




















Cheryl Anema PhD, RN

Cheryl Anema PhD, RN
Over the past few weeks, I have been watching and reading the unfolding of the COVID-19 pandemic I have been searching my soul for understanding as I watched friends pass away But I was also torn by the call of being a nurse I am currently not on the frontline I have been preparing novice nurses for our great profession for the past 30+ years As they called for nurses to come back into the hospitals to work, I hesitated and thought, "Can I do this?" I realized that I have moved beyond the bedside in my age and health I now qualify as the "atrisk" population for the virus So I continue to work passionately preparing the nurses of tomorrow
I continued to read and look for inspiration to offer my graduates, previous students, and nurse friends and family over these weeks I read about the stories of New York Nurses The sacrifice so many nurses have and are making at this time in history Yes, this will be in the history books I received an email from my cousin in Vermont She told me how her daughter, and ICU nurse, decided to move out of her home, away from her husband and preschool-aged daughter, so as not to bring home the possible virus
The sacrifice that nurses, and other healthcare providers, make daily cannot fully be understood Even before COVID, nurses gave up family holidays, social events, and weekends Now? They are on the front line of the Virus War! There is a lot of controversy about the numbers, testing, political blame, and over or underreacting to the virus invasion
Whatever you believe, nurses "have" risked their lives and continue to go to work and care for the needs of their patients I am proud to say I am a nurse Every nurse out there who is working in the field, preparing others to work in the field, or have retired and support nursing today through their words and support, need to be proud they are a nurse!
In a society of so many different races, cultures, customs, and beliefs, nurses are a universal gift to all,
and the dedicated work that they do and kindness they deliver on a daily basis should serve as a reminder of the fundamental humanity inside us all Becoming a nurse is one of the most selfless acts a person can undertake
The IL Nurses Foundation THANKS each and every nurse for all they have, are, and will be doing to bring health and comfort to people throughout the state and around the world What would the world be without nurses! Thank-you!
To support the work of the IL Nurses Foundation, please go to https://www illinoisnurses foundation/ and click on "Ways to Give " Every donation goes to promote collaboration with community partners in promoting the health of the public, supporting nurses through charitable research, and enhancing educational initiatives


INF Board of Directors
Officers
Cheryl Anema PhD, RN
Brandon Hauer MSN, RN
Cathy Neuman MSN, RN
Karen Egenes EdD, RN
Directors
Maureen Shekleton PhD, RN, DPNAP, FAAN
Alma Labunski PhD, MS, RN
Linda Olson PhD, RN, NEA-BC
Amanda Buechel, BSN, RN, CCRN
ANA-Illinois Board Rep
Karen Egenes EdD, RN
Stephanie Yohannan, DNP, MBA, RN, NE-BC
Lauren Wojtkowski, RN, CEN

ANA-Illinois Board of Directors
Officers
Elizabeth Aquino, PhD, RN
Karen Egenes EdD, MSN, MA, RN
Pam Brown, PhD, RN, ANEF
Colleen Morley, MSN, RN, CMCN, ACM
Directors
Susana Gonzalez, MHA, MSN, RN, CNML
Nicole Lewis, DNP, APRN, FNP-BC
Lauren Wojtkowski, RN, CEN
Crystal Vasquez, DNP, MS, MBA, RN, NEA-BC
Stephanie Yohannan, DNP, MBA, RN, NE-BC
Editorial Committee
Editor Emeritus
Alma Labunski, PhD, MS, RN
Chief Editors
Lisa Anderson-Shaw, DrPH, MA, MSN
Karen Mayville, MSN, PhD, RN
Members
Kathy Long-Martin, BSN, MSN, RN
Linda Olson, PhD, RN, NEA-BC
Lisa Hernandez, DNP, RN, CENP
Nancy Brent, RN, MS, JD
Executive Director
Susan Y Swart, EdD, MS, RN, CAE
ANA-Illinois/Illinois Nurses Foundation
Article Submission
• Subject to editing by the INF Executive Director & Editorial Committee
• Electronic submissions ONLY as an attachment (word document preferred)
• Email: kristy@sysconsultingsolutions com
• Subject Line: Nursing Voice Submission: Name of the article
• Must include the name of the author and a title
• INF reserves the right to pull or edit any article / news submission for space and availability and/or deadlines
• If requested, notification will be given to authors once the final draft of the Nursing Voice has been submitted
• INF does not accept monetary payment for articles
Article submissions, deadline information and all other inquiries regarding the Nursing Voice please email: kristy@sysconsultingsolutions com
Article Submission Dates (submissions by end of the business day) January 15th, April 15th, July 15th, October 15th
Advertising: for advertising rates and information please contact Arthur L Davis Publishing Agency, Inc , 517 Washington Street, P O Box 216, Cedar Falls, Iowa 50613 (800-626-4081), sales@ aldpub com ANA-Illinois and the Arthur L Davis Publishing Agency, Inc reserve the right to reject any advertisement
Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement
Acceptance of advertising does not imply endorsement or approval by the ANA-Illinois and Illinois Nurses Foundation of products advertised, the advertisers, or the claims made
Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use ANA-Illinois and the Arthur L Davis Publishing Agency, Inc shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of ANA-Illinois or those of the national or local associations
We know that nurses have always been heroes for their unwavering courage, compassion, resilience, trustworthiness, humility, and integrity But this year, the world has witnessed the Power of Nursing as nurses continue to show up to respond to the fight against novel coronavirus

Liz Aquino, PhD, RN
Thank you to each of you for answering the call in your own way, particularly nurses who are working on the frontlines I have heard many of your stories that include real fear, anger, sadness, hope, and strength COVID-19 has evoked many feelings because of the uncertainty about the virus, what we know about the epidemiology of infectious diseases and our awareness of what happens when healthcare providers are not adequately protected But because you continue to show up with compassion while caring for your patients, you have helped them be a little less fearful, a little less lonely, and a little less hopeless And despite all that your patients are going through, they will never forget the way you made them feel during this time
I know this has been quite a challenge, to say the least, and I pray that by the time you read this message, we are on the other side of "the curve " The response to the pandemic has stressed that nurse advocacy is needed now more than ever, and legislation impacting nurses must be prioritized Yes, nurses go into healthcare to help others, but not under unsafe conditions that risk their lives, their loved ones, and their patients We must make sure legislation and policies are in place that help protect nurses Relaxing the rules and modifying standard safety and infection control protocols to deal with the PPE shortage crisis is unacceptable and puts nurses and the public at risk We can not allow this to ever happen again to our frontline ANA and ANA-Illinois continue to listen to frontline stories and have taken immediate action at the national and local level The work being done includes advocating on behalf of all nurses to be provided appropriate PPE, continuing to share COVID-19 resources on the ANA COVID-19 resource center webpage and webinars, created a coronavirus response fund for nurses, and influencing policy that protects nurses We hope that you will join us by helping us continue to advocate on issues that impact the future of nursing To get involved, visit the ANA-Illinois advocacy portal and reach out to us with any concerns or ideas you would like to share COVID-19 has changed all of our lives in ways we might not even yet process I urge you to find time for self-care, even if it's just 3-5 minutes to clear your mind, join Healthy Nurse Healthy Nation if you haven't already, to learn about ways to recharge, and/or journal your thoughts Recording your feelings and experiences as frontline responders during the COVID-19 pandemic is an essential part of documenting history that will hopefully never be repeated My thoughts and prayers are with you during this difficult time; all nurses are in this fight together, and we will protect our own A lighthearted and truthful quote by Donna Wilk Cardillo reminds us of the weight of our responsibility as a nurse "Nursing is not for everyone It takes a very strong, intelligent, and passionate person to take on the ills of the world with passion and purpose and work to maintain the health and well-being of the planet No wonder we're exhausted at the end of the day!"
Wishing you wellness and peace, Sincerely,
Elizabeth Aquino, PhD, RN
President, ANA-Illinois
@LatinaPhDRN
The COVID-19 pandemic has impacted our day to day lives but has also changed how we practice nursing Prior to this event, I never considered how to provide care in a worldwide crisis While I have been interested in state and national legislative actions as they have an impact on nursing, I have never really considered how these decisions would cause changes in how I practice in a pandemic Each one of us has stepped up to the plate by working long hours and providing care in ways that one year ago may have caused us to be terminated from our employment We provide evidencebased care and use all the critical thinking and creativity possible For these talents, tenacity, long hours, the impact on your safety and the safety of those you love… for all of these things, I thank you from the bottom of my heart

Because we are practicing in a critical period and in ways that many of us had not envisioned, we are making on-the-spot modifications to policies and procedures, variations in how we acquire materials and transformations to care delivery It is crucial that we document these adjustments so that after this event has concluded (and it will conclude), we can make enduring changes in policy that are grounded in not only evidence but also in livedexperience Because of this, I would like to ask a favor As you think about your practice environment, please jot down the adaptations that your organization has made as well as the ones that you have personally made to allow you to provide patient care Some areas to consider include direct-care, staffing, personal and patient safety, supply acquisition and use, triage, and in-clinic vs telemedicine patient encounters I would ask that you jot these adaptations down and send them in an email to me (rsloar@ gmail com) I will compile the information, and we will use it to help us guide changes in policy If you are interested in a copy of this data set, please let me know in your email, and I will be happy to send it to you
One piece of federal legislation that has a direct impact on how we provide care is the CARES Act, passed in response to the COVID-19 pandemic A portion of this act permits Nurse Practitioners and Clinical Nurse Specialists to certify for Home Health services without a physician signature Even though this Act was in response to a pandemic, this is now a permanent expansion of our ability to practice
I would also like to ask one more favor I know that we aren’t thinking about selfcare at this moment, but I would ask that you take care of yourselves Remember to eat, sleep, exercise, practice kindness and patience, and if you find it helpful, pray, and meditate We can’t do our best for others unless we do our best for ourselves I would like to once again take this opportunity to speak for myself as well as for ISAPN: Thank You for your dedication to our profession and service to our patients Everything that you do is deeply appreciated

