

Foot Print
Bulletin of the British Orthopaedic Foot and Ankle Society





5 F rom T h E pr E sid E n Tro BE r T cl Ay T on
7 F rom T h E E di T orJi TE ndr A mA ngw A ni
8 A B ri EF his T ory o F B o FA s T im E
The story of the society's evolution from a nascent idea to a vibrant forum over the past five decades.

CONTENTS


16 puzzl E corn E r
18 pl A nning F or A n unpl A nn E d r ET ir E m E n T
28 p E rcu TA n E ous pos TE rol ATE r A l
m A ll E ous F ix AT ion
How percutaneous posterior to anterior screw fixation enables a safe method of reduction and stabilisation of the posterolateral fragment.
30 Th E mE di A l p os TE rom E di A l
Appro A ch in p os TE rior mA ll E ol A r
Fr A c T ur E Fix AT ion: sAFE r
Exposur E , i mprov E d rE duc T ion, A nd B ETTE r o u T com E s
The advantages and increasing evidence to support the medial posteromedial approach (MPM) over the more common posterolateral (PL) approach.to posterior malleolar fractures (PMFs).
45 T h E F irs T B o FA s r E s EA rch d Ay 46 ho BB i E s corn E r 18 22
Foot print is the Bulletin of the British orthopaedic Foot and Ankle society
Edited by Professor Jitendra Mangwani. Associate Editors - Mr Graham Chuter, Miss Verity Currall. Assistant EditorsMr Munier Hossain, Mr Kailash Devalia
BoFAs
Company Registration Number: 01610419
Charity Number: 326114
General enquiries: administrator@bofas.org.uk
34 A Fully Endoscopic T E chniqu E
F or Tr EAT ing rE c A lci T r A n T
p l A n TA r F A scii T is
Historically, the results of heel pain surgery often result in some degree of residual pain - possibly due to not addressing all the pain generators during surgery. Therefore, introducing the DORR (Debridement, Ostectomy, Release and Radiofrequency) procedure.
36 s ETT ing up A privATE pr A c T ic E
Key tips, questions to ask yourself and advice to know about, when setting up a private practice.
38 p A r T n E r soci ET y m E ss A g E s
open Box media & communications
l Director Stuart.Walters@ob-mc.co.uk
l Director Sam.Skiller@ob-mc.co.uk
l Studio Manager Mark.Lamsdale@ob-mc.co.uk
l Production Matt.Hood@ob-mc.co.uk
l Advertising Sales Andrew.Hull@ob-mc.co.uk
A personal story of dramatic change in the life of a Consultant foot and ankle surgeon and lesson learned.
22 chronic A chill E s rup T ur E : A nov E l TE chniqu E
A minimally invasive approach to chronic Achilles tendon repair.
40
Foo T A nd Ankl
s urg E ry Evidence from the BOFAS Registry. 42
44 v isu A lis AT ion in o r T hop AE dics How to convert complex procedures into routine work with visualisation.
Foot Print is produced on behalf of BOFAS by Open Box Media & Communications, Premier House, 13 St Pauls Square, Birmingham B3 1RB. T: 0121 200 7820.
For sales or design services, please discuss your requirements with a member of our team.
disclaimer Open box
The articles and advertisements in this publication are the responsibility of the contributor or advertiser concerned. The publishers and Open Box Media and Communications Ltd and their respective employees, officers and agents accept no liability whatsoever for the consequences of any inaccurate or misleading data, opinions or statement or of any action taken as a result of any article in this publication.
We are committed to sustainable forest management and this publication is printed by Buxton Press who are certified to ISO14001:2015 Standards (Environmental Management System). Buxton prints only with 100% vegetable based inks and uses alcohol free printing solutions, eliminating volatile organic compounds as well as ozone damaging emissions.


Tensionable and Knotless





Dear BOFAS members, friends and colleagues... WELCOME
BBOFAS Pre S ident, r OB ert CLAY t O n


OFAS continues to go from strength to strength. In writing this I must pay tribute to the Editor Jit Mangwani and his team who have created and maintained the success of this unique global platform of communication and collaboration in the foot and ankle community.
One key development in BOFAS this year is the move to make “The Foot” journal, once more, the official journal of the BOFAS. Under the editorial leadership of Tim Clough, the journal is already greatly increasing its reach and Impact Factor. Our goal is for this journal to become one of the world's leading foot and ankle surgical publications. Please do consider “The Foot” for submission of your research, and getting involved as a reviewer, editor or author of special articles.
Throughout 2025, BOFAS has continued to attempt to work with the Royal College of Podiatrists to follow up from

the Memorandum of Understanding, which was signed last year. This document set out the fundamental differences in governance, training, regulation, scope of practice, and title between orthopaedic surgeons and surgical podiatrists, and we continue to try to resolve these issues.
BOFAS has now formed the “BOFAS Global working group” which will run all the BOFAS humanitarian activities and overseas courses, which will be led by Graham Chuter.
In January 2026, we launch our new webinar series. This follows from on from the success of the “Lectures of Distinction” series created during the pandemic years. The new series, “Practice Ready Orthopaedic Foot & Ankle Surgery - PROFAS”, is aimed at registrars and new consultants. It will cover the entire range of foot and ankle conditions.
Sadly, tragedy is never far away. This year, we have had to mark the untimely deaths of my counterpart in the German Association for Foot and Ankle Surgery, Christina Stukenborg-Colsman, who many will remember speaking at our last meeting. We have also had the sudden deaths of AOFAS president Michael Aronow, and closer to home, of Graham Dall, consultant orthopaedic foot and ankle surgeon in the Borders in Scotland.
On a happier note, I look forward to welcoming everybody to Glasgow for the final part of the BOFAS 50th anniversary celebrations. The meeting will have the theme “Keeping out of Trouble” and will be packed with special tips and tricks which you will be able to incorporate into your own practice. Of course, there will also be the anticipated opportunities to catch up with friends both in the conference, at the gala dinner and throughout the remainder of the social programme. n

OrthoBiologics



Committees
Council Membership:
President: Robert Clayton
President Elect: Hiro Tanaka
Immediate Past President: Mark Davies
Honorary Secretary: Jitendra Mangwani
Treasurer: Callum Clark
Media & Comms Director: Karan Malhotra
Education Committee Chair: Anna Chapman
Clinical Practice Committee Chair: Joel Humphrey
Scientific Committee Chair: Dave Townshend
Chief Operating Officer: Jo Millard
Trustee: Steve Hepple
Trustee: Steve Bendall
EFAS Representative: James Ritchie
EDI Lead: Lauren Thomson
Clinical Practice Committee Membership:
Chair: Joel Humphrey
Secretary: Nilesh Makwana
Caldicott Guardian: Jitendra Mangwani
Data Protection Officer: Jo Millard
Member: Tim Clough
Member: Ben Hickey
Member: Shilpa Jha
Member: Robbie Ray
Co-opted Registry Lead: Lyndon Mason
Co-opted Registry Lead: Ed Wood
Co-Opted: Andy Goldberg
Co-Opted: Karan Malhotra
Education Committee Membership:
Chair: Anna Chapman
Secretary: Graham Chuter
Member: Maneesh Bhatia
Member: Jim Carmichael
Member: Yaser Ghani
Member: Rajesh Kakwani
Member: Nikki Kelsall
Member: Julie Anne Kohls
Member: Krishna Vemulapalli
Member: Matthew Welck
Overseas Comm: Tim Williams
Simulation Working Group: Togay Koç
MIS Working Group: Robbie Ray
Co-Opted: Vivek Dhukaram
Co-Opted: Verity Currall
Media & Communications Committee Membership:
Chair: Karan Malhotra
Secretary: Togay Koç
Member: Edward Dawe
Member: May Labidi
Social Media Fellow: Conrad Lee
Webinar Fellow: Benjamin Lau
Scientific Committee Membership:
Chair: David Townshend
Secretary: Sarah Johnson-Lynn
Member: Toby Jennison
Member: Dev Mahadevan
Member: Madhu Tiruveedhula
Member: Nijil Vasukutty
Co-Opted: James Ritchie

FROM THE EDITOR
A Golden Milestone: Celebrating Fifty Years of excellence, innovation and global collaboration in the field of foot and ankle surgery.
A50th birthday is an important milestone in the life of any individual, and certainly in the growth and development of organisations. This Golden jubilee of BOFAS marks half a century of dedication, collaboration, and significant achievement in improving patient care and outcomes in foot and ankle surgery.
It has been an amazing year of celebrations with two annual conferences in 2025, launch of BOFAS global, inception of Practice Ready Orthopaedic Foot Ankle Surgery series for 2026, The Foot being adopted as the official journal of BOFAS to name a few.
The Foot Print serves as a global platform of communication and dissemination of knowledge amongst healthcare professionals delivering foot and ankle care to the patients worldwide. The support and engagement of the partner societies have been a crucial element in its growth and success. I am so pleased to see that the support for this global platform continues to grow as we welcome more partner societies, Asian Federation of Foot and Ankle Surgeons Association and Egyptian Foot and Ankle Society, in this issue.
As outlined eloquently in the article 'A brief history of BOFAS Time', over the past five decades, our society has evolved from a nascent idea into a vibrant forum for critical debate, professional development, and engagement of the foot ankle community. We have navigated immense changes and challenges in our field, adapting to new technologies and shifting paradigms, while remaining true to our core mission of promoting high quality research and propagation of knowledge in foot and ankle surgery, ultimately helping our patients.
In this special issue, we not only look back at our rich history but also provide an insight into the remarkable developments in the field of foot ankle surgery. The articles within range from research at the cutting edge of newer techniques to more relaxing puzzle and hobbies corner. None of this would have been possible without the efforts of editorial board who generously devote their energy, time, and talent to the great benefit of this BOFAS bulletin. Special mention to Graham Chuter who will be relinquishing his role to take up the new position as the chair of BOFAS global. Also, we remain very grateful to the industry partners for continuing to support this endeavour. I very much hope that readers will be inspired by our rich offerings in this issue.
As we look towards the next 50 years, we are well-poised to take the society forward, addressing new challenges and embracing opportunities. The future of BOFAS will be shaped by continued innovation, a commitment to diversity of voices, and a focus on how our work affects the care of our patients and the wider community
Here's to 50 years of growth, leadership, and irreplaceable contributions, and to many more years of innovation, impact and global collaboration!
Jit Mangwani - Editor - Foot Print







Verity Currall Munier Hossain Kailash Devalia
Graham Chuter

A BrieF HiStOrY OF BOFAS time
Disheartening, isn’t it?
A new Labour government, promising the Earth, elected to replace a tired, in-fighting Tory regime, now struggling to cope with not only the conflicting pressures of a stagnating economy and spiralling energy costs, but also back-biting in its own ranks. There’s violence in the Middle East, widespread discontent at home and rising public sector pay demands. The NHS is bankrupt, the medical profession demoralised and junior doctors on strike.
But it’s not 2025; it’s 1975. Basil Fawlty is mentioning the war - but just about getting away with it - while David Bowie is telling Major Tom to put his helmet on, Freddie Mercury is seeing a little silhouetto of a man and Billy Connolly is enjoying an unlikely number one with a comedy song entitled D.I.V.O.R.C.E. On the continent General Franco dies on the 20th of November; on the 22nd Juan Carlos is crowned king of Spain. European fascism breaths its last and, at the Royal London Hospital in Whitechapel, a group of like-minded individuals meet to discuss foot and ankle surgery.
There were twenty-one of them, plus three guests from the Collège Internationale de Chirurgie et de Médecin de Pied, under the auspices of which organisation the meeting was convened. Their names read like a Who's Who of early British foot and ankle surgery but two really stand out as the drivers - and indeed architects - of the proto-BOFAS: Basil Helal and Michael Freeman.
Mike Freeman was born in Ockley, Surrey and educated at Stowe and Cambridge, where he attained a First in Natural Sciences from Corpus Christi College.


James Ritchie
Consultant Orthopaedic Foot and Ankle Surgeon; Kent Institute for Medicine and Surgery and Nuffield Tunbridge Wells Hospital
His medical career, however, centred on the London Hospital where he was an undergraduate, an orthopaedic registrar and, ultimately, a consultant, replacing Sir Reggie Watson Jones in 1968. An original and eclectic thinker, he cofounded the biomechanics unit at Imperial College with Alan Swanson (the Head of Mechanical Engineering at Imperial and not to be confused with Alfred Swanson of Grand Rapids, Michigan, Master of the Plastic Fantastic). Interested in articular cartilage and arthroplasty, Freeman developed the Imperial College of London Total Ankle Replacement. Like other early ankle prostheses, its success was underwhelming. At five-year follow-up, only 11 out of 62 implants showed “satisfactory” results, while almost half had been revised. Freeman lost interest in ankle arthroplasty, which
was unsurprising; let’s face it, if Waterloo hadn’t won Eurovision, ABBA might have eked out a living working in a Volvo factory. He did not, however, abandon joint replacement altogether; merely moved on to the less-demanding challenges of hip and knee surgery. He became president of the BOA and also founded the British Hip Society, but we can, perhaps, indulge him that as, along the way, he hosted the first meeting of the embryonic BOFAS.
Basil Helal was an altogether less establishment figure. Of Anglo-Egyptian extraction, he attended the English School in Cairo and then studied medicine at the London Hospital overlapping with Mike Freeman; it’s intriguing to speculate as to how well, if at all, they knew one-another. Like Freeman. he was appointed a consultant to the London Hospital group, although three years earlier and at the Enfield branch (now Chase Farm Hospital). Later, he became an honorary consultant at the London Hospital itself and at Stanmore. Helal published extensively and, unlike Freeman, had a particular and enduring interest in surgery of the hands and feet. His “Surgery of Disorders of the Foot and Ankle” has been a standard textbook for many years. He was vice president of the International Society for Surgery of the Foot and advised the British Olympic Association through the course of five Olympic Games.
But Basil Halal was something more than just an orthopaedic surgeon: he was a bon viveur. Described by his contemporaries as charming, cultured and erudite, he drove a Rolls Royce and was a member of the Savage Club - an institution named

