YOUR CALL. Issue 16 nwas.nhs.uk Paramedic Paul talks about his serious cycling accident and the impact it has had on his life. 8 Paramedic Irvine talks about his pioneering research into working nights. 6 3 SPECIAL MATERNITY TRAINING AND EQUIPMENT FOR AMBULANCE CREWS TO HELP WITH 999 CALLS
TO THE SUMMER EDITION OF YOUR CALL. Also in this issue...
Doesn’t it feel lovely to have a summer without restrictions? The first since 2019!

We hope whatever you have planned over the next couple of months you enjoy it!
We have spoken to and met some incredible people who are featured in this edition all of whom have a unique story and experience to share – hopefully some you will be able to relate to and some which may help you.
We talked to a very special family in Greater Manchester who witnessed their 12-year-old daughter have a cardiac arrest – their quick-thinking actions and her dad’s knowledge of how to do CPR saved her life.
Violence and aggression against our staff has been a hot topic since we can remember and it is well documented how ambulance staff wrongly suffer abuse at work from the very people they are there to help. Every day last year, a staggering 32 NHS ambulance staff were abused or attacked; more than one every hour of every day during the whole of last year; totalling 11,794 staff. This is an increase of 4,060 incidents over the last five years. We share Tammy’s story – we all have a right to #WorkWithoutFear.
There is no doubt that sustainability and saving the planet is a high priority on the world’s agenda, we share a little snippet of what we have been doing with Kendal ambulance station to make sure it is staying smart as part of a pilot scheme to cut down on wastage and inefficiencies.
Enjoy!
Take care and stay safe. COMMUNICATIONS TEAM
DO YOU HAVE A STORY TO SHARE WITH US? If so, please get in touch by emailing: communications@nwas.nhs,uk.
FIRST OF ITS KIND MATERNITY TRAINING AND EQUIPMENT FOR AMBULANCE CREWS. Providing safe and personal maternity care to our patients is important and we bring you exclusive news on this project.
PARAMEDIC’S PIONEERING PHD RESEARCH.
Irvine talks about his investigation into night shift working to understand the long-term effects it can have and how we can improve on it.
MY IVF STORY. We speak to Emergency Medical Technician Lynsey about her IVF story and how she is using her experience to educate fellow colleagues.
STREET DOCTORS. We’re teaching young people how to treat somebody if presented with a stabbing.
FROM THE NAVY TO WRITING POETRY. Meet Ryan the supervisor making his colleagues cry for the right reasons.
nwas.nhs.uk nwasofficial @nwasofficial @NWAmbulance
Welcome
18
6
20
7
3
2
SPECIAL MATERNITY TRAINING AND EQUIPMENT FOR AMBULANCE CREWS TO HELP WITH 999 CALLS.

Last year, we handled over 24,000 NHS 111 and 999 maternity-related calls combined from across the North West. This can include providing urgent and emergency care to pregnant women and babies suffering from complex health complications or when these patient groups may require transfers into hospitals.
Providing safe and personal maternity care to our patients is important and we have invested in a pre-hospital training package by PROMPT Maternity Foundation Charity to enhance this.
The training is the first of its kind to be delivered within our emergency service and funding was secured for it by our Consultant Midwife, Stephanie Heys, from Cheshire and Merseyside’s local maternity systems and Health Education England (HEE).


Stephanie says: “This brings so many opportunities for us as an organisation to work and train together with our local maternity units and community midwifery teams’’
“The first sessions which took place in Merseyside in May was well-received by clinicians in Team NWAS. Looking ahead, we would like to partner with local maternity systems across the NWAS footprint to secure additional funding and scale this training across the region.”
Catherine McLennan, Director of Women’s Health and Maternity (WHaM) Programme, Cheshire and Merseyside Health and Care Partnership said: “We are delighted to partner with NWAS and support another great initiative which puts the safety of women and their babies at the heart of care. Multi-disciplinary teams who train and work together are essential for continuous improvement, and we look forward to all other LMSs following this work in Cheshire and Merseyside.”
As part of the funding already secured via the Cheshire and Mersey Maternity Networks, we have been able to secure our first practice development midwife, Rachel, who has joined our midwifery team for six months to help scale and deliver this training.
It has also enabled us to successfully bid for HEE funding to purchase maternity training equipment, including a suite of preterm baby dummies with ‘real-life,’ accurate and functioning anatomy. This equipment will enable high-quality team training in rare emergencies that can occur during childbirth. It will also ensure that the simulated scenarios embedded within PROMPT training are realistic, engaging, and innovative.
We will keep you updated on our social media channels how this initiative progresses, it is a positive development for emergency care for pregnant women.

3
Experiencing
On the afternoon of Sunday 10 October last year, dad of two, Ben was at home recovering from injuries he had sustained just a few days before after a cycle accident.

