The Oley Foundation is a home nutrition therapy community and advocacy group.
LifelineLetter
Living
Medical Line Entanglement:
Are You Aware?
Note: The following article is based on “Medical line entanglement: the unspoken patient safety hazard of medical devices,” by C. Larimer, V. Sumner, and D. Wander, published in Nutrition in Clinical Practice in 2023. We asked the authors to share their research here so our readers will be aware of this potential hazard and can take steps to minimize risks.

To help assist in the awareness and education about medical line entanglement (MLE), Moog Medical put together a simple infographic that can be found at moogmedical.com/understandingmedical-line-entanglement. It was designed to help readers understand what MLE is and what the potential risk is. The infographic also presents several ideas designed to encourage further discussion on medical line entanglement between caregivers and clinicians.
The use of a medical device in the home can be a complicated and challenging experience, especially when the device is used on children. In February of 2022, the US Food and Drug Administration (FDA) published a safety communication called “Potential Risk of Strangulation in Children Who Use Enteral Feeding Delivery Sets.” The publication reports the death of two toddlers as a result of medical line entanglement (MLE) and advises “feeding set tubing can become wrapped around a child's neck and cause strangulation or death.”
The risk of strangulation is not specific to enteral feeding delivery sets, however. Most medical devices have some type of cord or tubing connected to them, such as administration sets used with IV pumps, feeding sets used with enteral pumps, oxygen tubing, cables for monitoring equipment, and even power cords. When any of these cords or tubing become trapped under a person, wrapped around a body part, or when they become twisted together, it is called medical line entanglement.
Medical line entanglement can cause strangulation, as noted by the FDA, but it can also cause ligature injuries, impaired circulation, falls, and device dislodgment. It can
CONTINUED, PAGE 3
Executive Director: Beth Gore • beth.gore@oley.org
Executive Director Emeritus: Joan Bishop
Editor, LifelineLetter; Director of Advocacy: Lisa Crosby Metzger • metzgel@amc.edu
Manager of Education and Innovation: Maisy Cyr • maisy.cyr@oley.org
Manager of Clinical and Corporate Engagement: Andrea Taylor, RD, CNSC • andrea.taylor@oley.org
Administrative Assistant: Cathy Harrington • harrinc@amc.edu
Science & Medicine Advisor: Manpreet Mundi, MD, FASPEN
Medical Director/Co-Founder: Lyn Howard, MB, FRCP, FACP
Oley Board of Trustees
Kelly Tappenden, PhD, RD, President; Shirley Huang, MD, Vice President; Steve Atkinson, Treasurer; Vanessa Kumpf, PharmD, BCNSP, FASPEN, Secretary; Lisa Epp, RDN, CNSC, LD; John Mahalchak; David F. Mercer, MD, PhD, FRCSC, FACS
Oley Advisory Council
Rhonda Arends; Jane Balint, MD; Kevin Baskin, MD; Melissa Bill; Elizabeth Bond, RN; Lynda Bosworth; Phila Breeding, RN; Alan Buchman, MD, MSPH, FACN, FACP, FACG, AGAF; Marcia Denenholz; Terry Edwards; Paula Foiw-Washesky, RD, LDN, MBA; Madalyn George-Thiemann, RN, CNS; Kathleen Gura, PharmD, BCNSP, FASHP, FPPAG, FASPN; Jocelyn Hill, MN, RN, CVAA(c), OCN, CRNI, VA-BC; Joy McVey Hugick; Kishore Iyer, MBBS, FRCS, FACS; Swapna Kakani, MPH; Barbara Kapuscinska Kelly, MD; Sivan Kinberg, MD; Sue Koprucki; Jack Leibee; Laura E. Matarese, PhD, RDN, LDN, CNSC, FADA, FASPEN; Russell J. Merritt, MD, PhD; Ann Michalek, MD; Jay M. Mirtallo, MS, RPh, BCNSP, FASHP; Laurie Reyen, RN, MN; Vicki Ross, RD, PhD, CNSC; Trish Skiendziel, RD, LD, CNSC; Michael Smith; Bob and Mary Smithers; Ezra Steiger, MD, FACS, FASPEN; Marion Winkler, PhD, RD, LDN, CNSC
Subscriptions
The LifelineLetter is a quarterly newsletter available free of charge at oley.org. The newsletter is available by mail upon request. Items published are provided as an open forum for the HPEN community and should not imply endorsement by the Oley Foundation.
All items/ads/suggestions should be discussed with your healthcare provider prior to actual use. Correspondence can be sent to the Editor at the address on the left . Medical/scientific content contained herein has been peer reviewed by an Oley advisor or trustee.
Our Mission
. . . is to enrich the lives of those living with home IV nutrition or tube feeding through advocacy, education, community and innovation.
The Oley Foundation provides its 27,000+ members with critical information on topics such as medical advances, research, and health insurance. The foundation is also a source of support, helping consumers on home IV nutrition and tube feeding overcome challenges, such as their inability to eat and altered body image.
All Oley programs are offered FREE OF CHARGE to consumers and their families.
Oley Foundation Programs
• LifelineLetter
• Peer to Peer Support
• Conferences and Webinars
• Resources to Promote Living Well on Tube Feeding and IV Nutrition
• Enteral Donation Program
• Advocacy and Awareness
How to Support Oley
Donations are tax deductible and are accepted at oley.org/donations or at the street address listed below. We appreciate your support. NEW ADDRESS!
Medical Line Entanglement, continued from cover
also lead to medication errors, caused by the misidentification of lines, as noted by Goodin et al. in a 2012 article on the topic in the Journal of Pediatric Nursing. These risks can be higher with certain patient populations, including patients with limited mobility or cognitive or developmental impairment, and with children.
SURVEY SHOWS A NEED FOR AWARENESS
The authors conducted a survey to evaluate the level of awareness of MLE and to determine if caregivers receive MLE education when being discharged home with a medical device. Three groups were identified as the target audience of the anonymous online survey:
• pediatric acute care clinicians
• clinicians from outpatient pediatric GI clinics
• caregivers of patients with a medical line
With the help of organizations like the Oley Foundation, the survey was published and distributed, and the data was collected. Table 1 (below) highlights several key findings of this study. The full results were published in the American Society for Parenteral and Enteral Nutrition (ASPEN) journal Nutrition in Clinical Practice (aspenjournals.onlinelibrary. wiley.com/doi/epdf/10.1002/ncp.11000).
At the end of the survey, participants were asked if they wanted to share and explain any additional medical line entanglement–related comments they felt were important (see below). It is important to caution caregivers that one cannot fully mitigate the risk of medical line entanglement, even with the tips and tricks noted in the comments. These only help to lower the risk, not to eliminate it.*
CONTINUED
ON NEXT
PARENTS/CAREGIVERS OF PATIENTS WITH A MEDICAL LINE
Caregivers who participated in the survey were asked what type of nutritional support the patient was receiving.
• 67% of patients were receiving tube feeding
• 16% of patients were receiving parenteral nutrition (PN)
• 13% of patients were receiving both tube feeding and PN
• 4% of patients were not receiving either
105 (88%) of 120 caregivers reported their child or patient had experienced medical line entanglement. Fifteen of these 105 were caregivers of children under the age of 3. Of these 15, 9 (60%) indicated that the entanglement had occurred around the child’s neck.
The survey asked caregivers if they had received education about MLE when first receiving the medical device. Only 11 (9%) of 116 respondents reported that they had received information about the risk of MLE.
CLINICIANS FROM PEDIATRIC ACUTE CARE FACILITIES (N=34)
30 (88%) of the acute care clinicians surveyed responded that they are aware of the risks of MLE while only 1 (3%) reported that their facility has a policy or procedure in place to address MLE.
TABLE
CLINICIANS FROM OUTPATIENT PEDIATRIC GI CLINICS (N=40)
32 (80%) of the clinicians from outpatient pediatric GI clinics surveyed responded that they are aware of the risks of MLE while only 3 (8%) reported that their clinic has a policy or procedure in place to address MLE.
SAMPLING OF CAREGIVER FEEDBACK
Participants were asked to share and explain any additional medical line entanglement related comments that they felt may be important:
• We now tape her two TPN lines together, so there is a reduced risk of entanglement.
TUBE TALK
Tube Talk will return with the next issue! Share your tips with the editor at metzgel@amc.edu or address given on page 2.
TABLE 2. CAREGIVER FEEDBACK, CONTINUED
• We now use a grip lock [Grip-loc] dressing! Risk of tube coming out with entanglement is moderate.
• We use Vygon curly tubing for her IV fluids, so it is stretchy and not a major risk for her IV usage. Her g-tube cord though has no curly tubing options, so it is more prone to catching and pulling at her g-tube site.
• My son wakes at least once in the night to use the bathroom, so he untangles himself to get there. He also doesn’t roll around a lot. We secure his lines downward with a sticky device lock and run them under and out the bottom of his shirt, so they don’t wrap high around him.
• [My daughter] was able to voice that she was entangled and waited for me to respond. My son wraps the line around his leg or waist while he is playing on the floor or is restless while sleeping. I keep him in my room at night, so I am usually able to clear his lines quickly and easily. I also actively secure his lines with medical tape or clips to reduce his risk of wrapping himself, especially at night when I will also be sleeping.
• My daughter is a twin and the two of them are very active. Usually, it is just the twin with tubing getting tangled but there have been times during the day that both of them are tangled up somehow. She has a Gus Gear vest that secures her line, and we grip lock [Grip-loc] it down her back to exit at bottom of pajamas or at her waist, depending on what she's wearing. We use Vygon spiral tubing so there is a little more freedom before line starts to pull. But the tubing can cinch very tight around body parts. Some people use [a] pool noodle as tubing holder during the night, but she would 100% try to use that as a teether so not a good option. We have fabric line cover that would help but if we put it over the Vygon spiral, the spiral tubing ends up kinking over the next day from being stretched out. She doesn't stay in one position in her crib so if we clip it to the bed, it would pull out of her when she starts rolling around and flipping directions and running back and forth, etc.
• I use a line cover that I made myself to prevent entanglement.
The above was condensed and reprinted with permission from Larimer, C, Sumner, V, Wander, D. Medical line entanglement: the unspoken patient safety hazard of medical devices. Nutr Clin Pract. 2023; 1–13
SUMMARY
Our study found that overall clinicians are aware of the risk of medical line entanglement. However, many clinical institutions do not have a policy or procedure in place to address these risks. Further, the study revealed there is often no education about the risks of medical line entanglement provided to caregivers when they receive a medical device with lines for home use. This limited study suggests:
• There is a need for increased awareness and education on the risks of medical line entanglement.
• Healthcare providers of those patients who are at risk of medical line entanglement should discuss with the caregiver how to properly manage and monitor the lines of the medical devices to reduce and prevent the occurrence of devastating consequences, such as strangulation.
• As a parent or caregiver, you should ask your healthcare provider if your child/patient may be at risk of MLE. v
*Note from the editor: Additional tips for securing lines and tubes can be found at oley.org/BrightIdeas_Landing.

