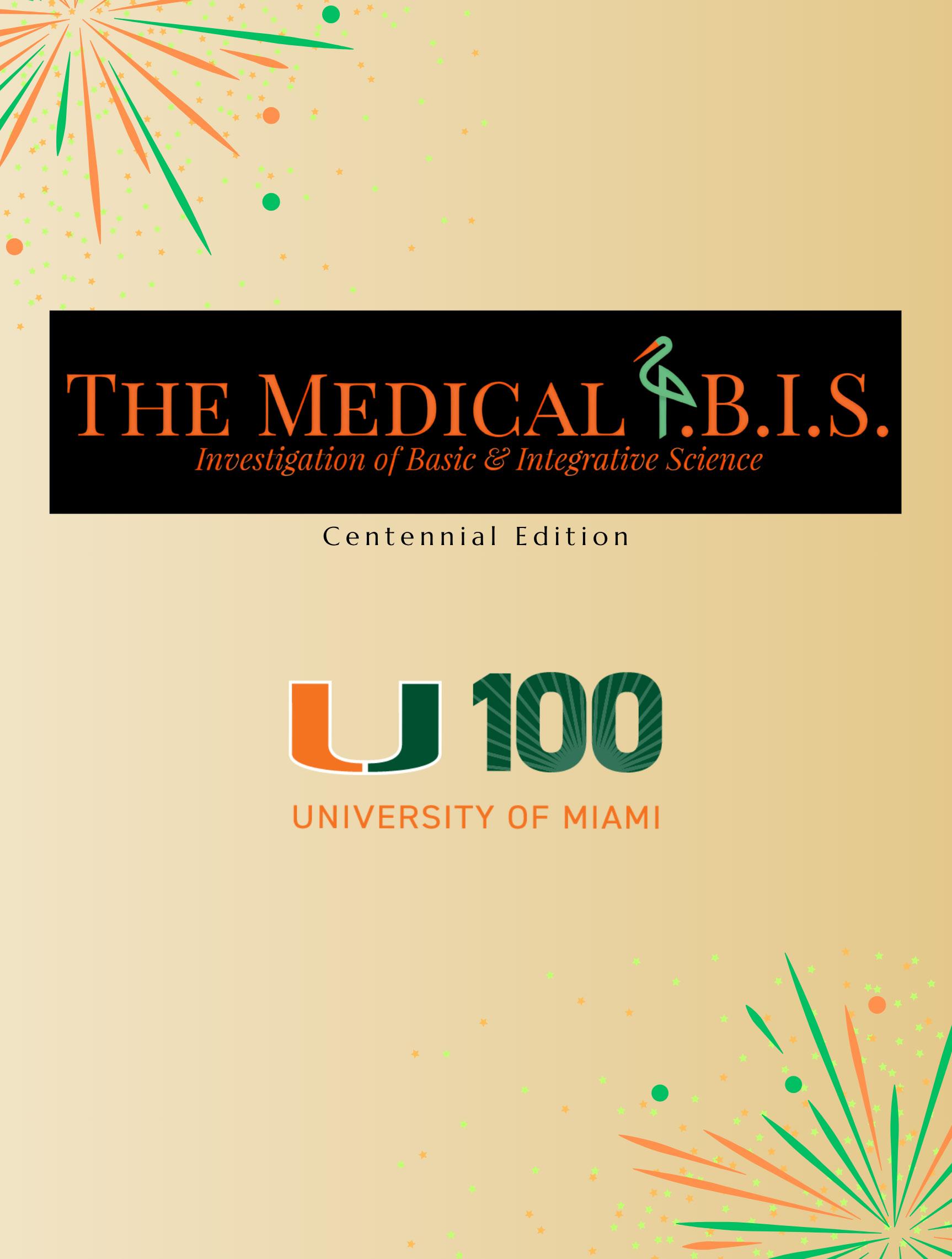
Dean’s Letter
Student discovery and innovation are flourishing at the University of Miami Miller School of Medicine. Our #MedCanes are pushing scientific boundaries and challenging existing dogmas with fresh minds and perspectives. They are working alongside our preeminent researchers, while leveraging advanced technologies to accelerate insights and drive progress.
Engagement in scientific discovery is a cornerstone of medical education, and I’m proud to share that more than 93% of our students are conducting research with a faculty member – well above the national average of 86%. This is no coincidence. Our novel NextGenMD curriculum paves the way for this scholarly activity, offering meaningful opportunities for students to immerse themselves in the research process and build confidence in navigating today’s complex scientific landscape.
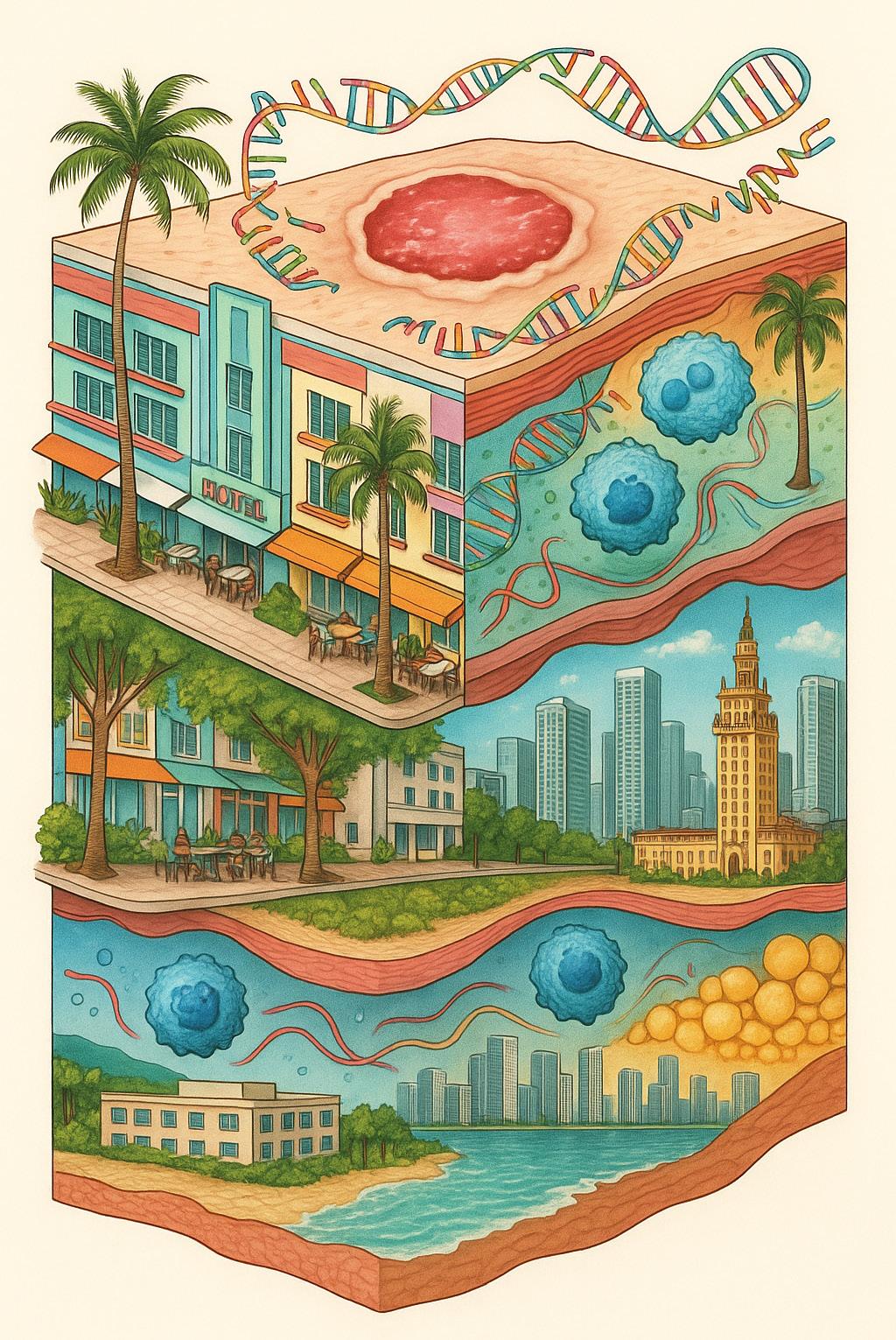
The scientific output of our students and faculty is more important than ever. At the Miller School of Medicine, we play a vital role on the national research stage. Our city’s diverse, multicultural communities allow us to study and enroll in clinical trials a population that closely
mirrors the future demographics of our nation and even the world. By translating our discoveries into new treatments and therapies, we’re advancing clinical care for patients everywhere.
To our students: Stay bold in your pursuit of knowledge. Your curiosity, dedication and drive will lead to discoveries that change lives and shape the future of medicine.
To our faculty: Thank you for your unwavering commitment to mentorship. Your guidance and investment in our students help ignite the next generation of physician-scientists whose work will transform health care.
As we reach new heights year after year, I am immensely proud of our Miller School of Medicine family. Together, we are truly improving medicine today and shaping a brighter future for generations to come.
Henri
Ford, MD, MHA
Dean and Chief Academic Officer, University of Miami Miller School of Medicine



