






















Welcome to this issue of Kidney Life, packed with an interesting mix of people’s experiences, new developments and opportunities to get involved.
We welcome Jessica Jones the NKF’s newest recruit as Policy & Public Affairs Manager. You can learn about her work and personal experience and read a couple of articles from her too.
We have two more inspiring patient stories for you, both of which feature transplantation. We’ve also built on our article in the last issue about the variation in waiting times for transplantation, with an article on the work of the Organ Utilisation Group (of which Jessica is a member) which I hope you find interesting. The next issue of Kidney Life will feature transplantation from the perspective of donor relatives and live donation. Your feedback on these articles is very welcome.
I would like to publish more stories focussed on living with kidney disease without a transplant. If you’d like to share your experiences please do get in touch, I can help with writing your story or you can just send it to me.
The results of this year’s Best Foot Forward fundraising activity has raised a staggering £20,000 in support of the NKF’s work. Well done to everyone who took part. I’m suffering a bit of FOMO – I will definitely join in next year – you can hold me to that!
Look out for connections between articles with topics ranging from improvement work, policy and individuals’ experiences. Together these demonstrate the influence, effectiveness and importance of the NKF’s work.
Best wishes
Annie Taylor Editor
PS – You will find three books of Chrismas Draw Tickets enclosed in this edition of Kidney Life, if you need more or have not received any tickets and would like some, please contact the NKF office on 01909 544999 and we will pop some in the post.
NKF OFFICERS
Chairman – David Coyle
Co Vice Chair – Caryl Bryant
Co Vice Chair – Tarsem Paul
Treasurer – Mike Sinfield
Secretary – Brian Child
NKF TEAM
Andrea Brown – Chief Executive
Pete Revell – Head of Marketing & Fundraising
Donna Blizard – Office Manager
Jessica Jones – Policy & Public Affairs Manager
Sharney Warren – Communications and Marketing Officer
Fiona Broomhead – Senior Office Administrator
Chloe Ainsworth – Social Media and Website Coordinator
Heather Mooney – Accounts Administrator
Chris Talbot – Membership Development Lead
Linda Pickering – Helpline Advisor
Stephen Emmerson – Helpline Advisor and Peer
Support Coordinator
When Friday 25th and Saturday 26th October 2024
Starting on Friday with a social evening and great food (a pie and pea supper!) and an entertaining quiz along with the chance to meet up with friends old and new. Saturday is a full day of learning, sharing and making connections. The full programme is just being finalised and can be seen at www.kidney.org.uk
Saturday evening will include a three course dinner with entertainment to bring the day to a close.
The NKF’s Annual Patients’ Event is a fantastic opportunity to learn, share, network and enjoy time with like-minded supportive people who understand what it means to live with kidney disease. A remarkable event, not to be missed.
Sessions this year include
• how peer support can help home therapies
• personal experiences of living with kidney disease
• symptoms in advanced kidney disease, dialysis and transplant medications
• exercise
• the importance of patients’ voices
• an update from NHS Blood & Transplant
Who
The Annual Patient Event is designed specifically for people living with kidney disease and their family members and carers. The NKF team will also be there with a host of guest speakers, including healthcare professionals who will deliver educational and informative sessions throughout the day.
Partners from industry and event sponsors will also be present.
The Patients’ Event is the only time in the year when we get everyone together. There’s chance to chat, share, learn, have fun, make new friends and increase your understanding or share your experience of living with kidney disease.
Turn to the back page of this issue where you’ll find a booking form to complete or go to kidney.org.uk or phone 01909 544999
Radisson Blu Hotel, East Midlands Airport, Herald Way, Pegasus Business Park, Derby, DE74 2TZ
Be prepared for insightful and educational sessions at this event designed for kidney patients, families, carers and healthcare professionals.
Registration is now open, and we encourage you to secure your spot early to ensure you don't miss out on this great event!
Forfulldetailsvisitourwebsite: www.kidney.org.uk/Event/ national-kidney-federationannual-patients-event-2024

Friday 25th and Saturday 26th October
Radisson Blu Hotel – East Midlands Airport


Jessica joins us as the NKF’s new Policy and Public Affairs Manager at a time when the broader political landscape is undergoing significant changes.
Jessica has over 15 years’ experience in health policy - in areas including welfare, access to new medicines, clinical commissioning and transplantation. Jessica has also been heavily involved in the Organ Utilisation Group (OUG), which was established by the Secretary of State for Health and Social Care in England to make recommendations on how to maximise the potential for organ transplantation from living and deceased donors.
Through this work Jessica helped ensure patients were kept at the heart of the programme and was keen to ensure those with ‘less heard voices’ were actively sought out as part of the patient engagement process. Many of the recommendations of the OUG report chime with the ongoing focuses of the NKF, with concerns around inequity, patient information and communication, and the need for services to take note of patient feedback in order to improve. Jessica has contributed to our article on the work of the OUG and her ongoing role on page 7.
Jessica has personal experience of life with a serious health condition and a high burden of treatment and intends to bring that insight to policy development with
the NKF. She is particularly interested in the challenges of younger people with kidney disease, and the difficulties of being in a vastly different place to your peers.
Learning of the rigid and demanding regime those in need of dialysis face Jessica said, “It is vitally important that the quality as well as quantity of someone’s life is taken into account, and NKF’s campaign to increase opportunities for home dialysis does just this. Current inequity in provision - apparent across geographic, ethnic and socioeconomic differences must be tackled to give everyone the best chance of living a fulfilling life. Top of my agenda is making sure the parliamentarians I will be working to develop relationships with, across all four nations, understand the realities faced by those with kidney disease.”
In her new role Jessica is excited to apply her previous knowledge in the areas of welfare, transplant and patient engagement, and expand her understanding of the vital role prevention can have in reducing the number of people who need dialysis and transplantation.