Suddenly Ben heard his daughter Charlotte, aged eight calling him to come to the garden. Sensing a little panic in her voice, Ben, holding his broken ribs, slowly made his way to the garden when he saw his elder daughter Grace, 12 lying on the trampoline with his wife Rebecca with her, so his first thought was Grace had fallen and hurt herself.
Ben quickly realised something was seriously wrong with Grace, after seeing vomit in her mouth and her eyes fixed. She wasn’t breathing, so Rebecca quickly called 999 while Ben started CPR, a skill he had learnt though a first aid course at work.
your 12-year-old daughter go into cardiac arrest is not something you would expect – this was a reality for parents Ben and Rebecca.
4
Realising immediately that trying to perform CPR on a trampoline was futile, they managed to drag the trampoline and quickly move Grace to a garden picnic bench.
Ben recalls: “I started chest compressions and breaths, but I was scared I was hurting her, but the 999-call taker was giving me clear instructions to ensure the chest was rising between pumps, and to slow my pace as I kept increasing the speed.”
Very soon after, the garden was full of emergency responders, who allowed Ben to continue with compressions while they started other interventions to help Grace. A defibrillator was used, and it took four shocks before there was any signs of life.
Grace, who is autistic and born with a heart condition that is regularly monitored, was quickly rushed to Manchester Children’s Hospital where she was placed in an induced coma. After a few days in ICU, it was time to slowly bring her out of the coma.
Ben said: “Due to Grace’s needs, we ensured either Rebecca or I were there for Grace the second she opened her eyes. It was a scary time as we didn’t know if Grace would have suffered brain damage as she had stopped breathing for 20 minutes.
“When she started to stir, despite all the noise around us, I spoke to Grace and her head turned in my direction, so I knew she recognised my voice. I then asked her to put her thumb up if she was ok, which she did, it was an amazing moment, I knew my little girl was going to be ok.”
Grace has since been fitted with an internal defibrillator, something which was planned for her in the future anyway, and she has made a remarkable recovery. She was back home two weeks later to recover in her own surroundings which made this much easier for Grace.
When asked about the overall care Grace received, Ben said: “There must have been around 100 people involved in Grace’s care; the 999-call handler, paramedics, nurses, doctors and surgeons, there are too many to mention, everyone played a huge part in saving Grace’s life and the care she received, and continues to receive, has been outstanding, we cannot thank them enough.
“We’re still coming to terms with what happened, and we are trying to focus on the positives. Grace is doing well, she’s even back on the trampoline, but with the added security that the internal defibrillator is keeping track of heart rate and keeping her safe.
WHAT TO DO IN THE EVENT OF A CARDIAC ARREST.
A cardiac arrest is the most extreme emergency and happens when the heart stops beating in a normal way, preventing blood from pumping around the body. Knowing how you can help could save a life.
For someone in cardiac arrest they will die within minutes unless treated immediately with CPR. You can be performing CPR whilst waiting for the ambulance to arrive.
If you come across someone in cardiac arrest, just think DRS ABC:
DANGER – keep calm and check the scene is safe to approach
RESPONSE – shout “are you alright?” and shake the person’s shoulders
SHOUT FOR HELP – send someone for help and call 999
AIRWAY – tilt the head back gently to open the airway
BREATHING – check for normal breathing by looking at the chest to see if it is rising and falling or listening for abnormal sounds such as infrequent and noisy gasps
COMPRESSIONS – if the patient is not breathing normally, start hands only CPR pushing hard and fast in the centre of the chest.
If there is a defibrillator nearby send someone to get it. You do not need prior knowledge of how to use one as it will give clear instructions. It could save someone’s life.
How to do CPR:
“I
reading this is, try and learn CPR. Starting CPR within a minute or two of a cardiac arrest can help a person’s survival, thankfully Grace is living proof of this.”
1. Kneel at the side of the patient 2. Put the heel of your hand in the centre of the chest with the other hand on top* 3. Keep your arms straight and elbows locked 4. Push down hard and fast – twice per second
5. Let the chest come back up before you press down again
*Use one hand for a child and two fingers for a baby.
think my message to everyone
5
PARAMEDIC’S PIONEERING RESEARCH INTO WORKING NIGHTS.


Due to the nature of working in the NHS and other organisations, in many job roles there are periods of time where working night shifts is inevitable. Whatever your job role and whether you are a night owl, people have ways and means of coping with night shifts.
It is a topic that has sparked an interest in Paramedic Irvine Larrier who has worked many night shifts in his 10 year career. Irvine, who is based at Toxteth ambulance station is embarking on his second year of a Doctor of Philosophy (PhD) to discover the impact prolonged nightshift work has on a person.
Following extensive achievements at university including a diploma and a masters, Irvine decided on top of his full-time job as a paramedic, he would take on a PhD in his spare time. He says: “My research looks at what light and dark does to our bodies including hormone changes and how long increased exposure to cortisol can affect us. Through collecting data from several participants over a period – it is intended that the research will help understand the long-term effects doing night shift work can have on a person’s overall health and how we can improve on this.”
IRVINE’S STUDY WILL LOOK AT:
Circadian disruption: our bodies have a natural 24hour cycle compatible with daylight and during the night. Working night shifts and being awake at this time, can disrupt our bodies natural cycle. Irvine intends to find ways to mitigate the effects of longterm disruption to this cycle.
Cellular level: light and dark affects our hormone changes and tells our bodies to produce the right amount of cortisol and melatonin depending on our environment. Irvine will be looking at participant hormone levels to analyse the effects of long-term hormone imbalance exposure, which can adversely affect human physiology.
Telomere length: Telomeres are protective caps around our DNA called chromosomes and the length of our telomeres shorten as we age. Irvine will be looking at how long-term exposure to cortisol can accelerate the natural chain process and shorten these lengths earlier in life.
Irvine’s important research will help pave the way for future studies, we look forward to seeing the results of his innovative work. In the meantime, if you are working shift, here are some tips to help you through:
1. Eat small portions throughout the shift to help keep energy levels up.
2. Limit your caffeine intake – it can make it difficult for you to sleep when you get home.
3. Stay hydrated to help keep alert and energised
4. Keep busy – keeping moving if you can, it will help keep your blood flowing and your mind awake
5. Talk with your colleagues – who better to get you through than fellow night shifters?
6
Emergency medical technician using her IVF experience to educate fellow colleagues

