September 2025
Volume 59, No. 4

“I HAVE
LITTLE PATIENCE FOR TIME WASTED.”
Greg Murphy reflects on how his career as a doctor shapes his service as a Member of Congress.


September 2025
Volume 59, No. 4

“I HAVE
LITTLE PATIENCE FOR TIME WASTED.”
Greg Murphy reflects on how his career as a doctor shapes his service as a Member of Congress.

by ROY BLUNT
Plus: Buddy Carter discusses the crisis facing America’s pharmaceutical supply chain.
And: Michael Baker explains what vaccines have meant to the U.S.

By Roy Blunt
The U.S. should commit itself to making the most of the next generation of healthcare and maintain our position as the world’s premier leader
The United States should never be dependent on the Chinese Communist Party for antibiotics and essential medicines, but that’s exactly the dangerous position we are in today.
By Michael Baker
The creation, development, and deployment of vaccines – a U.S. federal priority since the 1960s –has been one of the greatest health care achievements in history.
Story (cont’d)
The Cost of Chronic Disease By Matthew
E. Kahn
As of 2023, roughly 194 million American adults had at least one chronic condition, which costs our nation’s economy billions of dollars each year.
America the Overprescribed By Vikas Saini
The best way to prevent the downstream effects of overprescribing is to prevent it in the first place. That also means a concerted effort to prevent overdiagnosis.
The Future of AI in Health Care: Moving at the Speed of Trust By Lucy Orr-Ewing
For modernization to truly take hold, and for the adoption of artificial intelligence to be systematic and widespread, we need greater confidence in its safety and effectiveness.
Debate -- “Should the Government Control Drug Prices?” 26 No, It will Stifle Innovation By Sally C. Pipes
Yes, Wise Regulation Will Reform an Out-of-Control Industry By Paul Ginsburg & Steve Liberman
- Remembering Mike Castle
Profile of U.S. Rep. Greg Murphy

THE
RIPON
SOCIETY
HONORARY CONGRESSIONAL ADVISORY BOARD
U.S. Senators:
Shelley Moore Capito - Senate Co-Chair
Todd Young - Senate Co-Chair
Marsha Blackburn
Bill Cassidy, M.D.
Susan M. Collins
John Curtis
Steve Daines
Joni Ernst
Deb Fischer
John Hoeven
Jerry Moran
Mike Rounds
Thom Tillis
Roger Wicker
U.S. Representatives:
Frank Lucas - House Co-Chair
August Pfluger - House Co-Chair
Stephanie Bice - House Co-Chair
Mark Amodei
Jodey Arrington
Don Bacon
Troy Balderson
Andy Barr
Mike Bost
Rob Bresnahan
Vern Buchanan
Ken Calvert
Kat Cammack
Mike Carey
Buddy Carter
Juan Ciscomani
Tom Cole
Jake Ellzey
Tom Emmer
Ron Estes
Gabe Evans
Julie Fedorchak
Randy Feenstra
Brian Fitzpatrick
Scott Franklin
Andrew Garbarino
Tony Gonzales
Sam Graves
Pat Harrigan
Kevin Hern
French Hill
Ashley Hinson
Bill Huizenga
Dusty Johnson
Dave Joyce
John Joyce, M.D.
Mike Kelly
Jen Kiggans
Kevin Kiley
Young Kim
Darin LaHood
Bob Latta
Laurel Lee
Julia Letlow
Celeste Maloy
Brian Mast
Michael McCaul
Carol Miller
John Moolenaar
Blake Moore
Greg Murphy, M.D.
Dan Newhouse
Zach Nunn
Jay Obernolte
Guy Reschenthaler
Michael Rulli
María Elvira Salazar
Steve Scalise
Pete Sessions
Adrian Smith
Jason Smith
Lloyd Smucker
Pete Stauber
Bryan Steil
Glenn “GT” Thompson
Mike Turner
David Valadao
Ann Wagner
Steve Womack
Rudy Yakym
At a time when spending in just about every area of the federal government is coming under intense scrutiny and review, the latest edition of The Ripon Forum examines the importance of investing in health research and why is it critical that the United States remain a global leader in that regard.
“There has been more change in healthcare and how we think about healthcare in the last 25 years than the collective healthcare advances of all time before that,” writes former Missouri Senator Roy Blunt in the cover essay for this latest edition. “There are many reasons to believe that the next quarter century, and maybe even the next decade, will make the same kind of incredible progress.”
Blunt knows the issue better than most. Before his retirement from Congress in 2023, he served as Chairman of the Senate appropriations subcommittee that funds the National Institutes of Health and other key federal healthcare agencies. In this position, he helped lead the effort to make sure America was a global leader in medical research. It is a priority, he said, that the federal government should renew its commitment to invest in today.
“The United States should commit itself to making the most of that next generation of healthcare and maintain our position as the world’s premier leader in medical breakthroughs,” Blunt writes. “When a country is first in health research, the people of that country benefit the most, but the economic opportunity of being first is also significant. Just a few of the areas that will rapidly develop include CRISPR technology, microbial medicine, the AI applications in healthcare research, and analyzing healthcare data.”
According to Georgia Congressman Buddy Carter, lawmakers should also make it a priority to confront the crisis facing America’s pharmaceutical supply chain. “The United States should never be dependent on the Chinese Communist Party for antibiotics and essential medicines,” Carter writes. “But that’s exactly the dangerous position we are in today. In 2002, the United States manufactured 72 percent of the pharmaceuticals it consumed. By 2023, that number had dropped to just 37.5 percent. We didn’t just outsource manufacturing — we outsourced the sovereignty and safety of our health care system.”
In another essay, Michael Baker of the American Action Forum examines the vital role that vaccines have played in American life over the past six decades. “The creation, development, and deployment of vaccines – a U.S. federal priority since the 1960s – has been one of the greatest healthcare achievements in history,” Baker writes. “Routine childhood immunizations in the United States from 1994–2023 are estimated to have prevented around 508 million cases of illness, 32 million hospitalizations, and more than 1 million deaths.”
Also writing for this latest edition, Matthew A. Kahn of the Hoover Institution examines the cost of chronic disease in America, while Vikas Saini, the president of the Lown Institute, makes the case that America is overprescribed as a country and it is costing us billions of dollars each year. Lucy Orr-Ewing of the Coalition for Health AI shares her thoughts on the future of artificial intelligence in health care, and, in our featured debate, Sally Pipes, President & CEO of the Pacific Research Institute squares off against USC Professor Paul Ginsburg and Steve Lieberman of the Schaeffer Center in a discussion over drug prices and whether the government should step in to control them.
In our Politics & Perspective section, political observers Lee Drutman and Dustin Wahl look at Nebraska Congressman Don Bacon’s decision to retire from Congress and whether there is room for his brand of conservative centrism in American politics today. Alex Durante of the Tax Foundation examines the hype and reality of today’s trade wars, and strategist Matthew Bartlett assesses New Hampshire Governor Kelly Ayotte’s first six months in office.
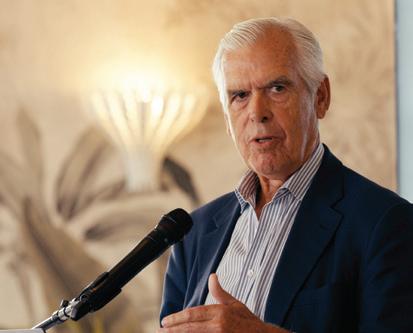
In another essay, I review government reform expert Philip Howard’s latest book, Saving Can-Do, which follows up on the DOGE cuts taking place in Washington and asks a simple question — what comes next? And in our latest Ripon Profile, North Carolina Congressman Greg Murphy discusses his career as a doctor and how that has shaped his service in the House.
As always, we hope you find this edition of The Ripon Forum interesting and informative, and welcome any questions or comments you may have.
Lou Zickar Editor of The Ripon Forum louzickar@riponsociety.org
by LEE DRUTMAN & DUSTIN WAHL
Omaha, Nebraska was the weirdest city in American politics last year. Nebraska’s Second District (consisting almost entirely of Omaha) was a blue dot for Kamala Harris in an otherwise bright red sea of support for Trump. Independent Senate candidate Dan Osborn piled on a 12 point lead ahead of Republican Sen. Deb Fischer in Omaha, not enough to win statewide but enough to make clear that Omaha was a bad place to be a Republican candidate. But in the Second District’s House contest, Republican Rep. Don Bacon defied political gravity like he has in every race since 2018: barely scraping by with almost exactly 51 percent of the vote.
And then, eight months later, he announced that he would retire.
Bacon’s success is thanks to strong relationships in his district and his brand as a centrist, opposing his party line just often enough to win over voters who otherwise prefer Democrats. But this type of politician appears to be going extinct. Bacon is one of only three Republican members of Congress in districts won by Kamala Harris. And he didn’t want to try again in 2026. In a country divided into two increasingly warlike camps, this raises a concerning question: is there no more room for centrists in American politics?
made it nearly impossible to survive in the House as a true political moderate. Now it’s also coming for moderate vibes, making it hard to break from one’s camp even on small issues.

