HOW A NEUROLOGIST FACES THE DISEASE THAT IS SLOWLY STEALING HIS COGNITIVE POWERS
SCHOLARSHIP FUNDS

HOW A NEUROLOGIST FACES THE DISEASE THAT IS SLOWLY STEALING HIS COGNITIVE POWERS
SCHOLARSHIP FUNDS
Understanding UV Risk in Fall and Winter


























/ (610) 346-8800




Captivating panoramas unfold through walls of glass, perfectly positioned in a stunning array of interior and exterior spaces. Set on 53 acres with woods, meadows, lake and pond. Offered for $3,995,000

Surrounded by 73 acres in the heart of the Pocono Mountains, this remarkable 13,000 sqft home includes an indoor pool, commercial gym, media room, library and more. Offered for $2,570,000
This 5,700 sqft home is ready to be built to your specifications and could be complete in under a year! Located on an expansive parcel surrounded by luxury homes on large lots. Starting at $3,495,000

Built when quality was the rule and not the exception, renovations and expansions have enhanced the original home with a nod to its rich history at every turn. Offered for $2,500,000


Set on 50 acres, this circa 1863 home is a culmination of many a heart’s desire - a historic home, in pristine condition, on generous acreage and under 2 hours from New York City. Offered for $1,650,000
A reimagined farmhouse nestled on 6.27 acres, this custom built home is complemented by traditional farm outbuildings, including an historic PA bank barn. Offered for $995,000




LEHIGH COUNTY MEDICAL SOCIETY P.O. Box 8, East Texas, PA 18046 610-437-2288 | lcmedsoc.org
2025 LCMS BOARD OF DIRECTORS* Chaminie Wheeler, DO President
Kimberly Fugok, DO President Elect
Mary Stock, MD Vice President
Oscar A. Morffi, MD Treasurer
Charles J. Scagliotti, MD, FACS Secretary
Rajender S. Totlani, MD Immediate Past President
*effective February 1, 2024 - for two-year terms
CENSORS
Howard E. Hudson, Jr., MD Gregory Wheeler, DO
TRUSTEES
Wayne E. Dubov, MD
Kenneth J. Toff, DO Alissa Romano, DO
EDITOR
David Griffiths Executive Officer
The opinions expressed in this publication are for general information only and are not intended to provide specific legal, medical or other advice or recommendations for any individuals. The placement of editorial opinions and paid advertising does not imply endorsement by the Lehigh County Medical Society.
All rights reserved. No portion of this publication may be reproduced electronically or in print without the expressed written consent of the publisher or editor.