Dear Readers,
Welcome to the thirteenth edition of The Medical I.B.I.S.!
The Medical I.B.I.S. is a student-run publication that showcases the innovative research being performed by medical students at the University of Miami Miller School of Medicine. This year’s issue examines a wide array of important topics, from quality improvement of nasogastric tube use to the genetics of pathologic fractures.
As the University of Miami celebrates its Centennial, the students and faculty continue to pursue key health-related projects that propel the University forward in achieving its goals through education, research, innovation, and service. We invite you to learn about student research in key scientific areas related to access, ethics, and more, showcasing their determination to better understand the healthcare landscape and contribute to improved patient care.
Thank you to The Medical I.B.I.S. staff for making this publication a reality. Your hard work and dedication is appreciated. Please enjoy this issue of The Medical I.B.I.S.!
Sincerely,
Haikel Haile & Yasmine Kamgarhaghighi Editors-in-Chief, The Medical I.B.I.S.















EDITORS IN CHIEF
Haikel Haile
Yasmine Kamgarhaghighi
MANAGING EDITORS
Shriya Patel
Mason Thornton
SENIOR EDITORS
Shreya Ingle
Megan Zou
WRITERS
Janice Huang
Marianna Lekakis
Andrew Sasser
EDITORS
Harini Adivikolanu
Jasmine Kannikal
PHOTOGRAPHERS
Allan George
SELECTION COMMITTEE
Janice Huang
Shriya Patel
Mason Thornton
LAYOUT
Supriya Dadi
Allan George
Mason Thornton

Haikel Haile Yasmine Kamgarhaghighi Shriya Patel
Mason Thornton
Marianna Lekakis
Andrew Sasser
Janice Huang
Megan Zou
Jasmine Kannikal
Allan George
Harini Adivikolanu
Shreya Ingle
Supriya Dadi
CONTENT

The Benefits of Medical Student Involvement in Hospital Policy Review
Integrated Multi-Omics Analyses Identify Activated T cells and PD-1/PD-L1 Signaling as Tissue Biomarkers of Healing Across Four DFU Patient Cohorts
feat. Rachna Rahul, Giselle De La Rua by Marianna Lekakis
feat. Sophie Bilik by Janice Huang
It’s in Your Bones: One Med Student’s Quest to Find the Connections Between Metastatic Cancer and Fractures
Apolipoprotein C3 Deficiency Mediates Podocyte Injury in Alport Syndrome
feat. Levi Travis by Andrew Sasser
feat. Vanessa Addison by Marianna Lekakis
feat. Rachna Rahul, Giselle De La Rua by Marianna Lekakis 09
Leveling the Playing Field: The Influence of Insurance on Treatment Outcomes of Pituitary Adenomas
Using Education to Optimize Identification and Management of Malfunctioning Nasogastric Tubes
feat. Nikola Susic, Khushi Shah by Andrew Sasser
feat. Sofie Janette, Rajan Ramdev, Gabrielle Meli
Evaluating the Information on Acute Knee Injury Presented by TikTok
The Benefits of Medical Student Involvement in Hospital Policy Review
feat. Natalie Blanc, Jacob Jahn, Levi Travis by Marianna Lekakis
Championing Inclusive Innovation in Dermatology
feat. Yasmine Mohseni by Janice Huang

Predicting Pathologic Fracture Risk in Patients with Metastatic Breast and Prostate Cancer
From Bedside to Breakthrough: Interprofessional Education and Surgical NG Tube Management
feat. Sofie Janette, Rajan Ramdev, Gabrielle Meli by Andrew Sasser
feat. Levi Travis by Andrew Sasser
Healing Wounds, Bridging Science and Community
Evaluating the Educational Quality & Accuracy of 163 Million Views of Acute Knee Injury Related Videos on TikTok
feat. Sophie Bilik by Janice Huang
Optimizing the 755 nm Picosecond Laser for the Treatment of Pigmented Lesions in Skin of Color: Insights and A Call to Action 22
feat. Natalie Blanc, Jacob Jahn, Levi Travis by Marianna Lekakis
Impact of Insurance on Outcomes of Patients
Exploring the Role of Apolipoprotein C3 in Alport Syndrome
Undergoing Endoscopic Transsphenoidal Surgery for Non- Functional Pituitary Adenomas: A Single Institution Study
feat. Nikola Susic, Khushi Shah by Andrew Sasser
feat. Vanessa Addison by Marianna Lekakis


The Benefits of Medical Student Involvement in Hospital Policy Review
By Marianna Lekakis
When future doctors confront the gray zones of medicine, their choices reveal more than clinical knowledge—they expose the core of ethical judgment. While physicians are trained to determine the most appropriate treatment for a given case, they are often confronted with challenging dilemmas that even philosophers have long debated.
were both on the medical interest group that had just restarted at UMMSM, and we were attending monthly meetings with the Jackson Ethics Committees. Dr. Goodman shared this opportunity for students to get involved in policy review. Our goal was to get immersed in that process.”

If you’re passionate about something, you have to find the time to make it happen, and that goes for academics, wellness, and other extracurriculars. You just have to find a way to manage your time effectively!”
- Rachna Rahul
“ “
Third-year medical students Rachna Rahul and Giselle de la Rua are no strangers to these complexities. As active members of UMMSM’s Medical Ethics Interest Group, they sought opportunities to go beyond theoretical discussions. “We
Rachna Rahul
MD/MBA Class of 2026
Mentor : Kenneth Goodman, PhD
Eager to do more than simply shadow, the students asked Dr. Goodman for a list of policies to review. Two stood out: one on non-beneficial treatment and another on organ donation after circulatory death. They began by studying current hospital policies and reviewing the latest literature. As the project progressed, they came to the realization that traditional medical education had not adequately prepared them to navigate such complex ethical issues. At that moment, they vowed to demonstrate the value of medical student involvement in hospital ethics committees.
Although many medical schools have begun incorporating bioethics into their curriculum, the content often remains limited to classroom instruction. Much of that education focuses on foundational principles like autonomy and beneficence through lectures, case discussions, and reflective essays. While valuable, this approach is not fully representative of the nuance of real-world scenarios encountered in the clinic or the
Honors : Annual Medical Student Ethics Conference (AMSEC)
Other Interests : Executive Board for Academic Societies; Co-President of the American Medical Women’s Association; Medical Ethics Interest Group; Class Council Information Officer
Future Goals: Internal Medicine; career at intersection of medicine and health policy


Giselle De La Rua
MD/MBA Class of 2026
Mentor: Kenneth Goodman, PhD
Honors: Annual Medical Student Ethics Conference (AMSEC)
Other Interests: Policy Coordinator for the Medical Ethics Interest Group; Vice President of the Ultrasound Interest Group; Ultrasound Team; Vice President for a chapter of the Kern National Network (KNN); OBIE Advisory Board; Senior Director for Harvey Academic Society
Future Goals: Anesthesiology; career at intersection of medicine and health policy
complexities of hospital policy development. As a result, ethics interest groups are emerging across medical schools in the U.S. to help bridge theory and practice. Through physician panels, case reviews, and committee shadowing, students gain exposure to dilemmas that cannot be resolved by textbook answers alone.