Jessica Jones, Policy & Public Affairs Manager for the NKF explains how you can influence membership of the APPKG with a simple call to action.
The All Party Parliamentary Kidney Group (APPKG), for whom the National Kidney Federation is the Secretariat, is keen to work with MPs from across the chamber and always invites new Members to get involved.
It is important your elected representative understands your experience of kidney disease, the effect it has on your life and the care you receive.
If you are keen for your MP to get involved with the APPKG and help raise the profile of kidney disease and transplantation in Parliament, please feel free to use the letter template on the NKF’s website at https://www.kidney.org.uk/allparty-parliamentary-group and contact them via their

parliamentary email address or send it as a letter. It is helpful if you personalise the template with your own experience, as your MP is more likely to take notice.
Please make sure to include your address on any correspondence, as MPs can only respond to people in their own constituency.
If you aren’t sure who your MP is you can find out here https://members.parliament.uk/members/commons
Please do let us know if your MP offers to support the APPKG, by emailing jessica@kidney.org.uk

Here’s how the new Bradford KPA was set up recently by Sofia Tsanou
My mum, Michaela and I attended our first NKF Patients’ Event in the East Midlands in September 2023, and this is where we learned that Bradford did not have a Kidney Patient Association, and so we thought we’d better put that right!
I spent four months in hospital last year, and as you can imagine things didn't always go to plan and I felt inspired to try and do something that may help others have a better patient experience. So when the opportunity came along to start our own KPA here in Bradford it was like it was meant to be, and I jumped at the chance.
There was a lot of form filling and creating lots of official documents, which was quite time consuming but we got there in the end. Mike May from the NKF was very helpful and we had a couple of online meetings with him.
Once we had established our governing body document, we then set about registering our KPA with the Charities Commission. Once we were granted charity status, we then opened a business bank account, which again was a little time consuming but we felt this was important. We also registered our account with HMRC.
While all this was going on, we also needed to apply for Enhanced DBS (Disclosure and Barring Service) checks for Adult Workforce to register our trustees and volunteers, as we will be working with vulnerable adults.
To be honest, it was fairly difficult finding out what we needed and how to do this. Fiona Broomhead at NKF helped out by forwarding details of a charity in Bradford that might be able to help with this.
After a phone conversation, I was referred to a lovely lady from another company, Action Point in Keighley who acted as an umbrella body, and so with her help, we were able to submit DBS forms. This is ongoing as and when we recruit more volunteers.
We also needed some guidance on producing a 'Safeguarding Policy', and again Fiona at NKF was helpful in forwarding NKF's own policy, and another one from an already established KPA. We've also produced an 'Ex Offender's Policy' and a 'Grant Making Policy'.
We've organised two events so far, both for World Kidney Day, one at Bradford Royal Infirmary (BRI) and one in the dialysis unit at St Luke’s. This was a great opportunity to share awareness about CKD, and also let people know who we are and what we are about.
We had 'guess the number of sweets in the jar' competition at BRI, as a way to engage with people and get them talking to us, and we also gave away bottles of water, sweets, and items
that had been sent by both the NKF and Kidney Care UK. At St Luke's we had a free raffle for patients and staff and again gave away goodies, similar to BRI with the addition of some 'posh' biscuits for patients to enjoy with a cup of tea!
In April we attended the NKF’s KPA weekend in Birmingham. We found this really useful and connected with people at other KPAs, who were all really welcoming. The NKF also funded us to attend, as we are so new and haven't built up any real funds yet - but we're working on that! We had a lovely message of support from Linda Pickering on the helpline at NKF.
Our goals for the year are to keep fundraising, hopefully take the patients for a day out to the coast, and purchase things needed to help give our patients a better experience, oh, and to attend the patient event again in the East Midlands in October, which is where it all started for us.
We're currently holding a raffle to generate some funds, and we've had lots of prizes donated.
So to summarise... here’s a few top tips to help set up a new KPA:
• Speak to someone who is involved in an existing KPA and get their help
• Create a Governing Body Document/ Constitution
• Register with Charities Commission if you want your KPA to have charitable status
• Open a business/ treasurer's bank account
• Register your account with HMRC for Gift Aid
• Ask the team at the NKF for help and guidance
• Apply to an umbrella body to get your enhanced DBS checks done.
Sofia & Michaela on their stand at Bradford RI promoting World Kidney Day

In the second of our features on transplantation we look at the work of the Department of Health and Social Care’s Organ Utilisation Group (OUG) which was set up to the review and improve the number of organs that are accepted and successfully transplanted, and to drive improvements to the transplantation service, to ensure equity of access and patient outcomes. Ongoing work is being delivered by the Implementation Steering Group for Organ Utilisation (ISOU). Kirit Modi MBE and the NKF’s Honorary President represents the NKF on both of these groups.
Deceased organ donation numbers have increased by 95% since 2008, driven in part by the opt-out legislation and though there had also been improvements in the transplant rate, these had not kept pace with donation. Increasing age and co-morbidity of both donors and patients were making successful organ utilisation challenging. The Covid-19 pandemic had also impacted on the waiting list. Whilst the first wave saw fast-tracked improvements to the transplantation service, the reduction in donors and temporary closure of units led to a five-year high of people on the transplant waiting list
Chaired by Sir Stephen Powis, Medical Director of NHS England, the OUG completed its review publishing a report 'Honouring the gift of donation: utilising organs for transplant' in February 2023.
In the introduction to the OUG report, Sir Stephen Powis states “The task of the review was to improve the number of organs that are accepted and successfully transplanted and drive improvements to the transplantation service, to ensure equity of access and patient outcomes. Organ donation is a precious gift of life. If our systems of donation and allocation are now optimised to ensure that an organ goes to exactly the right recipient - the most appropriate person to receive that precious gift - then it is incumbent upon us to do everything we can to ensure this happens in a timely manner. To do otherwise is to break the contract of trust we have with our donors and patients. It cannot be right that the certainty with which this happens varies from unit to unit, from one part of the country to another, or between patients. This disparity of service provision is the core issue that the report aims to resolve.”
Our thanks to the contributors of this article who have given their time to share the latest information on their work.

