
2023–24 Annual Report



2023–24 Annual Report

Our busy clinical schedules, active portfolios of research projects and several conferences to attend throughout the year don’t always leave enough time for reflection about where you are today and where you’re headed as a clinician, team or department.
Recently, a friend and colleague I hadn’t seen in a while stopped me at a conference, remarking at how much the Rush Department of Surgery has grown over the last few years. Since I see our great work from up close each and every day, our tremendous growth at Rush University System for Health is sometimes difficult to take into perspective. Often, I don’t take enough time to step back and see, as my colleague had mentioned, just how far we’ve come as a department in these few passing years — and since the beginnings of RUSH back in 1837. Our interaction gave me an opportunity to do just that, and I’m excited to share some of our highlights with you in the report that follows.
Our mission to provide first-rate care is not new, but I think many people around the country really got to know RUSH for the first time through all of the media coverage during the COVID-19 pandemic. From the way RUSH was built to handle such a widespread emergency, to the way we took the lead in treating the sickest of patients, this highlighted our overall strength as an academic medical center and national leader in the practice of medicine.
During that challenging time, our department found innovative ways to broaden the care we could offer. We provided telemedicine as a way to conveniently see patients before and after their surgery and hosted a series of webinars on a variety of topics to keep those patients engaged in their care — essentially bringing RUSH providers into their homes at a time when medical care and human interaction were vital our health and survival.
Once we could safely open our doors and welcome patients to our facilities again, we continued our push to expand into the communities we serve. We have since opened multispecialty clinics here in Illinois with Rush Oak Lawn and Rush Hinsdale as well as Rush Munster in Northwest Indiana. The key to our success in those locations isn’t that we simply set up shop. It’s that we listened to the needs of our patients and community providers and brought specialized care in surgical oncology, plastic surgery and bariatric surgery, among others, that only an academic medical center like RUSH could provide. That kind of specialization takes a significant investment by RUSH and thoughtfulness to know how we can make the greatest difference in Chicago and our neighboring communities.
We’ve worked hard to forge strong relationships with providers and partners in the community. When we can step in and collaborate to provide that next-level care to their patients, returning them home and into the capable hands of their trusted caregivers, it’s RUSH care at its finest. We’ve also made it easier for patients to get to our care: Instead of having to drive into Chicago, patients can now access a full complement of RUSH’s specialty care in a more convenient community setting, sometimes just minutes from their doorstep.
As department chair, I’m incredibly proud of all of our clinicians and their dedication to our patients. In this report, I hope you enjoy learning more about our team and the work that’s happening within the Rush Department of Surgery. It’s a privilege to practice medicine with these dedicated professionals every day.
Alfonso Torquati, MD, MSCI, FACS
Helen Shedd Keith Professor of Surgery
Chair, Department of Surgery

*Case

A conversation with Shaista Chatterji, MHA, department administrator of the Rush Department of Surgery
For nearly seven years, Shaista Chatterji has led strategy and business development for the departments of surgery and urology at RUSH. In this conversation, Chatterji highlights the strengths of Rush Surgery, the challenges the current financial climate brings to its operations and the opportunities RUSH has for continued growth in and around Chicago.
Q: In your role as department administrator, you’re responsible for managing the business administration of the Rush Department of Surgery What might surprise surgeons who don’t handle the day-in, day-out challenges you encounter with this unique aspect of surgical operations?
A: There’s a need to step back and look at how and where we can really help our community. Sometimes that can get overlooked. Our physicians excel at providing safe, high-quality care to our patients. I think there’s an inclination with our surgeons to provide that care in as many places as possible, but obviously there’s a limit to that capacity. We have to be thoughtful about how and where we’re putting our footprint down so that we can offer convenient care to as many patients as possible, while sustaining that positive impact in our communities.
With so many options for care in our city and in our region, patients are becoming more educated and more selective in choosing a provider — and even where they want to receive their care. One of the backbones for our growth into new areas are the relationships we develop with primary care and specialty care providers throughout the region. They are the trusted voice for their patients. We work hard to be their trusted partner and a place they want to refer their patients to for surgery. To me, these relationships have a greater impact on our success than any billboard or TV ad.
Our ethos at RUSH is to work collaboratively with these community physicians. Depending on the patient and the care they need, we can be there to handle the surgical aspect of care, and then return the patient back to their provider — or we can work together and partner throughout the patient’s care journey. This flexibility allows us to work symbiotically and do what’s best for the patient.
Q: The delivery of surgical care continues to evolve post-COVID-19 pandemic In what ways is RUSH still adapting to some of those unintended changes?
A: The costs of maintaining and staffing a surgical practice have really climbed. That’s not a phenomenon that’s unique to RUSH, as hospital systems and practices everywhere are struggling with higher costs for staffing and supplies.
Post-pandemic, we have developed creative ways to staff our clinics by expanding the support teams with not only medical assistants and RNs but also CNAs and LPNs. This allows us to utilize members of the team in the correct aspects of care while lowering the cost of services. We have also looked into the utilization of surgical techs in the OR to support Rush advanced practice providers running individual practices. As a result, we’ve been able to expand the care we offer in a timely fashion with further access.
The use of telemedicine greatly rose during the pandemic. Now we’re at a spot where we’re seeing a shift in patient preference, with people actually preferring to come in person to meet with their care team and appreciating those personal conversations. Telemedicine remains an option and is used on an as-needed basis.
Q: How would you say surgical research is affected by the new, challenging financial landscape that RUSH operates in right now?
A: When we talk about the overall financial health of the hospital, research is an area that can be a cost burden. Today, with many organizations in a financial crunch, there is a lot of pressure for surgeons to meet productivity goals. This priority takes away time for an academic surgeon to fully pursue all their research interests. In order to support those goals, we have a built-in infrastructure of research
Between adding new surgeons and managing the schedules of our current providers, making all of the pieces fit together feels a little bit like playing Tetris, but it’s incredibly rewarding and impactful when everything comes together just right .
support to partner with our clinicians so they can pursue their research interests.
It’s an ongoing process to find funding for this support. Grant awards are always the best, and philanthropy has been a great partner to help our department with funding.
Overall, our goal to continuously keep research at the forefront and find support for research,
while continuing to provide innovative care and incorporate the use of advanced technologies.
Q: How do you select new locations for expansion of Rush Surgery in the community?
A: There are several different factors we have to consider: What other competition is in the community? What surgical services are needed? Can we sustain our business
operations if we’re there, and are there partnerships and relationships we can build?
What makes it challenging is those variables change from community to community. The places where we’ve expanded — Oak Lawn and Hinsdale in Illinois as well as Munster in Northwest Indiana — are places where there has been good alignment in all of those areas.
When we feel like we know a community pretty well and the business operations aspect lines up, then we might do a slow build-out in that community. We want to make sure it’s a good fit for our surgeons, RUSH, the patients and providers in the community.
We also try to be proactive as well when we think about recruiting new surgeons. If we know we want to expand into a certain community, then we’ll consider aspects like the surgeon’s specialty or interest in practicing in communities outside of our main campus. For new surgeons, this can be a great opportunity to define their career and form new relationships with patients and area providers.
For our more senior surgeons, this can be a great opportunity to bolster the relationships they’ve spent years building and increase productivity. Between adding new surgeons and managing the schedules of our current providers, making all of the pieces fit together feels a little bit like playing
Tetris, but it’s incredibly rewarding and impactful when everything comes together just right.
Q: How do you anticipate Rush Surgery growing within the next five years?
A: Number one, we want to continue finding communities where we can partner with referring providers as we have in Oak Lawn, Munster and Hinsdale. The places where there’s the need for our care and the right opportunity for growth for RUSH, we’ll look to go there, too.
Number two, extending RUSH’s cancer care and offering our fellowship-trained surgical oncology services in the community setting. We want to bring our innovative technologies and collaborative approach to cancer closer to people’s homes.
Number three, our bariatric surgery and medical weight loss program is an area that’s also in great demand in and around Chicago. With several weight loss pharmaceuticals hitting the market lately, we’re seeing an even greater demand for the comprehensive and collaborative approach that our multidisciplinary team can offer. Lastly, we want to highlight our accountable care organization. We can streamline our patients’ care while also reducing our expenses at the same time. Staying within the RUSH network means patients stay on top of
their primary care and have the ability to see a specialist when their care calls for it. It’s a true win-win for our patients — and RUSH.
By Swathi B. Reddy, MD
In 2008, a female patient in her 50s had an open umbilical hernia repair with mesh, which was performed. The patient presented to the emergency room for pain once in late-2023 before seeing me in the office.
When the patient came to Rush, she had a 10-12 cm bulge above her umbilicus, which had steadily been growing over the last five years. The bulge was located slightly above the site of her prior hernia repair and caused her pain, particularly when lifting boxes at home.
She felt that the hernia used to be able to be reduced easily (i.e., holding the hernia while coughing; eating a fiber-rich diet). The hernia became more tender when she tried to reduce it and the patient experienced occasional nausea associated with the hernia.
CT imaging revealed two ventral hernias; the widest of the two was 8 cm in width and had attenuated the rectus muscles; the hernia also contained the colon.
I performed a robotic transversus abdominis release (TAR) to repair the patient’s ventral hernias. This minimally invasive approach utilizes posterior component separation whereby TAR is performed on each side of the patient’s abdomen. Once I repaired the patient’s hernia, I re-approximated the posterior rectus sheath at the midline. I then placed a retrorectus mesh with significant overlap over the surrounding tissue before I closed off the posterior sheath of the rectus muscle.
Two months post-procedure, the patient is doing well and has returned to work. However, she continues to wear a waist trainer and will do so until the area has completely healed.
Although the operating time is increased with robotic TAR compared to an open operation, I believe that patients are less traumatized by not having a large incision. Robotic TAR is the gold standard for repairing complex ventral hernias. This approach significantly reduces the length of hospitalization (one to two- days compared to four to five days with a traditional open operation), involves much smaller incisions (six lap incisions vs. a midline laparotomy incision) and overall reduced postoperative pain. As a result of these benefits with robotic TAR, patients can more quickly resume normal, daily activities.

