








At UPMC Hillman Cancer Center, we understand the complexity of cancer.
Our expert surgical oncologists in central Pennsylvania collaborate with medical and radiation oncologists, as well as pathologists, to tailor treatment plans for every stage of disease. With specialized expertise across all major cancers, we provide cutting-edge care for:
• Breast and gynecologic cancers
• Endocrine tumors (thyroid and adrenal gland)
• Melanoma and sarcoma
• Pancreatic, hepatobiliary, and gallbladder cancers
• Peritoneal cancers and carcinomatosis
• Upper gastrointestinal malignancies
To refer a patient or schedule an appointment, call 717-988-8451.
UPMC Hillman Cancer Center
2035 Technology Parkway, Suite 201 Mechanicsburg, PA 17050
1703 Innovation Drive, Suite 3136
York, PA 17408

2025 DCMS BOARD OF DIRECTORS
Andrew Lutzkanin III, MD President
Everett C. Hills, MD Secretary/Treasurer
Joseph F. Answine, MD Past President
MEMBERS-AT-LARGE
Michael D. Bosak, MD
Robert A. Ettlinger, MD
John Forney, MD
John D. Goldman, MD
Virginia E. Hall, MD, FACOG, FACP
Saketram Komanduri, MD
John C. Mantione, MD
Mukul Parikh, MD
Gwendolyn Poles, DO
Andrew J. Richards, MD, FACS, FASCRS
Jaan Sidorov, MD
Andrew R. Walker, MD
William Wenner, Jr., MD
EDITORIAL BOARD
Gerard Egan, DCMS Executive Director
Joseph F. Answine, MD, Editor in Chief
Robert A. Ettlinger, MD
Gloria Hwang, MD
Puneet Jairath, MD
Mukul L. Parikh, MD
Meghan Robbins
MEDICAL STUDENTS/ RESIDENTS/PENN STATE AMA REPRESENTATIVES
Denise Ocampo, President
Mariya Starostina



By ANDREW LUTZKANIN, MD, FAAFP
Groups such as the Dauphin County Medical Society mean that you and I don’t have to do it alone.
As physicians, we have all faced challenges over the course of our lives: Passing exams, surviving residency, complex patients, even finding enough free time to pursue our outside interests. This last one has been in greater focus over the past few years as people have become more aware of the burnout in our profession. If you’re like me, you constantly feel the tug and pull of wanting to be there for your patients; doing the things you enjoy; and meeting your obligations to your family. Even now, I sit here dictating this article as I scramble to tidy up loose ends before going on a family vacation that I have been looking forward to for the better part of the last two months.
Now, toss in there my role as a physician leader. Some might look at roles, such as these and say, “If you’re already so busy, why do you volunteer?” Taking the extra time over lunch during a busy clinic day to serve on a committee. Taking time away from family on a weekend to attend a meeting. Putting myself out there for my peers and facing negative criticism, or even worse, silence.
Leadership is hard.
But there is hope. And that hope comes from the community that our medical societies provide. Groups such as the Dauphin County Medical Society mean that you and I don’t have to do it alone.
We can work together to share a vision, advance our priorities, and make things better. And just like seeing my diabetic patients get their sugars under control or watching babies I’ve delivered grow and develop into unique individuals, having the opportunity to serve in a leadership role in a medical society brings me immense satisfaction when I see positive change occur like when we finally get that piece of legislation across the finish line or help a fellow physician in need.
So yes, leadership is hard. Are you up for the challenge?

Ihope this finds you well and that you spent the summer resting and recharging as well as creating new memories from the summer’s adventures!
As we now find ourselves in a transition with fall just around the corner, there is plenty to anticipate, both personally and professionally. For many of us, this time of year is a nostalgic one. It’s a season of fresh starts and new beginnings. We see it in the way kids—and some of us older students—prepare for the new school session, maybe even with that wonderful, familiar smell of new books (or perhaps now, the shiny gleam of new laptops and whiteboards). We feel the excitement in the air as we cheer on our favorite baseball team that made it to the postseason and, of course, with that big Pennsylvania tradition and the thrill of getting pumped for collegiate and Eagles football!
Just as a new season brings fresh energy to our personal lives, there is also much happening within our Pennsylvania Medical Societies. Front and center is the upcoming House of Delegates (HOD) meeting in October. The HOD is not just another meeting; it is your opportunity to directly shape PAMED’s leadership, governance, and agenda. This is where your voice
matters most, where your professional insights and experiences become the building blocks for our collective future. To that end, I urge you to take some time to review all the information and materials available regarding the HOD. The decisions made here will directly impact our profession and the well-being of our patients across the state.
We’re also thrilled to share the latest issue of Central PA Medicine Magazine, which continues to be an outstanding platform for member voices. In this issue, you’ll find a rich array of timely and thought-provoking articles:
• Leadership is Hard, an important message from the Dauphin County Medical Society President.
• An exploration of the transformative benefits of walking with a doctor, a paradigm shift in the doctor/patient relationship.
• The new entry in our Interview with a Physician series: Kenneth Conner, MD.
• A restaurant review of Benaiah’s Wood Fired Kitchen, one of the newest culinary ventures by Chef Scott Kemp.
• Plus, much more!