ISOU, ICE, ARC – what do all these letters mean?! by Professor John Forsythe, Senior Clinical Co-Chair of ISOU in the Department of Health and Social Care, Transplant Honorary Professor Edinburgh University. In the last few years I have been involved, not only in trying to promote organ donation but also working with many others to improve organ utilisation. First, what does organ utilisation mean? There is no accepted definition but for me it means making the best possible use of every precious donated organ where it is safe to do so.
The OUG’s report made 12 wide-ranging recommendations to the Implementation Steering group for Organ Utilisation (ISOU) which I am privileged to Co-chair along with a senior civil servant. The ISOU comprises representatives from the lead organisations with a role in implementation of the recommendations - NHS Blood and Transplant, NHS England, the British Transplantation Society, relevant professional societies and patient and lay representatives.
Together, we have set about taking the 12 OUG recommendations and putting them into practise. We established five sub-groups with the focus as listed below.
1. Patient engagement – see Claire Fuller, National Medical Director for Primary Care NHS England and Jessica Jones, Patient Representative and Policy and Public Affairs Manager, NKF section below.
2. Trust engagement
3. Xenotransplantation (transplanting organs from animals to humans)
4. Histocompatibility Innovation (better tissue matching techniques)
5. Organ Assessment and Repair Centres (ARCs)
Much of what happens at a transplant centre is governed by the Trust hospital where that centre is based. The Trust Engagement sub-group, Co-chaired by an expert Clinician and a senior Chief Executive of a major Trust, is working to improve the visibility of transplantation within hospitals and to ensure that the hospitals have the information needed to identify and address any local barriers to offered organs being accepted and transplanted.
Ongoing work will help ensure that commissioning of transplant services is optimised to deliver improvements for both those who provide and rely on transplant services, make the best use of available funding and help address inequalities.
Advances in science, often led from Britain, may be harnessed in the field of transplantation before their use in other aspects of healthcare. Xenotransplantation science – transplanting organs from animals (usually pigs) into humans – has seen rapid expansion in the past two years. You may have read about some of the pioneering procedures in the media. The Xenotransplantation subgroup is examining the field carefully. They will take into account public opinion and make recommendations on how this science may impact transplantation in this country in the future.
There have also been advances in DNA technology, which means that tissue typing may be even more fine-tuned and tests may be able to be performed more rapidly in the future. This is likely to have an impact on transplantation, particularly in kidney and heart procedures. The Histocompatibility Innovation sub-group is looking at these techniques and advising how they might best be used to improve patient outcomes.
Finally, there is a revolution in the preservation and perfusion of organs outside the body, when they do not have a blood supply. Some of this technology is already in use in the UK and we need to see how quickly we can utilise these new techniques to increase the number of organs which can safely be transplanted or perhaps improve the function of the organ after transplant either in the short or long term. The ARC sub-group brings together experts to identify how these new machine perfusion technologies can be built in to standard practice in the UK.
I hope that this brief summary gives you some information about the many activities that we are undertaking to make the OUG vision a reality. We remain incredibly grateful for patient engagement in all this activity, whether on an individual basis or from patient representatives such as those from the NKF.
by Dr Claire Fuller, National Medical Director for Primary Care NHS England and Jessica Jones, Patient Representative and Policy and Public Affairs Manager, NKF
There were two recommendations in the OUG report which were prioritised for focus - the first relates to ensuring there is equity of support and provision across patient groups; and the second that transplant services must be run in reference to patient feedback. ISOU is tasked with ensuring these recommendations are implemented, and the Patient Engagement sub-group ensures they are done in a way that keeps patients at the heart of the service, listens to their feedback and concerns, and involves patients in the development of more successful, sustainable transplant services.
The group is chaired jointly by lung patient, Jessica Jones, and the Director of Primary Care for NHS England, Dr Claire Fuller. The Group’s members bring many years of experience as transplant patients, experts in patient involvement and represent a diverse cross-section of our patient community. Our task is to extract examples of best practice from across transplant centres, and work with the other ISOU sub-groups to ensure these are ambitious yet can realistically be put in place to improve patient experience on the ground.
Alongside site visits to transplant centres, planned by the Group over the summer, a wider Patient Engagement Best Practice Group has been established. Many of you, representing transplant-adjacent KPAs, joined us for the inaugural meeting where we heard about the overall ISOU strategy, how patient experience is measured and had the opportunity to discuss examples of positive patient engagement, raise issues of concern from across communities represented and give insight as to where a service could benefit from increased patient input.
Our ultimate focus is to make sure that all patients, whatever their circumstances, get the care they need, feel truly informed about their options and treatment, and have a voice within the development of their transplant service- which is valued and listened to. We are committed to patients seeing the impact of their input, and value the contribution of anyone who has been generous enough to share their thoughts so far. Quality, as well as quantity of life is important, and this is a message we hear loud and clear.
In the next issue of Kidney Life we consider transplantation from the perspective of the donor’s family and how the UK Kidney Offering Scheme works, looking at the variation in acceptance and decline of organs for transplant with NHS Blood & Transplant
This year I’m celebrating 20 years since my kidney and pancreas transplant. Twenty years! I haven’t ever experienced rejection or had any other really troublesome concerns. For that, I have been blessed. But what people don’t realise is how much having a chronic condition and a transplant, shapes your perception of the world.
My health has always been something that I have consciously been aware of. I contracted Haemolytic Uraemic Syndrome through an E-coli bacteria aged 12 months. I was very poorly and spent some time in the intensive care unit at the Royal Manchester Children’s Hospital. I regained 22% renal function and my parents were told that I would likely need a kidney transplant in the future. As a child I was unaware of this as my parents were protecting me and possibly hoping the doctors were wrong.
Children create their own ways of understanding what is happening to them. For instance, I once fell asleep in our living room in front of the fire and woke up in hospital.
Apparently, I’d had a seizure because I was so unwell. I imagined it to mean I was magical and could transport myself to places. I didn’t ever share this

