The doctor's newspaper
SEPTEMBER 2024
The ethical tightrope of AI in healthcare
As AI continues to revolutionise healthcare, it brings with it a host of ethical challenges. From the opacity of AI decision-making to the risks of automation bias and inherited biases, the ethical landscape is complex and multifaceted.
RTIFICIAL INTELLIGENCE
(AI) is revolutionising various sectors, including healthcare. While AI offers numerous benefits, it also raises significant ethical concerns. Key ethical dilemmas in modern research due to the rapid developments of AI and big data were the focus of debate when the Wits Research Integrity Office along with SARIMA Community of Practice in Research Ethics and Integrity and Carnegie hosted its annual Ethics Colloquium last month.
Bioethicist and director of the Steve Biko Centre for Bioethics at Wits, Prof Kevin Behrens drilled down on generative AI in research and the need for transparency, caution, and regulation.

THE OPACITY PROBLEM
One of the most pressing ethical issues is the opacity of AI systems.
Prof Behrens explained that unlike

conventional programming, where the code and its functions are transparent, generative AI operates semi-autonomously, making its processes fundamentally unexplainable. This ‘black box problem’ means that even data scientists cannot fully explain how AI arrives at its outputs. This lack of transparency is particularly concerning in healthcare, where AI is used to make critical decisions about medical treatments.
“If AI is used to make critical decisions that could impact people’s lives and wellbeing like medical diagnosis or treatment, do these people have a right to know AI was used?” asked Prof Behrens. “Do they have a right of refusal?” But furthermore, would they even want to know, and is it even possible to meet the requirements of ‘full disclosure’ and ‘comprehension’ for informed consent?
Prof Behrens stressed that transparency was paramount and that whenever AI is used it should be fully disclosed. “The opacity problem and our inability to accurately assess risks should also be disclosed.”
Generative AI often gets things wrong, a phenomenon sometimes referred to as "AI stupidity." AI systems do not inherently know when their outputs are correct or incorrect. They mimic human language and behaviour patterns, sometimes inventing answers when they cannot find the right one. This unreliability is especially dangerous in healthcare, where a wrong diagnosis or treatment could lead to serious harm or even death. Prof Behrens explained that the issue is exacerbated by ‘automation bias’, where people tend to trust AI outputs over human judgment.
Prof Behrens gave the following example: “According to Bernstein et al. (Eur Radiol, 2023), in using AI to interpret X-rays, AI generates false positives in 11% of cases and false negatives in 13%. However, because of automation bias, AI results can cause radiologists to make incorrect decisions when they would have otherwise been correct. Without AI false negatives were 2.7%, but
was no abnormality, false negatives increased to 20.7-33%, depending on the AI results condition.” This again highlighted the need for the use of AI in any aspect of research to be disclosed.
MODEL COLLAPSE OR MODEL AUTOPHAGY DISORDER (MAD)
Another ethical concern is ‘Model Collapse’ or Model Autophagy Disorder (MAD). This occurs when AI models are trained on AIgenerated text, leading to a degradation in the quality of the model's outputs. In healthcare, this could mean that AI tools become less reliable over time, potentially compromising patient care. The study published in Nature on 24 July 2024, highlighted that as AIgenerated information polluted the training set, the model's outputs became gibberish, demonstrating the risks of relying too heavily on AI-generated data.
As such, Prof Behrens highlighted the need to be aware that AI can get worse at
Epigenetics in dermatology



tasks, that output quality isn’t uniform or predictable, and that
methods are not repeatable.
AI BIAS
AI systems inherit many of our human biases, which can have serious implications in healthcare. For example, face recognition software used for surveillance and criminal identification has been shown to generate more false positives and negatives for black faces than white. Prof Behrens warned that this bias extends to healthcare, where AI tools trained on biased data can perpetuate historical and social inequities. For instance, AI-based recruitment tools have been shown to favour male candidates, reflecting past patterns of gender bias. In healthcare research, such biases can impact findings and lead to unequal treatment of patients. Prof Behrens stressed the need for vigilance and mitigation.
AI RISK AND LIABILITY
The use of AI in healthcare also raises questions about data security, copyright, and liability. Current AI tools cannot guarantee the security of personal or proprietary data, making their use
a potential violation of data protection laws like the POPI Act. Additionally, if AI tools lead to harm or even death, it is unclear who would be liable – the researcher or the AI tool supplier. This legal uncertainty makes it difficult to obtain proper informed consent and exposes researchers to litigation risks.
REGULATION
Prof Behrens said there is an urgent need for international and state legislation to regulate AI in healthcare. This includes preventing copyright violations, rogue development, and misuse for harmful purposes. Legal clarity on liability is essential, and research regulators need to develop appropriate guidelines and standards. Voluntary disclosure of AI use in research could be a mitigating factor, but formal regulation is necessary to ensure ethical practices.
The ethical implications of AI in healthcare are complex and multifaceted. Transparency, caution, and regulation are crucial to addressing these concerns. As AI continues to evolve, it is imperative that healthcare professionals remain vigilant and proactive in mitigating the risks associated with its use.
EAR DEVOTED READERS, Welcome to our October issue. of Medical Chronicle. This month, we dive into a range of pressing health topics that are shaping the landscape of healthcare in South Africa and beyond.
Artificial intelligence (AI) in healthcare is a critical topic covered in this issue. We explore the ethical implications of AI, including decision-making transparency and automation bias, and stress the need for robust regulations to ensure patient safety and data security. Public health challenges are also at the forefront, with a detailed report on the recent mpox outbreak in South Africa. The article underscores the urgency of effective public health strategies and vaccination efforts to combat this outbreak.
The Health Quality Assessment 2024 report provides valuable insights into chronic disease prevalence, improvements in preventive care, and the ongoing challenges in mental health and drug shortages. The report advocates for the integration of AI in pharmaceutical supply chains to address these issues.
Cervical cancer prevention is another significant focus, particularly in low- and middle-income countries. We discuss the WHO targets for HPV vaccination and screening, highlighting the importance of early detection and prevention in a CPD-accredited article.
We also cover benign prostatic hyperplasia (BPH), chronic stable angina, and the benefits of traditional African diets. This article provides valuable insights into managing these conditions and improving overall health. The third CPD-accredited article is on the topic of innovative approaches to managing chronic
Don’t miss our feature on the role of epigenetics in dermatology. At the recent Combined Dermatology Congress of South Africa, held in Gqeberha, Dr Hassan Galadari, Associate Professor of Dermatology at the United Arab Emirates University, presented a compelling session on epigenetics. This article is based on his presentation.
Happy reading























SA is grappling with a significant Mpox outbreak, with 24 confirmed cases and three deaths reported across Gauteng, KwaZulu-Natal, and Western Cape provinces.
A Mpox in SA: high fatality rate and community transmission raise alarms
EPCLUSA® is indicated for the treatment of chronic hepatitis C infection irrespective of genotype in treatment naïve or treatment experienced patients aged 12 years and older and weighing at least 30 kg:
- without cirrhosis or with compensated cirrhosis
- with decompensated cirrhosis in combination with ribavirin 1

Footnotes: aDespite unknowns in baseline characteristics of some patients, such as: HCV genotype, fibrosis stage, former/current IV drug use, PPI use at baseline and treatment history.3 bA large-cohort international real-world study showed that patients with unknown genotype (n = 42), unknown fibrosis score (n = 82) and unknown treatment history (n = 33) were cured with EPCLUSA® for 12 weeks. Cure is defined as SVR i.e., undetectable HCV RNA after treatment completion.3,4 cCases of HBV reactivation, some of them fatal, have been reported during or after treatment with direct acting antiviral agents including EPCLUSA®. HBV screening should be performed in all patients before initiation of treatment. Treatment with EPCLUSA® should not be initiated in patients who screened positive for hepatitis B virus infection. HBV/HCV coinfected patients are at risk of HBV reactivation, and should therefore be monitored and managed according to current clinical guidelines. dPatients with decompensated cirrhosis use EPCLUSA® + ribavirin for 12 weeks.1
References: 1. Epclusa Professional Information approved by the medicine’s regulatory authority. 10 March 2022. 2. Lawitz E, Bourliere M, Han L, McNally J, Stamm LM, Brainard DM, et al. Treatment with SOF/VEL or SOF/VEL/VOX is well tolerated and results in high SVR12 in genotype 1-6 HCV-infected patients with minimal fibrosis: a retrospective analysis of the ASTRAL and POLARIS clinical studies. Poster THU-273 presented at the International Liver Congress 2017, April 19–21, Amsterdam, The Netherlands. Available at: https://www.natap.org/2017/EASL/EASL_07.htm [Accessed 24 March 2022]. 3. Mangia A, Milligan S, Khalili M, Fagiuoli S, Shafran SD, Carrat F, et al. Global real-world evidence of sofosbuvir/velpatasvir as simple, effective HCV treatment: Analysis of 5552 patients from 12 cohorts. Liver Int 2020;40:1841–1852. 4. National Guidelines for the Management of Viral Hepatitis. Department of Health Republic of South Africa Available at: https://sahivsoc.org/Files/SA%20 NDOH_Viral%20Hepatitis%20guideilnes%20final_.pdf [Accessed 10 March 2022]. For full prescribing information refer to the professional information approved by the Medicines Regulatory Authority. S4 EPCLUSA® 400 mg/100 mg film-coated tablets. Reg. No.: 51/20.2.8/0872. Each film-coated
gilead.com or drugsafetysouthafrica@gilead.com EPCLUSA® the EPCLUSA® Logo, GILEAD and the GILEAD Logo are trademarks of Gilead
FFECTING 13 AFRICAN COUNTRIES since the beginning of the year, Deputy Minister of Health, Joe Phaahla announced the first two deaths from mpox in SA in June.
By the end of August, the National Institute for Communicable Diseases (NICD) reported that 24 cases had been confirmed in SA with three deaths.
The cases were reported across three of the nine provinces: Gauteng (12 cases; 1 death), KwaZulu-Natal (11 cases; 2 deaths), and Western Cape (1 case).
AFFECTED DEMOGRAPHICS
The individuals affected are men aged between 17 and 43 years old. Of the first 16 cases, 11 self-identified as men who have sex with men (MSM). At least 15 cases are living with HIV with unmanaged or only recently diagnosed HIV infection and have advanced HIV disease (AHD), and one case has diabetes. The type of exposure contact reported by cases is sexual contact. Eighteen of the patients required hospitalisation, indicating the severity of the cases.
TRANSMISSION AND RISK
The sudden appearance of these cases, none of whom reported any history of international travel, suggests that confirmed cases are only a small proportion of all cases that might have occurred, indicating ongoing community transmission. The risk to human health for the general public remains low in the country. However, the risk for gay men, bisexual men, other men who have sex with men, trans and gender-diverse people, and sex workers is moderate.
According to the NICD: “The rise in cases and deaths, particularly among children, is linked to the discontinuation of the smallpox vaccine and high malnutrition rates in affected regions.”
PUBLIC HEALTH EMERGENCY
The Africa Centres for Disease Control and Prevention (Africa CDC) declared the ongoing mpox outbreak a Public Health Emergency of Continental Security (PHECS) on 13 August 2024, marking the first such declaration by the agency. This empowers Africa CDC to lead and coordinate health emergency responses across the continent, including mobilising resources, enhancing surveillance, and strengthening health systems.

With the demand for diagnostic tests on the rise, the World Health Organization (WHO) has asked manufacturers of mpox in vitro diagnostics (IVDs) to submit an expression of interest for Emergency Use Listing (EUL). Testing is key for people to get treatment and care as early as possible and prevent further spread of the disease and ensuring better health outcomes.
RESPONSE MEASURES
Several response measures have been put in place by national health authorities with the support of WHO. These include heightened surveillance, public health messaging, and efforts to secure mpox vaccines.
VACCINATION EFFORTS
SA began the process to approve and order vaccines in May when the cases were first discovered. The US committed to providing enough doses to vaccinate 25 000 people in the DRC, and Japan has also pledged vaccines. However, as of the latest updates, the deployment of these vaccines in affected areas has faced challenges.
Offer Neuroprotection1
The rise in cases and deaths,particularly amongchildren, is linked to the discontinuation ofthesmallpox vaccineandhigh malnutrition rates in affectedregions
PUBLIC HEALTH CONCERNS
The outbreak emphasises that the global mpox outbreak linked to clade IIb monkeypox virus (MPXV) is still ongoing, and the risk of cross-border and international spread persists in all WHO regions. This outbreak is particularly concerning due to the high case fatality ratio, the vulnerability of affected populations, and the challenges in vaccine deployment and public health response. The situation underscores the need for continued vigilance, effective public health strategies, and international cooperation to manage and contain mpox outbreaks.
multivitamin and mineral supplement containing a neuroprotective agent, Citicoline ( ) and other nutrients that contribute to:1

Despitethe availabilityof mammography services,there has been minimal progressinscreening womenaged50-74 for breast cancer

Call for enhanced healthcare quality in SA
Health Quality Assessment (HQA), a non-profit and public benefit organisation, has once again measured and reported on healthcare quality across 83% of medical scheme members in SA.
By Nicky Belseck, medical journalist
HEALTH QUALITY ASSESSMENT
(HQA) has released its 2024 Industry Report, underscoring the critical role of quality in healthcare for the sustainability of SA's health sector. This comprehensive report, derived from data provided by medical schemes covering 83% of insured beneficiaries (7.43 million lives), evaluates over 200 health quality indicators across various domains, including primary care, maternity, chronic disease management, and hospitalisations. A non-profit and public benefit organisation, HQA is SA’s leading health quality measurement organisation.
DEMOGRAPHIC INSIGHTS AND CHRONIC DISEASE PREVALENCE
The report reveals a balanced demographic among beneficiaries, with a slight increase in the average age to 35 years. Chronic diseases continue to be a significant concern, with 25.30% of beneficiaries diagnosed with at least one chronic condition. The most prevalent conditions include hypertension, HIV, and diabetes. These findings highlight the growing burden
of chronic diseases on the healthcare system and the need for effective management strategies.
POSITIVE TRENDS IN PREVENTIVE CARE
Encouraging trends have been observed in preventive care measures. Flu vaccine coverage has improved, particularly among older adults, which is crucial for reducing the incidence of influenza-related complications. Additionally, there has been an increase in HIV testing and antenatal screening, reflecting efforts to enhance early detection and management of these conditions.
CHRONIC DISEASE MANAGEMENT: PROGRESS AND CHALLENGES
The report notes significant improvements in the management of diabetes and hypertension. These advancements are attributed to better adherence to treatment protocols and increased patient education. However, mental health screening and asthma management remain areas of
concern. The progress in these domains has been limited, indicating the need for targeted interventions to address these gaps.
PRIMARY CARE AND MATERNITY SERVICES
Primary care services have shown notable successes, particularly in the uptake of flu vaccines among older adults. Despite the availability of mammography services, there has been minimal progress in screening women aged 50-74 for breast cancer. This highlights the need for increased awareness and accessibility of screening programmes. Maternity care continues to be a focal point, with a high C-section rate of 75.81%. This statistic has prompted medical schemes to collaborate with obstetricians to address the issue of unnecessary preterm deliveries. Efforts are being made to promote natural births and reduce the rate of elective C-sections.
HOSPITALISATION AND SURGICAL OUTCOMES
The report highlights improvements in hip and knee replacement procedures, leading to shorter hospital stays and reduced complications. However, there has been an increase in readmission rates for hip replacements, necessitating further investigation into the underlying causes. Asthma management remains a challenge, with a decline in lung function testing and low compliance among patients on controller therapy. Conversely, pneumonia hospital admissions have decreased, likely due to better infection control practices.
The 2024 HQA Industry Report provides critical insights into the healthcare landscape in SA. It emphasises the need for continuous improvement and collaboration among stakeholders to enhance the quality of care. The findings underscore the importance of preventive care, effective chronic disease management, and the optimisation of primary care and maternity services. As the healthcare sector continues to evolve, these insights will be instrumental in guiding future strategies to improve health outcomes for all South Africans.


AI to the rescue: tackling drug shortages with cutting-edge technology
Artificial intelligence is poised to revolutionise the pharmaceutical supply chain and tackle the persistent issue of drug shortages.
By Nicky Belseck, medical journalist
THE SAPICS 2024 conference,
a premier event for supply chain professionals, recently highlighted the critical issue of drug shortages and the potential role of artificial intelligence (AI) in mitigating these challenges.
We unpack the key points discussed at
the conference, providing valuable insights for doctors on how AI can revolutionise the pharmaceutical supply chain and address drug shortages.
UNDERSTANDING DRUG SHORTAGES
Drug shortages have been a persistent
issue globally, affecting patient care and treatment outcomes. These shortages can arise from various factors, including manufacturing disruptions, regulatory challenges, supply chain inefficiencies, and unexpected surges in demand. For doctors, these shortages can lead to treatment


