











































































Editor Kevin LaTorre, NCAFP Communications
Managing








Peter T. Graber, NCAFP Communications MEMBERSHIP SERVICES





INTEREST & INITIATIVES

Dr. Nicholas Pennings Receives NCAFP Distinguished Physician Award for His Committed Patient Care and Teaching

Why Precepting Is Good for Medical Students and For You


Avoiding Unlawful Practice and Supervisory Arrangements Have a news item we missed? NCAFP members may send news items to the NCAFP Communications Department for publishing consideration. Please






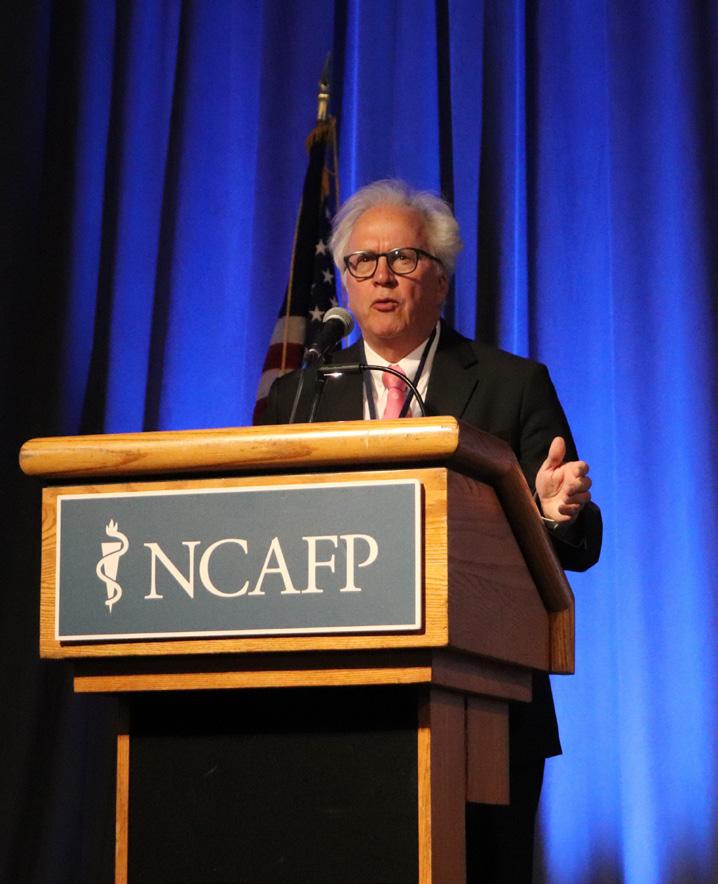
By Mark McNeill, MD NCAFP 2024-2025 President
Dr. McNeill delivered this speech during the 2024 Winter Family Physicians Weekend. You can hear the full recording of his speech in the January episode of the NCAFP podcast, NCFM Today!
I own and run a small Family Medicine office in Asheville called Trillium Family Medicine. Like many residents of western North Carolina, I’m working hard to recover from this once-in-a-lifetime catastrophe called Hurricane Helene. I would like to reflect on a few things I’ve learned so far, as my region recovers.
But first: know that this is not my first once-in-a-lifetime flood.
To understand, let me give you a little bit about my background. I’m a North Carolina native. I grew up in the southeastern part of the state in a little town called Raeford. I would head west to go to undergrad at Appalachian State University in Boone. There I would meet my clever wife, Shelley. I would then crisscross the state again to go to medical school at the Brody School of Medicine at East Carolina University in Greenville.
It would be my second year in medical school when Hurricane Floyd would come to bear. Like any good medical student, I had my head in the books and wasn’t really paying attention to current events like I should have. When the rain started coming down, I looked in my cupboard to see how much food I had in case things got tough. All I found was a mostly eaten jar of peanut butter and one box of Kraft macaroni and cheese. That was it. I got worried, so I called my dad. I said “Dad, this hurricane is starting, and

I’m not prepared. I don’t have any food. I’m not sure what I need to do here. Do I need to get out of here or do I need to stay put?” My dad said “Son, you stay exactly where you are. Don’t you get on the road.”
I said, “Thank you, Father, I now know exactly what I need to do.” I hung up the phone, packed a bag, hopped in my car, and drove as quickly as I could northwest out of Greenville. I would make my way to Washington, DC, where I would be a refugee and stay with my then-girlfriend, Shelley.
The flooding from Hurricane Floyd was particularly devastating for eastern North Carolina. The loss of life and destruction was so bad that the name “Floyd” has been retired as a name for future hurricanes.
I would graduate medical school and head west to Asheville to do my residency in Family Medicine. After finishing at MAHEC, I would spend a year in New Zealand doing locum tenens work. I would then return to western North Carolina to pursue my career as a family physician.

During my residency in September 2004, western North Carolina would receive the remnants of three hurricanes, back to back to back. It would be one of the wettest months on record and cause historic flooding, landslides, loss of power, and loss of water — my second once-in-a-lifetime flood. And now, Hurricane Helene is my third “once-in-a-lifetime” flood. How many am I supposed to experience?
What is tough is that I know I’m not the only one who can say this. North Carolina has experienced four 500+ year floods so far in my career. We all know why that is. The earth is getting warmer. Storms are supercharged. Extreme weather events are more common.
In Family Medicine, we care about the health of our patients, our communities, and public health. The World Health Organization notes that a warming planet is one the greatest threats to public health in the coming decades. And that brings me to the first thing I’ve learned so far from this Hurricane – that as family physicians, we need to be talking about this more.
During the pandemic, we all became experts in virology. We’re going to need the same level of commitment in the next few years to understand how a warming planet affects the health of our patients, our communities,
NCAFP Board of Directors
Executive Officers
President S. Mark McNeill, MD, FAAFP
President-Elect Benjamin F. Simmons, MD, FAAFP
Secretary/Treasurer Deanna M. Didiano, DO
Immediate Past President Garett R. Franklin, MD, FAAFP
Executive Vice President Gregory K. Griggs, MPA, CAE
At-Large Directors
D. Landon Allen, MD, MPH, MBA
Stacey Blyth, MD
Joshua T. Carpenter, MD
Lisa A. Cassidy-Vu, MD, FAAFP
Kelley V. Lawrence, MD, IBCLC, FABM, FAAFP
Amanda R. Steventon, MD, FAAFP
Patrick S. Williams, MD
Courtland D. Winborne, MD
Academic Position
R. Aaron Lambert, MD, FAAFP
Resident Director
Stephanie P. Wilcher, MD, MPH
Resident Director-Elect Irina Balan, MD
Student Director Nicholas Wells
Student Director-Elect Ryan Taylor
AAFP Delegates & Alternates
AAFP Delegate Tamieka Howell, MD, FAAFP
AAFP Delegate Rich Lord, MD, MA, FAAFP
AAFP Alternate Rhett Brown, MD
AAFP Alternate Thomas R. White, MD
NCAFP Committee Chairs
Workforce Committee Jay Patel, MD, MPH
Advocacy Committee Deanna M. Didiano, DO
Practice Environment Nichole Johnson MD, & Profesional Development MPH, FAAFP Committee
Academic Departments Margaret Helton, MD, FAAFP Chair
NCAFP Foundation President Maureen Murphy, MD
www.ncafp.com

and public health. It’s not just floods, hurricanes, extreme weather events, or the pathologies that follow. It’s worsening air pollution which worsens respiratory diseases and contributes to more heart disease and cancer. A warming planet is expanding the ranges and creating longer seasons for infectious diseases that we’re just not used to seeing.
But I’m not all gloom and doom. Make no mistake: the future has some challenges, but I remain hopeful about the future and especially the future of Family Medicine. And that brings me to the second thing that Hurricane Helene has taught me – to make it through a catastrophe, you must adapt.
While this may be my third major flood, this is the first one I’ve been through as a small business owner, with patients, staff, and a balance sheet that rely on me. To be honest, this one has been so much harder, and my need to adapt has been great.
My Helene adaptation story begins in Phoenix, AZ. I spent the few days before the hurricane hit at the American Academy of Family Physicians Congress of Delegates. I would spend two days trying to escape Phoenix. It gets so hot in Phoenix now that airplanes sometimes can’t take off. The air gets too thin, and the planes cannot generate enough lift. My flight kept getting canceled and delayed. After two days of that, I was finally able to get a flight out and back into Charlotte Thursday evening, the night when the first bands of the hurricane began to hit. I rented a car and this time, instead of driving away from the path of the hurricane, I drove directly into it.
I made it back to Asheville. On the radar, you could see a clear eye of the storm between Atlanta and Asheville. That’s pretty remarkable for a storm to still have such a well-defined eye that far inland. It just shows you how powerful this hurricane was. We would lose power. We would lose cell coverage and water. We wouldn’t get it back for weeks. We didn’t get access to potable water back until late November.
Within a couple of days, I learned that my staff members were okay and safe.So was my office. There was no flooding, and no trees on the office, so we considered ourselves fortunate. That is where our good fortune would end.
My practice manager would lose her home to the flood and be unable to return to Asheville. My first medical assistant would leave Asheville and be unable to return, since he would be evicted from his rental. My last medical assistant, who wanted to come back and help, couldn’t because she would be trapped in her home due to numerous fallen trees covering her driveway. And the office had no power, water, or Internet. The other clinicians in my office were available

to return, but they had responsibilities at home including small children. We decided it was best that they did not return at first.
That left me. Given that thousands of patients relied on my office to be available daily, I decided that despite this hell and high water, I would try to reopen. I started scrambling, and I was able to pay way too much for a porta-potty. My family members helped me with access to a small generator that I would lock to the side of my building with my bicycle lock. (I did not have that on my bingo card for 2024). My ACO would give me a Starlink device to put on the roof for Internet. That generator would power the Starlink and one computer. That was enough. I would open the following Monday seeing patients in the dark with a lantern and a headlamp.
I was a little worried that I would put in all this effort and no patients would show up. But when the doors opened, they were there and really grateful to be able to get care. It was just another example of knowing that in Family Medicine, in good times and in challenging times, our patients need us. If we are available, they will be there.
This wasn’t just me. You talk to any family physician from western North Carolina, and you will hear even more impressive stories of adapting to these challenging conditions. That is not a surprise. As family physicians, it is part

of our culture. In Family Medicine we adapt.
It starts with the breadth of our training. No other specialty is prepared to flow seamlessly from the outpatient setting to the hospital, to the emergency department, to a poststorm shelter, to a nursing home, to academic research. Our training has prepared us to adapt. Think about the pandemic and how much we changed our offices, particularly around telehealth and implementing that almost overnight. We continue to evolve with the use of information technology. We are on the cutting edge of collaborative care and incorporating behavioral health into our offices. We continue to adapt to alternative payment models and value-based care. The list goes on and on. When the needs of our patients, our communities, or ourselves change, our background as generalists makes us prepared to adapt.
We don’t just adapt; we innovate. Whether it is our academic departments doing innovative research on community health, small independent practices like mine innovating new models of care, or FQHCs incorporating social determinants of health to meet the needs of some of our most vulnerable, we innovate for the good of our patients, communities, and ourselves.
Whatever challenges come our way, be it a warming planet, political strife, financial constraints, restriction of reproductive health, (without undermining what is right)
Continues as "INAUGURAL" on back cover
By Greg Griggs, MPA, CAE NCAFP Executive Vice President and CEO
As we begin another new year, I would like to consider the new opportunities that we have as individuals and as an organization. Some of these opportunities are brand new, while others are tried and true with a whole new set of circumstances.
First, let me review the core opportunities in our new strategic plan. Your Board decided on three core objectives to suit our three core committees last year, to help move us forward for the next few years. Those core objectives are:
medical student interest, resident engagement, and new physician retention.
Our committees have already begun mapping out their plans for the next 12 to 18 months as we look for new ways to reach these goals. At the same time, there are new opportunities to advance these messages.
For example, in the legislature, we have seen some changes in leadership, with a new Speaker of the House and many new members in both the House and the Senate. We will be working to educate both new and experienced legislators alike about the importance of Family Medicine and how you work each day to improve health and lower costs.

