Adult Hydration and Nutrition Policy
Version: V7
Ratified by:

Quality Reference Group
Date ratified: 25/11/2025
Job Title of author:
Reviewed by Committee or Expert Group
Equality Impact Assessed by:
Related procedural documents
Review date:
Operational Lead
Mid & South Essex Community Adult Speech and Language Therapy Services
Quality Reference Group
Operational Lead
Mid & South Essex Community Adult Speech and Language Therapy Services
CPOL69 – Food Safety Policy
SGPOL10 – Mental Capacity Act Policy
QSPOL06 – Privacy, dignity and respect policy
EOL Care Policy
25/11/2028


It is the responsibility of users to ensure that you are using the most up to date document template – i e obtained via the intranet
In developing/reviewing this policy Provide Community has had regard to the principles of the NHS Constitution.
Version Control Sheet
Version Date
V1 November 2016

Author Status Comment
LorraineHollis
JohnBentley
AlisonCook
LibbyMarsden New
V6 September 2018 Assistant Director, Community Hospitals, Minor Surgery and Outpatient Services
Clinical Manager, Adult Speech and Language Therapy Ratified
V7 November 2025 Operational Lead Mid & South Essex Community Adult Speech and Language Therapy Services updated


1. Introduction
Provision of the right nutrition and hydration is a human right and a fundamental requirement in the delivery of health care.
It is estimated that malnutrition (undernutrition) affects over 3 million people in the UK.
In the secondary care setting disease related malnutrition results in increased complications (e.g. wound infections, chest infections, pressure ulcers), increased length of stay, increased mortality, and an increase in patients requiring readmission.
It is essential to screen patients for malnutrition or risk of malnutrition on admission to hospital to identify people who would benefit from active nutrition or hydration support. It is the responsibility of all healthcare professionals to ensure that nutritional care is an integral part of their practice.
Up to 30% of patients admitted to hospital are at risk of malnutrition. Poor nutrition increases morbidity and mortality, prolongs length of hospital stay and increases healthcare costs. Patients who are malnourished are more likely to be discharged to health care destinations other than their own home.
Providing good nutritional care improves outcomes and patient experience. It is essential that all patients are able to access food and fluids appropriate to their individual needs to support their therapeutic care. Individuals who are malnourished or at risk of malnutrition should be identified and treated.
2. Purpose
This policy has been developed by a multidisciplinary group of professionals to establish best practice with regard to the nutritional support of adult patients. This policy aims to help healthcare professionals working within Provide to correctly identify people who need nutrition support and enable them to deliver timely and appropriate interventions to ensure cost effective use of resources.
This policy has been devised to achieve and maintain high quality nutritional care for all. This policy contains information and practical instruction on equipment, management and monitoring in regard to nutrition.
The purpose of this document is to:
• Set out procedures for assessing and screening for malnutrition
• Detail management plans for those patients that are identified as malnourished or at risk of malnutrition.
3. Definitions
Malnutrition: A state of nutrition in which a deficiency or excess (or imbalance) of energy, protein and/or other nutrients causes measurable adverse effects on tissue/body form (body shape, size and composition), function or clinical outcome.
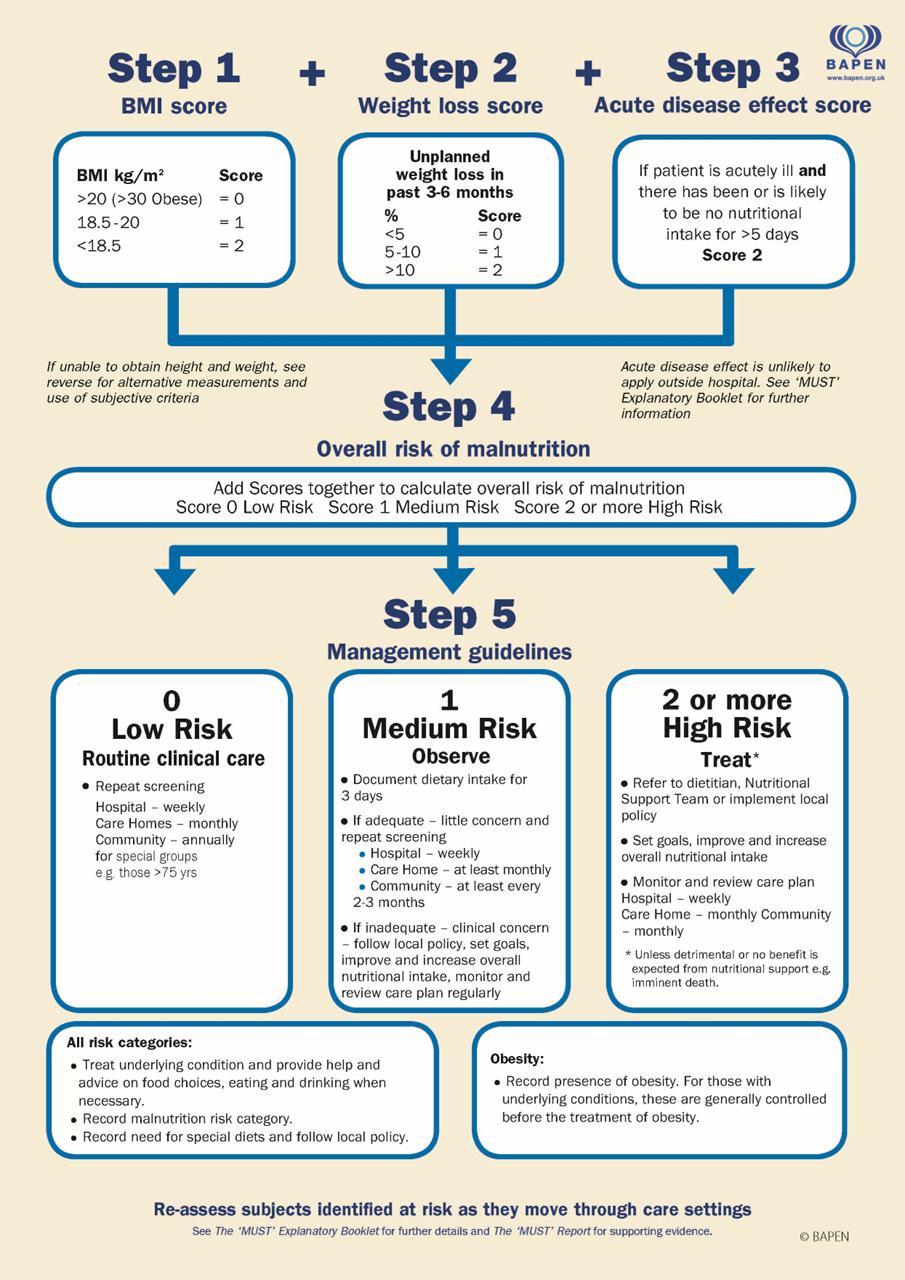
Malnutrition Universal Screening Tool (MUST): A five-step screening tool used to identify adults who are malnourished or at risk of malnutrition
Dysphagia: Medical term for eating, drinking and swallowing difficulties