delays, the need for alternative therapies, and increased healthcare costs.
THE ROLE OF AI IN ADDRESSING DRUG SHORTAGES
Experts at the conference emphasised the transformative potential of AI in the pharmaceutical supply chain. AI technologies, such as machine learning and predictive analytics, can enhance supply chain visibility, optimise inventory management, and predict potential shortages before they occur.
1. Predictive analytics: AI analyse data from multiple sources, including sales, manufacturing schedules, and market trends, to accurately predict future drug demand. This helps manufacturers and suppliers anticipate shortages and adjust production and distribution plans.
2. Inventory optimisation: AI inventory systems optimise stock by considering shelf life, demand, and lead times, ensuring drugs are available and minimising stockouts and overstock.
3. Supply chain visibility: AI systems optimise stock by considering shelf life, demand, and lead times, ensuring availability and minimising stockouts.
CASE STUDIES AND SUCCESS STORIES
Case studies at SAPICS 2024 showed AI success in the pharmaceutical supply chain. A company used AI to predict a medication shortage, adjusted production, and worked with suppliers to prevent it.
Another example highlighted the use of AI in optimising inventory levels for a hospital pharmacy. The AI system analysed usage patterns and external factors to recommend stock levels, reducing stockouts and improving patient care.
CHALLENGES AND CONSIDERATIONS
While AI offers promising solutions, its implementation in the pharmaceutical supply chain is not without challenges.
Data quality and integration, regulatory compliance, and the need for skilled personnel to manage AI systems are critical considerations. Additionally, the ethical implications of AI, such as data privacy and algorithmic bias, must be addressed to ensure fair and equitable outcomes.
Data quality, integration, compliance, and skilled personnel are key for managing AI. Ethical issues like privacy and bias must be addressed for fair outcomes.
SAPICS 2024 highlighted AI's potential to revolutionise the pharmaceutical supply chain and reduce drug shortages. Doctors can advocate for better supply practices and ensure medication availability. As AI evolves, it promises to enhance efficiency, cut costs, and improve patient care.
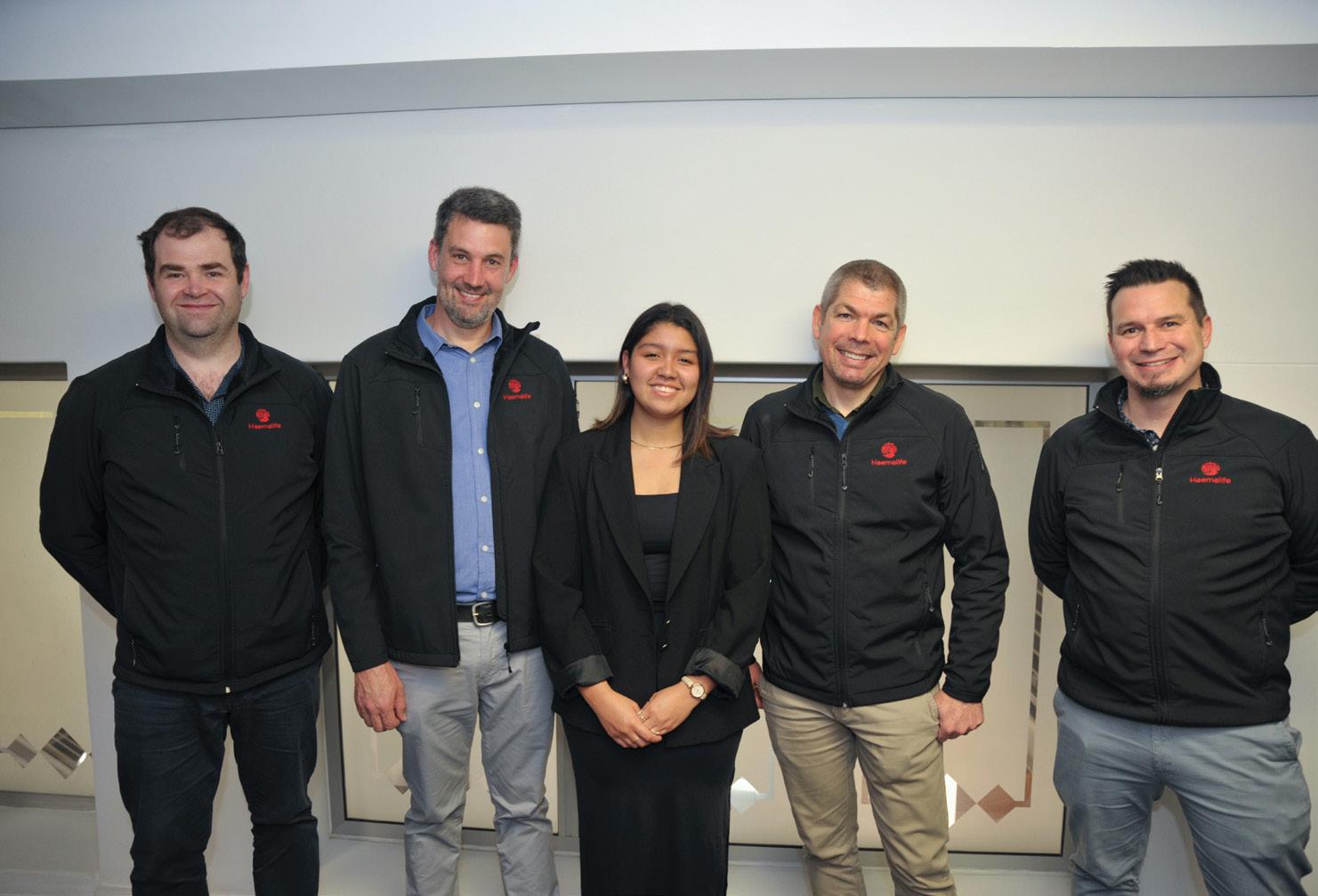
Expanded bone marrow transplant unit opens
For some people with life-threatening blood cancers, a bone marrow transplant may be their only remaining treatment option.
THE LAUNCH OF the upgraded and expanded Haemalife Bone Marrow Transplant (BMT) unit at Netcare Kuils River Hospital signals more hope and an opportunity to create lifesaving awareness of South Africa’s bone marrow donor registry programmes.
“The time sensitive and highly specialised nature of haematology treatments, and the growing need for such services in the Northern suburbs of Cape Town and for patients from further afield, emphasises the importance of the additional capacity that has been created with this larger bone marrow transplant unit,” says Dirk Truter, general manager of Netcare Kuils River Hospital.
“We thank Dr Hannes Koornhof and Dr Pieter de Witt, the founding haematologists of the Haemalife practice, as well as their colleagues Dr Michael Cass, Dr Simon Brett, medical officer Dr Liza Stockland, and all members of this immensely caring team for their dedication to improving the facilities and growing the expertise available to help our patients and their families.”
Dr Koornhof says that the BMT Unit opened eight and a half years ago with eight beds and was very soon at full occupancy. The unit’s first of many successful bone marrow transplants was performed in February 2016.
“While the expansion of capacity is welcome news for patients who urgently need treatment and their referring doctors, there is also an urgent need for more South Africans to consider registering as potential bone marrow donors to contribute more diversity to the international bone marrow
donor registry and increase the hope of finding suitable life-saving matches both at home and elsewhere in the world.”
“Specialised single isolation rooms, each with their own en suite bathroom and ventilation system, are required when a person has a bone marrow transplant or intensive chemotherapy,” adds Dr Cass.
“Before a bone marrow transplant, we need to suppress the person’s immune system with chemotherapy and specialised medications to reduce the risk of the patient’s body rejecting the introduced donated stem cells. For this reason, a very controlled environment is needed to protect the patient for three to six weeks,” he explains.
“With the Department of Health’s approval of the application, the BMT unit has now been expanded to 19 beds. The original isolation suites have been upgraded, and an upper level of isolation suites has been added on the floor above with an interlinking staircase, making this one of the largest bone marrow transplant units in the country.
“Bone marrow transplants may be indicated for leukaemia, multiple myeloma or lymphoma, or when a person’s body is unable to produce enough healthy blood cells due to a health condition or from the effects of prolonged treatment,” Dr De Witt says. The Netcare Kuils River Hospital unit is the only facility in the northern suburbs to provide bone marrow transplants and treat acute leukaemia. Although adult patients are the focus, the unit also treats patients as young as ten years old. Holistic, personalised services are provided for all stages of
treatment, including survivorship and palliative services that support the patient and their loved ones throughout.
The newest haematologist to join the multidisciplinary team, Dr Simon Brett, adds that some bone transplant patients may be able to receive a bone marrow stem cell donation from a family member if there is a close enough tissue match between them.
“For those who do not have a familial matching donor, there is only an average of one person out of every 100 000 tested who might be a compatible tissue match. The more people who register as bone marrow donors, the more patients with
LEUKAEMIA
blood cancers or other blood disorders can be matched for a potentially lifesaving bone marrow transplant.”
Registering as a bone marrow donor is free of charge and non-invasive, and could save a life. For more information, please visit https://sabmr.co.za/become-a-donor/ and https://www.dkms-africa.org/getinvolved/become-a-donor.
Contact the HaemaLife Bone Marrow Transplant Unit at Netcare Kuils River Hospital on 021 900 6277; via email reception@haemalife.co.za or visit https://haemalife.co.za/.
SURVIVOR RETURNS AS MEDICAL STUDENT
Bone marrow transplant inspired Joy’s career choice
Joy Schoor was just 14 when she was diagnosed with acute myeloid leukaemia. Now, celebrating eight years in remission, she is paying forward her second chance at life by studying to be a doctor and encouraging the public to join the registry of potential stem cell donors.
“I was returning with my parents from a holiday in the Kruger National Park when suddenly I started feeling sick and developed a fever. At first, doctors thought it could be a common infection and had to rule out malaria. After more tests at various hospitals, I was diagnosed on 10 January 2016 – although I didn’t fully understand what it meant at the time,” Joy, now 23, remembers.
“I have such a supportive family, and with my whole future in question, my parents heard that haematologists Dr Hannes Koornhof and Dr Pieter de Witt of Haemalife were equipped to offer the specialised bone marrow transplant procedure at the nearby Netcare Kuils River Hospital.”
As the first patient to receive a lifesaving bone marrow transplant at the hospital in 2016, it was a poignant moment when Joy was recently invited back as a guest of honour to cut the ribbon officially declaring the expanded comprehensive bone marrow transplant unit open alongside the haematologists who treated her then.
“My journey through three rounds of chemotherapy was not easy, but it is one of the reasons I was inspired to study to become a doctor. The warmth, compassion and kindness my family and I experienced at the unit during this difficult time in my teenage years stayed with me and made me want to help others in their time of need,” Joy says.
“Even though I was so young, the doctors explained everything so carefully to me and my parents and did everything they could to make us feel at home and as comfortable as possible in the circumstances.
“I am grateful that my brother, who was only 12 at the time, was an almost perfect tissue match and he agreed to donate stem cells to me for the bone marrow transplant I needed.
“There is only a 25% chance of a sibling being a match, and some people can have 12 brothers and sisters, and none of them are sufficient matches, so I was exceptionally lucky, and to this day can’t thank my brother enough – although he still teases me about it,” Joy says.
“Tragically, there are people in need of bone marrow transplants for whom matching donors can’t be found. As a survivor, this is why I would like to pay it forward by raising awareness of the need for more people to register as stem cell donors – you could save a life.”
Joy will also be job shadowing at the practice that saved her life as part of her medical studies later this year.
“I am making the most of my second chance at life, living my dream of becoming a healthcare professional and eight years cancer-free thanks to the specialised care I received here. I cannot tell you how significant it is for me to be cutting the ribbon at the same facility that will be a beacon of hope for many other families in the years to come,” Joy concludes.
We are pleased to invite you to join us for our Acino Anaemia Symposium focussing on
blood management, anaemia and the ethics of blood transfusion
This webinar is sponsored by Acino
Date: 19 October 2024
Time: 12pm - 4.30pm
Topic: Patient blood management, anaemia and the ethics of blood transfusion
Speakers: Prof Vernon Louw, Prof Nqoba Tsabedze, Prof Philip Kalra and Dr Petro-Lizé Wessels

Prof Nqoba Tsabedze
Prof Philip Kalra
Prof Vernon Louw
Dr Petro-Lizé Wessels
Shen
where we are globally and in South Africa in 2024

Prof Vernon Louw, South Africa
Prof Vernon Louw is chair and head of the Division of Clinical Haematology in the Department of Medicine at the University of Cape Town since April 2018. He held previous roles as professor and head of the Department of Internal Medicine at the Faculty of Health Sciences at the University of the Free State in Bloemfontein since 2013 and head of Division of Clinical Haematology from 2004 to 2013. After completing his MBChB and MMed in Internal Medicine at the University of Stellenbosch (both summa cum laude), he spent three years at the Katholieke Universiteit Leuven training in Clinical Haematology. In 2011, he obtained his PhD in Health Professions Education at the University of the Free State, on the development of a postgraduate training programme in transfusion medicine. In 2015 he received the National South African Registrar Association Award for Excellence in Teaching and Research Supervision. His research focuses on iron-related disorders (both iron deficiency and transfusional iron overload), patient blood management, transfusion medicine education, haematological malignancies and HIV-related haematological disease. Professor Louw has authored or co-authored more than 100 papers in peer-reviewed medical journals, with more than 300 poster and oral presentations at local, national and international meetings. Professor Louw is a member of several professional societies, including the American Society of Hematology, the Hematology Association, American Association for Blood Banking and the International Society for Blood Transfusion, and is a founding member of the South African Clinical Haematology Society. He also serves on the World Health Organisation Strategic Committee for Patient Blood Management, the Global Transfusion Forum Steering Committee and Education Subcommittee, the Global Standards Committee for Transfusion Medicine and the International Collaborative for Transfusion Medicine Guidelines Committee.
Patient blood management where we are globally and in South Africa in 2024
Time: 12:05 pm - 12:50 pm
Maternal anaemia and the neurocognitive effect on the foetus and child
Time: 2:30 pm - 3:20 pm

Prof Philip Kalra, United Kingdom
Professor, qualified from Cambridge University (distinction) and St Thomas Hospital, London 37 years in nephrology, 27 years as a consultant Nephrologist. Lead of the Renal Research Team in Salford (greater Manchester): 320 peer reviewed publications; 19 of his previous PhD students have become consultant Nephrologists. Director of research, Northern Care Alliance NHS Foundation Trust since October 2020. Major research interests are in Renovascular disease (Nephrology Lead of ASTRAL trial) CKD epidemiology/progression, iron management in CKD, RCTs in nephrology (IRONMAN, PIVOTAL), chairman of the NIHR CRN Renal Disorders Trials initiative (2010-2018) Academic vice President of the UK Renal Association (2016-2019) Chair of UK Kidney Research consortium (2016-2018), 'Editor of Essential Revision Notes for the MRCP' (first published 1999, now in fourth edition; used by many doctors preparing for the MRCP in the UK, South East Asia and Middle East
The safety of intravenous iron
Time: 1:40 pm - 2:30 pm

Prof Nqoba Tsabedze, South Africa
Prof Nqoba Tsabedze is the Academic Head of the Division of Cardiology of the University of the Witwatersrand. He is also the clinical head of the Division of Cardiology at the Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa. He is passionate about teaching and training both undergraduate and postgraduate students. He is an executive member of the Heart Failure Society of South Africa, and a founding and executive member of the South African Clinician Scientists Society. His research interests include acute and chronic heart failure epidemiology in sub-Saharan Africa, heart failure with preserved ejection fraction and hypertensive heart disease.
The relevance of anaemia in congestive heart failure
Time: 12:50 pm - 1:40 pm

Dr Petro-Lizé Wessels, South Africa
Lead consultant Patient Blood Management at South AfricanNational Blood Service South African National Blood Service - 10 years five months Medical Officer Free State / Northern Cape April 2011 - Present (10 years five months) Free State Northern Cape Provinces Drafting business plans and monitoring budget for Free State Northern Cape Medical division. Support to Technical division (Processing, blood banks, inventory) and Collections division (whole blood and apheresis donors) on all matters requiring medical input or advice within SANBS. Participation in SANBS research projects. Monitoring risk factors influencing a safe blood supply (medial, legal and ethical) and developing and implementation of risk containing interventions. Support to external medical practitioners concerning transfusion needs or challenges with patients. Developing and facilitating educational programmes to nurses and medical practitioners on all transfusion related topics in the public and private sector. Establishing, supporting and advising hospital transfusion committees in FSNC hospitals. Liaising with the public (media and donors) on all matters requiring medical input related to transfusion. All HR and IR related matters.
The ethics of blood transfusion in a patient blood management setting
Time: 3:20 pm - 4:05 pm

A Medical negligence: A legal perspective for healthcare practitioners
In today’s fast-paced healthcare environment, healthcare practitioners' responsibilities have become increasingly complex.

S the pressure to deliver top-tier patient care intensifies, so does the importance of understanding the legal obligations that govern medical practice. Medical negligence claims can have serious ramifications, affecting professional reputation and personal and institutional liability. To help healthcare professionals navigate these legal intricacies, GoodX Online Short Courses is excited to introduce our new Continuing Professional Development (CPD) course, Medical Negligence: A Legal Perspective, crafted through the expertise of Prof Magda Slabbert.
This course is specifically designed for healthcare practitioners who want to better understand how to avoid medical negligence claims. By equipping professionals with the legal knowledge they need, we aim to empower them to safeguard their practices, ensure patient safety, and minimise the risk of facing legal action.
WHY TAKE THIS COURSE?
There is undoubtedly an increase in medical negligence cases in South Africa. The consequences of a medical negligence claim can be profound, both personally and professionally. Even if a claim is ultimately dismissed, defending oneself against an allegation can be stressful, costly, and time-consuming. For this reason, a solid understanding of the legal principles surrounding medical negligence is essential. Our CPD course offers a unique legal perspective tailored to healthcare practitioners. It makes complex legal jargon and case law accessible. The focus is not only on the theory but also on real-world
applications, ensuring that participants come away with a practical understanding of how to prevent negligence claims from arising in the first place.
The course is divided into six comprehensive modules, each carefully curated to build a complete understanding of medical negligence from a legal standpoint. Here’s an overview of what you can expect to learn.
MODULE 1: A CONTRACT
The course begins by introducing the doctor-patient relationship from a legal perspective. In this module, participants will learn about the nature of the contractual relationship between a healthcare provider and a patient. This relationship underpins much of the legal framework surrounding medical negligence. You will gain a clear understanding of what constitutes an implied or express contract, as well as the rights and obligations both parties hold in this dynamic. Understanding this contractual foundation is essential for healthcare practitioners, as it forms the baseline for determining liability in cases where negligence is alleged.
MODULE 2: DELICT
Delict law is the second foundational pillar of medical negligence claims. This module introduces the concept of delict, focusing on the duty of care that healthcare practitioners owe their patients. We explain the legal principles of delict in a way relevant to medical professionals, ensuring that participants can identify situations
where their conduct could be classified as negligent. Case studies and real-world examples help illustrate how delict law is applied in medical contexts, providing participants with practical insights into avoiding potential legal pitfalls.
MODULE 3: THE TEST FOR MEDICAL NEGLIGENCE
Perhaps the most crucial aspect of this course is the detailed explanation of the legal test for medical negligence. This module breaks down how courts determine whether practitioners have breached their duty of care. Participants will gain a deep understanding of the legal standard applied to determine negligence, focusing on concepts like 'reasonable care' and 'foreseeability.’ This module will draw on case law to show how judicial decisions have shaped the definition of medical negligence over time.
MODULE 4:
POSSIBLE AREAS WHERE NEGLIGENCE COULD OCCUR
Medical negligence can manifest in various ways, often in areas that practitioners least expect. This module explores the common places where negligence is alleged, from misdiagnosis and errors of judgement to lack of skill. By identifying these potential risk areas, healthcare practitioners will be better equipped to implement practices that reduce the likelihood of negligence claims.
MODULE 5:
HOW TO PROVE A MEDICAL NEGLIGENCE CASE
In this module, participants will learn about
the process of a medical negligence case. This knowledge empowers healthcare professionals to defend against frivolous claims and, more importantly, take preventative action in their daily practice.
MODULE 6: CRIMINAL LIABILITY
The final module addresses the more severe consequences of medical negligence: criminal liability. While rare, cases of gross negligence can lead to criminal charges, significantly raising the stakes for healthcare practitioners. Participants will explore the legal standards that differentiate between civil and criminal liability, learning about instances where negligent acts may result in prosecution.
CONCLUSION
Our Medical Negligence: A Legal Perspective course is an invaluable resource for healthcare professionals looking to enhance their understanding of the legal framework that governs their practice. With comprehensive modules covering everything from the basics of the doctorpatient contract to the intricacies of criminal liability, this CPD course is designed to help practitioners minimise risk and deliver the highest standard of care. By the end of the course, participants will have the legal knowledge and confidence to navigate the complexities of medical negligence, ensuring that they are providing excellent care and protecting themselves and their practice from potential legal claims. Sign up today at courses. goodx.co.za and take the first step toward safeguarding your professional future.
Learn more about Medical Negligence: A Legal Perspective
The course aims to inform healthcare practitioners how to avoid claims due to medical negligence by explaining the doctor-patient contractual relationship, the doctor's duty under delict law, and the courts' negligence test, using case law to illustrate practical applications and judicial decisions on alleged negligence.


Module 1: A Contract
Module 2: Delict
Module 3: The test for medical negligence
Module 4: Possible areas where negligence could occur
Module 5: How to prove a medical negligence case
Module 6: Criminal liability




Date: 31 October 2024
Time: 6pm
Topic: Secondary dry eye with diabetes
Speaker: Dr. Marsha Oberholzer (D.Phil Optom - UJ)
CLICK TO REGISTER https://bit.ly/PharmacoWebinar31Oct24
Dr. Marsha Oberholzer is a proud South African that has earned three academic degrees from the University of Johannesburg in South Africa. After completing her B.Optom degree, she pursued her Master’s degree in Optometry and thereafter, her PhD in Visual Science which she completed in 2015. After her undergraduate studies, she embarked on a career starting out as an Independent Optometrist, practicing in Johannesburg, South Africa after which she spent four years assisting an Ophthalmologist and Refractive Surgeon in his practice. Dr Oberholzer joined the Optometry School of the University of the Free State in South Africa in 2008 as a senior lecturer, lecturing and training undergraduate and postgraduate students in especially the niche fields of Ocular Pathology and Neuro-Optometry. Her teaching background includes the management of the undergraduate Optometry program at this University and involvement in the Professional Board (HPCSA) accreditation and re-curriculation of the undergraduate Optometry programme. During this time, she travelled across the world lecturing and training clinicians in a variety of optometric fields, mostly in the field of Higher Order Aberrations, which was the focus of her PhD Studies. She also served as a key opinion leader for Alcon Laboratories during this time, after which she then permanently joined Alcon as the South African professional education



















and development manager in 2019. Her journey with Alcon has given her the opportunity to not only train within the field of contact lenses locally and export markets, but also the opportunity to travel globally, being involved in the extensive training to GEM (Growth and Emerging markets) associates, distributors and Eye Care Professionals. Since October 2023, Marsha has been appointed as the vision care professional education and product training head for GEM at Alcon. Dr Oberholzer has won multiple awards during her career, under which the most valued are the winner of the “Excellence in teaching and learning” award in the category Junior Lecturer at the UFS in 2011, Alcon AAA and GEM awards as well as the SA Alcon Hero award in 2022. Currently Dr Oberholzer is expanding her horizons with more extensive trainings globally at Alcon. She is also still an affiliated postgraduate lecturer at the University of the Free State where she continues to actively lead Masters and PhD Optometry students in their postgraduate studies. Even though her first love may be “eyes”, she is also a musician, actively playing the Violin and Viola in Professional Orchestras in South Africa. She is a wife, and mother of three (one daughter and two sons) which keeps her on her toes and humble.



CERVARIX helps prevent:
• persistent infection
• premalignant ano-genital lesions (cervical, vulvar, vaginal and anal)
CERVARIX
• cervical, vulvar, vaginal and anal cancers (squamous-cell carcinoma and adenocarcinoma) caused by oncogenic Human Papillomaviruses (HPV)
From the age of 9 years
could help PREVENT 9 out of 10 POTENTIAL cervical cancer cases IRRESPECTIVE OF
HPV* TYPE1

LEAD THE FIGHT TODAY!
CERVARIX has been formulated with AS04** for a strong and sustained immune response, up to 20 years2
Contraindications:
CERVARIX should not be administered to patients with known hypersensitivity to any component of the vaccine1
Very common adverse reactions (≥1/10): Headaches, myalgia, injection site pain, redness, swelling and fatigue1
* Human Papillomavirus
† applicable to TVC naive cohort
** an adjuvant system comprised of 3-O-desacyl-4’-monophosphoryl lipid A [MPL, 50 μg] absorbed on aluminum
All adverse events should be reported by calling the Aspen Medical Hotline number or directly to GlaxoSmithKline on +27 10 300 1000.