Remember, the magazine is always seeking new content—from research and opinion pieces to achievements and reflections. This is your platform. Share your voice and enrich our professional community.
Your dedication and commitment to DCMS are the driving force behind everything we do, and for that, I am deeply grateful. Your active participation ensures that our society remains relevant, responsive, and truly representative of the physicians it serves. Together, we can build a stronger future for medicine in Pennsylvania. Thank you for your ongoing support!
HOW STROLLING SIDE-BY-SIDE CAN REVOLUTIONIZE PATIENT-DOCTOR DIALOGUE AND WELLBEING

By EVERETT C. HILLS, MD, MS

The concept is delightfully simple: instead of sitting across from each other in an office, the patient and doctor walk side-by-side, engaging in open dialogue about health.
In these current times, healthcare often conjures images of sterile exam rooms, brisk appointments, and hurried conversations between doctor and patient. Yet, a quiet revolution is taking place—one that reimagines the traditional consultation by taking it outside, onto winding trails or leafy sidewalks. Walking with a doctor to discuss health issues, sometimes called a “walk-and-talk” appointment, is gaining momentum as a dynamic and holistic way to approach healthcare. This practice goes beyond mere novelty; it offers profound benefits for patients and doctors alike, fostering a deeper, more collaborative, and health-promoting relationship.
THE EVOLUTION OF THE WALK-AND-TALK APPOINTMENT
The idea of walking while speaking to a doctor is not new, but in recent years it has become more structured and widespread. Inspired by initiatives like “Walk with a Doc”—a global movement started by Dr. David Sabgir in 2005—these walking consultations have begun to challenge the sedentary norm of medical appointments. The concept is delightfully simple: instead of sitting across from each other in an office, the patient and doctor walk sideby-side, engaging in open dialogue about health.
THE PHYSICAL BENEFITS: MOVEMENT AS MEDICINE