Nutrition Support: The provision of nutrients and any additional therapeutic agents for patients orally, enterally or via the parenteral route
Oral Nutrition Supplements (ONS): A product for oral administration given with the aim of improving or maintaining a patient’s nutritional status.
Enteral Nutrition: For the purposes of this policy, enteral nutrition refers to the delivery of nutrition via a tube into the gastrointestinal tract, given for the purpose of improving or maintaining a patient’s nutritional status.
Parenteral Nutrition: The intravenous administration of nutrients. This may be supplemental to oral or enteral nutrition, or it may be the sole source of nutrition.
Refeeding syndrome: Severe fluid and electrolyte shifts and related metabolic complications in malnourished patients undergoing refeeding.
Protected Mealtimes: A national initiative designed to allow patients to eat their meals without disruption and enable staff to focus on aiding with those patients unable to eat independently. Routine activities such as cleaning or drug rounds are curtailed to create an environment conducive to people enjoying their meals and being able to consume their food and drinks in a safe environment.
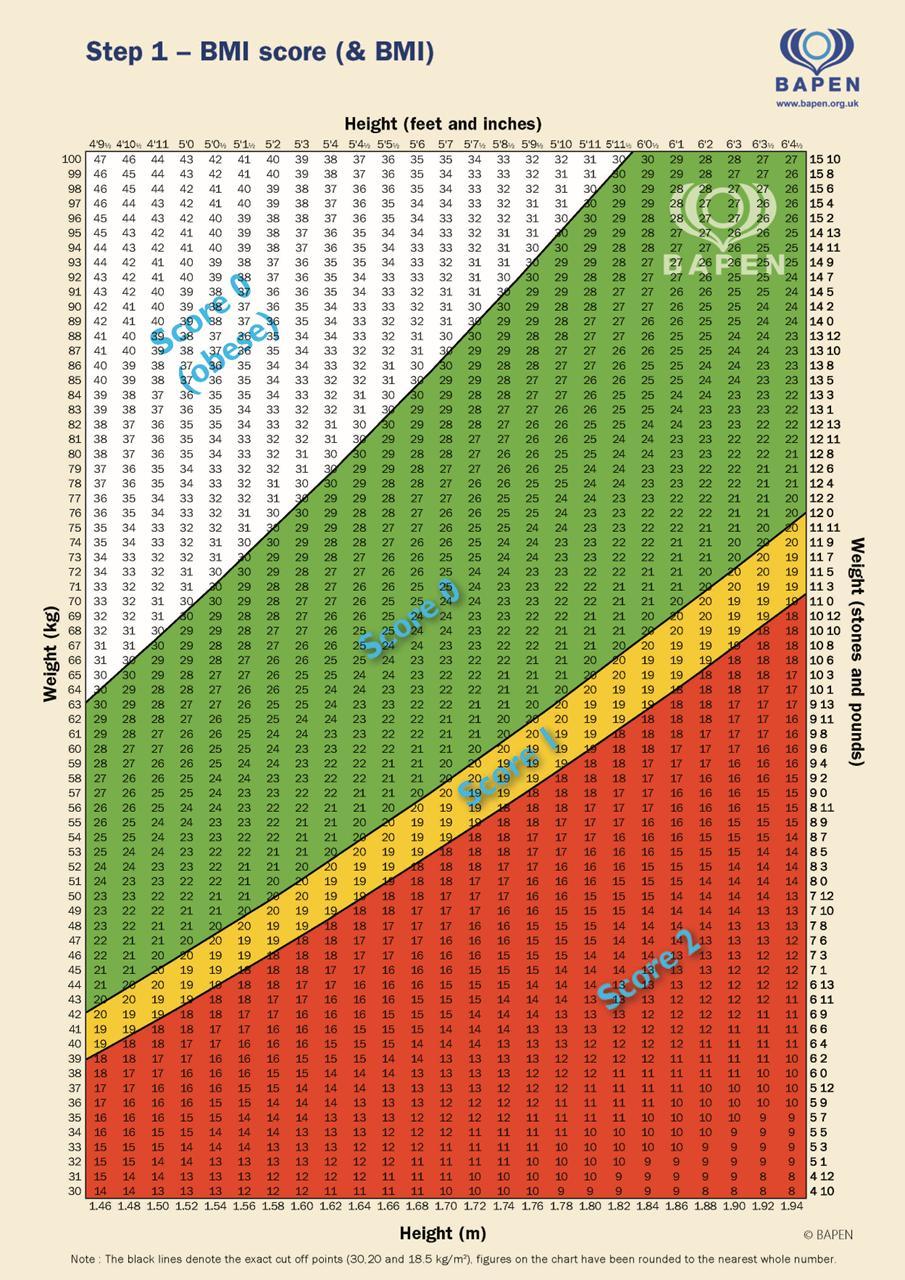
Body Mass Index (BMI): A measure of body weight relative to height (kg/m²) used to determine whether people are underweight, at a healthy weight, overweight or obese.
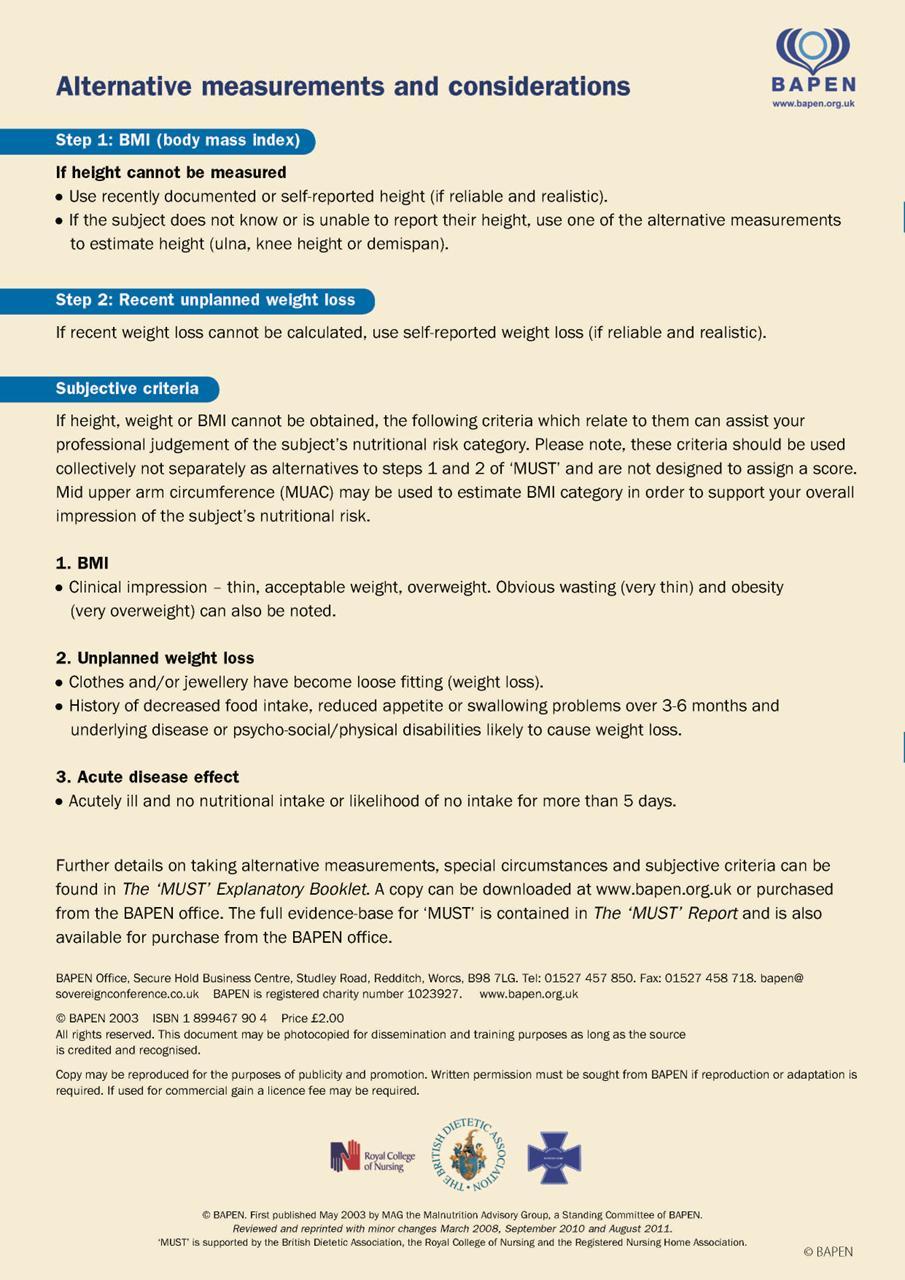
MUAC (Mid Upper Arm Circumference) If a patient is too unwell to be weighed Mid Upper Arm Circumference (MUAC) should be monitored however this should not be used to generate a MUST score
4. Roles and Responsibilities
Chief Executive
The Chief Executive has overall responsibility for ensuring that Provide has the necessary management systems in place to enable the effective implementation of this policy and overall responsibility for the health and safety of staff, patients and visitors.
Executive Clinical and Operations Director
The Executive Clinical and Operations Director has strategic responsibility for ensuring systems are in place to facilitate the clinical staff’s awareness of this policy and appropriate support is given to enable staff in delivering practice as outlined in this policy. All registered nurses must ensure they are competent and confident to deliver any care they provide for a patient (Nursing Midwifery Council 2008).
Responsibilities of hospital staff – Nursing
• Assess patients’ nutritional status using the MUST tool within 12 hours of admission and draw up an appropriate care plan.
• Monitor nutritional status on a regular basis and act on assessment outcomes.
• Refer to appropriate healthcare professionals to support patient’s nutritional needs (Dieticians) and assess dysphagia symptoms and advise on management (SALTs)
• Ensure patients receive appropriate nutrition and that people with dysphagia are given modified fluids and diets in line with SALT recommendations defined