14 PLAQUE BUILDUP IN THE NECKS OF STROKE SURVIVORS MAY BE LOADED WITH MICROPLASTICS
6 HOW A NEUROLOGIST FACES THE DISEASE THAT IS SLOWLY STEALING HIS COGNITIVE POWERS ON THE COVER
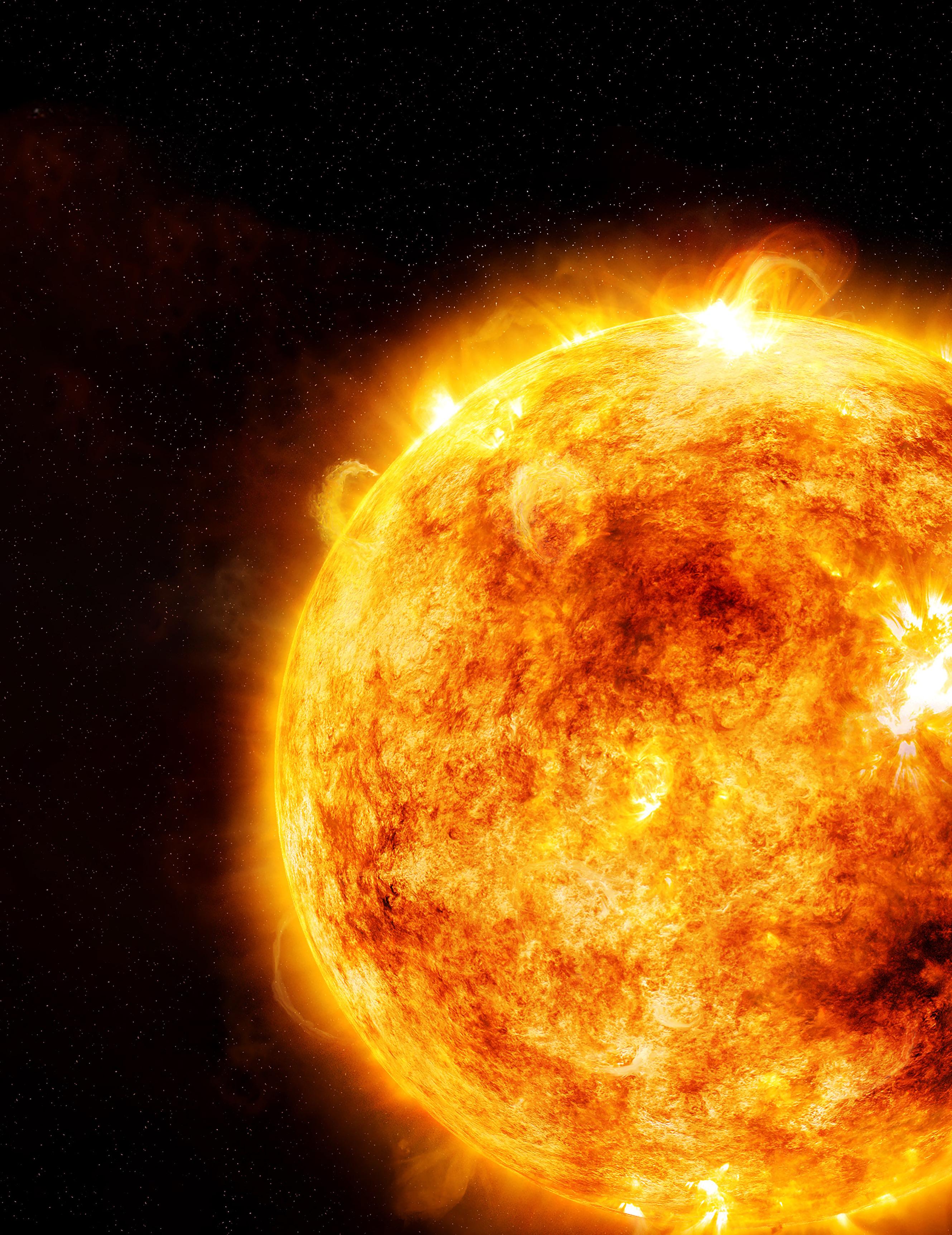
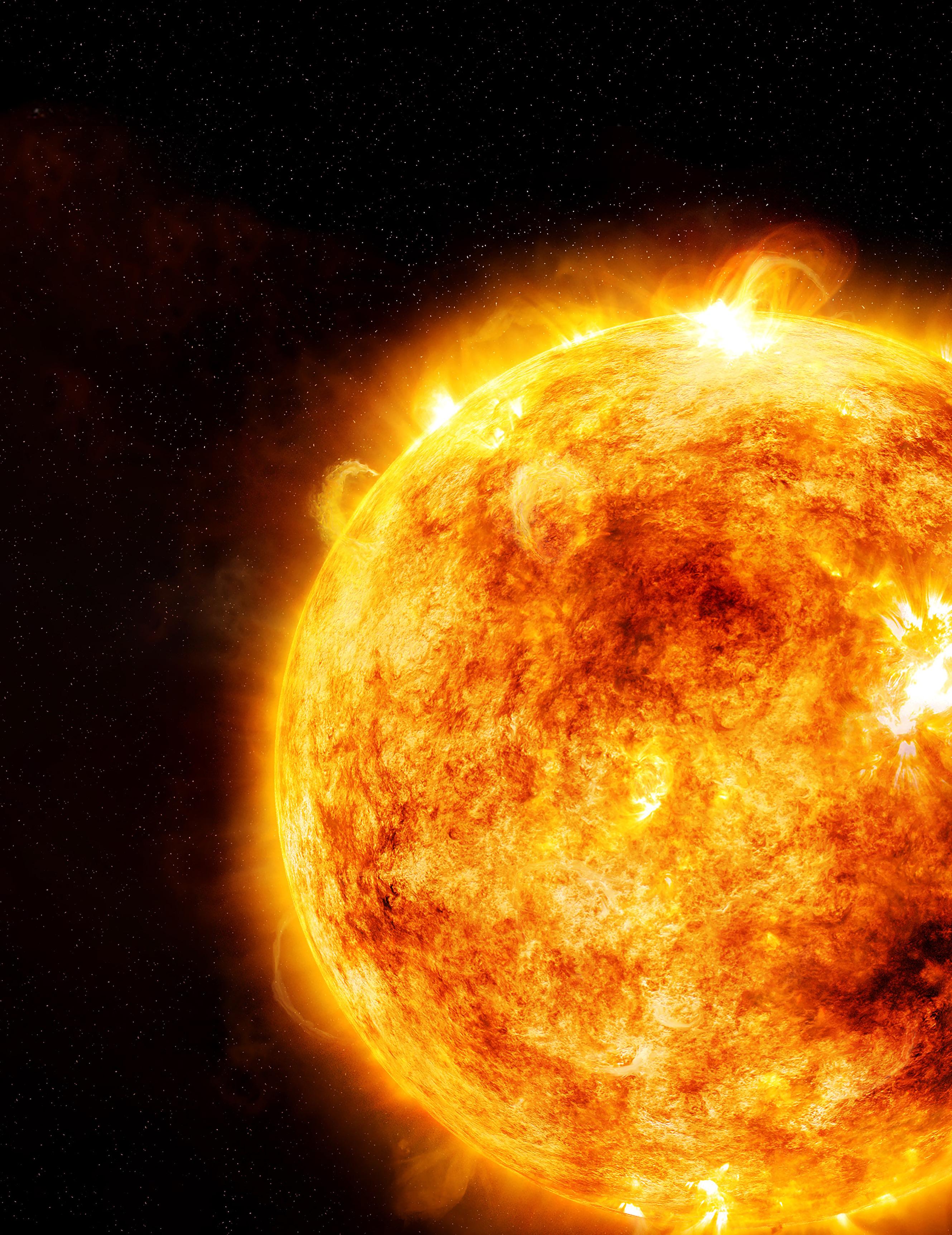
8 THE SUN DOESN’T TAKE A WINTER BREAK
Understanding UV Risk in Fall and Winter By Tina Nguyen, DO - PGY1 Transitional Year Resident, Dominique Jacobs, DO - PGY4 Chief Dermatology Resident, Stacey Blannett, DO - PGY4 Chief Dermatology Resident, Kevin Liu, DO - Advanced Dermatology Associates OPINION ARTICLE 10 DIRECT PRIMARY CARE: A STEP FORWARD By Kimberly Legg Corba, DO, CHCO, OHCC
17 LEHIGH COUNTY MEDICAL SOCIETY ESTABLISHES NEW SCHOLARSHIP FUND AT COMMUNITY FOUNDATION
18 THE FOUNDATION OF THE PENNSYLVANIA MEDICAL SOCIETY: Investing in the Future
20 FINANCIAL FREEDOM: What I Wish I Knew When I Was Younger By Wayne Dubov, MD
Lehigh County Health & Medicine is published by Hoffmann Publishing Group Sinking Spring, PA | HoffmannPublishing.com | (610) 685.0914 FOR ADVERTISING INFO CONTACT: Sales@HoffPubs.com, 610-685-0914 x715