One of the most obvious advantages of walking during a medical consultation is the direct impact on physical health. Movement is a cornerstone of wellness, and walking is an accessible, gentle form of exercise suitable for most people.
• Joint and Musculoskeletal Benefits: Regular walking helps to lubricate joints and maintain mobility. Discussing issues like arthritis or chronic pain while walking allows the doctor to observe the patient's gait and physical limitations in real time.
• Enhanced Metabolism: Walking can help manage weight, regulate blood sugar, and improve overall metabolic health. It models healthy habits, reinforcing the advice doctors often give verbally.
• Reduced Sedentary Time: Traditional appointments can contribute to a sedentary lifestyle. By walking, both patient and doctor directly counteract the risks associated with prolonged sitting.
THE PSYCHOLOGICAL BENEFITS: FRESH AIR, OPEN MINDS
Beyond the physical, the psychological advantages of walking outdoors are profound and well-documented.
• Reduction in Stress and Anxiety: Natural settings and movement have been shown to reduce cortisol levels, ease anxiety, and promote a sense of calm. Patients may feel more relaxed and open to discussing sensitive topics.
• Boost in Mood and Cognitive Clarity: Exposure to daylight, greenery, and rhythmic movement can elevate mood and sharpen focus, resulting in more effective communication and problem-solving.
• Improved Cardiovascular Health: Even a short, moderate-paced walk can help lower blood pressure, improve circulation, and strengthen the heart. For patients with cardiovascular concerns, a walk with the doctor can serve as both assessment and therapy.
• Breaking Down Barriers: The sideby-side format of walking can feel less confrontational than the face-to-face setup of an exam room, making it easier
Continued on next page
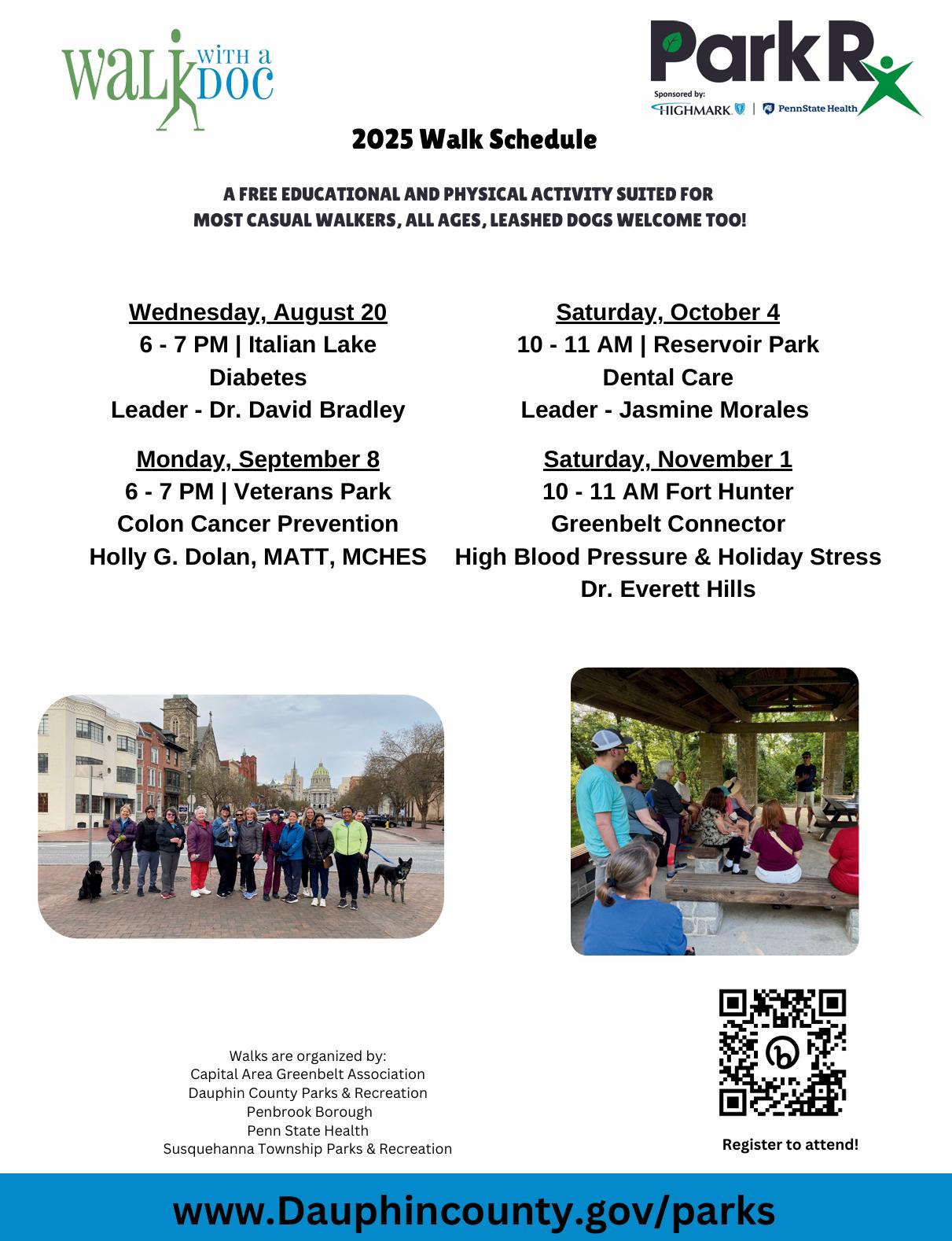
A free educational and physical activity suited for most casual walkers, all ages, leashed dogs

10 to 11 a.m. I Reservoir Park
High Blood Pressure & Holiday
Scan the QR code below, or visit DauphinCounty.org/parks

