
Rodriguez, S. Introduction to quality improvement. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. March 2024.
Saleh, A. Introduction to the hospitalist service. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. June 2024.
Sabbatini G. Let’s Talk About Sex: 2024 STI Update. APP Competency Days at St. Jude Children’s Research Hospital, Memphis, TN. September 2024.
Sabbatini G. Let’s Talk About Sex: 2024 STI Update. Tennessee Academy of Physician Assistant’s Spring Fling, Chattanooga, TN. April 2024.
Sabbatini G. DoxyPEP. Hughes Infectious Diseases Clinic at SJCRH Therapy Change Meeting, Memphis, TN. April 2024.
Simmons, A. Introduction to neurology. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. September 2024.
Simmons, A. & Pease, P. Neurology exam simulation. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. September 2024.
Sisam, J. Introduction to BMT at St Jude Children’s Research Hospital. [Quarterly Didactic APP Education Series]. St. Jude Children’s Research Hospital, Memphis, TN. March 2024.
Stone, S. “Nursing Competency and Assessment in Pediatric Hematology-Oncology“, Pediatric Oncology Summit of Chinese Children s Cancer Group, Shanghai, China. May 2024.
Stone, S. “Advancing Competencies in Pediatric Hematology-Oncology for Advanced Practice Nurses “, Pediatric Oncology Summit of Chinese Children s Cancer Group, Shanghai, China. September 2024.
Stone, S. Advanced practice provider productivity. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital, Memphis, TN. September 2024.
Stone, S & Ureda, T. “Journey to Accreditation: St Jude’s Story,” American Nurse Credentialing Center Transition to Practice Conference, Online National Presentation. May 2024.
Stone, S. & Ureda, T. “Operational readiness for Transition to Practice Program,” American Nurse Credentialing Center Transition to Practice Conference. New Orleans, LA. May 2024.
Traynom M, Pennington K, Howard V. Navigating Social Determinants of Health to Optimize Outcomes in Adolescents with Refractory Iron Deficiency Anemia Related to Heavy Menstrual Bleeding. Association of Pediatric Hematology Oncology Nurses. Salt Lake City, UT. September 2024.
Traynom M, Pennington K, Howard V. Developing an Integrated Clinic for Adolescents with Severe Anemia Secondary to Heavy Menstrual Bleeding: A Single Institution Experience. Association of Pediatric Hematology Oncology Nurses. Salt Lake City, UT. September 2024.
Turner, R. The Characteristics of a Successful Preceptor. APP Preceptor Course Series, St. Jude Children’s Research Hospital, Memphis, TN, United States. 2024.
Turner, R. Advanced practice provider-led projects: Awake. Annual Affiliate Conference. St. Jude Children’s Research Hospital, Memphis, TN. March 2024.
Ureda, T. & Stone, S. American Nurse Credentialing Center Transition to Practice Conference. “How to present a professional presentation,” New Orleans, LA. May 2024.
Ureda, T. & Pease, P. An Education Series to promote the clinical & professional development of the advanced practice provider. ANCC Accreditation Transition to Practice Symposium. New Orleans, LA. April 2024.
Ureda, T. Professional advocacy & networking. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. June 2024.
Ureda, T. & Neal, C. Professionalism. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. March 2024.
Walters, L. Everyone is a leader. Center of Advanced Practice Quarterly Didactic Education Meeting. St. Jude Children’s Research Hospital. Memphis, TN. September 2024.
Yoshida, M., Lewis, S., Gray, N., Sahoo, S., & Wlodarski, M. Comprehensive analysis of SAMD9 and SAMD9L variants using SAMD9/9L database [Conference session]. 2024 SIOP Asia Conference, Yokohama, Japan. June 2024.
Attardi, E*., Gray, N.*, Lewis, S., Boals, M., Sharma, R., Christakopoulos, G., Bhoopalan, S., & Wlodarski, M. Peripheral blood as a source for monitoring clonal hematopoiesis in bone marrow failure syndromes. 2024 ASPHO Conference. Seattle, WA.
