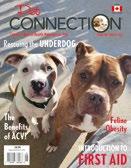
$4.95 Display until March 31, 2023 Made in Canada Proudly Canada’s Natural Health Magazine for Pets FEBRUARY-MARCH 2023 INTRODUCTION TO FIRST AID Feline Obesity Rescuing the UNDERDOG The Benefits of ACV!



2 FEBRUARYMARCH 2023 Proudly Made in Canada information@amorepetfoods.com 4540 Hastings Street, Burnaby, BC www.amorepetfoods.com
Food
& Dogs Since 2005 This Valentine’s Day, give the gift of good health. Add years to their life and life to their years.
We
We
START YOUR PUPPY OFF RIGHT! Real Food for Cats & Dogs
Real
for Cats
Amoré is the only Canadian company, that makes air dried raw food, on Susan’s list.
use human grade ingredients to make nutritionally dense, great tasting food.
feed the pickiest pets. Our processing ensures all the nutrition stays inside. Best thing, Little input = little output!



3 FEBRUARYMARCH 2023 Introduction to First Aid 8 by Dr. Roger Gfeller, Dr. Michael Thomas, Dr. Tony Johnson and Phyllis DeGioia The Many Benefits of 40 Apple Cider Vinegar! by Lucy Jabrayan Feline Obesity 42 by Anne Jablonski Rescuing the Underdog 48 by Kim Federico BONUS Treasure Hunt! 32-33 GETTING THE SCOOP ON CANADA’S PET CULTURE VOLUME 15 • ISSUE 6 • FEBRUARY - MARCH 2023 Inside: IN EVERY ISSUE Letter from the Publisher 4 Mark Your Calendars! 55 Cross Canada Dog Photo Contest 56 Cross Canada Cat Photo Contest 58 Blue Boon Cover Photo: Waylon and Angus, Chilliwack, BC Photo Courtesy of Malone Smith
PUBLISHER
Leslie Kennedy
Tel: 604.220.5346 info@petconnection.ca www.petconnection.ca
GRAPHIC DESIGN
Britton Design Services
CONTRIBUTORS
Phyllis DeGioia
Kim Federico
Dr. Roger W. Gfeller, DVM Anne Jablonski
Lucy Jabrayan
Dr. Michael W. Thomas, DVM
Pet Connection is published 6 times a year. Founded in 2008.

SUBSCRIPTIONS
To subscribe to the Pet Connection, please send $25.00 for a one year subscription. (6 issues). Single copies are available for $4.95 each. All taxes included. Either order online from our website, or mail a cheque or money order with your name, address and postal code to:
Pet Connection 2443 Beacon Avenue Sidney, BC V8L 1X7 Pet Connection does not disclose its subscribers list to anyone.
PET CONNECTION does not assume responsibility for any claims made by its advertisers, or for any information dispensed. The articles and information presented are for information only and do not necessarily reflect the views of the Publisher. Permission to reproduce any part of this publication must be approved by the publisher. All pictures, articles or emails sent in become the property of Pet Connection.
All Rights Reserved
©2023 - PET CONNECTION
Pet Connection is located on the traditional territories of the WSÁNEĆ People, on whose traditional territories, we live and work.
Stay Connected!
We have a lot going on this year - for you our readers.
If you are on Social Media please like, share and follow us on both Instagram and Facebook.
If you are not on Social Media, please stay connected with us on our website or by email, mail, or phone.
We love hearing from our readers and enjoy your stories, letters, cards, and connections. Thank you to everyone who reaches out.
Congratulations to Waylon and Angus for winning the 2022 Dog Photo Contest! They look amazing gracing this cover. We are grateful to the thousands of entries we have received, and good news - the contest is running again this year. Details inside.
We actually have 3 Contests going on this year. The Cat Photo Contest, the Dog Photo Contest and this year we brought back our Treasure Hunt! We are so very grateful for all the Sponsors stepping up and partnering with us to make it all possible again for another year.
Good Luck to everyone who enters, and may 2023 be a year of good health, fun times and more amazing connections.
- Leslie Kennedy Publisher
- Unknown
4 FEBRUARYMARCH 2023
OUR MISSION: To save innocent companion animals from any type of harm.
“He is your friend, your partner, your defender, your dog. You are his life, his love, his leader.
He will be yours, faithful and true, to the last beat of his heart. You owe it to him to be worthy of such devotion.”
PEFC
Letter from the Publisher











5 FEBRUARYMARCH 2023
Contributors
Phyllis DeGioia, Veterinary Partner Editor, Phyllis DeGioia, who passes out at the sight of blood (she can't even watch needles pierce skin on TV) and thus could not be a veterinarian, is the editor of Veterinary Partner and VetzInsight, VIN's client education blog. She also uses her highly scientific degree in English from UC Irvine to write for the VIN News Service. Over the years she has written and edited material for numerous pet-related companies and client education material for VIN. Phyllis fields panicky "What do I do?" phone calls from friends with the same practical response: "I think you should go to the vet."
Kim Federico, Director of Foster and Family Placement for HugABull, passionately leads the dog program. Kim manages all of the dogs that come through HugABull, helping them transition from the shelter into foster care, ultimately finding them their happily ever after. Kim has 2 bullies of her own and spends her free time exploring the outdoors with her dogs. www.hugabull.com


Dr. Roger W. Gfeller, DVM, Dr. Gfeller was a leading and long-standing veterinary emergency practician in Fresno, California. He died in an automobile accident in 2007, and the update to this collection was done as a memorial to him. A 1973 graduate of Kansas State University School of Veterinary Medicine, Dr. Gfeller was practicing emergency medicine nearly as long as anyone in the country and had been a Board Certified Diplomate of the American College of Veterinary Emergency and Critical Care since 1993. Dr. Gfeller supervised treatment of over 100,000 emergency cases. He lectured to local, national, and international audiences on emergency medicine and critical care.

Anne Jablonski lives in Northern Virginia with her husband and two ill-mannered, well-fed, and deeply-loved cats. She works as a freelance business consultant, teaches mindfulness and yoga, and credits a mellow orange tabby named Duke and Dr. Lisa Pierson for setting her on a path years ago to get good and educated about cat nutrition. www.catnutrition.org

6 FEBRUARYMARCH 2023
Lucy Jabrayan, is the owner and founder of Thrive4life Holistic Pet Food, she educates and empowers pet guardians to turn to natural alternatives and modalities to better help their pets in their health & wellness journey. Lucy has an extensive background in the nutrition and supplement industry for well over a decade, as she takes her broad knowledge to educate many pet guardians by conducting health seminars, contributing to numerous publications and making segment appearances in television. To learn more visit, www.thrive4lifepetfood.com


Dr. Michael W. Thomas, DVM, Dr. Thomas is a full professor in the Department of Animal Science at California State University, Fresno. A 1983 graduate of Washington State University, he has been teaching animal health courses since 1985. Dr. Thomas is a popular teacher, twice receiving meritorious teaching awards, and has received university and national recognition for his innovative multimedia educational techniques. He has received research and educational grants for the study of infectious disease and development of computeraided veterinary courseware. In addition to 3 years of practice experience prior to his university work, he continues veterinary practice as campus veterinarian and clinician at California State University, Fresno.

7 FEBRUARYMARCH 2023
Simple… just 1 ingredient noahsarkpettreats.com If you would like to join us as a distributor, or sell our products as a retailer, contact us at: noahsarkpettreats@gmail.com
Introduction: First Aid
 By Roger Gfeller, DVM, DACVECC; Michael Thomas, DVM; Tony Johnson, DVM, DACVECC
By Roger Gfeller, DVM, DACVECC; Michael Thomas, DVM; Tony Johnson, DVM, DACVECC
8 FEBRUARYMARCH 2023
This first aid collection is an emergency preparedness ready-reference for dogs and cats. Wise preventive measures, intelligent use of first aid principles, coupled with recognition of abnormal symptoms and treatment of disorders, diseases, and problems, lead to effective health care. A working knowledge of prevention and first aid will help you eliminate some potentially dangerous circumstances and help you prepare for emergency situations.

The collection covers prevention, normal values, first aid, and some specific conditions. Also, information is provided on what to do and what not to do in specific emergency situations.
The authors encourage careful reading and occasional rereading. Consultants from the Veterinary Information Network (VIN) who specialize in emergency medicine, along with the cooperation of the original co-author Michael Thomas, DVM, carefully review this material. This collection was written to be easy to understand, avoiding technical terms as often as possible, but defining them in context when they are necessary.
This information is provided as a guideline for you to learn what to do in an emergency situation, but it cannot replace emergency visits to the veterinarian. In an emergency, call your veterinarian or local emergency hospital and do not rely on anyone on the internet to help.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951311 06366378-82b7-4550-a1b0-751ade9ad700.1672273556
VeterinaryPartner.com is not affiliated with Pet Connection.
9 FEBRUARYMARCH 2023
Abscess: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM
Animal teeth and claws easily puncture skin, introducing bacteria under the skin. If the skin heals quickly, the bacteria become trapped and create pockets of infection commonly referred to as abscesses.
Abscesses may be very small or extraordinarily large, and may feel swollen and warm. These are often extremely painful. Typically, animals with abscesses become depressed, and may tend to hide in inconspicuous places. Occasionally abscesses may rupture prior to the onset of any other signs. Abscesses of the anal glands are common and can be mistaken for rectal bleeding if they rupture. They may cause the pet to “scoot” the rectal area on the ground. Tooth root abscesses typically form just below the eye, and start as a bump or swelling. They may break open and bleed, and the pet may stop eating due to the pain or experience pain upon chewing.
Small, uncomplicated abscesses may respond to medical therapy, while larger and more extensive abscesses may require surgical treatment. Proper surgical management of abscesses often requires placing a drain or latex tubing (either under sedation or general anesthesia) to provide an escape route for secretions from the wound's damaged tissues.
Tooth root abscesses require tooth extraction –antibiotics alone will only lead to a temporary solution, but the abscess will recur unless the affected tooth is pulled. This surgery requires general anesthesia.
What to Do
Abscesses should be examined by a veterinarian as soon as possible and within 24 hours.
• Fluid may normally drain from the site of an abscess. An abscess does not drain through the tube, but rather around the latex tubing. Therefore, it is important for you to clean the area around the drain if directed to do so by your veterinarian.
• Apply a hot compress to the affected site at least two
times daily for 3 to 5 days after your pet leaves the hospital. Wet a clean washcloth with very warm water and place it directly over the affected site, and then apply gentle pressure ideally for 5 to 10 minutes.
• Be sure you and/or other family members wash your hands thoroughly after contacting any fluids draining from the abscess site.
• Be sure to give all prescribed medications exactly and completely as detailed by your pet’s veterinarian. Some patients may appear to feel better after only a few days of treatment; however, it is crucial for medications to be administered according to schedule to prevent the infection from recurring.
• Restrict your pet to indoor activities until the infection has resolved completely.
• Notify your pet’s doctor should your pet experience any of the following:
– Increased redness and/or heat from the site of abscess
– Failure of the abscess to heal
– Worsening of your pet’s general health
– Loss of appetite lasting longer than 24 hours
What NOT to Do
• Do not attempt to open the abscess yourself.
• Do not attempt compressing the wounds of a fractious cat. Your safety is of utmost importance to us. Contact your veterinarian for assistance should this situation arise.
• Do not apply medicines, human medications (such as Tylenol/acetaminophen or Advil/ Ibuprofen), or any home remedies unless directed by a veterinarian.
URL: https:/1p/www.slowvetmed.com/pet-library.pml?id=4951328 fbfa78de-0623-422d-9c25-00b86f914407.1672272901
VeterinaryPartner.com is not affiliated with Pet Connection.
10 FEBRUARYMARCH 2023
Bandaging: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
We use bandages for several reasons: to protect wounds from the environment, protect the environment from wounds, and to discourage a pet from licking or irritating a wound. Bandages may be applied as support for strains or sprains or to prevent motion. Proper application is important – an improperly applied or too-tight bandage can cause decreased blood flow and potential loss of the limb.
Cleaning the Wound
The process of bandaging begins with careful cleaning of the wound. All dried blood, dirt, and debris should be washed away using mild soap and lots of water. Hair should be clipped away so that it cannot lie in the wound. If possible, the area should be patted dry.
Materials Needed
In an ideal setting, a bandage should have a contact layer, an absorbent layer, and an outer layer.
Antibiotic ointment, Telfa Non-Adherent Pad, cotton wrap, gauze wrap, and Vetrap
The Contact Layer
After cleaning the wound, apply antibiotic ointment to the contact layer and use it first. Ideally, this layer should:
• Be sterile and inert.
• Stay in close contact with, but not stick to, the wound.
• Be very absorbent.
• Be free of particles or fibers that might shed into the wound.
• Conform to all shapes.
• Allow drainage to pass to the next layer without becoming wet.
• Minimize pain.
A Telfa Non-Adherent Pad, available at most pharmacies,
comes closest to meeting these requirements.
It is desirable to apply an antibiotic ointment, such as Neosporin, to the pad but this is not absolutely necessary. Frequent bandage changes are more important. After cleaning the wound, place a new contact layer over the wound.
The Absorbent Layer
After the contact layer is in place, apply the second (absorbent) layer to hold the contact layer snugly, but not tightly, over the wound. This layer is usually a cotton or Dacron material that comes in various widths. Generally, 1-inch rolls are used for small limbs and the tail; 2-inch rolls are for medium-sized legs; and the 3- and 4-inch rolls are for large legs and the body. It is important to use the proper size. Materials that are too narrow often cause a tourniquet effect, especially if the wound becomes swollen.
If materials are too wide, they are difficult to apply smoothly. Any wrinkles or ridges may cause the bandage to become uncomfortable for your pet. Uneven pressure may cause necrosis (tissue death) of the underlying tissues.
Begin with just enough of an absorbent layer to hold the contact layer in place. If the wound is on a leg or the tail, wrap from the toes or the tip of the tail towards the body. If you begin at the top of the leg or the tail, the bandage is more likely to restrict blood flow and cause swelling, which may cause tissue damage. Apply several layers of absorbent material, which will soak up the fluid from the wound and increase the patient’s comfort by cushioning the wound.
Make sure the material you use as the absorbent layer is the proper width, and wrap from the toes or tail tip up towards the body.
Gauze wrap can be applied next to hold the cotton wrap in place and to add extra support. This step can be skipped for small wounds or for temporary bandages.
11 FEBRUARYMARCH 2023
The Outer Layer
Finally, apply the outer (third) layer, usually made up of porous adhesive tape or elastic tape (i.e., Elastikon, Vetrap). Wrapped from the toes up towards the body, this layer should also be smooth and snug. Do not stretch elastic tapes to their limits as this will interfere with circulation and result in bandage failure. It helps to unwrap the Vetrap or Elastikon first and then rewind it to remove the tension from the wrap before placing.
The tape should be in contact with the skin (hair) at the bandage margins, anchoring the bandage so it will not slip.
The outer layer of a bandage should be applied smoothly and snugly, but not tight enough to cut off blood circulation.
Bandage Changes
Bandages should be checked frequently for any signs of swelling, skin discoloration or coolness, odor, or saturation of the bandage material. The bandage should be changed whenever any of the above are noticed or any time it appears to be uncomfortable for the pet. If a bandage becomes wet, soiled or slips out of position, it should be replaced. Home bandaging is not a substitute for proper veterinary care and improperly applied bandages can result in limb loss. Be very careful when bandaging at home. Wounds that are draining heavily may require bandage changes every one or two hours. Bandages over wounds with little or no drainage should be changed every 24 hours.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951319 d1b11450-8fb4-4fc1-bc22-72f7c66d17ed.1672273622 VeterinaryPartner.com is not affiliated with Pet Connection.