To assess the benefits of medical student participation in policy review, Rachna and Giselle conducted a qualitative study grounded in their own experience. They found that hands-on involvement not only exposes students to interdisciplinary teamwork and real-world dilemmas but also fosters a deeper understanding of patient advocacy at a systems level— insight relevant to any specialty.
Hospitals, too, stand to benefit from student involvement, especially through reduced workloads and more efficient policy review processes. “When you have people looking at a policy that’s just been sitting there with fresh eyes, things get done faster,” Rachna noted. Giselle added, “As medical students, we have
much more time to go meet with these stakeholders, like the organ procurement organization, and actually spend time with them and hear their thoughts on the policies [and] areas for improvement, [and] learn their expertise. The people who are on the ethics committees tend to be very busy.”
Looking ahead, the two have several ideas for expanding the project. They hope to involve more students in policy development and collect additional feedback. Eventually, they aim to “further integrate with the ethics committees at each hospital to see how [they] can be more ingrained in the timeline for which policies are reviewed. Each policy has its own timeline, and it can be a little difficult to keep track of them.”
Giselle and Rachna also hope their study helps broaden the scope of the Medical Ethics Interest Group. One idea they are already exploring is having medical students take a more active role in policy creation. As Giselle explained, “Something that we’re now trying with the Medical Ethics Interest Group [is] drafting policies […] for things like posthumous reproduction [and] normal thermal regional perfusion. I think that broadly, medical ethics interest groups, in general, can kind of take up this kind of work to practice the practical implications of all these ethical conversations and topics we’re discussing in medical school. At the end of the day, these policies are going to guide what you end up doing later on, in practice.”




I think that broadly, medical ethics interest groups, in general, can kind of take up this kind of work to practice the practical implications of all these ethical conversations and topics we’re discussing in medical school. At the end of the day, these policies are going to guide what you end up doing later on, in practice.
- Giselle De La Rua
“ “
When asked about the most meaningful aspect of the project, Giselle and Rachna shared that working with members of the ethics committees provided invaluable insight into ethical complexities often overlooked in traditional classroom settings. Being able to witness the full organ donation process was a particularly impactful experience for both students, as one of the policies they reviewed involved donation after circulatory death. “We were with the patient when they passed away,” Rachna recalled. “I think it was during our first or second year, but [we were still on] Phase 1 before rotations started, so […] it was even a bigger deal to us.”
So how do they manage numerous extracurricular activities with the demands of a dual-degree program? For both students, the answer lies in doing what they are truly passionate about. “When you’re involved in so many things, it’s easy to make excuses,” Rachna noted. “But if you’re passionate about something, you have to find the time to make it happen, and that goes for academics, wellness, and other extracurriculars. You just have to find a way to manage your time effectively!”
Giselle agrees that passion drives her success, but she also emphasizes the role of accountability. “For this [research] project, Rachna and I were [...] each other’s accountability. Whenever one of us was overwhelmed […], the other one picked up the slack. I think that having an accountability partner, whether that’s someone who’s working on your project with you or just a friend who knows that you have deadlines coming up and can kind of send you a reminder text, is very helpful.”
Looking forward, Rachna and Giselle are eager to use their MD/MBA degrees and ethics experience to pursue careers at the intersection of medicine and health policy. Giselle, who plans to apply to anesthesiology, hopes to take on a leadership role in hospital administration, “whether that’s eventually heading a department or just being involved in committees like [the ethics committee].”
Rachna, who will be applying to internal medicine programs, is exploring fellowships such as palliative care, where complex ethical decision-making plays a central role. “As dual degree students, we already have that thought in our head of wanting to have kind of an interesting career in medicine that doesn’t necessarily follow the normal path,” she said.
In closing, both Giselle and Rachna expressed their gratitude to Dr. Goodman and the members of Jackson’s ethics committee for welcoming them into these important conversations around complex moral issues and for taking the time to teach them effective techniques for handling them.
It’s in Your Bones: One Med Student’s Quest to Find the Connections Between Metastatic Cancer and Fractures
By Andrew Sasser
When Levi Travis began his medical school journey at the University of Miami Miller School of Medicine, he brought with him an enthusiasm for science and a desire to make a real-world impact. What he did not expect so early in his career was to lead a research initiative that could one day help transform how clinicians approach fracture prevention in patients with metastatic cancer.
“I’ve always had an interest in orthopedics, especially the biomechanics of how the body moves and recovers,” Levi says. “What drew me in was the chance to explore how emerging genetic data might be used to guide orthopedic decision-making in real clinical scenarios.”
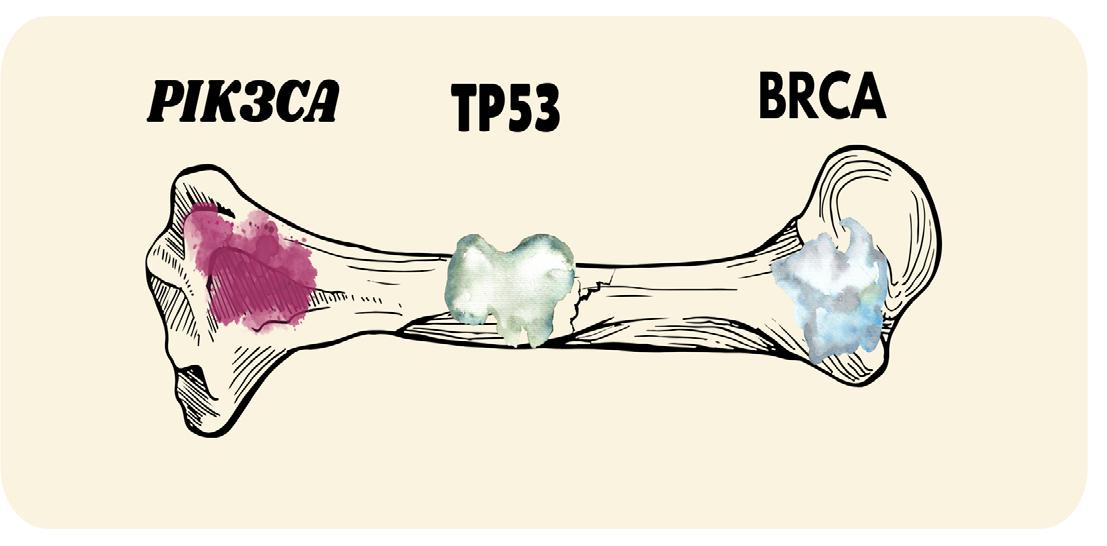
Levi’s research, titled Tumoral Biomarkers Predict Pathologic Fracture Risk in Patients with Metastatic Breast and Prostate Cancer , focuses on identifying whether certain tumor genetic mutations can help clinicians predict the likelihood of fractures in patients whose cancer has metastasized to the bones. His work represents a growing intersection between genomics, oncology, and orthopedic surgery, fields that traditionally functioned in separate silos but are now beginning to converge thanks to advances in precision medicine.
The project began during Levi’s first year of medical school, a time when many students are still finding their footing. “It was definitely a challenge balancing everything,” he admits. “But I knew this project had potential, and I was excited to dive into something meaningful.”
Working with a small but dedicated research team under the guidance of clinical faculty, Levi retrospectively reviewed data from patients diagnosed with metastatic breast and prostate cancer. The primary objective: to explore whether their genetic profiles could be correlated with pathologic fracture, events that often lead to significant pain, reduced mobility, and diminished quality of life. Additionally, he investigated if tumoral biomarkers were associated with the need for pain medication, radiation, or surgery, as well as tumor radiograph characteristics.
“
“Traditionally, clinicians rely on imaging and physical symptoms to determine fracture risk in cancer patients, but this often overestimates fracture risk,” Levi explains. “But what if we could identify patients in a more specific manner by analyzing the genetic mutations of their tumor? That’s what we’re trying to figure out.”
The team’s data collection process involved reviewing patient charts and sequencing reports, focusing on commonly mutated genes in breast and prostate cancer. Tumor mutations in genes that have known association with both tumor progression and skeletal metastases, like TP53 and BRCA1/2 , were of particular interest. By analyzing these patterns, the team hoped to uncover trends that could inform a new model of risk stratification.