Baughn B, Waters A, Reap L. 3K IMCU Unit Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Bedard B, Caldera S. Enhancing the Patient and Family Experience During Radiation Therapy: Tips from Radiation Oncology Nurses at St. Jude Children’s Research Hospital. SIOP Annual Congress, Honolulu, HI. 2024.
Buchanan J, Giles, J. 4 Kay Unit Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Cepowska, Zuzanna, Norman, Gina et al. “Implementation of patient reported pain assessment by nurses in a pediatric oncology inpatient setting in Poland: a single center pilot study.” International Society of Pediatric Oncology. October 2024. Honolulu, Hawaii.
Crabtree V Mc, Mandrell BN, Tushar P, Li Y, Flerlage J, Friedmann A, Marks L, Weinstein H, Link M, Ehrhardt M, Feraco A. Patterns of fatigue in adolescents and young adults with high-risk Hodgkin lymphoma. SIOP Annual Congress 2024. Honolulu, HI.
Craghead T, Ledford A, Spencer C. Nursing Informatics Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Davis E, Miali J. Skin Care for BMT Patients. SIOP Annual Congress 2024. Honolulu, HI.
Davis G, Gerke A, Northway A. Inpatient Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Dormois G, Hussein, A. Using Distraction with the PopIt for Patients Getting Inhalation Therapy. SIOP Annual Congress 2024. Honolulu, HI.
Draffin D, Eddy J, Mobley R. Magnet Champions Committee. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Feathers T, Touchstone L, Johnson D. Infusion Center/ Acute Care Clinic Unit Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Gattuso J, Saad R, Abraham M, Melancon M, Mandrell BN, Currie S. Design and implementation of an international evidence-based practice fellowship. SIOP Annual Congress 2024. Honolulu, HI.
Gibney K, Nisar S, Chakraborty K, Li C, Burman R, Hanby P, Guthrie S, Hudson MM, Ness KK, Mandrell BN, Krull K, Bagga P. Age is associated with myo-inositol in survivors of pediatric Hodgkin lymphoma but not control subjects. ISMRM Workshop, Boston, MA, October 2024.
Gray, N., Boals, M., Lewis, S., Yoshida, M., Sahoo, S., & Wlodarski, M. Signatures of somatic genetic rescue in SAMD9/9L syndromes: diagnostic and prognostic utility. The MDS Foundation 3rd Regional Symposium on Myelodysplastic Syndromes. March 2024.Kyoto, Japan.
Havens, H. It is all about that risk: what pediatric oncology/ hematology patients have taught us about their pressure injury risk. Symposium on Advanced Wound Care. October 2024. Las Vegas, Nevada.
Hines-Dowell S, McNamara E, Mostafavi R, Taylor L, Harrison L, McGee RB, Blake AK, Lewis S, Perrino M, Mandrell BN, Nichols KE. Genomes for nurses: Understanding and overcoming barriers to nurses utilizing genomics. SIOP Annual Congress 2024. Honolulu, HI
Hines-Dowell, S. Genomes for nurses: exploring barriers surrounding genomics education in pediatric oncology nurses. October 2024. Honolulu, HI..
Husband S, Haley J, Burchett M. ICU Unit Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Husband S, Aridah A. Initiating Early Mobility in ICU Patients Post Thoracic and Abdominal Surgery. SIOP Annual Congress 2024. Honolulu, HI.
Johnson LM, Sharma A, Young AJ, Acharya R, Boggs J, Caples M, Gattuso J, Olufadi Y, Kang G, Mandrell BN. Genetic knowledge among adolescent patients and parents of children with Sickle Cell Disease. ASPHO Conference, April 3-6, Seattle, WA 2024.
Jones J, Teems T. Utilizing an Outpatient Pediatric Hematology Oncology Acuity Tool to Trace Patient Acuity and Nurse Workload. Association of Pediatric Hematology Oncology Nurses. Salt Lake, UT. 2024.