after a colourful 18th-century poet and convicted (later pardoned) murderer who drank himself to death in a debtors’ prison. Describing itself as being for “gentlemen distinguished in literature the arts or science... And excisable alcohol”, the club now admits ladies, although only as guests of members. Basil’s contemporaries recall him being extremely well connected; apparently he “always knew someone who could make things happen”.
Orthopaedic surgeons are, of course, famous for being sensitive, softly-spoken individuals with negligible egos and a boundless tolerance for opinions at variance to their own, and one is forced, I think, to question how well such two such strong but contrasting characters as Mike Freeman and Basil Helal got on. Was the infant BOFSS, perhaps, a battleground of the titans? Rather disappointingly, it seems it was not. To quote their contemporaries “Mike would have made an excellent barrister; he could build a case supporting a theory one week and, rather alarmingly, could appear the following week with a new theory on the same subject, equally well supported”; “he was brilliant at chairing conferences and appearing on TV. Basil was the better technical surgeon and had a broader knowledge of orthopaedics. Neither looked for conflict.” Moreover “there was no enmity between them. Unlike Basil Helal, Mike Freeman never really involved himself in running BOFSS”.
The programme for that first meeting, the 22nd of November 1975, covered many familiar topics: diabetic foot infection, osteotomies of the first metatarsal, first MTP joint replacement and the subtalar joint, for example. Afterwards the delegates convened for a business meeting to address the question: “Is a British society for surgery of the foot a worthwhile project?” Fortunately, they concluded that it was. As Bernard Meggitt's annotations to that first programme, however, make clear, deciding a name for a name for the fledgling society was problematic, our founding fathers struggling to choose between the British Foot Surgery Society >>
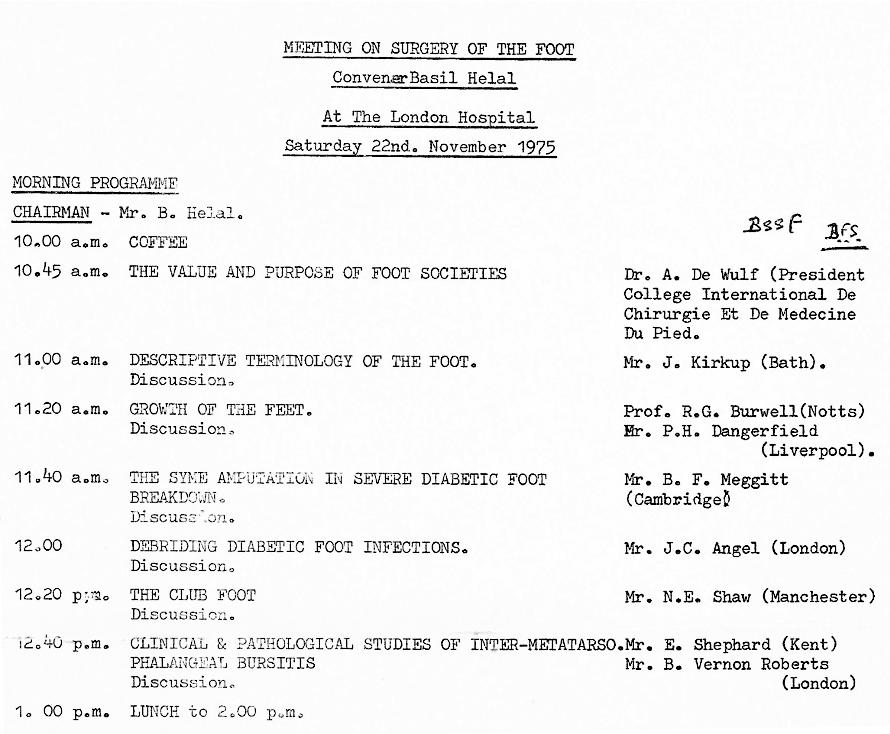



and the British Association for Surgery of the Foot, amongst others. It became an ongoing issue. In the 1976 April meeting the title of “British Foot Surgery Society” was adopted but the November meeting was described as that of the “Orthopaedic Foot Surgery Society - Britain” while at the 1978 meeting we became the British Orthopaedic Foot Surgery Society. BOFSS we were to remain until 2006 when we were rebranded as BOFAS in recognition of the increasing importance of ankle reconstruction to the speciality.
Although not exactly an anarchosyndicalist autonomous collective, the embryonic BOFAS was a fairly amorphous organisation. At the second meeting, in Harlow in June 1976 ,“it was decided not to have a constitution”; the structure and members of an executive, however, were agreed. Predictably, Basil Helal was to serve as both Secretary and Treasurer; Chris Walley was the editorial secretary, Jeffrey Fisk “host for the present meeting” and John Angel “host for the next meeting” which was to be held at Stanmore. There was no official president and indeed the title president does not appear in the early records of the society. The local host was “in the chair” - as opposed, presumably, to under the tablebut, as one of the founders put it, “it was always Basil pulling the strings”. To be fair, the early BOFSS had no need of a more complex structure. It was an intimate,
affable society small enough to fit into Basil Halal's swimming pool - as, indeed, it did on one hot summer's evening when, according to eyewitness accounts, the whole society stripped off and dived in in the buff. Fortunately, this was thirty years before the iPhone so we are spared fading photos featuring the pride of British foot and ankle surgery with their hardware well and truly on display.
Clothed or otherwise BOFAS has always been a very convivial society, and this included the members’ spouses who both organised and attended the social programme. As one early member put it: “We all knew each others’ wives”particularly after the swimming pool episode, presumably. Indeed, having a wife willing and able to host the annual
“The socie T y moved slowly forward un T il 1982, which was a year of seismic change for B ofss .”
dinner was one of the original criteria for becoming president; current aspirants to supreme office, take note. Although recently held in locations as diverse as Liverpool Cathedral and Belfast City Hall - as well as in more hotels than Oasis could trash on an extended farewell tour - in the early days the dinner was an affable affair at the president's home. Friendliness is the word most used by our longstanding members to describe their memories of the society, and it is perhaps friendliness, combined with a (relative) lack of ego and avarice that has distinguished BOFAS from other specialist societies.
The society moved slowly forward until 1982, which was a momentous year in lots of ways. Margaret Thatcher was busy liberating the Falkland Islanders from the shackles of Argentinian oppression - and the miners form the shackles of employment. Ozzy Osbourne bit >>

(left to right) Andy Taylor, Peter Briggs, Helen Taylor, Patsy Henry, Tony Henry and Jim Barrie at COMFAS Venice, 1998
(left to right) Eric Anderson, Suguro Inokuchi and Ravi Kunzru in Kyoto, 1999



the head off a bat live on stage. On a more wholesome level, we first met the Snowman and walked in the air, while poor ET struggled with the vagaries of the US phone network. It was a year of seismic change for BOFSS too. At the Glasgow meeting, the society was incorporated as a limited company and gained its charitable status. The constitution, which forms the basis of the one we still have today, was adopted. Under its provisions, Basil Helal was no longer Treasurer-In-Perpetuity, although he did continue as SecretaryFor-As-Long-As-He-Wants-To-Be. The office of president was established, and the first BOFSS instructional course was held. It was entitled “The Foot” - a name also adopted for the archived papers from the annual meeting (the forerunner of the modern journal), which had been produced in booklet form from the beginning.
The society continued to evolve structurally over subsequent years. The first committee, the Programme Committee, was set up in 1992 to “vet papers and plan instructional
courses”, effectively a mixture of the functions of the present SciComm and EdComm. It comprised the President, Secretary, Treasurer, President-Elect and “another member”. The following year the Chang Cheng prize was inaugurated and, in 2001, the Programme Committee was split into the Scientific and Educational committees and the Presidential Medal was purchased for the princely sum of £835. The website, initially part of the BOA site, was first crackled into e-life at the millennium under the mouse of Jim Barry, the first person to hold the rather sinister title of Web Master; the bespoke site was created under Nick Geary in 2006 and redeveloped by Robert Clayton in 2021. Apparently, we are now present on social media - as opposed, presumably, to antisocial media, which sounds much more fun, if you ask me - and have a YouTube channel, whatever that might be. I doubt it will catch on.
The increasing size and complexity of the Society of course meant that it would eventually require a secretariat and in
2011 Rosemarie Riccardi was appointed. Unfortunately, in her short tenure, she nearly managed to do for the BOFAS meeting what Attila the Hun did for Roman real estate. Fortunately, in 2013 she was succeeded by the inestimable Jo Millard: universally loved - and equally feared by those failing to meet their speaker submission deadlines.
Membership criteria and numbers have changed radically over the years. In the very early days, the main prerequisite for membership of BOFSS was to be prepared to turn up and present a paper. From 1992 to become an aspiring member needed to have two sponsors and be “deemed suitable” although apparently only one individual, a “complete bounder” has ever been truly black balled. From the 1991 the Dundee meeting, a new category of affiliate membership, intended to attract younger members, was introduced for trainees. The overall numbers grew steadily through the 1990s, but, between 1998 and 2000, growth accelerated rapidly and has
An early instructional course programme, 1985. Has anything changed?
remained roughly linear to our current total of over six hundred. The membership has diversified too. Our founding fathers, although not all white, were male and mostly from London and the southeast, with one notable exception. Look carefully at the list of members present at the first meeting and you will find one Mrs M Ellis. No relation to Sir Harold Ellis, Maggie Ellis was an occupational therapist at the London Hospital who had a particular interest in making splints for CP and CTEV. A “rather forceful character” she continued to attend BOFSS meetings until at least 1992. It must have been a rather lonely experience, although since then, we have had, in Trish Allen, a female president and it is estimated that around 10-15% of the current BOFAS membership are women.
BOFAS, of course, is not just an educational organisation: it is our de facto professional body. Unsurprisingly, therefore, the business meeting, a forum for discussion of professional matters, has been a feature of BOFSS

annual conferences since the beginning. The minutes reveal a number of recurring themes such as VTE, Bupa/ remuneration and surgical podiatry. One year the society was concerned about: “the BMA discussions.. with the chiropodists regarding the scope of surgery in chiropody. It was noted there was no representation of the orthopaedic association, the College of Surgeons or our own society….” It is sobering to note that those comments date not from 2007, or even 1997, but from the business meeting in 1977; surgical podiatry has been an issue to BOFAS from its earliest days.
The delivery of papers, however, has changed considerably. Seen through a 21st century optic the presentations at the early meetings have a charmingly informal, almost whimsical tone - ideas shared amongst friends rather than formal debate. Titles too were more erudite than today: “Thoughts on the Aetiology of Hallux Valgus” or, my personal favourite, “The Tale of the Talus”. Papers were hand-typed



on mechanical typewriters with basic, sometimes hand-drawn, graphics and projected from glass or plastic slides. These had to be mechanically loaded onto a carousel and shown on a pull-down screen in a hospital post-graduate centre, often with the tea lady acting as projectionist. The transcripts, however, make it clear that, for all the outward amateurishness, there was no lack of careful thought in the content of those early papers. Our founders were, in effect, trying to define foot and ankle surgery almost from scratch, including what the parameters of a normal foot actually were. We may congratulate ourselves on the scientific quality and slick presentation of our modern papers with sophisticated graphics and flashy videos but we should not forget that we are standing on the shoulders of giants.
There is, however, one lecture in the history of BOFAS that stands out a country mile from the rest: “The Erotic and Sadomasochistic Foot and Shoe” by Paul Benou, president of the AFCP. >>







A uniquely thorough and well-researched exploration of this important and worthy topic, it was illustrated with images from mainstream western cinema and Indian erotic art to dubious Dutch photography and what my laptop describes as “a drawing of a person holding a log” (which it arguably is, though not of the arboreal variety). Intriguingly, Monsieur Benou's wife, Jacqueline, insisted on being the projectionist for the talk; make of that what you will.
BOFAS has had a long but somewhat paradoxical relationship with its continental neighbours, being in effect, both child and midwife of EFAS. It was founded from CIP, but, by the 1990s, European foot and ankle surgery was bitterly divided between the rival European Federation of Foot and Ankle Societies, the European Society of Foot and Ankle
Surgeons, the Federation of European Foot & Ankle Surgeons and the Federated Society of European Foot & Ankle Surgeons. OK, I admit I made the last two up, but think the Judean Peoples’ Front and the Peoples’ Front of Judea and you’ll get the gist. It was through BOFSS, at a meeting in Liverpool, that a deal between the feuding societies was brokered - and duly celebrated with champagne in Leslie Klenerman’s garden.
International co-operation, however, is not without its dangers. In 1979 the young BOFSS agreed to host the CIP meeting. Eastbourne was chosen as the venue it being “easy for the Europeans to get to” presumably crossing the channel in an orthopaedic Germano-FrancoSpanish Armada. The French insistence on instantaneous translation into five languages with an individual translation unit for each delegate, however, proved
“fif T y years of B ofas as T he professional B ody of Bri T ish foo T & ankle surgery - a naive, op T imis T ic you T h, vigorous adul T hood, and, perhaps, more considered ma T uri T y.”
astronomically expensive and fewer than one hundred of the expected four hundred delegates attended. The meeting was a financial catastrophe, losing £3815, four times the total resources of BOFSS at the time. Fortunately, Basil Helal put not just his hand but his forearm in his pocket and covered the debt; disappointingly, the story that BOFSS became known as Basil’s Orthopaedic Foot Surgery Society at this time, appears to be apocryphal.
Sadly 1979 was not the only year in which the foot society flirted with insolvency. The other was 2020. The year in which you couldn't go out without a mask, otherwise normal people stood in the streets banging pots and pans and it became borderline acceptable to drink before 9:00 am. Unable to carry out its normal activities, BOFAS faced what Hiro Tanaka, Treasurer at the time, describes as a “very challenging situation, on the edge of bankruptcy” and James Davis, then president, more pithily, as a “F****** s*** s***”. Fortunately, judicious management allowed the society to survive, albeit by the skin of its teeth, and bounce back since.
So, fifty years of BOFAS as the professional body of British foot & ankle surgery. A naive, optimistic youth, vigorous adulthood, and, perhaps, more considered maturity. We have survived, even thrived, despite near two nearbankruptcies and a niche lecture that would have had us shut down on grounds of public decency in half the states in America. In Toe Jam, we even have a band. Their lineup may have had more perms and coms than a statistician’s password and they’ve suffered from the creative difficulties that beset all great artists, like having their statins confiscated at airports and squabbles over who gets to use the band knee-brace or play the Big Guitar. But they’re back by popular demand and heading for Glasgow. See you there. n
With grateful thanks to: John Angel, Paul Cooke, Mark Davies, James Davis, Nick Geary, Andy Goldberg, Don McBride, Karan Malhotra, Bernard Meggitt, Dishan Singh, Ian Stephen, Hiro Tanaka and The Borthwick Institute, University of York
BOFFS toasting the creation of EFAS



Treatment for:
• Avascular Necrosis (AVN)
• Complex Talar Fractures
• Bone Tumors
• OCD Lesions
• Failed Total Ankle Arthrodesis

COMPONENTS

• Anatomic component design for natural load-sharing and reduced stress shielding.
• Semi-constrained fixed-bearing system built for both primary and revision ankle arthroplasty.
• Broad sizing: UHMWPE inlays in 4 thicknesses and two offsets plus full tibial/ talar size offerings.
YEARS OF CLINICAL EXCELLENCE

COMPONENTS

• 3-component, non-constrained mobile-bearing design offering four degrees of freedom.
• Anatomic components + UHMWPE insert sizes in 4 thicknesses for precise fit and reduced stress.
• Titanium plasma & hydroxyapatite coatings on tibial/talar implants for uncemented fixation.

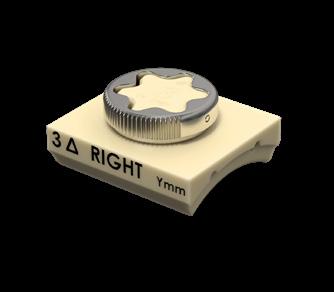
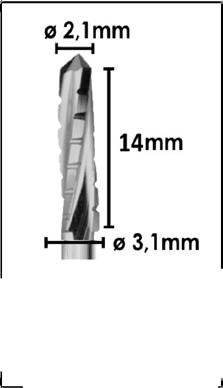
The VILEX MIS System provides comprehensive burr and titanium implant options for the minimally invasive, percutaneous fixation of the foot and ankle.
VILEX MIS Screws are sterile packed and offered in:
• 3.0mm and 4.0mm Diameter forefoot options and feature a 45O Chamfer Head to reduce soft tissue irritation.
• 4.6mm and 7.0mm Headless Mid and Hindfoot Screws.


