
Rush Social Work and Community Health


Rush Social Work and Community Health
Rush Social Work and Community Health (SWaCH) dismantles barriers to health and wellness by:
• Providing innovative programs that support patients and community members
• Advancing policies and practices that expand access to social care
The following pages contain snapshots of SWaCH’s work. For more detailed information about our programs and services, go to rush.edu/swach2024.
If you’re interested in helping SWaCH care for patients and community members, expand access to social care for everyone and make a real difference in our neighborhoods and nationwide, contact Michelle Boardman, senior director of development, at (312) 942-6884 or michelle_a_boardman@rush.edu.
Health promotion and disease prevention
Care for high-risk patients
Mental health care
Systems change
Workforce development
Policy advocacy
Research and development
Rush Generations
Health Legacy Program
Evidence-based workshops
Lectures and classes
Support groups
Rush@Home
Center to Transform Health and Housing
Virtual First
Outpatient Psychotherapy Clinic
Rush Wellness
Legacy Mental Health Fellowship
Community Practice Social Care
Caring for Caregivers (C4C)
Social determinants of health screening
Center for Excellence in Aging
Center for Health and Social Care Integration
CATCH-ON
E4 Center
Social care reimbursement
Housing
Mental health
Social care
Aging
Mental health
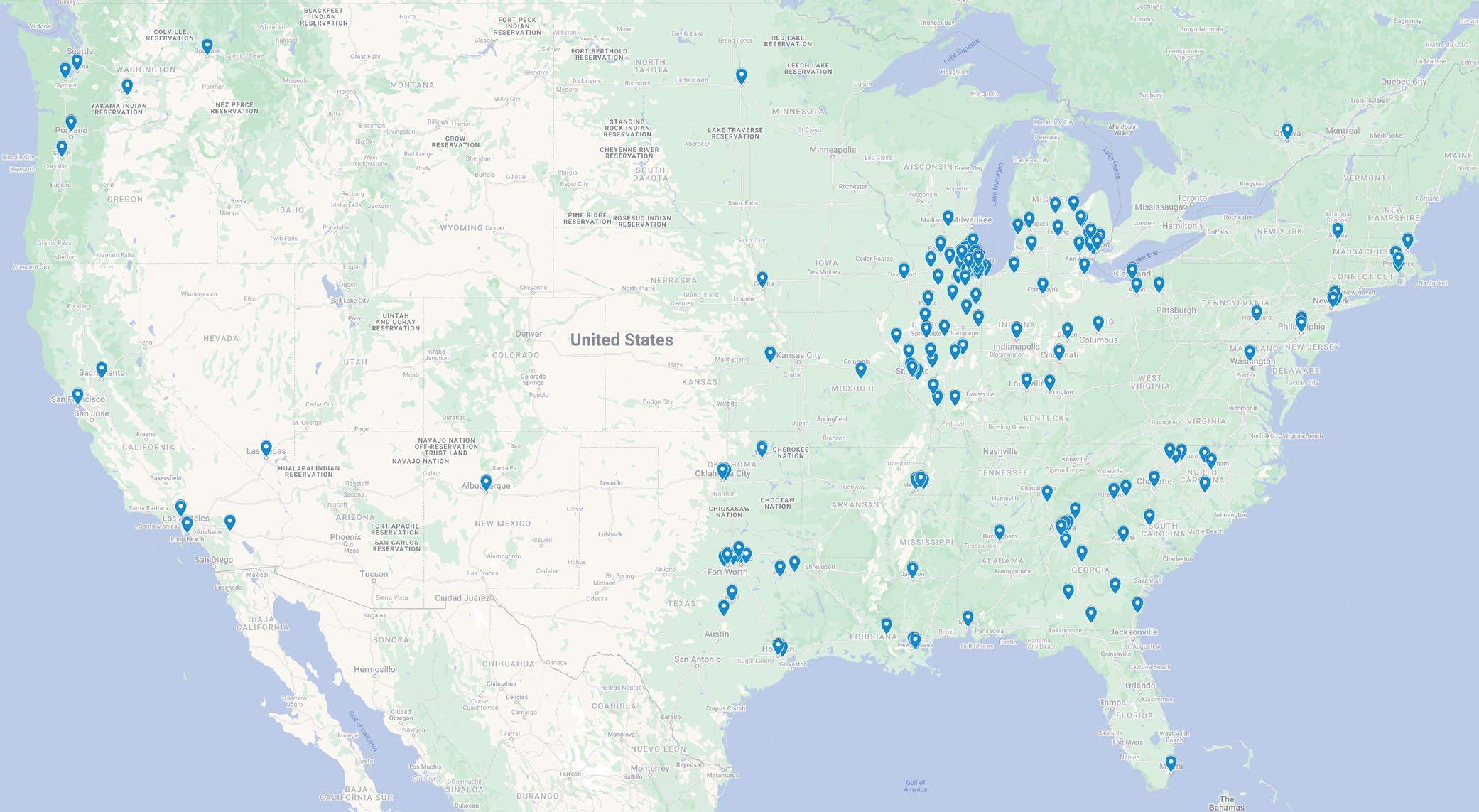
Rush’s SWaCH department makes a difference at Rush, in Chicago neighborhoods and across the country.
Nationally, SWaCH puts leading-edge social care research into practice by developing and sharing evidence-based curricula, programs and care models that are now used by dozens of organizations nationwide. We advocate for systems change and policy improvements, and manage coalitions that work to elevate the impact of social work, support integrated social care and improve access to social work services.
In our neighborhoods, SWaCH partners with other Rush teams and initiatives that focus on improving health equity on Chicago’s West Side. We also work
closely with community nonprofit organizations to screen people for social needs, provide social care and coordinate care for people with complex needs.
At Rush, SWaCH social workers are key members of interdisciplinary teams throughout the system, engaging with patients who have social care and behavioral health needs. We also offer group and individual psychotherapy in English and Spanish to patients, community members and Rush employees.
And we invite community members in by offering support services, classes and events at Rush University Medical Center and other Chicago-area locations.


