2022 RUSH Parkinson’s Disease Donor Impact Report





You empower us to help people achieve their best possible health.
People who are diagnosed with a movement disorder deserve specialized, high-quality care from physicians who deeply understand the complexities of their condition and the leading-edge treatment options available. With help from our generous supporters, the physician-researchers within the nationally renowned RUSH Parkinson’s Disease and Movement Disorders Program are uniquely positioned to provide their patients with the best possible care. We draw inspiration from the cases we see in the clinic to inform research studies, allowing us to discover superior treatments. At the same time, we share our findings with others in the field and prepare future specialists in movement disorders.
Though there are presently no known cures for Parkinson’s disease, our team at RUSH envisions a future where the disease — and all the challenges it can cause — can be slowed, stopped or prevented altogether.
In the following pages, we are proud to showcase a selection of our achievements that were only possible over the past year because of philanthropic support. These projects represent our team’s broad range of talent and our commitment to studying Parkinson’s disease across disciplines. We are also pleased to shine a spotlight on our fellowship program, which has propelled new experts into our field for 42 years and counting.
It is an honor to thank you for your support of RUSH and our program. By fostering exceptional care and improved quality of life, your partnership helps patients with Parkinson’s disease and other movement disorders and their care partners.


Sincerely,
Deborah A. Hall, MD, PhD Director, RUSH Parkinson’s Disease and Movement Disorders Program Christopher G. Goetz, MD Director, Strategic Growth and Innovation By the NumbersRUSH is the top-ranked neurology program in Illinois by U.S. News & World Report

RUSH is the fourth-ranked Neurology and Neurosurgery program in the nation by U.S. News & World Report — RUSH’s fourth-straight year in the top 10
Active research projects in the Parkinson’s Disease and Movement Disorders Program
Movement disorders research articles published by faculty in fiscal year 2022
Supported exclusively by grants and private philanthropy, RUSH’s long-running fellowship program shepherds specialists into the movement disorders field
Search for the nation’s leaders in Parkinson’s disease and movement disorders, and you will frequently discover they trained at RUSH — or collaborated closely with someone who did.
Established in 1980 by the late Harold Klawans, MD — a pioneer in the movement disorders field — the RUSH Movement Disorders Fellowship is one of the oldest and most respected training programs of its kind. Of the prestigious two-year fellowship program’s 39 alumni, 37 remain in practice, with 25 serving as leaders in academia, 10 working in private practice and two advancing the field in industry roles.
The fellowship program, which aims to launch more desperately needed Parkinson’s disease and movement disorders specialists into the field, is supported exclusively through grants and philanthropy.
Helping meet the need for more subspecialists
It is estimated that about 1 million people in the U.S. have Parkinson’s disease, and most do not receive care from a movement disorders specialist. That is because there simply are not enough of them in practice, says Katie Kompoliti, MD, professor of neurological sciences and director of the fellowship program over the past 12 years. Kompoliti herself was a fellow in Parkinson’s disease and other movement disorders at RUSH from 1995 to 1997.
“Most people with Parkinson’s disease, especially in more rural areas, are treated by a primary care physician — or perhaps a general neurologist if they live in a more urban area,” Kompoliti said. Studies suggest that patients with Parkinson’s disease treated by a movement disorders specialist have superior outcomes, especially when it comes to the non-motor symptoms of the disease.
“Care for Parkinson’s disease has advanced significantly since the 1970s,” Kompoliti said. “We have a lot of new treatment options and procedures, and there is a complicated management profile, which requires care from a specialist — someone who sees this disease every day and is highly knowledgeable about its many stages and evolution landmarks.”
A ‘second-to-none’ training experience
Each year, roughly 40 early-career physicians — individuals who have completed medical school and a three-year neurology residency — select RUSH in their application for fellowship training. From those, about 18 are invited for in-person interviews and oral presentations. Faculty rank the candidates, and two of the top choices are selected through a third-party matching process.
The two-year curriculum is immersive. The first year emphasizes clinical care, with supervised management of patients and extensive educational sessions. The second year provides more flexible time for fellows to pursue their areas of interest and conduct research. Fellows can obtain a master’s degree in clinical research from RUSH University, gain experience with clinical trials, attend the field’s preeminent conferences and publish manuscripts in peer-reviewed journals.