P uzzL e COrner
Crossword
Across
2. Grand entrance with a light touch (6)
3. Bone-cut oddly removes my toe tomorrow (9)
5. Position held by finest ancestors (6)
10. It's designed to straighten out your step (8)
11. Painful condition of untidy British trains, if bins removed (9)
12. Twist in Paris causes injury (6)
Down
1. Consolidate on us, if remixed (6)
4. My son's oddness is dynamic, forming a connection (11)
6. Dance venue goes the distance (8)
7. Painful lump formed of roll and charge (6)
8. Fascinating connective tissue (6)
9. Group of dolphins try to reverse AI (8)
Crossword solution can be found on page 39









m edioku
Fill in the grid so that every row, every column and every 3x3 box accommodates both of the icons, without repeating any.
Medioku solution can be found on page 39
Note: Medioku and Crossword created with TheTeachersCorner.net. Cryptic crossword clues written using CoPilot or from cryptics.georgeho.org.


Developed and Engineered with Surgeons




P LA nning FO r A n un PLA nned retirement
Background. It’s October 2020, 7am on a Saturday. Covid is still everywhere, messing with the world, and I am sleeping. My wife’s mobile rings and she immediately sounds concerned. It’s every parent’s worst nightmare: our 21-year-old son, studying Engineering at Bristol University, is on an Erasmus year in Spain. He has fallen 4 metres from an unenclosed viewing platform directly onto his head. Details are sketchy, as the friend making the call wasn’t with him. He is in a coma and ventilated in ITU 1500 miles away. So what do you do?
At the time, I was working as a consultant in the Sheffield Foot & Ankle and Trauma Units. My wife was a paediatric optometrist in The Children’s Hospital. By chance, our daughter – a newly qualified Foundation Doctor – was staying with us. Could we all just drop everything and fly out? Of course we could, and we did! By that evening, the three of us were there by his bedside; hastily arranged flights, a tearful lift to the airport from friends, then sneaking “illegally” into the Hospital (at that time only one person was allowed into the Covid ‘free’ public major trauma hospital). Our strong, fit, tanned and clever boy was helpless in ITU; intubated, an ICP monitor in situ, critically ill.
So began a dramatic change in all our lives which is ongoing. We couldn’t know that we would not return to Sheffield for 8 months, enduring unimaginable heartache and uncertainty. The three of us were a team: cooking and spending time with our son on a rota that was
drawn up and posted on our fridge –such is the method of clinicians, especially our F1! After two weeks, once he was extubated and transferred from ITU to a Neurosurgery Ward, we could be with him 24 hours a day. The evidence suggests that familiarity with those around you is a vital part of recovery from a severe Traumatic Brain Injury (he had sustained, amongst other injuries, a Grade III Diffuse Axonal Injury). In Spain, family support is both encouraged and needed to help with nursing care. We grabbed that opportunity with both hands and were there by his bed 24 hrs per day for 4 months – back to “shift work”! Mistakenly, after his second depressing MRI scan, I reached to the literature for answers to see how he may recover: roughly 1/3 chance of death, 1/3 chance of a chronic disorder of consciousness (persistent vegetative state) and 1/3 chance of some recovery with a very small chance of independent living. Sombre reading which threw me into a mixture of deep despair and frenzy: how do we adapt our three-story Victorian house for the unlikely event that he (or we) would


ever return to it? Epidemiological data such as this, however, is summative only – a guide, not a rule book. He was an individual not an aggregate.
Top Tip: when “it hits the fan” be a parent/sibling/carer not a clinician!
Our daughter selflessly gave up her dream F1 post – her North Thames foundation program was very supportive and, thankfully, she started afresh the following year. My wife and I had to be excused from work. As there was no system to facilitate this, we both used ‘sick notes’ quoting stress. For us both, in different Trusts, our colleagues were
“ s o B egan a drama T ic change in all our lives which is ongoing. w e couldn’ T know T ha T we would no T re T urn T o s heffield for eigh T mon T hs, enduring unimagina B le hear T ache.”
Chris M Blundell BMedSci (Hons), MB ChB, FRCS(Tr&Orth), MD; Consultant Foot and Ankle Surgeon (Retired)
amazing and supportive. In my Trust, the “non-clinical management” were handsoff. Despite being in a leadership role managerially for 20 years, I heard almost nothing from them. It was enlightening that it is your immediate colleagues that care. My CD (a friend who had worked with me as a trainee) was in touch monthly for formal “check-ins”. Our non-work friends rallied and were just amazing for us all – we needed them.
Top Tip: it’s only your friends who will really care.
FinAnCeS
Although this was by no means my priority, the practical reality was that we needed money to live. I remained on full NHS pay for 6 months and then half pay for a further 2 months. Our daughter had very little pay after 3 months as she was only 2 months into her foundation program. Clearly, I had no private income. Many colleagues had been affected by the loss of additional income during Covid and in my case this was extended. I have built my life to not depend on any income other than my NHS salary and – at this point – that was a blessing. I had paid for income protection for 20 years, with my policy taking effect after 6 months from work. However, this did not, in my case, support my loss of private income nor, in the end, offer me any payment. I cancelled the policy.
Top Tip: read the small print!
mentAL HeALtH SuPPOrt
There was no offer of support for 6 months from my employer. Eventually, I did have an Occupational Health appointment – over the phone by a clinician who was clearly at a station waiting for his train. It was of little or no value, very disappointing. At my switchedon daughter’s suggestion, the three of us were given counselling support through the BMA (despite her being the only BMA member). An amazing level of generosity, in my opinion, and one which was helpful, even though it was limited to six sessions for each of us. Just to have a dispassionate individual to hear my difficulties was great. We have each sought further >>






mental health support and I think this may well be ongoing – the impact of an event like this cannot be underestimated.
Top Tip: use all the support you can get; don’t be shy to ask.
returning tO wOrk
After 8 months away, I was feeling rusty and was supposed to have a gentle return. Day two, however, was a trauma case: a talus fracture in a 21 year old man on ITU with a Grade 3 DAI. I was the only F&A consultant available. Too close to home and very uncomfortable – I had to dig deep.
Covid recovery was ongoing and I could sense frustration amongst my colleagues and also growing in me. I was 55 years old. I felt that recovery would be 5 years in the making, taking me until 60 to recover the work I felt I had “lost”.
The options, as I saw them, were:
1. Kick back, relax, and let systems recover slowly
2. Get stuck in managerially and help plan the recovery
3. Leave
I felt that taking a back seat would be too hard for me; I am not built that way. Option 2 would have been more my style

but, having gone through what we had, I had simply run out of steam and now my focus lay elsewhere. That left option 3. I wasn’t sure that we were ready for this leap. But my sage wife said the immortal words “What exactly are we waiting for?”
So I left. I tendered my resignation with 6 months’ notice and retired from all clinical work 18 months after receiving the fateful phone call on that Saturday morning.
Then what? Well, I planned as much as I could once the decision had been made. We decided to both retire at the same time, although hers was a sabbatical initially as they didn’t want her to go (not so, my Trust!). My finances were ok. I needed my

pension which was going to be reduced by 48% to take retirement at 55. But we had savings and we had an AirBnB in Spain which my wife was running. We had made sure that additional private income was squirreled away from early in my career and my NHS lump sum would pay off our mortgage. There are published rules: 4% rule, 7% rule – that is, you can afford to spend all income plus either 4 or 7% of savings annually, depending on the prevailing rates of interest. In the current world of financial chaos, I think 1 or 2% might be a safer estimate. I found a Which report that allowed me to assess how much money I would need. It is surprisingly cheap to be retired if you lead a “normal” lifestyle. It is refreshing to step off the rat wheel and take stock of what matters. I am an active person with a searching mind. Friends said that some purpose would “find me”, yet no light bulb moment has happened. I think for a purpose to “find me” I must be looking for it and I am not (yet). I am “busy” learning Spanish, singing, reading and helping my family where and when I can. I still keep my hand in teaching, when approached (but less frequently now, of course). I’m often asked, “Do I miss work?” and the answer remains: I miss my colleagues, the patients and the clearer sense of purpose that work provides, but work itself? No I don’t, not really.
So, can you plan for an unplanned retirement? Well, by definition, of course you can’t. But I am hopeful that this provides some solace for any readers that might be going through a sudden, immensely tough time. My phone is always on.
I am a firm believer in the words of Ferris Bueller: “Life moves pretty fast. If you don’t stop and look around once in a while, you could miss it.” n
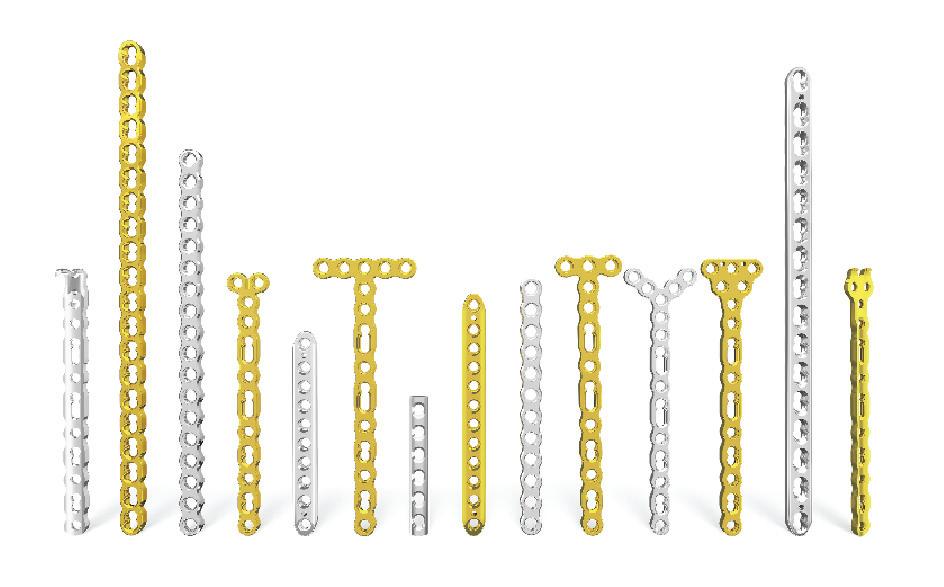
Plating. Powered up.


Powered by SYNTHES™
VOLT™ Mini Fragment Plating
System
VOLT: Variable Angle Optimized Locking Technology is an innovative evolution in fracture management from Johnson & Johnson MedTech designed to improve stability, enhance performance, expand options, and increase efficiency
For additional details, refer to the following:
https://www.jnjmedtech.com/en-US/product/volt-mini-fragment-plating-system or https://www.jnjmedtech.com/en-EMEA/product/volt-mini-fragment-plating-system
Important Information: Prior to use, refer to the instructions for use supplied with the device(s) for indications, contraindications, side effects, warnings and precautions.
© Johnson & Johnson and its affiliates 2025. M_US_ORT_TREX_404523.1

CH rOniC ACHiLL eS ru P ture


Pranav Patel, MBBS University Hospital Southampton Foundation Trust


Togay Koç, MBBS, MSc, FRCS (T&O) University Hospital Southampton Foundation Trust; University of Southampton
CA nOveL teCHnique
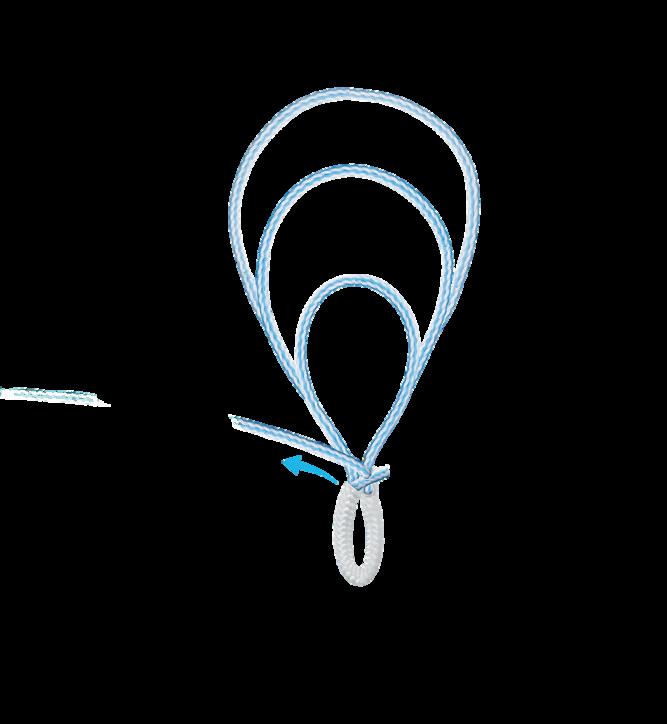
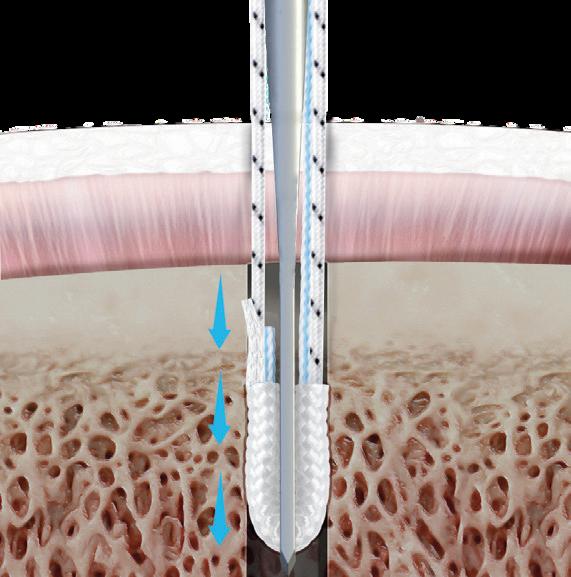
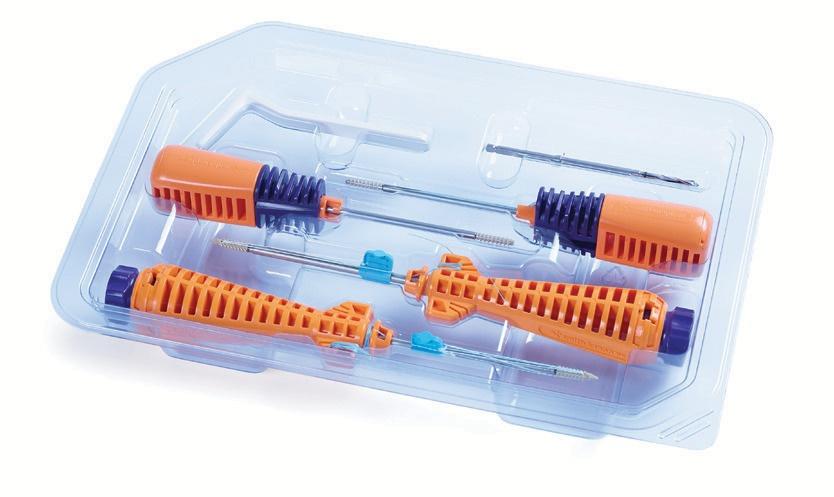
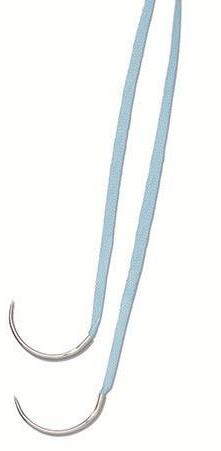
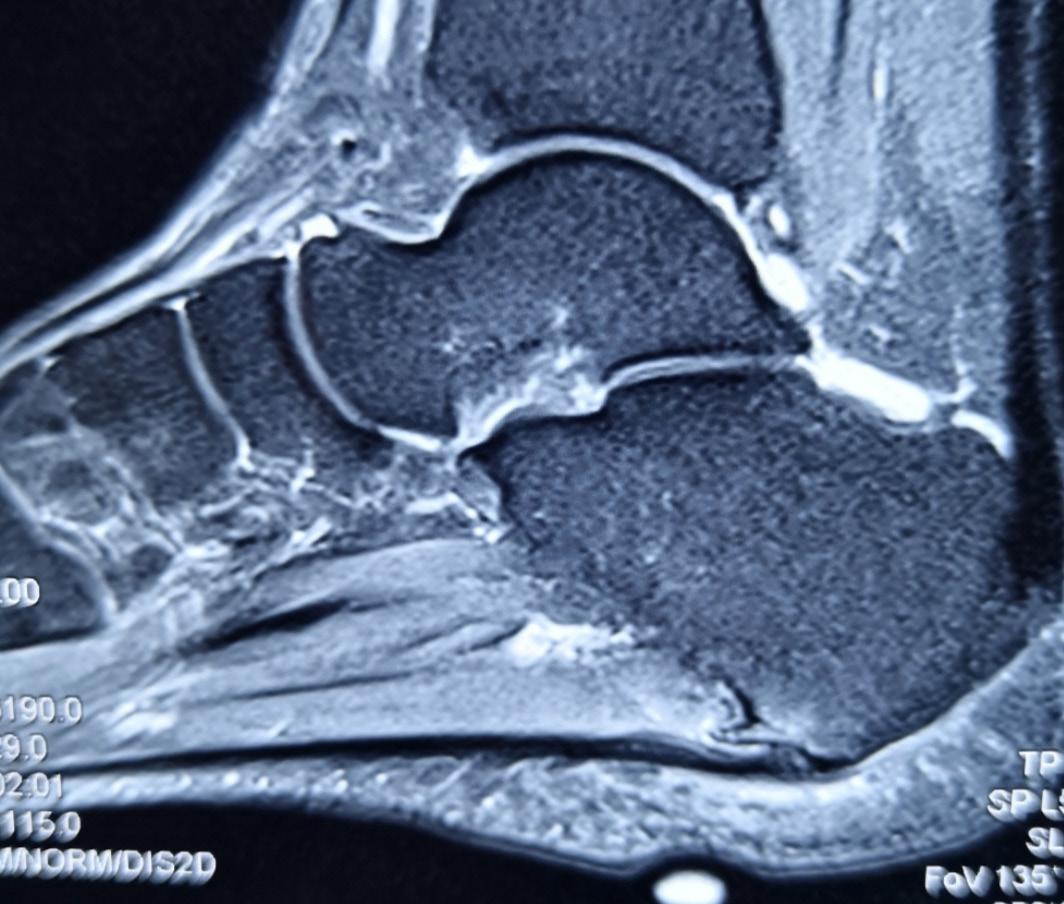
hronic Achilles tendon ruptures are injuries that present or are treated more than two to six weeks after the initial injury, although the time to presentation or treatment is debated in the literature. We present a novel minimally invasive approach to chronic Achilles tendon repair: a combination of endoscopic flexor hallucis longus transfer, the use of an ultrasound-guided less invasive Achilles repair involving intra-osseous fixation, and a Strayer/ Baumann recession with promising results. Our technique allows for the treatment of chronic Achilles tendon ruptures with a clinically visible gap (Hatchet sign) with less invasive techniques, thereby reducing the morbidity associated with the approaches to perform proximal lengthening procedures such as V-Y plasty or turn down techniques.
Contraindications for surgery include multiple uncontrolled medical morbidities, poor mobility, poor engagement with physiotherapy and other medical services. Prolonged quinolone use, such as for prophylaxis in the cystic fibrosis population, is a relative contraindication. Ultrasound imaging can be useful for dynamic images and a good measurement of the tendon gap. MRI imaging can also be used if there are concerns regarding the FHL and other tendons.
Surgical technique
The patient is anesthetised and positioned semi-prone /recovery position, with a thigh tourniquet on at 250mmHg of pressure. A pad of drapes is placed underneath the anterior