In vitro fertilisation (IVF) is a type of fertility treatment where fertilisation takes place outside the body. It’s suitable for people with a wide range of fertility issues and is one of the most commonly used treatments available.
Lynsey McMahon, Emergency Medical Technician, is currently going through IVF. Lynsey’s IVF journey started in 2020. After two years of trying to get pregnant naturally, she went for some tests that concluded both her and her partner had unexplained infertility issues. They were advised to try IVF.
Since starting IVF they have done one cycle and unfortunately haven’t been successful. She explained “Although I was disappointed at first, I discovered a failed cycle gives you more information due to them getting to see how your embryos develop after fertilisation and what’s going right and wrong. We now have a bit of a battle plan in place for round two!”
IVF can affect people differently, both mentally and physically. Lynsey told us, “I was quite lucky with how I felt during my first cycle. Physically I felt fine, there was just a lot of appointments to keep up with. Mentally I was a little up and down at times as the medication is hormonal and obviously, I had disappointment at the end which was hard. But I’m quite a mentally strong person so you take the positives and what you have learnt from round one and move on.”
With around one in six couples in the UK having difficulty conceiving, IVF is a common treatment. Lynsey said, “As IVF is very much an evolving journey, it can be a rollercoaster at times. It can affect your life in so many ways so it’s important to look after yourself. IVF isn’t a one size fits all process so it’s important to reach out if

you need more support or someone to talk to. It can be a daunting process so just take it step by step.”
Lynsey is now using her experience to help NWAS staff. She is working with our health and wellbeing team to create a page on our wellbeing intranet site specifically for those going through IVF.
If you have any concerns or are experiencing infertility issues, please contact your GP who can advise and support you.
7
.
“What doesn’t kill me makes me stronger.”
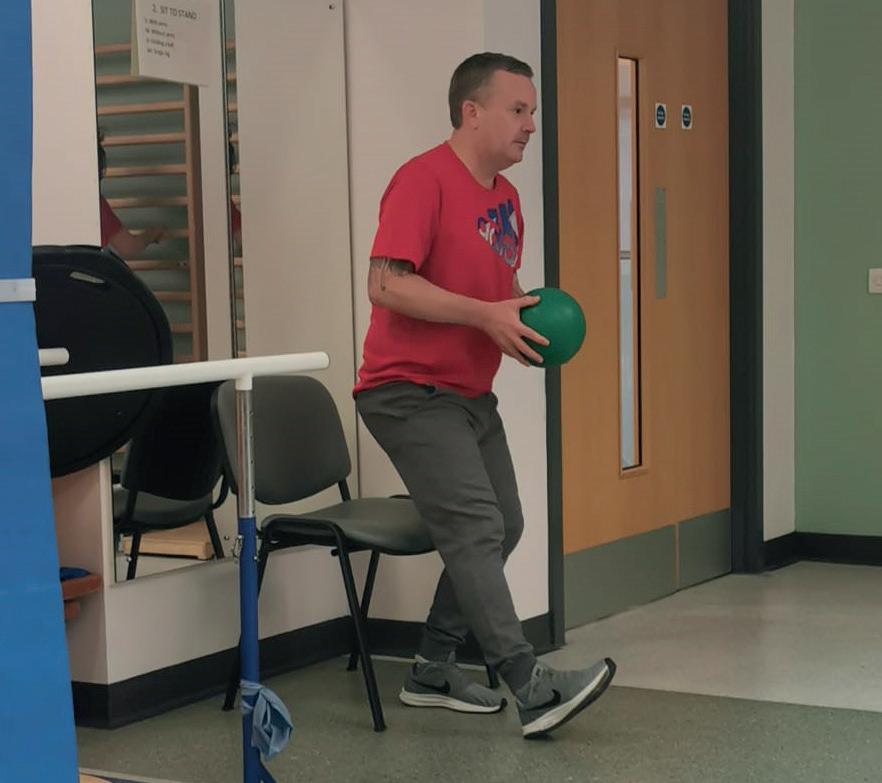
Salford-based Paramedic Paul Harvey has had an incredibly difficult 12 months – In July last year he was involved in a serious cycling accident after hitting a piece of debris in the road at high speed. He suffered traumatic head and potentially life-changing spinal injuries.