12 FEBRUARYMARCH 2023

Bee Stings and Insect Bites: First Aid
 By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Any insect or spider can cause problems if they bite or sting your pet. A bite or sting can cause swelling, redness, and itching. Some animals can have an allergic reaction to a sting or bite that may result in mild hives, facial swelling, vomiting, difficulty breathing or even collapse.
What to Do:
• If the stinger can be found, scrape it out with a credit card or other stiff material. Alternatively, use tweezers by grasping the stinger, which is located below the venom sac. Studies have shown that speed is of the essence in removing the stinger. If the only way is to pinch it and remove it, then do so. You'll do more good than harm and you'll get the stinger out faster. Don’t worry about squeezing more venom into the area - this has been disproven.
• Apply cool compresses to the area.
• To help neutralize some of the acidic venom, apply a paste mixture of baking soda and water to the sting area.
• Your pet should be examined immediately by a veterinarian if there is facial swelling, breathing difficulty or collapse.
What NOT to Do:
• Do not administer any medications without first contacting your veterinarian or a veterinary emergency hospital. The veterinarian may need to examine your pet before recommending medications.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951319 a70d8b01-1fc6-47b8-a9bd-cb9a709dae87.1672004465
VeterinaryPartner.com is not affiliated with Pet Connection.
14 FEBRUARYMARCH 2023
Bleeding: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Pets often suffer blood loss as a result of trauma or poisoning. Some bleeding is visible, and is a result of a cut or laceration, while internal bleeding occurs inside the body (such as in the chest or abdomen) and is not be visible to the naked eye. If bleeding is severe or continuous, the pet may lose enough blood to cause shock; loss of as little as 2 teaspoons per pound of body weight may cause shock, which doctors usually detect as a high heart rate and low blood pressure. Emergencies may arise that require you to control the bleeding, even if it is just during transportation to the veterinary facility. Pet owners should know how to safely stop hemorrhage (bleeding) if their pet is injured.


Techniques to Stop External Bleeding
The following techniques are listed in order of preference. The first rule when dealing with an injured pet is to avoid injury to yourself, so take appropriate precautions (such as the use of a muzzle) to avoid being bitten. For all techniques below, seek veterinary attention immediately after stopping the bleeding, or on the way to the veterinary hospital.
Direct Pressure
Gently press a compress (a pad of clean cloth, feminine sanitary product or gauze) over the bleeding area, so
15 FEBRUARYMARCH 2023
2443 Beacon Avenue, Sidney, B.C. Monday - Saturday 10:00am - 5:00pm Sunday 11:00 - 5:00pm 250.656.1350 www.petconnection.ca FOR THOSE ON VANCOUVER ISLAND VISIT US AT OUR HEAD OFFICE AND WELLNESS STORE! Get Connected! • Full Service Dog Grooming • Free weigh-ins • Real food • Single ingredient treats • Natural supplements • Complimentary Magazine “Saving the World One Dog and Cat at a Time”
it can absorb the blood and allow it to clot. Do not disturb blood clots after they have formed. If blood soaks through, do not remove the pad; simply add additional layers of cloth and continue the direct pressure more evenly. The compress can be bound in place using loosely applied bandage material, which frees the hands of the first provider for other emergency actions. If you don’t have a compress, you can use a bare hand or finger.
Direct pressure on a wound is the most preferable way to stop bleeding.
Elevation
If a severely bleeding wound is on the foot or leg, gently elevate the leg so that the wound is above the level of the heart.
Elevation uses the force of gravity to help reduce blood pressure in the injured area, slowing the bleeding. Elevation is most effective in larger animals with longer limbs where greater distances from the wound to the heart are possible. Direct pressure with compresses should also be maintained to maximize the benefits of elevation.
Elevation of a limb combined with direct pressure is an effective way to stop bleeding.
Pressure on the Supplying Artery
If external bleeding continues after you have used direct pressure and elevation, use your finger or thumb to place pressure over the main artery to the wound. Apply pressure to the femoral artery in the groin (on the inside of the thigh) for severe bleeding of a rear leg; to the brachial artery in the inside part of the upper front leg for bleeding of a front leg; or to the caudal artery at the base of the tail if the wound is on the tail. Continue application of direct pressure. Seek veterinary attention immediately.
Tourniquet
Use of a tourniquet is potentially dangerous and it should be used only for a severe, life-threatening hemorrhage in a limb (leg or tail) not expected to be saved. If you see blood spurting or pumping from a wound, which is a rare occurrence, consider the use of a tourniquet. Use a wide (2-inch or more) piece of cloth
and wrap it around the limb twice and tie it into a knot. Then tie a short stick or similar object into the knot as well. Twist the stick to tighten the tourniquet until the bleeding stops. Secure the stick in place with another piece of cloth and write down the time it was applied. Every 20 minutes loosen the tourniquet for 15 to 20 seconds. Remember this is potentially dangerous and can often result in disability or amputation.
A tourniquet should only be used as a last-resort, life-saving measure!
Internal Bleeding
Internal bleeding is a life-threatening condition, but it is not obvious like external bleeding. In internal bleeding, blood pools in the stomach or chest but does not result in blood in the stool or bleeding from the rectum. There are, however, some external signs of internal bleeding:
• The pet is pale (check the gums).
• The pet is cool on the legs, ears, or tail.
• The pet may cough up blood.
• The pet is unusually subdued.
If you see any of these signs, immediately transport your pet to a veterinary facility for professional help. Most cases of internal bleeding will require intensive therapy in a veterinary hospital. Remember: internal bleeding is not visible on the outside.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951317 90f89d8c-c378-415c-82cb-77457e1118bb.1672339728
VeterinaryPartner.com is not affiliated with Pet Connection.

16 FEBRUARYMARCH 2023
Wild Salmon Oil Blend & Shiny Coat™
Essential Fatty Acids for Your Cats & Dogs mega-3

Essential fatty acids (EFAs) are required for the proper structure and function of every cell in the body, and they are important for optimal health. EFAs increase the absorption of vitamins and minerals, they nourish the skin, hair/fur and nails, promote proper nerve functioning, and help produce hormones. EFAs ensure normal growth, development and help in the prevention of some diseases. Omega Alpha’s blend of EFAs are molecularly distilled, human-grade and contains only the best quality oils that are free of pesticide/herbicide residues, heavy metals, and other toxins or contaminants.
Wild Salmon Oil Blend is a natural omega-3 formulation with 60% salmon and 40% anchovy, mackerel and sardine. It is also formulated with mixed tocopherols (vitamin E) containing both d-alpha tocopherol and gamma tocopherol. It is important to have both forms of vitamin E as d-alpha tocopherol scavenges reactive oxygen species and gamma tocopherol provides protection against reactive nitrogen species which d-alpha tocopherol cannot do.


Ingredients per 1 tsp. (5 mL):
Blend of Omega-3 Essential Fatty Acids Fish Oil ....................................... 5 mL
Salmon (60%); Anchovy, Mackerel, Sardine (40%). Omega-3 .............................. 1375 mg EPA (Eicosapentaenoic acid) ..... 825 mg DHA (Docosahexaenoic acid) .... 550 mg

Additional ingredient: Vitamin E (mixed tocopherols).
Shiny Coat™ is an Omega 3-6-9 formula for healthy skin and coat. The general health of your pet may be improved by consumption of essential fatty acids. Whether your pet is a show animal or a much-loved member of the family, Shiny Coat™ will help maintain your pets’ healthy skin and coat while providing them the nutrients that they need.


