








At UPMC Hillman Cancer Center, we understand the complexity of cancer.
Our expert surgical oncologists in central Pennsylvania collaborate with medical and radiation oncologists, as well as pathologists, to tailor treatment plans for every stage of disease. With specialized expertise across all major cancers, we provide cutting-edge care for:
• Breast and gynecologic cancers
• Endocrine tumors (thyroid and adrenal gland)
• Melanoma and sarcoma
• Pancreatic, hepatobiliary, and gallbladder cancers
• Peritoneal cancers and carcinomatosis
• Upper gastrointestinal malignancies
To refer a patient or schedule an appointment, call 717-988-8451.
UPMC Hillman Cancer Center
2035 Technology Parkway, Suite 201 Mechanicsburg, PA 17050
1703 Innovation Drive, Suite 3136
York, PA 17408
Ihope this note finds you well and that you are taking a moment to enjoy the vibrant, colorful beauty of the Pennsylvania natural landscape this fall. It’s a wonderful time to take advantage of an energizing hike or a refreshing kayak paddle—just the thing to boost the spirit and perhaps, as the doctor ordered, make you feel better!
As the leaves turn, we’re also turning the pages on another exciting and productive year for both the Dauphin County Medical Society (DCMS) and the Pennsylvania Medical Society (PAMED). We’ve seen significant progress across our shared governance and initiatives aimed at supporting your pursuit of delivering excellent patient care throughout the region.
Congratulations to DCMS’s own Dr. Sean Mahase and Dr. Seyed Mansuri, both of whom are two of PAMED’s 2025 Top Physicians Under 40.
Our final and arguably most inspiring task for the year is fast approaching: the selection of the 2025 recipient of the Scott A. Gunder, MD, DCMS Presidential Scholarship. Thanks to the extraordinary generosity of the Gunder family last year, which we highlighted in the Fall 2024 issue of Central PA Medicine, this year’s award amount is set to be more than double what we awarded previously. This scholarship truly embodies the spirit of supporting the future of

medicine in Central Pennsylvania, a legacy that Dr. Gunder championed. Please stay tuned for a future update where we’ll proudly announce the exceptional student selected as our 2025 recipient.
The strength of our organizations is driven by you, our dedicated members. We are always actively looking for your input regarding activities, governance issues, and the specific resources you need to navigate the ever-evolving healthcare landscape and excel in patient care. Please don’t hesitate to reach out with your insights.
Furthermore, remember that Central PA Medicine is your professional platform. It remains readily available for you to share your insightful research, celebrate professional accomplishments, offer reflections on the practice of medicine, or voice your opinion on key issues affecting our community. We encourage you to utilize this valuable resource to connect with your peers.
Thank you, once again, for your deep commitment and continued support of our societies and our shared mission.
Wishing you and your families a wonderful, restful and rejuvenating Thanksgiving and Holiday season ahead. See you in 2026!

Fulton Mortgage Company has designed a mortgage program dedicated to making homeownership easy and affordable for medical professionals1 including Physicians, Pharmacists, Dentists, Veterinarians, and Podiatrists. If you have a medical doctorate degree, this program may work for you.
• 100% financing 2 available for loan amounts up to $1.5 Million
• 95% financing 2 available for loan amounts up to $2 Million
• 90% financing 2 available for loan amounts up to $3 Million
• Mortgage Insurance not required
• Up to 6% seller paid closing cost 3 and prepaids allowed
• Gift funds are allowed from immediate family members
• Student loan payments that are deferred for 12 months or longer are not included in the credit approval process
• Find and close on new home up to 90 days prior to start of new employment
• 30 & 15 Year Fixed Rate 4 as well as Adjustable Rate5 Options (5/6, 7/6, 10/6, & 15/6)
NMLS# 615627
717.418.0982
rhilgers@fultonmortgagecompany.com
NMLS# 1026538
717.658.7103
ecoldsmith@fultonmortgagecompany.com
NMLS# 490247
717.265.5955
dlord@fultonmortgagecompany.com
rbrennan@fultonmortgagecompany.com
NMLS# 1617043
717.580.5097
nshenk@fultonmortgagecompany.com

2025 DCMS BOARD OF DIRECTORS
Andrew Lutzkanin III, MD President
Everett C. Hills, MD
Secretary/Treasurer
Joseph F. Answine, MD Past President
MEMBERS-AT-LARGE
Michael D. Bosak, MD
Robert A. Ettlinger, MD
John Forney, MD
John D. Goldman, MD
Virginia E. Hall, MD, FACOG, FACP
Saketram Komanduri, MD
John C. Mantione, MD
Mukul Parikh, MD
Gwendolyn Poles, DO
Andrew J. Richards, MD, FACS, FASCRS
Jaan Sidorov, MD
Andrew R. Walker, MD
William Wenner, Jr., MD
EDITORIAL BOARD
Gerard Egan, DCMS Executive Director
Joseph F. Answine, MD, Editor in Chief
Robert A. Ettlinger, MD
Gloria Hwang, MD
Puneet Jairath, MD
Mukul L. Parikh, MD
Meghan Robbins
MEDICAL STUDENTS/ RESIDENTS/PENN STATE AMA REPRESENTATIVES
Denise Ocampo, President
Mariya Starostina


20 The Gunder Family Makes Substantial Contribution to Grow the Scott A. Gunder, MD, DCMS Presidential Scholarship

By JOSEPH F. ANSWINE, MD, FASA
The patient is a 35-year-old female. She underwent a dilatation and curettage (D&E).
Vital signs on admission that morning were as follows: Temperature 98.6 degrees F, pulse 84 beats per minute, respirations 16 breaths per minute, blood pressure 114/75 mmHg, arterial oxygen saturation 97%, height 5 ft 5 in, weight 187 lbs., BMI (calculated) 31.12 kg/m2. Her past medical history and pre-operative state by anesthesia review: American Society of Anesthesiologists physical status 2 (mild disease), gastroesophageal reflux disease (mild with food), previous C/S and D&E, no known drug allergies, no significant cardiac or pulmonary disease known, and appropriate preoperative fasting.
Physical examination noted no abnormalities in cognition/cardiac/ pulmonary areas. The hemoglobin was 14.5 g/dl, and the platelet count was 287,000/microliter. Other laboratory results of significance were urinalysis positive for glucose >500 mg/dl, protein 100 mg/dl, and positive HCG; as well as a positive urine qualitative toxicology screen for benzodiazepines.
An intravenous line was placed, and she arrived in the operating room.