for patients to share concerns they might otherwise withhold.
Capital Area Greenbelt Association
Dauphin County Parks & Recreation
Penbrook Borough
Penn State Health
Susquehanna Township Parks & Recreation
• Greater Engagement: The novelty and informality of the setting often lead to more genuine, free-flowing conversations, deepening the therapeutic alliance between doctor and patient.
The doctor-patient relationship is the foundation of effective healthcare. Walking together transforms this relationship in subtle but meaningful ways.
• Equal Footing: By literally walking side-by-side, the traditional power dynamics of the exam room are softened. Patients may feel less intimidated, and doctors more approachable.
• Active Listening: Without the distractions of computers, beeping devices, or paperwork, doctors can focus more intently on their patients’ words, body language, and emotional cues.
• Observation in Action: Doctors can observe their patients’ mobility, stamina, and breathing patterns, providing valuable diagnostic clues that might be missed in a static setting.
• Building Trust: Shared activity fosters a sense of camaraderie and trust, essential components for honest dialogue and better adherence to treatment plans.
EMPOWERING PATIENTS: TAKING HEALTH INTO THEIR OWN HANDS
Walk-and-talk appointments empower patients, turning passive recipients into active participants in their own care.
• Modeling Healthy Behavior: When doctors walk with their patients, they demonstrate a commitment to lifestyle medicine, inspiring patients to incorporate more movement into their daily routines.
• Motivating Change: The act of walking together makes the benefits of exercise tangible, motivating patients who may be ambivalent about physical activity.
• Personalized Guidance: Doctors can tailor advice based on real-time observation, offering practical tips on posture, movement, and overcoming barriers to exercise.
• Patient Autonomy: The informal setting invites questions and dialogue, encouraging patients to voice their concerns, preferences, and goals.
While the benefits are many, “Walk with a Doc” is subject to weather conditions; walk-and-talk is not suitable for bad weather days. Registering to attend a “Walk with a Doc” is highly encouraged in the event a scheduling change is necessary. All “Walk with a Doc” sessions start with a brief topic-driven presentation generally not longer than 10-15 minutes. The presentation is followed by
a walk of approximately two miles through a local park. Walkers are encouraged to ask any questions of the physicians (Hint—I often like to tag back with the slower walkers to make sure they feel included). Sensitive exams and procedures, of course, still require traditional consultation rooms. Specific medical advice is generally not given in these walks.
Walking with a doctor to talk about health issues is more than a pleasant diversion; it’s a transformative approach that puts movement and connection at the heart of healthcare. By stepping outside the walls of the exam room, doctors and patients open the door to richer conversations, better understanding, and improved wellbeing. Whether it’s a short stroll or an extended walk, the journey can lead to healthier lives—one step, and one conversation, at a time. If you are a physician and interested in conducting a walk in 2026, please contact Nancy Gates with the Dauphin County Parks & Recreation Department (717-599-5188, ext. 2113) or Doug Knauss with the Susquehanna Department of Parks & Recreation (717-909-9278).

https://www.qualityinsights.org/stateservices/


By EVERETT C. HILLS MD, MS
This article is the second in a new series of interviews with physicians who belonged to the Dauphin County Medical Society, in an effort to learn more about the doctors who have spent their entire life practicing medicine in central Pennsylvania and to share their stories with the readership. With ever-constant changes occurring in the practice of medicine, it is helpful and instructive to learn how early medical practices developed, particularly in our own medical community. What better way is there to learn about the rich history of medicine than to talk with colleagues who had a hand in creating it?
With those thoughts in mind, it was a distinct pleasure to talk with Kenneth Conner, MD, retired internist and past president of the Dauphin County Medical Society (2000-2003). During our conversation in May 2025, I asked Ken to reflect on his journey towards becoming a physician and who had the biggest influences on him. For him, it was his physician uncles and later on, it was his mentor and professional colleague Dr. Kenneth Quikel, MD (1909-2002).
Ken Conner is a native Pennsylvanian who grew up in Richboro, Bucks County, born five minutes after his twin sister, and alongside her, the oldest of four siblings. Even though his father was a mechanical engineer and his mother was an elementary school teacher, Ken was drawn to medicine by his two uncles (one an ophthalmologist and the other an anesthesiologist). He attended Ursinus College and was accepted to Hahnemann Medical School in Philadelphia where he earned his medical degree in 1968.
Ken met his wife in a unique fashion: one of his physician uncles gave tickets for a social event at a local county club to Ken (in medical school at the time) and a young nursing student. They married during his junior year of medical school. Ken was leaning towards the field of internal medicine and preparing for a rotating internship at Harrisburg Hospital. This is a good point in the story to introduce Dr. Kenneth Quickel.
Dr. Quickel, who opened his Harrisburg medical practice in 1936, and specialized in cardiology, had been an instructor at Hahnemann Medical School. He bought one of the first electrocardiograph machines in Harrisburg which at the time were large and bulky and used suction cups. In 1965, Dr. Quickel established the first coronary care/intensive care unit in Harrisburg Hospital consisting of 16 beds divided evenly between cardiac and general illness patients. Three years later, Dr. and Mrs. Conner moved west to Harrisburg where he began his rotating internship at Harrisburg Hospital and the two Kens made each other’s acquaintance. Upon finishing his internship, however, Dr. Conner was obligated by the Berry Program to serve two years of active duty military service which he performed in Korea from 1969-71 as a general
Continued on next page