The students are back in school and pumpkin spice is back in the conversation, so welcome to our fall edition of Lehigh County Health and Medicine. We hope you find the contents of this issue interesting and informative; we have both articles and opinion pieces in this edition.
You will find useful information on topics ranging from using sunscreen year-round to financial freedom for young physicians, and more.
Most of us know about sunscreen and protecting ourselves at the beach and pool, but as the title says, “The Sun Doesn’t Take a Winter Break.” As a winter sports enthusiast, I can tell you I have seen a lot of sunburned faces on frigid days. So, we have a great article explaining sun protection even at times when some may not feel it is necessary.
We hope you will enjoy the article “Financial Freedom: What I Wish I Knew When I Was Younger.” This piece contains thoughts from a physician on his experience and what he wished he knew when he was a younger physician.
You will find an opinion piece on how the President’s July 4th signing of the “One Big Beautiful Bill” can benefit those interested in Health Savings Accounts and how they can be used. This is an opinion piece, and in order to foster a balanced dialogue, we invite submissions that offer alternative opinions or critiques of those presented.
We hope you enjoy this and past issues as we add to the conversation about how medicine and wellness can help us form strong communities in Lehigh County. If you are interested in back issues, or just want to read Lehigh County Health and Medicine online, please visit our website at lcmedsoc.org/our-publication.
It was 2006 when Dr. Daniel Gibbs first noticed he was losing his sense of smell. But it wasn’t what he didn’t smell that tipped him off that something might be wrong.
It was what he did smell: perfume, mixed with baked bread. “The same thing, every time.”
Gibbs, a neurologist in Portland, Oregon, knew this was an olfactory hallucination. And that meant something wasn’t working properly in his brain.
“I attributed it to getting older, which is a common cause of decreased ability to smell,” he said. But Gibbs was just 57—not so old that he should be losing his sense of anything. “I also knew losing your sense of smell was an early sign of Parkinson’s disease, so I thought it might be that.”
It wasn’t.
Gibbs was experiencing an early symptom of Alzheimer’s disease. But it would be another six years before he knew it. He has since
written a book about his experience, which was turned into a documentary. He also keeps a regular blog to help people understand what it’s like to live with Alzheimer’s. These days, he spends a lot of his time learning and talking about how to slow progression of the disease, something he’s been trying to do since he got his diagnosis more than a decade ago.
Gibbs and his wife, Lois Seed, discussed what he’s learned about Alzheimer’s dementia and how he navigates the condition for “The Experts Say,” an American Heart Association News series in which specialists explain how they apply their professional knowledge to their own lives. Their remarks have been edited.
WHEN DID YOU REALIZE YOUR SYMPTOMS WERE DUE TO ALZHEIMER'S DISEASE?
In 2012, Lois was doing a genealogical project, so we did some genetic testing. Mine came back showing I had two copies of APOE4, a gene known to influence the risk of developing Alzheimer’s disease, which totally gob smacked me. Having two copies means it is almost certain to eventually cause Alzheimer’s.
I had no measurable cognitive impairment at that time. I was in charge of the neurology resident training program at Oregon Health and Science University in Portland, and I was seeing patients in the clinic, so it was a very busy year for me. Even though it was difficult, I was still able to get all the balls to balance in the air.
WHAT DID YOU DO ONCE YOU KNEW YOUR GENETIC RISK FOR ALZHEIMER’S?
The first thing I did was to go to one of my colleagues and have some cognitive testing done. It was essentially normal with the caveat that all of my cognitive domains were in the 90th percentile except verbal memory, which was in the 50th percentile. So, there was a strong hint that there was some incipient loss of function of verbal memory.
With that in hand, I went to my department chair and explained the situation. I had no impairment but did not feel it was safe for me to continue to practice. I retired in 2013.
Lois: You also went looking for studies you could join, because it’s a big deal to see people before they experience symptoms.
That’s right, I went to the University of California in San Francisco, because they have a ton of studies there. The first study I was involved with was a longitudinal neuroimaging study. I had PET scans of abnormal amyloid and PET scans for tau proteins—two protein clusters in the brain that play a role in the development of Alzheimer’s disease. And I had cognitive testing.
They loved having me down there because they rarely have people with as early a stage of disease as I showed up with. About a year later, I joined a clinical trial for an anti-amyloid antibody drug that is now approved by the Food and Drug Administration to treat early Alzheimer’s disease.
WHAT ELSE DID YOU LEARN ABOUT HOW TO SLOW PROGRESSION OF THE DISEASE?
This is not rocket science. The sort of things that are good preventive behavior for brain disease are also good for preventing heart and vascular disease.
There are evidence-based lifestyle changes that include getting daily aerobic exercise; eating a Mediterranean-style diet, such as the MIND diet; getting mentally stimulating activity; staying socially engaged; getting at least seven hours of sleep nightly; and getting good control of any cerebrovascular risk factors, such as diabetes, high blood pressure, high cholesterol, obesity and smoking.
What’s good for the heart is good for the brain!
HOW DO YOU PUT THIS KNOWLEDGE INTO PRACTICE?
Walking is just built into my day. I do it with my dog, Jack, an 11-year-old English cocker spaniel who is about to age out. He can’t keep up with 10,000 steps as easily anymore, so I take some walks by myself. We live in the hills, so I’m getting very good aerobic exercise, short of running.
I used to go to the gym, but that stopped at the start of the COVID pandemic.
I also have a short workout at home. The first thing I do is I use resistance bands, which is a strength exercise. That takes about 15 minutes and then I do tai chi pretty religiously,
something I started six months ago. I can clearly see that it helps my balance, but I can’t see if it helps my brain, which is continuing to do more poorly.
And thanks to Lois, I’ve been eating a healthy diet, really forever.
Lois: I didn’t have control over those French fries you were eating.
I don’t eat red meat anymore. I closely follow the MIND diet, which is essentially the Mediterranean diet with more berries and nuts. It includes a heavy focus on fruits and vegetables, especially green leafy vegetables, beans, nuts, whole grains, seafood, lean poultry and uses olive oil to cook. I’m quite happy with it.
Because I lost my sense of smell, which is totally gone now, I have virtually no taste either. I eat the same thing for lunch and breakfast every day. I enjoy it. I make a sandwich on whole wheat bread that has tuna salad and garbanzo beans, avocado and arugula to get the dark leafy greens. Then some grapes or bananas and half a dark chocolate bar.
Breakfast is homemade granola, and I add cranberries or blueberries. I throw walnuts in as well. Dinner is whatever Lois picks that I can eat.
I stopped drinking alcohol. There’s no safe amount of alcohol if you are on this trajectory. So, I got rid of it, but I used to love red wine.
DO YOU KNOW WHAT TO EXPECT AS THE DISEASE PROGRESSES?
That’s a difficult question to answer. In the old days, when people got a diagnosis of Alzheimer’s, they were only living three to five years after that because we made the diagnosis so late. There’s less information out there about people who have known they have the disease for a long time and how they will do going forward.
Lois: There's a lot of confusion and misconception because there are different types of dementia. Alzheimer’s tends to progress more slowly. The early stage can last 20 years. Here we are 13 years after his diagnosis and Dan’s really doing well. I'm a little more of a caregiver than I was a few years ago, but not by much. He dresses himself and monitors medications, and people who talk
to him casually wouldn’t even know. We’ve been at that plateau for quite some time.
HOW WOULD YOU DESCRIBE THE STAGE YOU'RE AT RIGHT NOW?
Right now, I have mild Alzheimer’s dementia. To say you have dementia is to say you are having trouble managing your personal affairs. I’m just at a stage now where I can’t balance a checkbook. And as things go along, I will have more problems with memory and the ability to recognize people and remember their names.
I’ve lost my train of thought.
Lois: You were talking about what stage you’re at.
When I’m not remembering where I am, then I will have severe dementia.
There are memories I have going back through my whole life. They tend to be events that are emotionally laden.
I’m terrible with names. I know my immediate family members. My neighbors, I forget their names.
Lois is taking over the things I can’t manage anymore, like the financial part of our lives, anything that involves planning ahead, scheduling, calendars, remembering all the family stuff, managing the household. She also goes with me when I have a talk to give.
Lois: He gives talks on Alzheimer’s, but almost every time that Dan is getting ready to speak to a group, he gets frustrated and says, “This is the last time I’m doing this,” because getting his thoughts together is challenging. He writes out notes. Most of the talks he gives now are screening events for the film with question-and-answer sessions.
It works well if Lois is there to find …
Lois: Words.
That makes it easier.
To learn more about the American Heart Association’s work in Lehigh Valley, email Development Manager Jessica Escobar-Eck at jessica.escobar-eck@heart.org or visit heart.org/ en/affiliates/pennsylvania.
TINA NGUYEN,