“The movement disorders fellowship at RUSH was an experience second-to-none,” reflected past fellow Gian Pal, MD, MS . “I was able to hone my clinical, research and educational skills under the supervision of world-class faculty.”
The critical role of philanthropy
The funding landscape for graduate medical education, particularly fellowships, is complicated — and growing bleaker. While federal funds may support certain fellowships
recognized by a national accrediting body, teaching hospitals are increasingly bearing the brunt of these costs alone. For movement disorders fellowships, donor support is essential.
A generous gift from Khurram and Sameera Hussain has been a critical source of support to the fellowship program while also fueling numerous Parkinson’s disease research efforts.

“We depend on philanthropy and grants,” Kompoliti said. “Our program is fortunate to have a strong community of donors, including the Hussain family and generous grant funders who recognize the importance of our educational mission.”
On multiple occasions, RUSH has received grants to support our trainees as Edmond J. Safra fellows through a grant
administered by the Michael J. Fox Foundation in partnership with the Edmond J. Safra Foundation. A similar grant program from the Parkinson’s Foundation has provided vital support. However, these are highly competitive grants that, when awarded, may not fully cover the costs of administering the program or fellows’ modest salaries and benefits. Private philanthropy from grateful patients and friends of RUSH makes a powerful difference.
“The movement disorders fellowship at RUSH, one of the very first in the world, has maintained its status as one of the best and continues to train leaders in the field,” said K athleen Shannon, MD, one of the first alumni of the fellowship program. “In large part, philanthropic support has facilitated this continued excellence.”
Gian Pal, MD, MS
2012-2014 Fellow
Current Position: Assistant Professor of Neurology at Rutgers Robert Wood Johnson Medical School
“The fellowship training and faculty opened many doors for me and have led to research funding through the National Institutes of Health and the Parkinson’s Foundation. This type of training opportunity provides comprehensive exposure to all aspects of movement disorders and allows for trainees to customize their experience based on their career interests, which is critical to the development of future generations of specialists.”


2010-2012
Current Position: Associate Professor of Neurology and Chief of Neuropalliative Care at the University of Colorado Anschutz Medical Campus
“I was grateful for the breadth of expertise of the group, and to this day, I continue to use phrases with patients that I adopted from faculty there. I still try to channel Dr. [Christopher] Goetz in my interactions with patients and families. I’ll never forget my mentor, Dr. [Deborah] Hall, coming to find me to show me a unique case of progressive ataxia and palatal tremor and, another time, of late-onset Alexander disease. These experiences led me to make these diagnoses on my own once I was in practice — both in instances where the patients were desperate to have explanations for symptoms that had previously been undiagnosed. I remain extremely proud to have been part of this dynamic and erudite group of colleagues.”
Kathleen
1985-1987
Current Position: Chairperson of the Department of Neurology at the University of Wisconsin School of Medicine and Public Health
“The years I did my fellowship were a time of explosive growth in movement disorders. The first studies were being done to see if drugs could slow down the progressive nature of Parkinson’s disease, and it was still a time of few treatments for other movement disorders. I can credit the fellowship with every bit of my subsequent success. I saw a full variety of movement disorders patients, including some children and conditions that were often unavailable to see in other programs in the country. I had my own clinic and worked in other clinics under close guidance. My development as a clinician was very in-depth.”
Just a decade ago, a minimally invasive, incisionless procedure that could effectively treat essential tremor and advanced motor symptoms of Parkinson’s disease was a dream. Such procedures have been a reality at RUSH since 2019, when we became the first health system in Illinois — and one of the first in the nation — to offer patients treatment with MR-guided focused ultrasound, or MRgFUS.
This nonsurgical procedure focuses sound waves inside the brain to interrupt faulty circuits that cause tremors and related motor symptoms. Patients receive the approximately one- to two-hour treatment inside an MRI scanner and are not exposed to any radiation. First approved by the FDA in 2016 to treat essential tremor, this technology has since been extended to patients with advanced Parkinson’s disease. Currently, the treatment is approved for one side of the body only. Some patients choose to treat the side of their body that aligns with their dominant hand, and others choose to treat the side with the most severe tremor.
