THE NORTH CAROLINA
Volume 9 Issue 1 / Winter 2013
quarterly news in north carolina family medicine
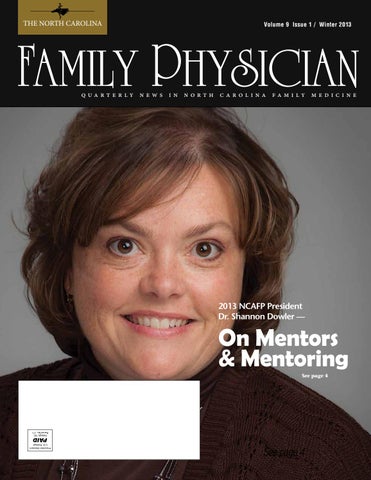
2013 NCAFP President Dr. Shannon Dowler —
On Mentors & Mentoring See page 4
See page 4 Winter 2013 • The NC Family Physician
1
THE NORTH CAROLINA
Volume 9 Issue 1 / Winter 2013
quarterly news in north carolina family medicine
2013 NCAFP President Dr. Shannon Dowler —
On Mentors & Mentoring See page 4
See page 4 Winter 2013 • The NC Family Physician
1