As per the anesthesia record: Anesthesia start time was listed as 0730. She was given supplemental oxygen at a rate of 4 liters/minute. The initial vital signs in the operating room were blood pressure 127/71 mmHg, pulse 82 beats per minute, respiratory rate 16 breaths per minute, and arterial oxygen saturation 100%. Versed (midazolam) 5 mg was given IV in divided doses over 10 minutes (0730-0740). Fentanyl IV 100 ug was given at about 0740. A total of 150 mg of propofol IV was given in divided doses. Lidocaine 200 mg via pericervical block (by the surgeon) (0746) and 100 mg IV (approximately 0740) was given during the case. Zofran 4 mg and Toradol 30 mg were given IV. And Cefazolin 2 gm IV was given at 0745. The surgical procedure started at 0747 and was completed at 0750.
Vital signs were noted to be stable throughout the case with arterial oxygen saturation of 100%, blood pressure ranging from 100-120/60-96 and end tidal CO2 +30 and +30. The total fluids given were 500 milliliters.
Out of room was listed as 0758.
The patient was then transferred to the recovery. She was transported with oxygen and monitoring. She was stable on transport.
On arrival to the PACU, which was listed as 0758, she was noted immediately by the PACU nurse to be unarousable with no noted respirations. Arterial oxygen saturation was not analyzable at that time and bradycardia (37 beats per minute) was noted by the monitor. There was no pulse by palpation of the carotid artery, however, there was a documented blood pressure of 62/28 mmHg. Bag mask ventilation was started as well as chest compressions and a code called by most accounts immediately upon noticing the unstable situation. The start time of the code was listed on the code sheet as 0804. Naloxone 0.4 mg IV and flumazenil 0.2 mg IV were given with no increase in level of consciousness. Epinephrine 1 mg + 1 mg was administered IV and the patient became hypertensive and tachycardic: 204-237/104-148 mmHg and 148-151 beats per minute. There was no increase in level of consciousness at that time. She was then transported for CT scan and other follow-up studies then moved to ICU care.
In the ICU, the ventilator peak airway pressures ranged from 38 cmH2O on admission to 20 cmH2O on transfer. The patient was acidotic by arterial blood gas analysis and was intermittently hypotensive.
The troponin level post-arrest was 0.4 ng/ml, and the creatine kinase was 1157 units/liter.
CT angiography: No evidence of pulmonary embolism or aortic dissection, ground glass densities throughout and illdefined nodules throughout the right and left lung…probably due to hypersensitivity pneumonitis.
Echocardiogram: Normal global left ventricular systolic function, regional wall motion abnormalities are absent, moderate to severe mitral valve regurgitation, mild thickening of the mitral valve leaflets. Also, right ventricular pressures were normal, aortic valve was normal, and there was mild pulmonic valve regurgitation. There was no pericardial effusion.
Chest x-ray: Pulmonary vascular congestion with perihilar infiltrates as well as infiltrate involving the right lung base. There was no pneumothorax.
CT of abdomen and pelvis: No intraperitoneal free air, high attenuation density fluid in the prevesical space and in the cul-de-sac suggestive of blood (small).
In the ICU, she was noted to have angioedema of the tongue.
Sadly, she remained with significantly impaired mental function requiring continuous care.
Etiology of the sudden cardiovascular and respiratory collapse: The cardiovascular collapse and respiratory compromise were sudden and severe; within seconds. Based on this, as well as the timing of the administration of the antibiotic, Cefazolin, being approximately 15 minutes prior to the event; the known relatively high incidence of peri-operative anaphylaxis, one of the most common initial findings with anaphylaxis under anesthesia being sudden cardiovascular collapse and airway obstruction; the positive response to IV epinephrine; the chest CT finding within hours post-event consistent with hypersensitivity pneumonitis; known reports of cephalosporin induced hypersensitivity pneumonitis; and angioedema of the tongue, anaphylaxis induced cardiovascular collapse, pulselessness and airway compromise is well at the top of the differential.
Quotes from a review article from 2012 titled “Anaphylaxis during the perioperative period” include:
• “Anaphylaxis during anesthesia can present as cardiovascular collapse, airway obstruction….”
• “…cutaneous manifestations of anaphylaxis are less likely to be apparent when anaphylaxis occurs in this setting.”
• “Antibiotics that are administered perioperatively can cause immunologic or nonimmunologic reactions.”
• “Various studies have proven that many anesthetic drugs, natural latex rubber and antibiotics can induce life-threatening anaphylaxis reactions.”
• “Diagnosis of anaphylaxis under anesthesia is not always straight forward.”
• “Mortality can be high (3.4%) and anaphylactic deaths can account for as many as 4.3% of all deaths occurring during general anesthesia.”
• “The mortality from these reactions is in the range of 3% to 6% and an additional 2% of patients experience significant residual brain damage.”
• “The incidence of anaphylaxis and anaphylactoid reactions during anesthesia is very difficult to estimate but has been calculated to range from 1 in 3,500 to 1 in 13,000 cases.”
Furthermore, quotes from an article titled “Hypersensitivity Pneumonitis Caused by Cephalosporins with Identical R1 Side Chains” include:
• “Drug-induced interstitial lung diseases have many clinical patterns, ranging from benign infiltrates to acute respiratory distress syndrome.”
• “Chest X-ray and computed tomography (CT) revealed diffuse ground glass opacities, consolidation, and a “crazy-paving” pattern in both lungs.”
• “CT also indicated enlargement of the paraaortic, right upper paratracheal, and right hilar lymph nodes.”
These are similar findings to those of this patient post-cardiopulmonary collapse and code.
DIAGNOSIS: Antibiotic Induced Anaphylaxis
WHY IS THIS SO DIFFICULT?