Bacon’s success is thanks to strong relationships in his district and his brand as a centrist, opposing his party line just often enough to win over voters who otherwise prefer Democrats. But this type of politician appears to be going extinct.
The first part of the answer is that there already wasn’t much room for centrists, even when Bacon was running. On most hot-button topics, Bacon, toed the party line. He voted against impeachment, and recently voted for President Trump’s budget bill, falling in line with many other Republicans who knew the unpopular bill would hurt their constituents. Worsening partisan polarization has already
Moreover, political moderates are not a monolith. A growing number of Americans are Independents, and 60-70 percent consistently say they want more than two parties. But research and polling show that these voters are not ideologically clustered together in the middle – they have a mix of beliefs from all over the political map. Third-party entrepreneurs like Elon Musk can’t corral them into just one group, and Musk himself is no moderate. America’s two-party system isn’t only repressing a third party; it’s repressing a fourth, fifth, and sixth party. And it’s repressing hidden diversity within its existing two parties. There are a number of reasons for this binary divide, but the biggest is a surprisingly simple fact of political science: America’s electoral system naturally produces just two parties. We use winner-takeall elections: a candidate that wins 51 percent of the vote in a district wins 100 percent of the representation. The 49 percent opposition wins no representation at all. If a third party tries to run a candidate in one of these contests, they will risk spoiling the election by taking votes away from the party that’s most ideologically similar to them and inadvertently helping the party that they most oppose.
Compared to proportional election systems used by most established democracies, America’s system is weirdly undemocratic. In proportional elections, 30 percent of the
vote translates into roughly 30 percent of the seats. To achieve this, most democracies use multi-member districts, where multiple representatives serve the same area. In America, this would let conservatives compete in liberal areas and liberals compete in conservative areas. With proportional representation, a Don Bacon-type, a MAGA Republican, a moderate Democrat, and a progressive Democrat might all win seats to represent the real ideological diversity of the district, instead of just one faction getting all of the representation.
In recent decades, this system has made dangerous trends more dangerous. Urban areas are becoming more liberal, rural areas are becoming more conservative, and the two parties are adjusting where and how they try to compete. Gerrymandering, where politicians cynically draw district lines to lock down their party’s control, has become easier and more shameless. That’s thanks in part to geographic self-sorting and in part to the rise of maximalist, doanything-to-win political strategies fueled by the very divisions they reinforce.
The biggest victim has been competitive districts –in the last several election cycles, around 80 percent of congressional elections have been safe seats for one party or the other. Even if gerrymandering were somehow eliminated, this would still be true. Most elections are uncompetitive not because of gerrymandering, but because of geographic partisan polarization in a system of single-member districts.
spiral deeper into the two-party doom loop until it hits rock bottom?
There’s a ray of hope in a few parts of the country that are similar to Bacon’s Omaha district. Reps. Marie Gluesenkamp Perez and Jared Golden – two of thirteen Democrats in districts won by Trump in 2024 – introduced legislation to create a select committee on electoral reform. Among other reforms, the committee would study proportional representation and multi-member districts and how they might weaken the two-party duopoly that has our country in a chokehold. Both MGP and Golden are almost alien in today’s politics: they’re young, working class, and they serve nearly equal numbers of Democrats and Republicans.
Worsening partisan polarization has already made it nearly impossible to survive in the House as a true political moderate. Now it’s also coming for moderate vibes, making it hard to break from one’s camp even on small issues.
But a few competitive patches of land remain, and Omaha is one. Don Bacon’s victories in the Nebraska Second District have all been epic, expensive battles, all decided by a hair. Bacon won with 49 percent in 2016, and with 51 percent in 2018, 2020, 2022, and 2024, making this the most consistently close district in the country. But now it appears to be trending away from Bacon’s party, and his retirement may mean that even Omaha becomes uncompetitive in the future.
And so goes the story of American politics today. Representatives like Don Bacon who need to craft a reputation for compromise in order to win have a harder and harder path. The idea of a third party, desirable in theory, is totally unworkable under the current rules: a third party that charges headlong into a winner-take-all system will most likely be spoilers. Independents like Dan Osborn show great promise, and this approach is likely to grow more attractive to outsiders over time. But an independent path requires a Herculean effort, and it only works when one of the two parties decides not to compete.
So what can we do about this? Is America doomed to
Their legislation points towards the crucial solution to the dangerous division in American politics. We are getting the results we should expect from the electoral system we use. To make politics work again, we need a system that represents all Americans – not just 51 percent of the voters in a given area. If Omaha elects a moderate Democrat in 2026, there will be plenty of disappointed Don Bacon Republicans. There will also be disappointed right-wing Republicans, and disappointed left-wing Democrats. That’s because Omaha isn’t a moderate city – it’s a diverse city, like America is a diverse country. We’ll never know if Bacon could again reach 51 percent in 2026, but it shouldn’t matter – coming up short of the magical majority threshold should not mean no representation at all. What made Omaha a weird city in 2024 was that its diversity was visible. To fix our failing politics, America needs an electoral system that makes our diversity visible everywhere. RF
Lee Drutman is a senior fellow in the Political Reform program at New America. He is the author of Breaking the Two-Party Doom Loop: The Case for Multiparty Democracy in America (Oxford University Press, 2020) and The Business of America is Lobbying (Oxford University Press, 2015), winner of the 2016 American Political Science Association’s Robert A. Dahl Award, given for “scholarship of the highest quality on the subject of democracy.” Dustin Wahl is the deputy executive director of Fix Our House. He has led a variety of advocacy campaigns, including Save71, an organization he founded to promote accountability at his alma mater, Liberty University.
by ALEX DURANTE
In 2018, President Trump proclaimed trade wars “are good and easy to win.” Now, six months into the President’s latest trade war, the results have proven to be anything but. While the President boasts about the billions in revenue the tariffs are generating and trade “deals” he is brokering, a closer look shows it is American firms and consumers ultimately getting fleeced.
The Trump administration has cited numerous goals for the tariffs, goals often in contradiction with each other. Some days, the tariffs are either a “negotiating tool,” in which case they are not intended to remain in effect for very long; other times, the tariffs are the end in themselves. Trump has frequently alleged that the tariffs will restore American manufacturing, fix the debt, and reduce the “trade deficit” — a purported “national security” threat to the U.S.
In all these cases, Trump is overpromising and underdelivering.

reducing their revenue-raising potential. Indeed, the Tax Foundation finds that if the reciprocal tariff rate on China goes into effect, which would increase the tariff by 115 percentage points , this would reduce imports of tariffed-goods from China to zero. But consumers would not be spared the price impacts: their alternatives would be either purchasing higherprice domestic goods or import tariffed goods from elsewhere, like Vietnam. Trump’s $150 billion in tariff revenue this year might look impressive, but it is a poor indicator of what we should expect going forward.
Alex Durante
Let’s start with the claim that tariffs will revive U.S. manufacturing. More than half of imports are capital goods and intermediate inputs — things used by businesses to produce final goods that we buy, from smartphones to cars. As tariffs rise, the costs of production for those firms also goes up. The Federal Reserve looked at the impacts of the tariffs in Trump’s first term and concluded that manufacturing output and employment actually declined because of them, contrary to what was promised. A United States International Trade Commission report studying the steel and aluminum tariffs reached similar conclusions.
While the President boasts about the billions in revenue the tariffs are generating and trade “deals” he is brokering, a closer look shows it is American firms and consumers ultimately getting fleeced.
On revenue, while it is true that tariffs can reduce the debt, they are an incredibly inefficient way to do so. Raise the tariff too much, and imports will collapse,
Nor should we have much confidence that these tariffs would reduce the trade deficit. Because tariffs raise production costs, they affect how much firms can produce and export abroad. As it turns out, tariffing imports also hurt exports. Factor in retaliatory tariffs from Canada and China (and potentially more down the road) and exports will be hurt even more. If Trump wants to support manufacturing by expanding their export markets, tariffs are a poor way of going about it.
Finally, we should look at how tariffs will affect prices. A Federal Reserve survey fielded in May found that 45 percent of firms had reported passing along some of the tariff increases to consumers, with a third indicating they had passed all the increase onto consumers. While some firms report absorbing tariffs , this could change with all of the reciprocal tariffs now in effect. Firms who operate on a contract basis might also experience lag time when they increase their prices. Right now, only a few products, such as audio equipment and certain foods , are showing significant price hikes. However, this does not imply that the tariffs are not currently having negative economic effects. If firms must spend more money to pay the tariffs, that’s
less money they have to put toward investments or job creation. This is why the Tax Foundation finds that on the whole tariffs will reduce economic growth and employment . Still, we should probably brace for higher prices going forward.
A
So far, it does not appear that any of the trade “deals” that Trump has announced will offer Americans much relief from the tariffs. While it would be ideal for countries in any arrangement to agree to reduce their tariffs to zero (free trade still benefits all parties), President Trump seems to be negotiating to higher tariffs on imports in exchange for purchase commitments and investment promises. The proposed EU deal, for instance, would increase the tariff on their imports to 15 percent, in exchange for the EU agreeing to buy more U.S. energy exports and invest in the U.S.
President Trump negotiated a similar agreement with China in 2020, where they agreed to purchase more of our agriculture exports for two years. Unfortunately, their purchases fell well below their commitments We should expect a similar result from the EU deal as their purchase promises are well above their actual energy needs . Negotiating trade deals is a worthwhile goal, but those deals should move us in the direction of increasing trade among both countries by reducing tariffs and expanding market access.
Sadly, the President’s approach is moving us in the opposite direction. RF
Alex Durante is a Senior Economist at the Tax Foundation, where he works on federal tax policy and macroeconomic model development.