in accordance with International Dysphagia Diet Standardisation Initiative (IDDSI) descriptors.
• Ensure the Protected Mealtimes Policy is adhered to at all times to minimise interruption to meals and encourage patient intake.
• Ensure use of Blue Tray system (and blue water jug lids) to help highlight people with assistive needs
• Ensure all patients receive the appropriate assistance or supervision to eat and drink
• Ensure Food charts are completed correctly (as required) and reviewed regularly with appropriate action being taken in a timely manner.
• Ensure all in-patients are discharged appropriately with all appropriate referrals to relevant healthcare professionals within the community.
Nutrition Link Nurses
• Nutrition Link Nurses (a representative from each inpatient ward and from the Integrated Care Teams) act as a resource in their clinical area and attend the Nutrition steering group on a quarterly basis. They should promote good nutritional practice in their work area and act as a role model for colleagues.
Lead Nurses and Ward Matrons
• Ensuring that resources are available for health care workers to provide adequate nutrition and hydration to all patients
• Ensuring that patients with complex nutritional requirements have appropriate support from expert staff. E.g. Dieticians, SLT Ensuring that training is provided so that registered and non-registered health care workers are aware of their responsibilities and how to carry these out.
• Ensuring that budgets are set and managed so that the nutritional requirements of all patients can be met whatever feeding route is deemed clinically appropriate, oral or enteral nutrition.
• Ensuring compliance to nutrition related policies (e.g. Protected Patient Mealtimes & Food and drink Policy.
• Ensuring that all clinical staff are aware of this policy and monitor compliance with the standards set out within.
Community Dietetic Team
• On receipt of a referral liaise with the nursing and medical teams.
• Assess and develop an individual nutritional care plan.
• Monitor and review nutritional care plan until patient is discharged.
• Prior to discharge, liaise with appropriate healthcare professionals.
• Prescribe oral and enteral supplements when required
• Post discharge, liaise with GP and community Dietetic teams for ongoing support
Speech and Language Therapists (SLT)
• To ensure that all community and in-patient referrals relating to suspected dysphagia (swallowing disorder) receive timely advice, assessment and the provision of an individual management plan (where appropriate), treatment/rehabilitative therapy (where indicated) and follow-up (as required) to minimise the risks of aspiration whilst seeking to optimise nutrition, hydration and medication intake as per individual requirements.
• To produce clear guidance on the appropriate consistencies for fluids and flood that people with dysphagia require, in line with the International Dysphagia Diet Standardisation Initiative (IDDSI) Levels 0 to 7

