













From advancing therapies that improve quality of life for patients with lung disease – to pioneering surgical approaches for the most complex conditions – physicians at the Temple Lung Center are developing new standards of care that are being adopted across the globe.
It’s this dedication that propels our cutting-edge research forward, translating discoveries into novel treatments for patients everywhere.
To improve the lives of those with lung disease, it takes the nation’s leaders in lung care and thoracic surgery.


Philadelphia County Medical Society
2100 Spring Garden Street, Philadelphia, PA 19130 (215) 563-5343
www.philamedsoc.org
EXECUTIVE COMMITTEE
Walter Tsou, MD, MPH President
David A. Sass, MD, FACP President Elect
John M. Vasudevan, MD Past President
Brian A. Hannah, MD, MSc Secretary
Sharon Griswold, MD Treasurer
Victoria Cimino, MD, MPH
Cadence A. Kim, MD, FACS
William King, MD
Pratistha Koirala, MD
Dale Mandel, MD
Elana McDonald, MD
Max E. Mercado, MD, FACS
Gillian Naro, MD
Natalia Ortiz, MD, DFAPA, FACLP
Dhruvan Patel, MD
FIRST DISTRICT TRUSTEE
Michael A. DellaVecchia, MD, PhD
EXECUTIVE DIRECTOR
T.J. Huckleberry www.philamedsoc.org
Editor Kevin Bezler
The opinions expressed in this publication are for general information only and are not intended to provide specific legal, medical or other advice or recommendations for any individuals. The placement of editorial opinions and paid advertising does not imply endorsement by the Philadelphia County Medical Society. All rights reserved. No portion of this publication may be reproduced electronically or in print without the expressed written consent of the publisher or editor.
4 Paul Offit & Ezekiel Emanuel: Defending the Physician’s Oath in Skeptical Times
10 The Philadelphia County Medical Society presents the Installation of Walter H. Tsou, MD, MPH, 164th President, and Annual Awards Night Presentations at the Philadelphia Country Club, June 21, 2025
18 Meet Dr. Walter H. Tsou, 164th President of the Philadelphia County Medical Society
20 Farewell: Q&A with outgoing Philadelphia County Medical Society Executive Director Mark Austerberry
21 Big Shoes to Fill
22 A New Model for Improved Maternal Outcomes: How to Increase Care Access and Quality in Diverse Urban Environments
24 Strengthening Care, Growing Impact: Q&A with Michael Young, President and CEO, Temple Health
26 250th Anniversary of the US and the History of Medicine
28 Story Slam: From Center City to the Cancer Center, and Back
29 PCMS at the Phillies!
30 Ways YOU Can Get Involved in PCMS



Cover: Bust of Hippocrates, Ancient Greek Physician, Father of Medicine

Philadelphia Medicine is published by Hoffmann Publishing Group, Reading, PA HoffmannPublishing.com | (610) 685.0914 FOR ADVERTISING INFO CONTACT: Ad Sales • Sales@Hoffpubs.com • 610-685-0914 x715


Monday, September 15
6:00 PM - 8:30 PM
College of Physicians of Philadelphia 22nd Street, Philadelphia, PA 19103



Monday, September 15
6:00 PM - 8:30 PM
The College of Physicians of Philadelphia 19 S 22nd Street, Philadelphia, PA 19103
is designed to bring physician and trainee members of the Philadelphia and College of Physicians of Philadelphia together over food and drink to expert panelists on how to use one's medical degree to advance their goals in leadership/administration, and politics. Attendees are welcome to bring a guest.
he practice of medicine is a challenge at every level of experience, and fortunately for the physician, it is bound by an Oath, epitomized by Primum Non Nocere: First, Do No Harm. The Philadelphia County Medical Society (PCMS) organizes physicians to convene, debate and help us determine the best path forward to serve our patients and society by first, doing no harm. Our Philadelphia physicians may face a formidable year of challenges at the local, state and federal levels as any year since our convening in 1849. In 2025, we watch with apprehension, the political turmoil of a new administration. This might be a great moment to look up from our individual practices, to consider the social, economic and political forces impacting our patients and our profession, and grasp for a common understanding within organized medicine.
The Doctors Lounge series is designed to bring physician and trainee members County Medical Society and College of Physicians of Philadelphia together socialize and learn from expert panelists on how to use one's medical degree business, public health, leadership/administration, and politics. Attendees are
Medical Society | stat@philamedsoc.org http://philamedsoc.org registration is required. https://philamedsoc.org/events code.
Who would have thought that the intense political debate around healthcare expansion in the 2000s, that resulted in the passage of the Affordable Care Act (ACA), would be seen as a bureaucratic bump in the road? Who imagined the fear of the COVID-19 pandemic that ensued in 2020 or that the relief and accomplishment the medical community felt as the pandemic ended would be overwhelmed with the backlash of skepticism, political fury and public rejection of the scientific institutions and medical administration? Societal whiplash is something we did not learn in medical school. In Philadelphia, we have a great tradition that goes back to Benjamin Franklin and Benjamin Rush: dialogue and debate. In 2025, Philadelphia doctors in organized medicine don’t have to cross oceans or continents for wise counsel; we can look across the Schuylkill River to two great public champions of healthcare.
Free to attend, but registration is required. Register at https://philamedsoc.org/events Or scan the QR code.
Philadelphia County Medical Society | stat@philamedsoc.org 215-563-5343 | http://philamedsoc.org
Dr. Paul Offit is the Director of the Vaccine Education Center at the Children’s Hospital of Philadelphia as well as Professor of Vaccinology and a Professor of Pediatrics at the Perelman School of Medicine at the University of Pennsylvania. He is currently a voting member on the FDA’s Vaccine Advisory Committee and previously served on the Advisory Committee for Immunization Practices to the Centers for Disease Control (CDC). He is also the co-inventor of the rotavirus vaccine, RotaTeq, recommended for universal use in infants by the CDC in 2006 and by the World Health Organization (WHO) in 2013.
Dr. Ezekiel Emanuel is the Vice Provost for Global Initiatives and Professor at the University of Pennsylvania. An oncologist and world leader in health policy and bioethics, he is also a Special Advisor to the Director General of the WHO, Senior Fellow at the Center for
Progress, and member of the Council on Foreign Relations. He was the founding chair of the Department of Bioethics at the National Institutes of Health (NIH) and held that position until August 2011. From 2009 to 2011, he served as a Special Advisor on Health Policy to the Director of the Office of Management and Budget (OPM) and National Economic Council. In this role, he was instrumental in drafting the ACA. Emanuel also served on the Biden-Harris Transition Covid Advisory Board.
The PCMS Editorial Board sat down with both eminent defenders of medicine to begin a dialogue that will continue at the Doctors Lounge conversation, September 15, 6:00 PM at the College of Physicians. For more information, go to the PCMS website: www.philamedsoc.org.
PCMS: The American healthcare system is the most complex in the world by far, with private insurance, public insurance, employer insurance and government insurance, layered on top of private, public and government institutions; served by forprofit, nonprofit, and government health systems, hospitals, medical groups and individual providers. When you undertook advising the White House on rationalizing and expanding healthcare delivery, what were you trying to do?
Emanuel: I like to say that there are five goals to a healthcare system. There’s universal coverage at reasonable costs with consistent high quality, with minimal disparities and high satisfaction by patients as well as physicians and other providers. We were far from that in 2009 when we began on the ACA, but we did make a lot of progress. We both brought the number of uninsured down from almost 17% down to 8% and consistently, as a percent of GDP, healthcare spending plateaued at 17.5%. But the last few years and looking forward, a lot of that’s gonna unravel. The “Big, Beautiful Bill” supposedly is going to throw 12 million people off of coverage. We’re going to have another big group of people lose coverage because the extra subsidies for the exchanges are going to go away. So, we’re going to lose a lot of people, maybe even half of the gains that we made from the ACA.
When you’re ready to make a difference, we’re ready to help
We are proud to support Philadelphia County Medical Society by advising them for more than a decade.

