* Correspondence:sisitha.jayasinghe@utas.edu.au;Tel.:+61-3-6324-3147
Despiteincreasedawarenessoftherisksofobesity,progressinpreventioninthepast 20yearshasbeenpatchyatbest[1].Toplacethescaleoftheobesityproblemincontext, itisestimatedthataround2.8%ofglobalGDP(~USD2trillion)iswastedonobesity andassociatedhealthcomplications[2].Asillustratedincomprehensivemodelssuchas Foresight[3],themultifariousandcomplexnatureofobesityetiologyiswidelyaccepted[4]. Traditionalinterventionistapproaches,predominantlybasedonthelinearmodelofcause andeffect,havepreoccupiedobesity-preventioneffortsformuchofthelate1990sand early2000s,withmanynowbeingoutdatedorobsolete.Accordingly,therehasbeena burgeoninginterestinwhole-systemsapproaches(WSAs)thatacknowledgethecomplex, dynamicnatureofoverweightandobesityandoperateacrossmultiplelevelsofsociety (individuals,communities,governments,healthsystems,etc.)[5].
Publisher’sNote: MDPIstaysneutral withregardtojurisdictionalclaimsin publishedmapsandinstitutionalaffiliations.
Unfortunately,thesustainabilityandeffectivenessofpreventativeinterventionshave commonlybeenhamperedbytheirrelativelynarrowfocusondeliveringa“package”of activitiesand/oreducationalmessages[6].Well-planned,well-resourcedandoptimally implementedWSAsprovidealogicalalternative.Communityengagement,program design/planning,evaluation,sustainableimplementation,andgovernancearereportedas “bestpracticeprinciples”ineffective/optimalcommunity-basedpreventioninitiatives[7].
Published:2September2022
Abstract: Despiteincreasedawarenessofitsrisks,forthemostpart,contemporaryeffortsforobesity preventionhavebeenpatchyatbest.Assuch,theburgeoninginterestinwhole-systemsapproaches (WSAs)thatacknowledgethecomplex,dynamicnatureofoverweightandobesityandoperate acrossmultiplelevelsofsocietyisparticularlytimely.Manycomponentsof“communitycapacity building”(CB),anessentialbutoftenneglectedaspectofobesityprevention,overlapwith“best practiceprinciples”ineffective/optimalcommunity-basedobesity-preventioninitiatives.Rhetoric urgingWSAsandcommunityCBinpublichealthaboundsalthoughoperativeandefficacious contemporaryexamplesoftheseapproachestoreducingobesitylevelsarescarce.Theaimofthis investigationwastoundertakeasystematizedreviewofthelevelofcapacitybuildingincorporated inpublishedliteratureonWSAstargetingobesitytobetterunderstandhowdomainsofCBhavebeen incorporated.A PubMed searchandarecentlypublishedsystematicreviewwereutilizedtoidentify WSAstoobesitypreventionbetween1995–2020.Ateam-basedapproachtoqualitativethematic dataanalysiswasusedtosystematicallyassessanddescribeeachinterventionregardingexplicit capacity-buildingpractice.Despitenotbeingspecificallydesignedforbuildingcapacity,asignificant proportionoftheWSAsstudiedinthecurrentreporthadimplementedseveralCBdomains.
Keywords: whole-systemsapproach;prevention;capacitybuilding;overweightandobesity; communityintervention
Copyright: ©2022bytheauthors. LicenseeMDPI,Basel,Switzerland. Thisarticleisanopenaccessarticle distributedunderthetermsand conditionsoftheCreativeCommons Attribution(CCBY)license(https:// creativecommons.org/licenses/by/ 4.0/).
International Journal of Environmental Research and Public Health Article
1.Introduction
Int.J.Environ.Res.PublicHealth 2022, 19,10997. https://doi.org/10.3390/ijerph191710997 https://www.mdpi.com/journal/ijerph
SisithaJayasinghe 1,*,RobertSoward 1,LisaDalton 1,TimothyP.Holloway 1,SandraMurray 1 , KiraA.E.Patterson 2,KiranD.K.Ahuja 1 ,RogerHughes 3 ,NualaM.Byrne 1 andAndrewP.Hills 1
2 CollegeofArts,LawandEducation,UniversityofTasmania,Launceston,TAS7250,Australia
Citation: Jayasinghe,S.;Soward,R.; Dalton,L.;Holloway,T.P.;Murray,S.; Patterson,K.A.E.;Ahuja,K.D.K.; Hughes,R.;Byrne,N.M.;Hills,A.P. DomainsofCapacityBuildingin Whole-SystemsApproachesto PreventObesity—A“Systematized” Review. Int.J.Environ.Res.Public Health 2022, 19,10997. https:// doi.org/10.3390/ijerph191710997
AcademicEditor:PaulB.Tchounwou
Accepted:31August2022
DomainsofCapacityBuildinginWhole-SystemsApproaches toPreventObesity—A“Systematized”Review
1 CollegeofHealthandMedicine,UniversityofTasmania,Launceston,TAS7250,Australia
3 SchoolofHealthSciences,SwinburneUniversityofTechnology,Melbourne,VIC3122,Australia
Received:27July2022
Int.J.Environ.Res.PublicHealth 2022, 19,10997 2of17
2.MaterialsandMethods 2.1.SearchStrategy
Interestingly,manyoftheseitemsarealsocomponentsof“communitycapacitybuilding”, anessentialbutoftenneglectedaspectofobesityprevention.Asisoftenthecaseinarange ofareas,theconceptofcapacitybuildinghasbeeninconsistentlydefined,andthishas resultedinthegenerationofaraftofdefinitionsovertheyears[8,9].Capacitybuilding(CB) isanincreasinglyimportantstrategyforcommunitiestopromotesecurity,development, andsustainability.Itencompassesabroadrangeofactivitiesthataimtostrengthenthe abilityofpeopletomanagetheirownchallengesandtoachievedevelopmentobjectivesin thecontextofsustainability.CBassumesthatlocalactorsarebestsituatedtounderstand andthereforeaddresstheirowncommunitychallenges,andassistingthemismorelikely toleadtoeffective,legitimate,andsustainableoutcomes.Inthisvein,CB,theorizedasa problem-solvingendeavor[10],isnowrecognizedasanalternativetotheambitiousand expensiveliberalinterventionismthatwaspopularduringthe1990sand2000s[11].CB isthereforeemergingasaneffectiveavenueforcommunitiestotakeownershipofissues withanopportunitytouseexistingcapabilitieswithinindividuals,organizations,and systemstomakeprogress.TheWorldHealthOrganization(WHO)hasdefinedcapacity buildingas“thedevelopmentofknowledge,skills,commitment,structures,systems, andleadershiptoenableeffectivehealthpromotionwithactionstoimprovehealthat 3levels: theadvancementofknowledgeandskillsamongpractitioners;theexpansionof supportandinfrastructureforhealthpromotioninorganizations,and;thedevelopmentof cohesivenessandpartnershipsforhealthincommunities”[12,13].
RhetoricurgingWSAsandcommunitycapacitybuildinginpublichealthabounds althoughoperativeandefficaciouscontemporaryexamplesoftheseapproachestoreducing obesitylevelsarescarce[4,14].Numerouspastexamplesrelatedtopublichealthemergenciesofglobalsignificance(suchastobaccosmoking,HIV,diabetes,etc.)haveillustrated howWSAscanbeeffectivelyutilizedtoachievepositivehealthoutcomes[15 18].Tothe bestofourknowledge,nopreviousresearchhasspecificallyinvestigatedCBwithinWSAs topreventobesity.Theaimofthisinvestigationwastoundertakeasystematizedreview ofthelevelofcapacitybuildingincorporatedinpublishedliteratureonWSAstargeting obesitytobetterunderstandhowdomainsofCBhavebeenincorporated.