with my family or medical team, believing that to do so would mean losing my powers.
Reflecting on it now, I can see how the little me was trying to survive. How leaving school mid-way through classes to have blood tests meant that I was important. How I translated chronic headaches to mean someone was trying to communicate with me from another dimension. Of course, the reality was that my pancreas was unable to cope with the hormone changes of a pre-pubescent body.
I was diagnosed with type one diabetes within the first few months of starting secondary school. My kidney function was sliding face-down off a cliff. My imagination took me to a magical world. It saved me and allowed me to cope as a young child with all the strangeness.
My kidneys were struggling going into adolescence. Again, I wasn’t exactly aware of what was happening to me but the most obvious indicator that things were afoot was that my mum began smuggling calcium carbonate tablets onto my sandwiches in my packed lunch. I don’t think she realised they were orange flavoured. Or maybe she did and was trying to make an exotic eater out of her tween child in a lunch of feta and spinach sandwiches, with a hint of orange. Either way, dietary changes and steady increases on the prescription list, plus more hospital appointments, were telling me that things were not okay and were changing.
I went into renal failure at 13, needing haemodialysis three times a week. I had a fistula in my wrist and a central line inserted under my collar bone. It impacted my schooling; revising for your GCSE’s whilst dialysing or having a plastic wire coming out of your skin, dangling just over your boob, is not the fun rite of passage people envisage when they think of their teenage years. So when Dr Plant, my paediatric consultant, broached the topic of having the double transplant a year later I didn’t hesitate.
14 year old Jess on dialysis. Celebrity Keith Duffy visited. We didn’t ever get the best celebrities because our ward was way at the back of the hospital.



I never discovered who my donor was. My mum wrote a thank you letter a few times, but we didn’t receive a response. I accept that.
He discussed the high risks as it hadn’t been done in the UK before. My thinking was that if I was going to go for one then why not try for both? I think my parents had their own reservations, knowing all the facts and risks!
My parents agreed and I was on the waiting list for around 9 months. The night before we received ‘The Call’, I’d had a fit while my mum was driving us home after dialysis. I had just turned fifteen and I remember not being able to control my arms which were bouncing up and down as if I was dancing to music. My mum did a U-turn in the middle of the road and zoomed us straight back to Pendlebury Hospital. I hadn’t ever responded well to dialysis so receiving ‘The Call’ the next morning felt like all our prayers had finally been answered.
I don’t have a vivid memory of my transplant, only two stand out tableaus. The first was watching Manchester Utd in the cup final on a TV, on a stand with wheels on. I was in a small side-room with sealed windows in May. It was hot, and the hospital was ancient. The second thing I remember was waking up to two tubs of Haagen-Dazs ice cream that I had made Dr Plant promise to buy for me because –I loved the stuff but hadn’t been able to have it since becoming diabetic - as I was having two transplants only two tubs of ice-cream would suffice – and because I was the absolute epitome of a cheeky fifteen year old! Oh, to be fifteen again!
I was in hospital for three weeks and three days. I never discovered who my donor was. My mum wrote a thank you letter a few times, but we didn’t receive a response. I accept that. The flip side of my absolute joy was the devastating loss for them, but I always think of them and send my gratitude outwards, vocally or inwardly. I wouldn’t be where I am now without them.
I’m 35 now. I’ve had kidney infections over the years, many UTIs, I’ve needed a reflux procedure and developed other health concerns which are indirectly due to the transplant. But really, I have been so incredibly lucky and I’m so grateful that I have the chance to experience any sort of life. A doctor once told me that kidney transplants last a maximum 20 years. I’ve read dozens of stories which refute this, including my own! However, being told this when I was young only inspired me. Upon reaching that milestone this year I threw a massive party to celebrate everyone who had helped me along this epic path: medical teams, family and friends.
And although I’m not actually gifted with any magical powers, this whole experience has been incredible, and that’s magical enough. Here’s to the next 20 years, and beyond!
Fouryears agothe NKFbegan a national campaignto encouragethetake-up ofhome dialysis recognisingthe significant impact on an individual’swellbeing. Here’s an update.
Homedialysishaslongbeenknowntodeliverabetter qualityoflifeforpatientsneedingtodialyseregularly –givingthemfreedomtochoosewhentheydialyse, fittingitinwithotherimportantaspectsoftheirlivesand reducingrisksofinfectionamongthemanybenefits. Homedialysisalsoallowsforlongerandmorefrequent sessionsthatcanleadtobetteroutcomes,including survivalandquickerrecovery.
TheNKFhasrecentlypublishedthefourthreportwhich disappointingly,showsareductioninthepercentage numberofkidneypatientsdialysingfromhome.A majorpartofthecampaignhasbeenregularcontact withkidneyunitsacrosstheUK.All80unitswereasked toreportthepercentagenumberofpatientsdialysing athomeandtodescribetheirplansforthefuture–in particularhowtheyplantoincreasethenumberand toshareexamplesofgoodpracticethatarehavingan impactonnumbers.Twenty-nineresponsescanbeseen atkidney.org.uk
Whilethekidneyunits’responsesintermsofnumbers weresomewhatdisappointing,theydoshowthatthereis significantenthusiasmfromhospitalstoadvancehome therapiesnationwide.TheNKF,throughthereportis urginghospitaltruststodeveloprobustplanstoimprove homedialysisrates.
NKF Chief Executive, Andrea Brown on the report’s findings said:
“Our Home Dialysis Campaign and annual findings will continue to be shared with hospital trusts until significant improvements are achieved. Not all kidney patients are familiar with why they should consider dialysing at home and how it can help improve their quality of life. The NHS is facing immense pressures, offering the opportunity for patients to undergo treatment at home is advantageous both for the patients and the NHS.”
The NKF’s Peer Support service provides information about home dialysis in the Shared Care Resource Centre web pages. The NKF has also recently announced an agreement with DAYLife – a KQUIP (Kidney Quality Improvement Partnership) programme which aims to increase the number of people dialysing at home by supporting renal teams to make home dialysis the first option for consideration. See more about DAYLife on the next page.
ToreadtheNKF'slatestreport, IncreasingHomeDialysisintheUK–ThreeYearsOn,visitkidney.org.uk or scanthisQRcode. INCREASING