While the research is still ongoing, Levi reports that preliminary findings have been promising. “Using Next-Generation Sequencing, we’re seeing certain mutations appear more frequently in patients who experienced fractures,” he says. “It’s too early to say definitively, but the data suggests we’re on the right track.”
If validated, these findings could have major implications for orthopedic surgeons, oncologists, and radiation therapists involved in the care of cancer patients. “Ultimately, our goal is to contribute to a predictive model, something clinicians could use to make earlier, more informed decisions,” Levi explains. “That might mean closer monitoring, or even prophylactic surgical interventions.”
This research also holds personal meaning for Levi. Breast cancer runs in his family, and he lost an aunt to the disease. “It’s one of the reasons I’ve always felt connected to cancer care,” he says. “Her story is part of my motivation to help improve outcomes for patients and families facing these diagnoses.”
The significance of the project is not lost on Levi, who will be applying to match orthopedic surgery this fall.
“Understanding the molecular drivers behind orthopedic outcomes is very exciting to me,” Levi says. “If we can combine surgical care with insights from tumor biology, we can prevent fractures before they happen in the first place.”
“If we can combine surgical care with insights from tumor biology, we can prevent fractures before they happen in the first place.”
The potential impact of this work was underscored during Levi’s inpatient internal medicine rotation, when he cared for a patient with a pathologic fracture from metastatic prostate cancer. “It was incredibly painful and left him with severe functional limitations,” Levi recalls. “He and his family were navigating the reality of limited time, and our job was to preserve his quality of life as much as possible. That experience reminded me why predictive tools matter. Even one less fracture can have a profound, tangible impact for someone in that position.”
Beyond its clinical implications, the project has also helped Levi grow personally and professionally. “One of the most rewarding parts has been developing relationships with faculty and other students who are passionate about research,” he says. “There’s a real sense of collaboration and shared purpose.”
He has presented the project at several academic conferences and is preparing a manuscript for publication. “There’s something powerful about standing up and sharing your work, knowing that it might inspire others or lead to further investigation,” he notes. “It’s also been a great learning experience in how to communicate complex ideas clearly and confidently.”
He also prioritizes wellness and makes time for activities that keep him grounded. “I play soccer every week, I powerlift, and I make sure to spend time with my partner and friends,” he says. “Medical school can be intense, but I’ve found that when I take care of myself outside the classroom, I’m much more effective inside it.”

Levi encourages other students interested in research to be proactive and fearless. “Don’t wait for the perfect opportunity to fall into your lap,” he advises. “I got involved by reaching out, asking questions, and just being open to learning. You never know where a conversation might lead.”
Looking ahead, Levi sees potential for this research to evolve into a long-term project. He hopes to expand the dataset and collaborate with other institutions, explore additional mutations, and perhaps even develop a predictive algorithm or clinical tool. “We’re really just scratching the surface,” he says. “There are many potential modalities that may serve as predictors for pathologic fracture, and by utilizing the newest technologies we will only get more accurate over time.”
He also sees this work as a stepping stone to a career that blends surgical skill with research innovation. “My goal is to be a great surgeon, and with that comes the ability to improve clinical guidelines and
Levi Travis MD Class of 2026
Mentor: Brooke Crawford, MD
Honors: Orthopedic Research Society Annual Meeting, February 2025, Phoenix, AZ. Musculoskeletal Tumor Society Annual Meeting, December 2025, Mexico City, Mexico.
Other Activities: OSIG treasurer, soccer
Future Goals: Orthopedic Surgery
management,” Levi shares. “I want to be someone who makes [a] meaningful impact on the way we approach patient care.”
At the heart of it all is a desire to make medicine more personalized, precise, and proactive. “Every patient’s cancer is different, and by identifying which tumors carry a higher risk of causing fractures, we can tailor care more precisely and avoid unnecessary surgeries,” Levi says. “Ultimately, this all leads to better care for the patient.”
In closing, Levi emphasizes the importance of mentorship, gratitude, and curiosity. “I’ve been incredibly fortunate to work with supportive mentors, including my amazing PI Dr. Crawford, and peers. None of this would be possible without them,” he says. “And I hope this project inspires other students to take a leap – because when you find something you’re passionate about, it stops feeling like work. It becomes part of your journey.”



Leveling the Playing Field: The Influence of Insurance on Treatment Outcomes of Pituitary Adenomas
By Andrew Sasser

In the summer of 2024, Khushi Shah and Nikola Susic began investigating a complex problem rooted in a simple question: how does insurance status affect neurosurgical outcomes? Their research focused on patients undergoing surgery for pituitary adenomas and revealed striking disparities in disease severity and postoperative results between insured and uninsured populations.
The project, conducted under the mentorship of Ashish Shah, MD, grew out of Khushi and Nikola’s prior collaborations within the Department of Neurosurgery. While working with a larger dataset on pituitary resections, the pair identified a specific gap they felt deserved closer analysis. “This project we came across… [was] an opportunity that we saw when we were performing larger studies on pituitary adenomas,” Nikola said. “Khushi sort of had the idea to go ahead and try to look more in-depth into some of the predictors of the outcomes… looking at patients’ insurance status and seeing how that correlated with their outcomes.”
For Khushi, who is pursuing a dual MD/MBA degree, the topic aligned closely with her interests in healthcare access and systemslevel equity. “In every single surgical specialty or even medical specialty, uninsured individuals or people who are underinsured usually have worse outcomes,” she said. “So we wanted to see if that would mimic in this way.”
The pair analyzed data from about 1,000 patients who had undergone endoscopic transsphenoidal pituitary surgery, narrowing their focus to the roughly 800 cases confirmed
as pituitary adenomas. After verifying the data, they performed statistical analyses on a range of variables—including tumor size, length of hospital stay, resection success, and complications—with a focus on insurance status. “We basically looked at a bunch of different surgical variables, demographic variables, as well as some of the outcomes in terms of the surgeries themselves,” Nikola explained.
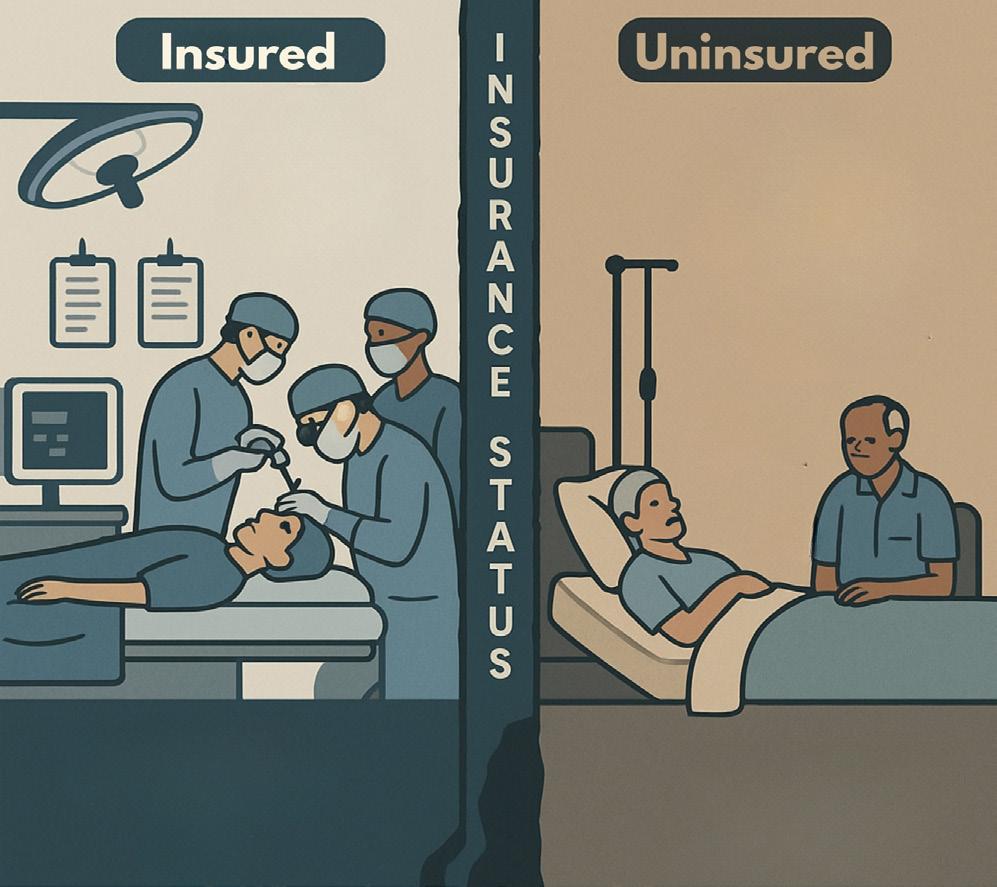
Their findings revealed a consistent trend: uninsured patients presented later, with more advanced disease. “They come in with a much poorer functional status,” Khushi said. “They have more neurological deficits, more visual disturbances, higher tumor volumes.” These patients were also less likely to receive a gross total resection and more likely to experience longer hospital stays—factors that increased the likelihood of postoperative complications.
Nikola noted that the findings extended to Medicaid patients as well. “We found similar findings where they had essentially