Nash Wealth Management Group
Merrill Lynch Wealth Management
1200 Howard Blvd. Suite 300 Mount Laurel, NJ 08054
856.231.5575
Merrill Lynch, Pierce, Fenner & Smith Incorporated (also referred to as “MLPF&S” or “Merrill”) makes available certain investment products sponsored, managed, distributed or provided by companies that are affiliates of Bank of America Corporation (“BofA Corp.”). MLPF&S is a registered broker-dealer, registered investment adviser, Member SIPC and a wholly owned subsidiary of BofA Corp. Investment products:
Are Not FDIC Insured Are Not Bank Guaranteed May Lose Value © 2023 Bank of America Corporation. All rights reserved. | MAP5448947 Vault-BA1KP6 | MLWM-243-AD 470945PM-0323 | 03/2023
Similarly, we’re seeing a lot of price pressure on health care spending, and we know that our quality is inconsistent. That’s a charitable way of putting it—it’s poor, especially when it comes to things like prevention and management of chronic illness. What really frustrates me most of all is we have no path to achieving any one of those five goals. We’re not going to get to universal coverage. We’re
not getting reasonable cost control, much less bring it down. And the quality, there’s no plan for improving quality, especially around chronic disease, which is the main problem facing Americans. And that’s, I think, very depressing. I like to call the original sin of the American healthcare system, complexity. There’s complexity when it comes to prices. There’s not a price, one price for anything, right?
Paul Offit & Ezekiel Emanuel: Defending the Physician’s Oath in Skeptical Times continued from page 5
There are multiple prices. There’s a price for Medicaid and a price for Medicare and a price for every different insurance company. And every different drug has a price. So, it does make it very complicated. And one of the things if you study this, is complexity adds administrative costs and therefore drives costs up. It adds frustration on the behalf of people, but it also adds a lot of gaming of the system.
PCMS: This is the middleman syndrome. I think any business, if you’re trying to bleed money and line your pockets, what you need is middleman, middleman, middleman.
Emanuel: That’s a hot point. And almost all the profits are going to middlemen. So that’s a huge problem. And what makes me upset is that I don’t see a solution given our current system. And that’s a big frustration of mine.
PCMS: Dr. Offit, one of the things that clinical physicians feel confident we’re practicing is a standard of medicine based on neutral scientific data; we’re standing on the science. As we navigate bureaucracy and prior authorization procedures, we
are looking at a common reference of evidence-based medicine. You have sat on two of these standard keepers: the Advisory Committee on Immunization Practices (ACIP) and the FDA vaccine advisory committee. These and several of our other healthcare standards boards are being disbanded or reconstituted with little input from physicians and scientists. Are we able to fight and advocate for these civic governmentally supported, but academically constituted, these organizations? Is there a way for us to be able to advocate to maintain their integrity?
Offit: I think the thing that’s most upsetting about what’s going on now is that science, I think it’s losing its place as a source of truth. People are just simply declaring their own truths, including scientific truths. I think that people like Robert F. Kennedy Jr., who has for 20 years been an anti-vaccine activist, science denialist and conspiracy theorist, is now the Secretary of Health and Human Services. So, he is no longer shouting his misinformation and disinformation from the sidelines. He is making policy.
So, what did he do? Very quickly after assuming his position, he fired all 17 members of the ACIP, people who had expertise in virology, immunology, public health, statistics, epidemiology, who were clinicians, would advise people about vaccines, would see people with vaccinepreventable diseases.
And he’s now replaced them with initially eight, now seven people who in many ways are like-minded, who have either published bogus papers about vaccine harm; have served as an expert witness in the midst of lawsuits against pharmaceutical companies against the HPV vaccine or the Mumps vaccine; or are members of antivaccine groups like the National Vaccine Information Center, it’s bad.
PCMS: What happened?
Offit: What he did at that last meeting is he had Lynn Redwood, who was a member of a group called Safe Minds, now a member of Children’s Health Defense, which is his anti-vaccine organization, present data. You basically had an antivaccine activist presenting data to the ACIP before a vote, and normally before
Do you dread the driving conversations with older drivers and their families? We can help.

Introducing the Beyond Driving with Dignity program
Older drivers and their families appreciate the human connection established during the session, as we help them through the complex and sensitive issue of driving retirement.

Randy Reardon, Certified Senior Advisor 888-299-9960
randyreardon@seniorcareauthority.com seniorcareauthority.com/neofphilly
a vote, you have something called ETR, Evidence to Recommendation, which is to say that her talk should have been reviewed by subject matter experts, and it wasn’t. And so, she gave a talk that was full of misrepresentations and didn’t include all the studies that exonerated thimerosal as a cause of harm. And then the vote came and by a vote of five to one, they had an anti-science vote against thimerosal in the influenza vaccine. And this is just step one. I think this was just testing to see where the weaknesses are.
PCMS: Where do you think this path will lead?
Offit: I think RFK Jr. is going to mess around with the Vaccine Injury Compensation Program (VICP). He’s already hired an Arizona-based law firm to do that, and if you really want to bring vaccines to its knees in this country,

meaning bring pharmaceutical companies who make vaccines to their knees, do that, ‘cause that’s what happened in the 1980s when we went from 18 companies that made vaccines in 1980 to four by the end of the decade.
PCMS: Wow. So, doctors understand that the VICP is this kind of umbrella that allows vaccines to be developed and administered, yet if there is an adverse event, it allows the patient to be compensated, it allows the doctors to report the events. It’s one of these systems that’s very similar to the way that aviation has a system that tries to quickly report and solve problems rather than pursuing blame and litigation and yet preserves the rights of anyone harmed. Dismantling the VICP would be devastating to the progress on protecting the population with vaccination. We are really in the midst of
What’s Beyond Driving with Dignity?
A trained professional facilitates an in-person session in your patient’s home. We get to know the person while gauging their cognitive, physical and emotional abilities. Directly following the session, we offer our recommendations to the older driver followed with a detailed report of our findings and recommendations.
The cost is just $450
Ask about our Senior Living Placement Solutions where we work with the family to find appropriate senior living arrangements.
this incredibly divisive campaign, what do we do about this very frustrated political moment in time?
Emanuel: Well, I think in the short term, there’s not going to be a lot to do. I think a lot of bad things are going to happen to people. I think in the longer term, our obligation is to think about how we want to re-think and re-imagine government. Social Security is 100 years old; Medicare and Medicaid are 60 years old. Most people, when they get to be 60, things begin to break down. And the same thing is true for institutions, especially institutions that you’ve sort of built on over the years. You get encrusted. And I think that the big obligation we have now is not to say, we’re going to just keep things as they are. We have to reimagine what we want and try, in that process, to make things both more efficient and
continued on next page
continued
Paul Offit & Ezekiel Emanuel: Defending the Physician’s Oath in Skeptical Times continued from page 7
simpler. I think one of the things many people who voted for Trump wanted, and one of the reasons is they just think the government is ossified or sclerotic, and they want it to improve. And it’s happening at some places, but we’re not having a comprehensive rethink. I think the public, not necessarily politicians, but the public are open to a lot of that rethinking. The problem is that we just don’t have a structure that facilitates this rethinking. Congress is at an impasse with itself, can’t really do much. And I think that’s created a lot of problems that aren’t expeditiously being fixed. So, I think that’s a major issue. Medicaid is going to be hurt really bad, and we don’t have the votes to reverse that, certainly at the moment. So how do we imagine going forward that we can fix it?
PCMS: Dr. Offit, what do you think?
Offit: I think in some ways the COVID pandemic did give birth to some of this distrust. I think in 2020, when we didn’t have anything, we didn’t have monoclonals or antivirals or vaccines till the end of the year. So, what did we do? We shuttered schools, we closed businesses, we restricted travel, we social distanced, quarantined, tested, and I think there was a segment of the population that felt that this was massive government overreach, especially with regard to how long we closed schools or how long we closed businesses. And then the following year when we had a vaccine, you couldn’t really go anywhere. You couldn’t go to your favorite bar, restaurant, sporting event, place of worship unless you had that vaccine card, and people were fired from their jobs. And again, the feeling was that it was done in a dictatorial manner, that we didn’t really include people in that sort of decision. This is what you’re going to do. And in many ways, I think it fueled what is now so-called medical freedom movement, meaning don’t tell me what to do. I’m gonna decide what to do. You have RFK Jr. sort of getting up on TV the other day
and no, don’t trust your experts, just trust yourself. And that’s the tension to me. I mean, public health at some level means you have to care about your neighbor. You have to care about the people you come in contact with. Medical freedom is, I’m gonna do whatever I want, period. You don’t tell me what to do. If I wanna have the right to catch and transmit a potentially fatal infection during the pandemic, that’s my right. And you hear him say that. Even in the face of a measles epidemic this year, which is bigger than anything we’ve had in the last 33 years. We’ve had two healthy little girls die of measles. That’s the first measles deaths in this country in a child since 2003. It’s bad and it’s only going to get worse. And yet you have him up there saying things like, it’s your choice. It’s personal choice.
And I don’t know, I just remember back in California when they had their measles epidemic in 2014, 2015.There was a state senator named Richard Pan who introduced Senate Bill 277 to eliminate the philosophical exemption in California. And the anti-vaccine people hated it. But there was this little boy whose name was Luke Crowett that would show up at these meetings and he had leukemia. And he put him on a stool so he could reach the microphone, and he would look at the anti-vaccine people and he would say, my name is Luca, I have a leukemia. I can’t be vaccinated. I depend on you to protect me, don’t I count? And I think from the answer, from the medical freedom movement motto, it’s no, you don’t.
PCMS: I think this does kind of remind us, as physicians that we are, as much as any profession, besides divinity, we’re one of those few professions that has an oath that we have a mission, a purpose to take care to do no harm. And it’s not just because we should, it’s because we must. We vowed to do it. So, I think that in this era, the way Dr. Emanuel was describing it, we might have to reset.
Emanuel: I was sitting next to a very wise person who works in Washington, and he said, “Look, you can’t take every one of Trump’s provocations and RFK Junior’s provocations.” You have a limited number of rocks in your bag, and so you have to figure the biggest high value thing you can do is to rally people. And I think Dr. Offit is probably right, (fighting for) thimerosal (in vaccines) is small potatoes, not worth fighting over. On the other hand, the VICP is the kind of thing that I think would be a disaster. Damage could be done. But I think that’s the kind of thing where we have to draw a line.
PCMS: So, what do we tell our fellow professionals? How do we advocate for our profession and the work we do? How do we convince the government, this needs to be paid for? How do we convince the citizens? What do you think?
Emanuel: (laughing) I think one thing is that doctors aren’t necessarily experts in health policy. We are experts on what we can do. And I do think it’s important for doctors at this moment to argue for the good of the system and the good of the people and population. One of the things that worries me is that there’s going to be a lot of cuts and worrying about the cuts to our salary, which are real, don’t get me wrong.
We have to elevate it to the next level of really trying to protect our patients. And we do know that when people become uninsured, mortality goes up. When we can’t give prevention, cost and mortality goes up. As Paul pointed out, we’ve had more deaths in the last nine months from measles than we’ve had in 25 years. No, it’s not a lot of deaths, but there’s a lot of hospitalizations and other problems going on, and a lot of waste of money. None of that was necessary. We have to emphasize the fact that there are real costs to this, and there are real costs both monetarily, but also for the public in terms of their health, the health of their children.

