




Welcome to this winter issue of Kidney Life. It’s been a busy few weeks and there’s lots of content this time. We’ve continued the theme of kidney donation with an article on organ donation utilisation from NHS Blood and Transplant and a personal perspective from Consultant Nephrologist, Gareth Jones.
Recognising how much people’s stories are appreciated in each issue of Kidney Life, there are four this time around. They are all tied to our theme of organ donation and are again from different perspectives. Some of the stories are tough to tell and detail difficult and very personal situations. My grateful thanks to all contributors. It’s been great working with you.
We also have one personal account of a bereavement, which as well as being heartfelt and touching, provides practical advice. We’ve included some information which is new to the NKF website about bereavement. Not an easy topic to cover but necessary for all of us to consider.
There’s also plenty to celebrate! Not least 25 remarkable years of the NKF Helpline, the recently held Annual Patients' Event and of course, Christmas is coming. I hope you enjoy reading this issue and, as ever, your feedback and comments are very welcome.
With best wishes for the coming festivities.
Best wishes
Annie Taylor Editor
09 Giving and Receiving the Gift of Life 10 Organ Donation – a Noble Act... 14 In Praise of Anonymous Donors.... 16 The Last Option: A Carer’s Perspective
04 NKF’s Annual Patients’ Event 2024
06 Kidney Transplantation
08 Understanding the process of receiving a donated kidney
12 NKF Helpline Celebrating 25 years
18 Managing the Death of a Loved One
20 TASTE – Devonshire Spiced Apple Cake PUZZLES
20 Spot the Difference FUNDRAISING
22 Round up of Fundraising Activities
NKF OFFICERS
Chairman – David Coyle
Co Vice Chair – Caryl Bryant
Co Vice Chair – Tarsem Paul
Treasurer – Mike Sinfield
Secretary – Brian Child
NKF TEAM
Andrea Brown – Chief Executive
Pete Revell – Head of Marketing & Fundraising
Donna Blizard – Office Manager
Jessica Jones – Policy & Public Affairs Manager
Sharney Warren – Communications and Marketing Officer
Fiona Broomhead – Senior Office Administrator
Chloe Ainsworth – Social Media and Website Coordinator
Heather Mooney – Accounts Administrator
Chris Talbot – Membership Development Lead
Linda Pickering – Helpline Advisor
Stephen Emmerson – Helpline Advisor and Peer
Support Coordinator

NKF Chief Executive, Andrea Brown provides a brief overview of what has been a very busy year.
NKF has had a very busy and productive year and we have been helping and supporting our wonderful kidney patients and their families like never before. We have had an unprecedented request for support this year, which is great, we want everyone to know we are here to help and support them.
Our wonderful Helpline is 25 years old this year and is the hub of our headquarters. The Helpline has been busy chatting and supporting almost 5,000 people, sending out over 70,500 patient information leaflets to individuals and renal units this year alone. Our peer support service, run through the Helpline is going from strength to strength, supporting patients and family members to speak to like-minded patients and family members to gain insights and knowledge into their disease.
We have been busy campaigning and lobbying the Government to improve kidney care in hospitals and renal units. Our increasing home dialysis campaign is in its fourth year and next year we will have a summit in Parliament and will produce a manifesto for change.
We have also been working closer with our member Kidney Patient Associations to make sure the local and regional voice is heard, as well as at a national level with NHS England.
For those of you who attended our Annual Patients’ Event, we hope you enjoyed it and for those of you who didn’t attend, please come and join us next year. It is a wonderful event to chat, socialise, have a great time with others and do a little bit of learning in between.
The NKF has been in demand, and all of this comes at a cost. We have sustained a huge financial loss this year and we need your help and support more than ever. We simply cannot survive and provide the help and support needed without income from our generous supporters like you. We do not get any Government support we rely totally on donations.
We have inserted a leaflet into this issue of Kidney Life where you can become a regular donor. You could try one of our fundraising events where you could take a hike, do a skydive or just organise a tea party.
Further information can be found on our website www.kidney.org.uk and by clicking on the tab ‘Get involved’. You could also support us by leaving a gift in your will. We provide a free will writing service and you can find more information on page 22.
Whatever pennies or pounds you can give will be very gratefully received. Kidney disease is for life, together we will continue the fight to help and support our kidney community.
May I take this opportunity to thank you for your support and wish you all a wonderful Christmas and a healthy and happy 2025.
We have been busy campaigning and lobbying the Government to improve kidney care in hospitals and renal units. Our increasing home dialysis campaign is in its fourth year and next year we will have a summit in Parliament and will produce a manifesto for change.
Sponsored by:

Remarkable shoes, shaking hands with your eyes shut, moving more and sitting less and how to get a tattoo when you’re needle phobic - what a day!
It was a cool and beautifully sunny morning as we gathered for the Annual Patients’ Event on Saturday 26th October. Many people had arrived the night before after long, tedious journeys but enjoyed an evening of pie and mash and a quiz which was won by Team Lister! The evening was kindly sponsored by Diaverum.
There was a lively vibe before the programme of speakers even began with lots of meeting up of old friends, introductions to new friends, catching-up conversations and exploration of the exhibitors’ stands. Before presentations started NKF Chair, David Coyle gave everyone a very warm welcome and we stood for a minute to remember people we have lost over the last year. He outlined progress and changes the NKF has made and described the competition for charities to be heard amongst all the noise as everyone wants the ear of
Presentation
Welcome & Introduction
Renal Social Work – The Role, Tips & Strategies
NHSBT Organ Donation
How Peer Support Helps Home Therapies
Me, My Kidneys & Eyes
Move More, Sit Less
Ready, Steady, Go – Empowering Patients Together
A Stepmother's Journey with a Child who has Additional Needs
Symptoms in Advanced Kidney Disease /Dialysis & Transplantation Medications