Thankfully Paul survived the accident and has been on a gruelling road to recovery ever since.
Your Call talked to Paul about his accident a year on from the life changing event.
“I had been cycling for over ten years before the accident and had worked my way up to owning an incredible bike, I used to call it my ‘Porsche of a road bike’. I went out
Despite wearing a helmet, Paul ended up in critical care for two weeks, unconscious after suffering from a bleed on the brain, a fractured spine, multiple facial fractures and three fractured ribs. He underwent spinal surgery and had metal rods placed in his mid-spine.
“From what I have been told, my colleagues who came to help me that day realised as soon as they had arrived to the scene how serious my condition was. I’ve been advised I was bleeding from my ears and highly agitated thrashing around. My colleagues, who didn’t know me at the time, made the decision to call in the North West Air Ambulance to provide enhanced pre hospital care.”
8
I don’t remember being in critical care for two weeks, but I do remember waking up once I had been moved from critical care unit to the trauma assessment unit. I had no idea why I was there and at the time I was sure I was being held there against my own will. I remember convincing myself that if I made it to A&E, I could find some colleagues and they would help me escape. I now realise that these strong thoughts and feelings were part of suffering a traumatic brain injury - I really wasn’t myself.
When the air ambulance arrived, the doctor made the decision to put Paul into a medically induced coma to protect his brain and his spine. After receiving vital treatment at scene, Paul was taken to Salford Royal Hospital by our ambulance crew.

“I went through all sorts of emotions, anger, upset you name it. I gave the hospital team looking after me a difficult time on one particular day and I was so aware of it that I apologised. My experience as a paramedic made me appreciate the things they did for me and I wanted them to know that this wasn’t me.”
Paul says it was the whole team of people that helped to save his life that day, from the person who called 999, to the call handler, to the ambulance crew, to the air ambulance doctor, the staff at the hospital, the consultants and the occupational therapists and physio team. An effort by all of them he will never forget.
“Without all the interventions, it could have been a completely different story for me. The fact that I’m still here for my family and I’ve got my life back – I want to thank them to the end of the earth.”
Although the road has been long, Paul has astounded his consultants and therapists with his continued strength and determination in his recovery. In addition, he started back at work early February this year – seven months after his accident.
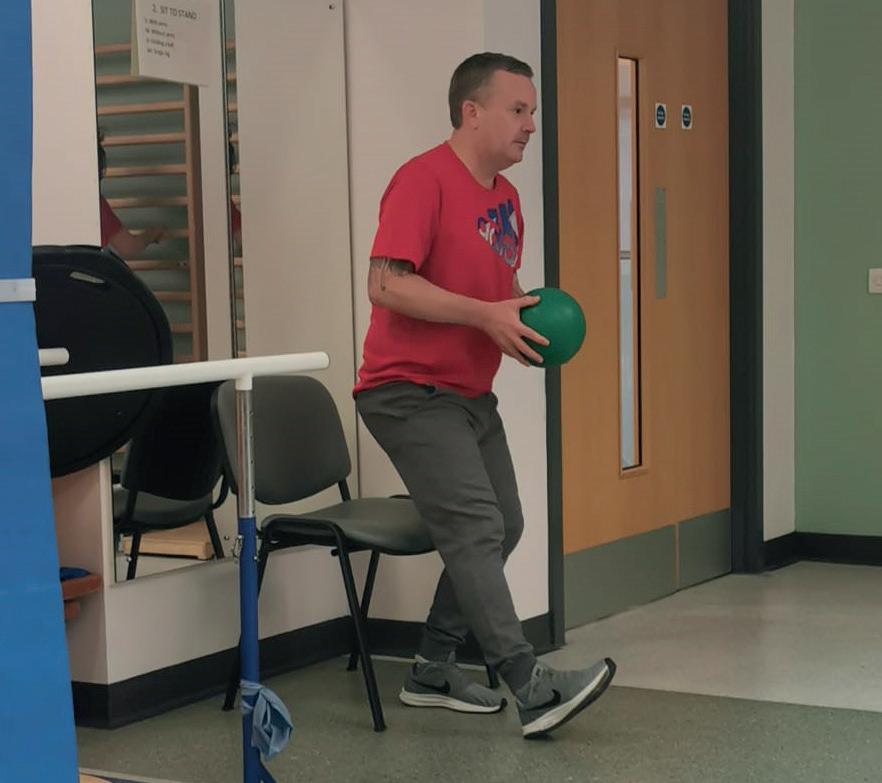
“My managers have been so incredibly supportive throughout this whole time, and I have returned now on alternative duties which has been a good introduction back into work. It is very different being station based, as I do like to be patient facing helping people, but I will just take each day at a time in my continued recovery.
“It is only in the last few weeks I have been able to run on the treadmill again – this week I managed to achieve a 2k run in under 13 minutes. I live by the motto - what doesn’t kill me makes me stronger.”
We wish you the best of luck Paul with your continued recovery.
“
9
“
felt like my blood was draining from my limbs.”
Anaphylaxis is a severe and potentially life-threatening reaction to a trigger such as an allergy. Triggers can often be foods, medicine, contrast agents such as dyes and latex. In the last year we have received over 8,000 calls relating to allergic reactions - for Stephen Lodge his trigger was a wasp sting.
In September 2021 Stephen was working on his garden renovation with a groundsman who was levelling the ground with a digger when he hit an underground wasp nest. The wasps immediately swarmed out from underground and started to attack the pair.
Stephen said: “I saw my groundsman dart out of the digger and run for the hills, I followed him as did the wasps. It was like something out of a horror movie.”
“I got about five stings on the back of my head and on my arms and within seconds I started to feel funny. My skin started to itch, and I felt immediate tightness in my jaw. I told my wife that I was having some sort of reaction and within two minutes I had gone grey. I fell to the floor and was being sick, my skin was bubbling, and masses of fluid started to come out of the blisters on my skin.”
Stephen’s wife immediately called 999 for an ambulance and in this time whilst on the phone to the emergency call handler, Stephen said his throat started to close. He continued: “I remember feeling like all the blood was draining out of my body and that my limbs were shrinking. I saw the ambulance crew turn up and the last thing I remember saying to my wife was ‘I really don’t want to die like this’, and I heard the male paramedic say; ‘His blood pressure is low’.”
John and Kimberley
John said: ”Stephen was obviously having an anaphylactic reaction and quite ill when we arrived. Thankfully he responded well to the treatment Kim and I gave him. It is great to hear he is doing well.”