Swathi B. Reddy, MD

By Naomi Parrella, MD, FAAFP, FOMA, DABOM; Deanne Fornelli, PA-C, MS; Frances Lee, FNP-BC; and Antoinette Murphy, NP
A male patient in his 50s presented at Rush with several comorbidities: tongue squamous cell carcinoma, melanoma, hypertension, hypercholesterolemia, type 2 diabetes, obstructive sleep apnea and heartburn. His highest reported weight was 410 lbs., and he had not been able to get below 320 lbs. despite multiple previous diet and exercise attempts. He had been taking enalapril, atorvastatin, dapagliflozin and sitagliptin-metformin to manage his high blood pressure, cholesterol and diabetes, respectively.
Prior to his initial consultation, the patient lost 70 lbs. through lifestyle changes. He went from weighing 410 lbs. to 340 lbs. and had a body mass index (BMI) of 44.91 kg/m². He desired additional weight loss and was interested in gastric bypass for weight loss and control of diabetes; he expressed a desire to not rely on taking medications to control his weight for the rest of his life. His primary care provider also had mentioned that he would soon need to start insulin for diabetes, which was also undesirable to him.
The patient underwent successful laparoscopic Roux-en-Y gastric bypass surgery by Jonathan Myers, MD, in April 2023. His postoperative course was remarkable for euglycemic diabetic ketoacidosis,
which was likely secondary to the dapagliflozin, an SGLT2 inhibitor. He was treated with continuous insulin infusion and dextrose and was discharged on postoperative day 6.
The patient was seen six months following the procedure and was feeling great. His weight was 248 lbs. and his BMI was 32.75 kg/m². He has had no further complications. He is taking bariatric vitamins and his post-bariatric surgery nutrition labs are normal. He exercises every morning, including running, which he had not been able to do previously. He is also off diabetes, blood pressure and cholesterol medications. He also attends regular bariatric support group meetings.
A male patient in his 40s presented with a history of paraplegia, neurogenic bowel and bladder, depression, hypertension and obstructive sleep apnea.
At his initial visit, the patient weighed 265 lbs. and had a BMI of 44.1 kg/m². During that visit, we obtained a thorough weight and medical history. The patient said he wanted to lose weight to protect his shoulders from injury, since he relies on them for
his ability to transfer in and out of his wheelchair. He also wanted to be able to transfer from the floor into his wheelchair should he ever fall from his bed or wheelchair or during a transfer. We requested additional data including a food log and labs.
At his second visit, we reviewed his food log and discussed his labs, which were consistent with prediabetes and insulin resistance. We designed a lifestyle and nutrition plan to build a foundation for long-term weight loss. We also started him on metformin to treat his pre-diabetes and insulin resistance and in order to prevent progression to diabetes.
By the third visit, the patient weighed 253 lbs., had integrated the recommended lifestyle and nutrition habits and was tolerating metformin. Through shared decision making, we added an injectable glucagonlike peptide-1 receptor agonist (GLP 1 RA) to augment the treatment of his insulin resistance and pre-diabetes.
At subsequent follow-up visits, we continued to monitor his bloodwork to be sure he tolerated the lifestyle, nutrition and medications that were recommended. At each visit, we assessed lifestyle, nutrition and medication tolerance and effectiveness. We also recommended an at-home device he could use to monitor and adjust his nutrition plan as needed, offering him a sense of control over his continued weight loss goals.
Approximately one year after he was first seen at Rush, in November 2023, the patient weighed 175 lbs. He was working on floor transfers but no longer required a sliding board to transfer from bed to wheelchair. His shoulders were feeling much better, he had improved stamina using his wheelchair and had ordered a new, narrower wheelchair that afforded him easier access in the community. His most recent labs showed a complete reversal of pre-diabetes and his insulin resistance continued to improve.
A female patient in her 30s had a history of polycystic ovary syndrome (PCOS), anxiety and ADHD. She previously had a laparoscopic sleeve gastrectomy performed by Philip Omotosho, MD, in September 2016. Her highest weight prior to surgery was 280 lbs. and lowest after surgery was between 180-185 lbs.
One year following the surgery, the patient started to see some of the weight slowly come back, despite her best efforts with diet and exercise management. She remained very active and stuck to
the recommended diet that was high in protein, but admitted to adding more carbohydrate to her diet over the past few years. The patient also reported an increase in hunger and cravings throughout the day as well. Overall, the patient still did well after her surgery, but gained about 20 lbs. from her lowest weight.
With her insulin resistance and PCOS, it was difficult for the patient to lose the weight, even with maintaining a healthy eating pattern and routine exercise. The patient presented to our medical weight loss clinic in September 2022 for additional help. We first made adjustments to her current diet and she started to see some movement in her weight.
The patient and her provider then decided to add on a GLP 1 RA medication to further help with weight loss and her insulin resistance. The patient responded very well and continued to incorporate routine exercise and a low-carb diet. By September 2023, the patient was able to decrease her weight from 208 lbs. to 146 lbs. She continues to take the GLP 1 RA medication to help her maintain this weight within a range of 5-10 lbs.
In determining the best intervention for weight loss for patients, several variables need to be considered.
Medication interventions, such as GLP 1 RA medications including as liraglutide (Saxenda for treating weight or Victoza for treating Type 2 diabetes), semaglutide (Wegovy for treating weight and Ozempic for treating Type 2 diabetes), or a novel GLP 1 RA /GIP medication, tirzepatide (Zepbound for treating weight and Mounjaro, for treating Type 2 diabetes), offer patients a way to effectively reduce their weight.
Patients with a BMI of at least 27 kg/m² with other comorbidities are candidates for these drugs; early results show between a 10-25% reduction in patients’ overall body mass. While access, which includes cost, coverage or supply, is a major issue, these medications can be effective if taken long-term. They may be useful for patients who either are not appropriate for bariatric and metabolic surgery or who prefer medication management over surgery. Due to their effective weight loss outcomes and evidence supporting their use in individuals with diabetes, heart disease and heart failure, fatty liver or kidney disease, they may be appropriate in many individuals regardless of bariatric surgery status.
The chief downside for these medications is lifelong adherence to them and the potential loss of lean mass if not exercising and eating adequate nutrition. Patients may experience a range of uncomfortable symptoms such as nausea, vomiting, diarrhea and/or
constipation. There are reports of gastroparesis. In most cases, patients must also make corresponding lifestyle changes with their diet and physical activity level while on these drugs to actualize the kind of weight loss they are hoping to achieve and to avoid developing sarcopenia and osteoporosis.
Additionally, a December 2023 study showed that GLP-1 medications have the potential to eventually be used in contexts outside of medical weight loss, including in the treatment of Alzheimer’s and Parkinson’s disease, heart and kidney disease and for other metabolic conditions.
For patients with a BMI of 35 kg/m² or greater, however, bariatric surgery may be a preferred option as a one-time intervention. There is strong evidence that bariatric surgery has long-term, positive health outcomes, such as the reversal of diabetes and reduction of cancer risk.
In addition, there are serious potential risks of using these newer injectable medications, such as a potential increased risk of tumor growth, pancreatitis, or gastroparesis and they cannot be used in certain populations, including those anticipating pregnancy or individuals with a personal or family history of medullary thyroid cancer, multiple endocrine neoplasia type 2. They should be stopped two months prior to planned pregnancy. They also can increase aspiration risks in those
In cases where patients who opt for surgery and are challenged to keep their weight off following the procedure despite following all the recommended lifestyle modifications, the new GLP-1 drugs offer clinicians a potential additional tool to support patients’ short and long-term health goals .
undergoing anesthesia due to the delayed gastric emptying effect of the medication, and patients must be counselled accordingly. Finally, because they are a newer class of medications, we do not have longterm data on the safety of these medications.
Surgery comes with potential long-term risks, too, that include, for example, nausea, bowel obstruction, malnutrition and ulcers. As with medication management, patients need to be supported through
lifestyle modifications and individual coaching and/or group support for long-term weight reduction.
In cases where patients who opt for surgery and are challenged to keep their weight off following the procedure despite following all the recommended lifestyle modifications, the new GLP-1 drugs offer clinicians a potential additional tool to support patients’ short and long-term health goals.
Using Multi-Institutional Consortiums to Investigate Pediatric Treatment

Brian C. Gulack, MD, MHS, FACS, FAAP, a pediatric surgeon at Rush, serves as Vice Chair of the Pediatric Surgery Research Collaborative (PedSRC), a group of pediatric surgical researchers working to improve the surgical care of pediatric patients. As part of the Collaborative’s work, Dr. Gulack is collaborating on three studies, the goals of which are to improve surgical decisionmaking.
The Papers I trial is an observational study to assess patients’ quality of life after being treated for primary spontaneous pneumothorax (PSP). The trial will also delve into why surgeons choose a particular pleural-based approach during surgical intervention over another, along with surgeons’ perceived risks and benefits of using each approach. Dr. Gulack is the principal investigator on the trial.
Primary spontaneous pneumothorax is a condition that results from the rupture of bullae in the lung in the absence of existing lung pathology or trauma. It most commonly affects adolescents and young adults and is characterized by the acute onset of pain and shortness of breath. If left untreated, PSP can be life-threatening; recurrence is common and can affect up to 50% of patients. In the patient population younger than 18 years, the overall incidence is 5 to10 cases per 100,000 children.
“Unfortunately, PSP is a chronic disease, not an acute process. While we can treat the individual occurrence, the real goal needs to be reducing the rate of recurrence so that our patients can go back to their normal unencumbered lives” Dr. Gulack says.
Although PSP may be managed through observation or a chest tube, recurrence of this condition can be reduced through surgical management. Primarily, surgeons use a stapled wedge resection of the affected lung via a thoracoscopic approach in
combination with a pleural-based procedure. While surgeons may use chemical pleurodesis, mechanical pleurodesis or pleurectomy, there is no agreement on which of the pleural-based approaches should be used.
Several small, single-institution studies have shown that chemical pleurodesis and pleurectomy have reduced rates of recurrence compared to mechanical pleurodesis. However, mechanical pleurodesis remains the most commonly used technique, suggesting that surgeons are not yet sold on this finding.
The multi-institutional collaborative under Dr. Gulack’s leadership has developed a multiphase study that will begin with twin qualitative analyses of patients and providers to develop a better understanding of current opinions regarding the different pleural procedures. The first phase of the trial will begin in mid-2024. It will culminate with a prospective, non-randomized trial to compare the three treatment options (see Figure 1).
Trial Description
Qualitative Analysis of Surgeons’ Perspectives on:
-Procedure Choice
-Perceptions of Outcomes
Qualitative Analysis of Patients’ Perspectives on:
- Fears
- Concerns
- Anxiety of Recurrence
Create Consensus of Optimal Approach
- Delphi process or Expert Panel
- Optimal Approach for Pleurodesis and Pleurectomy
Retrospective Analysis of Center Experience
- Volume - Outcomes
- Data for Power Calculation
High ligation remains an appropriate treatment for indirect inguinal hernias in the adolescent population. Although this approach has demonstrated low rates (between 1%-2%) of long-term recurrence, there are some subpopulations, such as those based on sex, body mass index and athletic history, who may benefit more from a mesh-based floor repair.
Pilot Trial/Feasibility
- Few center trial to prove feasibiity
Prospective Non-Randomized Trial
- Using Optimal Approach
- Primary Outcome Recurrence
Led by Dr. Gulack, who serves as the PI on the study, this hypothesis-generating trial will identify what, if any, patient characteristics predispose adolescents to a rate of recurrence at which time a floor repair with or without mesh should be considered. Furthermore, the study aims to better understand the heterogeneous relationship of age and recurrence after high ligation repair, taking into account sex, body mass index and other patient-specific factors.
The result of a birth defect, an indirect inguinal hernia is a common type of hernia that occurs when abdominal contents protrude through an open internal inguinal ring. Almost all pediatric hernias are of this type. If left untreated, indirect inguinal hernias can develop into incarcerated hernias, which could cause strangulation and eventual death of a portion of the intestines.
Typically, children are treated with a high-ligation repair, where sutures are used to close the peritoneum without repairing the inguinal floor. Adults are usually treated with a floor repair, with or without mesh, that directly repairs the floor of the inguinal canal. Adolescents fall into a gray zone where, although high ligation tends to be the preferred treatment approach in this population, the success of this approach hasn’t been demonstrated universally.
“No one’s exactly sure why high ligation works so well in children and not adults, but just closing the peritoneal layer only works for this group,” Dr. Gulack says. “However, it is unclear at what age we should stop treating patients like children and treat them like adults.”
For populations where recurrence rates for high ligation repair exceed 2%, mesh-based repair may be a more suitable approach. However, the choice of approach has to be weighed against potential complications. For instance, patients may be at a greater risk to develop chronic pain after a meshbased repair.
The trial is multiphase, and the retrospective phase is currently underway. A second phase of the trial to define recurrence rates after high ligation that should prompt a floor repair will begin in mid-2024.
Understanding caregiver preferences for the treatment of pediatric acute appendicitis is one avenue Dr. Gulack and a team of researchers are exploring to bolster collaborative, caregiver-provider communication and hopefully improve overall patient satisfaction with a chosen treatment.
The study, which is expected to begin enrollment in late 2024, will use focus groups with caregivers to gain insight into the reasons why pediatric caregivers prefer appendectomy or nonoperative management.
“Up until about five years ago, everyone who had an inflamed appendix got surgery,” he says. “But we found that certain patients could be treated with antibiotics instead with a high rate of success and low rates of recurrence. If your child had the option of a nonsurgical technique, wouldn’t you want to be told about it?” Dr. Gulack asks.
Appendectomy or non-operative management?
Acute appendicitis is a common surgical emergency that accounts for around 2% of all pediatric surgical admissions in the U.S., totaling approximately 80,000 cases annually. The majority of these cases have historically been treated with appendectomy.
Common complications for patients include bleeding, hernia formation, inability to partake in sports for some time and pain.
Recent studies, however, show that in cases where nonoperative management is used to treat acute appendicitis, between 70% to 85% of those patients had no increase in the incidence of surgery for appendicitis at their two-year follow up. Additionally, children can return to normal activity twice as fast with nonoperative management as compared to surgery, thus resulting in fewer disability days and less expense for patients’ families.
“This is an area where it’s very important to understand what patients want and why, and what barriers to using antibiotic treatment for appendicitis exist,” Dr. Gulack says.
The study, which will examine caregiver decisionmaking, will help Dr. Gulack and his fellow researchers understand what the barriers to implementation of using antibiotics are instead of surgery.
By George Kokosis, MD, and John A. Toms III, MS
History
A female patient in her 40s was initially diagnosed with bilateral ER+ and PR+ invasive lobular carcinoma of the breast. She underwent neoadjuvant chemotherapy, followed by bilateral mastectomy with axillary lymph node dissection and immediate breast reconstruction with permanent silicone implants.
Additionally, she received adjuvant radiation therapy targeting the chest wall and axillary regions. Approximately five months post-mastectomy, the patient presented with complaints of swelling, numbness and pain in her left upper extremity.
Presentation and Examination
The patient exhibited notable swelling in the left upper extremity without signs of cellulitis. Lymphoscintigraphy highlighted delayed uptake and dermal backflow, which suggested grade 2 lymphedema. The results of an upper left extremity MRI corroborated these findings.
Preoperative assessment of the patient’s left extremity lymphedema demonstrated increased swelling, erythema and limb volume compared to her right extremity.
Treatment
The patient's surgical history and presentation were indicative of secondary grade 2 lymphedema, likely secondary to her breast cancer axillary lymphadenectomy and radiation management. Secondary lymphedema is a condition marked by acquired lymphatic dysfunction resulting in proteinrich fluid accumulation, subsequent swelling, fat hypertrophy, tissue fibrosis and limb hypertrophy.