President, ISAPN

Susie Watkins PhD, RN, Assistant Professor Judy Neubrander, EdD, FNP-BC, Dean Illinois State University – Mennonite College of Nursing
Drastic changes in healthcare delivery have resulted from social distancing requirements after the initial month of the 2019 Novel Coronavirus (COVID-19) pandemic Even as essential healthcare service providers, primary care clinicians are faced with reduced practice capacity, revenue, and furloughs required to decrease operating budgets (Primary Care Collaborative [PCC], 2020) As many primary care practices still operate within a fee-for-service reimbursement model to receive volume-based payments, cash flow has been immobilized, resulting in clinic closures and clinician furloughs (PCC, 2020) Primary care telehealth platforms are proposed as the ideal option to provide symptom triage, medication access, and illness treatment services throughout this pandemic; however, service requirements are complicated while reimbursement is uncertain (PCC, 2020)
There have been many challenges preventing primary care telehealth implementation within Rural Health Clinics (RHC) RHC telehealth challenges include vulnerable patient populations, decreased informatic technology support, and access, along with complicated billing requirements (PCC, 2020) The lack of routine primary care service access in RHCs is detrimental to the vulnerable patient populations serviced in rural areas, who are at higher risk for health disparities due to the lack of resources (Lutfivya et al , 2012) Prior to the COVID-19 pandemic, less than 10% of primary care providers had implemented virtual visit platforms because of complicated technology requirements, confidentiality concerns, and reimbursement obstacles (Peabody, Dai, Turner, Peterson, & Mainous, 2019) During the COVID-19 54% of primary care practices are addressing mounting patient concerns related to psychosocial health issues, along with 72% of practices reporting patient difficulties participating in virtual visit platforms (PCC, 2020) This survey data has also revealed RHC’s are also struggling to implement virtual health platforms capable of offering non face-to-face accessibility for primary care needs during the COVID-19 pandemic for many reasons, including lack of information technology support, patient’s lack of resources for digital devices required for virtual visits, and uncertain reimbursement provisions (PCC, 2020) Rural social determinants are playing a major role in healthcare accessibility during the pandemic (PCC, 2020)
Healthy People 2020 describes the social determinants of health as being “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks” (United States Department of Health and Human Services (Office of Disease Prevention and Health Promotion [ODPHP], 2020) Critical components/key issues involved in health and health care include access to health care, access to primary care, and health literacy (ODPHP, 2020) “Rurality” is considered a fundamental social determinant of health and impact on health outcomes (Anderson, Saman, Lipsky, & Lutfiyya, 2015; Lutfivya et al , 2012) The incidence of such diseases as Type 2 diabetes, cervical cancer,
and lung cancer have been found to be influenced by rural locale (Lutfiyya et al , 2012) Rural areas experience disadvantaged rates of reported health care use (screenings and dental visits), compared to urban areas (Caldwell et al , 2016)
In looking at just the rural population of Illinois, the U S Census Bureau the segment of the rural population reaching the age of 65 and over has increased from 14 2% in 2010 to 17 6% in 2015, with the aging rural population at higher risk for both complex acute and chronic conditions (Norris, 2017) According to the United States Department of Health and Human Services (2017) National Healthcare Quality and Disparities Report Chartbook On Rural Health Care, rural residents as compared with their urban counterparts have higher age levels, lower socioeconomic values, and higher disease prevalence, injury rates, opioid dependence levels, tobacco use rates, and suicide rates, along with lower healthcare insurance coverage The life expectancy for U S residents decreases as the level of rurality increases (USDHHS, 2017) Causes of death contributing most to lower life expectancy in rural areas include heart disease, unintentional injuries, chronic obstructive pulmonary disease, lung cancer, stroke, suicide, and diabetes Demographic shifts are occurring as the rural physician workforce is aging, and there is growth in the rural elderly and near-elderly population, thus increasing demand for primary care services (National Conference of State Legislatures [NCSL], 2014)
Given changes occurring in health care related to population aging, expansion of coverage through the ACA, high rates of chronic disease, compounded by the COVID-19 pandemic, the Registered Nurse (RN) is essential in telehealth provisions in rural and urban primary care settings Prior research has demonstrated that RNs are an affordable option in primary care and can reduce the overall cost of health care delivery (Yang and Meniers, 2014) Yang and Meniers (2014) also found that nurses with expanded roles in team-based care coordination, including communication between the patient, family, and other health care providers, improves health care outcomes It will be essential for primary care RNs to participate in the rapid implementation of telehealth modalities to assist primary care providers with accessibility for vulnerable patient populations managing multiple comorbidities, experiencing illness symptoms, and needing behavioral health disease self-management support during the COVID-19 pandemic Telehealth platforms allow primary care providers to deliver routine services, remain accessible for emergent care needs, and prevent community spread of COVID-19, while reducing the economic burden to healthcare entities related to decreased face-to-face office visit volume-based revenue Within two weeks of the COVID-19 pandemic onset, public health efforts for the prevention of community spread significantly reduced primary care clinic revenue, and currently is threatening the financial viability for metropolitan and RHCs (PCC, 2020) In response to healthcare accessibility and revenue concerns, the federal government has initiated emergency legislation to reduce telehealth barriers (CMS, 2020)
The Centers for Medicare & Medicaid Services (CMS) reduced Medicare and RHC telehealth reimbursement challenges through the Coronavirus Aid, Relief, and Economic Security (CARES) Act (CMS, 2020) The federal government is also preparing the Creating Opportunities Now for Necessary and Effective Care Technologies (CONNECT) for Health Act of 2019 (CONNECT Act) proposal for 2021 to reduce Medicare telehealth obstacles within the Social Security Act (CMS, 2020) The CONNECT Act will reduce telehealth live-video, asynchronous store-and-forward, and originating patient/provider site, and service modality requirement obstacles impeding widespread adoption of telehealth services in primary care (CMS, 2020) While alleviating restrictive billing requirements for telehealth, the CARES and CONNECT legislation do not contain language permitting professional Registered Nurses to provide reimbursable telehealth services (United States House of Representatives, 2020)
Earn a MSN Degree or Post-MSN Certificate and prepare to become a Nurse Practitioner.
We are pleased to announce the 100% pass rate on 2019 AANP Certification Exams by our Adult Gerontology Primary Care Nurse Practitioner and Family Nurse Practitioner graduates!
Earn your Doctor of Nursing Practice Degree:
Online Program for master’s-prepared nurses
Learn more: www.northpark.edu/ANA Questions? (773)244-5508 (Campus Voicemail) (872)772-9103 (Call/Text/Facetime) gradadmissions@northpark.edu
School of Nursing and Health Sciences

By not including RNs within the CARES and CONNECT Act as eligible healthcare professionals to provide telehealth services, the team-based primary care model is compromised for accessible disease management, acute illness, and behavioral health care patient needs during the COVID-19 pandemic crisis Professional RNs are key interprofessional team members within team-based primary care models supporting patient-centric holistic care (United States House of Representatives, 2020, 42 USC 256a1) RNs supply the largest occupation within the American healthcare infrastructure (U S Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis, 2014), and RNs can lead the rural health chronic disease telehealth while increasing quality and revenue within pandemic affected primary care practices
RNs provide expert telehealth services within innovative interprofessional teambased care models utilizing evidence-based telehealth guidelines established by the American Academy of Ambulatory Care Nursing (AAACN, 2020) RNs provide telehealth triage utilizing clinical judgment, algorithms, and evidence-based guidelines to ensure patients receive the appropriate level of care (AAACN, 2020), which will remain a critical primary care service during the COVID-19 pandemic and dwindling revenues that threaten practice viability The expert RN telehealth assessment knowledge and skills utilized with clinical judgment allows the RN to prioritize urgent care needs, triage COVID-19 symptomatic concerns, and address escalating emotional health needs, and wellness concerns during the pandemic, along with the delivery of routine supportive patient education for treatment recommendations and evaluation of care outcomes (AAACN, 2020) Over 90% of primary care practices have reported ceasing all well-child and adult preventive care visits during the pandemic while limiting ongoing disease management visits during the COVID-19 pandemic, which will further compound population illness during these unprecedented times when healthcare is an essential service (PCC, 2020) Essential to vulnerable patient population continuity of care during the coronavirus pandemic, RN telehealth supports population health, care coordination, transitional care, disease self-management support, health promotion, ailment assessment, and palliative care for patients and families (AAACN, 2020) Modern advancements in RN telecare delivery through mobile devices and digital technologies parallel CMS (2020) "telemedicine" designation of utilizing virtual visit modalities to connect patients to health professionals to share audio, video, or graphic health data for receipt of quality healthcare services (United States House of Representatives, 2020, section 1395u(b)(18)(C) RN-led telemedicine interventions are linked to improved disease self-management behaviors associated with reduced HbA1C levels, improved blood pressure control, and decreased fragmentation of care (Massimi, et al , 2017; Yang and Meniers, 2014) It is essential for state and federal legislators to recognize the urgent need for RNs to qualify as one of the additional health professionals to provide reimbursable telehealth services to mitigate pandemic associated healthcare workforce shortages, accessibility to care, and declining revenues associated with viral public health infection control in primary care settings References available upon request
Your nursing experiences with the COVID 19 pandemic demonstrate the nursing profession at its best Your stories are of great interest to fellow nurses, as well as to the general public
Are you working with COVID 19 patients on an acute inpatient unit? What has the experience been like for you, your colleagues, and your patients? Do you have a memory of a particular patient (No names to maintain HIPAA)? Can you relay a particularly stressful event that impacted your staff members?
Do you work in a community health or a primary care setting? Can you relate the impact of the epidemic on persons from underserved populations? Were you able to teach individuals ways to protect themselves from the Coronavirus? How has the virus affected you and the communities that you serve?

How has the COVID 19 pandemic affected your practice of nursing? What measures have you taken to protect yourself, your family members, and your patients? What new skills or nursing knowledge have you acquired from the pandemic experience? What experiences have you had with distance learning, virtual clinical settings for nursing students, ZOOM meetings, social media, homeschooling, or other adaptive measures?
How has the COVID pandemic affected your personal life? Have you been furloughed, laid off from work, or moved to a different practice setting? What coping techniques have you used to deal with the stress generated by the pandemic? How have you and your family members coped with the self-quarantine experience? Have you experienced losses related to the pandemic, such as the death or illness of a significant other or colleague? Have you been forced to cancel a significant event, like a wedding, graduation, or even a funeral? Have you contracted COVID 19; what was the experience like for you? What are your fears and hopes for the future?
The Illinois Nurses Foundation (INF) would like to gather your stories for possible publication in the future By submitting your stories to us, you grant the INF permission to publish them in Nursing Voice or another public medium Please indicate your consent for us to publish your name or indicate that you would prefer that your story be published anonymously Institution names will not be published
Please submit your story (or stories) either by mail to: Illinois Nurses Foundation, PO Box 636, Manteno, Illinois 60950 or as an attachment to an email at: syswart@anaillinois org
Please include your name, daytime telephone number, email address, mailing address If you have photos to accompany your story, please send them by email in the JPEG format
We are living what will become a significant event in the history of nursing Your personal stories will document the contributions of nurses during this time We look forward to hearing from you!
We want YOUR COVID STORY!











For the Illinois population of 12,671,821, there are 172,466 RNs with an address in Illinois. What else do we know? Do we need to know more? Where is the data?
We know that the ratio of RNs to population is estimated to provide a basis to compare the number of RNs available to the workforce in a state We know that approximately 22% Illinois RNs indicate that acute care or critical care or intensive care is their specialty area (Illinois Nursing Workforce Center, INWC 2018 survey http:// nursing illinois gov/ResearchData asp) In this same 2018 RN survey, conducted with online license renewal, approximately 11% indicated that community or public health department is their specialty area, and approximately 13% indicated that medicine is their specialty area Where do these RNs work? In which county or zip code? How many are going to retire soon? Are they all currently employed in their area of expertise? We do not have this level of information, but we can do better with knowing if we have the nurses to care for Illinois citizens with your help
After completion of license renewal fee payment for Illinois RN or APRN license renewal, nurses will see a message with a link to click on to reach and participate in the short survey The Illinois Nursing Workforce Center (formerly the Illinois Center for Nursing) is requesting that you complete this short 26-question survey after paying the license renewal fee The RN survey completion time is approximately five minutes; all questions offer multiple-choice response options, with limited spots for comments
The survey captures data on the demographics, education, state distribution, and practice foci in Illinois The APRN survey also includes questions to be compared with data collected with license renewal in 2018 The Nursing Workforce Center will evaluate the impact of changes in the Nurses Practice Act, such as the number of APRNs practicing outside of a hospital who are no longer maintaining a collaborative agreement in their practice setting
Are there areas in the State where Registered Nurses (RNs) or Advanced Practice Registered Nurses (APRNs) are concentrated? Where are the greatest needs? How would the educational pipeline for RNs be best characterized? Where are the APRNs with full practice authority seeing patients? We need your help in answering these questions
All Illinois RNs and APRNs whose CE completion and license renewal deadline was May 31, 2020 now have a September 30, 2020 deadline In light of the challenges confronting all Illinoisans during the COVID-19 pandemic, the Illinois Department of Financial and Professional Regulation (IDFPR) has issued a series of variances that provide relief from the provisions of certain Administrative Rules pertaining to license renewal terms and to continuing education requirements These variances include granting an automatic extension to September 30, 2020, to complete RN and APRN license renewal and to participate in the survey
Please take five minutes after completing license renewal 2020 share info about you, your nursing specialty and workplace
If what we know is the ratio of RNs to Illinois population, is that enough? The limitations of comparing ratios are the assumptions that residents will receive nursing services in the region they reside and that the same types of health care services are available in each region The number and distribution of nurses in a region may need to be higher based on the needs of that region, which is why we need your help nursing