Stephen talks about how this experience has changed his life: “I can’t go anywhere without taking my epi pen now, it must be with me permanently as wasps can crop up in all sorts of places.
“I used to love being outdoors but now I have a sense of nervousness and anxiety about my exposure. I used to wear shorts and a t-shirt and now in hot weather I still make sure I wear trousers and long sleeves to minimise surface area of my skin on display. My wife and I have not been abroad due to my fear of being outdoors. I have to have my windows shut in the house and in the car, it really has changed me, and I was never a nervous person.”
Stephen is now receiving immunotherapy treatment at hospital which involves injections of wasp venom extract under the guidance of a consultant which should help him to become resilient to wasp stings.
Ambulance crew mates, Paramedic John and Emergency Medical Technician Apprentice Kimberley, arrived on scene to Stephen and immediately administered shots of adrenaline which helped to bring him round.
took Stephen to Countess of Chester Hospital where he was monitored for several hours, and discharged with antihistamines and an epi pen to help him manage his allergy to wasps.
10
“It
WHAT IS ANAPHYLACTIC SHOCK?
Consultant Paramedic Steve Bell talks about what happens to the body in an anaphylactic shock and what should be done to help it.

“Most people are probably aware of the painful nature of a wasp sting, the vast majority of which are limited to mild symptoms around the sting site which subside naturally over hours or days. More severe reactions can cause more extensive swelling and may affect the entire limb and be associated with hives (a red, itchy, raised rash) on areas of the body away from the sting site requiring medication from a pharmacist or indeed input from the GP. However, the most severe type of reaction is an anaphylactic reaction, also termed a severe systemic reaction, which is what Stephen suffered.
“Anaphylaxis in this case is caused as the sting produces the release of mediators throughout the entire body but which particularly affect the respiratory and circulatory systems. Mediators are released after the activation of the body’s mast cells and include a range of complex chemicals including histamine, neutral proteases and proteoglycans. The effects of these chemicals result in swelling of the throat and mouth (and resultant difficulty in speaking or swallowing), together with difficulties in breathing, widespread flushing or rash and a sudden drop in blood pressure leading to collapse and unconsciousness; all symptoms which Stephen experienced.
“Anaphylaxis is a life-threatening condition requiring emergency treatment. 999 should be contacted and an ambulance requested making sure the ambulance service is told that there is a suspicion of anaphylaxis or a person having an anaphylactic reaction. Immediate first aid should include the administration of the patient’s autoinjector of adrenaline (commonly known as Epi-pens) should they have one as well as keeping the patient laid down where possible.
If additional auto-injectors are available, they can be given after five minutes if the patient has not recovered. I would recommend that the patient should always go to hospital for a period of observation even if they appear to make a recover from either the auto-injectors or after treatment by the ambulance service as there is a chance of delayed or additional reactions occurring after the effects of treatment have worn off.
“It’s great to hear that Stephen made a full recovery and has now been given autoinjectors should the worst happen again.”

11
Talking about dying is uncomfortable, but it matters.
Paramedic Michelle Waddington’s mum, Lynn sadly passed away in April 2020 after fighting lung cancer. It was a devastating and emotional time for her and her family which sparked a professional interest in Michelle. She has since taken on a research internship looking at end-of-life/ palliative care with our Research Team to inform future training and service improvements.