By JOSEPH F. ANSWINE, MD, FASA
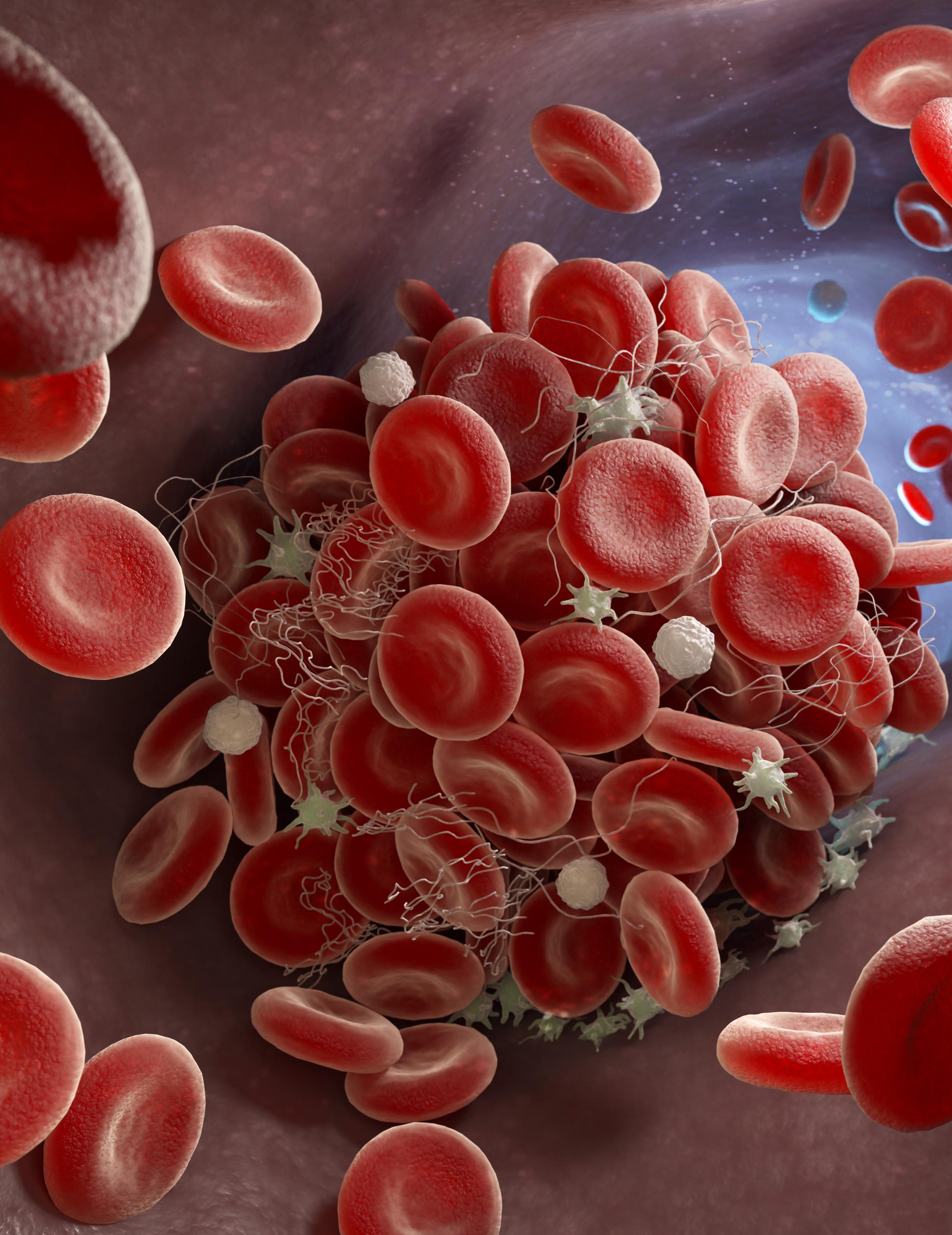
In my continuous pursuit to keep up with the ever-changing practice of medicine, I am trying to teach this old dog new tricks. Today, it is the origin of a clot. Over the years, I have attempted to forget everything about hemostasis other than warfarin inhibits the vitamin K dependent coagulation factors (2, 7, 9, and 10), and heparin increases the effectiveness of antithrombin 3. However, with the addition of a myriad of anticoagulants and antiplatelet drugs, all steps of hemostasis are now in play. So, I guess I should relearn all that I chose to forget. Let us see if we can make sense of the Ps, Gs, 3s, and 1Bs.
First, a few comments. 1) Tissue Plasminogen Activator and the like dismantle clots, the other drugs keep them from forming. 2) The numbered coagulation factors are not in perfect order, and they are not complete. When the great doctors of the past were studying the coagulation cascade from 36,000 feet, they would find what they thought was a new component in the process and gave it a number only to find that it really did not exist, was not a coagulation protein, or the order was wrong. They, however, decided to keep the numbering as is. 3) Von Willebrand Factor is not a coagulation factor but hangs out with one (Factor 8) prior to each going its separate way. 4) Anticoagulants and antiplatelet drugs are not the same thing. 5) Factors 10 and 2 (thrombin) seem most important. Everything meets at Factor 10 (intrinsic and extrinsic). It’s the “X” or the crossroad. Thrombin is the workhorse keeping control of the whole process. 6) Lastly, if the generic name has “xa” in it, it is an activated Factor 10 inhibitor (e.g., Apixaban). Pradaxa does not count because that is a trade name for the Factor 2 inhibitor, Dabigatran.
Blood normally flows through the vessels freely due to naturally occurring substances responsible for keeping platelet aggregation and coagulation in check. Knowing how quickly blood clots in a specimen tube, the process is amazing. These substances include nitric oxide (NO) and prostacyclin (PGI2) secreted by the vascular endothelial cells. They keep the circulating platelets inactive and therefore will not adhere to the endothelial lining. Furthermore, NO leads to smooth muscle relaxation and vasodilatation. Endogenous heparin is also present to bind and potentiate antithrombin 3 which degrades clotting factors 2, 9, and 10. Lastly, thrombomodulin is present
to bind thrombin (clotting factor 2) which then activates protein C. The activated protein C with its cofactor, protein S, inhibit factors 5 and 8. This last process demonstrates the importance of negative feedback mechanisms throughout our body. Thrombin is also a major part of the coagulation cascade leading to clot formation.
Now, when we need clot formation due to vascular injury, what occurs? Five steps are involved: 1) Vascular spasm 2) Platelet plug formation 3) Coagulation 4) Clot retraction and healing and 5) Fibrinolysis.
When damage occurs to the endothelium, endothelin is secreted causing vascular spasm by binding to the smooth muscle cells leading to intracellular calcium release and contraction therefore reducing blood loss into the tissues. Furthermore, the smooth muscle cells will naturally contract when damaged. Lastly, release of inflammatory mediators such as prostaglandins will stimulate local nociceptors leading to further vascular spasm as part of the pain response.
With vascular damage, the endothelial cells secrete Von Willebrand Factor. The injured endothelial cells are also not releasing the natural blood thinners, NO and PGI2. Therefore, the platelets are activated, and bind with the Von Willebrand Factor utilizing glycoprotein 1b (GP1b) present on the platelet surface. Using the bound Von Willebrand Factor, the platelets begin to adhere to each other and the endothelium. They also begin to secrete substances such as ADP, thromboxane A2, and serotonin. ADP and thromboxane A2 activate surrounding platelets leading to further aggregation. Platelet receptors involved include the P2Y12 ADP receptor. The binding of these receptors results in a series of events leading to an increase in intracellular calcium. The calcium increase triggers the calciumdependent association of GP2b and GP3a to form the activated membrane receptor complex GP2b3a which is capable of binding fibrinogen leading to further platelet adhesion since many can connect to the same strand of fibrinogen. Thromboxane A2 and serotonin then bind to the exposed smooth muscle causing further contraction around the newly formed platelet plug.