Figure 1: Positioning and Marking


ankle. The edges of distal and proximal edges of the tendon are palpated and marked [figure 1]. Posterolateral and posteromedial portals are created as originally described by Van Dijk1. After creation of the posterior viewing space, the FHL is identified, with the use of hallucis flexion to positively confirm. A tendon insertion site on the posterior dorsal surface of the calcaneum (as close as possible to the Achilles insertion) is prepared endoscopically to expose cancellous bone. The FHL sheath is released proximally and distally before it is harvested using laparoscopic scissors at the fibro-osseous tunnel with the ankle and hallux maximally plantarflexed. The end is whipstitched [figure 2].
Under fluoroscopic and endoscopic guidance, a guide pin is inserted into the previously prepared insertion site, followed by a 6 mm reamer, which is unicortical but up to the plantar cortex. The tendon is inserted and tensioned so that the foot is in a 15-20 degree plantarflexed position. A 6.25mm by 15mm Tenodesis screw is inserted, and then the repair is tested. Finally, both portals are washed out.

A small incision is made at the distal end of the proximal stump after palpation. It is important to visualise and protect the sural nerve as it passes laterally distally. A transverse incision is made into the sheath. Scar tissue is removed with debridement & curettage,which can be assisted endoscopically. Next, percutaneous blunt adhesiolysis is performed proximally and distally before the endon ends are delivered and freshened.
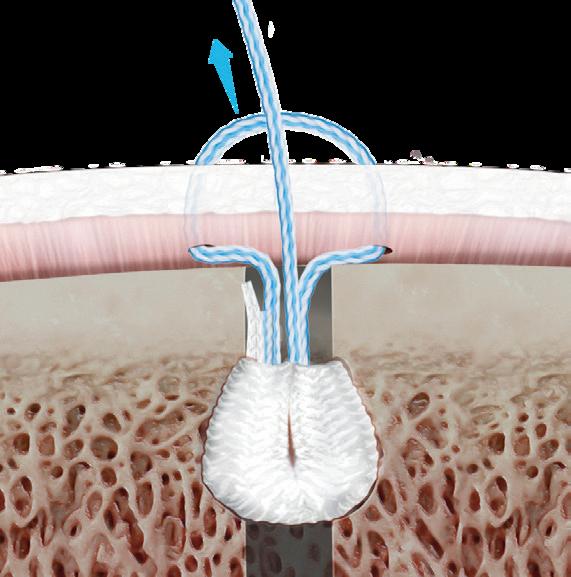
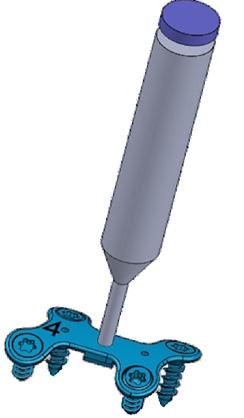
The Arthrex PARS jig is used to apply suture tape to the proximal stump of the tendon. The inner arms of the jig are inserted into the wound and sit on either side of the proximal tendon. The distance between the inner arms is adjusted using the wheel so that the tendon is snug between the arms. The outer arms have 7 numbered holes from 1 to 7. Ultrasound guidance is used to ensure that the passage of the provided A needle is inserted through hole number 1 to anchor the jig, which passes through the substance of the tendon [Figures 3, 4].

“ o ur T echnique allows for T he T rea T men T of chronic a chilles T endon rup T ures wi T h less invasive T echniques.”
A PARS needle with a nitinol loop is passed through hole number 2 using ultrasound guidance, followed by the blue SutureTape, leaving equal length on either side of the leg. Then, this process is repeated through holes 3 and 4, with white and green Suture Tapes being pulled through each hole, and an ultrasound is used to ensure that the needles, and therefore the Suture Tapes, are passed through the tendon substance. Then the PARS needle is passed through hole number 5, and the white and black SutureTape is pulled through. Finally, the white SutureTape is pulled through the leg at hole number 1. The needle is removed, and then the jig is pulled down, and the sutures are secured at the wound. The use of ultrasound ensures that the needles, and therefore the SutureTapes, are within the tendon substance.
The blue SutureTape is passed under the number 3 and 4 looped SutureTapes and backed through the loop of the white and green looped suture at each side. >>

Figure 2: Flexor Hallucis Longus after cutting, whipstitched and taken out of the posteromedial window
Figure 3: Insertion of the PARS needle through hole number 1 of the PARS Speedbridge under ultrasound guidance
Figure 4: Dynamic ultrasound image of the PARS needle going through the proximal tendon




By pulling on the non-looped side (simultaneously) of the number 3 and 4 white and green looped sutures. This locks the blue SutureTape in place, leaving a construct with 2 transverse sutures and 1 locked at each side of the tendon. After the sutures are cycled at least 10 times each to ensure sufficient relaxation of the soft tissues and tensioning of the SutureTapes, the sutures are put under tension, and the tendon gap is remeasured.
If there is still a gap after further endoscopic adhesiolysis, a small longitudinal incision is made in the
mid-posterior leg for a Strayer recession +/- Baumann recession. If, after a Strayer, there is still a large gap, a Baumann recession involving transverse division of the superficial soleus aponeurosis can be performed to close the gap.
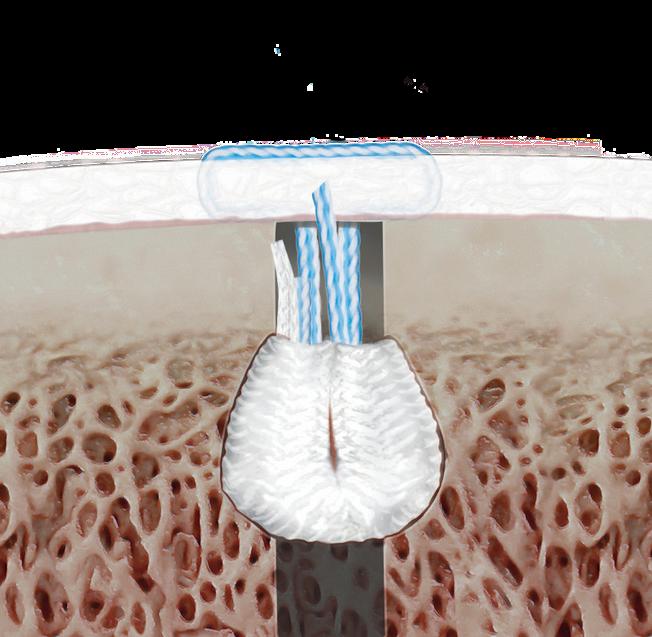
Two stab incisions are made 2 cm apart over the site of the insertion of the Achilles tendon at the calcaneus, approximately 1 cm below the superior aspect of the posterior calcaneal tuberosity. Through the incisions, a drill guide is utilised to drill at 45 degrees to the centreline of the Achilles in the coronal plane and 45 degrees in the
sagittal plane. The drill hole is tapped with the 4.75mm tap. It is helpful to place the PARS needles in the drill holes to facilitate later anchor insertion. Using a Banana suture lasso inserted from these distal holes retrograde through the distal tendon stump, the PARS SutureTapes are delivered. The SutureTapes are secured to the distal drill site with two 4.75mm SwiveLock Speedbridge anchors with the foot in plantar flexion, slightly tighter than the resting angle of the contralateral foot measured pre-operatively. Careful palpation is performed to ensure that the anchors are flush with the bone. The gap can be further repaired with a 0 Vicryl with a buried knot.
2-0 Vicryl is used for paratendon and deep for closure. Skin closure is performed with skin clips and/or 3-0 Monocryl. The leg is cleaned and dried and placed into an equinus front slab.
Post-operative management
Patients are encouraged to elevate the leg for at least 45 minutes every hour for two weeks. The first two weeks are spent non-weight bearing in an equinus front slab, after which the patient is put into an aircast boot with wedges, removing wedges slowly every 1 to 2 weeks until flat. If deemed necessary, the patient may need the use of crutches too.
Patients should be followed up at 2 weeks to check the wound and apply the boot, 6 and 12 weeks to assess progress and final review at 6 months to one year (Figure 5).
Conclusions
We present a novel approach to chronic Achilles tendon repair which combines endoscopic FHL transfer, the use of the PARS Speedbridge jig, intra-osseous fixation, and a Strayer/ Baumann recession to close residual gap present in cases with a Hatchet sign in a minimally invasive technique with promising results. n
Bibliography
1. van Dijk CN. Hindfoot Endoscopy. Foot and Ankle Clinics 2006;11(2):391-414. doi:10.1016/j.fcl.2006.03.002
Figure 5: 6 weeks postoperative result, no visible tendon gap


Powering the next step forward









Proudly Supporting BOFAS 2025

All in one evelled bunion system Bevelled screws Snap-offs Staples

Smith+Nephew steps forward with innovative Sports Medicine foot & ankle repair solutions in UK
Smith+Nephew steps forward with innovative Sports Medicine foot & ankle repair solutions in UK

Smith & Nephew UK Ltd
Smith & Nephew UK Ltd
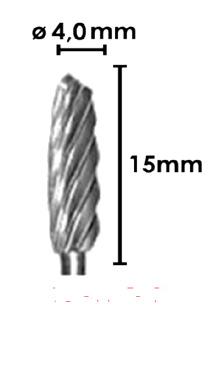
First in market to offer Adjustable Tensioning Technology* for insertional Achilles reconstruction and lateral ankle instability repair
First in market to offer Adjustable Tensioning Technology* for insertional Achilles reconstruction and lateral ankle instability repair
*After anchor insertion
*After anchor insertion
Smith+Nephew, the global medical technology company, today announces the launch of a comprehensive foot & ankle repair portfolio in the UK with proprietary adjustable tensioning technology. The ULTRABRIDGE◊ Adjustable Achilles Reconstruction and ULTRABRACE◊ Adjustable Ankle Instability Techniques are changing the way foot & ankle surgeons perform these repairs by allowing them to refine and optimise suture tension after anchor insertion.
Smith+Nephew, the global medical technology company, today announces the launch of a comprehensive foot & ankle repair portfolio in the UK with proprietary adjustable tensioning technology. The ULTRABRIDGE◊ Adjustable Achilles Reconstruction and ULTRABRACE◊ Adjustable Ankle Instability Techniques are changing the way foot & ankle surgeons perform these repairs by allowing them to refine and optimise suture tension after anchor insertion.
The ability to adjust tension for specific patients allows the surgeon to give the precise amount of range-ofmotion to that patient depending on their level of activity. The surgeon can check and revise the repair construct before locking the suture, which may help restore normal anatomy and deliver potentially better outcomes for the patient
The ability to adjust tension for specific patients allows the surgeon to give the precise amount of range-ofmotion to that patient depending on their level of activity. The surgeon can check and revise the repair construct before locking the suture, which may help restore normal anatomy and deliver potentially better outcomes for the patient
The new foot & ankle portfolio also includes Smith+Nephew’s best-in-class all suture anchor, Q-FIX◊, with consistent deployment and strong fixation, now integrated with needles for open procedures. The anchor inserter tensions the device on deployment, ensuring consistency every time.
The new foot & ankle portfolio also includes Smith+Nephew’s best-in-class all suture anchor, Q-FIX◊, with consistent deployment and strong fixation, now integrated with needles for open procedures. The anchor inserter tensions the device on deployment, ensuring consistency every time.
"Sports and active recreation in the UK adult population is at an all-time high of 63.7% with annual growth rates of over 5%.1 Our portfolio of foot & ankle solutions represents a truly groundbreaking introduction for today’s athletes by offering adjustable tensioning technology after anchor insertion, which is not currently available in the UK market,” said Joaquin Lasso, SVP of Sports Medicine, International Markets for Smith+Nephew. “This technology allows surgeons to personalise their treatment for each patient and returns them to living their Life Unlimited.”
"Sports and active recreation in the UK adult population is at an all-time high of 63.7% with annual growth rates of over 5%.1 Our portfolio of foot & ankle solutions represents a truly groundbreaking introduction for today’s athletes by offering adjustable tensioning technology after anchor insertion, which is not currently available in the UK market,” said Joaquin Lasso, SVP of Sports Medicine, International Markets for Smith+Nephew. “This technology allows surgeons to personalise their treatment for each patient and returns