that
since 1965.“
by LOU ZICKAR
“Is this America’s 1917 moment?ˮ
That is the opening question posed by author and attorney Philip Howard in his latest book on bureaucratic dysfunction and the need for a new governing vision in the United States.
Called Saving Can-Do: How to Revive the Spirit of America, the book postulates that the U.S. is in the midst of a “major shift in the social order” – a shift spurred on, much like the Russian Revolution 108 years ago, by the failure of the ruling elite to govern the country effectively, and the populist revolt that has transpired as a result.
Of course, the leader of the current revolt is President Donald Trump, and in swinging “a wrecking ball at the status quo,” as Howard describes it, the President is giving the people who voted for him what they want. Nowhere is this more evident than the effort by the Department of Government Efficiency to remake government that has so dominated the conversation in our nation’s capital since the beginning of the year.
ideas for governing, sometimes catastrophically, as with the Committee of Public Safety after the French Revolution or the Bolsheviks in Russia. Letting nature take its course after Trump’s wrecking ball is unlikely to end well, leaving a wreckage of public agencies, perhaps replaced by an AI-driven autocracy that would exacerbate populist alienation.
Philip Howard
Howard’s concern these days – and the focus for much of his latest book – has less to do with the DOGE wrecking ball that has been tearing through Washington than the question of what comes next.
As Howard rightly notes, a clear majority of Americans believe Washington needs “very major reform.” Howard is a member of that majority. He is also one of its leading voices, having testified, lectured, and written seven books on the need for government reform over the past three decades. His concern these days – and the focus for much of his latest book – has less to do with the wrecking ball that has been tearing through Washington than the question of what comes next.
“Where’s Trump’s vision of how government will work better the day after DOGE?,” Howard writes in the book’s introduction. “Toppling the old order leaves a vacuum that, without a new vision, can be filled by unpredictable new
“Democrats are strangely quiet, apparently content to wait until Trump fails. This works fine for Democrats as a business model: Opposing Trump is all they need to raise buckets of money. Interest groups will pay a lot to defend the status quo, and Democrats have no agenda to cut red tape or public pork. But standing for the status quo against the tides of change is not likely to be a winning strategy, however much money is funneled into party coffers.
“So here we are: Neither party has a vision for better government. Democrats are in denial, waiting their turn to run a bloated government that Americans loathe. Trump and friends can sack Washington, but, as Rome learned long ago, the destruction of what’s weak and corrupt can leave people worse off if there’s no new plan. Retribution is a recipe for civil strife, not a governing strategy.”
Howard devotes the remainder of the book to outlining what he believes that strategy should look like. The key tenets of the strategy will be familiar to anyone who has followed Howard’s work over the years, and are presented in three essays laying out a “new governing vision” for the United States. In the first essay, Howard
focuses on what he considers the secret sauce of American success — namely, that since our founding, we have been a nation of strivers.
“America’s culture of striving was born of exiles and explorers confronting the challenges of the wilderness,” he writes. “Americans were not locked in to predetermined paths of the old world. We formed our own communities, with our own values. Unlocking human potential proved powerful not only for the colonists but also for later arrivals. Immigrants two centuries after the Puritans not only worked their way to a better life, but sometimes achieved greatness and riches, where their ancestors had been peasant farmers for a thousand years.”
Unfortunately, Howard continues: “This spirit of America has been collapsing over the past fifty years. Americans no longer feel free to follow their instincts, or even to be themselves in daily dealings. That’s because of a flawed philosophy of governing — that law should preempt human judgment in daily choices.”
Howard’s previous book, called Everyday Freedom and reviewed in our pages, focused on this flawed philosophy and how it has crippled American culture over the past five decades. In Saving Can-Do, he picks up where that book left off by offering up a series of ideas and proposals that will move our country away from the legal framework that is suffocating everyday freedom and toward a culture that puts a premium, and not a penalty, on striving.
their judgement.”
In the second essay, Howard focuses on another kind of culture — one, he argues, that is not only critical to creating a culture of striving, but is essential to reviving the spirit of America and saving can-do in the United States. It is the culture that can be found in classrooms and, more specifically, in healthy schools. “An effective school,” Howard writes, “will generally have a culture where students feel cared for and inspired to do their best, where teachers feel a sense of ownership for their classrooms, and where principals have fostered a common feeling of aspiration and mutual trust.”
“Toppling the old order leaves a vacuum that, without a new vision, can be filled by unpredictable new ideas for governing.”
“Red tape is strangling the goose of American striving,” Howard writes. “The new governing framework must be an open framework, activated by human judgment on the spot. Law should set goals and principles, and provide a structure of authority and accountability. Actual decisions within this framework are made by Americans taking responsibility. The aspiration is not mainly to deregulate — although American regulation is long overdue for a spring cleaning. The critical change is to put in place a governing system that empowers officials and citizens alike to use
Unfortunately, he continues, public schools in America are providing anything but that kind of culture. Instead, he argues: “America’s schools are treated today like other arms of government. But most governing responsibilities are regulatory or reactive to possible violations of law, and are governed by laws and regulations that are supposed to be uniform and generally centralized. Schools are different from governing. There’s no reason for schools to be uniform … uniformity tends to destroy their spirit. Schools are supposed to provide the training and values for individuals to flourish, not to extrude them through a common mold. It’s hard to imagine a worse structure than one that organizes schools like a police function, handcuffing teachers and principals. Just as the country can’t flourish with decrepit infrastructure, so too it can’t flourish with schools that are organized with one-size-fits-all codebooks.”
Howard’s solution? Reduce administrative bureaucracy and unions and give more authority to parents, teachers, and principals to “make the everyday choices needed to build and support effectives schools.” He also argues that in some cases, public school systems are beyond reform and simply need to be rebuilt — which is exactly what happened in New Orleans following the devastation of Hurricane Katrina in September 2005. “The
transformation of New Orleans schools after Hurricane Katrina,” he writes, “demonstrates what is possible when communities can start over — after the public school system was replaced by independent charter schools, high school graduation rates improved from 52 to 72 percent, and gaps between racial groups narrowed. Not all the new schools were successful — about a quarter were shuttered for poor performance. But the ones that survived produced materially superior results with far better school cultures.
“The secret to success of new schools in New Orleans was not educational genius or even better people … but simply the authority to make basic choices. New schools worked because, according to one school leader, ‘teachers and school leaders have more autonomy to be adaptive in the new system — they can improve more quickly, they can more easily make the small changes and decisions that need to be made every week and every year to better meet the needs of students and parents and teachers.’”
Still, he concludes: “…no meaningful progress can occur until political and educational leaders acknowledge that the bureaucratic model of America’s public schools has failed. The control model fails because it crushes the human spirit and autonomy needed to build and sustain good school cultures. Those top-down frameworks should be abandoned, and communities empowered to rebuild America’s schools as local institutions rooted in local values and personalities.”
the Civil Works Administration in November 1933, which was headed by his friend Harry Hopkins and was intended to give jobs to the unemployed. Less than two months later, Hopkins and the CWA had hired over two million Americans — an achievement, Howard notes, which reflected the governing philosophy that was predominant in Washington at the time. “The New Deal projects worked not only because officials had the legal authority to push ambitious projects forward, but also because those officials viewed their responsibility as achieving results,” he writes.
“The aspiration is not mainly to deregulate — although American regulation is long overdue for a spring cleaning. The critical change is to put in place a governing system that empowers officials and citizens alike to use their judgement.”
Howard’s final essay, “Escape from Quicksand,” focuses on the kind of framework that he believes should be put in place to meet the needs of America with regard to modernizing our infrastructure. In trademark fashion, he studs the essay with recent examples of how the current legal and regulatory framework has let the country down. In 2009, Congress passed a bill which allocated $5 billion to weatherproof older homes. Under this legislation, it was estimated that 2,500 homes per month would be fixed in California alone. Unfortunately, by the end of 2009, the number of homes that had been weather proofed in California totaled only a dozen. More recently, in 2021, Congress passed a landmark infrastructure bill which allocated $7.5 billion to construct a national network of electric vehicle charging stations. Three years later, only eleven charging stations had been built.
Howard contrasts this under-performance with the over-performance of the federal government during the New Deal. As an example, he cites FDR’s creation of
Flash forward 90 years, Howard argues, and the governing philosophy in our nation’s capital has become just the opposite. It is a philosophy mired in bureaucratic procedures and shackled by a system that has replaced good judgement with rules and red tape. Howard’s solution is to take a page from the past by returning to a system that empowers the individual, much in the same way that FDR empowered Harry Hopkins. “Governing effectively is impossible until designated officials are empowered to make ultimate decisions,” he writes. “America must return to the human responsibility operating philosophy envisioned by the Framers. The current system is built on the wrong idea of law. Law cannot make public choices. Moreover, while law can protect against arbitrary choices, it cannot validate which choice is best among a wide range of plausible options. Law instead is supposed to frame the responsibility of officials who, within legal boundaries, make choices that are politically accountable.”
Howard concludes the essay with three recommendations for a new framework to guide public decision making when it comes to modernizing infrastructure in the United States. No spoilers here — you can read the recommendations for yourself when you read the book. But it’s safe to say that the ultimate goal of the recommendations and the book is to outline a new framework for governance in America, one that not only promotes accountability, but produces results.
Like Howard’s more recent works, Saving Can-Do is a slim volume, coming in at just under 140 pages, including notes. But don’t let its modest size fool you. This book packs a powerful punch, and provides a timely answer to those who support the underlying mission of DOGE, but are also concerned with what could – and should – come next. RF
Lou
Zickar is Editor of The Ripon Forum.
by MATTHEW BARTLETT
It has been roughly six months since Governor Kelly Ayotte was sworn into the corner office in New Hampshire. While it is still obviously early in her term, she remains popular and enjoys a double digit favorability rating as a Republican in a purple state that was also won by Kamala Harris. Her achievements in government thus far are cause for celebration, and possibly speculation, for the young common-sense conservative.
New Hampshire is part of New England, yet it is politically and culturally significantly different from the rest of its neighboring states. Ayotte herself highlighted this difference during last year’s campaign by running on the election-defining motto — “ Don’t Mass Up New Hampshire.” For sure, the motto was a not-so-subtle shot at the tax and spend Bay State to the south. But it was also a clear signal from Ayotte that she would stay true to the state’s independent identity and frugal Yankee ideology.
reform effort that emphasized safety across Granite State cities and communities. Her successful changes to the bail system ensure that those who are a danger to society in New Hampshire will face jail rather than a turnstile that puts them back on the streets.