Scan here for the professional information for comprehensive safety and efficacy information
References: 1. Lehtinen M, Paavonen J, Wheeler CM, Jaisamrarn U, M Garland SM, Castellsagué X, et al, for the HPV PATRICIA. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012;13: 89-99. 2. Naud PS, Roteli-Martins CM, De Carvalho NS, Teixeira JC, de Borba PC, Sanchez N, et al. Sustained efficacy, immunogenicity, and safety of the HPV-16/18 AS04-adjuvanted vaccine. Final analysis of a long-term follow-up study up to 9.4 years post-vaccination. Human Vaccines & Immunother. 2014; 10(8): 1-16. 3. CERVARIX Professional Information leaflet 04/2017.
S2 CERVARIX. Reg. No. 41/30.1/0366. Each 1 dose (0,5 ml) contains: Human Papillomavirus type 16 L1 protein 20 μg, Human Papillomavirus type 18 L1 protein 20 μg, 3-O-desacyl-4’-monophosphoryl lipid A (MPL) 50 μg, aluminium hydroxide, hydrated 0,5 mg Al3+ For full prescribing information refer to the professional information approved by the medicines regulatory authority (04/2017). HCR: GlaxoSmithKline South Africa (Pty) Ltd (Co. Reg. No. 1948/030135/07). 39 Hawkins Ave, Epping Industria 1, 7460. All adverse events should be reported by calling the Aspen Medical Hotline number or directly to GlaxoSmithKline on +27 10 300 1000. Trade marks are owned by or licensed to the GSK group of Companies. © 2024 Aspen Group of companies or its licensor. All rights reserved. Marketed by Aspen Pharmacare, Healthcare Park, Woodlands Drive, Woodmead, 2191. ZAR-VHP-09-23-00001 02/2024
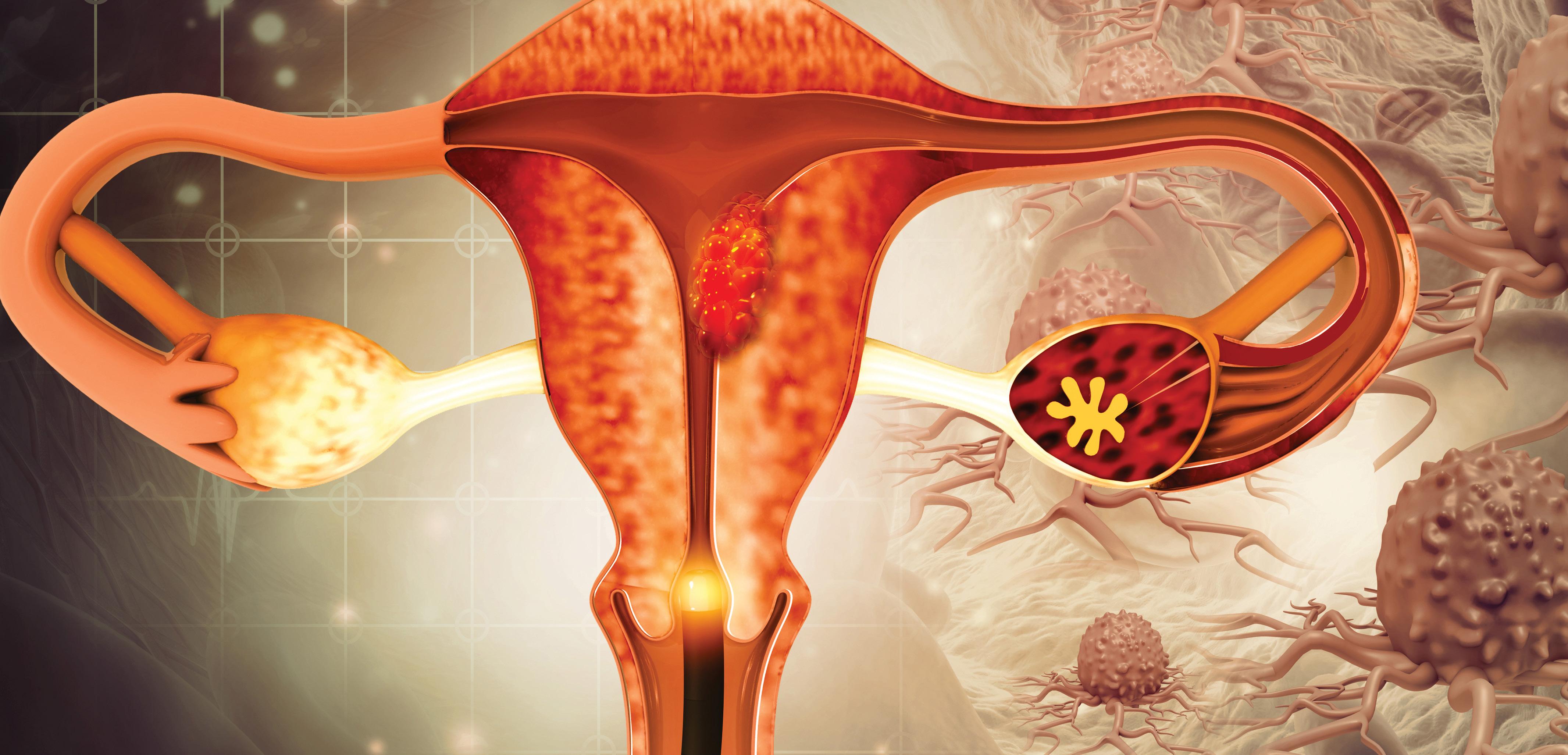
Paving the way to cervical cancer elimination in SA
Cervical cancer remains a significant public health challenge, particularly in low- and middle-income countries (LMICs) like South Africa. The World Health Organization (WHO) has set ambitious targets to eliminate cervical cancer as a public health issue by 2030.
THIS ARTICLE AIMS to provide healthcare professionals in South Africa with an overview of the latest guidelines and innovations in HPV screening and therapeutic vaccines, emphasising their importance in combating cervical cancer.
HPV AND CERVICAL CANCER: AN OVERVIEW
Human papillomavirus (HPV) is a common sexually transmitted infection, with certain high-risk types being the primary cause of cervical cancer. In 2022, approximately 662 000 women were diagnosed with cervical cancer globally, leading to around 349 000 deaths, predominantly in LMICs (WHO, 2022). In South Africa, cervical cancer is the second most common cancer among women, with a high mortality rate due to late-stage diagnosis and limited access to healthcare services.
HPV is transmitted through sexual contact, and most sexually active individuals will contract the virus at some point in their lives. While the majority of HPV infections are asymptomatic and resolve spontaneously, persistent infection with high-risk HPV types can lead to the development of cervical cancer. The most common high-risk HPV types associated with cervical cancer are HPV-16 and HPV-18, which together account for approximately 70% of cases.
WHO GUIDELINES FOR HPV SCREENING AND TREATMENT
The WHO has issued updated guidelines for the screening and treatment of cervical pre-cancer lesions to prevent cervical cancer. These guidelines emphasise the significance of HPV testing and aim to eliminate cervical cancer as a public health issue by 2030. Key targets include vaccinating 90% of girls against HPV by age 15, screening 70% of women with highperformance tests by ages 35 and 45, and ensuring that 90% of women diagnosed with cervical disease receive treatment (WHO, 2022).
SCREENING STRATEGIES
The guidelines propose two main screening strategies:
1. Screen-and-treat approach: Treatment is initiated based solely on a positive primary screening test. This approach is particularly beneficial in settings with limited access to healthcare services, as it reduces the need for multiple visits and minimises loss to follow-up.
2. Screen, triage, and treat approach: Involves a secondary triage test, such as dual-stain cytology, after a positive primary screening test. This approach allows for more accurate identification of women at highest risk of developing cervical cancer, ensuring that treatment is targeted to those who need it most.
HPV DNA testing is recommended as the primary screening method, starting at age 30 for the general population and age 25 for women living with HIV, with suggested screening intervals of five to 10 years for the general population and three to five years for women with HIV (WHO, 2022). HPV DNA testing is highly sensitive and can detect the presence of high-risk HPV types before any visible changes occur in the cervical cells, allowing for early intervention and treatment.
THERAPEUTIC HPV VACCINES: A NEW FRONTIER
The WHO's preferred product characteristics (PPCs) for therapeutic HPV vaccines emphasise their importance in combating HPV infections and cervical cancer, particularly in LMICs. Therapeutic HPV vaccines are designed to enhance existing interventions, particularly in regions with limited healthcare access. These vaccines aim to clear high-risk HPV infections and target cervical precancers, providing a comprehensive approach to HPV vaccination (WHO, 2022).
DEVELOPMENT AND FEASIBILITY
The development of therapeutic HPV vaccines is explored, focusing on their
feasibility, clinical considerations, and public health value. The WHO's PPCs aim to encourage innovation in vaccine development, ensuring that new vaccines are effective, safe, and accessible, particularly in LMICs. Collaborative efforts of various experts and organisations, including the Bill & Melinda Gates Foundation, have shaped these recommendations (WHO, 2022). Therapeutic HPV vaccines are currently in early clinical development, with several candidates showing promise in preclinical and early-phase clinical trials. These vaccines work by stimulating the immune system to recognise and eliminate cells infected with high-risk HPV types, thereby preventing the progression to cervical cancer. Unlike prophylactic vaccines, which are designed to prevent HPV infection, therapeutic vaccines are intended to treat existing infections and precancerous lesions.
STRATEGIC FRAMEWORK
FOR IMPLEMENTATION
The document outlines the characteristics of these vaccines, including their ability to clear infections and regress precancerous lesions, and emphasises the need for ethical considerations in clinical trials. It advocates for a comprehensive approach to HPV vaccination that integrates therapeutic vaccines into existing health systems, addresses the unique needs of different populations, and ensures cost-effectiveness for global access (WHO, 2022).
TARGET POPULATIONS AND STRATEGIES
Key points include the importance of targeting individuals who may not have received prophylactic vaccines, particularly women with positive cervical cancer screening results and those living with HIV. The document suggests a 'test and vaccinate' strategy, integrating vaccination into cervical cancer screening programmes, and emphasises the need for thorough safety evaluations, especially for pregnant

women (WHO, 2022). The 'test and vaccinate' strategy involves testing women for high-risk HPV types and vaccinating those who test positive, regardless of their vaccination history. This approach ensures that women who are at highest risk of developing cervical cancer receive the necessary intervention to prevent disease progression. Additionally, integrating vaccination into existing cervical cancer screening programmes can improve vaccine uptake and coverage, particularly in settings with limited healthcare infrastructure.
CONCLUSION
The WHO's updated guidelines and the development of therapeutic HPV vaccines represent significant advancements in the fight against cervical cancer. For healthcare professionals in South Africa, these innovations offer new opportunities to enhance cervical cancer prevention and treatment efforts. By adopting these guidelines and integrating therapeutic vaccines into existing health systems, South Africa can make significant strides towards eliminating cervical cancer as a public health issue by 2030. Healthcare professionals play a crucial role in this effort by educating women about the importance of HPV testing and vaccination, advocating for policy changes to improve access to cervical cancer prevention services, and providing high-quality care to women with positive HPV test results. Collaborative efforts between healthcare providers, policymakers, researchers, and communities are essential to achieving the WHO's targets and ensuring that all women in South Africa have the opportunity to live healthy, cancerfree lives.
REFERENCES
World Health Organization. (2022). WHO guidelines for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention. Retrieved from https://www.who.int/. World Health Organization. (2022). WHO preferred product characteristics for therapeutic HPV vaccines. Retrieved from https://www.who.int/.



Exploring BPH treatments Mono- vs combo therapy
Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland, common in older men, leading to bladder outflow obstruction (BOO) and lower urinary tract symptoms (LUTS).
This article is a summary of a CPD-accredited article featured in our sister publication, Specialist Forum, available here: https://www.medicalacademic.co.za/courses/exploring-bph-treatments-mono-vs-combo-therapy/

THE PREVALENCE OF
BPH
increases with age, affecting 50%60% of men in their 60s and 80%90% of men over 70 years old. BPH is rare in men under 40 but more common in those with a family history, obesity, and metabolic syndrome. BPH is diagnosed by the proliferation of smooth muscle, epithelium, and stromal cells in the prostate's transition zone. Symptoms result from static (hyperplastic tissue compressing the urethra) and dynamic (increased adrenergic nervous system activity and prostatic smooth muscle tone) mechanisms. Both mechanisms increase resistance to urinary flow, leading to detrusor muscle hypertrophy and symptoms like urinary frequency and urgency. Chronic BOO can cause bladder decompensation and detrusor underactivity, resulting in LUTS characterised by incomplete emptying, urinary hesitancy, intermittency, a weakened urinary stream, and urinary retention.
TREATMENT OPTIONS
Factors influencing treatment decisions include symptom severity, impact on daily activities, worry, embarrassment, and concerns about acute urinary retention (AUR) and surgery. BPH can lead to benign prostatic enlargement (BPE), which may cause benign prostatic obstruction (BPO) and LUTS. Treatment aims to alleviate symptoms and prevent disease progression and complications. Studies show that mild symptoms (IPSS <8) have a ~31% risk of progressing to moderate or severe symptoms (IPSS ≥8) in four years. Common complications include AUR, chronic urinary retention, urinary tract infections, haematuria, bladder calculi, bladder wall and kidney damage, incontinence, and erectile dysfunction (ED).
WATCHFUL WAITING
Watchful waiting is recommended for non-bothersome LUTS. Prof Shingai Mutambirwa supports this approach for asymptomatic or minimally bothered men, with treatment indicated for significant complications like urine retention, kidney issues, stones, or infections. Regular evaluation is essential to monitor for changes or complications. This approach is particularly suitable for men who prefer to avoid medication or surgery unless absolutely necessary. It involves regular check-ups to monitor the progression of symptoms and ensure that no severe complications arise.
MEDICAL/PHARMACOTHERAPY
Pharmacotherapy should start if
bothersome symptoms occur. Treatment selection should consider patient age, comorbidities, and potential side effects.
The AUA and EAU recommend alpha blockers (α1-blockers) like tamsulosin for moderate to severe LUTS. These medications work by relaxing the smooth muscle in the prostate and bladder neck, making it easier to urinate. They are usually effective within a few days to weeks. However, they do not reduce the size of the prostate.5-alpha reductase inhibitors (5-ARIs) like dutasteride are recommended for symptom improvement in BPE and can be used alone or with α1-blockers to prevent symptom progression, urinary retention, and future surgery. 5-ARIs work by blocking the conversion of testosterone to dihydrotestosterone (DHT), a hormone that contributes to prostate growth. This leads to a reduction in prostate size and improvement in symptoms over several months. Patients should be counselled about potential sexual side effects and the low risk of PCa before starting 5-ARIs.
COMBINATION THERAPY
The EAU and AUA recommend combining α1-blockers and 5-ARIs for BPE. Combination therapy is more effective than monotherapy in reducing the risk of AUR, BPH-related surgery, and clinical progression. The CombAT study found that combination therapy with dutasteride and tamsulosin provided greater symptom benefit and improved patient-reported QoL and treatment satisfaction compared to monotherapy. This approach is particularly beneficial for men with larger prostates or more severe symptoms. Combination therapy offers the advantages of both drug classes: the rapid symptom relief of α1-blockers and the long-term benefits of 5-ARIs in reducing prostate size and preventing disease progression.
IS COMBINATION THERAPY MORE EFFECTIVE THAN MONOTHERAPY?
A study by Roehrborn et al. (2009) investigated whether combination therapy is more effective than either monotherapy in reducing the relative risk for AUR, BPH-related surgery, and BPH clinical progression in men at increased risk of progression. The Combination of Avodart and Tamsulosin (CombAT) study was a fouryear, multicentre, randomised, double-blind, parallel-group study involving 4844 men aged ≥50 years with a clinical diagnosis of BPH, an IPSS of ≥12, a prostate volume of 30cm³ or larger, a PSA level of 1.5ng/ ml-10ng/ml, and a maximum urinary flow rate (Qmax) between 5ml/s and 15ml/s
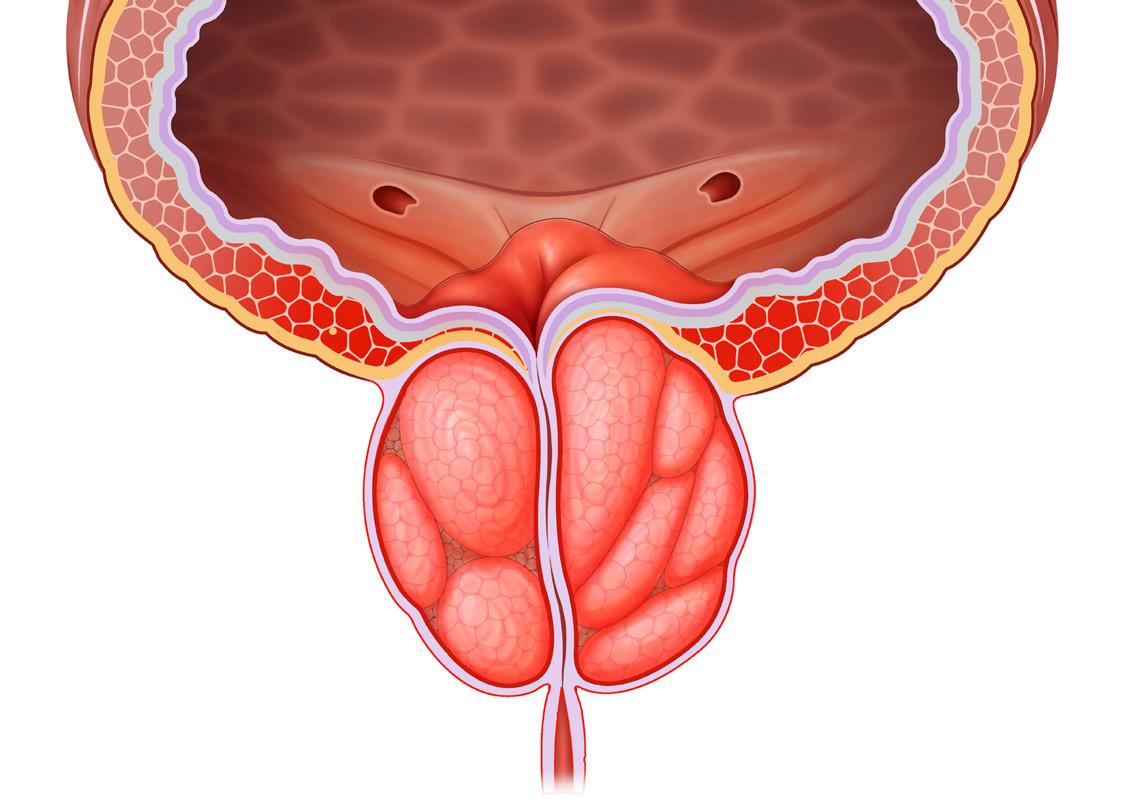
with a minimum voided volume of 125ml. Participants received oral daily tamsulosin (0.4mg), dutasteride (0.5mg), or a combination of both. The primary endpoint over the four years was the time to first AUR or BPH-related surgery. Secondary endpoints included BPH clinical progression, symptoms, Qmax, prostate volume, safety, and tolerability. The team found that combination therapy was significantly superior to tamsulosin monotherapy but not dutasteride monotherapy in reducing the relative risk of AUR or BPH-related surgery. It was also significantly superior to both monotherapies in reducing the relative risk of BPH clinical progression and provided significantly greater symptom benefit after four years. Several sub-analyses of the CombAT study were conducted.
One of these, by Montorsi et al., assessed the effects of dutasteride/ tamsulosin combination therapy on voiding and storage symptoms compared with those of dutasteride or tamsulosin monotherapy. At four years, the mean reduction in the storage subscore was significantly greater in the combined therapy group compared to the dutasteride (adjusted mean difference [AMD] −0.43) and tamsulosin (AMD −0.96) monotherapy groups.
Similarly, the mean reduction in the voiding subscore was significantly greater in the combined therapy group compared to the dutasteride (AMD −0.51) and tamsulosin (AMD −1.60) monotherapy groups.
The improvement in the storage subscore with combined therapy was significantly better than dutasteride from three months and tamsulosin from 12 months. Likewise, the improvement in the voiding subscore with combined therapy was significantly better than dutasteride from three months and tamsulosin from six months. Improvements in both storage and voiding symptom subscores with combined therapy were achieved irrespective of prostate volume but not in men with a prostate volume of ≥58ml.
SURGICAL OPTIONS
Surgical options for BPH in South Africa include open prostatectomy (transvesical, laparoscopic, or robotic-assisted), transurethral holmium laser ablation of the prostate, transurethral holmium laser enucleation of the prostate, holmium laser resection of the prostate, greenlight laser therapy, thulium laser therapy, transurethral incision of the prostate, transurethral vaporisation of the prostate, and TURP. TURP is widely regarded as the current gold standard for the management of BPH.
Available minimal invasive therapies include prostate arterial embolisation, rezum water vapour therapy, and transurethral stents. According to Prof Mutambirwa, surgery is a viable option at any stage of the BPH/LUTS journey. Some data suggest it may be more cost-effective than pharmacotherapy in the long term. Rare but significant side effects such as severe bleeding should be discussed with the patient before surgery. The patient should also be made aware that catheterisation will be necessary. Retrograde ejaculation is a notable side effect, particularly for surgeries like TURP and enucleation.
CONCLUSION
Combination therapy with dutasteride and tamsulosin offers significant benefits for BPH, providing earlier and sustained symptom relief and better long-term control of LUTS. This approach is superior to either monotherapy in reducing both storage and voiding symptoms, improving patient-reported health outcomes, and enhancing overall satisfaction.
The choice of treatment should be individualised, considering symptom severity, patient preferences, and potential side effects. Regular monitoring and evaluation are essential for optimal management and improved QoL for individuals with BPH.
References available on request.









