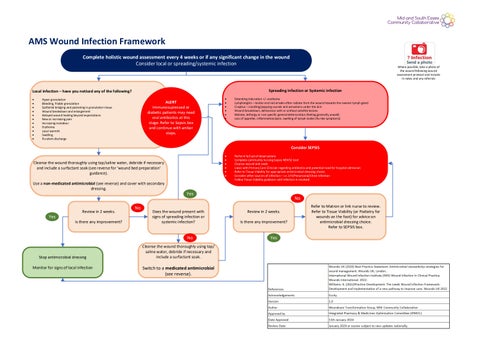
AMS Wound Infection Framework
Complete holistic wound assessment every 4 weeks or if any significant change in the wound
Consider local or spreading/systemic infection
Local infection – have you noticed any of the following?
• Hyper granulation
• Bleeding, friable granulation
• Epithelial bridging and pocketing in granulation tissue
• Wound breakdown and enlargement
• Delayed wound healing beyond expectations
• New or increasing pain
• Increasing malodour
• Erythema
• Local warmth
• Swelling
• Purulent discharge
ALERT
Immunosupressed or diabetic patients may need oral antibiotics at this stage. Refer to Sepsis box and continue with amber steps.
Cleanse the wound thoroughly using tap/saline water, debride if necessary and include a surfactant soak (see reverse for ‘wound bed preparation’ guidance).
Use a non-medicated antimicrobial (see reverse) and cover with secondary dressing.
Review in 2 weeks.
Is there any improvement?
Stop antimicrobial dressing
Monitor for signs of local infection


Where possible, take a photo of the wound following wound assessment protocol and include in notes and any referrals
Spreading infection or Systemic infection
• Extending induration +/- erythema
• Lymphangitis – tender and red streaks often radiate from the wound towards the nearest lymph gland
• Crepitus – crackling/popping sounds and sensations under the skin
• Wound breakdown, dehiscence with or without satellite lesions
• Malaise, lethargy or non specific general deterioration (feeling generally unwell)
• Loss of appetite, inflammation/pain, swelling of lymph nodes (flu -like symptoms)
Consider SEPSIS
• Perform full set of observations
• Complete community nursing Sepsis NEWS2 tool
• Cleanse wound and swab
• Liaise with Primary Care Clinician regarding antibiotics and potential need for hospital admission
• Refer to Tissue Viability for appropriate antimicrobial dressing choice
• Consider other sources of infection – i.e. UTI/Pneumonia/Chest Infection
• Follow Tissue Viability guidance until infection is resolved
Does the wound present with signs of spreading infection or systemic infection?
Cleanse the wound thoroughly using tap/ saline water, debride if necessary and include a surfactant soak.
Switch to a medicated antimicrobial (see reverse).
Review in 2 weeks.
Is there any improvement?
Refer to Matron or link nurse to review.
Refer to Tissue Viability (or Podiatry for wounds on the foot) for advice on antimicrobial dressing choice. Refer to SEPSIS box.

Wound Bed Preparation
Cleansing: Use tap water, saline or Octenilin®
Debridement: Remove slough and debris using either autolytic or mechanical debridement methods (eg. Debridement pads/cloth)
If infected, include a surfactant soak : Octenilin ® soak for 5 -15 mins
Sharp debridement: Refer as per local policy
Suspected Biofilm in the Chronic Wound
It is widely accepted that biofilm is present in 70–100% of chronic wounds Malone et al (2017)
Signs & Symptoms:
• Absence of healing progression, even though all obvious comorbidities and wound management issues have been addressed
• Failure of antibiotic / antimicrobial treatment
• Quick re -forming of slough, despite debridement
• Increase in exudate
• Poor quality granulation tissue possibly fragile and / or hypergranulation
• Signs of local infection (as Biofilm is a precursor to infection) e.g. heat, redness, swelling, pain, odour
Treatment:
• Thorough cleansing/debridement at dressing change (Debridement pad/cloth)
• Use of Octenilin ® to disrupt biofilm
• Use an appropriate antimicrobial to create an environment that prevents or delays biofilm reformation
Non-Medicated Antimicrobials to be used on local infections as part of Antimicrobial Stewardship Strategy:
Cutimed® Sorbact®
Flaminal® Hydro/Forte (consider cost and frequency of change, and may need Specialist advice)
Medicated Antimicrobials to be used for spreading or systemic infections or for local infection with clinical rationale:
Iodoflex Honey
Octenilin ® Gel
Silver dressings
Suspected Cellulitis
Signs & Symptoms: pain, redness (consider skin tone), hot skin, swelling/oedema.