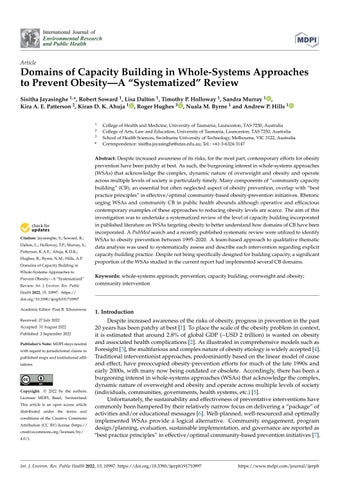
Twomainstrategieswereutilizedtoidentifywhole-systemapproaches(WSAs)to obesitypreventionbetween1995–2020.First,arecentsystematicreviewbyBagnalland colleagues[5]wasutilizedtoidentifyobesity-prevention-specificWSAsbetween1995 and2018.BagnallandcolleaguesdefinedWSAsasthosethat(1)consider,inconcert,the multifactorialdriversofoverweightandobesity;(2)involvetransformativecoordinated action(includingpolicies,strategies,andpractices)acrossabroadrangeofdisciplinesand stakeholders,includingpartnersoutsidetraditionalhealthsectors;(3)operateacrossall levelsofgovernance,includingthelocallevel,sothatsuchapproachesarereinforcedand sustained,and;(4)identifyandtargetopportunitiesthroughoutthelifecourse(frominfancy tooldage).Asubsequent Medline databasesearchwasconducted(April2020)tosource informationpertinenttootherWSAstoobesitypreventionfrom2018–2020(Figure 1).Key searchtermsincluded“obesityprevention”and“wholesystemsapproach”,andthesewere usedindividuallyandincombination.Allinterventionswerescreenedforappropriateness usingthecriterialistedinBagnalletal.[5]andtheNationalInstituteforHealthandCare Excellence(NICE)guidelinesforWSAs[19].Briefly,theexistenceofmultiple“features”, includingidentificationofasystem,capacitybuilding,creativity/innovation,relationships, engagement,communication,embeddedaction/policies,sustainability,leadership,and progressmonitoring,wasevaluatedtoascertaineligibility.Allstudiesthatdidnothavea focusonobesitypreventionordidnotsatisfytheWSAcriteriawerepromptlyexcluded. Asinterventionswerenotscreenedbasedonstudydesign,awidearrayofexperimental designswasincorporatedinthefinalanalysis.Theseincludedmixed-methodsevaluations,
Interventions identified through Bagnall et al (n = 22)
Identification
Figure1. Summaryofstudyselection.
2.2.CapacityBuildingAnalysis
Additional records identified through Medline search (n = 8)
Ateam-basedapproachtoqualitativethematicdataanalysiswasusedtomanagethe analyticalworkload.Eachoftheinterventionswasinitiallyanalyzedusinganin-house capacity-buildingassessmentmodeldevelopedbyoneoftheinvestigators(RH)[20].A frameworkof7domains(leadership,intelligence,partnerships,workforce,community, projectmanagement,andresourcemobilization)wasutilizedtosystematicallyassessand describeeachinterventionregardingexplicitcapacity-buildingpractice.Thecapacity domainswereextractedfromaDelphistudythatinvestigatedthecontentvalidityof capacitybuildingconceptualframeworkoriginallyproposedbyBaillieandcolleagues[21]. Focusquestionswereutilizedtoelicitpertinentinformationagainstthe7CBdomains (Table 1).Interventionsweregivenaqualityratingforeachofthedomainsbasedonthe levelofevidenceavailable(i.e.,1=littleevidenceofexplicitreference/strategy;2=some evidence;3=considerableevidence),andafinalcapacity-buildingscoreoutofamaximum of21wasderived.Subsequently,adescriptivethematicsummaryaboutcapacitybuilding wasgeneratedforeachintervention.TheCBanalysiswasperformedby3independent investigators,andthefinaltriangulatedresultsarepresentedinthisreport.Majority consensusandstabilityconsensuswerebothutilized[22]asameansofreachingagreement betweeninvestigators.
randomizedcontrolledtrials,non-randomizedcontrolledtrials,qualitativeorcasestudies, cross-sectionalstudies,naturalexperiments,andprospectivecohortstudies. ability, leadership, and progress monitoring, was evaluated to ascertain eligibility. studies that did not have a focus on obesity prevention or did not satisfy the WSA were promptly excluded. As interventions were not screened based on study design, wide array of experimental designs was incorporated in the final analysis. These included mixed-methods evaluations, randomized controlled trials, non-randomized controlled trials, qualitative or case studies, cross-sectional studies, natural experiments, and spective cohort studies.
2.2. Capacity Building Analysis
Interventionsexcluded(n=4)
Int.J.Environ.Res.PublicHealth 2022, 19,10997 3of17
Interventions included in the final analysis (n =26)
novation, relationships, engagement, communication, embedded action/policies,
A team-based approach to qualitative thematic data analysis was used to manage analytical workload. Each of the interventions was initially analyzed using an in-house capacity-building assessment model developed by one of the investigators (RH) framework of 7 domains (leadership, intelligence, partnerships, workforce, community, project management, and resource mobilization) was utilized to systematically assess describe each intervention regarding explicit capacity-building practice. The capacity mains were extracted from a Delphi study that investigated the content validity of ity building conceptual framework originally proposed by Baillie and colleagues cus questions were utilized to elicit pertinent information against the 7 CB domains 1). Interventions were given a quality rating for each of the domains based on the evidence available (i.e., 1 = little evidence of explicit reference/strategy; 2 = some evidence; 3 = considerable evidence), and a final capacity-building score out of a maximum was derived. Subsequently, a descriptive thematic summary about capacity building generated for each intervention. The CB analysis was performed by 3 independent tigators, and the final triangulated results are presented in this report. Majority consensus and stability consensus were both utilized [22] as a means of reaching agreement investigators.
Screening Included Eligibility
Figure 1. Summary of study selection.
Interventions screened (n = 30)
Intelligence
Community
• Evaluabilityassessment?
• Communityinvolvedinneedsidentification?
• Targetpopulationinvolvedinidentifyingissues/solutions?
• Stakeholdersengagedininterventionmanagementanddecisionmaking?
Table1. Focusquestionsforthedomainsofcapacitybuilding.
Project Management
• Interventionevaluation?
• Workforcedevelopmentstrategy?(training,CPD,upskilling?)
• Communityinvestingresourcestoaddressissue?
• Strategiestobuildpartnerships?
• Specificworkforceidentification?
• Sizeofinterventioninvestment(estimate:small(USD50K),medium (<USD250,000),large(>USD500,000)
Leadership
• Evaluationofpartnerships?
Partnerships
• Partnershipstoaddresstheissue?
• Communitydevelopmentstrategiesexplicitlydescribed?
• Interventiongoalsandobjectivescoherent(SMART)
Twenty-seveninstancesofWSAstoobesitypreventionwereselectedandincluded inthefinalanalysis(Figure 1,Table 2).Threeinterventionsthatdidnotmeettheinclusioncriteriawerepromptlyexcluded.Selectedinterventionswerefromfourgeographical regions,withthemajoritybasedintheUnitedStatesofAmerica(Table 2).Mostofthese interventionsfocusedonchildhoodobesityprevention,withasmallnumberinvestigating maternalobesityandobesityassociatedchronicdisease(Table 2).Similarly,mostofthe interventions(n=15)wereclusteredatthetopend(i.e.,>17)ofthecapacity-buildingscore spectrum—only2interventionsscored ≤8.Inmostinstances,therewasconsiderableevidenceonsubstantialcommunityengagementandintelligencegathering,whereasexplicit detailonleadershipandresourcemobilizationwerescarce(Figure 2).
• Communityinvolvedinstrategydecisionmaking?
• Typesofresourcesmobilized?
• Implementationmonitoring?
• Problemanalysisclear?
Capacity Domain FocusQuestions Evidenceof:
• Specificanalysistoinforminterventiondesign?
• Specificattemptstomobilizeresourcesexternaltoimmediateproject funding?
• Leadershipdevelopmentstrategy?
Resource Mobilization
3.Results
• Needsassessmentconducted?
Int.J.Environ.Res.PublicHealth 2022, 19,10997 4of17
ThecapacitydomainsutilizedinthecurrentinstancewereextractedfromaDelphistudy[20]thatinvestigatedthecontent validityofacapacity-buildingconceptualframeworkoriginallyproposedbyBaillieandcolleagues[21].Thepotential influenceofthesecapacitydomainsoninterventionoutcomesmayvarydependingonthecontext.Aswithmanyother “complexconcepts/systems”inpublichealth,capacitybuildingcancontainmanyheterogeneousandfleetingelements;an emergentcollectiveeffectthatisdifferentfromtheanyinfluenceoftheoriginalcomponentsbythemselves;andcomponents thataresubjecttochangingcircumstances.
Workforce
• Referencetoleadership(political,organizational,community,workforce)?
