

Method to the Madness ADVOCACY:

Managing
Peter
It's a Game of 4D Chess: What Our NCAFP Policy Elective Students Learned About Advocacy
PRESIDENT'S MESSAGE
By Mark McNeill, MD NCAFP 2024-2025 President
Method to the Madness ADVOCACY:
On a Tuesday afternoon in June 2016, I closed my solo office in Asheville early and drove east on I-40 to spend the night in downtown Raleigh. I was signed up for my first White Coat Wednesday as part of my leadership journey with the Western Carolina Medical Society (WCMS). As I drove down the mountain, my mind began to fill with regret. Here I was, reducing my availability to my patients, losing income, and putting hundreds of miles on my car in the hope that some of our legislators might be interested in my opinions. I was sure that our representatives were already well informed. What was I going to add to the conversation, and would they even care? This began to feel like a complete waste of precious time and energy.
My thoughts couldn’t have been further from the truth.
That day was a tectonic shift in my leadership interests for a few reasons. It was clear that our representatives were not as well informed on medical issues as I had assumed. Our legislators were metaphorically drinking from fire hydrants trying to absorb lots of information on bills that covered a variety of topics. And when a medical expert like me walked into their office wanting to help, they indeed wanted to hear what I had to say. That year would be my first time advocating for Medicaid expansion. I also was able to speak up about the NC Controlled Substance Reporting System and influence legislation to improve it.
After being able to positively influence legislation, coupled with developing relationships with other North Carolinians passionate about making the state I love a better place, I was hooked. The next year I would return, and by 2018 I would sign up for two White Coat Wednesdays, one with the WCMS and one (my first) with the NCAFP. Advocacy on behalf of patients and Family Medicine at home, in Ra-

My first visit in 2016.
leigh, and in Washington, DC, has been a top priority of mine ever since.
It’s been an interesting year, to say the least, to be a champion for advocacy. This year so far has seen a staggering number of executive orders and actions at the federal level. Many of these actions threaten our patients, our communities, and the practice of Family Medicine. They affect items we all care deeply about. Trying to keep up on all the issues is hard enough. Then you have to have enough mental energy left over to actually care and take any action. Many of us understandably feel overwhelmed and even helpless at times. It can be comforting to know that we have academies (the AAFP and the NCAFP) that are looking out for us, but only if we actually understand what they are up to and why.
There have been many lessons learned over the years with my journey in advocacy. One of those is knowing when and when not to engage on an issue. Within the NCAFP, it can be tempting right now to engage publicly on every single item that potentially threatens something we care about. Make no mistake, we need to be speaking up right now, and on some level we want to engage on everything! My wife has become a creative maven at making protest signs over the last decade and considers this good therapy for this year.
The reality is, if we want to have a successful impact, some strategy is required. Our CEO Greg Griggs, General Counsel and Senior Vice President Shawn Parker, the Executive Committee, the Board, and the Advocacy Committee have spent a significant amount of time this year making sure our efforts are directed appropriately. Significant guidance is also provided by our lobbying team at The Raleigh Group. I would like to share our thought process on when and how we engage.
First, know that our values, strategies, and stances have not changed. We remain committed to protecting our patients, our specialty, and our communities. Our policies and statements remain in place, specifically our stated views on discrimination, health disparities, women’s access to care, and keeping the government and insurance companies out of the exam room. If and when we are asked, our positions have not budged. We have not censored or scrubbed our website, magazine, or social media accounts. What I hope to do with the remaining article is give you insight into the thought process that goes into deciding when to act and how to act when a political issue comes to a head.
We first ask, does the current issue relate to NCAFP strategic priorities or established values? Our strategic priorities are outlined in our strategic plan. Established values are outlined in policy statements. If our strategic plan or policy statements are affected, then that is a very strong argument for engaging on the issue at hand.

Return trips to White Coat Wednesday allow you to develop ongoing relationships with your representative. Pictured here is my House Representative Brian Turner, whom I first metin 2016 and again this year. So who is aging better?
We then ask, will engagement meaningfully impact the eventual policy outcome? This is where we have to consider our sphere of influence, connections, and leverage. That sphere of influence is mainly within North Carolina, including the General Assembly and our NC private payers. Historically, when it comes to federal issues, we rely heavily on the AAFP to take the lead, as they are much more likely to affect the outcome in DC. While your NC Academy leadership cares deeply about many things happening on the federal level, frequently the best approach is to support the AAFP in their efforts, while staying focused on the NC issues that affect our membership the most. That is why our advocacy efforts this year will continue to be focused heavily on the state level, specifically to improve
Continues on next page
NCAFP Board of Directors
Executive Officers
President S. Mark McNeill, MD, FAAFP
President-Elect Benjamin F. Simmons, MD, FAAFP
Secretary/Treasurer Deanna M. Didiano, DO
Immediate Past President Garett R. Franklin, MD, FAAFP
Executive Vice President Gregory K. Griggs, MPA, CAE
At-Large Directors
D. Landon Allen, MD, MPH, MBA
Stacey Blyth, MD
Joshua T. Carpenter, MD
Lisa A. Cassidy-Vu, MD, FAAFP
Kelley V. Lawrence, MD, IBCLC, FABM, FAAFP
Amanda R. Steventon, MD, FAAFP
Patrick S. Williams, MD
Courtland D. Winborne, MD
Academic Position
R. Aaron Lambert, MD, FAAFP
Resident Director
Stephanie P. Wilcher, MD, MPH
Resident Director-Elect
Irina Balan, MD
Student Director
Nicholas Wells
Student Director-Elect
Ryan Taylor
AAFP Delegates & Alternates
AAFP Delegate Tamieka Howell, MD, FAAFP
AAFP Delegate Thomas R. White, MD, FAAFP
AAFP Alternate Rhett Brown, MD
AAFP Alternate Thomas R. White, MD
NCAFP Committee Chairs
Workforce Committee Jay Patel, MD, MPH Advocacy Committee Deanna M. Didiano, DO
Practice Environment Nichole Johnson MD, & Profesional Development MPH, FAAFP Committee
Academic Departments Margaret Helton, MD, FAAFP Chair
NCAFP Foundation President Maureen Murphy, MD
investment in Family Medicine, reduce our admin burden, and keep third parties out of the exam room. We have real opportunities to be impactful at the state level on increasing investment and decreasing admin burden, and much of our effort is and will be directed that way.
That being said, there absolutely is a time and place for NCAFP to engage more fully on the national level. A recent example would be Medicaid funding being under threat with budget negotiations. If there are cuts to Medicaid funding, trigger laws in NC would automatically threaten the recently enacted Medicaid expansion, leading to the end of health coverage for over 650,000 people in our state. Does that affect our strategic plan? You bet it does! Key items from our plan, such as increasing investment in Family Medicine, nurturing interest in Family Medicine, physician retention, and improving family physician job satisfaction, will all be hamstrung. And besides, the fact is that protecting Medicaid is just the right thing to do for our patients. This is a no-brainer. And we can have an impact on this issue! Know that your NCAFP staff, leaders, and many of our fellow NC family physicians have been reaching out to our Congressional Delegation in DC, making sure they know how important it is to the health of NC that Medicaid funding remains stable.
Once we have decided that we should act, the next item to consider is the appropriate channel. Sometimes formal, high-profile communication is the right choice. However, that is not always necessary or appropriate. Would a meeting suffice or be preferable? Are there other avenues to pursue our goal that would be more effective? This indirect engagement has its advantages, but its low-profile nature can sometimes leave members wondering if anything is being done at all. Frequently the answer is yes, as frankly a majority of advocacy within the NCAFP occurs in this behindthe-scenes fashion. While updates of this behind-the-scenes work are commonplace at board meetings and within the weekly NCAFPNotes e-newsletter, this still leaves routine members left out sometimes. Know that your NCAFP President and your CEO are always available to give you updates on action that is being taken, whether it is high-profile work or not. Please see my contact info at the end of this article and add it to your contacts.
Other items of consideration when choosing to engage are the political ramifications. Is this bill/hearing/issue a very high priority for NC General Assembly leadership, or key legislative allies (i.e., is endorsing, commenting, or participating important for cementing or strengthening our relationship with them)? Are there negative ramifications of not
weighing in (i.e., negative member reaction, fallout with legislative allies or leadership)? Will there be impact on other ongoing advocacy work or strategic priorities? This calculation is the part I enjoy the least, honestly. Being passionate about an issue but having to hold back knowing that a key relationship or advocacy goal is in jeopardy can test your patience and leadership determination.
I hope it is clear that successful advocacy requires thought, strategy, and patience. That can be hard work, but it should not hold us back from being there for our patients and our specialty during these challenging times. I don’t think we have seen a period in our professional lives where advocacy for the house of Family Medicine is more important. In my installation speech, I spoke of Family Medicine’s ability to adapt and how we get through tough times by supporting each other. When it comes to advocacy, if we need to be in the streets with our voices raised, we will do that. But if a more subtle approach is needed, we are prepared to adapt, and we will have each other’s backs in the process.
Thank you if you have spoken up this year. Your voice is needed. If you have been contemplating advocacy, this is a great year to start. Opportunities are usually available in NCAFPNotes. Resources are available on the website. And of course, myself, members of the board, and our wonderful NCAFP staff are always happy to direct you if you aren’t sure where to start.
I’ll finish by sharing that remaining involved in advocacy is part of my burnout prevention plan. When I get a case of the “screw its,” when I feel that inner cynicism and pessimism rising, I remind myself that I’m in a privileged position. I have a seat at the table. I’m part of an Academy that has been doing great work for decades and is an avenue for my voice to be heard. I can have an impact. After a White Coat Wednesday event, I usually return on a high that lasts a couple of weeks. While I don’t expect everyone to feel that way, I hope you can see despite its challenges, knowing you can speak up and matter can make you realize your own agency during challenging times.
Thank you for all continuing to keep your chin held high despite the continued chaos around us. We occupy the moral high ground together, and the NCAFP will continue to stand with us there, fighting the good and just fight.
S. Mark McNeill, MD markmcneill@gmail.com Cell: (828) 273-6229