medical officer for an artillery unit and, upon his return, as a medical screening physician in the Armed Forces Induction Center at the New Cumberland Army Depot. After his military discharge, Dr. Conner completed his internal medicine residency at Harrisburg Hospital and, along with Dr. James Rich, joined Dr. Quickel to open a group practice on the West Shore in Camp Hill, PA.
During this period, he was on staff at multiple hospitals, rehabilitation hospitals, and half a dozen or more nursing homes. He kept regular office hours for outpatients; saw patients in the emergency departments of the local hospitals; and even made house calls, which was an expectation of their clinical duties as Dr. Quickel was still making house calls until his retirement in the mid-1980s.
Early in his career, Dr. Conner was encouraged by colleagues to join the Medical Bureau of Harrisburg. The Medical Bureau was the method in those days for reaching physicians on call, before beepers became available. He recognized the importance of engagement with referring sources and the importance of involvement in organized medicine by joining county, state, and national medical organizations. Ken progressed through leadership positions beginning with Secretary/Treasurer and became the vice-president of the Dauphin County Medical Society (DCMS) under Scott Gunder, MD. When Dr. Gunder succumbed to cancer, Dr. Conner assumed the presidency of the DCMS in May 2000, finishing out the term, and then served a full second term from 2001-2002.
Dr. Conner continued practicing medicine until 2014 when UPMC bought the Connor-Rich Associates medical practice. His wife, Susan Conner, passed away in 2010. For many years, Ken remained active with the Scott Gunder, MD/Dauphin County Medical Society Scholarship Fund committee, a fund that presents a financial award to a sophomore medical student from the Penn State College of Medicine.
Since retirement, Ken remains busy with his immense family of nine children,
16 grandchildren, and three great-grandchildren. He and his partner Donna make it a point to gather the local family together weekly for brunch and to take them to the shore for a week in the summer. Ken continues his involvement with the Rotary Club; he partakes in a frequent gathering of retired physicians dubbed the “Over the Pill Gang,” and he is a member of the Diplomats of Harrisburg, a physician social organization. Ken and Donna take daily walks, and regularly attend the Harrisburg Symphony Pops and Hershey Symphony Series. Ken enjoys keeping his mind engaged with Sudoku and reading mystery stories.
Besides the two uncles in his family, Dr. Connor singled out Dr. Quickel as one of the largest influences, admiring him for his personal touch and for his philosophy of “putting the patient first,” which remains his guiding principle to share with young physicians. Dr. Conner also spoke favorably of Ray Grandon, MD, who understood the importance of forming relationships in the political area and of knowing people in the local, state, and national organizations who create policies and advance the practice of medicine. He spoke highly of George Jackson, MD, a specialist in nuclear medicine whose qualities of being a downto-earth teacher and physician rubbed off on Ken and helped form his core belief in his chosen calling to take care of people.
WHAT WERE THE BIGGEST CHANGES YOU OBSERVED IN YOUR MEDICAL CAREER?
Medicine, as Dr. Conner saw it, changed most dramatically with the decline in quality of the “personal touch.” As an internist, Dr. Conner recalled taking care of several generations of patients all in the same family. He kept track of family events in his outpatient notes and would call those events to mind with each succeeding patient encounter. These bits of history helped to foster a strong personal bond.
Change is inevitable and to Ken, it was interesting to hear his recollection of the advent of hospitalists. He talked about the days when ward services were comprised of patients who did not have a personal physician. These patients were served by resident physicians with oversight from attending physicians. When hospitalists started arriving on the scene, they picked up this role of managing inpatients. Early in the transformation of inpatient care, hospitalists started using the electronic medical record to chart patient progress. Then, along came intensivists and nocturnists to handle increasingly large numbers of patients, thus freeing up private practice physicians from having to round on their patients in the hospital.
Dr. Conner recognized the financial challenges to maintaining a private practice and the purchase of medical group practices. His practice joined Heritage Medical Group along with several other private practice groups to consolidate the business aspects of running a medical practice. Eventually many of these group practices would be purchased by larger health care systems. To Dr. Conner, the transformation of the practice of medicine was
an expected evolution. He cautions that there remain important axioms of medicine to be passed on to each succeeding generation.
WHAT ADVICE WOULD YOU GIVE YOUNG PHYSICIANS-IN-TRAINING?
Dr. Conner’s advice to the next generation of physicians:
1. Listen to the patient.
2. Have empathy for the patient.
3. Do a physical examination.
4. Explain in terms patients can understand.
Thank you, Dr. Ken Conner, for an enjoyable afternoon of conversation, for your perspective of medicine in a fulfilling career of service to our community, and for these wonderful words of wisdom. To the reader, ask yourself—who have I met that has made a major impact on my life and career? Take a moment to reflect on these words of advice, too.
(Additional information about Kenneth Quickel, MD, comes from the Patriot-News, November 11, 2002, Obituary)