The coagulation cascade now is initiated. By the way, although I am of Italian descent, I am not from Rome so I will avoid roman numerals.
There is the longer intrinsic pathway named because all the components are contained within the blood, and the shorter extrinsic pathway requiring contact with Tissue Factor (Factor 3 / thromboplastin) to be initiated. The coagulation cascade as described in the name is an amplification process with a greater number of components activated with each step, therefore, there is a relatively small amount of Factor 12 within the blood as compared to fibrinogen at the tail end of the process. Also, do not look for Factor 6 because similar to the right fielder on Abbott and Costello’s baseball team, it does not exist. For completeness of your scorecard, Factor 4 is just calcium.
The intrinsic pathway is initiated by activation of the zymogen (an inactivated protein precursor), Factor 12 or Hageman Factor. Factor 12 is activated by the negative charges of the phosphatidylserine groups on the aggregated platelets. Kallikrein, High Molecular Weight Kininogen (HMWK) and collagen can also activate Factor 12. Activated Factor 12 then activates Factor 11. Interestingly, the importance of the intrinsic pathway is questionable since deficiencies in Factors 12 and 11 have minimal clinical significance. Activated Factor 11 then activates Factor 9. Activated Factor 9 along with its cofactor, Factor 8, and calcium move the process into the common pathway by activating Factor 10. (As an aside, Factor 8 is secreted by endothelial cells and not from the liver. It circulates bound to Von Willebrand Factor as stated above. That is the only association between Von Willebrand Factor and the coagulation cascade. Its function is platelet adherence. Hemophilia A and Von Willebrand Disease, therefore, are not the same thing. Hemophilia B (Christmas Disease) is a deficiency of Factor 9 and since it is higher in the intrinsic pathway, it is not as serious.) Activated Factor 10 and its cofactor, Factor 5, along with calcium create the prothrombin activator complex which converts Factor 2 (prothrombin) to thrombin. Thrombin then converts the soluble Fibrinogen (Factor 1) to the insoluble fibrin. The fibrin monomers link together to form strands. Factor 13 and calcium then crosslink the strands together to form a mesh covering the platelet plug.
The extrinsic pathway which commonly occurs simultaneously with the intrinsic pathway is shorter and quickly initiated as blood travels outside the vessel walls allowing
Continued on page 10
Factor 7 to interact with Tissue Factor and calcium leading to the activation of Factor 10. Activated Factor 10 then proceeds through the common pathway as described above.
The fourth step is clot retraction and healing. Platelets contract utilizing the contained actin and myosin pulling the attached endothelium together. Platelet derived growth factor (PDGF) is released from the adhering platelets producing mitogenesis therefore proliferation of smooth muscle cells and fibroblasts (as well as other cells throughout the body) as part of the healing process of the vessel and underlying tissue. In the family of growth factors released is vascular endothelial growth factor (VEGF) which promotes revascularization of the damaged area.
The last step is fibrinolysis. Multiple processes are going on around the clot limiting its further growth so as not to significantly limit flow or occlude the vessel. Some of those processes were described earlier. Furthermore, to keep the clotting process in check, clot breakdown is quickly initiated. Endothelial cells produce tissue plasminogen activator (TPA). In the presence of fibrin, TPA converts circulating plasminogen to plasmin. Remember, exogenous TPA is the big clot buster used for early ischemic strokes. Plasmin proteolyzes proteins thereby destroying the fibrin cross linking and breaking down the formed clot. Fibrin degradation products are formed in the process. These are important to us since their levels can be measured to determine if clot formation is occurring within the body. One such fibrin degradation product is D-dimer. As an aside, Tranexamic Acid (TXA) is a mild antifibrinolytic that reversibly binds to plasminogen reducing its conversion to plasmin.
With the above described process, we can now hopefully better understand the mechanisms of action of the available anticoagulants and antiplatelet drugs. Here are a few commonly used drugs and their effects on the timing of the performance of neuraxial blockade. This is superficial because it does not include what to do about indwelling catheters, performing peripheral blocks, or timing of catheter removal. The ASRA guidelines cover that. When looking at published guidelines, it is common to see a range of time until regional techniques are appropriate. To reasonably understand the meaning behind it, you must assume the low end is the minimum time and the maximum is the ideal time to proceed.
Warfarin (Coumadin) is still widely used today. Warfarin inhibits the vitamin K epoxide reductase complex 1 which is needed for activating vitamin K. Warfarin therefore depletes functional vitamin K reserves. The hepatic synthesis of coagulation factors 2, 7, 9 and 10, as well as proteins C and S, require the presence of vitamin K. Of importance is that proteins C and S are much more labile than the clotting factors therefore a hypercoagulable state can occur prior to anticoagulation. This is the etiology of warfarin-induced skin necrosis, and where the heparin bridge comes in. Factor 7 is the most labile clotting factor therefore the first to be significantly diminished creating the value of the emergent use of Factor 7 concentrate. Vitamin K, Prothrombin Complex Concentrate, and Fresh Frozen Plasma have also been used for reversal of warfarin-induced anticoagulation. Since the clotting factors involved are part of the extrinsic and common pathways, and not the intrinsic pathway; the PT/INR and not the PTT (which looks at the intrinsic pathway) are the common tests performed for chronic management of warfarin therapy. Warfarin’s half-life is variable averaging about 40 hours. Therefore, the PT/INR could take days to normalize (INR <1.5) which is when neuraxial blockade can be safely performed.
Heparin is also still widely used. It potentiates the intrinsic anticoagulant, antithrombin 3, by as much as 1000 times which then inactivates Factors 2, 9 and 10 among others to a lesser extent. Heparin can cause heparin-induced thrombocytopenia (HIT). Heparin-induced anticoagulation can be reversed with protamine via ionic bonding between the two molecules. Heparin’s half-life is about 1.5 hours but is dose dependent. The level of anticoagulation can be monitored with the Partial Thromboplastin Time (PTT). SQ heparin 5000 units twice daily or less is not a contraindication for neuraxial blockade. Higher doses require a PTT less than 40 or greater than six hours from the last dose.
Enoxaparin (low molecular weight heparin) also potentiates antithrombin 3 however the complex formed, as apposed to heparin, cannot effectively deactivate thrombin. Therefore, enoxaparin preferentially deactivates Factor 10. It can also cause HIT. SQ enoxaparin 40 mg requires 12 hours from the last dose for neuraxial blockade. Higher doses require 24 hours.
Aspirin and NSAIDs produce their antiplatelet activity by inhibiting the formation of Thromboxane A2 leading to a reduction in
platelet aggregation. Aspirin and NSAIDs are not a contraindication for neuraxial blockade.
