
Hypertension Hypertension
\ The domino effect
Wound care
Wound care
\ The far-reaching impact of burns
Endocrinology
Endocrinology
\ Androgen deficiency









4
6


Hypertension Hypertension
\ The domino effect
Wound care
Wound care
\ The far-reaching impact of burns
Endocrinology
Endocrinology
\ Androgen deficiency









4
6
ED’S NOTE

May’s Specialist Forum unveils key insights
INDUSTRY NEWS
CombATing BPH with new generic combination therapy
9 WOUND CARE
Impact of burn injuries extends beyond physical health
14 CARDIOLOGY
CPD: The domino effect of hypertension
EDITORIAL
EDITOR: René Bosman
René.Bosman@newmedia.co.za
SUB EDITOR: Gill Abrahams
LAYOUT & DESIGN: Allison McCallum
ADVERTISING
ADVERTISING EXECUTIVE
Charissa Piek | 063 281 1205
Charissa.Piek@newmedia.co.za
DISTRIBUTION & SUBSCRIPTIONS
Felicity Garbers
Felicity.Garbers@newmedia.co.za
PUBLISHING TEAM
GENERAL MANAGER: Dev Naidoo
GROUP ACCOUNT DIRECTOR B2B: Johann Gerber
Johann.Gerber@newmedia.co.za
PRODUCTION MANAGER: Angela Silver
ART DIRECTOR: David Kyslinger
CONTACT
Johannesburg Office: Ground Floor, 272 Pretoria Avenue, Randburg 2194

04 28 32 24
04 28 32 24
20 Online CPD: Exploring the ARISTOPHANES Trial: Insights into anticoagulation strategies for special AFib patient populations
21 ENDOCRINOLOGY
Androgen deficiency: An unrecognised consequence of long-term opioid use
24 ALLERGOLOGY
Tackle seasonal sniffles with combination therapy
26 Online CPD: Unlocking relief: Harnessing the power of FDC therapy in AR management
Postal Address: PO Box 784698, Sandton, Johannesburg, 2146 T +27(0)11 877 6111 F +27(0)11 713 9024
www.medicalacademic.co.za
PRINTING Printed by CTP Printers COVER PRICE Specialist Forum per issue R80,00 VAT Incl. ISSN: 2218-8282
Published by New Media, a division of Media24 (Pty) Ltd

27 HEALTH AWARENESS
Protecting children from tobacco industry interference
28 INFECTION CONTROL
Let’s get back to basics
29 Irritant contact dermatitis: Protecting healthcare heroes
32 NEPHROLOGY
Prevalence of CKD is high, yet level of care remains low
34 PSYCHIATRY
Jumpstarting emotional flatlining in patients living with MDD
MANAGEMENT TEAM
CEO: NEW MEDIA: Aileen Lamb
COMMERCIAL DIRECTOR: Maria Tiganis
STRATEGY DIRECTOR: Andrew Nunneley
CHIEF FINANCIAL OFFICER: Venette Malone
CEO: MEDIA24: Ishmet Davidson
HEAD OFFICE
8th floor, Media24 Centre, 40 Heerengracht, Cape Town 8001 PO Box 440, Green Point, Cape Town 8051 Tel: +27 (0)21 406 2002
www.newmedia.co.za
Disclaimer: Please take note that the products featured in this journal are available in South Africa. Products may be marketed under a different name or might not be registered in your country. For more information, contact your local representative.
All content in Specialist Forum is sourced independently and under no circumstances should articles be considered promotional unless specified with a postscript. Please note that all advertising is intended for healthcare professionals only.

Unless previously agreed in writing, Specialist Forum owns all rights to all contributions, whether image or text.
SOURCES: Shutterstock, supplied images, editorial staff.
While precautions have been taken to ensure the accuracy of its contents and information given to readers, neither the editor, publisher, or its agents can accept responsibility for damages or injury which may arise therefrom. All rights reserved. © Specialist Forum. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, photocopying, electronic, mechanical or otherwise without the prior written permission of the copyright owners.

Welcome to the May issue of Specialist Forum, where we bring you a diverse range of articles covering crucial topics in healthcare. This issue is particularly special as it offers valuable insights worth 5 CPD points, helping you stay updated and earn credits simultaneously.
As the winter season descends upon South Africa, it’s essential to focus on maintaining optimal health, especially considering the increased prevalence of respiratory illnesses and other conditions during this time.
One of the key online CPD articles in this edition sheds light on non-vitamin K oral anticoagulants (NOACs) for patients living with AFib at risk of stroke. With advancements in medical science, NOACs have emerged as effective alternatives to traditional anticoagulant therapy, offering improved outcomes and safety profiles. Understanding the nuances of NOACs is crucial for managing patients with AFib, and this article aims to provide you with the latest evidence-based insights.
Our second online CPD article to look out for focuses on AR and combination therapy.
May is designated as High Blood Pressure Awareness Month, culminating in World Hypertension Day on May 17. Hypertension, often dubbed as a silent killer, can have farreaching consequences if left uncontrolled.
From stroke and coronary artery disease to heart failure and chronic kidney disease, the implications of hypertension are profound. Our comprehensive coverage on this CPD topic aims to raise awareness

and equip healthcare professionals with the knowledge and tools needed to effectively manage hypertension in clinical practice.
In addition to these critical topics, we also explore the launch of generic combination therapy for the management of benign prostatic hyperplasia, shedding light on costeffective treatment options. Furthermore, we address the often overlooked issue of androgen deficiency as a consequence of long-term opioid use and the role of testosterone therapy in management.
As National Burns Awareness Week approaches from 13 -17 May, we emphasise the importance of appropriate wound dressings in promoting optimal wound healing and preventing complications.

We hope that the articles featured in this issue of Specialist Forum will enrich your knowledge base and contribute to improved patient care.
Remember to take advantage of the CPD points offered and stay tuned for more insightful content in our upcoming editions. Thank you for your continued support, and we look forward to your feedback.
Hope you enjoy the read!
Regards
René Bosman
Visit https://newmedia.b2bcentral.co.za/cd50b100-536e-40f9adf8-147c6bad0b09/index.html to update your calendar



Pharma Dynamics, a leading provider of generic drugs in South Africa, has recently introduced dutasteride, a 5-alpha reductase inhibitor (5-ARI), and tamsulosin, an alpha-1 adrenergic receptor antagonist (alpha blocker), combination therapy for the management of benign prostatic hyperplasia (BPH). Alpha blockers and/or 5-ARIs are recommended as first-line treatment. These two classes of drugs exhibit distinct abilities in influencing disease progression.1
BPH is characterised by the non-cancerous enlargement of the prostate gland, primarily thought to be driven by dihydrotestosterone (DHT), a metabolite derived from testosterone through the action of the enzyme 5-alpha reductase. 2
At the age of 60, ~50% of men present with microscopic BPH, which increases to ~90% among 85-year-olds. However, only about half of individuals with this histological indication will exhibit a noticeable enlargement of the prostate gland. Furthermore, among those with an enlarged gland, ~50% will develop symptoms associated with BPH.2
BPH frequently manifests as lower urinary tract symptoms (LUTS). The prevalence of LUTS is between 10%-30% for men in their 60s and 70s, and 30% in their 80s. While LUTS due to BPH can significantly impair individuals’ quality of life, it is noteworthy that not all men with BPH necessarily experience these symptoms, and conversely, not all men with LUTS have underlying BPH.2,3
Long-term complications of BHP include acute urinary retention (AUR), recurrent urinary tract infections, bladder stones, and post-obstructive kidney failure. AUR is one of the most common complications, with a risk reaching up to 14% over a decade in patients exhibiting large prostates and moderate to severe symptoms. 2
8 warning signs of BPH and causes Symptoms associated with BPH commonly arise due to either a narrowed urethra or an overtaxed bladder, both resulting from the obstruction caused by the enlarged prostate. Symptoms suggestive of BPH include:4
1 Urinary frequency – urination eight or more times a day.
2 Urinary urgency – the inability to delay urination.
3 Trouble starting a urine stream.
4 A weak or an interrupted urine stream.
5 Dribbling at the end of urination.
6 Nocturia – frequent urination during periods of sleep urinary retention.
7 Urinary incontinence – the accidental loss of urine.
8 Pain after ejaculation or during urination urine that has an unusual colour or smell.
The cause of BPH is not well understood. Throughout their lifespan, men produce both testosterone, commonly known as a male hormone, and small quantities of oestrogen. However, as men age, the level of active testosterone in their bloodstream decreases, leading to a higher proportion of oestrogen.4
Studies have suggested that this shift in hormonal balance may contribute to the development of BPH by enhancing the activity of substances that stimulate the growth of prostate cells. 4
As mentioned, it has been hypothesised that BPH is driven by DHT, which play an important role in prostate development and enlargement. Despite declining testosterone levels, older men often maintain elevated levels of DHT in their prostates. This accumulation of DHT might promote the continued growth of prostate cells. Notably, researchers have observed that men lacking DHT production do not develop BPH.4
BPH risk factors
Apart from age, risk factors for developing BPH include the presence genetics, a lifestyle factors, and metabolic syndromes including diabetes as well as obesity. Genetic factors play a significant role, with evidence indicating a strong hereditary component to
BPH risk, particularly among male relatives. Male relatives and brothers have a 4- and 6-fold increased risk, respectively. 3
Lifestyle factors, such as diet, physical activity, and alcohol consumption, significantly influence BPH progression. Dietary patterns rich in certain macronutrients and micronutrients may impact BPH risk. 3
Evidence suggest that both macronutrients and micronutrients might influence the risk of BPH, though findings are somewhat inconsistent. When it comes to macronutrients, higher total energy intake, energy-adjusted total protein intake, consumption of red meat, fat, milk and dairy products, cereals, bread, poultry, and starch have all been linked to potentially increased risks of clinical BPH and BPH surgery. Conversely, intake of vegetables, fruits, polyunsaturated fatty acids, linoleic acid, and vitamin D may potentially decrease the risk of BPH.3
Regarding micronutrients, higher levels of circulating vitamin E, lycopene, selenium, and carotene have shown inverse associations with BPH. However, zinc’s association with BPH risk appears to be more complex, as it has been linked to both increased and decreased risk in different studies. The good news is that increased physical activity and moderate alcohol intake have been linked to decreased BPH risk. 3
Metabolic syndrome components, including obesity, diabetes, and disruptions in glucose homeostasis, are associated with increased prostate volume and heightened BPH risk. Obesity, in particular, is consistently linked to prostate enlargement and an elevated risk of urinary symptom progression and BPH-related interventions. While associations between lipids and BPH remain less explored, evidence suggests potential correlations. 3
INDICATED FOR THE TREATMENT OF MODERATE TO SEVERE SYMPTOMS OF BENIGN PROSTATIC HYPERPLASIA (BPH)
The 4-year CombAT study provides support for the long-term use of dutasteride and tamsulosin combination therapy in men with moderate to severe LUTS* due to BPH and prostatic enlargement1 *LUTS – Lower urinary tract symptoms