DAYLife is a national programme to promote and understand the uptake of home dialysis therapies. Together, the National Kidney Federation, UK Kidney Association, Fresenius Medical Care, and Kidney Care UK are working with patients and healthcare professionals to help make home dialysis more accessible and support centres in meeting national targets.
Our goals:
• By December 2025, all UK kidney centres will actively work on improving home dialysis therapy
• By December 2027, 20-25% of dialysis patients at each centre will be on home therapy
• Centres already meeting the 20% target will continue to improve each year.
Our approach:
• Learn from the Best: Use existing successful practices to avoid reinventing the wheel
• Collaborate: Bring together experts and patients to create a national movement
• Focus on What Matters: Identify priority areas for improvement with a bottom-up approach
• Tackle Big Challenges: Address issues that affect many patients and need a national effort.
We’ve been working to gather information from patients and healthcare professionals to help shape the project. This involved a number of different activities:
• WorkingGroups:FocusedonSharedCare(https:// shorturl.at/Dja6A),PeerSupport(https://shorturl. at/Ts2JW),PsychosocialSupport(https://shorturl. at/ADFdl),EducationandSharedDecisionMaking (https://shorturl.at/DzELE).We'redevelopingtools andresources,establishingbestpractices, andadvocatingatthenationallevel.
• NationalEvents:Hostingvirtualandin-person events throughouttheyear Checkoutourupcomingevents ontheknowledgehubhere: https:// education.ukkidney.org/course/daylife
Ournext event will focus on Shared Care, 8th October at 11am, to registeryourinterest please registerhere. https://forms.office.com/e/Fk8uMx6Fh1
• EducationandTraining:Providingeducationfor patientsandhealthcareprofessionals.
• KnowledgeHub:Anonlineplatformproviding healthcareprofessionalswitheasyaccesstoawealth ofinformationandresources.Accessithere. https:// education.ukkidney.org/course/daylife
Wewouldlovetohearyourviewsonhomedialysisand thesupportthatisavailabletopatientsintransitioning tohometherapies.Perhapsyoucouldjoinoneofour WorkingGroupsorattendanevent?
Ifyouwouldliketoknowmoreaboutanyofhomedialysis options,youcandiscussthesewithyourkidneyteamor joinasupportgrouptodiscusstheoptionsavailable.
NKFHomeDialysisPeerSupportService: www.kidney.org.uk/peer-support
NKFHomeDialysisPeerSupportServiceLeaflet: www.kidney.org.uk/Handlers/Download. ashx?IDMF=131c1691-3889-48b0bbae-6482f2084615
NKFHomeDialysisResourceCentre: www.kidney.org.uk/Pages/Category/home-dialysis KidneyCareUKSharedCare: https://kidneycareuk.org/shared-care
Wanttoknowmore?TogetinvolvedinDAYLifeortofind outmore,jointhemailinglisthere: https://forms.office.com/r/iKrpTUCZpg email Georgina at kqip@ukkidney.org




Sophie Blane describes the impact of illness on her young life and her hopes for the future.
My name is Sophie Blane, I am currently 30 years old. I was first diagnosed with my kidney condition when I was 18. At the time, I’d just been given a fantastic job at my local council which I’d worked very hard to get. Life was great, I was earning my own money and gaining my independence, four months in to the job I became very unwell, sleeping constantly, vomiting frequently and had swelling in most areas of my body.
Eventually after waking up so swollen I couldn’t open my eyes I went to the doctor who immediately sent me to Watford General Hospital with suspected ‘Nephrotic Syndrome’ or ‘FSGS’ as it’s also known. I was eventually diagnosed with FSGS through a biopsy which confirmed what my doctor had first thought.
I had to quit my job, I was treated with every medication known to reverse the disease, high dose steroids, antirejection (Adaport) and Rituximab. All had horrendous side effects and nothing worked. I became a recluse only leaving the house to attend appointments. After five years and many hospitals stays, during one of which I was given only 24 hours to live after a chest infection began shutting down all my major organs, I went into end stage renal failure.
A short time later, we found out my mother was a near perfect match. After years of being left behind by my peers enjoying their newly found freedom of turning 18, flying to new countries, learning to drive, planning days out, etc. I thought this was it, I was going to get my life back.
On 10th October 2018, we had the operation, the transplant went perfectly and for a short while I was finding myself again, learning who I was as a person and enjoying life. Four years passed and I had just found out that I was pregnant with my third child and I was so happy, but unfortunately I received a call late one evening telling me my creatinine was 780. My normal creatinine was 120. I was rushed to Hammersmith Hospital and after a biopsy and many tests, I was told my kidney had gone into complete rejection and could not be saved. I was to be
fitted a tesio line and was to be put on dialysis as soon as possible and could not keep my baby, as it would almost certainly cause death which, would mean leaving my two daughters without their mother.
As you can imagine the devastation was incredibly difficult, for some reason this time round I felt very morbid, I was certain I wouldn’t make it, and I was terrified of leaving my children and family behind, but I am strong, and I did make it.
After 10 months on dialysis, we found out that my best friend of over 20 years was a match in the paired scheme, so on 4th December 2023 I had my second transplant, this one however did not go so well. I suffered a bleed during surgery and came extremely close to losing my life, it was a very tough recovery, but the kidney began working.
In January I got a call to say the kidney was being rejected again, I felt broken. I have now been on a high dose steroid again for the last few months, they are working so far and I have just had my tesio line removed. Things are looking better.
I couldn’t have got through the last 12 years without my mum’s incredible, unconditional love and support. She held my hand and sat by my side through every appointment, operation and invasive treatment. She helped raise my eldest daughter and saved my life giving me her kidney.
I can see my future again and it’s looking bright. I hope to have many more years with this kidney and to watch my children grow up. My beautiful Marney 7, my sassy Ava 9 and my two quirky step daughters Olivia 12 and Brooke 14. And of course, my fantastic partner of 9 years, Brett.