Since taking office on January 9, Governor Ayotte’s top achievement occurred this summer, when she signed into law a fiscally responsible budget.
Since taking office on January 9, Governor Ayotte’s top achievement occurred this summer, when she signed into law a fiscally responsible budget. The negotiated budget balances the role and services of the state government and the budgets of families and taxpayers alike. The budget also continues the state’s historic notion of the “ New Hampshire advantage” which keeps taxes low and reduces the state’s bureaucracy, empowering local communities and individuals in making decisions they deem best. The Governor was also successful in the budget process in tackling longstanding issues involving retirement programs for first responders, saying New Hampshire must protect those who keep state residents safe.
Another signature Ayotte priority was a major bail
Governor Ayotte also put a major focus on kids and education. Under her leadership, New Hampshire dramatically expanded universal education freedom accounts, allowing even more parents to choose a personalized pathway in education. At the same time, she also provided more money than ever before for public education. Ayotte went even further and signed a parental bill of rights and enacted a bell-to-bell cellphone ban for children in school.
While New Hampshire is not immune from national trends and challenges such as housing and energy, Governor Ayotte made efforts to help mitigate the issues on a local level. She signed into law 60-day permitting reforms, limited local zoning regulations, and made allowances for mixed use housing.
As part of her all-of-the-above energy policy, the first bill she signed as Governor made it easier to finance energy efficiency projects and programs. She is also working with the EPA on the permitting process for a potential natural gas pipeline, exploring possible ways for the state to access competition and cheaper energy for the future.
Along the way, Governor Ayotte racked up a host of other significant legislative wins. She signed into law nation-leading crypto legislation, banned sanctuary cities, scored a deal with hospitals on reimbursement, cracked down on human trafficking, and prohibited sex change procedures for minors.
New Hampshire voters expect to engage with their elected leaders and hold them accountable. Kelly — as she is affectionately referred to by Granite Staters — excels when she is in the towns and communities and is able to meet with people, hearing directly from them and earning their trust. Her “Super 603 Days” initiatives shines a spotlight on all things New Hampshire, from business visits to 5k runs to Rotary groups and fairs. She epitomizes these Granite State traditions where politics is truly local and “in person” versus personal. In 2024, candidate Ayotte received a significant amount of Independent and even Democratic votes. While her policies certainly have crossover appeal, it is also quite possible that she met each and every crossover voter by always being in public around New Hampshire.
Ayotte has also provided more money than ever before for public education, signed a parental bill of rights, and enacted bell-to-bell cellphone ban for children in school.
and deliver in a purple state. Yet in the days of vicious partisan cable-news-game-show-politicians shouting at each other, Governor Ayotte seems quite happy and comfortable being the Granite State workhorse. While no one can say what the future may hold, it is clear that any future Republican candidate for President would be eager to score an Ayotte endorsement, or maybe even consider Ayotte for Vice President or a potential Cabinet role. But with no declared Democratic challenger to even announce a run against her, it seems, for now at least, Kelly Ayotte’s heels are firmly planted in the Granite State. RF
Many Washington insiders are whispering about Governor Ayotte as a possible future presidential candidate — a conservative who can win and then govern
Matthew Bartlett is the co-founder of Darby Field Advisors, a strategic communications and issue advocacy firm based in New Hampshire. He previously served in the State Department, on the staff of then-Senator Ayotte, and on Jon Huntsman’s 2011 presidential campaign.
Antimicrobial resistance (AMR) threatens our economy and people’s lives, with an estimated 1.27 million deaths worldwide each year1. To win the battle against AMR, we need diagnostics.
bioMérieux knows diagnostics—and we’ve invested 75% of our R&D budget to innovation that fights against AMR.
Learn more about our commitment to making the world a healthier place:
1. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis, The Lancet 2022; S0140-6736(21)02724-0.


by ROY BLUNT

For at least a century the United States has led the world in medical research. There has been more change in healthcare and how we think about healthcare in the last 25 years than the collective healthcare advances of all time before that. There are many reasons to believe that the next quarter century, and maybe even the next decade, will make the same kind of incredible progress. The United States should commit itself to making the most of that next generation of healthcare
and maintain our position as the world’s premier leader in medical breakthroughs.
In 2015, I had the great opportunity to become the chairman of the Senate Appropriations subcommittee that funds the majority of the healthcare agencies, including the National Institutes of Health (NIH). The Republican-led United States House of Representatives that was elected in 1994 had pledged to double NIH funding in a decade, and they did. The commitment
was fulfilled there and in almost every other area of the Contract with America.
However, in the 10 years which followed that decade of increased baseline funding for health research, there was little increase – not keeping up with inflation – and by 2015 the estimate was a loss of research buying power of about 22 percent.
Young researchers were leaving health research and taking their amazing brain power somewhere else. Promising research was moving forward at a pace that was way too slow. I decided this was unacceptable, and my top priority for the Appropriations Subcommittee that I led would be to make sure this funding was headed the right direction.
Congressman Tom Cole, who was Chairman of the House Appropriations Subcommittee at the time, and I had a shared determination to do more for diseases – from Alzheimer’s that affects tens of millions to equally devastating diseases that are incredibly rare. Our colleagues on the other side of the aisle also believed health research should be a priority and came on board to accept it as a top priority.
In 2003, NIH surprised the scientific world when it dramatically beat its own timeline for the human genome project and successfully mapped the human genome. How we think about and talk about healthcare changed dramatically. We began to use terms like personalized medicine, predictive medicine, precision medicine, stratified medicine, and next generation medicine.
In 2009 and 2010, the vaccine for pneumonia was improved and advancements were developed around rapid testing for tuberculosis. In 2015, we saw major advances in CRISPR technology, and with it came the possibility to eliminate some chronic genetic diseases before they would even occur in an individual.
In 2017, NIH invested in the evolution of a new way to accelerate vaccine development against epidemic threats, and four years later mRNA made it possible to have a vaccine for COVID in nine months instead of the more traditional time period of at least three years. In 2021, research improved the oral polio vaccine, and it was deployed for emergency use to control outbreaks in over 21 countries.

Roy Blunt
When a country is first in health research, the people of that country benefit the most, but the economic opportunity of being first is also significant. Just a few of the areas that will rapidly develop include CRISPR technology, microbial medicine, the AI applications in healthcare research, and analyzing healthcare data. Others will include injections for joints that could replace surgery, 3-D printed organs, miniaturization of healthcare monitoring devices, as well as patches and watches and other innovations that will monitor health.
The United States should commit itself to making the most of that next generation of healthcare and maintain our position as the world’s premier leader in medical breakthroughs.
We also began to focus on the limitless concept that each of us is individually different from all of the rest of us. No one else replicates you, and no other life experience replicates your life experience. With this new focus – from DNA to mental health – healthcare began to change.
And NIH continued to lead.
Exciting things were happening. NIH was encouraging research in every state and created an environment where that research ensured American leadership in healthcare advances around the world. In 2006, we had the first vaccine for cervical cancer, and that cancer now has a very different likely outcome.
Many Americans in the near future will be more likely to be contacted by their healthcare provider than they are to be calling their healthcare provider. Many more public private partnerships will occur in healthcare as these new technologies develop.
In this quickly changing world of healthcare, who leads will make a big difference. The answer to this challenge should be “America First.” RF
Roy Blunt served in both the U.S. House of Representatives (1997-2011) and the U.S. Senate (2011-2023), where he was Chairman of the Senate Appropriations Subcommittee on Labor, Health and Human Services, Education, and Related Agencies. He currently is the Chairman of Leadership Strategies Advisory Services at HB Strategies, and serves as a Fellow at the Bipartisan Policy Center and on the Tenet Healthcare Board of Directors.
by BUDDY CARTER
For want of a nail the shoe was lost; for want of a shoe the horse was lost; and for want of a horse the rider was lost, being overtaken and slain by the enemy, all for want of care about a horse-shoe nail.
-Benjamin Franklin, 1758
China is the United States’ pharmacy – it decides if we have the medicines we need to keep our citizens healthy.
When the health of our nation is put in the hands of a hostile foreign entity, a public safety crisis develops, one that requires an increase in domestic and friend-shored manufacturing to address.
The United States should never be dependent on the Chinese Communist Party for antibiotics and essential medicines; Republicans and Democrats alike agree on this concept. But that’s exactly the dangerous position we are in today, due to rampant outsourcing by pharmaceutical companies.
In 2002, the United States manufactured 72 percent of the pharmaceuticals it consumed. By 2023, that number had dropped to just 37.5 percent. We didn’t just outsource manufacturing — we outsourced the sovereignty and safety of our health care system. We traded our national security for a horse-shoe nail.