Mark your calendars for the 2025 Winter Family Physicians Weekend ! This year’s conference offers the perfect mix of professional development and relaxation. Under the leadership of Program Chair Dr. Katherine Haga, and Program Vice-Chair Dr. Amir Barzin, this is the perfect opportunity to connect with peers, expand your clinical expertise, enhance your skills, and recharge your love for Family Medicine. Whether you attend in person or virtually , you’ll earn valuable CME credits while engaging with expert -led sessions on the latest advancements in your specialty Here’s a peek at what’s on tap this December!
Cardio, Metabolic & Renal Health
• Diabetes Management
• Lipid Management
• Obesity Care
• NAFLD/NASH
• Cardio-Renal-Metabolic Health
• CGM Advances
Infectious Diseases & Prevention
• HIV Care
• RSV Prevention
• UTI Management
Women’s Health
• Hypertension in Pregnancy
• Menopause
• Perinatal Substance Use
Pediatrics
• Pediatric GI Concerns
• Urgent & Emergent Pediatric Conditions
Gastroenterology & Pulmonology
• GERD
• Lung Cancer
Musculoskeletal Health
• Weekend Warriors
• Rheumatology
Mental & Behavioral Health
• Depression
• Anxiety & Bipolar
• Adult ADHD
• Chronic Pain Management ( Non-Opioid)
• Neuromuscular Disorders
Innovations & Emerging Topics
• Climate Change & Medicine
• Best FM Studies of 2025
Regulatory & Policy Discussions
• NC Regulatory Update
• ABFM Update
Workshops & Seminars
• Hands-On Dermatology Workshop
• Care of Children KSA
• Women’s Health Seminar
• Practice Management Seminar
And Much, Much More!
We look forward to sharing this unforgettable experience with you ! Save the dates , watch your email and our conference site at www.ncafp.com/wfpw for the complete schedule and registration details coming this summer! We look forward to being with you in December!
By Shawn P. Parker, JD, MPA Senior Vice President & General Counsel
Your Legislative Update from the 2025-26 Long Session

The North Carolina General Assembly convened to start the 2025-26 biennial legislative session on Jan. 8. The General Assembly meets in a regular session beginning in January of each odd-numbered year (called the “long session”) and ad journs to reconvene the following even-numbered year for a shorter session (called the “short session), usually in May. In a long session, any member can introduce legislation. However, pursuant to rules adopted by each chamber, such bills must be filed by a certain date to be eligible for consid eration. As of this writing (with bill filing deadlines almost complete), over 1,800 bills have been introduced. Not all these bills will become law. For example, in the 2023-24 session, 1,659 bills were introduced but only 149 became law. There are a number of steps legislation must go through before it becomes law, and your NCAFP team is here to advocate for your interests at each step.
Your executive leadership, NCAFP staff, and lobbying team at The Raleigh Group have been actively monitoring these filings, and approximately 200 of them relate to health care delivery, regulation, or payment. Of these, there are about 40 bills that are viable and could potentially impact the legislative policy agenda which our NCAFP Board has adopted for the year. We will then focus our energy upon these bills. Our efforts include advancing reforms to primary care payment, supporting legislation that reduces (and opposing legislation which increases) administrative burden, protecting the integrity of your profession by limiting inappropriate expansion of other health professionals into medicine, as well as monitoring and counteracting activities that limit or threaten the physician-patient relationship.
Of the many bills filed in this session, there are two very noteworthy pieces of legislation in which we have expressed great interest and to which we have committed significant
ly and alongside our partners in the House of Medicine and stakeholders in the insurance industry with the North Carolina General Assembly.
1. Extending the Primary Care Task Force
Senate Bill 83 (Sen. Hise, primary; Sen. Adcock; Sen. Burgin; Sen. Lowe; Sen. Mayfield; Sen. Mohammed)
House Bill 629 (Rep. Reeder, primary; Rep. Cunningham; Rep. Ward)
If enacted, the bill would extend the activities of the North Carolina Primary Care Task Force through this biennium. The Task force was initially established in 2023 to gain an understanding of current spending on primary care services and an assessment of the current state of primary care in North Carolina. In addition to providing more time for the study and assessment, the bill expands the duties of the Task Force, directing the collection and compilation of data and other information related to health care spending on primary care services. Clarifying the data collected is not
considered public information, and the Task Force and the North Carolina Department of Health and Human Services are directed to develop and implement a detailed data security and safeguarding plan for this requested data (in a HIPAA-compliant manner.) The Task Force is directed to report its findings and recommendations to the Joint Legislative Oversight Committee on Health and Human Services and the Joint Legislative Oversight Committee on Medicaid by April 1, 2026. The findings and recommendations must include specific, concrete, and actionable steps to be undertaken by the State and upon which the General Assembly could act.
2. Supporting the CARE FIRST Act.
House Bill 434 (Rep. Bell, primary; Rep. Reeder, primary; Rep. Cotham, primary; Rep. Campbell, primary)
House Bill 434 aims to reform the process of patients seeking prior authorization from their health insurance provider and amends the utilization review process. The bill adds new definitions to the article governing utilization reviews in Chapter 58 of the North Carolina General Statutes to include prior authorization, and it sets forth specific clinical criteria and time-frames for decisions that every insurer must meet.
Specifically, the first part of the bill:
• requires that a denial of insurance coverage can only be made by a medical doctor who is of the same specialty as the provider managing the patient’s condition underlying the request for services and who has experience treating patients with that condition
• requires insurers to maintain a public list of services for which prior authorization/utilization review is required
• requires a 24-hour turnaround for urgent health care services and also sets out timelines governing non-urgent health care services and emergency services
• prevents an insurer from revoking, limiting, conditioning, or restricting services if care has been previously certified by the insurer
• requires payment to the provider with certain limited exceptions
• provides that any failure by an insurer to comply with the deadlines and other requirements of the law in regards to health care service subject to review be automatically deemed authorized by the insurer
The second part of the bill extends the definition of the practice of medicine to include performing any part of a utilization review/prior authorization governed by the forementioned statute. This gives the North Carolina Medical Board authority to subpoena an insurer for any records, documents, or other materials pertaining to the involvement of any physician performing utilization review and subjects that physician to the Board’s disciplinary process if the decision harms patients.
The Senate also introduced two bills (SB 287 and SB 315) to reform the utilization review process in North Carolina, which (while not as expansive as the House version) would prevent an insurer from using an artificial intelligence-based algorithm as the sole basis for a utilization review determination to, in whole or in part, deny, delay, or modify any health care services for an insured and includes provisions regarding continuity of care. We look forward to remaining involved in the process if these bills move forward.
While the first months of session came in like a lion, there is no indication that the next two years will go out like a lamb. Your NCAFP Leadership, staff, and our team at the Raleigh Group intend to advocate zealously on your behalf each step of the way. Please reach out to us if you ever have any questions or comments on the legislative process or specific bills.
NCAFP Staff:
Gregory K. Griggs, MPA, CAE Executive Vice President and CEO ggriggs@ncafp.com
Shawn P. Parker, JD, MPA Senior Vice President and General Counsel shawn@ncafp.com

