What You Need to Know
Vishal Gupta, MD
Associate Professor Department of Radiation Oncology
Icahn
School of Medicine at Mount Sinai
New York, NY
Outline
• Background
• Treatment Options
• Radiation Treatment
• Radiation Side Effects
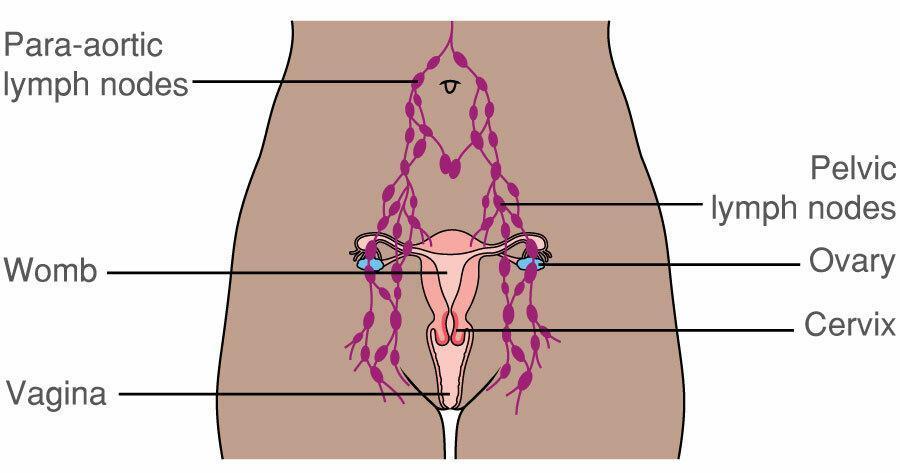
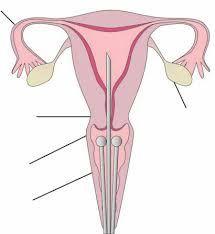
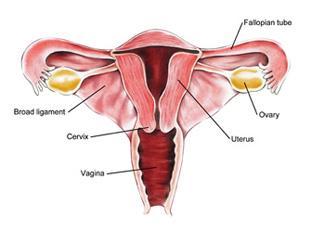
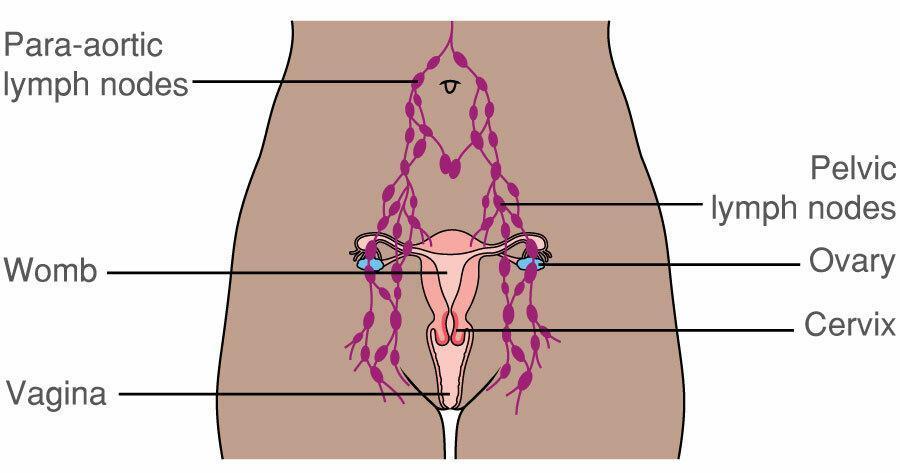
Background- Anatomy
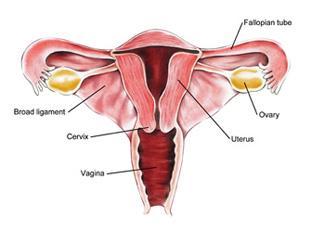