Step forward with adjustable tension
The ULTRABRIDGE Adjustable Achilles Reconstruction Technique offers the unique ability to adjust suture tension after anchor insertion to accommodate individual anatomic requirements The ULTRABRIDGE Kit is a step forward in insertional Achilles repair Learn more at smith-nephew.com
Kit









Percutaneous posterolateral malleolus fi xation
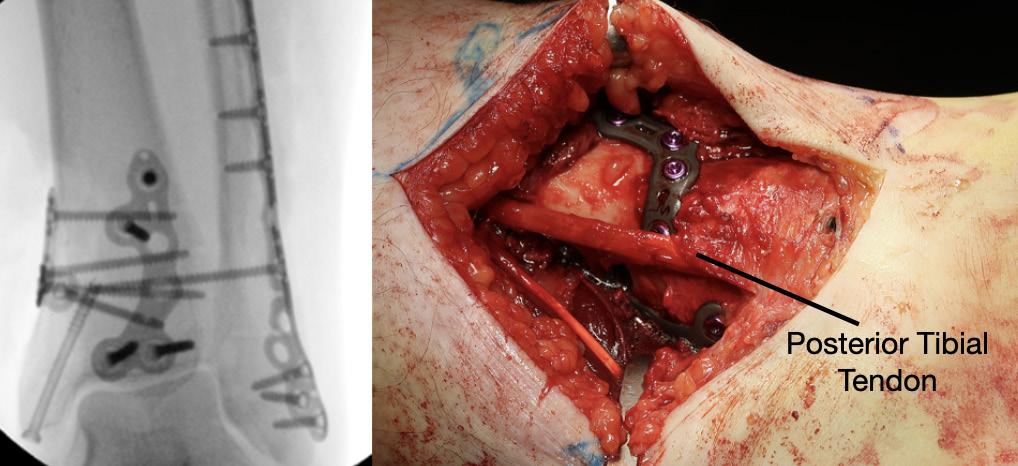
Posterior approaches to the ankle are not without morbidity, often causing increased swelling, stiffness and reduction in dorsiflexion due to posterior scar formation compared to direct medial and lateral approaches. Posterior approaches can also limit access to the medial and lateral malleoli and the trajectory of syndesmotic fixation. If posterior metalwork removal is required, approaching this through significant scar tissue can be challenging and causes further stiffness.


Ed Gee Consultant Trauma and Orthopaedics, Salford Royal NHS Foundation Trust
Percutaneous posterior to anterior screw fixation enables a safe method of reduction and stabilisation of the posterolateral fragment without the morbidity of a posterior surgical approach. This then frees the surgeon to perform a more favourable direct lateral approach to the fibula for fixation and syndesmotic stabilisation without having to utilise the posterolateral approach and apply metalwork through the peroneal tendon bed.
Technical aspects of case selection, pre-operative planning, patient position, dissection, reduction,

guidewire placement, screw insertion and radiological checks are all pivotal to perform this safely and effectively.
Mildly displaced posterolateral fragments are selected (Haraguchi 1, Mason 1, 2A and Bartonicek 1, 2). Pre-operative CT is obtained to assess the posterior malleolus fracture and screw trajectory.
The patient is positioned in a lateral position with the injured side up and on an elevating block, placed behind the non-operative leg. This gives a lateral view of the ankle and allows external rotation of the hip to enable mortise view fluoroscopy, access to the anterior ankle for trauma scope and access medially for medial malleolus fixation. Anatomy is marked on the skin using image intensifier and the level of incision is planned to approach the posterior malleolus.
The posterior malleolus should be fixed first to enable proper assessment of joint line and fracture fragment reduction. Once medial and lateral metalwork is in situ this will obscure fluoroscopic assessment of the posterior malleolus. If fibula reduction is required to restore the syndesmosis prior to posterior fixation the fibula can be approached through a direct lateral approach in this position, reduced and held with a clamp or K-wire in a manner that doesn’t obscure fluoroscopic assessment.
A 10mm incision on the lateral edge of the Achilles tendon at the level of the


posterior malleolus and a 10mm tunnel is blunt dissected down to bone using long dissecting scissors. The leg is rotated until the X-ray projection of the posterior malleolus cortex is separate to the posterior cortex of the fibula. A radiolucent depth gauge or 2mm syringe barrel is used as a wire guide to protect the soft tissues. A guidewire is placed on the posterior malleolus cortex by feel and the leg rotated until there is no overlap between cortex and wire to help judge the exact position in relation to the fracture
and to check the wire is on the tibial cortex and not the fibula.
The guidewire is passed into the fragment and the position is checked on the AP image. The fibula is reduced into the incisura with thumb pressure. The leg is then rotated until the fracture plane is visible on fluoroscopy. The depth gauge/ syringe and guidewire are used to joystick the fragment into position and the wire is passed across the fracture. If the fragment requires further inferior translation

the wire can be angled inferiorly so that screw compression will translate the fragment distally. Once the wire is across the fragment, the depth gauge is pushed against the posterior malleolus to check the fragment will compress. Wire position is checked on the mortise view with depth gauge or artery clip against the posterior tibial cortex to assess the exact entry point, ensuring it will not irritate the fibula or syndesmosis.
The near cortex only is drilled, and one unicortical 4mm cannulated partially threaded screw and washer is inserted under image intensifier. As the washer meets the posterior malleolus it should angle to meet the cortical contour of the posterior malleolus, further confirming correct positioning, and the fracture should be seen to compress. If the wire has been angled inferiorly the fragment should reduce more distally by 1mm or so. Final checks are performed, and the percutaneous portal can be closed with skin suture alone. The surgeon is then free to complete necessary fixation of the malleoli and syndesmosis through direct approaches. n



tH e m ediAL P OSterO mediAL A PP rOACH in P OSteri O r mALL eOLA r Fr AC ture
Fix Ati O n: Safer e
xpoS
ure, Improved r eductIon, and Better o utcome S
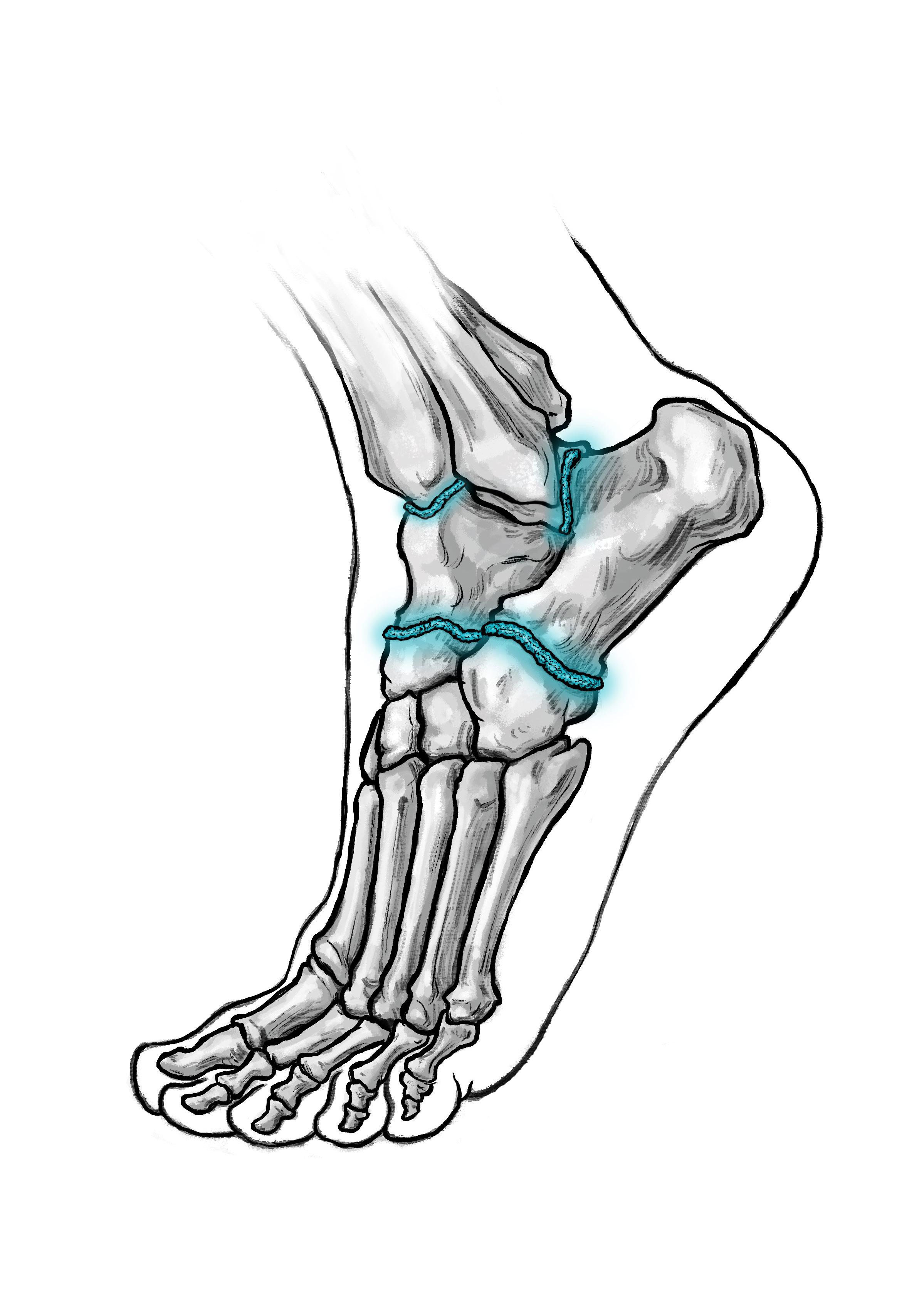
Posterior malleolar fractures (PMFs) account for up to 50% of ankle fractures when assessed with CT. The historical “one-third rule” guided fixation by fragment size; however, morphology and stability are now recognised as more important determinants of outcome.
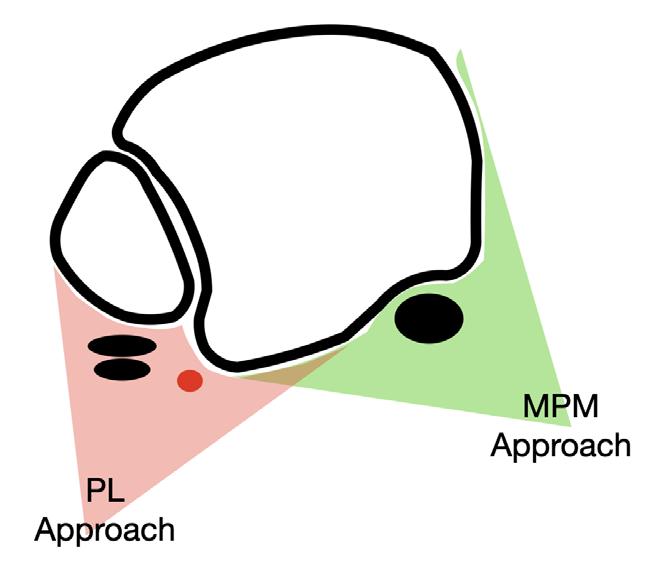
Surgical fixation of PMFs is commonplace in unstable and displaced fracture patterns. Having spent the last decade researching PMFs, one of the most significant findings has been the importance of the correct surgical approach. Although the posterolateral (PL) approach remains common, in my practice it has been completely abandoned. Increasing evidence supports the medial posteromedial (MPM) approach in the exposure and fixation of PMFs, which has substantial benefits over the PL approach.
I will discuss these advantages of the MPM over the PL approach in the following article.


what is the mPm Approach?
The MPM approach gains access to the posterior and medial aspect of the tibia. Figure 1 illustrates these steps on a cadaveric specimen. The skin incision is marked out 1cm posterior to the posteromedial edge of the tibia and can be extended anteriorly along the path of the posterior tibial tendon (PTT) if access to the anterior aspect of the medial tibia is required. The investing layer of fascia is opened longitudinally exposing the sheath to the PTT and separately the flexor digitorum longus tendon (FDL) sheath. The PTT and FDL sheaths are opened (although keeping the distal aspect intact) and access to the posterolateral tibia is gained between the PTT and FDL and the posteromedial tibia in front of the PTT.
Advantages of the mPm Approach over the PL Approach
1. Superior Exposure
The MPM approach allows good visualisation of the posterolateral,
posteromedial and medial (with anterior extension) aspect of the tibia. In comparison the PL approach allows access to a small aspect of the posterolateral tibia and the fibular (figure 2). Direct comparison of the exposures has shown almost double the surface area exposed by the MPM as compared to the PL1.
2. Soft-tissue Entrapment Clearance
PTT entrapment has been found in over 40% of PMFs when the fracture line enters the PTT sheath2. In the MPM approach, the PTT sheath is visualised, entrapment can be identified and released. With the PL approach, this is not possible.
3. Access to Die-Punch Fragments
Die-punch injuries are common in PMFs and most frequently occur under the posterolateral fragment. The MPM approach allows direct access to the die punch fragment, when the PL does not. It is easier to go through the open door than the hinge.
4. Vascular Safety
Vascular studies have shown two important aspects regarding the risks posed by the PL approach3. Firstly, the flexor hallucis longus (FHL) muscle is supplied by up to six perforators from the peroneal artery. By moving the FHL medially to get access to the posterior tibia during the PL approach, the FHL is moved away from the peroneal artery and can therefore lose its blood supply and become necrotic. If you have seen a FHL contracture following a PMF fixation, this is the reason.
Lyndon Mason Consultant, NHS University Hospitals of Liverpool Group; Honorary Associate Professor, University of Liverpool


The risk increases, the longer the incision. Secondly, and more importantly, in a twovessel limb (dominant peroneal artery and anterior tibial), the blood supply to the foot is supplied by a communicating vessel connecting the peroneal and tibial arteries (figure 3). This communicating branch is very commonly sacrificed in the PL approach If this is sacrificed in a two vessel limb, this can result in an avascular foot4. The MPM comes anterior to the FHL and communicating branch and does not have these risks.

5. Positioning and Practicality
The MPM approach can be performed in a supine, semi-prone or prone position (figure 4). This simplifyss anaesthesia, allowing easier fluoroscopy and access to the anterior tibia if required. and enabling simultaneous fibular or syndesmotic fixation.
6. Fibular fixation
Often the PL approach has been chosen due to the simultaneous access to the fibular. However, except for simple fractures, this can be problematic. In cases with high fibular fractures, anterior syndesmosis injury and significant shortening, it is technically less demanding to do a MPM approach with a supplementary direct lateral approach.
7. Revision procedures
Like in the case of die punch injuries, the MPM allows much easier access to the joint. This is achieved by hinging the PMF on the posterior inferior tibiofibular ligament. The PL approach only allows access from superior to inferior, therefore the incision has to be long.
8. Allows extension
The MPM approach is on the medial fasciotomy line and can therefore be extended as far as the knee. In contrast, the PL approach is crossed by the sural nerve, multiple muscles and the peroneal artery.
Clinical and radiological Outcomes
Recent CT-based studies have reported >90 % anatomical reduction within >>
“The mpm approach allows good visualisa T ion of T he pos T erola T eral, pos T eromedial and medial aspec T of T he
Figure 2: Schematic diagram showing access to the tibia form either the PL or MPM approach.
Figure 1: Surgical steps of the MPM approach, with the last picture illustrating the anterior extension allowing access to the medial tibia.