MRgFUS is offered at RUSH Oak Brook, where patient volumes have tripled initial forecasts. As of early September 2022, nearly 200 MRgFUS treatments have been completed, and many more patients are in the queue for treatment.
MR-guided focused ultrasound restores independence for many patients with essential tremor, advanced Parkinson’s disease
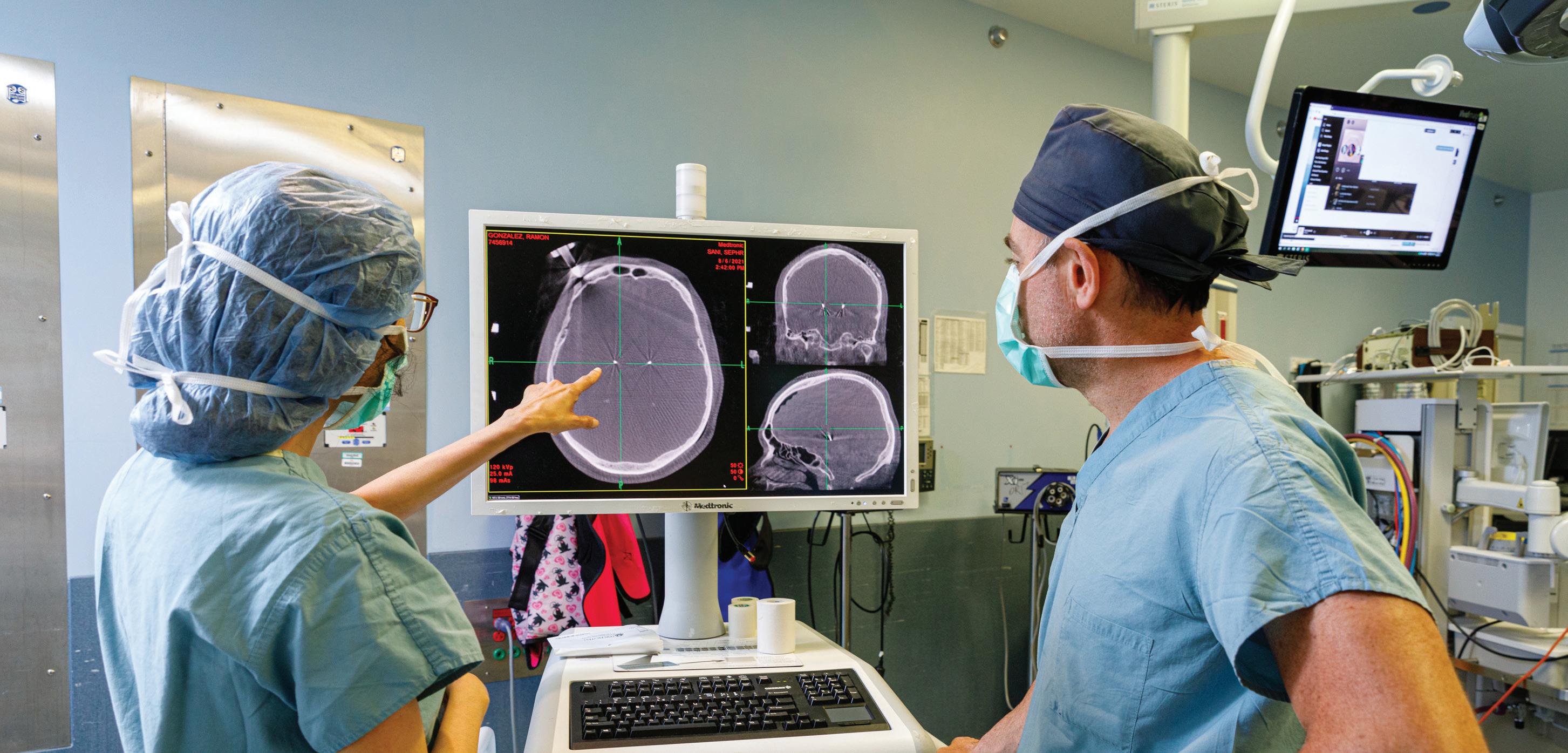
Most patients who receive the treatment report immediate, significant improvements to their tremors, enabling them to independently eat, dress, write and engage in other activities that previously limited their independence.