the new government. It’s a challenging environment. Needless to say each person presenting throughout the day gave us new insight, information and knowledge. All demonstrated passion, care and dedication for their subject, whether it was hugely practical or very personal. And whatever their role all were giving their time and had joined us to help make a difference to the lives of others.
The programme is below and each presentation was filmed. The films and slide presentations are all available to access on the NKF website at www.kidney.org.uk/ event/national-kidney-federation-annual-patientsevent-2024 If you weren’t able to be with us this year, have a look at how the day unfolded and hopefully join us next year. The date will be announced in the New Year and in the meantime – enjoy some photos from the day.
Speaker
David Coyle, NKF Chair
Alison Richards & Jayne Davis, Renal Social Workers
Jackie Brander – NHSBT Head of Operations
Patricia Gooden – NKF Peer Supporter
Sam Honeywill – Patient Speaker
Dr Pelagia Koufaki, Reader in Clinical Exercise, Physiology & Rehabilitation
Dr Arvind Nagra, Consultant Paediatric Nephrologist
Erica and Zac Stanley – Stepmum and Stepson
Amy Page – Renal Specialist Clinical Pharmacist – Renal Transplant / Cathy Pogson – Renal Specialist, Clinical, Academic Pharmacist (Sponsored by Stanningley Pharma)














































The third article in our series on kidney transplantation looks at how a donated kidney is offered to a patient on the transplant waiting list. Presented here are some of the details, including why some organs are declined. We are grateful to Jennifer Mehew, Principal Statistician and Lisa Mumford, Head of OTDT Studies, Statistics and Clinical Research at NHS Blood and Transplant who provided the information for the article. Following on is an article by Consultant Nephologist, Dr Gareth Jones who answered my questions with a more personal perspective from the Royal Free London, NHS Foundation Trust.
In the UK, deceased donor kidneys are offered through the UK Kidney Offering Scheme. This is a computer algorithm that orders all patients on the kidney waiting list by a score that is calculated according to a number of donor and patient factors. When a kidney becomes available, NHS Blood and Transplant (NHSBT) contacts the transplant centres in this order, where the centre considers whether the kidney is suitable for the patient to whom it will be offered. If the transplant centre declines the organ on behalf of the patient, the next centre and patient in the offering list is then contacted.
The UK Transplant Registry (UKTR), held by NHSBT, records information on every offer of a kidney that is made. This includes which transplant centre and patient were offered the kidney, and the offer result (i.e. if it was accepted or declined). If the offer was declined, the reason for decline is captured. If the offer was accepted, information on the removal, transport and transplant of the organ is captured. All patients who receive a transplant are followed up regularly and this information is also stored on the UKTR.

Organ Specific Report for each organ (www.odt. nhs.uk/statistics-and-reports/organ-specificreports/ ). The kidney report presents a wealth of information, often reported for each centre separately, including:
• Waiting list summaries
• Responses to kidney offers
• Transplant summaries
• Patient outcomes after the transplant
Understanding patterns in the response to kidney offers is important when assessing organ utilisation. We can do this by looking at the proportion of ‘transplantable’ kidney offers that were declined and can compare this between each centre. We call this an offer decline rate. Not all kidneys that are offered are suitable for transplant so we only consider kidneys that were eventually transplanted in this particular analysis.
The Annual Report of Kidney Transplantation (2023/24) presents adult offer decline rates for each centre, for DBD offers received between 1 April 2021 and 31 March 2024 where the kidney was eventually transplanted.


Reasons for non-use for kidneys removed from DBD donors in the UK, 1 April 2023 to 31 March 2024.
During the year 1 April 2023 to 31 March 2024, 1488 DBD kidneys were offered for donation; 1438 of these organs were removed from the donor. While 1276 (89%) of the removed kidneys were transplanted, 162 (11%) were not transplanted and the reasons for not being transplanted are shown below.
Adult standard criteria DBD donor kidney offer decline rates by transplant centre, 1st April 2021 to 31st March 2024 for kidneys that were eventually transplanted.
This table considers offers from ‘Standard Criteria Donors’ after Brain Stem Death (DBD) only and the full list of inclusion and exclusion criteria can be found in the report. Data on Donation after Circulatory Death (DCD), is not reported on here.
It is also important to understand why kidneys that were removed from the donor, were not used. For kidneys that were removed from DBD donors, the most common reasons for non-use are related to either the donor or the organ being unsuitable for medical or clinical reasons.

The demand for organs is far greater than the supply. We do not have enough organs to transplant everyone in need. By understanding why some organs are not utilised, we can work towards increasing the number of organs that could be transplanted. This will help to save and improve patients’ lives. This is the work of the Department of Health and Social Care’s Organ Utilisation Group (whose work was detailed in the last issue of Kidney Life).
Jennifer
Mehew, Principal Statistician and Lisa Mumford, Head of OTDT Studies, Statistics and Clinical Research, NHS Blood and Transplant.