BPH typically progresses slowly, with severe complications being rare. For those with mild symptoms, a watchful waiting approach alongside lifestyle adjustments, such as regular physical activity, may suffice. While clinicians often recommend avoiding irritants like coffee and alcohol, evidence supporting these suggestions is scant. 2
While surgery (transurethral resection of the prostate [TURP]) is the gold standard for managing BPH, medical therapy is often favoured over surgical intervention in older men when feasible. Pharmacotherapy selection should consider patient age, symptoms, prostate size, comorbidities, and potential adverse effects like ejaculatory dysfunction and changes in blood pressure.2,5,6
The 2023 updated American Urology Association (AUA) guidelines recommend alpha blockers as first-line treatment for individuals living with moderate to severe symptoms, offering choices such as tamsulosin. 6
For patients with prostatic enlargement, 5-ARIs are recommended for symptom improvement and to prevent progression or reduce the risk of urinary retention and future surgery. These inhibitors may also be considered to reduce bleeding and the need for blood transfusion after surgical interventions like TURP. 6
For AUR due to BPH, oral alpha blockers should be prescribed before a voiding trial, and patients newly treated for AUR should complete at least three days of medical therapy before attempting a trial without a catheter. 6
When is combination treatment indicated?
According to the AUA, combination therapy, particularly 5-ARIs with alpha blockers, should be offered to patients with demonstrable prostatic enlargement and predominant storage symptoms. 6
The use of tamsulosin for LUTS due to BPH provides a rapid response, manifesting as a significant reduction in both storage and voiding symptoms within hours or days compared to placebo. Clinical trials have shown that tamsulosin improves symptom scores by 20% to 48% and increases maximum flow rate (Q-max) by 13% to 44%.7
On the other hand, 5-ARIs like dutasteride induce apoptosis of prostatic cells by suppressing DHT levels, leading to a reduction in prostate volume. Dutasteride significantly reduces serum DHT levels by 95%, resulting in a reduction of 94-97% of DHT levels in the prostate. Dutasteride treatment for six to 12 months reduces prostate size by 18%-28%, decreases
circulating prostate-specific antigen (PSA) levels by 50% and increases Q-max by 1.52.0 ml/s in patients with BPH-associated bladder outlet obstruction.7
How effective is combination therapy with dutasteride/tamsulosin?
The Combination of Avodart® and Tamsulosin (CombAT) study investigated the efficacy of combination therapy with dutasteride/tamsulosin compared to monotherapy in men with moderateto-severe LUTS due to BPH and prostatic enlargement.1
Conducted over four years, this multicentre, randomised, double-blind study included 4844 men aged ≥50-years with a clinical diagnosis of BPH, International Prostate Symptom Score (IPSS) of ≥12, prostate volume of ≥30cm3 or greater, PSA levels between 1.5-10ng/ml, and Q-max between 5-15 ml/s with a minimum voided volume of 125ml.1
Participants were randomly assigned to receive oral daily doses of tamsulosin (0.4mg) or dutasteride (0.5mg), or a combination of both agents. The primary endpoint was the time to first AUR or BPH-related surgery, while secondary endpoints included BPH clinical progression, symptoms, Q-max, prostate volume, safety, and tolerability.1
The results showed that combination therapy with dutasteride/tamsulosin was significantly more effective than tamsulosin monotherapy in reducing the relative risk of AUR or BPH-related surgery. Combination therapy was also superior to both monotherapies in reducing the relative risk of BPH clinical progression.1
Additionally, combination therapy provided greater symptom relief compared to monotherapy at the four-year mark.
The safety and tolerability profile of combination therapy were consistent with previous experiences with dutasteride and tamsulosin monotherapies.1
The authors concluded that their results support the long-term use of combination therapy with dutasteride/tamsulosin for men with moderate-to-severe LUTS due to BPH and prostatic enlargement.1
Timing of combination therapy initiation
D’Agate conducted a study to assess the impact of delaying the initiation of combination therapy with dutasteride 0.5mg and tamsulosin 0.4mg on the risk of AUR or BPH-related surgery in patients with moderate-to-severe LUTS at risk of disease progression. 8
Using data from Phase III/IV dutasteride trials, they employed clinical trial
simulations to evaluate the risk of AUR or BPH-related surgery over 48 months in patients with moderate-to-severe LUTS/ BPH who did not respond to tamsulosin monotherapy. Various simulation scenarios were explored, including immediate start and delayed start of combination therapy (ranging from one to 24 months).
8
The results showed that patients who initiated combination therapy at months one or three did not exhibit significantly different outcomes compared to those who started immediately. However, a notable difference was observed in patients who switched to combination therapy after ≥6 months from the initial treatment.
8
By month 48, the incidence of AUR or BPH-related surgery was markedly lower (4.6%) in patients who received immediate combination therapy compared to those who switched after six, 12, or 24 months (9.5%, 11.0%, and 11.3%, respectively).
8
In conclusion, initiating combination therapy before month six was associated with a significantly reduced risk of AUR/S compared to delaying treatment by ≥6 months. These findings suggest implications for the treatment approach in men with LUTS/BPH at risk of disease progression.8
The management of BPH presents a multifaceted challenge, particularly in ageing populations where its prevalence is high. Understanding the interplay of hormonal changes, genetic predispositions, and lifestyle factors is crucial for effective intervention. While BPH typically progresses slowly, complications such as AUR can have significant implications for patients’ quality of life.
Combination therapy, notably with dutasteride/tamsulosin, has emerged as a promising approach to address the multifactorial nature of BPH. The CombAT study demonstrated the long-term efficacy of this combination in reducing the risk of AUR or BPH-related surgery, providing superior symptom relief compared to monotherapy. Additionally, D’Agate’s study underscores the importance of timely initiation of combination therapy to mitigate disease progression risks. Moving forward, integrating combination therapy into clinical practice, particularly in patients with moderate-to-severe BPH and prostatic enlargement, could enhance treatment outcomes and improve long-term prognosis. However, individualised approaches considering patient characteristics and preferences remain paramount in optimising BPH management strategies.
The reference list is available on www.medicalacademic.co.za SF

More than 95% of burn-related deaths occur in low- and middle-income countries. Africa contributes to 15% of the global burn mortality. In South Africa, children <2-years of age and those from minority (migrant) groups face the highest risk of burn injuries in South Africa.1,2
Arecent study by Banga et al, showed that about 50% of patients admitted to the Chris Hani-Baragwanath Hospital (Soweto, Johannesburg) were aged between 15- and 47-months, with a median age of 25-months. 2
Of the participants, 58% were boys. Scalding (84%) was the most common injury, primarily occurring in the winter season (32%). The upper limb was the most common site of burn (75%). Severe burns were associated with thermal injury mechanisms, and multiple burn sites. 2
A South African study of adult burn survivors showed that thermal burns were the most frequently reported type, accounting for 64.4% of cases, and the median total body surface area (TBSA) affected was 31% – predominantly the head (60.3%) and arms (71.2%). 3
Burns affect various aspects of patient’s lives
The impact of burn injuries extends beyond physical health, affecting various aspects of a patients’ lives, including social, physiological and economic dimensions.1
Social and physiological dimensions
Children and young people who have suffered burn injuries are more susceptible to developing psychopathology compared to the general population, according to Woolard et al. 4
Research shows an increased risk of posttraumatic stress disorder (nightmares and hypervigilance) within the first month after the burn injury, with long-term psychological issues such as anxiety, depression, sleep disturbances, social functioning, and diminished quality of life also being reported.4
The complexity of burn aftercare contributes to these challenges, involving invasive and painful treatments to improve function and reduce scarring. Frequent hospital visits serve as distressing reminders of the injury. 4
To design effective, trauma-informed, person-centred treatments for burn injuries, it is essential to understand the experience of the child or young person’s perspective, stress Woolard et al 4
In their study, the team categorised the impact of burn injuries into burn-specific impacts (appearance concerns, family factors, and lifestyle factors), psychological impacts, and the recovery journey (coping strategies and support services). 4
Participants reported appearance concerns due to scarring and the need for pressure garments, causing anxiety about how they would be perceived by others. 4
Caregiver guilt was a consistent theme, with participants acknowledging their caregivers often blamed themselves, which stresses the need for caregiver support. Disruptions to schooling and lifestyle activities had a significant impact, causing anxiety and affecting social support. 4
Participants also exhibited resilience, acknowledging negative emotions and adopting coping mechanisms like mindfulness and social support.
Participants advocated for mental health support to be a routine part of care for burn patients. 4
Considering the impact on caregivers, a trauma-centred approach for the family unit, including resilience building and healthy coping mechanisms, recommended Woolard et al Overall, understanding the experiences of burn patients is crucial for developing effective interventions and treatments, concluded the authors. 4
Appropriate burn injury dressing choices in primary management are extremely important
According to the World Health Organization, the direct expenses associated with burn care vary considerably. A systematic review conducted in 2014 showed an average overall healthcare expenditure of ~R1.7m ($88 218) per burn patient, ranging from ~R14 000 ($704) to ~R14m ($717 306). In South Africa, ~R500m ($26m) is spend annually on the treatment of burns resulting from kerosene (paraffin) cookstove incidents.5
Beyond direct costs, indirect expenses such as foregone wages, extended care for deformities and emotional trauma, and the utilisation of family resources also contribute significantly to the socioeconomic impact of burn injuries. 5
What does the optimal management of burn patients involve?
According to Allorto the optimal management of burn injuries relies on adherence to key principles. Each of these components significantly influences
outcomes in burn care:6
_ First aid measures
_ Prompt washing of burn injuries
_ Fluid resuscitation
_ Early enteral feeding
_ Appropriate dressing of burn injuries
_ Effective analgesia.
In primary care, first aid for burns involves cooling the burn with cool running tap water, demonstrating a decrease in cellular damage and swelling. This approach enhances the inflammatory response, promotes healing, and reduces the need for skin grafting.
Ice application is discouraged due to its potential to cause prolonged vasoconstriction. Immediate removal of clothing and jewellery, along with the application of cling film or a clean nonadhesive dressing, is advised.
6
In terms of blister management, Allorto highlighted a 2017 study indicating no significant difference in outcomes between deroofing or aspiration. Cleaning larger burns of all blisters and debris is recommended, although the choice of cleaning agent lacks clear evidence. 6
Fluid resuscitation is crucial, considering the inflammatory response, vasodilation, and capillary leak associated with burn injuries. Use of Ringers lactate or equivalent fluid is preferred, and early enteral feeding is advocated for burns >15%-20% TBSA. Avoiding over-resuscitation, and fluid continuation post-24 hours should be based on clinical signs of dehydration. 6
Dressing burn injuries involves avoiding prophylactic antibiotics, relying on good injury care, and using topical antimicrobial dressings judiciously (see below). Effective analgesia is crucial in burn care – especially considering the physiological and psychological impact of pain. 6
Ketamine and methoxyflurane are recommended for procedural analgesia, and a dynamic approach to background analgesia, considering changing needs, is advocated. Addressing itching and psychological aspects, including anxiety and depression, is essential. 6
According to Allorto, appropriate burn injury dressing choices in primary management are extremely important. Injury dressing is crucial as it serves multiple functions. Firstly, it shields the injured epithelium, curbing microbial colonisation and maintaining skin position. Secondly, it should be occlusive to retain heat and moisture, enhancing healing conditions. 6,7 Comfort provision to the sensitive injury
Effectively prevents and treats wound infection1,2
93 % of wounds were healed or improved1











Sorbact® Technology dressings reduce the bioburden in wounds3
Effective against the Top 5 WHO (World Health Organisation) pathogens, as shown in vitro.4
Can be used during the entire wound healing process.2
1Chadwick
2Kammerlander
3Mosti