• Advocacy: Strengthen the influence of Family Medicine with health systems, government agencies, and payers.
• Practice Environment and Professional Development: Support family physicians in their personal and professional development and satisfaction.
• Workforce: Grow the future family physician workforce in North Carolina.
Our advocacy priorities are to decrease the administrative burden you face and increase the state’s investment in Family Medicine to reflect the value you bring to the health care system. For practice environment, we are focusing on providing high-quality clinical education and increased networking opportunities, along with education on various practice models and ways to enhance practice efficiencies. Finally, in our workforce efforts, we plan to encourage policy makers and system leaders to incentivize precepting, teaching, and mentoring, while continuing to nurture
Which brings me to one opportunity for you: On Wednesday, March 19, we will hold a Family Medicine White Coat Wednesday at the General Assembly. To be successful there, we need your help. Sign up and take a day to advocate for your patients, your practice, and your profession. We make it easy for you. We will make your appointments, provide talking points based on our strategic plan and the hot topics at the legislature at that time, and even give you some quick training to start the day. If you are interested in participating, just email me at ggriggs@ncafp.com.
We also enter 2025 with a new governor for the first time in eight years, as Gov. Josh Stein moves into the Executive Mansion. While we have already met with his leadership and transition teams, we will need to continue to educate this new administration about Family Medicine. We are pleased that Gov. Stein named one of our own to lead the Department of Health and Human Services (NCDHHS): family physician and NCAFP member Dr. Dev Sangvai will serve as NCDHHS Secretary. While Dr. Sangvai fully understands the value of Family Medicine, there will be others to educate about the role that family physicians play.
Which brings me to another opportunity open to you.
When we talk to medical students and residents, we talk a lot about becoming a 15-minute advocate – taking 15 minutes a week (the equivalent of one patient visit) to advocate for your patients, your practice, and your profession. So, beyond attending White Coat Wednesday on March 19,
here are some other things we would encourage you to do:
• Make sure you respond when we send out a “Speak Out” alert asking you to contact either someone in the legislature or Congress. It’s easy, with your elected official already populated with an appropriate e-mail address and a comment stressing what you need. You just need to use the link when we send it to you.
• Send an email introducing yourself to your local elected officials, whether it’s a town council member, a county commissioner, or your local member of the General Assembly. Let them know that you are available as a resource to them on health care issues. Most elected officials aren’t experts in health care, and you can become their go-to-person on important issues. This process requires building a relationship in advance, not just calling when you need them.
• Go to a political event or even a fundraiser. It helps you get to know elected officials even better.
• Let us know if you have an existing relationship with an elected official.
• Give to our political action committee, FAMPAC. You can donate online at https://www. ncafp.com/advocacy-2/fampac-contribution. A small donation to us helps us build relationships with key health care leaders in the legislature.
Finally, remember this: no one seeks elected office to do harm. You may not agree with an elected official on every issue, and that’s OK. But to build a long-term relationship, it does take some common courtesy, so be nice even when you don’t agree with someone. We can respectfully disagree without being disagreeable or angry. You will find that more times than not, you can find some common ground, and even when you disagree about one issue, you can still build a relationship and discuss many issues where you have much in common.
It’s a new year. Together, let’s take advantage of the new opportunities that it brings. We will all be better advocates for Family Medicine if we do.
Our solutions are driven by a deep understanding of you. By actively listening and proactively creating tailored solutions, our advice is grounded in your priorities and elevated in your outcomes so you can do more and achieve more—in medicine, business, and life.

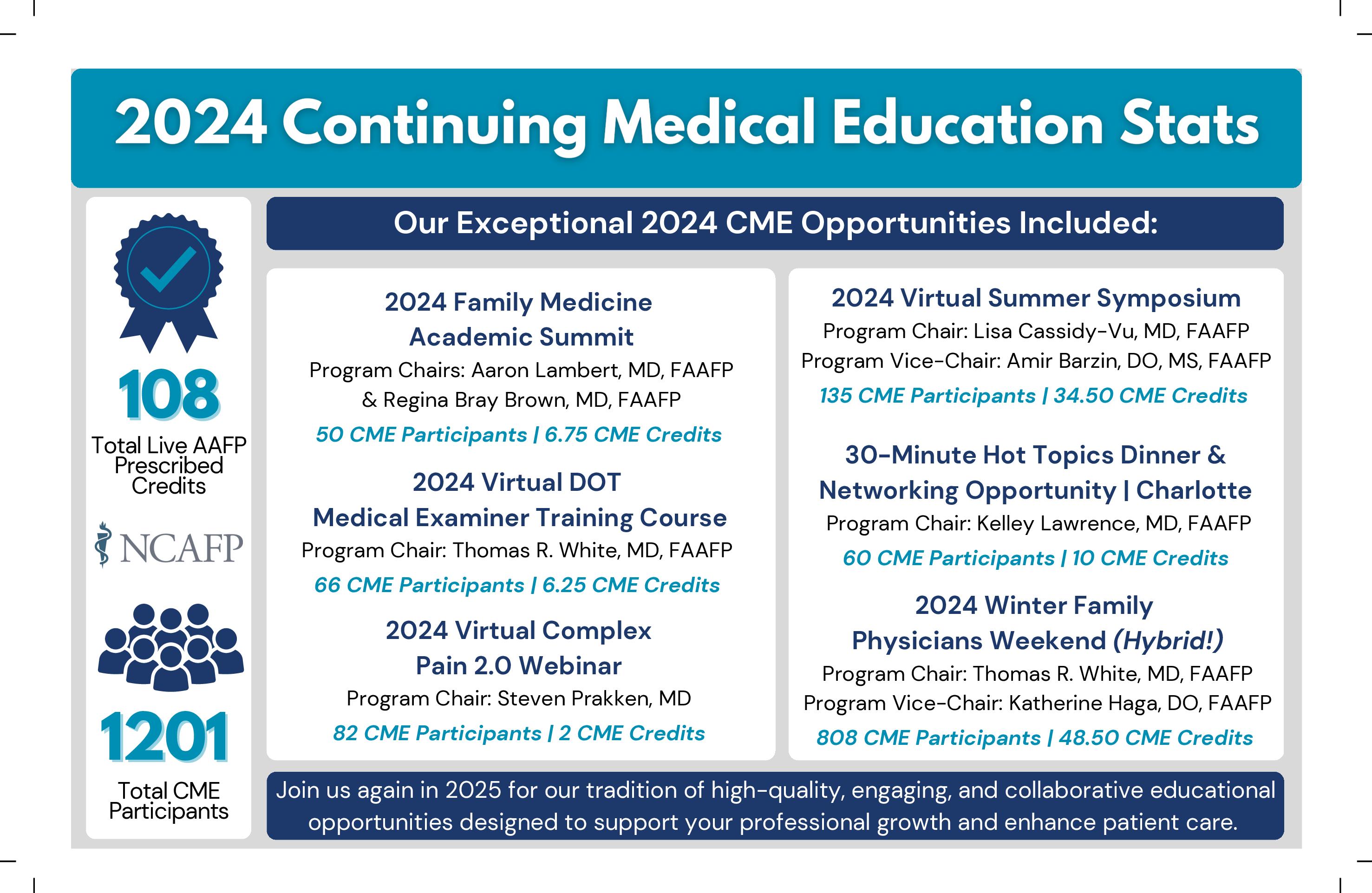
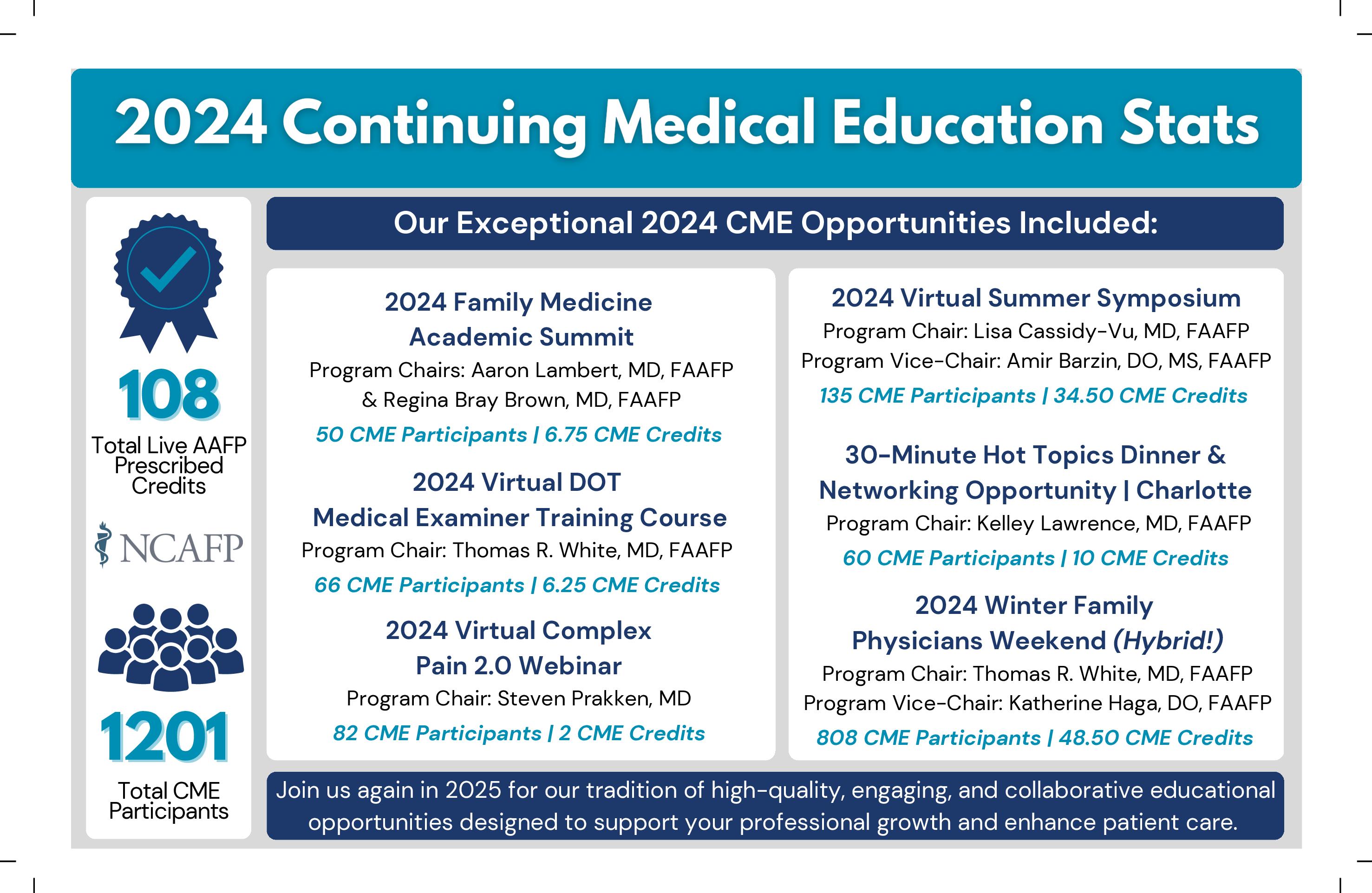
By Kathryn Atkinson, CMP NCAFP Director of CME & Events
Staying current with the latest medical knowledge while earning valuable CME credits provided by your NCAFP CME team will be one of the most rewarding things you do in 2025 — we promise!
This year’s educational lineup covers a wide range of topics, from cutting-edge medical advancements to practical strategies for improving patient outcomes. You can count on the NCAFP’s highly rated, convenient, and engaging learning formats, including timely interactive sessions with case studies, hands-on training, and group discussions.