• To ensure that guidance is effectively communicated to all team members via care plans, medical notes, bedside instructions and kitchen-based instructions (as appropriate).
• To highlight to the medical/nursing team issues pertaining to dysphagia that might compromise adequate oral intake/medication administration and to advise on the appropriateness of enteral nutrition options.
• To consider people’s capacity to consent to management options and to support the assessment and documentation of consent in relation to nutritional decision making as appropriate.
• To monitor and review people’s status (where change in presentation might be reasonably expected) and to optimise modified consistency guidelines in accordance with any fluctuations in clinical presentation.
• To provide education and support to all clinical and domestic staff with a responsibility to understand the need for good mouth-care practices and the specialist management of dysphagia.
Catering service staff and contracted menu providers
• Develop menus in conjunction with a qualified Dietician to ensure that all clinical nutrition and hydration needs are fully considered
• Develop menus that seek to address the reasonable dietary needs of people with differing clinical, cultural or religious requirements/lifestyles
• To be aware of and provide different dietary and fluid consistencies required by people with dysphagia (swallowing disorder) and to understand the rationale for specialist guidelines (as prescribed by Speech and Language Therapy services)
• To ensure the availability of meals and snacks (as required) 24 hours a day
• Liaise with nursing teams at ward level where there are concerns over a person’s meal intake.
Mealtime volunteers
• Assist patients who require help in selecting their preferred meals, assist in handing out meals during mealtimes, cut food and assist in feeding patients. They should receive training before beginning this role, particularly in respect to swallowing disorder (dietary and fluid consistency modification) and the benefits of supporting self-feeding.
Other healthcare professionals (e.g. Occupational Therapists and Physiotherapists)
• To have an awareness of the holistic management of the patient, including nutrition, and an awareness of the impact their treatment plan and timings may have on this.
• To be aware of the protection of patients’ mealtimes.
• To inform nursing/medical staff of any potential nutritional issue which may not be met.
Pharmacists
• Supplying and advising on supplements, enteral feed and parenteral nutrition.
• Advising on any interactions between nutrients and drugs.
• Dispensing of medicines in suitable form for optimal up-take
• Advising on suitability and timing of administration of medicines for enterally fed patients
Medical staff
• Liaise with the MDT to be aware of the nutritional needs of their patients