Lymphedema is a progressive and debilitating disease. Treatment of this condition should be centered on palliative symptom relief and disease progression management. After unsuccessful conservative treatment that involved manual lymphatic drainage and compressive garments, I believed surgical intervention was necessary to treat this patient’s early-stage lymphedema.
To achieve both symptomatic improvement and aesthetic outcomes, I incorporated a combination of physiologic and debulking procedures in a staged fashion. Initially, the patient underwent three lymphovenous anastomoses (LVA), while we simultaneously connected functional lymphatic channels to nearby subdermal venules to redirect lymphatic flow into the venous system; this allowed drainage of the lymphatic fluid from the distal arm. Intraoperative SPY imaging fluoroscopy with indocyanine-green (ICG) was used to identify these lymphatic channels and to confirm improved lymphatic flow post-intervention.
Post-lymphovenous anastomosis showed significant improvement of the swelling distally with the wrist bone, which was notable, given that it was the first time this was observed since her lymphedema ensued.
I performed liposuction as a debulking procedure to further reduce excess adipose tissue and limb volume while enhancing the extremity's cosmetic appearance.
I repeated this again about six months later.
Following surgery, the patient reported a marked improvement in her lymphedema symptoms, including reduced swelling, enhanced limb mobility, improved cosmetic appearance and an overall
increase in her quality of life. Recognizing the chronic nature of her condition, a comprehensive, long-term management strategy that includes ongoing lymphedema therapy was established to ensure the continued preservation of these benefits. Post-operative assessment of the left upper extremity demonstrated significant reduction in limb swelling and size with excellent aesthetic outcome. Given the extent of dermal backflow in the proximal arm, we discussed monitoring her symptoms and potentially offering vascularized omental transfer to the left upper extremity as an additional physiologic procedure to help with lymphangiogenesis and drainage of the excess lymphatic fluid.
Breast cancer-related lymphedema represents the most common cause of non-infectious lymphedema in the United States, occurring in up to 25-40% in patients who undergo a combination of axillary lymphadenectomy and radiation therapy.
This case highlights the successful management of lymphedema through a combination of physiologic and debulking procedures. The postoperative outcomes showcase significant symptom improvement, enhanced limb mobility and improved cosmetic appearance. Together, these underscore the potential benefits of surgical intervention in early-stage lymphedema along with lymphedema therapy.
Additionally, the patient may require an additional physiologic procedure (i.e., vascularized omental transfer to the left upper extremity) to further improve her lymphatic drainage and optimize her long-term extremity volume.
A Long Road to Healing
Melissa Byrne's breast reconstruction didn't go as planned — until she got to RUSH .
By Melissa Moore
After Melissa Byrne was diagnosed with breast cancer in 2020, a mastectomy completely removed the cancer. Her surgeon was also able to begin breast reconstruction during the mastectomy.
“I didn’t need chemo or radiation, which was a good thing for me,” Melissa said.
The problems came later: Melissa faced unexpected complications when the surgical wound failed to heal properly.
Setback after setback
Melissa had a second surgery to reverse her failed reconstruction. That turned into a third and fourth. Then, a fifth and sixth. None of the attempts to reconstruct her breast healed properly, and all of them needed to be reversed because of a complication.
After all these surgeries, she was right back where she started: no reconstruction after her mastectomy.
Her original breast surgeon was honest with her.
“He said this is as far as I can go with you — your case is too complex for me,” Melissa said. “But I have the perfect doctor for you at RUSH.”
Melissa had her first appointment with George Kokosis, MD, a plastic surgeon at Rush University Medical Center, in June 2022.
Successful reconstruction, at last
After six failed procedures, Melissa could have given up on reconstruction. But she knew she wanted to live without the visual reminder of her cancer.
“When I got to Dr. Kokosis, I was in a bad place,” Melissa said. “I knew if this wasn’t going to work, then I was going to have to live like this. I felt like an alien in a movie.”
Kokosis works with many patients who have had multiple failed attempts for breast reconstruction. And his experience and confidence were obvious.
“We immediately connected,” Melissa said. “He had done his homework and knew what was going on with me. He spent more than an hour talking to me and hearing my story. After the first appointment, I’m like, OK, I think he’s got this.”
“Like Melissa, a lot of my patients come to see me after failed reconstructions where simple solutions have not worked,” Kokosis said. “She was sent to me because we have expertise in taking care of challenging breast reconstruction cases.”
Kokosis wanted to use Melissa’s own tissue to create a base for her newly reconstructed breast. After discussing the different options, Melissa decided to have tissue from her back used for the reconstruction.
Even after her multiple surgeries, Melissa trusted that Dr. Kokosis would be able to care for her.
“I didn’t go into the surgery totally freaked out,” Melissa said. “He made me comfortable and able to trust the process. And, everything came out just as Dr. Kokosis explained.”
Melissa had a total of three total procedures with Kokosis, and she had no complications during her recovery. Her final procedure in January 2023 marked a complete breast reconstruction.
“Dr. Kokosis and his team have been nothing short of amazing, and I couldn’t have asked for a better surgeon or team working with me,” Melissa said.


Scan the QR code to view more of Melissa’s story
By Sean Wrenn, MD, FACS
An otherwise healthy female patient in her 30s self-referred to RUSH for hyperthyroidism due to a left thyroid nodule. In 2019, she began experiencing worsening panic and anxiety attacks, and she was found to have a suppressed thyroid stimulating hormone (TSH) suggestive of hyperthyroidism. An iodine uptake (thyroid scan) and thyroid ultrasound showed the source of her hyperthyroidism to be an autonomously functioning (“hot” or “toxic”) thyroid nodule on the left side. The nodule was biopsied via fine needle aspiration (FNA) and found to be benign.
Once she was diagnosed, the patient tried a variety of lifestyle changes, such as yoga, exercise and dietary changes, to improve her symptoms. Those changes helped her overall but did not resolve her issues or symptoms, which were intense and reducing her quality of life. She otherwise had no other medical conditions and was on no medications at home. She had no prior surgical history and no significant family history of endocrine or thyroid disorders. She also had no prior history of radiation exposure.
Prior to coming to RUSH in 2022, the patient was advised by multiple thyroid clinicians to pursue conventional treatments such as thyroidectomy, radioactive iodine (RAI), or thyroid-blocking drugs (Methimazole). She declined to pursue those options due to their risk profile and potential lifelong side effects, particularly lifelong endocrine disruption or acquired hypothyroidism. Rather, the patient researched thyroid radiofrequency ablation (RFA), and it was her preferred treatment of choice. However, until Rush University Medical Center offered this treatment in 2021, no other hospital in Chicago offered this approach to treat her condition.
During her physical exam, I noticed the patient had a protuberant thyroid on the left side of her neck, causing cosmetic deformity and easily visible in any neck position. Ultrasound imaging confirmed the patient had multiple
thyroid nodules. She had no overt manifestations of thyrotoxicosis such as tremor, tachycardia, flushing or diaphoresis. She had no evidence of thyroid eye disease or exophthalmos. She was otherwise well appearing with a normal neurological examination.
Imaging Data
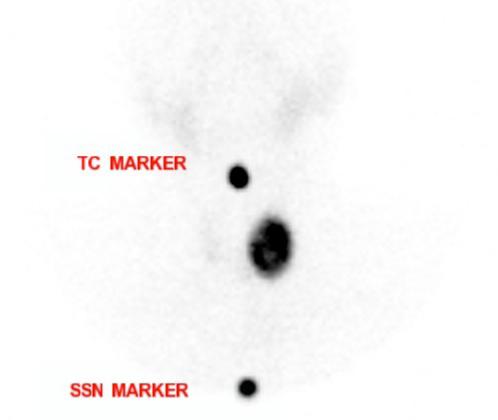
Thyroid uptake and scan
The patient had a thyroid uptake scan, which showed that her 24-hour radioiodine uptake was 39%, which was above the normal upper limit of 30%. There was a large, intense and focal area of increased radioiodine activity in the lower pole of the left lobe of the thyroid. Uptake in the remainder of the thyroid was partially suppressed. The findings were consistent with a toxic left thyroid nodule in the left inferior pole of the thyroid.
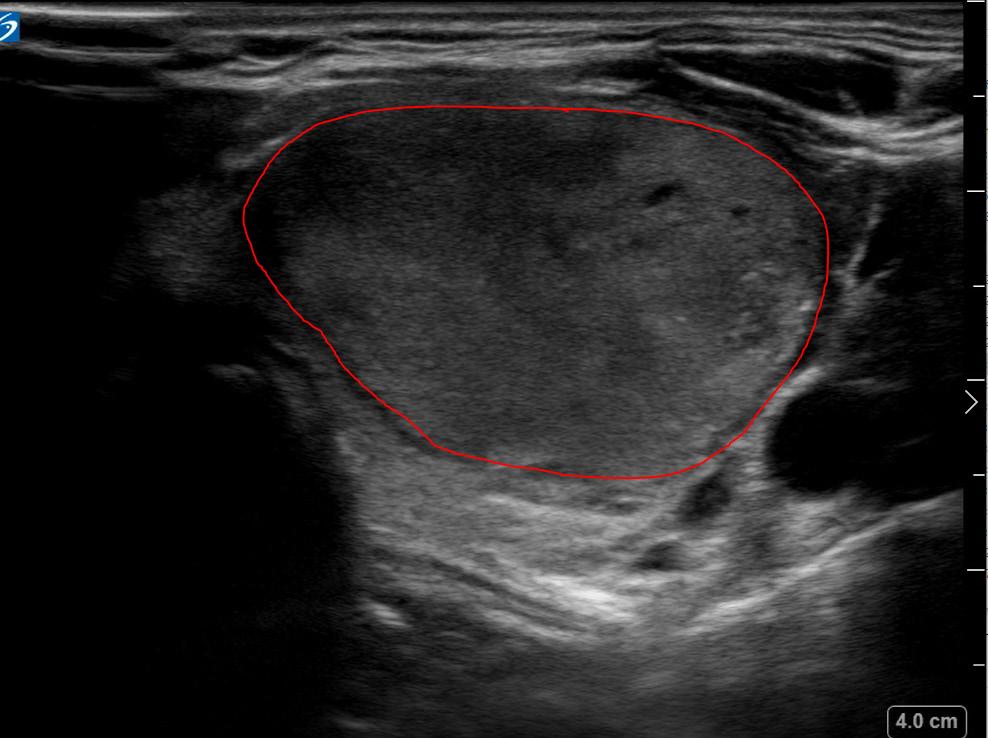
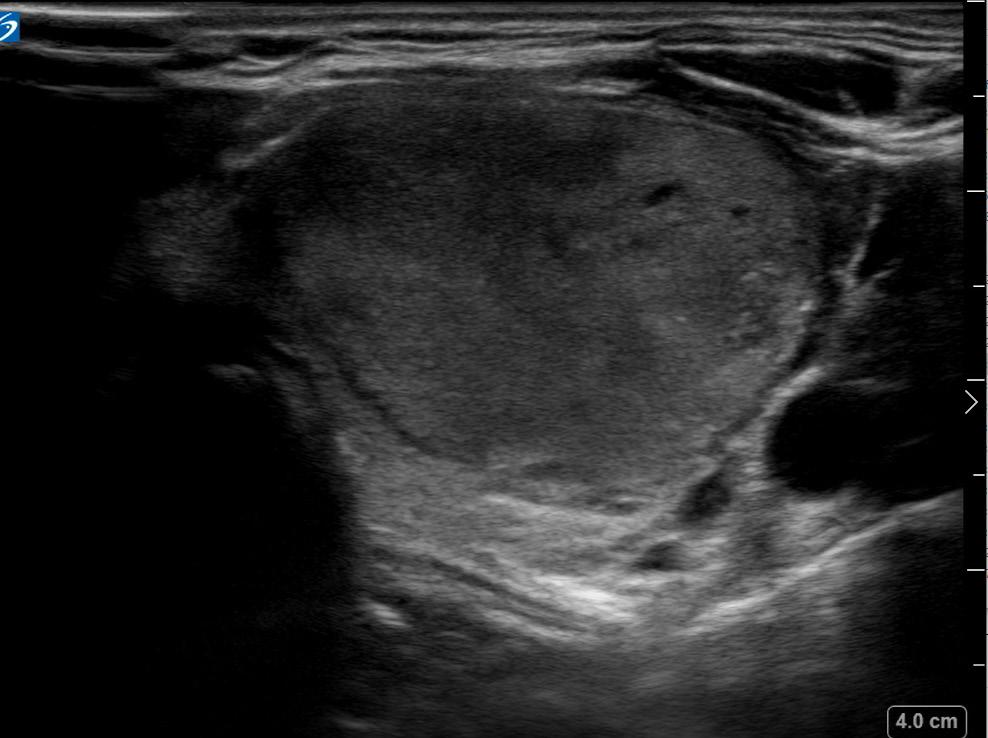
Thyroid Ultrasound
The right lobe was heterogeneous with parenchymal hypervascularity, measuring 4.9 x 1.5 x 1.1 cm. There were three nodules present, all of them less than a centimeter in size. None of the nodules had highly suspicious features. The isthmus also had no significant nodules and was not thickened.
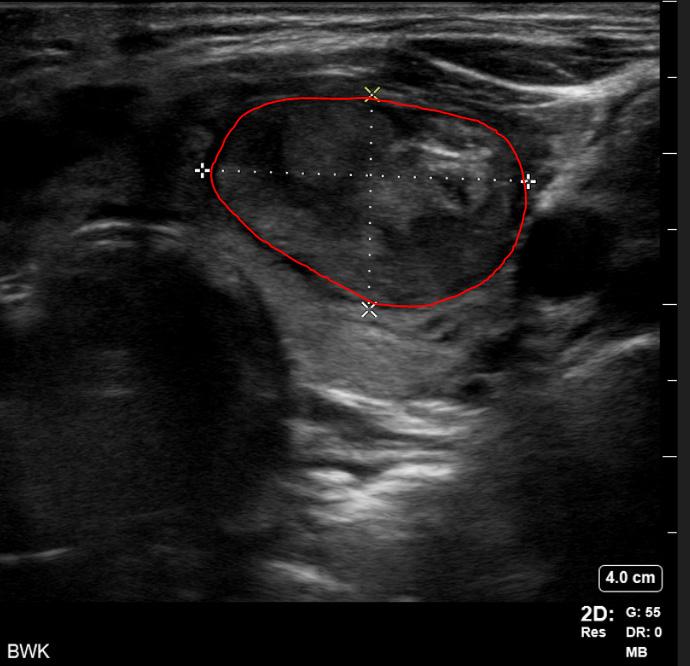
The left lobe was heterogeneous and measured 5.5 x 2.4 x 2.4 cm, with two notable nodules in her left thyroid lobe. There was a smaller mostly cystic nodule, which measured 2.2 x 2.1 x 2.2 cm. She also had a larger heterogeneous,