Led by expert guest faculty, these sessions are designed to address your needs, reignite your passion for Family Medicine, and provide excellent opportunities for networking and connecting with colleagues and peers.
Mark your calendars now for the events below and stay tuned for more details coming soon!
Visit www.ncafp.com/cme for more information, or contact me at Katkinson@ncafp.com. We look forward to seeing you soon!
2025 Virtual Alcohol Use Disorder Webinar
Wednesday, April 2, and Saturday, April 5, 2025
Flexible dates with two opportunities to participate Instructor: David Ryan, MD
Approximately 2.50 CME credits available www.ncafp.com/aud
2025 Summer Symposium | Chronic Health & Sports Medicine – HYBRID!
Saturday, June 7, 2025 – AM Chronic Health / PM Sports Medicine
Program Chairs: Thomas White, MD & Deanna Didiano, DO
The Proximity Hotel, Greensboro, NC
Pre-conference KSA on Friday, June 6, 2025
Approximately 6.00 CME credits available www.ncafp.com/summercme
2025 Winter Family Physicians Weekend – HYBRID!
Thursday, Dec. 4, through Sunday, Dec. 7, 2025
Program Chair: Katherine Haga, DO & Program Vice Chair: Amir Barzin, DO, MS
Omni Grove Park Inn, Asheville, NC
Pre-conference KSA on Wednesday, Dec. 3, 2025
Approximately 30+ CME credits available www.ncafp.com/wfpw

By Kristi Wright, MBA, CPCU, AIC Senior Vice President, Claims, Curi Insurance
Recently, Dr. Gita Pensa, creator of the popular podcast, “Doctors and Litigation: The ‘L’ Word,” delivered an impactful keynote to our Curi Insurance team. This gathering was a key opportunity for our team to connect, learn, and reaffirm our commitment to supporting physicians and clinicians in medicine, business, and life. Dr. Pensa's talk at our event on the stress of litigation resonated deeply with us, highlighting a crucial point: a lack of understanding about the litigation process can intensify this stress for the impacted physician or clinician.
At Curi, our philosophy is “We Defend Good Medicine,” meaning we are dedicated to supporting our clients through one of the most challenging times in their careers. Dr. Pensa’s insights reminded us that, just as patients need clarity about their medical procedures, our clients need a clear understanding of the litigation process. I realized it was time to roll up our “trusted advisor” sleeves and educate!
I’m excited to announce that we have launched a new educational program to demystify the litigation process: The Curi Litigation Education Hub. From blogs and videos to downloadable guides, this program breaks down the entire litigation process, including the roles of key professionals, depositions, mediation, trials, and more. Through our partnership with Dr. Pensa, we’re also providing our Curi clients with an opportunity to earn up to 11 hours of CME credit* through an informative video series. Dr. Pensa’s advice provides actionable tips and stress-reducing strategies to help you navigate this challenging process.
Our commitment to being your trusted partner is predicated on our key values at Curi, one of which is Service Commitment. This new program helps honor that commitment, in that we aim to make the litigation process much more transparent and less stressful.
To learn more and access the Curi Litigation Education Hub, visit curi.com/litigationeducation. You can also read and subscribe to our blog at blog.curi.com.
*This activity has been approved for AMA PRA Category 1 Credit™.

By Kevin LaTorre Communications and Membership Manager
From Dec. 5 through Dec. 8, the NCAFP hosted the 2024 Winter Family Physicians Weekend at the Omni Grove Park Inn (GPI) in Asheville. Over 800 guests attended and learned new techniques and insights during the four days of continuing medical education (CME), and they still had plenty of time to socialize with friends and colleagues.
“The Winter Family Physicians Weekend was a wonderful success, and it was a true pleasure to see so many familiar faces reconnecting and sharing experiences,” said NCAFP Director of CME and Events Kathryn Atkinson, CMP.
“The clinical sessions were engaging and informative, offering practical knowledge that attendees can immediately apply in their practices. Beyond the educational content, the weekend served as a much-needed reminder of the strength and support of our family physician community. It’s always inspiring to witness the camaraderie and enthusiasm that make this event so special year after year.”
“The speakers were dynamic and engaging,” said one attendee in a post-event survey. “Grateful NCAFP was able to provide this conference. And I hope the Asheville
community continues to heal. Thank you for all your efforts!” We at the NCAFP were fortunate to host the meeting at the GPI after the impact of Hurricane Helene earlier this fall, and we sincerely appreciate both the GPI staff who made this event possible and the attendees who returned to Asheville to support the hotel and other local establishments.
NCAFP MEMBERS AND OTHER ATTENDEES ENJOYED THE EVENT’S CME AND PROFESSIONAL CONNECTIONS
Thanks to the work of Kathryn, Program Chair Dr. Thomas White, and Program Vice Chair Dr. Katie Haga, attendees enjoyed four days of CME from top-notch guest speakers. Their subjects included obesity management, the causes of hypertension, the potential of AI in health care, pharmacological management of insomnia, osteoporosis, and many others, occurring in both the mainstage lecture hall and in smaller, hands-on workshop and seminar settings. The 2024 Winter Family Physicians Weekend was also the first-ever to offer a hybrid option of all its mainstage lectures, so that over 100 attendees could attend online from around the country.
Whatever the topic or venue, these sessions gave attendees the useful education they need. “I really enjoyed the topics presented and found the lectures high yield and relevant to my practice,” said one attendee.
“Fantastic content this year!” said another. “I greatly appreciated the option of mixing live and virtual attendance.”
However, the meeting provided much more than clinical advice. Attendees also enjoyed professional networking opportunities for connecting with their colleagues from around the state. On Friday evening, medical students and residents joined new physicians and NCAFP leadership at a social mixer to talk career advancement and residency choices (but also to enjoy refreshments and the laughing company of other attendees). And then on Saturday, over 80 attendees enjoyed the Health Heroes Roundtables Networking lunch to discuss administrative burden, the future primary care workforce, maternal health, primary care investment, and other key topics.
And for the Family Medicine residents ready to begin practicing in North Carolina, the career fair on Saturday afternoon gave them the chance to meet prospective employers in a relaxed setting. “We are thrilled to host this event each year to show North Carolina Family Medicine Residents the broad scope of career options available to them,” said NCAFP Workforce Initiatives Manager Perry Price, who organized and attended the career fair. “It’s a great opportunity for them to get to meet with health care organizations and practices from across the state, so they can have conversations about their options as well as share more with these companies about what they hope to be able to do in practice.”
One other new component added to this year’s meeting was the slate of one-to-one professional coaching sessions with Dr. Dael Waxman, emeritus professor of Family Medicine at Atrium Health – Wake Forest School of Medicine. He brought his own great experience to advise the attendees who met with him during the weekend. “This was by far the most welcoming, most connecting, best organized, and uplifting meeting I’ve attended,” said Dr. Waxman. “Very well done!”
2024 marked the 35th year that the NCAFP has hosted the annual winter meeting at the GPI in Asheville, and some

of the attendees who came have been attending for one or two decades of that span. “People catch up here after years apart,” said Dr. Mike Harris.
The event’s schedule included formal times for these social gatherings, such as the daily mid-morning breaks, the NCAFP Awards Lunch on Friday, and the Presidential Gala on Saturday night. But attendees regularly met with one another to sit and chat in the lounge outside the lecture hall or elsewhere around the hotel.
This social aspect often leads medical students or younger physicians to receive crucial mentorship from experienced family physicians, according to Dr. Elizabeth Ferruzzi. “I learned my own way by directly working with preceptors,” she told a meeting of medical students. “It’s really nice to get connected with those mentors and learn from them.”
Even the formal business of the meeting still included plenty of celebration. First up was the installation of new NCAFP board members by past American Academy of Family Physicians (AAFP) president Dr. Ada Stewart.
Continues as " WINTER MEETING" on page 33

























































2023-24 NCAFP President




A native of Drexel in the foothills of North Carolina, Dr. Franklin attended North Carolina State University graduating with a BS in engineering in 2003, a BA in chemistry in 2007 and a Masters of Physiology in 2008. He completed medical school at the Brody School of Medicine at East Carolina University in 2012 and went on to complete his family medicine residency and a primary care sports medicine fellowship at Wake Forest Baptist Medical Center. He became involved in the NCAFP’s advocacy efforts as a resident at Wake Forest and has served on the Board of Directors for the last several years. Dr. Franklin practices family medicine and sports medicine at Raleigh Medical Group/Cary Medical Group in Raleigh, while also working at NC State University as a team physician. He is active in academic and clinical research and many advocacy projects. Dr. Franklin and his wife have a son and two daughters and live in Raleigh.
























• Your top workforce concern (ranked in the top three concerns by 85% of respondents) was physicians leaving the practice of medicine due to increasing administrative burden.











• Your top causes of frustration as a family physician were administrative burden caused by payers, undervaluing Family Medicine, and recruiting and retaining.

At the beginning of 2024, we conducted our periodic Member Needs Assessment to find out what was on your minds and how we could better serve our members.
to move toward voluntary reporting by our state’s health plans, and set a target for relative improvement. As an Academy, we developed a communications campaign on the importance and value of primary care, including a website, radio ads, and targeted social media.

• Your top state-level advocacy priorities were increasing payment or investment in primary care and reducing administrative burden.
As a result of your feedback, we updated our strategic plan to be laser-focused on the areas where you expressed the greatest concern –payment and administration burden!



We were heavily involved in the legislatively mandated Primary Care Payment Reform Task Force, with Dr. Mark McNeill serving as our representative. The Task Force developed a specific definition of Primary Care, developed a data collection strategy








We also started a series of meetings with our state’s health plans, designed to work together to both increase investment in primary care and reduce administrative burden. One win we have already achieved from these meetings is agreeing on a reduced set of quality metrics for Medicaid. Together, we have requested that Medicaid use a core set of six quality metrics beginning in 2026, versus the current total of 32 that impact primary care today.
Beyond quality metrics, we also focused on prior authorizations, advocating both legislatively and with health plans. As a result of our advocacy, some plans have now taken action to reduce the number of prior authorizations, and United Healthcare implemented a gold card program.
















In government affairs, we had over 40 members participate in our primary White Coat Wednesday, with more than 15 others visiting the legislature at other times. In addition, our Political Action Committee, FAMPAC, supported 15 candidates this election cycle, with all winning their elections.