Roxborough Memorial Hospital
Bariatric Surgery and Wellness Program
Transform your life with Roxborough Memorial Hospital’s Bariatric Program. Our expert team offers personalized care, innovative treatments, and a supportive community to help you achieve your health goals. Start your journey today!
Medical Office Building, 5735 Ridge Ave., Suite 105 Philadelphia, PA 19128 | (610) 277-6131
PCMS: But what do you say to the young docs who are out there trying to actually get the next vaccine going, who are trying to get the existing vaccines disseminated and out to all the folks who need them across not just the U.S. but the world?
Offit: I think people make a calculation when they choose to get a vaccine and social media has made information much more fragmented and it’s hard to get the notion out there that vaccines are safe and effective, and so for people who hear that notion that vaccines cause autism or asthma or eczema or long-term chronic problems, they’re thinking, all right, I’ll take my chance with measles, you know which is at least a short-term illness and that way, I won’t have to suffer these other chronic long-term problems. It’s a bad calculation because the measles vaccine doesn’t cause those other problems. And that’s what you’re dealing with. Those two little girls who died in West Texas, a

six-year-old and an eight -year-old, those parents still didn’t think they made the wrong decision because they felt that if they had given the vaccine, they may have had to suffer something long-term. And I know it sounds impossible to believe that people still didn’t think that they made the wrong decision there. But I guess part of it is that, I mean, your number one job is to protect your child. And the worst thing that can ever happen to you is that you would lose a child. And worse than that is that you might have had something to do with it. And I just think that’s impossible to live with at some level.
But here’s the good news, so we can end on a positive note. Galileo was censured by the Roman Catholic Church for daring to put forward Copernicus’s notion that the earth revolved around the sun. And he was censured in front of this Roman Catholic tribunal. He said to them, even as he was being carried away in chains, “And yet, it

still moves.” The earth revolves around the sun. And you can put me in chains. And no matter how many times RFK Jr. says vaccines cause autism or how many sycophants or congressional representatives or fringe doctors or fringe scientists or media outlets, he gets to echo that, they don’t. And science is a powerful thing to have on your side in the long run.
PCMS: I think our students often forget we are part of this noble profession, you know, and that our mission is to take care of people. So, do you think that these young docs really have that courage, to be able to say, hey, this will pass, and we need to be ready?
Emanuel: I don’t know about that. I think they are idealistic. And that is one thing we have going for us. And I think these attacks make them probably a little fearful, but I think more idealistic.


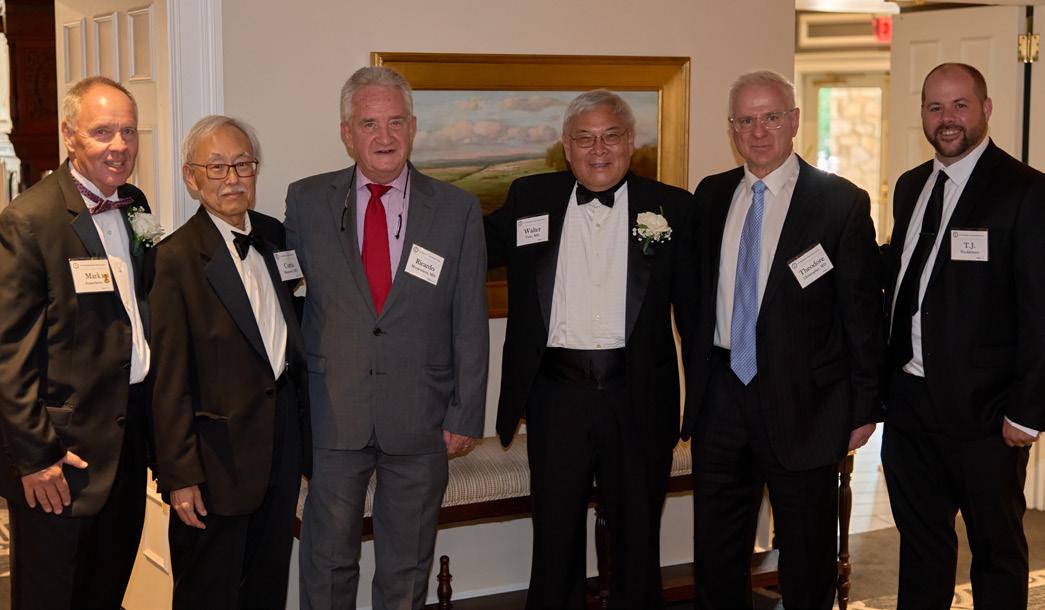
The Philadelphia County Medical Society presents the Installation of Walter H. Tsou, MD, MPH, 164th President, and Annual Awards Night Presentations at the Philadelphia Country Club, June 21, 2025

Good evening. I want to acknowledge my family who have been on this journey with me and whose love and support has meant the world to me. So many of the leadership of the Pennsylvania Medical Society are here today including Dr. Lynn Lucas-Fehm, our current president; John Pagan, former Speaker of the House; many of the past presidents of PMS and of PCMS. A special thanks to the 50-year members of our medical society who you will be hearing from later.
If you had told me when I was in medical school that I would one day serve as president of the Philadelphia County Medical Society and at an earlier time, Health Commissioner of Philadelphia and president of the American Public Health Association I would have told you “no way.” But in fact, it is “way!” Such has been my great fortune. Thank you for this honor.
In truth, I am an unusual choice to be president of a body of organized medicine. Although, I practiced for many years in caring for among the poorest in Philadelphia in our district health centers, I have spent most of my professional career in public health, helping to assure conditions so that people can be healthy. So, it is maybe a time when it is worth reexamining what has been seen as two separate worlds: one in public health and one in patient care.
Indeed, public health is something that wasn’t really talked about much when I went to medical school. Fortunately, that is changing. But I have learned that public health is the foundation of any health care system. We take for granted that clean air, clean water, protection from extreme weather, and nutritious foods (which my speech is delaying dinner from you) is a given. But in reality, the laws and regulations that have assured even these basic necessities of life are being challenged and even discarded. It will become increasingly problematic when we have to add damage to our environment as part of our differential diagnosis.