“They pull you out, they hold a piece of paper in front of you, and they say, ‘Sign your name,’” said Virginia Velez, who was one of the first patients to receive MRgFUS for essential tremor. “And I did, and it was perfect. It was just amazing that they could do something that changes your life so drastically, and you get up and walk out.”
The newness of this technology, coupled with the positive outcomes observed in patients, has spawned new research to maximize the benefits of this therapeutic approach. Neepa Patel, MD , director of RUSH’s interventional Parkinson’s disease program, is partnering with neurosurgeon Sepehr Sani, MD , to lead RUSH’s first study examining MRgFUS on both sides of the brain. Their goal is to explore how this treatment could alleviate Parkinson’s disease symptoms beyond tremors. This study will be a major step forward in expanding the applications of this breakthrough therapeutic approach.
Neuroinflammation, the activation of the brain’s immune response commonly caused by disease, injury, stress and aging, is thought to influence the onset and progression of movement disorders like Parkinson’s disease. To improve treatments and patient outcomes, Natalie Witek, MD, MS, hopes to identify a reliable way to measure neuroinflammation — a biomarker — to help physicians diagnose the condition and determine which patients may benefit from emerging anti-inflammatory and immunotherapy treatments.
Witek and her collaborators are finalizing their analysis of results from laboratory tests evaluating potential biomarkers in participants’ blood and cerebrospinal fluid through three screening techniques. Initial results
indicate abnormal autoantibody activity in patients with uncoordinated movement symptoms known as ataxia. They also found elevated levels of the protein suPAR in patients with Parkinson’s disease and their caregivers — an unexpected finding that Witek published in the August 2022 edition of the journal Parkinsonism & Related Disorders. Witek used preliminary results from her neuroinflammation research to apply for a grant award from the National Institutes of Health to continue studying immune dysregulation in Parkinson’s disease.
Evaluating disease severity via telemedicine
As COVID-19 rapidly advanced the adoption of telemedicine across the globe, it increased the accessibility to movement disorders specialists for people regardless of geography. Since this shift, RUSH experts identified a critical need to better integrate the Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) — the internationally accepted tool for evaluating disease severity — into virtual care.
Through
Christopher G. Goetz, MD, and Sheng Luo, PhD, a distinguished biostatistics researcher from Duke University, developed an algorithm that utilizes big data techniques anchored in more than 7,000 worldwide MDS-UPDRS records to calculate a valid surrogate score for patients’ rigidity and postural stability — two measures of Parkinson’s disease that cannot be assessed in a telemedicine visit. Preliminary results indicate this algorithm can support MDS-UPDRS motor scores that are 95% accurate or better — major progress toward disseminating this tool to elevate telemedicine approaches for the entire movement disorders field.