SWaCH services provide significant economic and social value by lowering costs of care across health care systems and improving outcomes for the people we serve.
By delivering needed services and screening for the social determinants of health, we’re able to connect people with the care and support they need before their
health issues reach a crisis point. When people have access to reliable care, resources for essentials needs like healthy food and stable housing, and education about managing chronic health conditions, they’re more resilient, better able to thrive and less likely to need emergency care.

Our Health Promotion and Disease Prevention team provides evidence-based workshops, lectures, screenings, classes and support groups to Rush patients and community members. Available in English and Spanish, our education and support groups help people learn strategies for everything from managing chronic conditions like diabetes to aging with confidence. These programs are proven to improve participants’ health outcomes and quality of life.

impact in FY24


Take Charge of Your Health gives people the tools and confidence to manage chronic health conditions.
Take Charge of Your Diabetes has content specific to those with pre-diabetes or Type 2 diabetes.
Chronic Pain Self-Management provides health education, exercise and peer support to empower people with chronic pain to maintain active, fulfilling lives.
Cancer: Thriving and Surviving teaches skills to manage fatigue, pain, nutrition, fear of recurrence and more.
Wellness Recovery Action Plan (WRAP) shows people with mental and physical health issues strategies for feeling less isolated and more in control.
WRAP for Healthy Aging is tailored to the unique needs and concerns of adults aged 60 and over.
“ Working with Rush’s patients directly in their communities is a great privilege and is essential to improving health outcomes.”

Walter Rosenberg, MSW, MHSM, LCSW Director, Social Work and Community Health

The Health Legacy Program is a free, six-week program that empowers women of color to attain better health. The program tackles diabetes, obesity and high blood pressure through a holistic approach that blends health education, exercise, meal planning and peer support. Participants forge meaningful connections with one another while they learn new habits, and nearly all report positive transformations in their food choices, overall health and quality of life.
Monthly and quarterly newsletters contain relevant health information and calendars of events.
Evidence-based health management and fall prevention workshops are available in English and Spanish.
Support groups for people with chronic pain and diabetes, and for caregivers of people with Alzheimer’s and related dementias, meet regularly.
Educational lectures throughout the year discuss topics related to health and aging.
Health screening and information sessions include balance testing, medication reviews and advice on creating advance directives.
“Attending programs at the senior center, particularly the exercise groups, has improved my health and helped me stay out of the hospital.”
Mary McChristian Rush Generations member