Khushi Shah
MD/MBA Class of 2027
Mentors: Ashish Shah, MD
Honors: presentation at the Congress of Neurological Surgeons; publication in Pituitary [https://doi.org/10.1007/ s11102-024-01483-z]
Other Interests: Neurosurgery Interest Group, Ethics Representative of Class Council, DOCS Senior Advisor for IDEA
Future Goals: Neurosurgery
a later presentation,” he summarized. “It may be related to other factors such as socioeconomic status, something that was in our future directions for the project.”
The delays were not minor. “We basically found that people without insurance and those with Medicaid, they’re presenting with a three-to-four-year delay compared to their insured counterparts,” Khushi stated. “Which is a huge delay to have in terms of [pituitary] adenomas—[they] can really affect your vision and sight.”
Khushi pointed out that pituitary tumors are not typically screened for and that betterinsured patients may gain earlier access to care. “They have better access to physicians
“This research showed me how the systems around us –not just the science – shape patient outcomes.”
-Khushi Shah
who will order the correct tests that will identify that they have a pituitary adenoma,” she said. That early identification often led to faster surgeries and improved outcomes.
Both researchers shared personal experiences that shaped their interest in the topic. Nikola, who had worked in a free healthcare clinic prior to medical school, noted, “A lot of the patients were uninsured or underinsured; I noticed that a lot of these patients ended up presenting later on.”
Khushi echoed that perspective, citing her time working with DOCS clinics. “Being underinsured or not having insurance can really be a huge barrier to care,” she said.
The project culminated in a presentation at the Congress of Neurological Surgeons in November and was published soon after in the journal Pituitary. For Nikola, the most memorable part of the experience came after the publication. While rotating with the endocrinology team—who co-manages pituitary adenoma patients—he saw the reallife connection between the data and those it represented. “It was honestly a surreal experience to see how the research that we do in medical school can actually translate to real patient care,” he said.
Khushi shared a similar sentiment. “Each of



those numbers is a particular patient and is their journey,” she commented. “This research gave me a glimpse into what are some things that might be affecting our patients, what we should be considering when we’re in clinic.”
The project has also influenced their professional goals. Khushi, who is interested in neurosurgery and the intersection of medicine and health systems, said it strengthened her commitment to exploring how socioeconomic factors influence surgical outcomes. Nikola, who is still exploring specialties, said the project reaffirmed his desire to keep clinical research as a central part of his career.
Balancing the demands of research, coursework, and leadership roles required discipline and planning. “It’s about prioritizing,” Nikola said. “There are certain times where research might take priority, certain times when school might take priority – but it’s important to always keep in mind wellness.”
Khushi added that wellness needed to be a consistent habit. “It doesn’t have to be four or five hours – even spending 15 to 20 minutes trying to meditate or do some wellness is huge,” she said. “Prioritizing wellness is a habit that you need to have, and not just something that you do whenever you’re free.”

As for advice to future students, Khushi encouraged intentional involvement. “Try to only commit yourself to things that you’re actually passionate about; that makes it much more easy to be able to do and prioritize,” she advised.
Nikola agreed and emphasized the importance of keeping an open mind. “If someone approaches you with a good opportunity, take advantage of those to do work that can actually translate and help people,” he said. “Research is one of the ways that, as a pre-clinical student, you can make a huge difference.”
Both agreed that communication was critical to managing expectations and responsibilities during medical school. “Instead of trying to break yourself trying to get everything done, communication is key,” Khushi recommended. “Never just disappear from your projects.”
“Research is one of the ways that, as a preclinical student, you can make a huge difference.”
-Nikola Susic

Nikola Susic MD Class of 2027
Mentors: Ashish Shah, MD
Honors: presentation at the Congress of Neurological Surgeons; publication in Pituitary [https://doi.org/10.1007/ s11102-024-01483-z]
Other Interests: Co-President of Miller Student Climate Committee, DOCS Assistant Director of Medical Informatics, Army Liaison for Trauma Interest Group
Evaluating the Information on Acute Knee Injury Presented by TikTok
By Marianna Lekakis
Anew beginning has never scared Natalie Blanc. From her first few weeks as a medical student, Natalie was eager to discover innovative research opportunities. “I just reached out to different interest groups and emailed potential mentors.” It was not long before her efforts gained traction – by October, Natalie embarked on a project that transpired from the intersection of data analytics, orthopedic medicine, and… Tik Tok.
Under the esteemed mentorship of Lee Kaplan, MD, MBA, Natalie’s unconventional research aimed to investigate the integrity of information on knee injuries disseminated on the social media platform, TikTok. Given the application’s popularity and its indomitable presence in modern culture,

its influence cannot be underestimated. “People are turning to social media platforms like TikTok to get healthrelated information, so we wanted to look at the accuracy and reliability of that information.” Using key terms
and hashtags related to knee injuries, surgeries, and recovery, Natalie and her team identified 234 TikTok videos that collectively served as a repository for vital health-related information. Video content ranged from those focused primarily on specific injuryrelated messaging to others with an emphasis on recovery. After sourcing user-generated media that met the study’s inclusion criteria, they then utilized the DISCERN scoring system to operationalize the method in which video quality was analyzed. This validated tool assesses reliability, clarity, and balance of information, among other key parameters, to derive numerical scores that can be compared across short-form media content. Not only did the team generate data appraising information accuracy, but they also went a step further to characterize the types of content that were associated with the most engagement, as defined primarily by likes and comments. Messaging formats, as well as creator demographics and qualifications, were also accounted for to reconcile any potential confounders.
Based on the study’s preliminary findings, Natalie found that users engaged to a greater extent with content incorporating medical recommendations. This not only highlights individuals’ tendencies to solicit social media platforms for advice but also reveals possible nuances pertaining to health literacy and self-empowerment that shape the physician-patient exchange. Such engagement could translate to profound implications for serving patients, but it should also be



approached with caution. Alarmingly, only a minority of the videos identified in the study were created by physicians. While this subset scored the highest in terms of quality, those created by non-professionals garnered the most views. Moreover, this research revealed an interesting caveat: “profit-oriented accounts” posted a considerable proportion of the sourced videos. At baseline, such accounts generally boast greater overall engagement, which invokes the deeper question of commercial interests and their potential bias on digital health information integrity.