firsthand during the COVID-19 pandemic. According to a conversation I had with the Administration for Strategic Preparedness and Response, or ASPR, under the Trump Administration, the United States saw a downtick in the amount of personal protective equipment and pharmaceuticals coming to our country from China in the fall of 2019. We didn’t learn about COVID-19 until January 2020. China knew there was an unidentified sickness in its own country, concealed it, and then withheld medical supplies so the United States was less prepared when COVID-19 hit our shores.
The United States should never be dependent on the Chinese Communist Party for antibiotics and essential medicines. But that’s exactly the dangerous position we are in today.
China is not our friend. Every product component that then turns into a vial of medicine or a piece of medical equipment that is made in China is a missed opportunity to strengthen our economy and protect our people. We need to view pharmaceutical and health care supply chain independence just as we are viewing energy independence.
We saw the impact of this dependence on China
As both a pharmacist and a member of Congress, I find this to be deeply concerning, and it is a situation we could find ourselves in again if we fail to take decisive action now. Under the Biden-Harris Administration, over 323 drugs were in shortage during the first quarter of 2024 – an all-time high – and cancer patients were often forced to switch treatments, adjust dosage regimens, or, in extreme cases, unable to receive their lifesaving medications. This is unacceptable in the United States of America. There was no comprehensive effort to support American manufacturers or reduce our reliance on foreign supply chains, even after the lessons supposedly learned during the pandemic. We can’t afford to learn this lesson the hard way twice.
Thankfully, President Trump is working around the clock to bring powerful investments to the United States that will unlock pharmaceutical dominance and bring an end to the poor policies that created the crisis we find ourselves in today, which harms patients most of all.
Under the leadership of President Trump, we are bringing
pharmaceutical manufacturing back to America. In just a few short months of his second term, Johnson & Johnson broke ground on a new $2 billion facility in North Carolina, Eli Lilly announced $27 billion in new U.S. manufacturing, Amgen announced a $900 million manufacturing expansion in Ohio, AbbVie committed $10 billion to invest in the United States, and Sanofi announced plans to invest at least $20 billion. These are just a few examples. This is just the start of an era of dominance.
In 2002, the United States manufactured 72 percent of the pharmaceuticals it consumed. By 2023, that number had dropped to just 37.5 percent.
My home state is showing up and doing its part as well. It is no coincidence that Georgia – the No. 1 state in the nation in which to do business – is home to Manus Bio, which has invested nearly $60 million and created over 100 jobs with the acquisition of a new manufacturing facility in Augusta. We need more policies at the federal level that mirror the progrowth ones we have in the state of Georgia, including low taxes and a high-quality workforce.
To make the rest of the nation look more like Georgia, House Republicans passed the One Big Beautiful Bill Act , which incentivizes domestic medical supply production by rewarding companies that build their products in America, like USAntibiotics, which is the last remaining end-to-end domestic U.S. manufacturer of amoxicillin, the most prescribed antibiotic in the country. With this bill, we are not only saving American lives, but we are also strengthening our economy, unleashing manufacturing dominance, and bringing hope to patients nationwide.
I am proud to stand with President Trump and all those committed to putting America First in our health care system — starting with the medicines we rely on every day. RF
Buddy Carter represents the 1st District of Georgia in the U.S. House of Representatives.
Serving approximately 100 million customers worldwide with TurboTax, Credit Karma, QuickBooks, and Mailchimp, Intuit helps put more money in consumers’ and small businesses’ pockets, saving them time by eliminating work and ensuring they have confidence in every financial decision they make.

by MICHAEL BAKER
Vaccines have had a transformative impact on public health by dramatically reducing the prevalence of vaccinepreventable diseases across the globe. The United States has traditionally been a leader in vaccine development and administration, and our national health and economy have benefited greatly. Nevertheless, increased skepticism surrounding vaccines threatens to reduce future vaccine uptake and erode the health and economic benefits Americans currently enjoy. While there is no easy solution to combat increased skepticism, concerted efforts by public health officials, policymakers, politicians, and the public alike can preserve the United States’ relatively high uptake of vaccines and continue to reap their numerous benefits.
The creation, development, and deployment of vaccines – a U.S. federal priority since the 1960s – has been one of the greatest health care achievements in history. President John F. Kennedy signed the Vaccine Assistance Act in 1962 to create a federal support system for vaccinations in states and communities. Widespread immunization programs have led to the near elimination of diseases that once caused significant morbidity and mortality. For example, before the introduction of the measles vaccine in 1963, an estimated 3–4 million people contracted measles annually in the United States. Today, case numbers are in the hundreds, largely among unvaccinated populations. Similarly, polio –which paralyzed more than 15,000 Americans each year during the early 1950s – has been eliminated domestically since 1979 thanks to aggressive vaccination efforts.
healthier, but their value is not limited to making Americans less likely to get sick. Both childhood and adult vaccinations create high resultant returns on investment. Vaccines significantly reduce direct health care expenditures by preventing diseases before they occur. This preventive approach is much more costeffective than treatment-based strategies. For instance, routine childhood immunizations in the United States from 1994–2023 are estimated to have prevented around 508 million cases of illness, 32 million hospitalizations, and more than 1 million deaths. In dollars, this prevention results in approximately $540 billion in direct medical cost savings, with almost $2.7 trillion in total societal savings due to illness prevention.

Michael Baker
The creation, development, and deployment of vaccines – a U.S. federal priority since the 1960s – has been one of the greatest health care achievements in history.
Reductions in morbidity should be enough to demonstrate that vaccinations make the United States
This calculation means that every dollar spent on general childhood immunization resulted in $11 of savings. The long-term benefits, however, aren’t limited to childhood. The broader impact on labor productivity gains is also substantial. Healthy employees perform better, contribute more effectively, and sustain fewer interruptions in their tasks. According to economic analyses, the aggregate productivity benefits of adult vaccinations extend beyond immediate reductions in absenteeism and presenteeism. According to one report, absent workers at U.S. companies cost around $150 billion each year, while those who came to work but weren’t fully functioning due to illness cost $1.5 trillion per year in lost productivity. In another instance, comprehensive immunization programs, including booster shots for COVID-19 and influenza vaccines, are estimated to return significant economic value, with some studies suggesting
returns ranging between $2–$4 for every $1 invested due to improved worker productivity and reduced health care costs.
There are even more benefits to vaccines. Private and public sector biomedical development have enormous associated economic gains for the United States. The U.S. bioscience industry, as measured by overall output, totaled more than $3 trillion in 2023. Another recent report underscores the substantial economic benefits generated by the National Institutes of Health (NIH) through its research funding. The analysis reveals that in fiscal year 2024, every dollar invested by the NIH resulted in approximately $2.56 in economic activity, highlighting the agency’s pivotal role in stimulating the U.S. economy. Over the past decade, NIH funding has been instrumental in driving over $787 billion in new economic activity and has supported an average of more than 370,000 jobs annually.
In recent years, however, Americans have become more skeptical of the safety and efficacy of vaccines – the effect of which has been to reduce their uptake – making the United States more susceptible to unpleasant and in many cases deadly illnesses. While individuals have reasons for their worries, these concerns have been repeatedly studied and central claims of this skepticism have been addressed.
data to the FDA for licensure. Independent FDA advisory panels review the data, and the FDA often holds public meetings to promote transparency. Only then is a vaccine approved.

Policymakers should enhance and modernize vaccine safety infrastructure, as well. This includes expanding data integration between federal and state immunization registries, upgrading monitoring platforms, and funding independent research into rare adverse events. Even after approval, vaccines undergo post-marketing surveillance. Emphasizing real-time safety surveillance systems – such as the Vaccine Adverse Event Reporting System (VAERS) and the newer V-Safe platform – can help reassure the public that vaccine safety is an ongoing priority. These systems ensure continued monitoring and rapid response to any unexpected issues, reinforcing public safety long after rollout. Increased transparency around safety data and adverse event investigations will help counteract the perception of secrecy surrounding vaccine research and production that fuels conspiracy theories.
Routine childhood immunizations in the United States from 1994–2023 are estimated to have prevented around 508 million cases of illness, 32 million hospitalizations, and more than 1 million deaths.
This leads to two key recommendations for addressing vaccine skepticism in the United States: transparent, plain-language, and proactive communication about vaccine development, testing, approval, and postlicensure monitoring; and modernization and promotion of vaccine safety infrastructure.
Vaccine development is one of the most rigorous and carefully regulated processes in modern medicine. On average, it takes 10 to 15 years for a vaccine to move from preclinical research to full regulatory approval. It begins with preclinical research, where scientists identify a target pathogen and test candidate vaccines for safety and immune response. Only promising candidates advance to human trials, which occur in three phases. If a vaccine proves safe and effective in each of the trials, manufacturers submit
Both of these efforts – improved literacy and modernization of vaccine safety mechanisms – combined with acknowledgement of the positive, communal (sometimes invisible) impacts of vaccination, are important steps to ensure that skepticism is addressed and declining uptake is slowed.
In the United States, vaccination efforts have significantly reduced disease burden, prevented millions of deaths, and saved billions in health care costs annually. To preserve these benefits, vaccine confidence must be restored. It will not be remedied overnight; it is earned through transparency and sustained engagement. By modernizing safety systems, improving access, and fostering trust, federal policymakers can protect the country’s health and preserve the life-saving legacy of vaccination. RF
Michael Baker is Director of Health Policy at the American Action Forum.
by MATTHEW E. KAHN
As of 2023, roughly 194 million U.S adults had at least one chronic condition. Chronic diseases, such as diabetes and hypertension, cost the United States economy billions of dollars each year. It has been estimated that 80 percent of the Medicaid expenditure is spent to improve the health of people with chronic diseases.
While increasing affordable access to new drugs such as the weight loss GLP-1 medications offer the promise of achieving significant weight loss, our society’s ability to reduce the costs associated with chronic conditions continues to be tied to encouraging behavioral change.
Throughout our lives, our health is influenced by the complex interplay between our genetic makeup, our investment in life skills, our choices regarding nutrition and exercise, our exposure to pollution and extreme weather conditions, and our access to affordable and effective medical care and medications. At every stage of life, we face trade-offs regarding how much time and effort we are willing to invest in our health.
in
of facing chronic conditions.
Economics research has extensively studied risky behaviors among teens and young adults, specifically in relation to nutritional choices and smoking. The rational addiction hypothesis posits that people are less likely to start smoking or indulge in excessive junk food consumption if they anticipate that the prices of these products will rise over time. Conversely, easy access to cheap, tasty fast food contributes to these behaviors. Some public finance economics research has explored how policies such as sugary drink taxes can change behavior. When he was the mayor of New York City, Michael Bloomberg championed these policies.