Ingredients per 1 tsp. (5 mL):
Proprietary Blend of Omega 3-6-9 Essential Fatty Acids
Flax Seed Oil 5 mL Salmon (60%)
Anchovy, Mackerel, Sardine (40%).
Omega-3 ...................................... 1375 mg EPA (Eicosapentaenoic acid) 825 mg DHA (Docosahexaenoic acid)......... 550 mg
Additional ingredient: Vitamin E (mixed tocopherols).
Anchovy, Mackerel & Sardine (small fish oils)
Borage & Flax seed oils
immune system functions
Has mixed tocopherols (vitamin E, d-alpha and gamma tocopherol)
17 FEBRUARYMARCH 2023 OmegaAlpha.com | Proudly Canadian | Trusted Since 1992
9
9
9
9
9
9 Helps
9 Provides
9 Source of
kidney and
9 Promotes
metabolism
Source of essential fatty acids for the maintenance of good health (skin, fur & joints)
Supports cognitive health
Enhances
9
9
Improves skin and coat health
improve cognitive health
immune support at the cellular level
essential fatty acids (omega-3) to support brain, heart, immune, muscles, joints,
liver health
healthy weight and
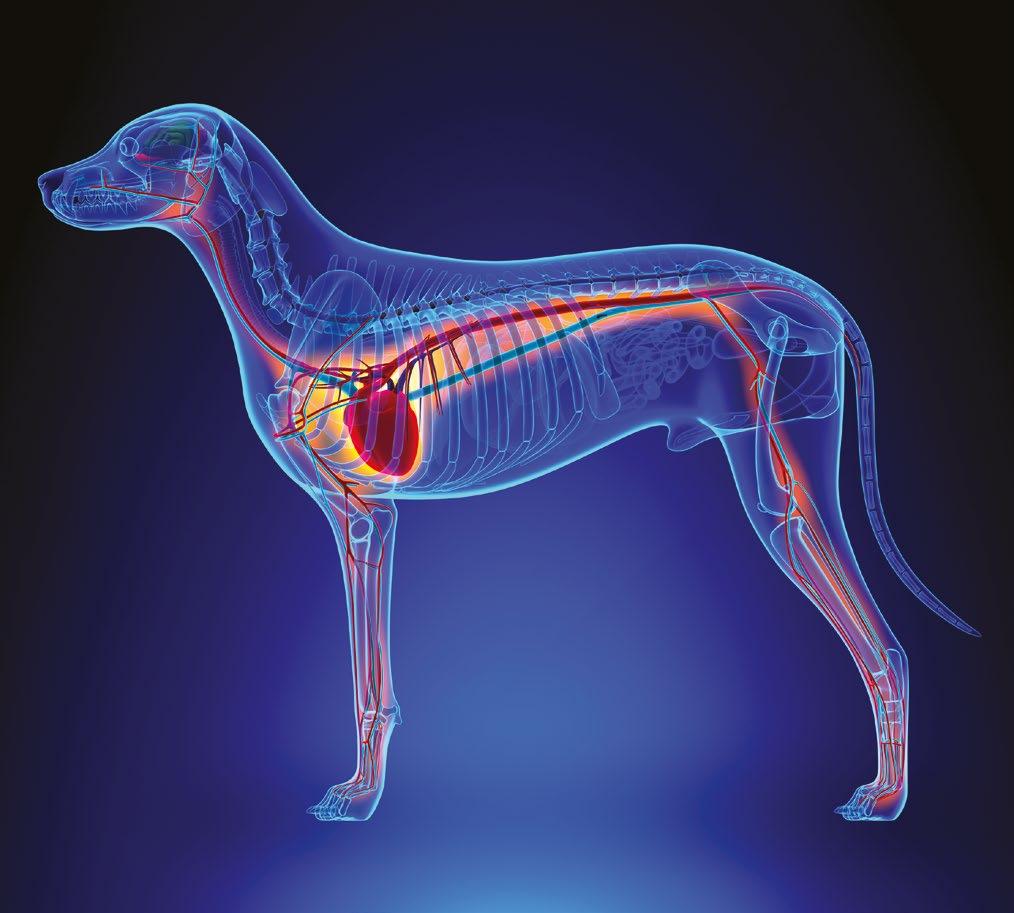
Bloat: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Bloat is a life-threatening condition in which the stomach fills with air (dilatation) and/or twists upon itself (volvulus). It’s also called GDVgastric dilatation volvulus.
What to Do
Transport to a veterinary hospital or emergency facility immediately. In all cases, this condition requires professional assistance. Most cases will require surgery.
What NOT to Do
• Do not attempt to relieve the gas from the stomach.
• Do not give anything by mouth.
It is imperative that this condition be recognized early. Your pet's abdomen may not have a bloated appearance. Signs of bloat include:

• Drooling of saliva
• Frequent retching and attempts to vomit (occasionally patients may be able to regurgitate a pool of foamy saliva)
• Anxiety, restlessness, and pacing
• Lethargy or agitation
• Depression and shock. Much has been learned about bloat in the past decade. Decades ago, a diagnosis of bloat was almost always a death sentence because only 25 percent survived. Today the survival rate is better than 80 percent with surgery. Part of the reason for this is increased owner awareness. The earlier the veterinarian gets started with treatment and takes the pet to surgery (after stabilization for shock) the better chance there is for survival. Extremely aggressive medical and surgical intervention early in the course of the disease has the most dramatic impact on overall treatment success.
Prevention
Research into this area is ongoing and many studies have produced conflicting results. No one intervention has been shown to prevent GDV. Elevated feeding may actually increase the risk of GDV in some patients. Smaller kibble size, feeding smaller more frequent meals, and not breeding animals with a history of GDV in their lineage may potentially decrease the risk of GDV for the animal and future generations.
In breeds with a high risk of bloat, such as Great Danes, German Shepherd Dogs, and Akitas (as well as other deep chested dogs), a preventive surgery called a prophylactic gastropexy can often be performed when the dog is being spayed or neutered. This involves surgically attaching the stomach to the inside of the abdomen to prevent rotation and can sometimes be done through ‘minimally invasive surgery’ or laparoscopy. Ask your veterinarian for details and advice if you would like to discuss preventive surgery for bloat.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951346 1061275f-d1c6-4f8a-b5fa-facda55a0dc4.1672685181
VeterinaryPartner.com is not affiliated with Pet Connection.
18 FEBRUARYMARCH 2023
Burns: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Aburn is any injury of tissue caused by heat, flame, chemicals, or electricity. Burn classification determines the severity of the wound based on the depth of the tissue injury.
First-degree burns are limited to redness and minor pain at the site of injury. These burns only involve the top layer of skin and heal quickly.
Second-degree burns have superficial blistering of the skin, and can involve deeper layers of the skin.
Third-degree burns occur when the top layer of skin is lost with damage to the deeper layers. Burns exhibit charring and extreme damage. Third-degree burns result in scarring and may require skin grafting.
What to Do
• Extinguish all flames.
• Use appropriate measures to avoid being bitten (muzzle your pet).
• Avoid touching any pet that has been electrocuted until the power has been turned off.
• If needed, move pet carefully away from electrical source with a wooden broom (not metal).
• For thermal or electrical burns, immediately apply cool water compresses with a clean cloth to the site of the injury, changing them frequently as necessary to keep the site cool and wet. Continue this for at least 30 minutes.
• For chemical burns, see chemical injuries.
• Transport your pet to a veterinary facility as soon as possible for further care. Burns can become worse before they get better, and may require several weeks of therapy, multiple surgeries and possibly skin grafting.
What NOT to Do
• Do not apply ointments or butter.
• Do not delay seeking veterinary attention.
• Do not attempt to remove burned hair or skin yourself.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951347 8be71074-1ba8-43bf-817b-c29e280ba8dd.1672685402 VeterinaryPartner.com is not affiliated with Pet Connection.
New Products!
Anchovy Oil is an excellent and highly concentrated source of Omega’s which are great for skin and coat


Coprophagia Deterrent can help stop your pet from eating stool Ear Care Formula can help with ear mites, ear infections and dirty ears

Canadian owned and operated. ww w.p e t-te k .c a We keep your pets healthy and happy.


19 FEBRUARYMARCH 2023
Can't Breathe: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Difficulty breathing is also called dyspnea and is a medical emergency.
Respiratory distress is recognized by increased effort to breathe; noisy or squeaky breathing; and cyanosis (a bluish tinge to the lips, tongue, and mucous membranes). In cats, breathing with the mouth open (panting like a dog) is a sign of severe distress and should be evaluated by a veterinarian right away.

heat or by surgically reconstructing the soft palate.
• Keep the pet and yourself calm.
• If the pet has choked on a foreign body, perform the Heimlich maneuver and/or a finger sweep (see Choking page 25).
• Perform rescue breathing if necessary (see rescue breathing in the Choking article page 25).
• If the pet is overheated, moisten the feet and ears with cool water to promote heat exchange.
• If you are driving to the veterinary hospital or ER, turn the air conditioner in the car on to its coldest setting
• Seek veterinary assistance as soon as possible.
What NOT to Do
• Do not upset the pet.
• Do not perform rescue breathing on a conscious pet.
• Do not give anything by mouth.
It is imperative to get the pet examined to determine the cause. Diagnostic tests such as x-rays, blood tests and ultrasound may be needed, but the pet must be stabilized (often with oxygen or by removing fluid from the chest) before they can withstand the rigors of testing if respiratory distress is severe.
What to Do
Brachycephalic (short-nosed) breeds (e.g., English bulldog, Pekingese, and Pug) warrant a special mention. Because of the short nose, the soft palate can interfere with breathing. On hot days or in hot, humid environmental conditions these dogs try to cool off by panting vigorously, and the soft palate interferes even more. This cycle continues until the dog is severely dyspneic and overheated. Cooling these dogs is imperative. Move them to a cool environment and seek immediate veterinary care. This syndrome is manageable only by protecting these breeds from
Dyspnea, or difficulty breathing, is a serious sign. Causes include:
• Congestive heart failure
• Asthma
• Cancer
• Fluid buildup in or around the lungs
• Bronchitis
• Pneumonia
•
Laryngeal paralysis (a condition usually seen in older pets in which they lose ability to open and close their airway)
• Obstruction of the trachea
• and many other conditions.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951325 f6cd7066-9436-45e7-ba46-af6ef6e06c2b.1672685559
VeterinaryPartner.com is not affiliated with Pet Connection.
20 FEBRUARYMARCH 2023
Cardiopulmonary Resuscitation (CPR): First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Cardiopulmonary resuscitation (CPR) is the treatment required to save an animal (or human) life when suffering cardiopulmonary arrest. The intent of CPR is to provide sufficient blood flow and oxygen to the brain and vital organs to support life until more advanced medical therapy can be started. Unlike what we see on television, most patients who suffer from cardiac arrest are unable to be saved, even with CPR. In a study from the University of California at Davis, researchers discovered that long-term survival among feline patients is extremely poor. In this study, only 2.3 percent of feline patients who received CPR survived to be discharged from the hospital alive. This closely parallels findings of similar studies in human medicine.
In 2012 the American College of Veterinary Emergency and Critical Care established a committee to evaluate the scientific evidence on how to best conduct CPR in pets, and generated evidence-based guidelines. The results of these guidelines are incorporated into the recommendations below.
CPR consists of two parts: rescue breathing and chest compressions.
These two techniques combine to keep the lungs supplied with oxygen and to keep blood circulating, carrying oxygen to the other parts of the body such as the brain and vital organs.
Basic CPR is CPR performed by trained bystanders at the scene of the arrest.
Advanced CPR is CPR performed by trained teams of professionals, generally in a hospital setting.
Basic CPR is the most important for pet owners, and is described in this section.
All body tissues require a steady source of oxygen. If the source is interrupted for only a few minutes, irreversible damage may be done. If cardiopulmonary arrest occurs, basic CPR must be initiated at the scene.
As long as the airway is open, compression of the chest may cause forward flow of blood and may cause enough movement of air that less frequent breathing is recommended for single-rescuer CPR. Therefore, if only one rescuer is available to perform CPR, a ratio of 30 compressions to 2 breaths is recommended.
Basic CPR: Rescue Breathing (If Two People are Present)
Make Certain the Animal is actually Arrested and Unconscious
Talk to the pet first. Gently touch and attempt to awaken the pet. You could be seriously injured should you attempt to perform CPR on a pet who was only sleeping heavily and was startled awake. Ensure an Open Airway
Extend the head and neck and pull the tongue forward. Look in the mouth and remove any saliva or vomitus. If it is too dark to see into the mouth, sweep your finger deep into the mouth and into the throat to remove any vomit or foreign body. Be aware of a hard, smooth, bonelike structure deep in the throat, which is likely to be the hyoid apparatus (Adam's apple). Serious injury could result if you pull on the hyoid apparatus.
Observe for Effective Breathing
Sometimes an animal will begin to breathe spontaneously when the head is put in the position discussed above (head and neck extended, tongue pulled forward). Watch for the rise and fall of the chest while
21 FEBRUARYMARCH 2023
listening closely for sounds of breathing. If no breathing is evident in 10 seconds, begin rescue breathing.
Begin Rescue Breathing
Rescue breathing is performed by covering the pet’s nose with your mouth and forcefully blowing your breath into the lungs. In cats and small dogs, you must hold the corners of the mouth tightly closed while you force the air in.
In larger dogs, the dog’s tongue should be pulled forward and the mouth and lips held shut using both hands cupped around the muzzle. Force air into the lungs until you see the chest expand. Take your mouth away when the chest has fully expended. The lungs will deflate
without help. Air should be forced into the lungs until you see the chest expand.
Give 3 to 5 Full Breaths
After several breaths are given, stop for a few seconds to recheck for breathing and heart function. If the pet is still not breathing, continue rescue breathing 10 times per minute in cats or dogs. Push down on the stomach area every few seconds to help expel the air that may have blown into the stomach. If the stomach is allowed to distend with air, the pressure will make the rescue breathing efforts less effective. Try to coordinate breaths with chest compressions for 2-person CPR.
22 FEBRUARYMARCH 2023
If Breathing is Shallow or Non-existent
If you find that breathing is either shallow or nonexistent and the pet is still unconscious, continue rescue breathing 10 times per minute and transport the pet to the nearest veterinary facility.
Basic CPR: Chest Compressions (If one or two people are present)
After Ensuring an Open Airway, Check for a Pulse
If no pulse is detectable, begin chest compressions.
In Small Dogs or Cats
Squeeze the chest using one or both hands around the chest. Depress the rib cage circumferentially. Do this 100-120 times per minute.
In Large Dogs
Compress the chest wall with one or both hands, depending on the size of the dog and the size of the rescuer (whatever works best for you). If the dog is on their side, place your hand(s) on the side of the chest wall where it is widest. If they are on their back (a position best for barrel-chested dogs like bulldogs), place your hand(s) on the breastbone. Depress the rib cage 1.5 to 4 inches, depending on the dog's size. Do this 100-120 times per minute.
Coordinate Rescue Breathing and Chest Compressions
If possible, give breaths during the compressions. If it is not possible, give two breaths after every 30 compressions.
Continue CPR until
• You become exhausted and can't continue.
• You get the animal transported to a veterinary facility and professionals can take over.
• The pulse is palpable or heartbeats are felt and they are strong and regular.
In the vast majority of cases, artificial ventilations will continue to be required for a period of time, even though heart function has returned. This is due to the nervous system depression that occurs as a result of the arrest.
All resuscitated animals should be transported to a veterinary facility for further examination and care!
URL: https://www.slowvetmed.com/pet-library.pml?id=4951315 56603275-89aa-4ff0-8b35-32d72793fe2b.1672685954. VeterinaryPartner.com is not affiliated with Pet Connection.