Lisa Lozeau, MSN RN CPN
Swedish Hospital, Nurse Manager
Dolly Leong-Dawson MSN RN CRRN
Swedish Hospital, Registered Nurse
Dimitra Loukissa PhD RN PMHN-BC
Professor of Nursing, School of Nursing and Health Sciences
Aim
North Park University, Chicago, Illinois
The aim of this project was to investigate how reeducation on bedside reporting would affect Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, medication errors, patient falls, and Registered Nurse’s (RN) perceptions of bedside report at a Magnet designated community hospital
Background
It has been well documented that bedside report improves patient safety and satisfaction, and nurse satisfaction However, bedside report at this particular institution was inconsistently performed
Method
Data was collected on HCAHPS scores, medication errors, and patient falls A pre and post-survey assessing nurse’s perception of bedside report was completed The Clinical Patient Experience Manager began training in June of 2016
Results
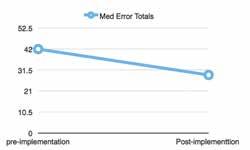
The results of the project suggested that bedside report shows improvement on HCAHPS scores, patient falls, medication errors, and nurse’s perception of bedside report
Conclusions
The improved outcome measures may be attributed to the communication between staff and the patients that occurs during bedside report
Implications for Nursing Management
Nurse leaders are responsible for ensuring the success of their team through effective communication, meeting quality measures, and improving patient satisfaction Innovative leaders should encourage and monitor this handoff process to maintain the practice of bedside report hospital-wide
According to the Joint Commission (2017), improving staff communication is a national patient safety goal Poor communication may play a role leading to sentinel patient events, such as falls or medication errors (SandJecklin & Sherman, 2014) Change of shift has the potential for miscommunication in an environment with frequent interruptions Handoff refers to the transfer and acceptance of responsibility of the patient through communication of information to promote continuity of patient care between caregivers (Joint Commission, 2017) Patients should be informed about their diagnosis and their plan of care to give them opportunities to ask questions or correct misinformation Bedside report is one strategy to improve communication between the staff and the patient Bedside report was not performed consistently across inpatient nursing units at a Magnet designated, 300-bed community teaching hospital on the north side of Chicago It was the goal of nursing leadership to implement consistency in practice regarding bedside report to increase patient safety in addition to patient and nurse satisfaction
Literature Review
Bedside report is an evidence-based practice; it is described extensively in the literature as a strategy to improve communication, and ultimately patient care The literature overwhelmingly supports that bedside report increases patient outcomes and patient and nurse satisfaction by establishing trust, enhancing communication, and facilitating information sharing with nurses, patients, and their families; thus, patients feel that they are actively involved in their care (Spivey, 2014; Vines, Dupler, Van Son, & Guido, 2014; Sand-Jecklin & Sherman, 2014) The literature suggests that there is a link between bedside report and HCAHPS scores, specifically, the communication dimension (Vines, et
al , 2014) The communication dimension for patient satisfaction includes patient communication with nurses and other providers delivering care (National Research Corporation, 2017) Patients feel that the staff were respectful to them and worked better as a team when they participated in the plan of care (Scheidenhelm & Reitz, 2017)
Furthermore, bedside report enhances patient safety by improving report accuracy, minimizing communication errors and allowing patients to express concerns, or ask questions during report (Sand-Jecklin & Sherman, 2014; Vines et al , 2014) When patients and their families are actively involved in discharge planning, they are more likely to understand and comply with the plan of care, improving patient safety Also, safety is enhanced when the nurses review medications, equipment settings, and patient care environment during bedside report (Scheidenhelm & Reitz, 2017, Boshart, Knowlton, & Whichello, 2016) Moreover, several studies demonstrated a decrease in patient falls and medication errors (Sand-Jecklin & Sherman, 2013; Scheidenhelm & Reitz, 2017; Boshart, et al , 2016)
Nurse satisfaction is another well documented benefit of bedside report as it promotes stronger communication among the nurses, which further improves teamwork and respect among staff with the end result of increased nurse accountability (Vines, et al , 2014) Report done with the patient present promotes professional communication among the nurses as it allows the oncoming nurse to check intravenous sites, surgical incisions, lines, and infusion rates (Spivey, 2014) Nurse satisfaction increases with improved time efficiency as a result (2014) In addition, when nurses are able to clarify information and assess patients immediately, they can prioritize care quickly (Spivey, 2014) Spivey (2014) reported that the time needed for shift change decreased from an average of 66 minutes to 39 minutes with bedside report On the other hand, report done away from the bedside has the tendency to be more disorganized, lengthier than necessary, and poses the risk for interruptions and socialization among the nurses (Vines, et al , 2014)
Methods
Our organization embraced the importance of communication at change of shift and decided to implement this quality improvement project Lewin’s theory of change was used as the theoretical framework for this quality improvement project According to the theory, change occurs in three stages: unfreezing, moving, and refreezing (Lewin, 1951) The unfreezing stage is about recognizing the need for change, building trust, and encouraging participation in the intervention During the moving stage, the focus is on planning change, initiating change, and revising the process based on feedback Finally, the refreezing stage involves integrating the change into practice (Lewin, 1951) One of the aims of the quality improvement project was to determine how improving bedside report would affect HCAHPS scores
HCAHPS is the first national, standardized publicly reported survey of patients’ hospital care developed by Centers for Medicare and Medicaid (CMS) and the Agency for Healthcare Research and Quality (AHRQ) (Studer, Robinson, & Cook, 2010) The survey had three main goals: 1) to allow patients to compare hospitals 2) to incentivize hospitals to improve quality of care, and 3) to provide transparency of the quality of care being rendered (Studer et al , 2010) HCAHPS also has an initiative that ties reimbursement to quality outcomes, moving from a pay for reporting to pay for performance The amount of reimbursement tied to the survey doubled in 2017 (Studer et al , 2010) There must be a minimum of 300 survey submitted by eligible patients for each quarter Eligible patients have had an acute care overnight stay, and over 18 years of age (Studer et al , 2010) The survey allows for comparisons to be made across hospitals citywide, state wide, and nationwide (2017) The survey asks patients about their hospital experience regarding communication with nurses and doctors, responsiveness of hospital staff, the cleanliness and quietness of the hospital environment, pain management, communication about medication, discharge information, overall rating of the hospital, and whether they would recommend the hospital (CMS, 2017) In addition to HCAHPS scores, the quality
improvement project sought to determine improvement in patient falls, medication errors, and nurse’s perception following re-education of bedside report
Pre-Implementation
To start, the Clinical Patient Experience Manager assessed the units on whether bedside report was being done at the bedside by documenting “yes” or “no” on a log An online survey that measured nurse perception of bedside report was conducted pre and post implementation included questions considering the effectiveness and efficiency of communication, stress level, and delays in patient care, accountability, timeliness, and patient involvement (Appendix A) Additionally, unit champions were solicited to promote buy-in to the change
Baseline HCAHPS scores were obtained from the Catalyst report on the National Research Corporation (NRC) Picker website during the 2nd quarter between April-June 2016 Data on post implementation of HCAHPS scores was retrieved during quarter 3 of 2016 through quarter 2, April to June of 2017
One of the quality metrics that the nursing leaders sought to improve was whether bedside report may improve the patient fall rate Baseline data was obtained on all patient falls with or without injury from the Informatics Nurse during the time period of March to May 2016 Data was also collected using the patient event reporting system The patient event reporting system is a database in which events such as falls, medication errors, as well as other safety events are stored Patient falls between June to September 2016 were examined as postimplementation data
In addition, baseline data on the number of medication errors related to nursing practice was collected four months pre and post implementation This data was also retrieved from the patient event reports
Implementation
During the unfreezing stage, the nurses were invited to take online surveys that assessed their current attitudes about bedside report (Appendix A) The Clinical Patient Experience Manager rounded on the units to review the barriers and benefits of bedside report Barriers included anxiety, fear, privacy, length of report time, feelings of being talked over were identified and addressed The benefits of report were explained during the in-services to raise awareness of the change Unit champions were recruited on the units to promote change Journal articles were available to all staff on the online hospital education center to further raise awareness of the need for change
During the moving stage, the Clinical Patient Experience Manager began training RNs on bedside report throughout June of 2016 The training included explaining methods to standardize the practice of bedside report In-services and interactive demonstrations of bedside report were conducted on the units Staff nurses were instructed to utilize the white boards in patient rooms as communication tools White boards were to be updated during handoff report Nurses were given a handout and a laminated card as a reminder of what to include in bedside report The laminated card contained the I-SHAPED (Introduce, Situation-Current Issue, History, Assessment, Plan, Error Prevention, and Dialogue) acronym (Appendix F) A video was created as a tool for learning and posted on the hospital intranet
During the re-freezing stage, unit managers promoted and encouraged nurses to perform bedside report as instructed to maintain consistency in practice Also, the clinical patient experience manager involved the unit leaders in monitoring compliance with the new practice The unit leaders were “secret shoppers” observed the nurses during shift change The Clinical Patient Experience Manager monitored and documented “yes” or “no” on a log
When assessing medication errors related to nursing practice, it was found that there was a 50% decrease in medication errors post implementation (Appendix D)
The average fall rate per 1,000 patient days preintervention was increasing (Appendix C) Postimplementation, there was a spike in June, but then a steady decline for July, August, and September across all data points HCAHPS scores were also impacted by
the bedside report process The percentile increased in the following areas: overall score, RN communication, care transitions, discharge information across all data points (Appendix E) Patient experiences regarding their stay at the hospital overall was found to be more positive in the months after implementation, from 60 2% initially preimplementation to 66 4% or above in the quarters post-implementation
Key drivers influence the overall rating score NRC Picker key driver questions have the highest correlation toward the overall score One of the key drivers is nurse’s ability to listen to patients, which is a component of communication Again, improvement was noted in RN communication across all data points (Appendix E)
The care transition dimension assessing the hospital staff preparing patients for discharge, improved from 45 6% at or above 48 8% Furthermore, the survey asked questions to gauge patients’ perception of discharge teaching involving knowledge of caring for oneself at home, including how to take medications, and signs and symptoms to report to doctor, and when to seek additional treatment for an emergency The dimension of discharge teaching was stronger in subsequent months after the project was launched 78 9% to 84 7% or above
In conclusion, the handoff process showed improvement in all surveyed questions after bedside report was reintroduced
Discussion
Compliance with bedside report increased throughout the hospital following this quality improvement project Our HCAHPS scores improved in the following Patient satisfaction percentile responses improved for RN communication, care transition, discharge information, and the overall score The average fall rate per 1,000 patient days decreased and total medication errors also decreased post implementation The nurses’ perception of the handoff process showed improvement in communication, nurse accountability, and patient involvement via the survey monkey survey In addition, RNs reported a decrease in stress and in handoff communication in a reasonable amount of time (Appendix B)
Overall, higher HCAHPS scores, reduction in medication errors, and patient falls post-implementation, may be attributed to enhanced communication among staff and patients related to the practice of bedside report There are factors to be considered that impacted these results First, the staff nurses were educated on the evidence that supports bedside report Second, benefits and barriers were discussed as well as how they can affect HCAHPS scores Third, the ISHAPED acronym was used to standardize what should be included in bedside report Finally, the support of the CNO and nursing leaders set the expectation of the rollout, and the monitoring after the education was done to ensure standardization
The intended outcome of the project was to standardize the practice of bedside report hospital-wide Nursing leaders observed both positive and negative challenges of the change The important benefit achieved from the quality improvement project was improved communication among nurses, patients and families, and other team members Effective communication is the key to patient safety, patient satisfaction, and nurse satisfaction
The results of the nursing handoff survey indicate that staff nurses have reaped the benefits of bedside report Nurse perception of time management improved; when nurses attended to patients immediately, they are able to address concerns promptly Increased consistency of performing report at the bedside after education and monitoring may have contributed to nurses’ perception that bedside report is less stressful and does not take as long as they once perceived Patients reported to the patient experience manager that they felt comfortable seeing the two nurses together, hearing the exchange of information, and having the opportunity to participate if desired The managers, who rounded on units other than their own, reported to the Clinical Patient Experience Manager their individual observations of compliance with the practice change Overall, nursing managers felt that the practice of bedside report was being performed more consistently than before the project began
Conclusion
Improving patient safety and quality outcomes are a top priority for healthcare organizations There is a direct correlation with HCAHPS scores and quality outcomes (Studer et al , 2010) Therefore, the metrics included in the survey are compensated for, and are likely to achieve maximum reimbursement Improvement was achieved in patient satisfaction, reduction of falls, and medication errors post implementation of this project Applying Lewin’s theory of change as a framework improved the consistency of the handoff report process throughout the organization, encouraged patient centered care, and enhanced communication between nurses and patients
References available upon request
Appendix A
Hand-Off/Report Processes
Report/Hand Off Communication Employee Survey
Thank you for taking the time to fill out this survey, there are only seven questions and it should only take you about two minutes to complete This information will help us understand your perception of report/hand off communication process
1 Report is an effective means of communication
Strongly Agree
Agree
Disagree
Strongly Disagree
2 Report is an efficient means of communication
Strongly Agree
Agree
Disagree
Strongly Disagree
3 Report is relatively stress free
Strongly Agree
Agree
Disagree
Strongly Disagree
4 Report helps prevent delays in patient care
Strongly Agree
Agree
Disagree
Strongly Disagree
5 Report is completed in a reasonable amount of time
Strongly Agree
Agree
Disagree
Strongly Disagree
6 Report ensures accountability
Strongly Agree
Agree
Disagree
Strongly Disagree
7 Report promotes patient involvement in care
Strongly Agree
Agree
Disagree
Strongly Disagree
Appendix B
Percentage RN Perception of the Handoff Process