• To be aware of the protection of patients’ mealtimes
• To advise the MDT on medical issues that may hinder the delivery of optimal nutritional support
Nutrition Steering Group
A multi-disciplinary professional group comprising experienced representatives from Adult Community Speech and Language Services, Community Dietetic Services and Inpatient Nursing. The group meet biannually in order to continually review, revise and disseminate policy directives - overseeing and advising on all aspects of nutrition pertaining to patients including screening/assessment, catering, oral nutritional supplements, and enteral nutrition. The minutes of each meeting are submitted to the Quality & Safety Committee for review.
5. Assessment and Screening
There is no 'gold standard' indicator that exclusively relates to the assessment of a patient’s nutritional status. A combination of tests needs to be applied, these include taking a dietary history, anthropometric measurements, a physical examination and biochemical analysis.
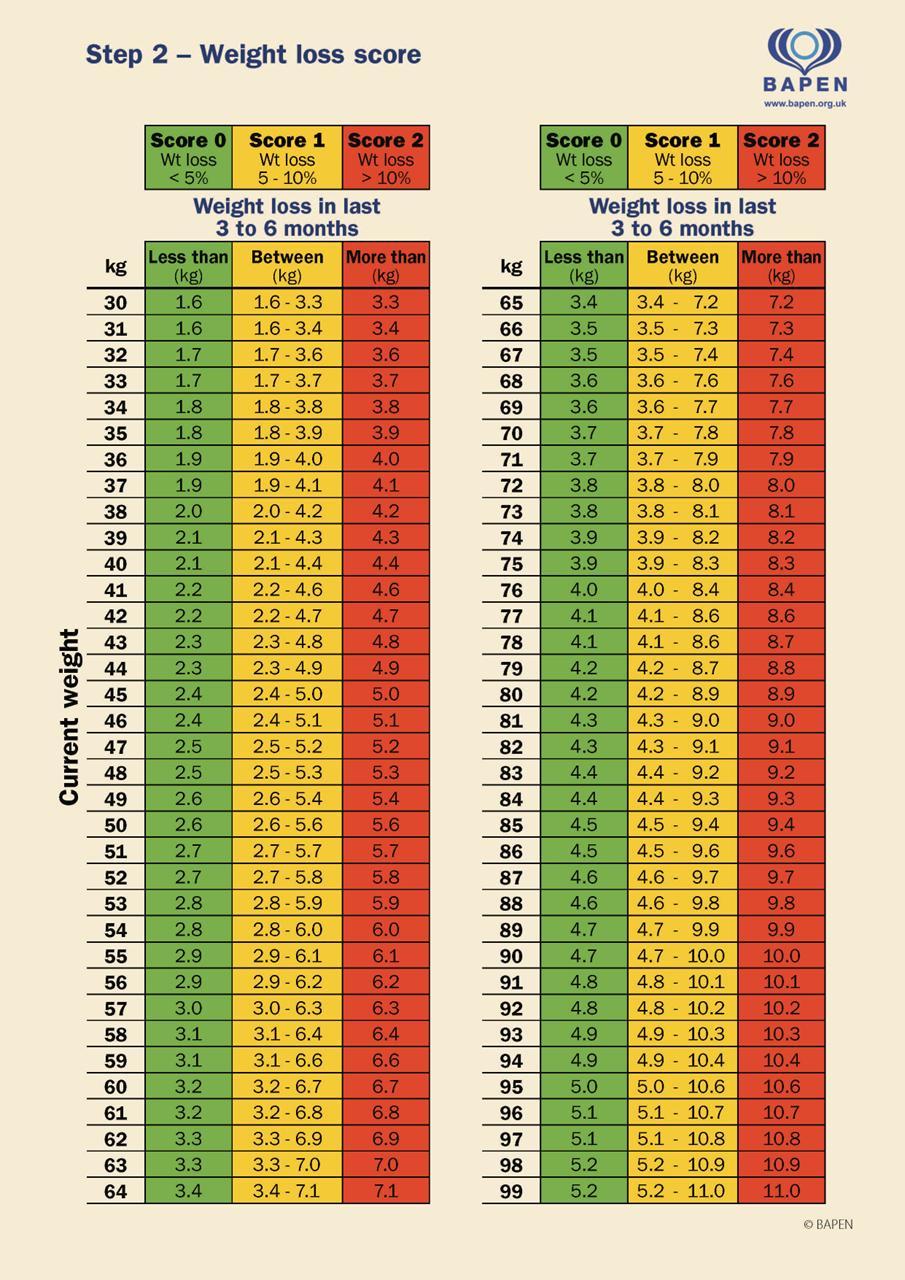
Adult patients requiring an in-patient stay within Provide will have their nutritional status screened on admission to hospital within 6 hours of admission using 'MUST' (Malnutrition Universal Screening Tool, Elia 2003) (Appendix 1).
Each ward will have weighing scales and a device for measuring height or use surrogate measurements to estimate height. It is the Ward Sister / Unit Manager’s responsibility to ensure that these devices are available, serviced and maintained according to the manufacturer instructions.
All patients should be weighed on admission and weekly thereafter, sooner if there is a change in the patient’s condition. Bed weighing scales should be utilised where available and appropriate.
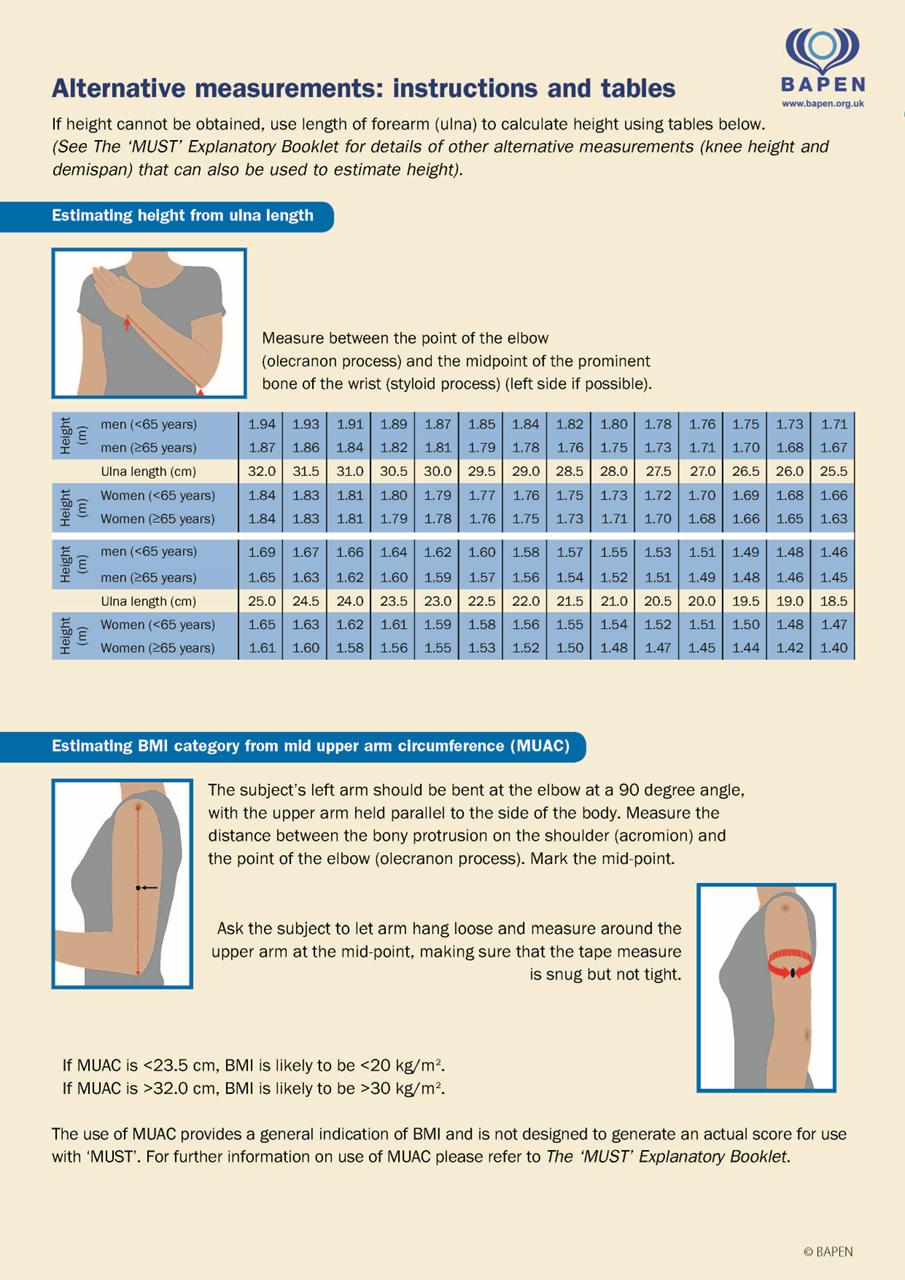
All patients should have their height recorded on admission. An actual height will be most accurate, but if this cannot be obtained a surrogate measure such as ulna length, or reported height may be used, but should clearly be documented as such.
The ‘MUST’ score will be documented into the patients’ healthcare records.
Patients with a learning disability may have additional needs and therefore will need to be assessed by someone with specialist knowledge of nutrition care in this condition, in the presence of their relative or carer who knows them and who can offerappropriate advice.
Patients with dementia may have additional needs and therefore will need to be assessed in the presence of their relative or carer who can offer appropriate advice.
Patient’s receiving assessment and care in the community (i.e. those not admitted to in-patient facilities) should receive a nutritional assessment using MUST as part of their initial nursing visit. Weighing scales are impractical for community working and MUAC should be used to inform nutritional status. Review assessment of nutrition and hydration status should be undertaken as indicated.