Chronic diseases, such as diabetes and hypertension, cost the United States economy billions of dollars each year.
Genetic predispositions can significantly influence our risk of chronic diseases as we reach middle age. Young people are often aware of the medical conditions that their parents and grandparents have faced, and this awareness provides a useful indicator of the risks they may encounter. Whether individuals choose to proactively protect themselves depends on several factors. Economic research highlights that parental involvement and early life interventions can help young people develop self-control and discipline. This "grit" enables individuals to avoid temptations and to be more self-disciplined in mid-life. This reduces their risk
In recent decades, access to medical care has increased for many Americans. A growing number of individuals are dealing with prediabetes, which can be identified through blood tests indicating elevated blood sugar levels. To lower the risk of developing diabetes, proactive measures such as weight loss, reduced sugar intake, a healthier diet, and increased physical activity can be beneficial. In recent decades, the health performance of many diagnosed diabetics has improved such that their risks of complications have declined relative to earlier birth cohorts of diagnosed diabetics.
When newly diagnosed with a chronic disease, some people are highly motivated to engage in behavioral change. Those who are more educated, possess greater self-control, and have a support network are more likely to pursue this path. Other people may be technological optimists who believe that
advancements in medical care will rescue them by subsidizing their access to medications that can mitigate the side effects of their condition.
In this age of Big Data, empirical economists have increased opportunities to test new ideas for cost-effectively bringing about behavioral change. One recent study set in India provided financial incentives to people at risk of becoming a diabetic to walk more steps each day. Since the study was careful to use a randomization approach to determine who was offered the walking incentive, the existence of a control group means that the researchers can test the hypothesis that well designed financial incentives are a cost-effective way to spur behavioral change among those with a key chronic condition.
Arnold Schwarzenegger recently said; “If you stop movement, then this is the first step to death,” he said. “If you rest, you rust,”
one’s health. Basic economic logic predicts that the incentives of both “carrots and sticks” are needed. A carrot would be to offer financial payments for those who engage in healthy habits that can be objectively measured such as walking steps being measured by Cell Phone GPS systems. This intervention could eventually pay for itself by lowering future Medicare and Medicaid expenditures.

It has been estimated that 80 percent of the Medicaid expenditure is spent to improve the health of people with chronic diseases.
This famous Republican is using his social media platform to nudge his fans. Unfortunately, I doubt that this is sufficient to change behavior and encourage greater personal responsibility in building up

As the United States now spends roughly 17 percent of GNP on health care, it is important to consider alternative “rules of the game” regarding insurance pricing. If insurers could charge different prices for annual health premiums based on personal attributes such as one’s blood sugar level and one’s weight, then this would introduce a strong financial incentive for people to invest more in being healthy. Our current system’s rules preclude this. Both the rates of chronic disease and their private and social costs are rising. Facing this reality, what steps are the American people willing to introduce to bend this curve? RF
Matthew E. Kahn is the Provost Professor of Economics at the University of Southern California and a Visiting Fellow at the Hoover Institution and a Senior Scholar at the USC Schaeffer Institute.
by VIKAS SAINI, M.D.
Overprescribing, or what we have termed “medication overload”, is a major feature of modern healthcare in the U.S. and around the world. It is the act of giving a patient a medicine that on balance adds more risk than benefit, because the drug itself is either unnecessary, duplicative, given in an excessive dose or duration, increases risks due to pre-existing “polypharmacy” or is simply not the best treatment option.
The scope of the problem in the U.S. is huge. A famous example is opioid overprescribing, which in the 2000’s was responsible for a large proportion of drug overdose deaths. Another well-known problem is that roughly 20-40 percent of antibiotic prescriptions are unnecessary or inappropriate. That is a real danger to us all because it contributes to the development of antibiotic resistance in bacteria which can then become untreatable if they successfully infect any of us, potentially leading to more severe illness and even death. Antidepressants, proton pump inhibitors, ADHD meds, and statins are all frequently overprescribed. A related but distinct problem is medication overload, when multiple drugs, each of which might be perfectly reasonable in isolation, create unnecessary risks when combined. More than four in ten older adults take five or more prescription medications.
reduced quality of life from the burden of managing multiple medications and dealing with their side effects; and increased healthcare costs.
Depending on what you count, overprescribing costs the United States anywhere from a few billion dollars a year in easily measurable drug waste to more than half a trillion dollars if you include hospitalizations, emergency visits, doctors visits, and deaths from inappropriate or excessive medication causes. There are lots of small niches of waste (antibiotics, oncology, vial sizes, etc.) that can each add hundreds of millions or a few billion dollars apiece and which together can really add up.

Vikas Saini
Depending on what you count, overprescribing costs the United States anywhere from a few billion dollars a year in easily measurable drug waste to more than half a trillion dollars…
The consequences of overprescribing include poor patient outcomes such as increased risk of side effects, including falls, fractures, cognitive impairment, and drug interactions; drug dependency and addiction,
Addressing overprescribing therefore represents a major opportunity for stewardship of healthcare dollars: curbing unnecessary prescribing would free up billions annually—and spare thousands of people from avoidable harm.
There are many interrelated drivers of unnecessary health care like overprescribing. Chief among them is a desire and expectation that the doctor do something. Equally important is the often fuzzy nature of diagnosis. It’s easy to over-diagnose a condition “just to be sure,” especially when there are no disincentives to do so. Fortunately, the U.S. has avoided situations like France or China, where there is an even bigger culture of prescribing (in China’s case, driven by financial rewards for doctors who can
make money dispensing medicines.) One example is the rising rates of diagnosis of ADHD in children, followed by alternative non-pharmacologic therapies minimized.
The MAHA “movement” has put a spotlight on the widespread problem of chronic diseases, the so-called “diseases of lifestyle”. There’s been a longstanding dichotomy in their management between prescribing a pill versus practicing prevention by changing lifestyle. The case of high blood pressure is an excellent example. There are many drugs to treat it, but there’s clear evidence that dietary salt, lack of exercise, and alcohol consumption all drive blood pressure up. Trying to control it by adding one pill after another can be expensive and frustrating. For chronic diseases like hypertension, especially when they are mild, our health care system isn’t currently configured to offer many options besides medications or a lecture.
them once the label is attached to the person needs to allow for flexibility and a step-ladder approach. For the lower risk end of an illness, early in its course, at younger ages, emphasizing lifestyle changes is crucial.
Other things we can do:
-Revise the curriculum in med school, continuing education, and in practice guidelines (e.g., for antibiotic prescribing).

The best way to prevent the downstream effects of overprescribing is to prevent it in the first place. That also means a concerted effort to prevent overdiagnosis.
In my experience, one common denominator of many chronic illnesses is psychosocial stress. This is understudied, but there is growing science showing how the mind and body interact through the nervous and immune systems. Maybe in the future that will lead to more drugs, but maybe it will show us how to improve health without drugs.
To change things, to improve health and wellbeing and to save money will take an integrated effort. Obviously, the best way to prevent the downstream effects of overprescribing is to prevent it in the first place. That also means a concerted effort to prevent overdiagnosis.
Many of the thresholds for labeling a disease as a disease are fuzzy. Most importantly, not all versions of a disease need the same treatment: how we treat
-Make deprescribing protocols into a major campaign, including funding pilots to implement standard protocols, making deprescribing protocols an essential element/ a requirement of insurance contracts, ACO’s etc.
-Change clinical training to emphasize better reasoning and risk calculations. (Pharma might be advertising that drug reduces risk by 50 percent, but if the absolute risk of the disease is only 1/10 of one percent, then the treatment is only buying you an absolute risk reduction of 1/20 th of one percent.
-Encourage, simple practical interventions like mandating vial size reform for expensive cancer agents to reduce drug waste.
-Push harder to make the NON-pharmacologic option visible, available, and attractive though changes in labeling, advertising, public service announcements, etc. This requires a massive educational campaign around lifestyle choices, but the payoff in savings would be big.
It’s equally important to recognize that not all lifestyle elements are subject to “choice” when we are trapped in unwalkable neighborhoods or holding down two jobs and struggling with child care, so efforts to level the playing field by making the healthy choice the easier choice through policy interventions are critical. RF
Vikas Saini, MD is president of the Lown Institute. He is a clinical cardiologist trained by Dr. Bernard Lown at Harvard, where he has taught and done research.
by LUCY ORR-EWING
Last month, the White House launched their AI Action Plan at an event entitled, “Winning the AI Race.” The plan lays out a U.S. roadmap to establish global dominance reminiscent of preceding races in space exploration and nuclear weapons.
This race, however, has a less obvious endpoint than putting a man on the moon. Indeed, the point at which the winner will be declared is unclear. It will unlikely be marked by the development of a single breakthrough AI tool that becomes widely used across society. Instead, success will rest on building the robust, secure infrastructure that enables many AI innovations to flourish while ensuring trust in the technology through the quality of its outputs and the responsibility with which it is applied.
While many nations are advancing in this race, the United States views China as its principal competitor. With both nations releasing increasingly capable new models, solutions, and robotics, public trust in AI has diverged sharply between China and the U.S. A recent United Nations Development Program survey measuring confidence that AI systems are designed in society’s best interest found trust levels at 83 percent in China compared with just 38 percent in the U.S.