23 FEBRUARYMARCH 2023
Chemical Injuries: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Chemical injuries to tissue are caused by contact with harmful chemicals such as lye, acids, and strong cleaning supplies. Also called chemical burns, they can be similar to thermal (heat) burns and treatment can be complex and last many weeks. Prompt removal of the chemical agent and rapid veterinary medical attention can help minimize the injury and speed healing.
What to Do
• Wash the contaminated area with large volumes of tepid flowing water for at least 15 minutes.
• In the case of dry chemicals, brush them away carefully, taking care to protect the eyes, nose, and mouth of both you and your pet.
• If the chemical is in the eye, flush the eye with large volumes of water or contact lens saline for 15 minutes. (See below for saline recipe.)
• Seek veterinary attention as soon as possible.
• Avoid being bitten by using a muzzle on your pet if your think there is a risk of being bitten.
• Make sure the area is well ventilated as some chemicals can release strong fumes.
What NOT to Do
• Do not apply neutralizing agents to the skin or eyes. They can cause a chemical reaction that produces heat and cause further injury to tissues.
• Do not immerse your pet in non-flowing water if a dry chemical has spilled on him or her. These dry chemicals are usually activated by water. The water must be flowing in order to rinse the chemical away.

Pure water can be quite irritating to the eyes and raw skin. It is much more comfortable for your pet if you use saline: simply dissolve 2 teaspoons of table salt in one quart of water (metric: 9 grams of salt in 1 liter of water).
URL: https://www.slowvetmed.com/pet-library.pml?id=4951348 0607d091-9e59-412d-9505-f07c58848453.1672688227
VeterinaryPartner.com is not affiliated with Pet Connection.
24 FEBRUARYMARCH 2023
Choking: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Choking is interference with breathing caused by foreign material in, or compression on, the trachea (windpipe). Thankfully, true choking is a very rare occurrence. Many pet owners will seek veterinary care because they believe their pet has something stuck in its throat, and this is rarely the case. It is far more likely that your pet has something mild and infectious such as tracheobronchitis (commonly called kennel cough) and is coughing rather than choking.
Frequently, coughing is confused with choking. Both cause the pet to forcefully exhale. With choking, the pet has difficulty inhaling. When coughing, the pet can inhale almost normally. Be careful to distinguish the two: attempting to give first aid to a pet who is merely coughing can cause injury.
If you are in any doubt, have your pet evaluated by a veterinarian. To evaluate the throat, most pets will require sedation and some will require evaluation with a fiber-optic endoscope or X-rays to look for foreign material.

If the Pet is Unconscious
Perform a Finger Sweep
Open your pet’s mouth and do a finger sweep by placing your finger along the inside of the mouth, sliding it down toward the center of the throat over the base of the tongue, and gently “sweeping” toward the center to remove any foreign material. Warning: there is a structure deep in the throat (the Adam's apple) that feels like a smooth bone. Do not attempt to pull it out!
Begin Rescue Breathing
Rescue breathing is described in the article on CPR. If air is not entering the lungs, slap the chest wall firmly or perform the Heimlich maneuver by putting the pet on his back, placing your hands over the abdomen near the bottom of his rib cage, and gently but firmly
thrusting toward the spine. Perform a finger sweep and begin rescue breathing. Repeat until the foreign body is clear and the lungs can be inflated. Transport to the veterinarian.
If the Pet is Conscious
Stay calm and try to keep the pet calm. If the pet is overheated, cool them with cold water applied to their extremities (ears and feet) and belly, and transport them to the nearest veterinarian. Perform a finger sweep only if it will not excite the pet. Do not perform a finger sweep if you believe your pet will bite you.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951320 a3ae2b9c-4c8a-4d2a-ad31-cb86ee19707c.1672688892
VeterinaryPartner.com is not affiliated with Pet Connection.
25 FEBRUARYMARCH 2023
Dehydration: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Dehydration is excessive loss of water from the body (typically through vomiting and/ or diarrhea) or inappropriate intake of water into the body (decreased thirst). The most common mistake with a vomiting pet is to encourage food and water intake while the pet is still vomiting. This actually makes matters worse by not allowing the stomach and intestinal tract time to rest, and can cause additional vomiting and water loss. Removing access to food and water for a short period of time may seem like it would make dehydration worse, but it can help your pet avoid further dehydration. Dehydration makes your pet feel lethargic, and can potentially cause severe problems with the kidneys and other internal organs if untreated.
What to Do
• If moderate or severe dehydration, seek veterinary attention. (See below for how to assess if dehydration is potentially severe in your pet.)
• If dehydration is mild and the pet is not vomiting, give frequent, small amounts of water by mouth; that means in the range of 1 tsp for a cat or small dog to 1 tbsp to 1/4 cup for a medium to large dog every few hours.

• If your pet is lethargic, in pain, or has not eaten for 24 hours, seek veterinary attention.
What NOT to Do
• Do not allow your pet to have immediate free access to large amounts of water or other liquid.
• Do not feed your pet any dry food until directed to do so by a veterinary professional. Dehydration often accompanies symptoms like vomiting, diarrhea, hypothermia (low body temperature), fever, no access to water, and other conditions. It can be detected by several tests:
Mouth: Are the tongue and gums moist or dry?
If they are dry, there is a chance your pet may be dehydrated. Is the saliva thick or ropey? Normally, saliva is quite watery and hardly noticeable.
Eyes: Are they normal, or do they sink into the sockets? Sunken or dry eyes may indicate dehydration, and warrant veterinary attention.
Skin: Do the skin turgor test outlined in the Physical Exam Checklist. If the skin is slow to return to position, the pet may be moderately to severely dehydrated. If the skin does not return fully to its position, your pet may be severely dehydrated and may be in critical condition. Seek veterinary attention immediately. The skin turgor test is not always accurate and several factors such as age, weight loss and condition of the skin can give misleading results. A veterinary professional can help you determine how dehydrated your pet is, what the cause may be, and the best course of treatment.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951322 415f701c-ef94-4e1e-836d-56166ac5d98c.1672689283
VeterinaryPartner.com is not affiliated with Pet Connection.
26 FEBRUARYMARCH 2023
Diarrhea and Vomiting: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Diarrhea is the frequent evacuation of watery stools. Vomiting is the forceful expulsion of stomach contents through the mouth.
What to Do
• Remove all food and water.
• Check for signs of dehydration.
• If the diarrhea and/or vomiting continues or the pet acts ill, seek veterinary attention. Diarrhea and vomiting can quickly lead to serious fluid loss and electrolyte imbalance, especially in very young and very old animals.
• If no vomiting occurs for 6 to 8 hours, begin to frequently give small amounts of clear liquids (water, Gatorade, Pedialyte, or other electrolyte solution).
A rule of thumb is to give 1 teaspoon per pound of body weight every 2 or 3 hours throughout the day and night. If your pet does not vomit the fluid, the following day offer small frequent meals of boiled hamburger and rice or boiled chicken and rice. If your pet does not want to eat, starts to vomit, or continues to have diarrhea, go to the veterinarian for medical care.
• Isolate the sick pet from other pets.
What NOT to Do
• Do not administer any over-the-counter or prescription medications to your pet without talking to a veterinarian first.
• Do not allow the pet to eat or drink anything until there has been no vomiting for 6 to 8 hours.
Diarrhea and vomiting
Vomiting and diarrhea are associated with a host of problems that are referred to collectively as gastroenteritis. Some cases are quite severe (e.g., poisoning), and some are not (e.g., dietary indiscretion). If fever is present, infection may be a cause. Most infections that cause diarrhea and vomiting are contagious, so it is wise to assume that other pets might be vulnerable if they are exposed.
If your pet is not feeling well and has vomiting and/or diarrhea, see a veterinarian.

URL: https://www.slowvetmed.com/pet-library.pml?id=4951323 c5a08dae-4470-4149-88c3-c4dc486a6d18.1672689651
VeterinaryPartner.com is not affiliated with Pet Connection.
27 FEBRUARYMARCH 2023
Difficult Birth: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Puppies are born 58 to 72 days after mating. Because canine spermatozoa live 4 to 11 days in the bitch’s reproductive tract, it is not possible to accurately determine the day of birth from the time of mating. If purposefully breeding, ovulation timing can be performed to determine with much greater accuracy the expected delivery date. A cat’s gestation period is similar at 63 to 65 days.
If the contractions are frequent, regular, and strong, and no young is produced in 15 to 30 minutes, the pet should be taken to a veterinarian. Intermittent
contractions with no kitten or puppy should be evaluated after 1.5 to 2 hours as long as the dam appears comfortable. A dark green vaginal discharge called lochia should be followed within 5 to 10 minutes by a puppy or kitten, but only before the first one. Heavy bleeding requires an immediate veterinary examination.
While a few cats can take up to 24 hours to complete the birthing process, most should follow the same protocol as for dogs.
About two out of three cases of difficult birth (known as dystocia) that need to be seen by a veterinarian will

28 FEBRUARYMARCH 2023
need to have an emergency C-section performed. It is good practice to know long before the due date where your local veterinary emergency facility is, and when and if they can perform a C-section. C-sections are risky and expensive surgeries and careful consideration should be given to the decision to breed your pet or not. X-rays taken after the 44th day of gestation (not necessarily from breeding) can show how many babies will be born but they are much easier to count when the skeletons are fully mineralized later in gestation, after day 50. This will allow you to know when the mother is done giving birth.
Reddish to brownish vaginal discharge can continue for several weeks after a normal birth. If the mother is eating normally and is normally active, this isn’t a problem. If she becomes lethargic, stops eating, has a fever or acts ill, prompt veterinary attention is needed.
Some new mothers can experience a condition called eclampsia in which their blood calcium levels drop dangerously low. This is due to the large amount of calcium secreted in milk for the newborns. Dogs with eclampsia experience poor mothering, severe muscle tremors, difficulty walking, and seizures. Immediate veterinary care is needed if your dog is showing any of these signs. Eclampsia can happen anytime around birth, but is most common during peak milk production (2 to 4 weeks after birth).
What to Do
• Prepare a clean, warm, and easy-to-clean area for the birth. Puppy rails for whelping boxes are lifesavers for puppies.
• Check on the mother frequently without disturbing the process. Repeated interruptions will only delay birth.
• If a baby is visible in the birth canal and appears stuck, gently grasp the foot or feet with a clean cloth. With a steady motion gently pull upwards towards the dam’s tail on the baby only when the female is contracting. If the baby does not come out easily, transport the pet to a veterinarian.
• When the baby is born, it will likely be covered in a membrane. If the mother doesn't remove it, tear this membrane and remove it from the baby’s head region.
• If the mother doesn’t remove the umbilical cord, or is being rough with it, tie it with a piece of string or dental floss one-fourth of an inch from the baby’s abdomen. Then cut the cord one half of an inch from the abdomen with a sharp scissor on the dam’s side of the cord. Apply 2 percent tincture of iodine to the entire umbilicus (buy this beforehand, just in case).
• Keep the babies warm. It is best to leave them with their mother, but sometimes she doesn't stay with them. In that instance, put a plastic bottle filled with warm water near the babies. A hot water bottle covered with a towel works as does a Snuggle Safe™ disc. Neonates must have room and be strong enough to move away from the heat source. Room temperature should be around 85F. Allow room for the babies to move toward or away from the heat source.
What NOT to Do
• Do not put your fingers in the birth canal as you can cause trauma or infection.
• Do not forcibly attempt to remove a baby.
• Do not assist delivery by pulling on the head of a baby or on the umbilical cord as it exits the mother.
• Do not lift the baby by the umbilical cord.
• Do not use a heating pad.
• Most kitten and puppy births go smoothly with the mother doing all the work. The babies contentedly nurse on the mother soon after birth.
• You may not see the afterbirth (placenta) being passed. Many mothers will eat this after it is passed without anyone noticing. It’s usually not a problem if all of the placentas are not immediately passed as the dam usually passes them later, but on occasion retained placentas do not pass and in those cases can cause serious illness.
(Reproduction specialist Dr. Joni Freshman contributed to this article.)
URL: https://www.slowvetmed.com/pet-library.pml?id=4951324 571c075d-5ab2-4f73-b1b7-d0a7721a873e.1672704437
VeterinaryPartner.com is not affiliated with Pet Connection.
29 FEBRUARYMARCH 2023
Drowning or Near Drowning: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Suffocation by drowning is caused by lungs filling with water or other fluid. Some pets can seemingly recover from a near drowning incident, only to succumb to a collection of fluid in the lungs (known as pulmonary edema) hours later. This phenomenon is known as ‘dry drowning’ and can be fatal. For this reason, all pets that have fallen into a pool or other body of water should be evaluated by a veterinarian and observed for complications.
What to Do
• Remove your pet from the water if it can be done safely.
• Place him on his side with his head and neck extended. It's preferable to have the head slightly lower than the body to promote drainage of water from the lungs and to avoid inhalation of stomach contents (aspiration).
• To expel water from the lungs and stomach, pull the tongue forward and gently push on the chest wall and stomach. Take care to avoid being bitten.
• Begin CPR as required.
• Cover the pet with a blanket to avoid further heat loss.
• Seek veterinary help as soon as possible.
• Secure the water source to prevent other pets and children from gaining access and falling in.
What NOT to Do
• Do not fail to seek veterinary help just because your resuscitation is successful and your pet seems to be recovering. Numerous secondary complications (i.e., electrolyte imbalance, hypothermia, pneumonia, fluid in the lungs) can occur.
• Do not leave the pet unattended as they may be confused and wander back to the water.
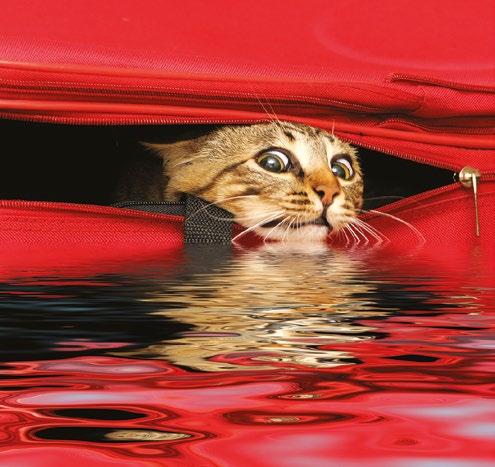
Almost all cats and dogs instinctively know how to swim. Unfortunately, they also instinctively swim to the nearest edge of a pool to get out. Usually that is not the right decision. Most animals are unable to get out of a swimming pool at the edge and must swim to a step. If your pet has access to a swimming pool, you must teach them where the steps are. If they don’t know where the steps are and fall in, they will swim to the nearest edge and attempt to get out until they either accidentally arrives at a step or tires and drowns.
If your pets have access to a swimming pool, you must teach them where the steps are located.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951326 2ca63664-2b55-4ff1-948b-07ab444609c5.1672704813
VeterinaryPartner.com is not affiliated with Pet Connection.
30 FEBRUARYMARCH 2023
Electrocution: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
In order to avoid injury to yourself, it is imperative that you do not touch the pet until the electrical source has been turned off or moved. Electricity can flow through your pet and affect you as well.