Sponsored content
is another essential aspect. Furthermore, an ideal dressing should possess various properties including moisture control, efficient exudate removal, gas exchange facilitation, low skin adhesion, mechanical stability, injury necrosis reduction, costeffectiveness, non-toxicity, biocompatibility, and biodegradability.7
The choice of dressing depends on the burn injury characteristics. Superficial first-degree injuries with minimal barrier loss may not necessitate dressing, instead, topical balms, panthenol, and aloe vera gels suffice for pain relief and moisture maintenance.7
Conversely, second-degree superficial injuries may require daily dressing changes with topical antibiotics or temporary biological or synthetic dressings. Deeper burns often require excision and grafting, necessitating dressings focused on bacterial control and injury closure pre-surgery.7
Injury dressings come in various materials including natural polymers (chitosan, cellulose, collagen), synthetic polymers (polyvinylpyrrolidone, polyethylene oxide/ polyethylene glycol, polylactic acid), and combinations thereof, available as hydrogels, films, foams, and more.7
Many dressings incorporate silver and other antimicrobial agents. The efficacy of these dressings varies. For partialthickness superficial burns, biosynthetic epithelial substitutes like or advanced injury bioengineered alternative tissue-superficial can be used for post-injury cleaning. Despite their proven efficacy, availability remains an issue in South Africa.7
Hydrocolloid dressings are notable for their ability to absorb exudate and promote injury healing and is often preferred over paraffin-based gauze. Hydrogels offer flexibility and moisture retention, and often contain additional therapeutic agents for enhanced healing.7
Inorganic materials like silicate minerals and metal-containing materials possess haemostatic properties, while nanomaterials exhibit antibacterial activity and aid injury regeneration. Nanoparticles, both organic and inorganic, show promise in injury healing due to their unique properties and controlled release mechanisms.7
Overall, the choice of dressing significantly impacts burn injury healing, with a plethora of options available catering to diverse injury types and patient needs.7
The efficacy of antimicrobial dressings
Numerous studies have shown the critical association between a wound’s microbial bioburden and its healing trajectory.
Antimicrobial dressings offer promise in both healing and infection control. 8
Wound bacteria are categorised as contamination, colonisation, or infection, each with distinct implications for healing. Symptoms of infected wounds include erythema, warmth, and increased drainage. Antimicrobial dressings are indicated for suspected colonisation or infection to impede bacterial growth and aid healing. 8
Wound dressings play a dual role: Creating an ideal moisture environment for re-epithelialisation and acting as a barrier against microbial infiltration. Various dressing types such as hydrocolloid, hydrogel, foam, alginate, and antimicrobial variants, offer diverse clinical benefits. Antimicrobial dressings incorporate disinfectants, antiseptics, or antibiotics to diminish local wound bioburden, contributing to improved wound healing. 8
The use of dressings that rely on a physical mode of action has proved extremely effective in managing bioburden. Dialkylcarbamoyl chloride (DACC™) a fatty acidderivative, utilises hydrophobic interation, where hydrophobic particles aggregate in an aqueous environment.9
The dressings are coated with a fatty acid derivative, making them strongly hydrophobic. Since wound bacteria also have hydrophobic characteristics, they bind to the dressing fibres and are removed when the dressing is changed.9
In a multicentre investigation led by Kammerlander et al, examined a hydrophobic wound dressing in the management of patients with chronic wounds. The study assessed the dressing’s efficacy in binding and removing bacteria from wounds without introducing chemically active agents. Evaluation criteria included its capacity to reduce inflammation, eradicate local infections, and enhance wound healing progression, alongside patient tolerance and clinician usability.9
Results showed that 81% of patients with infected wounds experienced effective treatment, with 21% of all wounds healing during the study period and 72% demonstrating improvements. Additionally, notable enhancements in pain symptoms were observed, and most patients expressed positivity towards the product. Clinicians also rated it highly, with 97% evaluating it as ‘good’ or ‘very good’.9
Kleintjes et al used a wound dressing with hydrophobic interaction as a skin substitute based on previous observations suggesting successful healing of partial thickness burn wounds. The study included 27 patients with superficial and mid-partial thickness burns. Wound assessments were done
weekly, evaluating factors such as wound appearance, slough, pus, biofilm, granulation, epithelium, smoothness, and colour.10
Results showed that most wounds appeared clean (59%), dry (51%), and pink (51%), with 27% appearing healed. Subjective pain related to the dressing was minimal. Minor complications, such as punctate bleeding points upon dressing removal, were noted in five patients (18.5%). The study concluded that the hydrophobic dressing serves as a cost-effective skin substitute with antibacterial and antiviral properties, making it a valuable addition to available skin substitutes.10
How long does it take for a burn injury to heal?
The healing process of burn injuries varies depending on their severity, ranging from superficial to complete injuries. Superficial burns typically affecting the epidermis heal within weeks without scarring, while deeper injuries necessitate longer healing times due to extensive tissue damage.7
Rapid injury cleansing, whether through surgical debridement or specialised dressings, plays a pivotal role. Autologous skin grafts remain the gold standard, although alternatives like artificial skin substitutes are actively explored for their potential to enhance closure, minimise scarring and streamline treatment processes.7
Effective treatment strategies for burn injuries require a multifaceted approach, considering both physical and psychological factors. With a disproportionate burden in low- and middle-income countries, particularly in Africa, understanding regional epidemiology and socioeconomic impacts is crucial.
Optimal management, as outlined by Allorto, emphasises adherence to key principles from initial first aid to injury dressing choices. By integrating evidencebased practices and prioritising patientcentred care, healthcare systems can mitigate the profound and far-reaching consequences of burn injuries on individuals and communities alike.
References are available on request. SF
EPCLUSA® is indicated for the treatment of chronic hepatitis C infection irrespective of genotype in treatment naïve or treatment experienced patients aged 12 years and older and weighing at least 30 kg:
- without cirrhosis or with compensated cirrhosis
- with decompensated cirrhosis in combination with ribavirin 1
a,b,c 1,2,3
Proven cure ratec: 98,9 % in real-world analysis2,3
Suitable for patients with various levels of liver disease severityb,d 2,3


Pan-genotypic and pan-fibroticb,d 3
1 tablet once daily, with or without food, for 12 weeks1
1,2,3
Footnotes: aDespite unknowns in baseline characteristics of some patients, such as: HCV genotype, fibrosis stage, former/current IV drug use, PPI use at baseline and treatment history.3 bA large-cohort international real-world study showed that patients with unknown genotype (n = 42), unknown fibrosis score (n = 82) and unknown treatment history (n = 33) were cured with EPCLUSA® for 12 weeks. Cure is defined as SVR i.e., undetectable HCV RNA after treatment completion.3,4 cCases of HBV reactivation, some of them fatal, have been reported during or after treatment with direct acting antiviral agents including EPCLUSA®. HBV screening should be performed in all patients before initiation of treatment. Treatment with EPCLUSA® should not be initiated in patients who screened positive for hepatitis B virus infection. HBV/HCV coinfected patients are at risk of HBV reactivation, and should therefore be monitored and managed according to current clinical guidelines.1 dPatients with decompensated cirrhosis use EPCLUSA® + ribavirin for 12 weeks.1
Abbreviations: HCV = Hepatitis C Virus; RNA = Ribonucleic acid; IV = Intravenous; PPI = Proton pump inhibitor; SVR = Sustained virological response; HBV = Hepatitis B virus.
References: 1. Epclusa Professional Information approved by the medicine’s regulatory authority. 10 March 2022. 2. Lawitz E, Bourliere M, Han L, McNally J, Stamm LM, Brainard DM, et al. Treatment with SOF/VEL or SOF/VEL/VOX is well tolerated and results in high SVR12 in genotype 1-6 HCV-infected patients with minimal fibrosis: a retrospective analysis of the ASTRAL and POLARIS clinical studies. Poster THU-273 presented at the International Liver Congress 2017, April 19–21, Amsterdam, The Netherlands. Available at: https://www.natap.org/2017/EASL/EASL_07.htm [Accessed 24 March 2022]. 3. Mangia A, Milligan S, Khalili M, Fagiuoli S, Shafran SD, Carrat F, et al. Global real-world evidence of sofosbuvir/ velpatasvir as simple, effective HCV treatment: Analysis of 5552 patients from 12 cohorts. Liver Int 2020;40:1841–1852. 4. National Guidelines for the Management of Viral Hepatitis. Department of Health Republic of South Africa Available at: https://sahivsoc.org/Files/SA%20NDOH_Viral%20Hepatitis%20guideilnes%20final_.pdf [Accessed 10 March 2022]. For full prescribing information refer to the professional information approved by the Medicines Regulatory Authority. S4 EPCLUSA® 400 mg/100 mg film-coated tablets. Reg. No.: 51/20.2.8/0872. Each film-coated tablet contains 400 mg sofosbuvir and 100 mg velpatasvir. Gilead Sciences South Africa (Pty) Ltd., Reg No.: 2014/063761/07, Ground Floor Mac Mac Building, Maxwell Office Park, Magwa Crescent, Waterfall. (Tel: +27 10 346 1920). For any adverse events, please contact: Safety_FC@gilead.com or drugsafetysouthafrica@gilead.com | EPCLUSA®, the EPCLUSA® Logo, GILEAD and the GILEAD Logo are trademarks of Gilead Sciences, Inc. or its related companies. All other trademarks referenced herein are the property of their respective owners. ©2023 Gilead Sciences, Inc. All rights reserved. Date of preparation: 02/2023 | Job code: ZA-EPC-0022

An estimated 1.28 billion adults between 30- and 79-years are living with hypertension globally.
More than 60% live in low- and middle-income countries. In South Africa >30% of adults are currently living with the condition, which are responsible for ~50% of strokes and ~40% of MIs. 3,4
Often referred to as a ‘silent killer’, hypertension typically manifests without noticeable symptoms or visible warnings, leaving >50% of affected individuals unaware of their condition. 4
While symptoms like headaches, visual disruptions, nosebleeds, nausea, vomiting, facial flushing, and sleepiness may arise in cases of exceptionally high blood pressure (BP), the absence of overt signs highlights the urgent need for proactive monitoring and awareness of this potentially lifethreatening condition.
Men have a higher risk of hypertension (34%) compared to women (32%).
Furthermore, only ~20% of adults living with hypertension have it under control. 2,3,4
May is designated as High Blood Pressure Awareness Month, with the culmination being World Hypertension Day on May 17. The American Heart Association describes hypertension as a domino effect, which can lead to an increased risk of stroke, coronary artery disease (CAD), heart failure (HF), myocardial infarction (MI), vision impairment, chronic kidney disease, dyslipidaemia, impaired glucose tolerance, type 2 diabetes, and sexual dysfunction.1,2
According to the 2023 European Society of Hypertension (ESH) guidelines, hypertension is defined as: Repeated office systolic BP (SBP) values of 140mmHg and/or diastolic BP (DBP) 90mmHg. The society cautions that life-threatening cardiovascular (CV) and renal events can also occur at low BP levels (eg 115mmHg/75mmHg). 2
Hypertension is classified into:2,5
Responsible for the majority of cases.
Caused by an interplay between genetic and environmental factors, as well as the ageing process. Genetic and environmental factors induce changes in CV regulatory systems, leading to increased systemic vascular resistance – a key haemodynamic abnormality in hypertension. Studies show that alterations in major CV control systems, including the renin-angiotensinaldosterone system (RAAS), autonomic
cardiac and vascular regulation, the endothelin system, nitric oxide, natriuretic peptides, and gut microbial dysbiosis, contribute to chronic BP elevation. 2
The immune system, particularly inflammation, has also been implicated in the pathophysiology of hypertension. Inflammation is thought to influence BP regulation and has been implicated in the onset of, and progression to hypertensive target organ damage (HMOD). 2
Secondary hypertension
Accounts for 5%-10% of cases. More common (prevalence ~30%) in younger individuals (18- to 40-years). Arises from specific causes such as:2,5
_ Renovascular hypertension: Defined as systemic hypertension that manifests secondary to the compromised blood supply to the kidneys, usually due to an occlusive lesion in the main renal artery
_ Renal disease
_ Aldosteronism: A disorder caused by autonomous production of aldosterone
Losartan potassium 50/100 mg