They developed an AI tool called EchoNext that accurately identified structural heart disease from electrocardiogram readings more frequently than cardiologists, flagging more than 7,500 high-risk patients in eight months. Meanwhile, at least 70 percent of healthcare providers still exchange medical information using a fax machine (according to Steve Posnack, deputy assistant coordinator in the Office of the National Coordinator for Health Information Technology). Many still are not able to access a complete patient record digitally. For modernization to truly take hold, and for adoption of AI to be systematic and widespread, we need greater confidence in its safety and effectiveness.
A recent United Nations Development Program survey measuring confidence that AI systems are designed in society’s best interest found trust levels at 83 percent in China compared with just 38 percent in the U.S.
Experts are far more optimistic about AI than the general public. For example, Pew Research found that AI experts feel that “AI will have a very positive impact“ on the United States over the next 20 years (56 percent vs. 17 percent). China’s high-trust environment could enable it to close the AI adoption gap more quickly and take the lead in global AI. Ultimately, the AI race will be won or lost by the country that succeeds in building genuine public trust in the technology.
The health sector’s uptake of technology remains uneven. Some partnerships, like that of NewYork-Presbyterian and Columbia, show the extraordinary transformation within reach.
The precedent exists for our achieving that goal. Indeed, in 1968, the U.S. National Highway Traffic Safety Administration (NHTSA) mandated seatbelts and introduced new crash safety standards. From 1968 through 2019, NHTSA’s safety standards prevented more than 860,000 deaths on the nation’s roads, 49 million nonfatal injuries, and damage to 65 million vehicles. Today, automakers now compete on safety features (see Volvo’s consistent seatbelt marketing). In the 1950s, air travel was perceived as dangerous, with a fatal accident rate of roughly 5 deaths per 100,000 flight hours. After the Federal Aviation Administration introduced stringent pilot training, mandatory black box monitoring, and advances in aircraft design, that rate has dropped to 0 deaths per 100,000 flight hours for scheduled service flights, with the U.S. National Airspace System now operating more than 45,000 commercial flights a day.
Other sectors have signaled that policy change to prioritize safety can and does restore trust and confidence in the marketplace, which in turn fuels adoption, drives competition, and accelerates growth. As U.S. Sen. Mike Rounds (R-SD) said
at the top of a July 30 Senate Banking insurance subcommittee hearing, “we need regulatory frameworks that both support innovation and protect consumers.” Hard policy levers, in the form of regulation, legislation, and funding incentives, can support innovation in healthcare by investing in three essential building blocks:
1. Privacy-preserving data systems that let information stay local (e.g. in a health system) so that developers can securely access the right data;
For modernization to truly take hold, and for adoption of AI to be systematic and widespread, we need greater confidence in its safety and effectiveness.
2. Continuous monitoring to track safety, bias, and performance in real time so that failures or degradation can be corrected in real-time; and,
3. Public benchmarks and registries so AI tools can be tracked, compared, reproduced, and improved to raise quality and lower cost.
These investments would make it easier for innovators to develop safe, effective tools and for health systems to adopt them quickly, ensuring that people in rural, tribal, and urban communities alike can benefit from AI.
Building a clear, strong national infrastructure for AI in healthcare is not just about technological progress, it is

about building trust, closing care gaps, and guaranteeing that every patient has access to tools that can improve care. As Senator Rounds noted, the AI Action Plan “recognizes the urgency to accelerate innovation, incentives to build AI infrastructure and lead in international diplomacy and security, all while acknowledging the need to address potential risks and promote trustworthy AI.”
The “move fast and break things” slogan that was coined by Mark Zuckerberg and is at the heart of AI development in Silicon Valley today is diametrically opposed to the credo of “do no harm” in healthcare. Therefore, AI moves at the speed of trust. If the United States is to maintain global leadership, we need to radically prioritize transparency and trust because only then will we see meaningful adoption, better performance, and real-world impact for patients. RF
Lucy Orr-Ewing serves as Chief of Staff and Head of Policy for the Coalition for Health AI (CHAI), a nonprofit coalition dedicated to ensuring widespread development and deployment of Responsible AI in healthcare.







by SALLY C. PIPES
In a May 12 executive order, President Trump announced a "most favored nation" policy that intends to lower prescription drug prices.
Among other things, the order directed the Secretary of Health and Human Services to "communicate most-favored-nation price targets to pharmaceutical manufacturers to bring prices . . . in line with comparably developed nations." The Trump administration wants to peg U.S. drug prices to the lowest price available in our peer nations.
Other countries have lower prices on drugs because their governments forcibly cap them. Most favored nation amounts to the importation of socialist foreign price controls. As a matter of principle, the U.S. government should not have the power to dictate the prices of goods and services in a free society.
Further, pharmaceutical price controls have significant long-term costs that far exceed any short-term benefits for patients today. Price controls dampen investment and thereby deprive people now and in the future of the benefits of medical innovation.
At present, the United States leads the world in pharmaceutical development. Two in three new drugs are developed here.
Consider the consequences of the Inflation Reduction Act, which President Biden signed into law in 2022. It levies price controls on a steadily increasing number of drugs through Medicare, starting with 10 drugs dispensed through Medicare Part D effective January 1, 2026.

Sally C. Pipes
At present, the United States leads the world in pharmaceutical development. Two in three new drugs are developed here.
Price controls could knock us from our perch. That's because they reduce the potential return on investment in drug research. Such work is already risky. It takes between ten and fifteen years and roughly $2.6 billion to bring a drug from the lab to the patient's bedside. Roughly nine in ten drug candidates fail.
If price controls threaten the returns of the few drugs that succeed, then investors will deploy their capital elsewhere.
We're already seeing as much in the United States.
In response, pharmaceutical research has been drying up. Since the passage of the IRA, drug companies have discontinued at least 51 research programs and 26 drugs. One study projects that the IRA's price controls will result in the development of 139 fewer drugs by 2035.
Most favored nation would further devastate drug research. If applied to Medicare, it would lead to 869,000 fewer jobs over a decade, according to a June report from research firm Vital Transformation. The cumulative earnings lost thanks to the destruction of those jobs would be $2.8 trillion. Tax revenue would decline by $700 billion.
People might even find themselves paying more for drugs. A recent study from the Pioneer Institute found that MFN could distort the prescription drug market in ways that raise seniors' out-of-pocket costs.
That conclusion rings true, given the impact of the IRA's price controls thus far. A study published last year found that most enrollees in Medicare's Part D prescription drug benefit who take price-controlled medications will see their out-of-pocket costs increase from 2025 to 2026.
There are far less destructive ways to make prescription drugs more affordable.
For starters, policymakers can address the manipulation of the pharmaceutical market perpetrated by pharmacy benefit managers, the middlemen that negotiate with drug
(cont’d on page 28)
by PAUL GINSBURG & STEVE LIEBERMAN
Prices for brand drugs in the United States are three times as high as prices paid in other wealthy countries. With prescription drugs accounting for 10.1 percent of national health expenditures in 2024, high prices substantially burden individuals, employers and governments, the proverbial payers in American health care. One of the dominant political debates of this century has been over how to relieve that burden while not damaging pharmaceutical innovation.
Those seeking to lower drug prices by championing market solutions over regulation discount the extensive barriers to a functioning market. Those advocating for price controls downplay the critical relationship between expected prices and the flow of new treatments.
There is a way forward, what we call “wise regulation,” based on assessing the value of new drugs to patients. It could result in a uniquely American solution, but to get there, we need to understand why high drug prices are so resilient.