While the phenomenon remains to be studied, the impact of user-generated media as prevalent reference points could point to both an opportunity and challenge as it relates to patient behavior. “This could help patients realize that they shouldn’t be relying on
TikTok for information regarding their health conditions. It just emphasizes the fact that they should be speaking to their doctors about their treatment plans and diagnoses. It’s also good for physicians to know that their patient population is likely consuming a lot of content [from social media].” The study highlights the desperate need for credible health content developed by those formally qualified to deliver it.
As for Natalie, she and her research team have submitted a manuscript detailing their findings to peer-reviewed scientific journals for publication and look forward to sharing their insights with the medical community. While her role in this phase of the project has concluded, Natalie intends on further inquiring how social media affects patient behavior. “I think it would be interesting to see how the different quality levels of different TikTok videos actually influence patient behavior, their expectations about their treatment, and satisfaction with their treatment. This was actually a limitation of our study— we weren’t able to look at whether these videos were actually influencing patient behaviors. It would also be interesting to examine the efficacy of a verification tool on content with accurate information.”
Reflecting on her contributions, Natalie is grateful for the opportunity to align her research interests with her professional
“As a medical student, I think it’s important to do research to learn about things that we might not necessarily learn about in our first-year curriculum.” “ “

aspirations in orthopedics. “I want to do research in the future, so building that strong foundation now will help me continue to do it throughout residency and after.” Natalie endorses research as an important component of medical education – especially in the first year. “As a medical student, I think it’s important to do research to learn about things that we might not necessarily learn about in our first-year curriculum.”
So how does Natalie find time for something as rigorous as research? “I personally try to set aside a chunk of my day and just block out time on my calendar to focus on research because, otherwise, it’s really easy to just get caught up in school and other extracurriculars.” This approach seems to be working exceptionally well for Natalie.
But that is not to say research is the only extracurricular activity on Natalie’s agenda. She serves as the Assistant Project Coordinator for the DOCS Big Pine Florida Keys Health Fair and frequently volunteers at various DOCS clinics and events hosted by the Dudes for Dads organization. She is also a member of CHAMP, an organization in which medical students act as mentors for children in Jackson’s pediatric dialysis unit.

When not busy studying on campus, working on research, or volunteering, you will undoubtedly see Natalie on the yoga mat, mastering the Adho Mukha Svanasana pose. Natalie is Co-President of Zen Med, UMMSM’s yoga club. She also teaches and attends classes at Core Power Yoga. Her active lifestyle has always served as a significant stress reliever and is now an essential component of her wellness routine.
Aside from yoga and other extracurriculars, Natalie prioritizes nurturing meaningful relationships by spending time with her loved ones. She always makes it a point to FaceTime with family and friends back home in California. She also enjoys frequenting Miami’s vibrant dining scene and taking advantage of everything the Magic City has to offer.
In closing, Natalie would like to acknowledge her fellow medical students, Levi Travis and Jacob Jahn, who worked diligently alongside her on this project. She goes on to express her immense gratitude to Dr. Kaplan for his mentorship throughout the study. Last, but certainly not least, she would like to recognize her talented research team colleagues for instilling the skillset that has contributed to her ongoing success in research, as well as future biomedical endeavors.
Natalie Blanc MD Class of 2028
Mentor: Lee Kaplan, MD, MBA
Other Interests: Assistant Project Coordinator for the DOCS Big Pine Florida Keys Health Fair; Co-President of Zen Med; Yoga Instructor at Core Power Yoga; Volunteer at Dudes for Dads; Volunteer at DOCS; CHAMP
Future Goals: Continue involvement in research and explore orthopedics


Championing Inclusive Innovation in Dermatology
By Janice Huang
When first-year medical student Yasmine Mohseni began serving patients seeking dermatologic care, she discerned a troubling pattern. Advanced treatments—particularly laser therapies—frequently lacked sufficient evidence-based data for patients with darker skin tones. This marked underrepresentation served as the impetus for Yasmine’s path to advocacy and scientific inquiry, culminating in meaningful innovation early in her medical training.
Under the mentorship of Dr. Alyx Rosen Aigen and guidance of research fellow Lauren Dender at the University of Miami Miller School of Medicine, Yasmine conducted a comprehensive review of the 755 nm picosecond laser. This is a popular FDA-approved device that targets melanin and is effective in treating pigmentary conditions such as melasma, Nevus of Ota, and tattoo removal. Her research revealed a notable oversight— statistically significant clinical studies largely excluded patients with Fitzpatrick skin types V and VI. These skin types are predominant in African American and Hispanic populations.
“Our research showed a significant lack of representation for darker skin types,” Yasmine explains. “Without inclusive data, patients and clinicians lack the guidance needed to confidently pursue advanced treatments.”
Uncovering gaps in care was only the initial step; Yasmine was determined to directly address them. Inspired by patient experiences and motivated by her findings, she co-founded SkinSmartTM Inc., a pioneering startup driven by artificial intelligence to improve dermatologic care among underserved communities.
Seeing the gaps in dermatologic research made me want to be part of the solution - that’s what inspired me to build SkinSmart. “ “

SkinSmartTM aims to enhance diagnostic accuracy, personalize treatments, and support equitable outcomes for patients with skin of color, in an effort to combat longstanding disparities ingrained in the field.
“With SkinSmartTM, we are leveraging technology to fill critical gaps in care within dermatology,” Yasmine says. “It is not just innovation for innovation’s sake—it is innovation for health equity.”
Yasmine’s vision quickly gained momentum when she earned the prestigious USTAAR grant. Not only is this an early career award validating her startup’s potential, but it also funds advanced technological development.
Honors: ESRF Poster Presentation (February 2025), USTAAR Grant Winner for startup SkinSmartTM Inc.
Future Goals: Dermatology
Yasmine Mohseni MD Class of 2028
Mentor: Alyx Rosen Aigen,
MD
Other Interests:
• CEO, SkinSmartTM Inc.
• Chair, Student Teaching Excellence Awards
• Communications Chair, Dermatology Interest Group
• Sponsorship Director, SunSmart 5K
• Volunteer, DOCS Health Fair Dermatology Station
• Social Outreach Chair, UV&Me
• Instagram mentorship (@sweets.n.scrubs)
Balancing her demanding first-year curriculum with her entrepreneurial responsibilities, Yasmine exemplifies how medical students can meaningfully integrate research, clinical insights, and innovation to impact patient care.
In addition to her entrepreneurial efforts, Yasmine actively participates in campus and community initiatives. She serves as Communications CoChair for the Dermatology Interest Group, chairs the Student Teaching Excellence Awards, and is Sponsorship Director for the SunSmart 5K, a fundraiser supporting skin health awareness. She also regularly volunteers at the Department of Community Service (DOCS) health fairs to help expand dermatologic care for underserved populations across South Florida. Through her UV&Me outreach platform, she continues to educate communities about skin health, sun protection, and preventive care.

Her commitment to mentorship and wellness extends beyond formal programs. Through her Instagram account, @sweets.n.scrubs, Yasmine curates wellness tips, nutritious recipes, and practical advice for thousands of premedical students navigating their personal and professional journeys. Entwined within her content are the reverberant themes of balance, self-care, and purposeful growth in medicine.
Looking ahead, Yasmine plans to pursue a residency in dermatology with a continued emphasis on health disparities, technological innovation, and advocacy. Her ultimate goal is to reform clinical practice and health policy, ensuring dermatologic advancements serve every community equitably. “Innovation isn’t meaningful unless it reaches everyone,” Yasmine reflects. “Dermatology can and should set the standard for inclusive, precise, and compassionate care.”



