Jena R. Eggert
Founder&CEORCR|HUB





Jena R. Eggert
Founder&CEORCR|HUB
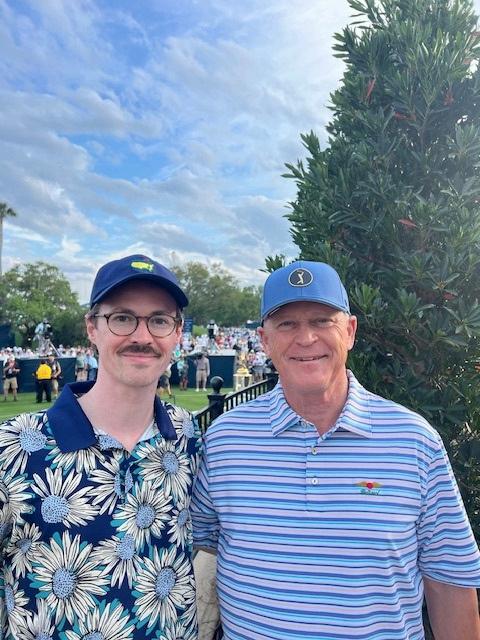
Welcome to our February special edition, featuring Philip Boyce from Baptist Health in Jacksonville. I couldn’t be more excited to launch this edition, and I know both my team and Philip’s team share that excitement.
But before we flip the pages, I want to take a moment to talk about Philip his kindness, generosity, and unwavering support for what we’re building at RCR|HUB.
When I first started this journey, I had a simple vision: to create a space where providers could connect effortlessly without tracking cookies, without friction just a straightforward way to see who’s doing business in bad debt, prior authorization, or any of the 95 categories that make up the revenue cycle. Providers needed that kind of open, digital resource and so did our business partners
Business partners needed more than just visibility; they needed a place to showcase their technology, their people, their offerings a RCM CommUnity-driven platform where they could stand out without breaking the bank That’s what we set out to build, and Philip was one of the first to say, “I like what you’re doing, and I support you.”
Our veryownBaptistBaby!
That said, Philip was very clear about one thing he didn’t want to do the magazine. I spent over a year asking, but he held firm… until now.
When we discussed October 2024, where we’ll be highlighting cancer statistics, survivors, and technology, Philip didn’t just decline—he pointed me in the right direction. He told me, “You need to speak to Michele Bear.” And he was right. That conversation led to one of the most powerful interviews we’ve had if you haven’t read it yet, I highly recommend you do
So, here we are today, with Philip finally agreeing to take the lead on this edition, and I promise you’re going to love it.
Our sponsors have leaned in with creative, Valentine’s-themed contributions, adding a fun and engaging touch to this issue. And before I wrap up, I have to take a moment to thank Paulina Molina, my incredible marketing manager She’s the real deal the one who keeps everything running smoothly behind the scenes Now, I’ll leave you to it enjoy the magazine, see you online, and yes, I want your input. If you’re a provider or business partner with a story, a relationship, or an innovation worth highlightingwe’re all ears



Happy Valentine’s XOXO
Jena Eggert Editor-in-Chief, RCM Connections
Philip Boyce- SVP & Chief Revenue Officer
How Healthcare Leaders Should Be Thinking About AI
Everything Philip’s team has to say
Keith Eggert & Philip Boyce ask each other their ‘burning’ questions
Everything you need to know