Change Maker: A New Look at Shortages




When Laura Bray was told that one of the critical drugs her daughter needed was on shortage, she responded by asking supply chain questions because of her extensive background as a business professor. Once she navigated the system for her own daughter, she recognized the dire needs of other patients who are reliant upon medications and drugs for survival.


Laura formed Angels for Change (angelsforchange.org) and named herself “Chief Change Maker.” The impact she is having is getting noticed locally and nationally. Laura gave testimony in a June 2023 Congressional hearing on shortages, talked about shortages at the White House in July and co-coordinated a visit from Kathy Castor to Tampa Bay area hospital roundtable and press conference.
Laura didn’t set out to specifically address the nearly twodecade parenteral nutrition (PN) drug shortage, she accidentally stumbled over it. With a complicated and well thought out algorithm, she discovered that the vast majority of the most vulnerable drugs were related to PN. Meanwhile, Oley Director of Advocacy and Outreach, Lisa Metzger, stumbled onto an article about Laura and connected her with Oley Executive Director Beth Gore.
Angels for Changeʼs Project Protect in 2022 helped reduce a major shortage related to potassium chloride and sodium chloride, two main components of PN. As Laura described this complex process, Beth asked how Oley could help protect the entire class of PN drugs, sterile injectables and fluids. Since then, Angels for Change and Oley have been working towards that goal. Oley is also working towards addressing the enteral formula shortages.
Our collaboration with Angels for Change has just begun. In July, Lisa Metzger and Oley Ambassador Crystal Killian attended Summit One, Angels for Change's annual meeting. There, representatives from all part of the supply chain-including competitors-joined with the common goal of ending shortages.
In August, Beth was interviewed by CNN for their upcoming feature about Laura in their Champions for Change segment with Dr. Sanjay Gupta. In September, Beth spoke at the Angels for Change Gala (more about that in the next issue). And much more.
Laura says, “Since our founding, Angels for Change has been ending drug shortages for our most vulnerable patients. As
Get started with Customer Care
we work to end all healthcare crises created by drug shortages, we are advocating for, and supporting, proactive, public-private partnerships at the beginning of the supply chain to create more resiliency reducing patient impact.” We are excited to be working with such a change maker as Laura. v

