8 minute read
Medical Line Entanglement: Are You Aware?
by Cara Larimer, RD; Vanessa Sumner, MBA, MSN, RN; Diane Wander, RN, BA
Note: The following article is based on “Medical line entanglement: The unspoken patient safety hazard of medical devices,” by C. Larimer, V. Sumner, and D. Wander, published in Nutrition in Clinical Practice in 2023. We asked the authors to share their research in the Oley Foundation newsletter so our readers will be aware of this potential hazard and can take steps to minimize risks.
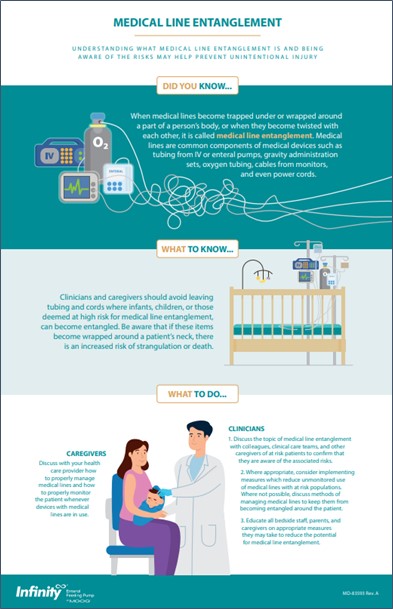
To help assist in the awareness and education about medical line entanglement (MLE), Moog Medical put together a simple infographic that can be found at moogmedical.com/understandingmedical-line-entanglement. It was designed to help readers understand what MLE is and what the potential risk is. The infographic also presents several ideas designed to encourage further discussion on medical line entanglement between caregivers and clinicians.
The use of a medical device in the home can be a complicated and challenging experience, especially when the device is used on children. In February of 2022, the US Food and Drug Administration (FDA) published a safety communication called “Potential Risk of Strangulation in Children Who Use Enteral Feeding Delivery Sets.” The publication reports the death of two toddlers as a result of medical line entanglement (MLE) and advises “feeding set tubing can become wrapped around a child's neck and cause strangulation or death.”
The risk of strangulation is not specific to enteral feeding delivery sets, however. Most medical devices have some type of cord or tubing connected to them, such as administration sets used with IV pumps, feeding sets used with enteral pumps, oxygen tubing, cables for monitoring equipment, and even power cords. When any of these cords or tubing become trapped under a person, wrapped around a body part, or when they become twisted together, it is called medical line entanglement.
Medical line entanglement can cause strangulation, as noted by the FDA, but it can also cause ligature injuries, impaired circulation, falls, and device dislodgment. It can also lead to medication errors, caused by the misidentification of lines, as noted by Goodin et al. in a 2012 article on the topic in the Journal of Pediatric Nursing. These risks can be higher with certain patient populations, including patients with limited mobility or cognitive or developmental impairment, and with children.
SURVEY SHOWS A NEED FOR AWARENESS
The authors conducted a survey to evaluate the level of awareness of MLE and to determine if caregivers receive MLE education when being discharged home with a medical device. Three groups were identified as the target audience of the anonymous online survey:
• pediatric acute care clinicians
• clinicians from outpatient pediatric GI clinics
• caregivers of patients with a medical line
With the help of organizations like the Oley Foundation, the survey was published and distributed, and the data was collected. Table 1 (below) highlights several key findings of this study. The full results were published in the American Society for Parenteral and Enteral Nutrition (ASPEN) journal Nutrition in Clinical Practice (aspenjournals.onlinelibrary. wiley.com/doi/epdf/10.1002/ncp.11000).
*****
TABLE 1. KEY FINDINGS
PARENTS/CAREGIVERS OF PATIENTS WITH A MEDICAL LINE
Caregivers who participated in the survey were asked what type of nutritional support the patient was receiving.
• 67% of patients were receiving tube feeding
• 16% of patients were receiving parenteral nutrition (PN)
• 13% of patients were receiving both tube feeding and PN
• 4% of patients were not receiving either
The survey asked caregivers if they had received education about MLE when first receiving the medical device. Only 11 (9%) of 116 respondents reported that they had received information about the risk of MLE.