Jennifer Mehew Lisa Mumford
I (Ed) recently talked to Gareth Jones, Consultant Nephrologist at the Royal Free in London to help me understand the process of receiving a transplant. I wanted to gain a more personal perspective and this is what Gareth told me.
The most common way we receive a kidney is as a name offer through the UK Kidney Offering Scheme. The national allocation algorithm takes many factors into account and allocates points to the 6,000 people on the transplant waiting list. Whoever has the most points will have the kidney allocated to them.
However it’s not completely straightforward. When the call comes through to the Transplant Centre we have to consider donor characteristics and establish if that donor’s kidney is the correct kidney for the named recipient. The algorithm takes blood group and matching into account and considers the risk category of the donor, of which age is the strongest predictor of long term transplant survival.
Before changes were made to the system in 2019, if you had an identically matched kidney from a 20 year old donor, it could be allocated to someone who was 70 or 80 years old or vice versa, just because it matched perfectly. Now we consider whether that’s the correct use of the organ, because the younger person transplanted with a very old kidney will need retransplanting sooner, while the older person may not outlive their kidney. The kidney may still have many years left, so we have to consider if it should go to someone younger who would get more use out of that kidney. These were some of the arguments that went through the ethics of allocation. The algorithm also considers how difficult the person needing the kidney is to match, how long that person has been waiting, how well it matches the prospective recipient, where the kidney is in relation to the potential recipient and a few other factors.
When the call comes through and you have a kidney allocated to a person, you then go through all these questions in your head and ultimately ask “Is this the right kidney for this person?”
An extreme example would be if you are someone who has been on dialysis for a few years, that’s the highest risk part of your journey. So you may be prepared to accept a higher risk donor than someone who isn’t yet on dialysis. The risk is not just age and whether the donor has diabetes or high BP but what if the donor had been involved in risky behaviours – did they take IV drugs, were they a sex worker, did they have brain cancer, did they have hepatitis? Balancing the risk for someone who is well, not yet on dialysis and easy to match is harder as you’re not going to take a higher risk. There are ways of looking at donor risk through scoring and calculations, but at the end of the day you can never 100% predict what’s going to happen to that kidney.
At some transplant centres, it’s the surgeon or coordinator who phones the patient to tell them a kidney is available. I get

to make the call when I am on duty. I usually tell the person a little about the donor, just broad information, to help them make up their mind. If the donor is a young healthy, fit person with excellent kidney function and no medical history then it’s straightforward. I’m saying, ‘This is an amazing kidney you really need to come in and have this!’. But if the donor is someone who had high BP and diabetes or may have had a past knock to their kidney function or a previous cancer, then you have to talk those issues through. It’s interesting how people have different ideas about getting a kidney from someone who may have used drugs. Some people will say absolutely not, while others say yes, if you tell me the risk is small, I need to get off dialysis and I want this kidney now. Risk is a very personal issue for everyone when they make the decision. A few people ask what I would do. Some make their mind up very quickly and say yes while others say no, I don’t want this kidney.
Generally it’s a really great thing to do – to tell someone a kidney is available. There are not many things I love about being on call, but it’s great to phone a person up and say, ‘Hello, we’ve got a kidney for you and you need to come in’. The response is often ‘I’m on my way!’ Some people are really excited and can’t believe it because they’ve been on dialysis for a long time. It’s not surprising people remember the day, the time, the minute they got the call and how they responded – it’s a massive thing, because it’s life changing.
Some people turn the offer down. They ask if they really need to come now. We recently phoned one person to tell them a kidney was available and they said they were not sure and needed time. We tried to call them back but we couldn’t get hold of them. Sometimes it’s a very difficult thing when you’ve been waiting a long time and you’re finally facing a transplant. I think this is because when people have health problems it can be overwhelming and you can’t always see the potential difference it’s going to make.
The patient journey to transplant begins when the person is assessed as suitable and added to a waiting list following a visit to the consent clinic. We always tell patients to make sure they always answer their phone and answer calls from private numbers. When the person arrives for their transplant surgery they are seen by the transplant surgeon who will look after them post-transplant before referring them back to the nephrologist and team. Here at the Royal Free, patients see a surgeon and a nephrologist every day after surgery until discharged home. As a transplant nephrologist I look after people for around three months and then hand them back to the team who were caring for them before their transplant.
Ruth Colebrook shares her family’s story on how her son, Nic became a deceased donor and why she believes we should all think about carrying donor cards.
Our connection with the National Kidney Federation (NKF) began soon after our son Nic died in a motorcycle accident. He was carrying a donor card and we actually had to ask the hospital to use whatever organs they could. This was in 1982 and there was no transplant coordinator at the hospital at that time.
In the very hot summer of 1976, my cousin’s young son had lost all kidney function following a nasty infection. He had frequent transfusions and was limited to a quarter of a pint of fluid a day. Two years later he had a kidney transplant which completely changed his life. So having seen at first hand the impact transplantation had on someone’s life, when donor cards became available Nic and all our family carried them.
When Nic died there was little help available to the families of donors. We had absolutely no feedback. Martin my husband, who was a doctor wrote to the British Medical Journal about his experience of losing our son and that at least we had fulfilled Nic’s wishes to be a donor in the event of his death. Other bereaved parents contacted us and we became part of a group trying to get better support for families of donors. At some point we became involved with the NKF and were asked to speak at their Annual Patients’ Event.
Then in 1985 to our great joy our eldest son Tim became engaged to Jane. However, it was shortly after that Jane became seriously ill and was rushed to Addenbrookes with acute kidney failure. Dialysis was a difficult procedure for her.


They tried to make it as special as possible the night before their wedding and gave them an extra day for their honeymoon.
Three weeks later she had a kidney transplant which did not take at all and within two weeks they had to remove the kidney. The next two years were really difficult for them and then it was suggested that she might do better on peritoneal dialysis. Slowly her life improved and she was able to work full time and eat and drink most things, she even went swimming regularly.
On September 27th 1989 I had a phone call in the night and it was Tim to say Jane had been offered another transplant. This time it was a completely different experience and she was home just eight days later.
This second transplant was so successful they presented me with a grandson on January 12th 1991. They called him Peter after the surgeon who performed Jane’s transplant. He was 7 weeks early and in an incubator to start with.
Less than a year later, his brother William was born and in 1995 they were joined by Joe. These three boys have grown into wonderful young men and in November 2021 Peter and his fiancée presented me with my first great grandchild, Daisy.
All these lives because someone became a kidney donor for Jane. Such a generous gift gave us our miracle family.
Jane’s story can be found in the Spring 2024 issue of Kidney Life on Page 16.
and Jane with Daisy