We also attended approximately 20 legislative and executive branch events to advocate for our members. And of course, we engaged in the implementation process for Medicaid expansion.
Finally, we spent significant energy advocating for our western North Carolina members after Hurricane Helene. Our staff worked with the NC Medical Society, the NC Medical Board, and others to help determine which practices were operational and what they needed. We worked with the state to help meet practice needs and also advocated for stabilization payments to practices from health plans, with most of our state’s Medicaid plans undertaking such payments.








We worked with our state Area Health Education Center to select five new community precepting hubs and begin a study to examine how we can make it easier for community physicians to teach medical students.

Executive Officers
President


Here are a few other milestones we met throughout the year:

• We worked with the state, NC AHEC, and CCNC to finalize plans to provide up to $50,000 grants to help practices implement the Collaborative Care Model of integrating


Secretary/Treasurer



behavioral health into primary care.
• Our Senior VP and General Counsel Shawn Parker assisted over 60 members with contracting, employment, and regulatory questions.



• And finally, we still provided the strong Continuing Medical Education programs you’ve come to expect. All in all, we had six CME events this year, three in person and three virtually.

As you can see, the state of our Academy is strong with numerous accomplishments in 2024. We could not do what we do without the support of our members, and we thank you for continuing to remain members, attend events, and advocate for your profession.
At-Large Directors





Garett R. Franklin, MD, FAAFP
Joshua T. Carpenter, MD
Lisa A. Cassidy-Vu, MD, FAAFP
Deanna M. Didiano, DO
Nichole L. Johnson, MD, MPH, FAAFP
President-Elect S. Mark McNeill, MD, FAAFP
Benjamin F. Simmons, MD, FAAFP

Kelley V. Lawrence, MD, IBCLC, FABM, FAAFP
Amanda R. Steventon, MD, FAAFP
Patrick S. Williams, MD
Courtland D. Winborne, MD
Academic Position
R. Aaron Lambert, MD, FAAFP






Immediate Past President Shauna Guthrie, MD, MPH, FAAFP
Executive Vice President Gregory K. Griggs, MPA, CAE
Resident Director
Morgan Parker, DO
Student Director
S. Evan Morgan
AAFP Delegates & Alternates
AAFP Delegate
AAFP Delegate
Resident Director-Elect
Stephanie P. Wilcher, MD, MPH
Student Director-Elect
Nicholas Wells

Richard W. Lord, Jr., MD, MA, FAAFP
Robert "Chuck" L. Rich, Jr., MD, FAAFP

AAFP Alternate Tamieka Howell, MD, FAAFP
AAFP Alternate




Thomas R. White, MD, FAAFP


























NCAFP’s Political Action Committee (FAMPAC) ensures that North Carolina’s family physicians have a persistent and trustworthy voice in the state legislature. By supporting NCAFP advocacy efforts, FAMPAC impacts health policy in both the state legislature and in the everyday practice environments of our members.





Tactically, this impact comes through political fundraising and attending campaign events. Pragmatic and bipartisan results at the legislature begin well before its session starts.


Christina Albert, MD
Muhammad Bhatti, MD, MPH
Holly Biola, MD, MPH
Karolen Bowman, MD


David Brendle, DO
Rhett Brown, MD
Christopher Danford, MD
Andrea DeSantis, DO
Deanna Didiano, DO

Suzanne Eaton Jones, MD, MPH
Conrad Flick, MD


Eric Gavour

Drew Griggs


Donald Goodman, Jr., MD
FAMPAC provides our members with the opportunity to attend events and start early conversations with lawmakers and other stakeholders. In 2024, we were able to attend a record number of political events, often accompanied by Board members and other NCAFP leaders. 100% of the candidates which NC FAMPAC supported were elected.





Greg Griggs, MPA, CAE
David Hall, MD
George Hall, MD
Tamieka Howell, MD
Ronald Johnson, MD
Eugenie Komives, MD











We would like to extend appreciation for the following individuals who generously made one or more contribution to FAMPAC this year:



Ronnie Laney, MD, MPH

Kathryn Lawrence, MD
Richard Lord, Jr., MD

Robert McConville, MD

Tommy Newton, MD
Shawn Parker, JD
David Rinehart, MD
Cecile Robes, DO
Netra Thakur, MD





Robert Toborg
Dr. R. W. “Chip” Watkins





























The Distinguished Family Physician Award is the Academy’s most prestigious honor, and Dr. Pennings earned it through his commitment to holistic patient care, clinical excellence, and mentoring medical students.







He treats patients in Lillington and also serves as the Family Medicine Chair at the Campbell University School of Medicine (CUSOM), where he is the faculty advisor for the CUSOM Family Medicine Interest Group. In both of these roles, Dr. Pennings provides opportunities for medical students interested in Family Medicine to experience the specialty through CUSOM curriculum, educational events, and in-clinic shadowing.



Shannon Dowler, MD, FAAFP AAFP Board of Directors (Began term October 2024)









Karen L. Smith, MD, FAAFP AAFP Board of Directors (Completed term October 2024)
Mott P. Blair IV, MD, FAAFP American Board of Family Medicine Board of Directors



Viviana Martinez-Bianchi, MD, FAAFP President-Elect, WONCA (World Organization of Family Doctors)
T. Austin Witt, MD Society of Teachers of Family Medicine Board Resident Representative






































During 2024, the Foundation had three organizations make gifts of at least $500,000 each and become “Capstone” donors: the Blue Cross and Blue Shield of NC Foundation, Community Care of North Carolina, and Novant Health.


In late 2024, Novant Health became the first health system to make a significant contribution. During comments at the Winter Family



The Student Endowment Campaign Surpassed $3.1 million — More than Halfway to Its Goal!
Raised for the Medical Student Endowment


The NCAFP Foundation’s “Growing Tomorrow’s Family Doctors” campaign is now more than halfway to meeting its goal, just over two years into the five-year campaign. As of the end of 2024, the campaign had received contributions and pledges worth more than $3.1 million.











Physicians Weekend, Dr. Chan Badger, President of Novant’s Primary Care Services Division and Senior Vice President of Novant Health, discussed the important role that family physicians and the NCAFP can play as the health system transitions to value. “Our North Carolina roots, along with our commitment to being physician led, make our sponsorship of the NCAFP a natural fit,” Badger noted. “We’ve heard directly
















from our own physicians how valuable this organization is to them, and we want to partner to build the family physician pipeline for years to come.”
We'd like to thank these three organizations, along with the many other individual and corporate contributors, for their ongoing support of our medical student endowment. You can find a list of all the campaign’s contributors on the next page.

President

Vice President
Secretary-Treasurer
Exec. VP & CEO
Physician Trustee
Physician Trustee
Physician Trustee
Physician Trustee

Physician Trustee

Medical Students and Residents Attended the Winter Meeting
Medical Students Attended Famly Medicine Day
Maureen E. Murphy, MD

Eugenie M. Komives, MD

Kyle Melvin, MD
Greg Griggs, MPA, CAE
Amir H. Barzin, DO

Christopher P. Danforth, MD
Vickie A. Fowler, MD
Michael J. Harris, MD
Kenneth Herring, MD




Students Completed NCAFP Summer Programs
2023-24 NCAFP Foundation Leadership
Physician Trustee
Resident Trustee
Resident Trustee
Student Trustee
Student Trustee
Corporate Trustee


Franklin Niblock, MD, MPH


Academy President
Academy President-Elect

Sofia Gkoulgkountina, DO
Caleb Smith, MD
NCAFP Student Members MATCHED into Family Medicine Residency Programs
Andrea Augustine, MPH
Mabelle Mathew
Steven Parker (Curi)
Corporate Trustee Tom Wroth, MD (Community Care of NC)
Garett R. Franklin, MD
S. Mark McNeill, MD















Robert Agnello, DO
Christina Albert, MD









Landon Allen MD, MPH, MBA

Michael Alston, MD

Vickie Fowler, MD
Jorge Franco, MD
Joanne Fruth, MD
Deepak Gelot, MD
Kathryn Andolsek, MD, MPH
Amanda Austin, DO
Andrea Augustine, MPH
Johnny Bagwell, MD
Erin Baker, DO
Robert Barnabei, MD
Kathleen Barnhouse, MD
Sanjay Batish, MD




Ted Bauman, MD
Caren Beasley, MD
Mary Bengtson, MD
John Bennett, MD
Mary-Emma Beres, MD


Sofia Gkoulgkountina, DO
Jason Glass, MD
Anne Gonzalez, MD

Renee Goodison-Ollivierre, DO
Donald Goodman, MD
Greg Griggs, MPA, CAE
Andrew Griggs

Shauna Guthrie, MD, MPH
Katherine Haga, DO
David Hall, MD
Caleb Hancock
Michael Harris, MD



Janalynn Beste, MD
Rex Bently, MD
Holly Biola, MD, MPH
Muhammad Bhatti, MD, MPH
Dalia Brahmi, MD
Regina Bray Brown, MD
David Brendle, MD
Caroline Brewster, MD
Samantha Brothers, MD
Rhett Brown, MD
Melinda Brown

Ellen Brubeck Brogden, MD
Christopher Bullers, MD
Swapna Omraju, MD
William Hedrick, MD
Margaret Helton, MD
Joshua Carpenter, MD
Lisa Cassidy-Vu, MD
Dawn Caviness, MD
Ku-Lang Chang, MD
Karen Coward, MD
Vanessa Crerar, DO
Mark Crissman, MD
Gary Curran, MD
Madeleine Cutrone, MD

Doug Henley, MD
Casey Henritz, DO
Kenneth Herring, MD
Terry Hess, MD
Mark Hester, MD
Mark Higdon, DO
Dimitrios Hondros, MD
Tamieka Howell, MD

Karen Isaacs, MD
Ronald Johnson, MD
Nia Johnson, MD
Kevin Johnson, MD
Audrey Jones, DO
Mary Jones, MD
Pulak Patel, MD and Jay Patel
Domenic Palagruto, DO
Bill Parker, MD
Shawn Parker
Steve Parker, JD
Peter Partee, MD
Robin Peace, MD

Margaret Pearce, MD
Edward Plyler, MD
Renda Powell
NCAFP members and supporters of the Academy are encouraged to make gifts of ongoing significance or annual contributions to the NCAFP Foundation. The following individuals and organizations contributed to the Foundation in 2024:



Bradley Propst, MD and Ashley Sedlak-Propst
Kathleen Punger, MD
Hannah Rayala
John Redding II, MD
Robert Rich, MD
Elizabeth Richards
Charles Rhodes, MD

Cecile Robes, DO
Donald Ruth, MD

Christopher Danford, MD
Andrea DeSantis, DO
Deanna Didiano, DO
Allen Dobson, MD
Shannon Dowler, MD
Matthew Drake, MD
Kawanta Durham, MD
Megan Easterday, MD
Suzanne Eaton Jones, MD, MPH
Fernando Escabi-Mendez, MD
Alison Evanoff, MD
Walter Ezeigbo, MD
Hannah Faeben, MD
Bert Fields, MD
Debbie Fields
Denise Finck-Rothman, MDR
Conrad Flick, MD
Terry Fokakis, DO