Our Health Innovations Program is improving health outcomes by connecting our emergency network with healthcare providers.
Interested in helping? Contact us at info@centralpafoodbank.org

SUMMARY OF HEALTH CARE PROVISIONS AND PENNSYLVANIA IMPACT

On July 4, 2025, President Trump signed H.R. 1, the “One Big Beautiful Bill Act,” into law. The legislation includes sweeping changes to federal health care programs, most notably Medicaid and the Affordable Care Act (ACA), with significant long-term implications for states like Pennsylvania.
PAMED submitted a letter to Pennsylvania’s U.S. Representatives, Rep. Robert Brenshan and Rep. Brian Fitzpatrick, expressing concern over the bill’s projected impacts. PAMED also submitted a letter to Governor Josh Shapiro and made a statement following the vote on its worry for patients in Pennsylvania.
While full fiscal modeling is still underway at the state level, several key provisions already raise red flags for access to care and Medicaid sustainability across the Commonwealth.
NATIONAL AND PENNSYLVANIA COVERAGE & FISCAL IMPACT ESTIMATES
• $1 trillion cut to federal Medicaid funding over 10 years (CBO).
• 17 million individuals nationally projected to lose coverage through Medicaid and ACA marketplace rollbacks (CBO).
• 3 million Pennsylvanians currently receive Medicaid, including:
• 1.3 million children
• 123,000 people with disabilities
• 312,000 individuals over age 65
• 10,000 veterans
• Over 310,000 Pennsylvanians are projected to lose Medicaid coverage under H.R. 1, with disproportionate impact on rural and low-income populations.
• Approximately 200,000 Pennsylvanians could lose coverage due to new Medicaid work requirements for adults ages 19-64.
• Six-month eligibility redetermination cycles, down from the current annual process, are estimated to affect 110,000 individuals and cost the
Commonwealth $18 million annually to administer (requiring around 250 new state staff).
• Changes to the provider tax structure starting in fiscal year 2028-29 could cut over $20 billion in Medicaid funding for Pennsylvania over the next 10 years.
Note: Additional state-level fiscal impacts are still being calculated as budget negotiations continue.
RURAL HEALTH RISKS
• At least 25 rural hospitals in Pennsylvania are at risk of closure under Medicaid and provider tax changes. These facilities already operate at financial deficits and depend heavily on Medicaid reimbursements.
• While H.R. 1 establishes a $50 billion Rural Health Fund (2026-2030), PAMED remains concerned that this funding will not offset the deep federal cuts jeopardizing rural care access.
PHYSICIAN PAYMENT AND PRACTICE IMPACTS
• A 2.5% Medicare physician payment increase is scheduled for 2026, but this does not address current payment shortfalls or stop pending sequestration cuts.
• Medicare sequestration cuts will increase to 4% from 2026-2034, compounding existing strain on physician practices.
• PAMED remains concerned about the long-term effects on physician recruitment, practice viability, and access to care, particularly in underserved areas.
PAMED continues to work closely with health care partners and state officials to analyze the fiscal implications and advocate for protection for patients and physicians.
For more information about advocacy priorities for PAMED, go to https://www. pamedsoc.org/advocacy-priorities.
This article was originally published in The Dose, PAMED’s e-newsletter.
By JOSEPH ANSWINE, MD, FASA
OPINION ARTICLE: This article is intended to make you laugh. If I offend anyone, I sincerely apologize.
Iwas born at the tail end of the Baby Boomer generation. I grew up with mantras such as “Sticks and stones can break your bones, but words will never hurt you,” “Snitches get stitches,” and “Life isn’t fair.” When I went to medical school, another one was added by a cardiac surgeon: “Your mother is the only one who loves you, and she can’t help you here.” Those sayings gave me perspective throughout my life. They helped me during those times when I was asked whether I considered other careers or if I read comic books or textbooks to prepare for the day. My answers were “yes” and “on occasion.”