In this article, Dhiru Galani shares his family’s story of losing his wife, Indira, and the decision they made to donate her organs.
My name is Dhiru Galani. I’m 76 years old. I was born in Mombasa, Kenya and I have lived in London since 1972. My wife, Indira passed away in April 2022. She had been unwell for some time and I was her primary carer but she was living a relatively full and active life, and her death was nonetheless sudden and unexpected. She was 74 years old and was born outside of Kampala in Uganda. We raised three daughters in the UK. We are Gujarati Indians by ethnic heritage and were born into the Jain religion.
My wife was initially rushed to hospital in April 2022 after struggling to swallow food and suffering a cardiac arrest. My wife’s condition was diagnosed as 90% brain damage. We were informed of this after the doctors had stabilised her breathing.
With my two daughters present, we looked at each other and without any discussion we rapidly concluded that as this was the case Indira’s quality of life would be zero. As a family we often talk about the importance of quality of life.
The next day, the doctors informed us that there was no progress and that they would like to do a clinical test called “Brain Stem Test” which determines if someone is clinically brain dead. The clinical test is done twice, once by two doctors who are not connected to the transplant team. And the second time in front of the family. However, the time of death is when the first test is done.
The tests include:
1 A torch shone into the eyes to see if there is a reaction to light
2 The eye is stroked with a tissue to see if it reacts
3 Ice cold water is inserted into each ear to see if the eyes move
4 A ventilator is disconnected for a short period to see if the patient makes any attempt to breathe on their own
5 A thin plastic tube is inserted into the windpipe to see if it provokes coughing.
If the person does not respond to these tests, they are deemed to be brain dead.

Dhiru and Indira in happy times
After these tests were done to Indira, myself and my daughters unanimously decided to take the organ donation route. Most importantly, Indira had already registered to donate any organs that were suitable. I remember that we had both made the decision to donate our organs at a Navnat Vanik Association Janmasthami Mela a good few years ago. This is an annual summer fair organised for our Jain and Hindu community in the Greater London area.
For me personally, I am one of the youngest siblings in a large family and was always more open minded than the others. The age-gap with my eldest siblings is almost an entire generation.
Indira was more open-minded too because she was a hospital and care-home nurse for most of her working life. And it was the decision of the immediate family.
As far as I know Jainism to a very large extent is about seva (which means service) and compassion. However, religion played very little part in our decision.
When I met Indira back in 1974, I quickly noticed that she had a very charitable nature and was always willing to serve without any expectations. After her health deteriorated and she stopped working as a nurse, she continued to volunteer at an Oxfam store for nearly 15 years. For Indira, organ donation was a final act of charity to help others in need.
All that said, if we want the wider Jain and Hindu community to sign up for organ donation – it is helpful to present it as an act of seva. It is also

important to share personal experiences as much as possible. This will help to normalise it within the community. If a few people do it and talk about it, many more will follow.
Once clinical death was confirmed, we were told that a specialist nurse would come and talk to us about organ donation. The nurse showed a lot of empathy. She was aware that Indira had filled in her organ donation form.
She still asked us if the family was in favour of organ donation. When I queried why she was asking if the family was in favour of organ donation, she replied that they would respect family’s views. I’m unsure if the family’s decision could have over-ridden Indira’s personal wishes.
She also asked what music would Indira like played during the organ removal procedure. She then informed us the likely time and in which hospital the organ transfers would take place and the time when the ventilator would be switched off. It was comforting to know these details, and we shared them with the extended family.
In terms of the funeral arrangements, we had selected a funeral parlour that would take care of cremation and they would liaise with the hospital to collect the body of Indira. The funeral parlour asked if we have any preference for a venue and what religious service we would like.
Indira’s kidneys and eyes were successfully transplanted in four recipients. However, we are not aware if the rest of the organs contributed to lives improved or were used for research.
We as a family are very happy and proud that Indira had signed the form for organ donation earlier and are very pleased that Indira’s final act was true to her nature of service.
My message to our community is that I urge your family to fill in the organ donation form.

I wholeheartedly will promote Organ Donation within our community and I’m more than happy to give our example of how we can benefit those still waiting for transplants.
I also believe religious scholars can play a big part. When we invite scholars from India to talk here during our religious festivities, they could explain that religion does not forbid organ donation. In fact, they should encourage donation and explain that it is a good service that may earn good karmas.
It is worth quoting from Bhagvad Gita, Chapter 2, Text 25. It says, “The soul is invisible, inconceivable, and immutable. Knowing this you should not grieve for the body.” That means once the soul has departed, the body is an empty shell. So, taking organs out should not be an issue.
Thank you and I hope you all will spread the message of organ donation within your wider family and friends.
To register your decision on the NHS Organ Donor Register visit: www.organdonation.nhs.uk/ register-your-decision/


The NKF is proud to share a significant milestone—the 25th anniversary of its Helpline services. For a quarter of a century, the NKF Helpline has been a lifeline of hope and an essential support system for patients and their families affected by kidney disease.
Since 1999 the NKF Helpline, which is based in Worksop in Nottinghamshire, has provided free guidance, support and information to more than 100,000 people.
NKF’s two dedicated Helpline advisers, Stephen Emmerson and Linda Pickering, have first-hand experience and deep understanding of the challenges that come with kidney disease. Stephen has undergone two kidney transplants and has spent time on dialysis, and so brings a wealth of knowledge and empathy to the role. Meanwhile Linda, who cared for her late husband with kidney disease and has previously worked as an advocacy officer for kidney patients, offers another unique perspective.
Together Stephen and Linda have knowledge of a wide range of topics, from renal diet information, end of life care to travel insurance, and much more. Their expertise ensures that callers to the Helpline receive the guidance they need and are signposted to the right specialised services when necessary.
Sue Collins, a retired health professional aged 66 from Southampton, shares her experience of using the NKF Helpline. She explains that the Helpline became an integral part of her and her 65-year-old husband Michael’s journey through kidney disease.