CLINICIANS FROM PEDIATRIC ACUTE CARE FACILITIES (N=34)
30 (88%) of the acute care clinicians surveyed responded that they are aware of the risks of MLE while only 1 (3%) reported that their facility has a policy or procedure in place to address MLE.
CLINICIANS FROM OUTPATIENT PEDIATRIC GI CLINICS (N=40)
32 (80%) of the clinicians from outpatient pediatric GI clinics surveyed responded that they are aware of the risks of MLE while only 3 (8%) reported that their clinic has a policy or procedure in place to address MLE.
*****
At the end of the survey, participants were asked if they wanted to share and explain any additional medical line entanglement–related comments they felt were important (see table 2, below). It is important to caution caregivers that one cannot fully mitigate the risk of medical line entanglement, even with the tips and tricks noted in the comments. These only help to lower the risk, not to eliminate it.*
*****
TABLE 2. SAMPLING OF CAREGIVER FEEDBACK
Participants were asked to share and explain any additional medical line entanglement related comments that they felt may be important:
• We now tape her two TPN lines together, so there is a reduced risk of entanglement.
• We used to place the IV pole with his feeding tube toward the head of the bed, like in the hospital. At least three times, the line wrapped around his neck regardless of all precautions we thought would help. We then moved the IV pole holding his pump to his feet. Once we did that, he only had the occasional lower body entanglement. It is more than unnerving to see the line anywhere near a child’s head. Proper pole (or hook) placement is important.
• We now use a grip lock [Grip-loc] dressing! Risk of tube coming out with entanglement is moderate.
• We use Vygon curly tubing for her IV fluids, so it is stretchy and not a major risk for her IV usage. Her g-tube cord though has no curly tubing options, so it is more prone to catching and pulling at her g-tube site.
• My son wakes at least once in the night to use the bathroom, so he untangles himself to get there. He also doesn’t roll around a lot. We secure his lines downward with a sticky device lock and run them under and out the bottom of his shirt, so they don’t wrap high around him.
• [My daughter] was able to voice that she was entangled and waited for me to respond. My son wraps the line around his leg or waist while he is playing on the floor or is restless while sleeping. I keep him in my room at night, so I am usually able to clear his lines quickly and easily. I also actively secure his lines with medical tape or clips to reduce his risk of wrapping himself, especially at night when I will also be sleeping.
• My daughter is a twin and the two of them are very active. Usually, it is just the twin with tubing getting tangled but there have been times during the day that both of them are tangled up somehow. She has a Gus Gear vest that secures her line, and we grip lock [Grip-loc] it down her back to exit at bottom of pajamas or at her waist, depending on what she’s wearing. We use Vygon spiral tubing so there is a little more freedom before the line starts to pull. But the tubing can cinch very tight around body parts. Some people use [a] pool noodle as tubing holder during the night, but she would 100% try to use that as a teether so not a good option. We have fabric line cover that would help but if we put it over the Vygon spiral, the spiral tubing ends up kinking over the next day from being stretched out. She doesn’t stay in one position in her crib so if we clip it to the bed, it would pull out of her when she starts rolling around and flipping directions and running back and forth, etc.
• I use a line cover that I made myself to prevent entanglement.
The above was condensed and reprinted with permission from Larimer, C, Sumner, V, Wander, D. Medical line entanglement: the unspoken patient safety hazard of medical devices. Nutr Clin Pract. 2023; 1–13.
*****
SUMMARY
Our study found that overall clinicians are aware of the risk of medical line entanglement. However, many clinical institutions do not have a policy or procedure in place to address these risks. Further, the study revealed there is often no education about the risks of medical line entanglement provided to caregivers when they receive a medical device with lines for home use. This limited study suggests:
• There is a need for increased awareness and education on the risks of medical line entanglement.
• Healthcare providers of those patients who are at risk of medical line entanglement should discuss with the caregiver how to properly manage and monitor the lines of the medical devices to reduce and prevent the occurrence of devastating consequences, such as strangulation.
• As a parent or caregiver, you should ask your healthcare provider if your child/patient may be at risk of MLE.
*Note from the editor: Additional tips for securing lines and tubes can be found at oley.org/BrightIdeas_Landing.