Bisoprolol fumarate 2.5/5/10 mg

Losartan potassium/hydrochlorothiazide 50/12.5 mg, 100/25 mg

Perindopril tert-butylamine 4/8 mg

Metformin hydrochloride 500/850/1000 mg







Amlodipine besilate 5/10 mg
Ezetimibe 10 mg
Torasemide 5/10 mg
SAHPRA approved ANNIN professional information. Date of publication: 18 September 2021. S3 ANNIN 50 mg (tablet). Reg. No.: 43/7.1.3/0494. S3 ANNIN 100 mg (tablet). Reg. No.: 43/7.1.3/0495. Each film-coated tablet contains 50 mg or 100 mg losartan potassium respectively. Contains sugar: 40 mg or 80 mg lactose respectively. SAHPRA approved ANNIN CO professional information. Date of publication: 24 February 2023. S3 ANNIN CO 50/12,5 mg (film-coated tablet). Reg. No.: 45/7.1.3/1054. S3 ANNIN CO 100/25 mg (film-coated tablet). Reg. No.: 45/7.1.3/1055. Each film-coated tablet contains 50 mg losartan potassium/12,5 mg hydrochlorothiazide or 100 mg losartan potassium/25 mg hydrochlorothiazide respectively. Contains sugar: 111 mg or 222 mg lactose respectively. SAHPRA approved APRATE professional information. Date of publication: 30 December 2023. S3 APRATE 5 mg (tablet). Reg. No.: 41/7.1/00754. S3 APRATE 10 mg (tablet). Reg. No.: 41/7.1/0755. Each tablet contains 5 mg or 10 mg amlodipine besilate respectively. Sugar free. SAHPRA approved BISBETA professional information. Date of publication: 11 February 2022. S3 BISBETA 2,5 mg (tablet). Reg. No.: 45/5.2/0789. S3 BISBETA 5 mg (tablet). Reg. No.: 45/5.2/0790. S3 BISBETA 10 mg (tablet). Reg. No.: 45/5.2/0791. Each film-coated tablet contains (2:1) 2,5 mg, 5 mg or 10 mg bisoprolol fumarate respectively. Sugar free. SAHPRA approved EZOTAK professional information. Date of publication: 17 August 2021. S3 EZOTAK (tablets). Reg. No.: 52/7.5/0279. Each tablet contains 10 mg ezetimibe. Contains sugar: 62 mg lactose. Sugar free. SAHPRA approved REPREX professional information. Date of publication: 18 September 2021. S3 REPREX 4 mg (tablet). Reg. No.: 43/7.1.3/1033. S3 REPREX 8 mg (tablet). Reg. No.: 43/7.1.3/1034. Each uncoated tablet contains 4 mg or 8 mg perindopril tert-butylamine respectively. Contains sugar: 59,33 mg or 118,66 mg lactose respectively. SAHPRA approved RISAT professional information. Date of publication: 13 December 2022. S3 RISAT 5 mg (tablet). Reg. No.: 43/18.1/1042. S3 RISAT 10 mg (tablet). Reg. No.: 43/18.1/1043. Each uncoated tablet contains 5 mg or 10 mg torasemide anhydrous respectively. Contains sugar: 79 mg or 158 mg lactose respectively. SAHPRA approved ROMIDAB TABLETS professional information. Date of Publication: 7 October 2021. S3 ROMIDAB 500 mg (tablet). Reg. No.: 45/21.2/0207. Each film-coated tablet contains 500 mg metformin hydrochloride. Sugar free. S3 ROMIDAB 850 mg (tablet). Reg. No.: 45/21.2/0208. Each film-coated tablet contains 500 mg metformin hydrochloride. Sugar free. S3 ROMIDAB 1000 mg (tablet). Reg. No.: 45/21.2/0209. Each film-coated tablet contains 500 mg metformin hydrochloride. Sugar free. SAHPRA approved URODOXA professional information. Date of publication: 20 December 2023. S3 URODOXA 4 mg (tablet). Reg. No.: 45/7.1/0152. Each uncoated tablet contains doxazosin mesilate equivalent to doxazosin 4 mg. Contains sugar: 48 mg lactose. For full prescribing information refer to the professional information approved by the medicines regulatory authority.
HCR: AUROGEN SOUTH AFRICA (PTY) LTD. Woodhill Office Park, Building 1, First floor, 53 Phillip Engelbrecht Avenue, Meyersdal Ext 12, 1448, Johannesburg, South Africa. Tel: (011) 867 9100, Fax: (011) 867 9111 or visit us at www.auro-space.com ASA.24.04.1103
by the adrenal cortex due to hyperplasia, adenoma, or carcinoma _ Obstructive sleep apnoea. Secondary hypertension can also be caused by mutations in specific genes, mostly coding for proteins involved in sodium tubular reabsorption or steroid metabolism. 2,5
A diagnosis of secondary hypertension should be considered when a young individual presents with symptoms such as either severe hypertension (>180mmHg/120mmHg), resistant hypertension (defined as BP that remains >140/90mmHg despite optimal use of three antihypertensive medications of different classes, including a diuretic), or malignant/accelerated hypertension (defined as a recent significant increase over baseline BP that is associated with target organ damage).2,5
Management of hypertension: Antihypertensive treatment
Antihypertensive treatment is crucial to reduce CV events, mortality, and organ damage associated with hypertension. The main objective of antihypertensive treatment should be to lower BP to <140/90mmHg in all patients. 2
If treatment is well tolerated, treated BP values should be targeted to ≤130/80mmHg, with the caveat that in some clinical conditions (eg chronic kidney disease), the evidence for this lower BP target is uncertain. It is also recommended that treatment should never target BP values to <120/70mmHg because of the lack of consistent evidence.2
The benefits of antihypertensive treatment are well-supported by numerous outcomebased randomised controlled trials (RCTs). While lifestyle changes (see below) can improve BP and overall CV risk, the majority of patients will require pharmacotherapy.2
Meta-analyses have consistently shown that a 7mmHg average reduction in SBP lowers the risk of major CV events such as stroke, CAD and HF, as well as all-cause mortality.2
Antihypertensive treatment has also demonstrated a protective effect against asymptomatic CV and kidney damage. Furthermore, increasing evidence suggests that antihypertensives resulting in lowered BP levels can prevent cognitive decline and dementia, irrespective of baseline BP, CV risk, comorbidities, age, sex, or ethnicity.2
Recent meta-analyses indicate that the advantages of antihypertensive treatment remain consistent, even with the concomitant use of other pharmacotherapies such as lipid-lowering, antidiabetic, and antiplatelet agents. 2
Furthermore, comprehensive costeffectiveness analyses support the use of pharmacological treatment for hypertension. The prevention of fatal and non-fatal events, which can lead to hospitalisation and morbidity, result in a substantial reduction in healthcare-related costs. The cost-effectiveness is attributed to the use of inexpensive drug classes, often available as generics. 2
According to the ESH, the decision to initiate treatment should be based on office BP levels rather than CV risk alone. Grade 2 or 3 hypertension typically requires drug treatment (see Table 1). Together with pharmacotherapy, lifestyle changes (see below) is recommended for the treatment for grade 1 hypertension in patients at high risk of CVD. 2
Regarding treatment initiation in patients with BP <140/90mmHg, the guidelines discourage antihypertensive treatment in patients who have a low-to-moderate risk of CVD with high-normal BP. Lifestyle changes are recommended for these patients. In patients with BP >140/90mmHg, but at high risk of CVD, treatment initiation is warranted.2
For patients aged 60- to 79-years, the

guidelines recommend initiating treatment when SBP is ≥140mmHg, regardless of DBP levels. This recommendation includes patients with isolated systolic hypertension even if DBP is <90mmHg or <80mmHg. 2
Recent trials have shown significant CV benefits with BP-lowering treatment in this age group. In patients aged ≥80-years. However, the Hypertension in the Very Elderly Trial (HYVET) demonstrated benefits in patients with SBP ≥160mmHg. 2
The recommended SBP threshold for pharmacotherapy in this age group is 150mmHg based on extrapolation from HYVET data. A critical recommendation is to continue antihypertensive treatment in patients who tolerate treatment. Discontinuation is associated with a rebound increase in adverse outcomes. 2
Exceptions can be considered for very old patients with low SBP values (≤120mmHg) or severe orthostatic hypotension, especially those who use polypharmacy and have high frailty levels. 2
Key drug classes include: _ Angiotensin-converting enzyme inhibitors (ACEis) _ Angiotensin II receptor blockers (ARBs) _ Beta-blockers (BBs) _ Calcium channel blockers (CCBs) _ Thiazide/thiazide-like diuretics. These agents along with their combinations, are recommended as first-line therapy in the management of hypertension. Initiation of therapy with a two-drug combination is recommended for the majority of patients living with hypertension. 2
Single- or multi-pill combinations are preferred. Recommended combinations are an ARB with a CCB or a thiazide/ thiazide-like diuretic. BBs should be used at therapy initiation or any treatment step – particularly in conditions like HF with reduced ejection fraction, antiischaemic therapy in chronic coronary syndromes, and heart rate control in atrial fibrillation. However, caution is advised, when considering BBs appropriate patient selection is crucial. 2
Furthermore, combinations that provide 24-hour BP control and once-daily drug administration are preferred. Extendedrelease formulations and bedtime administration may be considered, with evidence suggesting no harm in taking antihypertensive drugs at bedtime. 2
In certain cases, initiation with monotherapy may be considered for patients with grade 1 hypertension and low risk, highnormal BP with very high CV risk, or those exhibiting frailty and advanced age.2

We can control 60% of patients in the general hypertensive population with dual therapy3
- Prof Reinhold Kreutz, co-chair of the ESH Hypertension Guidelines
Perindopril tosilate and Amlodipine
5 mg / 5 mg; 5 mg / 10 mg; 10 mg / 5 mg; 10 mg / 10 mg


S3 TEPRILAM 5 / 5 (tablets) Reg. No. 55/7.1.3/0809. Each tablet contains Perindopril Tosilate 5 mg and amlodipine 5 mg.
S3 TEPRILAM 5 / 10 (tablets) Reg. No. 55/7.1.3/0810. Each tablet contains Perindopril Tosilate 5 mg and amlodipine 10 mg.
S3 TEPRILAM 10 / 5 (tablets) Reg. No. 55/7.1.3/0811. Each tablet contains Perindopril Tosilate 10 mg and 5 mg amlodipine.
S3 TEPRILAM 10 / 10 (tablets) Reg. No. 55/7.1.3/0812. Each tablet contains Perindopril Tosilate 10 mg and amlodipine 10 mg. For full prescribing information please refer to the professional information approved by the Medicines Regulatory Authority. Recommendations, side effects and precautions to be followed by healthcare professionals and patients for the safe and effective use of Teprilam have also been included in the Professional Information and the Patient Information Leaflet. For more information, see the Professional Information/Patient Information leaflet.
References:
1. Manolis et al. (2015). ‘Blood pressure reduction and control with fixed-dose combination perindopril/amlodipine: A Pan-Hellenic prospective observational study’, Journal of the Renin-Angiotensin-Aldosterone System.,16(4), pp 930– 935.
2. Bahl, V.K., et al. (2009). ‘Management of hypertension with the fixed combination of perindopril and amlodipine in daily clinical practice’. AM J Cardiovasc Drugs., 9(3),pp.135-142.
3. Hughes, S., 2023. ‘New ESH hypertension
If BP control is not achieved with the initial two-drug combination, escalation to a three-drug combination is recommended, typically comprising a RAAS blocker, CCB, and thiazide/thiazide-like diuretic. The combination of two RAAS blockers is discouraged due to an increased risk of adverse events, particularly acute kidney injury (AKI). In cases where BP remains uncontrolled with a three-drug combination, treatment for true resistant hypertension is recommended. 2
Several arguments support the use of two antihypertensives at the onset of treatment. Firstly, evidence suggests that initial combination therapy is consistently more effective in lowering BP than monotherapy. Even low-dose combination therapy tends to surpass the efficacy of maximal dose monotherapy. 2
This approach not only reduces the heterogeneity of BP response but also provides a steeper dose-response effect compared to escalating doses of monotherapy. Moreover, it is considered safe and well-tolerated, with minimal increase in the risk of hypotensive episodes, even in patients with grade 1 hypertension. 2
Secondly, the use of a two-drug combination leads to a faster reduction in BP compared to monotherapy. Observational evidence indicates that the time taken to achieve BP control is a critical determinant of clinical outcomes, particularly in high-risk patients, with shorter time to control associated with lower risk. 2
Thirdly, studies show that patients starting treatment with a two-drug combination are more likely to achieve frequent BP control
after one year. This is attributed to the prevention of therapeutic inertia, better long-term adherence, and persistence to the prescribed treatment regimen. 2
For patients whose BP is not adequately controlled with two-drug combination therapy, options include:2
_ Using a different two-drug combination
_ Increasing the dose of the current combination components
_ Transitioning to three-drug combination therapy, usually involving a RAAS inhibitor, a CCB, and a thiazide/thiazide-like diuretic.
What about fixed-dose combination therapy?
Although single-pill combinations are preferred, Verma et al found that fixed-dose combination (FDC) therapy improves patient adherence to treatment. The team conducted a retrospective cohort study comparing clinical outcomes and medication adherence in a real-world setting between FDC therapy and single-pill combination therapy.5
The study included 13 350 participants who were newly prescribed either an ACEi or ARB in combination with a thiazide diuretic, with a