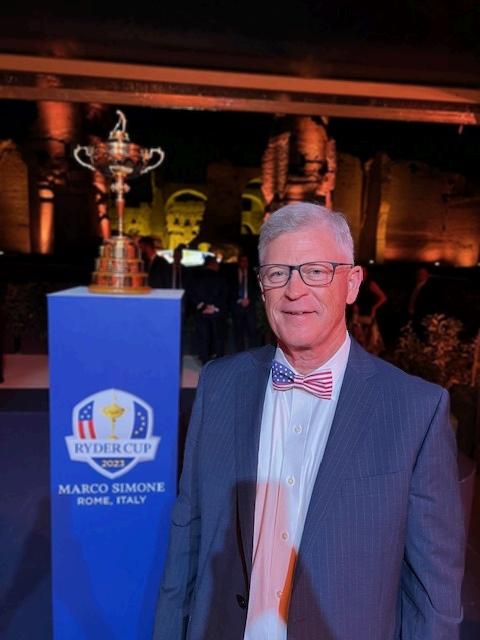
Jena: Hello, my friend Thank you for joining us for another episode of RCM Connections Magazine. We're thrilled to have you, Philip Boyce. Please give me your official title.
Philip: Well, thank you, Jena I'm honored to have this opportunity I wore one of your hats, and I’m happy to rep your enterprise today. So, Philip Boyce, Senior Vice President and Chief Revenue Officer for Baptist Health, serving the greater Jacksonville area and Northeast Florida I lead the Revenue Cycle for our hospitals and physician groups with managed care (now called payer strategy) also reporting to me.
Jena: So, let's talk about your why how did you get into the position you're at, and why revenue cycle? Or maybe it wasn’t revenue cycle initially, since I know you've been in this position for seven-plus years. Can you share how you got where you are, the people who helped you, and your story?
Philip: Well, I’ve been at Baptist for almost 30 years; 30 years in August. I started in as VP of managed care and I did that for the first 22 years (I was promoted to Senior VP during that time) I also was given Utilization Review after a few years. I really enjoyed those areas.


Prior to Baptist, I had worked at Florida Blue as Director of Network Development contracting with hospitals I went to the other side of the table when I came to Baptist After many years, I started voicing concerns about denials we were experiencing.
We’d negotiate contract rates and language, and then see money leaking out the back door due to denials and takebacks. I tried to get involved but back then, the revenue cycle and managed care didn’t work that closely together I expressed my frustration to the CFO about things that I saw
KayakingwithCharles