"My husband had been in chronic renal failure for many years before he was diagnosed with renal cancer," Sue recalls. "He was told that the treatment for the cancer would be a nephrectomy, but he would need to commence dialysis prior to surgery, which would continue for life. He did not want surgery or dialysis and chose to go down the palliative care route."
Sue needed information and guidance to help her support her husband. Sue told us "As a retired health professional, the first thing I did when we arrived home was turn to the internet for information. I found the National Kidney Federation’s website and ordered some relevant leaflets which were free and arrived quickly. They were so helpful."
The NKF Helpline continued to provide much-needed support when other avenues fell short. She continued; "Whilst palliative care support was available and still is, care from the acute teams stopped. This wasn’t a problem for my husband — he didn’t want to know about his kidney function. However, it was a huge problem for me. I wanted to understand the issues and side effects."
Sue reflects on how the NKF Helpline became a continuous source of support: "My memories from the initial diagnosis years ago were that my husband’s life was very limited. It was then I commenced a friendship journey with the NKF Helpline. Little did I know then how long that journey of friendship would be, and is still ongoing.
I have had the same adviser throughout my journey, and they have been empathetic, knowledgeable, and nonjudgmental."
Sue added; "There is something unique about writing to someone you haven’t met but feel you know a tiny bit about, who understands you and replies in a caring, knowledgeable way. I have been able to share things with them that I haven’t spoken to family and friends about."
The busy Helpline office
There is something unique about writing to someone you haven’t met but feel you know a tiny bit about, who understands you and replies in a caring, knowledgeable way. I have been able to share things with them that I haven’t spoken to family and friends about.

Information leaflets are in high demand
Sue encourages other caregivers to utilise the NKF Helpline, noting its importance: "The Helpline is something for me, when you are caring for someone 24/7. It’s also not always appropriate to ask questions that relate to the patient when they are there, so being able to share experiences and issues helps and puts everything in perspective."
She concludes, "My husband doesn’t seem to fit into other support groups. I therefore really value the Helpline and would encourage other carers in similar situations to use it."
The Helpline provides a safe and supportive space for patients and carers to seek guidance, share their experiences, and receive empathetic and knowledgeable guidance.
In the last 12 months, the Helpline has posted free of charge 70,500 information leaflets to patients and carers, and has had over 5,000 helpline connections, whether that be a call to the Helpline, letters, email queries, or messages via the live web chat facility on the NKF website.
Duncan, another caller to the NKF Helpline commented on the free support service and how the Helpline was able to provide assurance around his dialysis treatment; “I was growing despondent and increasingly depressed due to a long-running problem with my dialysis treatment. I contacted the NKF Helpline and the positive response I received from the advisers not only made me
feel empowered, but offered suggestions on how I might solve the issue around my treatment. Without the help from the NKF’s Helpline, I might have given up in despair.”
Linda and Stephen, NKF Helpline Advisers commented; “We are immensely proud to serve as Helpline advisers for kidney patients and their families. Having experienced the effects of kidney disease first-hand, we understand its impact and find it incredibly rewarding to offer guidance and support to others. We would like to thank all of our callers, people who have written to us or emailed us, both past and present for confiding in us."
Andrea Brown, NKF Chief Executive commented; “We are so pleased to know that Sue, Duncan and many other individuals over the years have had a positive and reassuring experience with the Helpline support that we offer. Long may our Helpline and patient support services continue. Without the help of our supporters, we would not be able to provide our free services. Our valued supporters show dedication day in and day out, either by taking up a fundraising challenge, making a regular donation, or taking part in their own activities for the NKF.”
For more information about our free patient support services please visit www.kidney.org.uk, contact the NKF Freephone Helpline on 0800 169 09 36 or email helpline@kidney.org.uk.
To donate and make a difference visit: www.kidney.org.uk/donate
Long may our Helpline and patient support services continue. Without the help of our supporters, we would not be able to provide our free services. Our valued supporters show dedication day in and day out, either by taking up a fundraising challenge, making a regular donation, or taking part in their own activities for the NKF.
by Roger Wilks

I received a kidney transplant in July of 2014 at St George’s Hospital, Tooting in South London. I want to share my experience of receiving a donated kidney from an anonymous donor with some emphasis on the benefits of the anonymity in contrast to receiving a kidney from a known donor.
My transplant journey began with a diagnosis of Polycystic Kidney Disease which was made just before Christmas 1997. This condition was inherited from my father who then sadly died a few months later after a long battle to stay alive on dialysis. I was under the care of the Renal Department at St Helier Hospital, Carshalton, and following a rising tide of cyst aggravated kidney infections, and decreasing renal function, I commenced continuous ambulatory peritoneal dialysis, (CAPD), in 2013. I also went on the waiting list for a kidney transplant where there was a suggested waiting time of up to five years. I decided that CAPD was the best choice for me so that I could continue working in the NHS as a Psychotherapist in Mental Health. With CAPD I had to perform four exchanges each day and I was able to dialyse at work in between seeing patients and all the other tasks of a busy outpatient Psychotherapy Department. However, while this new lifestyle came with significant compromises, dialysis gave me a new lease of life and hope for the future which was immensely valuable and the ability to continue working.
Once I was on the transplant register a few valiant friends came forward to offer me a kidney, but in the end only one of them had the right blood group to be in the running to take the next step. One might think that this noble and generous act of friendship would be received by me with unequivocal gratitude and relief, but this was not entirely the case. I already had mixed feelings about the psychological impact of having someone else’s organ functioning in my body, and inevitably this feeling intensified with the knowledge that this organ could be coming from someone that I knew well which at once exacerbated my hesitancy
with this new trajectory in my renal journey. With the clock ticking, I felt like I had to make a quick decision while at the same time I had a burgeoning sense that an anonymous donor might be a better solution for me without fully realising the full implications of making this choice.
I had been informed that a live donation offered a better outcome in terms of the life of the kidney versus one donated from a deceased donor, therefore, live donorship seemed to be the option to aim for. Transplantation is a combination of serious scientific and non-scientific considerations like compatibility, expediency and time limits. The friend who was able to offer me a kidney once that was confirmed said to me one day “You will look after it won’t you?”. This was not said in jest and left me with an increasing sense of foreboding, especially if I decided to take up the offer. I thought, “Does that mean if I don’t look after it, you will want it back?”. It was beginning to feel like my future life might be at risk of unwanted interferences and a peculiar sense that my own body didn’t entirely belong to me. Overall, this offer at once seemed to be conditional, somewhat controlling and invasive. These are not desirable characteristics at any time and certainly not when one is waiting for a kidney transplant. It further crystallised my thinking that an anonymous donor might be the most preferable way forward as it simply avoided a debt that could never fully be paid off. As my hesitancy and anxiety about this looming clash of interests intensified, complicating an already challenging time, I was saved by the bell.
One warm Tuesday afternoon in July I was at home doing a dialysis exchange when the landline screamed from the hall. I couldn’t answer it because I was