follow-up period of up to five years.5
To minimise selection bias, the researchers employed high-dimensional propensity score matching to compare outcomes between those receiving FDC and single-pill therapy.5 The primary outcome was a composite of death or hospitalisation for acute MI, HF, or stroke. Two analyses were performed to assess the association between medication adherence and patient outcomes.5
In the on-treatment analysis, where patients were censored upon discontinuation of treatment, no significant difference in the primary outcome was observed between the two groups. 5
However, in the intention-to-treat analysis, which allowed for breaks in treatment, FDC recipients showed a significantly higher proportion of total follow-up days covered with medications (70%) compared to the single-pill combination group (42%). The primary outcome was less frequent in the FDC group (3.4 versus 3.9 events per 100 person-years). 5
Lifestyle changes in preventing and managing hypertension is extremely important. These interventions not only contribute to lowering BP but also have broader CV benefits.2
Individuals following a healthy lifestyle have 4mmHg-5mmHg lower BP, regardless of underlying genetic risks. Lifestyle changes not only lower BP but also improves the effectiveness of pharmacological interventions, potentially reducing the need for multiple therapies.2
Various lifestyle interventions have demonstrated heart-healthy benefits beyond BP reduction, with the most established approaches being weight loss, the Dietary Approaches to Stop Hypertension (DASH) diet, salt reduction, increased potassium intake, regular physical activity, and moderation of alcohol consumption. These interventions are pivotal in reducing premature CV morbidity and mortality.2
Weight reduction: Being overweight or obese is directly associated with hypertension. Weight-loss interventions, particularly through a low-caloric diet and exercise, have shown significant reductions in both systolic and diastolic BP. Modest weight loss is recommended and should be tailored to individual needs.2
Restriction of sodium intake: High sodium consumption is strongly associated with increased BP. Lifestyle interventions restricting sodium intake to <5.844 grams per day have been shown to result in an average 5/2mmHg reduction in BP. However, the debate over optimal sodium

restriction levels and potential adverse effects requires further research. 2
Augmentation of dietary potassium intake: Dietary potassium is associated with BP regulation, with evidence supporting both the effectiveness of potassium supplementation and potassium-rich diets in lowering BP. The recommended population goal for potassium intake is ~3.5 grams.2 Increase in physical activity: Habitual physical activity has an inverse relation with the incidence of hypertension. Structured exercise, especially dynamic aerobic exercise, has demonstrated BP-lowering effects, contributing to ~2-4mmHg and 5mmHg-8mmHg reductions in systolic BP for normotensive and hypertensive adults, respectively.2
Moderation of alcohol intake: Observational studies highlight a positive linear association between alcohol consumption and BP. Reduction in alcohol intake, especially close to abstinence, has been associated with a 3.3mmHg/2mmHg reduction in systolic and diastolic BP. The
hypertensiogenic effect of binge drinking should be avoided. 2
Smoking cessation: Tobacco smoking is a significant contributor to hypertension and cardiovascular risk. Smoking cessation is crucial, and health professionals should counsel and support individuals in quitting. Water pipe and e-cigarette smoking, once considered alternatives, have been associated with increased BP and CV risks.2
Other dietary interventions: Diets, such as the DASH and Mediterranean diets, have synergistic effects on BP reduction beyond individual foods or nutrients. These diets promote the consumption of fruits, vegetables, low-fat dairy, and whole grains. Coffee consumption, within moderation, appears not to adversely affect BP.2
Stress management: Stress and anxiety are linked to an increased risk of hypertension. Mind-body stress-reducing interventions, such as meditation and yoga, have shown promise in reducing both stress levels and BP.2
Exposure to noise and air pollution:
Environmental noise and air pollution contribute to increased BP and CV risks. Reduction in exposure to traffic noise and air pollution, both on a policy level and individual efforts, can contribute to better BP control and overall CV health.2
Hypertension is a global healthcare challenge, affecting >1.28 billion adults, with a significant burden in low- and middleincome countries. Often asymptomatic, it earns its ‘silent killer’ moniker, leading to severe consequences, including strokes and myocardial infarctions.
The interplay of genetic, environmental, and immunological factors underscores the complexity of hypertension. Management, primarily through antihypertensive treatment is essential, supported by robust evidence of reduced CV events and mortality. Lifestyle changes complement pharmacotherapy.
1. American Heart Association. Consequences of High Blood Pressure. 2022. [Internet]. Available at: https://www.heart.org/-/media/files/health-topics/ high-blood-pressure/consequences-of-highblood-pressure-infographic.pdf
2. Mancia G, Kreutz R, Brunström M, et al. 2023
ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension. Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). Journal of Hypertension, 2023.
3. World Health Organization. Hypertension. Updated 2023. [Internet]. Available at: https:// www.who.int/news-room/fact-sheets/detail/ hypertension
4. The Heart and Stroke Foundation South Africa. Blood Pressure. [Internet]. Available at: https://heartfoundation.co.za/bloodpressure/#:~:text=In%20South%20Africa%20 more%20than,that%20blood%20pressure%20 is%20high
5. Verma AA, Khuu W, Tadrous M, et al. Fixeddose combination antihypertensive medications, adherence, and clinical outcomes: A populationbased retrospective cohort study. PLoS Med, 2018.
6. Vemu PL, Yang E, Ebinger J. 2023 ESH Hypertension Guideline Update: Bringing Us Closer Together Across the Pond. JACC, 2024. SF

This is a summary of an online CPD article that is available on Medical Academic.
Atrial fibrillation (AFib) has been described as the cardiovascular (CV) epidemic of the 21st century, affecting millions worldwide and posing substantial risks of morbidity and mortality.
Patients with AFib have increased risks of stroke, cognitive impairment, myocardial infarction, heart failure, and other CVDs. As the prevalence of AFib continues to increase globally due to factors like an aging population and increased detection rates, effective management strategies are imperative.
The management of AFib involves a comprehensive and patient-centred approach, focusing on risk factor management, lifestyle modifications, and tailored treatment plans.
Recent guidelines emphasise the importance
of proactive risk factor management and lifestyle modifications to reduce the burden of AFib and associated complications.
Anticoagulation therapy plays a pivotal role in stroke prevention for patients with AFib. Direct oral anticoagulants (DOACs), also known as non-vitamin K antagonists, have emerged as preferred options over warfarin due to their superior efficacy and safety profiles.
DOACs, including apixaban, dabigatran, and rivaroxaban, have consistently demonstrated lower rates of stroke/systemic embolism and major bleeding compared to warfarin across various patient subgroups.
Apixaban stands out among DOACs, consistently showing favourable outcomes compared to other agents and warfarin in diverse patient populations, including the
elderly, frail, obese, and those with prior bleeding events.

Subgroup analyses from studies like ARISTOPHANES have provided valuable insights into the comparative effectiveness of DOACs in different patient populations, including the elderly, frail, obese, and those with prior bleeding events. Apixaban, in particular, has shown favourable outcomes compared to other DOACs and warfarin, making it a preferred choice in many clinical scenarios.
To access the article and quiz, go to https://www.medicalacademic.co.za/ courses/ or scan the QR code. SF




Long-term opioid use in individuals living with chronic non-cancer pain can result in opioid-induced androgen deficiency (OPIAD) by inhibiting gonadotropin-releasing hormone (GnRH) via the μ-opioid receptor. Inhibition of GnRH indirectly lowers production of testosterone. Studies show that that the prevalence of OPIAD is >50%. OPIAD can also lead to poor pain control and hyperalgesia.1,2
Clinically low testosterone levels can lead to the development of hypogonadism in men. Signs indicative of hypogonadism –defined as failure of the testis to produce physiological levels of testosterone and the normal number of spermatozoa caused by disruption of one or more levels of the hypothalamus-pituitary-gonadal (HPG) axis include:2
_ Testicular atrophy
_ Anaemia
_ Diminished facial hair growth
_ Infertility in both genders
_ Muscle wasting
_ Decreased bone density (osteopenia or osteoporosis)
_ Alterations in body composition such as increased fat mass and decreased lean body mass.
Opioid prescribing is a balancing act
Apart from the effect on the endocrine system, long-term opioid use has also been linked to the onset of metabolic syndrome, which is a major risk factor for cardiovascular (CV) disease, as well as mood disturbances, stress reactivity and aggression in men.4
Furthermore, long-term opioid use has been shown to affect the gastrointestinal tract and the respiratory control centres in the brain causing a reduction in respiratory function, emphasising the need for vigilant opioid therapy management.1,2,4
Before prescribing opioids, pain relief benefits should be weighed against potential risks. Extended-release opioids have been linked to a higher risk of androgen suppression compared to equivalent doses of immediate-release opioids. Fentanyl is associated with the highest risk, followed by methadone and oxycodone.1,3
Coluzzi et al stress that testosterone levels should be measured in all men before opioid treatment is prescribed, and opioids with a low affinity for the μ-opioid receptor should be prioritised.1
How do opioids impact testosterone levels?
As mentioned, opioids exert their effects on
the HPG axis primarily by interacting with μ-opioid receptors in the hypothalamus. This interaction inhibits the pulsatile release of GnRH from the hypothalamus, subsequently reducing the secretion of luteinizing hormone and, to a lesser extent, follicle-stimulating hormone from the pituitary gland. 5
Consequently, testosterone release from the gonads declines. Furthermore, opioids may elevate prolactin levels, leading to galactorrhoea (a milky nipple discharge) and gynaecomastia (overdevelopment or enlargement of the breast tissue). 5
In a systematic review and meta-analysis by Bawor et al, investigated the relationship between opioid use and testosterone levels, providing a comprehensive estimate of testosterone suppression. 4
The review included 17 studies, comprising seven cohort studies and 10 cross-sectional studies. Their analysis revealed a significant reduction in testosterone levels among men using opioids compared to controls, with a mean difference of 5.7nmol/l. 4
How effective is TTh in relieving pain?
The good news is that OPIAD is potentially reversible, with testosterone levels often normalising within a month after opioid withdrawal. Continuing opioids with a low impact on the HPG axis can be considered for symptomatic men with reduced testosterone levels.1
If opioid cessation is necessary, alternative non-opioid therapies should be explored for managing chronic pain. Current guidelines suggest considering testosterone therapy (TTh) if pain relief with non-opioids is inadequate or if patients cannot discontinue opioid treatment.1
Basaria et al (2015) conducted a randomised, double-blind, parallel placebo-controlled trial to assess the efficacy of TTh on pain perception and other androgen-dependent outcomes in men living with OPIAD who experience chronic non-cancer pain and have total testosterone levels <12.2mmol/l. Participants were randomly assigned to receive either daily transdermal TTh or a placebo for 14 weeks. 6
The study observed a significant improvement in pain sensitivity among participants receiving TTh, indicated by increased pressure pain threshold at the thumb and reduced punctate mechanical pain ratings. TTh also led to lower temporal summation scores for mechanical pain and showed trends towards improvements in cold pain after-sensations. 6
Furthermore, men in the TTh group experienced an increase in sexual desire and improvements in certain domains of quality of life, including role limitations secondary to emotional problems. There was also a significant reduction in fat mass and an increase in lean body mass observed in the TTh group compared to the placebo group. Importantly, the frequency of adverse events did not differ between the TTh and placebo groups, suggesting that TTh was well-tolerated. 6
The authors concluded that their findings indicate that TTh may offer benefits in alleviating pain sensitivity and improving other androgen-dependent outcomes in men living with OPIAD. 6
OPIAD is potentially reversible, with testosterone levels often normalising within a month after opioid withdrawal
Raheem et al (2017) investigated the treatment of OPIAD and its impact on opioid requirements and quality of life in patients with chronic pain. Data from men undergoing TTh were compared with a nontreatment group.7
Participants with total testosterone levels of <10.4mmol/l were identified. Follow-up total testosterone levels were significantly higher in the TTh group compared to the nonTTh group (17.2mmol/l versus 8.4mmol/l).7
Median follow-up numeric rating scale scores were significantly lower in the TTh group compared to the non-TTh group (0 versus 2). Additionally, the mean morphine equivalent dose (MED) decreased by 21mg in the TTh group, whereas it increased by 2.5mg in the non-TTh group.7
The study highlights that TTh treatment can lead to reduced opioid requirements in men living with chronic pain and the effectiveness of TTh in correcting opioidinduced endocrine abnormalities.7
Jasuja et al (2020) conducted a cohort study comparing health outcomes among long-term opioid users (n=21 272) with testosterone deficiency who were either prescribed TTh therapy (n=14 121 [66.4%]) or received other prescriptions (n=7151 [33.6%]). Primary endpoints included all-cause
mortality, major adverse CV events (MACE), vertebral or femoral fractures, and anaemia during the six-year follow-up.8
Participants who received TTh were more likely to have obesity, hyperlipidaemia, and hypertension but had a lower prevalence of coronary artery disease and stroke at baseline. 8
After adjusting for covariates, opioid users receiving TTh exhibited significantly lower all-cause mortality and incidence of MACE, femoral or hip fractures, and anaemia compared to those without TTh prescriptions.8
In covariate-adjusted models, opioid users receiving both opioids and TTh were more likely to resolve anaemia compared to those receiving opioids only. Similar findings were observed in propensity scorematched models and among opioid users living with non-cancer pain or those not receiving glucocorticoids. 8
The study suggests that long-term opioid users with testosterone deficiency who were treated with both opioid and TTh experienced significantly improved health outcomes over a multi-year follow-up. 8
Opioid use in individuals living with chronic non-cancer pain can lead to OPIAD, which contributes to poor pain control and hyperalgesia, posing significant challenges to effective pain management.
Beyond its endocrine effects, androgen deficiency is linked to metabolic syndrome, mood disturbances, and CV risk factors, further complicating the clinical picture.
Given the diverse manifestations of OPIAD, the management of chronic pain with opioids necessitates a careful balancing act, weighing the benefits of pain relief against the risks of androgen suppression.
TTh has emerged as a promising intervention for alleviating pain sensitivity and improving androgen-dependent outcomes in men with OPIAD. Clinical trials have demonstrated the efficacy of TTh in enhancing pain control, improving quality of life, and reducing opioid requirements.
Observational studies have shown that long-term opioid users with testosterone deficiency who receive TTh experience significantly overall improved health outcomes. Overall, recognising and addressing OPIAD as a consequence of the opioid epidemic is crucial for optimising pain management strategies and improving the well-being of affected individuals.
For more information on the subject, please watch this free webinar available at: https://live.arealive.org/webinars/public/ index.html#webinar&id=webinar4
References are available on request. SF