Uterus
Treatment Options



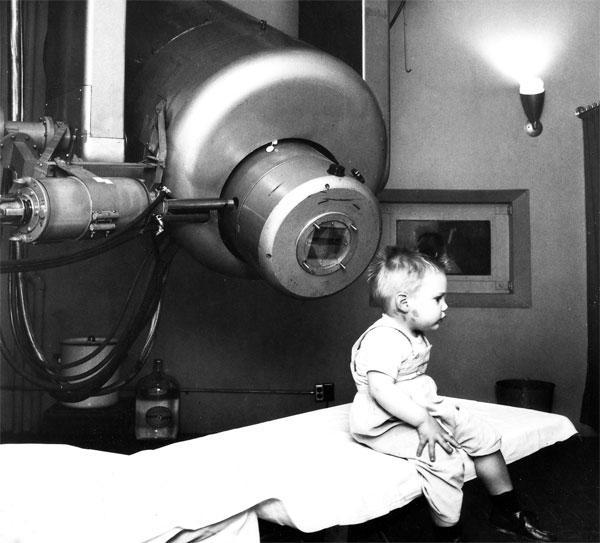
History of Cancer Treatment
• >5,000 years ago – Surgery for cancer
• 1895- Wilhelm Rontgen discovers X-rays
▪ 1896 – Emil Grubbe (medical student) opens first radiation treatment facility for cancer in Chicago
▪ 1940s – Nitrogen mustards used for lymphoma (1st chemotherapy)



Cancer Treatment
• Surgery – removes all or some of tumor
• Curative or palliative
• Radiotherapy – kills tumor cells
• Curative or palliative
• Chemotherapy – kills tumor cells


• Used in conjunction with surgery and/or radiotherapy in curative setting
• Rarely cures cancer on its own
• Exceptions: Leukemia, lymphoma
• Primary treatment in metastatic setting

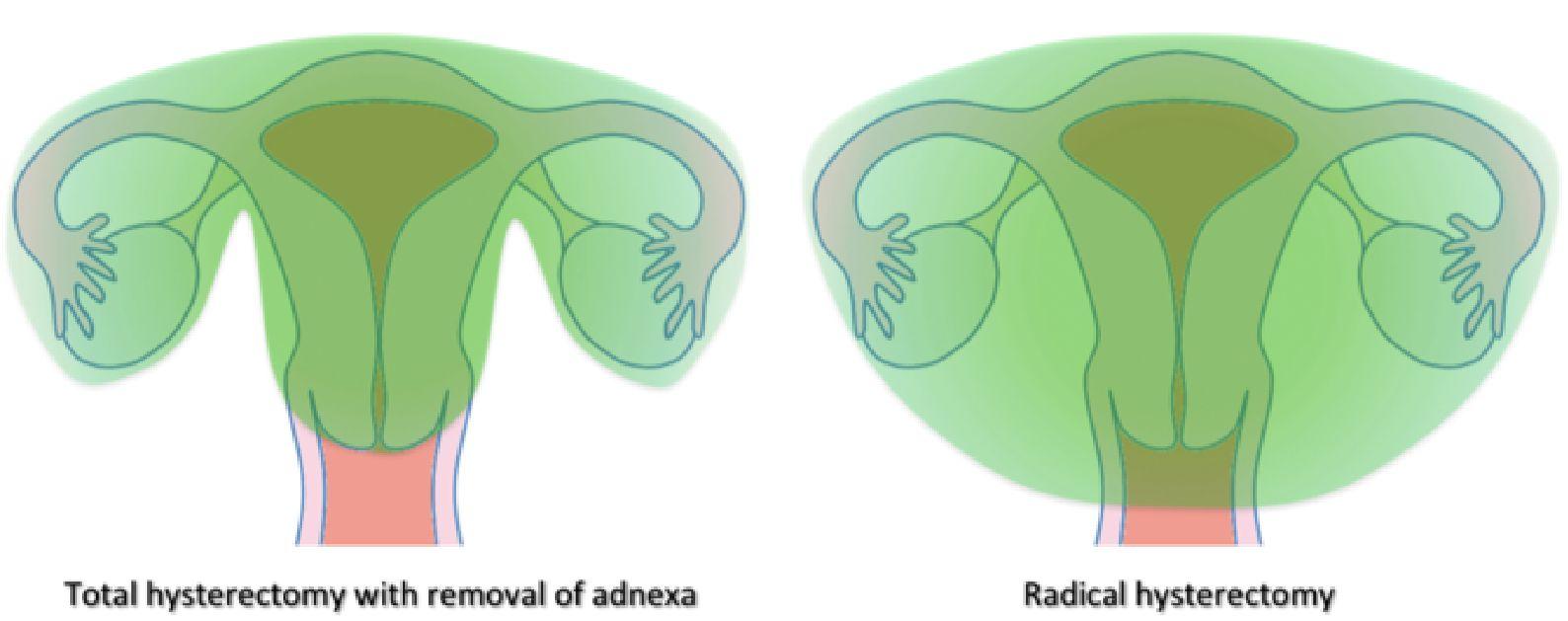
Hysterectomy- 1st step in endometrial cancer
• 5 types: based on extent of surgery
• Type I: removes uterus/cervix only (most common for uterine cancer)
• Type V: removes uterus, cervix, vagina, bladder, rectum
• Potential side effects:
• Pelvic pain – NSAIDs, opioids
• Ileus – bowel rest
• Urinary retention/leakage
• Wound complications
• Nerve damage: lateral thigh numbness, leg weakness – physical therapy
• Surgical menopause
• Lymphedema – compression stockings, PT Type
Anatomy After Hysterectomy