Consider a recent decision made by our Secretary of Health, RFK, Jr., who has is now widely known, disbanded all 17 members of the Advisory Committee on Immunization Practices. A lot of justifiable concern has been raised that the new members may politicize immunization practice, forcing a new role that medical societies will have to be the defenders of scientific facts. Dr. Ashish Jha, Dean at the Brown School of Public Health, wrote in his Washington Post op-ed four days ago, “The medical and public health communities must speak with one voice. Pediatricians, pharmacists and professional associations must reassure families: Approved vaccines have been rigorously tested, are safe, effective and essential — even as the systems delivering them are under assault.”
There will be many further examples where the public health world and medical practice will need to come to some agreement. In southeastern PA, we have witnessed hospitals under enormous financial stress. The recent closures of Crozer Chester and Taylor hospitals, on top of the previous closure of Hahnemann, have brought to light the pernicious way that private equity has dismantled essential health services in order to enrich its private investors. The proposed severe cuts to Medicaid and the ACA Marketplace could force many rural hospitals and our own city hospitals to severely limit or deny services to patients or even close. The state legislators have already said that they do not have the resources to rescue these draconian cuts. Now is the time to call our U.S. senators to restore these announced health care cuts. Yes, they do count how many calls they receive and yes, your calls matter.
Most of us went to medical school to use our education and skills to help people. But we have created a financing system of care where we limit our skills to “covered lives” or “customers” or


whatever market terms we have created. And the new laws will force us to look differently at immigrants who arrive in our ERs even though we will have to realize that they are more likely desperate because they have nowhere else to turn. Policy is one thing. But faced with an emergency or uninsured patient who has delayed care creates an ethical dilemma which these laws do not recognize.
As a nation, we have never had a serious discussion about health policy in America. What is our health mission as a nation? What are our values? The result is we spend 50% more than any other nation on earth while living two to four years less. A country with our wealth can and must do better. Not everyone agrees, but I believe that health care is a public good, not a market commodity.
All this to say that I assume the presidency of our esteemed medical society, one that is over 160 years old, at a time of great change. It is a time of transition where Mark Austerberry, who has been our Executive Director for 18 years, is retiring, and T.J. Huckleberry will be stepping into his shoes. The importance of organized medicine will be more important than ever. No one will be able to wend their way through these turbulent waters alone, but collectively we can speak with a more powerful voice.
Thank you for the opportunity to lead at this moment in time and I will need all of your wisdom and energy to restore the meaning of practicing medicine and putting our patients first. Thank you.

continued
164th Inaugural and Awards Night Program of The Philadelphia County Medical Society continued from page 11













FEATURE continued
164th Inaugural and Awards Night Program of The Philadelphia County Medical Society continued from page 13


Welcome, honored colleagues, guests, friends and family to the 164th Inaugural and Awards Night of The Philadelphia County Medical Society.
Thank you for joining our annual celebration of medicine in our city. The Philadelphia County Medical Society continues a proud, steadfast tradition from its beginning in 1849 of advocating for patients, public health and high professional standards in medical practice and medical education. We will continue to collaborate with institutions, insurers and providers to address all issues of healthcare on a local, state and national level. Right now, it is critical that we address the challenges that confront us on social, economic and political fronts.
Tonight is a time to salute our physician and health care professionals who have served as positive role models for our colleagues. It is also a time to reflect on the contributions of all the members of our society who have cared for and enhanced the lives of countless patients, by their selfless acts of kindness, outstanding medical care and research.
Aside from the many notable physicians listed in this booklet, we are indeed lucky to have countless teachers at our many schools of medicine and their students who go out and offer their skills to those who live in our communities.
Congratulations to our awardees. Philadelphia has long been a beacon of medical and osteopathic education in our country and a leader in all fields of medical care. Our Society continues to serve as a voice for reform in education and physician issues. We ask you to join with us so that we can continue to advocate for our patients and fairness in physician practice.
We hope that you enjoy this special evening celebrating the very best in Philadelphia Medicine!

Walter H. Tsou, MD, MPH
164th President, The Philadelphia County Medical Society
The annual Strittmatter Award is the highest honor presented to a physician who has made the most valuable contribution to the healing arts. Established in 1923 by I. P. Strittmatter, MD, the award commends the recipient’s contribution to one of the fundamental sciences of medicine, having a beneficial influence on either surgery or medicine.

Larry R. Kaiser, MD, FACS, is an internationally known thoracic surgeon. Dr. Kaiser served in leadership positions in academic medicine for over 20 years. Prior to joining the international consulting firm, Alvarez and Marsal, as a managing director in the Health Care Industry Group, he served for almost nine years as President and Chief Executive Officer of the Temple University Health System, a $3.0B system, Senior Executive VicePresident for Health Affairs, and the inaugural Lewis Katz Dean of the Lewis Katz School of Medicine at Temple University.
Before joining Temple University, Dr. Kaiser served as President of the University of Texas Health Science Center at Houston, the largest of the six health-related institutions of the University of Texas, where he had responsibility for the schools of Medicine, Dentistry, Nursing, Public Health (with five regional campuses), Biomedical Informatics, and the combined Graduate School with the MD Anderson Cancer Center. In addition, he had responsibility for a 1000-member physician practice and held the Alkek-Williams Distinguished Chair.
Dr. Kaiser graduated AOA from the Tulane University School of Medicine in 1977 and completed his residency in general surgery, as well as a fellowship in surgical oncology at the University of California, Los Angeles. He then completed a residency in cardiovascular and thoracic surgery at the University
of Toronto. Following that, he held positions as attending thoracic surgeon at Memorial Sloan-Kettering Cancer Center and Assistant Professor of Surgery at Cornell University Medical College (New York) and subsequently as Associate Professor (with tenure) at the Washington University School of Medicine (St. Louis). Recruited to the University of Pennsylvania in 1991, Dr. Kaiser held a variety of positions, including Chief of General Thoracic Surgery, founder and director of the university’s lung transplantation program, the first in the Northeast, and Director of its Center for Lung Cancers and Related Disorders, and Co-Director of the Thoracic Oncology Laboratory.
In 2001 Dr. Kaiser was named the John Rhea Barton Professor and Chair of the Department of Surgery as well as Surgeon in Chief for the University of Pennsylvania Health System.
He is the author or co-author of 20 books and more than 350 original papers, and he serves on multiple editorial boards including the Annals of Surgery and as Associate Editor of the European Journal of Cardiothoracic Surgery.
Dr. Kaiser has served in several leadership capacities for professional societies and associations and has been a Director of both the American Board of Surgery and the American Board of Thoracic Surgery, and in 2005 was elected to the National Academy of Medicine (formerly the Institute of Medicine).
At Alvarez and Marsal, Dr. Kaiser worked at the intersection between academic medical centers and health systems with a special interest in strategy, physician practice management, and performance improvement. A sample of major engagements in which he was a principal, include the restructuring of Unity Point Health, financial turnaround at Bassett Health System, and as the clinician specialist as part of the federally mandated Quality Review Organization for the Providence Health System. In January 2025, Dr. Kaiser transitioned to a part-time position as senior advisor to the firm when he was appointed as the President and CEO and Thomas W. Langfitt Chair, at the College of Physicians of Philadelphia.
Congratulations Dr. Kaiser, The Philadelphia County Medical Society is proud and honored to add the Strittmatter Award to your many accomplishments.
164th Inaugural and Awards Night Program of The Philadelphia County Medical Society continued from page 15
The Cristol Award is presented to a physician member for their significant contributions to the Society furthering and enhancing the educational and charitable goals, purposes and functions of organized medicine. The award honors the memory of David S. Cristol, MD, an outstanding member of PCMS.
Stephen R. Permut, MD, JD