This article was independently sourced by Specialist Forum.

Allergic rhinitis (AR) is characterised by an immunoglobulin E (IgE)-mediated inflammatory response triggered by allergen exposure in sensitised individuals. This systemic immune reaction often leads to evidence of systemic atopy, such as positive skin test reactions.1
Symptoms of AR include sneezing, nasal congestion, rhinorrhoea, nasal itching, and airflow obstruction, which significantly impact quality of life, sleep, exercise tolerance, productivity, and social functioning. The condition affects both adults and children, with up to 50% of adults and 45% of children experiencing disruptions in daily life and sleep due to nasal allergy symptoms. 2
The direct medical costs of AR are substantial, highlighting the importance of effective management. AR also leads to lost work and school days, decreased productivity, and impaired school performance, with absenteeism and presenteeism affecting up to 10% and 25% of workers, respectively. 2
AR is classified as seasonal or perennial, intermittent, or persistent based on symptom duration and frequency. Treatment is tailored to symptom severity, with allergen avoidance and environmental controls as primary strategies. 3
The management of AR involves a tailored approach
The management of AR involves a tailored approach, considering the efficacy, safety of the agents selected, and patient preferences. The 2023 International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis (ICAR-AR 2023) recommends allergen avoidance, which may provide some benefit in controlling AR symptoms.4 However, pharmacologic treatments often have to be used to control AR symptoms. These treatments are available
on prescription or over-the-counter.
ICAR-AR 2023 recommends AH, CS, and their combinations, both orally and intranasally as key interventions. 4
Newer-generation oral AH have become the cornerstone of AR treatment due to their efficacy and improved side effect profile compared to first-generation agents. They are recommended as first-line therapy, offering reduction in AR symptoms with minimal adverse effects (AEs)particularly in the elderly population. 4
INAH offer rapid onset and are more effective for nasal congestion than oral agents. They are considered first- or second-line therapy for AR due to their consistent efficacy and safety profile. 4
While oral CS can attenuate AR symptoms and allergen-induced inflammation, their use is limited due to the potential for AEs, such as hypothalamicpituitary axis suppression and growth retardation, especially in paediatric populations. Therefore, their routine use is discouraged in favour of safer alternatives like intranasal (IN) CS (INCS). 4
INCS sprays are highly effective in reducing nasal and ocular symptoms of AR and are thus recommended as first-line therapy. Although they may cause local AEs like epistaxis, the benefits outweigh the risks.4
Combining oral AH with INCS has shown improved symptom control, particularly for nasal congestion. However, caution is advised, especially in patients with comorbidities, and long-term use should be avoided due to the potential for AEs. Combining INCS with INAH has demonstrated superior efficacy compared
to monotherapy or placebo, making it a recommended second-line therapy for AR. 4
Efficacy of combination azelastine/ fluticasone nasal spray
The safety and efficacy of combination azelastine/fluticasone nasal spray have been studies in various settings. Ratner et al showed that the combination improved total nasal symptom score (TNSS) by improved 37.9% and Hampel et al showed that combination azelastine/fluticasone nasal spray improved TNSS, including nasal congestion, runny nose, itchy nose, and sneezing, by 28.4%.5,6
Debbaneh et al recently conducted a systematic review and meta-analysis, revealing the superiority of combination azelastine/fluticasone nasal spray in reducing the TNSS compared to placebo (60%).7
The authors concluded that current evidence strongly supports both the efficacy and superiority of combination azelastine/fluticasone in reducing patientreported symptom scores among those living with AR. Therefore, combination nasal spray should be considered as a secondline therapy for patients whose AR is not adequately controlled with monotherapy.7
Overall, effective management of AR involves a multifaceted approach incorporating patient education, allergen avoidance, and pharmacological interventions based on symptom severity and response to treatment. Referral to specialists and consideration of allergen immunotherapy may be necessary for refractory cases.
References are available on request. SF













































































































































Scan for the quiz
This is a summary of an online CPD article that is available on Medical Academic. The link to access the article and the quiz is available at the end.
Allergic rhinitis (AR), commonly known as hay fever, affects a significant portion of the population, causing nasal and ocular symptoms upon exposure to allergens. This article explores the prevalence, risk factors, and management strategies for AR, emphasising the efficacy of fixed-dose combination (FDC) therapy. AR, triggered by allergens like pollen and dust mites, affects 10% to 40% of the population, with around 80% developing symptoms <20-years. It significantly impacts quality of life (QoL), leading to cognitive dysfunction and sleep disturbances.
Risk factors include family history, gender, and high serum IgE levels. Notably,
















breastfeeding and early pet exposure may have protective effects against AR.
AR arises from an immune-mediated reaction of the nasal mucosa to allergens, involving mast cell activation and subsequent inflammation. Clinical diagnosis involves a detailed history, examination, and laboratory tests confirming allergic sensitisation.
Local guidelines recommend intranasal corticosteroids (INCS) as first-line treatment, with fixed-dose combination therapy (INCS/INAH) considered for moderate-to-severe cases.
Combination therapy offers tailored approaches to symptom relief, with INCS effectively managing all nasal symptoms associated with AR. However, it is noted

that newer-generation oral antihistamines (AH) primarily address symptoms like pruritus and sneezing, with minimal effects on nasal congestion compared to INCS.
FDC therapy, particularly combinations of INCS and INAH, offers promising options to alleviate symptoms and improve patient outcomes. By prioritising patient needs and considering the efficacy and safety profiles of different therapies, healthcare providers can optimise AR management and enhance patients’ QoL.


















To access the article and quiz, go to https://www.medicalacademic.co.za/ courses/ or scan the QR code. SF
































































































This article was independently sourced by

The theme of this year’s World no Tobacco Day campaign (31 May) is Protecting Children from Tobacco Industry Interference. According to the World Health Organization, young people worldwide are urging governments to implement policies safeguarding them from the manipulative tactics of tobacco and associated industries. This includes curbing the incessant promotion of their hazardous products on social media and streaming platforms.
Tobacco use among young people is on the rise, with many starting during adolescence and continuing into adulthood due to nicotine addiction. Data from a Global Youth Tobacco Survey indicates an increasing trend in tobacco use among individuals aged 13- to 15-years worldwide.
Why do young people start smoking?
Several factors contribute to the initiation of tobacco use among young people. Adolescents often turn to tobacco to boost low self-esteem, manage stress, control body weight, or cope with negative emotions.
Additionally, the social acceptability of tobacco use in homes and public spaces, coupled with influence from parents, family members, and peers who smoke, contributes to its uptake among youths.
Role of tobacco advertising
Tobacco advertising and promotion play a significant role in enticing young people to start smoking. The tobacco industry strategically markets its products to potential smokers, using misleading
messages and appealing imagery to create a positive association with tobacco use. Through advertising in youth-oriented media and the design of attractive branding and packaging, tobacco companies target young people, associating smoking with vitality, sports, sophistication, friendship, independence, and beauty.
The health consequences of tobacco use among young people are severe. Smoking negatively impacts physical fitness, lung function, and respiratory health, increasing the risk of lung cancer and other diseases later in life.
Furthermore, children exposed to second-hand smoke suffer from respiratory infections, asthma, and ear infections, as they absorb more toxins due to their smaller lungs. Many young individuals are exposed to second-hand smoke at home and in public spaces, posing significant health risks.
Beyond health effects, tobacco use can have detrimental socio-economic impacts on young people. Families with adults who
smoke may allocate fewer resources to essential needs like food, healthcare, clothing, and education, compromising the well-being and future prospects of their children.
Additionally, many youths from lowincome families are employed in the tobacco industry, exposing them to health risks associated with nicotine poisoning and exposure to harmful agrochemicals, thus impeding their rights to health, education, and social development.
The increasing trend of tobacco use among young people is alarming, with many starting during adolescence and continuing into adulthood due to nicotine addiction. Factors like low self-esteem, stress management, and social acceptability contribute to tobacco initiation.
Tobacco advertising plays a significant role in enticing young people to start smoking, using misleading messages and attractive imagery. Addressing this issue requires strict regulation of tobacco advertising and promotion, along with measures to protect children from secondhand smoke. SF