Zoe Plummer, Senior Project Manager for RaDaR gives us an insight into the service that provides doctors with information about rare kidney diseases which they may only treat once in their career. You can get involved too.
For every 100,000 individuals in the UK, between 60-80 will be living with a rare kidney condition. These people account for more than 25% of patients receiving kidney replacement therapy, that is, treatment to help replace the usual blood-filtering function of the kidneys because the kidneys are not working well. People with rare diseases are 28 times more likely to face kidney failure than those in the general population with chronic kidney disease. They are however less likely to die before needing dialysis or a kidney transplant.
In 2010 the Renal Association and the British Association for Paediatric Nephrology jointly launched the first UK strategy to improve the standard of care for patients with rare kidney diseases and to drive the development of rare disease research in the UK. An essential first step towards understanding and optimizing the management of any rare disease is the collection of informative clinical data. The strategy proposed that a national registry was needed, to bring data together and create an essential resource for healthcare professionals and researchers.
RaDaR’s data is used to:
• Publish clinical guidance/make clinical recommendations

Nearly 15 years on The National Registry of Rare Kidney Diseases (RaDaR) holds data provided by more than 33,000 UK patients and is now the largest collection of rare kidney disease patients in the world!
• Inform Specialised Commissioning (the process by which health and care services are planned, purchased, and monitored)
• Write national letters to improve patient care
• Establish disease specific hubs and specialised centres
• Improve coordination of Multi-Professional Team care
• Identify people suitable for clinical trials and inform potential participants
• Introduce novel and improved therapies
• Identify disease biomarkers and genetic profiles
• Drive change in biological sampling techniques
• Engage with international and/or global research communities
• Lead and/or participate in UK and International trials and studies
There have been many developments in rare disease medicine over the past 15 years, relating to the classification, diagnosis, and treatment of rare kidney diseases. RaDaR will continue to expand and ensure the development of care pathways alongside the provision of high-quality information for both patients and healthcare professionals. In addition, we are excited to be focussing on two new areas over the next five years.
Studying a person’s genes - genomics - can detect and diagnose disease early and tailor healthcare to individuals or groups. The UK is leading the integration of genomics into general healthcare and RaDaR is perfectly placed to support/drive this. We will bring already available genetic diagnoses into RaDaR and will work to sequence the genomes of more RaDaR patients. A collaboration with Genomics England will help us to ensure as much genetic information as possible is made available for research.
Clinical trials are research studies in which people volunteer to help find answers to specific health questions. £10m of funding has been invested to set up a new rare kidney disease research centre and RaDaR will be a major collaborator. As part of this, several research nurses will be improving the data held by RaDaR. Having higher quality data will allow us to support clinical trials and identify areas where new treatments are needed. Though this initiative will focus on rare kidney diseases in children first, adult trials will follow as well as work on the more common kidney diseases.
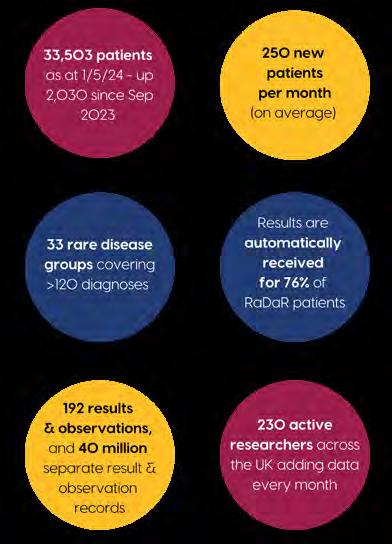

RaDaR simply could not function without the support of patients, and we are committed to empowering them and their families to have a voice, be heard by those with the power to change policy and practice and to provide the data needed to make tangible, positive changes to their care. To achieve this, we invite patients or their parents/ guardians to participate in all aspects of RaDaR’s oversight and development, assist the production of educational material, advise healthcare professionals leading our rare disease groups, participate in clinical trials and research surveys and share their lived experiences. All patients within the RaDaR community receive a newsletter twice a year describing how their data is being used, the results of studies and any new findings, events, and plans. The RaDaR website provides useful information for both healthcare professionals and patients and is open access.
If you are a patient with a rare kidney disease and you are interested in joining RaDaR or would simply like to know more, please contact your kidney centre. Alternatively visit the website https://ukkidney.org/rare-renal/homepage or email us at radar@ukidney.org.


RaDaR has been developed, maintained, and supported by the UK Kidney Association for over 10 years with over £1m to date invested by the charity. Initial significant grants from Kidney Research UK and Kidney Care UK funded a series of rare disease groups within RaDaR and both charities along with the PKD Charity have provided further funding for project work and annual funding to maintain the registry on the National Institute of Health Research portfolio.
Between 7 and 8 million adults in the UK are prescribed statins. Robert Brown, Senior Specialist Renal Pharmacist at North Bristol NHS Trust has created a new NKF patient information leaflet on statins and their use. Here’s everything you need to know…
What are statins?
Statins are a group of medicines that lower blood cholesterol levels. They work in the liver to reduce the synthesis of blood cholesterols. There are at least five different statin medicines available in the UK. Their drug names always end in 'statin'. The recommended first choice of statin for most people is atorvastatin.
Atorvastatin is taken once daily. Atorvastatin is usually prescribed with directions to be taken at night, but it can be taken at any time of the day. With or without, food or a meal.
What are the benefits of statins?
Statins reduce cholesterol levels in the blood. This contributes to the slowing, and in some people reversing, of the build-up of cholesterol in the blood vessels that pump away from the heart to the rest of the body (the arteries).
Over time (usually a period of years) a build-up of cholesterol in the arteries can narrow and or harden the arteries. This can lead to partial or full blood clots in the arteries and cause cardiovascular events.
What is cardiovascular disease?
Cardiovascular disease is a broad term that includes conditions and events that are associated with the blood vessels that take blood away from the heart (the arteries).
Examples of cardiovascular disease conditions or events are:
• heart attacks (myocardial infarction)
• transient ischaemic attacks (mini stroke)
• strokes (ischaemic stokes)
• poor blood flow in the arteries that take blood to the legs and feet (peripheral vascular disease)
The risk of cardiovascular disease increases with smoking, age, raised blood pressure, raised cholesterol, a family history of cardiovascular disease, and previous cardiovascular disease or events.
There is lots of evidence that Chronic Kidney Disease (CKD) is a risk factor for cardiovascular disease.
What is cholesterol and what are the different types of cholesterol?
Cholesterol is a type of fat found in foods and synthesized in our bodies by the liver. Traditionally laboratory tests
used to measure total blood cholesterol. It is now important to measure the individual components that make up total blood cholesterol.
We now know that it is important to reduce the levels of 'bad' cholesterol and increase the levels of 'good' cholesterol.
Good cholesterol is made up of:
• HDL cholesterol (high-density lipoprotein cholesterol)
Bad cholesterol is made up of:
• LDL cholesterol (low-density lipoprotein cholesterol)
• Triglycerides
Together these are called non-HDL cholesterol.
Adding these three components together gives a person's total cholesterol:
Total cholesterol = LDL cholesterol + triglycerides + HDL cholesterol
Current evidence tells us that it is important to reduce the levels of the bad (non-HDL) cholesterol and increase the levels of good (HDL) cholesterol.