Treatment: appropriate antibiotics, urgent referral if signs of systemic infection or sepsis are also present
Signs of Sepsis: Red flags
Sepsis is a life-threatening condition in which the body’s response to infection causes injury to its tissues and organs. Organ dysfunction is a key component in any diagnosis of sepsis (The UK Sepsis Trust).
Act on a Red Flag assessment
S = Slurred speech or confusion
E = Extreme shivering or muscle pain
P = Passing no urine (in a day)
S = Severe breathlessness
I = It feels like you’re going to die
S = Skin mottled or discoloured
Diabetic Foot Ulcers
Patients who have a diabetic foot ulcer and present with 2 or more signs of local infection (see reverse) should be seen by the Podiatry Services (e.g. Community Podiatry Services, Basildon DFC and MDFT at SGH) within 24 hours.
Antimicrobial Stewardship
Use non-medicated options (e.g. non-medicated dressings) to manage infection when possible, reserving broad-spectrum agents (e.g. medicated dressings) for more resistant bacterial infections, and therapy should continue for an ‘appropriate’ duration, guided by appropriate and timely monitoring of therapeutic response.
Skin Tone
Skin inspection with an awareness of skin tone should be carried out as part of a full holistic assessment that includes the patient’s skin, their overall health and medical history, and their wound, ensuring that care is tailored to the individual and their needs.
How to Identify Wounds at Risk of Infection
Patient Risk Factors:
• Previous MRSA colonisation
• Poorly controlled diabetes (i.e. hyperglycaemia)
• Peripheral neuropathy (sensory, motor and autonomic)
• Neuroarthropathy
• Radiation therapy or chemotherapy
• Conditions associated with hypoxia and/or poor tissue perfusion (e.g. anaemia, cardiac disease, respiratory disease, peripheral arterial disease, renal impairment or rheumatoid arthritis)
• Immune system disorders (e.g. acquired immune deficiency syndrome)
• Connective tissue disorders (e.g. Ehlers-Danlos syndrome)
• Corticosteroid use
• Malnutrition or obesity
• Alcohol, smoking or illicit drug use
• Poor compliance with treatment plan
Wound Risk Factors:
• Contaminated or dirty wounds
• Traumatic injuries
• Operation is classified as contaminated or dirty
• Inappropriate hair removal
• Operative factors (e.g. prolonged surgery, blood transfusion or hypothermia)
• Duration of wound
• Large wounds
• Anatomically located near a site of potential contamination (e.g. perineum or sacrum)
• Foreign body presence (e.g. drains, sutures or wound dressing fragments)
• Haematoma
• Necrotic or sloughy wound tissue
• Impaired tissue perfusion
• Increased exudate and oedema that is not adequately managed
• Wounds over bony prominences or probing to bone
• Involvement of tissue deeper than skin and subcutaneous tissues (e.g. tendon, muscle, joint or bone)
When to Swab a Wound
• Patients with a known MRSA colonisation must have a full MRSA screen including the wound.
• Patients with a diabetic foot wound with signs of infection must have a swab taken.
• Acute or chronic wounds with signs of spreading or systemic infection
• Infected wounds that have failed to respond to antimicrobial intervention, or are deteriorating despite appropriate antimicrobial treatment
• In compliance with local protocols for the surveillance of drug-resistant microbial species
• Wounds where the presence of certain species would negate a surgical procedure (e.g. beta haemolytic streptococci in wounds prior to skin grafting)