Dr. Permut is a Professor Emeritus and former Chair of the Department of Family and Community Medicine at the Lewis Katz School of Medicine at Temple University (LKSMTU). Dr. Permut received his bachelor’s degree from the University of Pennsylvania in 1967 and his MD from LKSMTU in 1972. Dr. Permut completed his internship and residency in internal medicine at Indiana University Medical Center, Indianapolis; he also received a juris doctorate degree from Widener University School of Law in 1985. Dr. Permut retired from practice in 2023.
Dr. Permut began his career in Delaware, where he reluctantly joined the New Castle County Medical Society and the Medical Society of Delaware. Reluctantly, because he was not a joiner, but the only way that you could obtain medical liability insurance at the time was by being a member of the medical society. Thus, began his career in organized medicine.
He became a member of the Board of Trustees of New Castle County Medical Society and was the founding Chair of its Community Relations Committee. He served on the Board of Trustees of the Medical Society of Delaware (MSD); he was the founding Chair of its Legislative Action Committee; and was elected President of MSD from 1992 to 1993. During his term as President, in collaboration with the state’s hospital association, MSD formulated a state-wide health system reform plan. For his leadership, MSD awarded Dr. Permut both the Distinguished Service Award and the President’s Award. When Dr. Permut finished his Presidency at MSD, he became the Chair of Delaware’s Delegation to the American Medical Association’s House of Delegates. Dr. Permut soon became a member of the AMA Council on Legislation and eventually served on the AMA
Board of Trustees from 2010-2018, where he was elected Chair in 2017.
Dr. Permut joined The Philadelphia County Medical Society/ Pennsylvania Medical Society (PCMS/PAMED) in 2005 and was elected to the PCMS Board of Directors, where he served as Treasurer and President. In addition, Dr. Permut continues to serve as a Delegate to the PAMED House of Delegates. Dr. Permut has also served on the Board of Commissioners for the Joint Commission and as a member of the Executive Committee of the Board of Trustees of the College of Physicians of Philadelphia.
Dr. Permut is a Fellow of: American Academy of Family Physicians, American College of Physicians, College of Physicians of Philadelphia, and American College of Legal Medicine. Dr. Permut’s numerous Awards include Babcock Honor Society, LKSMTU; Alpha Omega Alpha; Preceptor of the Year, LKSMTU; Temple University Gallery of Success; Laureate’s Award, American College of Physicians; and Honored Professor Award, LKSMTU.
Dr. Permut is married to Marylene Permut. They have two daughters, Laura (married to Andrew) Sparks and Irene (married to Alex) Swift, as well as four grandchildren: Casey, Haoshun, Max, and Owen.
Congratulations Dr. Permut and thank you for your years of dedication and service to PCMS!
The Vanitha Appadorai Vaidya, MD. Award for Humaneness in Medicine honors the memory of the devoted and loving wife of our past President, Shailendra Vaidya, MD. The purpose of this Award is to commend humaneness demonstrated by a Resident Physician member of PCMS. This humaneness is characterized by particular skills in working with people, patients, and their families, and understanding human, as well as clinical needs, especially in the kindness of treatment.
Suraj Malhan, DO, MS

Dr. Suraj Malhan is currently a Headache Medicine Fellow at the Jefferson Headache Center, where he is recognized not only for his clinical expertise, but for the compassion and kindness he brings to every patient encounter. A graduate of the Philadelphia College of Osteopathic Medicine, Dr. Malhan completed his neurology residency at the University of Maryland Medical Center and has been inducted into both the Gold Humanism Honor Society and Omega Beta Iota, the national political honor society for osteopathic physicians.
Known among peers and patients for his ability to listen without judgment, to advocate with conviction, and to lead with heart, Dr. Malhan exemplifies the ideals of humanistic care. Whether he is delivering lectures on migraine management, mentoring medical students, or simply holding space for a patient in pain, he is guided by the belief that every person deserves to be heard, seen, and treated with dignity.
Dr. Malhan has earned national recognition for his work in headache medicine, research, and advocacy. He is the recipient of the Pennsylvania Medical Society’s Top Physicians Under 40 Award; the American Headache Society’s Frontiers in Headache Research Award; and was recently named a scholarship winner of the International Headache Academy. He is also the founder of Headache Guru, a growing patient education platform aimed at bridging gaps in care through accessible, evidence-based resources.
Outside the clinic, Dr. Malhan is a passionate advocate for underserved populations, a published author, and a frequent speaker on topics including migraine, cervicogenic headache, and physician wellness. He is deeply honored to receive this award, which reflects the core values that drew him to medicine in the first place: empathy, service, and human connection.
Congratulations Dr. Malhan! We thank you for your very special care and humanistic touch in medicine!
PCMS presents the annual Practitioner of the Year Award to a physician who has been nominated for dedication to the medical profession in the areas of quality patient care and community service. The award is supported by the Wiener Fund established by the late Jacob S. Wiener, MD, past member of PCMS.
Patricia C. Henwood, MD
Dr. Patricia Henwood is the Executive Vice President, Chief Clinical Officer, and James D. and Mary Jo Danella Chief Quality Officer for Jefferson Health. She is also an Associate Professor of Emergency Medicine and Population Health at Thomas Jefferson University. Dr. Henwood has been leading Jefferson’s nationally awarded OnPoint quality and safety program across Jefferson’s 17-hospital system since 2021. She recently expanded its scope to support clinical integration for quality and safety across the 32-hospital system as part of the Jefferson Health and Lehigh Valley Health Network merger.

Throughout her impactful career, Dr. Henwood has successfully led initiatives to strengthen health systems both globally and locally. Her multidisciplinary approach focuses on building more effective systems to improve outcomes by advancing safety, quality, and reducing care disparities. She has been a principal investigator on numerous research and operational grants, including a focus on pandemic response and community health equity since the onset of COVID-19, including work leading Jefferson’s mobile community COVID-19 vaccination efforts and vulnerable community COVID-19 testing sites. She currently serves as co-PI for Jefferson Health as a selected member of the PCORI Health System Implementation Initiative.
Dr. Henwood led Jefferson Health’s work with the United States Departments of Homeland Security, Defense, and State, as well as the Philadelphia Department of Public Health in the development and execution of a novel family-centered, traumainformed medical care delivery model on arrival for more than 25,000 Afghan evacuees arriving through Philadelphia International Airport as part of Operation Allies Welcome.
Dr. Henwood attended Georgetown University (BA, Government); worked in the pharmaceutical industry; and then completed her medical degree at Jefferson’s Sidney Kimmel Medical College. She trained and served as chief resident at the Harvard-Affiliated Emergency Medicine Residency at Massachusetts General and Brigham and Women’s Hospitals prior to fellowship training in Emergency Ultrasound with a focus on global health at Brigham and Women’s Hospital. Ahead of joining Jefferson in 2019, she held various faculty and clinical leadership roles at the Hospital of the University of Pennsylvania and Brigham and Women’s Hospital/Harvard Medical School based in the Department of Emergency Medicine. She serves as a board member for Health Share Exchange.
Congratulations, Dr. Patricia Henwood! PCMS is proud to honor and recognize your dedication to the medical profession.



Walter H. Tsou, MD, MPH, inducted on June 21 as the 164th President of The Philadelphia County Medical Society (PCMS), is a public health physician with experience in several leadership roles both locally and nationally.
Dr. Tsou is a past Clinical Director of Ambulatory Health Services for the Philadelphia Health Department; a Founding Medical Director of the first Public Health Department in Montgomery County; a Fellow of the College of Physicians of Philadelphia; on the board of Physicians for Social Responsibility PA; and a past Health Commissioner for the City of Philadelphia. He was also an Adjunct Professor of Family Medicine and Community Health at the University of Pennsylvania where he taught community health at their Center for Public Health Initiatives.
Born in Boston and raised in Abington, Pennsylvania, he graduated from the University of Pennsylvania with a degree in Chemistry. Dr. Tsou received his medical degree from the University of Pennsylvania School of Medicine and completed his internal medicine residency at Presbyterian Hospital in Philadelphia; he has a Master’s in Public Health from Johns Hopkins; and he received an honorary Doctorate in Medical Sciences from Drexel University.
An active member of PCMS since 1996, Dr. Tsou serves on the PCMS Board of Directors and has served as Chair of the active Public Health Committee which coordinates the PCMS community Block Captain Health Care Advisory Council.
Dr. Tsou is an expert on health reform and health care financing and has frequently briefed members of Congress on health care issues, having served as past president of the American Public Health Association. He is also a founding member of the National Board of Public Health Examiners and is a Board Adviser to Physicians for a National Health Program.

Dr. Tsou is the recipient of numerous awards including Practitioner of the Year from PCMS; the Leadership Award from the Delaware Valley Healthcare Council; the Broad Street Pump Award from Physicians for Social Responsibility; and the Public Health Recognition Award from the College of Physicians of Philadelphia.
As President, Dr. Tsou has many goals and aspirations for PCMS and hopes to set groundwork for physicians to gain more autonomy and control in today’s changing medical profession. Keys to Dr. Tsou’s plans in the coming months, are the fostering of camaraderie among PCMS physicians through community-based activities and the continuation of Doctors Lounge programs with speakers on topics such as business and government. Additionally, Dr. Tsou hopes to inspire even more interest in our organization with a program he calls, “The Soul of Medicine.” Dr. Tsou believes that bringing students into group settings with speakers who draw from experiences as medical practitioners in other cultures, will provide a setting in which to discuss the humanity and art of medicine. “It’s very easy in this very technical world where we live to forget why we went to medical school in the first place, namely, to help people.”
Dr. Tsou is married to Dr. Jean Lee, a nephrologist at Temple University Hospital. They have one daughter, Casey Tsou, who is studying bilingual education as a graduate student in Chicago. Dr. Tsou is an avid gardener and continues to advocate for sound public health.
Congratulations, thank you and good luck, Dr. Tsou! We look forward to a great year under your leadership as President of The Philadelphia County Medical Society.