The broadest offering of plant-based, clinically demonstrated formulas
Nutrition Support Concerns and Priorities Survey Results
In March 2023, Oley conducted a survey titled “Patient/Caregiver Nutrition Support: Concerns and Priorities.” We had two hundred people respond. (Thank you if you were among the two hundred!) Of these, 53 percent indicated they were patients/consumers and 47 percent caregiver/family. Here are some of the overall results of that survey.
Nearly half (over 47 percent) of those responding indicated they, or the person they help care for, have been on nutrition support therapy one to five years. Thirty percent have been on therapy over ten years; 12.5 percent on therapy for less than one year; and 10 percent on therapy for six to ten years. There was an even split between those receiving enteral therapy (tube feeding) and parenteral (IV) therapy.
PATIENT/CAREGIVER SURVEY
WE ASKED PEOPLE TO RANK THE THINGS THAT MOST CONCERN/STRESS THEM
ITEM TO RANK NOTE
1 Complications related to my devices (such as G-tube clogging, central line infection/occlusion, etc.)
2 Fighting with the system (such as expenses, insurance, home care supplier, school/work, inequality, discrimination, health equity)
3 Complications related to my therapy (such as electrolytes, trace minerals, maintaining weight, etc.)
4 Mental/emotional health. (Poor quality of life. Poor balance of life responsibilities such as travel, school, work, activities of daily living. Relationships. Not knowing resources.)
5 Shortages and supply issues (not getting what I need, how much I need or a decrease in quality of the products I am receiving)
6 Attitudes of healthcare professionals. (Not feeling heard/understood by healthcare professionals. Not being a priority for my providers, my needs being put on the back burner until it becomes an emergency.)
7 Worsening symptoms of my/my loved oneʼs medical condition
8 Worried that my best isnʼt enough to keep myself/my loved oneʼs safe and I might miss something
9 Physical tasks connected to therapy (such as connecting/ disconnecting, pump set up, medication administration, organizing supplies, etc.)
10 Finding and keeping a qualified professional or team to manage my nutrition support needs
Top ranked composite answer, and with the most rankings of 1st, 2nd and 3rd
Tied for second ranked composite answer
Tied for second ranked
Tied for second ranked
More people put this as their number one issue than any other single issue
Lowest ranked overall, no one ranked it as number one, and only 3 people ranked it as 2nd or 3rd issue
You’ve been heard! We will keep these in mind as we consider educational materials and resources for our community. Thanks to those who participated in our survey.
What do YOU think about these results? Do they line up with your experiences or are they surprising to you?
At the same time, we launched a survey for clinicians. About one hundred clinicians responded. Of these, 67 percent were clinical dietitians; 12 percent were nurses; 9 percent were physicians; 7 percent were pharmacists; and the remaining were “other.”
We asked them, as a clinician/healthcare provider related to nutrition support, to rank the top things that concern them regarding caring for nutrition support patients. Here are the results.
1 Complexities of coordination of care
2 Shortages and supply issues
3 Lack of other healthcare providers in the pipeline to care for complex nutrition support patients
4 Complications related to the therapy
5 Insurance/reimbursement related concerns
6 Complications related to the devices
7 Patient mental/emotional health
8 Patient non-compliance of treatment/therapy plan
9 Not enough quality time with patients
10 Patients not being truthful with themselves or staff and/or ineffective communication to/from patient/family
We also asked them to rank how they thought patients would rank the issues included in the patient/caregiver survey. Here are three issues clinicians thought patients would rank most highly.
1 Shortages and supply issues (not getting what I need, how much I need or a decrease in quality of the products I am receiving)
2 Fighting with the system (such as expenses, home care supplier, school/work, inequality, discrimination, health equity)
3 Attitudes of healthcare professionals. (Not feeling heard/understood by healthcare professionals. Not being a priority for my providers, my needs being put on the back burner until it becomes an emergency.)
Patients had this ranked as 5th
Patients ranked as 2nd
Patients ranked as 6th
Update on CMS, Short Bowel Syndrome and Intestinal Failure
Earlier this year, the Centers for Medicare and Medicaid Services (CMS) announced the inclusion of disease-specific codes for short bowel syndrome (SBS) and intestinal failure (IF) in the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) in the proposed FY 2024 Medicare Inpatient Prospective Payment System proposed rule. We are pleased to share that the Centers for Disease Control and Prevention (CDC), which maintains the ICD-10-CM, has included these codes in the FY 2024 update of the ICD-10-CM. They will be available for use on October 1, 2023.
Why is this important?
The Oley Foundation joined other organizations in encouraging this change. Drs. Mundi, Mercer, and Iyer note
that the lack of such codes “has complicated clinical practice and forced healthcare providers to use a variety of other diagnostic and treatment codes for their patients with CIF [chronic intestinal failure]. [Inclusion of] these codes [will] facilitate management of, and reimbursement for, patients with CIF. The lack of a uniform coding system,” they add, “has not only limited an assessment of the true prevalence of CIF in the United States, it has also hampered analysis of healthcare resource utilization and other characteristics associated with CIF, which would enable the establishment of appropriate regulations and frameworks for its management.” (Characteristics of chronic intestinal failure in the USA based on analysis of claims data, Journal for Parenteral and Enteral Nutrition 2022:1-9) v
COCCI’S Equity in GI 2023
ANDREA TAYLORI am passionate about health equity and was excited to attend the Color of Crohn’s and Chronic Illness (COCCI) Equity in GI conference in Atlanta, Georgia, on behalf of Oley. This year’s theme was “G.R.E.A.M.—Gastro Rules Everything Around Me,” a play on Wu-Tang Clan’s “C.R.E.A.M.” Starting with the “Ode to Hip Hop” opening reception, this was unlike any other conference I had attended. There was music, dancing and an overwhelming sense of community. Patients, care partners, clinicians, other nonprofit organizations and industry professionals all gathered for the same goal: health equity.
Health equity means that everyone, no matter who they are or where they come from, should have the same chance to be healthy and get the care they need. It’s about making sure that everyone has access to the same quality of care and treatment.
This may not come as a surprise, but did you know that certain forms of digestive disease are more common in some racial, ethnic or gender groups? Often, the groups who are more prone to these diseases also face greater barriers to receiving the care they need. One reason is due to disparities (unfair disadvantage) in access to care. Many individuals from marginalized communities (communities that experience discrimination and exclusion) have difficulty getting timely and appropriate care for GI diseases. Factors such as limited or lack of healthcare insurance coverage, lack of transportation, language barriers and cultural differences can contribute to disparities in access to diagnostic tests, treatments and specialist care. Delayed diagnosis, inadequate treatment and
limited access to follow-up care can result in poorer outcomes, increased morbidity, and even higher mortality rates among these populations.
How can we improve this? Advocating for health equity involves increasing awareness and providing accessible and culturally sensitive education about GI disease in underserved communities so the people in these communities are better prepared to actively participate in their own healthcare. Addressing implicit bias (unintentional bias that affects decisions and behaviors) in healthcare workers can help foster a more inclusive and equitable healthcare environment. Achieving health equity requires active involvement from healthcare providers, policymakers, patient advocacy groups and community organizations. The Oley Foundation is committed to playing an active role in achieving health equity.
Founded by Melodie Narain-Blackwell, COCCI’s mission is to improve the quality of life for BIPOC who are affected by irritable bowel disease (IBD), digestive disorders and associated chronic illnesses, through community, research, education and advocacy. In 2024, COCCI will change to COGI, Color of Gastrointestinal Illnesses. COCCI’s membership program is available to IBD patients and care partners at no cost. Check out cocci.org for more information! v
Research Announcement
The following research study has been deemed appropriate for home parenteral/enteral nutrition consumers by the Oley Research Committee; however, the Oley Foundation strongly encourages anyone considering participating in medical research to discuss the issue with their managing physician before signing up.
Clinical Research Study of Injectable Trace Element Supplement
American Regent, Inc. is the sponsor of two clinical research trials studying the injectable trace element supplement product TRALEMENT® (trace elements injection 4*). The Phase IV studies will enroll newly prescribed home parenteral (IV) nutrition patients, comparing TRALEMENT versus a non-manganese containing comparator for longer term safety assessment.
Information on the adult study, including inclusion and
exclusion criteria, is available here: clinicaltrials.gov/ct2/ show/NCT05661682
Information on the pediatric study, for children over 3 years old, is available here: clinicaltrials.gov/ct2/show/ NCT05677126
If interested, please discuss with the healthcare professional managing your home parenteral nutrition. To learn more about the study and find out if you are eligible, please contact Rebekah Sandhu at rebekah.sandhu@ fraserhealth.ca
Health equity means that everyone should have the same chance to be healthy and get the care they need.