One day, a little over 7 years ago, as I was walking past his office, he called me in and showed me the new org chart he created for a reorganization. To my surprise, it had me over the revenue cycle VP, not as a peer He put the revenue cycle under me and asked if I’d take it He offered no additional pay, just the challenge.
I thought, "Well, I’ve been complaining about it, so I can’t now say no" Plus, I was ready for a new challenge I decided to myself that I’d give it a year and then reassess. I went from managing a team of six in managed care, and some nurses in Utilization Review, to overseeing a staff of about a thousand in dozens of departments
It was a steep learning curve I understood the basics like accurate registration is important, and getting a bill out prior to the timely filing limit, but coding, CDI, cash posting, etc, was new. It took two years to get my arms around things, all the while still over managed care
I attended as many revenue cycle conferences as I could, and a main focus was to integrate managed care and revenue cycle to further reduce denials and improve revenue capture Integrating managed care with the revenue cycle was the only topic I could speak about at conferences since revenue cycle was so new to me. Over time, I met incredible mentors and gained a better understanding of our departments and leaders.
Two and a half years in, COVID hit, and we had to transition to remote work. We then shut down elective services for five months, and when they resumed, not everyone wanted to reschedule. Just as we adjusted to this new dynamic of remote work, our system decided to migrate to Epic.
Jena: Epic went live about two years ago, correct?
Philip: Yes, a little over two years ago. We prepared for about a year and a half for Epic, and when we went live, it was chaotic, as you’d expect For the first year after implementation, my hair was on fire. But after two years in, around October 2024, for the first time, I felt like I could take a deep breath and say, "Okay, we’re doing okay"
Jena: You have a great team. Did you inherit most of them, or have you built the team along the way?
Philip: It’s been an evolution Some people didn’t take to me being over revenue cycle since I’d been over managed care. I can understand that perspective "Why put the managed care guy over revenue cycle?" Over time, there’s been transition and growth Some leaders stepped up and excelled, others retired, and some moved on. We’ve also brought in new leaders who’ve been outstanding, and we’ve also raised up young leaders who have blossomed. I was assisted by a longstanding consultant at Baptist, Kim Sevening, without which, we wouldn’t be where we are. The team we have is fantastic, and I’m so proud of them.
Jena: Speaking of your team, you have a large one. Can you share how it’s structured and what departments you oversee?
Philip: Sure. We have 52 departments with about 1,250 people and an annual budget of $108 million. That includes managed care, which we’ve integrated with the revenue cycle I oversee areas like PAS, HIM, CDI, hospital and physician coding, billing, SBO, education, quality, and employee engagement. I have nine direct reports who manage various functions, including vendor management, system access, education and QA, analytics, etc. . It’s a lot, but the team is amazing.
Jena: Are most of your team members remote, hybrid, or in-person?
Philip: We’re about 70% remote. Most employees are within 50 miles of Jacksonville, so we’ve worked hard to maintain in-person connections through events We hold monthly mingles, quarterly meet-and-greets for new hires, a wonderful Fall Festival, and departmental meetings. Jacksonville is geographically large, so we host events in different areas to make them accessible. I think we’ve found a good balance between remote and in-person engagement
Jena: Baptist is deeply rooted in Jacksonville. Can you talk about its community involvement?
Philip: Baptist has been here for nearly 70 years and is the only locally governed health system in the region.
We have the only children’s hospital and a comprehensive behavioral health program Even in areas that aren’t profitable, like psychiatry, we’re committed to providing needed services because the community needs them. We’re heavily involved in charity work and partner with other organizations to support our community
Jena: Anything else you’d like to share about your story, your team, or the industry?
Philip: I want to highlight how incredible the revenue cycle leaders are across our country. They face complex challenges and often aren’t fully understood within their organizations.
Yet, there’s a camaraderie in this field that’s remarkable. I’ve benefited immensely from peers who were willing to share their knowledge and support me as I transitioned into revenue cycle. I also appreciate the organizations that bring revenue cycle leaders together for support. It’s been a privilege to be part of this community. Finally, any success I’ve experienced in my career has been due to the prayers of my parents, my wife and my in-laws
Jena: Well, you’re one of those incredible leaders, Philip. Thank you for taking the time to share your story.
Philip: Thank you, Jena I really appreciate the opportunity
there’s a camaraderie in this field that’s remarkable. I’ve benefited immensely from peers who were willing to share their knowledge and support me as I transitioned into revenue cycle

Throughout my life, I have encountered numerous variations of my name, which has led me to develop a lighthearted perspective on its pronunciation. Philip is one of the few individuals who has taken the time to ask how to pronounce it correctly. This considerate approach has left a lasting impression on me during our years of collaboration. Philip demonstrates a genuine care for others and is sincerely interested in building meaningful connections.
-Michiko Bird
It’s such a blessing to work where people are valued. Philip genuinely cares about his team members, no matter how many levels of leadership are between him and the member. I love that he recognizes the efforts and talents of team members and shows an interest in what affects them.
-Melissa Caperton
Philip is a thoughtful, even keel, and fearless leader who seems to be able to multitask better than any of us and always has time to give you his undivided attention. He shows us how to work hard and have fun while we are doing it!
-Stefani Duran
I have tremendous respect for Philip's leadership style. It promotes teamwork, collaboration across the organization and challenges us to find solutions that are more efficient and effective than current processes. Philip leads with a clear vision that aligns with the core values of Baptist Health. He has had a tremendous impact on the revenue cycle having transformed it from working in silos into an integrated revenue cycle team that is highly functional and engaged. I am honored to be working side by side with him.
Heartfelt thanks to Philips leadership style and approach. He empowers us to think critically, approach challenges with confidence, and always prioritize innovation in problem-solving.
Philip Boyce is a rare leader; the wisdom to know his limits, the humility to ask questions, and the courage to act on his convictions
A true leader, like Philip, stands strong in support of his team, yet leads with a heart of wisdom, compassion, and unwavering family values.
What I appreciate most about Philip is his unwavering support of our leaders and teams, commitment to our Baptist core values and keeping the patient/customer at the center. His leadership inspires us innovate, disrupt the status quo and constantly optimize our workflows, systems, and processes. Philip assembles great teams and fosters collaboration and relationship building. He is an amazing leader!
Dear Philip,
I want to express my sincere gratitude for your outstanding leadership. Your vision, dedication, and unwavering commitment to excellence inspire not only me but everyone around you. You’ve created an environment where growth, collaboration, and creativity thrive, and your support has made a profound impact on my personal and professional journey.
Thank you for always leading with integrity, for your constant encouragement, and for being a true example of what it means to lead with purpose and heart. I’m incredibly grateful for your guidance and look forward to continuing to learn and grow under your leadership.
-Michele Bear
Philip, thank you for your leadership and extraordinary support. We would not be the team we are without you!
-Greda Mandi
My education of the Revenue Cycle has been extensive under Philip. He has always given me the freedom to grow and learn new things. His leadership style encourages collaboration and accountability, helping us all to succeed.
-Catherine Frey