Appendix C Fall Rate per 1,000 Patient Days
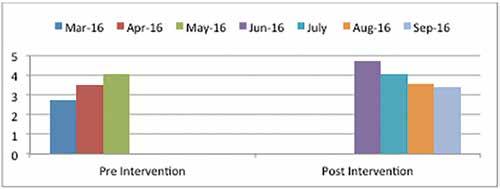
Appendix D Medication errors pre and post implementation
Appendix E
HCAHPS Scores Pre and Post Intervention
Nursing Perspective PreIntervention Q2 2016 (Apr-June) Intervention Q3
Sept) 2016
Continued Education Offering continued on page 18
By Christine Herman – Side Effects Public Media
Health care workers and first responders face serious risks dealing with people who have COVID-19 Bryce and Brittanny Budimir, a married couple in Kankakee, Illinois, both work on the front lines of the pandemic
Because of the risks they face in their jobs, the Budimirs decided in mid-March to send their three young children to live with their grandparents They spoke with reporter Christine Herman about that decision and the other ways the COVID-19 crisis has affected their family
The following transcript has been lightly edited and condensed for clarity.
Bryce: My name is Bryce Budimir I'm a paramedic firefighter
Brittanny: My name is Brittany Budimir, and I have been an emergency room nurse for the last three years
Bryce: Most of the 911 calls we’re getting are still your typical emergency medical calls But we are taking precautions, assuming everybody could have COVID-19 We wear N95 masks, and we bring in surgical masks for the patient and family, no matter what the call is
Brittanny: I'd say for over a month now we've been seeing patients with COVID-19 symptoms The consensus seems to be that we've been seeing this since January, we just didn't know what it was

CREDIT COURTESY OF BRITTANNY BUDIMIR
It definitely is anxiety-provoking You know, I've heard a lot of nurses say, ‘Well, we didn't sign up for this ’ But we did sign up for this, and that's why we all continue to show up because we love our patients
The problem we're seeing with this virus is that patients are showing minor symptoms and are absolutely okay to discharge, and then suddenly people are progressing and worsening We've had lots of patients have cardiac arrest, when they were fine just an hour ago
One of the hardest things is that when you see these patients are crashing, trying to stop yourself from just running into the room without any kind of gear on It’s extremely heartbreaking You have to make sure that you're covered
There have been several times where, you know, if we can just get a mask and goggles on, we’ve got to go because these patients are dying very quickly It's been a completely new experience for us

I had a patient that I sat with as he died, because the families can't come into the hospital That has been extremely hard, because nobody should ever have to die alone And we will always make sure no one ever dies alone We will always be there with them
We started seeing these really extreme cases, and since my husband is a firefighter paramedic and I'm an emergency room nurse, we are both around it and we both can't take time off So we decided to have our three children go live at my parents’ house
Bryce: Knowing what Brittanny has seen, what she's dealing with, you know, that helped me decide to agree with her, to have the children go over and stay at her parents’ house for the time being
It was a hard decision But they understood what was going on They know what Brittanny and I do for our jobs Especially our oldest, who's 11, he does understand
Brittanny: Our middle child is eight and our youngest is only a year and a half So he's the only one who doesn't understand

CREDIT COURTESY OF
Bryce: We text back and forth, video chat with them a couple times a week We see if they need anything We drop stuff off, and if they come outside, we stay away from them, you know, no hugs, no kisses, anything like that
But, you know, they'll show us some stuff that they've been doing at their grandparents' house, making forts and driving tractors around
Our youngest, Tyler, doesn't understand why mom and dad can't pick him up, and why after 10 or 15 minutes, you know, we blow him kisses and we get in the car and leave
Brittanny: It's been extremely hard My children are pretty much everything in the world to me
Bryce: It's so quiet in our house, you could hear a pin drop It's so strange
What I'm looking forward to most is having the kids back in the house, having them yelling and screaming, toys all over the place, having them in the backyard jumping on the trampoline, you know, just being able to be their dad and hold them and hug them
I just want the kids to know that mom and dad love them, that we're doing this for their best interests and that this is all going to be over soon
And nothing like this, hopefully, will ever happen again
I can't wait to hold them again
This story was produced by Side Effects Public Media, a news collaborative covering public health. Follow Christine on Twitter: @CTHerman

Achieve your goals with a leader in nursing education and receive special tuition savings.
You have the drive to pursue your passion and make a difference in the field of nursing We have the support and the innovative learning platform you need to make it happen
As an ANA-Illinois, you may be eligible to receive a 10% tuition reduction when you advance your education with Walden * Visit WaldenU.edu/ANA-Illinois to learn more.
Experience the Walden Difference:
• Coursework grounded in actionable learning and transferable skills
• 80+ degree programs including CCNE-accredited Bachelor of Science in Nursing RN-BSN Completion and Doctor of Nursing Practice (DNP) programs
• Multiple start dates to fit your schedule
• A global professional network of peers ready to support you
Achieve your goals and advance your career with Walden University
Learn more: WaldenU edu/ANA-Illinois | 1-855-628-1499
*A 10% tuition reduction is available to eligible members ANA-Illinois. The Family Nurse Practitioner specialization in the MSN program is excluded from this tuition reduction. No tuition reduction will be made retroactively. Tuition reductions are applicable to tuition only and do not apply toward books, materials, and other supplies or fees needed for a course.
Walden may change the tuition reduction offered hereunder at any time, but such change will not affect the tuition reduction for students who are currently enrolled at Walden and using the existing tuition reduction. All tuition reductions, grants, or scholarships are subject to specific eligibility requirements. Contact a Walden University enrollment advisor for details.
The baccalaureate degree program in nursing (BSN), master’s degree program in nursing (MSN), and Doctor of Nursing Practice (DNP) program at Walden University are accredited by the Commission on Collegiate Nursing Education (http://www. ccneaccreditation.org).
Sharon Pearce, MSN, CRNA
Ask yourself- who is always the most prepared for an emergency in a health care setting? Is it a nurse? I am sure your answer is yes Ask yourself- who designs policy about healthcare? Is it a nurse? I am sure your answer is no Ask yourself- who always implements healthcare policy designed by someone else? Is it a nurse? I am sure your answer is yes
It needs to change and change now! How do we change it? Nurses need to run for elected office!
I had the opportunity to interview Bethany Hall-Long, RN, PhD, the current Lieutenant Governor of Delaware, and the first nurse in the country to serve in that office Also, she will become the Chair of the National Lieutenant Governors Association in July Again, the first nurse to serve in this capacity! She shared that it is vital to have the “calming voice” of nursing in the policymaking world and, most notably, in light of the current Covid-19 crisis

As in the case of most nurses, the idea of becoming involved in politics had never entered Bethany’s mind While taking a policy course at the Medical University of South Carolina in her graduate studies, she was late to class As we all know, you can be volunteered quickly for a task when you are not there To her surprise, “Policy and Politics” was written on the board with her name beside it Her first thought was, “Oh, no! Why would nurses want to be involved in politics?” She admits, it changed her life
“What is the No. 1 profession that people trust? Nurses. So, when I campaign, I don’t introduce myself as a politician. I’m a nurse.”
-Bethany Hall-Long, Lt. Governor of Delaware
Bethany learned during that experience how clinical skills that a nurse has can translate into population health Opportunities arise by being at the table formulating policy or by serving in elected office and making decisions about health policy It shocked her to see how few nurses were serving in elected office and how few nurses were at the table when healthcare decisions were made Alternatively, the few nurses that were present were making monumental differences leading huge efforts that affected many patient’s lives
Through these experiences, Bethany decided to quit being a spectator and to join the arena She ran for the Delaware House of Representatives unsuccessfully Not one to accept defeat, she returned the next election cycle to win She encourages nurses to not give up if defeated in an initial run
She goes on to share why nurses should be making policy Nurses need to be proactive, not reactive because, as nurses, we know the issues Additionally, nurses are good listeners, decisionmakers, communicators, and advocates Furthermore, the nation is relying on nurses and need our expertise This is even more apparent today in the COVID crisis She continues saying, “who better to determine the quality of care than nurses?”
What are the risks of nurses not being involved? It affects patients, and most everyone will be a patient at some point Nurses are driven in large part by their hearts, but we must be driven by our heads also American voters today are driven by the “heart, the head, and the pocketbook ” Nurses have an understanding, whereas policymakers, by and large, do not understand healthcare unless it is through their own lived experience The lack of knowledge that policymakers and politicians have encompasses what nurses do and what they are capable of doing Ultimately, if nurses are not at the table, they are going to be left behind If nurses do not speak for themselves, someone else will speak for them
Who will speak for nurses? Physicians, hospital administrators, or federal system administrators, for example, who may or may not speak effectively on behalf of nursing Bethany says that as nursing science evolves with advanced education, such as the Doctorate of Nursing Practice, the profession needs to be distinct from medicine and other providers Again, nursing needs a seat at the table
How can nurses gain a louder voice? Run for elected office Long says nurses “need to be involved ” Nurses are excellent campaigners because they know how to connect with people and are the number one most trusted profession To illustrate, Hall-Long shared that during door to door campaigning, she was frequently invited into homes to look at rashes, or to discuss other health issues after learning she was a nurse
Long encourages nurses to take any frustrations they may have with healthcare or the profession and put it into action “Be the positive change” because nurses have the skills and ability to do so Nurses have the “perfect” skillset to listen, analyze, and prioritize, but more importantly, they will do what is right based on the data and not necessarily what is popular Nurses can see the big picture
Long says, “Nurses are educated for the political journey ” Will you take that journey? If you would like to listen to Bethany Hall-Long go to: https:// beyondthemaskpodcast com/ep-66-nursing-public-policy-why-nurses-need-to-beinvolved-with-lt-governor-of-delaware/2353/
Reprinted with permission from the Texas Nurses Association
By Amy McCarthy MSN, RNC-MNN, NE-BC Secretary, Texas Nurses Association
COVID-19 has forced nursing to enter the world of unknowns A world of unprecedented change where the rules are modified several times a day and new research is presented on almost a daily basis We can no longer look to years of solid data or examples of similar experiences to guide us in our clinical practice We are creating practices as we go along and what we did yesterday, may not work today
While our colleagues in the tech industry may see this as business as usual, what many don’t understand is that this level of change and disruption is not commonplace in nursing For instance, the practice changes in emergency departments are happening within days, when they typically would take months to implement before COVID-19
Reaching for Innovation
Over the past few years, I began to see nursing embrace the word innovation and nurses become more comfortable with seeing themselves as change agents While nurses are some of the most innovative people within health care, they sometimes fail to see themselves in that light
Change can make many nurses uncomfortable as it signals a shift in the way “it’s always been done ” The status quo also represented safe, reliable patient care
Why would we want to change something that was safe and reliable? While the answer to that is multi-faceted, the simple answer is this: It could be better.
It could be more convenient More reliable Safer It could be advanced in such a way that helps to remove the social determinants of health and brings care directly to the patient when they need it most It could be less invasive Less expensive
Beyond patient care, it could also relieve health care workers of some of the burdens they have carried for years and help to decrease the rates of burnout and suicide within these professions
So how do we begin this journey of reformation in health care? It starts by changing the lens we use to view the unknown and consciously engaging in it When we look at the unknown as something that can’t be tackled, we instantly become our own barrier We become so focused on holding on to what used to be and grieving the loss of what we had, that we fail to see the possibilities and silver linings this new unknown could provide
COVID-19 has certainly caused an overwhelming amount of grief and destruction worldwide It’s important that we take time to process through emotions, turn to others for support and remind ourselves that we aren’t alone All of us will process this event differently – what’s important it to take the time to do so and give ourselves grace throughout
Yet what it has also done is shine a giant spotlight on the gaps in our health care systems It has shown the world the reality nurses and other health care workers live every day And as the dust begins to settle, we will have two choices: return to the familiar or help pave the way for a system that takes better care of its patients and those working within it
Will it be messy? Yes Will we fail at times? It’s inevitable
Despite this, there is the potential of creating a health care system that fully embraces creativity and disruptive innovation and eliminates the red tape that has been associated with the change process Evidence will always have a place in informing change, but we can now see that hesitation and delays can also diminish outcomes (read how evidence-based PPE reuse is protecting nurses during COVID-19)
With the increasing use of telehealth, we have the ability to remove barriers to care and offer services to those in areas that have struggled for decades to establish centers for care We also have seen how removing restrictions on practice have allowed health care providers to work within their communities and travel across the country to render aid where it was most needed
As our world begins the complex task of emerging from this pandemic, it will be important for health care workers to help take the lead in this work In order for us to do so, we must embrace the uncertainty, accept that we may not always be experts and boldly move forward Rebuilding our programs will be no easy feat, but neither is saving lives We owe it to ourselves, our patients and our communities to create a healthier system of care for generations to come