hypervascular solid nodule that contained internal microcalcification located in the left middle inferior lobe. This nodule measured 3.0 x 3.1 x 2.3 cm (calculated tumor volume = 11.3 mL).
When comparing the imaging to the nuclear medicine iodine scan, the dominant left solid hypervascular nodule appeared to correspond to the area of increased uptake on the thyroid scan, and clinically this was deemed most certainly the hot or toxic nodule.
Laboratory Data
Free T4 1.1 (normal range 0.8-1.5)
TSH <.0008 (undetectable) (normal range 0.4-4.50)
Free T3 3.7 pg/nL (normal range 2.2-4.0 pg/nL)
FNA biopsy of left dominant nodule
The left thyroid nodule underwent a fine needle aspiration which noted normal appearing follicular
cells present, histiocytes, and thyroid colloid. Overall, these cytology findings are consistent with benign goiter (Bethesda class 2), implying a very low risk of cancer (<2%).
Assessment
This otherwise healthy young female presented with a 3 cm autonomously functioning (“hot”) thyroid nodule that was causing distressing symptoms of hyperthyroidism and presented a threat to her long-term health. She had numerous treatment options; however, she was motivated to avoid the risks of radioactive iodine and surgery. She was felt to be a good candidate for radiofrequency ablation of the thyroid nodule, to decrease its size and restore a euthyroid state. I informed her that the procedure had risks, including risk of persistent hyperthyroidism, voice change, nerve injury, infection, bruising or nodule regrowth.
She consented to proceed and was prepared for outpatient RFA.
Treatment
I performed the procedure in the endocrinology clinic as an outpatient. The patient took an oral anxiolytic one hour prior to the procedure. She was then positioned comfortably in the procedure room. I cleaned her neck with chlorhexidine and gently extended and numbed it with cold spray and subdermal lidocaine.
Once the perithyroidal block was completed, the RFA electrode (the size equivalent of an 18-gauge needle) was inserted using ultrasound guidance into the known dominant toxic nodule on the left. Utilizing a transisthmic approach and the “moving shot” technique, I sequentially ablated the dominant left-sided nodule. A maximum of 40 watts was used via a 7 mm active tip electrode, with a total ablation time of about 20 minutes.
I monitored each segment of ablated nodule for hyperechoic “bubbling” visible on ultrasound, and for rising impedance from the electrode generator, to assure adequate ablation throughout. During the critical portion of the procedure, I asked the patient to vocalize to assure that no acute voice changes or hoarseness was observed. None were noted and the patient tolerated the procedure well. A bandage was placed over the needle site and the patient was observed for one hour prior to discharge home. Follow-up was arranged for set intervals (one, three, six and 12 months following the ablation) with ultrasound examination of the nodule and thyroid function lab testing.
Just a few months following the procedure, the patient had completely normal thyroid function restored and is doing very well. Her TSH returned to the normal range following the procedure (1.08)
and she reports that her hyperthyroid symptoms resolved. She feels like the nodule is reducing in size with less compression symptoms in her neck, and she has a more normal neck contour. Volumetric ultrasound analysis of her treated nodule at six months shows that her nodule is now less than 3 mL in volume, a 75% decrease in volume from pre-procedure baseline. Further, the procedure did not cause hypothyroidism necessitating thyroid hormone replacement, a known complication of both surgery and radioactive iodine.
Subclinical hyperthyroidism refers to a state of suppressed TSH levels without elevations in serum thyroxine (T3, T4) levels. It can cause longterm health concerns, such as worsening heart or bone health, and can also cause bothersome symptoms, such as anxiety, poor sleep, weight loss or palpitations. Hyperthyroidism can also be due to
Graves disease or toxic multinodular goiter; however, in cases such as this, a single autonomously functioning or “hot” nodule can be the cause of the problem.
Patients who have toxic thyroid nodules are typically treated with RAI or thyroid lobectomy. RAI is typically considered first-line care, but may not be the best choice for large nodules that are causing compression symptoms or cosmetic deformity of the neck. Thyroid lobectomy, or hemithyroidectomy, is a safe, one- to two-hour outpatient procedure that removes half of the thyroid. It is still considered frontline therapy for large toxic thyroid nodules such as this. Surgery remains an effective and safe treatment for this condition. However, there are significant risks or downsides to thyroidectomy that might make surgery unappealing for certain patients. Risks of thyroidectomy include nerve injury or



voice change (5% short term; 1% longer-term or permanent), hematoma (1%), infection (1%), hypoparathyroidism (0% for lobectomy; 1%-2% risk for a total thyroidectomy). Patients have between a 20% to30% chance of needing thyroid hormone pills after a lobectomy and a 100% chance after a total thyroidectomy.
Additionally, lobectomy or total thyroidectomy leave patients with a scar, unless it is done via a remote access or endoscopic approach. Typically, scars heal well and fade within a year or two, but patients are sometimes not satisfied with the temporary or permanent appearance of their healed scar.
RFA is a newer, minimally invasive treatment that can be an excellent therapeutic option for patients who don’t want to undergo the risks of surgery or RAI. It can be performed in clinic under local anesthesia and takes between 30 to60 minutes to treat large, benign thyroid nodules. In this particular case, the patient’s symptoms resolved almost immediately and her relatively large toxic nodule reduced in size effectively without apparent complication.
There is a very low risk of complication from RFA and no scar is produced. The recovery is often faster than recovery from thyroidectomy, and all patients go home the same day from their clinic-based treatment. Patients may experience a less than a 1% chance of nerve injury. Other rare complications include nodule rupture, infection, hematoma, vagal reaction, Horner syndrome and skin burns. There is also an extremely low risk of damage to internal structures,
such as the esophagus, trachea and carotid artery. Selecting a proceduralist with experience and skill in RFA is essential to a safe procedure.
However, while RAI or surgery produces very high rates to cure a patient’s hyperthyroidism, RFA, at this time, is estimated to be less effective based on cohort studies. An estimated 60% of patients return to normal thyroid functioning after RFA, but in some cases hyperthyroidism might persist leading to potential need for repeat intervention. Toxic nodules treated at RUSH have had an extremely high rate of resolution and normalization of TSH.
In this case, given the patient’s values and goals of care, thyroid RFA was an excellent option for her which allowed her to resolve her symptoms, restore her neck contour and improve her quality of life. She remains scar-free and continues to be on no chronic medications.
Overall, I would highly recommend the use of RFA as a safe and excellent primary option to treat benign, toxic nodules in select patients.