Brian Forrest, MD
Michelle Jones, MD
Jessica Kafer, MD
William Kelly, MD




Thomas Koinis, MD

Victoria Kaprielian, MD
Eugenie Komives, MD
Krista Kozacki, MD
Aaron Lambert, MD
Sarita Lavani, MD
Kelley Lawrence, MD
Katherine Lee, MD, MSPH
Yvonne Lowne-Chase, DO

Gerald Mabe, MD
John Mangun, MD
Alfred May, MD
Mallory Mcclester, MD
Brian McCollough, MD

Elizabeth Saft, DO
Bailey Sanford, MD, MDiv, MEd
Maria Santos, MD
Judy Schauer, DO
Allen Shepard, MD
James Shepherd, MD
Frankie Simmons, MD
Nadine Skinner, MD
John Smith, MD
Varshaba Songara, MD
Catherine Sotir, MD
Barbara Stagg, MD
Jessica Triche Staton, MD
Erika Steinbacher, MD
Amanda Steventon, MD
Ada Stewart, MD
Vickeima Sydney, MD
Ryan Taylor
Netra Thakur, MD


Maureen Murphy, MD
Stephen Musial, DO
Alisa Nance, MD
Claire Namboodri, MD
J. Thomas Newton, MD
Franklin Niblock, MD, MPH

Steve North, MD, MPH and Amanda North
Thomas Nowatka, MD
Tambetta Ojong, MD




Robert Toborg, MD

Elizabeth Trout, MD
Ying Vang, MD
Eugene Wade, MD
Edward Washington, MD
R.W. “Chip” Watkins, MD, MPH
Robert Wergin, MD
Nicholas Wells
Adam Wenzlik, MD
Craig White, MD
Thomas White, MD
Amanda Whitley, MD
Stephanie Wilcher, MD, MPH
Courtland Winborne, MD
Sondra Wolf, MD
Karen Wood, MD
Daniel Yoder, MD


Mississippi AFP Foundation





By Kevin LaTorre NCAFP Communications & Membership Manager
On Dec. 7, 2024, Dr. Nicholas Pennings received the NCAFP Distinguished Physician Award during a ceremony at the Winter Family Physicians Weekend in Asheville. The award is the Academy’s most prestigious honor, and Dr. Pennings earned it through his commitment to holistic patient care, clinical excellence, and mentoring medical students.
During the presentation of the award, NCAFP Immediate Past President Dr. Garett Franklin said, “While his clinical acumen alone could warrant this award, Dr. Pennings’s greatest achievements come from molding the next generation of physicians, particularly family physicians.”
Family Medicine after first learning it through years of practice, he says.
He completed his undergraduate degree at Cornell University, his medical degree at the Philadelphia College of Osteopathic Medicine, and then his Family Medicine residency at Parkview Hospital in Philadelphia, PA. From there, Dr. Pennings and his wife went to live in the town where they grew up, 60 miles west of New York City. He practiced Family Medicine there until he felt it was time for a change: “I was practicing for 22 years before I went into teaching,” Dr. Pennings says. “After my kids had grown up, I decided that I really wanted to teach.” Thanks to a long-time connection with Dr. John Kauffman (the founding dean at CUSOM), Dr. Pennings ended up in Lillington, NC.

Dr. Pennings treats patients in Lillington and also serves as the Family Medicine Chair at the Campbell University School of Medicine (CUSOM), where he is the faculty advisor for the CUSOM Family Medicine Interest Group. In both of these roles, Dr. Pennings provides opportunities for medical students interested in Family Medicine to experience the specialty through CUSOM curriculum, educational events, and in-clinic shadowingmore. He even opens his own clinical workdays to the students and residents who want to receive his hands-on mentorship.
Dr. Pennings originally came to North Carolina to teach
“When John became the Dean, he invited me to be part of the department,” he says. “It was part-time for two months, and then it was full-time and I was running the health center. And then three years later, I became vice chair. Four years later, I became chair.” Based on the work he has done at Campbell, this growth makes sense: “Luck is when preparation meets opportunity, and I felt like I worked hard to establish myself. And when the opportunities came, I was very fortunate to be where I was but also to be prepared to step into these roles.”
When Dr. Pennings became Vice Chair of the department, he became more involved with the medical students. “What first excited me about coming to Campbell was the chance to work with students and share my experience as a clinician,” he says. “I could bring a lot of real-world, Family Medicine experience, which has helped me to introduce students to Family Medicine.”
Under his leadership, hundreds of CUSOM students have entered Family Medicine. “I’m very proud of how many students that we’ve matched into Family Medicine for the past few years,” Dr. Pennings says. “To be a part of that has really been just a wonderful experience.”
Testimonies from the Campbell medical students who nominated Dr. Pennings for his NCAFP award say that their experience has also been wonderful, thanks to his influence. “One can tell he genuinely cares about our well-being and wants to see us all succeed,” they wrote in a letter. “He has all the qualities of a great educator, sets a great example, and above all else deeply cares for his students and patients.”
Care for his patients led Dr. Pennings to take up and teach obesity medicine, in addition to Family Medicine.
Beyond Family Medicine, he is also board-certified in obesity medicine, and he first pursued that training because he saw first-hand how obesity worsened his patients’ health. “I saw my patients getting heavier and having a lot of complications from their obesity,” Dr. Penning says. “But when I started a program in my practice that helped them lose weight, I saw all these improvements in their health. To me, that was the perfect way to help people get healthier.”
Seeing these real benefits to his patients, Dr. Pennings wanted to teach obesity medicine to medical students so their future patients would receive the same benefits. “No medical schools for Family Medicine had any obesity educa-
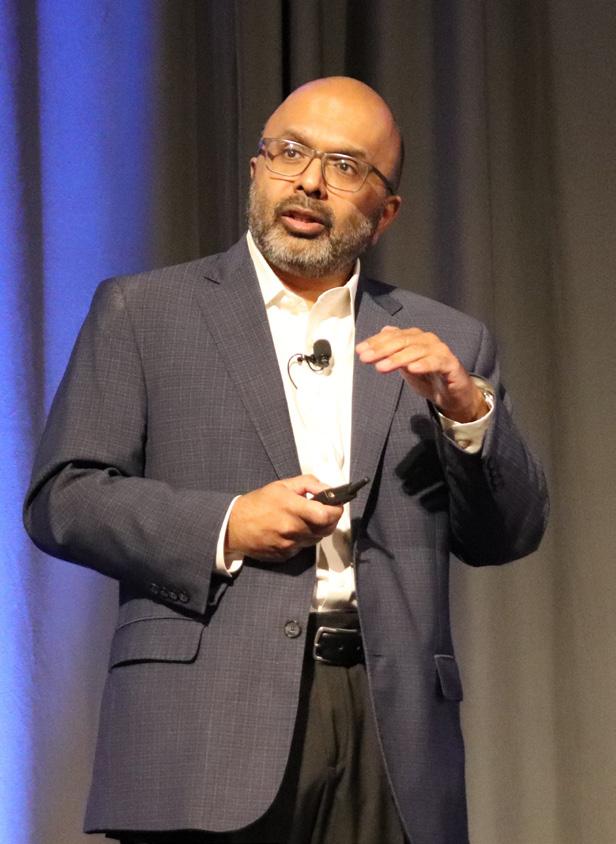
Dr. Devdutta Sangvai Installed as NCDHHS Secretary
tion as part of their curriculum,” he says. “It just wasn’t taught, even though obesity is the most common thing we see now.”
But Dr. Kauffman gave him the chance to teach obesity medicine at CUSOM, Dr. Pennings says: “That was one of the things that inspired me to come to Campbell. I trained to become board certified in obesity medicine before I started teaching it, and then we started incorporating that training into the curriculum. It has resonated well with the medical students.”
Dr. Pennings also expanded this obesity-medicine training beyond CUSOM through Think Healthy, the coaching program he founded and leads. Think Healthy trains health care professionals to coach their patients on losing weight and creating healthier mindsets, in addition to healthier outcomes. Its work, combined with his leadership at CUSOM, is what Dr. Pennings most values as a family physician and teacher: “My next real mission is to help family physicians integrate obesity medicine into their own practices,” he says. “It’s not easy to do, because it takes time. It’s going to be a process to make this skill more accessible to family physicians and students.”
Hospital, vice president for Population Health Management at Duke University Health System, and president of the NC Medical Society in 2013. He has also been an NCAFP member since 2001.

On Dec. 16, NC Gov. Josh Stein announced that NCAFP member Devdutta Sangvai, MD, JD, MBA would become the new secretary of the NC Dept. of Health and Human Services (NCDHHS). “I am looking forward to Dev’s leadership at the Department of Health and Human Services,” said Gov. Stein. “He is incredibly hard-working, knowledgeable about health care, and ready for the challenges of improving health and lowering health costs for people all across our state.”
Dr. Sangvai (pictured) is a professor of Family Medicine, pediatrics, and psychiatry at the Duke University School of Medicine. He serves as president of the NC Medical Board and has previously served as president at Duke Regional
“We are thrilled that Dr. Sangvai has been named Secretary of the Department of Health and Human Services,” said Greg Griggs, NCAFP EVP and CEO. “He brings the unique perspective of a family physician to the role, able to examine the health care issues of today from an individual patient level and from a population health perspective. Dr. Sangvai truly brings a unique set of experiences and expertise to the position.”
On Jan. 12, Dr. Sangvai was sworn in. “I am honored to lead the Department of Health and Human Services and build on the already strong foundation toward creating a healthier North Carolina for all,” said Dr. Sangvai said. “I look forward to working with the incredible team at NCDHHS and Governor [Josh] Stein to ensure every North Carolinian has access to the right services to support their health, safety and well-being – no matter where they live or how much money they make.”
continues on next page

Past NCAFP President Dr. Karen L. Smith has joined the National Advisory Committee on Rural Health and Human Services at the U.S. Dept. of Health and Human Services (HHS)! In the invitation which outgoing HHS Secretary Xavier Becerra sent to Dr. Smith, Becerra wrote, “It is my pleasure to invite you to serve as a member of the [committee] for a four-year term.”
According to the committee’s charter, Dr. Smith (pictured) and the other committee members will “focus attention and existing resources on rural health and human service problems, such as the provision and financing of health care and human services in rural areas.” In addition to reporting on key health care issues in rural communities, the committee will also coordinate at the federal level to advise on solutions. Dr. Smith, who in 2023 received the Larry Wooten Rural Leadership Award for her 31 years of community service in Raeford, knows plenty about the medical needs and obstacles which rural patients face. We at the NCAFP look forward to what she can accomplish alongside her fellow committee members.

NCAFP member Dr. Emma York Vomer has been named to the American Academy of Family Physicians (AAFP) Delegation to the American Medical Association! Dr. Vomer (pictured) received a message of congratulations from AAFP President Dr. Jen Brull: “You have been appointed to the AAFP AMA Delegation,” Dr. Brull wrote. “It is through the hard work of dedicated members like you who accept leadership roles that we are able to accomplish our goals. I look forward with pleasure to working with you during this year while I am serving as President.”
The delegation term began Dec. 15 and will last until Dec. 14, 2025. Congratulations, Dr. Vomer!

In November 2024, past NCAFP president Dr. Thomas Koinis delivered two sessions to over 680 attendees at the International Council on Active Aging (ICAA) Conference in Raleigh. His lunchtime session, “How Flu, RSV, and COVID infections impact you and your community,” was a hit, according to the ICAA and to Dr. Koinis. “I had a great time,” he said. “Quite nice to have a captive audience since they were eating their lunch as I talked!”