Michelle hopes that sharing her personal story will help those who may be facing the same harrowing situation now as she did back then.
“In 2017, my mum had had a cough for months, it was diagnosed as a chest infection, and she was given antibiotics which did not resolve it. She went back to the GP who sent her for a scan and that was when she was diagnosed with cancer.”
Michelle was with Lynn when the devastating news was broken and, on that day, they went home and had to break the news to Michelle’s sister, Heather. They sat and cried into the night, trying to get their heads around it.
“Mum could only have a specific type of chemo with eight sessions as the cancer she had was right by her heart so she couldn’t be operated on. Sadly, this did not help as the tumour had aggressively spread to her liver, and it was at this point we were told she was on palliative care.
“This hit my mum hard as she was devastated. She was a nanna and so close to my daughters and heavily involved in their lives, she wanted to see them grow up. Having that taken away from her was unthinkable. “
Lynn went through every emotion; she was angry, in denial and at her lowest point. Michelle and Heather had to hold it together for Lynn when they were with her, so she felt supported. They saved their tears for each other and helped one another through it.
Not long after returning, they all started to talk about Lynn’s dying wishes. Lynn had specific requests such as not having lilies at her funeral as she didn’t like them.
“We never pushed these conversations with mum. Once she got her head around what was happening, she took control of her funeral. Heather and I found we got great comfort in finding out what she wanted – one of the things was for us to have a ring made each containing her ashes, something she looked into herself.
“One evening, Heather, mum and I found ourselves sitting in mum’s conservatory talking about the funeral. We were looking at coffins and Heather was pulling up pictures of weird and wonderful options – some we found hilarious. It was the most bizarre feeling as we found ourselves laughing and crying simultaneously. It felt nice, and it lightened the mood. Mum picked the most beautiful coffin – she loved the beach, and it had a sunset beach theme.
“Mum sadly passed away in April 2020. It was devastating even though we were prepared. When we were going through her things, we found a book she had hidden and made with pictures of her favourite moments of all of us. At the end of the book, she had written a personal letter each to Heather and me, telling us how much she loved us and how proud she was of us. I can’t describe how amazingly happy and heartbroken this made me – it is something we will keep forever.”
Michelle is championing for people to open up and talk about dying as it matters.
“People are going through this right now, and it is traumatic. I can only say that starting a conversation about dying with your loved one means they have a choice in what will happen to them – something that was so important to my mum and us.”
12
Walking to boost mental health.
Physical activity can be one of the best factors to enhancing your mental wellbeing. The positive correlation between walking or other physical activity and mental health has been long known by general practitioners and mental health specialists. Even just a short burst of 10 minutes’ brisk walking increases our mental alertness, energy, and positive mood.
Anna De Stefano, 111 Quality Assurance Officer, has discovered this for herself and is now encouraging colleagues to use exercise as a form of mental health support.
Anna set up a walking group at the start of this year to combat isolation, a topic often raised and something many staff suffer from. She explained, “I wanted to create something which would be inclusive so everyone can get involved whatever their skill set, improve staff morale, retention, and relationships with each other, help staff who suffer with their mental health to get out, get some fresh air and make them feel that slightly bit better.”
Anna started the group small by inviting all North West 111 bases in the hope to cement a team ethic.
She added, “The group supports staff who may feel lonely at work to socialise with others and to make new friends. I have experienced myself as a health advisor previously, it can be lonely. You can sit there all shift and speak only to the people who are at the end of the phone.”
What started off with just a few members has now grown into a fully-fledged walking group, with members of the senior membership team even getting involved. She told us, “Our recent walks have included health advisors, quality assurance officers, team managers, clinicians, clinical duty managers and service delivery managers. I genuinely couldn’t be any happier with the staff from all departments getting involved.”

The 111 team walks take them all over the North West. So far, they have explored Entwistle and Wayoh Reservoirs, Delamere Forest, Pennington Flash and Borsdane Woods. They have more planned and with summer on the horizon, they are set for an enjoyable few months.
If you are wanting to improve your physical activity but concerned with any ongoing health issues you may have, consult your GP.

13
ADHD - A PARENT’S PERSPECTIVE.
Katie Ridge works behind the scenes in our Project Management Office, she passionately champions neurodiversity as her nine-year-old son was diagnosed with attention deficit disorder (ADHD). We talk to Katie to find out about the journey her family has been on and how she struggles with the judgement that is so often passed around ADHD.
“My son was nicknamed by his nursery from the age of 18 months as the ‘whirlwind’. As first-time parents we embraced this as an accurate description of our hyperactive, speedy, widely emotional little boy and rode the rollercoaster of extreme ups and downs believing it was normal for parenting to be this challenging.

It wasn’t until Eddie started school and found it enormously difficult socially and emotionally to interact with the class and display appropriate behaviours that we started to see that maybe his behaviours weren’t ‘normal’.
“Sadly, we didn’t gain a full understanding of how we needed to manage Eddie until he was diagnosed with ADHD in March 2020, at sevenyears-old, after four years of referrals to several different services, positive parenting classes, calls to the head teachers office for reprimands over behaviour, threats of being banned from wrap around childcare, violent outbursts, anger, aggression, and limited support. All of this contributed to the decline of my mental health as anxiety, paranoia and stress slowly amplified as I doubted my parental abilities more and more.”
14
Katie says Eddie’s diagnosis was a welcome relief and opened the door for her and her husband to get the support they desperately needed as a family. They were finally able to understand what Eddie was going through and that he is not just a ‘naughty child’ as he is so often judged to be.