Will the nursing conferences and meetings typically held in the fall of each year be happening this year? Will universities and colleges of nursing be able to open in September? These and many other questions are being asked across the State The answer is, ‘we do not know ' Governor Pritzker, on May 5th, began to answer these and all questions about getting back to our normal lives, with the economy, with social and educational gatherings, and with our freedom to move 'out and about ' The plan establishes a five-phase regional process to open the State Nursing agrees with the Governor that we must follow a safe and deliberate path forward based on scientific data
Key is to a ‘Restored Illinois’ is a five-phased in plan with health metrics, business, education, and recreational activities characterized in each phase From Rapid Spread to Illinois Restored allows for reopening of each of the four regions, adopted from the IDPH’s eleven EMS systems
Each region can move forward toward fully reopening or move backward if health metrics indicate such There are five phases for each region to progress toward 'normalcy’:
PHASE ONE: RAPID SPREAD.
All regions have currently passed through this phase, which included stay-at-home and social distancing
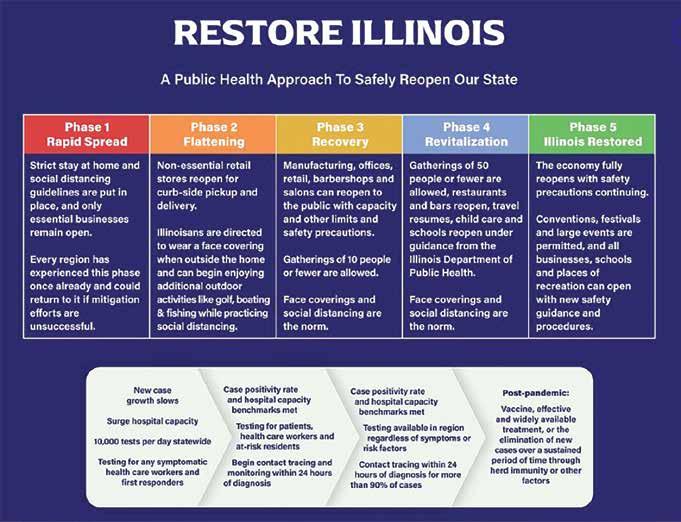
guidelines Only essential businesses could be opened No non-essential gatherings of more than 10 people are allowed Each region could return to this phase if health metrics show an increase of positive COVID testing and/or an increase in hospitalization and ICU beds for COVID-19
PHASE TWO: FLATTENING.
This is where the State started on May 1st Hospital beds and ICU census moved toward a flattening rate; non-essential businesses can open with curbside pick-up and delivery All are to wear a face mask when outside, some recreational activities may open with IDPH guidance while practicing social distancing No non-essential group meetings of 10 or fewer allowed
PHASE THREE: RECOVERY.
The rate of infection, hospitalizations, and the need for ventilators must show a downward trend Manufacturing, offices, retail, barbershops, and salons may reopen with capacity and other limits Gatherings limited to 10 or fewer allowed Face masks and social distancing are the norm
PHASE FOUR: REVITALIZATION.
Hospitalization, positive testing continue to decline Gatherings of 50 people or fewer are allowed Restaurants and bars reopen, travel resumes, child-care, and school may reopen under IDPH guidelines Face coverings and social distancing are the norm
PHASE FIVE: ILLINOIS RESTORED.
With a vaccine or a proven effective medical treatment available coupled with an elimination of new cases, the economy fully reopens Conventions, festivals, large group gatherings are permitted All schools open, all businesses open, places of recreation may fully open—all with safety guidance learned by this virus
Again, each region may progress forward once the announced benchmarks are met But, each region may go backward if there is an upward trend in hospitalizations and positive tests
While most are glad to have this road map in place, there are no clear-cut answers to all the questions Will conferences meet as planned? We just don’t know and have no way to predict the answer at this time Watch for announcements once decisions are made And, remember, for a state-wide meeting, there are people coming from throughout Illinois

The IDFPR home page https://idfpr.com/ has a direct link to the following
The State of Illinois Coronavirus Response Site with up to date information on how Illinois is handling the Coronavirus Disease 2019 (COVID-19) https:// coronavirus illinois gov/s/ Coronavirus Helps, Resources for Illinois Residents and Licensees Impacted by Coronavirus Disease 2019 (COVID-19) https://www idfpr com/COVID-19 asp
- Guidance for Healthcare Providers using Telehealth Services in Illinois
- Health Care License Reinstatement Application (LPN, APRN, RN, PA and RCP) -if your last active license was 2016 or more recent, application is one page, no fee, expires September 30, 2020)
- Out of State Temporary Practice Permit Application -this temporary permit application is two pages, no


fee, expires September 30, 2020
- Prescriber Guidelines During COVID-19 Emergency Declaration
- Guidance to Advanced Practice Registered Nurses Regarding COVID-19 there are additional guidelines in this section
Join the Fight Against Covid-19 This section also has COVID-19 applications for former nurses and out-ofstate nurses https://idfpr com/COVID-19%20HC asp
IDPH and local health department COVID-19 Resources https://coronavirus.illinois.gov/s/
In response to the COVID-19 pandemic, Gov JB Pritzker has ordered Illinois residents to stay at home Executive Order No 10 requires all residents to stay home, with exceptions for essential needs or business activities Gatherings of ten people or more are prohibited For guidance, testing questions, additional information or questions, please contact your local health department If your local health department is not available, please contact the IDPH Communicable Disease Section at 217- 782-2016 The IDPH after hours number 800-782-7860
If you are not currently receiving alerts from the State of Illinois Rapid Electronic Notification (SIREN), you can complete the self-registration at https://www siren illinois gov/ to receive importation future notifications from the Illinois Department of Public Health If you need assistance completing the registration process, please contact dph siren@illinois gov
COVID-19 Call for Support: In the COVID-19 event, Illinois is looking for medically trained individuals to join the fight Individuals that register here may be potentially
contacted to work in a hospital surge or alternative housing setting https://www illinoishelps net/
What if I don’t have a medical background but want to volunteer during COVID-19? The website www serve illinois gov is the state’s Commission on Volunteerism and Community Service, Serve Illinois There will be consistently updated opportunities to volunteer that are received by the state At this time, we only intend to activate medical professionals through the Illinois Helps system, but anyone can register in the system for future opportunities Please remember the most important thing we can do to stop the spread of COVID-19 is to stay home and practice good social distancing
To print your license or download an electronic copy to your phone: use the icon under the blue, middle of the IDFPR homepage www idfpr com
Address update: Please note that all IDFPR correspondence are now delivered electronically, including renewal reminders (in lieu of the paper postcard sent by U S Mail) Licensees are strongly encouraged to visit IDFPR’s online address change webpage (https:// www idfpr com/applications/LicenseReprint/ ) to provide a current email address and ensure contact information is up-to-date and accurate
Name change: Change of name CANNOT be completed via this online process If your name has changed, you must submit a written notice to the Department and include documentation of the name change (marriage license, court order, or divorce decree) For a copy of the written notice, please use this link https://www idfpr com/Forms/DPR/DPRCOAnamechange pdf
If you have questions, assistance is available Monday through Friday by contacting the IDFPR call center at 1-800-560-6420, or by email at FPR PRFGROUP09@ illinois gov
Jalen Benson, MS1 (Founder and Director, Harvard Medical School), Julia Walczak, BSN4 (National Nursing Coordinator, Benedictine University)
networks at their disposal Furthermore, nursing students have more skills earlier in training and are often better connected to the day-to-day needs of hospitals and patients

One of many NSRN volunteers assisting in the dissemination of PPE to hospitals in need in the Maryland, Virginia area.
As COVID-19 continues to spread across the US, hospitals and public health departments are faced with continual challenges in their responses Namely, critical staff and PPE shortages threaten to derail the efforts of healthcare workers Some states like Maryland and California have begun to call on nursing, medical, and physician assistant students to join state health corps and support healthcare systems While academic medical centers have access to robust student networks to support their systems in a variety of ways, many hospitals around the nation lack these resources Moreover, after the virtualization of training programs, students themselves are spread around the nation, away from their institutions, eager to help but uncertain how or where to best provide aid Nursing programs and students are especially well positioned to provide aid and support their local hospitals and communities as nursing schools are located in both large and small cities, unlike medical schools, which are often found in larger cities with greater support
The National Student Response Network (NSRN) aims to field the volunteer needs of hospitals, public health departments, and support organizations and match them with nearby health professions students These thousands of displaced health professions students are an excellent resource for their communities NSRN is mobilizing our growing network of students in a way that is both impactful and appropriate; to connect eager and capable volunteers with organizations in need of assistance
We support all students in our network in volunteering only in manners that align with their personal health and safety The vast majority of volunteer position requests will likely involve no patient contact While the institutions in need will ultimately outline student volunteering roles, we've come up with a few potential roles that health professions students might be qualified to fulfill, including calling patients with COVID-19 lab results or offering childcare for busy healthcare providers Roles available for health professions students may vary based on a multitude of factors, including educational and clinical experience Still, these differentiations will be left to institutions' discretion in describing the role needed to be filled
Our model for providing aid is intentionally flexible and meant to be a reflection of what hospitals, health departments, and other community organizations need as these needs arise
Students are stepping up to support healthcare systems in ways that national and state leaders are not If you are a student that wants to join a hospital that needs help or an organization that needs volunteers, please contact us at nsrnhealth org
By Susana Gonzalez MHA, MSN, RN, CNML
Past-President - National Association of Hispanic Nurses-Illinois Board Member - National Association of Hispanic Nurses Board MemberAmerican Nurses Association-Illinois