Innovative approaches to managing chronic stable angina
Innovative approaches to managing chronic stable angina are essential due to its prevalence as a manifestation of coronary artery disease (CAD), which is characterised by chest pain or discomfort resulting from myocardial ischemia.
DESPITE ADVANCEMENTS IN pharmacological and revascularisation therapies, many patients still experience symptoms, highlighting the need for innovative management strategies.
NOVEL PHARMACOLOGICAL TREATMENTS
Novel pharmacological treatments include isosorbide, a medication primarily used to treat and prevent angina pectoris in patients with coronary heart disease. It works by releasing nitric oxide (NO) to induce vasodilation. The two main forms are isosorbide mononitrate and isosorbide dinitrate, with the latter being FDA-approved for treating angina and congestive heart failure, particularly in African Americans when combined with hydralazine. A comparative analysis suggests that isosorbide-5-mononitrate (5-ISMN) may be more effective and safer than isosorbide dinitrate (ISDN) in real-world management of coronary heart disease, as patients on 5-ISMN showed lower usage of sublingual nitroglycerin. In terms of novel pharmacological treatments, isosorbide remains a cornerstone in angina management. Comparative studies between isosorbide mononitrate and dinitrate suggest a preference for mononitrate due to its lower association with hypotension and less frequent dosing, underscoring the importance of personalised medication strategies based on patient responses and side effects.
Stem cell therapy is emerging as a promising treatment for ischemic heart disease (IHD), which is caused by reduced blood supply to the heart. Mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs) have shown potential therapeutic benefits, with clinical trials indicating improvements in cardiac function, reduced infarct size, and enhanced quality of life for patients with chronic myocardial ischemia. The therapeutic potential of extracellular vesicles, particularly exosomes from MSCs, is also being explored in cardiovascular diseases.
The 2024 ESC Guidelines for managing chronic coronary syndromes (CCS) provide a comprehensive framework for diagnosis and treatment. Key components include a combination of clinical assessments and imaging to confirm obstructive CAD, guideline-directed therapy emphasising patient education and lifestyle modifications, criteria for myocardial revascularisation, long-term management strategies, risk assessment for high-risk patients, and personalised treatment approaches based on individual circumstances. The 2024 ESC Guidelines for managing chronic coronary syndromes advocate for a structured approach to diagnosis, initial therapy, revascularisation, and long-term management. These guidelines emphasise the need for personalised treatment plans that consider individual patient factors, including genetic background, lifestyle, and comorbid conditions, to ensure comprehensive care.
NON-PHARMACOLOGICAL INTERVENTIONS
Non-pharmacological interventions are gaining attention, particularly for patients with refractory angina pectoris (RAP), which affects 5% to 10% of those with stable CAD. Traditional treatments may not adequately address the complex nature of angina. Emerging therapies include viral transfer-based angiogenesis, CD34+/CD133+ cell therapy, coronary sinus reducers, enhanced external counterpulsation, extracorporeal shockwave myocardial revascularisation, and transmyocardial laser revascularisation. The ORBITA-COSMIC trial specifically evaluated the coronary sinus reducer (CSR), which, while not improving myocardial perfusion, effectively reduced angina symptoms, suggesting its potential as an additional treatment for refractory angina.
Key therapies include:
1. CSR: The ORBITA-COSMIC trial demonstrated that CSR significantly reduces angina episodes, although it
does not improve myocardial perfusion, indicating its role primarily as a symptom management tool.
2. Enhanced external counterpulsation (EECP): This therapy employs pneumatic cuffs on the legs to enhance venous return and coronary perfusion, showing potential in reducing the frequency of angina and improving exercise tolerance.
3. Extracorporeal shockwave myocardial revascularisation (ESMR): ESMR promotes angiogenesis and improves myocardial blood flow, representing a novel approach to enhance myocardial perfusion.
4. Transmyocardial laser revascularisation (TMLR) and spinal cord stimulation (SCS): TMLR has yielded mixed results in clinical trials, while SCS has been effective in providing symptomatic relief by modulating pain perception.
PRECISION MEDICINE
Precision medicine plays a crucial role in tailoring treatment strategies based on genetic factors. The ALDH22 genetic variant, common in East Asian populations, reduces the activity of aldehyde dehydrogenase 2 (ALDH2), increasing the risk of CAD, myocardial infarction, and stroke, while also diminishing sensitivity to nitroglycerin. Understanding such genetic susceptibilities is vital for developing personalised management strategies, especially for the growing Asian American population.The role of precision medicine is gaining recognition, particularly regarding genetic factors in managing CAD. The ALDH2*2 genetic variant, common in East Asian populations, affects the metabolism of aldehydes and nitroglycerin, influencing both the risk of coronary events and treatment efficacy. Tailoring therapies to individual genetic profiles can significantly improve treatment outcomes.
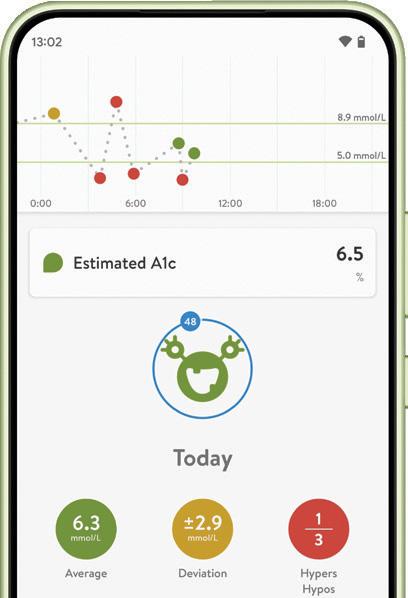
WEARABLE TECHNOLOGY
Wearable technology has evolved significantly, now encompassing a wide range of physiological measurements beyond exercise metrics. These devices

are increasingly utilised for identifying and managing cardiovascular diseases, including hypertension, arrhythmia, heart failure, and CAD. Wearable medical devices, such as ambulatory blood pressure monitors and electrocardiogram (ECG) monitors, along with consumer devices like smartphones and smartwatches, enhance symptom assessment and overall health management. However, there remains some uncertainty regarding their evidence base and appropriate usage in clinical practice.
Advancements in wearable technology have transformed cardiovascular health monitoring and management. Modern devices now offer capabilities beyond simple heart rate monitoring, including ECG, blood pressure measurement, and biochemical markers. Their integration into clinical practice allows for continuous, real-time data collection, facilitating early intervention and personalised care.
CONCLUSION
In conclusion, innovative strategies for managing chronic stable angina encompass a variety of approaches, including nonpharmacological interventions, precision medicine, wearable technology, and novel pharmacological treatments. These advancements, along with comprehensive guidelines and personalised care, hold promise for improving patient outcomes and quality of life. Further research and clinical trials are necessary to validate the efficacy and safety of these emerging therapies, ensuring their integration into chronic stable angina management. In conclusion, the management of chronic stable angina is evolving through the integration of innovative non-pharmacological interventions, precision medicine, wearable technologies, and novel pharmacological treatments. These advancements, along with detailed guidelines, hold the promise of enhancing patient outcomes and quality of life. Ongoing research and clinical trials are essential to validate these new approaches and effectively incorporate them into clinical practice.
Fish oil cuts diabetes complications
Research has shown that regular consumption of fish oil supplements and elevated levels of omega-3 polyunsaturated fatty acids (PUFAs), particularly docosahexaenoic acid (DHA), can lower the risk of vascular complications in individuals with type 2 diabetes (T2D).
Tian et al’s study aimed to explore this association in depth.
Methodology: Fish oil, known for its cardiovascular benefits in the general population, has not been extensively studied in T2D patients, who are at increased risk for vascular diseases. This prospective cohort study analysed data from 20 338 T2D patients (median age 60; 39% women) from the UK Biobank, and an additional 4 874 participants with T2D who had plasma PUFA data. Fish oil use was evaluated through an electronic questionnaire administered between 2006 and 2010, while blood samples for omega-3 fatty acids were collected from June 2019 to April 2020. The study focused on various diabetic complications: macrovascular (coronary heart disease, heart failure, peripheral artery disease, and stroke) and microvascular (diabetic kidney disease, retinopathy, and neuropathy).
Key findings: Over a median follow-up period of 13.2 years, 5 396 participants developed macrovascular complications and 4 868 experienced microvascular complications. Fish oil supplementation was linked to a 10% reduction in the risk of composite macrovascular complications (adjusted hazard ratio [HR], 0.90; 95% CI, 0.85-0.97) and an 11% reduction in composite microvascular complications (HR, 0.89; 95% CI, 0.83-0.95). Notably, this association did not extend to heart failure and stroke. Higher plasma levels of total n-3 PUFAs, particularly DHA, were associated with reduced risks of both macrovascular and microvascular complications in a nonlinear dose-response manner (P overall <0.05; P for nonlinearity <0.05). These benefits were also linked to regular fish oil supplementation. The study identified seven biomarkers related to lipid profiles and inflammation, which accounted for 54% and 63% of the association between plasma DHA levels and reduced risk for macrovascular complications and coronary heart disease, respectively.
Practical implications: According to the study, regular fish oil consumption and higher plasma levels of omega-3 PUFAs, especially DHA, are associated with decreased risks of macrovascular and microvascular complications in T2D patients. The positive effects of plasma DHA on diabetic complications were partially mediated through improvements in lipid profiles and inflammation biomarkers.
Limitations: As an observational study, it
cannot establish causality. The research lacked detailed information on the dosage, composition, and duration of fish oil use, focusing solely on total omega-3 PUFAs
and DHA.
REFERENCE
Oil, Plasma n-3 PUFAs, and Risk of Macro- and Microvascular Complications Among Individuals With Type 2 Diabetes, The Journal of Clinical Endocrinology & Metabolism, 2024;,dgae482, https://doi.org/10.1210/ clinem/dgae482.





By Dr Mothomang
A Beyond the clinic, nurturing wellness through the six pillars of lifestyle medicine
S A YOUNG DOCTOR in Soweto, I witnessed firsthand the devastating impact of chronic diseases on my patients. My heart ached each time I prescribed medication, knowing that many of these conditions could be alleviated or even prevented through lifestyle interventions. The statistics for chronic illnesses are scary. According to the World Health Organisation1, noncommunicable diseases (NCDs) kill 41 million people each year, equivalent to 74% of all deaths globally. Each year, 17 million people die from an NCD before age 70; 86% of these premature deaths occur in low- and middle-income countries. These staggering statistics underscore the urgent need for effective interventions to address the global burden of NCDs.
This experience ignited a passion for holistic wellness and led me to explore the power of lifestyle medicine (LM), an evidence-based approach that emphasises the importance of adopting healthy behaviours to prevent and manage diseases. It is grounded in the six pillars of lifestyle medicine2 – nutrition, exercise, healthy relationships, stress management, sleep, and substance avoidance. These pillars form the foundation of a balanced and fulfilling life, and by nurturing them, we can significantly enhance our overall health.
One of the key principles of lifestyle medicine is the concept of harm reduction, a patient centred strategy used in medicine and social policy to minimise harm from hazardous behaviours or practices that cannot be completely avoided or prevented.
This approach recognises that it may not always be feasible to eliminate unhealthy behaviours entirely, but it is possible to minimise their negative consequences. By focusing on gradual improvements and sustainable changes, we can effectively reduce the risks associated with harmful habits. Lifestyle medicine often advocates for setting realistic, small behavioural goals that focus on progress over perfection.
This reduces the likelihood of failure and discouragement, which can be harmful to mental and physical health, as cited in Foundations of Lifestyle Medicine and its Evolution3
Although LM may be thought of as a newer medical speciality, its principles have roots that extend back for centuries. Hippocrates, an ancient Greek philosopher, and physician often thought of as the father of medicine, famously said “in order to keep well, one should simply avoid too much food, too little toil.” Around the same time, but several thousand miles to the East, the Chinese philosopher Confucius was also recognising the impact that moderation in diet and alcohol, along with persistent practices of mindfulness and meditation, had on the quality of life.3
1. NUTRITION AND REDISCOVERING OUR ROOTS AND THE POWER OF TRADITIONAL AFRICAN DIETS
Likewise, as Africans, we too have a rich heritage of balanced lifestyle living including healthy eating practices that have been passed down through generations. By returning to our roots and embracing traditional African diets, we can tap into a wealth of nutritional wisdom. These diets often emphasise whole, unprocessed foods, plant-based proteins, and healthy fats, which are essential for optimal health.
2. WALKING THE TALK AND INTEGRATING MOVEMENT INTO DAILY LIFE
The word exercise sounds laborious and can be intimidating to many people as is the idea of the gym. Our ancestors were accustomed to active lifestyles that involved walking, gardening, and working the land. By incorporating similar activities into our daily routines, we can reap the benefits of regular exercise. If you are working from home, make it a habit to get up every hour to walk around, grab a glass or water or tea, and walk outside. Those 100 or 200 steps
add up during the day. If you are at the office, take the stairs and not the lift or park in the furthest parking and walk.
3. BUILDING HEALTHY RELATIONSHIPS AND THE IMPORTANCE OF SOCIAL CONNECTION
Africans have a strong tradition of community and togetherness. By fostering strong social connections and building supportive relationships, we can enhance our emotional and mental wellbeing. Strengthening and maintaining relationships and connections with others brings meaning and purpose to life. Studies show that isolation is associated with increased mortality. Community-based activities, social clubs and events can provide opportunities for social interaction and a sense of belonging. Encouraging people to build strong social networks and relationships can mitigate the harm caused by loneliness and isolation, which are linked to various chronic health conditions.
4. STRESS MANAGEMENT AND FINDING CALM IN A CHAOTIC WORLD
Traditional African cultures often emphasised mindfulness and meditation as ways to cope with stress and maintain inner peace. By incorporating these practices into our modern lives, we can develop effective coping mechanisms and reduce the harmful effects of stress. Reframing negative thoughts can reduce the harm caused by chronic stress, which can contribute to various health problems.
5. SLEEP RESTORES AND RENEWS THE BODY FOR OPTIMAL HEALTH
Adequate sleep is essential for physical and mental health. Prioritising sleep and creating a sleep-conducive environment can help improve our overall well-being. Many of us brag about sleeping less as if it’s a badge of honour to show how hardworking we are but this comes at a cost to our overall

wellbeing. Make small, achievable changes in their sleep habits (eg, setting regular sleep times, reducing screen time before bed) to improve overall sleep quality, reducing harm from sleep deprivation. During sleep, our bodies are working to support healthy brain function and maintain our physical health.
6. SUBSTANCE ABUSE AND OVERCOMING ADDICTION AND EMBRACING WELLNESS
Many people resort to using vices like substance abuse including drinking, smoking, binge eating or drugs as coping mechanisms because the five pillars of wellness are out of sync. This can have devastating consequences on individuals, families, and communities. By making healthy choices and seeking support when needed, we can break free from addiction and embrace a healthier lifestyle. For those who struggle with substances like alcohol or tobacco, lifestyle medicine often focuses on reducing intake rather than complete abstinence as a first step. For smokers tobacco harm reduction is key – switching to better alternatives like non-combustible products like oral nicotine and heat ‘not burn’ products are less harmful than continuing to smoke cigarettes.
Embracing lifestyle medicine is more than a choice – it's a transformative shift in how we live. By reconnecting with our roots, embracing community, and fostering family structures that support open dialogue and healthy eating, we can fend off chronic diseases, elevate our quality of life, and unlock our full potential. The time to take control of our health is now – let's seize it, one mindful step at a time.
REFERENCES
1. https://www.who.int/news-room/fact-sheets/detail/ noncommunicable-diseases
2. Home - American College of Lifestyle Medicine
3. Foundations of Lifestyle Medicine and its Evolution - PMC (nih.gov)
A Navigating spring’s allergic rhinitis
Spring is a time of flowering and pollination, which can be frustrating for those with seasonal allergies. These allergies can cause nasal symptoms, known as allergic rhinitis, or chest symptoms like cough and wheeze in those with asthma.
LLERGIC RHINITIS is an allergic reaction of the nasal mucosa to environmental allergens, leading to the release of chemical messengers inside the nose and surrounding tissue, causing swelling, itch, sneezing, and rhinorrhoea (copious mucus).
Allergens can be present all year round (such as house dust mite, mould, and animal dander) or seasonal (such as grass and tree pollens). In South Africa, tree pollen levels peak from August to October, and grass pollen season spans from October to March. Climate change may intensify and prolong pollen seasons in the future.
DIAGNOSIS OF SEASONAL ALLERGIC RHINITIS
If allergic rhinitis is suspected, it is important to rule out other conditions. Viral colds and allergic rhinitis can mimic each other, although colds may cause general unwellness. Correct testing for allergic rhinitis is crucial. Environmental allergies can be checked by a skin prick test or blood test.
Skin prick tests involve gentle pricks on the forearm, introducing a bit of allergen into the top layer of the skin. A weal and flare will form if the patient is allergic. Results are accurate and can be assessed within 15 minutes. Blood tests can check for various environmental allergens and can be done even if someone is on antihistamines. Results take between one and a few days to come back.
MANAGEMENT OF SEASONAL ALLERGIC RHINITIS
Management includes avoiding the allergen as much as possible, such as staying indoors during peak pollen times and avoiding freshly cut grass. Medications are often needed, depending on the dominant symptoms. Nasal corticosteroid sprays are the best overall treatment, with minimal absorption into the system, making them safer than steroid pills or injections. Nose bleeds are a potential side effect if sprays are angled incorrectly.
Antihistamines may help if itch and sneeze are predominant. Newer generation antihistamines are preferred due to their minimal sedation. Medications should be taken daily during the allergy season for best results. If asthmatic, the controller asthma pump needs to be used daily.
If basic treatment is inadequate, specialist referral for further management options is advised. Desensitisation, or immunotherapy, involves giving tiny amounts of the allergen regularly for several years to help the immune system tolerate it. The most common form of immunotherapy for seasonal allergies is sublingual drops,
given daily under the tongue for three or more years. Immunotherapy is generally safe and effective but expensive in South Africa.
CLOSING THOUGHTS
Seasonal allergies can be accurately
diagnosed and effectively managed.
Self-diagnosis is discouraged, as accurate diagnosis and relevant allergens lead to optimal treatment planning.
Poorly managed seasonal allergies can cause headaches, concentration difficulties, and complications such as asthma, ear infections, and sinusitis. It is best to get the right diagnosis and an effective management plan. Specialist allergy centres are available to optimise diagnosis and treatment.










Community influencers Unsung heroes of HIV prevention for young women
Dr Ziyanda Makaba, Clinical Specialist for HIV and Paediatrics at BroadReach Health Development, highlights that women and girls accounted for over 60% of new HIV infections in sub-Saharan Africa in 2022.

SIX OUT OF seven new infections among 15-19-year-olds in the region are among girls. However, initiatives like the USAID-led DREAMS programme are making a difference. DREAMS stands for Determined, Resilient, Empowered, AIDSfree, Mentored, and Safe, and it supports high-risk young women and girls across the country.
“We’ve moved away from a one-sizefits-all approach to HIV prevention and care, adopting a human, tailored, and caring approach to reduce HIV transmissions by 2030. Community ambassadors are making all the difference. We have incredible people in our communities who enable their peers, especially teenage girls, to protect
themselves and their loved ones from HIV,” says Goodman Ntshangase, BroadReach Health Development’s Acting District Director of Gert Sibande in Mpumalanga. This is one of the districts where BroadReach delivers public healthcare in partnership with USAID and the Department of Health.
“We call these community ambassadors ‘Influencers for Good’. They encourage their friends and neighbours to take preventative measures for HIV, including pre-exposure PrEP, post-exposure PEP, and condoms. They also encourage their peers to get tested for HIV and start taking antiretrovirals (ARVs) if they test positive. This is very helpful for preventing
mother-to-child transmission, as mothers taking ARVs can protect their babies from becoming HIV positive,” says Ntshangase.
THE POWER OF FIGHTING STIGMA
Dr Makaba explains that the local ‘Influencers for Good’ work within the Differentiated Models of Care framework.
“This means you look at the community to identify who is most vulnerable to HIV and reach out to them in ways that empower them in their unique contexts. There is no judgment, patronisation, or shame. These nano influencers make it possible for more adolescent girls to take steps to live happy, healthy lives unhampered by HIV.”
These influencers take client-centred approaches to helping people depending on their HIV status. “For someone living with HIV, the goal is to get them to take their ARVs every day so that they can become ‘virally suppressed’, meaning their viral count is so low that it becomes virtually undetectable and untransmittable. Suppose someone is HIV negative but in a relationship with someone who is HIV positive or injecting drugs. In that case, they might be encouraged to take preventative PrEP – a medication that if taken 7 days before HIV exposure, can prevent the HIV-
negative person from getting HIV,” says Dr Makaba.
PROOF
IN
THE PUDDING: HIV NUMBERS ARE IMPROVING IN MPUMALANGA
The data shows that influencer interventions, coupled with other community health interventions at clinics, have resulted in significant improvements in HIV rates. In the Nkangala and the Gert Sibande districts in Mpumalanga, where BroadReach and their community brigades have been working for five years, the numbers speak for themselves.
In 2018, 1 520 people were initiated on PrEP, and that number has reached 30,094 in the last year. “This tells you our outreaches are working and we’re convincing a lot more people to get onto life-saving preventative medications,” says Dr Makaba. Mother-to-child (perinatal) transmissions have also halved, thanks to more mothers taking ARVs today than five years ago. “In Year One, 251 HIV+ infants needed ARVs and now we have half that at 124 infants. That means the ARVs that more mums are taking while pregnant are effectively protecting babies.”
A 6 key drivers of the HIV epidemic
The Human Sciences Research Council (HSRC) recently released the key findings of the Sixth South African HIV Prevalence, Incidence, and Behaviour Survey (SABSSM VI) for Gauteng Province (GP).
ccording to the overall principal investigator of the study, the HSRC’s Prof Khangelani Zuma, the HIV prevalence peaked at 32.2% among those aged 50–54 years in 2022.
Here are six issues that were identified as being key risk factors influencing the spread of HIV.
SEXUAL DEBUT BEFORE THE AGE OF 15 YEARS
Regarding the key drivers of the HIV pandemic, Prof Zuma noted that, in Gauteng, there was a change in the proportion of adolescents and youth aged 15–24 years who reported having sex before the age of 15 years in 2017 (14.8%) compared to 2022 (13.2%).
In 2022, the percentage of adolescents and youth aged 15-24 who had their sexual debut before the age of 15 was higher among males (17.8%) than females (7.9%). The prevalence was lowest in Ekurhuleni (9.5%) and highest in West Rand (18.1%),
followed by City of Johannesburg (14.1%)
MULTIPLE SEXUAL PARTNERS
The survey revealed that in Gauteng, 7.8% of people aged 15 years and older reported having multiple sexual partners in 2022 compared to 12.8% in 2017. The proportion of people aged 15 years and older who reported having multiple sexual partners was fourfold higher among males (12.3%) compared to females (3.1%), and twofold higher among those aged 15-24 years (17.1%) compared to those aged 15-49 years (8.6%). The proportion who reported having multiple sexual partners was highest in City of Tshwane (13.7%) and lowest in West Rand (2.9%).
CONDOM USE WITH THE MOST RECENT SEXUAL PARTNER
Regarding condom use, the survey found that, in Gauteng, 30.3% reported using a condom with the most recent sexual partner in 2022 compared to 36.3% in 2017,
representing a decline of six percentage points. Condom use with the most recent sexual partner among people aged 15 years and older was lower among those aged 25–49 years (29.6%) compared to other age groups, females compared to males (27,6% vs 32.9%), and among those residing in rural formal or farm areas (18.9%) compared to other localities. Condom use with the most recent sexual partner among people aged 15 years and older ranged from 24.7% in City of Tshwane to 37.9% in West Rand. Nationally, more than 70% of individuals aged 15 years and older had never or sometimes used a condom with their most recent sexual partner. In Gauteng, a higher proportion (53.8%) also reported that they never used a condom with their most recent sexual partner. Only 4.7% reported that they used a condom almost every time.
Consistent condom use with the most recent sexual partner among people aged 15 years in the province was higher among
adolescents and youth aged 15-24 years (32.1%) compared to those aged 25-49 years (19.3%). However, over 70% of those aged 25-49 years reported only using a condom sometimes or never. Consistent condom use with the most recent sexual partner among people aged 15 years and older was highest in Sedibeng (23.4%) and lowest in City of Tshwane (17.0%).
MALE CIRCUMCISION
In Gauteng, self-reported male circumcision decreased from 64.4% in 2017 to 64.0% in 2022. In 2022, self-reported male circumcision in the province was lower among those aged 25-49 years (67.4%) and those residing in rural formal or farm areas (42.2%), and highest among those aged 25-34 years (71.9%).
Regionally, self-reported circumcision among males aged 15-24 years ranged from 63.3% in Ekurhuleni to 81.1% in Sedibeng. Among males aged 25-34 years, it ranged