ON THE GROUND
NCAFP Members Connect and Advocate During the 2025 White Coat Wednesday Event at the NC Legislature
By Kevin LaTorre NCAFP Communications & Membership Manager
On March 19, the NCAFP brought over 45 members and staff to the North Carolina General Assembly to meet with their lawmakers. During their meetings, NCAFP members stressed the need for increased investment in primary care, called for prior authorization reforms, and requested a higher cap for the forgivable education loans for service (FELS) program to help bring medical students into primary care. “White Coat Wednesday gives our members the chance to bring their insights directly to our legislators,” NCAFP Executive Vice President and CEO Greg Griggs said. “It’s invaluable for building relationships and sharing how family physicians improve outcomes and lower costs.”
This group is the largest number of NCAFP members to ever attend a White Coat Wednesday event. 2025 attendance topped the 2024 attendance, which had been the previous record. Attendees met with their senators and representatives across more than 35 scheduled meetings, and many more had the chance to drop by their lawmakers’ offices.
“You’re the experts today,” NCAFP President Dr. Mark McNeill told attendees. “You can share your story as physicians and medical students today.”
NCAFP members continued building relationships with their lawmakers.
Many White Coat Wednesday attendees had attended in previous years, while many others came for the first time. But everyone had the chance to strengthen relationships with their representatives and senators. The Raleigh Group Vice President of Government Affairs and NCAFP lobbyist Sue Ann Swift told attendees, “Building these relationships does really make a difference.”
Dr. McNeill echoed Swift, saying, “The most important thing you’re going to do today is start or strengthen relationships. As family physicians who build trust with our patients, we’re well positioned to do that.”
NCAFP Advocacy Committee Chair and Secretary-Treasurer Dr. Deanna Didiano has been strengthening her ties to
NCAFP attendees in the House Chamber with Rep. Dr. Grant Cambpell (R) and Rep. Dr. Timothy Reeder (R).
her lawmakers for over 10 years. “That first time I attended White Coat Wednesday as a resident was really eye-opening,” she said. “They really wanted my perspective as someone explaining how their constituents were struggling with health care access. Our conversations have become easier over time, and I know they really respect where we’re coming from and will listen.” She enjoyed sharing that experience with all her fellow attendees during White Coat Wednesday: “It was fun to have this group of physicians, residents, and students share these conversations while walking around the General Assembly today. It’s even better that we’re making actual change.”
After some last-minute schedule adjustments, past NCAFP president Dr. Jessica Triche met for the second year in a row with Rep. Keith Kidwell (R) for a brief but supportive conversation about prior authorization reform. “It was a classic in-the-hallway meeting,” Dr. Triche said.
Third-year medical student Collette Cambey enjoyed meeting with Sen. Dan Blue (D) and Rep. Renée Price (D). “They were very receptive,” Cambey says. “We talked in great detail about the medical student loan programs and even went over the scheduled time limit. I lucked out by having a nice day full of amenable people to talk to.”
NCAFP members advocated for Family Medicine reforms during their White Coat Wednesday meetings.
During this long legislative session, the NCAFP is advocating for increased primary care investment, prior authorization reforms, and increases in the FELS funding for medical students entering primary care in North Carolina. The prior authorization reforms took a big step forward on March 18, when Rep. Dr. Tim Reeder (R), Rep. Dr. Grant Campbell (R), Rep. Tricia Cotham (R), and Rep. John Bell (R) introduced the Care First Act. The bill would standardize authorization timelines, give exemptions to clinicians with high approval rates, and create transparent lists of which kinds of care require prior authorization, among other key provisions. Because these reforms would reduce the administrative burden and delayed care that prior authorizations cause, the NCAFP supports the bill. During their meetings, White Coat Wednesday attendees explained how prior authorizations can harm their patients by delaying their care or even forcing them to use emergency departments.
Many attendees found that their lawmakers were receptive to the reforms. Dr. Kelley Lawrence said, “Rep. Todd Carver (R) signed on to co-sponsor the Care First Act while we were meeting with him.”
Dr. Corinna Myer said, “Sen. Woodson Bradley (D) was very receptive. She said she would reach out to her counterparts in the House to co-sponsor the bill.”
As of March 21, the Care First Act has received 56 new co-sponsors from both parties. Many of the House members whom NCAFP representatives met with signed on as co-sponsors. During White Coat Wednesday, two of its primary sponsors, Dr. Tim Reeder and Dr. Grant Campbell, met for nearly an hour with the NCAFP attendees in the House Chamber. They discussed their experience as the only physicians currently serving the legislature and answered questions from attendees. In particular, they discussed how much of their best legislative work happens through preventing unhelpful legislation from becoming law. “Calvin Coolidge said, ‘It’s much more important to kill bad bills than pass good ones,’” Rep. Dr. Reeder said. “When we do that, it’s still a victory for health policy in North Carolina.”
Rep. Dr. Campbell also stressed the incremental and sometimes slow-moving work of reforming the many health policy concerns. “The way we improve health care is to identify individual issues and then solve them one by one,” he said. For this, he welcomed help from NCAFP members. “I’ll impress on you guys the critical importance of physician involvement. If you’re thinking of running for office as a physician, please do it.”
Rep. Dr. Reeder agreed by explaining how much more the legislature can learn from NC physicians. “There’s a huge part of health care that even we don’t know,” Dr. Reeder said. “The fun part is that that there’s a lot for us to learn, often with your help.”
“I never realized how easy it is to get in touch with my state legislators,” said Dr. Victoria Boggiano. “White Coat Wednesday helped it seem more possible and way less daunting to get involved in advocating for policies that impact my work as a physician and my patients here in North Carolina.”
Thank you to everyone who participated in the 2025 White Coat Wednesday event!
To the family physicians, residents, and medical students participating, and to the representatives, senators, and legislative aides who gave their time to meet with NCAFP members: the NCAFP thanks you for your time and for your ongoing work to improve NC health care policies!
CHAPTER AFFAIRS
By Greg Griggs, MPA, CAE NCAFP Executive Vice President and CEO
Independent Family Medicine Alive and Well in Rural North Carolina
On the last Saturday of March, I had the opportunity to make the beautiful drive from the Triangle to the mountains of western North Carolina and the rural communities in Ashe County. During the trip, I had the opportunity to visit not one but two independent Family Medicine practices owned by young family physicians serving the people of Jefferson and West Jefferson, NC.

SEVEN PEAKS FAMILY MEDICINE
Seven Peaks Family Medicine, a three-physician practice, held its ribbon cutting on March 29 and opened for patients on April 1.
This practice germinated out of joint presentations from NCAFP and Community Care of North Carolina (CCNC) to residents at the MAHEC-Boone Family Medicine Residency about three years ago. After hearing a discussion about models of care, which included independent practice, a few of the residents became hooked. With the idea growing, CCNC took over to mentor these young physicians and provide the insight, back-office assistance, and financial acumen to make the dream a reality through CCNC's Primary Care Venture Mentoring Service.
“At Seven Peaks Family Medicine, we are consciously choosing to build our clinic literally and figuratively from the ground up with innovative and ambitious plans for providing comprehensive, evidence-based, and compassionate Family Medicine in an ever-more complicated health care environment,” Toria M. Knox, DO, one of the three owners of the practice, said at the ribbon cutting. Dr. Knox also discussed how the three physicians formed an LLC with the administrative and financial support of CCNC.
“This is great,” past NCAFP president and CCNC co-founder Dr. Allen Dobson said at the event. “It’s a new generation of family doctors who decided to build their own practice in an area of need.”
Jessica Stevens, MD, another partner in the practice, discussed the name and vision of the new clinic, noting that it was “born out of a shared desire to provide full-scope Family Medicine.” The name of the clinic highlights the seven peaks you can see from their brand-new building in the small town of West Jefferson. Each of the patient care rooms shares the name of one of those peaks, such as Howard Knob and Rich Mountain.
Jason K. Karimy, MD, is the third partner of the clinic, which all the physician owners said would not have been possible without the support of CCNC.
Christina Page, Senior Vice President of Product Development at CCNC, led the team that supported the practice startup, which included CCNC President and CEO Dr. Tom Wroth, Dr. Dobson, past NCAFP president Dr. Conrad Flick, NCAFP Foundation Board member Dr. Vickie
Dr. Toria Knox, Dr. Jessica Stevens, and Dr. Jason Karimy.
Fowler (who happens to be a native of West Jefferson), and others.
“One thing that has been crazy and interesting about this work is that it took no effort at all to find patients and staff members,” Page said. “When you put access in the right place, this is what happens. It is such a great opportunity to invest in a group of physicians that are going to serve their community forever.”
All three of the physician owners are graduates of the MAHEC-Boone Family Medicine Residency Program, and all of them wanted to stay and serve the people of the high country in western North Carolina.
MAHEC-Boone Family Medicine Residency Program Director Dr. Molly Benedum and her son joined over 100 individuals who turned out for the ribbon cutting, building tours, and other festivities to celebrate the opening of the new clinic.
One other attendee was Landon Allen, MD, MPH, MBA, a member of the NCAFP Board of Directors. Dr. Allen is also the owner of New River Family Wellness Center, another relatively new Family Medicine practice just a few miles down the road in Jefferson.
NEW RIVER FAMILY WELLNESS
After the ribbon-cutting ceremony, I followed Dr. Allen to his new location on Main Street overlooking Mount Jefferson.
Dr. Allen and his practice partner, Caitlin M. Downing, MD, had started New River Family Wellness several years ago in a leased space but then recently moved into the location they had purchased a few months ago. They had renovated the new location, a house that had previously been a Mexican restaurant.
Dr. Allen and Dr. Downing opened New River Family Wellness, a Direct Primary Care practice, after Dr. Allen finished his residency at MAHEC-Hendersonville Family Medicine Residency in 2019. Dr. Downing also attended residency in Hendersonville after completing medical school at the University of Connecticut. Dr. Allen had first become involved with the NCAFP as a medical student when he completed the Blue Cross and Blue Shield of NC Scholars Program through our Foundation’s medical student initiatives (once again showing that the work of the NCAFP Foundation produces results!).
Dr. Allen is a lifelong native of North Carolina, attending undergraduate, graduate, and medical school at East Carolina University. He grew up in more metro areas, but the whispers of the rural western NC mountains caught his ear.
In our discussion as I toured his practice, Dr. Allen raved about caring for the people of a small rural town, noting the sense of community he gets from seeing his patients outside of the office and taking care of multi-generational families, including one family in his practice that includes five generations. The practice’s vision is to “strive to provide exceptional care at a more affordable price to the people of Ashe County and the High Country, regardless of whether they have health insurance.” In addition to his outpatient practice, Dr. Allen still delivers babies (both his own patients and unassigned call) and provides inpatient care in the nearby hospital.
As I drove back toward the Triangle, I reflected on the excitement of these young family physicians as they embark on the careers they have worked so hard to achieve. I smiled to myself as I felt my own sense of excitement that young family physicians have so many options and can still choose to practice independently, if they so desire. It’s simply one more reason to feel great about the work we do at the North Carolina Academy of Family Physicians, along with our