Two NCAFP members and leading family physicians, Dr. Chip Watkins and Dr. Jana Watts, recently joined with World Central Kitchen to provide food to those communities impacted by Hurricane Helene. “Slinging hash with Jana was fun today,” Dr. Watkins told the NCAFP. “We both have been supporters of World Central Kitchen for years, but neither of us thought we’d be serving meals to our neighbors in Asheville.” Dr. Watkins is a past NCAFP president, and Dr. Watts is a former NCAFP board member. Both continue to lead and serve in their community, which especially needs that work in this time of recovery. Thank you to Dr. Watkins and Dr. Watts!
Capstone Donors ($500K+)


Truss Donor ($250K+)

Cornerstone ($50K+)

Blueprint Donors (Up to $10K)

Belmont Savings Bank • HomeTrust Bank • Triangle Wealth Management
Mentor Donors ($50K+)
Dr. Allen Dobson • Dr. Mary Hall & Dr. David Hall • Dr. & Mrs. Thomas Koinis • Dr. Maureen Murphy & Mr. Scott Maxwell • Dr. Thomas White
Advocate Donors ($25K+)
Drs. Eugenie Komives & Rex Bentley • Dr. Robert L. (Chuck) Rich, Jr.
Ambassador Donors ($10K+)
Dr. Christopher P. Danford
Dr. & Mrs. William A. Dennis
Dr. L. Allen Dobson
Dr. Johnny Bagwell
Dr. Amir Barzin
Dr. Rhett Brown
Dr. Joshua Carpenter
Dr. Lisa Cassidy-Vu
Dr. Richard Adelman
Dr. Robert Agnello
Dr. Kira Alatar
Dr. Christina Albert
Dr. Chelly Alexander
Dr. D. Landon Allen
Dr. Michael Alston
Dr. Christina Anderson
Ms. Kathryn Atkinson
Dr. Amanda Austin
Dr. David Baker
Dr. Erin Baker
Dr. Robert Barnabei
Dr. Monica Barnes-Durity
Dr. Kathleen Barnhouse
Dr. Sanjay Batish
Dr. Ted Bauman
Mr. Morgan Beamon
Dr. Gary Bean
Mr. David Belinke
Dr. Mary Bengtson
Dr. Mary-Emma Beres
Dr. Janalynn Beste
Dr. Muhammad Bhatti
Dr. Holly Biola
Dr. & Mrs. Mott Blair
Dr. Victoria Boggiano
Dr. Karolen Bowman
Dr. Akhila Boyina
Dr. Dalia Brahmi
Dr. Kirsten Bray
Dr. Regina Bray-Brown
Dr. David Brendle
Dr. Caroline Brewster
Ms. Melinda Brown
Dr. Samantha Brothers
Dr. Ed Bujold
Dr. Cristopher Bullers
Ms. Amy Burger
Mr. Mark Bushhouse
Dr. Donna Capps
Dr. Michele Casey
Dr. Dawn Caviness
Dr. Eric Chen
Ms. Sara Cotten
Dr. Caroline Coward
Dr. Vanessa Crerar
Dr. Mark Crissman
Dr. Gary Curran
Dr. Madeleine Cutrone
Dr. Samuel Dail
Mr. Mark & Mrs. Diane Darrow
Dr. Lavanya Desai
Dr. Andrea DeSantis
Dr. Shannon Dowler
Dr. Matthew Drake
Dr. Kawanta Durham
Mr. Megan Easterday
Dr. Suzanne Eaton Jones
Dr. Ken Edel
Dr. Howard Eisenson
Dr. Fernando Escabi-Mendez
Dr. Walter Ezeigbo
Dr. Hannah Faeben
Dr. Karl “Bert” Fields
Mr. Shane Flaherty
Dr. Conrad Flick
Dr. Clewell “Cy” Fogleman
Dr. Terry Fokakis
Dr. Brian Forrest
Mr. Greg Griggs
Dr. Shauna Guthrie
Dr. Dimitrios Hondros
Ally Donors ($5K+)
Dr. Deanna Didiano
Dr. Allison M. Evanoff
Dr. Jim Jones & Dr. Michelle F. Jones
Dr. Rich Lord & Dr. Pat Lord
Dr. S. Mark McNeill
Dr. & Mrs. Tommy Newton
Friend Donors (Up to $5K)
Dr. Vickie Fowler
Dr. Garett Franklin
Dr. Joanne Fruth
Dr. Randall Gehle
Dr. Deepak Gelot
Dr. Sofia Gkoulgkountina
Dr. Jason Glass
Dr. Anne Gonzalez
Dr. Renee Goodson-Ollivierre
Dr. Donald Goodman
Mr. Andrew Griggs
Dr. Katherine Haga
Dr. Caleb Hancock
Dr. Michael Harris
Dr. William Hedrick
Dr. Lori Heim
Dr. Margaret Helton
Dr. Douglas Henley
Dr. Casey Henritz
Dr. Mark Hester
Dr. Terry Hess
Dr. Melissa Hicks
Dr. Tamieka Howell
Dr. Kevin E. Johnson
Dr. Nichole Johnson
Dr. Ronald Johnson
Dr. Audrey Jones
Dr. Mary Jones
Dr. Victoria Kaprielian
Dr. Susan Keen
Dr. Krista Kozacki
Dr. Aaron Lambert
Dr. Kathryn Lawrence
Dr. Kelley Lawrence & the
Rev. D. Robert Lawrence & Family
Dr. Frank Leak
The Chuck Lewis Family
Dr. Shelly Lowery
Dr. Yvonne Lowne-Chase
Dr. John Mangum
Dr. Amy Marietta
Dr. J. Paul Martin
Dr. Alfred May
Dr. Brian McCollough
Dr. Robert McConville
Ms. Marion McHugh
Mr. Ken Melton
Dr. Jon Kyle Melvin
Dr. Paul Meyer
Mr. Bryce Miller
Ms. Corinna Miller
Mr. S. Evan Morgan
Ms. Joy Mothorpe
Dr. Jennifer Mullendore
Dr. James Muller
Dr. Stephen Musial
Dr. Sara Neal
Dr. Franklin Niblock
Dr. Steve North
Dr. Thomas Nowatka
Ms. Kelly Ogrin
Dr. Tambetta Ojong
Dr. Swapna Omraju
Dr. Domenic Palagruto
Ms. Heather Palmer
Ms. Janice Paris
Dr. Morgan Parker
Mr. Shawn Parker
Mr. Steve Parker
Dr. Peter Partee
Dr. Alisa Nance
Dr. Bradley Propst & Mrs. Ashley Sedlak-Propst
Dr. David Rinehart
The Pennings Family Charitable Fund
Dr. & Mrs. J. Carson Rounds
Dr. Christopher Street
Dr. Erin Wagner & Mr. Sean Wagner
Dr. Tom Wroth
Dr. Jay Patel & Dr. Pulak Patel
Dr. Dean Patton
Dr. Robin Peace
Dr. Edward Plyler
Ms. Renda Powell
Dr. Tanya Pratt
Dr. Kathleen Punger
Ms. Hannah Rayala
Dr. John Redding II
Mr. Dave Richards
Ms. Elizabeth Richards
Dr. Cecile Robes
Dr. Mark Robinson
Dr. Wesley Roten
Dr. Charles W. Rhodes
Dr. Donald Ruth
Dr. Elizabeth Saft
Dr. Bailey Sanford
Dr. Maria Santos
Mr. John Sauer
Dr. Judy Schauer
Dr. Allen Shephard
Dr. James Shepherd
Dr. Benjamin F. Simmons III
Dr. Nadine Skinner
Dr. John Smith
Dr. Richie Smits
Dr. Varshaben Songara
Dr. Neil Sparks
Dr. Barbara Stagg
Dr. Jessica Triche Staton
Dr. Erika Steinbacher
Dr. Michael Steinbacher
Dr. Beat Steiner
Dr. Amanda Steventon
Dr. Ada Stewart
Mr. Stephen & Mrs. Kathy Stilwell
Dr. Sharon Swede
Dr. Vickeima Sydney
Dr. Paul Sykes
Dr. Netra Thakur
Dr. Robert Toborg
Dr. Elizabeth Trout
Ms. Teresa Van Duyn
Dr. Ying Vang
Dr. Anthony Viera
Dr. Talia Vogel
Dr. Eugene Wade
Dr. Thomas Ward
Ms. Nancy Washburn
Dr. R. W. “Chip” Watkins
Dr. Jana Watts
Dr. Edward Washington
Dr. David Wells
Mr. Nicholas Wells
Dr. Adam Wenzlik
Dr. Robert Wergin
Dr. Craig White
Dr. Amanda Whitley
Dr. Stephanie Wilcher
Dr. Gustav Wilde
Dr. Patrick Williams
Dr. Courtland Winborne
Dr. Cynthia Witt
Dr. Karen Wood
Ms. Colleen Yang
Dr. Daniel Yoder
By Perry Price NCAFP Workforce Initiatives Manager
Like most things in our world, Family Medicine is evolving rapidly. The expectations of family physicians are also evolving – both from your patients and also from yourselves.
All these changes can be challenging to navigate, whether they are workforce challenges, AI integration, or shifts in care models. But one way to ensure that you’re remaining in the know is to welcome medical students into your practice. The best way for a potential family physician to understand the intricacies and wonders of Family Medicine is to spend time in real-world practice settings, and to build relationships with practicing family physicians. Yet, having medical students also benefits you. Medical students bring new perspectives and ask questions that force self-reflection and self-evaluation, while also bringing fresh energy into any clinic. We asked four of our own Summer Preceptors to share a bit about their experiences and why they decided to get involved.
Andrew Nance, MD Medical Director | Atrium
Medicine
“Wake Forest University medical student Jaelen King already planned to spend a summer with me researching the impact of my Lifestyle Medicine at Home program. Thanks to the NCAFP summer externship program, we took it a step further to make sure Jaelen could see firsthand that family physicians like me provide care in the clinic, in the hospital, at the home, and in groups. For a variety of reasons, I feel that medical students may wrongly assume that primary care is straightforward. It’s easy to be distracted by all of the specialties and technology. I think our time together helped Jaelen recognize that Family Medicine is the specialty for building relationships with patients. I found our time together to be rewarding, because Jaelen was engaged at a level that made me feel that what I taught him could impact his practice for decades to come.”
“Precepting is such a joy. There is hard work, planning, and patience that goes into it, AND there is so much good that comes from time given to those in training. Simply, it is the idea of giving back to the community in which you were able to train. I had the pleasure of precepting first-year medical student Zoe Green from the Brody School of Medicine in the summer of 2023. She stayed in my home while we spent two weeks together in my clinic. She came to the experience ready to learn, and she even taught me about her recent experience with lifestyle medicine and how beneficial it is to incorporate that knowledge into my patient care. My patients loved having her, and I was re-energized in teaching her for those two weeks. We were all there once, and those in training deserve enthusiastic preceptors, to continue to demonstrate the richness of Family Medicine.”
“I decided to serve as a summer preceptor for the NCAFP summer program to share my experience as a full-time family physician with a medical student. I love the setup of this program and that it allowed me to share my work life as well as my home with a medical student. My student, Alex, was able to have a glimpse into my work as a family physician and the importance of relationships and Family Medicine. We develop such close meaningful relationships with our patients, their families, and nearby specialty physicians. We have the opportunity as family physicians to see patients when they are doing well and celebrate with them. We also have the opportunity to heal and advocate for patients when they are not doing well.
“One of my favorite parts of this program was the ability to show my student what my life is like outside of the office. Since he spent an entire week with me, he was able to see the work-life balance that I have as an outpatient family physician. I am able to exercise, travel, and engage in my favorite hobbies (including dog training and pottery) due to the balance I have in both my work and home life. I absolutely love being a family physician, and it was an incredible experience to be able to share this with a medical student early on in their experience. I look forward to having another student join me again this coming summer.”
Brittany Hipkins, MD Blue Ridge Health | Sylva
“This past summer, I was offered the opportunity to be a host and preceptor for an NCAFP program, and I immediately jumped at the chance to ‘pay it forward’ after all the support I received from the NCAFP during my med school years. During the week, the incredibly bright and eager student I was matched with shadowed my full-spectrum Family Medicine clinic in rural western NC and spent time with my family after hours to see what being a ‘real-life’ family doc is like.
“This experience really helped remind me of some of the reasons that I love Family Medicine so much. I think it’s
easy to get bogged down in the daily minutiae of clinic. Hosting a student in such an immersive week helped me see the specialty through their fresh eyes. It gave me the opportunity to slow down and appreciate the joys of Family Medicine, and I highly recommend the experience.”
There are endless ways to engage with medical students, as well as endless need. We are in the midst of a preceptor shortage in North Carolina, and the need for family physicians in our state only continues to grow. The work of the NCAFP Foundation and its mission to support the advancement of Family Medicine starts with fostering student interest in the specialty. Can you find a way to precept a medical student and support their crucial future in Family Medicine?
By Joel Edwards, MD
Carolina Honduras Health Foundation Board President
In September I got to lead a medical mission trip to Limon, Honduras with Carolina Honduras Health Foundation (CHHF). CHHF is a nonprofit organization that works collaboratively with the communities in the district of Colón. Our mission is to improve overall health via health education, community development, medical referrals, and primary care clinics.
I have been going on short-term medical mission trips at least once a year to this same area since 2001 (except the COVID years, during which CHHF started telemedicine). During that time, seeing the incredible improvement in the health status of the people of Limon has been a true blessing to me. CHHF has been able to expand services to nearly 10 smaller towns and villages in the district of Colon.