Electrocution can cause severe tissue damage (like a thermal or heat burn can) and can also lead to serious internal complications like pulmonary edema (fluid in the lungs). Immediate veterinary care is needed, but several things you can do at home can minimize the extent of the injury and promote healing.
What to Do
• Unplug the electrical cord or shut off the electricity.
• If this is not possible, use a dry wooden broom or other non-conductive object to move the pet away from the source of the electricity.
• Check for breathing and pulse. Begin CPR if necessary.
• If the pet is breathing, check the mouth for burns if this can be done safely. Apply cool compresses to burns.
• Cover the pet with a blanket to prevent heat loss.
• Seek veterinary attention as soon as possible.
What NOT to Do
• Do not fail to get the pet examined even though he or she seems perfectly normal after being separated from the source of electricity.
• Do not give any medications or liquids unless instructed to by a veterinarian.
Any animal that has suffered electrocution should be taken to a veterinarian, even if there are no apparent complications. Electrocution is a life-threatening emergency. It may cause abnormal electrical activity of the heart or a build-up of fluid in the lungs that could be fatal hours after the shock. Most patients are observed for several hours or overnight to make sure the lungs are normal, and chest X-rays may be recommended.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951327 f79221a5-a111-4deb-a286-beaee15cc0d1.1672705201
VeterinaryPartner.com is not affiliated with Pet Connection.
31 FEBRUARYMARCH 2023

32 FEBRUARYMARCH 2023 Treasure Hunt Where are we going?: Longitude: -119.38907 Latitude: 50.18845 X Over $4000.00 in Treasures to be WON! Treasure Hunt Courtesy of Predator Ridge! Watch for 8 Clues for a Chance to Win a Resort Stay!



33 FEBRUARYMARCH 2023 1,300 Acres of Space | 1 Dog Park | Pet-Friendly Programming A COMMUNITY THAT LOVES YOUR PET JUST AS MUCH AS YOU With 1,000 homes and over 30 years of history, Predator Ridge is the most amenity rich four season community in the Okanagan. There is as much for your pet to do as there is for you! » Pet-Friendly Accommodations » Golf With Your Dog » 35km+ Hiking & Walking Trails » Pet-Friendly Patios & Retail » 1,200+ Events Year-Round LEARN MORE AT PREDATORRIDGE.COM Golf with your dog every Sunday afternoon. 42% of our Homeowners are pet owners.
Eye Injuries: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
If you notice any of the following:
• Your pet squinting or protecting an eye
• Any suspected trauma to the eye
• Abnormal appearance of the eyeball
• Excessive redness to the white part of the eye (sclera)
• Any time the eyelid cannot cover the eyeball
You should seek veterinary attention immediately as these signs can indicate potentially serious eye problems that can risk your pet’s vision.
Conditions like trauma, glaucoma, perforation of the cornea (the clear membrane in the front of the eye), serious infections, foreign bodies and autoimmune diseases can all affect your pet’s eye and may need medical care.

Take care not to get bitten when treating your pet, and use a muzzle when needed to stay safe.
What to Do
• If an eye has been dislocated from the socket (proptosis) or the lids cannot close over the eyeball, keep the eyeball moist with contact lens wetting solution, K-Y jelly, water, or moist compresses.
• If an irritating chemical or other product accidentally gets into the eye, flush it with running water, contact lens saline or homemade saline solution squeezed from a compress or a sponge for a minimum of 15 minutes. (Saline: dissolve 2 teaspoons of table salt in 1 quart of water)
• Always seek veterinary attention immediately. Eyes are quite fragile and just a few minutes could mean the difference between sight and blindness. Referral to an eye specialist (ophthalmologist) may be needed for more severe cases.
What NOT to Do
• Do not attempt to treat the eyes, or remove a foreign object, yourself.
• Do not try to push a proptosed eyeball back into the socket. This must be done under anesthesia so as not to cause damage to the eyeball’s interior.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951329 0c3cd45e-65bb-4a69-af16-8cff9aeead2e.1672858625
VeterinaryPartner.com is not affiliated with Pet Connection.
34 FEBRUARYMARCH 2023
Fainting and Dizziness (Syncope): First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Fainting is the sudden loss of consciousness or a sudden and marked weakness. It may be associated with numerous medical conditions and can be caused by anything from low blood sugar and neurological diseases to heart disease.
What to Do
• Immediately position the pet with the head down and the hind quarters elevated. This will improve brain blood flow.
• Cover the pet with a blanket to preserve body heat.
• If the pet vomits, make sure he does not inhale any of the vomitus into his lungs by keeping his head down.

• Seek veterinary attention.
What NOT to Do
Do not give anything by mouth. It can be aspirated into the lungs and cause serious problems.
• Do not slap the pet or douse him with cold water trying to shock him into consciousness.
• Do not fail to seek veterinary attention just because the animal recovered quickly and seems fine now. Several of the conditions that cause fainting or dizziness are serious and require diagnostic tests in order to determine the cause and prevent future episodes.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951330
3c3a4822-2330-4126-a895-9f89f01854cd.1672858843
VeterinaryPartner.com is not affiliated with Pet Connection.
35 FEBRUARYMARCH 2023
Fever: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Fever is an elevated body temperature that occurs as a response to infection or inflammation (also see hyperthermia). It is a common misperception that fever always indicates infection – this is not the case. It may be due to autoimmune diseases, heat stroke, or cancer as well. Normal body temperature is 101 to 102.5°F for both dogs and cats. The temperature is most accurately taken with a rectal digital electronic thermometer; these usually give results in less than one minute. Lubricate the thermometer with a water-based lubricant (such as K-Y jelly, baby oil or soap), and then insert the thermometer about 1-2 cm (about 1/2 to 1 inch).
Ear thermometers designed for humans do not work well in pets.
What to Do
• Take and record the rectal temperature if you pet feels ill or warm. If it is above 103°F, call your veterinarian or local emergency center. A temperature above 106°F can be life threatening and demands immediate attention.

• If the animal's temperature is over 105.5°F, moisten the pet's hair coat with cold water and pay particular attention to the ears and feet, which are sites of heat exchange. Direct a fan on the moistened areas.
• Encourage (but do not force) your pet to drink small, frequent quantities of water unless she has vomited in the past 4 to 6 hours.
What NOT to Do
• Be careful not to overtreat! Discontinue cooling once the rectal temperature reaches 103°F or the pet may become too cold (hypothermic).
• Do not give aspirin, ibuprofen, acetaminophen or other drugs as many of these are poisonous to pets.
• Do not demand antibiotics from your veterinarian for all causes of fever.
When a pet is lethargic, depressed, shivering a lot, or you see any other reason to suspect that she is not well (not eating, or is vomiting, coughing, has greenish nasal discharge), suspect a fever. The only way to confirm this is to take her temperature using a medical thermometer. Detailed information on taking rectal temperature can be found in the in the temperature section of the Physical Exam Checklist.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951331 99f53e80-3086-43ac-8704-a9c339e9a082.1672859070
VeterinaryPartner.com is not affiliated with Pet Connection.
36 FEBRUARYMARCH 2023
Fractures and Injuries: First Aid
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
Afracture refers to a break or crack in a bone. There are several different types of fractures, and each type has different complications and methods of repair. Your veterinarian can help you decide how best to fix the fracture and if referral to a specialist is in your pet’s best interest. Although splinting will allow a small number of fractures to heal, most will require surgery to ensure the best outcome. Toy breeds of dogs (such as Pomeranians, rat terriers and similar small, longlegged dogs) always require surgery on foreleg fractures due to the high failure rate of splinting.
Fracture Types
Open (formerly known as compound) fracture: Fractures associated directly with open wounds (the bone may or may not be visible through the wound).
Dislocation: An injury to the connective tissues holding a joint in position that results in displacement of a bone at the joint.
Sprain: An injury to a joint, ligament, or tendon in the region of a joint. It involves partial tearing or stretching of these structures without dislocation or fracture.
Other types of orthopedic injuries can involve torn ligaments, particularly in the knee. Many athletic, large breed dogs will tear the cranial cruciate ligament in their knee, which results in a sudden loss of use of the leg, and joint pain and swelling in the knee. Surgical stabilization is the best means to repair this injury.
What to Do
• Before treatment, precautions should be taken to prevent biting injury to the first aid provider. Muzzle your pet.
• Stop bleeding with direct pressure.
• Open fractures should be covered with a sterile gauze dressing if possible. If this is not available, use a clean cloth or feminine pad applied over the opening and bone.
• If possible, the pet should be immobilized on a large board for transport.
• If the pet can still use three legs, support the rear legs with a towel under the abdomen (with the ends held together above the back) used as a sling.
• Discuss treatment options with your vet, including referral to an orthopedic specialist.
• Splinting the fracture at home without pain medication greatly increases the risk of being bitten, and may actually make the fracture worse. Some fractures, such as thigh or femur fractures, cannot be splinted. The best advice is to keep the pet quiet and calm, protect yourself and head directly to a veterinary hospital.
What NOT to Do
• Do not flush the wound with saline or water as this only risks driving contaminants deeper into the wound.
• Never attempt to set or reduce a fracture or try to push a protruding bone back into position.

37 FEBRUARYMARCH 2023
Closed fracture: Fractures in which there is no related external wound.
• Do not give any over-the-counter or prescription medications to your pet unless directed to do so by a veterinarian


A fracture, dislocation or severe sprain may be suspected when the animal suddenly appears lame on a leg, or picks up a leg and won’t use it. These may also be suspected following any major fall or blunt injury. Obvious findings of a bone sticking out from (protruding) a wound are rare. What is more common is the unusual
angle or deformation of the fractured area, and swelling. Accurate diagnosis requires the use of X-rays, which usually must be taken with sedation or anesthesia to get the most accurate results.
An X-ray is the only way to accurately diagnose a fracture.
URL: https://www.slowvetmed.com/pet-library.pml?id=4951333
4c99471b-5f1d-4eee-99eb-10c46b4076b3.1672859518
VeterinaryPartner.com is not affiliated with Pet Connection.