From Bedside to Breakthrough: Interprofessional Education and Surgical NG Tube Management
By Andrew Sasser
As a third-year medical student at the University of Miami Miller School of Medicine, Sofie Janette never expected her most impactful research project to begin not in a lab, but in the halls of a hospital. Her quality improvement initiative addressing nasogastric (NG) tube mismanagement was sparked by simple clinical observations and driven by a fundamental question: Could enhanced nursing education prevent devicerelated complications?
T he project stemmed from observations made by surgical resident Dr. Rebecca Saberi, who noted frequent issues with NG tubes on the general surgery service, from gastric content leakage and patient discomfort to serious complications like intestinal bleeding. Further investigation revealed many nurses lacked formal training on proper NG tube management.
“It came from problems seen at the bedside,” Sofie explained. “There was this disconnect between what the device was designed to do and how it was actually being managed on the floor.”
Under the guidance of Carl Schulman, MD, PhD, MSPH, and Sabrina Taldone, MD, MBA, Sofie joined forces with classmates Gabrielle Melli and Rajan Ramdev to launch the initiative. They aimed to transform informal bedside teaching into a structured educational intervention for nursing staff, and hypothesized that brief, targeted training sessions could reduce mismanagement incidents.
Rajan began the project in Summer 2022, documenting NG tube conditions in West Wing 10 through photographs and conducting on-service trainings using real examples of improper setups. These visual demonstrations highlighted how misinterpretation of the NG tube’s dual-lumen system could lead to preventable errors.
In Summer 2023, Sofie and Gabrielle expanded the initiative to include Ryder Trauma Center’s third and fourth floors. They conducted comprehensive room-by-room assessments, collaborated closely with nurse managers to tailor sessions, and organized multiple training sessions across all shifts despite scheduling challenges.
Their assessment applied to approximately two dozen NG tubes across the units. Following the educational intervention and placement of visual reference cards in patient rooms, they found zero malfunctioning tubes—all sump tubes were properly connected to suction, with correctly functioning air-only channels.
Beyond quantitative improvements, qualitative feedback affirmed the intervention’s value. Nurses described the training as beneficial, with some specifically citing the reference cards as a helpful resource when uncertain about proper procedures.
The project’s impact has extended well beyond its initial scope. The team presented their findings at multiple venues, including the Jackson Health Quality Improvement & Safety Conference and the National IHI Patient Safety Congress in Orlando, where their work generated significant interest from attendees looking to implement similar programs at their own institutions. In response, the team developed standardized training materials, including a PowerPoint module and instructional video, to support broader integration throughout Jackson Health System and other hospitals.
What struck Sofie most was the immediate and visible impact of their work. Unlike traditional clinical research that can take years to affect patient care, their quality improvement work produced tangible, realtime change.


Sofie Janette MD Class of 2026
Honors: Jackson Memorial Hospital Quality Improvement and Safety Conference, March 2024; IHI Patient Safety Congress, Orlando, FL, May 2024; Manuscript submitted
Mentor: Carl Schulman, MD, PhD, MSPH; Sabrina Taldone, MD, MBA
Other Interests: Public Relations Director for WAC, DOCS Medical Informatics Director
For Sofie, who also serves as Public Relations Director for the Wellness Advisory Council and technology manager for the Department of Community Service, the project provided valuable lessons about interdisciplinary collaboration. “If you want to change something in medicine, you can’t do it alone,” she reflected. “It has to be collaborative—physicians, nurses, administrators. Everyone has to be on board.”
She also emphasized the team’s nonjudgmental approach to education: “It was never about blaming anyone. In our trainings, we’d tell people, ‘This isn’t just you—most people don’t know how this device works.’”
Balancing the bulk of the project during her M1 summer and the following academic year, Sofie credited careful planning and effective teamwork with her ability to manage research alongside the demands of medical school. The nursing education sessions—despite scheduling obstacles—
If you really want to improve anything, it has to be interdisciplinary. It can’t just be physician-only — it’s about finding ways to communicate without blame and work together to make change. “ “
became her favorite aspect of the project. She observed how initial reluctance transformed to genuine engagement, as nurses actively participated and drew connections between the material and their clinical practice.
The experience ultimately reshaped Sofie’s perspective on her future in medicine. “It showed me how to identify a problem, implement a solution, and assess its impact,” she said. “That’s something I’ll carry with me into residency and beyond.”
To maintain balance while managing research and academics, Sofie prioritizes wellness through cooking, exercise, and staying connected. “Cooking dinner with friends or going on walks has been key,” she noted. “Even during rotations, I made it a priority. I may not have finished all the UWorld questions, but I felt mentally well— and that made a difference.”
For students beginning their research journey, Sofie offers this advice: “Do something you genuinely care about. Don’t pick a project just because it looks good on paper or matches your specialty. If you’re excited about it, you’ll go further and enjoy it more.”
The team recently submitted a manuscript to the Journal of Surgical Education , contributing to broader conversations in medical training and patient safety. While proud of this upcoming publication, Sofie remains most grateful for the collaborative teamwork and shared purpose that brought the project to life.



Healing Wounds, Bridging Science and Community
By Janice Huang
Sophie Bilik’s path to medicine began at the laboratory bench. As a master’s student and research associate in the Stone Lab at the University of Miami Miller School of Medicine, she immersed herself in translational research on diabetic foot ulcers (DFUs)—a condition she would later encounter firsthand through her clinical work with Miami Street Medicine.
Her research focuses on understanding how T cells—a type of immune cell— influence wound healing. She investigates the role of immune checkpoint proteins like PD-1 and PD-L1 in healing outcomes, using sophisticated techniques such as RNA sequencing, spatial profiling, and single cell analysis. “What inspires me most is translating scientific discoveries into meaningful patient care,” Sophie says. “Knowing that my work in the lab could lead directly to better treatments motivates me every day.”
As her research progressed, Sophie became involved with Miami Street Medicine, a nonprofit clinic providing mobile healthcare services to people experiencing homelessness. Her work added a new dimension to her research, highlighting the real-world challenges patients face. Many of the individuals she encountered were living with poorly managed diabetes, resulting in chronic, complex wounds—the very condition she studies in the lab. “I didn’t anticipate how deeply my lab research would connect with my clinical experiences,” Sophie reflects. “Seeing patients in the community dealing with chronic wounds
made me appreciate even more how vital our research could be for their healing and overall quality of life.”
Mentorship has been a cornerstone of Sophie’s growth in research and medicine. Under the guidance of Rivka Stone, MD, PhD, she has grown as an independent researcher with a clear scientific vision.
“Dr. Stone has shown me how powerful mentorship can be,” Sophie explains. “She encourages me to ask challenging questions, think independently, and trust my instincts.” Inspired by Dr. Stone’s example, Sophie now mentors younger students through Miller Mentors and the M.S. in Biomedical Sciences program, seeking to provide others with the same guidance that
shaped her own path. “I love mentoring because it allows me to support others the way I’ve been supported,” she says. “It’s one

Sophie Bilik MD/MBA Class of 2028
Mentors: Rivka Stone, MD, PhD
Honors: Oral Presentation, Innovations in Wound Healing Conference, Key West, FL, December 2024; Oral Presentation, Wound Healing Society Conference, May 2025; Images selected for display at the American Academy of Dermatology and featured at RMSB
Other Activities: Miami Street Medicine Care Coordinator; Class Council Member; Dermatology Interest Group Youth Outreach Coordinator; Mentor for MiBS students and Miller Mentors; Running and outdoor recreation
Future Goals: Dermatology with a focus on immunodermatology, wound healing, and healthcare leadership through academic medicine
of the most fulfilling parts of my medical school experience.”
Beyond research and mentorship, Sophie serves as a class council member and youth outreach coordinator for the Dermatology Interest Group, where she helps lead community engagement and education efforts. She maintains balance through structure, meticulous time management, and consistent exercise. An accomplished runner who has completed eight half marathons, Sophie finds strength and clarity in the routine of outdoor training. “Running has always helped me clear my mind and manage the demands of medical school,” she says. “It’s a way to stay grounded and reconnect with myself.”
Looking ahead, Sophie plans to leverage her dual MD/MBA training to pursue a dermatology residency with a focus on immunodermatology and wound healing. She envisions a career in academic medicine that integrates clinical care, translational research, mentorship, and healthcare leadership. Driven to create lasting change, she hopes to contribute to both patient care and healthcare strategy and innovation by building systems that improve outcomes, particularly for underserved populations.
Through each stage of her journey, Sophie remains guided by a simple yet profound vision: “To make healthcare more personalized, equitable, and effective for every patient I encounter.”
Working with a mentor who values curiosity and independence shaped this project into a defining part of my training. “ “