As summer fades into crisp autumn days and chilly winter nights, many people put away their sunscreen, thinking the sun damage season is over. The reality is that ultraviolet (UV) radiation penetrates the skin year-round, no matter the temperature. Regardless of the weather, UV rays can cause skin cancer and speed up skin aging.
In the Lehigh Valley, the average UV index from September through March ranges from one to four, which is classified as “low” to “moderate” risk.* Once the UV index hits three, experts recommend sun protection. While these numbers may seem mild compared to summer’s average of six, “low” does not equal “no risk.” Pair moderate UV exposure with no sunscreen, and you get steady, invisible damage which may not be immediately apparent but will make itself known later.
Two types of UV rays can harm your skin: UVA and UVB. UVB rays peak around midday, while UVA rays are present from sunrise to sunset. UVA rays penetrate deep into the dermis (the inner layers of skin), causing skin aging, fine lines, and wrinkles. UVB rays target the epidermis (the outer layer of skin), causing sunburns and contributing to certain skin cancers. Broad-spectrum sun protection defends against both types of damage.
ACTIVITY-BASED
As summer winds down, outdoor fun locations shift from beaches to hiking trails, football games, and ski slopes. Even under layers of clothing, the face, ears, neck, and lips stay exposed and vulnerable. For skiers and snowboarders, higher altitudes mean stronger UV rays, and snow can reflect up to 80% of that radiation, doubling the UV ray hit to the skin. Without sun protection, these conditions can lead to sunburn, premature aging, and skin cancer.
UV exposure isn’t merely an outdoor problem. While most window glass blocks UVB rays, UVA rays can still slip through, damaging skin over time. During
commutes or holiday travel, the skin soaks up sunlight through car windows. Air travel adds another layer of risk since one is traveling at higher altitudes. The fix is simple: apply sunscreen before hitting the road or boarding a flight.
The American Academy of Dermatology (AAD) recommends avoiding direct sun exposure between the hours of 10 a.m. and 2 p.m., when UV rays are strongest. Since this avoidance is not always practical, consistent sun protection is key. It is imperative to block both UVA rays and UVB rays using a broad-spectrum sunscreen with at least a Sun Protection Factor (SPF) of 30. SPF measures the approximate time it takes your skin to redden with sunscreen versus without. SPF 30 blocks about 97% of UV rays; SPF 50 blocks 98%. A higher SPF does not mean longer-lasting protection, however, so reapply every two hours regardless of SPF or “water resistant” labeling. Adults generally need about one ounce of sunscreen (roughly a shot glass’ worth) to cover exposed areas. Don’t forget commonly missed areas like the eyelids, ears, and neck.
Other sun protection strategies include wearing photoprotective clothing, widebrimmed hats, and UV ray-blocking sunglasses or snow goggles (for winter sports). Remember the lips too! It is recommended to use a lip balm with SPF 30 to protect against UV damage.
Sun safety isn’t seasonal; it is a yearround commitment. The easiest way to make sunscreen part of a daily routine is through “habit stacking,” where one pairs a new habit with an already established one. For example, keep the sunscreen next to the toothbrush so morning brushing acts as a cue to apply the sunscreen.
For dry winter skin, choose a moisturizing sunscreen to get UV protection and hydration in a single product. Tinted formulas containing iron oxide offer extra defense against visible
*UV index: Low (1-2), Moderate (3-5), High (6-7), Very High (8-10), and Extreme (11+)
light, which can cause hyperpigmentation and age spots. The options can be overwhelming, but the best sunscreen is the one that will be used regularly. Need ideas? The AAD website lists dermatologistrecommended options: www.aad.org/.
While highly common, skin cancer is one of the most preventable cancers. As fall activities, winter trips, and holiday travel commence, daily sunscreen is a simple, effective way to protect the skin and lower one’s long-term risk. Don’t let summer habits fade with the warm weather. When hitting the Poconos this winter, make sure the travel checklist includes three essentials: helmet, goggles, and sunscreen. A travelsize sunscreen makes a thoughtful stocking stuffer and a subtle reminder that good habits last all year.
References:
1. Allentown Weather AveragesPennsylvania, US. Accessed August 6, 2025. https://www.worldweatheronline. com/en-us/allentown-weather-averages/ pennsylvania/us.aspx.
2. Radiation: The ultraviolet (UV) index. World Health Organization. Accessed August 5, 2025. https://www.who.int/news-room/ questions-and-answers/item/radiationthe-ultraviolet-(uv)-index.
3. Sunscreen faqs. American Academy of Dermatology. Accessed August 4, 2025. https://www.aad.org/media/statssunscreen.
4. Shade, clothing, and Sunscreen. American Academy of Dermatology. Accessed August 6, 2025. https://www.aad.org/public/everydaycare/sun-protection/shade-clothingsunscreen.
5. Moradi Tuchayi S, Wang Z, Yan J, Garibyan L, Bai X, Gilchrest BA. Sunscreens: Misconceptions and misinformation. J Investig Dermatol. 2023;143(8):1406-1411. doi:10.1016/j.jid.2023.03.1677.