Using short-term medical mission teams, telemedicine, and medical referrals, CHHF provides free medical, dental,
ophthalmological, and pharmaceutical services to the poor and needy in several small towns in Colon. Ongoing health education and community development projects increase knowledge and support lifestyle changes to increase healthy choices.
Short-term medical mission teams are comprised of physicians, advanced care practitioners, nurses, dentists, pharmacists, translators, lab technicians, and other supporting staff. Each year, we send 18 to 19 trips to Limon and the surrounding areas. On our most recent trip, our team consisted of two physicians, two nurse practitioners, two nurses, a dentist, an EMT, a pharmacist and two other support staff.
After months of preparation that included recruiting team members, ordering medications and supplies, scheduling continues on next page

flights, working on logistics both in the United States and Honduras, and many prayers, we were ready for our medical mission trip to Honduras. Fortunately, all of our flights to San Pedro Sula were routine and arrived on time.
However, our first major problem began when we learned that the Honduran government had not processed the needed paperwork, though we had sent in our required documentation months in advance. Unfortunately, this kept our team from bringing our medications and medical/dental supplies through customs. After several conversations with the airport staff and our in-country support staff, we left everything at the airport. (Eventually, these supplies would arrive on our last day at the clinic in Limon. Fortunately, the pharmacy and dental room were adequately supplied so that we could function without these supplies.)
After picking us up at the San Pedro Sula airport, our Honduran director, Pastor David Kelly, drove us nearly four hours to our hotel in La Ceiba for our first night. But in the morning, we awoke to another problem: no water in the hotel — meaning no showers and no breakfast. However, the water issue was quickly fixed, and so we were eventually able to shower and eat the typical Honduran breakfast of eggs,
beans, sausage, fruit, and coffee at the last minute.
Back on the road, we made another four-hour ride to our clinic in Limon. The paved road had lots of potholes, and the last 25 miles were dusty, rough dirt roads. On arrival in Limon, we were warmly greeted by the CHHF Honduran staff who would be part of our family for the next six days. After dinner, we had a team meeting to discuss preparations for seeing patients the next day. Our last job was to ensure that everyone was OK both emotionally and physically. They all were, despite the travel!
After breakfast the next day, we made final clinic and pharmacy preparations. The primary CHHF clinic was amazingly well supplied with medications, and the exam rooms were spacious and equipped with window air conditioners. The dental room was also well equipped and comfortable. As expected, there was a crowd of children and adults waiting to be seen hours before the clinic started. Patient flow went well. The Honduran people exude patience and are used to long waits. In general, patients seen in all our clinics had similar needs. Children typically have parasites, mal-
nutrition, skin disorders (particularly scabies), insect bites, wounds, asthma, anemia, and fever. Adults have similar problems, plus multiple chronic illnesses such as diabetes, hypertension, and heart failure. In recent years, we have been able to treat these chronic illnesses through sending multiple mission teams and the use of telemedicine.
Dr. Wham, the first dentist to join the CHHF team in quite some time, was very busy with extractions, restorations, and dental education. Since our clinic has an existing dental room, he worked in our primary clinic throughout the week and treated patients there.
The following morning, we began our three remote clinic days: first in Icoteas, then in Plan de Flores, and then in Toujica. On remote clinic days, we have to bring all the medications, supplies, and equipment that we expect to need. Throughout these days, we had none of the amenities in Limon — no air-conditioned exam rooms, flushable toilets, exam tables, or reliable electricity. Here are some of the things we enjoyed and did during our remote clinic days:
• In all three towns, we were greeted by large crowds of adults and children glad to see us.
• In Icoteas, we saw over 100 patients.
• We treated more skin infections with scabies and lice, since in these rural areas they are more common.
exposed bone in the upper left tibial area. We gave him an IV and cefuroxime, irrigated and dressed the deep wound, splinted his leg, and arranged transportation to a hospital two hours away.


• Unlike in years past when using birth control was opposed by the Catholic Church in Honduras, many women asked for birth control pills. Also, many women had received injectable birth control from the government clinic and had many questions about irregular menses.
• After a busy day in Plan de Flores, we had a true emergency come to the Limon clinic just as we were sitting down for dinner. A local man who had just crashed his motorcycle was brought to the clinic by his family. Everyone quickly left dinner to respond to this emergency. After the appropriate ABC evaluation, he was found to have deep abrasions over much of his body. The worst injury was a deep wound with
• In Toujuca, we saw 225 patients. Afterward, the school staff thanked us for coming and asked us to return. The school percussion band had been practicing for the upcoming local Independence Day parade and took time to play and march for us!
Back in Limon after our remote clinic days, we saw fewer patients than on other days. In earlier years, we were often overwhelmed with patient needs. However, the health of the town has remarkably improved since that time. There has been some improvement in access to health care locally, and the economic status has improved. After a busy morning seeing patients and closing up the clinic, we were able to rest and relax for the afternoon.
After our last breakfast in Limon, we said our good-byes to the staff at the clinic and started the four-hour drive to our lodge near La Ceiba. Together with other CHHF team leaders, I believe that a day of rest and relaxation after a long week of work is a good end to our mission trip. This trip, we stayed at a lodge nestled in the forest adjacent to the Congrejal River.
In order to avoid getting delayed, we were up early the next morning. Our Honduran director picked us up at 5 a.m. for our four-hour trip back to the airport in San Pedro Sula. Flights back home were on time, and so we arrived in Greensboro just before midnight, where the church bus was waiting on us to bring us back to Mocksville. What a wonderful 10 days for our patients and our team!
If you would consider going on a future medical mission, please contact us at www.CHHF.org. You are also welcome to contact me directly at joeledwardsmd@gmail.com.
By Stephanie Wilcher, MD NCAFP 2024-25 Resident Director
In December 2024, I had the privilege of attending the NCAFP Winter Family Physicians Weekend. The Winter Weekend has been a highlight for me each year throughout my medical training journey: this past event was my third time attending as a resident, after I had already attended twice as a medical student. As always, it was truly an enriching experience. It provides an invaluable opportunity to deepen one’s understanding of the diverse and evolving landscape of primary care by providing excellent lectures and connections with vendors.
I was able to network with many of these lecturers and vendors, who graciously offered to come to my residency program to share their expertise with my peers during our didactic time. I was also able to network with my peers in formal and informal settings. Alongside Dr. Morgan Parker (the outgoing NCAFP resident director), I led the resident section meeting, where we had a discussion with the residents in attendance that allowed them to share their experiences and discuss the challenges they face in their perspective programs. I shared with them all the Academy has to offer, from insurance plans to scholarship opportunities. It was great reconnecting with familiar faces and meeting new ones to continue fostering these great connections with my peers and mentors.
hind-the-scenes look at how decisions are made at a higher level within the field. I gained insight into the strategic priorities of the NCAFP, the policies shaping Family Medicine, and the challenges which family physicians and their institutions face. The discussions were thought-provoking, and it was inspiring to see leaders in the field collaborate and advocate for improvements in training, patient care, and health care policy. I look forward to attending the next Board meetings in February, June, and December (during the next Winter Meeting!).