Oley 2023: A Mom’s Perspective by Emily Hoopes
I was at paint night with the ladies at my church comparing plans for the summer. “I’m taking my family to the lake,” one said. “I’m going to be stuck doing swimming lessons,” chimed in another. “My husband and I are splurging and going to Hawaii!!” And then they turned to me. I give the odd answers. My son was born with short bowel syndrome and had an intestinal transplant. So usually, I listen and nod. When I do answer, it doesn’t usually match what everyone else is saying.
We splurged this summer. I cashed in my frequent flyer miles. My husband took the week off work to stay home with our children. I’m going on my first solo trip in five years! “I’m going to a medical conference in St. Louis,” I say. “About tube feeding.”
Why? That’s the thing people want to know. Why would I take this “me trip” and go to a medical conference?
LEARNING
Part of it is education. When you live with a rare medical condition, you don’t count on your doctors to know the latest research or your homecare company to offer you the hot new products. Especially not when you live somewhere with as many wide-open spaces as Utah. You have to be the expert. You have to go get that information yourself. When it comes to PN,* enteral feeding,** and nutrition support, the place to get that information is the Oley Foundation, and there is no place better than the Oley annual conference. I am as invested in my own continuing education as any nurse or doctor caring for my son. So I soak up opportunities to learn, and this conference is at the top of my list.
It’s exhilarating to get to listen and ask questions of expert clinicians in a presentation. It’s thrilling to walk through a vendor hall and hold a product in your hand that solves a problem you’ve battled for years. It’s exciting to have emerging research presented to us as patients in a forum where we are treated as equals. In most contexts, patients are talked about, explained to. At the Oley conference, patients have an equal voice. In fact, often we’re the ones teaching them.
I love the opportunities for learning at this conference. But it goes deeper than that. At this one conference and in this one place, I can be my whole self.
At paint night and everywhere else, I’m always reading the room, keeping my cards close to my chest. I know my situation is too much. If I talk too openly about our lives, I step into taboo territory. My paint night friends might feel bad for me, might worry, might cry, might be grossed out, might not understand. So I don’t. I hold back.
Even if I’m not concerned about taboos and feelings, I want to talk about nutrition support in a way few others do. I have studied this topic and care about it deeply. It is rare to find others who feel passion about blended feeds or the price of
ethanol locks or vascular access choices or syringe brands or how long you should scrub a hub with alcohol. Except, of course, at the Oley conference
Nutrition support consumes most of my time and energy. I spend hours a day on this one thing. I fight for it. Learn about it. Study it. Except in medical settings, I mostly have to keep it to myself.
BELONGING
At the Oley conference, we are virtually strangers. Still, the first time you sit down to eat with someone and find yourself discussing ports vs. Broviac lines, you suddenly feel like you’ve come home.
I say strangers, but that’s not entirely true. Many of us moms have turned to Facebook, trying to fill the gaps of knowledge and care in the healthcare system. We know each other by name and profile picture, even though we’ve never met. Finding each other in real life is half celebrity sighting, half reunion with a long-lost friend. We belong to each other. So things moved quickly from “let’s take a selfie together” to “of course you have to sing karaoke with us.”
It’s different from relationships with other mom friends. In all my years as a mother, on playdates and in the pickup line, I’ve just sat back and smiled and nodded while the other moms talk—about feeding and potty training and the first day of school. I’ve smiled, but held back. Known in my heart we weren’t quite the same. Those things are different for me. I’m the mom who calls ahead when there’s a birthday party to talk about the menu. I send an alternative treat for when they’re serving cake. I’m the mom who Saran Wraps my child before water games at field day. I’m the mom who doesn’t flinch at her own kid’s vomit or diarrhea but freaks OUT if your kid has a runny nose. Different. Explaining why there are tubes. Explaining why we can’t come. Explaining. Excusing. Apologizing.
So there is something remarkably comforting in being with moms where there are no explanations, excuses or apologies needed. Where you just are. Where all someone has to say is, “It’s time to go hook up TPN. I’ll be right back,” or “Hang on, we’re gonna do a bolus real quick,” and everyone just knows what you mean.
You can finally just be yourself. You can finally have a conversation on equal footing. You have conversations that matter. That’s magic.
I had lunch with a young woman who grew up on TPN and a
CONTINUED, NEXT PAGE
"For one whole week, I was able to be my whole self."
Oley 2023: Feeling the Love by Jaden Maynard
Oley 2023 in St. Louis was the first time Oley Ambassador Jaden Maynard attended an Oley conference. He shared these thoughts with us some weeks later.



I have really been trying to find a way to put into words the way that Oley has completely changed my life. The way that I am responding to a progressive medical condition has been so drastically different than I would have responded just a year ago. I have hope for the future and am not super worried about quality of life, connection, community, or so many other things because of Oley! I feel for the first time that I will be accepted no matter how clinically sick or well I am. I feel like I have friends and support, and can curate a life that I am so excited to be a part of; rather than being a part of the life that being on nutrition support dictates for me.
I am formulating and processing every day about the ways my life is medically changing. I am feeling overwhelmed knowing I am likely going to progress in needs for nutrition support rather than wean off of them. Ultimately, I know that wherever Iʼm at, I am cared for, loved, and accepted by my Oley family. Thank you so much for your continued support and opportunity to be a part of this amazing organization!
Oley 2023: Emily Hoopes, continued from previous page
mom of a toddler. I have a teenager at home. The three of us talked about what it’s like to be a teen on nutrition support. We talked about how parents can help. That’s magic.
I ran around with my son on a video call during every break for a whole day so he could “see all the people like him,” and people just smiled and said hi and showed him their tubes. That’s magic.
I sat up until 1 a.m. with other moms talking. We are stickto-the-schedule, go-to-bed-early, stay-focused-becausemistakes-kill moms, but we stayed up late talking. Talking about feeding, and school, and inclusion. We talked about being scared. We talked about not knowing how to explain things to our kids that we don’t really know how to cope with ourselves. We laughed a little irreverently about the things we cope with. We compared notes. We commiserated. Moms from all over the country with kids of all different ages, different diagnoses, different experiences. But all with this one big thing in common. Our lives all revolve around nutrition support for our kids.
For once, we didn’t have to filter what we said or explain who we were. And that’s magic.
When it was time to go home, I stayed till the last moment I could without missing my flight.
I was tired from staying up all night and sore from dancing like I was a young mom instead of an old one. I had a notebook full of things I’d learned and new ideas. My head was full. So was my heart.
My life revolves around nutrition support. However, it often feels like something I keep to myself and handle alone.
I won’t be able to explain it to my paint night friends. They can’t understand. A medical conference doesn’t sound like a self-care getaway. But my Oley friends know what I mean. At Oley, you don’t have to filter, explain, or apologize. You learn, you connect, you celebrate. Oley is my Comic Con. An oasis.
For one whole week, I was able to be my whole self.
Totally worth the sky miles. v
*PN = parenteral (IV) nutrition
**enteral nutrition = tube feeding
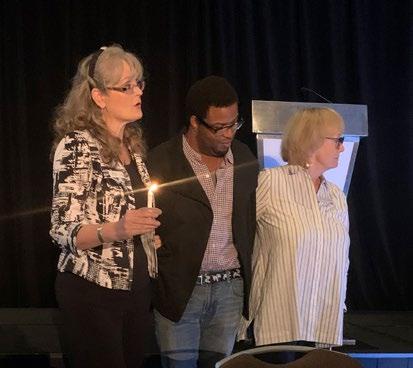
Oley 2023: Joan Bishop Honored with Lifetime Achievement Award