The most innovative model of healthcare delivery in the United States, Direct Primary Care (DPC), took one HUGE step forward on July 4, 2025, when the One Big Beautiful Bill (OBBB) was signed into law.
Provisions in this bill, outlined below, will strengthen the ability of Americans who have a Health Savings Account (HSA) to have expanded choices and control over how, where, and when they obtain their primary care, including a DPC practice:
• Health Savings Accounts are only permitted by the IRS when attached to certain health insurance plans such as HDHP (high-deductible health plans). Some HDHPs cover telehealth services BEFORE patients meet the plan’s deductible. Prior to the OBBB, this would have disqualified that plan from being a HDHP offering plan participants the option to have an HSA account. Safe harbor now permanently applies for the absence of applying telehealth services toward a deductible, allowing these specific high-deductible plans to officially qualify to be eligible to offer HSAs to participants. (Sec. 71306 - https://www.congress.gov/ bill/119th-congress/house-bill/1)
• Previously many bronze and catastrophic plans had deductibles that were higher than the allowed amount by the IRS to meet criteria to be defined as a HDHP. (Section 71307 - types of health coverage)
• The most impactful provision for DPC is Section 71113 (https://www.congress. gov/bill/119th-congress/house-bill/1).
This part of the OBBB states that Direct Primary Care is NOT a secondary form of health insurance. Previously, there was no official ruling in the Federal Registry from Treasury as to whether DPC was considered a form of health insurance. If DPC was considered a health insurance plan, then belonging to a Direct Primary Care office would disqualify patients from contributing to their HSA and they would not be able to pay for the periodic medical fees characteristic of subscription-based medicine using HSA
funds. This provision finally puts this long-debated issue to rest.
All three of these sections of the OBBB increase the number of Americans who can choose to access the tax advantages of Health Savings Accounts which exist in triplicate (funded by PRE-TAX earnings, funds that are invested grow tax-free, and funds are not taxed at the time of withdrawal).
It is hard to believe it has been ten years since the concept of subscription-based health care was first introduced to the US Congress.
There has been legislation regarding the tax treatment of Health Savings Accounts for DPC circulating on The Hill since 2015 when The Primary Care Enhancement Act of 2015 (S. 1989 - https://www.congress. gov/114/bills/s1989/BILLS-114s1989is. pdf) was introduced by Senator Bill Cassidy (R-LA). This bill only had two co-sponsors and contained simple language that seemed to ensure larger support on both sides of the aisle.
Every year since, some form of The Primary Care Enhancement Act bill was introduced to either the House, Senate, or both chambers as mirroring bills.
And, as time passed and Congressional sessions came and went, DPC became more of market model by growing rapidly and steadily (growth even occurred DURING the lock-down of the COVID-19 pandemic) across the country. In 2015, there were between 141 and 500 DPC offices in 39 states. When I opened my Direct Primary Care office in January of 2016, there were reportedly 800 offices in the country. By 2020 the number grew to about 1200 DPC practices, and currently, it is reported that there are approximately 2600 or more offices in all 50 states.
Therefore, it was not totally surprising to learn that some “extra” and unnecessary language turned that original bill from 2015 into proposed legislation that could have enacted some restrictions and guardrails on direct primary care offices. The added language was not favored by the independent DPCs across the country and would have limited the growth of the
model and, more importantly, reduced value-added benefits DPC patients enjoy as part of their membership. Thankfully, many of the unfavorable provisions of the last DPC/HSA bill introduced prior to the OBBB were removed. But it took some time and hard work by many supporters of the independent DPCs to get there!
In 2018, a group of five DPC physicians from five separate states officially formed a lobbying group (501c4) named DPC Action (dpcation.com). Lee Gross, M.D. (FL), Katarina Lindley, D.O. (TX), Chad Savage, M.D. (MI), Josh Umbehr, M.D., and I (representing our great Commonwealth) comprised the small, yet mighty, team. We realized it was imperative that physicians who owned and operated successful DPC practices had to have boots on the ground in DC/The Hill or we would not have any input or control over potential legislation or rulemaking. Our group wanted to represent all the private practice DPCs across the country. The lawmakers and key cabinet members/staff needed to speak with us face-to-face, since we were the doctors delivering health care to our patients through this model. They needed to hear how it was different and how it was helping patients directly from the source.
Self-funding our transportation and lodging costs, we went back and forth at least monthly (sometimes twice/month) for nearly two years. We still deeply appreciate the opportunities given to our group to talk with domestic/health policy staff in the White House, HHS, Treasury/IRS, SBA, and CMS. This was in addition to hours of meetings with lawmakers and their staff, thousands of emails, many op-eds/ articles, etc. As a group, we welcomed and supported Executive Orders which included health coverage initiatives; as members of DPC Action, we attended three EO signings. On June 8, 2019, Executive Order 13877 (https://www.federalregister. gov/documents/2019/06/27/2019-13945/ improving-price-and-quality-transparencyin-american-healthcare-to-put-patients-first) asked Treasury to clarify tax language to allow HSAs to pay for DPC and allow patients who did so to be able to continue funding their HSAs. Treasury did not opine continued on next page >
within the timeline given in the EO. Little did we know that our last meeting together to work on getting a favorable opinion and regulatory change from IRS/Treasury, would be the last week of February 2020.
Fast forward to 2025. After EO’s working to expand choices and control of health care for Americans were rescinded at the end of February 2020 due to a change in White House Administration, the House Budget and Ways and Means Committee moved quickly and worked very hard to add accepted language regarding HSAs/ DPC from H.R. 5688, the Bipartisan HSA Improvement Act of 2023 (Smucker-PA / https://www.congress.gov/118/bills/ hr5688/BILLS-118hr5688rh.pdf) into the OBBB. We are incredibly thankful to Chairman Arrington (R-TX) of the House Budget Committee for championing the inclusion of the DPC provisions into the OBBB. We are all also forever grateful for the many key opportunities and access given to DPC Action prior to codification of our initiatives, starting in 2018 and leading up to this historic point.
Do you dread the driving conversations with older drivers and their families? We can help.
So, here’s a discussion point: DPC now has legislation which will be beneficial for patients who have and use HSAs for Direct Primary Care memberships. And for those who don’t use DPC, many more will have the ability to fund an HSA due to inclusion of more qualified health insurance plans.
What about the people who don’t have, or can’t access, a Health Savings Account because their insurance plan isn’t a qualified HDHP or they are uninsured? Unfortunately, those patients pay with money that does not receive the triple tax benefits of HSA accounts.
The discussion now must focus on working toward universal reform of Health Savings Accounts. In this doctor’s humble opinion, it is incredibly discriminatory that the tax benefits of a Health Savings Account are not available as a choice for EVERY AMERICAN CITIZEN, even if they only want to save $20.00/month, and regardless of whether they are interested in a DPC doctor or not, and regardless of what type of insurance they have or don’t have. ALL

Introducing the Beyond Driving with Dignity program
Older drivers and their families appreciate the human connection established during the session, as we help them through the complex and sensitive issue of driving retirement.