from 70.1% in the City of Johannesburg to 84.7% in Sedibeng. Among males aged 2549 years, it ranged from 66.4% in City of Tshwane to 73.9% in West Rand. Gauteng had the fourth highest proportion of medical circumcisions in the country at 70.6%.
The survey further revealed that willingness for voluntary medical male circumcision among uncircumcised men in Gauteng was highest among adolescents and youth aged 15-24 years (39.6%). Male circumcision among children aged 14 years and younger in Gauteng increased with age from 4.5% among those aged 0-4 years to 52.5% among children aged 12-14 years. Male circumcision among children aged 14 years and younger was lowest in the West Rand (6.2%).
AWARENESS OF HIV TESTING SITES
Awareness of HIV testing sites is critical for accessing HIV testing services. In 2022, awareness of HIV testing sites by selected demographic characteristics among people aged 15 years and older was generally high. However, awareness was lower among adults aged 50 years and older (88.3%) compared to those aged 25-49 years (98.0%).
Access to HIV testing sites is important for scaling up the utilisation of HIV testing services. In Gauteng, a higher proportion of people aged 15 years and older
KEY RECOMMENDATIONS
The survey recommends key actions to address the HIV epidemic as a public health threat in South Africa by 2030. These include a long-term strategy to care for individuals in an ageing HIV epidemic, as well as addressing health inequalities and combining prevention strategies to address specific HIV prevalence and treatment rates of concern at district levels.
Prof Zuma recommends enhancing public awareness of effective HIV prevention measures, such as regular HIV testing, condom use and PrEP. He also emphasised a continued focus on increasing voluntary medical male circumcision uptake among uncircumcised males aged 15 years and older.
“We also recommend enhancing prevention efforts targeted at groups that are disproportionately affected by the drivers of HIV infection, such as women and young people,” concluded Prof Zuma.
The HSRC conducted the survey in partnership with the US Centers for Disease Control and Prevention (CDC), the South African Medical Research Council (SAMRC), the University of Cape Town (UCT), and the National Institute for Communicable Diseases (NICD).
accessed public clinics or doctors for HIV testing (53.5%).
AWARENESS AND UPTAKE OF PRE-EXPOSURE PROPHYLAXIS (PREP)
Overall, in 2022, 33.3% of sexually active adults aged 15 years and older had heard of
PrEP, and 4.6% of them had taken PrEP. Of those who had taken PrEP, 1.5% were taking PrEP at the time of the survey.
More females (39.1%) compared to males (27.3%) had heard of PrEP and were willing to use PrEP to prevent HIV (68.7% versus 58.9%). Compared to other age groups, more adolescents and youth aged
15-24 years had heard of PrEP (41.2%). Of those, 2.2% were currently taking it and 67.4% were willing to take it. Overall, 65.0% of respondents who had heard of PrEP but had never taken PrEP, reported they would consider taking it to prevent HIV infection. Current use of PrEP was highest in City of Johannesburg (1.7%).


Management of non-specific low back pain: A clinical update
Low back pain is a prevalent condition affecting approximately 9% of adults globally and is a leading cause of disability.
HIS CLINICAL UPDATE focuses on the management of non-specific low back pain, emphasising the limited effectiveness and significant risks associated with commonly prescribed analgesics, including opioids and benzodiazepines. Non-steroidal antiinflammatory drugs (NSAIDs) may offer slight benefits for short-term relief, but their gastrointestinal risks must be carefully considered.
ACUTE vs CHRONIC LOW BACK PAIN
Acute low back pain typically improves within a few weeks without treatment.
In contrast, chronic low back pain, which persists for over three months, requires a focus on non-pharmacological strategies to enhance function and address psychosocial factors. Current guidelines advocate for non-drug treatments and cautious use of analgesics, encouraging patients to remain active, avoid prolonged bed rest, and utilise self-management techniques such as heat therapy.
EFFICACY OF ANALGESICS
Paracetamol (acetaminophen)
- No significant effect over placebo for both acute and chronic low back pain.
- Systematic review of 13 RCTs showed a mean difference in pain score of −0.5.
- No increased risk of harms in low back pain trials, but potential for abnormal liver function tests in osteoarthritis or low back pain trials.
- Observational data show a dosedependent increase in risk of cardiovascular, gastrointestinal, and renal harms, potentially confounded by NSAID use.
Non-steroidal anti-inflammatories
- Moderate certainty evidence of small benefit for acute low back pain (mean difference in pain intensity −0.9).
- Increased risk of gastrointestinal harms (risk ratio of 2.5).
- Low certainty evidence of small benefits for chronic low back pain (mean difference −0.7).
- Increased adverse events with longterm use, including gastrointestinal, cardiovascular, and renal harms.
Antidepressants
- No data for acute low back pain.
- Moderate certainty evidence that serotonin-norepinephrine reuptake inhibitors (eg, duloxetine) may have a small effect for chronic low back pain.
- Low certainty evidence that tricyclic antidepressants are ineffective.
- Associated with nausea, weight gain, sexual dysfunction, and sleep problems in
broader populations.
Opioids
- Strong evidence of no effect for acute low back pain and worse long-term outcomes.
- Moderate certainty evidence of a small effect for chronic low back pain (mean difference −1.0).
- Not recommended for chronic pain due to risks of dependence, misuse, overdose, and tolerance.
Anticonvulsants
- No data for acute low back pain.
- High certainty evidence of no effect for chronic low back pain (mean difference 0.0).
- Increased risk of harms, including drowsiness, somnolence, dizziness, and nausea.
Benzodiazepines
- Small trials from the 1970s to 1990s report some effect, but other studies indicate no meaningful analgesic properties.
- A 2017 RCT found no improvement in functional outcomes or pain with diazepam addition.
- Associated with increased falls, cognitive impairment, and risk of addiction.
Non-benzodiazepine muscle relaxants
- Low and very low certainty evidence of small benefits for both acute and chronic low back pain (mean difference −0.8).
- Increased risk of harms, primarily sedation.
Oral corticosteroids
- Limited evidence suggests they may not be effective for acute or chronic low back pain.
- May not cause harm in short courses.
Non-pharmacological strategies
Non-pharmacological strategies are essential in managing both acute and chronic low back pain. These strategies focus on improving function, reducing pain, and addressing psychosocial factors that may contribute to the persistence of pain. Here are some key non-pharmacological approaches:
1. Physical therapy and exercise: Engaging in regular physical activity and exercise is crucial for managing low back pain. Physical therapy can help improve flexibility, strength, and posture, which are essential for reducing pain and preventing future episodes. Specific exercises, such as stretching, strengthening, and aerobic activities, can be tailored to the individual's needs and abilities.
2. Cognitive behavioural therapy (CBT): CBT is a psychological intervention that

helps patients manage pain by changing negative thought patterns and behaviours. It can be particularly effective for chronic low back pain, as it addresses the emotional and psychological aspects of pain, helping patients develop coping strategies and improve their overall quality of life.
3. Mindfulness and relaxation techniques: Mindfulness-based stress reduction (MBSR) and other relaxation techniques, such as deep breathing, progressive muscle relaxation, and guided imagery, can help reduce stress and tension, which may exacerbate low back pain. These techniques promote relaxation and improve the patient's ability to manage pain.
4. Manual therapy: Manual therapy, including chiropractic adjustments, massage, and spinal manipulation, can provide short-term relief for some patients with low back pain. These hands-on techniques aim to improve mobility, reduce muscle tension, and alleviate pain.
5. Acupuncture: Acupuncture, a traditional Chinese medicine practice, involves inserting thin needles into specific points on the body. Some studies suggest that acupuncture can provide pain relief and improve function in patients with low back pain, although the evidence is mixed.
6. Education and self-management: Educating patients about low back pain, its causes, and management strategies is crucial for empowering them to take an active role in their care. Self-management techniques, such as using heat or cold therapy, maintaining good posture, and avoiding activities that exacerbate pain, can help patients manage their symptoms effectively.
7. Ergonomic modifications: Making ergonomic adjustments in the workplace and at home can help reduce the risk of low back pain. This may include using supportive chairs, adjusting the height of workstations, and ensuring proper lifting techniques to prevent strain on the back.
8. Weight management: Maintaining a healthy weight can reduce the strain on the lower back and decrease the risk of developing low back pain. A balanced diet and regular exercise are essential components of weight management.
9. Sleep hygiene: Poor sleep quality can exacerbate pain and reduce the body's ability to heal. Encouraging good sleep hygiene practices, such as maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime, can help improve sleep quality and reduce pain.
10. Multidisciplinary approach: A multidisciplinary approach to managing low back pain involves a team of healthcare professionals, including physicians, physical therapists, psychologists, and occupational therapists, working together to develop a comprehensive treatment plan. This approach ensures that all aspects of the patient's pain are addressed, leading to better outcomes.
CONCLUSION
The management of low back pain is complex and necessitates tailored care strategies for patients. This update highlights the significance of non-invasive treatments, the limited efficacy of many analgesics, and the importance of individualised patient care. Clinicians should prioritise non-pharmacological strategies and engage in thorough discussions with patients about their treatment options. By adopting a holistic approach that includes physical therapy, psychological interventions, and lifestyle modifications, healthcare providers can help patients manage their low back pain more effectively and improve their overall quality of life.
REFERENCE
Jones C, Underwood M, Chou R et al. Analgesia for non-specific low back pain. BMJ 2024;385:e080064. http://dx.doi.org/10.1136/bmj-2024-080064.
Diclofenac potassium 50 mg
K-Fenak OTC contains diclofenac potassium, which dissolves and absorbs faster than diclofenac sodium.2
INDICATIONS1
For the treatment of fever or mild to moderate pain of inflammatory origin, for a maximum treatment period of 5 days.
The emergency treatment of acute gout attacks, for a maximum treatment period of 3 days.

Anti-Inflammatory1
Pain, Swelling & Inflammation1
S2 Reg. No. A38/3.1/0651. K-Fenak OTC. Each film-coated tablet contains Diclofenac potassium 50 mg. For full prescribing information, refer to the Professional Information approved by the medicines regulatory authority.
References:
1. Professional Information: K-Fenak OTC (Film-coated tablets).
2.Chuasuwan, B. et al. Biowaiver monographs for immediate release solid oral dosage forms: Diclofenac sodium and diclofenac potassium. Journal of Pharmaceutical Sciences 98(4) 1206–1219 (2009).
CIPLA MEDPRO (PTY) LTD. Co. Reg. No. 1995/004182/07. Building 9, Parc du Cap, Mispel Street, Bellville, 7530, RSA. Website: www.cipla.co.za. Customer Care: 080 222 6662. [1453996205]
Epigenetics in dermatology
At the recent Combined Dermatology Congress of South Africa, held in Gqeberha, Dr Hassan Galadari, Associate Professor of Dermatology at the United Arab Emirates University, presented a compelling session on epigenetics.
DR GALADARI HIGHLIGHTED
the significant role of epigenetic mechanisms in skin health and disease. He emphasised how understanding these processes can lead to innovative treatments for various dermatological conditions. The presentation underscored the potential of epigenetics to revolutionise dermatology, offering new avenues for research and therapy.
INTRODUCTION TO EPIGENETICS
Epigenetics refers to the study of heritable changes in gene expression that do not involve alterations to the underlying DNA sequence. These changes can be influenced by various factors, including environmental stimuli, lifestyle choices, and disease states. In dermatology, epigenetics plays a crucial role in understanding how skin cells respond to different internal and external factors, leading to various skin conditions and diseases.
MECHANISMS OF EPIGENETIC REGULATION
Dr Galadari's presentation looked at the primary mechanisms of epigenetic regulation, which include DNA methylation, histone modification, and non-coding RNA molecules. Each of these mechanisms can influence gene expression in skin cells, contributing to the development and progression of dermatological conditions.
1. DNA methylation: This process involves the addition of a methyl group to the DNA molecule, typically at cytosine bases. DNA methylation can suppress gene expression by preventing the binding of transcription factors to the DNA. In the context of dermatology, abnormal DNA methylation patterns have been associated with various skin diseases, including psoriasis and melanoma.
2. Histone modification: Histones are proteins around which DNA is wrapped, forming a structure called chromatin. The modification of histones through processes such as acetylation, methylation, and phosphorylation can alter the accessibility of DNA to transcription factors, thereby regulating gene expression. Histone modifications have been implicated in the regulation of skin cell proliferation, differentiation, and response to environmental stressors.
3. Non-coding RNA molecules: These RNA molecules do not code for proteins but can regulate gene expression at the transcriptional and post-transcriptional levels. MicroRNAs (miRNAs) and long non-coding RNAs (lncRNAs) are two types of non-coding RNAs that have been extensively studied in dermatology. They play critical roles in skin development, wound healing, and the pathogenesis

Understandingthese epigeneticchanges canprovideinsights into the mechanisms of melanoma developmentand identifynovel therapeutictargets
of skin diseases.
EPIGENETICS AND SKIN DISEASES
Dr Galadari emphasised the importance of epigenetic research in understanding the pathogenesis of various skin diseases. By studying the epigenetic changes associated with these conditions, researchers can identify potential biomarkers for early diagnosis and develop targeted therapies to modulate gene expression.
1. Psoriasis: Psoriasis is a chronic inflammatory skin disease characterised by hyperproliferation of keratinocytes and immune cell infiltration. Epigenetic studies have revealed abnormal DNA methylation and histone modification patterns in psoriatic skin lesions. These findings suggest that epigenetic dysregulation contributes to the pathogenesis of psoriasis and may serve as a target for therapeutic intervention.
2. Atopic dermatitis: Atopic dermatitis (AD) is a common inflammatory skin condition associated with genetic and environmental factors. Epigenetic research has identified altered DNA methylation and miRNA expression profiles in AD patients. These epigenetic changes are thought to influence immune responses and skin barrier function, contributing to the development and severity of AD.
3. Melanoma: Melanoma is a highly aggressive form of skin cancer arising
from melanocytes. Epigenetic alterations, including DNA methylation and histone modifications, have been implicated in melanoma progression and resistance to therapy. Understanding these epigenetic changes can provide insights into the mechanisms of melanoma development and identify novel therapeutic targets.
EPIGENETIC THERAPIES IN DERMATOLOGY
One of the most exciting aspects of Dr Galadari's presentation was the discussion of epigenetic therapies in dermatology. These therapies aim to reverse or modulate the epigenetic changes associated with skin diseases, offering a novel approach to treatment.
1. DNA methylation inhibitors: Drugs that inhibit DNA methylation, such as 5-azacytidine and decitabine, have shown promise in preclinical studies for the treatment of skin diseases. By demethylating specific genes, these inhibitors can restore normal gene expression and improve disease outcomes.
2. Histone deacetylase inhibitors: Histone deacetylase (HDAC) inhibitors, such as vorinostat and romidepsin, have been investigated for their potential in treating skin cancers and inflammatory skin conditions. HDAC inhibitors can alter histone acetylation patterns, leading to changes in gene expression that promote cell
differentiation and apoptosis.
3. miRNA-based therapies: miRNA-based therapies involve the use of synthetic miRNAs or miRNA inhibitors to modulate gene expression. These therapies have shown potential in preclinical models of skin diseases, including psoriasis and melanoma. By targeting specific miRNAs, researchers can influence the expression of multiple genes involved in disease pathogenesis.
FUTURE DIRECTIONS IN EPIGENETIC
RESEARCH
Dr Galadari concluded his presentation by highlighting the future directions in epigenetic research in dermatology. He emphasised the need for further studies to elucidate the complex interactions between genetic, epigenetic, and environmental factors in skin diseases. Additionally, he called for the development of advanced technologies to analyse epigenetic changes at single-cell resolution, which could provide deeper insights into the heterogeneity of skin diseases. By understanding the epigenetic mechanisms underlying skin diseases, researchers and clinicians can develop innovative therapies to improve patient outcomes.
The potential of epigenetic research to revolutionise dermatology is immense, offering new avenues for diagnosis, treatment, and prevention of skin conditions.


































































Cardiovascular Diseases in South Africa: Understanding Prevention, Treatment, and Management


Cardiovascular diseases (CVDs) are a group of disorders of the heart and blood vessels that are the leading cause of death worldwide.1,2 CVDs are grouped into four categories: coronary artery disease, cerebrovascular disease, peripheral artery disease, and aortic atherosclerosis.3 An estimated 17,9 million people died from CVDs in 2019, representing 32 % of all global deaths.2 Of these deaths, 85 % were caused by myocardial infarction (MI) and stroke.2 MIs and strokes are primarily caused by obstructed blood flow to the heart or brain, often as a result of atherosclerosis.2
Cardiovascular Disease and Stroke in South Africa
CVDs are the leading cause of death in South Africa, accounting for 18,9 % of nationwide deaths.4 In fact, more South Africans die of CVDs than all cancers combined.5 Strokes are the second most common cause of death, and it is estimated that 75 000 South Africans experience a stroke each year.6 Moreover, strokes are the primary cause of disability among South African adults, imposing significant burdens on both social and healthcare services.6
Cardiovascular Disease Risk Factors
No single risk factor has been identified to be responsible for causing CVDs.7 Multiple interrelated factors seem responsible for its development.7 Major, modifiable risk factors include hypertension, hypercholesterolaemia, smoking, obesity, diabetes, physical inactivity, unhealthy diet, and stress.7 CVD risk increases with age, with men exhibiting a greater risk than women.7
Stroke Risk Factors
Modifiable risk factors for stroke include hypertension, hypercholesterolaemia, smoking, obesity, physical inactivity, and alcohol abuse.8 Hypertension is the most common modifiable risk factor for stroke.9
Cardiovascular Disease Prevention
It is essential to detect CVD and CVD risk factors as early as possible to implement effective treatment and preventative strategies.7 The most significant way to prevent CVD is to promote a healthy lifestyle.10 Adult patients should be advised to engage in at least 150 minutes of accumulated moderate-intensity physical activity per week or 75 minutes of accumulated vigorous-intensity physical activity per week.10 Individuals with co-morbid diseases, such as diabetes, should be advised to manage these conditions through their lifestyle or with medication if necessary.10 Adult patients who are 40 to 75 years of age should be routinely assessed for traditional cardiovascular risk factors.10

Stroke Prevention
It is critical to recognise a stroke early and treat it rapidly to prevent or minimise morbidity and mortality.9 According to the National Institute of Neurological Disorders and Stroke (NINDS), individuals who have had a stroke should be admitted to the hospital as soon as possible to receive thrombolytic therapy if appropriate, for better survival and overall outcomes.11 Strokes can be prevented by advising patients to make behavioural and lifestyle changes that address modifiable risk factors, undergoing regular stroke risk assessment, and prescribing medication if necessary.10,12

Global Initiatives
World Heart Day – observed annually on 29 September – serves as a global initiative aimed at raising awareness about cardiovascular health and encouraging individuals, communities, and governments to take proactive measures against heart diseases.13 This initiative emphasises lifestyle modifications to reduce the prevalence of CVDs worldwide.13
Pharmacological Treatment
Aspirin is one of the oldest and most widely used medical treatments worldwide.14,15 Previously used for its anti-inflammatory properties, aspirin is now used as an anti-platelet, which reduces the risk of MIs and strokes by supressing platelet aggregation and preventing atherothrombotic events in patients at risk of coronary and cerebrovascular events or minimising their severity should these events occur.14-17
Current clinical guidelines indicate that low-dose aspirin can be used to reduce the risk of MIs in patients with unstable angina or who have had a previous MIs as well as reduce the risk of recurrent transient ischaemic attacks or strokes in men who have had disrupted blood flow to the brain due to fibrin platelet emboli.10,15,17,18 When it comes to providing cardio-protection, Ecotrin® is the #1 low-dose aspirin prescribed by South African cardiologists and physicians and is a cost-effective option that balances efficacy and


1. Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol 2019;74(20):2529-32.
2. World Health Organisation. Cardiovascular diseases (CVDs) [online]. 2021, Jun 11 [cited 2024, Feb 5]. Retrieved from: URL: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
3. Edgardo Olvera Lopez, Jan A. Cardiovascular Disease [Internet]. National Library of Medicine. StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535419/.
4. Stats SA. Mortality and causes of death in South Africa: Findings from death notification [pdf]. 2018.
5. Ntusi NA. Cardiovascular medicine in South Africa. SA Heart 2022;19(1):2-4.
6. van Niekerk SM, Kamalakannan S, Inglis-Jassiem G, Charumbira MY, Fernandes S, Webster J, et al. Towards universal health coverage for people with stroke in South Africa: a scoping review. BMJ 2021;11(11):e049988.
7. Hajar R. Risk factors for coronary artery disease: historical perspectives. Heart Views 2017;18(3):109.
8. Matizirofa L, Ranganai E. An analysis of recent stroke cases in South Africa: Trend, seasonality and predictors. S Afr Med J 2020;110(2):92-9.
9. Khaku AS, Tadi P. Cerebrovascular Disease [online]. 2022, Aug 08 [cited 2024 Feb 5] Retrieved from: URL: https://www.ncbi.nlm.nih.gov/books/NBK430927/.
10. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;140(11):e596-646.
11. Yang H, Huang X, Yang C, Zhu S, Chen X, Zhang M, et al. Time window for acute stroke management: a cross-sectional study among community healthcare practitioners in primary care. Int J Gen Med 2022:4483-93.
12. Visseren FL, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies with the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J 2021;42(34):3227-337.
13. World Heart Federation. About World Heart Day [Internet]. World Heart Day. [cited 2024 Feb 5]. Available from: https://world-heart-federation.org/world-heart-day/about-whd/.
14. Stuntz M, Bernstein B. Recent trends in the prevalence of low-dose aspirin use for primary and secondary prevention of cardiovascular disease in the United States, 2012–2015. Prev Med Rep 2017;5:183-6.
15. Ittaman SV, VanWormer JJ, Rezkalla SH. The Role of Aspirin in the Prevention of Cardiovascular Disease. Clinical Medicine & Research. 2014;12(3-4):147–54.
16. Husain S, Andrews NP, Mulcahy D, Panza JA, Quyyumi AA. Aspirin Improves Endothelial Dysfunction in Atherosclerosis. Circulation. 1998;97(8):716–20.
17. Patrono C, Baigent C. Role of aspirin in primary prevention of cardiovascular disease. Nature Reviews Cardiology. 2019;16(11):675–86.
18. Ecotrin 81 mg professional information. 2 February 2023.
19. Impact Rx data, October 2022.
20. South African Medicine Price Registry. Database of Medicine prices 23 December 2022. http://www.mpr.gov.za/.
21. Steinhubl SR, Bhatt DL, Brennan DM, Montalescot G, Hankey GJ, Eikelboom JW, et al. Aspirin to prevent cardiovascular disease: the association of aspirin dose and clopidogrel with thrombosis and bleeding. Ann Intern Med 2009;150(6):379-86.
This article was brought to you by Acino.
Unintended pregnancies a critical issue in reproductive health
Unintended pregnancies remain a significant public health concern worldwide, with profound implications for women's health, socio-economic status, and overall well-being.
ESPITE THE AVAILABILITY of various contraceptive methods, the prevalence of unwanted pregnancies continues to be alarmingly high. This article delves into the prevalence of unwanted pregnancies, drawing insights from recent studies on emergency contraception. In 2012, there were approximately 213 million pregnancies globally, of which 85 million (almost 40%) were unintended. Of these unintended pregnancies, 50% ended in abortion, 38% resulted in unplanned births, and 13% led to miscarriages. The high rate of unintended pregnancies
underscores the need for effective contraceptive methods and education.
EMERGENCY CONTRACEPTION: A CRITICAL TOOL
Emergency contraception (EC) plays a crucial role in preventing unwanted





• ella
is
• Favourable safety and side effect profile.1
• ella® is a selective progesterone receptor modulator.3
pregnancies. EC methods, including hormonal pills like levonorgestrel (LNG) and ulipristal acetate, are designed to be used within a specific timeframe after unprotected intercourse. Despite their availability, the use of EC is often surrounded by myths and a lack of knowledge among both healthcare professionals and users.
A study by Glasier et al., published in The Lancet, found that ulipristal acetate is an effective alternative to levonorgestrel, particularly when used up to 120 hours after unprotected intercourse. The study highlighted that ulipristal acetate prevented more pregnancies than levonorgestrel, especially when administered between 72 and 120 hours after intercourse.
EFFICACY
AND SAFETY
Hormonal emergency contraception, such as levonorgestrel, is effective when used within 72 hours of unprotected intercourse. However, its effectiveness declines when administered beyond this period. In contrast, ulipristal acetate maintains consistent effectiveness up to 120 hours after unprotected intercourse. Both levonorgestrel and ulipristal acetate are well-tolerated, with mild and self-limiting side effects. Common side effects include nausea, headache, abdominal pain, and dizziness. The progestin-only pills, such as levonorgestrel, are better tolerated than combined oestrogen-progestin regimens.
BARRIERS TO USE
Barriers include lack of awareness, misconceptions about the safety and efficacy of EC, and limited access. In many countries, emergency contraception is available without a prescription, yet the uptake remains low. Efforts to increase the use of emergency contraception have focused on improving access and education. Advanced provision, where women are given a supply of EC to keep at home, has been shown to increase use. However, increased use has not necessarily translated into reduced rates of unintended pregnancies. This suggests that consistent use of regular contraceptives and comprehensive sexual education are crucial.
CONCLUSION
Emergency contraception, including levonorgestrel and ulipristal acetate, plays a vital role in preventing unintended pregnancies. However, barriers to their use need to be addressed. Healthcare professionals must educate women about the availability and proper use of emergency contraceptives to reduce the incidence of unwanted pregnancies.
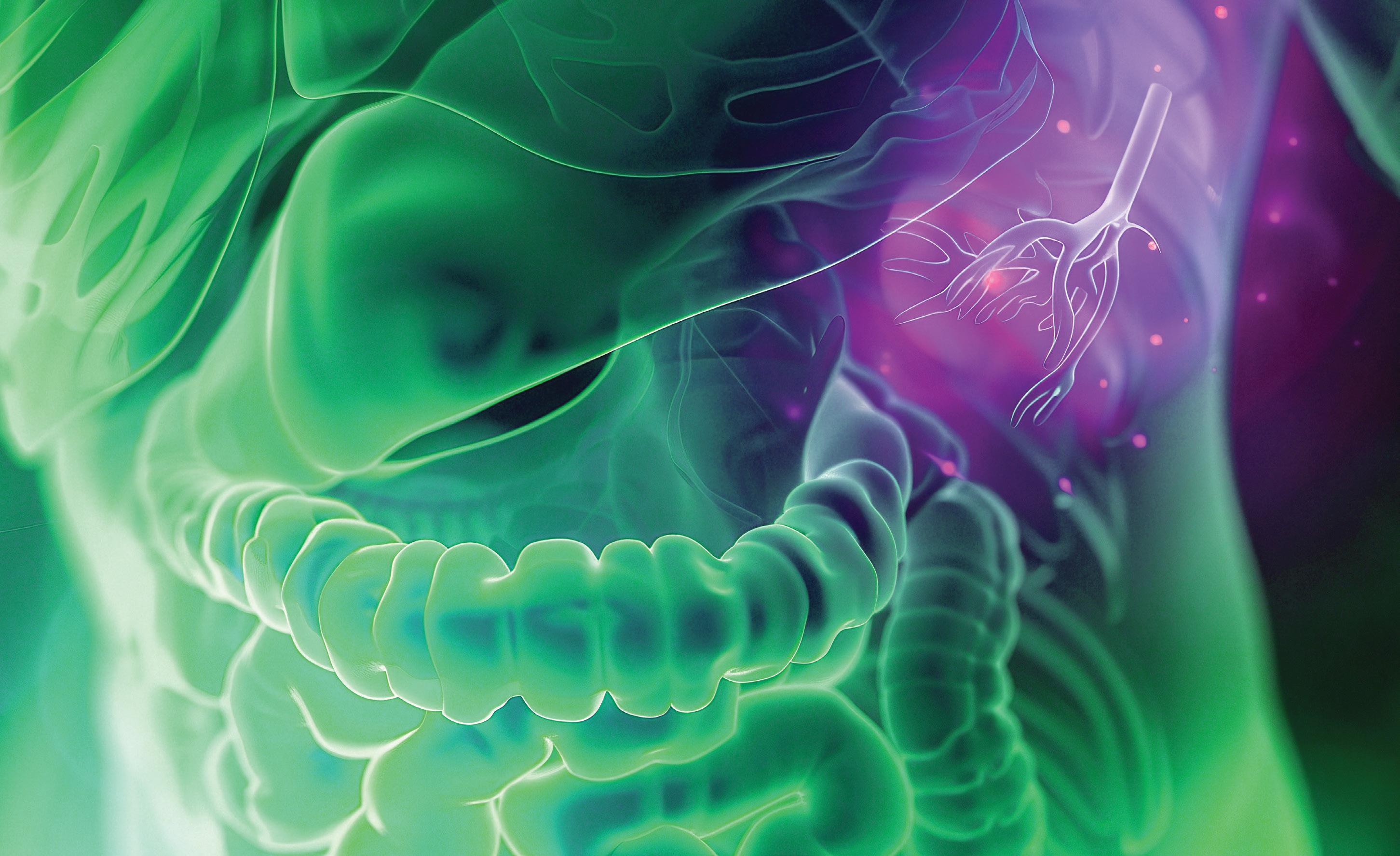

Dr Peter Barrow
Gastroenterologist
Date: 15 October 2024
Time: 7pm
Topic: Managing Ulcerative Colitis: A Survival Guide for Healthcare Workers (and their Patients)
Speaker: Dr Peter Barrow

CLICK TO REGISTER https://bit.ly/AdcockIngramWebinar15Oct24
Dr Peter Barrow is a consultant gastroenterologist trained at the University of Witwatersrand, with a special interest in interventional endoscopy including double balloon endoscopy (DBE) and endoscopic ultrasound (EUS). He has extensive clinical and research experience in inflammatory bowel disease (ulcerative colitis and Crohn’s disease), celiac disease, oesophageal motility disorders and GERD. He is a well-recognised speaker and respected by his peers. Dr Barrow readily shares his practical and clinical expertise and often engages in clinical meetings and elements. Dr Barrow currently serves as an Honorary Lecturer at School of Clinical Medicine,
ChronicleMED
Witwatersrand University and has numerous achievements during his career, amongst which are the following:
- He was involved as an investigator in several clinical trials and is currently working on three new clinical trials on Crohn’s Disease and Ulcerative Colitis
- Presented at International congresses, as recently as International Association of Gastroenterology in Cape Town, Aug 2019 on: “Evaluation of Pancreatic Cystic lesions. What is state of the art?”


U Revolutionising UC treatment
MMX mesalamine is a novel formulation of 5-aminosalicylic acid (5-ASA), for treating mild-to-moderate ulcerative colitis (UC).
C IS A CHRONIC inflammatory bowel disease characterised by symptoms such as bloody diarrhoea and abdominal pain, significantly impacting patients' quality of life. The primary aim of UC management is to induce and maintain remission, with mesalamine being the firstline treatment option.
Traditional mesalamine formulations often require multiple daily doses and may
not effectively target inflamed areas of the colon due to rapid absorption in the small intestine. In contrast, MMX mesalamine uses Multi Matrix System technology, allowing for a high-strength, once-daily oral formulation that ensures delayed and prolonged release of the active ingredient throughout the colon. This targeted delivery minimises systemic absorption, reduces the risk of adverse events, and enhances patient
adherence to treatment regimens.
In a review article, D’Amico et al. conducted a literature review, analysing data from various clinical trials to assess the efficacy and safety of MMX mesalamine. The findings indicate that this formulation is effective in inducing and maintaining both clinical and endoscopic remission in patients with active mild-to-moderate UC. The unique delivery system of MMX mesalamine



contributes to its superior efficacy compared to traditional mesalamine products, allowing for a more localised effect in the colon.
Clinical trials highlighted in the review demonstrate that MMX mesalamine achieves comparable or superior remission rates compared to other mesalamine formulations. For instance, a phase II trial showed similar clinical remission rates between MMX mesalamine and mesalamine enemas, with higher compliance for the oral therapy. Subsequent phase III trials confirmed these findings, revealing significant remission rates in patients treated with MMX mesalamine.
The study emphasises the importance of personalised treatment approaches based on the extent and severity of UC. While rectal preparations may benefit patients with distal colitis, a combination of oral and rectal mesalamine is recommended for those with more extensive disease. The review suggests that MMX mesalamine may provide a greater local effect on the colon than other formulations, although current guidelines do not favour one mesalamine product over another.
SAFETY
Safety assessments indicate that MMX mesalamine is well-tolerated, with a low incidence of treatment-emergent adverse events. The formulation's pharmacokinetics allow for minimal systemic absorption, ensuring that the drug exerts its therapeutic effects primarily in the intestinal lumen. Long-term safety data further support the favourable profile of MMX mesalamine, with no new safety concerns arising during extended treatment periods.
In paediatric populations, while higher doses may be more effective for initial treatment, long-term maintenance of clinical response does not significantly differ between dosages. The study advocates for once-daily dosing of MMX mesalamine, which simplifies treatment regimens and potentially improves adherence.
CONCLUSION
MMX mesalamine presents a significant advancement in the management of mildto-moderate UC, offering a more effective and patient-friendly treatment option. The findings show the potential of MMX mesalamine to improve treatment outcomes and enhance the quality of life for individuals living with UC. Overall, MMX mesalamine represents a promising therapeutic option that addresses the challenges associated with traditional mesalamine formulations, particularly in terms of compliance and localised drug delivery.
Source: D'Amico F, Lusetti F, Peyrin-Biroulet L, Danese S. MMX mesalamine in ulcerative colitis: Major advantages towards classical mesalamine formulations. Dig Liver Dis. 2024;56(9):1425-1432. doi: 10.1016/j. dld.2024.04.012
The fine art of mental health treatment … discovered
Live life in colour
Venlafaxine HCI:
• Treatment of depression, and depression associated with anxiety1
• Prevention of depression episode relapse*1
• Generally fewer drug interactions vs. SSRIs2
Putting back the pieces
Mirtazapine:
• Treatment of major depressive illness3
• Unlike SSRIs, mirtazapine has no sexual side effects4
*In patients responding to an initial six to eight weeks of treatment HCI – hydrochloride; SSRI – selective serotonin reuptake inhibitor
References: 1. Venlafaxine XR Adco Professional Information (Approved PI, November 2021). 2. Stahl SM. Selecting an Antidepressant by Using Mechanism of Action to Enhance Efficacy and Avoid Side Effects. J Clin Psychiatry 1998;59(18):23-29. 3. Adco-Mirteron approved package insert, July 2006. 4. Anttila SAK, Leinonen EVJ. A Review of the Pharmacological and Clinical Profile of Mirtazapine. CNS Drug Rev 2001;7(3):249-264.
S5 Venlafaxine XR 37,5 Adco. Each extended-release capsule contains venlafaxine HCl equivalent to 37,5 mg venlafaxine. Reg. No.: 43/1.2/0577. S5 Venlafaxine XR 75 Adco. Each extended-release capsule contains venlafaxine HCl equivalent to 75 mg venlafaxine. Reg. No.: 43/1.2/0578. S5 Venlafaxine XR 150 Adco. Each extended-release capsule contains venlafaxine HCl equivalent to 150 mg venlafaxine. Reg. No.: 43/1.2/0579. S5 Venlafaxine XR 225 Adco. Each extended-release capsule contains venlafaxine HCl equivalent to 225 mg venlafaxine. Reg. No.: 52/1.2/0438 (Approved PI, November 2021). S5 Adco-Mirteron 15. Each film-coated tablet contains mirtazapine 15 mg. Reg. No.: 39/1.2/0217 (Approved PI, July 2006). S5 Adco-Mirteron 30. Each film-coated tablet contains mirtazapine 30 mg. Reg. No.: 39/1.2/0218 (Approved PI, July 2006).
For full prescribing information please refer to the Professional Information approved by SAHPRA (South African Health Products Regulatory Authority). Adcock Ingram Limited. Co. Reg. No.: 1949/034385/06. Private Bag X69, Bryanston, 2021, South Africa. Customer Care: 0860 ADCOCK/232625. www.adcock.com 202409041018311. September 2024.


Date: 16 October 2024
Time: 7pm
Topic: My patient is suicidal. What now?
Speaker: Dr Frans Korb
CLICK TO REGISTER https://bit.ly/AdcockIngramWebinar16Oct24
Dr Frans A Korb received the following university qualifications: B.Sc (Hons) (UFS), M.A. Clinical Psychology (Wits), M.B. Ch.B. (UCT), M.Med. Psychiatry (Wits). He is registered with the Health Professions Council of South Africa as a Psychiatrist (MP 0294705) and Clinical Psychologist (PS 0011533). He is currently in full-time private practice as a Psychiatrist (PR 2203022). Frans is a general psychiatrist with extensive experience in the management of mood disorders (major depression and bipolar disorder), anxiety disorders, psychosocial rehabilitation of psychotic disorders, ADHD in children and adults as well as psychiatric aspects of sleep disorders. Besides being in private practice, Frans is also a clinical consultant at the Siyathuthuka Care Centre for Life Esidimeni (Belfast, Mpumalanga) and consult for PHI Discovery Health and Sasolmed. Since 1987 he has been a vicepresident and the chairman of the Medals and Merit Committee of the Southern African Association for the Advancement of Science (S2A3). He has been involved with the South African Depression and Anxiety Group (SADAG) (and is currently on their board) almost since its inception in 1994. He is also a guest lecturer in the Department of Psychology, University of Johannesburg. He is frequently invited as an examiner for the Department Psychiatry, University of the Witwatersrand and Colleges of Medicine of South Africa. Frans completed his clinical psychology internship at Tara Hospital the H Moross Centre (Johannesburg) and his medical
Live life in colour
Venlafaxine HCI:
• Treatment of depression, and depression associated with anxiety1
• Prevention of depression episode relapse*1
• Generally fewer drug interactions vs. SSRIs2
S5 Venlafaxine XR 37,5 Adco. Each extended-release capsule contains venlafaxine HCl equivalent to 37,5 mg venlafaxine. Reg. No.: 43/1.2/0577. S5 Venlafaxine

internship at the No 1 Military Hospital (Pretoria). He was a registrar in psychiatry at the Department of Psychiatry University of the Witwatersrand before entering into full-time private practice in Johannesburg in 1991. Past executive appointments include the University Science Students’ Association of Southern Africa (USSASA), Associated Scientific and Technical Societies of South Africa (AS&TS), Southern African Association for the Advancement of Science (S2A3), University of the Witwatersrand Psychiatry Registrars’ Association, South African Association for Child and Adolescent Psychiatry and Allied Professions (ACAPAP), South African Society of Psychiatrists (SASOP), Southern African Society of Biological Psychiatry, the Rotary Club of Sandown, South African Sexual Health Association (SASHA), and the South African Depression and Anxiety Group (SADAG). In 1989 and 1992 he received a Certificate of Merit from the Southern African Association for the Advancement of Science. Frans is also an invited full member of ‘Die Suid-Afrikaanse Akademie vir Wetenskap en Kuns’ (from 1993). Frans regularly attends and presents at local and international conferences, runs workshops, presents posters, courses and CPD programmes. He has written several scientific articles, authored and consulted on numerous magazine and newspaper articles, and is widely recognised as a radio and television guest psychiatrist.

Putting back the pieces
Mirtazapine:
• Treatment of major depressive illness3
• Unlike SSRIs, mirtazapine has no sexual side effects4

Ketamine: Lifesaver or lethal?
The anaesthetic drug ketamine can bring life-saving hope for people suffering treatment-resistant major depression or at severe risk of suicide, but unsupervised use or excessive dosages hold addictive and even lethal risks.
THIS IS THE warning sounded by the South African Society of Psychiatrists (SASOP) against the 'recreational' or unsupervised use of a drug for which scientific evidence is mounting worldwide as a new treatment for adults with severe depression that has not improved with conventional anti-depressant treatments.
“There is good evidence that ketamine in low doses, administered under controlled conditions with the necessary medical supervision, is an effective treatment for treatment-resistant major depression. It is also effective in acute cases of suicidal ideation, rapidly reducing the risk of lifethreatening thoughts and acts.
“However, ketamine is a powerful anaesthetic agent, and a too-high dose can cause sedation and loss of consciousness, and in very high doses may cause dangerously slow breathing and the risk of death.
“Even at lower doses, if administration of ketamine is not adequately supervised and the person is not in a safe, controlled setting they may become confused and inadvertently harm themselves. Ketamine is also potentially addictive and open to abuse,” said SASOP spokesperson, psychiatrist Dr Bavi Vythilingum.
Ketamine is an anaesthetic originally used in animals since the 1960s, in humans since the 1970s, and is listed in the World Health Organization’s List of Essential Medicines as an anaesthetic. It is registered in South Africa for induction and maintenance of anaesthesia.
The drug’s efficacy in sub-anaesthetic doses as a novel treatment for treatmentresistant depression in adults has gained evidence over the past two decades.1
However, Dr Vythilingum said the rising
number of 'independent' clinics offering ketamine treatment for depression and other mental health conditions is cause for concern, regarding correct diagnosis and whether ketamine is the appropriate treatment, as well as monitoring and management of possible side-effects.
She also emphasised that ketamine is indicated only for treatment of adults with treatment-resistant depression; evidence does not support its use in treatment for children.
Although some claim that ketamine is effective in treating other mental health conditions such as post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder (OCD), SASOP cautions that there is limited scientific evidence for this.
Dr Vythilingum said research had shown several positive effects of ketamine on the brain which contribute to its efficacy in treating treatment-resistant major depression, including that it improves the production and functioning of the neurotransmitter glutamate, which plays a role in mood, thought patterns and cognition.2 Ketamine has a different mechanism to traditional anti-depressant medications, which is believed by medical researchers to be at least part of the reason for its effectiveness where other treatments have failed.3 Ketamine is administered by intravenous infusion (a drip) over 40 to 50 minutes, and the patient given enough time to recover afterwards. The patient should be fetched after the treatment and should not drive until after they have had a full night’s sleep. Initial treatment takes place in six sessions over two to three weeks, and the treating psychiatrist may prescribe maintenance treatment on a case-bycase basis. The dissociative state ('trip'
in common language) caused by ketamine can produce feelings of a trance-like state or hallucinogenic experience, feelings of an 'out-of-body experience', feelings of unreality, visual and sensory distortions, and euphoria or 'a buzz'.
“For this reason, it is important that the setting is safe, meaning that it is quiet and private, that treatment is medically supervised, that the patient is not left alone during treatment and recovery, and that the facility is equipped to manage any adverse side effects,” Dr Vythilingum said.
While the dissociative side-effects can also be a positive in improving depressive symptoms, she said other negative side effects could include nausea and vomiting, raised blood pressure, respiratory depression (slowed breathing), sedation and unconsciousness.
Long-term use of ketamine at high doses can cause bladder, kidney, liver and stomach pain or toxicity, as well as addiction demanding increasingly higher, life-threatening, doses.
“Ketamine for psychiatric treatment must be prescribed by a psychiatrist, as only a psychiatrist can diagnose that depression is treatment resistant. That diagnosis is made following at least two courses of conventional anti-depressant medication with no improvement in symptoms.
“The drug must be administered by a medical doctor, and both physical and psychological safety are paramount during administration of ketamine,” Dr Vythilingum said. SASOP advises that the guidelines issued by the South African Society of Anaesthesiologists (SASP) should be adhered to. These guidelines state that the medical doctor administering ketamine must be an anaesthesiologist
or registered sedation practitioner who is qualified in advanced cardiac life support and resuscitation.
“Ketamine must be administered in a facility equipped for physiological monitoring (blood pressure, pulse rate, oxygen saturation), with medication, equipment and qualified personnel to manage adverse physical or neurological events, including hypertension, cardio-respiratory events, airway management and resuscitation.
“The administering clinician or member of the team should also have expertise in mental health and managing patients who may become agitated, anxious or otherwise distressed. A psychiatrist should be available in case of a psychiatric emergency,”
Dr Vythilingum said.
Ketamine is not considered safe for patients diagnosed with schizophrenia, nor for those with a history of substance abuse. Dr Vythilingum also cautioned that while there was clear evidence for the off-label use of ketamine in treatmentresistant major depression, more research was needed on the drug’s long-term effects, side effects and safety as a psychiatric treatment.
REFERENCES
1. McElvery, R. 2022. The Past, Present and Future of Using Ketamine to Treat Depression. Smithsonian Magazine. https://www.smithsonianmag.com/sciencenature/a-brief-history-of-ketamines-use-to-treatdepression-180980106/
2. Meisner, Robert C. 2019. Ketamine for Major Depression: New tool, new questions. Harvard Health. https://www.health.harvard.edu/blog/ ketamine-for-major-depression-new-tool-newquestions-2019052216673
3. Meisner, Robert C. 2019. Ketamine for Major Depression: New tool, new questions. Harvard Health. https://www.health.harvard.edu/blog/ ketamine-for-major-depression-new-tool-newquestions-2019052216673