Joan Bishop, Oley Foundation Executive Director Emeritus, officially retired at the beginning of June 2023, after nearly forty years of serving the Oley Foundation and the home nutrition support community. Her contributions were acknowledged at Oley’s 2023 annual conference as Joan received a Lifetime Achievement Award that was both named for her and presented to her as the first recipient.
Joan has been working for Oley since 1985 and was at the helm as Executive Director for over twenty years. Her fierce dedication to the mission and members of Oley is unsurpassed. She has weathered many ups and downs as the captain of this ship and has always had Oley’s best interest at heart. To many, she has been “the help along the way.”
The newly established Joan Bishop Lifetime Achievement Award will be given annually by the Oley Foundation to a person who has dedicated their time, talent and passion to advancing the field of home nutrition support therapy across the decades. This is the only award decided by the Oley Board of Trustees and given to a person who has gone above and beyond in their years of selfless dedication to working towards advancing the mission of the Oley Foundation.
Congratulations, Joan! We wish you the very best in retirement. You will be missed!
Oley 2023: Being Part of a Community by Sarah Ellis
Maisie and I loved our first Oley conference! A couple months later, I can see how big of an impact the community made on both of us. Of course I loved the time with other moms—it is the very best support out there. And this was one of the first times I also got to meet and talk with older kids and young adults on nutrition support. Hearing what's important to them and seeing how they thrive is amazing and helps me see what might be ahead on our journey.
Maisie would tell you her favorite part was playing with her friends! Never has she ever before stayed up late watching movies and playing hide and seek in a hotel lobby—she was living her best life. And as her mom, I
once again saw there are really no limits to what she and we can do—we can hook up parenteral nutrition (PN) in the hotel lobby and not miss a moment.
I can also hear a difference in how Maisie talks about things, with a little more awareness and confidence in her voice. On the plane home from St. Louis, she made a friend with someone sitting in the row in front of us. Her new friend asked if she'd been on vacation in St. Louis. Maisie said, "No, I was at a PN conference! My friends have a line like me!" I am so grateful for the community and the connections and support we both experienced at Oley. Looking forward to next year!
Oley 2023: Walk and Roll-a-thon raised $4,495

Thank you to all of the walkers, both in St. Louis and remotely, for support. Their efforts raised funds for and awareness of the Oley Foundation. Together, the walkers raised $4,495, as of early autumn, when we went to press with this issue.




OLEY 2023 WALK AND ROLL-A-THON PARTICIPANTS
Jack Alexander; anonymous; Jim and Jackie Bain; Kelly Baker; Stephanie Baker; John Cody Bakkila; Joan Bishop; Anthony Bishop; Bettemarie, Ashleigh and Kyleigh Bond; Joy Boyd-Rodriguez; Allie Broaddus; Anna Cooper; Janice Cooper; Maisy Cyr; Debbie Dean; Tiffany Dodd; Sarah Ellis; Todd Friedman; Erica George; Tracey Giambertone; Joy and Colman Gulden; Lyn Howard; Nick Jackson; M. Crystal Killian; Clarissa LaMora; Team Lincoln; Gaby Luna; Al and Annette Mackay; Katie Marschilok; Jaden Maynard; Melissa McCausland; Eoin McCausland; Alaina McCormick; Michael Medwar; Lisa and Ron Metzger; Maddie, Mark and Tammy Morris; Cindy Nichols; Tesia Nichols; Jackie Pellitier; Katie and Robert Peters; Javier Ramirez; Cynthia and Layne Reddick; Jayme, David and Olivia Scali; Adam Singer; Mary, Bob, Catherine and Noah Smithers; Mollie Squires; Andrea Taylor; Cathy Tokarz; Pam and Ally Winter
"The Oley Conference was AWESOME and filled with many exciting DISCOVERIES. Discovery of new information, finding out products and services I didn't know existed, and most importantly relationships with people who understand."
— Janice Cooper, first-time attendee, “alongsider”
Oley 2023: Oley Recognizes Award Winners

The Oley Awards Program recognizes home parenteral and enteral nutrition (HPEN) consumers, caregivers and clinicians who exhibit courage and perseverance in overcoming the adversities of illness and are generous in helping others. The stories clinicians, family members, peers, caregivers and patients relay in the nominations are truly inspiring. It is a difficult job to select just one winner for each award from the outstanding pool of nominees! We congratulate everyone who was nominated for an Oley award.
Please consider nominating someone who inspires YOU. There are so many worthy candidates! Nomination forms will be available January through April at oley.org/nominations or by calling (518) 262-5079.
We hope you enjoy reading about this year’s winners. Awards were presented at the Oley 2023 annual conference in St. Louis, Missouri.
Sponsored by Nutrishare, this award recognizes a consumer on home parenteral nutrition or caregiver, 19 years old or older, who demonstrates courage, perseverance, and a positive attitude in dealing with their illness and living a more fulfilling life on HPN.
Garrett Taira was born in Shady Grove, Maryland, with chronic intestinal pseudoobstruction, a rare medical condition that requires daily parenteral (IV) nutrition. He has had multiple hospitalizations and surgeries throughout his life.
In spite of all the medical hardships, Garrett is a visionary leader with a positive attitude. Garrett constantly overcomes life obstacles and exceeds ordinary expectations. Garrett is known as an actor and dancer. His videos have been shown on The Ellen Show and The Rock’s Instagram, and he was a featured speaker at TEDx Bethesda.