A good leader is a mentor who leads with compassion, and integrity, inspiring their team to achieve greatness
-Lata Mitchell
-Judy Mitzlaff



Philip on the racing experience his leaders gifted him

Connecting you to YOUR future
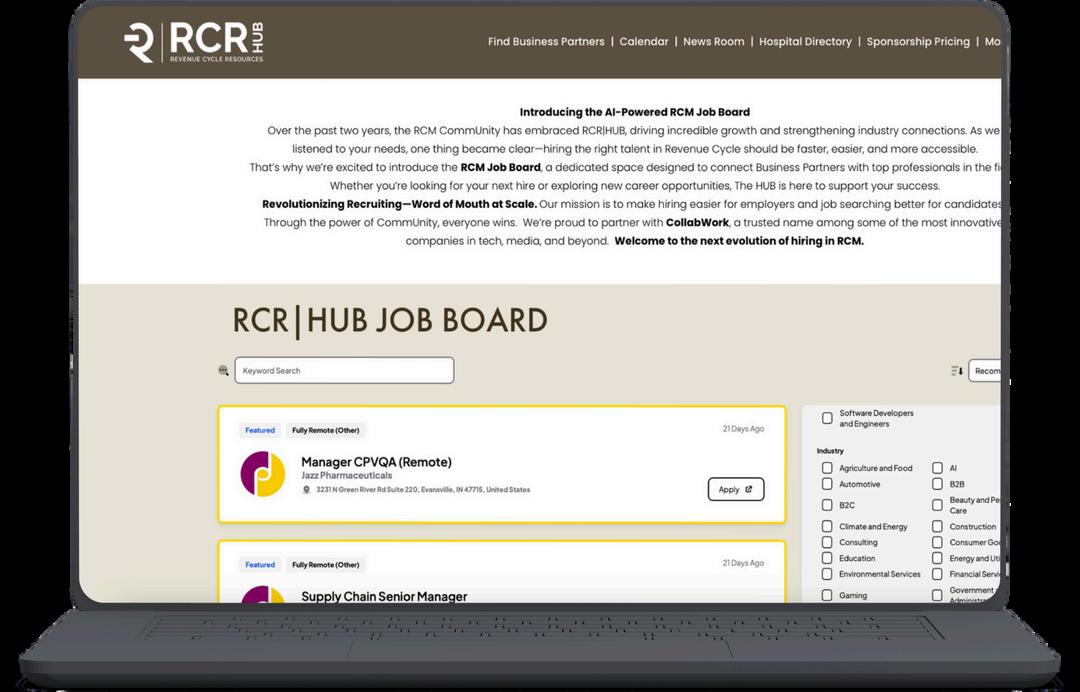
A JOB BOARD CREATED SPECIFICALLY FOR RCM