Scan the QR code learn how RFA helps patients
Overall, I would highly recommend the use of RFA as a safe and excellent primary option to treat benign, toxic nodules in select patients .
- Sean Wrenn, MD

How radiofrequency ablation helped Melania Nunez get her confidence back
By Emma Rose Johnson
Steve had been bothering Melania Nunez for four years.
“Steve” is what Nunez calls her thyroid nodule, also known as a goiter or enlargement of the thyroid.
For several years she managed it at home in Cicero, Illinois, with diet, exercise and naturopathic medicine. But after a case of COVID-19 in January, she says the nodule and her symptoms grew worse and became unmanageable.
It was time for Steve to go. And a nonsurgical treatment at Rush University Medical Center was the answer.
Thyroid nodules, typically benign solid masses, can be caused by several conditions. Nunez’s was caused
by Hashimoto’s disease, an autoimmune disorder where the immune system attacks the thyroid and causes it to swell.
The nodule caused Nunez to have trouble breathing and swallowing, and it sapped her energy. But she said the worst symptom was its effect on her selfconfidence after the nodule changed the shape of her face and neck.
“I was not aligned with myself,” she said. “I didn’t like looking at myself in the mirror. I had a profound lack of self-love from having such a large goiter.”
When she was diagnosed in 2018, and at further follow-up visits, her endocrinologist told her the only treatment was partial or full removal of the thyroid. This was going to mean surgery under general anesthesia, followed by recovery and a scar on her
neck. It would potentially mean lifelong medications to replace the hormones that her thyroid made naturally. And it would mean precious time away from her 13-year-old son, who has high-functioning autism, and a major disruption of their daily routine.
“As a special needs mom, I needed to know that there was something available that wasn’t going to interrupt my day-to-day life,” she said.
So she waited for another option.
She first heard about radiofrequency ablation, or RFA, not from one of her physicians, but on Instagram, where she found a video of a physician discussing the procedure as an alternative to surgery for nodule treatment. She spoke with her endocrinologist, who referred her to Sean Wrenn,
I have so much more energy . There is a shift in my labs as well . But most important is my self—confidence . . .RFA has been life changing for me . - Melania Nunez
MD, an endocrine surgeon at RUSH, who offers the procedure alongside standard thyroid surgery.
Instead of surgery, RFA uses electrical impulses to kill off the cells in the nodule. Over time, the nodule then shrinks as the body removes the dead tissue. The procedure uses a needle inserted into the nodule, similar to when a thyroid biopsy is performed.
“It’s an office-based procedure, similar to a regular doctor’s appointment,” Wrenn said. “Many of the patients who’d undergo this have already had a thyroid biopsy before, so they may have an intuitive understanding of what the procedure’s like.”
Patients are awake during the procedure, though the area is numbed. Patients are able to go home the same day and treat any discomfort afterward with over-the-counter pain medication, Wrenn said. If medically possible, he offers both RFA and surgery as options to his patients, to go over the benefits of each.
“Thyroid surgery is very safe and effective, and for some people it’s the right option,” Wrenn said. “I usually talk them through both choices and do a custom approach that works best for them.”
For Nunez, the decision was easy.
“Dr. Wrenn made me feel comfortable, and made me feel safe,” she said. “He listens to you and explains the pros and cons. He said, ‘I can’t assure you 100% resolution, but I can assure you some improvement, and that’s what I needed.”
On April 17, she went in to try to get rid of Steve. Road to recovery
“It is up to a one-year process,” Wrenn said. “I always brace patients that after the procedure the nodule won’t seem any different. Some people will see a lot of changes within the first few months, and then sometimes it will slow down a little after that, but you’ll continue to see effects for up to a year.”
Nunez estimates that since she had her RFA procedure, her nodule has decreased about 30%, which she’s very satisfied with. She looks better and has noted a distinct change in her energy — she has even switched to decaf coffee.
“My eyes have started to look even,” she said. “There isn’t as much pressure when I swallow. I have a neck again, I have a face again. I have so much more energy. There is a shift in my labs as well. But most important is my self-confidence.”
Wrenn said that patients like Nunez who are looking for a nonsurgical option to treat their thyroid nodules should ask their doctors about RFA.
“If folks are worried about general anesthesia or have medical conditions that would put them at higher risk for general anesthesia, RFA helps them get around that,” he said. “It helps them avoid a scar, and it helps them potentially avoid thyroid hormone medication.
“But it’s important to note that surgery may be a better option, or the only option, for other patients, depending on their case.”
Nunez has shared her health experience with followers on social media. She emphasizes that patients, particularly women, should work to advocate for themselves when navigating the health care system.
“RFA has been life-changing for me,” she said. “I would say make sure you ask the questions that need to be asked. It may feel uncomfortable. Feel uncomfortable! But ask the questions. Ask what else may be available to you.”
In July 2024, RUSH and Gift of Hope Organ & Tissue Donor Network will open Illinois’ first hospital-based donor care center — a world-class intensive care and surgical unit for deceased organ donors, staffed with leading clinicians and allied multidisciplinary services to optimize the impact of every organ donation and save more lives.
“This collaboration to open the Gift of Hope Organ Donor Care Center at Rush University Medical Center is a shining example of RUSH’s mission to improve the health of the individuals and diverse communities we serve through the integration of outstanding patient care, education, research and community partnerships,” says Edie Chan, MD, division chief of Rush Transplant.
Donor care centers are dedicated facilities for optimizing donor management and the surgical recovery of lifesaving organs for transplant. They have emerged as a national best practice to
better serve donors and their families, increase the availability of organs for transplant and offer improved transplant outcomes.
“This partnership positions RUSH to be a leader in transplantation and donation,” says Anjali Basu, transplant administrator. “It serves our region and our community partners and advances the mission of RUSH as a system.”
Deceased donors will be transferred from hospitals across Gift of Hope’s donation service area in Illinois and Northwest Indiana to the Gift of Hope Organ Donor Care Center at Rush for specialized, timesensitive clinical management that optimizes each donor’s gifts. Close collaboration with area hospitals will ensure seamless operations transferring deceased donors to the Gift of Hope Organ Donor Care Center at Rush for organ recovery surgery. As a result, this will allow transferring hospitals to use their own ICU beds, operating rooms, ventilators and critical care
staff to care for other patients — while the donation process is managed by specialized clinicians and allied teams at the organ donor care center.
For families of donors, the 24/7 availability of Rush’s dedicated donor care center will expedite the donation process and the ability to proceed with arrangements following a loved one’s loss and lifegiving donation.
The Gift of Hope Organ Donor Care Center at Rush will include six intensive care bays, two operating rooms, and 24/7 medical and allied services dedicated to donor management and recovery. A family lounge and support services will provide a comfortable and caring experience for donors’ families.
“Our organ donation center will continue to build on our long-standing efforts to increase organ and tissue donation and advance equitable access to transplantation throughout the region and nationally,” Chan says.
Gift of Hope is one of only three organ procurement organizations in the nation to work with more than 500 donors and their families in a single year and has recovered more than 30,000 organs since its inception in 1986.
More than 7 million Illinois residents have registered to become donors in the Illinois Organ/Tissue Donor Registry. Fewer than 3% of all individuals who die are medically eligible to donate at the time of their death — making every registered decision critical in the authorization and time-sensitive donation process when donation is a possibility.
To learn more about donation and register as a donor, visit www .giftofhope org and join the Illinois Organ/Tissue Donor Registry or Donate Life Indiana registry .
Our organ donation center will continue to build on our longstanding efforts to increase organ and tissue donation and advance equitable access to transplantation throughout the region and nationally . - Edie Chan, MD
RUSH has been recognized nationally and internationally as a health system leader in health equity. Transplant equity, as part of our overall health equity initiatives, is a strategic priority for our institution.
Our advocacy and partnership with the community, Gift of Hope and the Illinois Transplant Fund have advanced access to transplantation and increased organ donation on both the regional level and national level. RUSH led the initiative in Illinois to advance access to transplantation for undocumented patients. In partnership with Gift of Hope and the Illinois Transplant Fund, RUSH helped to pass state legislation focused on increasing access for undocumented patients seeking transplant services. In addition, RUSH partnered with Gift of Hope to devise novel ways of leveraging insurance coverage to fund transplantation care. These efforts have increased organ donation rates in our region and specifically in communities where organ donation rates have historically lagged.

Curious to learn how RUSH has consistently been a top hospital in organ donation referrals, family approaches and authorized cases for the last several years?
Scan the QR code to find out more.
By Henry Govekar, MD, FACS, FASCRS, George Kokosis, MD, FACS, and Summer Dewdney, MD
History
Prior to coming to Rush, a female patient in her 60s was treated for a stage III, grade 1 anal squamous cell carcinoma in August and September 2021. She received the Nigro protocol-radiation therapy combined with 5-FU and mitomycin-C.
She had anal pain in the perineum, felt a lump in that area and had discharge; a CT scan showed two sinus tracts and small fluid collection. She then presented to RUSH for further consultation.
In late June 2022, Dr. Govekar noted a large 7-8 cm fungating anal mass, which caused the patient a considerable amount of pain. A biopsy of the right perianal mass showed invasive, welldifferentiated anal squamous cell carcinoma. A pelvic MRI performed two weeks later confirmed this diagnosis.
Treatment
In September 2022, Dr. Govekar performed a robotic-assisted abdominoperineal resection to excise the 12 cm tumor; additionally, the patient was given ureteral stents and a permanent stoma. In combination with this part of the surgery, a posterior vaginectomy was performed by Dr. Dewdney to ensure negative margins.


Once the vaginal resection was complete, Dr. Kokosis performed a posterior vaginal and perineal reconstruction with a right pedicled gracilis myocutaneous flap. The skin paddle was used to recreate the missing posterior vaginal wall as well as bridge the gap in the perineal defect. The muscle and subcutaneous fat of the flap were utilized to obliterate the dead space following the abdominoperineal resection. The surgery was successful.
Eight months following the surgery, the patient continues to do well and has no evidence of disease. She also has a well-healed perineal wound and vaginal canal.
Initially, the patient’s recurrent tumor was diagnosed and treated as a fistula. It is uncommon for patients to develop fistulas at the same site where cancer would develop; thus, I was concerned that the patient’s cancer had recurred. Given the poor prognosis of patients with relapsed anal cancer, it’s critical for them and their providers to closely monitor the area posttreatment for any areas that don’t appear completely normal. Although anal cancer accounts for less than 1% of all new cancers diagnosed every year in the U.S., the incidence of this type of cancer has risen about 2% each year over the last decade. Any suspicious area that could indicate relapse should be biopsied and treated as soon as possible.
Once we were able to determine that the patient’s cancer had recurred, we treated it appropriately through a salvage abdominoperineal resection, which has been shown to produce adequate, five-year survival rates at 41.6%.