Cholesterol can vary from day to day and can be higher in the time after eating a meal. However, as with many blood tests results, it is trends over time that are useful rather than a single result.
Why would I be prescribed statins?
Statins reduce the risk of cardiovascular disease when taken for a long period of time. For many people statins are a long-term treatment (usually a period of years).




Chronic Kidney Disease (CKD) is a risk factor for cardiovascular disease. National guidelines recommend patients with CKD stages 3a to 5 or those with raised protein in the urine (albuminuria) should be prescribed a statin.
Patients with CKD at earlier stages and those on kidney replacement therapy (including dialysis and kidney transplant) are likely to benefit from being prescribed a statin too.
My cholesterol and blood pressure are perfect; so I'm not sure why doctor is prescribing me statins?
For people with CKD without previous cardiovascular events prescribing a statin regardless of their cholesterol levels will help to reduce the risk of cardiovascular events in the future.
If after 2-3 months, your level of ‘bad’ cholesterol (nonHDL cholesterol) should have reduced by at least 40% from baseline (the level it was at before starting statin treatment). If your level has not reduced your doctor or specialist may increase your statin dose.
In some areas of the country, it may be that the non-HDL cholesterol or LDL cholesterol levels are used as the target to achieve a satisfactory level for reducing the risk of cardiovascular events:
•non-HDLcholesterollessthan2.5mmol/L
•LDLcholesterollessthan1.8mmol/L
Can statins damage my kidneys?
Rhabdomyolysis is a rare side effect of statins where the body’s muscles can become inflamed and damaged. Severe rhabdomyolysis can lead to kidney damage.
Speak to your doctor or pharmacist if you have muscle
pain, tenderness or weakness that can’t be explained – for example, pain that is not caused by physical work. Statins are well tolerated by many people.
What if I can't take a statin?
Sometimes trying a different statin can be helpful. Other options include reducing the dose after temporarily stopping the statin or using an alternative medicine that can be prescribed for patients with CKD too.
Are there any medicines or foods I need to be careful with or avoid if I am taking statins?
Statins can react unpredictably with certain other medicines and herbal remedies (known as 'interacting'), potentially increasing the risk of serious side effects, such as muscle damage.
Medicines that can interact with statins include:
• certain antibiotics and antifungals
• certain HIV medicines
• ciclosporin – a medicine that suppresses the immune system and is used to treat a wide range of conditions, including psoriasis and rheumatoid arthritis
• verapamil and diltiazem – types of medicine called calcium channel blockers, which are used to treat various conditions affecting the heart and blood vessels
• amiodarone – a medicine sometimes used to treat arrhythmia (irregular heartbeats)
• fibrates – medicines that, like statins, help reduce cholesterol levels in the blood
• roxadustat – a type of medicine that can increase the levels of haemoglobin for anaemia in CKD
If you are taking statins and need to take one of these medicines, you may be prescribed an alternative statin or your current statin at a lower dosage. In some cases, they may recommend that you temporarily stop taking your statin. Please speak to your health professional if you have any concerns or questions about your other medicines with statins.
Food and herbal remedies that can interact with some types of statins include:
Grapefruit juice can affect some statins and increase your risk of side effects. You may be advised to avoid it completely or only consume small quantities.
Robert is a kidney specialist pharmacist at Southmead Hospital, North Bristol NHS Trust. Before this he worked as a heart specialist pharmacist for 12 years. Robert has a keen interest in all aspects of kidney medicine and is an active member of the UK Renal Pharmacy Group. On Saturday mornings Robert can be found either running or volunteering at a local park run.
I’m enjoying trying out the recipes in TASTE! So I thought I’d include a foodie theme for this issue’s word search. Good luck!
APPLE STRUDEL
BURGERS
CHICKEN GOUJONS
FRITTATA
ICE CREAM
KEBAB
KOFTE
KORMA
KRISPY CAKE
MEATBALLS
MOUSSE
PANACOTTA
PEACH MELBA
PORK
RANCH SLAW
RISOTTO
ROASTED SALMON
ROSTI
RUM BABAS
SALAD
SA LSA
SHAKSHUKA
THAI GREEN CURRY
I thought this curry might warm us up on one of those chilly July evenings (when we should have been barbecuing) and it didn’t disappoint. Not too hot but plenty tasty, I can recommend this recipe which was quick to create and also quick to disappear! Remember to look for a Thai green curry paste that’s low in salt as your base. Using microwaveable rice means this dish can be ready in under 20 minutes. Ed
160g tender stem broccoli, halved if long
160g fine green beans, halved
160g sugar snap peas
2 carrots, peeled then peeled into thin ribbons
50g vegan Thai green curry paste
200ml reduced fat coconut milk
Method
1. Set a kettle to boil.
160g tinned baby corn, drained and rinsed
160g frozen peas
2 limes, zested and juiced
2 tbsp chopped mint leaves
2 tbsp chopped fresh coriander
500g microwaveable wholegrain rice
2. Place the broccoli, beans and sugar snaps into a saucepan. Add enough cold water to just cover, then bring to the boil. When boiling, simmer for 3 minutes then add the carrot ribbons and simmer for another minute. Drain, discarding the water, and set the vegetables to one side.

Ready in 20 mins
Serves 4
3. Heat a sauté pan or saucepan until medium hot. Add the curry paste and fry for 1 minute until just coloured, then add 500ml of boiling water and the coconut milk and return to the boil.
4. Stir in the tinned baby corn and frozen peas, return to the boil, then stir in the cooked vegetables and mix well.
5. Stir in the lime zest and juice and half the mint and coriander.
6. Meanwhile, heat the rice according to packet instructions.
7. Divide the curry and rice between serving bowls then top with the remaining mint and coriander.