In partnership with Rush University, Rush Generations offers a unique volunteer opportunity: Older adult volunteers work with health professions students to help create health systems that focus on providing high-quality care for older adults. In the Community Health Mentor program, older adults with chronic health conditions meet via telehealth with students in the university’s “Interprofessional Patient-Centered Teams” class. They help educate the students about what matters most to older adults in seeking health care. In return, the students work with the volunteers to make personalized wellness goals and action plans.


Virtual First is an innovative telemedicine clinic where primary care patients benefit from a comprehensive care team that includes SWaCH social workers alongside physicians, advanced practice providers, nurses and other professionals.
“This is a blessing to have somebody come to the house. My 92-year-old beautiful mother has dementia and can’t do anything for herself. Not a lot of seniors have this kind of service. I am very blessed to have you guys here.”
Carmen F. Daughter of Rush@Home patient Matilde
Rush’s Center to Transform Health and Housing has two goals: providing high-quality, well-coordinated health and social care to improve the health of people experiencing homelessness, and collaborating with others to end homelessness in Chicago.
We envision a center of excellence for interprofessional collaboration; the delivery of person-centered physical, mental health and social care; advocacy; and the improvement of health and housing equity for people experiencing homelessness.
“One of the things that the center works to do is increase access to health care by providing care where [people] are — care where they call home, care at shelters, care on the streets, care in several other congregate settings.”
Eugenia Olison, LPC Program manager

Our impact in FY24

214 encounters per month, on average


23 social care encounters per month, on average
1,197 harm reduction kits distributed to prevent overdoses
890 1,197

The center supports advocacy and collaboration efforts through the Chicago Homelessness and Health Response Group for Equity (CHHRGE). Co-founded in 2020 by Rush University students, faculty and staff to mitigate the spread of

COVID-19 among shelter guests, CHHRGE has evolved into a citywide forum for anyone who works with people who are experiencing homelessness or are vulnerably housed. Together, we help to identify and overcome barriers to their health and well-being. Our goal: to build a community where all people can achieve good health and stable housing.
The Center to Transform Health and Housing was featured in a 2024 Healthcare Financial Management Association story about the role of health care in addressing homelessness. Click here for more.
The SWaCH Outpatient Psychotherapy Clinic provides mental health services to Rush patients and community members, focusing on the intersections of complex trauma, psychosocial need and medical diagnoses. We offer trauma-informed, strengths-based, patient-centered psychotherapy services in English and Spanish.
Providing outpatient psychotherapy in a medical setting enables us to collaborate with other providers while advocating for and empowering our patients around their full plan of care. Our collaboration includes formal partnerships with Rush teams that work in epilepsy, infectious diseases and obstetrics and gynecology.
Trauma-informed treatment uses an array of evidencebased approaches.
LGBTQIA+ psychotherapy group gives members an affirming space to share their experiences and concerns while learning from others and working on personal goals related to growth and mental health.
Access to mental health services fills a need in underserved neighborhoods. The top ZIP codes we serve are concentrated on Chicago’s West Side; nearly 80% of our patients are people of color, and 76% have Medicaid or Medicare.
11,283
“Knowing that I can trust the SWaCH psychotherapy team to provide excellent care results in improved health states and satisfaction for patients.”
Valerie Davis, RN Family Focus at Rush