38 FEBRUARYMARCH 2023



Good for all animals, people and the environment! • Natural (no dyes, no salt, no parabens, no phosphates) • Water Based, Extra Hydration (non-oily, non-slip) • PH Balanced, Natural Perservatives • Biodegradable & Hypoallergenic • Naturally soap & detergent free • No petroleum, pyrethrins or alcohol based chemicals Long or Short Because You & Your Pets Deserve the Best! To Order in Canada www.petconnectionstore.ca 250-656-1350
The Many Benefits of Apple Cider Vinegar!
 By Lucy Jabrayan
By Lucy Jabrayan
40 FEBRUARYMARCH 2023
Probably not the most glamorous of ingredients, but for those who know the benefits of ACV will rarely ever go without it!
Although considered an old folk remedy, it has been backed numerous times by science for its numerous health claims.
ACV is a special type of vinegar made out of apples, sugar and yeast, although after the fermentation process there is not much sugar left in it.
ACV can be used in numerous ways, both internally and externally. The great benefit that comes from ACV is because of its fermentation properties, the ‘mother’, as they call it, is the heart of what makes it so glorious. That is referring to the colony in which there is beneficial bacteria, similar to kambucha ‘scoby’ that helps to create vinegar through a secondary fermentation process.
You’re probably going to want to make a trip to the health food store to locate it, or at the grocery store however, make sure you ask for the one containing the ‘mother’, as this is no ordinary grocery store vinegar.
The range of animals it can be used on is quite vast, from our canine and feline pets, to our equine friends, including livestock.
Here are some benefits of using it externally;
• Skin microbiome and coat health.
• Itchy and yeasty paws and skin, by making a soak, using equal parts of water and ACV.
• Insect repellent, including lice.
• Used as an astringent.
• Used for warts.
• Cleaning minor wounds.
• Dry skin patches and hot spots.
Here are some benefits of internal use;
• Great for obese pets, as studies have shown with good results that ACV can help with aiding
• Weight-loss.
• Digestive health.
• Acid reflux
• Lowering blood sugar levels.
• Lowering triglyceride levels (the bad fat in the body).
• Can help ‘keep things at bay’, with its antifungal and antimicrobial properties.
The best way to practise using AVC is to not overdue its use, as there is such a thing as too much of a good thing, because it is so effective, one must use it cautiously, especially with smaller animals, and to constantly take breaks, I have found cycling its use to be best effective with some breaks in between.
Who Should Not Use ACV internally?
Pets or people who are on insulin or on insulin stimulating medications should not take it or at least not in therapeutic doses as it can drop potassium and blood sugar levels to dangerously low levels. Always best to consult your veterinarian or doctor when starting a new regimen.

41 FEBRUARYMARCH 2023
FELINE OBESITY An Overweight Cat Suffers
 By Anne Jablonski
By Anne Jablonski
42 FEBRUARYMARCH 2023
Obesity in cats is not a joke. It’s an extremely serious condition that leads to all kinds of health disorders, including a potentially fatal condition called hepatic lipidosis (fatty liver disease), diabetes, nonallergic skin conditions, and even urinary tract disorders.
Just as important is the effect that obesity has on the ability of a cat to be catlike. As carnivores, cats naturally use stealth and speed to outrun and capture their prey.
An overweight cat is sluggish, weighted down, and she simply cannot partake of her most basic, instinctive behavior. Yes, some cats are just more naturally active than others. But a fat cat has no choice.
Imagine you’re a human whose healthy weight is roughly 120 pounds. And imagine that your most beloved activity–the thing that makes you you–is to run marathons or take long swims or hikes. Then imagine that every day, you are forced to carry around another 40 or 50 or 60 pounds. You’re compelled to do this because the person that has 100 percent control over everything you eat is feeding you a food that makes you carry more and more weight with each passing year. You feel tired, sluggish, and it’s just too much for your joints, your heart, and your lungs to do much more than sit around all day. And imagine that on top of this, you can’t bathe yourself as you’d like. Your skin itches, your blood sugar runs amok putting you at serious risk for diabetes if you don't already have it, and you are at risk for other life-threatening health troubles including urinary disorders.
“actually where the most dangerous calories are.” The cat, she notes, “is uniquely adapted to get energy from protein and fat; the cat’s natural prey contain very little carbohydrate. For most cats, carbohydrates are converted to fat, rather than be burned for energy. Clearly, this is the opposite of where we want to go!”
Dr. Hofve, by the way, has done cat caregivers a magnificently generous favor by maintaining a wonderful, free, online library that is packed with short, easy-to-understand essays on a wide variety of feline health, nutrition, and behavior issues. If you haven’t already perused that site, I strongly suggest bookmarking it and keeping it handy for future reference.
It’s not simply a matter of cutting calories or reducing fat. The concern about doing grave harm to an obese cat by cutting calories and allowing them to skip too many meals is echoed in Dr. Hofve’s article, which notes that “dieting” to reduce calories “may cause even worse problems, such as life-threatening liver disease. Skipping a single meal can throw a sensitive cat into a serious problem.”
Yes, some cats are just more naturally active than others. But a fat cat has no choice.
The message couldn’t be clearer. When it comes to obesity in cats? It’s the carbohydrates that are the culprit.
That is what life is like for an overweight cat. It’s not a pretty picture, is it?
Reducing or eliminating carbohydrates–a good idea for any carnivore, overweight or not–is absolutely essential for safe and lasting weight loss. That is why there is no way to safely reduce an obese cat’s weight using a diet that contains any dry food. Ever. Dry food doesn’t help a cat safely lose weight and never will.
Dr. Jean Hofve hits the nail on the head in her insightful article on feline obesity, observing that dry food is
According to a November 2004 article in Medical News Today summarizing a study funded by the Morris Animal Foundation, Drs. Deborah Greco and Mark Peterson–staff endocrinologists at The Animal Medical Center in New York– demonstrated that feline diabetes, caused by too much fat, occurs most often in obese cats. Most importantly, the results of the study showed that diabetic cats on the “Catkins” diet often can ditch daily insulin shots altogether. So? Getting an obese cat to safely lose weight is not only critical to keeping your cat feeling well and cat-like, but is critical to help avoid a costly and miserable malady like diabetes. The same Medical News Today article observed that the traditional approach of giving diabetic cats a high-fiber diet to help them lose weight may help the cats lose fat, but the animals also lose muscle. A far more sane choice is a low-carbohydrate/high-protein diet.
Patients at The Animal Medical Center and Colorado State University participated in a clinical trial and of the
43 FEBRUARYMARCH 2023
cats on the high-protein diet, a remarkable 68 percent went off insulin. Dr. Greco noted that the high-protein fare worked best because it is similar to what cats in the wild would eat.
Again? Common sense prevails. Using Mother Nature as a guide is the wisest way to approach dealing with all kinds of feline ailments.
“The thing that convinced me that this was the right diet was the improved quality of life for these cats,” Dr. Greco says. “They became kittens again.”
Okay, so just for kicks, let’s look at the nutritional breakdown of a mouse carcass–something that is akin to the food that oh-so-wise Mother Nature intended for carnivores. A mouse carcass is about three percent carbohydrate. Dry cat food? It has between 35 and 50 percent carbohydrates. And what happens if you feed a cat more carbohydrates than she was anatomically designed to eat? Dietary carbohydrate that is not used for energy is stored as fat. It doesn’t take a degree in nutrition to figure out that if you put an obligate carnivore on a highcarbohydrate diet, she is going to become obese more easily than a cat on a low-carbohydrate diet.
On her lovely website, Dr. Lisa Pierson says it more succinctly than I ever could: “Carbohydrates are minimally used for energy and those that are not used are converted to and stored as fat. The so called ‘light’ diets that are on the market have targeted the fat content as the nutrient to be decreased, but in doing so, the pet food manufacturers have increased the grain fraction, leading to a higher level of carbohydrates. Hence, many overweight cats eating these diets are still obese. These ‘light’ diets are among the most species-inappropriate, unhealthy diets available to cat caretakers. Many caretakers feed very small amounts of these diets hoping that their cat will lose weight but feeding a small amount of a diet that is inappropriate for the species is NOT the answer! The caretaker simply ends up with a crabby, overweight cat.”
will come as no surprise that I think a home-prepared, balanced, grain-free raw diet like the one I recommend on this site is the very best way to go. Or you could purchase a truly quality pre-made raw diet that contains no grains or vegetables. Cats are carnivores. They have simple stomachs that are made to digest meat–not grains or vegetables. They don’t have salivary amylase to break down plant matter in their mouth.
And look at the beautiful teeth of a cat! Those lovely, sharp, prominent canines are there for stabbing. The entire structure of a cat’s mouth is designed to shear off chunks of meat and swallow it whole. Those raspy tongues can lick the meat off of bones. Instead of grinding molars that move back and forth, a cat has carnassial back teeth that act like scissors to slice off flesh. Look at the pads of your cat’s feet. They are ringed with fur because Mother Nature designed her to stalk silently and come closer to her prey. Her whiskers allow her to move confidently in darkness and guide her to the nape of the neck for a killing bite.
Cats are carnivores. And getting your cat on the diet nature intended is the finest way to get her back to her true, svelte, self.
Cats are carnivores. And getting your cat on the diet nature intended is the finest way to get her back to her true, svelte, self. Feeding her carbohydrate-heavy, meatflavored cereal will keep her fat and abbreviate the quality and quantity of her life.
If you’re not willing or able to make a home-prepared diet, then please safely wean your cat your cat off of all dry food and move her on to a quality canned food that has minimal or no grains. Once she’s eating a good canned food, don't give her dry food again.
If you have a devoted and stubborn dry food addict on your hands, the first thing to do is to stop free-feeding kibble. This is absolutely essential.
So? What should you feed? If you’ve already spent any time looking at the other parts of my website, it
Having food available 24/7 is NOT a good idea for any cat, and if your cat has constant access to that food, you’ll have a very hard time getting her weaned onto a healthier, low-carbohydrate, moist, high-protein canned food. One way to approach this is to offer two or three meals a day of a very small amount of dry food (perhaps 1/8 to 1/4 of a cup) and, after 30 minutes,
44 FEBRUARYMARCH 2023
take up the food she hasn’t eaten. Then do not give in if she pleads for a between-meal snack. You want your cat to get accustomed to eating on a schedule this way–at mealtimes.
You MUST stop free-feeding dry food.
Next, after you’ve established set meal times for a few days or a week, begin setting out meals of ONLY good canned food. If your cat refuses to touch it, take up the food and try again a few hours later.
Yes, it takes some patience to get a cat off of dry food and onto something healthier, but think how much time it would take if your cat develops diabetes or some other disease and you’re forced to spend time, money, and energy coping with that.
If, after 18 hours or so, your cat still has refused canned food, then offer them a tiny bit of dry food–about a tablespoon. At this point, you may have to try serving another kind of canned food to see if she’ll try that. Another trick is to generously sprinkle some of the crushed dry food onto a quarter cup of the canned food and offer that and then, over a period of two to three days, start using less and less of the crushed kibble and more and more of the canned. You will be the best judge of how quickly to do this, based on how your cat is adapting.
Another trick is to dip some of the dry food into the 'juice’ of canned food to begin to accustom her taste buds to the taste of the better food.
The idea here is simple and tricky at the same time. You want to get your cat moved on to a good, preferably grainless, canned food as quickly as possible, but you do not want to starve her into submission and risk hepatic lipidosis by permitting her to go without any food whatsoever for longer than 18 to 24 hours. It’s not very safe to let an overweight cat go longer than 24 hours without food. Hepatic lipidosis becomes a serious concern once an overweight cat has gone without food for 48 hours.
Hepatic lipidosis is a condition in which fat accumulates in individual liver cells and is a real risk for overweight cats that stop eating altogether. Without food, the body starts sending fat cells over to the liver to process lipoproteins for fuel. Lipoproteins are
composed of a simple protein and a fat component that carry fats in the blood. Left untreated, the liver can fail and the cat can die. The veterinary literature suggests that about 70 percent of cats will recover from hepatic lipidosis if they are hospitalized and fed via tube feedings. Who wants to put their cat through that? No one. So, again, remember that starving an overweight cat is not an option. They cannot ‘live off their fat.’ Their fat, in fact, can kill them. So be mindful of this as you approach a sensible weight loss program for your fat cat.
Ideally, your feline weight loss client should eat at least a little something every 12 hours. It really is okay to let her go 12 hours without food; hopefully a bit of hunger will help as an incentive to get her to eat healthier, nondry, food. Once she is successfully switched over to a high-protein, low-carbohydrate diet and is off of all dry food, then begin to feed her two to three small meals of canned food a day.
Remember, even the worst canned food is better than dry food, because it will invariably be lower in carbohydrates and have much more moisture in it. The water in canned food is not a wasted, useless, filler that’s only there to take up space. It’s insurance that a cat is getting her moisture with her food, as nature intended. A cat eating dry food, even if she is drinking supplemental water, still has roughly only half the water intake of a cat eating canned food.
One of the most heartwarming stories I’ve heard is of a very lovely, gentle, sweet cat named Molly. When she first arrived in her foster home, Molly was grotesquely overweight. Her previous ‘caregiver’ had tried using “portion control” with dry food–and even a shock collar–to get Molly to eat less of her dry food and lose weight. These approaches, naturally, didn’t work.
When she
started at Dr. Pierson’s Fat Camp for Wayward Cats, Molly weighed over 20 pounds...
Read Molly’s story on page 41...
45 FEBRUARYMARCH 2023
46 FEBRUARYMARCH 2023
Molly's Story
Molly before...
Poor Molly could hardly walk carrying around all that extra weight. She had terrible dandruff and could not even manage to keep her back end clean. We know how naturally fastidious a cat is about personal hygiene. Just imagine how awful it is for a cat that is unable to clean herself.