Currently Garrett is making comedic and inspirational medical life content while going through a kidney and bowel transplant.
Congratulations to our nominees: Ann Anderson; Amie Rhodes; Charles Songer; Diane Wakashige
Distinguished Clinician Award
This award, sponsored by Baxter, recognizes a healthcare professional practicing in the field of home IV nutrition, tube feeding or a related field, who sets an example by promoting innovation in nutrition therapy, or by advocating for someone in their care, and demonstrates a willingness to give of themselves, to educate, empower, and improve the quality of life for home IV nutrition and/or tube feeding consumers.
Christina Ritchey is a clinical program manager for Optum Infusion Pharmacy’s nutrition team. She is a registered dietitian (RD) and certified nutrition support clinician (CNSC) and has worked in the home infusion industry since 2009. Christina has a Bachelor of Science in Biomedical Science from Texas A&M University and a Master of Science in Nutrition from the University of the Incarnate Word.
Christina has authored numerous abstracts and publications related to nutrition support, outcomes, patient support, health equity and literacy. She is the recipient of the 2021 National Home Infusion Foundation Outstanding Abstract Award; 2022 American Society for Parenteral and Enteral Nutrition (ASPEN) Home Parenteral and Enteral Nutrition Trailblazer Award: and 2023 ASPEN Fellow Class. Christina is an active member of ASPEN. She serves as cochair of the Home and Alternate Site Section and on the Membership Committee. She is

CONTINUED, NEXT PAGE
Sponsored by VectivBio, this award recognizes a caregiver/supporter to a consumer on home IV nutrition or tube feeding, of any age, who demonstrates patience, compassion, and dependability, and provides effective care in helping a consumer live more fully on home nutrition support.
Jayme Scali is a nutrition patient liaison for Optum Infusion Pharmacy, with over fifteen years of personal and professional experience supporting patients and families who are managing complexities associated with home parenteral (IV) nutrition support. Jayme is a parent to three children. The oldest, Olivia, has been on parenteral nutrition and enteral support long term. As both a parent and a patient liaison, Jayme can support others and help them achieve a higher quality of life, despite the challenges of nutrition support therapy.
Jayme is also a member of the Nemours Children’s Health System Family Advisory Board, Nemours CLABSI Taskforce Board, Pennsylvania Medicaid Parent SubCommittee, and Pennsylvania Medicaid MCO Shift-Nursing Work Group. She passionately supports the home parenteral nutrition community by sharing resources and education via social media and helping with the Nutrition Group-4-All support group, among many other advocacy and legislative projects.
Congratulations to our nominees: Anika
CONTINUED, NEXT PAGE
Damian Herrera Rising Star Award
Sponsored by Abbott, this award recognizes a consumer on home IV nutrition or tube feeding, 18 years old or younger, who shows a positive attitude in adapting to life on therapy which encourages and inspires others.
Damian Herrera was born in Pennsylvania at thirty-five weeks with vanishing gastroschisis. He was diagnosed with short bowel syndrome when he was three weeks old. He has been on parenteral (IV) nutrition since birth and has learned to navigate life with it. Damian also has a G-tube and receives enteral nutrition. His family relocated to Massachusetts for medical care when he was only four months old.

Damian is known for being a high-energy leader and the joy of the classroom. He loves playing with action figures every day. His parents note that he loves music and “has some good moves.” They continue, “He is an incredible big brother, a son who always makes us laugh, and a miracle. Damian’s positive attitude towards life is contagious and he makes anywhere he is at a happier place for all. Damian is caring and kind and is a friend to all.”
In spring of 2023, Damian graduated from kindergarten and in the fall was on his way to first grade. “Damian is only 6.5 years old,” they add, “but he is an advocate, a volunteer, an international traveler, a purple belt in karate, an athlete that plays soccer, basketball and t-ball, and swims and loves to ride his scooter in his spare time.”
Damian attended and shared his story at Rare Disease Week in DC in 2023, then presented to his kindergarten class about it. In pre-k, he read My Special Line with his tubie bear to his class to spread awareness. He has attended and helped put on six gastroschisis awareness events. Damian is an international traveler who has traveled to Italy and France, New York City and Niagara Falls in New York, Pennsylvania, New Jersey, New Hampshire, Connecticut, Rhode Island, California, Washington DC, North Carolina, Virginia and Florida. He loves meeting new friends.
Congratulations to our nominee: Albert Otero
David Rowland Unsung HEN Hero Award
Sponsored by Nestlé Health Science, this award recognizes a consumer on home tube feeding (enteral nutrition or HEN) or caregiver, 19 years old or older, who demonstrates courage, perseverance, and a positive attitude in dealing with their illness and living a more fulfilling life on HEN.
July 26, 2023, marks eleven years that David has been on tube feeding. He writes, “I am thankful my feeding tube has worked so well for me. I enjoy each day of life to the fullest. I am 83 years old and very active. I am a widower, having lost my wife in 2022. She was a wonderful lady and a strong supporter and encourager with my tube feeding things.”

David’s health issues began with throat cancer in 1997. He had a major surgery and thirty-seven radiation treatments. Radiation damage, he writes, “played a part in my having to go on a feeding tube fifteen years later. The first year or so with a feeding tube was quite a learning experience. I knew nothing about tube feeding and didn’t garner a lot of information from the medical community. I was blest to find the Oley Foundation within a few weeks and discovered there were lots of people on feeding tubes and that there was so much great information on Oley’s site. I am very thankful for Oley!”
He continues, “It is a blessing and joy to help others and share information and various methods of tube feeding. I am active on Inspire (Oley) and tube feeding Facebook pages where I endeavor to provide helpful information. Many times, I video chat with tubies so they can see a picture of different methods of tube feeding. I share my experiences, encouragement, product knowledge, etc. I also help tubies in need of formula find it and sometimes I drive and pick formula up for them.
“It has been enjoyable to be in touch with so many tube feeders. My life has been so enriched by each of them. I have made so many new friends over the years. I am inspired by so many tube feeders, especially the children. I admire how they press on in spite of their circumstances.”
Congratulations to our nominees: Bethany D’Amico; Ron Patun; Diane Wakashige
Jayme Scali, continued from previous page also currently president of the Texas Alamo Society of Parenteral and Enteral Nutrition (TASPEN) and is a member of the National Home Infusion Association Clinical Practice Committee.
Christina Ritchey, continued from previous page
Congratulations to our nominees: American Society for Parenteral and Enteral Nutrition (ASPEN) and its Public Policy Committee; June Greaves, RD, CNSC, LD, LDN, LRD; Karen Sexton Hamilton, MS, RD, LD, CNSC; Lisa Miller, MD; Lauren Schwartz, MD; Tiffani J. Tobe















Thank You to All Who Contributed to Oley 2023
Our heartfelt thanks to the many who contributed to make the Oley 2023 conference a success. To volunteers who helped at the registration desk, in Kidz Klub, and all around; to the faculty who prepared and presented information without compensation; to the exhibitors who made the
exhibit hall such a fun place to be; to the corporate and individual sponsors who helped make the meeting possible; and to all the attendees who opened their hearts and arms to each other—a huge thank you.
CONTRIBUTORS (sponsorships, speaker support, donations, etc. that help offset conference costs)
Abbott Nutrition; Amerita Specialty Infusion; Amsino; Avanos; Aveanna; B. Braun Medical, Inc.; Baxter; Jarol Boan, MD; Frona Brown; Brown University School of Medicine, Providence, Rhode Island; Cardinal Health, Inc.; Care + Wear; CHOC Children’s Hospital, Orange, California; Color of Crohn’s and Chronic Illness; Columbia University Medical Center, New York, New York; Coram/CVS specialty infusion services; GBUK Enteral; Gus Gear; L&B Worldwide; Kate Farms; MagicWig Productions; Massachusetts General Hospital, Boston, Massachusetts; Mayo Clinic, Rochester, Minnesota; Moog; Nestlé Health Science; New Directions Counseling Services; Nutrishare; Optum Infusion Pharmacy; Real Food Blends; Saint Luke’s East Hospital, Lee’s Summit, Missouri; SBS Cures; Soleo Health; St. Paul’s Hospital, Providence Health Care, Vancouver, BC, Canada; Staley House, LLC, creator of the FreeArm; Takeda Pharmaceuticals; University of Nebraska Medical Center, Omaha, Nebraska; University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; VectivBio; the Witt family; Zealand