CHECK IT OUT


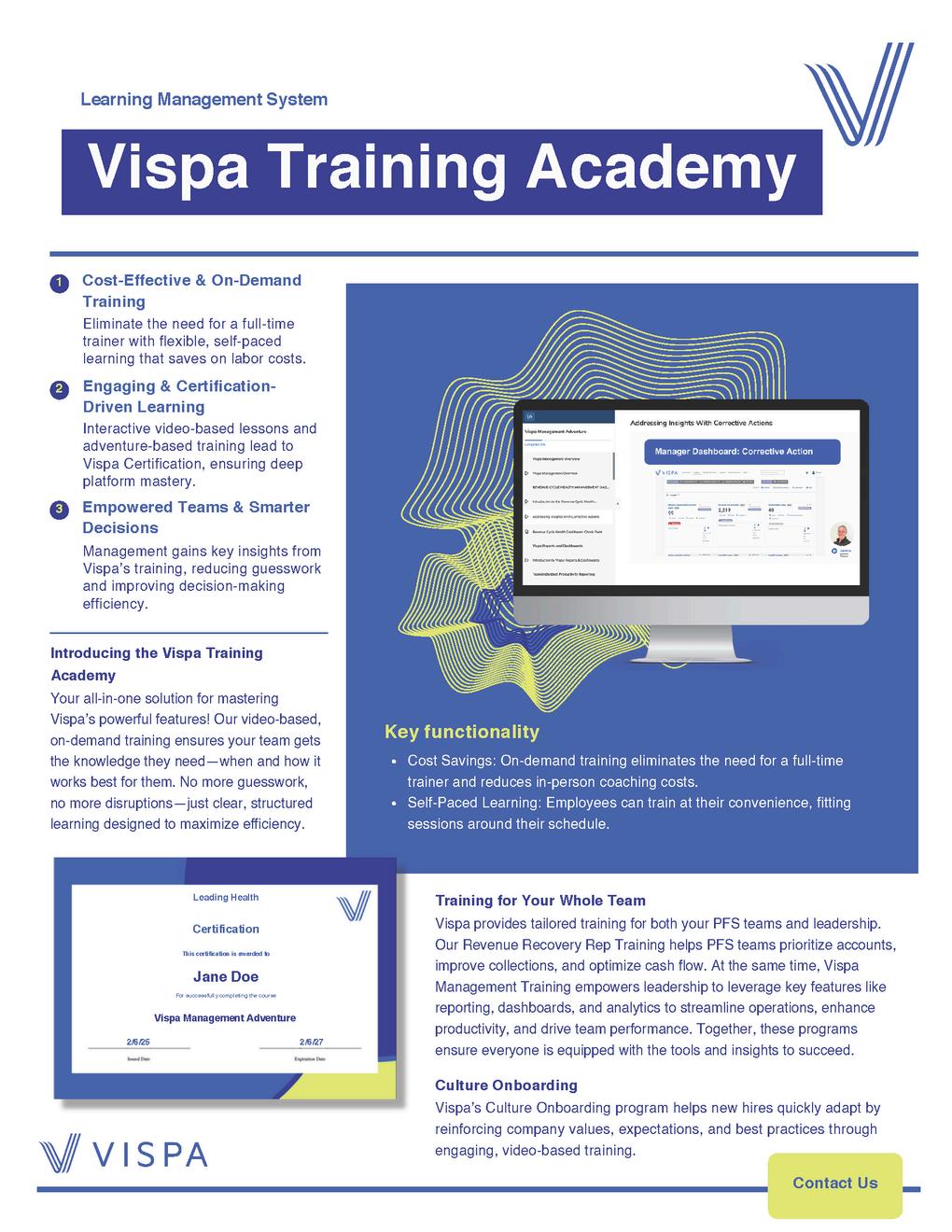
We take the frustration out of payor portals. No more manual logins, endless clicking, or portal fatigue. Just seamless, automated access that saves time, boosts efficiency, and makes your team’s job a whole lot easier.
Because loving payor portals? It’s possible—with the right technology.
Let’s make your team believers.