Launched in 2022, the Legacy Mental Health Fellowship supports emerging minority social work clinicians who want to reduce health disparities and improve mental health access for residents of Chicago’s West Side. Two graduates of the first cohort now work at Rush, and we hope to hire many more as the fellowship continues. All of the graduates are making a significant impact not only at Rush but also through partnerships with the Institute for Non-Violence Chicago and the MAAFA Redemption Project. The fellowship is a collaboration among SWaCH, the Garfield Park Rite to Wellness Collaborative and Chicago State University’s MSW program.
Quality patient care is directly tied to the well-being of providers, students and staff — and health care providers nationwide are experiencing high levels of anxiety, depression and burnout. Rush Wellness supports personal and professional well-being for Rush employees and students with offerings that include coaching and programming along with mental health services provided by SWaCH.
Rush is one of just 25 organizations nationwide recognized by the American Medical Association for dedication to ensuring care teams’ health and well-being. Click here for more.
Psychotherapy services are provided free to Rush employees, students and house staff. SWaCH therapists use a person-centered, trauma-informed approach to evidence-based therapy. This team helps address burnout and increase workplace satisfaction.
Our Wellness Pager, staffed 24/7 by therapists, provides mental health support to Rush employees and students in urgent situations. The clinicians covering the pager connect people to what they need, from community resources to an appointment with Rush Wellness to a higher level of care.
Increased access to Rush Wellness services with the addition of a dedicated psychotherapist to Rush Copley in 2024.

5,391 wellness sessions provided

106 responses to the “wellness pager” requesting a wellness consult for staff members

300+ employees, students, and staff received individual psychotherapy services


“I felt heard, understood and supported. Every visit, I feel like I am closer to my personal goals. [My therapist] never judges and truly is trying to help.”
Rush Wellness client

Birth Equity works to ensure more optimal birth conditions for all and address the racial and social impact of current disparities and inequities in birth outcomes.
Wellness West is a collaboration of leading hospitals, health systems and community organizations representing hundreds of years of experience on the West Side. Working together, this coalition is closing gaps in the health care delivery system.
E3 Clinic focuses on engaging with high-risk cardiovascular patients in West Side communities. A three-pronged remote monitoring program targets hypertension, diabetes and elevated cholesterol.
Center for Trauma Recovery provides no-cost therapy and care management services for people impacted by gun violence and other forms of trauma.
800 Community Helpline, a toll-free number, can be used by any community member regardless of their location, insurance, or condition to talk with social workers and community health workers for assessment and connection to resources and care.

Caregivers completed mental health assessments before and after participating in C4C. Results showed decreases in depression, anxiety and overall caregiving burden.
“Caregiving can have a significant impact on life. It can stress your career, your family, your friendships. It can also affect finances and lead to serious health problems. But by making some changes and getting help, caregiving and the stress that often goes with it can become more manageable.”
Ellen Carbonell, MSW Consultant, caregiver programs

According to the Institute for Clinical Systems Improvement, social determinants have a far bigger impact on people’s health than medical care. Only 20% of health outcomes tie directly back to health care, while at least half are influenced by factors like education, income and where people live.
“By addressing [people’s] social determinants of health and providing some of the resources that they so need, they have the time and the mind to focus on their health.”
Teresa Berumen Senior community health worker supervisor

This year, SWaCH completed the fifth year of an AmeriCorps program that expands our ability to screen and intervene with patients discharged from the Emergency Department.
4 AmeriCorps members
1,272 patients screened
401 patients received interventions

The Rush Center for Excellence in Aging (CEA) takes the lessons learned from research and applies them to clinical and community settings, improving how health professionals deliver care and prevent disease. CEA’s research-based initiatives include health care and aging education, evidence-based clinical practice, community engagement and local and national policy change.
Our health care provider members work together closely and share information, providing services and collaborating across five core areas:
• Research
• Older adult and family care
• Education
• Community health equity
• Health policy
All five exemplify our focus on the health and wellbeing of older adults, their families and caregivers, with particular emphasis on improving cognitive health and addressing health disparities.


unique users viewed E4 online modules
The Collaborative Action Team training for Community Health — Older adult Network (CATCH-ON) has two objectives. First, we educate and train the primary care and geriatrics workforce to care for older adults in integrated geriatrics and primary care. We also partner with community-based organizations to address gaps in health care for older adults, promote age-friendly health systems and dementia-friendly communities and address the social determinants of health.