888-299-9960
randyreardon@seniorcareauthority.com seniorcareauthority.com/neofphilly
Americans should be able to open a Health Savings Account: Veterans, Medicare and Medicaid patients, uninsured, parents for their children, etc. Having a way to save money for health costs that people can use to pay directly for HSA qualified medical expenses, strengthens that individual’s ability to have some control and choice in their healthcare, when so many feel they do not have too much of either. It helps them engage in their health care.
Maybe we can pull off a second major reform to Americans’ health care if we all work together and continue to advocate tirelessly for our patients. Because it is ALL about the patients.
To foster a balanced dialogue among peers, Lehigh County Health & Medicine invites submissions that offer alternative opinions or critiques of those presented. This article is an opinion piece and is representative of the opinion of the author; it does not imply endorsement by the Lehigh County Medical Society.
What’s Beyond Driving with Dignity?
A trained professional facilitates an in-person session in your patient’s home. We get to know the person while gauging their cognitive, physical and emotional abilities. Directly following the session, we offer our recommendations to the older driver followed with a detailed report of our findings and recommendations.
The cost is just $450

Ask about our Senior Living Placement Solutions where we work with the family to find appropriate senior living arrangements.
Your new digital gateway to the latest WellSpan advances.
With articles, research updates and exclusive insights tailored for physicians, MacroScope is our new content platform to inform and inspire. We look forward to sharing medical innovations, clinical research and new technologies that will empower and inform your professional journey.
• Stay up to date: Keep abreast of the latest developments across various specialties.
• Gain insights: Benefit from expert analyses and studies that can directly impact your practice.
• Expand your network: Connect with other experts shaping the future of healthcare.
For another healthy dose of valuable medical content, subscribe to our companion publication. Complete the subscription form on MacroScope online for delivery to your home or office three times a year.


Tiny pieces of plastic are infiltrating the large arteries in the neck that carry blood from the heart to the head, with the highest amounts found in fatty buildup in the arteries of stroke survivors, a small study suggests.
The concentration of so-called micronanoplastics in carotid arteries was 51 times higher in plaque from people who'd had a stroke, mini-stroke or temporary blindness compared to amounts found in the walls of plaque-free carotid arteries. Even people with carotid artery plaque who had not experienced any of those conditions still had 16 times more micronanoplastics in their plaque.
“It's not just that diseased arteries have more plastics,” said the study’s lead researcher, Dr. Ross Clark, a vascular surgeon and an assistant professor of vascular surgery at the University of New Mexico in Albuquerque. “That is clear. But those with diseased arteries causing symptoms have far more plastics.”
The results, considered preliminary until full findings are published in a peerreviewed journal, were presented April 22 at the American Heart Association's Vascular Discovery Scientific Sessions conference in Baltimore.
Microplastics and nanoplastics mainly result from larger plastic consumer products degrading in the ocean, soil, rivers, lakes or air. Microplastics are less than 5 millimeters in size—about the size of a pencil's eraser—while nanoplastics are microscopic at less than 1,000 nanometers. By comparison, a human hair is about 80,000 to 100,000 nanometers wide.
Micronanoplastics are omnipresent in the environment and enter the human body when people inhale or ingest them. Previous studies have shown that they are
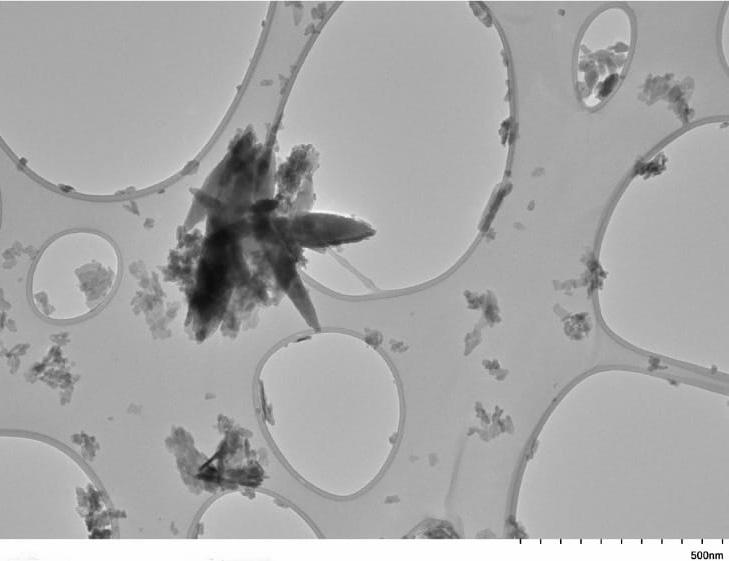
A transmission electron microscopy image showing microplastic and nanoplastic fragments in carotid artery plaque. (Photo courtesy of University of New Mexico)
present in the lungs, liver, placenta, breast milk, urine and blood.
The new research comes on the heels of a study published in February in the journal Nature Medicine revealing the presence of microplastics in brain tissue and a 2024 study in the New England Journal of Medicine that found people whose carotid artery plaque contained microplastics had a higher likelihood of having a stroke, heart attack or dying within three years.
“These new findings add another small piece of data to the growing pile of evidence to guide our thinking on what is the current state of microplastics and nanoplastics in human tissue and give the first glimpse as to what they could be associated with,” Clark said.
In the study, researchers looked at carotid artery tissue samples from 48 people: 35 deceased tissue donors with no plaque; six people whose arteries were more than 80% filled with plaque and who had surgery to clear it but never had symptoms; and seven people whose carotid arteries were more than 50% filled with continued on next page >
“Even if we stopped creating plastics today, these substances continue to break down and bioaccumulate.”
plaque who had surgery to remove the buildup and also had symptoms, which the researchers defined as a stroke, ministroke or temporary loss of vision caused by clogged neck arteries.
People with plaque but no symptoms had an average 895 micrograms of micronanoplastics for every gram of plaque analyzed, compared to 57 micrograms of micronanoplastics for every gram of healthy carotid artery tissue. People who'd had symptoms had 2,888 micrograms of micronanoplastics per gram of plaque.
Among people with a high concentration of plastics in their plaque, researchers noted differences in gene activity in plaque-stabilizing stem cells and less activity in anti-inflammatory genes of macrophages, a type of white blood cell, compared to people with low plastic levels.
“Not only do we see the plastic concentrations correlate with how
dangerous the plaque is for the patient, but these findings may give some insight into why,” said Dr. Kimberly Kicielinski, a cerebrovascular neurosurgeon and an associate professor in the department of neurosurgery at the Medical University of South Carolina in Charleston.
“The findings hint that the white blood cells respond differently in the presence of plastics,” said Kicielinski, who was not involved in the study. “This suggests that the immune process is out of whack.”
Clark said more research is needed before drawing any conclusions about whether the micronanoplastics were destabilizing or accelerating carotid artery plaque formations or affecting the immune system.
“It is far too early to really understand what role these things are playing, if any,” he said. “The microplastics might be inert and simply attracted to areas where other biological things are going on.”
But the fact that micronanoplastics are so pervasive in what we eat and drink that people cannot prevent them from penetrating human tissue is troubling on its own, Clark said.
“And it’s getting worse,” he said. “Even if we stopped creating plastics today, these substances continue to break down and bioaccumulate. That in and of itself should give us some concern. But we don't have any idea what they are doing when they get into our bodies. We are just discovering that they are there.”
To learn more about the American Heart Association’s work in Lehigh Valley, email Development Manager Jessica Escobar-Eck at jessica.escobar-eck@heart.org or visit heart. org/en/affiliates/pennsylvania.
Bathtub to Walk-In-Shower Conversion Experts offer aging in-place bathing solutions
Using the TubcuT® process, One Day Bath cuts out a section of the existing tub wall, then installs a seamless, color-matched factoryappearance step-through, converting any existing tub into a walk-in shower. A shower curtain is all that is needed to keep the water in. Other options and features include:
• Handicapped accessible options meet ADA Standards
• Users keep dignity by maintaining independence in the bathroom
• Customizable opening width to accommodate individual needs
• Reduce falling risk with the low 4” threshold
• Increase safety with professionally installed grab bars, built-in seats and shelves
• Most installations take less than a day minimizing home disruption
• Reversable should the tub need to be restored to its original condition
• TubcuT® can be installed on existing fiberglass, acrylic, steel or cast-iron bathtubs.
• VA Reimbursable in some cases
• Save thousands over complete bathroom remodels, plus a lifetime guarantee
• Also offering bathtub to barrier-free shower conversions and bathtub to low threshold walk-in shower conversions