Dr. Landon Allen.

Hybrid Summer Symposium This June!
- Advancing Education and ConnectionPractical Insights on Metabolic Syndrome and Weekend Warriors for the Family Physician
By Kathryn Atkinson, CMP NCAFP Director of CME & Events
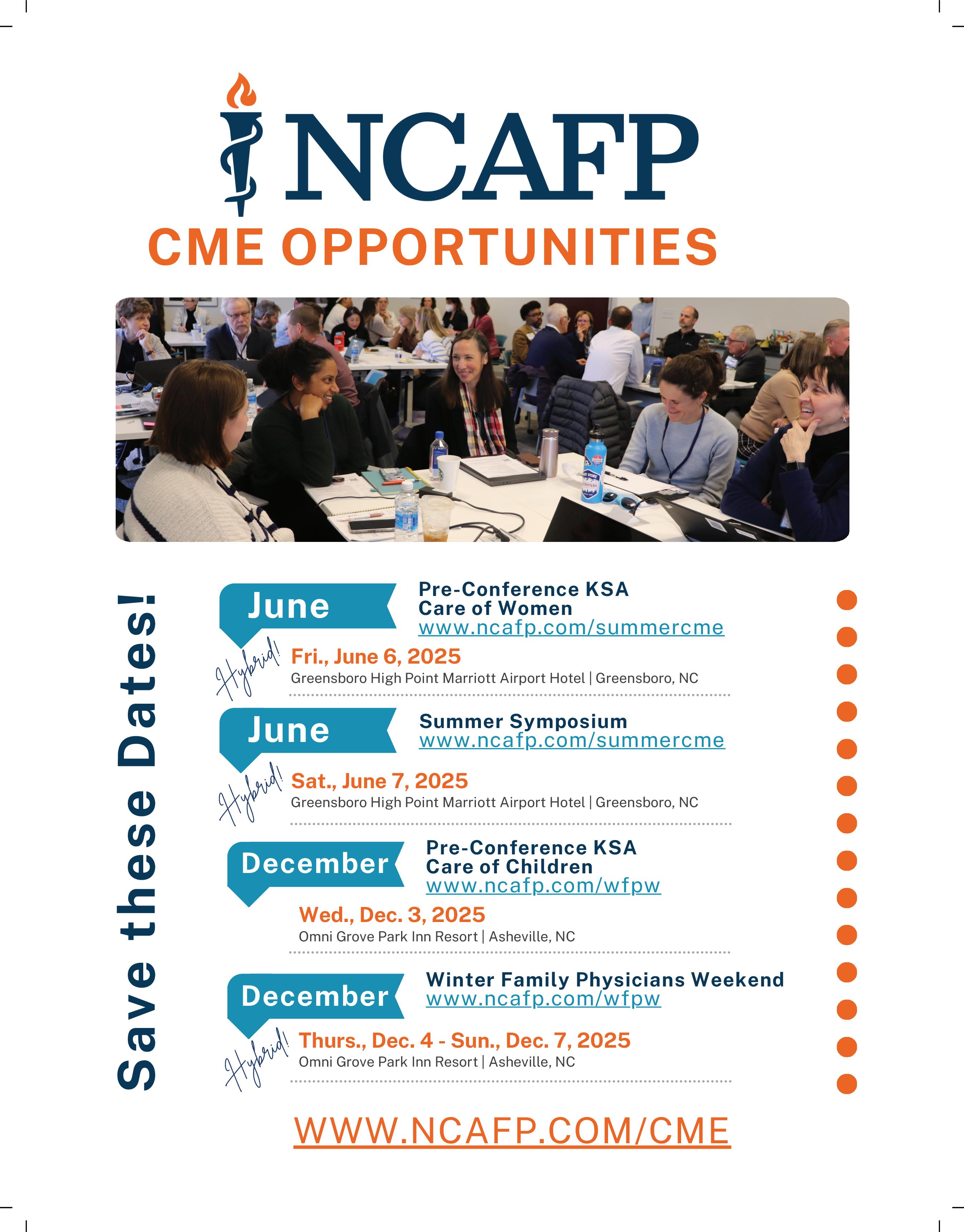
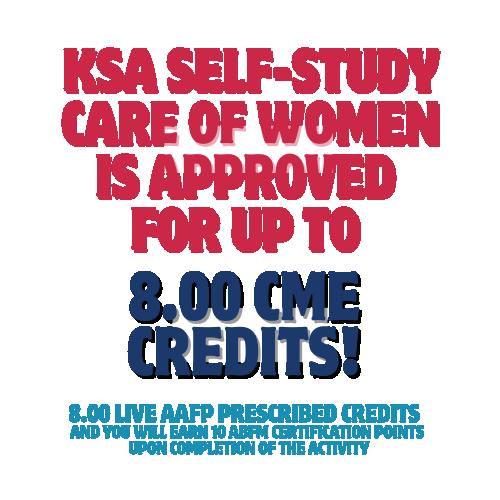
The NCAFP’s annual Summer Symposium is getting a fresh new twist with a hybrid format and two distinct tracks. This year’s must-have summer CME opportunity offers you the flexibility to participate as much as you wish, in the best way for you. Whether you attend in person or virtually, you’ll have access to either a half-day or a full day of practical, relevant education designed to support you and your patients. And it's accredited to receive up to 26.50 Live AAFP Prescribed credits! (See the credit breakdown below.)
Set for Saturday, June 7, 2025, at the Greensboro High
Point Marriott Airport Hotel, the Symposium will feature two distinct learning tracks. The morning sessions, led by Program Co-Chair Dr. Thomas White, will dive into metabolic syndrome, covering key topics like hypertriglyceridemia, obesity and GLP-RAs, and prediabetes. These presentations will be followed by a panel discussion complete with case studies and interactive Q&A, providing a unique opportunity to discuss clinical applications.
In the afternoon, Program Co-Chair Dr. Deanna Didiano will shift the focus to sports medicine and explore the



diagnosis, treatment, and prevention of common injuries in active patients by focusing on the shoulder, elbow, foot, ankle, hip, and knee. Following the same dynamic format as the morning sessions, this segment will provide practical, actionable strategies for managing weekend warrior injuries in primary care.
Here’s a quick preview of the expert guest faculty set to join Drs. White and Didiano on the stage and in the discussions:
• Dr. Thomas Barringer III: “Hyperglyceridemia – When and How to Treat”
• Dr. Dawn Caviness: “An Evidence-Based Approach to Prediabetes – Empowering Patients to Achieve Lasting Lifestyle Changes”
• Dr. Michelle Keating: “Obesity – Is There More Than GLP-RAs?”
• Dr. Shane Hudnall: “Keeping Patients Moving: Managing Hip and Knee Injuries in Primary Care”
• Dr. Landon Irvin: “Beyond the Ache: Diagnosing and Managing Common Shoulder and Elbow Injuries”

• Dr. Heath Thornton: “Step by Step: Diagnosing and Treating Common Foot and Ankle Injuries”
The Symposium officially begins on Friday, June 6, with a pre-conference KSA Workshop on the Care of Women (led by Dr. Johnathon Firnhaber). This KSA is also available in the hybrid format. That evening, you’re invited to the complimentary and casual networking social at the Marriott, which will reconnect you with your colleagues and expand your professional network. Plus, there will be prizes!
This year’s new summer CME format and focus makes learning more accessible than ever. Whether engaging in person or tuning in from your home or office, whether you participate in one track or both, you’ll gain valuable insights you can immediately apply to your practice. Make plans now to attend the 2025 Summer Symposium and register today to take advantage of this opportunity to learn, connect, and grow.
Full schedule, registration, guest faculty, and hotel reservation information are available at www.ncafp.com/summercme.
We look forward to seeing you in June!