Age-friendly health systems are committed to addressing the four Ms: What matters to older adults and their families; keeping as much mobility as possible; medication at safe and appropriate levels as needed; and mentation, or screening for and treating depression, delirium and dementia.
The E4 Center’s mission is to engage, empower and educate health care providers and community-based organizations around equity in behavioral health for older adults and their families. We do so by providing education, implementation resources and technical assistance for mental health, substance use and the intersection of both with physical health.
Schaalman Senior Voices, housed in the CEA, is a collection of films, educational opportunities and programs that aim to strengthen the well-being of older adults and their communities. Inspired by Rabbi Herman Schaalman of Chicago’s Emanuel Congregation, the collection provides new avenues to enhance older adults’ engagement in sharing what matters most in the process of aging, and to support the training of students and health professionals in Chicago, the region and nationwide.

Social care drives better health and health equity by addressing social risk factors, but the U.S. health care system is not equipped to adequately address healthrelated social needs. CHaSCI, a training and policy center based at Rush and housed within SWaCH improves and expands access to social care to improve the health and well-being of individuals, families and communities. By training the social care workforce, supporting integration of social care into health care systems and advocating for policies that create payment pathways for social care providers, CHaSCI’s work supports Rush’s mission to remove barriers to health and reduce inequitable outcomes in health and
115 trainees took 51.5 hours of training with 8 training partners
5 curriculum development projects completed for external partners
6 Social Work Grand Rounds webinars organized and hosted
10 enrollees in the first year of the Social Work in Health Care training program
well-being. The Coalition for Social Work and Health (CSWH), led by CHaSCI, is a national network of leaders in social work practice, education, research and policy whose goal is to advance social work’s role and value in improving our nation’s health. With representation from more than 50 social work professional organizations, academic and research programs and individual members, the coalition focuses on amplifying social work’s impact in transforming health care, improving health and advancing health equity.
CHaSCI spreads the word nationally about the critical role clinical social workers play in health care settings. Click here and here for more.
4 modules developed and delivered for HRSA-funded CHW CONNECT training program run by UIC OCEAN-HP
12 students and social workers pilot-tested a Certificate of Social Work in Health Care as part of a health workforce diversity grant from Cigna
2 Rush University faculty participated in Interprofessional Education course
8 graduate students in social work, public health and health systems management from Chicago-area programs learned with us

Policy
2 coalitions hosted: National Coalition on Care Coordination and the Coalition for Social Work and Health
Supported creation of H.R. 4638, the Integrating Social Workers Across Health Care Settings Act
Research and dissemination
6 presentations at conferences, panels and other professional gatherings
4 publications