Dabigatran (Pradaxa) is a direct thrombin inhibitor. Its half-life is about 12 hours with normal renal function, but prolonged as renal function is reduced. Three days are required from the last dose with normal renal function for neuraxial blockade. Greater than 4 days are required with reduced renal function.
Apixaban (Eliquis) and Rivaroxaban (Xarelto) are direct activated Factor 10 inhibitors. Three days are required from the last dose for neuraxial blockade. Activated Factor 10 levels may be drawn if sooner than 3 days is desired. As a little bit of a disconnection between surgery and anesthesia, major surgery can be performed after 2 days of discontinuation as per guidelines, but 3 days are required for spinals and epidurals.
Clopidogrel (Plavix), prasugrel (Effient) and ticlopidine (Ticlid) reduce platelet aggregation by blocking the binding of ADP to the platelet P2Y12 receptor irreversibly, and ticagrelor (Brilinta) blocks the P2Y12 receptor reversibly. Clopidogrel must be held at a minimum of 5 days but ideally at least 7 days prior to neuraxial blockade. Again, that is my way of interpreting 5-7 days. Prasugrel and ticlopidine must be held 10 days and ticagrelor must be held at least 5 days prior to neuraxial blockade.
Abxicimab (Reopro), eptifibatide (Integrilin), and tirofiban (Aggrastat) are GP2b3a inhibitors decreasing the ability of fibrinogen to link the platelets together. It is important to note that patients are usually on dual therapy when taking these medications. Abxicimab requires 1 to preferably 2 days before neuraxial blockade can be performed. Eight hours are required for eptifibatide and tirofiban.
Full dose TPA requires at least 48 hours and normalization of clotting studies before neuraxial blockade. Low dose TPA for line clearance is not a contraindication for neuraxial blockade.
This list is far from complete, but you get the picture.
What was easy is now very complicated. I dumbed it down for me to understand, so I am sure you got this.
Originally published in the Sentinel: Pennsylvania Society of Anesthesiologists Newsletter, Winter 2023.

By JOSEPH F. ANSWINE, MD, FASA
For years, research and common belief have supported the idea that patient education altering patient behavior has improved patient outcomes. Lifestyle changes instituted after improved physician-patient engagement have demonstrated clinical benefit in a wide range of illnesses such as cardiovascular disease, diabetes and arthritis.1
During perioperative care, enhanced recovery after surgery (ERAS) programs have utilized patient education as an important pre-operative component to achieve the goals of improved patient satisfaction, shorter hospital stays, reduced readmission rates and less complications.2
Traditionally, the first time an anesthesiologist interacts with a patient is usually the day of surgery, especially for minor outpatient procedures. This short period of physician-patient interaction often does not create issues for the healthy patient. However, an estimated 48 million ambulatory surgeries occurred within hospitals and ambulatory surgery centers in 2010, with approximately 35% of all patients having an ASA Physical Status (PS) III or greater identifying patients with severe preoperative disease processes.3,4,5
Over the past few decades, there has been an increasing trend to schedule more complex patients for an assessment by an anesthesiologist in a preoperative evaluation clinic (PEC). There are many benefits to a well-established PEC, including a reduction in mortality, decreased surgical cancellations caused by nonmedical issues, reduction in unnecessary testing, increased patient and physician satisfaction, reduction in patient anxiety, and improved compliance with preoperative instructions.1,5 A patient in a PEC can be fully informed in a calm environment days or weeks before an elective surgery.
Over the past few decades, there has been an increasing trend to schedule more complex patients for an assessment by an anesthesiologist in a preoperative evaluation clinic (PEC).
A thorough discussion about a patient’s relevant past medical history and medications (prescribed or otherwise) is important. An estimated 44% of patients take some sort of daily herbal supplements, with 16.5% taking a supplement that could interact
with anesthetics or other medications received during the perioperative period.6 The discussion can help ensure that the anesthesiologist provides the necessary information to avoid potentially unsafe medication interactions.7
Daily, patients undergo elective surgeries such as hysterectomies (removal of the uterus), cystectomies (removal of the bladder), laparoscopic sleeve gastrectomies (removal of stomach), partial hepatectomies (removal of part of the liver) and colorectal procedures (removal of part of the small or large intestines). ERAS, as mentioned above, is a treatment pathway for these patients designed to reduce the stress response to surgery. ERAS incorporates preoperative counseling, optimization of chronic diseases, preoperative nutrition, standardized anesthetic and analgesic techniques, and early mobilization and enteral feeding.8 Patient education also helps with protocol adherence.9,10
Studies show that pre-operative discussions for joint replacement procedures have significant benefit. Which anesthetic a patient receives can influence patient outcomes, and so an early discussion of anesthetic choices may allow patients to ask appropriate questions and learn about all the options. For instance, spinal anesthesia is associated with better outcomes and patient satisfaction when used in joint replacement cases. There may be a 30-50% reduction in mortality with neuraxial anesthesia.11,12 When patients attended an optional three-hour class about their upcoming surgery with a discussion about the pros and cons of various anesthetic techniques, they were more likely to choose spinal anesthesia.13
A potential area for advancement of perioperative care with education is in obstetric anesthesia. In 2015-2016, a survey demonstrated that more than 39% of the population is obese, BMI > 30, which is up from 30% in 2001-2002.14 Obesity comes with complications, including increased risk of diabetes, hypertension, stroke, and cardiac disease.15 Obesity in pregnancy is increasingly more common. In pregnancy, obesity can also increase the risk of gestational diabetes, pre-eclampsia, and sleep apnea, as well as an increase in the risk of miscarriage, birth defects, macrosomia, preterm birth and still birth.16,17 Furthermore, obesity increases the risk of anesthetic complications especially involving airway compromise. Patient knowledge on effects of obesity on anesthetic complications were
influenced by BMI > 30, nulliparity, and lack of tertiary education.18
As with utilizing patient education to mitigate chronic illness, the addition of patient education as a major part of preoperative care improves perioperative patient safety. In the high stress, fast paced world of anesthetic care, patient acuity is vitally important for overall success.
1 Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20(6):64–78. Poland F, Spalding N, Gregory S, et al. Developing patient education to enhance recovery after colorectal surgery through action research: a qualitative study. BMJ Open 2017;7:e013498. doi:10.1136/ bmjopen-2016-013498
Edwards, A. F. & Slawski, B. Preoperative Clinics. Anesthesiol. Clin. 34, 1–15 (2016).
2 Young, S., Shapiro, F. E. & Urman, R. D. Officebased surgery and patient outcomes. Curr. Opin. Anaesthesiol. 31, 707–712 (2018).
3 Nagrebetsky, A., Gabriel, R. A., Dutton, R. P. & Urman, R. D. Growth of Nonoperating Room Anesthesia Care in the United States: A Contemporary Trends Analysis. Anesth Analg 124124, 1261–7 (2017).