1 3 1 1 3 3 1 13
Australia
ProjectManagement ResourceMobilization
1 3 2 3 3 3 2 17
Campbelltown—ChangingOurFuture: Thefive-stepapproach:(1)setupachildhood obesity-monitoringsystembycollectingbaselinedatafromchildreninprimaryschoolsacross CampbelltownLGAtogivealocalcontexttothecommunitywhendevelopingthesystemsmap;(2) keystakeholdersdevelopsystemsmapsthatinformthedevelopmentoftheinterventions;(3)key stakeholdersandcommunitygroupsidentifypriorityareasforactionandformworkinggroups;(4) implementationoftheinterventions;(5)evaluationoftheinterventions,entailingseveralimportant domainsofCB[30].
Romp&Chomp: Theinterventionactivitieshadastrongfocusoncommunitycapacitybuilding anddevelopingsustainablechangesinareasofpolicy,sociocultural,andphysicalenvironmentsby usingasocioecologicalframework.TheRomp&Chompactionplanwasdevelopedwithextensive communityconsultationandstakeholderengagement,andamanagementcommitteeof stakeholdersoversawitsimplementation[23 26].
StudyRegion
Table2. Capacity-buildinginterventions.
StudyDescription/SummaryofCapacity-BuildingEvidence
2 3 3 2 3 3 1 17
Int.J.Environ.Res.PublicHealth 2022, 19,10997 5of17
Workforce
SustainableEatingActivityChangePortland: Thisinterventionutilizedasset-basedcommunity development(ABCD)—astrategypromotingsustainablecommunitydevelopment—alongside applicationsofacollectiveimpactframeworkthatfocusedoneffortstoconnectandmobilizethe communitytoact[31].
1 3 1 1 3 3 1 13
WHOStopsChildhoodObesity: Intensivetrainingandsupportwithineachcommunitywas orientedaroundstrengtheningWHOsystemsbuildingblocks(e.g.,workforcedevelopment, resourcesintelligence)andtheNewSouthWalescapacity-buildingframework(e.g.,partnersand networks)incommunitysettings.Akeyfocusincludedmappingexistingsystemsandusingthese mapstodevelopandimplementwhole-systemschangewithcommunitymembersand implementationsupporttooptimizeinterventions[32].
BeActiveEatWell: Buildingcapacitywasoneofthekeyfociofthisintervention(Objective1outof 10).Itincludedbroadactionsaroundgovernance,partnerships,coordination,training,andresource allocation[27 29]. 2 3 2 3 3 3 3 19
Leadership Intelligence Partnerships Community Capacity-BuildingScore
1 3 2 2 3 2 2 15
ChildhoodObesityPreventionDemonstrationProject: Thisincludedanimplementationof numerousmulti-level,multi-settinginterventionsforpreventingandreducingobesityamong childreninacommunity,whichforthemostpartranasacollaborationbetweengovernment-and community-levelstakeholders.Aspecificfocusincludedtheapplicationoflessonslearned (regardingobesityprevention)fromothergeographicalregions[37].
Leadership Intelligence Partnerships Workforce Community ProjectManagement ResourceMobilization Capacity-BuildingScore
StudyDescription/SummaryofCapacity-BuildingEvidence
2 3 3 3 3 3 3 20
UnitedStates
TheSanDiegoHealthyWeightCollaborative: JointlyimplementedstrategiesinaLatino, underservedcommunityincluded:(1)buildinganeffectiveandsustainablecollaborativeteam;(2) disseminatingahealthyweightmessageacrosssectors;(3)assessingweightstatusandhealthy weightplansinprimarycare,school,andearlychildhoodsettings;and(4)implementingpolicy changestosupporthealthyeatingandphysicalactivity[38].
Table2. Cont.
HealthyLivingCambridgeKids: Acommunity-basedparticipatoryresearchapproach(i.e.,The HealthyChildrenTaskForce(TaskForce)wasutilizedtoengagecommunitymembersinallaspects oftheinterventionprocessfromresearchquestionstodesign/implementationofthestudyand analysis/disseminationoffindings[36].
StudyRegion
Int.J.Environ.Res.PublicHealth 2022, 19,10997 6of17
It’sYourMove—ACT: Capacitybuildingamongschoolprojectofficersandstudentambassadors (workshopandtrainingopportunities)wasaprimarygoal.TheAnalysesGridforEnvironments LinkedtoObesity(ANGELO)frameworkwasmodifiedtoincorporatetheWorldHealth Organizationsystemsbuildingblocks,whichincludeleadership,information,financing/resources, partnerships,andworkforcedevelopment,intothedevelopmentandimplementationoftheproject toreduceunhealthyweightgainamongadolescentsthroughcomprehensiveschool-and community-basedsystemschange[23,33 35].
3 2 2 18
3 3 3 2
1 1 3 3 1 2 3 14
StudyDescription/SummaryofCapacity-BuildingEvidence
1 3 3 2 3 3 1 16
HealthyStartPartnership: Effortsweremadetobetterunderstandthechallengesfacedbypublic healthprofessionalsinimplementingenvironmentalandpolicyinterventionsrelatedtopublic healththrough(1)participantobservationofregional-andcounty-levelmeetingsandconference calls;(2)qualitativeinterviewswithHSPpartners;and(3)self-administeredstructured questionnaireswithHSPpartners[40].
Int.J.Environ.Res.PublicHealth 2022, 19,10997 7of17
Cont. StudyRegion
1 2 3 2 2 2 1 13
HealthyEatingandExercisingtoReduceDiabetes: Acommunity-basedparticipatory interventionwasimplementedtoidentifyfacilitatorsofandbarrierstosustainedcommunityefforts toaddresssocialfactorsthatcontributetodiabetes(andhealth).Aconcertedeffortwasputinto identifyproximate(e.g.,knowledge,diet)andintermediate(e.g.,accesstofreshproduce)factors thatcontributedexistinghealthtrends.Educationandcommunitytrainingsessionswereconducted throughthemediationofthesteeringcommittee.Further,partnershipbuildingandsourcing additionalfundswasactivelyaddressedthroughoutthelifetimeofthestudy[41].
ShapeUpSomerville: Acommunity-basedparticipatoryresearchapproachwasimplementedthat focusedonfacilitatingcollaborativepartnershipswiththecommunitiesinallphasesoftheresearch: identifyingtheproblem;designing,implementing,andevaluatingtheintervention;andidentifying howdatawouldinformactionstoimprovehealthwithinthecommunity.Communityengagement consistedofseveralforms,includingmeetings,focusgroups,andkeyinformantinterviews,andled totheformationofseveralShapeUpSummervilleadvisorycouncilsthatremainedactively involvedthroughoutthestudy[39].
2 3 2 3 2 2 2 16
Leadership Intelligence Partnerships Workforce Community ProjectManagement ResourceMobilization Capacity-BuildingScore
Table2.
1 3 2 2 2 2 1 13
Int.J.Environ.Res.PublicHealth 2022, 19,10997 8of17
Cont. StudyRegion
HealthyEating,ActiveCommunitiesProgram: Changesinfoodsandbeveragessoldatschools andinneighborhoods;changesinschoolandafter-schoolphysicalactivityprogrammingand equipment;individual-levelchangesinchildren’sattitudesandbehaviorsrelatedtofoodand physicalactivity;andHEAC-relatedawarenessandengagementonthepartofcommunity members,stakeholders,andpolicymakerswereachievedthrough:(1)Engagingparentsand familiesasadvocatesforhealthierfoodandphysicalactivity;(2)developingpolicyadvocacy capacityinresidents;(3)committinghealthcarespokespersonstotestifyingatschoolboard meetings,planningcommissionmeetings,andcitycouncilmeetings,and(4)educatingparentson howsomebusinessesmarketunhealthyfoodandphysicalactivitytochildren[42].
BaltimoreHealthyCommunitiesforKids: Amixtureofpolicyworkinggroups,systemsscience modelling,regularmeetingswithkeystakeholdergroups,trainings(inpersonandonline)offood sourceownersandyouthleaders,andsocialmediacampaignswereutilizedtoincrease affordability,availability,purchase,andconsumptionofhealthyfoodsbylow-incomeAfrican Americanchildrenandreduceobesity[43].
3 3 2 3 3 3 1 18
CentralCaliforniaRegionalObesityPreventionProgram: Promotingofsafeplacesforphysical activity,increasedaccesstofreshfruitsandvegetables,andsupportingthecommunityandyouth engagementinlocalandregionaleffortstochangenutritionandphysicalactivityenvironmentsfor obesitypreventionwasundertakenusingaregionallylocalized/focusedworkforcedevelopment, communityengagement,andpolicychangeapproach[45].
Table2.