“As a parent I have particularly struggled with the aspect of judgement and misconception when it comes to ADHD. Unfortunately, it is not something that is widely understood, even in schools where it is not considered a priority for funding in the development and training of teachers. It’s an uphill battle for most parents trying to ensure their child is treated fairly and equally taking into consideration their condition. The main thing I have learnt from all of this is to be more understanding. You never know what that person or family are going through, or what difficulties they may be dealing with. Before going to that place of judgement it is important to shift your mind set, stay neutral, be curious and ask yourself ‘what else could be true’ in that situation.
“I have learnt so much in the last two years about ADHD and this learning has opened my eyes to the world of neurodiversity. Eddie’s ADHD is a part of him, he may need adjustments putting in place to support him in life, but in response to this he brings so much to the table. He is intelligent, inquisitive, can hyper focus intensely on things that interest him, is highly passionate and has a strong sense of justice. He is a loyal and fiercely supportive friend, highly competitive and has a knowledge bank of facts at his disposal.
“As a parent of a child with ADHD my days are usually intense, very loud, involve lots of repeated instructions and require lots of patience. They are full of surprises, I learn something new every day (usually a random interesting fact that Eddie has read or heard somewhere and will remember for life), the ups and downs are very much still there but they are understood and are managed. Eddie fully understands his ADHD and is proud to be an ‘Adventurous Determined Hyper-focused Dreamer’ and I am proud that he has opened our eyes, made us more understanding, more compassionate and more empathetic as a result.
“There are a lot of ups and downs looking after a child with ADHD, lots of unknowns and last-minute dashes to school to do the pickup early due to one incident or another, lots of meetings in the headteacher’s office and catch ups with the SENDCo (Special Education Needs Coordinator), therefore lots of flexibility is needed. NWAS and my team have been amazing at supporting me with this. My work pattern is flexible to fit around any lastminute changes, my line manager is fully supportive and understands, I can talk openly and honestly about the bad days as well as the good and how it might be impacting my workday. This has been instrumental to my mental health and in allowing me to continue bringing my full self to work and getting the job done.
“Had I not been on this journey I would not be the person I am today. Prior to Eddie, I was the person judging the parents with the ‘naughty’ child having a meltdown in the supermarket.
I was the person who thought ADHD wasn’t real and was an excuse for bad behaviour and I was the person that thought SENDCo got involved at school when parents weren’t doing something right - all of which I am ashamed to admit! Eddie has made me a better person, I have grown and developed so much and look at the world and the people in it completely different because of him, of which I am truly grateful for. I am more compassionate, more understanding and more open to people’s unique needs. It’s just a shame it takes lived experience to change our view of the world.”
For anyone going through something similar, don’t be afraid to speak out, fight for your child’s differences and most importantly give yourself a break, be kind to yourself.
15
Saving time and staying smart.
We know our staff are an intelligent bunch, but did you know our buildings are too?
Kendal station is the smartest of them all, literally, as it has been transformed using new technologies, digital systems and solutions to become a ‘smart station’.
As one of the smaller stations, it holds 140 staff, 12 ambulances and a range of challenges including its remote location and close links to the Lake District, which sees high demand during the summer.

Since July 2020, the station has been the focus of a new smart station pilot scheme to transform the hub after an idea, born out of our Clinical and Digital Innovations Team.
Matt Dugdale, Head of Clinical and Digital Innovation at NWAS, said: “We decided on Kendal as our test site after finding there were lots of inefficiencies and wastage in terms of how staff would flow through the building, there was lots of paper used around the site and some issues with security as often generic key codes were shared. With its good connections to local health care partners, we decided Kendal was a really great place to start.”
In a short space of time, the project has seen some key results including a 70% saving on energy use thanks to a new ultra-smart and energy-efficient lighting system. The team has also seen a saving of 49 hours over four months on staff time because of a new access control system that allows a clinician to swipe their ID card to open and close the site’s garage rather than using a traditional mechanical chain.
In addition, an interactive digital wallboard has been introduced to reduce paper wastage across the site. The board allows staff to find different information such as news bulletins and staff briefings and the ability to email the information direct to their personal inbox
Matt added: “Our staff co-designed the changes with us and feel proud that they were part of the process - they feel that this project has really put Kendal on the map. In time, we hope to roll out these innovations across the trust.”

16
ABUSE YOU CAN’T IGNORE.
Paramedic Tammy Edwards paints an uncomfortable picture as she shares her experience of being abused at work.
She feels the regular abuse she receives from some patients is part of the job. However, there was one experience five years ago that almost made her give up the job she loves.
While working as a solo responder, she was called to a male patient whose mother had expressed concerns about his health. During the examination, the patient became agitated and angry and started to assault his mum. As Tammy tried to drag her to safety he started punching and kicking her, until she managed to escape from the house.

“I didn’t suffer much physical harm just a few bruises, but the emotional impact was huge”, Tammy tells us, “I lost all my confidence, I started to think what if one day I am not able to come home to my children. The next day I handed in my notice.
“However local management was very supportive. After a three-hour meeting, it was decided I would no longer work as a solo responder, and I was placed with a crew mate on an ambulance. I also started to see a psychotherapist, helping me deal with the trauma.”
We supported Tammy in bringing a prosecution against her attacker, although he only admitted responsibility on the day of his trial. Unfortunately, this isn’t the only example of abuse on the job.
“I’ve also had a knife pulled on me at the front door,” Tammy says, “but most of it is quite low-level driven by drink, drugs or mental health issues. It’s a patient swearing or calling you names. It shouldn’t be that way.
“I’ve just got used to it and I ignore it. You build up that much of a tolerance to it, recently, I only realised a patient threatened to kill me when my colleague pointed out their behaviour in an effort to make them realise how unacceptable it was.
“Having said that, I’ve just been through a period where it feels constant and that does get me down.”
Earlier this year the Association of Ambulance Chief Executives launched a campaign to highlight the violence and abuse ambulance service staff receive every day with the hope they can work without fear.
More information is available at aace.org.uk/vaa or search #WorkWithoutFear on Twitter.