Hand hygiene is a fundamental pillar of effective infection prevention and control (IPC) programmes, playing a pivotal role in reducing the transmission of pathogenic microorganisms within healthcare settings and thereby decreasing the incidence of healthcare-associated infections (HCAIs).1
According to the World Health Organization (WHO), initiatives aimed at improving hand hygiene can prevent up to 50% of avoidable infections acquired during healthcare delivery and yield economic savings about 16 times the cost of implementation.2
High-risk patients, especially those treated in intensive care units (ICUs), are at high risk of HCAIs. In these settings,
infection prevalence rates range from 9.7% to 31.8% in Europe and 9% to 37% in the United States, with mortality rates ranging from 12% to 80%. In Africa, the prevalence of HCAIs is 12.76%, with varying rates across different wards, including ICUs, neonatal ICUs/ wards, and paediatric medical wards. 2,3
Surgical site infections
(SSIs) constitute the most common type of HCAIs (41.6%), followed by bloodstream infections and respiratory tract infections/ pneumonia. 3 Despite the proven effectiveness of hand hygiene in preventing HCAIs, global implementation remains substandard.
The WHO’s Multimodal Hand Hygiene Improvement Strategy, launched in 2009, aimed to address this issue. However, a 10-year study assessing global implementation levels revealed that >25% of healthcare facilities, primarily in low-income nations, reported basic or inadequate levels of hand hygiene implementation.1
Resource availability significantly influences hand hygiene implementation levels, with lower scores observed in lowincome and public healthcare facilities compared to high-income and private ones. Investment in IPC measures, including hand hygiene, is crucial to enhancing patient safety and mitigating the financial burdens associated with HCAIs.1
Healthcare-associated pathogens are not confined to infected wounds but also inhabit intact patient skin and environmental surfaces, contributing to cross-contamination. 2
Healthcare workers’ hands become contaminated during patient care activities,
with gloves offering limited protection. Hand hygiene is essential in mitigating the spread of pathogens. 2
Various hand hygiene options are available including plain soap, alcohol-based hand rubs, chlorhexidine, chloroxylenol, iodine, quaternary ammonium compounds, and triclosan. 2 Alcohol-based hand rubs are recommended by the WHO due to their evidence-based effectiveness, suitability for resource-limited areas, promotion of adherence, economic benefits, and safety. 2
Effective surgical hand preparation is crucial in reducing the risk of SSIs. Modern protocols involve shorter preparation durations and the use of antiseptic agents like chlorhexidine and povidone-iodine. Alcohol-based hand rubs are recommended for surgical hand preparation due to their broad-spectrum antimicrobial activity and convenience. 2
Hand hygiene significantly reduces the transmission of pathogenic microorganisms within healthcare settings and ultimately saving millions of lives annually. Effective implementation of hand hygiene programmes is essential to improve patient safety and mitigate the financial burdens associated with HCAIs.
References are available on request. SF

Healthcare workers (HCWs) have an increased risk of developing occupational contact dermatitis (OCD) due to frequent hand washing with soaps and disinfectants, as well as the use of personal protective equipment (PPE), such as gloves, masks, goggles, and other protective equipment. OCD is described as a skin inflammation caused by exposure to external irritants or allergens. It can present as allergic contact dermatitis (ACD) or irritant contact dermatitis (ICD). OCD has a significantly impact on quality of life, and work productivity.1,2,3
ACD involves an adaptive immune response to chemicals penetrating the skin, triggering a non-specific immune response, while ICD is a non-specific skin reaction to irritants and is more common (44%) in the healthcare setting.1,2
Skin reactions in the healthcare setting
ICD results from repeated exposure
to hand hygiene products, leading to symptoms like dryness, irritation, itching, and even cracking and bleeding. The pathophysiology involves damage to the skin’s protective barrier, particularly lipid depletion, which increases susceptibility to irritation. While alcohol-based hand rubs are generally well-tolerated, they can still cause dryness and irritation, albeit to a lesser extent than detergents. 4
In ACD, fragrances, preservatives, and
emulsifiers are common culprits, and symptoms can range from mild localised reactions to severe generalised ones, including anaphylaxis in extreme cases. While allergic reactions to alcohol-based hand rubs are rare, they can occur, usually due to compounds present as inactive ingredients rather than the alcohol itself. 4
How do HCWs view hand hygiene?
Observational studies reveal wide
variations in hand hygiene frequency, ranging from five to 42 times per shift and 1.7 to 15.2 times per hour. Opportunities for hand hygiene also vary by hospital ward, with nurses in paediatric wards having fewer opportunities compared to those in intensive care units (ICUs). 4
In some acute settings, as many as 82 hand hygiene opportunities per patient per hour have been observed. However, despite high opportunities, adherence to hand hygiene practices remain variable. 4
Observed adherence rates to recommended hand hygiene procedures range from 5% to 89%, with an average of 38.7%. Improvements in adherence have been reported following interventions, but sustained improvements are rare. 4
Factors influencing adherence include professional category, hospital ward, time of day/week, and type and intensity of patient care. Nurses generally exhibit higher adherence compared to doctors or nursing assistants, with adherence being lowest during weekends and in ICUs where hand hygiene opportunities are more frequent. 4
Perceived barriers to adherence include skin irritation, inaccessible hand hygiene supplies, interference with HCW-patient relationships, patient needs perceived as a priority over hand hygiene, glove usage, forgetfulness, lack of knowledge of guidelines, high workload, and understaffing. Some HCWs believe they only have to wash their hands, when necessary, despite evidence suggesting otherwise. 4
A study showed that frequent use of hand hygiene products (100%) was the number one cause of ICD in HCWs followed by
infrequent hand moisturising (>50%). 5
The study also showed that all participants had an improvement rate of 70%-90% from their baseline signs and symptoms, with a mean improvement of 80% following procurement of a gentler hand hygiene product (consisting of 70% ethanol, emollients, and moisturiser) by the healthcare facility, regular use of a topical steroid cream or moisturiser, and adjustment to their clinical duties, which resulted in a temporary reduction in hand hygiene activities. 5
Alcohol-based rubs with humectants tend to be better tolerated than plain or antimicrobial soaps. Furthermore, certain practices, such as washing hands with soap and water immediately before or after using alcohol-based rubs, should be avoided to prevent skin irritation. 4
Selecting hand hygiene products involves assessing multiple factors to ensure efficacy, acceptability, and costeffectiveness. Pilot testing, considering local factors and HCWs’ preferences, is essential, with a focus on product efficacy, dermal tolerance, aesthetic preferences, practical considerations, and cost. 4
When selecting hand hygiene products, several factors need consideration to ensure their efficacy, acceptability, and cost-effectiveness. Pilot testing is recommended to assess the acceptability of products among healthcare workers (HCWs), involving them in the selection process to increase hand hygiene adherence. 4
Characteristics such as fragrance, consistency, and colour can influence HCWs’ adherence, and structured

questionnaires should be used to evaluate their preferences. Pilot testing should be conducted considering local factors like climate and sociocultural backgrounds, and products should be compared with those already in use. 4
Factors influencing product selection include relative efficacy, dermal tolerance, cost, aesthetic preferences, and practical considerations. Efficacy of antiseptic agents, dermal tolerance, and skin reactions should be evaluated using standardised methods, with products tested by several users over a period of weeks. Products should be at least as good as existing ones to prevent a decrease in hand hygiene adherence. 4
Aesthetic preferences, such as fragrance and consistency, are important considerations. Fragrance should be mild or absent to avoid discomfort or allergic reactions among HCWs and patients. Consistency, whether gel, solution, or foam, affects user experience, but it does not significantly impact efficacy or tolerance. 4
Practical considerations include product accessibility and risk of contamination. Accessibility of hand hygiene facilities influences frequency of use, and a reliable supplier is essential for continuous product availability. Products should have a low risk of contamination, especially for soap, to maintain hygiene standards. 4
Cost is another crucial factor, although the level of HCWs’ acceptance is prioritised over price. While hand hygiene promotion is cost-effective, inexpensive products with undesirable characteristics may discourage adherence. 4
Basic therapy for the prevention of ICD involves basic therapy with skin care products aimed at restoring the skin barrier, reducing inflammation and itching, and sparing the use of glucocorticoids. 6
Experimental studies have shown that basic skin care therapy can promote healing of both ICD and ACD without requiring additional specific treatments. The choice of skin care product should be tailored to the stage of the condition, with hydrophilic preparations like gels, lotions, or creams suitable for acute dermatitis, while water-in-oil-based preparations like ointments are more appropriate for chronic stages. 6
It is crucial to select skin care products with appropriate water and lipid content and without allergenic ingredients to avoid delaying healing. 6
References are available on request.

This article was independently sourced by Specialist Forum.
Did you know that globally, patients living with chronic kidney disease (CKD) surpass twice the population of those affected by diabetes and exceed over twenty-fold the number affected by human immunodeficiency virus/acquired immune deficiency syndrome?1
The prevalence of CKD in Africa is estimated to be around ~4.2% (~50 million), compared to the global prevalence of ~9.5% (~760 million). This is according to a new report published by the International Society of Nephrology and the Global Kidney Health Atlas.2
The prevalence of CKD in South Africa ranges from 6.4% to 8.7%. This means that between 3.8 million and four million South Africans have CKD. Women (12.1%) have a higher risk of CKD compared to men (8.1%).1
The number of disability-adjusted life years (DALYs) attributable to CKD is 491.4 per 100 000 population. The median proportion of deaths attributable to CKD is 2.4%.2
The report, published in the March issue of the Lancet, also assessed the availability, accessibility, quality, and affordability of medicines, kidney replacement therapy (KRT), and conservative kidney management (CKM, defined as planned, holistic, patient-centred care that did not include KRT for people living with stage 5 CKD [see Table 1]).2
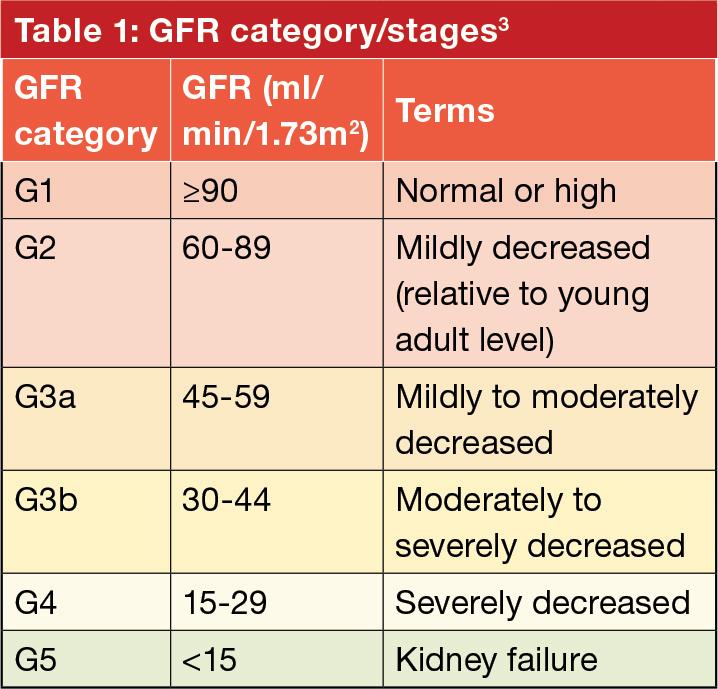
Kidney Disease: Improving Global Outcomes (KDIGO) defines CKD as abnormalities of kidney structure or function, present for >3 months, with implications for health and CKD is classified based on cause, glomerular filtration rate (GFR) category (see Table 1), and albuminuria category (see Table 2).3
Risk factors for CKD include diabetes, hypertension, obesity, smoking, and a familial predisposition to kidney disease. Hypertension and diabetes are the main causes of CKD:2,4
_ Type 2 diabetes: 30% to 50%
_ Type 1 diabetes: 3.9%