4 Sankar, A., Johnson, S. R., Beattie, W. S., Tait, G. & Wijeysundera, D. N. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br. J. Anaesth. 113, 424–432 (2014).
5 Blitz, J. D. et al. Evaluation Clinic Visit Is Associated with. Anesthesiology 125, 280–294 (2016).
6 Levy, I. et al. Perioperative Risks of Dietary and Herbal Supplements. World J. Surg. 41, 927–934 (2017).
7 Willems, J., Jan Stolker, R., Kruip, M., Hoeks, S. & van Fessem, J. Making safer preoperative arrangements for patients using vitamin K antagonists. BMJ Qual. Improv. Reports 6, u212617.w5031 (2017).
8 Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 78, 606–617 (1997).
9 Gottumukkala, V. et al. Patient-Reported Outcomes Accurately Measure the Value of an Enhanced Recovery Program in Liver Surgery. J. Am. Coll. Surg. 221, 1023–1030.e2 (2015).
When patients attended an optional three-hour class about their upcoming surgery with a discussion about the pros and cons of various anesthetic techniques, they were more likely to choose spinal anesthesia.13
10 Kalogera, E. & Dowdy, S. C. Enhanced Recovery Pathway in Gynecologic Surgery. Obstet. Gynecol. Clin. North Am. 43, 551–573 (2016).
11 Chiu, Y.-L. et al. Perioperative Comparative Effectiveness of Anesthetic Technique in Orthopedic Patients. Anesthesiology 118, 1046–1058 (2013).
12 Rodgers, A. et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised. BMJ 321, 1493–1493 (2000).
13 Kase, B. et al. Patient education and anesthesia choice for total knee arthroplasty. Patient Educ. Couns. 100, 1709–1713 (2017).
14 Hales, C. M., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. (2017).
15 Jensen, M. D. et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults. J. Am. Coll. Cardiol. 63, 2985–3023 (2014).
16 ACOG. FAQ182 Obesity and Pregnancy. (2016). Available at: https://www. acog.org/-/media/For-Patients/faq182. pdf?dmc=1&ts=20190316T1719095553.
17 Practice Bulletin No 156. Obstet. Gynecol. 126, e112–e126 (2015).
18 Tulp, M., McDermott, L., Paech, M. & Nathan, E. Maternal knowledge of the impact of obesity on complications relevant to obstetric anesthetic care. J. Obstet. Anaesth. Crit. Care 7, 37 (2016).

The Pennsylvania Medical Society (PAMED) convened its annual House of Delegates (HOD) using a hybrid format and culminating in the main business session held October 17–19, 2025, at the Hershey Lodge in Hershey, PA. Serving as the legislative and policymaking body of organized medicine in Pennsylvania, the 2025 HOD provided a crucial platform for physicians, residents and medical students to deliberate on foundational policies addressing the most pressing challenges in healthcare across the Commonwealth.
This year’s HOD was marked by vigorous debate on issues spanning physician economic security, regulatory burdens and critical public health concerns, reinforcing PAMED’s role as the unified voice for Pennsylvania physicians. Over the course of the weekend, delegates passed resolutions, approved key reports and elected new leadership, setting a decisive agenda for advocacy and action in the coming year.
The core mandate of the HOD is to determine official PAMED policy. While the specific final resolutions remain confidential to members, the substance of debate among the various committees centered on four defining themes impacting the state’s healthcare ecosystem.
Firstly, a significant portion of debate focused on the viability of physician practices and the rising tide of administrative complexity. While prior authorization requirements continue to plague physician workflow and compromise timely patient care, the HOD took decisive steps toward strengthening PAMED’s mandate to advocate for legislative and regulatory reforms aimed at minimizing insurer interference. Similarly, discussions around the future of telehealth flexibilities, which faced legislative uncertainty earlier in the year, led to a clear policy directive of advocating for the permanent extension and adequate reimbursement of virtual care services to ensure continuity of access, especially for rural and underserved populations.
Secondly, the delegates addressed the critical issue of scope of practice. Recognizing the essential need for physician-led teambased care, resolutions sought to establish firmer policy guidelines against nonphysician providers seeking independent practice without rigorous medical training oversight, thereby prioritizing patient safety and the maintenance of quality standards across all care settings.
Lastly, the Physician Unionization Task Force delivered an update and hosted an open forum. Given the growing interest among employed physicians in collective bargaining, the resulting policy actions focused on providing educational resources and legal support to members exploring unionization options, ensuring they are wellinformed regardless of their career path. The resolutions affirmed PAMED’s commitment to supporting physicians in all practice settings—independent, academic or employed.
The 2025 HOD schedule was also packed with educational and town hall sessions, underscoring the interconnectedness of clinical practice and public policy. The Friday session began with a CME offering, “The Bermuda Triangle: Searching for Lost Opportunities and Missed Conversations,” which addressed the growing complexity of caring for Pennsylvania’s large senior population. This session, highly relevant given the demographic trends in the state, focused on multidisciplinary strategies to improve communication, patient safety and holistic care for elderly patients managing multiple medical conditions.
A key highlight was the Government Health Panel, “Emerging Issues in PA,” featuring direct participation from highlevel representatives of the Department of Aging, the Department of Drug and Alcohol Programs (DDAP), and the Department of Human Services (DHS). This critical dialogue provided delegates with an unfiltered view of the state’s current health priorities—from the opioid crisis response led by DDAP to the looming challenges
in managing Medicaid and long-term care services overseen by DHS—and outlined how physicians could partner with state agencies to leverage existing resources.
Further cementing PAMED’s commitment to political engagement, the “Becoming a Political Advocate” panel, featuring leadership from the American Medical Association (AMA) Board of Trustees and PAMPAC, delivered a powerful message on physician responsibility in the legislative arena. This session armed delegates with actionable strategies for effective advocacy, stressing that policy is often decided by those who show up.
The HOD concluded its formal business with the election of officers and trustees who will guide the organization’s strategic direction.
Key Election Results Included:
• Vice President: John R. Mantione, MD (Dauphin County)
• Speaker, House of Delegates: Todd M. Hertzberg, MD, FACR (Allegheny County)
• Vice Speaker, House of Delegates: Andrew Lutzkanin III, MD, FAAFP (Dauphin County)
These newly elected individuals, along with various Trustees representing specific geographic districts and sections (Early Career Physicians, Medical Students, etc.), will be instrumental in translating the adopted resolutions into tangible results for physicians and patients across Pennsylvania.
The 2025 PAMED House of Delegates meeting was a powerful demonstration of physician leadership and collective resolve. The policies adopted—focused on practice viability, patient safety and advocacy—will form the foundation of PAMED’s legislative and regulatory efforts in the coming year, driving forward the mission to advance the science and art of medicine in Pennsylvania.