17
HELPING TO TACKLE VIOLENCE AND INSPIRING FUTURE PARAMEDICS.
Street violence and knife crime has been hitting the headlines all too frequently in recent years as more and more young people are getting caught up in the devastating impact it is having across communities within our towns and cities in the North West.
With the increase in ambulance staff attending these type of fatal and distressing incidents, Advanced Paramedic Kirsten McDermott, through her work with the Greater Manchester Violence Reduction Unit, took the opportunity last autumn to partner up with the charity StreetDoctors to deliver their StepWise programme to students aged 17 to 18 at Oldham College.
The programme was created by StreetDoctors and teaches young people emergency life-saving skills with a focus on injuries sustained from stabbings. The course also provided young people with information about their legal rights if they get caught up in a violent situation,

builds their social and emotional skills and by the end of the course they receive a first aid at work qualification so they can then to deliver first aid training to their peers.
The 10-week course was funded via proceeds of crime through Greater Manchester Police and was the first time StreetDoctors had provided the course outside of London.
Kirsten recruited a team of fellow paramedics and emergency medical technician volunteers to help deliver the sessions at Oldham College and explains why it was so important:
“This was the first time the ambulance service had been fully involved. Normally it is student doctors or student nurses that volunteer but when StreetDoctors pitched this, I said it’s a really good opportunity for the ambulance service to be promoted and actually assist and have that community engagement with young people.
18
“Not only were we giving them life-saving skills of how to put pressure on wounds if someone was stabbed but we were able to break down some of the concerns that they have if someone was stabbed, such as would they get in trouble. We were able to answer real questions they had but also teach them what they needed to know to keep themselves and their friends safe.”
Scott McAughtrie was one of the paramedics that decided to volunteer alongside Kirsten to help teach the course each Wednesday afternoon in Oldham. He was struck when talking to the students at just how many of them knew others that carried a knife and how tragically many had already been caught up in violence of some kind. He explains why he decided to take part in teaching the course:
“Street violence obviously is a big thing, no matter where you are in Manchester. Knife crime is quite high and just having the chance to make a difference to a group of young adults, with my knowledge, that can only better them for the future.”
The students that took part in the course were studying either health and social care or uniformed studies and so did already have an interest in a career in the NHS or with the police or fire services. However, throughout the programme they learned more about the professional work of paramedics and as they practiced on realistic prosthetics depicting various types of wounds and scenarios. As Scott says, this helped to ignite their imagination to consider a future career in the ambulance service:
“Just showing them what we do from the inside changed people’s minds. They wanted to be paramedics, they realised what such a good job it is and the satisfaction we get from caring for people.
And we could see that coming out in them as well because they were showing their caring side, even though it was a dummy on the floor or even one of their peers on the floor putting a bandage on them, they showed their caring nature. It wasn’t just thrown on them and they weren’t just there for the time, they wanted to learn.”
At the end of the course the students graduated with a special ceremony and Kirsten says why she felt so humbled and proud to be part of it: “It brought back to me why I wear this uniform and why I do my job. It’s not just necessarily about saving lives but inspiring young people to make better choices for the future and stay away from violence. We’re not going to stop it but hopefully we can give them the tools to make better choices for themselves."
Kirsten and Scott, along with a team of other NWAS paramedics and EMTs are continuing to engage with young people by visiting schools and colleges with the GM Navigator project. Teaching and supporting young people with those first aid skills and delivering prevention activity.


19
Meet the supervisor making his colleagues cry for the right reasons.
Ryan Flynn is a supervisor in our Liverpool Emergency Control Centre (EOC) – we have three EOCs across the North West and its where all 999 calls are answered. He has been in Team NWAS for just over two years, starting as an emergency medical dispatcher answering 999 calls. It is fair to say it hasn’t been the easiest of introductions to the service for Ryan or anybody else who joined us in the last two years. But in that time, Ryan has handled every type of call imaginable from a cardiac arrest to a birth.

With a background in the Navy, Ryan was unsure about starting life in a desk-based job after being a sea boat coxswain – in his words ‘the jobs are worlds apart.’ He joined our team with an open mind and has never looked back.
“It’s a hands on job in a different way, it is a hard job, there is no two ways about it. There were times where I questioned if I could do it, you have one bad call after another but the support we give each other is phenomenal and it keeps you going. We are all on the same boat, all lived and breathed the same nightmares, and it brings you closer together.
RYAN’S POEM.
Serving the Queen Facing the screen Living the dream Wearing green Ready to intervene When the ambos on scene It’s mainly a fall That’s no problem at all Sometimes we’re in tears We’ve heard it all in our ears Working together And being at our best Making a difference Getting hands on chest Most importantly of all Confirming the address Calming down callers In times of distress Exceptional patient care That’s how we roll
Not all heroes wear capes Just headsets in control
Always ready for a shift, focussed and raring Empathetic, dedicated, willing and caring Our patients are always in the centre of our heart From the minute we meet until the minute we part Times are hard and friends are few But we are Team NWAS and we’re here for you!

20