_ Hypertension: (27.2%). Furthermore, factors such as obesity and smoking have also been linked to an increased risk of developing CKD.2
Availability, accessibility, quality, and affordability
The report alluded to above, revealed significant variations in health spending, workforce, and infrastructure. The median total health spending for CKD treatment was R6700 ($353) per capita, with a median government health spending of R4081 ($216) per capita and a median out-ofpocket health spending of R1738 ($92) per capita. Health spending increased with country income level. 2
For in-centre haemodialysis, the annual median cost ranged from R32 000 ($1646) in Burkina Faso to R1.9m ($103 443) in Costa Rica. Similarly, peritoneal dialysis (median R358 213 [$18 959]) and kidney transplantation (median R508 307 [$26 903]) costs also demonstrated considerable variation. 2
The health workforce varied widely, with overall densities per 1000 population of 36.2 nurses, 17.7 medical doctors, and 1.9 specialist physicians. Regional and incomelevel disparities were evident. 2
Regarding KRT delivery, there was significant variability in capacity across countries. Home haemodialysis services were provided in high-income countries (HICs), and the availability of services like peritoneal dialysis and kidney transplantation varied across regions. 2
Dialysis accessibility for those with kidney failure showed disparities by country income level, with HICs having higher accessibility rates. CKM was available in
53% of countries, mostly in HICs. 2
Infrastructure for patient support and shared decision-making was present in >50% of countries. Essential medicines for pain and palliative care were available in 59% of countries, with disparities in infrastructure across regions. 2
Public funding for chronic haemodialysis varied, with 45% of countries providing free services at the point of delivery. Payment methods for KRT varied, with private and out-of-pocket payments reported in some countries, particularly in Africa. 2
The nephrology workforce demonstrated significant variations globally, with a median prevalence of 11.8 nephrologists per million population. Shortages of nephrologists, paediatric nephrologists, transplant surgeons, dietitians, and dialysis nurses were reported, particularly in low- and middle-income countries. 2
Registries for CKD, dialysis, kidney transplantation, and CKM varied in availability. CKD detection programmes were implemented reactively in many countries, limiting proactive management. 2 Leadership and governance structures for CKD management were present in 63% of countries. Only 25% had national CKD-specific strategies, and less than half recognised CKD as a health priority. 2
Comparing data from 2019 to 2023 indicated increases in the density of haemodialysis and peritoneal dialysis centres, kidney transplantation centres, and nephrologist prevalence. Changes in public funding and free services for KRT and essential medications were also noted. 2
According to the authors of the report, the data underscores the complex landscape of CKD treatment, highlighting


the need for targeted interventions and resource allocation to address disparities and improve global kidney care. 2
The latest update (2020) KGIDO guideline stresses the importance of optimising patient care and treatment outcomes. To achieve these goals, the organisation recommends:5
_ Initiating treatment with angiotensinconverting enzyme inhibitors (ACEi) or angiotensin II receptor blockers (ARB) in patients living with diabetes, hypertension, and albuminuria. The medications should be titrated to the highest approved dose tolerated. For patients with diabetes, albuminuria, and normal blood pressure (BP), consideration of ACEi or ARB is warranted.
_ KDIGO recommends the following ACEis: Benazepril, captopril, enalapril, fosinopril, lisinopril, perindopril, quinapril, ramipril, trandolapril. The organisation recommends the following ARBs: Azilsartan, candesartan, irbesartan, losartan, olmesartan, telmisartan, valsartan.
_ Continuous monitoring of BP, serum creatinine, and serum potassium within two to four weeks of initiation or dose increase is emphasised. ACEi or ARB therapy should be continued unless serum creatinine rises by more than 30% within four weeks. Contraception advice is recommended for women on ACEi or ARB therapy, with discontinuation advised for those considering pregnancy.
_ Hyperkalaemia associated with ACEi, or ARB use can often be managed by measures to reduce serum potassium levels, avoiding immediate discontinuation or dose reduction. However, in the presence of symptomatic hypotension or uncontrolled hyperkalaemia despite medical intervention, dose reduction or discontinuation is warranted.
_ The combination of ACEi with ARB or with a direct renin inhibitor is considered potentially harmful, using only one agent at a time to block the renin-angiotensinaldosterone system.
_ While effective for managing refractory hypertension, mineralocorticoid receptor antagonists may cause hyperkalaemia or a reversible decline in glomerular filtration, particularly in patients with a low estimated GFR.
_ Monitoring glycaemic control through HbA1c is recommended, with twice-yearly measurements for long-term control. In cases of advanced CKD, a glucose management indicator derived from continuous glucose monitoring (CGM) data may be considered due to reduced
reliability of HbA1c measurements. _ An individualised HbA1c target can be considered, ranging from <6.5% to <8.0%, is recommended for patients with diabetes and CKD not on dialysis. The achievement of lower targets may be facilitated by CGM, and alternative metrics such as time in range and time in hypoglycaemia.
As noted above, T2DM is the main driver of CKD. Effectively managing T2DM in patients living with CKD requires a multi-faceted approach that includes lifestyle changes and pharmacotherapy with metformin, sodium–glucose cotransporter-2 inhibitors (SGLT2i), glucagon-like peptide-1 receptor agonists (GLP-1RA), and additional medications (insulin, sulfonylureas, meglitinides) as needed for glycaemic control, according to the KDIGO guidelines. 5 KDIGO recommends initiating treatment with metformin for most patients with T2DM, CKD, and an estimated GFR ≥30ml/min/1.73m². Kidney transplant recipients living with T2DM and an estimated GFR >30ml/min/1.73 m² should also be treated with metformin, with careful monitoring and dose adjustments based on estimated GFR levels. Long-term use requires monitoring for vitamin B12 deficiency.5
For patients with T2DM, CKD, and an estimated GFR >30ml/min/1.73 m², KDIGO recommends SGLT2i as a first-line treatment, which provides benefits beyond glycaemic control (eg cardiovascular [CV] protection).5
The choice of SGLT2i should consider documented kidney or CV benefits and estimated GFR levels. KDIGO suggests cautious consideration for patients at risk of hypovolemia and emphasises continuing SGLT2i therapy even if estimated GFR falls <30 ml/min/1.73 m², unless not tolerated or kidney replacement therapy is initiated.5
For patients with T2DM and CKD who have not achieved individualised glycaemic targets with metformin and SGLT2i or cannot use those medications, KDIGO recommends long-acting GLP-1RA as an additional treatment. Prioritising agents with documented CV benefits is advised.5
To minimise gastrointestinal side effects, a low starting dose is recommended, and titration should be gradual. When GLP-1 RA is used concomitantly with other medications such as sulfonylureas or insulin, the doses of sulfonylurea and/or insulin may need to be reduced. GLP-1RA should not be used in combination with dipeptidyl peptidase-4 inhibitors. 5
KDIGO recommends a personalised dietary approach. The diet should be rich
in vegetables, fruits, whole grains, fibre, legumes, plant-based proteins, unsaturated fats, and nuts. Conversely, it should be limited in processed meats, refined carbohydrates, and sweetened beverages. 5
Specifically for patients undergoing haemodialysis, and especially those on peritoneal dialysis, a protein intake between 1-1.2 grams/kg of body weight per day is suggested. Furthermore, KDIGO recommends keeping sodium intake <2 grams of sodium/day (equivalent to <90mmol of sodium per day, or <5 grams of sodium chloride per day [salt]) for patients living with diabetes and CKD. 5
Physical activity is considered an essential component of managing diabetes and CKD. Patients living with diabetes and CKD should be encouraged to engage in moderateintensity physical activity for a cumulative duration of at least 150 minutes per week. However, the level of physical activity should be tailored to each patient’s CV and physical tolerance. Smokers should be encouraged to quit. 5 Patients living with obesity, diabetes, and CKD, should be encouraged to lose weight. This recommendation is particularly relevant for patients with an estimated GFR ≥30ml/min/1.73 m². 5
These lifestyle interventions aim to optimise the overall health and well-being of patients living with diabetes and CKD. However, it is important for healthcare providers to individualise recommendations based on the patient’s specific health status, preferences, and any other relevant medical considerations. Regular monitoring and adjustments to the treatment plan may be necessary to achieve and maintain positive health outcomes. 5
The alarming prevalence of chronic kidney disease (CKD) in Africa, affecting >2.5 million South Africans, emphasises the urgent need for comprehensive and equitable healthcare interventions. The disparities in health spending, workforce, and infrastructure revealed in the Global Kidney Health Atlas report highlights the complex landscape of CKD treatment.
While improvements in haemodialysis centres, transplantation facilities, and nephrologist prevalence have been noted, challenges persist, especially in low- and middle-income countries.
The KDIGO guidelines recommend personalised approaches, advocating for optimised patient care, the crucial role of lifestyle modifications, pharmacotherapy, and targeted interventions in improving global kidney care.
References are available on request. SF
This article was independently sourced by Specialist Forum.
Anhedonia, defined as a noticeable diminished interest or pleasure in all, or almost all, activities, is one of the key features of major depressive disorder (MDD). Anhedonia is considered a major suicide risk factor. Up to 70% of patients living with MDD experience anhedonia.1

Anhedonia is also common in patients living with other psychiatric disorders.1,2
According to Serretti, the definition of anhedonia include a broad spectrum of deficits in reward processing such as interest, motivation, effort expenditure, valuation, reward anticipation, learning, pleasure, and satiation.1
Anhedonia can be subcategorised as:1
_ State anhedonia: Can manifest as a reduced capacity to find pleasure –individuals may cease to enjoy activities that were once pleasurable, particularly evident during acute MDD episodes.
_ Trait anhedonia: Some patients may exhibit a persistent and general impairment in experiencing pleasure, irrespective of temporal considerations. This trait may be associated with conditions like dysthymia or substance abuse.
_ Social anhedonia: Defined as getting little or no pleasure from interpersonal situations.
_ Physical anhedonia: Defined as getting little or no pleasure from non-social physical sensations like smell, taste, touch, or sound.
The disease course of anhedonia is not stable and may change, depending on the phase of the disorder and may decrease or disappear completely after recovery.1
Anhedonia and suicide risk
Suicide is a growing public health crisis, contributing to >700 000 deaths globally. Suicide is currently the second leading cause of mortality among individuals aged 15- to 24-years. A meta-analysis conducted by Gillissie et al shows a substantial and moderate correlation between anhedonia and suicidality in both general and psychiatric populations (9.61% and 10.24%, respectively).2
The neurophysiological and genetic basis of MDD and anhedonia
Multiple factors contribute to MDD. It has been linked to a combination of genetic, environmental, biological, and physiological
factors. The neurophysiological basis of anhedonia has been investigated in numerous studies.1
These studies found that the prefrontal cortex, which include the ventromedial and dorsolateral regions, plays a crucial role in reward processing and decisionmaking. A key mechanism underlying anhedonia involves striatal hypoactivation for anticipatory anhedonia (an inability to predict the future experience of pleasure as well as lower motivation to act toward achieving pleasure) and prefrontal areas for consummatory anhedonia (a lack of pleasure when participating in an activity that others would consider gratifying).1
Various brain regions, including the nucleus accumbens, striatum, ventral pallidum, ventral tegmental area, amygdala, insula, anterior cingulate cortex, orbitofrontal cortex, and prefrontal cortex, have been implicated in studies, highlighting the multifaceted nature of reward deficits.1
Dopamine has been extensively studied as the neurotransmitter most associated with anhedonia, with clinical support for its role in regulating anticipation, motivation, effort, and learning. Furthermore, other neurotransmitters such as serotonin (5HT), epinephrine, opioids, glutamate, gamma-aminobutyric acid (GAMA), and acetylcholine may modulate consummatory pleasure and motivation.1
A genome-wide analysis identified 11 loci explaining 5.6% of anhedonia, with polygenic risk scores showing promise in predicting an individual’s risk for developing the condition based on their genetic makeup.1
These scores were associated with structural brain changes, linking genetic risk to brain white matter integrity and volumes of regions involved in reward and pleasure processing.1
Epigenetic modifications, chemical changes to DNA influencing gene expression without altering the sequence, have also been explored in relation to anhedonia. Reports suggest that epigenetic modifications to genes involved in reward processing and mood regulation are associated with anhedonia.1
Guidelines for the treatment of MDD recommend the following interventions based on the severity of the disorder:3
_ Initiate monotherapy with either cognitive behavioural therapy (CBT) or a second-generation antidepressant as the primary treatment for patients in the acute phase of moderate to severe MDD.
_ Consider combination therapy with CBT and a second-generation antidepressant as an alternative initial treatment for patients in the acute phase of moderate to severe MDD.
_ The decision between monotherapy and combination therapy should be individualised, considering factors such as potential treatment benefits, adverse effects, cost, feasibility, specific symptoms (eg insomnia, hypersomnia, appetite fluctuations), comorbidities, concomitant medication use, and patient preferences.
_ Consider monotherapy with cognitivebehavioural therapy as the initial treatment for patients in the acute phase of mild MDD.
_ For patients in the acute phase of moderate to severe MDD who do not respond to initial treatment with an adequate dose of a second-generation antidepressant, consider the following options:
• Switching to or augmenting with CBT
• Switching to a different secondgeneration antidepressant or augmenting with a second pharmacologic treatment.
Anhedonia, a prominent feature of MDD, poses a substantial suicide risk, affecting up to 70% of patients. The multifaceted nature of anhedonia includes anticipatory and consummatory components, with various subcategories like state, trait, social, and physical anhedonia. Anhedonia correlates significantly with suicidality, emphasising its role as a fundamental risk factor. The treatment landscape for MDD involves various interventions, with secondgeneration antidepressants. References are available on request. SF













































































































