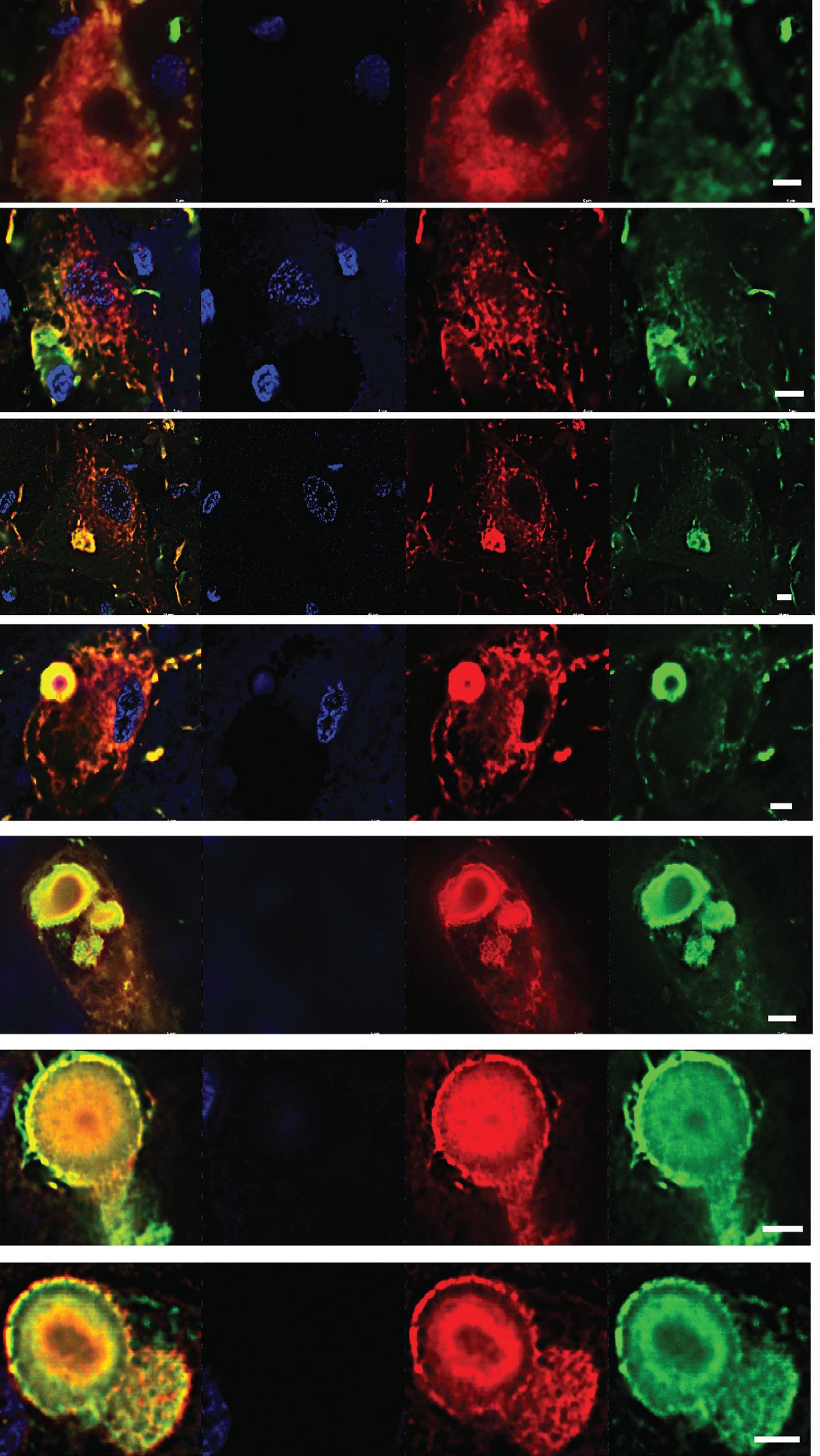
Philanthropic support provides RUSH’s expert physician-researchers with the resources to launch projects that are setting the stage to transform future patient care and outcomes. The following progress in Parkinson’s disease research underway at RUSH has been made possible by our generous donor community.the use of advanced staining techniques, the researchers studying neuroinflammation identified abnormal autoantibody activity in patients with uncoordinated movement symptoms known as ataxia.
Examining the gut microbiome’s effects on dopamine loss in RBD and Parkinson’s disease
REM sleep behavior disorder, or RBD, is understood to be a common precursor to Parkinson’s disease. To better understand how to prevent or delay disease onset, a team of RUSH researchers led by Deborah Hall, MD, PhD, is examining if people with RBD have differences in their guts’ microbiomes that can be targeted with therapeutic interventions. Hall is collaborating with experts from RUSH’s movement disorders, gastroenterology and sleep medicine programs to study the gut-brain axis — the biochemical signaling that occurs between the gastrointestinal tract and central nervous system — and its influence on various dimensions of Parkinson’s disease.
Researchers are enrolling people with RBD and Parkinson’s disease and age-matched household controls (typically a spouse) in a study to examine their microbiomes. The outcomes of this study will inform a subsequent therapeutic trial to determine if microbiome-directed interventions, like prebiotics, or lifestyle interventions, such as exercise, could effectively prevent dopamine loss in the brain. This highly collaborative study is also poised to increase researchers’ knowledge of the biological connections between RBD and Parkinson’s disease.