Empowering Independent Practices to Thrive!


We offer independent practices the opportunity to participate in our group as affiliates, receiving all the benefits of our large group without losing ownership or independence. Continue to own your practice while participating in the benefits of our large group
“We
- Dr Jing Zhang (Waverly Primary Care)


NCAFP Members Enjoy 2025 NC Family Medicine Academic Summit and Family Medicine Day Events
By Kevin LaTorre NCAFP
& Membership Manager
On Feb. 21 and Feb. 22, NCAFP members joined together in Durham to collaborate on the best topics and skills in Family Medicine. On Friday afternoon, guests attended the 2025 Family Medicine Academic Summit at the Estes Conference Center. On Saturday morning, medical students and representatives from most of the NC medical schools and Family Medicine Residency programs attended the 2025 Family Medicine Day at the Sheraton Imperial Hotel RTP. At both events, attendees enjoyed the learning and the company.
During the Academic Summit, Residency Program and Medical School leaders and faculty gathered to learn the newest ideas and skills to improve residency training, under the direction of program co-chairs Dr. Aaron Lambert and Dr. Regina Bray Brown. The event’s sessions included developing adaptive learners, handling remediation, better understanding physician burnout, and other topics which were practical for the audience members’ work. “It was a great afternoon of learning!” one attendee said in a postevent survey.
During Family Medicine Day the following morning, over 90 medical students attended workshops hosted by NC
Family Medicine residency faculty and residents. In those workshops, the students experienced the entire scope of the medical care that family physicians practice. “I got to learn many aspects of Family Medicine that I didn’t know before,” said one attendee in a post-event survey.
These applied sessions taught students to perform joint injections, suturing, point-of-care ultrasound tests, and other skills that helped students understand what they might do for their patients as family physicians. “I enjoyed the number of hands-on activities!” said one attendee. “I loved learning all the procedures that family physicians can do.”
Both NCAFP events served the future of Family Medicine in North Carolina.
The Academic Summit included top-notch education on training family physicians during medical school and residency. Family Medicine Day helped to recruit those future family physicians while they are still medical students. “You are the future of Family Medicine,” NCAFP President Dr. Mark McNeill told students before the keynote lunch address from Dr. Lenard Salzberg.
Conference Recap
Communications
Attendees listen to Dr. Nikki Binz at the NC Family Medicine Academic Summit.
The last part of the day focused on recruiting medical students to our state’s Family Medicine residency programs. “We find it a great way to access strong North Carolina medical students interested in Family Medicine,” said one residency leader.
The recruiting is also immersive thanks to the residencies’ workshops. Medical students got to try many of the procedures which family physicians provide for their patients.
“There is a wide diversity of skills and niches available in Family Medicine,” said one medical student. “NC has lots of amazing residency programs!”
This exposure to the specialty helped medical students commit to Family Medicine, according to their own survey reports. 35.8% of students reported they were more likely to consider Family Medicine as their future specialty, thanks to attending Family Medicine Day. “I am very convinced that Family Medicine is the direction I want to go and I’m excited to learn more!” said one attendee.
Attendees enjoyed coming together at both NCAFP events.
“The Family Medicine Academic Summit was a fantastic opportunity for Family Medicine educators from across the state to connect, exchange ideas, and explore strategies to enhance medical education,” NCAFP Director of CME and Events Kathryn Atkinson, CMP, said. “We’re currently looking for even more ways to help attendees come together for discussion during next year’s Summit.”
During Family Medicine Day, the social connections among like-minded attendees proved just as important. Students gathered in the lobby more than 30 minutes before the day’s first workshop started. “I’m having to keep calm right now with how excited I am for this,” Campbell University medical student Jacob Ortega said.
Throughout the day, students continued to gather and chat over coffee, cookies, and apples between their workshops. “It was wild to see how many people were here,” said Wake Forest University medical student Stuart Lewis. Like his fellow attendees, Lewis spent time discussing the workshops and meeting fellow medical students from around North Carolina. “I most enjoyed meeting new medical students as well as touching base with old friends,” said one attendee.
NCAFP staff see this camaraderie among medical students as one of the most important parts of Family Medicine Day.

“It was inspiring to see students so excited and engaged together,” said Atkinson. “It’s why Family Medicine Day was full of energy and enthusiasm from start to finish!”
Thank You to Our Attendees and Residency Programs!
We’d like to thank all the guests who joined us for the programs.
We’d also like to thank the residency programs who hosted workshops or exhibited this year:
• Atrium Health Carolinas Medical Center Family Medicine Residency
• Atrium Health Cabarrus Family Medicine Residency
• Cone Health Family Medicine Residency Program
• Duke Family Medicine Residency Program
• Duke Rural Family Medicine Residency Program
• ECU Family Medicine Residency Program
• Harnett Health Family Medicine Residency Program
• Hugh Chatham Health Family Medicine Residency Program
• MAHEC-Asheville Family Medicine Residency Program
• MAHEC-Boone Family Medicine Residency Program
• MAHEC-Hendersonville Rural Family Medicine Residency Program
• Novant Health Family Medicine Residency Program Cornelius
• Novant Health NHRMC Family Medicine Residency Program
• Sampson Regional Medical Center Family Medicine Residency Program
• Southern Regional AHEC Family Medicine Residency Program
• UNC Family Medicine Residency Program
• Wake Forest University Family Medicine Residency Program
Medical students learn from a resident teacher.


















Dr. Nikki Binz.
Dr. Victoria Boggiano and Kayla Bonnell.
Dr. Varshaben Songara, Dr. Regina Bray Brown, and Dr. Mark Higdon.
Medical students and residents make a memory at Family Medicine Day.
Dr. Aaron Lambert and Dr. Michelle Keating.
Attendees enjoy a break at Family Medicine Day.
Dr. Regina Bray Brown.
Dr. Garett Franklin and Dr. Robert Agnello.
Dr. Bailey Sanford teaches an injection workshop.
A medical student tests a new procedure at Family Medicine Day. Dr. Taiwona Elliott comments during the Family Medicine Academic Summit.
Dr. Mark McNeill and Dr. Michelle Jones.
Duke medical students at Family Medicine Day.
Attendees converse at the 2025 Academic Summit.












Ethan Agritelley and a fellow medical student practice injections.
Dr. Haley Craig-Kovach and Dr. Kelley Lawrence.
Jackson Wheatley and other medical students chat at Family Medicine Day.
Drew Griggs speaks during his mock residency interview.
Attendees from the Harnett Health Family Medicine Residency.
Dr. Victoria Kaprielian, Dr. Christine Khandelwal, Dr. Robert Agnello, and Dr. Nicolas Pennings.
Dr. Maureen Murphy with the winners of the 2025 Murphy Cup.
Dr. Taiwona Elliott and Dr. Benjamin "Frankie" Simmons.
Jay Ortega practices wound care at Family Medicine Day.
Medical students learn about point-of-care ultrasound at Family Medicine Day.
Dr. Karen Smith, Dr. Mark McNeill, Dr. Michelle Jones, and other NCAFP members.
Dr. Taiwona Elliott, Dr. Mark Higdon, and other attendees at the Family Medicine Academic Summit.













Medical students practice wound care at Family Medicine Day.
A medical student practices suturing at Family Medicine Day.
Dr. Audy Whitman and other Family Medicine Academic Summit attendees.
Sreenidhi Nair, Austin Kinne, and other medical students enjoy Family Medicine Day.
Medical students at Family Medicine Day.
Wake Forest School of Medicine attendees at Family Medicine Day.
A resident helps teach a medical student to suture.
Medical students learn to interview for residency at Family Medicine Day.
Dr. Lenard Salzberg.
Dr. Landon Allen, Dr. Deanna Didiano, and other White Coat Wednesday attendees.
Dr. Deanna Dididano, Rep. Todd Carver, and Dr. Kelley Lawrence.
NCAFP White Coat Wednesday attendees. Sen. Kandie Smith, Hannah Rayala, Dr. Dawn Caviness, and another NCAFP member.