But you move on.
As a Baby Boomer, I like just getting a job to do and do it. I really don’t need feedback at the end of the day. No, I don’t want to do a group project. I have no interest in calling a meeting. And I only “zoom” if I have too much coffee.
But I am now the oldest of multiple generations working together in medicine. And, as an older physician, I am struggling with fitting in with my younger, more “sensitive” colleagues. Actually, I always considered myself a sensitive guy. I like dogs and cats, and I do sometimes smell the flowers. Not much though. The pollen gets me. But I am frequently called to the “principal’s office” for something I said, did, or wrote in an email.
First and foremost, I never liked bullies, and I never was one. A bully is someone struggling with deeply rooted insecurities that compel them to act like fools. Some grow up to regret their bullying ways, and some just fade into beer-belly obscurity. Instead, I like to make people laugh a little in this tough healthcare world.
Usually, my offensive activity is my attempt to add a little humor to whatever point I’m trying to make. But, it never fails. Joe, can you come to my office please? That question then triggers a need to scour my brain for whatever I said or wrote during the last week or so. There are so many possibilities that I give up and wait to be told which deed, whether spoken or typed, created a need for a meeting. Honestly, I never worry if I offend someone anymore. Why worry about “if” since I know I offended someone?
Of interest is that most of the time, the intended target of my humor isn’t the individual offended. It is someone who overheard something I said or possibly was told about something I wrote about someone else. My first thought is, why are you eavesdropping on my conversation, or obsessing over a joke that wasn’t about you?
Furthermore, you can talk to 30 people, entertain 29, offend 1, and get in trouble. Yes, I know. Everyone’s opinion means something. Could it be possible that that one opinion is, let’s say, wrong? Nope! I’m guilty until proven…..
No, I’m guilty. 29/30 or 96.7% success rate at being funny but guilty as charged.
I’m always told that I cannot talk to my accuser. Accusers are anonymous. I am told that I can’t even attempt to tell him or her I am sorry. I really don’t have an interest in saying I am sorry. I just want to ask the individual why it wasn’t funny. Striving for 100%, over-achiever.
Sometimes, the emails are printed out and shown to me. I read them, and say “Yes, that’s funny.” Then I look up and realize “I’m in trouble again.”
Before we go any further with this flight of ideas, what actually is the purpose of HR anyway? I thought the “Human Resources Code” involves fostering a positive work environment. They never make me feel “positive.” And, what and where is this file that is continuously being added to with each invite to “a meeting”? I imagine a file cabinet with a sticker on it that says “Joe.”
I have developed a list of protective statements when accused that I will share if you ever need them:
1. “No, that’s definitely not me.”
2. “Does this have something to do with my age?”
3. “Darn, my email was hacked again.”
4. “Why are we here again? I forget sometimes.”
5. “I’m represented by Dewey, Cheetum, and Howe, attorneys at law.”
6. “Am I allowed to be offended that someone is offended?”
7. “Do you have any cookies?”
8. “I like squirrels.”
9. “Do you need a hug?”
10. “I understand. This is definitely the last time you will see me in here.”
When I leave the meeting, I really plan to do better. However, when I find myself at the end of a “sterile” email or pleasant conversation, there is that feeling of unfinished business, that annoying little voice in my head that says “Yea, go for it.” Then in a few days, I get a call.
I think my biggest question is whether when I die, are my files protected or does God have access to them?
This editorial was an attempt at humor. Remember the 1st amendment. “Thou shall not kill the messenger.”