For more information view our video at RenewYourBath.com or call 866-927-8247 to schedule a free in-home consultation.

The Lehigh County Medical Society (LCMS) has established the Lehigh County Medical Society Scholarship Fund at the Lehigh Valley Community Foundation. This fund will create new opportunities for Allentown School District graduates by giving them a financial boost to pursue education and training in a variety of healthcare fields at Lehigh Carbon Community College (LCCC).
“The healthcare workforce is vital to the well-being of our community,” said representatives of the Lehigh County Medical Society. “Through this scholarship, we’re investing in students who will one day be on the front lines of patient care right here in the Lehigh Valley.”
Three scholarships of $2,500 each will be awarded annually, starting in spring 2026. These scholarships are designed to help students that demonstrate both financial need and academic promise to pursue careers in fields such as nursing, radiologic
technology, and medical assisting. These fields are ones that provide strong career pathways as well as family-sustaining wages in the Lehigh Valley community.
Donors who support this scholarship will help local students achieve their dreams and at the same time, strengthen the future healthcare workforce in the Lehigh Valley.
HOW TO SUPPORT THE SCHOLARSHIP
Community members are invited to contribute and grow the fund:
• Online at https://lehighvalley.fcsuite.com/erp/donate/create/ fund?funit_id=2683
• Through the United Way of the Greater Lehigh Valley campaign. Be sure to designate the Lehigh Valley Community Foundation – Lehigh County Medical Society Scholarship as the desired donation recipient.
The Foundation of the Pennsylvania Medical Society, the charitable arm of the Pennsylvania Medical Society (PAMED), is a pivotal force in sustaining the future of medicine within the Commonwealth. Established in 1954, this 501(c)(3) organization is dedicated to improving the well-being of Pennsylvanians and ensuring that access to medical education remains a core priority. Through its Student Financial Services, the Foundation has become an indispensable resource for aspiring physicians and since 1948 has distributed over $24 million in loans and scholarships to more than 4,700 medical students with financial needs.
The Foundation’s commitment to fostering a new generation of healthcare leaders is most evident in its diverse portfolio of scholarship programs. These opportunities are made possible by the generous contributions of PAMED, its alliances, county medical societies, physician members, and other partners in the medical community. Rather than a single, monolithic fund, the Foundation administers many distinct scholarship funds, each with a unique purpose and set of eligibility criteria designed to address specific needs within the medical student population and the broader healthcare landscape.
One of the cornerstone scholarships is the Foundation Education Award Scholarship, which recognizes students who demonstrate significant economic hardship and a profound commitment to serving medically underserved communities. This scholarship, valued at $8,504 for the 2025-2026 academic year, is a testament to the Foundation’s mission to support future physicians who will make a tangible impact where it is needed most.
Another key offering is the Alliance Medical Education Scholarship (AMES) Fund, which awards multiple $2,500 scholarships to second- and third-year Pennsylvania residents enrolled fulltime in an accredited Pennsylvania medical school. This fund, a legacy of the Pennsylvania Medical Society Alliance, continues to uphold its original mission of supporting promising students from the Commonwealth.
Beyond these broad-based awards, the Foundation provides a range of regionally and academically focused scholarships that serve students from specific Pennsylvania counties. For instance, they administer the LeCoMASE Fund Scholarship for medical students who are residents of Lehigh County. This scholarship is made possible by contributions from the Lehigh