2009 Endometrial Cancer
Staging
• Stage I – limited to uterus
• IA: <50% myometrial invasion
• IB: >50% myometrial invasion
• Stage II – cervical stroma
• Stage III
• IIIA – adnexa/serosa involvement

• IIIB – parametrial or vaginal involvement
• IIIC – pelvic (IIIC1) or para-aortic (IIIC2) involvement
• Stage IV
• Invasion into bladder, rectum
• Distant metastases
2023 FIGO Staging


Staging
Molecular subtyping highly recommended
• p53 abnormal: poor prognosis
• POL-E mutated: good prognosis
• DNA polymerase epsilon gene is involved in DNA replication/repair in cancer cells
• Mismatch repair deficient: intermediate prognosis
• Linked to Lynch syndrome
• No specific molecular profile (NSMP): intermediate prognosis
Treatment After Surgery
• Depends on pathology report from surgery and other risk factors
• Most women do not need any further treatment after surgery
• Risk factors
• Type of uterine cancer (adenocarcinoma is most common)
• Stage (including depth of uterine invasion)
• Grade (aggressiveness of cancer)
• Lymphovascular invasion (highways to lymph nodes)
• Patient age (older patients tend to have more aggressive cancers)
• 3 Groups: Low, Intermediate, High
• Based on above risk factors
Low Risk Group
• <5% risk of recurrence after surgery alone
• No further treatment needed

Intermediate Risk Group
• 10-25% risk of recurrence after surgery alone
• Radiation may be recommended to reduce risk of recurrence
• Vaginal cuff most likely site for recurrence
• Radiation after surgery improves risk of recurrence to 3-15%
• Radiation does not improve survival

High Risk Group
• >50% risk of recurrence after surgery alone
• Recurrence may be distant (lungs/bones) or in pelvis
• Chemotherapy with/without radiation
• Chemo improves survival
• Radiation reduces risk of pelvic recurrence

• Radiation can be given during or after chemo
Carboplatin/Paclitaxel
• Every 3 weeks for 6 cycles via IV infusion
• Possible side effects:
• Neuropathy – gabapentin, Lyrica
• Hair loss– cooling cap, hair prostheses
• Nausea – antiemetic, steroids
• Fatigue
• Low blood counts– transfusion, Neupogen
• Decreased appetite– Megesterol acetate, Marinol
Immunotherapy
• Immunotherapy used in some stage III, stage IV and recurrent/metastatic disease
• Pembrolizumab or Dostarlimab typically used with chemo
• Chemo + immunotherapy has been shown to be more effective than chemo alone
• Most effective in patients with deficient mismatch repair (dMMR)
• Mild-moderate side effects
Radiation Treatment

Types of Radiotherapy
Teletherapy (“distant” in Greek; aka External Beam RT)
• Linear Accelerator
• Cyber Knife – not used in Gyn
• Gamma Knife – Brain tumors only
• Proton Therapy



Types of Radiotherapy
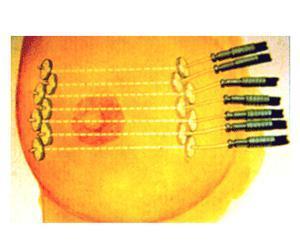
Brachytherapy (“short” in Greek)
• Intracavitary – Breast, Cervix, Endometrium
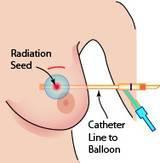

• Interstitial – Prostate, Lip, Sarcoma, Breast, Vagina


Endometrial Cancer – RT Options
Brachytherapy - Cylinder
•Treats vaginal cuff only (most common site of recurrence in intermediate risk)
•1-2x per week for 3 weeks
•Intermediate risk patients

External Beam Radiotherapy
•Treats vaginal cuff, parametrium, pelvic lymph nodes
•Daily treatment (M-F) for 5 weeks
•High risk patients

Background- Anatomy

Radiation Dose
• Dose: Gray (Gy)
• Brachytherapy
• Total dose: 21-30 Gy
• 4-7 Gy, 1-2x per week
• 3-6 treatments over 3 weeks
• External beam RT
• Total dose: 45-50 Gy
• ~2 Gy daily
• 25 treatments over 5 weeks
EBRT vs Brachytherapy