As Resident Director, I look forward to serving as a voice for my fellow residents and contributing to the advancement of Family Medicine in our state. I look forward to advocating for better educational resources, promoting resident wellness, and fostering a supportive community where residents can connect, collaborate, and learn from one another. Much of this is facilitated through the resident section meeting, as I had mentioned. But another great opportunity to practice this goal is through a new opportunity for residents that the NCAFP offered during this recent Winter Weekend: the Chief Resident meeting. I attended this meeting and joined the Chief Residents from seven different programs across North Carolina to understand their issues and celebrate their successes. It was great seeing everyone build relationships and workshop ideas for one another’s programs. I will be able to attend the next chief meeting in February. I look forward to reuniting and learning how things changed for their programs after our last meeting. These collaborations are the strength of the Winter Family Physicians Weekend.
As I mentioned above, I have attended this conference as a medical student and a resident, and in December I will go as an attending physician. The Winter Family Physicians Weekend is an inspiring and informative event that provides a platform for learning, networking, and collaboration. Each year it serves as a reminder of the importance of staying engaged with the broader medical community and contributing to the ongoing growth and improvement of the field. I am so grateful to have attended this conference over the years, and I am so proud to be a part of this academy as your Resident Director.
I was also able to attend the Board of Directors meeting in my new role as Resident Director. Attending this meeting was a unique and eye-opening experience. It offered a be-
Congratulations to the following members who took office during the installation ceremony during the Presidential Gala:
• Dr. Mark McNeill as the 2024-25 NCAFP President
• Dr. Benjamin “Frankie” Simmons as the 2024-25 NCAFP President-Elect
• Dr. Deanna Didiano as the 2024-25 NCAFP Secretary-Treasurer
• Dr. Landon Allen as an NCAFP At-Large Board Member
• Dr. Stacey Blyth as an NCAFP At-Large Board Member
• Dr. Lisa Cassidy-Vu as an NCAFP At-Large Board Member (second term)
• Dr. Kelley Lawrence as an NCAFP At-Large Board Member (second term)
• Dr. Patrick Williams as an NCAFP At-Large Board Member (second term)
• Dr. Tamieka Howell as an AAFP Delegate
• Dr. Rhett Brown as an AAFP Alternate Delegate
• Dr. Stephanie Wilcher as the 2024-25 NCAFP Resident Director
• Dr. Irina Balan as the 2024-25 NCAFP Resident Director-Elect
• Nicholas Wells as the 2024-25 NCAFP Student Director
• Ryan Taylor as the 2024-25 NCAFP Student Director-Elect
Meanwhile, NCAFP award ceremonies throughout the meeting gave recognition to leaders in NC Family Medicine, teaching, public health, and research. One of those leaders was Dr. Nicholas Pennings, who received the NC Distinguished Family Physician Award for his committed patient care and teaching. During his acceptance speech, Dr. Pennings thanked his supporters and said, “The NCAFP has been integral to so many students entering Family Medicine.”
In addition, NC Dept. of Health and Human Services (NCDHHS) Chief Medical Officer and State Health Director Dr. Betsey Tilson received the NCAFP Public Service Award during the Presidential Gala, for her longtime work bridging behavioral health, child and family well-being, and social drivers of health. During her tenure at NCDHHS, Dr. Tilson helped lead the state through
COVID-19 and the recent response to Hurricane Helene, and the NCAFP was pleased to recognize her tireless effort and leadership.
We were glad to host all our attendees, guest faculty, and vendors throughout the event. We are grateful for your efforts and input, because the meeting wouldn’t happen with all of you in attendance. “Greatest conference in the world!” said one attendee.
“I want to extend my deepest thanks to all the individuals and teams who played a part in making this weekend such a tremendous success,” said Kathryn. “This much-anticipated event wouldn’t have been possible without the incredible guest faculty and their timely, relevant CME sessions, as well as the generous support from our sponsors, vendors, and all those who champion Family Medicine. A special thank you goes to the Omni Grove Park Inn and their attentive staff for their exceptional service and hospitality, and to the Pinnacle AV, Alloy Sound, and EZAV teams for producing the NCAFP’s first-ever (and very successful) hybrid conference. I also want to express my sincere appreciation to our program chairs, Dr. Tom White and Dr. Katie Haga, for their tireless work and commitment in crafting another exceptional program. Lastly, a big thank-you to the 800+ attendees who joined us in-person and virtually for a weekend filled with professional development, connection, and camaraderie.”
We would also like to thank the sponsors who supported the 2024 Winter Family Physicians Weekend and made it possible to bring so many attendees back to Asheville: Novant Health, Community Care of North Carolina, Healthy Blue NC, Curi, Novo Nordisk, Abbvie, WellCare of North Carolina, Avance Care, Carolina Complete Health, Molina Health, CVS Accountable Care, UnitedHealthcare Community Plan, Aetna Health, Amerihealth Caritas of NC, Hopscotch Primary Care, NC-PAL, Holologic, and NC Area Health Education Centers.
And be sure to mark your calendars now for the 2025 Winter Family Physicians Weekend in Asheville on Dec. 4-7.
“We can’t wait to see everyone again next year as we continue to raise the bar for this annual event,” Kathryn said.
By Josiah Irvin and Robert Shaw
Attorneys at Smith, Anderson, Blount, Dorsett, Mitchell & Jernigan, LLP
Last fall, the North Carolina Medical Board published online guidance titled, “Lessons from NCMB’s Disciplinary Committee: Are you aiding the unlicensed practice of medicine?” (You can review it at https://www.ncmedboard.org/ resources-information/professional-resources/publications/ forum-newsletter/article/print/lessons-from-ncmbs-disciplinary-committee-are-you-aiding-the-unlicensed-practiceof-medicine)
The guidance largely serves to emphasize the Board’s existing concerns regarding the corporate practice of medicine in North Carolina and articulates the potential for unlawful “straw” practices and other inappropriate arrangements where the licensee is essentially “rent[ing]” her license to a business that otherwise could not provide medical services. In addition, in a potential expansion, the guidance indicates that physician supervision of individuals employed by a non-licensed entity, standing alone, can trigger corporate practice of medicine concerns. This article summarizes that guidance and offers some takeaway tips for physicians.
The guidance centers on a case study of conduct that likely warrants Board sanctions against the at-issue physician. Specifically, an experienced physician agreed to serve as a “medical director” of a med spa, pursuant to an employment agreement for which he is paid $2,000 per month, but he is assured that he does not need to be on site. All the physician appears to be doing is collecting checks. The med spa is owned and operated by a non-licensed individual, and it uses nurse practitioners (“NPs”) and physician assistants

(“PAs”) to provide clinical services. The physician does not know that he is the supervisor for the NPs and PAs. Inevitably, a patient is harmed, a complaint is filed with the Board, and both the treating PA and the physician are subject to Board investigation and presumed sanction.
Thus, guidance links the issues of physician supervision and corporate practice of medicine. If a physician formally or informally supervises an PA or NP employed by a non-licensed entity, then the physician is potentially implicated in the unlawful medical care provided at the non-licensed entity — even if the physician herself does not perform any direct medical care at the non-licensed entity. This appears to expand the reach of the corporate practice doctrine, giv-
en the ubiquitous utilization in North Carolina of PAs and NPs under supervision by third-party physicians.
The guidance also lists other ownership and employment arrangements that are viewed as inappropriate and unlawful in North Carolina. In addition to the scenario above (i.e., a medical spa directorship where the physician medical director had no active role in the med spa), the guidance also finds concern with:
• Arrangements where the licensee is involved in the practice, even on a full-time basis, but has little autonomy to determine how care is provided, because “treatment protocols are dictated by the non-licensed owners.”
• A “straw ownership” arrangement, where the physician is made the sole shareholder of a “practice controlled and operated” by a non-licensed person. The guidance regards management agreements that “results in the bulk of the practice’s revenue going to the non-licensee” as indicia of unlawful straws arrangement.
• A physician acquiring the titular ownership or becoming the sole shareholder of a medical practice or business, without investing money, property, or anything else of value.
• Arrangements where the physician has no meaningful responsibilities or duties, such that the substance of the agreement is just an unlawful rental of a professional license to a non-licensed entity.
While the guidance largely serves to emphasize, and conforms with, existing Board policy and enforcement activity, some takeaways for the physicians and other health care industry participants in North Carolina include:
1. An arrangement where a non-licensed entity employs PAs or NPs, who are supervised by a third-party physician, can potentially run afoul of the North Carolina corporate practice of medicine prohibition, especially if the physician has little or no role in the clinical operation.
2. The Board will likely carefully scrutinize physician practices’ arrangements with third-party management companies, to assess whether they amount to unlawful “straw” arrangements. In particular, the guidance makes clear that this review is likely to assess the actual clinical involvement or economic risk on the part of the physician owner. For
example, professional entity ownership arrangements with respect to clinical enterprises for which the owning physician lacked prior involvement may be higher risk.
3. Management agreements which provide for significant payments to third-party management service organizations are common in the health care industry. Participants in these arrangements need to structure them carefully to ensure that “control and decision-making authority” remain with the licensees.
4. The Board regularly investigates and sanctions licensees for violations of North Carolina’s actively enforced corporate practice of medicine prohibition. But the issuance of the guidance may signal a heightened Board enforcement priority.
As part of the Smith Anderson Health Care team located in Raleigh, Josiah and Robert regularly advise clients on North Carolina corporate practice of medicine matters, including transaction structuring, proactive compliance, and Board investigation responses.
Josiah provides advice to physician practices and other health care enterprises on a wide variety of other corporate and regulatory issues, including Stark Law and Anti-Kickback Statute compliance; HIPAA and other privacy laws; licensure requirements; relationships with payors; contracting with vendors, personnel and other health care business; and practice sales and affiliations.
Robert is co-chair of the health care practice and has extensive experience advising physician practices and health care clients on value-based care, strategic planning, mergers and acquisitions, reimbursement, tax planning, and navigating the regulatory landscape.
INAUGURAL continued from pg. 7
we will adapt, we will innovate, and we will do it together.
Which brings me to the next thing this Hurricane has taught me – you also get through challenging times by relying on your support network.
Let me tell you more about my support network. It begins with my neighbor Dennis Seely, a retired physician assistant who had a career in Family Medicine in rural Western North Carolina. Dennis is a jack-of-all-trades and can fix anything. Not very far from the street Dennis and I live on, is a block of low-income housing called Mountain Spring Apartments. Guess what is in the woods behind Mountain Spring Apartments? Yes, a mountain spring.
Dennis would use a pump and lots of PVC pipe to get that spring running into large water containers, providing flushable water for the residents of Mountain Springs. That was a big deal in October. What was also a big deal was that Dennis was one of the few houses that still had electricity. I would store my vaccine fridge in his garage, saving my office tens of thousands of dollars and allowing my patients to still have access to vaccines in October. When NCDHHS would send a temporary employee to help my office, she would stay in Dennis’s AirBnB. Dennis really adapted to meet the needs of his community. It should come as no surprise that he had a career in Family Medicine.
There were heroes all over WNC, with communities and support networks stepping up to help. My support network also included:
• In-laws, who provided a break from Asheville where we could access drinkable water, electricity, and needed supplies.
• Friends: when my good friend Beth, a public school teacher, heard I was running the office alone, she came down and sat at the front desk, greeting patients, so I could stay focused on seeing patients in the back.
• Colleagues: The other wonderful clinicians, Dr. Hannah-Marie Roberts and PA Julie Midkiff, returned and really stepped up to meet the needs of our patients. They even allowed me to get away a few days so I could catch my breath.
• My ACOs: both Aledade and CCPN provided me with my Starlink and earlier access to my value-based care dollars to keep revenue up.
• NCDHHS: when they learned I was so short on staff, the agency sent a temporary employee to help out.
• Payers: they stepped up with stabilization payments for offices in western North Carolina.
• FEMA: the agency helped out so many with housing, food, water, and financial assistance.
• And, of course, the NCAFP – making sure I was plugged into every support resource possible through this.
As tough as it has been, it warms my heart to know how many people don’t want to see my office or any Family Medicine office in Western North Carolina fail.
Speaking of support networks: that is what NCAFP and our annual meeting does – help us reconnect, network, become part of one another’s support system. Through good times and bad, the NCAFP continues to support us all in many ways.
That frequently is through advocacy. The NCAFP is constantly working to strengthen the influence of Family Medicine at the NC General Assembly, with payers and with health systems. I’m particularly excited about our advocacy on increasing investment in primary care. This year I was proud to represent the NCAFP on the Primary Care Payment Reform Task Force. The NCAFP and I will continue to lead the charge for getting us paid what we deserve and reducing the administrative burden.
The NCAFP continues to support family physicians in their personal and professional development, including educational conferences and networking opportunities. The Academy continues to grow the future workforce, nurturing medical student interest in Family Medicine and engaging our residents and new physicians.
Since leaving residency, no other organization has influenced and supported my career like the NCAFP. Make no mistake, we’ve got some serious challenges ahead. But we will adapt, we will innovate, we will support each other, and as family physicians we won’t just survive, we will thrive.
I’m so proud to be among such an amazing group of colleagues, peers, and friends.
Again, it is my honor to be your president for the next year.