What was your favorite part of being Exec for PCMS?
As the Executive Director of the Philadelphia County Medical Society (PCMS) for the last 18 years, one of the most rewarding aspects of the role was the opportunity to foster a collaborative environment that advances medical practice and enhances patient care within Philadelphia. Directing and working with the PCMS Board of Directors, we played a pivotal role in uniting healthcare professionals, facilitating meaningful dialogue, and promoting continuous education and professional development for the membership. The positive impact of our efforts was evident in the strengthened relationships among the physician members, the successful organization of impactful events, and the implementation of initiatives that support physicians in their vital work.

Our dedication to advocating for the interests of medical practitioners as the annual House of Delegates and improving healthcare standards not only elevates the society’s reputation but also directly benefits the community at large, such as the Block Captains program. I was able to witness the tangible outcomes of our strategic vision and commitment to excellence that provided a profound sense of fulfillment and motivation. Overall, I believe my role as Executive Director has helped shape a vibrant, supportive, and forward-thinking medical community in Philadelphia, which has been undoubtedly a very rewarding experience.
As T.J. assumes the role of Executive Director of the PCMS and steps into a leadership position with the new Board of
Directors, it is essential to approach this responsibility with strategic foresight, effective communication, and a commitment to advancing the society’s mission. They all should focus on strategic leadership, effective communication, member engagement, advocacy, and organizational sustainability. By doing so, they can effectively guide The Philadelphia County Medical Society through its next chapter of growth and influence, ultimately benefiting physicians, patients, and the broader healthcare community.
What was your greatest challenge?
Perhaps positioning PCMS as a strong advocate for physicians and patients since this was ongoing. Also staying informed about healthcare policy changes at local, state, and federal levels and then helping to develop strategic advocacy programs to influence these policy decisions that impact our physicians and public health.
What was the biggest change you have seen in medicine over your 18 years?
The closure of the Hahnemann Hospital and the medical residency program presents a range of significant problems and challenges that impact various stakeholders, including residents, faculty, the healthcare system, and the community. I was very proud to be of assistance since this closure involved legal proceedings related to contractual obligations, liabilities, and the rights of residents and the physicians on staff. Coordinating the transfer of residents to other programs and managing the administrative aspects of the closure required meticulous planning and resources with the help of so many stakeholders.
Over the next decade, the field of medicine in Philadelphia is poised to undergo significant transformation driven by technological advancements, evolving healthcare policies, and increasing patient expectations. Philly, as you know, with its rich medical history and vibrant healthcare community, is expected to become a hub for innovative medical research, personalized medicine, and integrated healthcare systems. Certainly, technological innovations such as AI, telemedicine, and advanced diagnostic tools will likely become commonplace, enhancing the accuracy of diagnoses and the efficiency of treatment plans.
I feel also as someone who was trained in public health, the emphasis on preventive care and population health management will grow, requiring physicians to adopt new approaches to patient engagement and health education. The integration of EMR and data analytics will facilitate more personalized and proactive care strategies and improvements in overall community health.
In this evolving landscape, the PCMS will play a crucial role in supporting its members. The society can assist by providing continuous medical education focused on emerging technologies and best practices, ensuring physicians stay current with rapid advancements. It can also advocate for policies that promote equitable access to innovative treatments and support the adoption of new healthcare models.
Additionally, PCMS can foster a collaborative environment through networking events, mentorship programs, and forums for sharing research and clinical experiences. By championing physician well-being and addressing issues such as burnout and administrative burdens, the society can help maintain a resilient and motivated medical workforce. Overall, the next ten years will be pivotal for medicine in Philadelphia, and the PCMS will be instrumental in guiding its members through this transformative period, ensuring they are well-equipped to deliver high-quality, innovative care to their communities.
Thanks again to The Philadelphia County Medical Society physician leadership and the members for allowing me to serve as your Executive Director. It has been a genuine honor to work alongside such dedicated professionals and to contribute to the advancement of our medical community. I was blessed with great staff during my time too.
Moving forward, I remain committed to supporting the PCMS’s mission and to continuing collective efforts to improve patient care, advocate for physicians, and strengthen our community. Thank you once again for this incredible opportunity and for your ongoing dedication to the medical profession.

My name is T.J. Huckleberry, and I am honored to serve as your new Executive Director. Allow me to share a bit about my background: I previously held the position of Executive Director at the Berks County Medical Society and spent a decade working in the Pennsylvania State Senate. I am genuinely excited and humbled to take on this role and look forward to collaborating with each of you.
As many of you are aware, my predecessor, Mark Austerberry, is retiring. Mark has been both a mentor and a central figure in organized medicine throughout Pennsylvania for many years. If I had a dollar for every time someone mentioned that I have “big shoes to fill,” I might be retiring alongside Mark!
On behalf of our Society, I wish to thank Mark for his years of dedicated service and hard work.

T.J. Huckleberry, Executive Director, Philadelphia County Medical Society



n the United States, maternal morbidity and mortality rates, especially among marginalized populations, remain alarmingly high after a three-decade climb. Today, disparities continue, yet maternal and birthing centers across the nation continue to close, leaving women and families without trusted, high-quality providers.
In the current landscape, there is more need than ever before to increase access to high quality maternal care. Kimberly Hanson, VP and CNO, Temple Women & Families, offers insights to overcoming these disparities through innovative programming and investments to better care access for a diverse population facing complex challenges.
What are some of the current challenges facing maternal health in Philadelphia, particularly among the North Philadelphia patient population?
KH: The challenges are significant, especially in our patient population. Many of our patients have comorbidities and face barriers to accessing care, including transportation issues, time off from work, or a lack of health literacy. These factors contribute to unaddressed health conditions, making maternal health complex to manage. We often encounter patients who haven’t received adequate preventative care, even before pregnancy, leading to a higher risk of complications. Addressing these barriers is a key priority for us.
Tell us about the soon-to-be-opened Temple Women and Families Hospital. What makes it unique?
KH: The Temple Women and Families Hospital, slated to open in 2025, is a groundbreaking initiative. We’re creating a hospital dedicated to women and families, providing services including OBGYN, primary care, pediatrics, specialty services, labor and delivery, a level III NICU, and med-surg ICU. What makes this hospital unique is our focus on care gaps, social determinants of health, and critical wraparound services that address improvements in maternal
and fetal outcomes. Our goal is to eliminate the barriers women often face in navigating large health systems. Everything from labor and delivery to breast care will be under one roof, designed to enhance the patient experience and improve outcomes.
What specific initiatives or programs are being implemented to improve maternal health outcomes at Temple Health?
KH: We are very focused on trauma-informed care. Many of the communities we serve have experienced trauma, and we are designing our hospital environment to alleviate the fear often associated with healthcare settings. From the lighting to the furniture, we want to create a healing environment. One of the most exciting programs we’re launching is the Mama Model, which pairs high-risk patients with perinatal-trained community health workers. These trusted community members help ensure that our patients meet all important milestones during pregnancy and beyond.
How is Temple leading in addressing maternal health inequities, and are there any unique programs in place?
KH: Maternal health equity is a significant focus for us. We’ve developed dashboards that allow us to drill down, leveraging data through our electronic medical records to identify gaps in care, particularly in terms of racial and ethnic health disparities. By tracking this data, we can focus on improving maternal health equity and care quality across the board. We’re also establishing a hospital-based doula program, which will provide additional support during labor and delivery. Doulas are essential, particularly for patients who need a trusted, familiar figure by their side. We believe these initiatives will significantly enhance the care experience and improve outcomes.
To learn more about Temple Health’s initiatives in women’s and maternal health, visit www.templehealth.org/ advancingequity.