Exploring the Role of Apolipoprotein C3 in Alport Syndrome
By Marianna Lekakis
Unlike many peers who charted their path to medicine early on, secondyear medical student Vanessa Addison did not always envision becoming a physician. A biophysics and biochemistry major at the University of Arizona, medical school was not brought into focus until she began working as an EMT during the COVID-19 pandemic. Immersed in patient care, Vanessa fell in love with the medical field.
Vanessa’s unexpected journey to medicine was paralleled by a growing passion for research. As an undergraduate student, she studied neurodegenerative diseases. Now in medical school, she continues to pursue basic science through KIIMERA, an NIH-funded summer research program in nephrology. Under the mentorship of Alessia Fornoni, MD, PhD, and Sandra Merscher, PhD, she investigated the role of apolipoprotein C3 (APOC3) in Alport syndrome, a genetic kidney disorder often marked by hematuria, proteinuria, earlyonset hypertension, and hearing or vision defects.
APOC3, a protein involved in lipid metabolism, had recently been found to be markedly downregulated in patients with focal segmental glomerulosclerosis (FSGS). Given that Alport syndrome may also cause lipid accumulation in podocytes, Vanessa’s team explored whether APOC3 might contribute to its pathogenesis. “This project grew out of previous FSGS research (the NEPTUNE study) showing that downregulation of APOC3 was associated with lipid toxicity—a driver of disease in that model,” she explained.
Using podocyte cell cultures and mouse models, Vanessa’s team discovered elevated mRNA levels despite low protein expression of APOC3. Further, they found that sialylation—a post-translational modification important for APOC3 stability—was defective in Alport syndrome. These insights could pave the way for precision medicine approaches. Potential therapies may involve recombinant APOC3 replacement or drugs
that enhance sialylation to restore protein function—interventions already explored with apolipoprotein M in FSGS. “Targeting sialylation offers a more specific strategy with fewer off-target effects,” Vanessa noted.
In addition to her involvement in research, Vanessa is currently the research coordinator of the Nephrology Interest Group and the CHAMP pediatric dialysis mentorship program. She is also the president of SCOPE (the GI Interest Group), Project Lead of the Miller Student Climate Committee, and an active member of Medical Students for Choice. Her advice on juggling multiple commitments? Choose wisely. “There’s definitely an incentive [for medical students]
There’s definitely an incentive [for medical students] to be involved with as many activities as they can, and I don’t think that’s right [...] I think it’s super-important to be involved in things that you are genuinely passionate about because that’s when you’ll do well at them.
“ “
to be involved with as many activities as they can, and I don’t think that’s right,” Vanessa said. “I think that there’s a misconception that people would feel when looking at the [number of] things I’m involved in. But I think it’s super-important to be involved in things that you are genuinely passionate about because that’s when you’ll do well at them.”
Vanessa adds that not all her involvements are medically related—and that’s intentional. “You should pursue things that aren’t just [related to the profession you want to pursue]. You should do things that you actually enjoy.”

Vanessa Addison
MD Class of 2027
Mentor: Alessia Fornoni, MD, PhD; Sandra Merscher, PhD
Honors: KIIMERA award for the summer of 2024; poster presentations at the Florida Society of Nephrology Annual Meeting (January 2025), EasternAtlantic Student Research Forum (ESRF) (February 2025), and Global Health Symposium (April 2025)
Other Activities: President of SCOPE; Research Coordinator of the Nephrology Interest Group; Vice President of UMMSM’s Run Club; CHAMP pediatric dialysis mentorship program; Project Lead of the Miller Student Climate Committee; Medical Students for Choice
Future Goals: Continue pursuing research
To stay on top of her many commitments, Vanessa relies heavily on structure. “I am definitely a planner. My entire life is essentially organized on my calendar, and that helps keep me sane.” Equally important to maintaining balance is finding time to decompress. A dedicated runner, Vanessa serves as vice president of UMMSM’s Run Club and also enjoys running solo in her free time. “I love [going] on a long run and either think through a lot of things or not think about anything at all. I’ve always been into that! Whenever I have a big life problem, or I’m at
a stall in my research or schoolwork, taking anywhere from 30 minutes to an hour to go on a run is nice.”
In addition to planning and exercise, Vanessa emphasizes the impact of a strong support system. “Spending time with my friends is important because hearing about the collaborative struggle can actually be kind of uplifting. Knowing that you’re not in this alone [is important]. I’m fortunate for my roommate and a lot of my friends. I think without them I would be in a world of struggle because we all kind of teach each other to be a bit gentler with ourselves, and to take breaks, and to maintain our hobbies […]. Having that outside support is really important [for] maintaining your wellness.”
Vanessa has not yet decided on a specialty and is keeping an open mind. “I know that’s a very boring answer that everybody gives, but I think it’s important to [stay open-minded]. With many rotations, I’m like, ‘Wow, I really love my experience!’ I haven’t found a single rotation that I [completely hate], so it makes it hard to choose.”
Regardless of what she ultimately chooses, Vanessa remains committed to engaging in research throughout her career as a physician and urges other medical students to do the same. “One thing that is very central to why I wanted to become a physician and not a different healthcare professional is the practice of evidence-based medicine.



To many people, being a physician-scientist means having an MD/PhD. But I think that we can all be physician-scientists by engaging in research at any level continuously throughout our careers.”
She adds, “Being able to ask a novel question, come up with a hypothesis, and then pursue a plan to answer that question […] is a lifelong skill [for] physician[s]. I think that those skills are very translatable to whatever type of research you engage in. That’s super important to me and is actually one of my biggest motivations for wanting to come to medical school.”
While Vanessa is currently working on a project involving hormone replacement therapy and menopause, she has temporarily stepped away from wet lab research during her demanding Phase 2 schedule. “[In basic science], you can work for four years to accomplish one publication, and it’s massive,” she said. Still, she plans to return to the lab in her third or fourth year.
When she does, she hopes to study the role of apolipoproteins in other kidney diseases and engage in more interdisciplinary research. “One thing I found really interesting is that APOC3 is a target already in cardiovascular and liver research,” she explained. “[Scientists] understand the model of fatty liver disease better than that of kidney disease […] I think it would be interesting to try to understand if there is a common mechanism that underlies its role in nephrology-related diseases, cardiovascular diseases, and liver diseases. I think that this collaborative research could be very cool.”
Vanessa also challenges the notion that basic science is disconnected from clinical care. “One of the [misconceptions] about basic science research is that it’s obscure,” she noted. Her experience in Dr. Fornoni’s and Dr. Merscher’s labs has proven otherwise. “[Their research] is intended to have therapeutic benefits. We always ask, ‘What’s the point of this? Is this actually going to change how we help patients? Is this going to have some sort of therapeutic impact?’”
Reflecting on her journey, Vanessa expressed gratitude to her research mentors, Drs. Alessia Fornoni and Sandra Merscher,
and their research teams for giving her the opportunity to pursue work she is passionate about and for equipping her with skills she will carry throughout her career as a physician-scientist.
Dr. Fornoni also shared her appreciation for Vanessa’s contributions: “As Director of the newly established UMMSM Research Innovation and Scholarly Engagement (RISE) office and Assistant Dean for Research Training and Development, I am extremely proud of seeing talented students like Vanessa become passionate about a career as a physician-scientist, as it is only through students like her that new evidencebased medicine can be generated.”
“Being able to ask a novel question, come up with a hypothesis, and then pursue a plan to answer that question […] is a lifelong skill [for] physician[s]. I think that those skills are very translatable to whatever type of research you engage in.”