upstairs and plugged in to a bag and I had no mobile phone to utilise. This was the call from St George’s to say that they had a kidney for me and I nearly fell off my chair in shock. I had only been on dialysis for nine months and I had settled in to a mindset of waiting for several years before this kind of call came through. Following a strange expectant afternoon, I eventually went off to Tooting in South London for a transplant. What followed was a whirlwind of medical activity and by late evening I was wheelchaired off to theatre which seemed to be about as far away from the Renal Department as was possible in an enormous hospital. En route, Germany were busy thrashing Brazil 7 – 1 in the semi-finals of the World Cup, and the hospital seemed to have evacuated its entire population to outlying offices where the ghostly glow of television screens punctured the night-time gloom of empty corridors. This just added to the drama of such a momentous occasion and sometime before midnight I nodded off and woke up the next morning with an extra kidney and that was that.
It became evident to me pretty quickly as my new normal life gradually gained momentum that this immediate response to the offer from a deceased donor was undoubtedly the right choice. It also took the decision for me to choose the right form of donation completely out of my hands. This in itself was a huge relief. I didn’t weigh up the pros and cons of accepting this offer for a second, whereas I most certainly did when it came to considering offers from known live donors, which says something positive about the decision that I had already made without realising it. I am hugely indebted to the donor of whom I know nothing apart from age and gender and a letter of thanks and good wishes was promptly sent to the donor’s family via the hospital administration. Without wishing to diminish this extraordinary act of benevolence, it became very clear to me how liberating this anonymity shaped my own post-transplant
psychology. It was almost like going to Halfords and getting a new oil filter; free of personal ties and all that goes with that. Anonymity is hugely advantageous simply because it depersonalises human tissue in such a way that normal life can resume, completely unencumbered by invasive emotional considerations in a similar way to the implantation of a coronary stent which I am also a recipient of.
The overall emphasis in renal transplantation is inevitably biological and while the transplant team have to deal with some of the psychological aspects of this process especially with regard to donorship, the value of anonymised kidney donation can be underrated because it has a most valuable part to play in shaping the freedom of one’s future life. Ultimately, a kidney transplant from an anonymous donor is simply a triumph of function over feeling which helpfully circumnavigates any power differential that can be encountered in some circumstances if one goes down the route of known donorship. Ten years on, I don’t even consider that my life depends on a plumbed in organ from the body of someone else whom I have never met and never known. This blissful ignorance is comforting and it gives me the freedom to live without additional relational complications for which I am thankful. I am even more convinced now that I made the right decision and I am glad that I didn’t hesitate when that rather unanticipated telephone call came through on that warm Tuesday afternoon.
This article is dedicated with enormous gratitude to the anonymous donor of my kidney, St Helier Hospital, Carshalton, St George’s Hospital, Tooting, Derriford Hospital, Plymouth, and my wife who over many years has had rather a lot to put up with.
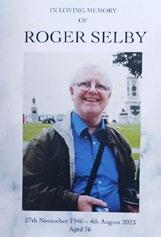
In this article Peggy Selby describes her experience of caring for her husband Roger as he made the difficult decision to stop his treatment. Recognising what a difficult and sensitive subject this is to share, we are grateful to Peggy for her candour, honesty and pragmatism which we hope readers will find inspiring. These are Peggy’s words.
Anyone with kidney problems will be considering at various times a number of different options: transplant, dialysis in centre or at home, peritoneal or haemo, different types of dialysis machine and regime.
Once on dialysis there is then always the option of stopping dialysis, which means bringing life to an end. This is not often talked about, it’s not something you want to think about, but in the same way that it’s sensible to make a will, it’s also good to be aware of the option and to have given it some thought.
Everyone’s circumstances are different. You may not be much involved with your partner’s dialysis; you may be doing just about everything for him/her. Or something in between.
My experience:
My husband Roger, aged 76, found himself, after nine years of haemodialysis at home, in critical care, very ill with internal bleeding and heart problems. He came to the decision that he wanted to stop dialysis, which meant returning to the renal ward while the palliative care team found him a place in the local hospice. Roger died 36 hours after moving there and around 6 days after his last dialysis session.
A transplant was never an option for Roger; dialysis was his gift of life. We trained to do it together at home right from the start. And we worked as a team – Roger put the needles in, I attached him to the machine. He set the machine up, I did the preparation, cleaning and admin.
I’ve never liked the terms 'patient' and 'carer'. To me, it implies the “patient” is helpless, which Roger certainly wasn’t. There’s no getting away from the fact that illness and the developing health conditions of your partner
brings an added dimension to your relationship though. And when someone is ill and becoming very ill, they tend to focus in on themselves, finding it difficult to think about anything else. This is totally understandable, but adds to the stress for their partner, who is also worried about the “patient’s” health anyway. I didn’t realise what a toll it was taking on me until after he died.
In later years, I found that the part of my role which included keeping records of changes in medication, which doctor advised what, contacting the various health professionals and negotiating NHS systems, became increasingly important – and towards the end, essential. Fortunately, I was never in the position of having to make an end-of-life decision for him. He was able to make the decision himself – and made the decision himself. He was always very practical and philosophical about life, there was no great drama and certainly no brave warrior heroics about it all, he’d reached the end and just wanted to go. At no point did any of the health professionals show anything but the greatest respect for his decision; the emphasis was always on carrying out his wishes and making him as comfortable as possible.
We never really managed to talk about the fact that his decision to bring his life to an end was also bringing our 45-year marriage to an end. I didn’t feel I could broach the subject in case he thought I wasn’t supporting him in his decision, which I absolutely was. Another example of how conflicted life can be for a partner, the “But-what-aboutme-followed-by-guilt” syndrome.
The last time I saw him wasn’t a happy occasion. Uncharacteristically grumpy, he wasn’t pleased to see me, all his systems, including hearing and bowels, were packing in. He didn’t want to see anyone, he just wanted to go to sleep and not wake up. Fortunately that was what happened just a few hours later. The nurse starting her evening shift looked in to see him and found that he’d died in his sleep.