In September, The Pennsylvania Medical Society (PAMED) held its Top Physicians Under 40 Awards ceremonies in Hershey and Latrobe, recognizing exceptional early-career physicians who are making a profound impact in medicine. Nominated by their peers and carefully selected by a committee of PAMED members, these outstanding professionals represent the “best of the best.”
“These candidates truly set themselves apart,” said Arvind R. Cavale, MD, FACE, FCPP, PCEO, president-elect and member of the awards committee. “Their unwavering commitment to patient care and forwardthinking ideas will undoubtedly shape the future of medicine.”
The awards shine a spotlight on the dynamic leaders, compassionate clinicians and groundbreaking innovators who are actively shaping patient care, research and medical education across Pennsylvania.
The medical profession is a demanding one and those in it often experience burnout and disillusionment. For young physicians wrestling with the pressures of their profession, this award provides tangible recognition of the recipients’ accomplishments in the field. PAMED sends a powerful message with these awards: excellence and dedication are noticed and valued. It also inspires peers, residents and medical students to strive for clinical excellence, community engagement and innovative practice.
The recipients of the Top Physicians Under 40 Awards are often physicians who bring fresh perspectives and innovative approaches to medicine. Past recipients have been recognized for their work in community health centers, their passion for mental health support, or their dedication to global voluntary service. In recognizing these achievements, PAMED encourages the cultivation of forward-thinking practices and the resulting successes. It serves as a catalyst for other healthcare institutions to adopt new methods championed by these young honorees, ultimately advancing the quality of care for all Pennsylvania patients.
The Under 40 honorees often become more engaged in advocacy and professional leadership. Recognition of these rising stars helps to consolidate and to strengthen the collective voice of the physician community. They contribute to PAMED’s mission of protecting and promoting the profession as well as the well-being of patients. Their diverse experiences—spanning multiple specialties and practicing in rural, suburban and urban settings across Pennsylvania—provide a powerful, unified perspective on the current challenges and opportunities in healthcare. The visibility that comes with the award empowers them to advocate more effectively for sensible health policy, patient safety, and physician wellness, ensuring that the physician’s viewpoint remains central to the future of Pennsylvania’s healthcare landscape. By celebrating the dedication and groundbreaking work of its youngest members with the Physicians Under 40 Awards, the Pennsylvania Medical Society ensures a vibrant, innovative, and highly committed future for medicine throughout the Commonwealth.
To learn more about the 2026 PAMED Awards and how to nominate an outstanding young physician for the Top Physicians Under 40, go to pamedsoc.org/membership/awards.

The Pennsylvania Medical Society’s (PAMED) Top Physicians Under 40 awards celebrate the brightest young medical minds, and two Dauphin County Medical Society members, Dr. Sean Mahase and Dr. Seyed Mansouri, have earned this esteemed recognition. These accomplished professionals from Penn State Health Milton S. Hershey Medical Center were nominated by peers for their significant contributions to medicine, demonstrating exceptional patient care, innovation and dedication to the future of healthcare.
Dr. Mahase, a specialist in Radiation Oncology, was recognized for his innovations in education, clinical care and research. His work has notably elevated standards within his department and across central Pennsylvania. Dr. Mahase focuses on complex and sensitive cases, including pediatric, head and neck, and adult brain tumors, balancing direct, compassionate patient care with the precision of leading-edge technology.
“Radiation oncology offers a personally ideal balance of direct and longitudinal patient care, multidisciplinary collaboration, innovative technology providing precise treatments with sub-centimeter accuracy and seemingly unlimited research opportunities,” Mahase said.1
Dr. Mansouri, an expert in Neurological Surgery (specifically NeuroOncology), was lauded for transforming brain tumor care through pioneering clinical work, liquid biopsy research and interdisciplinary collaboration. An Associate Professor, Dr. Mansouri is committed to mentoring the next generation of physicians, channeling his drive for innovation to inspire others to push the boundaries of treatment for brain tumors.
Mansouri said his commitment to mentoring the next generation of physicians fuels his drive for innovation and lifelong learning.
“By sharing my expertise and experience, I aim to inspire others to push the boundaries of what is possible in the treatment of brain tumors,” he said.1
Together, the work of Dr. Mahase and Dr. Mansouri exemplifies the highest standards of medical excellence, underscoring their profound impact on patient health and medical science in Pennsylvania and beyond.
On behalf of the Dauphin County Medical Society, congratulations, Dr. Mahase and Dr. Mansouri!
REFERENCE:
1 “Mahase and Mansouri receive Top 40 Physicians Under 40 award”, Penn State Health News, pennstatehealthnews.org/2025/05/ mahase-and-mansouri-receive-top-physicians-under-40-award
By JOSEPH F. ANSWINE, MD, FASA
Marijuana, cannabis, CBD; our patients are coming to the OR utilizing these substances in one form or another at a very high rate. Some may be smoking marijuana recreationally, however, many are utilizing the cannabinoids which are found in marijuana for medical reasons.
What are cannabinoids? They are a large group of lipid-based substances, many commonly found in the cannabis or marijuana plant, that bind to cannabinoid receptors. Also included in this group are the endocannabinoids (endogenously produced), anandamide and 2-arachidonoylglycerol (2-AG).
Within our bodies, we have the endocannabinoid system with receptors located throughout the central nervous system, the peripheral nervous system and many organs. What does the endocannabinoid system do? It is involved with a wide variety of processes throughout the body maintaining homeostasis. It is involved in regulating physiologic and cognitive processes including immunocompetence, controlling inflammation, appetite, fertility, pain sensation, mood, and memory; creating synaptic plasticity responsible for learning. Endocannabinoid stimulation may also be responsible for exercise-induced euphoria. There are two commonly described receptor types, CB1 found mainly in the central and peripheral nervous system especially in the brain and is responsible for functions such as mood stabilization and pain modulation; and CB2 found mainly in peripheral tissues and is responsible for immune function and control of inflammation. They are part of a large receptor family called G protein coupled receptors not unlike the opioid receptors.
To shed some light on one reason the endocannabinoid system exists; imagine a warrior that has just come from battle tired and injured. The endocannabinoid system kicks in, increasing appetite for high calorie foods to increase energy stores, stabilizes mood and reduces pain, allowing that warrior to recover; maintaining homeostasis.