Q&A with Michael Young, President and CEO, Temple Health

Under Michael Young’s leadership, Temple Health is advancing maternal care, attracting top talent, and achieving financial growth amid an evolving healthcare landscape.
What milestones have marked Temple Health’s progress over the past year?
MY: Temple Health continues to defy national trends in healthcare. While many systems face financial strain, Temple has maintained stability and growth. Over the past year, the health system improved its budget, grew revenue, and kept expense growth low. These operational improvements, paired with a 25% year-overyear increase in transplant volume and a boost in research funding, position Temple Health as a leader in clinical innovation and financial stewardship.
Fox Chase Cancer Center’s 100th anniversary celebration and Temple’s strategic partnership with Microsoft to build an AIdriven clinical trial system further demonstrate Temple’s ability to innovate across clinical care, research, and patient access.
How is Temple Health addressing critical gaps in maternal healthcare?
MY: Recognizing the urgent need to improve maternal health outcomes, Temple Health is opening the region’s only hospital exclusively dedicated to women and families’ health. Amid a national backdrop where many health systems are reducing OB services, Temple’s investment represents a bold commitment to reversing trends in maternal mortality and health disparities.
The new women’s hospital will create vital opportunities for expanded clinical services and research, helping Temple Health lead the way in improving women’s health outcomes in Philadelphia and beyond.
How is Temple Health succeeding in physician recruitment amid national workforce shortages?
MY: Temple Health’s brand strength and reputation for innovation are powerful draws for clinical talent. Over this year, Temple has added 45 new physicians, with plans to add 55 next fiscal year. Physicians and staff cite the organization’s streamlined decision-
making, access to leadership, and mission-driven culture as key reasons for joining.
While other systems lay off workers and freeze salaries, Temple continues to expand. Our emphasis on clinician autonomy, access to cutting-edge technologies, and deeply rooted mission have made us one of the most sought-after healthcare employers in the region.
What steps is Temple Health taking to increase healthcare access?
MY: Temple is investing in new primary care facilities, including the transformation of former retail space into modern clinical settings. By the end of fiscal year 2026, Temple will have doubled its primary care footprint.
Innovations such as AI-driven patient appointment scheduling and self-scheduling tools are helping improve access and reduce delays, while major investments in ICU and outpatient expansions support the growing demand for specialized care. Temple’s expansion ensures that more patients across Philadelphia—especially in underserved neighborhoods—can receive timely, comprehensive healthcare.
How do you see Temple Health evolving in the coming years?
MY: Temple Health’s future priorities focus on accelerating lab-to-bedside research, expanding genomics capabilities, and strengthening Philadelphia’s life sciences corridor. Investments in AI, advanced imaging technologies, and interdisciplinary collaboration across Temple University are already paying dividends—cutting project timelines dramatically and fueling new research breakthroughs.
As Temple builds a new women and families hospital in partnership with the state, and invests deeply in North Philadelphia communities, it reinforces our role as Philadelphia’s health system: committed to the city, its people, and its future.


By Sebastiano Porcu, Medical Student - Sidney Kimmel Medical College at Thomas Jefferson University
July 4th, 2026, will mark the 250th anniversary of the Declaration of Independence and the birth of the United States of America as an independent nation. Centered in the celebrations is Philadelphia, the nation’s first capital from May 10, 1775, until December 12, 1776, and on four subsequent occasions until 1800, when construction of the new national capital in Washington, D.C. was completed.1 In addition to the political arena, Philadelphia holds a vital role to the birth and subsequent development of American medicine.
Beginning prior to the Declaration of Independence, Philadelphia emerged as a nucleus among colonial cities in the development of medicine. In 1751, Benjamin Franklin and Dr. Thomas Bond established Pennsylvania Hospital, the first hospital in what would become the United States and with the explicit intent to care for the indigent and mentally ill. Largely reflecting its Quaker origin, Pennsylvania Hospital would come to develop a reputation for its humane treatment, particularly at a time when psychiatric disease and mental health were poorly understood and supported. Soon after, in 1765, the first medical school in the American colonies was founded at the University of Pennsylvania by Dr. John Morgan. The school’s curriculum drew from the experiences of Morgan and other early faculty who had trained in Edinburgh and London, highlighting and incorporating bedside teaching as a supplement to medical lectures.2,3 Knowledge and experience gained from European training contributed to the
public health efforts of the city in the face of chronic disease and recurring epidemics, as for example with the smallpox epidemic of 1775-82. Inoculation was a source of both medical innovation and controversy, with Philadelphia serving as a major center for the practice.
The growth of Philadelphia, driven largely by immigration, served as a catalyst for continued expansion of medical institutions within the city. The College of Physicians of Philadelphia was founded in 1787, Friends Hospital opened in 1813, the Fairmount Water Works for the improvement of public health opened in 1820; the first college of pharmacy (1821); Jefferson Medical College (1824); Wills Eye Hospital (1832); Hahnemann Medical College (1848), the Woman’s Medical College of Pennsylvania (1850, the first of its kind in the world), Children’s Hospital of Philadelphia (1855), Woman’s Hospital of Philadelphia in 1862 by Dr. Ann Preston, the Medico-Chirurgical College (1881), the Philadelphia Polyclinic and College for Graduates in Medicine (1883), and the Philadelphia College of Infirmary of Osteopathy in 1899. Lastly, the Medical Department of Temple College, later Temple University School of Medicine, opened in 1901. As Dr. Steven Peitzman details in his article City of Medicine, “The availability of strong medical education for women, and the presence of several women’s hospitals, fostered growth of a sizeable community of women physicians and surgeons who practiced and taught here.” This led to Philadelphia
As the nation looks ahead to celebrating its milestone semiquincentennial anniversary, we should remember Philadelphia not just as the birthplace of America but as the fountainhead of American medicine.
developing a transformative medical legacy within the United States.
Medical institutions in the city have always served as beacons of scientific discovery. For example, the Philadelphia chromosome was discovered in 1959 by Dr. David Hungerford of the Fox Chase Cancer Center and Dr. Peter Nowell of the University of Pennsylvania. It was the first genetic abnormality conclusively linked to cancer—specifically, chronic myelogenous leukemia (CML). This discovery laid the foundation for the field of cancer cytogenetics and ultimately led to the development of targeted therapies. Later, in the 1960s, Dr. Paul Parkman, Dr. Harry Meyer, and others at the Children’s Hospital of Philadelphia (CHOP) and the Wistar Institute were key figures in isolating the rubella virus and developing a safe and effective rubella vaccine. Approved in 1969, this vaccine dramatically reduced birth defects caused by congenital rubella syndrome (CRS).4,5
However, the history of medical innovation within Philadelphia, and by extension the United States, is not without its lapses. As in other parts of the country, unethical medical experimentation without informed consent or compensation occurred on vulnerable populations, including the incarcerated and communities of color. Notably, in the mid-20th century Dr. Albert Kligman, a dermatologist at the University of Pennsylvania, experimented on incarcerated Black men at Holmesburg Prison. His research culminated in linking sun exposure to wrinkles and the discovery of Retin-A, but at the expense of individuals’ autonomy. The University of Pennsylvania eventually issued an apology, though Dr. Kligman defended his work until his death in 2010, noting, “Legality, of itself, does not excuse these activities, which are not now, and never were, morally acceptable, even if Dr. Kligman and his contemporaries believed them to be.”6,7
Compared to the breathtaking expansion of hospitals, medical institutions, and colleges within the City of Philadelphia in past centuries, the modern medical landscape has shifted and stalled in recent decades amid consolidation and closures. Hahnemann University Hospital encapsulates this trend. A key academic center, Hahnemann closed secondary to financial and private equity pressures, leaving many thousands of Philadelphians in the lurch and with disjointed healthcare. Moreover, thousands of physicians, nurses, techs, and ancillary and support staff needed to find new jobs. Sadly, the story of Hahnemann is not unique, but it does reveal broader challenges in sustaining academic and publicserving hospitals and medical institutions.
Through both the highs and lows of medical discovery, innovation, and education in Philadelphia, The Philadelphia County Medical Society (PCMS) has served to advance physicianpatient care, professional standards, and public advocacy.
Established in 1796, PCMS has fostered professional education and unity, creating an extensive, multi-generational connectivity that has helped maintain a cohesive medical community in the city. PCMS demonstrated its impact throughout its history. For example, under the leadership of President George P. Muller and Chair Philip F. Williams, the Society established a Committee on Maternal Welfare in 1930, which conducted a multi-year study on maternal mortality. Their findings and advocacy helped drive a dramatic reduction in Philadelphia’s maternal death rate—from 6.8 per 1,000 births in 1931 to just 0.9 per 1,000 by 1949.8
As the nation looks ahead to celebrating its milestone semiquincentennial anniversary, we should remember Philadelphia not just as the birthplace of America but as the fountainhead of American medicine. From its pioneering institutions in the 18th and 19th centuries to its continued leadership in research, education, and public health, Philadelphia has been central to American medicine. Through organizations like the PCMS and College of Physicians, the city continues to shape ethical standards, clinical innovation, and physician advocacy, preserving a crucial medical legacy into the present day.