6. Referral
In-Patients should be referred to the Community Dietetic Service in the event of:
• A MUST score of 2 or above
• A specific clinical concern with a low MUST score (0-1) for example for a Grade 3 or 4 pressure sore. This referral must include detailed clinical reasoning for the referral.
Department of Nutrition & Dietetics, Mid and South Essex University Hospitals Group, Broomfield Hospital, Court Road, Chelmsford, Essex CM1 7ET Telephone: 0300 44 35844
NB Community based patients with nutritional issues cannot be referred to community dietetics directly. Nutrition concerns should be raised with a patient’s GP in the first instance. It is then the responsibility of the patient’s GP to consider referral to Community dietetics as per individual risk and requirements.
7. Treatment
Patients identified at risk of malnutrition should have an individual care plan instigated as per screening recommendation. This may include the following interventions:
• Food record chart
• Red Tray / red jug
• Ensuring the patient gets assistance to eat and drink
• Identifying patient preferences
• Helping the patient to choose appropriate meals from the menu, including ensuring appropriate consistency of food/fluid is provided to those patients with dysphagia.
• High energy/protein menu options
• Care Plan
• Nutritional supplement drinks
• Referral to the dietitian
• Referral to the Speech and Language Therapy Service (adult or paediatric depending on age)
• Referral to the Nutrition Support Team
8. Training Requirements
There are no formal requirements for staff to complete dysphagia training and SLT led dysphagia training to inpatient ward staff is offered on an ad hoc basis.
The Adult Community Service has produced a set of 4 training packages primarily aimed at supporting people with dysphagia and their families/carers. These educational resources are freely available via the links below or by visiting Speech & Language Therapy - Adult - Provide
Dysphagia – General education - https://vimeo.com/1119789480
Dysphagia and breathing problems – https://vimeo.com/1119786214
Dysphagia and neurological changes - https://vimeo.com/1119786956
Dysphagia and cognitive changes - https://vimeo.com/1119788977