Encouraging results offer hope that a prebiotic fiber bar may improve some Parkinson’s disease symptoms New insights into the gut-brain axis offer hope that interventions targeting the gut could alter the progression of Parkinson’s disease or prevent its onset. Last year, RUSH researchers introduced a new research project toward that goal, examining the effects of a specially designed prebiotic fiber bar created by our gastroenterology experts, led by Ali Keshavarzian, MD, in collaboration with food scientists at Purdue University. The bars yielded encouraging results in 20 participants who consumed them as part of the pilot study. Gastrointestinal and motor symptoms improved, pro-inflammatory bacteria were reduced, and a relative abundance of beneficial bacteria that produce short-chain fatty acids increased.
While the sample size is too small to draw conclusions, the positive results provide a solid scientific rationale for continued study. Deborah Hall, MD, PhD, delivered a well-attended presentation on the study at the American Academy of Neurology’s annual meeting in April in Seattle. The team is now exploring funding opportunities to improve this intervention and study it at scale.
Caregivers of people with Parkinson’s disease typically face significant burdens as they provide increasing support to their loved ones along the disease’s stages. Jori Fleisher, MD, MSCE (pictured above), and her team are invested in improving caregivers’ quality of life. They created a peer mentorship model that connects caregivers to peers with similar lived experiences while providing them with training, which has proven successful in initial studies. Mentees who completed the peer mentorship program expressed interest in becoming mentors for other caregivers. Fleisher’s team also created a manual that combines lessons on health topics, such as hallucinations, with caregiver support topics, like anticipatory grief, to improve health literacy and support caregivers. The manual is paired with virtual reality training technology for familial caregivers and employees of home health agencies to increase empathy and raise the bar on the quality of care.

State-of-the-art imaging research capabilities come to RUSH