Nicolas Wells and Colette Cambey.
Dr. Lisa Cassidy-Vu, Sen. Paul Lowe, Dr. Landon Allen, and another NCAFP member.
Dr. Mark McNeill addresses White Coat Wednesday participants.
Jamie Crews, Hannah Rayala, Dr. Jessica Triche, and Sen. Bob Brinson.
Dr. Tamieka Howell, Sen. Dan Blue, and three NCAFP members.
Dr. Jessica Triche, Rep. Gloristine Brown, Hannah Rayala, and two NCAFP members.
Sue Ann Swift addresses the White Coat Wednesday participants.
Hannah Rayala and Dr. Jessica Triche.
Rep. Dr. Grant Campbell, Dr. Mark McNeill, and Rep. Dr. Timothy Reeder.
The 2025 White Coat Wednesday participants.
MEMBERSHIP SERVICES
By Kevin LaTorre NCAFP Communications & Membership Manager
Member Profile: Dr. Nichole Johnson
We are thrilled to feature Dr. Nichole Johnson in the NCAFP Member Spotlight! Dr. Johnson works as a family physician at Novant Health University Physicians. In addition, she serves as chair of the NCAFP Practice Environment and Professional Development Committee.
Dr. Johnson became a family physician because it was the best specialty for giving all kinds of care to all kinds of patients.
Since she was a child, Dr. Johnson had wanted to be a physician. But she had always thought she would be a pediatrician. After she began attending Johnson C. Smith University, Dr. Johnson then considered becoming an OB-GYN. “I really didn’t know what Family Medicine was until my senior year of college,” she says. “When I started researching it, I realized that the specialty incorporates everything that I wanted. It was really cool: family physicians do everything. And when I learned that family physicians could treat any patients at any age, that really appealed to me. They were the physician I wanted to be.”
Family Medicine Residency in Charlotte, where Dr. Hendrix taught. “It was a full-circle moment,” Dr. Johnson says.
After completing her residency, Dr. Johnson remained in Charlotte to practice Family Medicine.
Her responsibilities as a family physician there are similar to her interests as a curious undergraduate. “The work is a pretty fair mix of everything,” Dr. Johnson says. “I still get to do procedures, pediatrics, women’s health, preventive care, and chronic disease management.”
But her work today also includes mentorship like the support she received from Dr. Hendrix. Dr. Johnson now opens her workdays to students and residents who want to learn more about Family Medicine by shadowing her. “I’ve had medical students, undergraduates, and high school students come here,” she says. “I have someone shadowing me who isn’t in school. She’s planning to go back to school and is getting a taste for what Family Medicine is.”

This precepting is personally important to Dr. Johnson. “I’m trying to pay forward what was done for me,” she says. “It helps pass on that love of Family Medicine to people. They can see that medicine isn’t just specialties, because there’s this foundation of getting to care for patients who you really know well.”
But precepting is professionally important to her too. “Precepting is a great way to re-energize yourself when you’re feeling tired or burned out,” Dr. Johnson says. “It helps me remember the excitement of just starting out in Family Medicine, which can get lost in the shuffle. And it keeps me on my toes!”
NCAFP leadership has also kept Dr. Johnson on her toes.
To learn more, Dr. Johnson shadowed Dr. Nneka Hendrix at Atrium Health Biddle Point. “She was great,” Dr. Johnson says. “Working with her was my first taste of Family Medicine. Thanks to her, I really started pursuing it.” Dr. Johnson eventually attended the Atrium Health
She first joined the chapter during medical school, and after she had attended the Winter Family Physicians Weekend several times and enjoyed the community of family physicians there, she wanted to engage more. “I wanted to do
Dr. Nichole Johnson.
more than just the clinical day-to-day stuff as a family physician,” Dr. Johnson says. “Friends of mine got me in touch with Greg [Griggs, NCAFP Exec. VP and CEO]. He got me involved.”
This new involvement included the American Academy of Family Physicians (AAFP) National Conference of Constituency Leaders (NCCL). “NCCL is one of my favorite conferences,” Dr. Johnson says. “You get to meet so many people who are passionate about the bigger picture of why we practice and how we care for people. You get to work with them on solving real problems. It’s something else that reignites my passion for doing this work.” Today, Dr. Johnson works on solving some of these problems through her role as chair of the NCAFP Practice Environment and Professional Development Committee.
Dr. Johnson also found a good group of fellow NC family physicians who became her fast friends. “My first year at NCCL, [past NCAFP president] Dr. Tamieka Howell, [past NCAFP president] Dr. Jessica Triche, and [NCAFP President-Elect] Dr. Frankie Simmons were there,” she says.
MEMBERS IN THE NEWS
By Kevin LaTorre NCAFP Communications & Membership Manager

Dr. Bryan Hodge Appears in AAFP Spotlight
Earlier this year, the American Academy of Family Physicians (AAFP) profiled NCAFP member Dr. Bryan Hodge, who currently practices in Hendersonville. The article discussed how Dr. Hodge came to treat patients, teach residents, and train students there. “I recognized that if you don’t have the opportunity to get health care it changes the trajectory for your life,” Dr. Hodge said. A medical mission trip into Central America began his own trajectory: “In rural Honduras, I saw clinicians doing full-scope care. I tied that directly back to family medicine, which allows you to provide the majority of the care your community needs. I applied to medical school thinking I was going to be a family doc.”
“Dr. Jewell Carr might’ve been there too. There was always a good group.”
Thanks to the work that this group does at the state and national level, Dr. Johnson says there’s good reason for family physicians to be hopeful, not apprehensive. “It can feel like things aren’t great for medicine in general,” she says. “But what keeps me grounded is remembering that we’re helping to really take care of people. I’m hopeful for the future of our specialty: there’s a lot of change happening, but you can’t ever replace the relationship between patients and family doctors. There will be a lot of benefit for Family Medicine in the future.”
We’d like to thank Dr. Johnson for her patient care, precepting, and NCAFP leadership.
If you or one of your colleagues is providing a unique service, contact us at kevin@ncafp.com so we can consider spotlighting you or your colleague!
He began in Family Medicine at a federally qualified health center in St. Louis. But in 2010, Dr. Hodge arrived at the Mountain Area Health Education Center (MAHEC) in Hendersonville. Today, he is the Chief Academic Officer for MAHEC. His interests in both teaching and medicine include new models of care delivery, rural workforce development, and interdisciplinary health professions training. “My passion is figuring out how to provide basic, essential primary care for people who need it the most, and how to do it in a way that is impactful, meaningful and allows them to live healthy lives,” Dr. Hodge said.
The NCDHHS Oral Health Program We Helped Found Celebrated 25 Years
In March, the NC Dept. of Health and Human Services (NCDHHS) celebrated 25 years of “Into the Mouths of Babes,” the preventive oral health service insured by NC Medicaid. “Since 2000, this program has helped medical providers across the state give infants and toddlers early dental evaluations, preventive oral health care and other dental services that lay the foundation for good health,” the NCDHHS announcement stated.
continues on next page
“Since Into the Mouths of Babes began, more than 2.8 million claims have been submitted for preventive oral health services,” said Dr. Mark Casey, DDS, MPH, Dental Officer for NC Medicaid. That’s why the NCAFP has been glad to support the program as one of its key founding partners, and why we’re glad to celebrate its 25th anniversary along with NCDHHS.
“The NC Academy of Family Physicians is proud to support this program,” says NCAFP Exec. VP and CEO, Greg Griggs. “It has made a huge difference in reducing tooth decay for children across North Carolina.”

NCDHHS Releases New Measles Testing and Treatment Guidance
On March 3, NC State Epidemiologist Dr. Zack Moore and Immunization Branch Director Carrie Blanchard sent a reminder memo about measles reporting, testing, and vaccination to NC clinicians, due to the ongoing outbreak of measles in Texas, New Mexico, and Oklahoma.
The memo states that “vaccination is highly effective and the best way to prevent measles,” especially in under-vaccinated or unvaccinated patients who plan to travel internationally. It also recommends several steps for diagnosing measles cases and preventing their spread:
• Consider diagnosing measles in patients presenting with a febrile rash illness and symptoms of cough, coryza, and conjunctivitis (especially if they have traveled to a region reporting recent measles cases)
• Contact the state Communicable Disease Branch (919733-3419) or your local health department immediately if you suspect measles
• Implement airborne isolation precautions for any patient with suspected or confirmed measles, including disuse of rooms occupied by suspected or confirmed measles patients for two hours after their visit
In addition, we recommend that you review guidance from the Centers for Disease Control and Prevention (CDC). “[Measles] is easily imported by unvaccinated travelers and can spread in under-immunized communities,” the guidance begins. From there, the one-page guidance includes:
• The measles disease course
• The common symptoms of measles
• The complications of measles
• The steps you can take if you have a suspected measles case
If you have other questions, you can review the state memo, CDC guidance, and many other public health resources at our online resources overview (https://www.ncafp.com/ miscellaneous-public-health-resources).
NCAFP Workforce Initiatives Manager Perry Price Welcomes New Baby Boy!
In late January, our very own Perry Price gave birth to her second son! Both she and the baby are healthy and happy at home. Perry will return from maternity leave in mid-May. If you need questions answered or other information from Perry’s work up until then, here’s how you can contact the NCAFP staff as we fill in for her:
• For information about the AAFP National Conference (FUTURE), the NCAFP Foundation, the Campaign to Grow Tomorrow’s Doctors, or student and resident programming generally, please reach out to Greg Griggs at ggriggs@ncafp.com
• For scheduling a Family Medicine Residency program visit or didactic presentation, please reach out to Shawn Parker at shawn@ncafp.com
• For information about membership or member resources, please reach out to Kevin LaTorre at kevin@ncafp.com
Congratulations to Perry and the rest of the Price family!