ShapeUpUnder5: Stakeholder-drivencommunitydiffusion—anovelconceptualframework whichentailsmanydomainsofcapacitybuilding—wasimplementedtobetterunderstandhowand whystakeholdergroupssucceedandtheconditionsunderwhichtheycreatecommunity-wide changeinthecontextofchildhoodobesity[44].
StudyDescription/SummaryofCapacity-BuildingEvidence
2 3 2 3 3 2 18
3
Leadership Intelligence Partnerships Workforce Community ProjectManagement ResourceMobilization Capacity-BuildingScore
2 3 3 3 3 3 1 18
Int.J.Environ.Res.PublicHealth 2022, 19,10997 9of17
1 3 3 3 3 3 1 17
Leadership Intelligence Partnerships Workforce Community ProjectManagement ResourceMobilization Capacity-BuildingScore
CaliforniaHealthyCitiesandCommunities: Numerousnewhealthandwell-beingprograms weredeveloped,organizationalpoliciesandpracticesadopted,andnewfinancialresources leveragedacross20participatingsitesthroughorganizationaldevelopment(citygovernments,lead agenciesandcommunityorganizations),enhancingleadershipskillsamongcommunityresidents, strengtheningrelationshipsamongneighbors,andprovidingopportunitiesforresidentstoget involvedintheciviclifeoftheircommunities[46 48].
Children’sHealthyLiving: ChildhoodobesityamongPacificchildrenwasinvestigatedusing multipleapproachesincluding(1)program/datainventoriesandsituationalanalyses;(2)trainingof professionalsandparaprofessionalsinobesityprevention;(3)developmentofaPacificfood, nutrition,andphysicalactivitydatamanagementandevaluationsystem;(4)developmentand conductofacommunity-basedenvironmentalinterventiontoprevent,maintain,orreduceyoung childoverweightandobesity;(5)evaluationoftheenvironmentalintervention;and(6)incurringat leastoneobesity-preventionpolicychangeperjurisdiction[43,49,50].
StudyDescription/SummaryofCapacity-BuildingEvidence
2 2 3 2 3 2 3 17
Cont. StudyRegion
Pacific
Canada
HealthyFoodNorth: Attemptstoincreaseconsumptionoftraditionalfoods(e.g.,caribou,fish)and nutrient-dense,store-boughtfoodslowinfatandsugar(e.g.,fruits,vegetables);decrease consumptionofnon-nutrient-dense,high-fat,high-sugarfoods(e.g.,soda,chips);andincrease engagementinmoderateandvigorousphysicalactivitywhilereducingsedentaryactivitywere madeincludingpromotionalmaterials,media,andinteractiveeducationalactivitiesheldinfood shops,worksites,andothercommunityvenuesaswellascommunity-wideevents[51].
1 3 3 3 3 3 1 17
Table2.
HealthyAlbertaCommunities: Attemptsat:(1)reducingprevalenceofoverweightandchronic diseaserisk,(2)increasingcommunitycapacitytopromotehealth,and(3)informingpolicy,practice, andresearchdecisionsaboutpublichealthweremadethroughamultitudeofphysicalactivityand nutritioninterventionapproachesthatwerebuiltuponthepremiseofcommunity-based participatoryresearch[52,53].
3 3 3 3 3 3 3 21
1 3 1 3 2 2 1 13
Workforce Community ProjectManagement ResourceMobilization Capacity-BuildingScore
UnitedKingdomandEurope
1 1 1 1 1 1 1 7
1 1 2 1 1 1 1 8
SundhedogLokalsamfund: PromotionofhealthierlifestylesamongDanishchildrenaged3–8 yearsandtheirfamilieswasachievedthroughcollaboratingwiththelocaleducationalprogramsfor nurses,school,andkindergartenandbyplanningforatrainingofprogramambassadorsamongthe localworkforces[43,62,63].
Int.J.Environ.Res.PublicHealth 2022, 19,10997 10of17
StudyDescription/SummaryofCapacity-BuildingEvidence
2 3 3 2 3 3 1 17
HealthyLifestyleProgram: Asystematicprocess—InterventionMapping(IM)—wasappliedto planaschool-basedobesity-preventionintervention.Severaldomainsofcapacitybuilding, includingneedsassessments,intelligencegathering,andstakeholderconsultations,wereincluded inthisprocess[60,61].
HealthytownsEngland: Morethan200individualinterventions,primarilyfocusedonpromoting healthydietandphysicalactivity,wereimplementedwithnoreferencetocommunitycapacity building[57,58].
Table2. Cont.
Leadership Intelligence Partnerships
SustainableChildhoodObesityPreventionthroughCommunityEngagement(SCOPE): A multi-setting,multi-componentprogramdesignedtoenhancecommunitycapacitytocreateand deliversolutionstopromotehealthyeating,physicalactivity,andhealthyweightsamong school-agedchildrenwasimplemented.Underpinnedbysocialecologicaltheory,community-based andcommunity-drivenactionfacilitatedbythebestevidenceandsharedstrategiesacrossmultiple stakeholderswasutilizedtopromotehealthybodyweights[54 56].
NeighbourhoodRenewalFund—ObesityPrevention: Aseriesofinterventionsaimedat changingnutritionandphysicalactivitybehaviorsinthelocalcommunitywasimplemented withoutanynotableemphasisoncapacitybuilding[59].
StudyRegion
2 3 3 3 3 3 1 18
Int.J.Environ.Res.PublicHealth 2022, 19,10997 11of17
Table2. Cont.
StudyRegion
StudyDescription/SummaryofCapacity-BuildingEvidence
Leadership Intelligence Partnerships Workforce Community ProjectManagement ResourceMobilization Capacity-BuildingScore
EnsemblePrévenonsl’Obésité desEnfants: Acoordinated,capacity-buildingapproachaimedat reducingchildhoodobesitywasimplementedthroughtheengagementoflocalenvironments, childhoodsettings,andfamilynorms.Specificemphasisonminimizingculturalorsocietal stigmatization,step-by-steplearning,andanexperienceofhealthylifestylehabitstailoredtothe needsofallsocioeconomicgroupswasincludedwithallobjectivesbasedaround(1)political commitmentandpolicychange;(2)securingsufficientfiscalandphysicalresources;(3)planning, coordinating,andprovidingthesocialmarketing,communication,andsupportservicesfor communitypractitionersandleaders;and(4)usingevidencefromawidevarietyofsources[64 66]. 1 3 2 2 3 3 3 17
1=littleevidenceofexplicitreference/strategy;2=someevidence;3=considerableevidence.Cronbach’salpha=0.77.
Theideaofanuancedand/orcomprehensiveunderstandingofCBasapublichealth strategyshouldbeentertained,andtheroutineincorporationofcomponentsofCBinto publicheathinterventiondesignshouldbeactivelyencouraged.
4.Conclusions
ThepresentstudyassessedtheextenttowhichcomponentsofCBareingrainedwithin thedesignsofkeyWSAstoobesitypreventionfromtherecentpast.Asystemusually containsmanycomponentpartsthatareinaperpetuallydynamicinteraction.Hence,the hallmarkofasystemisthatnoneofitspartsiscompletelyindependent[67].Tothisend, practicabilityofWSAstoobesitypreventioncanbeextremelycomplicated.Therefore,itis feasibleneithertohaveanoverarchingworkingmodelofCBthatwillbeunequivocally effectiveinawiderangeofsettingsnortoexpectvariousWSAstohaveimplemented thedifferentdomainsofCBtothesameextent.However,despitenotbeingexplicitly designedforbuildingcapacity,asignificantproportionoftheWSAsstudiedinthecurrent reporthadimplementedseveralCBdomains,whichispromising.Thisimpliesthatobesity preventionandCBarenotmutuallyexclusiveandthatWSAapproachesmustincludeas manydomainsofCBaspossibleintheirdesign/implementationapproaches.Thisalso negatesthetypicalnotionthatCBshouldbeandisasubconscious,invisiblepractice[68].
4. Conclusions
Int.J.Environ.Res.PublicHealth 2022, 19,10997 12of17 Int. J. Environ. Res. Public Health 2022, 19, x 11 of 16
Figure 2. Levels of evidence pertaining to capacity building domains.
Thelackofexplicitevidenceofreferenceand/orstrategyregardingleadershipand resourcemanagementwasofparticularconcern.“Leadership”isavitalcomponentthat playsamajorroleinseveralaspectsofanyWSAtoobesityprevention,includingadoptionoftheintervention,implementation,evaluation,anddisseminationofthefindings.