Ankuda, C. & Ewald, B. (2024). Applied research in aging: Advancing health equity and addressing social needs. Generations Journal, 48(2), 1-5.
Byrne, T., Millheiser, A., Moro, T., McFadden, A., Powell, N., & Davis, E. (2024). Rush@Home: Serving the community where they are most comfortable. Clinical Social Work Journal, 52(1), 71–78. https://doi.org/10.1007/s10615-023-00885-z
Ewald, B., & Golden, R. (2023). Strengthening community supports and health services: An imperative for health equity and aging in community. Public Policy & Aging Report, 33(3), 134-142. https://doi.org/10.1093/ppar/prad014
Greene, R., & Cummings, E. (2023). Transitioning from hospital to home: Resilience-enhancing skills for health care social workers. In R. Greene, N. Greene, & C. Corley (Eds.), Resilience enhancement in social work practice (pp. 81–97). Springer. https://doi.org/10.1007/978-3-031-38518-6_6
Escalante, E. (2023, October). Trauma-informed care for older adults. Presentation at the Re-Imagine Conference.
Golden, R., & Ewald, B. (2023, September 26). Paying for social care: Investing in what matters. CHAS (Center for Health Administration Studies) Lecture Series, University of Chicago Crown Family School of Social Work, Chicago, IL.
Moro, T., Johnson, T., Avery, L., McFadden, A., & Ewald, B. (2023, September). Social workers and community health workers in primary care: A RE-AIM impact study. Presentation at the Chicago Chronic Care Equity Network (C3EN) Annual Meeting, Chicago, IL.
Moro, T., Petruzzi, L., McFadden, A., Guan, T., Franceschini, D., Chen, Q., Wilsnack, C., Nelson, K., Otis-Green, S., Westrick, J., & Jones, B. (2024, January 12). Value of social work (SW) interventions in healthcare: Current research and future directions. Paper presentation at The Society for Social Work and Research (SSWR) Annual Conference, Washington, DC.
Moro, T., & McGinley, J. (2024, January 12). Accessibility in social work internships: Barriers to and opportunities for inclusion. Poster presentation at The Society for Social Work and Research (SSWR) Annual Conference, Washington, DC.
Moro, T., & McGinley, J. (2024, February 28). Caring for patients with intellectual and developmental disabilities. Coleman Palliative Medicine Training Program, University of Chicago, Chicago, IL.
Novack, L., Carroll, A., Rodríguez-Morales, G., Sergi, A., & Getahun, E. (2024, March 25). It’s all in your head: How to cultivate an innovator mindset. Presentation at the American Society on Aging, On Aging 2024 Conference, San Francisco, CA.
Rodríguez-Morales, G., & Odiaga, J. A. (2024, March 25). Empowering older adults through mentorship-centered interprofessional learning experience. Presentation at the American Society on Aging, On Aging 2024 Conference, San Francisco, CA.
Hunt, M., Moro, T., & Stanley, P. (2024). Unmet mental health care needs: Layered marginalities in older adult populations. Generations, 48(1), 1-11.
Moro, T., Rowe, J., & Rizzo, V. (2024). A balance of art and science: Promoting collaborative aging research. Generations, 48(2), 1-11.
Steven, T., Odiaga, J. A., Gierlowski, T., Guglielmo, M. J., Little, L. M., Rodríguez-Morales, G., Richter, S., & Souza, S. (2023). Transforming interprofessional pedagogies: Pivoting from the flipped classroom to an online approach. Journal of Interprofessional Education & Practice, 22, Article 100683. https://doi.org/10.1016/j.xjep.2023.100683
Stanley, P., Cervantes-Vázquez, Y., & Ortiz, P. (2024, May). The aging undocumented community: How the aging network can prepare and advocacy needs. Panel presentation at the Age+Action Conference, National Council on Aging, Arlington, VA.
Stanley, P., & Siegel, T. (2024, March). Immigrant health and social care. CEU event at the Society for Social Work Leadership in Health Care, Chicago, IL.
Stanley, P. (2023, November). Updates and disparities in immigrant health care coverage and access. Training at the Illinois Medical District Palliative Care Collaborative, Chicago, IL.
Stanley, P. (2023, November). Understanding and challenging imposter syndrome. Training for the Schweitzer Fellowship Mid-Year Retreat, Health and Medicine Policy Research Group, Chicago, IL.
Stanley, P., & Cervantes-Vázquez, Y. (2023, November). Integrating peer-led group interventions into community and behavioral health to empower CHWs and communities. Workshop at Putting Care at the Center, Camden Coalition National Center for Complex Health and Social Needs, Boston, MA.
Stanley, P., & Cervantes-Vázquez, Y. (2023, September). Effective group interventions to empower CHWs and communities. Poster presented at the IPHA 82nd Annual Conference, Illinois Public Health Association, Oglesby, IL.
Williams, S., Rodríguez-Morales, G., Cooper, K., Calloway, J., & Wayland, S. (2024, May 7). Let’s re-balance: Addressing disparities in health/social care integration. Presentation at the National Council on Aging, Age+Action 2024 Conference, Washington, DC.

In fiscal year 2025, SWaCH plans to focus on the following four strategic priorities.
Quality and innovation
• Expand program evaluation and research opportunities
• Conduct a scoping review on the value of social work in health care settings
Team culture and development
• Activities and supports to create a welcoming, inclusive and equitable culture within the department
• Transparency in department and program decision-making

Efficiency and essentialism
• Identify opportunities to improve efficiency
• Develop an intentional approach to developing and maintaining internal and external partnerships
Financial sustainability
• Optimize financing models, including value-based care, grants and donors
• Maximize opportunities for reimbursement for social care services
“ The future will be bright if we can have a social worker at every table.”
Eve Escalante, MSW, LCSW Manager of program innovation