2mm and >90 % syndesmotic congruity after MPM fixation, however other studies using PL approach only achieve approximately 50% anatomical reduction5, 6 Our own data has shown complication rates up to 66% following PL fixation, compared with 8% using MPM when using the Clavien-Dido classification for complications.
discussion
The MPM approach overcomes the three principal limitations of PL approach, restricted exposure, unaddressed entrapment, and vascular risk. Its direct vision of the posterior and medial tibia enables true anatomical reduction, particularly in die-punch and 2B PMFs. The ability to clear PTT entrapment prevents secondary displacement and pain. Preservation of the posterior vasculature markedly decreases complication rates. Adoption requires anatomical familiarity, but reproducibility and outcomes justify its broader implementation. In my view, due the vascular risks of the PL approach specific to a two-vessel limb, continued use of the PL approach should instigate a CT angiogram pre-surgery.
Conclusion
The MPM approach provides:
• Comprehensive exposure of the posterior and medial tibia.
• Effective clearance of posterior tibial tendon entrapment.
• Direct management of die-punch fragments.
• Superior vascular safety compared with posterolateral dissection.
Across anatomical, biomechanical, and clinical domains, the MPM approach is showing safer and more accurate fixation than PL. It should be considered the preferred exposure for most posterior malleolar fractures with medial or central involvement. n
References
1. Philpott MDG, Jayatilaka MLT, Millward G, Molloy A, Mason L. Posterior approaches to the ankle - an analysis of 3 approaches for access to the posterior malleolar fracture. Foot (Edinb). 2020;45:101725.

2. Aamir J, Syziu A, Andritsos L, Caldwell R, Mason L. Tibialis posterior tendon entrapment in posterior malleolar and pilon injuries of the ankle: a retrospective analysis. Eur J Orthop Surg Traumatol 2024;34(2):781-7.
3. Heeran N, Gomaa AR, Mason L, Bond AP. The arterial risk posed by the posterolateral approach: An anatomical cadaveric study of the fibular artery and its variability. Clin Anat. 2024;37(8):840-8.
4. Sandelin H, Tukiainen E, Ovaska M. Amputation following internal fixation of an ankle fracture via the posterolateral approach - a case report. Acta Orthop. 2017;88(3):358-60.
5. Franx AL, Verhage SM, Krijnen P, Twiss ELL, Schipper IB, Hoogendoorn JM. Open reduction and fixation does not improve short-term outcome of mediumsized posterior fragments in AO type B ankle fractures: one-year results of the POSTFIX randomized controlled trial. Bone Joint J 2025;107-b(4):461-9.
6. Pino F, Lagos L, Urbina C, Vargas F, Parra M, Bravo F, Bastias C. Reduction Quality in Posterior Malleolar Fractures Using a Modified Posteromedial Ankle Approach. Foot Ankle Orthop. 2024;9(4):24730114241290201.
Figure 3: CT angiogram pre fixation of a PMF, showing a 2-vessel leg due to sclerosis of the posterior tibial artery, where the peroneal artery becomes dominant through the communicating branch.
Figure 4: Intraoperative fluoroscopy and clinical images showing placement of the metalwork in a 2B fracture type, through the MPM approach in the supine position.


•
•

•


Endoscopic Debridement, Ostectomy, Release and Radiofrequency (DORR)

A Fully endoscopic technique for treating recalcitrant Plantar Fasciitis: Endoscopic
Debridement, Ostectomy, Release and Radiofrequency
(DORR)
Plantar heel pain is a common problem. There are many potential pain generators; enthesopathy, fasciopathy, tension and mechanical effects of the heel spur have all been implicated in causing heel pain.
Historically, the results of heel pain surgery often result in some degree of residual pain. We hypothesize that this could be due to not addressing all the pain generators during surgery. Therefore, we have introduced the above procedure which we call DORRDebridement, Ostectomy, Release and Radiofrequency.


Keen-Wai Chong
President, Singapore
Orthopaedic Association
Vice President, Asian Federation of Foot and Ankle Surgeons
Past Chairman, Orthopaedic Foot Ankle Society Singapore
International Program Editor, AO Foot Ankle Education TaskForce 2021-2023
Procedure
This is a supra-fascial technique. A needle is used under fluoroscopy to identify the spur. Through a medial incision, blunt entry of the trocar is made at about a 30° angle. The lateral portal is identified by tenting the lateral skin (Figure 1).
A 4.0mm scope is inserted medially, above the plantar fascia, and instruments introduced laterally (Figure 2).
Visualization of the plantar fascia and the plantar heel spur is achieved (Figure 3).
Synovial debridement is achieved with an arthroscopic shaver or radiofrequency ablation to achieve haemostasis. The calcaneal spur is burred until no longer prominent or impinging on the fascia. Imaging may be used to confirm.
The medial third of the plantar fascia is released with arthroscopic scissors or a radiofrequency probe (Figures 4 & 5).
Radiofrequency micro-tenotomy is performed to cover the entire footprint
1

Figure

of the proximal plantar fascia (e.g. Smith & Nephew Topaz XL tendon Microdebrider) (Figure 6).
Post operative MRI shows resolution of intraosseous oedema of the bone spur and calcaneum, another potential contributor to pre-operative heel pain (Figure 7).
Conclusion
The DORR procedure may simultaneously eliminate many of the potential pain generators in plantar heel pain syndrome. n
Reference
Arthroscopy Techniques 13 (12), 103150, 2024. WSY Wong, D Gengatharan, IS Rikhraj, KW Chong, WX Png, EWL Cher.


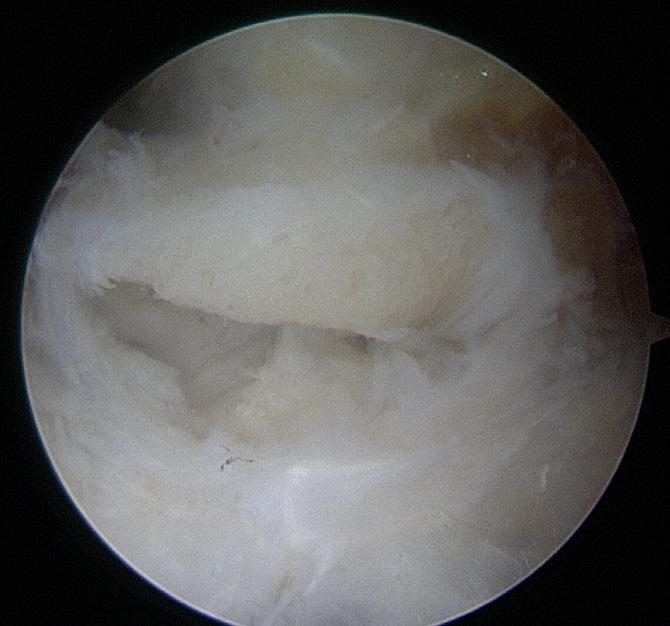
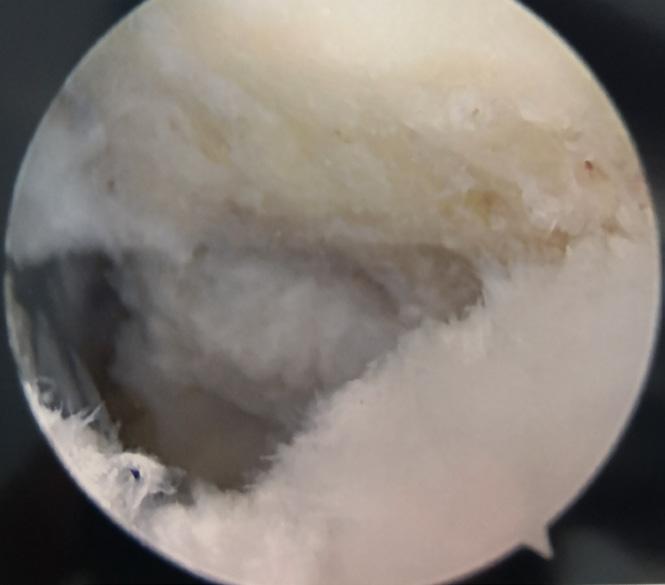



Figure 2
Figure 3
Figure 4
Figure 5
Figure 6
Figure 7

Setting up a private practice

Joel Humphrey Consultant Trauma and Orthopaedic Surgeon, Milton Keynes University Hospital

Robbie Ray Consultant Orthopaedic Surgeon, PRUH, Farnborough
why private practice tempts (and scares) us?
Private practice promises autonomy, time with patients, and potentially better pay. It also brings paperwork, upfront costs, and the uncomfortable truth that you’re running a small business. Both reactions— excitement and dread—are reasonable. This article aims to help you reflect, plan, and avoid the common traps, and most importantly, minimise the dread.
Start with some honest questions.
What’s your motive?
More income? More operating? More control over clinics and follow-up? Be honest, because your answer shapes everything from case mix to marketing.
run the numbers
Revenue builds slowly. Factor in indemnity, secretarial support, room hire, practice management software, and your time.
reality check
Private practice takes time to fill. Clinics rarely run at capacity from day one, and securing a regular theatre slot can be tricky. It’s also a competitive landscape: colleagues may view you as a rival just as you may see them as one. A little politics is inevitable, so signal your intentions early, be collegiate, and ask how you can complement—not cannibalise—the existing service.
There are upsides. You’ll have more time with patients than in the NHS—and yes, someone might even appear with tea in a

Andy Goldberg Consultant Orthopaedic Surgeon, The Wellington Hospital, London

Robert Clayton President, BOFAS
China cup—but you won’t have the same team scaffolding (no juniors to lean on) and may not have a colleague whose shoulder you can cry on.
Fit it around your nHS job properly
• Make sure there is no overlap with your job plan. Allow travel time and clinic/ theatre overruns.
• Trusts may expect you to offer an 11th PA before external work; whilst this is rarely actioned due to service constraints, it is wise to write to your clinical lead and medical director to inform them that you are starting private practice, and that you will do this in your own time and that it will not impact your NHS duties. You should also add private sessions to your job plan for transparency.
• Consider full-time private work only once you’re established. You’ll need your own appraisal, MDT and CPD setup—and without a solid peer network, the move can be daunting and lonely.
Build in stages, not in leaps
• Start in an established private hospital. One clinic a week is fine. You are likely to need to run ad-hoc theatre lists to start with, but to work on getting regular slots as demand grows.
• At the start, consider NHS Choose and Book patients. Although less well remunerated, there is usually a steady
supply of patients, and the NHS provides indemnity (reducing your indemnity costs) that can help to start to recuperate some of the upfront fees whilst increasing your elective operating volume.
• Add infrastructure as you grow. A good secretary is jet fuel. Shared services are cost-effective early; there are outsourced practice management services, which are an excellent way to kick-start the practice. They take a proportion of your income but can offer everything from a secretary to billing services. In addition, in some parts of the country, there are orthopaedic groups that offer the same service, which can help you feel part of a bigger picture, but as you grow, having your own dedicated secretary can be transformational and also provide a lot more control and autonomy and offer a much more personalised patient service.
• Invest in basics before bells and whistles. A simple website, accurate hospital profiles, and clean patient information beat flashy campaigns. Remember, if you are too exposed online, your colleagues may feel you are a self-publicist, and that can count against you.
• Remember referrals. They come from GPs, physios, colleagues, insurer directories and word-of-mouth. Your NHS reputation is an important key in this process, but it doesn’t guarantee referrals. Keep GP letters crisp, simple, and timely. Avoid too much jargon and spell out acronyms (e.g., osteochondral defect, not just “OCD”) so nothing gets lost - or misread by the GP as obsessive-compulsive disorder.
• Keep information up to date: Make insurer profiles (e.g., Bupa Finder) accurate and up to date. A professional headshot helps more than you think.
Your online footprint (keep it simple)
You need three things:
1. A personal website you control: who you are, what you treat, where you work, how to book, and patient resources. Use language that speaks to the patient, not your colleagues.
2. Polished hospital profiles with a professional photo. Many allow direct bookings, so explore this option early.
3. A review trail that reflects your care. Remember, a happy patient is often your best marketer. There are many review sites such as Doctify, Top Doctors, Iwantgreatcare, Google business reviews, and some charge a monthly fee, and so you cannot do all, but best to choose one, and populate that at the start - remember some platforms feed into insurer finders –ask your hospital team which.
the nuts and bolts: privileges, governance, data
Practising privileges
There are registration and regulatory requirements to be aware of. Any doctor fully registered with the General Medical Council (GMC), in accordance with the provisions of the Medical Act 1983, is entitled to set up in private medical practice; nevertheless, you must practise within your scope of practice. A licence to use the facilities of a private hospital is known as practising privileges, and consultants are independent contractors of the hospital. Apply to one reputable hospital to start with. You’ll need: GMC licence, references, indemnity, DBS, vaccinations, and appraisal/revalidation evidence. You may have an interview and a probationary period. Admitting rights are generally approved through the hospital's medical advisory committee (MAC). Expansion to other hospitals should be slow, deliberate, and driven by your patient flow.
Records & data protection
Pick a secure, compliant electronic records system (ERS). If you process patient data, you need to register with the Information Commissioner’s Office (ICO) and pay

their fee. Follow UK GDPR, use encrypted devices, secure email, and keep a clear written data policy. AI scribing can be worth it if it saves time and clinic costs. Finally, check your ERS plays nicely with your hospital’s IT—some sites run strict firewalls to reduce cyber-risk, and incompatibility will stall your workflow.
Indemnity
NHS cover does not extend to private work. Shop around: Medical defence organisations (MDU/MPS) and commercial insurers offer different structures. It’s your largest early outlay—budget accordingly. Most will offer special rates for your first year of practice, so it's not disabling.
Private Practice Register (PPR)
The PPR is a centralised system for your professional details used by many hospitals and insurers. It’s run to streamline credentialing and cut down on repetitive form-filling. Complete it early; update at least every six months. Once your privileges are confirmed, apply to the major insurers for recognition and fee schedules.
Healthcode & invoicing
Healthcode is the backbone for e-invoicing to insurers, acting as the electronic clearing house. You’ll still need to collect patient excesses and shortfalls—either inhouse or via a billing service. Be aware that Healthcode is jointly owned by the major UK private medical insurers (and Nuffield Health), so it's not necessarily acting with your best interests at heart.
Fees, billing and the awkward bits
Fee-assured or not?
• Fee-assured: you agree to the insurer’s rates; fewer shortfalls, smoother referrals.
• Non-fee-assured: you set higher fees; patients pay the shortfall. Early on, this can dampen referral flow. Most insurers now do not offer you the option of being non-fee assured, and hence you either accept their terms or choose not to see their patients.
Billing: Who does it?
• A switched-on secretary can manage codes, claims and reconciliations.
• Outsourced billing takes a percentage but usually lifts collection rates and saves your evenings. Most of the work is chasing small policy excesses— labour-intensive and morale-sapping if you do it alone.
Competition law—don’t get burned
Private practice fees from insurers have been effectively frozen since the early ’90s, so in real terms, surgeons are being paid far less for doing more. However unfair that feels, the CMA rules are crystal clear: surgeons must not discuss or agree fees collectively or organise any joint action to pressure insurers. Societies (including BOFAS) are no exception—there are precedents of heavy fines for groups and even hospitals when lines were crossed. Keep your pricing decisions strictly your own. Play it smart and stay lawful. Don’t swap notes on fees; if you see insurers restricting patient choice or diverting referrals, report it to the BOFAS private practice committee, the Independent Doctors’ Federation, BMA, or FIPO.
Transparency for patients
For non–non-fee-assured and selfpay patients, be transparent: publish your charges and keep your profile on the Private Healthcare Information Network (PHIN) up to date so patients can see fees, performance and feedback and make informed choices.
Money management (we weren’t taught this)
• Separate bank account, even if you start as a sole trader; treat it like a business from day one.
• Hire an accountant who knows medical practice. Worth every pound.
• Tax pot: park 20–30% of every payment until you have tailored advice.
• Allowable expenses may include indemnity; professional fees; room hire; software; billing/secretarial support; travel to clinics/theatres; conferences and CPD; and genuine home-office use. Keep meticulous >>

receipts and records. Most directly provided medical services are VAT exempt.
• Structure: sole trader (simple) vs limited company (more admin, more flexibility). Decide with your accountant; it’s personal.
A
quick checklist for starting PP
Define your motive and case mix.
Cost your first 12 months (indemnity, rooms, secretary, software).
Secure one hospital practising privilege.
partner