Traditionally,leadershiphasbeenlinkedwithinfluenceandpowerandhasoftenbeen associatedwithindividuals,agencies,organizationsthathavetheknowledge,control,and responsibilitytochangeenvironments,policies,andpracticesrelatedtoobesity.However, ifwedrawonFoucault’s(1991)argumentthat“poweriseverywhere”,wecandepart fromtheassumptionthatonlyparticularactorsusepowerasaninstrumentofcoercionor influenceandevenawayfromthediscreetstructuresinwhichthoseactorsoperate.Instead, werecognizethatpowerisdiffusedandembodiedindiscourseandknowledge[69,70].By doingso,weacknowledgethatthereisaconsiderabledegreeofvariabilityinwhoand/or whatcanbeconsidereda“leader”inthecontemporaryobesity-preventionlandscape.To thisend,currentliteratureisrepletewithexamplesoftheimportanceof“moversand shakers”ofthecommunity,i.e.,“communitychampions”,intheefficaciousimplementationofWSAstopreventobesity[71 75].Thisindicatesthatadiverserangeofformal andinformalinfluencersandrolemodelscanfulfilltheleadershipthatisrequiredin
The lack of explicit evidence of reference and/or strategy regarding leadership and resource management was of particular concern. “Leadership” is a vital component that plays a major role in several aspects of any WSA to obesity prevention, including adoption of the intervention, implementation, evaluation, and dissemination of the findings. Traditionally, leadership has been linked with influence and power and has often been associated with individuals, agencies, organizations that have the knowledge, control, and responsibility to change environments, policies, and practices related to obesity. However, if we draw on Foucault’s (1991) argument that “power is everywhere”, we can depart from the assumption that only particular actors use power as an instrument of coercion or influence and even away from the discreet structures in which those actors operate. Instead, we recognize that power is diffused and embodied in discourse and knowledge [69,70]. By doing so, we acknowledge that there is a considerable degree of variability in who and/or what can be considered a “leader” in the contemporary obesity-prevention landscape. To this end, current literature is replete with examples of the importance of “movers and shakers” of the community, i.e., “community champions”, in the efficacious implementation of WSAs to prevent obesity [71–75]. This indicates that a diverse range of
Figure2. Levelsofevidencepertainingtocapacitybuildingdomains.
The present study assessed the extent to which components of CB are ingrained within the designs of key WSAs to obesity prevention from the recent past. A system usually contains many component parts that are in a perpetually dynamic interaction. Hence, the hallmark of a system is that none of its parts is completely independent [67]. To this end, practicability of WSAs to obesity prevention can be extremely complicated. Therefore, it is feasible neither to have an overarching working model of CB that will be unequivocally effective in a wide range of settings nor to expect various WSAs to have implemented the different domains of CB to the same extent. However, despite not being explicitly designed for building capacity, a significant proportion of the WSAs studied in the current report had implemented several CB domains, which is promising. This implies that obesity prevention and CB are not mutually exclusive and that WSA approaches must include as many domains of CB as possible in their design/implementation approaches. This also negates the typical notion that CB should be and is a subconscious, invisible practice [68]. The idea of a nuanced and/or comprehensive understanding of CB as a public health strategy should be entertained, and the routine incorporation of components of CB into public heath intervention design should be actively encouraged.
InstitutionalReviewBoardStatement: Notapplicable.
ConflictsofInterest: Theauthorsdeclarenoconflictofinterest.
Giventheenormityofthechallenge,theimportanceofresourcemobilizationinobesity preventioncannotbeunderestimated.Anyefficaciousattempttocurtailthecurrenttrends ofobesitywillundoubtedlyrequireavastamountofhuman,financial,andotherresources. Assuch,itisperplexingthatspecificstrategiesforresourcemobilizationandmanagement havenotbeenincludedinmanyoftheWSAsconsidered.Itisalsonoteworthythat effectiveresourcemanagementcanalsohaveasignificantimpactonthesustainabilityof obesity-preventionefforts[77].Forinstance,thereissubstantialevidencethatavailability offinancesandeffectivemanagementofsuchresourcescansingle-handedlydetermine thelongevityandscalabilityofmostobesity-preventionefforts[78].Accordingly,there isincreasinginterestbycontemporaryinterventionistsregardingnovel,cost-effective strategiesinimplementingWSAstoobesityprevention.Tothisend,asset-basedcommunity developmentapproaches,whichconsidersustainabilityasacoreaspectandactivelyseek outopportunitiestolinkextantmicro-assetstothemacro-environment,areastepinthe rightdirection.
Funding: ThisresearchwasfundedbyaNationalHealth&MedicalResearchCouncil(NHMRC) grant(#113672)aspartoftheCAPITOLProject.Thestudyfunderhadnoroleinstudydesign, collection,analysis,orinterpretationofthedata;inwritingthereport,orinthedecisiontosubmitthe articleforpublication.Thecontentsofthisarticlearetheresponsibilityoftheauthorsanddonot reflecttheviewsoftheNHMRC.
The“systematized”andconvenientnatureofthestudyselectionapproachimplementedinthecurrentstudycouldhavepotentiallyintroducedbiasandhumanerror,which mayhaveresultedinsomerelevantstudiesbeingmissed.Nevertheless,theapproach undertakenwasapragmaticnecessity.Italsonoteworthythatthesomeoftheincluded studiesdidnotentailCBasoneoftheirprimaryaims,whichmayhaveaffectedthelevel ofoverallidentifiableCBelements.Further,thegeneralizabilityofthefindingsmaybe limitedgiventhelackofWSAsfromsomegeographicalareas.Itiswell-knownthatobesity prevalencedisplaysheterogeneousepidemiologicalpatternsthatarenotreadilyexplained indivergentgeographicalsettings[79].Futureresearchmayalsobenefitfrominvestigating whetherthereisadose–responserelationshipbetweendomainsofCBimplementedand positiveresearchoutcomes.
InformedConsentStatement: Notapplicable.
DataAvailabilityStatement: Notapplicable.
community-basedobesityprevention.Ashasbeenpostulatedinnumeroustheoretical examples,differenttypesofleadersandleadershipstylesmaybepertinentinapublic healthcontext.However,giventhecentralityofcommunityparticipationandcoalition formationinWSAapproaches,itcouldbearguedthatademocraticand/oralaissez-faire typeofleadershipismostsuitableforeffectiveoutcomes[76].Theseleadershipapproaches lendthemselvestofacilitatingcapacitybuildingfromabottom-upapproachthatdraws onandstrengthensexistinglocalcapacitiesbyacknowledgingallstakeholdersascapable agents.
AuthorContributions: Conceptualization,S.J.,R.H.andA.P.H.;methodology,S.J.,K.A.E.P.,T.P.H., R.S.,K.D.K.A.,R.H.,N.M.B.,S.M.andL.D.;formalanalysis,S.J.andR.S.;investigation,S.J.andA.P.H.; resources,K.A.E.P.,K.D.K.A.,R.H.,N.M.B.,L.D.andA.P.H.;datacuration,S.J.;writing—original draftpreparation,S.J.;writing—reviewandediting,K.A.E.P.,T.P.H.,R.S.,K.D.K.A.,R.H.,N.M.B., S.M.,L.D.andA.P.H.;supervision,A.P.H.;projectadministration,R.H.,N.M.B.andA.P.H.;funding acquisition,K.A.E.P.,K.D.K.A.,R.H.,N.M.B.andA.P.H.Allauthorshavereadandagreedtothe publishedversionofthemanuscript.