Division of Colon and Rectal Surgery
Marissa Anderson, Assistant Professor
Henry R Govekar Assistant Professor
John Konen, Assistant Professor
Bruce A Orkin Professor Emeritus
Theodore J Saclarides Professor
Division of General Surgery
(Section of Acute Care Surgery)
Daniel J . Deziel Professor Emeritus
Alexander Doolas Professor Emeritus
Raelene D Kennedy Kim Assistant Professor
Keith W Millikan Professor
Keith M Monson Assistant Professor
Donald D . Nash Assistant Professor
Thea P Price Assistant Professor
Kevin Ricci, Assistant Professor
Harry Richter Associate Professor Emeritus
Nicole Siparsky Associate Professor
Jose M Velasco Professor
Division of Minimally Invasive and Bariatric Surgery
Sylvia Herbozo, PhD, Associate Professor
Jonathan A . Myers Professor
Philip A . Omotosho Associate Professor
Naomi Parrella Associate Professor
Swathi Reddy Assistant Professor
Scott W . Schimpke Assistant Professor
Nicholas Skertich, Instructor
Alfonso Torquati Professor
Benjamin R . Veenstra Associate Professor
Division of Pediatric Surgery
Brian Gulack Assistant Professor
Nathaniel Koo Assistant Professor
Mary Beth Madonna Associate Professor
Srikumar B Pillai Associate Professor
Ami N . Shah Associate Professor
John J Tackett, Assistant Professor
Thomas Weber Professor Emeritus
Division of Plastic and Reconstructive Surgery
John Q Cook Assistant Professor
Gordon Derman Assistant Professor
Matthew Doscher Adjunct Assistant Professor
Alvaro Figueroa Adjunct Assistant Professor
Krista Hardy, Assistant Professor
Keith C . Hood Assistant Professor
Kristin Jacobs, Instructor
Liza Johannesson Adjunct Associate Professor
George Kokosis Assistant Professor
David Kurlander Assistant Professor
Stan Monstrey Adjunct Professor
James Murphy Assistant Professor
Soumya Padala Assistant Professor
Mamtha Raj, Assistant Professor
Tulsi Roy, Assistant Professor
Loren Schechter Professor
Deana S Shenaq Assistant Professor
Karen Tessler Assistant Professor
Christina Tragos Assistant Professor
Robert Walton Adjunct Professor
Norman Weinzweig Professor
Division of Surgical Oncology
Rosalinda Alvarado Assistant Professor
Matthew Dixon, Assistant Professor
Andrea Madrigrano Associate Professor
Cristina M O’Donoghue Assistant Professor
Sam G Pappas Professor
Claudia B . Perez Assistant Professor
Thomas R Witt Associate Professor Emeritus
Sean Wrenn Assistant Professor Division of Transplant Surgery
Lloyd Brown, Associate Professor
Edie Y Chan Professor
Edward F . Hollinger Assistant Professor
Stephen C Jensik Assistant Professor
Oyedolamu Olaitan Associate Professor
Erik Schadde Associate Professor
Nathalie Sela Assistant Professor Research
Katrien Corbeels, Adjunct Assistant Professor
Kajal Gupta Assistant Professor
Department of Surgery (Includes Cook County faculty and any faculty member not tied to a division or section)
Ariane Abcarian Assistant Professor
Amna Khokar Assistant Professor
Bashar Attar Professor
Steven Bonomo Assistant Professor
William Brigode Assistant Professor
Cynthia Brincat Professor
Caroline Butler Assistant Professor
Fadi Dahdaleh Adjunct Assistant Professor
Andrew Dennis Associate Professor
Erin Farlow Assistant Professor
Jacqueline Harrison Assistant Professor
Daniel Kacey Assistant Professor
Matthew J . Kaminsky Assistant Professor
Richard Keen Assistant Professor
Syed I . Khalid Adjunct Instructor
Thomas Komar Assistant Professor
Kristina Kramer Assistant Professor
Gianluca Lazzaro Assistant Professor
James Lubawski Assistant Professor
Minh B . Luu Adjunct Associate Professor
Gerald Lynch Assistant Professor
Kristine Makiewicz Assistant Professor
Brian McCann Adjunct Assistant Professor
Nathalie Mantilla Assistant Professor
Elizabeth Marcus Assistant Professor
Thomas Messer Assistant Professor
Patrick L . Molt Adjunct Professor
Jennifer Rickard Adjunct Assistant
Professor
Margaret Rigamer Assistant Professor
Victoria Schlanser Assistant Professor
Neha Sheng Assistant Professor
Kathryn A . Solka Assistant Professor
Frederic Starr Assistant Professor
Irving Waxman Professor
Julie Wescler Assistant Professor
Kenya Williams Assistant Professor
PGY-5 (Chief Residents)
Elizabeth Anderson
Joel Braverman
Miles Grunvald
Cheryl Hornsby
Seungjun Kim
Amanda MacQuoid
Niel Page
Joshua Underhill
PGY-4
Samantha Demoss
Andrew Donaldson
Jemma Flood
Chassidy Grimes
Tyan Kuhn
Jacky Kwong
Lilia Lunt
Melissa Rangel
Maya Volodarskaya
Michael Williams
PGY-3
Talib Chaudhry
Alison Coogan
Samantha Demoss
Jemma Flood
Sarah Keshwani
Vaishnavi Krishnan
Melissa Goczalk
Juan Garcia Macias
David Mondeschein
Oliver Ralph
Gwyneth Sullivan
PGY-2
Julia Alexieva
Maria Benavidez
Samantha Betman
Airirel Bouie
Santiago Ceron
Jaimie Chang
Emily Hejna
Lisvette Hernandez Cobian
Stephanie Trautman
PGY-1 Categorical
Marc Altimari
Joseph Atangan
Sierra Broad
McKenna Chalman
Mary Coomes
Arthur Cross Najafi
Keri Denson
Alex Nadelman
Ashley Roberts
PGY-1 Preliminary/Specialty Categorical
Omar Alrashid
Mustafa Farooqi
Mason Forchetti
Hannah Forristall
Tamar Gordis
Neil Jain
Puja Laroia
Anjali Mehta
Joe Puthumana
Ramiz Memon
Samuel Schick
Derron Yu
John Atcheson – IR
Shivraj Grewal – IR
Subhash Gutti – IR
Cassidy Williams - IR
LAB
John Sincavage
Sarah Beckwith
Lindsay Frieman
Jimmie Knight
Savan Shah
Johanna Stecher
Integrated Plastic and Reconstructive Surgery
Residency Program
PGY-6 Chief Resident
Marek Hansdorfer
PGY-5
Charalampos (Harry) Siotos
Aaron Wiegmann
PGY-4
Brandon Alba
RESEARCH
Elizabeth (Liz) O’Neill
PGY-3
Idanis Perez- Alvarez
Ian Nolan
Jaime Pardo Palau
PGY-2
Sydney Horen Arnold
Teresa Veselack
PGY-1
Elise Hogan
Sabrina Wang
Alba B, Weinstein B, Arnold SH, Jacobs KM, Schechter L. The Use of Acellular Tissue Matrices in Gender-Affirming Surgery: Review of the Literature and Institutional Experience. Adv Biol (Weinh). 2023 Dec 5:e2300507. doi: 10.1002/adbi.202300507. Online ahead of print.
Alsayid M, Taftaf A, Harmouch KM, Alabkaa A, Pappas SG, Singh A. Sarcoidosis of the Bile Duct. ACG Case Rep J. 2023 Feb 1;10(1):e00964. doi: 10.14309/crj.0000000000000964. eCollection 2023 Jan.
Armstrong KA, Kang A, Kuzon WM, Peters BR, Laungani AT, Schechter LS. “Regret after Gender-Affirming Surgery: A Multidisciplinary Approach to a Multifaceted Patient Experience”. Plast Reconstr Surg. 2023 Oct 3. doi: 10.1097/PRS.0000000000011115. Online ahead of print.
Arnold SH, Figueroa AA, Wiegmann AL, Lee J, Padala S, Hamati F, Hansdorfer MA, Tragos C. Long-Term Outcomes After External Maxillary Distraction Surgery in Patients With Down Syndrome. J Craniofac Surg. 2023 Mar 8. doi: 10.1097/SCS.0000000000009203. Online ahead of print.
Arnold SH, Harmon KA, Jazayeri HE, Figueroa AA, Tragos C. TMJ Ankylosis Following Mandibular Distraction Osteogenesis: Management With Simultaneous Midface External Distraction and Bilateral Temporomandibular Joint Replacement. J Craniofac Surg. 2023 May 29. doi: 10.1097/SCS.0000000000009444. Online ahead of print.
Balbale SN, Schäfer WLA, Davis TL, Blake SC, Close S, Sullivan GA, Reiter AJ, Hu AJ, Smith CJ, Wilberding MJ, Johnson JK, Holl JL, Raval MV. A mixed-method approach to generate and deliver rapid-cycle evaluation feedback: lessons learned from a multicenter implementation trial in pediatric surgery. Implement Sci Commun. 2023 Jul 18;4(1):82. doi: 10.1186/ s43058-023-00463-x.
Canady J, Murthy SRK, Zhuang T, Gitelis S, Nissan A, Ly L, Jones OZ, Cheng X, Adileh M, Blank AT, Colman MW, Millikan K, O’Donoghue C, Stenson KM, Ohara K, Schtrechman G, Keidar M, Basadonna G. The First Cold Atmospheric Plasma Phase I Clinical Trial for the Treatment of Advanced Solid Tumors: A Novel Treatment Arm for Cancer. Cancers (Basel). 2023 Jul 20;15(14):3688. doi: 10.3390/cancers15143688.
Carter M, Prendergast F, Krauss J, Zeineddin S, Pitt JB, Sullivan GA, Abdullah F, Gulack BC, Goldstein SD. Evaluating Skeletal Maturity at Time of Surgical Correction of Pectus Excavatum Based on Medial Clavicle Epiphyseal Ossification. Am Surg. 2023 Oct 12:31348231207296. doi: 10.1177/00031348231207296. Online ahead of print.
Chaudhry T, Krishnan V, Donaldson AE, Palmisano ZM, Basu S, Geissen NM, Karush JM, Alex GC, Borgia JA, Liptay MJ, Seder CW. Conditional survival analysis of patients with resected non-small cell lung cancer. JTCVS Open. 2023 Sep 18;16:948-959. doi: 10.1016/j.xjon.2023.09.010. eCollection 2023 Dec.
Cheng L, Lashmanova N, Reddy SB, Yan L, Gattuso P. Histopathological Findings in Hernia Sacs: A Clinical and Pathological Review. Int J Surg Pathol. 2023 Jun 8:10668969231177706. doi: 10.1177/10668969231177706. Online ahead of print.
Cheng L, Tariq H, Yan L, Reddy SB, Gattuso P. Fine-needle aspiration of intramammary lymph nodes: a clinical, radiographic, and cytologic review. J Am Soc Cytopathol. 2023 Jan-Feb;12(1):41-47. doi: 10.1016/j. jasc.2022.09.004. Epub 2022 Sep 22.
Chu JJ, Nelson JA, Kokosis G, Haglich K, McKernan CD, Rubenstein R, Vingan PS, Allen RJ, Coriddi MR, Dayan JH, Disa JJ, Mehrara BJ, Matros E. A Cohort Analysis of Early Outcomes After Alloderm, FlexHD, and SurgiMend Use in Two-Stage Prepectoral Breast Reconstruction. Aesthet Surg J. 2023 Aug 8:sjad246. doi: 10.1093/asj/sjad246. Online ahead of print.
Coogan AC, Lunt LG, Keshwani SS, Sandhu O, Zhang Y, O’Donoghue C, Madrigrano A. Screening Practices for Breast and Nonbreast Cancers in High-Risk Mutation Carriers. J Surg Res. 2023 Nov;291:388-395. doi: 10.1016/j.jss.2023.06.001. Epub 2023 Jul 27.
Coogan AC, Lunt LG, O’Donoghue C, Keshwani SS, Madrigrano A. Efficacy of Targeted Axillary Dissection With Radar Reflector Localization Before Neoadjuvant Chemotherapy. J Surg Res. 2023 Dec 13;295:597-602. doi: 10.1016/j.jss.2023.11.061. Online ahead of print.
Coogan AC, Williams MD, Krishnan V, Skertich NJ, Becerra AZ, Schimpke S, Torquati A, Omotosho P. Ursodiol Prescriptions Following Bariatric Surgery: National Prescribing Trends and Outcomes. Obes Surg. 2023 Aug;33(8):2361-2367. doi: 10.1007/s11695-023-06710-3. Epub 2023 Jul 1.
Coon D, Morrison SD, Morris MP, Keller P, Bluebond-Langner R, Bowers M, Brassard P, Buncamper ME, Dugi D 3rd, Ferrando C, Gast KM, McGinn C, Meltzer T, Monstrey S, Özer M, Poh M, Satterwhite T, Ting J, Zhao L, Kuzon WM, Schechter L. Gender-Affirming Vaginoplasty: A Comparison of Algorithms, Surgical Techniques and Management Practices across 17 High-volume Centers in North America and Europe. Plast Reconstr Surg Glob Open. 2023 May 30;11(5):e5033. doi: 10.1097/ GOX.0000000000005033. eCollection 2023 May.
Coughlin JM, Terranella SL, Ritz EM, Xu TQ, Tierney JF, Velasco JM, Myers JA. Understanding Opioid Prescribing Practices of Resident Physicians. Am Surg. 2023 May;89(5):1554-1560. doi: 10.1177/00031348211060412. Epub 2021 Dec 31.
D’Angelica MI, Ellis RJ, Liu JB, Brajcich BC, Gönen M, Thompson VM, Cohen ME, Seo SK, Zabor EC, Babicky ML, Bentrem DJ, Behrman SW, Bertens KA, Celinski SA, Chan CHF, Dillhoff M, Dixon MEB, FernandezDel Castillo C, Gholami S, House MG, Karanicolas PJ, Lavu H, Maithel SK, McAuliffe JC, Ott MJ, Reames BN, Sanford DE, Sarpel U, Scaife CL, Serrano PE, Smith T, Snyder RA, Talamonti MS, Weber SM, Yopp AC, Pitt HA, Ko CY. Piperacillin-Tazobactam Compared With Cefoxitin as Antimicrobial
Prophylaxis for Pancreatoduodenectomy: A Randomized Clinical Trial. JAMA. 2023 May 9;329(18):1579-1588. doi: 10.1001/jama.2023.5728.
Daniels P, Cassoday S, Gupta K, Giurini E, Leifheit ME, Zloza A, Marzo AL. Intratumoral Influenza Vaccine Administration Attenuates Breast Cancer Growth and Restructures the Tumor Microenvironment through Sialic Acid Binding of Vaccine Hemagglutinin. Int J Mol Sci. 2023 Dec 22;25(1):225. doi: 10.3390/ijms25010225.
Eddy K, Gupta K, Pelletier JC, Isola AL, Marinaro C, Rasheed MA, Campagnolo J, Eddin MN, Rossi M, Fateeva A, Reuhl K, Shah R, Robinson AK, Chaly A, Freeman KB, Chen W, Diaz J, Furmanski P, Silk AW, Reitz AB, Zloza A, Chen S. A SPONTANEOUS MELANOMA MOUSE MODEL APPLICABLE FOR A LONGITUDINAL CHEMOTHERAPY AND IMMUNOTHERAPY STUDY. J Invest Dermatol. 2023 Mar 28:S0022202X(23)01951-6. doi: 10.1016/j.jid.2023.03.1664. Online ahead of print.
Erickson SG, Siparsky NF. Assessing Communication Quality in the Intensive Care Unit. Am J Hosp Palliat Care. 2023 Oct;40(10):1058-1066. doi: 10.1177/10499091221139427. Epub 2022 Nov 11.
Figueroa AA, Harmon KA, Arnold S, Xu H, Roy T, Reid RR, Tragos C. The Role of Digital Surgical Planning and Surgical Guides in the Treatment of Unilateral Condylar Hyperplasia. J Craniofac Surg. 2023 Oct 27. doi: 10.1097/SCS.0000000000009778. Online ahead of print.
Gasteratos K, Vlachopoulos N, Kokosis G, Goverman J. Efficacy and Safety of Microsurgical Pharyngolaryngeal and Pharyngoesophageal Reconstruction: A Systematic Review of the Literature. Plast Reconstr Surg Glob Open. 2023 Apr 27;11(4):e4958. doi: 10.1097/ GOX.0000000000004958. eCollection 2023 Apr.
Goldufsky JW, Daniels P, Williams MD, Gupta K, Lyday B, Chen T, Singh G, Kaufman HL, Zloza A, Marzo AL. Attenuated Dengue virus PV001-DV induces oncolytic tumor cell death and potent immune responses. J Transl Med. 2023 Jul 19;21(1):483. doi: 10.1186/s12967-023-04344-8.
Gulack BC, Shah AN. Letter to the Editor: Alternative Stomal Closure Technique. J Pediatr Surg. 2023 Nov 17:S0022-3468(23)00689-9. doi: 10.1016/j.jpedsurg.2023.11.005. Online ahead of print.
Hamidian Jahromi A, Arnold S, Konofaos P. APPLICATIONS OF VISCOELASTIC TESTING IN MICROSURGERY: A SYSTEMIC REVIEW AND META-ANALYSIS. Georgian Med News. 2023 Apr;(337):6-12.
Hamidian Jahromi A, Arnold SH, Bonett AM, Schechter LS, Dorafshar AH. Laryngochondroplasty: A Systematic Review of Safety, Satisfaction, and Surgical Techniques. Plast Reconstr Surg. 2023 Apr 1;151(4):857-866. doi: 10.1097/PRS.0000000000010010. Epub 2022 Dec 9.
Hamidian Jahromi A, Ferraro J, Arnold SH, Schechter LS, Dorafshar AH.