Dr Anersha Pillay Neuropsychiatrist
Date: 11 November 2024
Time: 7pm
Topic: Managing Treatment Resistance in Major Depressive Disorder
Speaker: Dr Pillay
CLICK TO REGISTER https://bit.ly/AccordHealthWebinar9Oct24
Dr Pillay graduated from WITS University in 1995 with her MBBCh. Following her internship at CHBH, she worked in Psychiatry (primarily Neuropsychiatry) in the UK for three years, returning to specialise in Psychiatry in 2000. She completed her FCPSYCH in 2003 and commenced employment as a Specialist consultant at Charlotte Maxeke Johannesburg Academic Hospital from 2004 -2017. She completed her MMED in Psychiatry in 2013. She was granted subspecialist registration as a Neuropsychiatrist in 2015. Dr Pillay is currently in full-time
ChronicleMED

private practice at the Life Riverfield Lodge Hospital and the Wits Donald Gordon Medical Centre. She has special interests in Neuropsychiatry training, Psychoneuroimmunology, Epilepsy and TBI. She has played an active role in the South African Society of Psychiatrists (SASOP), where she has served various leadership roles including that of Honorary Treasurer from 2021-2023. She is the current President-Elect. She also serves as a specialist Neuropsychiatrist on the Aeromedical Committee of the SACAA.

The do’s and don'ts of isotretinoin therapy for GPs
Isotretinoin, a potent retinoid, is widely used in dermatology for the treatment of severe acne. While its efficacy is well-documented, the management of patients on isotretinoin requires careful consideration due to its potential side effects and teratogenicity.
Medical Chronicle recently hosted a CPD-accredited webinar on this topic, presented by dermarologist Dr Hetesh Pitamber. The webinar was sponsored by Adcock. Here, we outline the key messages from his presenation for prescribing and managing isotretinoin therapy.
DO’S
1. Comprehensive patient evaluation: Before initiating isotretinoin, conduct a thorough patient history and physical examination. Assess for contraindications such as pregnancy, liver disease, and hyperlipidaemia. Baseline laboratory tests, including liver function tests, lipid profile, and a pregnancy test for women of childbearing potential, are essential.
2. Informed consent: Educate patients about the potential side effects of isotretinoin, including teratogenicity, mucocutaneous effects, and psychiatric symptoms. Obtain informed consent, ensuring that patients understand the importance of adherence to contraceptive measures and regular follow-up
appointments.
3. Contraceptive measures: For female patients of reproductive age, ensure the use of effective contraception one month before, during, and one month after isotretinoin therapy. Dual contraception methods are recommended to minimise the risk of pregnancy.
4. Regular monitoring: Schedule monthly follow-up visits to monitor for side effects and assess treatment efficacy. Repeat laboratory tests, including liver function and lipid profile, at regular intervals. For female patients, conduct monthly pregnancy tests.
5. Patient education: Provide detailed instructions on the proper use of isotretinoin, including the importance of taking the medication with food to enhance absorption. Educate patients on managing common side effects such as dry skin and lips, and advise on the use of moisturisers and lip balms.
6. Psychiatric assessment: Monitor patients for signs of depression, anxiety, or other psychiatric symptoms. While a direct causal relationship between isotretinoin
Investigations in drug allergy
and psychiatric effects is not established, it is crucial to remain vigilant and provide appropriate referrals if needed.
DON'TS
1. Avoid in pregnancy: Never prescribe isotretinoin to pregnant women or those planning to become pregnant. The teratogenic effects of isotretinoin can lead to severe congenital malformations. Ensure strict adherence to contraceptive measures and regular pregnancy testing.
2. Do not overlook side effects: Be proactive in managing side effects. Common adverse effects include dry skin, cheilitis, and epistaxis. Educate patients on preventive measures and provide symptomatic treatment as needed. For severe side effects, consider dose adjustment or discontinuation of therapy.
3. Avoid excessive sun exposure: Advise patients to minimise sun exposure and use broad-spectrum sunscreen with a high SPF. Isotretinoin increases skin sensitivity to UV radiation, leading to a higher risk of sunburn.

4. Do not ignore mental health: Pay attention to any changes in the patient's mood or behaviour. Promptly address any psychiatric symptoms and consider collaboration with mental health professionals for comprehensive care.
5. Avoid alcohol consumption: Advise patients to limit or avoid alcohol intake during isotretinoin therapy. Alcohol can exacerbate liver toxicity and hyperlipidaemia, increasing the risk of adverse effects.
6. Do not prescribe without proper training: Isotretinoin should only be prescribed by healthcare professionals experienced in managing its use. Ensure that you are familiar with the guidelines and protocols for isotretinoin therapy to provide safe and effective care.
In conclusion, isotretinoin is a valuable treatment for severe acne, but it requires careful patient selection, education, and monitoring. By adhering to these dos and don'ts, healthcare professionals can optimise treatment outcomes while minimising the risk of adverse effects.

In a recent webinar, Prof Lena Heiser-Garvey, an expert in anesthesiology and allergology, provided an in-depth exploration of drug allergies, particularly focusing on penicillin and nonsteroidal anti-inflammatory drugs (NSAIDs).
SPONSORED BY THERMO FISHER, the session highlighted the growing prevalence of drug allergy referrals in clinical settings, with a significant number linked to antibiotics, especially penicillins. Prof Garvey presented findings from a comprehensive five-year study involving 1 913 drug provocations. The data revealed that while specific IgE tests for penicillin could identify allergic responses, approximately 11% of patients with negative IgE tests still exhibited positive reactions during provocations. Notably, most of these reactions were delayed-type, such as rashes from amoxicillin, rather than immediate. This finding emphasises the necessity for thorough investigations into reported drug allergies, as many patients may experience non-allergic side effects rather than true allergies.
The discussion underscored the critical importance of addressing penicillin allergies, particularly in light of the rising issue of antimicrobial resistance. In Denmark, where penicillin is a first-line treatment for various infections, accurately identifying patients with genuine allergies is essential. Prof Garvey noted that about 10% of hospital inpatients report a penicillin allergy, yet 80%-90% of these cases can be disproven through proper investigation. To effectively manage drug allergies, Prof Garvey advocated for a risk stratification approach. This method involves tailoring investigations based on the patient's reported history and the associated risk level of their symptoms. For patients at high risk of severe reactions, such as anaphylaxis, more extensive testing is warranted, including specific IgE blood tests prior to any skin testing. This approach
aims to minimise the risk of provoking an allergic reaction during the diagnostic process. The presentation also addressed NSAID allergies, which vary geographically and are often not IgE-mediated. Prof Garvey explained that while NSAIDs can cause various allergic reactions, many patients tolerate selective COX-2 inhibitors, which are frequently used in clinical practice.
A significant portion of the webinar focused on perioperative hypersensitivity, a challenging area in drug allergy investigations. Prof Garvey emphasised the need for collaboration between anesthesiologists and allergists to ensure comprehensive patient care. She shared a case study of a patient who experienced a reaction during surgery, illustrating the complexities of identifying the true allergen in a setting with multiple potential triggers.

Through careful testing, the patient was found to be allergic to chlorhexidine, highlighting the importance of thorough investigation in perioperative settings.
In conclusion, Prof Garvey's presentation emphasised the critical need for accurate diagnosis and management of drug allergies, particularly in the context of rising antimicrobial resistance and the complexities of perioperative care. By employing a risk-based approach to investigations and fostering collaboration among specialists, healthcare providers can improve patient outcomes and reduce the burden of unnecessary drug allergy labels. The insights shared during the webinar are vital for clinicians navigating the intricate landscape of drug allergies in their practice, ultimately aiming to enhance patient safety and treatment efficacy.
Join Medical Chronicle for a free, one-hour, CPD-accredited webinar

This webinar is sponsored by Activo

Dr Dion Craig Opperman
Date: 17 October 2024
Time: 7pm
Topic: Disease modification therapy in MS
Speaker: Dr Dion Craig Opperman
CLICK TO REGISTER https://bit.ly/ActivoWebinar17Oct24
Fellow of the College of Neurologists of South Africa (FC Neurol) by peer review since 2008.
Research: MMed dissertation on Myotonic Dystrophy
Clinical trials: We took part in various clinical trials including: Alnitidan, Aricept, SP511, Lamictin, Elitriptan, Zomitriptan, Topiramate (for migraine prophylaxis), Epilepsy, three Migraine trials, Devco D.
Specific fields of interest
• Multiple Sclerosis
• Parkinson’s Disease


• Dystonia (operates a Botox clinic for dystonia)
• Headache
• Epilepsy
• Peripheral Neurology (Nerve Conductions and EMG)
Publications
Co-author: Giampaolo, D, Bhigjee, A, Retief, C, Isaacs, M, Britz, M, Opperman, D, Govender, R, and van Rensburg, M (2013). Guideline for the diagnosis and management of multiple sclerosis: A Southern African perspective. South African Medical Journal, 103(9), 670-691.


The dry eye wheel
Dr Marsha Oberholzer, recently presented a webinar on dry eyes. This was sponsored by Pharmaco. The following is a summarised version of her presentation. To watch a replay of this webinar and still earn a CPD point, go to: https://event.webinarjam.com/replay/792/ q7647f635h1wquxowsyw1r. Email john.woodford@newmedia.co.za to let him know to allocate your point/ request an
DRY EYE DISEASE
(DED) is a complex and multifaceted condition that significantly impacts patients' quality of life. It is characterised by a loss of homeostasis of the tear film, leading to ocular symptoms such as dryness, irritation, and potential damage to the ocular surface. The tear film itself is a sophisticated structure composed of three primary layers: the lipid layer, aqueous layer, and mucous layer. Recent advancements in our understanding of the tear film have shifted the perspective from viewing these layers as distinct entities to recognising them as a single dynamic functional unit. This article explores the dry eye wheel, a conceptual framework that aids healthcare professionals in the mitigation, measurement, and management of dry eye disease.
REIMAGINING THE TEAR FILM
Historically, the tear film was perceived as a series of separate layers. However, contemporary research indicates that it functions as a gradient of aqueous through mucins, forming a viscoelastic gel with a lipid bilayer on the surface. The total thickness of the tear film is approximately 2-6 micrometres, with variations influenced by factors such as reflex tearing. The lipid layer, primarily composed of triglycerides, free fatty acids, and phospholipids, plays a crucial role in reducing evaporation and maintaining tear stability. Rheological studies have demonstrated that the tear film exhibits non-Newtonian shear-thinning






behaviour, meaning its viscosity decreases with increased shear rates, such as during blinking. This dynamic nature is essential for the tear film's protective and lubricating functions.
THE DRY EYE WHEEL: A COMPREHENSIVE FRAMEWORK
The dry eye wheel serves as a comprehensive model for understanding the various aspects of dry eye disease, including its mitigation, measurement, and management.
1. Mitigation: This aspect focuses on identifying and addressing risk factors associated with dry eye disease. Factors such as environmental conditions, screen time, and contact lens wear can exacerbate symptoms. Education on lifestyle modifications, such as increasing humidity in living spaces and taking regular breaks from screens, can help mitigate the impact of dry eye.
2. Measurement: Accurate assessment of dry eye disease is crucial for effective management. Various clinical tools and questionnaires are available to evaluate symptoms and signs of dry eye. The ocular surface disease index (OSDI) and the dry eye questionnaire (DEQ) are commonly used to assess patient-reported outcomes. Additionally, objective measures such as tear break-up time (TBUT) and osmolarity testing can provide valuable insights into the severity of the condition.
3. Management: The management of dry eye disease is multifaceted and












may include pharmacological and nonpharmacological interventions. Artificial tears and lubricating eye drops are often the first line of treatment. In more severe cases, prescription medications such as cyclosporine A or lifitegrast may be indicated. Punctal plugs can also be utilised to reduce tear drainage and enhance tear film stability. Advanced therapies, such as intense pulsed light therapy, have shown promise in treating meibomian gland dysfunction, a common cause of evaporative dry eye.
THE INTERPLAY OF PHYSICAL AND SOCIAL FACTORS
Physical health factors, such as obesity and physical inactivity, have been linked to dry eye disease. Obesity can lead to structural changes in the meibomian glands, which are essential for producing the lipid layer of the tear film. Furthermore, conditions such as obstructive sleep apnoea may exacerbate dry eye symptoms.
Social factors, including smoking and exposure to environmental irritants, also play a role in the development and exacerbation of dry eye disease. While smoking rates are declining globally, the association between smoking and dry eye remains a topic of interest. Recent studies suggest that vaping may also contribute to dry eye symptoms, necessitating further research in this area.
THE PATIENT EXPERIENCE: A SPECTRUM OF SYMPTOMS
Patients with DED often report a range of

symptoms, including burning, irritation, dryness, stinging, and fatigue. However, the experience of these symptoms can vary widely among individuals.
This variability underscores the importance of a patient-centred approach in clinical practice. Understanding the individual’s perspective on their symptoms and how these affect their daily life is crucial for effective management. Factors such as age, occupation, psychological traits, and personal habits can all influence how patients experience and cope with DED.
CONCLUSION
The dry eye wheel provides a valuable framework for understanding the complexities of dry eye disease. By addressing the multifactorial nature of the condition, healthcare professionals can develop comprehensive management strategies that improve patient outcomes. As our understanding of the tear film and its dynamics continues to evolve, it is essential to remain vigilant in recognising the realworld impact of dry eye disease on patients' quality of life.
A multidisciplinary approach that encompasses ocular health, mental wellbeing, and lifestyle factors will be crucial in effectively managing this prevalent condition. By prioritising patient education, accurate measurement, and personalised management strategies, healthcare professionals can significantly enhance the quality of life for individuals suffering from DED.



Impact of antibiotics on the microbiome
Medical Chronicle recently hosted a webinar on the collateral damage and the potential role of probiotics. This webinar was sponsored by Austell and presented by clinical microbiologist.
To watch a replay of this webinar and still earn a CPD point, go to: https://event.webinarjam.com/ replay/837/10wo0up78t8mwcw89h5xwz. Email john.woodford@newmedia.co.za to let him know to allocate your point/ request an attendance certificate for those who don’t fall under the HPCSA.
BHE FOLLOWING ARTICLE is based on Dr Coetzee’s informative presentation. Antibiotics are one of the most significant discoveries in the pharmaceutical industry. Alexander Fleming discovered penicillin in 1927, which was later purified by Dr Howard Florey and Dr Ernest Chain. The first patient treated with penicillin was Albert Alexander in 1941, who unfortunately died when the supply ran out. Antibiotics have since revolutionised medical practice, enabling major surgeries, cancer chemotherapy, organ transplantation, and neonatal intensive care.
THE PROBLEM WITH ANTIBIOTICS
Despite their benefits, antibiotics are not without drawbacks. They are often broadspectrum and non-specific, leading to side effects in approximately 20% of patients. The term 'collateral damage' describes the unintended consequences of antibiotic use, including antibiotic resistance, Clostridium difficile infection, and disturbances in the microbiome.

COLLATERAL DAMAGE AND ANTIBIOTIC RESISTANCE
Antibiotic resistance is a significant community-wide issue, while individual patients may suffer from infections with ESBL- and MRSA organisms. Studies have shown that bacteria exposed to antibiotics can develop resistance over time, complicating treatment efforts.
THE CONCEPT OF COLONISATION RESISTANCE
The gut microbiome plays a crucial role in colonisation resistance, where normal flora prevent pathogenic bacteria from establishing themselves. This involves nutrient competition, production of antagonistic peptides, and modulation of the host immune system. Antibiotics can disrupt this balance, leading to adverse effects.
THE HUMAN MICROBIOME
The human microbiome consists of approximately 1000 species and three million microbial genes, compared to 23 000 human genes. Each body site hosts a unique microbial community. However, only 0.4% of these species can be characterised through culture techniques, highlighting the complexity of the microbiome.
FACTORS INFLUENCING THE MICROBIOME
Several factors influence the microbiome, including mode of birth, diet, exposure to bacteria, and antibiotics. Modern genomic techniques allow for the classification

and comparison of bacterial communities, providing insights into the microbiome's role in health and disease.
CLOSTRIDIUM DIFFICILE INFECTION (CDI)
Clostridium difficile, an anaerobic, Grampositive, spore-forming bacillus, releases enterotoxins TcdA and TcdB, causing colitis in susceptible individuals. CDI can range from asymptomatic colonisation to severe diarrhoea and death. Risk factors include advanced age, hospitalisation, gastrointestinal surgery, and exposure to certain antibiotics and antineoplastic agents.
DIAGNOSIS AND MANAGEMENT OF CDI
Early recognition of CDI is essential. Diagnosis involves a high index of clinical suspicion and laboratory tests, including tissue culture cytotoxicity assays, enzyme-linked immunoassays, and PCR. Management includes stopping the offending antibiotic and administering vancomycin or fidaxomicin as first-line therapy.
POTENTIAL ROLE OF PROBIOTICS
Probiotics are live microorganisms that confer health benefits when administered in adequate amounts. They include Lactobacilli, Saccharomyces boulardii, and some E. coli and Bacillus species. Probiotics can potentially reduce the collateral damage of antibiotics by preventing antibioticassociated diarrhoea (AAD) and reducing

the need for antibiotics.
PREVENTION OF ANTIBIOTICASSOCIATED DIARRHOEA
Probiotics may restore intestinal microbial balance and have immunomodulatory effects. A pilot study showed that patients treated with Lactobacillus reuteri had a significantly lower frequency of diarrhoea compared to placebo.
REDUCING THE NEED FOR ANTIBIOTICS
A randomised, double-blind, placebocontrolled trial in preschool children found that L. reuteri significantly reduced the frequency and duration of diarrhoea and respiratory tract infections, leading to fewer doctor visits and antibiotic use.
CAUTION WITH PROBIOTICS
While probiotics offer benefits, caution is necessary. A case study of a 23-year-old male with osteosarcoma revealed persistent bacteremia with Bacillus clausii, a probiotic organism. This highlights the need for careful use, especially in immunocompromised patients.
CONCLUSION
Antibiotics have transformed medical practice, but their use comes with risks. Probiotics offer a promising approach to mitigating some of these risks, but their use must be carefully managed. Ongoing research and clinical vigilance are essential to optimise patient outcomes.