For
the
best careers in healthcare You want Novant
Reignite your dedication to practicing family medicine with us at Novant Health. As a valued team member, you will have time to focus on getting to know your patients, their families and their needs. You’ll also be working with a team that shares your values and leaders who care about your work-life balance.
Remarkable reasons to pursue a career with us:
• Physician-led and physician-driven at every level of leadership and in every strategic decision
• Access to technology to help reduce administrative work, including AI charting
• Committed to patient-centered care, where physicians spend more time with each patient
• Lowest turnover rate in the Southeast with more than 2,000 physicians and 40,000 team members at nearly 800 locations across North Carolina and South Carolina
Take a minute to schedule a chat with one of our recruiters to learn more or apply today at NovantHealth.org/PhysicianCareers. Best physicians. Amazing nurses. Remarkable
STUDENT INTEREST & INITIATIVES
By Kevin LaTorre NCAFP Communications and Membership Manager
“It’s a
Game
of 4-D
Chess”: WHAT OUR NCAFP POLICY ELECTIVE STUDENTS LEARNED ABOUT ADVOCACY
In March, four NCAFP members completed their policy elective rotations with the NCAFP team: fourth-year medical student Jamie Crews, fourth-year medical student Maebelle Mathew, third-year resident Dr. Ishan Sahu, and thirdyear resident Dr. Stephanie Wilcher. During their program, these up-and-coming leaders learned about advocating for improved health policy, met with state health care leaders, and joined the 2025 White Coat Wednesday event to advocate directly with their lawmakers.
We were glad to have their help during the rotation and look forward to the good work they will do as family physicians and advocates. We’re also glad to share what they each enjoyed most about the experience:

Jamie Crews 2025 Graduate of the Campbell University School of Osteopathic Medicine
I chose to take the NCAFP policy elective because I wanted to learn how to better advocate for my patients. Throughout my clinical rotations, I have seen how many factors outside of clinic, including access, legislation, and insurance, have significant impacts on patients. While I love caring for my patients in clinic, I wanted to learn how I could advocate for them outside of clinic as well.
The main takeaway I have gotten from this rotation is that there are many different avenues for pursuing health policy and advocacy work. For instance, this elective gave us the opportunity to meet with advocacy leaders in North Carolina from diverse backgrounds. They included leaders from the NC Medical Board, the NC Dept. of Health and Human Services, and Medicaid plans. Many of these meetings opened my eyes to numerous approaches to improving patient outcomes and access to primary care.
I particularly enjoyed learning about the NC Advisory Committee on Cancer Coordination and Control during this elective. Learning more about the impact the committee can have on patient guidelines has given me an idea of what I could do in my future career. Similarly, I enjoyed the opportunity to listen to a NC Immunization Coalition HPV Task Force meeting. I found it interesting to learn how the task force is developing plans to increase access to the HPV vaccine to positively impact communities in NC.
I also participated in my first White Coat Wednesday during this elective, during which I met with legislators and advocated for increased funding for primary care. Prior to White Coat Wednesday, the other learners in the elective and I reviewed and made suggestions to the materials to be handed to legislators that highlighted the significance of primary care in terms of cost-savings and better patient outcomes. This made me feel like I had more ownership of the materials and helped me have successful conversations with legislators about the issues that primary care faces in our state. This experience prepared me to have thoughtful discussions about legislation in the future, and I look forward to the next White Coat Wednesday that I can attend.
Through this elective, I have gained a better understanding of how factors such as legislation, Medicaid plans, and various health committees have an impact on patient care. This rotation has inspired me to find advocacy opportunities as I begin my career as a physician.
Jamie Crews is a fourth-year medical student at Campbell University School of Osteopathic Medicine. She recently matched into Family Medicine at the Novant Health Family Medicine

Residency Program in Charlotte, NC.
Dr. Stephanie Wilcher
NCAFP Board Resident Director 2025 Graduating Resident, Duke University Family Medicine Rural Track Residency
Participating in the NCAFP Health Care Policy and Advocacy Elective was a transformative experience that deepened my understanding of health care leadership, policy, and the critical role that family physicians play in shaping the future of health care. I wanted to complete this elective to learn more about how and why policy decisions come into existence. I also wanted to learn more about the ways I can be involved in health care advocacy right now and in the future.
During this elective, I was able to participate in many meetings, discussions, and hands-on activities to gain perspective on health care policy and its impact on health care delivery, particularly at the community level. These opportunities included attending committee meetings of various advocacy groups in the health care sector, meeting with leadership of health insurance companies, trainings on how to optimize messaging with politicians, and visiting the North Carolina Medical Board to learn about their role in physician practice standards and patient safety. I believe that Family Medicine is not just about medical knowledge or what happens in the exam room with your patient but also about navigating complex health care systems, engaging in advocacy, and addressing social determinants of health. These invaluable experiences allowed me to have a much greater understanding of the “hidden curriculum.”
As my graduation quickly approaches, I feel more prepared to leave residency and enter my first attending position with sharpened skills in advocacy. The people I have met and the experiences I have had during this elective have prepared me to take on active leadership roles, particularly in areas that require policy, advocacy, and the promotion of health care reforms. It has equipped me with tools and perspectives that will help me approach leadership with a focus on systems change, patient-centered care, and social equity. I walk away from this elective feeling inspired and armored, ready for the challenges ahead.
Dr. Wilcher is a third-year resident at the Duke Rural Family Medicine Residency program in Oxford. She grew up in Jacksonville, NC, attended undergrad in Charlotte, and completed
medical school at the East Carolina University (ECU) Brody School of Medicine. She has also earned a master's of public health from ECU. She has been supported along this journey by her husband and two children.
Dr. Ishan Sahu
2025 Graduating Resident, UNC Southeastern Family Medicine Residency

My time in the NCAFP policy elective was a transformative experience that reinforced my deep desire to contribute to meaningful health care policy in North Carolina. As a resident physician proudly serving rural North Carolinians in Robeson County, I have witnessed firsthand the challenges that underserved communities face: barriers to access, physician shortages, and social determinants of health that adversely impact patient outcomes. I pursued this elective to better understand how policy can be leveraged to address these disparities and to become a more effective advocate for my patients.
One of the most impactful experiences during this elective was participating (again) in White Coat Wednesday, where I had the opportunity to meet with policymakers and discuss critical health care issues facing North Carolina. Engaging with legislators and health care leaders, including Rep. Jarrod Lowrey, gave me a clearer understanding of the policy process and the role that legislatures can play. These conversations strengthened my commitment to ensuring that rural communities like Robeson County are not overlooked in health care decision-making.
Beyond policy discussions, the elective provided an eye-opening look at the power of teamwork in health care. Visiting Healing Transitions and Oak City in Raleigh with my fellow NCAFP member Dr. Derrick Hoover, I saw how coordinated, community-driven efforts can profoundly impact individuals struggling with homelessness, addiction, and mental health challenges. These experiences made me reconsider how similar models of integrated care and support could be implemented in rural North Carolina, where such resources are often lacking. I am more determined than ever to advocate for collaborative health care solutions that extend beyond the clinical setting to address the broader needs of patients.
continues as "POLICY ELECTIVE" on back cover
RESIDENTS & NEW PHYSICIANS
By Greg Griggs, MPA, CAE NCAFP Executive Vice President and CEO
North Carolina Enjoyed a Promising Match Day!
On March 21, more than 800 Family Medicine residencies around the U.S. filled 4,574 positions during Match Day! “Family medicine residencies offered a record number of positions in the National Resident Matching Program for the 16th year in a row,” the American Academy of Family Physicians (AAFP) stated. The overall match performance dipped slightly from the 2024 match (by 21 matches). However, the final performance will improve on that number in the end, thanks to the Supplemental Offer and Assistance Program (SOAP) matching.
Thanks to the advocacy of AAFP, the number of national Family Medicine residency slots has increased by more than 100 in four of the past five years.
cess dropping. And those positions that remained available in North Carolina were filled through the SOAP process!
The percentage of North Carolina medical students entering Family Medicine dropped slightly, from just under 12% of our graduates in 2024 to approximately 10.5% this year. That said, their reasons for staying here match the care for others that has historically been the hallmark of NC family physicians.