full amount above an annual out-of-pocket maximum), health insurance limits market competition in making drugs affordable by sharply diluting patients’ incentives to use less expensive drugs. Recent insurance reforms that have limited per enrollee annual drug cost and have expanded coverage have likely facilitated higher prices when drugs launch and increasing prices for existing drugs.
Under pressure from regulators to keep patient out-of-pocket costs for expensive drugs low and yet not raise premiums, insurers rely more heavily on administrative tools, such as prior authorization and step therapy, to restrain spending. In addition to facing increasing resistance, these tools have modest impact when highpriced drugs effectively treat the patient’s condition.
The main constraint on manufacturers’ monopoly pricing occurs only when effective therapeutic alternatives — different drugs that treat the same condition — are available.
First, most branded drugs have market exclusivity through their patents or FDA requirements. The main constraint on manufacturers’ monopoly pricing occurs only when effective therapeutic alternatives—different drugs that treat the same condition—are available. (One savings opportunity involves ending manufacturer abuses of current rules to extend exclusivity far beyond statutory expectations.)
The same comprehensive health insurance that makes drugs more affordable to patients severely limits the role of demand in constraining prices. By paying most prescription costs (and the
Price controls could ease the impact of drug exclusivity and reduce pressures on insurers, but there are two key challenges: The first is the absence of meaningful information on costs of developing specific new drugs, a key component for assessing returns on investment. Many attempts to develop new drugs fail; for investors, these failures are part of the overall cost of developing successful drugs. As a result, approaches to regulate prices of services, such as hospital stays, cannot transfer to prescription drug price regulation.
Second, drug price regulation needs to focus on value, allowing the highest prices for drugs that most significantly improve patient health or reduce mortality. When incentives are revised to focus on value, investors will differentiate high-value opportunities from high-revenue opportunities under current
(cont’d on next page)
(Ginsburg
& Lieberman, cont’d)
rules. By incentivizing capital markets to steer investment to innovations with the strongest prospects, a revised system will reward development opportunities that are projected to have the highest value.
Organizations such as Institute for Comparative Effectiveness Research increasingly measure the value of high-priced drugs, with these assessments informing regulators and insurers when deciding coverage and pricing. The field is advancing, including development of methods that do a better job in measuring how patients themselves value treatments, such as GRACE (Generalized Risk Adjusted Cost Effectiveness). The key will be allowing those drugs with the largest patient outcome improvements the highest prices.
Drug price regulation needs to focus on value, allowing the highest prices for drugs that most significantly improve patient health or reduce mortality.
The Inflation Reduction Act (IRA) has initiated regulating drug prices for Medicare beneficiaries and for long-established high-cost drugs, with rules heavily favoring the government. Although regulating prices in Medicare for drugs that have generated many years of high profits limits reducing returns on investment, the approach omits a very large and growing part of the drug cost problem—prices paid by other payers and for newer, high-cost drugs.
Less funding for innovation is inevitable if drug prices are to be controlled, although the market will, to some extent, respond by setting higher initial launch prices. The key to effectively
constraining spending on drugs without stifling innovation is regulating drug prices wisely, with the goal of having reductions in funding concentrated in innovations that have the most limited prospects of increasing value to patients. In addition to funding the measurement of value, wise regulation would involve all payers and create a meaningful process for manufacturers and payers to negotiate prices, fairly balancing the competing interests of manufacturers, patients, and payers while maintaining adequate incentives for innovation. If unable to agree, a multi-stakeholder group could set the price, perhaps through “baseball style” arbitration that chooses from each side’s “best and final” offer. Yes, there are risks to regulation, but the burden of high drug costs is now so great that the only realistic alternative to wise regulation today is eventual unwise regulation tomorrow. RF
Paul Ginsburg is a senior scholar at the USC Schaeffer Center for Health Policy & Economics, Professor of the Practice of Health Policy at the USC Price School of Public Policy and is a former vice chair of the Medicare Payment Advisory Commission. Steve Lieberman is a nonresident senior scholar at the Schaeffer Center, a former assistant director at both the Congressional Budget Office and the White House Office of Management and Budget, and a former senior adviser to the Administrator of the Centers for Medicare and Medicaid Services.
(Pipes,
cont’d)
manufacturers on behalf of insurers. In exchange for giving drugs preferential placement on a health plan's formulary, or list of covered drugs, PBMs command massive rebates and fees from pharmaceutical companies.
Those rebates are typically calculated as a percentage of a drug's list price. So, the higher the list price, the bigger the payday for a PBM. As a result, PBMs have a financial incentive to favor pricier drugs on health plans' formularies.
Most favored nation would further devastate drug research.
PBMs' rebates and fees sometimes exceed a drug's price in other countries. A 30day supply of Eliquis generates $250 in kickbacks for PBMs. The same drug costs $72 in the United Kingdom – and $33 in Australia.
It's no wonder that PBMs scrape off 42 cents from every dollar consumers spend on brand-name medicines in the commercial market.
Requiring PBMs to pass along the savings they negotiate to patients at the pharmacy counter would do won-
ders to make prescriptions more affordable. Similarly, "delinking" PBMs' compensation from drug prices would remove their incentive to favor the most expensive drugs. Foreign freeloading is also a problem. Americans bankroll the majority of drug development because we pay higher prices. Other countries want access to our market, the world's largest. Our leaders should insist that they shoulder a greater share of the global research bill as a condition of trading with us.
The Trump administration's focus on lowering drug prices is understandable. But price controls are the wrong prescription. RF
Sally C. Pipes is President, CEO, and Thomas W. Smith Fellow in Health Care Policy at the Pacific Research Institute. Her latest book is The World's Medicine Chest: How America Achieved Pharmaceutical Supremacy -and How to Keep It (Encounter 2025). Follow her on X @sallypipes.


July 2, 1939 – August 14, 2025
The Honorable Mike Castle, who was the sole representative of Delaware in the U.S. House of Representatives, passed away at the age of 86 on August 14, 2025.
Throughout his remarkable fourdecade career in public service, Mike earned a reputation of kind and bipartisan leadership, extending from his early days in the Delaware General Assembly through his tenure as state legislator, Lieutenant Governor from 1981 to 1985, and two terms as Governor from 1985 to 1992, before representing the First State in Congress from 1993 to 2011.
In addition to leaving a strong legacy of bipartisanship both in Washington and at the helm of the state’s legislature as Governor, Lieutenant Governor, and state legislator, Mike regularly lent his invaluable expertise to The Ripon Society as a member of the Congressional Advisory Board as well as influencing The Ripon Forum, where he served on the editorial board for nearly a decade.
but fail to work with their colleagues on the other side of the aisle. We can respect each other and find common ground without dismissing opinions that differ from our own,” he shared with our group.
His advocacy for this legislation
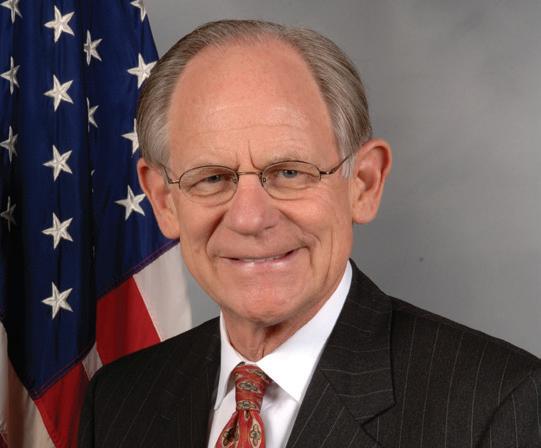
2010. “We must work together to protect the safety and future of our children, families, and communities by updating our country’s juvenile justice system and providing effective supports and alternatives to at-risk youth,” he wrote. Throughout his career, Mike remained steadfastly focused on building a better America for future generations. Whether through education reform, juvenile justice initiatives, or his famous school visits as Governor, where he personally visited every single school in Delaware, Mike understood that a nation’s true strength lies in how it nurtures and protects its young people.
“Mike understood that a nation’s true strength lies in how it nurtures and protects its young people.”
In one of his memorable appearances before our organization, Mike championed the FAIR Act, bipartisan redistricting reform legislation he co-authored to reduce partisan gerrymandering and encourage greater cooperation in Congress. “So often, legislators elected in their home districts come to Washington with good intentions
reflected his lifelong commitment to strengthening democratic institutions and fostering the kind of principled dialogue our democracy requires.
Mike, who served as Ranking Member of the Subcommittee on Early Childhood, Elementary and Secondary Education, and was a leading sponsor of “No Child Left Behind,” shared his insight on how to help younger generations stay away from crime with The Ripon Forum in the spring of
Mike was also a staunch advocate for America’s fiscal institutions as a senior member of the Financial Services Committee. Among many other notable pieces of legislation, he spearheaded the creation of the 50-state quarters program.
A fiscal conservative and social moderate not afraid to challenge the party line, Mike Castle leaves behind a remarkable legacy that reminds each of us of what dedicated public service can accomplish. His unwavering commitment to putting people before politics will continue to serve as a model for future leaders who understand that effective governance requires both conviction and compromise. RF


Occupation: Representative for North Carolina’s 3rd Congressional District
Previous Positions held: Former President of Eastern Urological Associates in Greenville and Affiliate Professor of Surgery and Chief of the Division of Urology at the ECU School of Medicine; Chief of Staff of Vidant Medical Center; Member of the North Carolina House of Representatives.
In your work as a medical missionary, what was the one medical case that had the biggest impact on you personally? I have probably traveled over 30 times overseas to provide medical relief work. However, the experience in Haiti in 2010 was by far the most influential. Tragically and indiscriminately, hundreds of thousands of lives were lost in an instant because of the earthquake. To add to the suffering of an already devastated nation, months later relief workers introduced cholera which ended up claiming tens of thousands more lives. I will never forget the anguish of a mother, who had already lost three of her children to the earthquake, now devastated by the loss of her daughter the night before to cholera. Within hours, a healthy and joyful child was infected and died in her mother’s arms. I will never forget the cries of unparalleled anguish from that poor mother. I could express a lot more happier stories, but I think this one teaches us a lesson. The joy we all experience should never be taken for granted.
You’re Co-Chair of the GOP Doctors Caucus. What’s your top priority that you’re hoping the group can accomplish this congress? Our goal is to continue working with our colleagues to effectuate meaningful change that will improve access to affordable, high-quality care and lower drugs costs for patients across the country. We are composed of 14 members with real-world experience, eager to deliver solutions to the challenges facing American health care.
How does your background as a doctor shape the way you approach your job on Capitol Hill? As a surgeon, I have little patience for time wasted and the silliness that is sometimes politics. I am wired to act judiciously and decisively when faced with a problem. Washington needs leaders who are swift to take on challenges, averse to delay and dawdling, and driven by the satisfaction of a job well-done to benefit someone else.
Finally, what one bill or initiative would you like to see Congress pass that would make a positive difference in the lives of every Tar Heel? Reimbursements for physicians who see Medicare patients have fallen an inflation-adjusted 33 percent since 2001. Private practice doctors are being forced to close their doors or sell out to large hospitals as a result of these devastating cuts, even though the care they provide is more personal, higher quality, and cheaper than the alternative.