By JOSEPH F. ANSWINE, MD, FASA
The patient was a 45-year-old female taken to the operating room for emergent exploratory laparotomy for bowel perforation. Her past medical history was significant for hypertension, morbid obesity with a BMI of 44, and previous abdominal surgery for diverticulitis. Induction of anesthesia and endotracheal intubation occurred without difficulty.
The procedure was complicated due to significant intraperitoneal adhesions. At the end of the procedure, exchanging an orogastric tube to a nasogastric tube proved difficult, however, the tube placement was successfully performed utilizing a laryngoscope as a guide. No other complications were noted.
Due to inadequate tidal volumes and poor respiratory effort, the patient was taken to the recovery area intubated and ventilated with an Ambu bag. Vital signs prior to transport were stable.
Upon arrival to the recovery area, it was noted that she was tachycardic and hypotensive. This quickly deteriorated into pulseless electrical activity. Advanced life support was initiated with chest compressions and epinephrine administration. Fluids were administered rapidly, assuming significant blood loss. During the resuscitation, decreased breath sounds were noted bilaterally. Appropriate endotracheal tube placement was verified. Thoracic needle decompressions were done bilaterally due to the clinical diagnosis of bilateral pneumothoraces. Bilateral chest tubes were placed. Eventually, return of circulation occurred. Chest x-ray confirmed the pneumothoraces. Subcutaneous emphysema was noted on physical examination. Despite the efforts, the patient never regained consciousness and passed away 2 days later.
The question is: “What caused the bilateral pneumothoraces eventually leading to the patient’s arrest and death?”
The only thing that was emphasized on the anesthesia record was difficulty in placing the nasogastric tube intraoperatively. This occurred at the end of the procedure. Esophageal perforation, however, was ruled out prior to the patient’s death. Furthermore, the tension pneumothoraces did not become evident until PACU arrival.
Answer: “Bilateral pneumothoraces due to gastric tube trauma.”
On review of the literature, pneumothorax is the most common pulmonary complication from nasogastric tube insertion. Furthermore, it occurs more commonly from inadvertent bronchial placement rather than esophageal perforation. A cuffed endotracheal tube turns out to not be as large of a deterrent for bronchial placement as we commonly think. The cuff is easily passed. Furthermore, it frequently occludes the esophageal opening making appropriate placement more difficult. Also, it has been noted that once you pass a nasogastric tube into the trachea, a second inadvertent placement is much more common. Multiple passes would be required to cause bilateral pneumothoraces. Once in the trachea, bronchial perforation is relatively easy because of the stiffness of a nasogastric tube. (1)
My assumption as to why the tension pneumothoraces did not become evident prior to transfer is because the peak inspiratory pressures generated by the anesthesia machine were kept low (usually about 20 mmHg). But those generated by the positive
pressure ventilation via the Ambu bag were significantly higher and much more difficult to control. Furthermore, the higher airway pressures required as the tension pneumothoraces worsened may have been easily overlooked, however, more forceful squeezing of the bag would be needed without prompting an alarm as would occur with the anesthesia machine.
Cardiovascular compromise is a common and expected secondary complication of tension pneumothoraces.
The subcutaneous emphysema was secondary to the tension pneumothoraces. Pneumothoraces are one of the most common causes of subcutaneous emphysema of the chest, neck and face.
1. J. B. Pillai, et al. Thoracic complications of nasogastric tube: review of safe practice, Interact CardioVasc Thorac Surg 2005;4:429-433. doi:10.1510/icvts.2005.109488
© 2005 European Association of Cardio-Thoracic Surgery
By ROBERT ETTLINGER, MD
Following the departure of Koda at Union Station early in the pandemic, the earthy aroma of a wood-fired grill has returned with Benaiah’s. Located in a townhouse development off Union Deposit Road near Nyes Road, Chef Scott Kemp has continued the eclectic concepts of his former kitchen at Cafe Fresco. The name Benaiah is from the bold protector of Kings David and Solomon, and the chef strives for boldness in his cooking.
Many of the creative dishes, especially the fish and beef (plus the broccolini served with many of the entrees), are perfectly charred with the right amount of smoke. Before dinner, enjoy a selection of wines and non-alcoholic cocktails (a rising choice among Gen Z diners, they say), or one of the creative cocktail offerings. King of the Mule had rye, blood-orange infused triple sec, basil/grenadine syrup and cold ginger beer. Warm bread easily melted the mixed berry butter.
Appetizers include crab fries, Shoya deviled eggs, wood grilled shishitos (blistered roulette peppers topped with bulgogi sauce), and fried green tomatoes served with fresh burrata cheese and duck-fat focaccia. Hand-rolled pastas include crab fettucine, with charred sweet corn and roasted cherry tomatoes. The smoked garlic Caesar salad featured grilled, not chilled, romaine; what a difference it makes!
Beef entrees include a filet with a fig glaze; a 16-ounce bone-in Angus ribeye with moody bleu compound butter and cremini mushrooms; and an attractive marinated pepper flank steak with a scallion relish pyramided over steamed rice. Crispy grilled salmon is glazed with Harissa citrus on a pearl couscous salad, and the ahi tuna poke bowl with sushi rice has sweet, salty, and pickled garnishes with a tangy gochujang aioli. The meatloaf is nothing like your mama’s, smoked and roasted with a sweet and savory onion glaze on a creamy bed of mac and cheese.

Room for dessert? You wish! PB&J Cheesecake with a peanut graham cracker crust and a Concord grape reduction, or warm butter cake with macerated strawberries and vanilla ice cream.
Casual dining is next door and across the street, with two brewpubs and Shakedown BBQ (late of the neighborhood near Hollywood Casino). But a night at Benaiah’s (or a weekend brunch if you prefer) is worth the trip.
BENAIAH’S WOOD FIRED KITCHEN
8001 Union Station Blvd., Harrisburg 17111 717-982-6003












At MADJ, we specialize in helping medical practices and health systems of all sizes thrive in competitive landscapes. From small beginnings to significant success, our tailored strategies have transformed healthcare providers into community cornerstones.

Here, the most talented minds and most compassionate hearts unite for lifesaving results. In collaboration with Johns Hopkins Medicine Kimmel Cancer Center, our cancer patients have access to expanded clinical trials, world-class second opinions and advanced genomics. This will bring the next generation of care to our community — all delivered by our dedicated team who cares from the heart.
Learn more at WellSpan.org/Cancer