She couldn’t run. Heck she could barely move. Her foster caregiver – Dr. Lisa Pierson as luck would have it–pulled out all the stops for Molly. She took away the dry food and started her on a ‘tough love’ program to get her eating only a grain-free canned food. And it wasn't easy. Molly’s metabolism was a mess and she simply refused her food. Because her condition put her at serious risk of hepatic lipidosis and because Dr. Pierson was well-versed and had the skills, she safely syringe-fed Molly a good canned food, and continued feeding her that way for a time so she could start getting regular, nutritious meals. After that, Molly slowly started showing an interest in food again.
Slowly, steadily, over time, Molly’s weight began to drop–and it continued. She lost weight eating 5.5 ounces each day of a good quality grainless canned food. (There’s an excellent list of the better grainless canned foods on Dr. Lisa Pierson’s website.)
...and Molly after, well on her way to her appropriate weight.
Once Molly was on the right track, Dr. Pierson found her a loving home with a very devoted and committed caregiver who understands how important it is to keep her off all dry food, and ensure she continues to eat only the grainless, canned food that helped her begin to drop all that terrible extra, unhealthy weight that the poor sweetheart had been carrying.
When she started at Dr. Pierson’s Fat Camp for Wayward Cats, Molly weighed over 20 pounds. Five and a half months later, Molly weighed around 16 pounds. A few months after that–under the loving eye of her new caregiver who stuck with the grain-free diet and has kept Molly away from all that fattening and dangerous dry food–Molly weighed in at under 15 pounds. This means that since beginning her weight loss program, she safely lost over 26 percent of her body weight.
She is now well on the way to being the correct size for her frame. For the first time in ages, she can clean herself. Her coat is sleek, silky, and altogether lovely. And the happiest news of all is that her new caregiver reports that Molly is running and jumping again. She can even stand on her hind legs.
Molly was able to be a real cat again.
47 FEBRUARYMARCH 2023
Rescuing the Underdog
By Kim Federico
In animal rescue, the one thing you learn extremely fast is that the work never stops. You might think, during a moment of quiet, that you finally have a chance to take a break, but then out of nowhere a litter of puppies appears and they end up in your kitchen. But even though the work is exhausting and seemingly never ending, it is also often the reason that you get up in the morning and feel fulfilled at the end of the day. At least that’s how it is for the volunteers who run HugABull Advocacy & Rescue Society. Founded in 2003 by a group of strong-minded, intelligent and passionate women, HugABull is committed to rescuing pit bulltype dogs (or bully breeds, as we prefer, since pit bull is an umbrella term) from local shelters and working to change the way the world feels about them. While the faces at HugABull have changed many times over the years, the mission has remained the same, and we have been fortunate to grow as an organization, expanding our reach by offering several truly special programs to better support our communities.
Why bully breeds?
Bully breeds are the underdogs of the dog world, and unfairly so. As a result of breed stigma and irresponsible ownership, bully breeds are by far the most surrendered and abused dogs within the shelter system. But there is so much to love about them – the majority of bullies that we’ve come across are affectionate, the best cuddlers, goofy, people-oriented and unconditionally loving – not even close to the image that's portrayed in the media. However, as a result of their bad rap, they suffer at the hands of humans in so many ways. They attract the wrong people. Unfortunately, because of their reputation, bully breeds attract irresponsible owners who want dogs that seem tough and mean. In fact, the biggest predictors of whether a dog will be aggressive are poor breeding, improper training,

48 FEBRUARYMARCH 2023

49 FEBRUARYMARCH 2023 Diego


50 FEBRUARYMARCH 2023
Mavis at home (above), Mavis at the shelter (right inset)
insufficient socialization during development and improper behavioral management by owners. When bully breeds are tested on The American Temperament Test, which is the gold standard in canine temperament testing, they have some of the highest pass rates (86%) and are amongst the top ten most tested breeds. The bottom line is that poor treatment of any dog of any breed will result in bad behavior.
Bully breeds are victims of Breed Specific Legislation (BSL). Despite having clear evidence that it is ineffective, inhumane and very expensive, many cities still implement BSL,which entail varied practices ranging from mandatory muzzling, leashing and containment restrictions, higher licensing fees, higher penalties for violations, mandatory liability insurance, mandatory spay/neuter, automatic euthanasia in shelters, and even complete breed bans. It is important to point out that BSL is not supported by organizations like the Canadian and American Kennel Clubs, the BC and Canadian Veterinary Associations, Humane Societies, and the SPCA.
Why doesn’t BSL work? You can’t, with any degree of certainty, determine a dog's breed through visual identification, and abiding by laws that use such methods is fundamentally flawed. BSL is also very expensive as it poses additional legal challenges and requires more animal control services. And let’s be real,when it comes
to compliance, irresponsible owners are unlikely to abide by such laws, which means that BSL is more likely to punish responsible dog owners.
So what does work? Promoting responsible ownership and addressing dog behavior holistically reduces the number of dog attacks. We can leave breed out of it. At the end of the day, owners need to be held accountable for their dogs and their behavior, not the other way around.
Bully breeds are villainized by the media. There is an undeniable bias towards ‘pit bull’ stories in the media. In fact, many news websites use them as clickbait. However, the reality is that there is absolutely no scientific evidence to suggest that bully breeds attack more often, or more severely, than other breeds. Unfortunately, that's the impression that the public is left with when the only dog attacks that are reported on the news involve bully While more progressive media outlets are choosing to leave dog breeds out of their stories altogether, it is an uphill battle. That’s why HugABull works so hard to change the perception of bully breeds by promoting responsible ownership, educating the public and adopting out breed ambassadors.
Throughout the years, we have come across bullies who have endured immense trauma – dogs that have been beaten, burned, starved, attacked by other animals, who


51 FEBRUARYMARCH 2023
If it’s too cold for you, it’s too COLD for them. Don’t let them suffer… bring them indoors!
were injured and left for dead. We welcome these bullies into our program and are continually amazed at their resiliency and ability to remain so loving. This is why we fight so hard for them.
Where do our dogs come from?

While we serve the entire province of British Columbia, our rescue efforts often take us from one end to the other and sometimes even to other parts of Canada. HugABull works primarily with local shelters in a supportive capacity, taking in high-need medical cases, terminal dogs, dogs with behavioral issues, as well as those who cannot cope with kennel life. We also work with several reputable rescues and occasionally accept owner surrendered dogs on a case-by-case basis.
HugABull prioritizes helping bully breeds in Canada and therefore we do not take in dogs from other countries.
We believe that the public holds themisconception that Canada doesn’t have a dog overpopulation problem, or that dogs in Canada are treated better than in other countries, but that's not true. We have entered a companion animal crisis of sorts. Shelters across the country are bursting at the seams and the number of homeless animals is at an all-time high. Dogs are being abandoned, they are starving and dying outside, and they are also being culled in parts of Canada. For these reasons, we are proud to support our local Canadian dogs.
We are incredibly grateful for the relationships we’ve built with our local shelters and especially our partner rescues – Bully Buddies, Bullies in Need, The Farm Rescue and Victoria Humane Society. We are so thankful to work alongside such wonderful people as these relationships are invaluable and enable us to collaborate to transfer dogs to one another and share resources, as we work towards the same goals.
52 FEBRUARYMARCH 2023
Lexi and pups
What do we do?
The past year has been a busy one for HugABull and we successfully rescued/fostered/adopted/transferred a total of 104 dogs! This is something we are extremely proud of considering we’re an entirely volunteer-run, non-profit and are funded solely by donations, fundraising efforts and grants. What’s special about our rescue program is that all of our dogs reside in foster homes until they find their forever homes. We hope that someday we will have a physical facility to alleviate some of the challenges we face at times, like needing emergency foster spots for dogs, the ability to provide further assessments, the convenience of having storage space, and being able to utilize additional volunteers. For now, however, that remains a dream. When we welcome dogs into our care, they spend the first month decompressing with their new foster family which gives us enough time to get to know them, and understand what their needs are before we begin looking for their


forever family. We cover the costs of all of their care (food, supplies, vet care- you name it) which allows our foster families to focus on providing a loving, caring home. To date we have adopted over 1500 wonderful breed ambassadors to responsible and loving homes!
One of our most meaningful programs is our Compassion Care program. Sometimes we take a dog out of the shelter only to learn that a medical issue is more serious than anticipated. Other times, we knowingly take dogs into our program that have terminal illnesses so that they can live out the rest of their days in the comfort of a loving home, and where we can ensure that they receive the best care possible. This past year we lost three of our Compassion Care dogs, Marvin, Diego and Mavis. Diego came into our program at 15 years old when his owner couldn’t care for him any longer – he passed peacefully at the incredible age of 17. Marvin came to us after being found as a stray and was

53 FEBRUARYMARCH 2023
Fridget and foster Angus Therapy Dog
Breed Ambassador Pirate
diagnosed with a debilitating mobility issue. Although he was only with us for a year before he crossed the rainbow bridge, he touched the hearts of so many. Mavis was a severely neglected senior with the kindest soul. She was diagnosed with terminal cancer and spent her last months with a family who treasured every minute she was with them. Another Compassion Care dog, Ted, has been with HugABull for over three years after being diagnosed with an aggressive cancer and we are grateful for every day that he’s with us.
Last year we created a new program called Canines in the Community. We wanted to offer free training support, education, and resources to dog owners in an effort to build safer communities. We believe that by providing these services at no charge we can help to remove any barriers that may prevent dog owners from receiving professional help. On a monthly basis, HugABull runs reactive dog classes led by Certified Professional Dog Trainers from Magnolia Dog Training. These classes are open to all breeds and the feedback that we’ve received has been incredibly positive. We also offer a free collar exchange program that allows people to exchange their aversive training collar – which HugABull disavows – for a brand-new harness. We also plan on hosting low-cost spay and neuter initiatives in various cities where we know pet overpopulation is an issue. Our programs are always evolving as we try to meet the needs of our communities.

We were extremely excited when we launched the Reach Program in 2021 as a way of giving back and sharing our resources with those in need. We work with vulnerable populations to provide food and supplies, low cost spay/ neuter initiatives and veterinary care assistance. Up to now we have successfully spayed/neutered over 70 pets and have distributed thousands of pounds of food and supplies! Most importantly, through Reach we have built positive relationships with several new communities, including SROs on the Downtown Eastside, and several Indigenous communities throughout the Fraser Valley. To expand on this success we plan to start a new branch of Reach which we are calling Indigenous Reach. We recognize that there is a strong need for support in many of our local Indigenous communities and we are really passionate about helping in whatever ways we can. For example, in BC, December was especially cold this year and we partnered with the Hope Pet Food Bank to
supply straw and food for many animals in the area. It really does take a village sometimes.
HugABull is truly a team effort and none of what we’ve accomplished could have been possible without our incredible volunteers and donors. As a charity that relies solely on the kindness and generosity of others, we are eternally overwhelmed and grateful for the support we receive, and the many forms it comes in. It is so easy to get lost in the flurry of dogs that we encounter through our programs, but when we finally have a moment to step back and reflect, we are truly amazed at what HugABull has accomplished (on top of our full-time jobs). Funnily enough, as we finish writing this very article, eleven puppies and their mama sleep soundly at our feet, rescued from an abandoned house the night before. Our hearts are full knowing brighter days lay ahead of them and that we were able to play a part in their journey to a better future.