Management of vulvovaginal candidiasis An update on guidelines
Vulvovaginal candidiasis (VVC) is a common fungal infection characterised by inflammation of the vulval and vaginal epithelium, affecting up to 75% of women at least once in their lifetime.
THE PRIMARY CAUSATIVE agent is Candida albicans, responsible for 85-95% of VVC infections, with other species like C. glabrata, C. tropicalis, and C. krusei also implicated.
RISK FACTORS AND CLINICAL PRESENTATION
Risk factors for VVC include disruptions in normal vaginal ecology due to broad-spectrum antibiotics, poorly controlled diabetes mellitus, immunosuppression, and hormonal changes. Clinically, VVC can present asymptomatically or with symptoms such as itchiness, vaginal swelling, soreness, dyspareunia, dysuria, and increased discharge. On examination, signs include vaginal discharge, erythema, and abrasions or cracks of the vulva or vagina.
DIAGNOSIS AND DIFFERENTIAL DIAGNOSIS
VVC is diagnosed based on clinical features supported by laboratory confirmation of Candida species from a vaginal sample. Differential diagnoses include trichomoniasis and bacterial vaginosis, which present with different discharge characteristics and pH levels.
CLASSIFICATION AND MANAGEMENT
VVC is classified into uncomplicated and complicated forms. Uncomplicated VVC is typically managed with topical or oral antifungals. Complicated VVC includes severe VVC, recurrent VVC, VVC caused by non-albicans Candida species, and VVC in immunosuppressive conditions.
RECURRENT VVC
Recurrent VVC, defined as three or more

To watch a replay of this webinar and still earn a CPD point, go to: https://event.webinarjam.com/go/replay/819/q7647f6n8h1yvsxy6tk. Email john.woodford@newmedia.co.za to let him know to allocate your point/ request an attendance certificate for those who don’t fall under the HPCSA.
episodes in less than a year, affects less than 5% of women but has significant economic and psychosocial impacts. Management involves an induction regimen to achieve clinical remission, followed by a maintenance regimen. Recommended induction includes fluconazole 150mg orally every 72 hours for three doses, followed by maintenance with fluconazole 150mg orally once a week for six months.
NON-ALBICANS VVC
Non-albicans VVC, often resistant to fluconazole, may require alternative treatments such as local nystatin or boric acid. However, boric acid is not recommended for women of reproductive age due to its potential embryotoxic effects.
VVC IN SPECIAL POPULATIONS
In pregnancy, VVC management aims
Update on acne management
to prevent complications while ensuring safety. Topical azoles are recommended, with fluconazole avoided due to potential associations with congenital malformations. In HIV-infected women, VVC tends to be more severe and recurrent, but conventional therapy remains effective. Diabetic women are at increased risk due to hyperglycaemia, which promotes fungal adhesion and impairs immune response.
FOLLOW-UP AND PATIENT EDUCATION
Routine follow-up is unnecessary for acute uncomplicated VVC, but recurrent VVC requires monitoring and culture testing if symptoms persist. Educating and reassuring patients, along with addressing exacerbating factors, are crucial components of management.
We recently helda CPD-accredited webinar on acne management. This webinar was sponsored by Austell and presented by Dr Imraan Jhetam, a specialist dermatologist. The following article is based on his presentation.
ACNE IS A PREVALENT inflammatory condition affecting the pilo-sebaceous units, primarily seen in adolescents but also persisting into adulthood. This article provides an overview of the epidemiology, pathogenesis, clinical features, and management strategies for acne, with a focus on new technologies and molecules.
EPIDEMIOLOGYA
Acne is the most common skin disease among adolescents, affecting 80% of teenagers aged 12-18 years. It can persist into adulthood, with 3% of men and 12% of women experiencing acne up to 25 years. Notably, 1% of men and 15% of women continue to have acne into their 40s and beyond. Adult-onset acne, first described by Kligman in 1991, predominantly affects older women with high-stress jobs, often related to chronic stress, excessive cosmetic use, certain medications, and hormonal imbalances such as PCOS.P
ATHOGENESIS
Acne development involves five key factors:
1. Follicular epidermal proliferation leading to obstruction of the pilosebaceous duct.
2. Sebum production regulated by
hormones, particularly androgens.
3. Comedone formation due to excess sebum and follicular hyperkeratosis.
4. Proliferation of Cutibacterium acnes (C. acnes) in the presence of excess sebum.
5. Inflammation stimulated by C. acnes. Diet also plays a role, with studies indicating that cow's milk, particularly skim milk, and high glycaemic load diets can exacerbate acne.
CLINICAL FEATURES
Acne presents with various lesions, including comedones, papules, pustules, nodules, and cysts, primarily in sebaceous gland-rich areas like the face, chest, back, and upper arms. The severity of acne can range from mild (comedones and a few papulopustules) to severe (nodulocystic acne with large nodules and scarring).
Severe variants like acne fulminans and acne conglobata can be associated with systemic symptoms.
MANAGEMENT
General principles:
- Cleanse the face twice daily with a mild cleanser.
- Avoid overwashing and scrubbing.
- Use oil-free moisturisers.
- Avoid popping or picking pimples.

To watch a replay of this webinar and still earn a CPD point, go to: https://event.webinarjam.com/replay/817/ xq0nqam1miz6zavlxizp2w. Email john.woodford@newmedia.co.za to let him know to allocate your point/ request an attendance certificate for those who don’t fall under the HPCSA.
Skincare:
- Cleansers should effectively cleanse without compromising the skin barrier.
- Moisturisers should counteract the drying effects of acne treatments and provide sun protection.
Medical treatment:
- Mild acne: Topical agents like benzoyl peroxide, retinoids, and antibiotics.
- Moderate acne: Combination of topical agents and systemic antibiotics or hormonal therapy.
- Severe acne: Systemic agents like isotretinoin, antibiotics, and hormonal therapy.
Bacterial resistance:
- Resistance to antibiotics like erythromycin and tetracyclines is common.
- Benzoyl peroxide can prevent bacterial resistance and is recommended alongside antibiotics.
Hormonal therapy:
- Combined oral contraceptives (COCs) are effective for inflammatory acne in females.
- Spironolactone can be used in selected patients.
Isotretinoin:
- Recommended for severe nodular acne and treatment-resistant moderate acne.
- New formulations like lidose and micronised isotretinoin improve bioavailability and reduce food dependency.
New and emerging therapies:
- Adapalene 0.3/BPO 2.5%, clascoterone, tifarotene, IDP-126, and oral sarecycline are promising new treatments.
Acne scarring:
- Early and appropriate management of active acne can prevent scarring.
- Treatments for acne scars include chemical peels, microdermabrasion, microneedling, fillers, laser therapy, and steroid injections.
CONCLUSION
Effective acne management requires a comprehensive approach, including early intervention, appropriate skincare, and the use of both topical and systemic treatments. New formulations and emerging therapies offer promising options for improving patient outcomes and adherence.
Challenges facing healthsystems in Africa
How does this impact SA as we plan for NHI?
NDERSTANDING THE CHALLENGES faced by health systems across Africa offers valuable insight into the obstacles South Africa may encounter as it moves forward with implementing the National Health Insurance (NHI). Many health systems in Africa are struggling with severe inefficiencies and suboptimal health outcomes, highlighting potential pitfalls and areas that need careful consideration in the NHI rollout.
CHALLENGES FACING HEALTH SYSTEMS IN AFRICA
Leading challenges in the healthcare sectors were:
1. Inadequate human resources for health
2. Inadequate budgeting allocations to the health sector
3. Poor leadership and management.
These three challenges accounted for two thirds of all the perceived problems in the health sector. The WHO proposed a framework that describes health systems in terms of six core components or building blocks:
1. Service delivery
2. Healthcare workforce
3. Health information systems
4. Medicines and technology
5. Financing
6. Leadership and governance.
When viewed through the six WHO healthcare system pillars, the main problems centred on leadership, governance, workforce, and service delivery and financing. Healthcare delivery challenges exist in all countries even with High Human Development Index (HDI), but resource issues demand more attention in those with low HDI. These issues help prioritise the segments of the healthcare system that are most affected or in urgent need of attention.
Work done by Roncarolo and colleagues reported challenges which are similar:
Human resources (22%), leadership and governance (21%) and Health Service Delivery (24%). Therefore, addressing these issues may solve over two thirds of the problems associated with the healthcare system in Africa. Most of the African countries are unable to meet the basic requirements for a good healthcare system.
Poor governance and human resource challenges are linked to ineffective integration of services in resource-limited nations. At an individual level, it showed inadequate human resources is the leading challenge in the health sector in Africa. This is both overt and covert, which reflects the complexity of the challenge.
Overt: Inadequate numbers, mix, and distribution are lacking due to insufficient output from training institutions. This is
compounded by outward migration / brain drain to Europe, America, and Asia. Covert: Poor availability of engaged healthcare workers to deliver services, resulting in health worker strikes.
WHO findings showed sub-Saharan Africa faces the greatest challenges in shortage of human resources for health. Over the years attention to this has not received the priority it deserves. African countries are experiencing a disproportionate global disease burden of 24% with the least share of a healthcare workforce at only 3%. The study revealed that out of 57 countries with critically low healthcare workforce numbers, 36 are in sub-Saharan Africa, with some European countries now facing similar challenges.
Inadequate healthcare resources can limit access to quality care in rural areas, leading to poor health outcomes and hindering national and global health goals.
This can drive people to seek healthcare abroad, costing Nigeria's economy about $1.2 billion. Also, healthcare systems may not be able to respond to public health emergencies such as outbreaks of diseases leading to increased mortality and morbidity in these countries. The major solution to these key challenges centres around capacity building of healthcare workers, to address the challenge to some extent.
INADEQUATE FINANCING OF HEALTHCARE IN AFRICA
Other healthcare system issues in Africa include financial barriers to healthcare services with high out-of-pocket expenditure, owing to ineffective national healthcare insurance systems and poor service integration. Work done by Musango and colleagues endorsed that most African countries, scarcity of funds is a chronic problem. There was difficulty to keep up with rising healthcare costs in the face of ongoing economic downturn.
Another study found that 40% or more of total healthcare expenditure is made up of out-of-pocket expenditure – the most regressive way of funding healthcare.
The average Total Healthcare Expenditure (THE) in African countries stood at US$135 per capita in 2010 but is only a small fraction of the US$3150 spent on healthcare in an average highincome country.
The poor healthcare financing indices are prevalent in Africa despite several declarations signed by African heads of state, which among others include the Abuja Declaration of 2001 on increasing government funding for health and the 2012 Tunis Declaration on the value of money, sustainability, and accountability in the health sector. Although low budgetary allocation to the health sector and poverty
are the key financial challenges faced by healthcare systems, they contrast with those outlined by Roncarolo and colleagues which included: Increasing healthcare costs; financial unsustainability; and lack of financial autonomy. Lack of financing by government leaves the burden for healthcare financing on households, usually through out of pocket, which have been shown to be catastrophic to households, pushing some households into poverty. The solution suggested is to increase budgetary allocation to healthcare and health insurance for all. The solution may be dependent on prevailing economic situation in the countries and other underlying factors, which account for the complexity of this challenge. However, many insurance programmes leave out the poor. They therefore bear the highest burden of diseases or experience high levels of financially crippling healthcare expenditure in many sub-Saharan countries.
POOR LEADERSHIP AND MANAGEMENT
This includes lack of political will, corruption in the healthcare systems, poor resource management, inefficiencies, and poor integration of healthcare programmes.
Inappropriate leadership can create inefficiencies in the healthcare delivery.
Work done by Dye and German states that one of the biggest challenges in the coming decades will be the selection and development of leaders who are trained and prepared for leadership in increasingly complex healthcare systems.
One of the areas for poor leadership in healthcare was managers unfamiliarity with leadership techniques. These factors on the leadership vacuum hinge on poor governmental role in health policy and poor oversight of the whole health system.
The results are that poor leadership could lead to:
• Increased healthcare costs
• Reduced efficiency and effectiveness
• Dissatisfaction among staff
• Ultimately resulting in lower patient satisfaction
• Poor health outcomes.
Appropriate leadership can create an organisational culture that is committed to quality, reducing conflicts, improving efficiency and productivity, enhancing selfsatisfaction, advancing healthcare system performance, and meeting personal and organisational goals.
UNIQUE CHALLENGES OF AFRICA’S HEALTHCARE LANDSCAPE
Covid-19 Pandemic has brought into focus the unique challenges and limitations that continue to degrade Africa’s

medical landscape. To redefine Africa’s healthcare journey towards a sustainable healthcare system and future health strategies, we need to understand the continent’s demographics and needs; the accessibility issues and increased demand for healthcare.
Africa’s current population is 1.3 billion with a population density of 45/km2
The median age is 19.7 years and 43.8% of the population is urban.
There are two fundamental challenges that the Government across the continent must address. Africa has the world’s largest burden of disease and experiences the most severe shortage of healthcare workers. Accessibility to healthcare is one of the greatest challenges. A possible solution is implementation of Universal Health Coverage. This will provide access to more people for healthcare.
In African countries, professional healthcare services are concentrated in urban areas leaving those in rural areas unable to access even the most basic levels of preventive healthcare.
DEMOGRAPHIC CHALLENGES
Africa currently is experiencing the world’s highest rate of urbanisation with roughly 65 million additional residents per year.
Sub-Saharan Africa is home to 17 million Internationally displaced persons according to the UN Refugee Agency. These people have very little access to healthcare, particularly preventive primary care. In these environments communicable diseases spread very quickly as physical distancing is near impossible
POTENTIAL SOLUTIONS
First: Economic investment in healthcare workers and infrastructure can build a more reliable medical landscape to withstand future healthcare challenges.
Second: Investment into human development, education, and improved governance, we can continue to build the healthcare systems.
Third: Medical workers need to fill the shortage of highly skilled medical experts; to allow them to work at the top of their licence. International collaboration may bring knowledge from outside the continent. Healthcare needs to be seen as an investment rather than being seen as solely a financial and environmental resource. Finances into healthcare must be seen as an investment and not a spend.
Solutions: Training and capacity building for healthcare workers in Africa, will need increased budgetary allocation to health, advocacy for political support and commitment, health service for all and improved leadership and management.


Dr Carla van Heerden
Date: 30 October 2024
Time: 7pm
Topic: The Diagnosis of Seasonal Allergies
Speakers: Dr Carla van Heerden
CLICK TO REGISTER https://bit.ly/ThermoFisherWebinar30Oct24
Dr Carla van Heerden is a chemical pathologist who is currently employed in the Immunology Department at the Ampath National Reference Laboratory in Centurion. She obtained her MBChB degree at the University of Pretoria in 2012 and completed

her postgraduate training in chemical pathology at the University of the Witwatersrand in 2021. Her special interests include allergies and autoimmune diseases.




Radiation therapy system a first
for private healthcare
in Western Cape
Netcare N1 City Hospital radiation unit has introduced the first Align RT advanced marker-less patient tracking system in the Western Cape, which together with the Surface Guided Radiation Therapy (SGRT) delivery system ensures accuracy within a millimetre to avoid exposing healthy tissue and nearby critical structures. The system is particularly well suited for delivering Deep Inspiration Breath Hold (DIBH) treatment for breast cancer to spare radiation doses to the heart and lungs.
ONCOLOGY IN THE Western Cape is making significant strides with the introduction of an additional improvement in the delivery of radiation treatment through the first Align RT advanced marker-less patient tracking system in the province. This marks an important milestone for private sector Surface Guided Radiation Therapy (SGRT). With growing international support for the use of SGRT in treating breast cancer, brain tumours, head and neck cancers, sarcomas, and other conditions, the recent installation of this sophisticated radiation therapy delivery system at Netcare N1 City Hospital’s radiation unit represents a major advancement in cancer care options for the Cape region. Dr Cindy Aitton, head of Netcare Cancer Care, emphasises the significance of this development.
Dr John Sauer, a radiation oncologist practising at Netcare N1 City Hospital, highlights the enhanced accuracy and safety of radiotherapy treatments with the province’s first Align RT advanced system. “The system uses fixed cameras in the treatment room to track patients’ skin surface in three dimensions, for both setup and motion management during radiotherapy, ensuring precise positioning and monitoring during radiation treatment. This is a significant development as the radiation beams are directed exactly where they are needed, minimising exposure of surrounding healthy tissue while delivering the full therapeutic dose,” he says.
Three cameras continuously monitor the position of thousands of points on the skin surface to identify patient positioning in three dimensions and detect any tiny shift in position during treatment. If the person moves during radiation therapy, the system automatically cuts off the radiation beam to pause treatment to prevent accidental exposure. During the entire treatment delivery procedure, the system ensures accuracy within a millimetre to ensure
the radiation is kept away from healthy tissue and nearby critical structures. The system is particularly well suited for delivering Deep Inspiration Breath Hold (DIBH) treatment for breast cancer with submillimetre positional accuracy to spare radiation doses to the heart and lungs. The state-of-the-art system is also geared to improve treatment times for other advanced therapies offered at Netcare N1 City Hospital’s radiation therapy unit, including stereotactic body radiotherapy (SBRT), which delivers high doses of radiation from various angles to target a lesion.
“In treatment for left breast cancer, the DIBH technique requires patients to breathe in deeply and hold their breath for a few seconds, guided by the radiation therapists, so that the heart moves away from the treatment area to ensure minimal radiation exposure,” Dr Sauer explains.
DIBH BREAST CANCER PATIENT EXPERIENCE
Mrs Ingrid Williams is one of the first patients in the Western Cape to be treated using this new sophisticated patient tracking system recently installed at Netcare N1 City Hospital’s radiation unit. She is currently undergoing this specialised course of radiation therapy following surgery to remove a tumour in her left breast.
“With the help of this new SGRT system, the treatment intends to eliminate any cancer cells that may remain around the surgical site, and this requires great precision as it is so near to her heart,” Dr Sauer says. Williams says that she was pleasantly surprised that her treatment sessions last only up to ten minutes so that she can schedule them during her lunch break from work. “The treatment team are so friendly. They explained exactly how to do the breathing technique without arching my back. When I breathe in, I can see on the indicator screen when I am in exactly the right position. Only then
EDITORIAL
EDITOR: Claire Rush McMillan
Claire.Rush@newmedia.co.za
NEWS WRITER: Nicky Belseck
Nicky.Belseck@newmedia.co.za
SUB-EDITOR: Gill Abrahams
EDITORIAL CONTRIBUTORS
Contributors: Prof Morgan Chetty
LAYOUT & DESIGN: Naresh Budraj
ADVERTISING
ADVERTISING EXECUTIVES
Anel du Plooy - Tel: 082 786 9517
Anel.duPlooy@newmedia.co.za
Cindy Riederer - Tel: 082 492 0229
Cindy.Riederer@newmedia.co.za
DISTRIBUTION & SUBSCRIPTIONS
Felicity Garbers
Email: felicity.garbers@newmedia.co.za
Update your details here: www.medicalacademic.co.za
does the beam of radiation start and I hold my breath like that for 30 seconds, which isn’t hard as it goes by so quickly, and then the radiation therapists tell me over a speaker when I can relax and breathe normally again,” Williams says.
TIMESAVING AND MARKER-LESS
Marilyn Lameyer, Netcare’s regional radiation therapy manager, says that a significant amount of time in radiation therapy sessions is usually dedicated to positioning the patient for the prescribed dose of radiation to be administered.
“The convenience of this technology dramatically reduces setup and manages motion during treatment sessions, which leads to an approximately 22% reduction in setup and treatment time, while pinpointing the areas prescribed in the radiation treatment plan in real time.
“The new system also eliminates the use of excessive daily X-ray imaging to verify skin marks, so people can spend less time on the treatment bed. Another benefit of the new system is that it is a completely non-invasive, contactless technology,” she says.
Lameyer adds that another advantage of the new marker-less system is that medical tattoos are not required to provide the reference points for treatment and treatments that previously required an enclosed mask can now be administered with an open face mask for greater patient comfort.
“The rapid advances in treatment technologies are not only important in improving outcomes, but in terms of quality of life, these developments are also helping to make the practical aspects of treatment a little easier for people living with cancer,” Dr Aitton says.
“Netcare continues to invest in the latest cancer care services so that practitioners and their patients have world-class treatment options, supported by our caring, holistic multidisciplinary approach,” she concludes.
PUBLISHING TEAM
GENERAL MANAGER: Dev Naidoo
GROUP ACCOUNT DIRECTOR: B2B: Johann Gerber
Email: Johann.Gerber@newmedia.co.za
DIGITAL MANAGER: Varushka Padayachi
PRODUCTION MANAGER: Angela Silver
ART DIRECTOR: David Kyslinger
CONTACT
Johannesburg Office
Building 13, The Woodlands Office Park, 20 Woodlands Drive, Woodmead, Sandton PO Box 784698, Sandton 2146 +27 11 867 6111
COVER PRICE
Medical Chronicle per issue R60.00 VAT Incl.
Published by New Media, a division of Media24 (Pty) Ltd Printed and bound by Novus Print - Montague Gardens, Cape Town
MANAGEMENT TEAM
CEO : Aileen Lamb
COMMERCIAL DIRECTOR: Maria Tiganis
STRATEGY DIRECTOR: Andrew Nunneley
CHIEF FINANCIAL OFFICER: Venette Malone
Interim CEO: MEDIA24: Raj Lalbahadur
HEAD OFFICE
Cape Town
11 Shelley Road, Salt River, Cape Town PO Box 440, Green Point 8051 +27 021 406 2002
Unless previously agreed in writing, Medical Chronicle owns all rights to all contributions, whether image or text.
SOURCES: AdobeStock, supplied images, editorial staff. While precautions have been taken to ensure the accuracy of its contents and information given to readers, neither the editor, publisher, or its agents can accept responsibility for damages or injury which arise therefrom. All rights reserved. © Medical Chronicle. No part of this publication be reproduced, stored in a retrieval system or transmitted in any form or by any means, photocopying, electronic, mechanical or otherwise without the prior written permission of the copyright owners. Attention African readers: Please note that some products might not be available in your region and product names could vary. Please contact your local distributors, agents or pharmaceutical companies concerned for any discrepancies.





Prof Fasanmade Olufemi Adetola
MBBS, FWACP, FACE, MPA, MD, FAMedS, Consultant Physician/ Endocrinologist
Date: 13 November 2024
Time: 7:00pm
Presenters: Prof Fasanmade Olufemi Adetola, Dr Ankia Coetzee
Prof Fasanmade Olufemi Adetola is a distinguished medical professional with expertise in surgery and endocrinology. With an outstanding academic journey, he passed all preliminary science and medical exams at first sitting. His residency in surgery led to him becoming a Fellow of the West African College of Surgeons. He passed primary exams at the West African Postgraduate Medical College and Nigerian Postgraduate Medical College. His commitment culminated in him being recognised as a Fellow of the American College of Endocrinologists in 2008.




Dr Ankia Coetzee is a prominent consultant chysician and subspecialist endocrinologist affiliated with Stellenbosch University and Tygerberg Hospital, alongside a private practice in Cape Town. Specialising in diabetes in pregnancy and complex endocrine disorders, she boasts over a decade of experience. Dr Coetzee holds degrees from the University of Pretoria and Stellenbosch University, including an M.Phil in Endocrinology. Her Ph.D. submission focused on hyperglycemia in pregnancy. An adept educator, she mentors students at Stellenbosch University and actively contributes to international conferences and publications, earning recognition for her contributions to South African medicine.