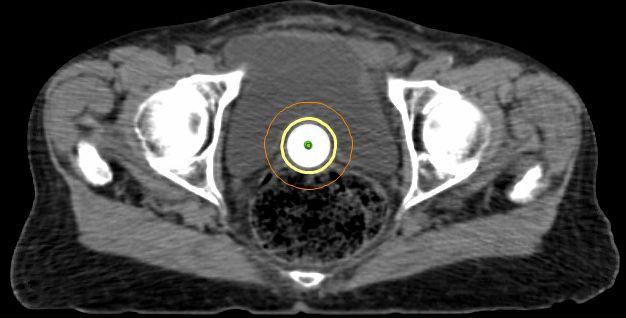

Simulation
• CT scan
• Immobilization device

• Draw tumor and normal structures on CT slice-by-slice (“contouring”)

• Entire treatment based on this CT scan

Patient Flow
Diagnosis (typically by Gynecologist)
Surgery
if RT needed
RT Consultation
~1 week
Simulation
1-10 days for RT planning
RT Course (3-5 weeks)
Follow-Up (5 years)
Possible Side Effects of EBRT
•Acute- during or shortly after EBRT
• Diarrhea, rectal bleeding - loperamide, diphenoxylate/atropine
• Urine frequency, urgency – ibuprofen, oxybutinin
• Pain or bleeding with urination - phenazopyridine, ibuprofen
• Skin peeling - topicals, aloe vera, silver sulfadiazine
• Nausea/vomiting - antiemetics
• Fatigue
• Resolve 2-4 weeks after treatment
Possible Side Effects of EBRT
•Chronic- >3 months after EBRT
• Diarrhea, rectal bleeding - coagulation (APC)
• Urine frequency, urgency
• Urine/Fecal leakage <1%
• Bowel obstruction, perforation <1%
• Leg edema
• Bone fracture
• Rare to have significant chronic side effects
• Medications or minor procedures may be needed to treat
Possible Side Effects of Cylinder
Brachytherapy
•Acute- during or shortly after brachytherapy
• Diarrhea
• Pain with urination
• Fatigue
• Rarely require medications to treat
• Resolve within 24 hours of each procedure
Possible Side Effects of Cylinder
Brachytherapy
•Chronic- >3 months after EBRT
• Vaginal dryness – lubricant, topical estrogen
• Vaginal fibrosis, shortening – dilator for prevention
• Urethral stricture
• Urine/Fecal leakage <1%
• Fistula – opening between vagina and bladder or rectum
• May affect sexual function and make pelvic exams uncomfortable
Brachytherapy vs. EBRT
•Similar cure rates in intermediate risk patients
•Brachytherapy has fewer side effects
•European study compared them:
•Similar cure rates
•Less long-term bowel issues with brachytherapy
•Slightly less long-term bladder issues with brachytherapy
•No difference in sexual function* or overall quality of life
de Boer, et al. International Journal of Rad Onc Biol Physics 2015. Nout, et al. Lancet 2010.
Recurrence – What if the cancer comes back?
• Vaginal cuff only
• If no prior radiation, then external radiation and brachytherapy
• If prior radiation, re-irradiation is not typically offered
• Surgery may be an option
• Lymph nodes only
• Surgery and then external radiation, if no prior radiation
• Distant (lungs, bones, etc)
• Chemotherapy and/or immunotherapy
• Targeted radiation (SBRT) can be given if only a few sites
• Palliative radiation can be given for pain or bleeding
Current Trials
RAINBO Trials - 4 trials to help guide treatment based on molecular classification
• p53 mutation: chemo/radiation vs. chemo/radiation/Olaparib
• Mismatch repair deficient: radiation +/- durvalumab
• POL-E mutation: eliminating radiation for “intermediate” risk
• No specific molecular profile (NSMP): if ER+, radiation/progestin vs. radiation/chemo
Conclusions
•Surgery is 1st step in treatment of endometrial cancer
•Post-operative treatment depends on risk factors
•Low Risk – no further treatment
•Intermediate Risk – Radiation may be recommended
•High Risk – Chemo +/- radiation +/- immunotherapy
•Radiation treatment - brachytherapy or external beam (or both)
•Intermediate Risk – brachytherapy
•High Risk – external beam and/or brachytherapy
•Radiation well tolerated, but may have long term side effects
•Radiation prevents recurrence, but does not improve survival in endometrial cancer
•Balanced discussion with your doctors about pros/cons