Mackay V, Lavoie P, Stone S. Advanced Practice Provider Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Magness S, McElroy L, Kjellin M, Warner F. Nursing Policy Committee. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
McElroy L, Reap L, Kjellin M. Coordinating Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
McElroy L. Nursing Shared Governance. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Meredith, C., Aldridge, S., DuLaney, M., Pickett, D., & Rochester, R. Improving cohesiveness among highly diverse Advanced Practice Provider Teams. Advanced Practice Provider Leadership Summit. September 2024. Nashville, TN.
Morgan S, Ferreira D. Initiating Thrombolytic Therapy on Patients whose Central Lines were Occluded. SIOP Annual Congress 2024. Honolulu, HI.
Navarrete M, Mulrooney DA, Roop J, Guthrie S, Ogg S, Ness KK, Hudson MM, Mandrell BN, Krull KR. Examining cardiac radiation and sleep on psychological distress in adult survivors of pediatric Hodgkin lymphoma without breathing sleep disorders. 3rd International Symposium on Late Complications After Childhood Cancer, Lucerne, Switzerland, 2024.
Norman G, Cepowska Z. Patient Reported Pain Assessment. SIOP Annual Congress 2024. Honolulu, HI.
Orman A, Alexander A, Kjellin M. Nursing Leadership Team (NLT). St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Ousley M, Bock S, Mobley R. Healthy Work Environment Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Ovelar K, Connolly K, Elizarraras, J. Kay 5 Unit Based Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Patrick D, Harrison J, Dorsey M. Quality Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Pease, P. & Dodson, M. Empowering & educating advanced practice providers through emergency management simulation. Nursing Research & Psychosocial Services Symposium. May 2024. St. Jude Children’s Research Hospital, Memphis, TN.
Potter B, Sabin ND, Mandrell BN, Ness, KK, Hudson MM, Krull KR. Neurocognitive Decline among Long-term Survivors of Pediatric Hodgkin lymphoma: A Report from the St. Jude Lifetime Cohort. American Society of Hematology Annual Meeting 2024. San Diego, CA.
Reap L, Nabakooza S. Implementing Standardized CPR Guidelines. SIOP Annual Congress. 2024. Honolulu, HI.
Rees, M., Kannady, R., Pearson, T., Risinger, A., Meredith, C., Aldridge, S., Ballinger, N., LaPlante, R., Wade, A., Stone, S., Inaba, H., & Bhatt, N. Improving fellow continuity clinic with multiple specialty clinics: A quality improvement initiative. American Society of Pediatric Hematology/Oncology. April 2024. Seattle, WA.
Saad R, Gattuso J, Melancon M, Currie S, Mandrell BN, Abraham M. Taking excellence to the world through adaptation and implementation of an international evidence-based practice fellowship for pediatric oncology nurses. Association of Pediatric Hematology Oncology Nurses 2024. Salt Lake, UT.
Shoulders L, Delaney V, Mandrell B. Nursing Research & Evidenced Based Practice Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Sisam, J. Preventing Immobility Harm in Hospitalized BMT Patients at St Jude Children’s Research Hospital. QI Academy poster presentation. St. Jude Children’s Research Hospital. January 2024.Memphis, TN.
Smith I, Bedard B, Pepper A. Nursing Surgical Services (NSS) Service Line Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Stratton A, Zeig C, Bock S. Bone Marrow Transplant Unit Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.
Tidwell A, Hoy J, Key M. Outpatient Unit Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.

Ureda, T. & Pease. Advanced practice provider education: Bringing current clinical knowledge to the advanced practice provider. APHON Annual Conference. September 2024. Salt Lake City, UT.
Woodruff, C. Pre-Assignment of Weekend Infusion Center Patients at St. Jude Children’s Research Hospital. Association of Pediatric Hematology Oncology Nurses. 2024. Salt Lake City, UT.
Woodruff, C. Role Assignment in the Ambulatory Care Unit Weekend Clinic at St. Jude Children’s Research Hospital. Association of Pediatric Hematology Oncology Nurses. 2024. Salt Lake City, UT.
Wright D, Edwards C, McElroy L. Professional Achievements & Advancements Council. St. Jude Children’s Research Hospital: Shared Governance Fair 2024. Memphis, TN.