These should ideally be had at a time when they’re not an issue. Easy to put off, but necessary. It’s important to talk about:
• Making a will, making your wishes clear
• Power of attorney
• Funeral preferences
• The circumstances under which you would want to stop dialysis
• What your wishes are about 'Do Not Resuscitate'. It can feel a bit negative to agree to DNR – as if you’re giving up – but resuscitation can be a brutal process, involving broken ribs and trauma. Agreeing to DNR gives medical staff clear direction.
You may be contacted soon after your partner has died by:
• Organ and Tissue Donation Service
• A Medical Examination Officer
This is a comparatively new service, set up after the Shipman inquiry to conduct independent scrutiny of deaths not investigated by the coroner. The MEO checks all the clinical notes and talks to the bereaved before issuing a Medical Certificate of the Cause of Death, which then goes to the Registrar so that the death certificate can then be issued. At first this feels like an unwelcome extra layer of bureaucracy but may be useful if you have any questions about what happened around the death.
If you’ve dialysed at home, the home renal team will arrange for the machine(s) you have to be removed and if necessary, any plumbing restored. They will also arrange for your supplier to come and take away any unopened boxes of medical supplies. Any opened boxes will be yours to dispose of. And they will adjust/cancel any payments made to you by way of contribution to electricity and/or water bills.
After the patient dies, that appears to be it as far as NHS systems are concerned.
But of course NHS systems are operated by people –and some incredibly kind and thoughtful individuals I particularly appreciated:
• Lovely messages from the Kidney Choices team we’d got to know over the years.
• The renal sister who carried out our initial Home Hamodialysis training, who had moved on to another hospital but who took the time to phone and have a chat.
• The anemia sister who was warm and supportive on a chance encounter in the hospital
• Our GP, who absolutely amazed me by phoning after Roger died with condolences and to ask how I was
• And (best of all) the renal technician who came to disconnect the RO and the dialysis machine, despite – or maybe because – he’d had a lot to bear himself. We talked and laughed about Roger’s time on dialysis, talked about the funeral, talked about all the admin. He reassured me that it was all going to take time and gave me a hug. Better than any bereavement counsellor.
Carers are used to mixed emotions. For me, the sadness that illness and his kidney condition robbed Roger of the retirement he should have had is tempered by thankfulness that dialysis gave us nine years we would otherwise not have had. Without dialysis he would never have met his five grandchildren. Being able to dialyse at home was overall hugely beneficial, it gave him focus, control and independence.

At some point in our lives, we all have to face the loss of a loved one, and it’s never easy. During such an emotional time, managing life’s responsibilities and putting affairs in order can feel overwhelming and stressful.
The NKF has developed an online guide to help you through this difficult process. This resource aims to help you understand what needs to be done and highlights the support that’s available during challenging times.
All the information provided below can be found on our website with links to click through to more information: www.kidney.org.uk/bereavement
Pronouncing the Death
If someone dies at home in the UK, you can call NHS 111 to arrange a healthcare professional to visit and confirm the death. If the death was unexpected, you should call 999
Register the Death
• Register the death within 5 days
• The death has been reported to a coroner
• The death happened outside the UK
• You're registering a stillbirth
• Someone is missing and you think they're dead
Tell the Government About the Death
The ‘Tell Us Once’ service allows you to inform the death to multiple government organisations at once. If you cannot use ‘Tell Us Once’, you will need to tell the government yourself.
Create a list of immediate family and close friends to inform about the death, using phone calls or messages for personal notifications.
Contact the deceased’s employer to notify them of the death and inquire about any outstanding money owed or life insurance benefits.
Check if the deceased made any arrangements for after their death, such as pre-paid funeral plans or specific wishes documented.