By: Devon Mobley Chief Growth Officer at Calvient


As a leader in healthcare, it's easy to feel pressure to keep up with the times. Technology advances very quickly, and this feels doubly true in the age of AI
Whether you're ready or not, you feel thrust into a position to think about Artificial Intelligence. Maybe you hoped this day would come after you retire, or perhaps you thought this was initially just another hype cycle that would fade away quickly. It's scary and could do real damage to our industry.
But what I'd like to present to you here is a more optimistic or at least pragmatic picture.
One that helps you realize that the issues that have made healthcare technology as much of a burden to care (as a blessing) are much easier to solve with AI. And also perhaps to help you peer inside the black box that is AI and Large Language Models (LLMs)
The reality is, that healthcare is an overly burdened industry. So I propose strategies that would help us relieve burdens on personnel, rather than replace them In other words, let's find the right way to align this seemingly unstoppable wave of technology with everyone from the front-line staff up to the boardrooms of healthcare.


You can take a second to appreciate the trends we've seen even in just the past 25 years. From the advent of the EHR, cloud, mobile, social, VR/AR, blockchain, and now AI. Some of these have had more impact than others There are iPhone moments and there are Oculus moments They both have an impact, but the iPhone revolutionized so much about technology in a way that VR/AR never could.
Turns out, we're in an iPhone moment
The way our primary tools of productivity and business which is to say oursoftware tools/systems are fundamentally changing before our very eyes. Like when desktop apps went mobile. Having witnessed the evolution from EHRs to cloud computing, data analytics, mobile technology, and now AI, I can confidently say that AI represents a fundamental change in how we use technology.
Sure healthcare will take some time to catch up. But I think this time it will happen more quickly than we realize. It's important to know and understand your options now, so that when strategy can meet execution, you are prepared
So first let me start with why AI can be great and then discuss how to think about using it practically in your work.
The reason healthcare information systems are so tedious and difficult to use (read: THEY SUCK!) is because of the following two reasons:
Healthcare information is largely "unstructured" (document-based), which is notoriously hard for computers to work with We've tried to make it work for over two decades, however, with marginal success.Square peg, round hole problem. Healthcare has extremely high administrative demands due to insurance This requires secure communication, sharing of aforementioned documents (lots of them), and coordination of multiple parties.
The implication is that most tasks feel like it's easier to do manually on paper, rather than in a computer system. The biggest beneficiaries are admins, who can now aggregate the data, etc.
This is because computer software likes working with bits of data, things like numbers. This is partially why EHRs and existing technology feel like something's missing. There's tons of unspoken rules, inferential information, and context that we convey to one another through language and visuals This context likely makes up over half of the data within healthcare. And computers can't act on it.


AI models such as ChatGPT and Claude however love language (text) and visuals (images). Since we also have a lot ofgreat techniques nowadays for turning documents into text or images (most systems can do this reasonably well) and since AI models now have basic reasoning capabilities, you have a more robust tool for accomplishing healthcare-related tasks than we've ever seen.
Ok, I see the point, but how?
I think one of the ways that AI researchers went wrong is that they were itching to take on clinical tasks. Things that doctor's brains do well (for example) like thinking through diagnoses, working with patients for treatment, etc
To be sure there are many tedious workflows providers, like creating notes that have a high success rate on claims. It's a part of the business
But there is so much other work in healthcare that can be made more efficient through AI, such that we free up those moments providers get with their patients. And by starting elsewhere and gaining the trust of clinical and nonclinical staff alike, AI has a bigger chance for success as a transformational tool.
So let me give you what I see as the prime ways to identify where AI can help.
The rules e.g. creating a proper prior authorization or how various outpatient teams handle outbound referrals/transitions of care are unique to every healthcare organization They have their preferences, community relationships, and rapport with payors. What this means is that certain staff have to learn the rules over time. These staff are invaluable. If you spend any time in healthcare you know these people and they are rock stars
However, this puts a major bottleneck on growth, for the organization or even the individual. The buck in many waysstops with this person, so a well-deserved promotion would mean taking them out of doing the work it seems only they can do with 90+% success.