Int.J.Environ.Res.PublicHealth 2022, 19,10997 13of17
4. Rutter,H.;Savona,N.;Glonti,K.;Bibby,J.;Cummins,S.;Finegood,D.T.;Greaves,F.;Harper,L.;Hawe,P.;Moore,L.Theneedfor acomplexsystemsmodelofevidenceforpublichealth. Lancet 2017, 390,2602–2604.[CrossRef]
12. Bergeron,K.;Abdi,S.;DeCorby,K.;Mensah,G.;Rempel,B.;Manson,H.Theories,modelsandframeworksusedincapacity buildinginterventionsrelevanttopublichealth:Asystematicreview. BMCPublicHealth 2017, 17,914.[CrossRef]
8. Goodman,R.M.;Speers,M.A.;McLeroy,K.;Fawcett,S.;Kegler,M.;Parker,E.;Smith,S.R.;Sterling,T.D.;Wallerstein,N. Identifyinganddefiningthedimensionsofcommunitycapacitytoprovideabasisformeasurement. HealthEduc.Behav. 1998, 25, 258–278.[CrossRef]
21. Baillie,E.;Bjarnholt,C.;Gruber,M.;Hughes,R.Acapacity-buildingconceptualframeworkforpublichealthnutritionpractice. PublicHealthNutr. 2009, 12,1031–1038.[CrossRef][PubMed]
11. Jackson,P.Securitysectorreformandstatebuilding. ThirdWorldQ. 2011, 32,1803–1822.[CrossRef]
14. Millar,L.;Robertson,N.;Allender,S.;Nichols,M.;Bennett,C.;Swinburn,B.Increasingcommunitycapacityanddecreasing prevalenceofoverweightandobesityinacommunitybasedinterventionamongAustralianadolescents. Prev.Med. 2013, 56, 379–384.[CrossRef][PubMed]
19. Garside,R.;Pearson,M.;Hunt,H.;Moxham,T.;Anderson,R. IdentifyingtheKeyElementsandInteractionsofaWholeSystem ApproachtoObesityPrevention;PeninsulaTechnologyAssessmentGroup(PenTAG):Exeter,UK,2010.
22. Rowe,G.;Wright,G.TheDelphitechniqueasaforecastingtool:Issuesandanalysis. Int.J.Forecast. 1999, 15,353–375.[CrossRef]
9. Traverso-Yepez,M.;Maddalena,V.;Bavington,W.;Donovan,C.Communitycapacitybuildingforhealth:Acriticallookatthe practicalimplicationsofthisapproach. SageOpen 2012, 2,2158244012446996.[CrossRef]
23. Bell,A.C.;Simmons,A.;Sanigorski,A.M.;Kremer,P.J.;Swinburn,B.A.Preventingchildhoodobesity:Thesentinelsiteforobesity preventioninVictoria,Australia. HealthPromot.Int. 2008, 23,328–336.[CrossRef]
24. deGroot,F.P.;Robertson,N.M.;Swinburn,B.A.;deSilva-Sanigorski,A.M.Increasingcommunitycapacitytopreventchildhood obesity:Challenges,lessonslearnedandresultsfromtheRomp&Chompintervention. BMCPublicHealth 2010, 10,522.
25. deSilva-Sanigorski,A.;Elea,D.;Bell,C.;Kremer,P.;Carpenter,L.;Nichols,M.;Smith,M.;Sharp,S.;Boak,R.;Swinburn,B. Obesitypreventioninthefamilydaycaresetting:ImpactoftheRomp&Chompinterventiononopportunitiesforchildren’s physicalactivityandhealthyeating. Child:CareHealthDev. 2011, 37,385–393.
26. deSilva-Sanigorski,A.M.;Bell,A.C.;Kremer,P.;Nichols,M.;Crellin,M.;Smith,M.;Sharp,S.;deGroot,F.;Carpenter,L.;Boak,R. Reducingobesityinearlychildhood:ResultsfromRomp&Chomp,anAustraliancommunity-wideinterventionprogram. Am.J. Clin.Nutr. 2010, 91,831–840.[PubMed]
20. Swanepoel,E.;Fox,A.;Hughes,R.Practitionerconsensusonthedeterminantsofcapacitybuildingpracticeinhigh-income countries. PublicHealthNutr. 2015, 18,1898–1905.[CrossRef][PubMed]
13. Smith,B.J.;Tang,K.C.;Nutbeam,D.WHOhealthpromotionglossary:Newterms. HealthPromot.Int. 2006, 21,340–345. [CrossRef]
3. Butland,B.;Jebb,S.;Kopelman,P.;McPherson,K.;Thomas,S.;Mardell,J.;Parry,V. TacklingObesities:FutureChoices-ProjectReport; Citeseer:ForestGrove,OR,USA,2007;Volume10.
1. Roberto,C.A.;Swinburn,B.;Hawkes,C.;Huang,T.T.;Costa,S.A.;Ashe,M.;Zwicker,L.;Cawley,J.H.;Brownell,K.D.Patchy progressonobesityprevention:Emergingexamples,entrenchedbarriers,andnewthinking. Lancet 2015, 385,2400–2409. [CrossRef]
18. Marcus,S.E.;Leischow,S.J.;Mabry,P.L.;Clark,P.I.Lessonslearnedfromtheapplicationofsystemssciencetotobaccocontrolat theNationalCancerInstitute. Am.J.PublicHealth 2010, 100,1163–1165.[CrossRef][PubMed]
Int.J.Environ.Res.PublicHealth 2022, 19,10997 14of17
References
2. Dobbs,R.;Sawers,C.;Thompson,F.;Manyika,J.;Woetzel,J.R.;Child,P.;McKenna,S.;Spatharou,A. OvercomingObesity:An InitialEconomicAnalysis;McKinseyGlobalInstitute:SanFrancisco,CA,USA,2014.
6. Hawe,P.;Shiell,A.;Riley,T.Theorisinginterventionsaseventsinsystems. Am.J.CommunityPsychol. 2009, 43,267–276.[CrossRef]
7. King,L.;Gill,T.;Allender,S.;Swinburn,B.Bestpracticeprinciplesforcommunity-basedobesityprevention:Development, contentandapplication. Obes.Rev. 2011, 12,329–338.[CrossRef][PubMed]
10. Denney,L.;Valters,C. EvidenceSynthesis:SecuritySectorReformandOrganisationalCapacityBuilding;DepartmentforInternational Development:London,UK,2015.
16. Leykum,L.K.;Pugh,J.;Lawrence,V.;Parchman,M.;Noël,P.H.;Cornell,J.;McDaniel,R.R.Organizationalinterventions employingprinciplesofcomplexitysciencehaveimprovedoutcomesforpatientswithTypeIIdiabetes. Implement.Sci. 2007, 2, 28.[CrossRef]
17. Lanham,H.J.;Leykum,L.K.;Taylor,B.S.;McCannon,C.J.;Lindberg,C.;Lester,R.T.Howcomplexitysciencecaninformscale-up andspreadinhealthcare:Understandingtheroleofself-organizationinvariationacrosslocalcontexts. Soc.Sci.Med. 2013, 93, 194–202.[CrossRef][PubMed]
5. Bagnall,A.-M.;Radley,D.;Jones,R.;Gately,P.;Nobles,J.;VanDijk,M.;Blackshaw,J.;Montel,S.;Sahota,P.Wholesystems approachestoobesityandothercomplexpublichealthchallenges:Asystematicreview. BMCPublicHealth 2019, 19,8.[CrossRef] [PubMed]
15. Wutzke,S.;Morrice,E.;Benton,M.;Wilson,A.Systemsapproachesforchronicdiseaseprevention:Soundlogicandempirical evidence,butisthisviewsharedoutsideofacademia? PublicHealthRes.Pract. 2016, 26,2631632.[CrossRef][PubMed]
43. Mikkelsen,B.E.;Novotny,R.;Gittelsohn,J.Multi-level,multi-componentapproachestocommunitybasedinterventionsfor healthyliving—Athreecasecomparison. Int.J.Environ.Res.PublicHealth 2016, 13,1023.[CrossRef]
45. Schwarte,L.;Samuels,S.E.;Capitman,J.;Ruwe,M.;Boyle,M.;Flores,G.TheCentralCaliforniaRegionalObesityPrevention Program:ChangingnutritionandphysicalactivityenvironmentsinCalifornia’sheartland. Am.J.PublicHealth 2010, 100, 2124–2128.[CrossRef][PubMed]