Monitoring and Audit
This policy applies to all staff employed by Provide who have direct and indirect contact with patients in respect to the provision of their nutrition and hydration. It should be applied by all healthcare practitioners to the care of every patient.
The Nutritional Steering Group will continue to review all nutrition related policies.
Staff will ensure that any breaches of this policy are recoded via DATIX, and necessary action is taken as a result. The NSG will develop a plan for audit, monitoring and review of outcomes.
9. Ethical Principles of Nutrition
Key points include:
• The provision of food and water constitutes ‘basic care’ and is mandatory for all patients (BAPEN 2004).
• The administration of nutrition via a feeding tube is a medical intervention and requires consent being documented in the patient records, subject to the mental capacity of the patient
• A patient’s nutritional care plan must focus on their needs and wishes
• Patients should have the opportunity to make informed decisions about their care and treatment in partnership with their healthcare professionals
Carers and relatives should have the opportunity to be involved in decisions about the patient’s care and treatment, if the patient agrees to this. Carers and healthcare professionals involved in starting or stopping nutrition support should:
• Obtain consent from the patient if he or she has capacity
Please refer to PROVIDE CIC Mental Capacity Act Policy SGPOL10: https://provide.metacompliance.com/View/Policy/2232649
• Act in the patient’s best interests if he or she lacks capacity (refer to Mental Capacity Act Policy)
• Be aware that the provision of nutrition support is not always appropriate. Decisions on withholding or withdrawing of nutrition support require a consideration of both ethical and legal principles and staff should always consider taking legal advice
When a patient lacks capacity or when the decision is made not to provide nutritional support, a Mental Capacity Assessment must be completed.
10.Nutrition Screening
There is no 'gold standard' indicator that exclusively relates to the assessment of a patient’s nutritional status. A combination of tests needs to be applied, these include taking a dietary history, anthropometric measurements, a physical examination and biochemical analysis.
Nutritional Screening is the first step in identifying individuals who may be at nutritional risk or potentially at risk, and who may benefit from appropriate nutritional intervention. It is a rapid, simple and general procedure used by nursing, medical, or other staff on

first contact with the subject so that clear guidelines for action can be implemented and appropriate nutritional advice provided.
NICE CG 32 (2006) recommends screening for malnutrition and risk of malnutrition across all healthcare settings.
• Adult patients requiring in-patient stay within Provide will be screened using the Malnutrition Universal Screening Tool (MUST) within 6 hours of admission and weekly thereafter or if there is a change in the patient’s clinical condition which affects their nutritional status. A personalised plan of care should be developed following this assessment (see Appendix 1).
• The MUST assessment tool is included within the nursing documentation booklets used across Provide for adult in-patients. BAPEN explanatory guidance is available in the ward Nutrition folders.
• All staff using the screening tool must be trained in its use.
• MUST Should aid rather than replace clinical judgement. Improving the food intake of malnourished patients is the first step in nutritional intervention. Oral nutritional supplements are only to be used when this has not been successful and after full assessment by a registered dietician.
• Each ward or department will have weighing scales and a device for measuring height or use the alternative measurements to estimate height as recommended by BAPEN. It is the Ward’s responsibility to ensure that these devices are available, serviced and maintained according to the manufacturer instructions.
• All patients should be weighed on admission and weekly thereafter. Where it is impossible to weigh patients, the Registered Nurse must exercise his/her clinical judgement. The use of alternative measures such as mid upper arm circumference for estimating BMI, should only be used by healthcare professionals competent to do so. Estimated BMI should be recorded as such in the healthcare records. Patients with estimated BMI should have an accurate measured weight as soon as clinically possible, if not able to do so, this should be clearly documented in the patients’ notes and, on the MUST, recording chart.
• All patients should have their height recorded on admission. Where it is impossible to measure a patient's height, an alternative measurement, such as the ulna length should be used and recorded as such in the patient’s notes. Patients with capacity are usually able to report their height. There is evidence in research that reported height in patients with capacity is as accurate as a recorded height and is therefore acceptable to use.
• Patients with a learning disability may have additional needs and therefore will need to be assessed in the presence of their relative or carer who knows them and who can offer appropriate advice.
• Patients with dementia may have additional needs and therefore will need to be assessed in the presence of their relative or carer who can offer appropriate advice.
A summary of the patients’ weight, MUST scores and nutritional care plan will be included on the discharge summary if appropriate. To ensure that interventions can be continued on discharge
11.Advice for Improving Nutritional Intake
The first course of action for treating malnutrition is through normal food. Exploring the underlying reasons for a patient’s poor nutritional status, and treating those conditions,

is an effective way of dealing with their malnutrition. Wherever possible, the aims of the nutritional intervention needs to be discussed with the patient and documented in their notes.
Making the mealtime experience as conducive to eating as possible is essential in ensuring the patient’s nutritional care. Protected Mealtimes are implemented on all wards.
12.Referral to the Nutrition and Dietetic Department
In-Patients should be referred to the Community Dietetic Service in the event of:
• A MUST score of 2 or above
• A specific clinical concern with a low MUST score (0-1) for example for a Grade 3 or 4 pressure sore. This referral must include detailed clinical reasoning for the referral.
Department of Nutrition & Dietetics, Mid and South Essex University Hospitals Group, Broomfield Hospital, Court Road, Chelmsford, Essex CM1 7ET Telephone: 0300 44 35844
NB. Community based patients with nutritional issues cannot be referred to community dietetics directly. Nutrition concerns should be raised with a patient’s GP in the first instance. It is then the responsibility of the patient’s GP to consider referral to community dietetics as per individual risk and requirements.
13.The Dying / Terminally Ill Patient
When a patient is thought to be in the last few days or hours of life, an individualised care plan that includes food and drink must be developed to meet the patient’s needs and wishes and of those important to them.
The patient must be supported to eat and drink as long as they wish to do so and their comfort and dignity prioritised. This may involve considering risk or comfort feeding with advice from Speech and Language Therapists on safest consistencies of food/drink as appropriate.
If the dying person is unable to swallow, decisions about clinically assisted hydration and nutrition must be in line with the General Medical Council 2010 guidance ‘Treatment and care towards the end of life: good practice in decision- making’.
14.Risk Feeding
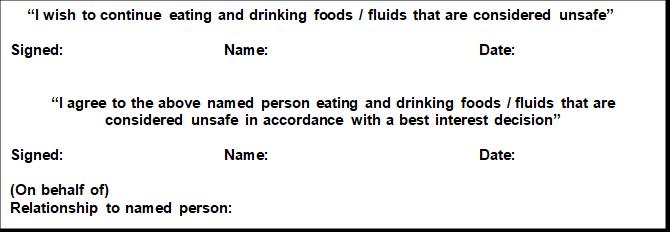
Eating and drinking with an acknowledged risk of aspiration has commonly been known as ‘risk feeding’ or ‘comfort feeding’. Recently, the Royal College of Speech and Language Therapists have produced guidance, using the terminology ‘eating and drinking with acknowledged risks’ (RCSLT 2021). The principle of this approach is to allow individuals to continue to eat and drink, maximising comfort and minimising risk where possible through strategies and modifications. Whilst there are acknowledged risks in doing so (such as choking or aspiration), this approach is typically applied when individuals are nearing the end of their life or have a life limiting or progressive illness (although not exclusively). People with capacity to make an informed decision about