Knowledge Base Creation: AI is good at creating knowledge bases that make it easier to extract what you need. Just drop in documents, and images, or even talk it out to a microphone Google on Steroids: Tools like Perplexity are "answer machines" not unlike Google (but way better). As such, these models can be "primed" with the complex rules specific to your organization The kicker is they are mucheasier to retrieve useful information from. All you have to do is ask a few questions in natural language, instead of searching and clicking around a bunch of documents
Leveraging Expert Knowledge: Putting your best staff's brains into these knowledge bases is like having an extra senior employee assisting with training a host of new team members The value of retaining a central, language-driven knowledge base can help alleviate staff turnover and efficiency issues in a major way.
Tasks such as prior authorizations, referrals, and medication refills have to be coordinated between payors, providers (referring and internal), and patients.
A lot of time these communications are sitting in an inbox somewhere, waiting for a response or to be processed by eligibility, billing, or a clinician
However, it's also really hard to create "ifthis-then-that" rules in an EHR or inbox (if you even have that capability) A lot of it has to be reviewed with a decently keen eye for patient safety reasons Otherwise, you could be filling a now contraindicated medication or failing to get a payor more records (delaying care).
Agent Functionality: When prompted correctly, AI models can act as "agents" who have one, singular job They can read documents or messages and provide a context-sensitive summary/action plan with little effort.
Rapid Summarization: AI is good at ingesting, contextualizing, and summarizing large volumes of data
Muchbetter than humans Even simple tools like a suggested next action can go a long way in speeding workflows up.
Workflow Acceleration: Most of these applications of AI agents act as "workflow accelerants" - so where automation is hard or impossible, they can at least help the humans working (and reduce errors in the process).


Many healthcare organizations still monitor their revenue cycle through periodic reports and manual reviewsoften waiting until end-of-month summaries or deep-dive analyses to understand issues like claim denials or revenue leakage. This reactive approach means that by the time problems are detected, they may have already compounded, leaving teams scrambling to resolve them.
This is compounded by the unstructured data problem. There are tons of documents, faxes, claims, and even internal conversations that could help unlock operational insights that are difficult to incorporate into any data project (which are already notoriously risky).


Real-Time Monitoring: AI systems continuously monitor both structured and unstructured data, flagging anomalies as soon as they occur and enabling teams to address issues before they escalate.
Unlocking Hidden Insights from Unstructured Data: AI-powered language processing transforms messy, low-ROI unstructured data into actionable insights by revealing hidden patterns and extremely specific insights for your organization
Proactive Interventions: An AI model might not always provide perfect answers, but it can contextualize your data to suggest reasonable action steps. This helps kickstart team responses and frees up valuable time for forward-looking initiatives an outcome every organization desires and finds much more achievable with AI.
I understand that we've worried about AI completely taking over tasks in healthcare.
Technologycompanies/commentators have done a poor job of being on friendly terms with real healthcare on the ground, such that staff and leaders can trust it
But most folks are feeling that they can no longer resist this trend. I think that's right, but I hope that I've given you some mental models of how AI can be used in areas where it excels, as well as helping staff rather than scaring them.
I have hopes that we can adjust course and get healthcare on board in the right ways that help patients Sure there are much deeper problems in our industry, but I think the first step is learning how to survive in a sustainable way.
And fortunately, that path is more clear now than it has been for a long time
Hi, I'm Devon Mobley. I'm the Chief Growth Officer at Calvient, a Practical AI platform for healthcare
I have worked in specialty care designing and building workflows with software as well as in Big Tech as a senior engineer. My mission is to serve the real people doing the real work in healthcare. For me, innovation happens at the margins in healthcare, so I aim to bring people together to push the boundaries: slowly, practically, but progressively
If you would ever like to chat about AI, strategy, or healthcare technology/operations, I am an open book!