EXHIBITORS (exhibit fees help offset conference costs)
4U Medical Designs; Abbott; Actuated Medical; Alcresta Therapeutics; Amerita; Amsino; Avanos; Aveanna; B Braun; Baxter; Ben Guard Healthcare Solutions LLC; Cambrooke; Cardinal Health; Coram/CVS specialty infusion services; Covalon Technologies; ENClean; ēzalife; FreeArm Tube Feeding Assistant; Fresenius Kabi USA; Functional Formularies; GBUK Enteral; GEDSA; Kate Farms; Luminoah; Moog Medical; Nestlé Health Science; Nutrishare; Option Care; Optum; Real Food
Blends; Resilience Medical; Rockfield Medical; Soleo Health; Takeda; Vesco; Whole Story Meals
FACULTY (donate their time and expertise)
Steve Atkinson; Kelly Baker; Kevin Baskin, MD; Aly Becker, MA, LMHC, NCC; Katherine Bennett, RD, MPH, CLE; Joan Bishop; Bettemarie Bond; Luccas Borges; Amy Braglia-Tarpey, MS, RD, CNSC; Anne Brettschneider, RD; Rebecca Brown, RDN, CNSC; Valeria Cohran, MD; Amy Cole; Carolyn Crumley, DNP, RN, ACNS-BC,CWOCN; Maisy Cyr; Hassan Dashti, PhD, RD; Vicki Emch, MS, RD; Lisa Epp, RDN, LD, CNSC, FASPEN; Roy George; Tracey Giambertone, MS, RDN, LDN, CNSC; Beth Gore, PhD, MBA; Jamie Haselhorst, RDN, LDN, CNSC; Jocelyn Hill, MN, RN, OCN, CVAA(c), VA-BC; Lyn Howard, MD; Shirley Huang, MD; Maria Karimbakas, RD, CNSC; Crystal Killian; Sivan Kinberg, MD; Cara Larimer, RD, CNSC; Gaby Luna; Beth Lyman, RN, MSN, CNSC; Al Mackay; Katie Marschilok; Alaina McCormick; David Mercer, MD; Lisa Metzger; Reid Nishikawa, PharmD, FASPN, FCSHP; Jessica Pitt, PharmD, MBA; Chaitnya Razdan; Cynthia Reddick, RD, CNSC; Lauren Reimer; Jayme Scali; Andrea Taylor, RD; Kelly Tappenden, PhD, RD; Marion Winkler, PhD, RD, LDN, CNSC; Jodi Wolff, MS, RD, LD, FAND, FAACPDM; Ryan Yoo


VOLUNTEERS (give their time and talents)
Julie Andolina; Rhonda Arends; John Bacon; Ashleigh Bond; Betty Bond, RN; Anthony Butler; Kim Butler; Tiffany Dodd; Jeff Hoelle; Emily Hoopes; Nicholas Jackson; Cara Larimer, RD; Katie Marschilok, RN; Ron Metzger; Jackie Pellitier, RN; Ben Peterson; Javier Ramirez; Laney Reddick; Olivia Scali; Cathy Tokarz; Natalie Wootten
Developed the FIRST and ONLY fish oil lipid injectable emulsion (ILE) for pediatric patients with parenteral nutrition-associated cholestasis (PNAC)



Developed the FIRST and ONLY 4-oil ILE for patients of every age and stage www.FreseniusKabiNutrition.com

Developed the FIRST and ONLY three-chamber bag for adult parenteral nutrition in the U.S.


HPN Awareness Week: October 9-13

For many Oley members, home parenteral nutrition (HPN) is part of life. But many people don't know what parenteral nutrition is, why it is used long term, how it helps, and what struggles and challenges it brings.
HPN Awareness Week is meant to bring some light to these things. It is a chance for HPN consumers and caregivers to share their stories; to build bridges to HPN consumers and caregivers who are not yet connected to a community; to provide hope to others; and an opportunity to talk about the challenges.
Watch oley.org and our social media pages to see how you can participate!
Oley Glossary Continues to Grow
In August, in honor of Gastroparesis Awareness Month, we added several words related to gastrointestinal motility to the Oley glossary. Here is a sampling. We hope you find the glossary a good resource. Please visit oley.org/ ResourcesGlossary often! Your feedback on it is always welcome.
breath test (breth test): a simple, noninvasive test used to measure gases in the breath you exhale. See hydrogen breath test for one type that is used to help diagnose gastrointestinal conditions. Another type of breath test can be used to measure gastric emptying. Also, breath tests can be used for other indications, such as to check for the infection with helicobacter pylori, that can cause ulcers.
chronic idiopathic constipation (KRON-ik ID-ee-oh-PATH-ik KON-stih-PAY-shuhn): an inability to have bowel movements on a routine basis for unknown reasons. It is also known as CIC.
chronic intestinal pseudo-obstruction (KRON-ik IN-tessTIN-uhl SOO-doh-ub-STRUK-shuhn): a condition in which symptoms of intestinal blockage are present without any physical blockage. After a while, the intestines are unable to contract enough to push food, stool, and air through the gastrointestinal tract. It is due to underlying neuro-muscular dysfunction of the GI tract.
delayed gastric emptying (dee-LAYD GAS-trik emp-tee-ing): see gastroparesis
dysmotility: see motility disorder
functional gastrointestinal disorders (FUHNK-shuhn-uhl GASS-troh-in-TESS-tin-uhl diss-OR-durz): in the past, this term was used to describe disorders that are not well understood.
gastric emptying scintigraphy (GASS-trik EMP-tee-ing sinTIG-ruh-fee): a test that involves eating a bland meal, such as eggs or an egg substitute, that contains a small amount of radioactive material. An external camera scans the abdomen to show where the radioactive material is located. A radiologist is then able to measure the rate of gastric emptying at different time periods after the meal. Doctors can use this test to diagnose gastroparesis. Also called a
gastric emptying scan.
gastroparesis (GASS-troh-puh-REE-siss): a disorder that slows or stops the movement of food from the stomach to the small intestine. With gastroparesis, the stomach muscles work poorly or not at all, and the stomach takes too long to empty its contents. The delay in digestion can lead to various symptoms and complications, including bloating, nausea, and vomiting. Gastroparesis can occur when illness or injury damages the vagus nerve and the stomach muscles stop working normally. Gastroparesis may be referred to as a motility disorder. Also called delayed gastric emptying.
Hirschsprung disease (HURSH-spruhng dih-ZEEZ): a birth defect in which some nerve cells are missing in the large intestine, causing the intestine not to move stool and become blocked. The blockage can cause severe constipation or intestinal obstruction. People are born with Hirschsprung disease and are usually diagnosed as infants. Hirschsprung disease is a type of megacolon.
hydrogen breath test (HY-droh-jen breth test): a simple, noninvasive test used to diagnose gastrointestinal conditions, including lactose intolerance and small intestine bacterial overgrowth (SIBO). It helps evaluate your digestion of certain sugars by measuring the gas in the breath you exhale. There are different kinds of hydrogen tests, used to measure the digestion of different sugars. See breath test
megacolon (MEH-guh-KOH-lon): severe swelling of the colon or rectum, or both, with constipation or intestinal obstruction. Megacolon can result from one of several conditions, such as Hirschsprung disease
microvillus inclusion disease (my-kroh-VIL-uhss in-KLOOzhuhn dih-ZEEZ): a life-threatening condition characterized by severe diarrhea beginning the first few days after birth.
mitochondria (MY-toh-KON-dree-uh): a part of all cells, except for red blood cells, that convert energy from food into a form of energy that the body uses to function properly.
mitochondrial disease (MY-toh-KON-dree-uhl dih-ZEEZ): a result of mitochondrial failure, resulting in little energy
CONTINUED, PAGE 21
YOU’RE