County Medical Auxiliary’s Scholarship and Educational (LeCoMASE) Fund.
Another example is the Myrtle Siegfried, MD, and Michael Vigilante, MD, Scholarship, established in honor of Drs. Siegfried and Vigilante, both of whom practiced medicine in Allentown for over 50 years. This $2500 scholarship is awarded to a first-year medical student who is a resident of Berks, Lehigh, or Northampton County.
These essential scholarships offered by the Foundation of the Pennsylvania Medical Society create opportunities for a wide range of students, ensuring that financial barriers do not impede a student’s journey to becoming a physician and that talented individuals have the financial assistance they need to pursue their medical education. The scholarships are not merely money; they are an investment in the people who will one day lead the charge to improve the health and wellbeing of all Pennsylvanians, securing a vibrant and sustainable future for medicine in the Commonwealth.
To learn more about financial resources offered by The Foundation of the Pennsylvania Medical Society, go to www. foundationpamedsoc.org/.
What I Wish I Knew When I Was Younger
WAYNE
DUBOV, MD
Iam writing this article after an interesting financial discussion at our monthly Lehigh County Medical Society Board meeting. We realized that a topic covering investing and student loans could be supportive for medical students, residents and young physicians starting out in practice.
I am not an investment nor a financial expert, but there is information that I know now that would have been helpful to know earlier in my career. I will share my thoughts, and you can decide whether it is useful for you.
Achieving financial independence (having sufficient wealth to cover living expenses without actively working for income) is an aspiration of many medical students, residents, and physicians, yet it often takes a backseat
to the demanding focus on patient care and everyday life. Short term priorities of essentials like housing and childcare costs leave little money left to funnel into a fund for use 40 years in the future.
Understanding personal finance is crucial for long-term well-being and can significantly affect both your career and home life. One approach that has gained popularity among healthcare professionals is the FIRE movement, which stands for “Financial Independence, Retire Early.” This article will introduce you to the FIRE concept.
I have found that subscribing to the White Coat Investor (WCI)* emails and newsletter is extremely helpful. A physician started WhiteCoatInvester.com because he felt that doctors often lacked the knowledge and time necessary for investing and financial independence. The email sign-up is free, along with access to all prior emails, articles, and podcasts. I would have loved exposure to this resource many years ago. WCI gives practical advice on managing student loans and investing for the long term, with or without a hired financial advisor.
The FIRE movement encourages aggressive saving and investing to achieve financial independence and retire earlier than the traditional retirement age. The core tenets include saving a high percentage of your income by temporarily living below your means; investing wisely in stocks, bonds, and real estate to grow wealth; and exploring streams of passive income to sustain your lifestyle without requiring active work. For medical professionals, who often face high income potential, countered by significant debt, the FIRE philosophy can seem daunting. But it is achievable.
The motivation being that eventual financial independence allows you to work solely for enjoyment. It offers the possibility of reducing work hours to spend more fun time with your family.
WCI has information tailored to healthcare professionals. It provides educational articles, podcasts, and webinars that cover wellness topics, personal finance, investing, and debt management. Their insights into managing student loans include understanding loan forgiveness programs and avoiding common pitfalls. WCI enables informed decision-making by sharing detailed investment strategies, covering options like retirement accounts and tax-efficient methods.
Being part of the WCI community also opens access to like-minded people who share experiences and encouragement on your financial journey. Subscribers can utilize WCI financial tools, like budgeting calculators for retirement projects. Although most of the WCI information is free, there are paid Wellness and Financial Literacy Conferences to attend, and that expense may be covered by your Continuing Medical Education (CME) allowance.
Managing student loans is critical for medical students, who often graduate with overwhelming debt. Familiarizing yourself with the type of loans you have, whether private or federal, is essential for effective repayment strategies. Exploring income-driven repayment plans can help lower monthly payments during residency by adjusting them based on current income. Additionally, if you plan to work in qualifying non-profit or government positions, investigating loan forgiveness programs like Public Service Loan Forgiveness (PSLF) could prove beneficial. When seeking a job, some employers offer loan repayment options, in exchange for a committed period or underserved location of your employment. Once you find yourself in a stable financial position post-residency, consider refinancing your loans for lower interest rates.
When you have a sustainable plan for reducing your debt, it is time to
shift focus toward long-term investing. Starting early is key. The sooner you begin investing, the more you can take advantage of compound interest, allowing even small contributions to grow significantly over time. Aim to start by saving at least 15–20% of your net income. As your income increases and your debt (student loans, mortgage, etc.) decreases, consider saving significantly. Diversifying your portfolio across asset classes, such as stocks, index funds, bonds, and real estate, can help mitigate risk. A simplified but not necessarily the best option, might be a Target Retirement Fund which balances your asset class and risk, based on age and projected retirement date. It is also wise to maximize contributions to retirement accounts like 401(k)s, 403 (b)s, IRAs, and if available, Healthcare Savings Accounts (HSA) and 457 plans, which all offer tax benefits. I found that setting up automatic investment contributions can ensure consistency and help prevent the temptation to overspend. The automation makes saving painless, and it strikes another task off your To Do list.
The journey to financial independence through the FIRE movement can be transformative for medical students, residents, and practicing physicians. By using resources like the White Coat Investor, you can navigate the complexities of student loans and investing, with confidence and great outcomes.
Remember that achieving financial independence is not solely about accumulating wealth: It is about real-life value. There is great joy to be gained in the ability to live life to the fullest, reduce the stress of your practice, and provide better care for your patients. Start today and take control of your financial future!
*I have no arrangement with White Coat Investor and receive nothing for my recommendation.
VANESSA PEREZ WEISS, BCH, FNP, NP-C
Pain is a part of the body’s system, designed to keep one safe and to ensure survival. It’s the signal to the brain that sounds the alert that something needs attention.
Chronic pain is pain that continues to send the pain signal to the brain, like a continuous alarm that is not helpful nor necessary for safety or survival. It reaches into all areas of a person’s life from employment to finances, relationships, hobbies, emotions, sleep and spirituality.
There is neuroscientific evidence that chronic pain can be imprinted in the brain. The perpetual impulses cause a lasting effect that is evidence that the statement “It’s all in your head” may in some ways be true.
Hypnosis offers people hope to regain freedom and comfort. It helps with neuroplasticity, a phenomenon in which the brain grows and adaptively improves given the right conditions and experiences.
Clinical hypnosis helps people manage pain. It is an evidenced based treatment for a variety of problems, including pain management. Hypnosis is a safe, effective means to empower people to feel better and have a meaningful quality of life.
Contact Vanessa Perez Weiss, BCH, FNP, NP-C, at Stream Hypnosis, LLC to learn more: vperweiss@streamhypnosis.com or 570-617-5325.















John Sankari – Class of 2028 | Northampton, PA
Northampton Area High School
Muhlenberg College

Temple/St. Luke’s student John Sankari believes that when it comes to medical care, everyone deserves to feel heard and understood. Sankari views his medical training as a gateway to advocating for those who can’t always advocate for themselves. “There is a place for me in medicine to connect in one-on-one situations, take away the middleman, and make the patient more comfortable,” he says. “I could have gone anywhere and tried to work on the things I really care about, but I’m so glad I had the chance to stay in my hometown for medical school. Here, you can throw out an idea and they’ll try to find a way to help make it happen. I’m so grateful to have the opportunity to learn at Temple/St. Luke’s.”
sluhn.org/SOM