34. Mathews,L.B.;Moodie,M.M.;Simmons,A.M.;Swinburn,B.A.TheprocessevaluationofIt’sYourMove!,anAustralian adolescentcommunity-basedobesitypreventionproject. BMCPublicHealth 2010, 10,448.[CrossRef]
37. Cousins,J.M.;Langer,S.M.;Thomas,C.;Rhew,L.K.PeerReviewed:TheRoleofStateHealthDepartmentsinSupporting Community-basedObesityPrevention. Prev.ChronicDis. 2011, 8,A87.[PubMed]
Int.J.Environ.Res.PublicHealth 2022, 19,10997 15of17
31. Jenkins,E.;Lowe,J.;Allender,S.;Bolton,K.A.Processevaluationofawhole-of-communitysystemsapproachtoaddress childhoodobesityinwesternVictoria,Australia. BMCPublicHealth 2020, 20,450.[CrossRef]
47. Kegler,M.C.;Painter,J.E.;Twiss,J.M.;Aronson,R.;Norton,B.L.EvaluationfindingsoncommunityparticipationintheCalifornia HealthyCitiesandCommunitiesprogram. HealthPromot.Int. 2009, 24,300–310.[CrossRef]
29. Sanigorski,A.M.;Bell,A.;Kremer,P.J.;Cuttler,R.;Swinburn,B.A.Reducingunhealthyweightgaininchildrenthroughcommunity capacity-building:Resultsofaquasi-experimentalinterventionprogram,BeActiveEatWell. Int.J.Obes. 2008, 32,1060–1067. [CrossRef]
27. deSilva-Sanigorski,A.M.;Bolton,K.;Haby,M.;Kremer,P.;Gibbs,L.;Waters,E.;Swinburn,B.Scalingupcommunity-based obesitypreventioninAustralia:BackgroundandevaluationdesignoftheHealthPromotingCommunities:BeingActiveEating Wellinitiative. BMCPublicHealth 2010, 10,65.[CrossRef][PubMed]
35. Millar,L.;Kremer,P.;deSilva-Sanigorski,A.;McCabe,M.;Mavoa,H.;Moodie,M.;Utter,J.;Bell,C.;Malakellis,M.;Mathews,L. Reductioninoverweightandobesityfroma3-yearcommunity-basedinterventioninAustralia:The‘It’sYourMove!’project. Obes.Rev. 2011, 12,20–28.[CrossRef][PubMed]
48. Twiss,J.M.;Duma,S.;Look,V.;Shaffer,G.S.;Watkins,A.C.Twelveyearsandcounting:California’sexperiencewithastatewide HealthyCitiesandCommunityprogram. PublicHealthRep. 2000, 115,125.[CrossRef][PubMed]
40. Gantner,L.A.;Olson,C.M.Evaluationofpublichealthprofessionals’capacitytoimplementenvironmentalchangessupportiveof healthyweight. Eval.ProgramPlan. 2012, 35,407–416.[CrossRef]
38. Serpas,S.;Brandstein,K.;McKennett,M.;Hillidge,S.;Zive,M.;Nader,P.R.SanDiegoHealthyWeightCollaborative:Asystems approachtoaddresschildhoodobesity. J.HealthCarePoorUnderserved 2013, 24,80–96.[CrossRef]
46. Kegler,M.C.;Norton,B.L.;Aronson,R.Achievingorganizationalchange:Findingsfromcasestudiesof20Californiahealthy citiesandcommunitiescoalitions. HealthPromot.Int. 2008, 23,109–118.[CrossRef][PubMed]
49. Fialkowski,M.K.;DeBaryshe,B.;Bersamin,A.;Nigg,C.;Guerrero,R.L.;Rojas,G.;Vargo,A.;Belyeu-Camacho,T.;Castro,R.; Luick,B.Acommunityengagementprocessidentifiesenvironmentalprioritiestopreventearlychildhoodobesity:Thechildren’s healthyliving(CHL)programforremoteunderservedpopulationsintheUSaffiliatedpacificislands,HawaiiandAlaska. Matern. ChildHealthJ. 2014, 18,2261–2274.[CrossRef][PubMed]
30. Maitland,N.;Williams,M.;Jalaludin,B.;Allender,S.;Strugnell,C.;Brown,A.;Hayward,J.;Crooks,N.;Tredoux,J.;Li,V. Campbelltown–ChangingourFuture:StudyprotocolforawholeofsystemapproachtochildhoodobesityinSouthWestern Sydney. BMCPublicHealth 2019, 19,1699.[CrossRef]
28. Johnson,B.;Kremer,P.;Swinburn,B.;deSilva-Sanigorski,A.MultilevelanalysisoftheBeActiveEatWellintervention: Environmentalandbehaviouralinfluencesonreductionsinchildobesityrisk. Int.J.Obes. 2012, 36,901–907.[CrossRef][PubMed]
36. Chomitz,V.R.;McGowan,R.J.;Wendel,J.M.;Williams,S.A.;Cabral,H.J.;King,S.E.;Olcott,D.B.;Cappello,M.;Breen,S.;Hacker, K.A.HealthyLivingCambridgeKids:Acommunity-basedparticipatoryefforttopromotehealthyweightandfitness. Obesity 2010, 18,S45–S53.[CrossRef][PubMed]
39. Economos,C.D.;Hyatt,R.R.;Goldberg,J.P.;Must,A.;Naumova,E.N.;Collins,J.J.;Nelson,M.E.Acommunityintervention reducesBMIz-scoreinchildren:ShapeUpSomervillefirstyearresults. Obesity 2007, 15,1325–1336.[CrossRef]
44. Appel,J.M.;Fullerton,K.;Hennessy,E.;Korn,A.R.;Tovar,A.;Allender,S.;Hovmand,P.S.;Kasman,M.;Swinburn,B.A.; Hammond,R.A.DesignandmethodsofShapeUpUnder5:Integrationofsystemsscienceandcommunity-engagedresearchto preventearlychildhoodobesity. PLoSONE 2019, 14,e0220169.
41. Schulz,A.J.;Zenk,S.;Odoms-Young,A.;Hollis-Neely,T.;Nwankwo,R.;Lockett,M.;Ridella,W.;Kannan,S.Healthyeating andexercisingtoreducediabetes:Exploringthepotentialofsocialdeterminantsofhealthframeworkswithinthecontextof community-basedparticipatorydiabetesprevention. Am.J.PublicHealth 2005, 95,645–651.[CrossRef]
32. Allender,S.;Millar,L.;Hovmand,P.;Bell,C.;Moodie,M.;Carter,R.;Swinburn,B.;Strugnell,C.;Lowe,J.;DelaHaye,K.Wholeof systemstrialofpreventionstrategiesforchildhoodobesity:WHOSTOPSchildhoodobesity. Int.J.Environ.Res.PublicHealth 2016, 13,1143.[CrossRef]
42. Samuels,S.E.;Craypo,L.;Boyle,M.;Crawford,P.B.;Yancey,A.;Flores,G.TheCaliforniaendowment’shealthyeating,active communitiesprogram:Amidpointreview. Am.J.PublicHealth 2010, 100,2114–2123.[CrossRef]
33. Malakellis,M.;Hoare,E.;Sanigorski,A.;Crooks,N.;Allender,S.;Nichols,M.;Swinburn,B.;Chikwendu,C.;Kelly,P.M.;Petersen, S.School-basedsystemschangeforobesitypreventioninadolescents:OutcomesoftheAustralianCapitalTerritory‘It’sYour Move!’. Aust.NewZealandJ.PublicHealth 2017, 41,490–496.[CrossRef]
58. Sautkina,E.;Goodwin,D.;Jones,A.;Ogilvie,D.;Petticrew,M.;White,M.;Cummins,S.Lostintranslation?Theory,policyand practiceinsystems-basedenvironmentalapproachestoobesitypreventionintheHealthyTownsprogrammeinEngland. Health Place 2014, 29,60–66.[CrossRef]
65. Borys,J.M.;LeBodo,Y.;Jebb,S.A.;Seidell,J.;Summerbell,C.;Richard,D.;DeHenauw,S.;Moreno,L.;Romon,M.;Visscher, T.EPODEapproachforchildhoodobesityprevention:Methods,progressandinternationaldevelopment. Obes.Rev. 2012, 13, 299–315.[CrossRef]
69. Foucault,M. DisciplineandPunish:TheBirthofthePrison;Lane,A.,Translator;VintageBooks:NewYork,NY,USA,1991.
70. Foucault,M.;Rabinow,P. TheFoucaultReader:[AnIntroductiontoFoucault’sThought,withMajorNewUnpublishedMaterial];Penguin Books:London,UK,1984.