1. “How Philly lost the nation’s capital to Washington”. National Constitution Center. May 14, 2020. Accessed August 10, 2025. https://constitutioncenter. org/blog/how-philly-lost-the-nations-capital-to-washington
2. Peitzman SJ. City of Medicine. Encyclopedia of Greater Philadelphia. Published by Encyclopedia of Greater Philadelphia. Accessed August 10, 2025. https://philadelphiaencyclopedia.org/themes/city-of-medicine/
3. Pennsylvania Hospital Timeline. University of Pennsylvania Health System. Accessed August 10, 2025. https://www.uphs.upenn.edu/paharc/timeline/ index.html
4. Office of the Dean, Perelman School of Medicine. Legacy of the Philadelphia Chromosome. University of Pennsylvania. Published August 20, 2021. Accessed August 11, 2025. https://www.med.upenn.edu/ evpdeancommunications/2021-08-20-283.html
5. Plotkin SA. History of rubella and rubella vaccination leading to elimination. Clin Infect Dis. 2006;43(Suppl 3):S164-S168. doi:10.1086/505950
6. 50 years after Philadelphia halted prison medical testing, families seek reparations. AP News. Accessed August 11, 2025. https://apnews.com/article/ philadelphia-prison-experiments-black-reparations-ff8a08483fb13d1b949d9 38d7ae29656
7. University of Pennsylvania. Statement on Penn Medicine’s Recognition of the Legacy of Albert Kligman, MD, PhD. Office of the Dean, Perelman School of Medicine; August 20, 2021. Accessed August 11, 2025. https:// www.med.upenn.edu/evpdeancommunications/2021-08-20-283.html
8. College of Physicians of Philadelphia. Records of the Philadelphia County Medical Society Committee on Archives and Committee on Maternal Welfare (1912–1950). Finding Aids, University of Pennsylvania. Accessed August 11, 2025. https://findingaids.library.upenn.edu/records/CPP_MSS3013
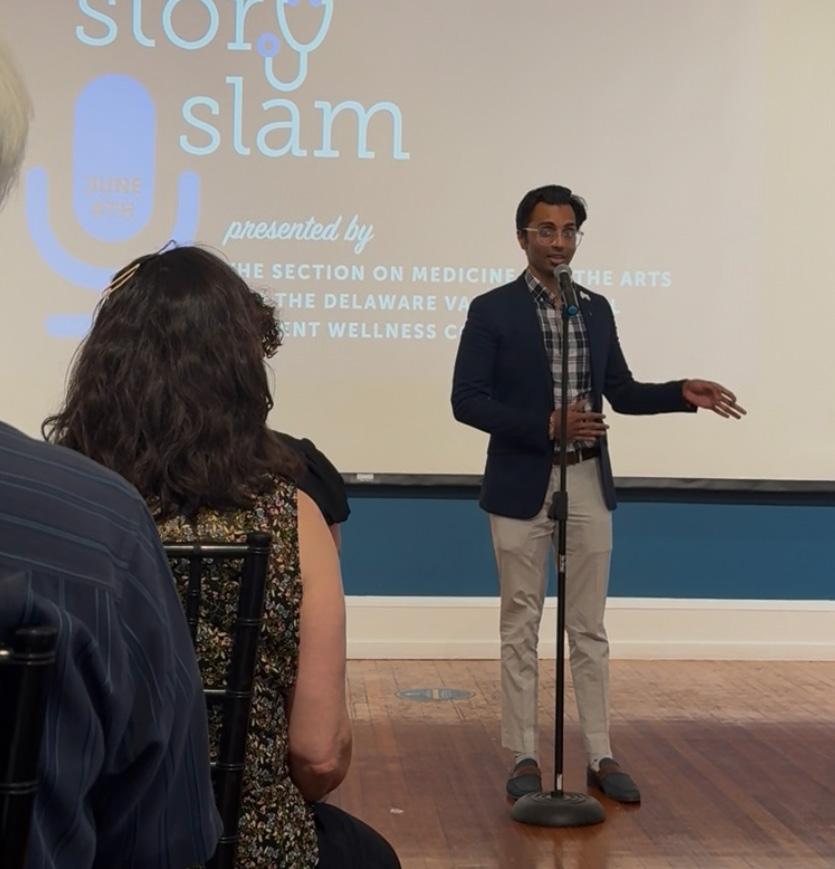
By Kishan Patel, MD Candidate - Sidney Kimmel Medical College at Thomas Jefferson University, 2025 COP Story Slam
The College of Physicians of Philadelphia hosts the annual Story Slam event, where local medical students and healthcare providers share their personal experiences through stories. The metropolitan Philadelphia medical schools are each invited to field a team of two storytellers, including at least one medical student and one healthcare provider at any level. Each contestant has five minutes to tell their medically-related story and at the end, the audience selects the three best stories.
This story takes place in 2022: Kiteh was a first-year medical student here in Center City. One day, he was studying renal physiology in the library on his campus. After many hours of studying what gets reabsorbed and secreted in the proximal convoluted tubule and the loop of Henle, he decided to call it quits and go to his apartment for a break. He opened the door of the library to go back home, and he could not remember the way home; he was able to navigate the nephron, but he could not navigate the streets of Philadelphia. He only lived three blocks away, and like a typical medical student, he had walked from his apartment to the library almost every day. He remembered his address, so he was able to put it into his phone and used the GPS to find his way home. Once he got to his apartment, he just thought, “Oh, I had so much to study, so maybe that’s why I had a lapse in my memory,” so he brushed it off.

A few weeks later, his sisters came to pick him up from Philadelphia and take him home. They had that plan set for months, but that morning, they came and texted him, “Hey, we’re outside your apartment. Come downstairs.” He was so confused. He wondered, “Why are they here?” He went downstairs to see them, and his sisters already knew something was wrong: Kiteh was in his pajamas. Kiteh was the type of person who immediately showered right after waking up, so you would only see him in his pajamas if he was going to bed. His sisters immediately took him home and told his parents about what happened. His parents then got him an appointment with his primary care doctor that same week. His mom took Kiteh to his doctor, but right when they got to the doctor’s office, Kiteh could not move out of the car. His mom called the nurse, and the nurse said, “He’s having a tonic seizure. Take him to the hospital
now.” His mom took him to the hospital, and he would ultimately be admitted there for four months. During those four months, he went into a comatose state. The doctors did many MRI scans and found a mass growing on the right side of his brain.
After a while, a tumor board was called because the doctors realized that they couldn’t just let him sit there in a comatose state; they had to do something. They eventually started him on chemotherapy, which was life changing. After four cycles of chemotherapy, Kiteh was sent to a rehabilitation hospital where he did physical, occupational, and speech therapy. Kiteh had to learn how to walk again, eat again, and use the toilet again. Kiteh is now cancer-free. He is back in medical school after having to restart from the beginning. Kiteh is in the middle of his clinical rotations in the same hospital system where he got his cancer care. Kiteh is now writing this story. Kiteh is me.
After being discharged, I’ve been using my cancer journey to inspire others and improve humanism in medicine. My main message is that patients are humans, too. There were times in the hospital when I was treated as a human and other times when I wasn’t, and the latter made me feel horrible on top of receiving a cancer diagnosis.
I genuinely think of coming out of that comatose state as being reborn again. I had to learn how to eat, walk, and do all the things little babies learn to do. Cancer is not my whole story. It is a chapter. For years, my dream has been to write a memoir about my life. Hopefully, one day I will find a publisher and you will all have a copy of my evolution in life in your hands, and that evolution will have a chapter dedicated to my cancer journey, but it won’t be the whole story.


Thank you to everyone who came to our third annual tailgate on August 2nd! Members, family, and friends of all ages attended. It was a beautiful day, and although the Phillies had a rare loss, we had a great time! Here are some pictures we took—We hope to see you next year!









Each year, PCMS members are given the opportunity to participate in a rich diversity of committees that impact the practice of medicine in Philadelphia County, Pennsylvania and beyond. Because active participation in PCMS strengthens the voice of organized medicine, we encourage all members (including medical students, residents and fellows) tohelp make an impact on the role PCMS plays in the medical community.
• Editorial Review Board – Works on the Philadelphia Medicine magazine and newsletter.
• Delegate Caucus to Pennsylvania Medical Society’s Annual Meeting –Participates in PAMED’s House of Delegates as a representative of PCMS.
• Public Health Committee – Tackles issues related to public health and manages the Block Captain Healthcare Council.
• Membership Committee – Works on membership recruitment and retainment.
• Early Career Section – Represents the needs of early career physician membership.
• International Medical Graduates Section – Represents the needs of International Medical Graduate (IMG) membership.
• Senior Physician Section – Provides a platform for physicians aged 65 and above to remain active and involved in the medical community.
• Women Physician Section – A forum to encourage women physicians to participate in leadership, policymaking, advocacy, and other activities of PCMS.
• Residents/Fellows Section – Represents the needs of resident and fellow membership.
• Medical Student Section – Works to improve medical education and advocates for the future of medicine.
To find out more about specific committees, go to https://philamedsoc.org/pcms-committee-form/ or call us at 215-563-5343 or email us at stat@philamedsoc.org.






















At MADJ, we specialize in helping medical practices and health systems of all sizes thrive in competitive landscapes. From small beginnings to significant success, our tailored strategies have transformed healthcare providers into community cornerstones.