In North Carolina, the number of first-year residency positions in Family Medicine also increased, with the total number matched into NC Family Medicine residencies increasing and the number of unfilled positions prior to the SOAP pro-
Amanda Nemecek will train at the Cone Health Family Medicine residency in Greensboro after she completes her medical degree at the Univ. of North Carolina School of Medicine (UNC). “I was born and raised in NC and love this state and its people,” she said, “so staying in NC to finish my medical training before becoming a family physician who cares for North Carolinians was an easy decision to make.” She looks forward to the versatility of the specialty: “I am most looking forward to growing my autonomy as a jack-of-all trades family physician during my residency, to then care for all kinds of patients with all kinds of medical concerns.”
Jamie Crews, who after completing her medical degree at the Campbell University School of Osteopathic Medicine will complete her residency at the Novant Health Family Medicine residency program, enjoyed the reward of getting to pursue such work. “Match Day has such a wide range of emotions – anticipation, excitement, anxiety, relief,” she said. “I was ecstatic to learn I had matched into Family Medicine. I had known since before applying to medical school that I wanted to pursue Family Medicine, and that day felt like a major step towards accomplishing my career goals. And so, the pure joy and excitement of opening the envelope and
Maebelle Mathew, Jamie Crews, and Dr. Stephanie Wilcher.
Immediate Past President Dr. Garett Franklin and Amanda Nemecek.
learning I matched at my top choice was incredible. I am so thankful to have matched at Novant!”
And for one NCAFP student member who matched into Family Medicine in a residency outside of North Carolina, returning to the Old North State one day to practice is already the plan: “Just like that, I was headed to the University of Colorado!” said UNC medical student Maebelle Mathew. “I am so excited to train to be a full-spectrum Family Medicine physician. And I’m even more excited to bring what I learn back to North Carolina after residency.” The experience of Match Day itself was its own reward, Maebelle said: “It felt like the pinnacle of my education. Four years of undergrad, one gap year, four years of medical school with one additional year for an extra degree — all of it culminated on Match Day. I hope that every year in residency and beyond, I reflect back to the excitement that I felt on Match Day 2025, and that I grow into a doctor motivated by the same passion, joy, and hope that I felt that day.”
(Both Jamie and Maebelle completed the NCAFP policy elective this past spring, which you can read about on pg. 26.)
And I want to be sure to mention that there are several ways you can help more students match into Family Medicine:
• Serve as a preceptor and mentor to medical students participating in the NCAFP Foundation’s summer programs (reach out to me at ggriggs@ncafp.com if you are interested)
• Donate to the Foundation’s medical student endowment to help fund our ongoing work with medical students (you can do that here: https://www.ncafp.com/ foundation/foundation-donation)
• Complete the Family Medicine Champions program! This free, self-paced AAFP certificate is designed to help champion students entering Family Medicine (you can learn more at https://www.aafp.org/about/who-is-theaafp/initiatives/family-medicine-champions.html)
50 years behind us. Your best future ahead.

CORPORATE SPONSOR OF THE NORTH CAROLINA ACADEMY OF FAMILY PHYSICIANS
PRACTICE MANAGEMENT
The Life of a North Carolina Medical Board Complaint
By Jean Fisher Brinkley NC Medical Board Communications Director
Imagine checking your email and finding a message indicating that you are the subject of a complaint to the North Carolina Medical Board (Board). While no licensee of the Board wants to receive such a message, knowledge of the Board’s investigatory process may help reduce the stress and anxiety related to the experience. It should be noted that in most Board investigations, the Board’s case review process determines that there is not evidence of misconduct or substandard care.
This article will walk you through the life of a Board complaint from start to finish, to demystify the process and provide you with information to respond appropriately, should the need arise.
Step 1: Information Received
The Board is a complaint-driven organization that receives information from a variety of sources, the largest source being complaints from patients and the public. Staff carefully review each complaint to determine if there is a possible basis for Board action in the form of a violation of the NC Medical Practice Act, the Board’s authorizing statute. In a typical year, staff determine about one in four patient complaints do not allege actionable misconduct or they allege matters outside the Board’s jurisdiction, and the matter ends there with no further investigation. Licensees are notified of ALL complaints but are only asked to respond if the Board investigation advances. You should never ignore a request for information — failure to respond to a Board inquiry is itself a basis for the Board to take disciplinary action, and the

Jean Fisher Brinkley is the North Carolina Medical Board Communications Director, a role that involves developing and overseeing production of communications materials and strategies needed to enhance public and professional awareness and understanding of the Board and its mission. She joined NCMB in 2008, after an 11-year career in newspaper journalism, most of it dedicated to reporting on medicine, health policy, and the business aspects of health care. She lives in Raleigh with her husband and two high school-aged daughters.
written response is your first chance to tell your story and ensure that the Board has enough information to understand what occurred.
Step 2: Investigation
Next, Board staff will investigate the allegations. If the case involves the quality of medical care provided, staff review the licensee’s statement, the medical records and, when appropriate, an outside medical review by a medical professional who practices in the same specialty as the licensee, to determine whether care met accepted standards. In some instances, a Board investigator may also seek to interview you and others involved in the case. If you have any doubt about whether you are being contacted by a legitimate agent of the Board, contact the Board by telephone at (919) 326-1100 and ask to speak with the Investigations Department.
Step 3: Senior Staff Review
At this stage, a committee of senior staff members (including representatives from the Office of the Medical Director and the Investigations and Legal Departments) reviews the results of the investigation and recommends a possible resolution for each case. If senior staff find insufficient evidence of a violation, the case is closed without further action, and the licensee and complainant are notified. If senior staff determine the case involves one or more violations, they will recommend the Board take either public or private action to resolve the case and submit those recommendations for
Step 4: Board Review and Case Resolution
The Board’s Disciplinary Committee reviews all cases in which private or public action is recommended. Board Members who serve on the Committee may accept the staff recommendation, recommend something new, or request more information. The Board does not decide cases lightly and has the authority to extend an investigation if it does not feel it has a clear understanding of what occurred.
Once the Board votes on a case, the licensee is notified of the resolution. If public action is authorized, Board attorneys negotiate the specific terms of the case resolution with the licensee or, if applicable, their attorney. If the licensee refuses to accept the authorized case resolution, they have the right to a hearing, which is a process similar to a trial, with a panel of Board Members sitting as judges. The Board strongly encourages licensees to obtain counsel to advocate for their interests, but it is ultimately up to you to decide.
At the end of the day, each case is decided on its unique facts and circumstances. Where discipline or remediation is called for, the Board favors a targeted approach to ensure any concerns are addressed fairly and the public is protected.


Dr. Ishan Sahu (continued): The NCAFP policy elective has prepared me to take a more active role in health care advocacy and policy development. It has reinforced my belief that improving health care in North Carolina requires both direct patient care and strategic policy engagement. Moving forward, I am excited to continue participating in advocacy by serving as the resident member on the NCAFP Advocacy Committee. This role will allow me to further contribute to shaping policies that directly impact my patients and communities like Robeson County.
It was excellent to spend time and learn from Mr. Greg Griggs and Mr. Shawn Parker. I assure you that they are deeply committed to the same goal that we all share: creating a health care system that is equitable, accessible, and sustainable for all North Carolinians.
Dr. Ishan Sahu is a third-year resident at UNC Health Southeastern and will be matriculating into the Atrium Health Cabarrus Sports Medicine Fellowship next year. He is currently serving as the resident member of the NCAFP Advocacy Committee.

Maebelle Mathew 2025 Graduate of the UNC School of Medicine
I chose to participate in this elective because I was very interested in learning what being involved in upstream advocacy could look like as a physician. I also wished to supplement my master’s in public health with hands-on experience in political advocacy. I ultimately hope to have a career that combines downstream, individualized patient care with population health interventions and policy, and this rotation felt like an important way to explore what that career could look like. This rotation was incredibly enlightening, and I learned so much!
During the rotation, we sat in on meetings with Greg Griggs and Shawn Parker and watched how they advocated for Family Medicine physicians, whether it was in the state legislature with our representatives, with insurance companies, or with pharmaceutical representatives. We also had the opportunity to meet with family physicians who went on to become leaders in these spaces, such as the chief medical officers of multiple NC Medicaid Managed Care Organizations.
My main takeaways were:
1. There is so much more advocacy beyond what happens in the state and national policy spheres. Every meeting has the potential to build a relationship or move the needle in one direction or the other. There’s also a lot of value in knowing when and how to advocate – it’s a game of 4-D chess, as Greg said.
2. As someone who is deeply frustrated with how our health system is currently built, I frequently walked into our meetings with Medicaid CMOs expecting to feel similarly frustrated with them. Yet, after hearing their journeys and the perspectives with which they approach their work, it was impossible for me to dislike them. In fact, I left the meetings not only having learned a lot but being grateful that if someone had to be in the position, it was these wonderful family physicians.
This past month made it obvious that advocacy can happen in a multitude of ways, especially as a family physician. It also showed that effective advocacy requires building relationships and approaching all situations and people with a mind open enough to be able to listen to all stakeholders at the table, whether we agree or disagree on a certain topic. I am very grateful for the opportunity to learn and work with the NCAFP, Greg, and Shawn this month, and I’m excited to apply what I’ve learned throughout my career.
Maebelle Mathew is a 4th-year medical student at the UNC School of Medicine and will be starting her Family Medicine residency at the University of Colorado in July. She is originally from Raleigh and completed her undergraduate degree and master’s in public health at UNC.
To read more about the White Coat Wednesday event that these students and residents mention, read the full event recap article on pg. 10!