51. Gittelsohn,J.;Roache,C.;Kratzmann,M.;Reid,R.;Ogina,J.;Sharma,S.Participatoryresearchforchronicdiseasepreventionin Inuitcommunities. Am.J.HealthBehav. 2010, 34,453–464.[CrossRef]
57. Goodwin,D.M.;Cummins,S.;Sautkina,E.;Ogilvie,D.;Petticrew,M.;Jones,A.;Wheeler,K.;White,M.Theroleandstatusof evidenceandinnovationinthehealthytownsprogrammeinEngland:Aqualitativestakeholderinterviewstudy. J.Epidemiol. CommunityHealth 2013, 67,106–112.[CrossRef][PubMed]
67. Lee,B.Y.;Bartsch,S.M.;Mui,Y.;Haidari,L.A.;Spiker,M.L.;Gittelsohn,J.Asystemsapproachtoobesity. Nutr.Rev. 2017, 75, 94–106.[CrossRef][PubMed]
68. Hawe,P.;King,L.;Noort,M.;Gifford,S.M.;Lloyd,B.Workinginvisibly:Healthworkerstalkaboutcapacity-buildinginhealth promotion. HealthPromot.Int. 1998, 13,285–295.[CrossRef]
54. Amed,S.;Naylor,P.-J.;Pinkney,S.;Shea,S.;Mâsse,L.C.;Berg,S.;Collet,J.-P.;Higgins,J.W.Creatingacollectiveimpacton childhoodobesity:LessonsfromtheSCOPEinitiative. Can.J.PublicHealth 2015, 106,e426–e433.[CrossRef]
55. Amed,S.;Shea,S.;Pinkney,S.;WharfHiggins,J.;Naylor,P.-J.WayfindingtheLive5-2-1-0initiative—attheintersectionbetween systemsthinkingandcommunity-basedchildhoodobesityprevention. Int.J.Environ.Res.PublicHealth 2016, 13,614.[CrossRef] [PubMed]
56. McIntosh,B.;Daly,A.;Mâsse,L.C.;Collet,J.-P.;Higgins,J.W.;Naylor,P.-J.;Amed,S.Sustainablechildhoodobesityprevention throughcommunityengagement(SCOPE)program:Evaluationoftheimplementationphase. Biochem.CellBiol. 2015, 93,472–478. [CrossRef][PubMed]
62. Bloch,P.;Toft,U.;Reinbach,H.C.;Clausen,L.T.;Mikkelsen,B.E.;Poulsen,K.;Jensen,B.B.Revitalizingthesettingapproach–supersettingsforsustainableimpactincommunityhealthpromotion. Int.J.Behav.Nutr.Phys.Act. 2014, 11,118.[CrossRef]
Int.J.Environ.Res.PublicHealth 2022, 19,10997 16of17
52. Raine,K.D.;Plotnikoff,R.;Nykiforuk,C.;Deegan,H.;Hemphill,E.;Storey,K.;Schopflocher,D.;Veugelers,P.;Wild,T.C.; Ohinmaa,A.Reflectionsoncommunity-basedpopulationhealthinterventionandevaluationforobesityandchronicdisease prevention:TheHealthyAlbertaCommunitiesproject. Int.J.PublicHealth 2010, 55,679–686.[CrossRef]
66. Romon,M.;Lommez,A.;Tafflet,M.;Basdevant,A.;Oppert,J.M.;Bresson,J.L.;Ducimetiere,P.;Charles,M.A.;Borys,J.M. Downwardtrendsintheprevalenceofchildhoodoverweightinthesettingof12-yearschool-andcommunity-basedprogrammes. PublicHealthNutr. 2009, 12,1735–1742.[CrossRef][PubMed]
64. Borys,J.-M.;LeBodo,Y.;DeHenauw,S.;Moreno,L.;Romon,M.;Seidell,J.;Visscher,T. PreventingChildhoodObesity:EPODE EuropeanNetworkRecommendations;Lavoisier:Cachan,France,2011.
71. Olstad,D.L.;Raine,K.D.;McCargar,L.J.Adoptingandimplementingnutritionguidelinesinrecreationalfacilities:Publicand privatesectorroles.Amultiplecasestudy. BMCPublicHealth 2012, 12,376.[CrossRef]
53. Raine,K.D.;Plotnikoff,R.;Schopflocher,D.;Lytvyak,E.;Nykiforuk,C.I.;Storey,K.;Ohinmaa,A.;Purdy,L.;Veugelers,P.;Wild, T.C.HealthyAlbertaCommunities:Impactofathree-yearcommunity-basedobesityandchronicdiseasepreventionintervention. Prev.Med. 2013, 57,955–962.[CrossRef]
60. Lloyd,J.;Creanor,S.;Logan,S.;Green,C.;Dean,S.G.;Hillsdon,M.;Abraham,C.;Tomlinson,R.;Pearson,V.;Taylor,R.S. EffectivenessoftheHealthyLifestylesProgramme(HeLP)topreventobesityinUKprimary-schoolchildren:Aclusterrandomised controlledtrial. LancetChildAdolesc.Health 2018, 2,35–45.[CrossRef]
63. Toft,U.;Bloch,P.;Reinbach,H.C.;Winkler,L.L.;Buch-Andersen,T.;Aagaard-Hansen,J.;Mikkelsen,B.E.;Jensen,B.B.;Glümer, C.ProjectSoL—Acommunity-based,multi-componenthealthpromotioninterventiontoimproveeatinghabitsandphysical activityamongDanishfamilieswithyoungchildren.Part1:Interventiondevelopmentandimplementation. Int.J.Environ.Res. PublicHealth 2018, 15,1097.[CrossRef]
72. Sarrafzadegan,N.;Rabiei,K.;Wong,F.;Roohafza,H.;Zarfeshani,S.;Noori,F.;Grainger-Gasser,A.Thesustainabilityof interventionsofacommunity-basedtrialonchildrenandadolescents’healthylifestyle. ARYAAtheroscler. 2014, 10,107.
50. Wilken,L.R.;Novotny,R.;Fialkowski,M.K.;Boushey,C.J.;Nigg,C.;Paulino,Y.;Guerrero,R.L.;Bersamin,A.;Vargo,D.;Kim,J. Children’sHealthyLiving(CHL)ProgramforremoteunderservedminoritypopulationsinthePacificregion:Rationaleand designofacommunityrandomizedtrialtopreventearlychildhoodobesity. BMCPublicHealth 2013, 13,944.[CrossRef][PubMed]
61. Lloyd,J.J.;Wyatt,K.M.;Creanor,S.BehaviouralandweightstatusoutcomesfromanexploratorytrialoftheHealthyLifestyles Programme(HeLP):Anovelschool-basedobesitypreventionprogramme. BMJOpen 2012, 2,e000390.[CrossRef]
59. Middleton,G.;Henderson,H.;Evans,D.Implementingacommunity-basedobesitypreventionprogramme:Experiencesof stakeholdersinthenortheastofEngland. HealthPromot.Int. 2014, 29,201–211.[CrossRef]
76. Khan,M.S.;Khan,I.;Qureshi,Q.A.;Ismail,H.M.;Rauf,H.;Latif,A.;Tahir,M.Thestylesofleadership:Acriticalreview. Public PolicyAdm.Res. 2015, 5,87–92.
78. Tran,H.N.Q.;Killedar,A.;Tan,E.J.;Moodie,M.;Hayes,A.;Swinburn,B.;Nichols,M.;Brown,V.Cost-effectivenessofscalingup awhole-of-communityintervention:TheRomp&Chompearlychildhoodobesitypreventionintervention. PediatricObes. 2022, 17,e12915.
73. Greaney,M.L.;Hardwick,C.K.;Spadano-Gasbarro,J.L.;Mezgebu,S.;Horan,C.M.;Schlotterbeck,S.;Austin,S.B.;Peterson,K.E. Implementingamulticomponentschool-basedobesitypreventionintervention:Aqualitativestudy. J.Nutr.Educ.Behav. 2014, 46, 576–582.[CrossRef]
,10997 17of17
74. Jain,A.;Langwith,C.Collaborativeschool-basedobesityinterventions:Lessonslearnedfrom6southerndistricts. J.Sch.Health 2013, 83,213–222.[CrossRef]
79. Finucane,M.M.;Stevens,G.A.;Cowan,M.J.;Danaei,G.;Lin,J.K.;Paciorek,C.J.;Singh,G.M.;Gutierrez,H.R.;Lu,Y.;Bahalim, A.N.National,regional,andglobaltrendsinbody-massindexsince1980:Systematicanalysisofhealthexaminationsurveysand epidemiologicalstudieswith960country-yearsand91millionparticipants. Lancet 2011, 377,557–567.[CrossRef]
77. Whelan,J.;Love,P.;Millar,L.;Allender,S.;Bell,C.Sustainingobesitypreventionincommunities:Asystematicnarrative synthesisreview. Obes.Rev. 2018, 19,839–851.[CrossRef]
Int.J.Environ.Res.PublicHealth 2022, 19
75. Dreisinger,M.L.;Boland,E.M.;Filler,C.D.;Baker,E.A.;Hessel,A.S.;Brownson,R.C.Contextualfactorsinfluencingreadinessfor disseminationofobesitypreventionprogramsandpolicies. HealthEduc.Res. 2012, 27,292–306.[CrossRef]