Chondrolaryngoplasty with Endoscopic Direct Visualization of the Vocal Cords: Demonstration of Technique. Plast Reconstr Surg. 2023 Mar 3. doi: 10.1097/PRS.0000000000010337. Online ahead of print.
Hansdorfer MA, Sadowsky RL, Horen SR, Becerra AZ, Shenaq DS, Kokosis G. Safety and Efficacy of Extended Postdischarge Venous Thromboembolism Prophylaxis in Microsurgical Breast Reconstruction. Plast Reconstr Surg Glob Open. 2023 Feb 27;11(2):e4839. doi: 10.1097/ GOX.0000000000004839. eCollection 2023 Feb.
Harmon KA, Fegan A, La-Anyane O, Theis SM, Tragos C. Uvular Dermoid Cyst: More Than Just a Lump in the Throat-Management of Resultant Velopharyngeal Insufficiency. J Craniofac Surg. 2023 May 29. doi: 10.1097/ SCS.0000000000009425. Online ahead of print.
Hejna E, Price T. Dr. Olga Jonasson: A Pioneer for Women in Surgery. Am Surg. 2023 Apr;89(4):528-532. doi: 10.1177/00031348211054558. Epub 2021 Nov 8.
Herbozo S, Brown KL, Burke NL, LaRose JG. A Call to Reconceptualize Obesity Treatment in Service of Health Equity: Review of Evidence and Future Directions. Curr Obes Rep. 2023 Mar;12(1):24-35. doi: 10.1007/ s13679-023-00493-5. Epub 2023 Feb 2.
Jazayeri HE, Lopez J, Khavanin N, Xun H, Lee UK, Best DL, Reategui A, Urata MM, Dorafshar AH. Comparative Benefits of Open versus Closed Reduction of Condylar Fractures: A Systematic Review and MetaAnalysis. Plast Reconstr Surg. 2023 Apr 1;151(4):664e-672e. doi: 10.1097/ PRS.0000000000010009. Epub 2022 Dec 9.
King CA, Bartholomew AJ, Dabic S, Sogunro O, Perez-Alvarez IM, Welschmeyer AF, Sosin M, Thibodeau RM, Fan KL, Song DH, Greenwalt IT, Tousimis EA. Nipple-Sparing Mastectomy With Immediate Reconstruction After Breast-Conserving Therapy and Radiation: Complications and Oncologic Safety. Ann Plast Surg. 2023 Dec 1;91(6):709-714. doi: 10.1097/ SAP.0000000000003692. Epub 2023 Sep 4.
La-Anyane O, Alba BE, Harmon KA, To J, Siotos C, Adepoju J, Madrigrano A, Alvarado R, O’Donoghue C, Perez CB, Kurlander DE, Shenaq DS, Kokosis G. United States insurance coverage of immediate lymphatic reconstruction. J Surg Oncol. 2023 Nov 29. doi: 10.1002/jso.27512. Online ahead of print.
Larsen CG, Schaffler BC, Neufeld EV, Alba B, Doering TA, Chen YH, Kasabian AK, Nellans KW, Lane LB, Grande DA. The Effects of Autologous Fat Transfer in an In Vitro Model of Basal Joint Osteoarthritis. J Hand Surg Am. 2023 Apr;48(4):406.e1-406.e9. doi: 10.1016/j.jhsa.2021.11.011. Epub 2021 Dec 30.
Mann A, Shah AN, Thibodeau PS, Dyrbye L, Syed A, Woodward MA,
Thurmon K, Jones CD, Dunbar KS, Fainstad T. Online Well-Being Group Coaching Program for Women Physician Trainees: A Randomized Clinical Trial. JAMA Netw Open. 2023 Oct 2;6(10):e2335541. doi: 10.1001/ jamanetworkopen.2023.35541.
Markewych A, Hansdorfer M, Blank A, Kokosis G, Kurlander DE. Forequarter Amputation: Reconstruction With Targeted Muscle Reinnervation to the Filet of Forearm Free Flap. Tech Hand Up Extrem Surg. 2023 Jan 10. doi: 10.1097/BTH.0000000000000424. Online ahead of print.
Mony MP, Harmon KA, Hess R, Dorafshar AH, Shafikhani SH. An Updated Review of Hypertrophic Scarring. Cells. 2023 Feb 21;12(5):678. doi: 10.3390/ cells12050678.
Najafali D, Camacho JM, Galbraith LG, Reiche E, Dorafshar AH, Morrison SD. Ask and You Shall Receive: OpenAI ChatGPT Writes us an Editorial on Using Chatbots in Gender Affirmation Surgery and Strategies to Increase Widespread Adoption. Aesthet Surg J. 2023 Apr 25:sjad119. doi: 10.1093/asj/ sjad119. Online ahead of print.
Najafali D, Camacho JM, Reiche E, Galbraith L, Morrison SD, Dorafshar AH. Truth or Lies? The Pitfalls and Limitations of ChatGPT in Systematic Review Creation. Aesthet Surg J. 2023 Apr 5:sjad093. doi: 10.1093/asj/ sjad093. Online ahead of print.
Najafali D, Dorafshar AH. Commentary on: Evaluating Chatbot Efficacy for Answering Frequently Asked Questions in Plastic Surgery: A ChatGPT Case Study Focused on Breast Augmentation. Aesthet Surg J. 2023 Jun 8:sjad186. doi: 10.1093/asj/sjad186. Online ahead of print.
Najafali D, Reiche E, Camacho JM, Morrison SD, Dorafshar AH. Let’s Chat About Chatbots: Additional Thoughts on ChatGPT and its Role in Plastic Surgery Along With its Ability to Perform Systematic Reviews. Aesthet Surg J. 2023 Mar 11:sjad056. doi: 10.1093/asj/sjad056. Online ahead of print.
Nolan IT, Farajzadeh MM, Boyd CJ, Bekisz JM, Gibson EG, Salibian AA. Do we need acellular dermal matrix in prepectoral breast reconstruction? A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2023 Sep 21;86:251-260. doi: 10.1016/j.bjps.2023.09.042. Online ahead of print.
Nolan IT, Vranis NM, Levine JP. Utilizing augmented reality for Deep Inferior Epigastric Artery Perforator (DIEP) flap perforator selection. Microsurgery. 2023 Mar;43(3):300-301. doi: 10.1002/micr.31012. Epub 2023 Feb 3.
Nolan IT, Weinstein B, Schechter L. Low Rate of Regret After GenderAffirming Mastectomy Highlights a Double Standard. JAMA Surg. 2023 Oct 1;158(10):1077. doi: 10.1001/jamasurg.2023.3358.
Nowicki C, Ray L, Engen P, Madrigrano A, Witt T, Lad T, Cobleigh M, Mutlu
EA. Comparison of gut microbiome composition in colonic biopsies, endoscopically-collected and at-home-collected stool samples. Front Microbiol. 2023 Jun 1;14:1148097. doi: 10.3389/fmicb.2023.1148097. eCollection 2023.
Papakonstantinou M, Siotos C, Gasteratos KC, Spyropoulou GA, Gentile P. Autologous Platelet-Rich Plasma Treatment for Androgenic Alopecia: A Systematic Review and Meta-Analysis of Clinical Trials. Plast Reconstr Surg. 2023 May 1;151(5):739e-747e. doi: 10.1097/PRS.0000000000010076. Epub 2022 Dec 19.
Patel AA, Marquez JL, Agarwal CA, Gallagher S, Schechter LS. A Summary of WPATH Standards of Care 8 th Edition for Gender Affirming Plastic Surgery. Plast Reconstr Surg. 2023 Nov 7. doi: 10.1097/ PRS.0000000000011192. Online ahead of print.
Petit HJ, Sullivan GA, Hughes IM, Pittman KL, Myers JA, Cocoma SM, Gulack BC, Shah AN. Exploring Barriers and Facilitators to Reducing the Environmental Impact of the Operating Room. J Surg Res. 2023 Aug 26;292:197-205. doi: 10.1016/j.jss.2023.07.045. Online ahead of print.
Price T. Use of a synthetic hybrid-scale fiber matrix in the management of chronic and complex wounds: a retrospective case series. Wounds. 2023 Jun;35(6):E197-E202.
Ralph O, Sullivan G, Chan E, Olaitan OK. Environmental Benefits of Electronic Table of Contents of Journals Over Print. Cureus. 2023 Oct 29;15(10):e47907. doi: 10.7759/cureus.47907. eCollection 2023 Oct.
Ralph OG, Siparsky NF. Necrotizing Vaginitis in a 45-Year-Old Woman With Metastatic Breast Cancer. Am Surg. 2023 May 5:31348231173962. doi: 10.1177/00031348231173962. Online ahead of print.
Rivera Z, Escutia C, Madonna MB, Gupta KH. Biological Insight and Recent Advancement in the Treatment of Neuroblastoma. Int J Mol Sci. 2023 May 9;24(10):8470. doi: 10.3390/ijms24108470.
Roblee C, Hamidian Jahromi A, Ferragamo B, Radix A, De Cuypere G, Green J, Dorafshar AH, Ettner R, Monstrey S, Schechter L. “Gender Affirmative Surgery: A collaborative approach between the surgeon and mental health professional”. Plast Reconstr Surg. 2023 Feb 27:e010326. doi: 10.1097/PRS.0000000000010326. Online ahead of print.
Seu MY, Aminzada A, Harmon KA, Guidetti M, Espinoza Orías AA, Figueroa AA, Tragos C. Spontaneous Closure of Congenital Cranial Defect: Is Early Surgical Intervention Warranted?. J Craniofac Surg. 2023 Jan-Feb 01;34(1):e96-e98. doi: 10.1097/SCS.0000000000009117. Epub 2022 Nov 15.
Seu MY, Esmaeeli S, Wiegmann AL, Akin J, Jaraczewski T, Dadrass F, Xu TQ, Dorafshar AH, Shenaq D. Nationwide Bibliometric Analysis of Integrated Plastic Surgery Program Directors. Plast Reconstr Surg Glob Open. 2023 Jan 10;11(1):e4711. doi: 10.1097/GOX.0000000000004711. eCollection 2023 Jan.
Siotos C, Amizanda A, Whitney N, Najafali D, Toms J, Mpontozis A, Kokosis G, Shenaq D, Derman G, Dorafshar AH, Kurlander D. Trends of Medicare Reimbursement Rates for Lower Extremity Procedures. J Reconstr Microsurg. 2023 Aug 29. doi: 10.1055/a-2161-7947. Online ahead of print.
Siotos C, Arnold SH, Aminzada A, Sadowsky RL, Siotou K, Kurlander DE, Kokosis G, Shenaq DS, Dorafshar AH. Pressure injuries in COVID-19 patients: A tertiary center experience. J Plast Reconstr Aesthet Surg. 2023 May 18;83:89-93. doi: 10.1016/j.bjps.2023.05.028. Online ahead of print.
Siotos C, Ferraro J, Arnold SH, Siotou K, Lopez J, Dorafshar AH. The Burden of COVID-19 on Surgeons’ Financial Relationship with the Industry. Plast Reconstr Surg Glob Open. 2023 Feb 17;11(2):e4825. doi: 10.1097/ GOX.0000000000004825. eCollection 2023 Feb.
Siotos C, Underhill JM, Sykes J, Jones KB, Schechter L, Dorafshar AH, Hamidian Jahromi A. Trends of Medicare reimbursement rates for gender affirmation procedures. J Sex Med. 2023 Dec 6:qdad160. doi: 10.1093/ jsxmed/qdad160. Online ahead of print.
Song S, Park KM, Parmeshwar N, Dugi D, Schechter L, Berli JU, Kim EA; Group GAS Research. Developing Gender-Affirming Surgery Curricula for Plastic Surgery Residency and Fellowship via Delphi Consensus. Plast Reconstr Surg. 2023 Apr 20. doi: 10.1097/PRS.0000000000010569. Online ahead of print.
Sulejmani P, Lunt L, Mazur M, Coogan A, Steuer A, O’Donoghue C, Madrigrano A. Enhanced Recovery After Surgery and Postoperative Nausea and Length of Stay in Mastectomy Patients With Reconstruction. J Surg Res. 2023 Sep;289:158-163. doi: 10.1016/j.jss.2023.02.003. Epub 2023 Apr 27.
Sullivan GA, Harmon K, Gill-Wiehl GF, Kim S, Velasco JM, Chan EY, Schimpke SW. Measuring Impact of Simulation-Based Informed Consent Training on Surgical Intern’s Long-Term Confidence. J Surg Educ. 2023 Mar 24:S1931-7204(23)00074-0. doi: 10.1016/j.jsurg.2023.02.018. Online ahead of print.
Sullivan GA, Huang LW, Schäfer WLA, Tian Y, Reiter AJ, Essner B, Hu A, Ingram MC, Balbale S, Johnson JK, Holl JL, Raval MV. Association of Multimodal Pain Control with Patient-Reported Outcomes in Children Undergoing Surgery. J Pediatr Surg. 2023 Feb 18:S0022-3468(23)00149-5. doi: 10.1016/j.jpedsurg.2023.02.028. Online ahead of print.
Sullivan GA, Petit HJ, Reiter AJ, Westrick JC, Hu A, Dunn JB, Gulack BC, Shah AN, Dsida R, Raval MV. Environmental Impact and Cost Savings of Operating Room Quality Improvement Initiatives: A Scoping Review. J Am Coll Surg. 2023 Feb 1;236(2):411-423. doi: 10.1097/ XCS.0000000000000478. Epub 2022 Nov 30.
Sullivan GA, Reddy S, Reiter AJ, Zeineddin S, Visenio M, Hu A, Mackersie R, Kabre R, Raval MV, Stey AM. Does Trauma Center Volume Account for the Association Between Trauma Center Verification Level and In-Hospital Mortality among Children Injured by Firearms in California?. J Am Coll Surg. 2023 Nov 1;237(5):738-749. doi: 10.1097/XCS.0000000000000818. Epub 2023 Aug 15.
Sullivan GA, Reiter AJ, Hu A, Smith C, Storton K, Gulack BC, Shah AN, Dsida R, Raval MV. Operating Room Recycling: Opportunities to Reduce Carbon Emissions Without Increases in Cost. J Pediatr Surg. 2023 Apr 23:S0022-3468(23)00253-1. doi: 10.1016/j.jpedsurg.2023.04.011. Online ahead of print.
Sullivan GA, Sincavage J, Reiter AJ, Hu AJ, Rangel M, Smith CJ, Ritz EM, Shah AN, Gulack BC, Raval MV. Disparities in Utilization of Same-Day Discharge Following Appendectomy in Children. J Surg Res. 2023 Mar 17;288:1-9. doi: 10.1016/j.jss.2023.02.033. Online ahead of print.
Sullivan GA, Skertich NJ, Jones KB, Williams M, Gulack BC, Shah AN. An Infant with COVID-19-Associated Intussusception. Am Surg. 2023 Nov;89(11):4921-4922. doi: 10.1177/00031348211047456. Epub 2021 Sep 22.
Sutthatarn P, Lapidus-Krol E, Smith C, Halaweish I, Rialon K, Ralls MW, Rentea RM, Madonna MB, Haddock C, Rocca AM, Gosain A, Frischer J, Piper H, Goldstein AM, Saadai P, Durham MM, Dickie B, Jafri M, Langer JC. Hirschsprung-associated inflammatory bowel disease: A multicenter study from the APSA Hirschsprung disease interest group. J Pediatr Surg. 2023 Jan 24:S0022-3468(23)00037-4. doi: 10.1016/j.jpedsurg.2023.01.018. Online ahead of print.
Tirrell AR, Chang BL, Perez-Alvarez IM, Dekker PK, Kim KG, Fan KL, Del Corral G. Selecting a chest masculinization plastic surgeon: a survey of transgender patients. Eur J Plast Surg. 2023 Jan 5:1-9. doi: 10.1007/s00238022-02020-6. Online ahead of print.
Van Jacobs A, Williams MD, Ralph OG, Becerra AZ, Chan EY, Olaitan O. Pancreatic Exocrine Secretion and Weight Gain After Pancreas Transplantation. Prog Transplant. 2023 Sep;33(3):236-241. doi: 10.1177/15269248231189877. Epub 2023 Jul 30.
Veenstra BR, Dixon ME, Pappas SG. Editorial: Different Methods of Minimally Invasive Esophagojejunostomy After Total Gastrectomy for Gastric Cancer: Outcomes from Two Experienced Centers. Ann Surg Oncol. 2023 Oct;30(11):6316-6317. doi: 10.1245/s10434-023-13858-w. Epub 2023 Aug 12.
Wakefield CJ, Jochum SB, Hejna EE, Peterson SB, Vines DL, Shah PN, Hayden DM, Balk RA. Respiratory Musculature Evaluated by Computed Tomography in the Setting of Prolonged Mechanical Ventilation. Respir Care. 2023 Apr 25:respcare.09491. doi: 10.4187/respcare.09491. Online ahead of print.
Williams MD, Gupta V, Chan EY, Olaitan O. Perspectives on Donor-Derived Cell-Free DNA in Kidney Transplant Recipients with Systemic Lupus Erythematosus. Prog Transplant. 2023 Mar 28:15269248231164175. doi: 10.1177/15269248231164175. Online ahead of print.
Williams MD, Skertich N, Sullivan GA, Harmon K, Madonna MB, Pillai S, Shah AN, Gulack BC. Prophylactic antireflux procedures are not necessary in neurologically impaired children undergoing gastrostomy placement. Pediatr Surg Int. 2023 Feb 14;39(1):122. doi: 10.1007/s00383-023-05398-x.
Williams MD, Sullivan GA, Nimmagadda N, Gulack BC, Madonna MB, Hayden DM, Govekar H, Shah AN. Laser Ablation of Pilonidal Sinus Disease: A Pilot Study. Dis Colon Rectum. 2023 Mar 6. doi: 10.1097/ DCR.0000000000002745. Online ahead of print.
Wood SJ, Goldufsky JW, Seu MY, Dorafshar AH, Shafikhani SH. Pseudomonas aeruginosa Cytotoxins: Mechanisms of Cytotoxicity and Impact on Inflammatory Responses. Cells. 2023 Jan 3;12(1):195. doi: 10.3390/cells12010195.