Locate important documents such as wills, trusts, and other end-of-life planning paperwork that may guide further actions.
• Estimate the value of the estate to find out if you need to pay Inheritance Tax
• Find out how to report the value of the estate
• Pay Inheritance Tax if it’s due
Discuss with family members memorial service preferences and make necessary arrangements based on what the deceased would have wanted. The website provides information regarding:
• Arranging the funeral
• Getting help to pay for a funeral, and
• Where to get help to pay for a child's funeral
You may want to collect donations for your chosen charity during the funeral in memory of your loved one. Giving a gift in memory of someone can be a special way to honour a loved one while providing hope to people living with kidney disease. To organise a collection in memory, call the NKF office on 01909 544999 or email nkf@kidney.org.uk with your chosen address, we can provide collection envelopes to share with family and friends.
Ensure that the deceased’s home and valuables are secure while decisions are being made regarding their estate. You may will also need to
• Check if you need to apply for probate
• Apply for probate
• Deal with the estate
• Update property records
You may be entitled to bereavement benefits:
• If your partner has died
• Statutory Parental Bereavement Pay and Leave if your child has died or you’ve had a stillbirth
• Guardian's Allowance if you're bringing up a child whose parents have died
Dealing with your Own Benefits, Pension and Taxes
Information on our online bereavement page includes how to manage your tax, pensions and benefits if your partner has died and how to check how benefits are affected if a child dies.
Leave from work
You may be entitled to some bereavement leave if you are employed when one a loved one dies. In many circumstances, there is currently no set legal amount of leave. It can really help to know your rights, how the system works and what the rules are around pay. This will be dependent on your employer’s policy.
Check if you need to apply to stay in the UK
If you have the right to live in the UK depending on your relationship with someone who died, you might need to apply for a new visa in the following circumstances:
• You're in the UK as the partner of a British Citizen or someone with indefinite leave to remain
• Your partner who died served as a member of HM Forces
• You can contact UKVI to check the rules for other visas

Many organisations can help and support you through bereavement, there are many links on the NKF website and include:

• NHS advice on dealing with bereavement, grief and loss
• Cruse Bereavement Support
• National Bereavement Service
• The Good Grief Trust
Many other links included are to organisations who can help you speak with someone about bereavement. These include the Marie Curie Helpline and AtaLoss among others.
Set up mail forwarding to prevent overflowing mailboxes and check emails for important information regarding accounts and bills.
Bereavement can lead to a wide range of emotions including sadness, confusion, guilt, and even relief. Each person’s experience is unique and influenced by factors such as the relationship with the deceased and their own personal ways of coping.
When a loved one dies, coping can be challenging. Accept your emotions, allowing yourself to grieve without judgement. Talk about your feelings with trusted friends. Preserve memories by creating a memory box or by engaging in activities that remind you of them.
These feelings may not be constant, and strong emotions can come on suddenly and unexpectedly. It can sometimes be difficult to recognise that grief or loss is the root cause of behavioural or emotional changes.
Lastly, take the support you need from family, friends, or professionals to help navigate this difficult time. Remember, healing takes time and it’s okay to seek help.
For further support visit: www.kidney.org.uk/ bereavement
Why not give our autumn themed spot the difference a try. Spot the ten variations between these two images.



a recipe on p90 from TASTE!
A friend gave me a big bag of cooking apples from her tree so I used them in this recipe instead of the tinned cooked apples. My version may not look like the one in the book, but it was absolutely delicious! It’s more like a torte in texture than a sponge cake and is very moist. We ate it warm and cold and with a little cream. The cinnamon hit is great. Enjoy! Ed
110g caster sugar
110g softened butter
1 egg
1 x 397g tin cooked apples, drained
1 tbsp ground cinnamon
3 tbsp soft light brown sugar
170g self-raising flour
150ml semi skimmed milk
1. Preheat 180°C, fan 160°C, gas mark 4. Grease a 20cm round cake tin then line the base with parchment paper.
2. Tip the butter and sugar into a large bowl and beat until light and fluffy, then beat the egg in.
3. Tip the cooked apples into a separate bowl, then stir in the ground cinnamon and 1 tbsp soft light brown sugar.
4. Fold the apples into the butter mixture then fold in the flour and mix until combined.
5. Pour in the milk and mix to a soft batter.

Ready in 75 mins
Serves 12
6. Pour into the prepared tin and bake in the oven for 40 minutes until golden brown and risen. Gently open the oven and pull the cake out on the oven shelf then scatter the remaining 2 tbsp soft light brown sugar over the top – you want it to just melt slightly, so shut the oven and cook for another 10-15 minutes until the cake is cooked.
7. To check the cake is cooked through, insert a skewer in the centre of the cake – if it comes out clean, the cake is cooked, if not return to the oven for 5 minutes and check again.
8. Allow to cool for at least 1 hour in the tin before decanting and serving in slices.


This year’s Christmas raffle is all about winning cash! There’s a top prize of £1,500 and four other cash prizes which lucky winners can spend however they like. You could use the cash for Christmas presents, a holiday, pay some bills or treat the family to something nice, if you are a winner it will be a nice position to be in. If you would like to purchase our raffle tickets online please visit: www.kidney.org.uk/shop/nkf-christmas-draw2024
It's not too late to buy your Christmas cards and support the NKF at the same time. We have a fantastic selection with prices starting at just £2.50 for a pack of ten, we also have gift wrap and money wallets – please visit:
www.kidney.org.uk/ shop

Here at the NKF we have so many fundraising events to offer next year from running, skydiving, treks and more – it’s going to be a busy year and we would love you to be part of it. Please go and have a look at www.kidney.org.uk/Pages/Events and if anything interests you or you have a question please call Pete on 01263 722287 or email pete@kidney.org.uk


Combine top quality dialysis treatment with amazing holidays, on the island
Dialysis Centre is a state-of-the-art dialysis unit, located within the Euromedica General Clinic of Rhodes, in Greece, that complies with European standards of health and safety while providing quality dialysis services in a modern setting.
The centre is located just 10 minutes from Rhodes town, 4Km from the resort of Kallithea and 9Km from the popular resort of Faliraki.


Contact Us: info@euromedica-rhodes.gr / int@euromedica-rhodes.gr
T. +30 22410 45000 / 45280 / 45222
euromedica-rhodes.gr

ad_Euromedica_MTN-uk_267x180_131023.indd 1
We accept the European Health Insurance Card (EHIC)