54 FEBRUARYMARCH 2023
Piper and Tucson
Reach Support
FEBRUARY 2023 Sporting Detection Events Take Place all Year Visit sportingdetectiondogs.ca for locations near you.

Wednesday February 1st, Clue # 2 for the 2023 Treasure Hunt will be on our Social Media.

Tuesday February 14th Valentines Day

MARCH 2023
Wednesday March 1st, Clue # 3 Will be released for the 2023 Treasure Hunt on our Social Media

TREASURE HUNT CLUES

55 FEBRUARYMARCH 2023
The Pet Connection assumes no responsibility for any information listed for any of these events. While every attempt is made to double check information submitted, we are not responsible for any cancelled events, rescheduled events, wrong dates or times, location changes, wrong address’s or wrong phone numbers. If you have an event you would like to mention, please submit it to,
. Due to space limitations there is no guarantee that it will be listed. Follow us on Facebook PetConnectionCanada Follow us on Instagram Petconnectionmagazine Follow us on Twitter
Mail to: Pet Connection 2443 Beacon Avenue Sidney, BC V8L 1X7 Or order online with Paypal. See the subscription section on our website: www.petconnection.ca/subscriptions Name: _____________________________________ Email:_________________________________ Address: City, Province: ________________________________Postal Code:___________________________ Amount Enclosed (In Dollars): PRINT SUBSCRIPTIONS ARE ONLY $25.00 for 1 year or BONUS $40.00 for 2 years! Never miss an Issue!
Do you have all the Clues for the Treasure Hunt? Clue # 1 Where are we starting? Clue # 2 Where are we going?
info@petconnection.ca
@PetConnectionCa
FINN AND FLETCHER
Finn and Fletcher is Canada’s Online Store for Pets! www.finnandfletcher.com
RULES
Contest is only open to Canadian pets alive and living in Canada. If you have multiple pets, you can send in multiple photos, but please only one photo per pet per month.
Prizes must be accepted as awarded. No purchase required.
PHOTO SIZE: your jpg (photo) must be over 1MB in size to be considered.

Preference will be given to photos that have room above the pet. Please no professional photographers. To enter, email a high resolution photo of your pet to: info@petconnection.ca
information: www.petconnection.ca


56 FEBRUARYMARCH 2023
$4.95 Display until March 31, 2023 Made in Canada Proudly
2023
PHOTO CONTEST FOR DOGS
Canada’s Natural Health Magazine for Pets FEBRUARY-MARCH
Your dog can be on a magazine cover!
PROUDLY SPONSORED BY
Grand Prize Winner of the 2023 Dog Photo Contest will be announced on December 15, 2023!
Please visit our website for more
&
Contest Winner in 2022!
Waylon
Angus Dog Photo














57 FEBRUARYMARCH 2023 PetConnectionCanada TheFinnandFletcherCo Petconnectionmagazine finnandfletcherco @PetConnectionCa 2023 Photo Contest FOLLOW US BOTH! #chanceforthecover #finnandfletcherco #petconnectionmagazine
September Open
entries
WIN A $500.00 ONLINE SHOPPING SPREE FOR YOUR DOG! Visit www.finnandfletcher.com and see what you could order if you win! Monthly Prizes Get a Mini Spree! $50.00 to spend!
Dog Photo Contest runs January 1, 2023 to December 15, 2023. The Grand Prize Dog Winner will be chosen from our Monthly Winners below. July Open to entries from dogs living in Canada. August Open to entries from dogs living in Canada. February Open to entries from dogs living in Canada. January March Open to entries from dogs living in Canada. April Open to entries from dogs living in Canada. May Open to entries from dogs living in Canada. June Open to entries from dogs living in Canada. November Open to entries from dogs living in Canada. October Open to entries from dogs living in Canada.
to
from dogs living in Canada. December Open to entries from dogs living in Canada.
PHOTO CONTEST FOR Cats
RULES
Contest is only open to Canadian pets alive and living in Canada. If you have multiple pets, you can send in multiple photos, but please only one photo per pet per month.


Prizes must be accepted as awarded. No purchase required.
PHOTO SIZE: your jpg (photo) must be over 1MB in size to be considered.
Preference will be given to photos that have room above the pet.
Please no professional photographers. To enter, email a high resolution photo of your pet to: info@petconnection.ca
58 FEBRUARYMARCH 2023
Your cat can be on a magazine cover!
visit our website for more information:
PROUDLY SPONSORED BY IRON WILL RAW Monthly Winners! Grand Prize Winner will receive $500.00 worth of Prizes from Iron Will Raw!
Please
www.petconnection.ca
Sloop Cat Photo Contest Winner in 2022!
February Open to entries from dogs living in Canada.
January March Open to entries from dogs living in Canada.
April Open to entries from dogs living in Canada.
December Open to WIN Over $500.00 Worth of Prizes From Iron Will Raw! Cat Photo Contest runs January 1, 2023 to December 15, 2023. The Grand Prize Dog Winner will be chosen from our Monthly Winners below.



May Open to entries from dogs living in Canada.

July Open to entries from dogs living in Canada.
August Open to entries from dogs living in Canada.
June Open to entries from dogs living in Canada. November Open to entries from dogs living in Canada.
October Open to entries from dogs living in Canada. PetConnectionCanada IronwillRaw Petconnectionmagazine ironwillraw @PetConnectionCa


entries













from dogs living in Canada.
September Open to entries from dogs living in Canada. FOLLOW US BOTH! #chanceforthecover #ironwillraw #petconnectionmagazine
59 FEBRUARYMARCH 2023
2023 Photo Contest
BRITISH COLUM
4 Paws Pure 3110 15th Avenue, Prince George, BC Amore Pet Foods 4540 Hastings Street, Burnaby, BC
Healthy Spot Pet Nutrition #5 - 1050 - 10th Avenue, SW Salmon Arm, BC

Healthy Spot Pet Nutrition 3115 48 Avenue #200, Vernon, BC
Healthy Spot Pet Nutrition #12 - 1516 Fairfield Road Victoria, BC
Pawsitive Veterinary Care Clinic 500 - 1950 Harvey Avenue,
Pet Connection Head Office & Retail Store 2443 Beacon Avenue, #100 - 1135 Stevens Road, West Kelowna, BC

Simply Natural Raw Pet Food 5565 West Blvd, Vancouver, BC

60 FEBRUARYMARCH 2023
Single Issues are available at www.issuu.com Single Digital Issues available. Only $2.99 CDN 100% in Canada
Digital
Print copies available at select locations.
ALBERTA
AARCS
Safe Haven and Veterinary Hospital 5060 - 74th Avenue SE, Calgary, Alberta
AARCS
North Haven 8108 Coronet Road NW, Edmonton, Alberta
Edmonton Holistic Veterinarian Clinic 8215 - 102 Street, Edmonton, Alta.
SASKATCHEWAN
Fido & Felix Foods We Deliver all across Saskatchewan
MANITOBA
Head to Tail Canine Nutrition www.headtotailcaninenutrition.com
ONTARIO
Bones Pet Boutique 1500 Upper Middle Road, Burlington, Ont.
The Hungry Pooch - Lakeshore 486 Advance Blvd, Tecumseh, Ont.
The Hungry Pooch 2451A Dougall Avenue, Windsor, Ont.
Thor’s Healthy Pet Foods 3-3840 Dominion Road, Ridgeway, Ont.
Thrive 4 Life Holistic Pet Food Store 16572 York Durham Line, Whitchurch-Stouffville, Ont.
QUEBEC
Only available by subscription. In English only.
NEW BRUNSWICK
Only available by subscription.
PRINCE EDWARD ISLAND
Blue Ribbon Pet Supply and Grooming 420 Queen Street, Charlottetown, PEI
NOVA SCOTIA
Valley WAAG Animal Shelter 12-112 Front Street, Wolfville, Nova Scotia
NEWFOUNDLAND
The Doghouse 204 Duckworth Street, St. John’s, NL
NORTHWEST TERRITORIES
Borealis Kennels & Pet Supplies Box 2195, Yellowknife, NT
NUNAVUT
Iqaluit Humane Society PO BOX # 11089, Iqaluit, NU
YUKON TERRITORY
Humane Society Yukon 126 Tlingit Street, Whitehorse, YT
The Feed Store Pet Junction 9006 Quartz Road, Whitehorse, YT












61 FEBRUARYMARCH 2023
Follow us on Facebook PetConnectionCanada


Trusted since 1992


Visit us at www.petconnection.ca


Follow us on Instagram Petconnectionmagazine

62 FEBRUARYMARCH 2023
Follow us on Twitter @PetConnectionCa WE COULDN’T DO IT WITHOUT YOU.



Canada’s original WHOLE ANIMAL raw food diets SPECIES APPROPRIATE TM FRESH FROZEN WHOLE ANIMAL DIETS FOR DOGS AND CATS WHOLESOME FOOD SUPPLEMENTS OMEGA FATTY ACIDS SKIN & JOINT CARE PRODUCTS to promote wellness from the inside out! www.carnivora.ca Proudly MADE IN CANADA












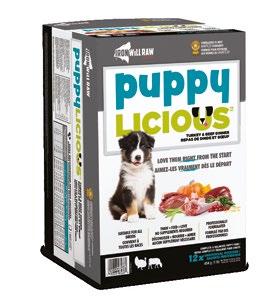














 By Roger Gfeller, DVM, DACVECC; Michael Thomas, DVM; Tony Johnson, DVM, DACVECC
By Roger Gfeller, DVM, DACVECC; Michael Thomas, DVM; Tony Johnson, DVM, DACVECC



 By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants
By Dr. Roger Gfeller, DVM, DACVECC; Dr. Michael Thomas, DVM, The VIN Emergency Medicine Consultants













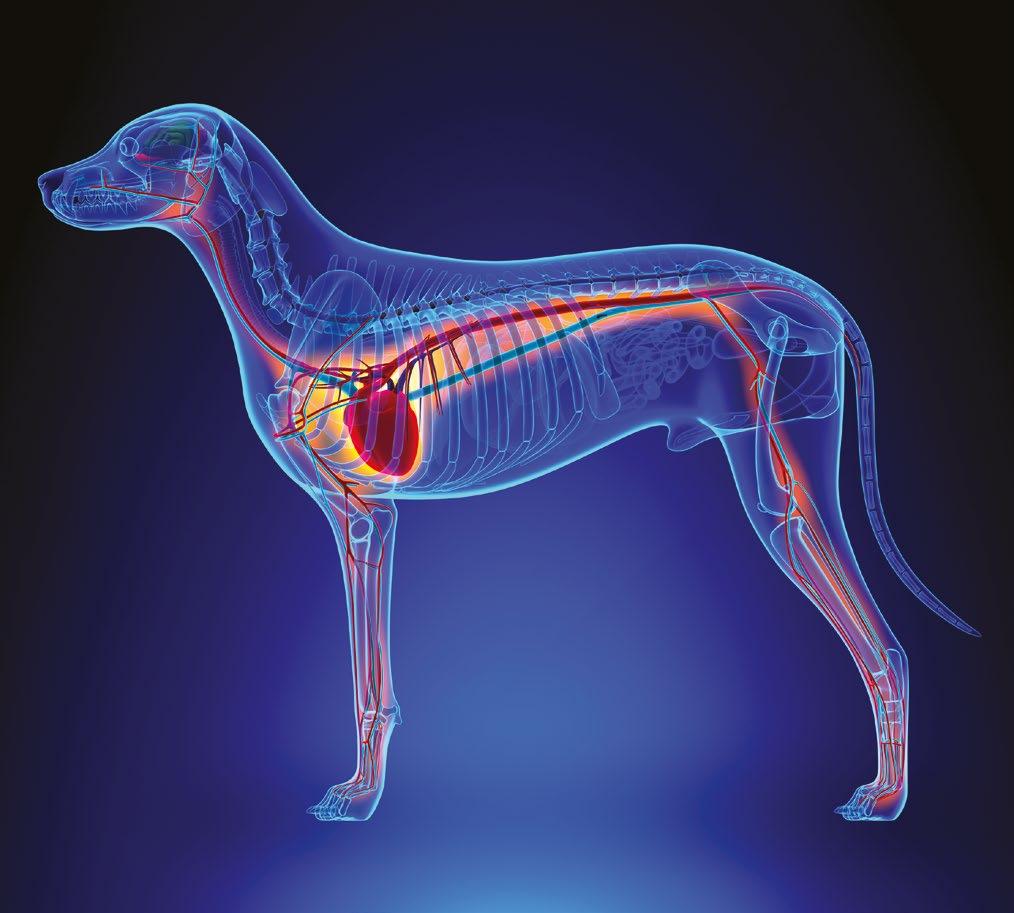



















 By Lucy Jabrayan
By Lucy Jabrayan

 By Anne Jablonski
By Anne Jablonski