On July 3, 2019, NAHN-Illinois launched its Inaugural Mentorship Program with a vision to continue to champion Chicagoland’s future nurse leaders The program offered a formal curriculum that facilitated personal and professional growth while building fellowship among participants The mentorship program was interactive and included a leadership workshop with guest speaker, and executive leadership coach, Angel Gomez; a Leadership Panel with Gloria E Barrera, Susana Gonzalez, and Sonia Esparza to discuss leadership on the unit versus in the community; and a complete toolkit with tips on fostering an effective mentor/mentee relationship to promote active participation and for each to remain engaged Anna Lozoya and Nancy Ramirez spearheaded the program as the NAHN-Illinois Mentorship Co-chairs and worked hard to make it a success The overall feedback has been positive We're proud of our inaugural cohort and look forward to welcoming our new cohort this summer To learn more about NAHN-Illinois, visit nahnillinois org

She does all this to keep us safe Once she is clean from work duty, we are so happy to get lots of hugs, kisses and snuggle holds

My name is MAYA; I am a two-year-old Yorkie rescue I had a lovely owner, but she had some surgeries, and with a long recovery, she couldn't take care of me anymore She tried hard to find me a home, and I got lucky when she called two sisters that knew my mom Ellena and Titi Sussie and loved dogs Two sisters who have rescued other doggies and didn’t mind rescuing and adopting me as well So, I am excited to be a new member of this lovely family My Titi Sussie says I am cute and a wild thing However, they can’t help but love me

I feel blessed to have two moms They are sisters who work hard, love me, and take good care of me and the other rescues in the family I am glad I am not an only-doggie
My mom works in an office, and most recently, after a trip when she returned home, she needed to self-quarantine somewhere else away from home
It was my Titi Sussie who submitted my pictures as a supportive pet As a LATINA Style magazine reader, when she saw the request for pets who heal and support their owners, she sent my profile for consideration I am what she calls a supportive and therapeutic dog I woo her with my smiles, and I snuggle really close Well, let me tell you how I am therapeutic and how I am her healer I am just like my favorite Titi Sussie, who is a Registered Nurse, and she has been hard at work during the current COVID19 pandemic I am present when Titi Sussie gets home, but I am not allowed to be petted or touched No hugging or kisses We must wait while she bathes quickly She takes all her clothes off, puts them in the basket, and goes straight into the shower with lots of soap and water to scrub the germs off

Typically when Titi Sussie returns home from work, she really needs her snuggles and loving stares from me to pet and massages me so she can be stress-free That's how I have become therapeutic for her I help her feel good after a hard day at work I like to give her my sweet little stare with my dressy wear, and it makes her smile!
Titi Sussie works at a wonderful home care agency in Chicago, and they take care of many elderly and disabled people in their homes Her other nurse Diana is also seeing new patients with COVID19 sent home to recover My Titi Sussie loves teaching the home care staff and making sure they are safe when they care for patients in their homes Safety and proper personal protected wear are necessary during these uncertain and very challenging times
These are tough times, especially for healthcare workers and many other first responders and frontlines workers So, I am glad I am a healer Call me MAYA, the therapeutic doggie owner healer That’s what you should call me
So please stay at home, stay safe and sound, and snuggle with doggies like me

We are all in this together Let's help heal our world This too, shall pass Love, MAYA






"I don't go out of my house, but you go into the exact situation we are told to avoid Thank you for all your bravery and kindness to the victims of this epidemic "
"A BIG THANK YOU to all of those who are serving others during this time you are brave, and you are kind and you are selfless We thank you!"
"Thank you all for what you've done to help and protect us I wish you all the best of luck and stay safe from COVID-19!"

Representative Lauren Underwood
"I want to thank all the doctors, nurses, policemen, teachers and everyone who is working at this time and serving us "
"Thank you for everything! It does not go unnoticed and is very appreciated!"
"I am really appreciating those who are risking themselves to help save the lives of people infected with COVID-19 It takes a lot of risks to continue to work as a doctor, nurse, or paramedic You take the risk to bring home COVID-19 but yet here you are helping us the citizens of the country trying our best to help you guys with all the things we could possibly do for you guys I wish the best of luck for every doctor, nurse, and paramedic out there taking the risks of a lifetime right now "
"Hi, I just wanted to thank you No matter who you are Thank you for risking your life in order to keep out county safe Thank you for doing what you are doing I will continue to stay home in order for things to go back to normal and to help this pandemic pass Once again thank you for all you have done "
"Thank you for risking your lives to protect ours! I appreciate you guys so much Thank you for caring and serving our communities Thank you for working together to try and help bring the best possible outcome Please stay safe!"
"I want to thank all the people still working, still going out each day, still facing this pandemic without hesitation in order to provide us with all the things we need to maintain a semi-normal existence in these strange times You are heroes whether you know it or not and you will go down in history as such You are brave for us while we stay home, and we are lucky to have you there for us; the majority of us people you do not even know Thank you for continuing to be who you are and do what you do We can never fully express our gratitude for the sacrifices you have all made for us You make humanity proud "
"Thank you for all you do every day You are continually thinking of others before yourselves and your families We are all grateful for the work that you do, today and every day!"

A successful conference was held by the Illinois Healthcare Action Coalition (IHAC) Public Health Nurse Leaders Workgroup on March 12, 2020 What a day! Dr Patti Scott, DNP, RN, PNP, NCSN, Consultant, Office of Primary Prevention, Tennessee Department of Health, presented the keynote address: Bedside to boardrooms and beyond: the value of partnerships Because of the partnerships of the planning committee and presenters, we were able to include everyone who signed up to attend as well as those who presented That may sound odd, but think back, March 12 was early in March, when employers were just initiating travel restrictions, employees beginning stay-at-home-work, local health departments were increasing disaster plans that had begun weeks before, and schools of nursing were canceling clinicals and transitioning students to hybrid classes Our host, McKendree University in Lebanon, Illinois, welcomed us to the day-long event, and we had the foresight to schedule the keynote and morning sessions also to be broadcast via zoom In the 24 hours before the conference start time, we transitioned to the majority of registrants and some of the presenters attending via zoom and not in-person
The morning presentations included academicpractice pilot project presentations with Robin Hannon, MSN, RN as panel moderator Dr Melodie Rowbotham, SIUE presented on the breast-feeding friendly initiative, and Dr P Ann Solari-Twadell, Loyola University of Chicago, Niehoff School of Nursing presented with students about the nurse internship in primary care nursing, serving the underserved
The afternoon began with a panel discussion: Aligning to promote outcomes: building collaborative workforce development through academic/practice partnerships: panel discussion Presenters: Dr Jan Albers, McKendree University and Telligen grant PI, partners: Rhonda

L-R: Dr. Krista Jones, UIC-Champaign and planning committee; Dr. Patti Scott, keynote speaker; Dr. Jan Albers, McKendree University and planning committee; and Robin Hannon, MSN, RN, St. Clair County Health Department, RWJF grant PI and planning committee lead. As conference lead, Robin had a reserved parking spot – a first!!
Andrews-Ray, ED/Public Health Administrator Southern 7 Health Department; Angie Bailey, MPH, MS, Ed, CHES System Director for Community Health, Community Benefits, SIH, Southern Illinois Healthcare; Angie Charlet, DBA, MHA, RN, Illinois Critical Access Hospital Network and Linda B Roberts, MSN, RN, Illinois Nursing Workforce Center The partnerships were between Illinois Critical Access Hospitals and local county health departments in addition to McKendree University students – who received a scholarship
The day ended with Mark Peters, MS, Executive Director HEALTHIER TOGETHER, who presented on creating a culture of health in southwest Illinois through collective impact
The panels of nurse leaders and experts from partnerships in Illinois focused on lessons learned from successful and sustainable collaborations between local health departments or community agencies and schools of nursing and student nurses The presenters shared how they positively impacted deliverables for the agencies while the students gained experience in population health These projects were supported by mini-grants funded by the Robert Wood Johnson Foundation (RWJF)
In addition, with the generous support of the RWJF and the Illinois Nurses Foundation, the Public Health Nurse Leadership Workgroup was able to offer this workshop for a nominal fee of $10 00 per person Participants and presenters were able to explore innovative public and community health nursing academic-practice partnerships All participants received CE credits from ANCC

Our hosts, McKendree University, welcomed us at the Hettenhausen Center for the Arts, easy access, plenty of parking, catering, and an excellent IT team that partnered with the Illinois Nurses Foundation staff. This picture is L-R, Dr. Jan Albers, MSN Program Director, and Dr. Richelle Rennegarbe, Nursing Division Chair.

by Denise Remo-Nunez, MSN, RN
The year 2020 opened with unforeseen challenges for us Filipinos in healthcare January 13, 2020, saw the eruption of the Taal Volcano, spewing ashes up to nine miles in altitude, causing a public health threat throughout Calabarzon and the displacement of residents from nearby towns The fear over the Taal Volcano lasted until February 13, 2020 Before the country could completely recover from the Taal Volcano disaster, another disaster unraveled, this time internationally, that of the 2019 Novel Coronavirus, now known as Covid-19, now declared "a public health emergency of international concern " Despite these challenges, the Midwest's Philippine Nurses Association of Illinois (PNAI) started 2020, The Year of the Nurse, strongly In the midst of the Taal Volcano disaster, PNAI President-Elect Florence Palmaira, Vice President Marilou Dangalan, Treasurer Bessie Baldovino, and Past President Imelda Cuevo met with Sister Fidela Maamo, the founder of Our Lady of Peace Mission, and her staff, last January 30, 2020, to turn over the fundraising proceeds of Php 20,000 to their foundation Our Lady of Peace supports the medical needs of the indigent, especially the children, and are in constant need of medical equipment and supplies (Please reach out to us in the PNAI if you would like to donate to Our Lady of Peace Mission ) Also, in the Philippines, PNAI Immediate Past-President Alma Jaromahum served as a juror in the Oral Podium Research Presentation at the International Conference on Translational Research The two-day event, the theme of
which was “From Bench to Bedside: Improving Outcomes of Care of Surgical and Transplant Clients Through Translational and Quality Improvement Facilities” was held on January 22-23, 2020, at the Central Philippine University
Locally, on February 28, at Gibson’s Bar and Steakhouse, Otsuka Pharmaceuticals hosted the PNAI to a packed private interactive dinner presentation on the pathology, diagnosis, and prognosis of autosomal dominant polycystic kidney disease (ADPKD) We were graced with two experts, Dr Sachin Hajarnis, Ph D , Medical Liaison and a Chicago local, and Dr Sandra Chase, Phar D , Midwest Regional Director, from Otsuka Pharmaceuticals A total of 30 attendees came, members networked with nonmembers, and as with any dinner between healthcare professionals enthusiastically looking at cystic kidneys, the meals of steak, salmon, and pork chop was followed by rich and decadent chocolate cake over discourses around current healthcare trends, specifically the Covid-19 and different countries' responses to the outbreak and the heroism of nurses and other healthcare professionals They are once again at the forefront of yet another unknown deadly enemy
The dinner ended with a long list of volunteers for our future event, the diabetes and kidney screening outreach program, which we will be having on May 15, 2020 Our Midwest family, through hard work and dedication, will continue to work hard to realize the strong start that our leadership has done to set off this year dedicated to lifting up the nursing profession


PNA-ILLINOIS President-Elect Florence Palmaira, Vice President Marilou Dangalan, Treasurer Bessie Baldovino, Past President Imelda Cuevo, family members and friends met with Sister Eva Maamo the founder of Our Lady of Peace Mission and staff in Paranaque, Philippines





Nurses want to provide quality care for their patients.
The Nurses Political Action Committee (Nurses- PAC) makes sure Springfield gives them the resources to do that.
Help the Nurses-PAC, help YOU!
So. . . . . . . if you think nurses need more visibility if you think nurses united can speak more effectively in the political arena if you think involvement in the political process is every citizen’s responsibility.
Become a Nurses-PAC contributor TODAY!
❑ I wish to make my contribution via personal check (Make check payable to Nurses-PAC).
❑ I wish to make a monthly contribution to NursesPAC via my checking account. By signing this form, I authorize the charge of the specified amount payable to Nurses-PAC be withdrawn from my account on or after the 15th of each month. (PLEASE INCLUDE A VOIDED CHECK WITH FORM)
❑ I wish to make my monthly Nurses-PAC contribution via credit card. By signing this form, I authorize the charge of the specified contribution to Nurses-PAC on or after the 15th of each month.
❑ I wish to make my annual lump sum Nurses-PAC contribution via a credit or debit card. By signing this form, I authorize ANA-Illinois to charge the specified contribution to Nurses-PAC via a ONE TIME credit/debit card charge.