Complete PPR, apply for insurer recognition.
Choose ERS, pay ICO, set GDPR policies.
Decide billing (secretary vs outsourced).
Build a simple and clear website to start with; update hospital/ insurer profiles.
Set up a review site and ask for reviews early on
Plan clinics + theatre to match demand; grow slowly.
S ocIetIe S

Dear Colleagues,
Tell your clinical lead/MD; align with your NHS job plan.
Find an accountant; open a business account; ring-fence tax.
Final thought
Private practice can be hugely rewarding— clinically and financially—if you respect it as a business, grow it deliberately, and always keep patients at the centre. But remember, it’s as much a lifestyle choice as a career move. Start small, be transparent, stay on the right side of governance and competition law, and build a team (however lean) that lets you spend your time where it matters: looking after patients. n
The Egyptian Foot and Ankle Society (EGYFAS) is a professional organization devoted to advancing knowledge, education, and training in the field of foot and ankle surgery.
Founded in 2009 by leading Egyptian orthopedic foot and ankle surgeons, the society today includes more than 165 active members and hundreds of participants from across the Arab world. I am delighted to introduce myself and the society to BOFAS bulletin footprint and looking forward to deepened collaboration with the British Orthopaedic Foot and Ankle Society (BOFAS) in the coming years.
Ossama El Shazly, MDA in Shams University President Of EGYFAS
It is my pleasure to represent the Asian Federation of Foot & Ankle Surgeons (AFFAS) in making this introduction to the members of BOFAS.
AFFAS traces it's history to 1993 when the first Asian Symposium on Foot Surgery was held. This was in Japan and it was organised by Professor Takakura.
Eventually it evolved into a formalised grouping with triennial meetings. In recent years, because of the strong interest in Foot & Ankle Surgery, it has now evolved into a biennial congress.
The next congress is going to be held in Singapore on October 30th- November 1st. This is the premier foot and ankle event in the Asian calendar. I would like to extend an invitation to any

interested British colleagues to come and participate in this scientific event. All the Asian foot and ankle thought leaders and clinicians will be there.
In addition, I am grateful to Dr Jitendra for starting this point of contact between BOFAS and AFFAS. I'm looking forward to a fruitful and engaging relationship in the coming years.
Dr CHONG Keen-Wai Vice President and incoming President, AFFAS





Practice Ready Orthopaedic Foot & Ankle Surgery (PROFAS) 2026 Webinar Series
NEW JOINT INITIATIVE FROM BOFAS, BOA AND BJJ
PROFAS, a webinar series designed to deliver world-class training in clinical excellence, leadership and team development.
Essentials
Date: starts Tuesday 13 January 2026 (sessions every other week) th Time: 19:45 (GMT)
Format: online and on-demand
Price: Member* £500 | Nonmember £700 | Trainee £300 *member of BOFAS or BOA
Course leads:


Designed for senior trainees, Fellows and new consultants
Real-world clinical decision making. Case-based discussions, interactive polls and peer engagement. Tips and tricks. Practical learning, deeper clinical insight and immediate relevance to everyday practice.
Brought to you by The T&O Education Partnership






















Mrs Anna Chapman Mr Yaser Ghani Register here!

PrOteC ting vALue in
n HS FOOt And Ank L e SurgerY - evidence from the Bofa S registry -
introduction – when Proven Procedures Are removed
The recent decision by NHS Hampshire and Isle of Wight Integrated Care Board to add first metatarsophalangeal joint (MTPJ) fusion to its list of “procedures of limited clinical value” has exposed a growing disconnect between evidence of effectiveness and commissioning policy. At a time of unprecedented financial pressure, NHS commissioners are tasked with prioritising high-value interventions. Yet paradoxically, 1st MTPJ fusion, a reproducible, durable, and clinically proven operation, has been restricted. Musculoskeletal disease now represents one of the leading causes of disability and long-term NHS expenditure1. In this context, the challenge is not to remove procedures, but to identify and protect those that deliver demonstrable value.
registry data – evidence for Clinical and economic value
The recent publication by Feroz et al on the clinical outcomes of 1st MTPJ fusions from the British Orthopaedic Foot & Ankle Society (BOFAS) registry showed significant and sustained improvements in all domains of the patient-reported outcome measures (MOXFQ and EQ-5D) at six and twelve months, encompassing pain, walking and standing, social interaction, and overall quality of life2. It is also possible to use the BOFAS registry to enable health economic modelling to quantify value in the same terms used by NICE and NHS commissioners: cost per quality-adjusted life year
Authors: Lyndon Mason, Robert Clayton, Karan Malhotra, Joel Humphrey, Dave Townshend
(QALY) gained; this is also known as the incremental cost-effectiveness ratio (ICER), and can be used to fairly compare interventions spanning differing specialities
economic evaluation – defining Surgical value
A soon-to-be-published study using EQ-5D-derived QALYs and NHS tariff costs (£1,955–£4,209 per procedure plus implant costs) was conducted using both sensitivity analysis and Markov models. The BOFAS registry-derived outcomes showed a mean EQ-5D improvement of +0.24 within one year. This is well above the UK minimally important clinical difference for the EQ5D (0.082). When extrapolated over the mean remaining lifespan of 15.4 years, this equates to a lifetime QALY gain of 1.88 to 3.954. For the Markov model, complication rates
were derived from the literature, with weighted pooled annual incidences of complications including nonunion 5.4%, symptomatic non-union 1.8%, malunion 6.1%, and hardware removal 8.5%5. The discounted lifetime cumulative cost was £4,698.15, and the incremental cost-effective ratio was £1,410.58 per QALY, confirming exceptional value for money and dramatically below the NICE costeffectiveness threshold of £20,000–£30,000 per QALY6
Comparative Context – Hip and knee replacement Benchmarks To place these findings in context, a study on total hip replacements, which included an analysis of over 240,000 patients from the National Joint Registry, found lifetime QALY costs between £10,781 and £28,6777 Cost per QALY reported in total knee replacement in a study on over 1.5 million patients showed a range from £14,881 to £48,248. In comparison, 1st MTPJ fusion demonstrates a comparable QALY gain per patient but at a much-reduced cost, due to the comparable improvement in patient
“The findings from T he B ofas r egis T ry show T ha T T his procedure delivers long- T erm B enefi T , excep T ional cos T efficiency, and significan T quali T y-of-life improvemen T .”
outcomes, low cost of primary surgery, comparable low cost of revision surgery and a low rate of complications.
Conclusion – the value of data in Protecting Patients
The findings from the BOFAS Registry show that this procedure delivers long-term benefit, exceptional cost efficiency, and significant quality-of-life improvement. In economic terms, it performs better than many procedures long accepted as NHS standards. Restricting such a procedure undermines both clinical outcomes and economic stewardship. Removing access to proven, low-cost interventions will not save the NHS money; it will shift costs downstream to chronic pain management, mobility loss, and social care. As the NHS continues to face difficult funding decisions, this evidence should guide policy: 1st MTPJ

fusion is not a procedure of limited value; it is a procedure of proven value. n
References
1. Clayton R. Healthcare Inequality. The Times. 2025 11th October 2025.
2. Feroz J, Nilesh M, Lyndon M, Paul H, Alison R. Accuracy and quality of the British Orthopaedic Foot and Ankle Society (BOFAS) Registry - Ankle Arthrodesis Pathway. Foot Ankle Surg 2022;28(3):362-70.
3. Karski M, Ajis A, Clough T. Using service line reporting software to evaluate income and cost of hallux valgus surgery in an NHS Hospital: coding is critical! British Orthopaedic Foot and Ankle Society 2013.
4. Disparities OfHIa. Economic evaluation: health economic studies. How to use an economic evaluation to evaluate your digital health product. In: Disparities OfHIa, editor. 2021.
5. Roukis TS. Nonunion after Arthrodesis of the First Metatarsal-Phalangeal Joint: A Systematic Review. The Journal of Foot and Ankle Surgery 2011;50(6):710-3.
6. McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold: what it is and what that means. Pharmacoeconomics. 2008;26(9):733-44.
7. Clarke A, Pulikottil-Jacob R, Grove A, Freeman K, Mistry H, Tsertsvadze A, et al. OP75 NICE Hips: hip replacement interventions for osteoarthritis in the UK – a clinical and cost-effectiveness analysis. Journal of Epidemiology and Community Health. 2014;68(Suppl 1):A37-A8.
8. Mari K, Dégieux P, Mistretta F, Guillemin F, Richette P. Cost utility modeling of early vs late total knee replacement in osteoarthritis patients. Osteoarthritis and Cartilage 2016;24(12):2069-76.
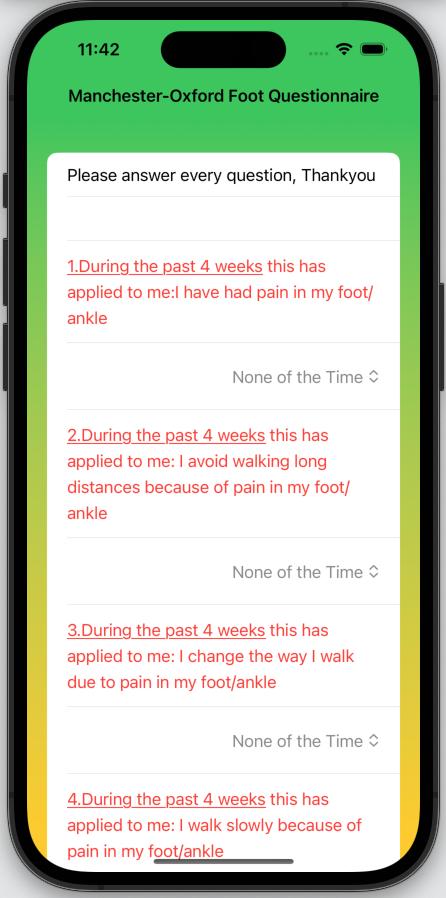

and
is now available For use on any iOS device (iPhone,iPad and Mac) on the app store.
in clinics and the preoperative situation for patients undergoing foot and ankle surgery.
paper questionnaires and can be sent to patients by email for postoperative follow-up
Developed under licence from Oxford University Search MOXFQ on app store or use QR code below to access The validated
Calculates total and metric MOXFQ scores
Calculates walking, pain and social interaction scores

Manchester-Oxford-Foot
Ankle-Questionnaire

national guidance relevant to foot and ankle published over the past one year
BOA Specialty
Standards (SpecS)
Management of End Stage Ankle Arthritis
April 2025

https://www.boa.ac.uk/asset/A811FC01 %2DEFC3%2D44B7%2DBF6C4B0D4D4C 2C85/?_gl=1*1nd8b52*_up*MQ..*_ga*Mz QzNzkxNzI3LjE3NTEyNzc5NDU.*_ga_GZ M76H2EF6*czE3NTEyNzc5NDQkbzEkZz AkdDE3NTEyNzc5NDQkajYwJGwwJGgw
Background and Justification
End stage ankle arthritis is usually treated with Total Ankle Replacement (TAR) or Ankle Fusion (AF) and patients should have either option available. Outcomes may be improved with discussion in an ankle arthritis network and concentrating TAR to centres where they are regularly performed. This facilitates referral and communication, reduces clinical variance, and ensures equitable, cost-effective access to high quality care.
Inclusion: All patients being considered for primary or revision AF and TAR. Ankle fusion in the context of limb reconstruction should be discussed either in an ankle arthritis network or limb reconstruction MDT that follows the same guidelines. Exclusions: Immediate ankle fusion following trauma.
Summary of Standards
1. Healthcare teams providing surgical treatment for ankle arthritis should have access to, and engage with, an ankle arthritis network.
2. An ankle arthritis network should:
a. reflect local resources and geography
b. have access to patient records and all relevant imaging
c. have a designated co-ordinator or lead
d. occur with sufficient frequency to avoid delays in treatment
e. record the outcome in the patient’s record
f. facilitate training of all relevant healthcare providers.
3. Imaging protocols should be agreed and standardised across the network.
4. Transfer and discussion between units should not delay definitive treatment.
5. The discussion with the patient must include and document:
a. non-operative options
b. surgical risks, benefits and longterm outcomes of TAR and AF c. patient information resources
6. All patients scheduled for primary or revision TAR must be admitted to a ring-fenced facility that follows GIRFT guidelines and practices.
7. All primary and revision TAR should be performed in a dedicated clean air orthopaedic theatre.
8. Dual surgeon operating is recommended for complex cases and training.
9. Surgeons performing TAR must submit data to a national joint registry.
10. Primary TAR must have clinical and radiological follow up for a minimum of 2 years with direct clinical review available for the lifespan of the implant.
11. AF must have clinical and radiological follow up until clinical and / or radiological evidence of fusion.
12. Revision TAR must have annual clinical and radiological follow up for the lifespan of the implant.
13. Infection must be considered in all failing TARs and management should be directed by the peri- prosthetic joint infection SpecS: https://www.boa.ac.uk/resource/ speciality-standards-specs-periprosthetic-joint-infection.html
14. Access to plastic and vascular surgeons should be available for all revision TAR, either locally or through the ankle arthritis network.
BOA Standard
Mobilisation and weightbearing after orthopaedic surgery/ musculoskeletal injury August 2024 https://www.boa.ac.uk/ resource/mobilisationand-weightbearing-afterorthopaedic-surgerymusculoskeletal-injuryboast.html

Inclusion: All patients with orthopaedic conditions affecting the pelvis, upper, and lower limbs.
Standards for Practice
1. All patients should have a clearly documented rehabilitation plan detailing instructions for weightbearing as an integral part of their mobilisation status.
2. Patient instructions should be provided in a format that is tailored to their individual needs.
3. A weightbearing status should be attributed to each affected limb.
4. The following specific terms should be used to define weightbearing status:
a. Non Weightbearing
b. Limited Weightbearing
c. Unrestricted Weightbearing
5. Terms such as touch, partial, proportional, permissive, or progressive weightbearing should no longer be used.
6. All instructions for non- and limited weightbearing require the following detail to be documented:
a. Clinical justification - including the rationale for prevention / limitation of weightbearing by the clinician making the recommendation
b. Quantification
i. Limitations should include accurate descriptions of functional restrictions (e.g. no stairs, no sports) or distance restrictions (e.g. indoor only, bed to chair)