their eating, drinking and swallowing management may choose to continue to eat and drink whatever they want, irrespective of explained health risks.
A feeding at risk assessment should be completed in all situations where aspiration risk has been identified by a dysphagia competent speech and language therapist as unrelated to a transient issue or treatable cause and where the affected individual demonstrates a preference to eat and drink material consistencies that arenot clinically recommended.
Feeding at risk assessment and decision making should operate along the following process:
• In cases where an individual is recognised as having capacity to make a fully informed decision to feed at risk (i.e. eat foods or drinks that carry a clinically determined increased risk of aspiration) that person should read, date and sign appendix 3 ‘Feeding at Risk recording form.’ The form should also be signed by a health professional witness and be countersigned by a medical practitioner for inclusion in the medical record. In-patients for whom feeding at risk decisions have been determined should have a countersigned ‘Feeding at Risk recording form’ positioned at the front of their paper medical records behind any DNAR form that might be in effect. Community patients should have an alert placed on their electronic record (i.e. via SystmOne)
• In cases where an individual’s capacity to consent to a fully informed decision to feed at risk is questionable then an MCA capacity assessment should be conducted to examine whether they can be supported to understand, retain, reason and relay the key aspects of the decision. Where capacity to consent is confirmed the person should be assisted to complete appendix 3 ‘Feeding at Risk recording form’ for inclusion in their medical record (as above). The completed MCA and additional paperwork should also be included in the medical record.
• In cases where an individual is considered to lack capacity to consent to feeding at risk then a best interest decision should be determined. Best interest decisions should derive from collaborative discussion involving relevant medical professionals, the person feeding at risk and their family/carers. Best interest discussions relating to people living in the community should try and involve the registered GP.
• If the best interest decision is made to support ‘feeding at risk’ then a family member of the person concerned should be assisted to complete, date and sign Appendix 3 ‘Feeding at Risk recording form.’ A relevant medical professional should sign as witness and a medical practitioner (GP for community-based individuals), should countersign the document before it is transferred to the medical record as detailed above.
• Discharge of people with completed feeding at risk documentation should involve handover of a copy of the original recording form to destination care personnel and the individual’s registered GP.
15.Oral Nutrition Supplements (ONS)
Oral nutritional supplements can be liquid, semi-solid or powder formulations that are designed to increase nutritional intake. There are a variety of types of supplements,

from single macronutrient e.g. liquid fat supplements or glucose polymer powders to provide energy, to supplements which can be used as a sole source of nutrition. These should only be used under the guidance of and if recommended by a registered dietician
ONS are costly and must be used appropriately.
ONS should only be used when efforts to improve a patient’s nutritional intake using normal food have been unsuccessful.
The Dietician will assess referred patients to decide the need for more specialised nutritional products.
No samples of ONS are to be given to patients or healthcare professionals by Company Representatives.
Patients needing on going oral nutritional supplements will have them prescribed, with a record of their administration detailed on their drug chart.
Nursing staff should document the type and amount of oral nutritional supplement consumed on the food and fluid charts.
Nursing staff should inform the Dietician if the patient is not taking their oral nutritional supplements.
ONS on discharge from hospital
On discharge the efficacy of hospital-based nutrition interventions should be reassessed and ongoing goals for the patient negotiated. The need for ONS should be reviewed as part of this process.
If a patient has been referred to the Dietetic Service for oral nutritional support during their hospital stay, the supervising Dietician will decide if the patient needs ONS on discharge and will write to the patient’s GP giving a summary of Dietetic care and to request on going supplies if necessary.
A 14-day supply of ONS for discharge will be supplied to the patient by the Pharmacy Department if authorised by the dietician.

16.References
Bowling T, British Association for Parenteral and Enteral Nutrition (2004), Nutritional Support for Adults and Children: A Handbook for Hospital Practice. Radcliffe Publishing.
General Medical Council, 2010. Treatment and care towards the end of life: good practice in decision-making, May 2010 (updated 2024) http://www.gmcuk.org/guidance
Leadership Alliance for the Care of Dying People, 2014. One Chance to Get It Right, Improving people’s experience of care in the last few days and hours of life, June 2014.
NICE Guidance 32 Nutrition Support in Adults (February 2006).
Royal College of Physicians, 2010. Oral Feeding Difficulties and Dilemmas – A guide to practical care, particularly towards end of life.
Russell CA, Elia M. Nutrition screening survey in the UK and Republic of Ireland in 2010 .A report by BAPEN, 2011.
The Nursing Midwifery Code of professional conduct: standards for conduct, performance and ethics 2008 www.nmc.org.uk
BAPEN – British Association for Parenteral and Enteral Nutrition www.bapen.org.uk
Royal College of Speech and Language Therapists (2021) Eating and drinking with acknowledged risks: Multidisciplinary team guidance for the shared decision-making process (adults). Available from: EDAR-multidisciplinary-guidance-2021.pdf (rcslt.org)