The Joan and Paul Rubschlager Building at RUSH is slated to open in January 2023 on the RUSH University Medical Center campus. The multidisciplinary building will house numerous exam, treatment and office spaces, as well as the new RUSH Imaging Research Center. Anchored by a state-of-the-art 3T MRI scanner — the fastest and most advanced in our health system — the center greatly expands opportunities for MRI research into Parkinson’s disease and other movement disorders. Donor support will be critical to launching pilot projects using this new state-of-the-art research MRI.
RUSH’s physician-scientists have an exceptional track record of using donor funds to gather preliminary data that supports competitive grant applications to external funders, including the National Institutes of Health, or NIH — the peer-reviewed gold standard in medical research funding. We have continued that tradition over the past year. Experts in our Parkinson’s Disease and Movement Disorders Program received three new awards from the NIH to drive progress in health equity, nonmotor symptoms and Parkinson’s disease pathology.
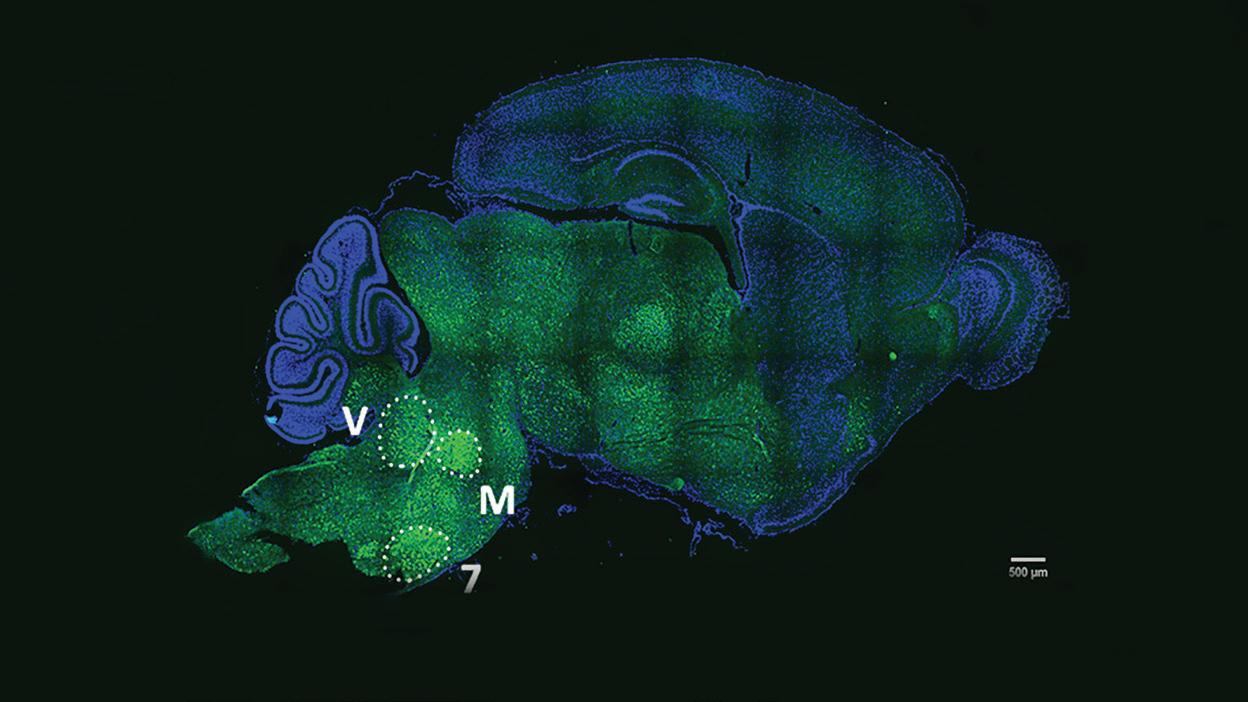
Seeking an understanding of the disease process underlying Lewy pathology
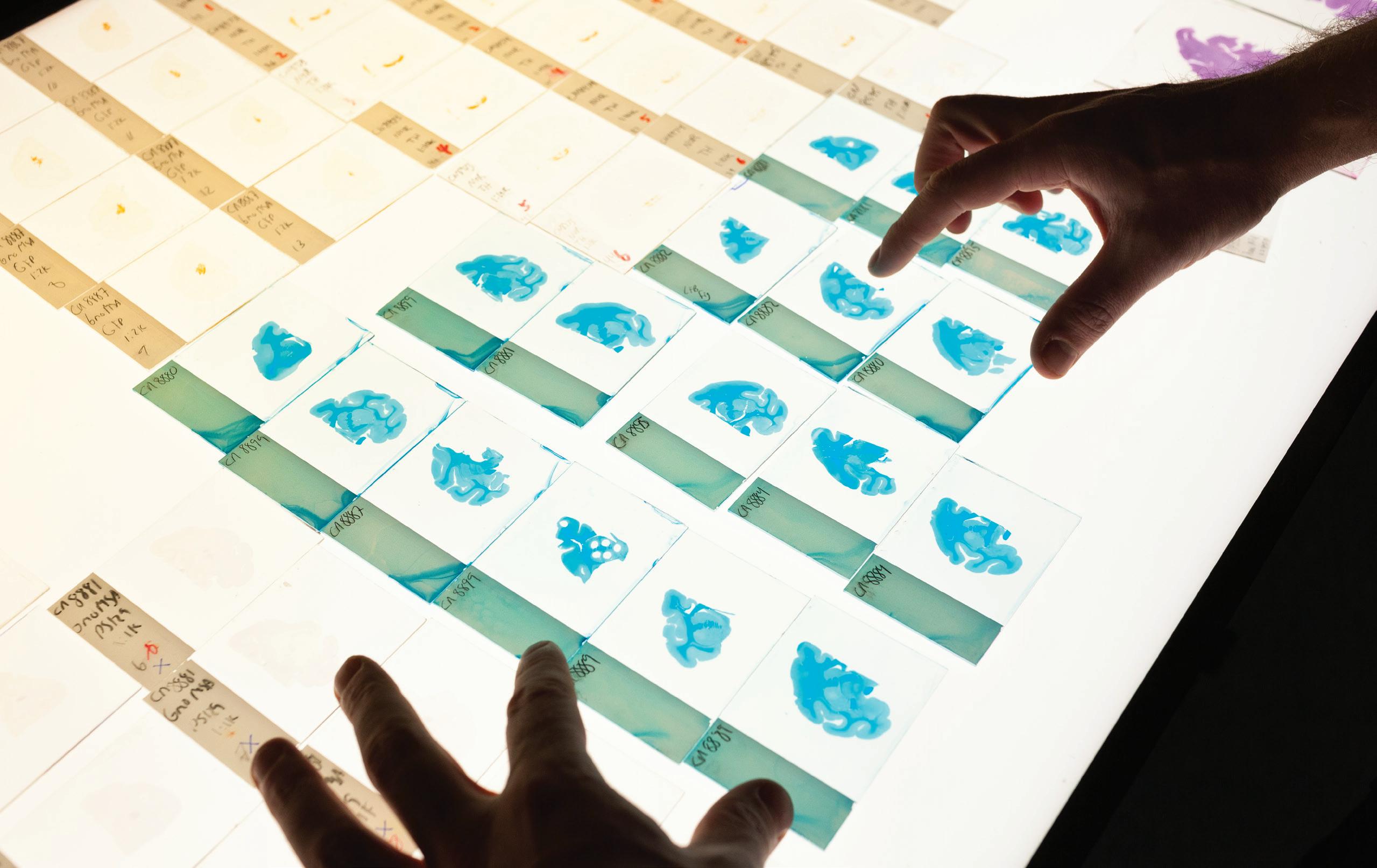
The accumulation of Lewy bodies, or abnormal aggregations of the protein alpha-synuclein, in the brain is a hallmark of Parkinson’s disease and other neurodegenerative diseases. To study the disease process underlying the pathology of Lewy bodies, Bryan Killinger, PhD, applied for and received an R01 grant from the NIH. This study aims to determine Lewy pathology interactions in neurodegenerative diseases in the human brain and investigate Lewy pathology interactions in the rodent brain as neurodegenerative diseases develop. Mapping many more tissue samples from RUSH’s brain bank offers hope that cellular processes will be discovered that could shape new drug discovery efforts and better ways to study potential therapeutics in animal models of Parkinson’s disease.
Studying racial disparities in patients with Parkinson’s disease
Our current understanding of Parkinson’s disease is disproportionately based on studying its effects on white people, leaving a significant gap in knowledge about the clinical characteristics, life experiences and outcomes of Black people with Parkinson’s disease. To fill this gap, Deborah Hall, MD, PhD, applied for and received an R01 grant from the NIH to study disease symptoms, signs and management as well as genetic factors in Black people with Parkinson’s disease compared to their white