Alfonso Torquati, MD, MSCI, FACS
Helen Shedd Keith Professor of Surgery
Chair, Department of Surgery
Chief, Division of Plastic & Reconstructive Surgery (Interim)


Shaista Khan Chatterji, MHA
Department Administrator


Philip Omotosho, MD
Vice Chair, Quality & Clinical Effectiveness
Chief, Division of MIS & Bariatric Surgery
Director, Minimally Invasive and Bariatric Surgery Fellowship

Rosalinda Alvarado, MD
Diversity Officer

Edie Y Chan, MD
Chief, Division of Abdominal Transplantation
Keith W Millikan, MD, FACS
Senior Vice Chair
Chief, Division of General Surgery
Vice Chair, Education

Jonathan A Myers, MD, FACS
Vice Chair, Clinical Operations
Sam Pappas, MD
Chief, Division of Surgical Oncology
Chief, Division of Colon and Rectal
Surgery (Interim)
Vice Chair, Network Surgery

Naomi Parrella, MD
Director, Strategic Development and Implementation
Chief, Lifestyle Medicine
Medical Director, RUSH Centers for Weight Loss and Lifestyle Medicine

Srikumar Pillai, MD
Chief, Division of Pediatric Surgery


Scott Schimpke, MD
Program Director, General Surgery Residency Program


Nicole Siparsky, MD
Chief, Section of Acute Care Surgery
Vice Chair, Academic Affairs

Ami N . Shah, MD
Vice Chair, Research


Sean Wrenn, MD
Co-Director, Surgical Clerkship Program
Deana Shenaq, MD
Residency Program Director, Integrated Plastic and Reconstructive Surgery
Innovation