Foot Print
ii. Limitations should not be quantified by percentage body weight, kilograms of force or similar descriptors
c. Duration, including planned phases of care progressing through any weightbearing statuses outlined in 4 a-c
7. Any requirement for walking aids or additional specific rehabilitation protocols (e.g. braces) should be
recorded alongside the weightbearing and mobilisation instructions.
8. Inpatients should have a weightbearing status review at intervals no longer than 72 hours.
9. Any patient whose weightbearing status directly affects their ability to be discharged from hospital should have it reviewed within 24 hours.
10. All weightbearing prescriptions should be reviewed at each point of follow up. n
BOFAS and partner societies events calendar 2026
13-14 December 2025 EFAS hindfoot
Augsburg, Germany
22-23 January 2026 BOFAS minimally invasive surgery course Bristol, UK
22-24 January 2026 AOFAS Winter Meeting
5-6 February 2026 EFAS forefoot course and hindfoot deformities in relation with forefoot pathologies
The Meritage Resort and Spa, Napa, California, USA
Barcelona, Spain
10-11 February 2026 BOFAS principles of foot and ankle surgery Liverpool, UK
26-27 February 2026 EFAS sports and arthroscopy course Vienna, Austria
6 March 2026 AOFAS/LLRS Specialty Day
Morial Convention Center, New Orleans, Louisiana, USA
20 April 2026 BOFAS diabetic foot principles Milton Keynes, UK
23-25 April 2026 AOFAS Complete Foot Care Course
Omni Charlotte Hotel, Charlotte, North Carolina, USA
24-25 April 2026 EFAS instructional course Lisbon, Portugal
15 May 2026 BOFAS Allied Health Professionals course (AFAP) Bournemouth, UK
21-22 May 2026 EFAS degenerative ankle arthritis
Copenhagen, Denmark
29-30 May 2026 AOFAS Basic and Advanced Minimally Invasive Surgery Training Course National Bioskills Laboratory, Farmers Branch, Texas, USA
3-5 June 2026 Advanced Fellows Forum (via invite only) Coventry, UK
10-12 June 2026
2 July 2026
3 July 2026
3-4 July 2026

EFAS minimally invasive surgery course
BOFAS basic arthroscopy skills
BOFAS advanced arthroscopy skills
Nottingham, UK
Solihull, UK
Solihull, UK
British Indian Orthopaedic Society (BIOS) annual conference Leicester, UK

viSuALiSAtiOn in OrtHOPAediCS How to convert complex procedures into routine work
As junior orthopaedic trainees, most of us have scrubbed into countless operations - some of which ran smoothly and others which unravelled before our eyes. In nearly every instance where things went wrong, a retrospective analysis reveals the same uncomfortable truth: the complications were avoidable. They stemmed not from lack of skill, but from a lack of foresight. This is where the practice of visualisation becomes not just helpful, but essential.
visualisation:
Breaking the whole into Parts Visualisation, in the surgical context, is the mental rehearsal of an operation before stepping into the theatre. It involves breaking down a complex procedure into distinct stages and mentally walking through each part. This isn’t daydreaming, it’s structured cognitive preparation1
At each stage, the surgeon must ask:
• What are the instruments required to complete this part efficiently?
• What challenges might arise here, and how can I pre-empt them?
• Which team members do I need particularly engaged at this step?
This kind of anticipatory thinking doesn’t just prevent intraoperative surprises, it also sets the tone for precision, preparedness, and professionalism.
wisdom in Planning
Abraham Lincoln said, “Give me six hours to chop down a tree and I will spend the first four sharpening the axe”. This quote is more relevant to orthopaedic surgery than it may initially appear. Every major operation is a project - one that, like any large undertaking, demands meticulous preparation.

Hisham Shalaby Consultant Orthopaedic Surgeon, Royal Infirmary of Edinburgh
In their 2023 book “How Big Things Get Done”, authors Bent Flyvbjerg and Dan Gardner analyse why major projectsfrom construction to IT - fail. The culprit, more often than not, is poor planning.
Successful projects are those whose leaders spend more time in the planning phase, anticipating friction points and aligning their teams around a shared vision2. For orthopaedic surgeons, big procedures are our big projects, and they fail for the same reasons.
Preference Sheets: tools for Surgical Clarity
Two critical planning tools can help translate this visualisation into practice:
1. Preference Sheets: These are global lists of required instruments, implants, and consumables. They are static and non-time-specific—a master checklist for what the operation might need.
2. Walk-Through Sheets: These are more dynamic, stage-based documents that outline what is needed at each time point during the procedure. They help scrub staff and circulating nurses organise the kits in a sequence that mirrors the operation itself. By staging equipment in this way, we reduce clutter, avoid last-minute scrambles, and improve theatre flow.
From individual vision to team execution
No major procedure is completed by the surgeon alone. Successful surgery is a coordinated ballet involving anaesthetists, ODPs, scrub nurses, radiographers, and assistants. It is difficult for a team to perform well without knowing what’s coming next.
This is why the process of visualisation must be shared. During the pre-operative briefing, key elements of the surgical plan - and the rationale behind them -should be conveyed to the theatre team. This shared mental model improves performance and reduces frustration. It also builds psychological safety: when the team members know the plan, they are empowered to intervene or suggest adjustments if deviations arise (3).
team deployment in Surgery: matching Skills to moments
Each phase of an operation may require a different level of attention and expertise. For example:
• Exposure phase: Meticulous retraction may require a senior trainee to assist.
• Implant positioning: Image intensifier quality and radiographer experience are crucial.
• Closure: A junior trainee may be ideal for skin closure, freeing the senior surgeon to prepare for the next case.
Team deployment should be intentional. Just as you wouldn’t begin a procedure without confirming the right implant is on the shelf, you shouldn't proceed without knowing the right person is doing each task.
why it matters
The benefits of visualisation are not abstract. They include:
• Improved intraoperative efficiency
• Better patient outcomes
• Higher team morale and less stress in theatre
• Greater respect and trust from your team
• A reputation for professionalism and surgical excellence
Put simply: “Failing to plan is planning to fail”4. However, planning is not about knowing every answer in advance. It is about creating a framework in which you - and your team - can think clearly under pressure and adapt as needed5, 6
making it routine
Ultimately, the goal of visualisation is to convert complex operations into routine work. When we mentally walk through

procedures, communicate clearly with our teams, and anticipate every critical moment, we take operations that were once daunting and make them feel controlled, predictable and even elegant. This mindset - of preparation, structure, and shared vision - is the hallmark of a mature surgical practice2,7. n
References
1. Walshaw J, Huo B, Barach P, Banks P, McClean A, Lebon F, Mushtaq F, Jayne D, Miskovic D, Yiasemidou M. Embedding mental rehearsal in surgery: a comprehensive review of the evidence. Br J Surg 2023;110(5):457–466. doi:10.1093/bjs/ znad020
2. Flyvbjerg B, Gardner D. How Big Things Get Done: The Surprising Factors That Determine the Fate of Every Project,
the first BOFAS research day
On Monday 29th September, the BOFAS Scientific Committee held the first BOFAS Research Day at the Royal College of Surgeons of England. The purpose of the day was to raise the profile of foot and ankle research in the UK and provide opportunities for networking with research interested clinicians.
We were pleased to have attracted a mixed group of enthusiastic delegates including consultant orthopaedic foot and ankle surgeons, resident doctors, fellows and AHPs with a research interest. The variety of experience in the room provided ample opportunity for cross-pollination of ideas and discussion.
Faculty included Prof. Joy Adamson from York Clinical Trials Units, who advised delegates on trial design and working with clinical trials units and the research support service and sparked debate about how patient and public involvement be used to enhance grant applications.
Daniel Marsland, a consultant from Hampshire, who has a research interest in biomechanics, used his experience

as an editor with the Bone and Joint Journal to talk about writing for publication, which gave immediately applicable writing and editing advice and was very well received, particularly by the early career researchers.
Toby Jennison, a consultant working in Plymouth, previous NJR fellow and member of the NJR scientific committee, give a talk aimed at residents and fellows was full of tips on getting involved in research during training and making space for research as a consultant.
Dave Townshend, visiting Professor at Northumbria University and Chair of the Scientific Committee, spoke about the importance of commercial research and how to work with companies on investigator-initiated research, drawing on his own experience from the Infinity and Adaptis studies.
Adrian Kendal, consultant in Oxford, provided insight into working with big data, including HES data and registries, and how this be used for research questions that are not suited to randomised controlled trials.
from Home Renovations to Space Exploration and Everything in Between. Penguin Random House; 2023.
3. Pavlidis TE, et al Teamwork in the Operating Room: Surgical Teams' Attitudes Toward Team Performance and Safety. Surg Today 2020;50(5):458–464. doi:10.1007/ s00595-020-01956-0
4. Covey SR. The 7 Habits of Highly Effective People. Free Press; 1989.
5. Gawande A. The Checklist Manifesto: How to Get Things Right. Metropolitan Books; 2009.
6. Klein G. Sources of Power: How People Make Decisions. MIT Press; 1999.
7. Royal College of Surgeons of England. Good Surgical Practice. London: RCS England; 2014.

Rhian Milton-Cole, a researcher from Bart’s Health with a physiotherapy background presented an eye-opening talk on developing and testing complex interventions, providing insights into an area of research new to many of the faculty and delegates.
We rounded out the day with an open forum for delegates to pitch their research ideas for advice from the faculty on methodology and funding sources.
The day was successful in providing opportunities for learning, networking and collaboration and we look forward to expanding this further in future years. n
If you have a hobby you would like to share with us, please email the editor at honorarysecretary @bofas.org.uk
HOBB ie S CO rner


With limited time for relaxation and so many things I like, I often find myself struggling to decide which avenue to pursue in my spare time. Therefore combining my interests always seems like the most efficient use of my free time! Most recently I've bought a 3D printer at home - this has allowed me to combine my passions of technology and learning new skills, with creativity and a little bit of

PriCkLY PeArS & PeAnutS, OrgAn PiPeS!
Those are some cacti common names you see in garden centres but they are labelled as such, simply because the nomenclature of these ubiquitous plants is a mind boggling challenge to anyone's memory. For the last quarter of a century I've been growing cacti & succulents.it started when we bought a farmhouse with ample space for a large 30ftx8x8 greenhouse. There are over 300 species of these mesmerising and sometimes challenging plants.
Myth 1: Folk say to me "You must feel you're back to your native Egypt?" Nothing, not even cacti grow in the Sahara. It never rains!
Myth 2: "But cacti don't need water!?" Wrong again, they do require plenty of water in the growing season. In habitat, South America, Mexico, California and the RSA, either it rains copiously for 3 weeks yearly, or the air is heavily misted up ie the Andes. Plants store water there and then, in their bulbous domes and large stems. That's usually enough as a yearly supply.
Myth 3: "I thought cacti never flower". Equally wrong! If you don't get flowers, you're doing something wrong. Flowers are plentiful, colourful and regularly bloom.
Large columnar species can't flower in cultivation..They need freerooting. When potted, they grow slowly and vertically in adequate conditions.


manual dexterity. I love the process of finding 3D models, or creating new models on Blender. Once printed the models require sanding and prepping, priming, and finally painting. There is a peace to shutting yourself off from the world and other thoughts and just focussing on painting a model whilst listening to appropriately themed music! This has also been a hobby I can work on with my son who is very involved in the whole process.
Karan Malhotra n
repotting, propagating, fighting mealy bug or redspider mite. Rain water is essential. Its PH is slightly acidic mimicking habitat conditions.
My 200 plants do not rule my life, but I spend at least an hour daily attending to them from March to October.
In winter, "supervised neglect" is required making sure heating and ventilation are provided round the clock. Most survive down to 6°C no less.
I've inherited many a poorly or neglected plant reviving them for their dismayed owners,only to be told "You've done wonders with my plant, you may as well keep it; it looks happier with you!"
Why cacti? I don't know the answer to the question. But, orthopods are mostly visual and creative individuals, craftsmen rather than scientists, and most do like a challenge.
Magdi Greiss
n
Myth 4: "Cacti don't need care or looking after". They require dedication, spring to autumn, diligent watering, feeding,
PS
…
Peanut Cactus real name is Chamaecereus Sylvestrii; Prickly Pear is Opuntia Macrodasys and Organ Pipe Cactus is Stenocereus Thurberii. See what I mean for the need to simplify!
DUROLANE hyaluronic acid (HA) therapy:
• Provides longer-lasting OA knee pain relief versus intraarticular steroid*1
• DUROLANE has a half-life of 30 days in the human joint with a single-injection treatment regimen.2
• HA may, with repeated courses of single-injection treatment, delay the need for joint replacement surgery3


UK/IR
Email: cc@BioventusGlobal.com
UK toll free: 0800 05 16 384

Fax: 0207 147 1430 IR toll free: 00800 02 04 06 08 and 00800 03 05 07 09 Fax: 0165 39103 Germany
Tel toll free: 0800 - 183 37 35 Fax: 032 - 22 10 94 056
*Based on OMERACT-OARSI responder rate at 26 weeks vs methylprednisolone acetate (MPA).
References: 1. Leighton R, Åkermark C, Therrien R, et al. NASHA hyaluronic acid vs methylprednisolone for knee osteoarthritis: a prospective, multi-centre, randomized, non-inferiority trial. Osteoarthritis Cartilage. 2014;22(1):17-25. doi:10.1016/j.joca.2013.10.009 2. Edsman K, Hjelm R, Lärkner H, et al. Intra-articular duration of Durolane™ after single injection into the rabbit knee. Cartilage. 2011;2(4)384-8. doi:10.1177/1947603511400184 3. Romero Jurado M, Enrique Fidalgo A, Rodríquez Villar V, Mar Medina J, Soler López B. Factors related with the time to surgery in waiting-list patients for knee prostheses. Reumatol Clin. 2013;9(3):148-55. doi:10.1016/j.reuma.2012.09.003
Summary of Indications for Use: DUROLANE (3 mL): Argentina, Australia,† Brazil, Chile, Colombia, EU,† India, New Zealand,† Russia, Switzerland,† Turkey,† United Arab Emirates: Symptomatic treatment of mild to moderate knee or hip osteoarthritis. In addition, DUROLANE has been approved in Australia, EU and New Zealand for the symptomatic treatment associated with mild to moderate osteoarthritis pain in the ankle, shoulder, elbow wrist, ingers, and toes.
Mexico: Symptomatic treatment of mild to moderate knee osteoarthritis.
Taiwan: Treatment of pain in OA of the knee in patients who have failed to respond adequately to conservative non-pharmacologic therapy and simple analgesics, e.g., acetaminophen.
Canada:† Symptomatic treatment of mild to moderate knee or hip osteoarthritis. In addition, DUROLANE has been licenced for the symptomatic treatment associated with mild to moderate osteoarthritis pain in the ankle, fingers and toes.
Summary of risks: You should not use DUROLANE if you have infections or skin disease at the injection site. DUROLANE has not been tested in pregnant or lactating women, or children. Risks can include transient pain, swelling and/or stiffness at the injection site.
†DUROLANE is also indicated for pain following joint arthroscopy in the presence of osteoarthritis within 3 months of the procedure. Full prescribing information can be found in product labeling, or at DUROLANE.com