counterparts. She will lead the efforts of eight Parkinson’s disease academic clinics around the country in this project and recruit more than 600 patients. The results will inform clinical guidelines and the development of educational materials for clinicians and patients. The study aims to improve health care delivery and quality of care by increasing recognition of differences in disease manifestations and management in Black patients, who are historically underserved and understudied.
Pursuing leading-edge solutions for mood and cognitive symptoms of Parkinson’s disease
Over the past year, Alana Kirby, MD, PhD, has made significant strides in establishing a new optogenetics (a technique to selectively activate and inactivate brain circuits using fiber optic technology) laboratory at RUSH. This laboratory is an addition to the scientific program that especially reinforces our team’s strengths in research related to deep brain stimulation, or DBS, and the nonmotor symptoms of Parkinson’s disease. Kirby’s initial studies focus on apathy, a loss of motivation that is a common non-motor symptom of Parkinson’s disease that can worsen after DBS. Apathy and how it may be affected by DBS are under-researched issues in the field that desperately require better approaches. Kirby recently received an R21 grant from the NIH to identify biomarkers that can be used to predict when DBS may result in disorders of mood or cognition and ways to improve DBS protocols to reduce non-motor adverse effects.
As we look with hope toward a future where there are viable preventions and cures for Parkinson’s disease, your investment in our research allows us to take steps forward in the present. We do this through the compassionate care and training we provide and the innovative research we conduct. Thank you for your ongoing commitment to our work.
To support the Parkinson’s Disease and Movement Disorders Program at RUSH or learn how you can continue your legacy of support through an estate gift, visit rushgiving.com/pdimpact or contact:
Brigid Mullen Executive Director of Development (312) 942-4460
brigid_t_mullen@rush.edu