Your future starts now, so make the Year of the Nurse your year to inspire, grow, and celebrate! Throughout the year, we encourage you to seek opportunities and engage in activities to promote nursing excellence, infuse leadership, and foster innovation Below are suggestions for how you can excel, lead, and innovate EXCEL
Go beyond the ordinary in 2020 and make this the year you focus on your professional and personal development
• Find a mentor Is there a colleague, nurse friend, or former instructor who has useful insights to share or inspires you to be your best? Having a mentor who can help you navigate your career and offer advice could be the motivation you need to excel and advance your nursing career ANA also offers its members a Mentorship Program Enrollment for 2020-2021 will open in the summer
• Take your nursing to the next level. Do you want to build your leadership ability or improve your nursing practice? Webinars and online courses can help enhance your knowledge and give you the skills you need to succeed Sign up for the free webinars Ten Steps to Becoming a Successful Nursing Manager or What’s Happening in Nurse Staffing?
• Knowledge is power. Make 2020 your year for professional development Whether you are looking to achieve your first certification, explore new ones, or renew a certification, The American Nurses Credentialing Center Certification Program lets you demonstrate your specialized knowledge and continuing competence
• Make self-care a priority. Join the Healthy Nurse Health Nation Grand Challenge, an initiative to connect and engage nurses, employers, and organizations around improving health in five areas: physical activity, nutrition, rest, quality of life, and safety If you’re looking for an inspiring way to focus on your well-being in 2020, join the monthly challenges
• Give back to your community. Help promote the value of nursing by supporting a special health screening event in your community or volunteering at a health clinic Consider joining a local organization that supports something you are passionate about and could benefit from your insight as a health care professional
As a nurse you inspire, influence, and innovate — all leadership qualities In this Year of the Nurse, commit to elevating your voice to show the influence you have as the backbone of health care

• Inspire the next generation. Your outreach this year is critical to engaging with the next generation of nurses and increasing workforce diversity Visit elementary and middle schools, career fairs, community centers, and youth clubs to talk about your path to nursing and inspire future nurses
• Exercise leadership skills. Make this the year you learn more about how you can serve on a board of directors Start by visiting Nurses on Boards for resources and updates on nationwide board opportunities If you are already contributing to board leadership, inspire others to serve on boards by sharing your “bedside to boardroom” story
• Impact political change. In this critical election year, make a commitment to engage in political advocacy Visit RNAction to learn how you can ensure nurses’ voices are heard by politicians Learn more about candidates, priority issues, voter registration, and ways to volunteer on campaigns Share what you learn with your friends, family, and colleagues If you want to engage more in political advocacy, participate in your state or constituent nurses association’s Legislative Day and ANA’s Hill Day in June These annual events provide the opportunity for you to share your perspective as a nursing professional and gain elected officials’ support for crucial legislation
• Raise your voice with the media. Share your perspective about the value of nursing and nursing leadership with your local media Reach out to a reporter in your city who covers health issues to recommend they do a story about the “Year of the Nurse,” submit an editorial to your local newspaper, or send a letter to the editor commenting on recent coverage that would have benefited from the nursing perspective
• Elevate your profession. Look for opportunities to self-identify as a nurse Introduce yourself to patients, colleagues, and members of the community as “Nurse [Last Name] ” Include your RN credential on business cards, checks, credit cards, emails signatures, and more Take every opportunity to educate others about nursing and show pride in your profession
• Get social. Share a week of posts on your life as a nurse Give your social media followers a glimpse into all you do with highlights about your activities, colleagues, and nursing moments where you make a difference When making work-related posts, be attentive ANA’s Social Networking Principles #YON2020
• Inspire colleagues. Words of encouragement and random acts of kindness can make all the difference in a person’s day, especially for nurses Share inspirational messages or a handwritten

“words from a nurse” letter to give the support, encouragement, and motivation we all appreciate and occasionally need to brighten our day
• Celebrate the power of great nursing. Honor a nurse mentor, celebrate a nurse colleague, or thank a special caregiver, nurse friend, or family member with a contribution to the American Nurses Foundation in their name Your donation will support innovations to make care more patientcentered, financial aid to students in need, and programs that help nurses achieve better health
Nurses are natural problem-solvers and innovators Innovations occur at all levels of health care and nurses can and should be at the forefront, just like Florence Nightingale, the first nurse innovator
• Initiate an innovation program. Nearly 70 hospitals and health systems across the U S are recognized for their innovation programs If your organization has an innovation program, are there opportunities for you and your nurse colleagues to support it? If your organization does not have an innovation program, how can you start one that improves workflow, efficiency, and patient care?
• Join or host a hackathon. Champion nurse-led innovation by participating in or organizing a platform that encourages nurses to bring their ideas to life Live-action events such as pitch competitions or hackathons are fun ways to learn about innovation, design thinking, and even failure Check for corporate-sponsored events, or competitions at local nursing schools or your state nurses association
• Share your experience Are you a nurse innovator or aspiring visionary who wants to help build a culture of innovation? Consider sharing your ideas, thoughts, and advice in a blog post or writing an article for a nursing, health care industry, or nursing school publication
• Launch your idea. Do you have a nursing-led innovation you want to see through from concept to reality? Consider launching your idea at NursePitch™, a live, interactive event for nurses to compete for a chance to turn their innovation dreams into reality There is no time like now to start planning for the 2021 competition

As an academic institution that educates future healthcare leaders, Resurrection University Chicago (ResU) wanted to be proactive in educating former, current, and future nurses, as well as advanced practice nurses on the topic of COVID-19 during this critical time After hearing Governor Pritzker's call to action, leadership from Resurrection University sprung into action! "We wanted to provide education to promote the understanding of this novel viral infection," stated Dr Reem Azhari, Associate Professor and Endowed Chair of Interprofessional Education at ResU "We knew that nurses would be returning to the workforce and that many RNs and APRNs could have modifications from their current position based on the needs of their place of employment and current patient base," stated Dr Melissa Murphey, Assistant Dean of Graduate Nursing Drs Azhari and Murphey brainstormed with Dean Dr Connie Zak on how they could quickly develop an educational program for nurses throughout the state and beyond Their goal was to ensure that, once the participant completed these modules, they would understand not only how to safely care for themselves and their family; but, also how to best care for patients and their families who are affected by COVID-19
Leadership, including President Dr Therese Scanlan and Dean Zak, led the charge Dr Kristine Tohtz worked with graduate students on delivery and streamlining
content The modules include Prevention of Viral Illnesses in Alternative Medicine, Hygiene and CDC Recommendations, Basic Assessment and Telehealth of Suspected COVID-19 Patients, Pregnancy and Breastfeeding during COVID-19, Learning Strategies for COVID-19 Success from Other Countries, Support of COVID-19 Family Members, Counseling and End of Life Care, Crisis Intervention and Stress Management for Health Care Providers, and, Self Care for Healthcare Workers These modules are self-paced and can be completed via an online platform for 3 5 Continuing Education Units (CEU) to all registered and advanced practice nurses Our course of modules are titled "Nursing Readiness in the Face of COVID-19 " Our team of faculty and graduating nurse practitioner students worked to create these modules in a short time frame, releasing the content in just under two weeks Special thanks to our graduate nurse practitioner students who participated in this series of modules: Haley DeCero, Iyeokan Ativie, Camille Raz, Latura Stigall, Tracy Omorogieva, Irene Oh, Claudia Roldan, Stephanie Stanley, and Ana Romero We wish them the best as they prepare for their certification test and a new role as a nurse practitioner
To register for the complimentary 3 5 CEU modules, please visit https://www resu edu/ schoolofemergingeducation/

The World Health Assembly, the governing body of the World Health Organization, in honor of Florence Nightingale’s 200th birthday, declared 2020 the International “Year of the Nurse” and Midwife The National Black Nurses’ Day Committee decided to take part in this celebration by honoring Legendary Nurses and Nurse Midwives The program offered 1 CEU Alpha Eta chapter of Chi Eta Phi Sorority, Inc is the approved provider
The celebration was held on February 28, 2020 at Apostolic Faith Church where the Bishop Horace Smith is the Pastor National Black Nurse’ Day was proclaimed on February 3, 1989 to applaud black health care practitioners “February is the month we set aside to honor the contributions made by black Americans to this country,” therefore it is only fitting that black nurses be recognized and honored for their outstanding contributions to our community and country ” (Congressman Charles Rangel)

a collage of old negro spirituals songs such as “Swing Low, Sweet Chariot ” (1909 Fisk University Jubilee Singers of Fisk University), “God’s Gonna Trouble the Water ” (African American Spiritual from 1800)
Rev Evelyn Collier-Dixon, RN of the Chicago Chapter National Black Nurse’s Association delivered the Invocation Her message was on Faith
Dr Algean Garner of Apostolic Faith Ministry gives

a warm welcome and congratulatory remarks to The National Black Nurse’s Day Committee on its 32nd Annual Celebration Dr Garner shared with the audience some of the Legendary nurses of the past and their contributions to society and the profession of nursing



ourselves Dr Lawrence discussed the many obstacles she faced during her career and how through prayer and hard work she was able to succeed Dr Lawrence served as Director of Provident Hospital School of Nursing and was instrumental in getting the nursing program NLN accredited She later became the Director of Evangelic Hospital in Oaklawn and was again instrumental in getting their nursing program NLN accredited She was offered assistant nursing position with IDPR as Education Coordinator Dr Annie Lawrence spent twenty-one years at Governors State University where she was appointed Director of Health Sciences and later became the Chair, she retired in 1997 from Governors State University Dr Annie Lawrence-Brown worked in other educational leadership capacity during her forty-nine-year nursing career
The Legacy of Dr. Annie Lawrence-Brown

The National Black Nurse’ Day Committee decided to hold its celebration on the 4th Friday of February each year in order not to conflict with the National Celebration that is held in Washington, DC the first Friday of February Opening remarks were given by Adrianne Priester – Coary, President Alpha Eta Chapter of Chi Eta Phi Sorority, Inc ; Ethel L Walton, Vice President The Chicago Chapter National Black Nurse’ Association; Valerie Hubbard, President Beta Mu Chapter of Lambda Pi Alpha Sorority and Dr Sandra Webb- Booker on behalf of Louise Broadnax, President of Provident Hospital Nurses Alumni
Evangelist Shelia Tate set the tone for the evening by starting off with the Black National Anthem by James Weldon Johnson’s “Lift Every Voice and Sing ” The audience joined in and sang along with her She also did
If you are looking for a rewarding career opportunity and want to make a difference in the lives of others...
COME JOIN OUR TEAM! Nursing Opportunities Available RN - LPNs
PREFERENTIAL DEPARTMENTS:
Behavorial Health, Emergency Room, Medical Specialty Clinic and Home Health
Will assist with licensing from one state to another up to $500
We offer competitive compensation, a wide range of benefits to include health/dental/life insurance, paid time off (PTO), tuition reimbursement, employer match 401K plan & a GREAT work environment.
SUBMIT RESUMES TO: applytowork@touchette.org Or contact us at 618-332-5303

and Valerie Hubbard



Dr Lawrence gave the audience a historical view of what nursing was like in the Early Years She graduated from Freeman Hospital in Washington, DC in 1948 (now known as Howard University)