The endocannabinoid system is too diverse to talk about in one short article, therefore, we will concentrate on how it relates to controlling pain only. Remember, a nociceptive signal moves through a primary afferent axon to the spinal cord. The signal reaches a synaptic cleft where a secondary afferent awaits and an influx of calcium at the presynaptic terminal causes the mobilization and release of glutamate which travels across the synaptic cleft and binds to AMPAtype and NMDA receptors, again causing the intracellular release of calcium which stimulates the opening of sodium channels and the continued propagation of the signal up the spinal cord to the brain. Some signals find their way to the periaqueductal grey in the midbrain as well as the locus coeruleus in the pons and locus raphe magnus in the medulla. This stimulates the descending pain modulation pathway which sends signals down the spinal cord and decreases the signaling from the primary to the secondary afferent nerves. The descending pathway is suppressed by GABAnergic inhibition until the incoming signal arrives.
During nociceptive transmission within the spinal cord and GABAnergic inhibition within the descending pathway, calcium influx into the post-synaptic cleft stimulates the formation and release of endocannabinoids. They travel across the synaptic cleft and bind to the presynaptic G protein coupled
is an important warning system that injury may or is occurring, however, too much pain is a hinderance.
So, what do we do when a patient that is exposed to cannabinoids comes to the OR? Very few human studies are available. Due to the potential negative effects on the tracheobronchial tree such as acute bronchospasm, patients with recent exposure to inhaled cannabis should not undergo elective surgery. Also, the effects of cannabinoid exposure on the cardiovascular system such as significant hypotension, and an exaggerated response to antihypertensive agents must be understood. However, withdrawal may be a possibility after chronic exposure leading to agitation and poor pain control. Therefore, continuation of noninhaled cannabinoids may be reasonable.
So much more must and will be learned about cannabinoids and anesthesia. These are interesting times.
Originally published in the Sentinel: Pennsylvania Society of Anesthesiologists Newsletter Winter 2019.
Within our bodies, we have the endocannabinoid system with receptors located throughout the central nervous system, the peripheral nervous system and many organs.
cannabinoid receptors. Binding of these presynaptic receptors leads to a reduction of calcium influx, therefore, a reduction in neurotransmitter release. Nociceptive signals are reduced within the spinal cord and GABAnergic inhibition of the descending pathway is reduced. The result is a reduction in pain. Why does this process exist? Pain

By JESSE GUNDER
The Scott A. Gunder, MD, DCMS Presidential Scholarship and the Dauphin County Medical Society are excited to announce a generous contribution from the Gunder Family along with changes to the scholarships’
Continued on page 21
administration, allowing for larger scholarship awards and for the first time giving multiple annual awards to deserving medical students at Penn State College of Medicine.
The Scholarship is named for and honors the legacy of Dr. Scott A. Gunder, a Dauphin County Gastroenterologist and past President of the Dauphin County Medical Society (2000). A native of central Pennsylvania, Dr. Gunder received his Doctor of Medicine from Hahnemann University and subsequently his internal medicine residency was completed at Pennsylvania State University. He was also a clinical instructor of Gastroenterology at Penn State University. Dr. Gunder had an enduring dedication for providing compassionate care for his patients and at the same time providing leadership to the medical community. In May of 2000, Dr. Gunder lost a brief but courageous battle with cancer and died at the young age of 39. His wish was to continue his contributions to the community even after his far-too-early passing.
Dr. Gunder recognized the challenges faced by many medical students, one of them the financial costs associated with entering the profession. The scholarship was his vision to ease some of that burden and support passionate and deserving medical students in their 2nd year of learning at the Penn State College of Medicine. Eligible candidates must also be residents of Pennsylvania.
“The Gunder Family is delighted to be able to help in the continuance of Dr. Gunder’s wishes with this contribution,” said Scott’s brother, Jesse K. Gunder, III. “My brother had a heart for medicine and a love
of people that our family is delighted to perpetuate through this scholarship. We see the gift as a means of paving the way for a new generation of Pennsylvania physicians well into the future.”
The Scholarship is named for and honors the legacy of Dr. Scott A. Gunder, a Dauphin County Gastroenterologist and past President of the Dauphin County Medical Society (2000).
The committee is reviewing significant enhancements to scholarships for the 2024–25 school year, with the goal of providing awards to second-year PSCoM students.
“On behalf of the Dauphin County Medical Society, we express our deep gratitude to the Gunder Family for their tremendous support of students, the community, and the medical profession here in Pennsylvania,” said Dr. Joseph Answine, current President, DCMS. “Our county has always been a place where medical professionals can thrive, and at DCMS we have the pleasure of supporting physicians throughout their entire careers. Supporting a thriving medical community in Pennsylvania is our core mission. Thanks to the Gunder Family’s generous philanthropy, we’re excited to inspire even more young talent in the practice of delivering high quality healthcare in the state of Pennsylvania.”
This article originally appeared in Central PA Medicine , Fall 2024.
By ROBERT ETTLINGER, MD
Head up the hill to the beautiful Hotel Hershey and bear right to its backyard. 1933 Restaurant & Tavern opened earlier this year, replacing the elegant Harvest. A bit more casual this time around, the fare presented by Chef Dakota Bowers is just as fabulous.
1933 was the year that Milton Hershey began his Great Building Campaign, partly to provide jobs to Central Pennsylvanians during the Depression. Along with the Hotel Hershey, other eventual projects during that decade included Hershey Theater, Hersheypark Arena, and Hersheypark Stadium. The eatery and its artwork are a homage to that year, the end of Prohibition. The cocktail menu celebrates that era, reviving the classics popularly crafted around that time.
With some outdoor seating around a big fire pit for the warmer months, 1933 overlooks the mini-golf course and the hotel cottages, with vistas of Blue Mountain. It’s divided into a classy dining area topped by a stained-glass ceiling and a tavern with multiple TVs for sports fans.
Appetizers include Fried Burrata Caprese with a creamy center, a Bavarian Pretzel Cheese Board, and Steamed PEI Mussels in a fragrant coconut red curry broth.
Steaks and chops are the signature entrees, with cast iron filets, Wagyu Denver Steak, and a certified Angus Ribeye. All include a side and a selection of six sauces. I enjoyed a big Duroc Pork Rib Chop with bearnaise sauce, lasting the next two nights as well. Other recommended entrees include the 1933 Steak & Ale Pie, Adobo Lacquered Swordfish, and Smoked St. Louis Pork Ribs. And, if in the mood to go wild and celebrate something, a huge $99 Seafood Tower.
When you’re ready for dessert, word has it that they make some decent chocolate close by in the neighborhood.

101 Hotel Road, Hershey, PA 17033 717-534-8800


The “best” cancer care is only the best if it’s exactly what your patient needs. That’s why we start by gaining a deep understanding of where each individual’s at — medically, emotionally and situationally. Because here, the question isn’t if the right tools exist but how to apply them for a truly personalized plan — for your patient, their family and you.
Dig deeper into our services at WellSpan .org /Cancer.
RECONS