FreeArm Emerging Innovator Partnership

One of the priorities outlined in our 2023–25 Strategic Initiatives is to support the patient-centered evolution of nutrition therapy to improve care and enable patients to live their best life possible. Toward that goal, earlier this year, Oley launched a new partnership level: Emerging Innovator.
It is with great honor that we announce FreeArm as Oley’s very first Emerging Innovator partner. By combining our collective expertise and resources, we plan to support future innovations, as well as expand our support for pediatric enteral consumers and caregivers. If you don’t already, be sure to follow FreeArm on LinkedIn, Instagram and Facebook to stay up to date on their news, giveaways and “Super Cutie Alerts”!

FreeArm
The FreeArm holds gravity feeds, pump feeds and infusions at the hospital, home and on-the-go. It attaches to flat and rounded surfaces and bends up easily to fit in your bag, making eating on the run a breeze. The FreeArm is billable for insurance coverage and available through many DMES.
Thank You Corporate Partners!
Please join Oley in thanking the companies that provide unrestricted grants to support the foundation year-round. Learn about our most recent corporate contributors in their own words below. For a complete list of corporate partners, go to oley.org/ PartnerShowcase.
Zealand Pharma A/S
Zealand is a biotechnology company focused on the discovery and development of peptide-based medicines. More than ten drug candidates invented by Zealand have advanced into clinical development, of which two have reached the market and three are in late-stage development. The company has development partnerships with a number of blue-chip pharma companies as well as commercial partnerships for its marketed products. Founded in 1998 and headquartered in Copenhagen, Denmark, with a presence in the U.S., Zealand’s focus is in the areas of metabolic and gastrointestinal disorders, including SBS.
Oley Glossary Continues to Grow,
made within the cell. It can lead to cell injury, cell death, and failure of whole body systems. The disease is most common in children, but adult-onset mitochondrial disease is starting to become more common.
motility (moh-TIL-ih-tee): the movement of food through the gastrointestinal tract.
motility disorder (moh-TIL-ih-tee diss-OR-duhr): any of several conditions affecting the gastrointestinal (GI) tract that are caused by abnormal muscle contractions. Achalasia, gastroparesis, and Hirschsprung disease are some examples of motility disorders.
continued from page 19
postvagotomy stasis (POST-vay-GOT-uh-mee STAY-siss): disordered stomach and other upper GI motility emptying that can occur after surgery affecting the vagus nerve.
vagotomy (vay-GOT-uh-mee): surgery to cut the vagus nerve. This procedure causes the stomach to produce less acid. It can also cause the stomach to empty abnormally (see postvagotomy stasis).
vagus nerve (VAY-guhss nurv): the nerve in the stomach that controls production of stomach acid and stomach emptying.
• Nutrition, nursing and pharmacy expertise

▸ Keep up with the latest research and evidence-based practices in nutrition support
▸ Join live presentations, discussions, and chat rooms
▸ Ask questions, connect with experts and peers
▸ See product innovations
Notable Individual Contributions
Among the contributions we receive, there are always several dedicated to those who have inspired the donor. We share this list of honorees below. We are grateful for the following gifts received from May 14 to August 15, 2023.
Memorials: In memory of Ronald Adelson; Pat Anthony; Kathryn Bundy’s brother; a former Oley Ambassador; Donald Guzzetta; Bertram Jaffe; Elizabeth Kellerman; Dr. Darlene Kelly; David McGee; Peter Joseph Michalski; Joseph A. Reale; Stephanie Salerno; Steven H. Vogler

Tributes: In honor of Joan Bishop; Dr. Lyn Howard; the birth of Hanna Aviva Jacobson; Aidan Koncius; Jeff Nemeth
Fundraisers: Amazon Smile; and Facebook fundraiser campaigns for the birthdays of Betty Bond, Leighanne Boone, Erin Castellano, Jennifer Ephraim, and Malik Saunders
Thank you for all gifts and the kind comments we receive throughout the year. Your support overwhelms us and continues to be a source of inspiration.
OLEY CORPORATE PARTNERS

















2023 Oley Calendar
Please check oley.org or other appropriate websites for the most up-to-date information on the events listed below.
Ongoing: Applications being accepted for Oley Tim Weaver Camp Scholarship.
Oley Ambassador Virtual Support Groups

Last Sunday of every month: Teens HPEN (ages 13–17) support group meeting, hosted by Kelly Baker
Second Wednesday of every month: Young adult HPEN (ages 18–35) support group, hosted by Darla Burr
First Thursday of every month: Nutrition Group 4 All Feeding Tube/TPN Support Group, hosted by Crystal Killian
Second Thursday of every month: Tube Feeding/TPN Support Group for Patients and Caregivers, hosted by Barbara Rudzin
Fourth Thursday of every month: TPN Support Group for Consumers and Caregivers, hosted by Amber Gates
October 9–13: HPN Awareness Week
*For more information on support groups and Kidz Klub meetings, go to oley.org/SupportGroups; for other meetings, email harrinc@amc.edu or call (518) 262-5079.
Additional Meetings of Interest:
October 15–17: National Organization for Rare Disorders (NORD) Rare Diseases and Orphan Products Breakthrough Summit, Washington, DC
Mark Your Calendars
Oley’s mini meetings and webinars offer a variety of opportunities to learn and engage with other members virtually. Oley webinars cover a singular topic in one to two hours, often featuring an expert clinician. Mini meetings are three to four hours, and cover several topics. They may include educational topics, consumer stories, sponsor-coordinated sessions, and interactive breakouts or Q&A sessions.
Webinars and mini meetings are coordinated for home nutrition support consumers and family members/caregivers, but everyone is encouraged to attend and learn!
November 17, 6:00 p.m. ET: Food for Thought: Navigating the Holiday Season on Nutrition Support An open forum to share experiences and challenges, ask questions, and find support and community during what can be a challenging time of year for folks on nutrition support. More details to come.
Stay tuned for a November webinar! More details to come. Visit oley.org/Enrichmentprograms for upcoming events. Visit oley.org/oleyminimeetings and oley.org/webinars for recordings.
Our mailing address is now: The Oley Foundation, Albany Medical Center, MC-28, 43 New Scotland Avenue, Albany, NY 12208. Our physical address is: 66 Hackett Boulevard, Albany 12209 WE’VE