According to Dr Lawrence black nurses had their own organization called the Colored Nurses Association However, in 1948 when she graduated the American Nurses’ Association had started to open their membership to blacks and she was encouraged to apply by one of her nursing director, in which she did and was accepted She said that it is vital that we belong to our professional organizations in order to meet other nurses, to learn from other nurses and to become educated
“The most rewarding part of my nursing career is to be recognized as a mentor to so many men and women ” Dr Lawrence told the audience that in choosing the nursing profession you must go to school and continue to advance your education Her eyes lit up when she said that she saw many of her former students at the celebration and they had gone on to advance in education Dr Lawrence has had the opportunity to encourage people in all walks of life She not only provided encouragement but led by example Dr Lawrence holds two doctorate degrees one from the University of Sarasota and one from ISU She was one of the first blacks to be accepted in the 1940’s to DePaul University and obtained her bachelor and master’s degrees She proudly told the audience that when she graduated with her Master Degree , there were two other blacks that graduated with her and they were Betty Gross who worked as Director of nursing at Provident Hospital and Christine Allen who served as Director of Nursing at Malcolm X College “Can you believe three black nurses graduating from DePaul University at the same time " "My journey has not easy " She is indeed a living legend, a mentor, and an Icon


about
Is the Chief Executive Officer of Near North Health Service Corporation Under her leadership the health center has grown from one on the northside to nine comprehensive health centers, in addition to two women and children health centers Mrs Mills-Thomas focus was on Health Determinants and over all Public Health She discussed the fact that nurses have always understood that health and wellbeing are social determinants of health According to Mrs Mills that despite the implementation of the Affordable Care Act the number of uninsured is increasing instead of seeing a decrease Mrs Mills says that the time for action is now ” Black nurses should receive regular training regarding social determinant of health and that it should be taught in schools of nursing She listed and discussed some of the determinants of health such as employment or unemployment, working conditions food insecurities, lack of housing, education, health care primary, secondary and territory, social exclusion, social safety nets, gender, race, social class, disability, and sexual orientation Mrs
some of the provisions in the Affordable Care Act that promote the elimination of health disparities through impacting the social determinants of health (SDoH) health disparities pathway “Organizations should be sure to take advantage of these new opportunities to reduce health disparities through increased workforce diversity, improving the collection of data by race/ethnicity and languages, strengthening workforce diversity Enforcing cultural competence and organizational support, elevating, or establishing offices of minority health in various agencies, encouraging research in health disparity and development of strategies to reduce them, and addressing health disparities in insurance forms " Black nurses are in the best position to work and influence the people who trust and look like them "
The 32nd Annual National Black Nurses Day Celebration can be viewed on CAN TV or U Tube.
Submitted by Carolyn Rimmer- Owens, BSN-RN-C Public Relations Chair for NBND Committee For additional information please contact us at RNCCNBNA@gmail com

Dr. Beverly M Harper (Midwife), Dr. Annie Lawrence (Legendary Nurse), Bernice MillsThomas, MSM, MPH, MBA (Legendary Nurse), Rev. Dr. Shirley Fleming (Legendary Nurse and Midwife), Dr. Eva Smith (Legendary Nurse), Ruth Slauhter, BSN, MPH (Legendary Nurse), Charlene Sanders, BSN, MSN (Midwife) and Paula Manuel, BSN, MSN (Midwife) Ms Manuel award was accepted by a relative.


National Black Nurses Day Committee members: Carolyn Rimmer-Owens, Adrian Priester-Coary, Valerie Hubbard, Marilynn Parker, Ethel Walton, guest attendee, Louise Broadnax, Evelyn CollierDixon, Dr. Sandra Webb-Booker and Ronald Campbell. Not shown is Jacki Smith.


By: Fran LaMonica, M.S., Executive Director Chicago Bilingual Nurse Consortium
The COVID-19 pandemic has resulted in an acute nursing shortage throughout the country and the world We have been anticipating a significant nurse shortage
Esposito (2017) cites an American Nurses Association prediction that by 2024, "nearly 690,000 nurses will leave the labor force through retirement and other reasons, causing a nurse vacancy rate of an estimated 1 2 million," in the United States alone A report by the Migration Policy Institute (2017) states that nearly two million college-educated immigrants and refugees in the United States (are) unable to utilize their professional skills fully " Although not able to practice as registered nurses in Illinois yet, there are internationally educated nurses (IENs) who could be available to strengthen our healthcare workforce
Many of these internationally educated nurses desire to continue their professional practice in the United States and are working toward that goal They, however, face several barriers, including knowledge of the process, financial, difficulty getting credentials information from their countries (especially those experiencing political turmoil at this time), and misinformation provided by those seen as resources To compound the challenges internationally educated nurses (IENs) face, each State has its own rules for allowing them to become licensed
The Chicago Bilingual Nurse Consortium (CBNC), a 501 (c)(3) was established in 2002 to assist IENs to navigate the process of professional licensure and to prepare for the examinations required in Illinois CBNC teaches IENs about the requirements and coaches candidates through the process It also provides preparation courses geared toward the passage of the English Proficiency and NCLEX-RN examinations Working with professional organizations, the State Board of Nursing, and the Illinois Department of Finance and Professional Regulation, CBNC advocates for candidates as they seek to meet all requirements for licensure
In 2017, CBNC was invited to join a sub-committee geared toward, “Cutting Illinois Nurse Red Tape," as related to foreign nurses It in collaboration with several professional nursing organizations, CBNC presented suggestions for streamlining the process By comparing requirements across various States and recommending changes to the Illinois Nurse Practice Rules and Regulations, the group identified ways to make it easier for IENs without compromising the high standards Illinois appreciates Examples of the recommendations include the following
Rule 1300 300 requires candidates to have completed a total of 12 years primary and secondary education, and at least two years of nursing education that is comparable to education in the U S This is known as the ‘14 year rule ' In most countries, this is not a problem; however, the educational system in Eastern European countries initiates nursing education during the last year of high school Their nursing education program is for two years Therefore the total education often falls short of the total 14 years that Illinois requires In a review of State Boards in the U S , only 18% of the states have the 14year requirement States surrounding Illinois, including




Indiana, Iowa, Wisconsin, Michigan, and Missouri, require IENs to have only comparable nursing education programs Illinois has lost qualified IENs to these states
The CBNC recommendation is that Illinois rules and regulations change to considering equivalent nursing education as other states
Rule 1300 320 Licensure by Endorsement requires RN applicants educated outside of the U S must submit another credentials evaluation report although during the nurse’s licensure process in the other State, credentials evaluation was completed and nursing education was found equivalent to that in the U S This is costly to candidates and often delays processing for more than six months as the evaluation agencies need to receive new transcripts from the candidates' nursing schools
Not all States accept reports from the same agencies Illinois only accepts the Commission on Graduate of Foreign Nursing Schools (CGFNS) or Credentials Evaluation Services (CES) reports It should be noted that although the pre-requisite reports are different, the nurse licensure examination, NCLEX-RN is the same in all states The CBNC recommendation is that Illinois the requirements for a new credentials evaluation report be waived as related to endorsement of an RN who is already licensed in another state
Another requirement for endorsement is that if the candidate’s first language is not English, the applicant must provide certification of passage of either the Test of English as a Foreign Language (TOEFL) or the International English Language Testing System (IELTS) Some states do not have this requirement Recognizing that the NCLEXRN examination is written at a 9th to 11th-grade level, as is the English proficiency examinations, candidates who have passed the NCLEX-RN should be considered to be proficient in English CBNC, therefore, recommends that in cases of RNs seeking endorsement in Illinois, this rule be waived
The Nurse Practice Act Rules and Regulations are designed to safeguard patients and the profession Ensuring the safety and quality of patient care is essential to the State of Illinois as it is to every registered nurse Other states have this purpose in mind as they develop Rules and Regulations as well Logically reviewing the rules, especially in light of an impending nurse shortage, is needed Without sacrificing safety and quality, a serious review of barriers, as related to the licensure process of Internationally Educated Nurses, is required Streamlining the process for IENs helps Illinois patient care in the long term
References: Esposito, Lisa; “Immigrant Nurses: Filling the Next U S Nurse Shortage;” U S News and World Report Web; March 29, 2017 http//health usnews com
“What makes for Success? News Report Examines Initiatives that Help Highly Skilled Immigrants with Foreign-Earned Degrees Contribute More Fully to the U S Economy;” Migration Policy Institute Web February 28, 2017 http// www migrationpolicy org

Appendix F ISHAPED acronym
- Introduce/ask permission
- Situation-current issue
- History-relevant to current diagnosis
- A ssess-drains, pain, IV drips, incisions
- Plan-goals, test, procedures, d/c plans
- Error prevention-safety, fall risks, restraints, ETOH
- Dialogue-questions/answers involve patient
CE Offering: #2020-0353- Bedside Report and its Effects on Patients and Nurses
1 0 Contact Hour
This offering expires in 2 years: June 10, 2022
Learner Outcome:
Learners will demonstrate knowledge of a quality improvement initiative related to bedside reporting by passing a post-test with a score of 80%
HOW TO EARN
CONTINUING EDUCATION CREDIT
This course is 1.0 Contact Hour
1 Read the Continuing Education Article
2 Go to https://www surveymonkey com/ r/20200353BedsideReportSelfStudy to complete the test and evaluation This link is also available on the INF website www illinoisnurses foundation under programs
3 Submit payment online
4 After the test is graded, the CE certificate will be emailed to you
HARD COPY TEST MAY BE DOWNLOADED via the INF website www illinoisnurses foundation under programs
DEADLINE
TEST AND EVALUATION MUST BE COMPLETED BY June 1, 2022
Complete online payment of processing fee as follows:
ANA-Illinois members & Affiliates - $8 00 Nonmembers- $15 00
ACHIEVEMENT
To earn 1 0 contact hour of continuing education, you must achieve a score of 80% If you do not pass the test, you may take it again at no additional charge
Certificates indicating successful completion of this offering will be emailed to you
DISCLOSURE
There is no conflict of interest for anyone with the ability to control content of this activity
ACCREDITATION
This continuing professional development activity was approved by the Ohio Nurses Association, an accredited approver by the American Nurses Credentialing Center’s Commission on Accreditation (OBN-001-91)
CE quiz, evaluation, and payment are available online at https://www surveymonkey com/ r/20200353BedsideReportSelfStudy or via the INF website www illinoisnurses foundation under programs


IDFPR Extends Illinois RN and APRN CE Completion and License Renewal Deadline to September 30, 2020
In light of the challenges confronting all Illinoisans during the COVID-19 pandemic, the Illinois Department of Financial and Professional Regulation (IDFPR) has granted an automatic extension to complete continuing education requirements and to complete license renewal for all Illinois RN and APRNs The license renewal deadline is now September 30, 2020
To renew your Illinois RN and APRN license use the license renewal icon on the IDFPR home page https://idfpr com/ The icon is located on the far right under the blue section






After paying the renewal fee, please click the link and complete a 26-question survey. It only takes five minutes to complete.
Continuing education requirement FAQs for LPN, RN and APRNs are available on the Illinois Nursing Workforce Center (INWC) website http://nursing illinois gov/ NursingCE asp
There are new CE requirements for Illinois LPNs, RNs and APRNs beginning January 1, 2020:
1) All LPNs, RNs and APRNs shall complete a one-hour CE course in sexual harassment prevention training from a pre-approved provider
a) This one-hour of sexual harassment prevention training CE course is intended to fit into the licensee’s regular CE requirements For LPNs and RNs, one of the 20 hours of required CE must be a sexual harassment prevention training course For APRNs, one of the 80 hours of required CE must be a sexual harassment prevention training course
b) Additional information regarding this new requirement for license renewal in 2020 is available http://nursing illinois gov/PDF/201911_IDFPR_SexHarassPreventTraining_final pdf
2) Safe opioid prescribing practices Continuing Education (CE) requirement is in effect for all prescribers renewing in 2020 Prescribers with Controlled Substances Registrations are required to complete three hours of CE to renew their controlled Substances Registration This requirement can be included in the total number of hours required to renew a professional license https://www idfpr com/FAQ/DPR/Safe%20 Opioid%20RX%20CE%20FAQ pdf
General Continuing Education (CE) requirements for Illinois LPNs, RNs and APRNs are also available on the Illinois Nursing Workforce Center (INWC) website http:// nursing illinois gov/NursingCE asp