Chocolate is a delightful treat for many, but those affected by kidney disease often have to forgo this simple pleasure due to dietary restrictions.
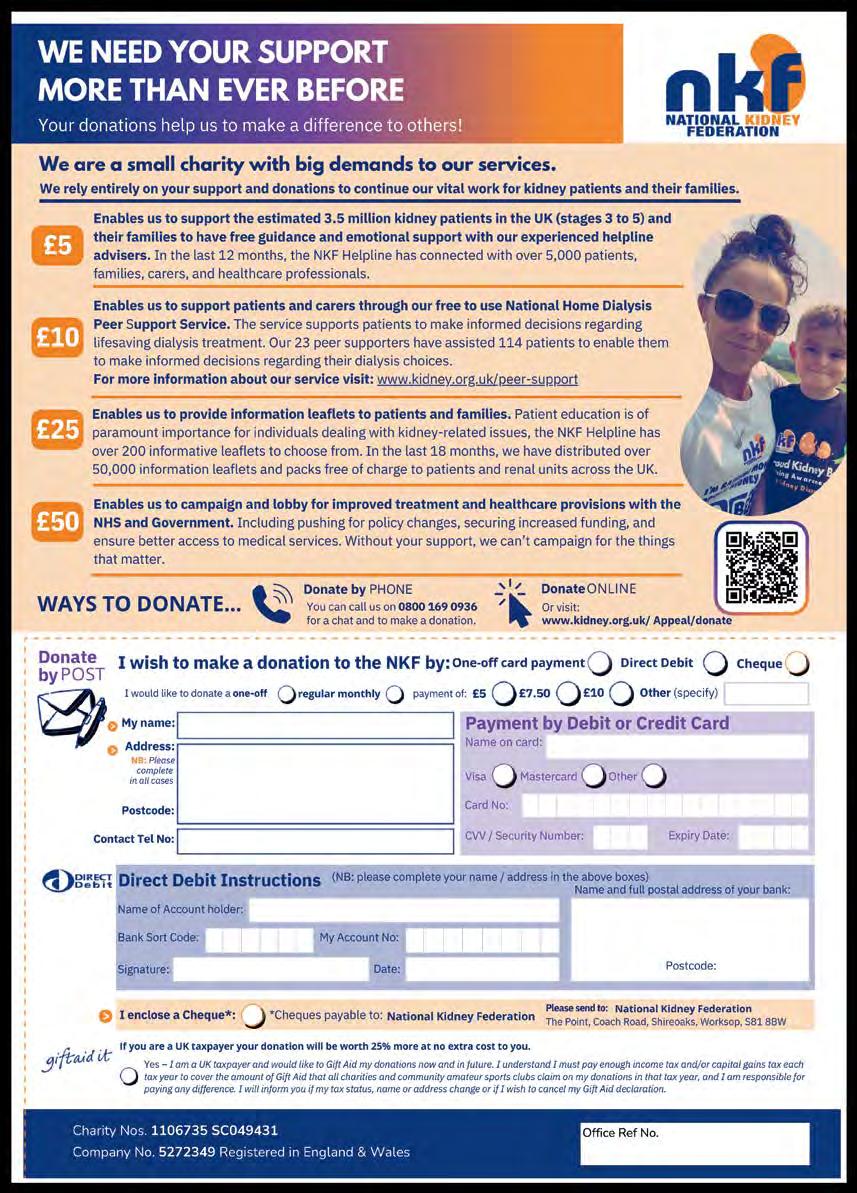
By asking your loved ones to give up chocolate for an entire month, they can show support for the kidney community, raise awareness plus much-needed funds for the National Kidney Federation’s patient support services that are a lifeline to so many.
The Choctober Challenge offers a unique way to step into a family member or friend's shoes affected by kidney disease, even if it is just for a short time.
By encouraging your family members and friends to pledge to give up chocolate for the month of October, you help them demonstrate their commitment to understanding and alleviating the struggles faced by those with kidney disease.
Participating in the Choctober Challenge is simple and rewarding.
Start by asking your friends and family to sign up for the Choctober Challenge on the NKF’s website and spread the word among their social circles.
Throughout the month, they can share their journey on social media using the hashtag #ChoctoberChallenge, inspiring others to take part.
All of our supporters' efforts will not only highlight the importance of kidney health but also contribute to our vital patient support services and campaign work for kidney patients.
So, encourage your loved ones to ditch the chocolate for a month and be heroes for those who need it most.




into the shoes of a loved one with kidney disease and drop the choc this, Choctober. Your participation will not only raise awareness about kidney health but also support our essential patient services and

Your donations help us to make a difference to others!

In this issue of Kidney Life we are stepping into the Christmas spirit with our enclosed Christmas brochure, packed full of festivity! We have Christmas cards, wrapping paper, money wallets and so much more available via our online shop. www.kidney.org.uk/shop












It's not too early, honest, get ready for 2025!
The NKF Calendar is for sale at just £5 and is perfect for writing down all your important appointments and special occasions and each month has a stunning photo reflecting the time of the year.
To get yours while stocks last, please visit www.kidney.org.uk/shop or order over the phone at 01909 544999.
Thanks to industry partners and KPAs for sponsoring each month in the calendar.
This year’s Christmas Draw has a top prize of £1,500 and entry is only £1 for your chance to win big. We also have four other cash prizes up for grabs for you to spend on whatever you desire, use the cash for Christmas, pay some bills or treat the family to something nice. If you would like to purchase our draw tickets at £1 each online visit: www.kidney.org.uk/pages/shop/department/drawtickets


Please select how many tickets you would like and at the checkout make sure you choose free post, we will then allocate your tickets and put them in the draw and email the ticket numbers to you. Or if you’d prefer you can call 01909 544999 to enter.

We are delighted to announce the successful completion of our Best Foot Forward Challenge.
Thanks to the generosity and enthusiasm of our supporters, we have raised to date an amazing £20,000 this year.
Participants were encouraged to complete 70,951 steps throughout the month of June.
Individuals, families, and colleagues came together with a shared goal, to make a positive impact on the lives of kidney patients and show their support for the National Kidney Federation. The funds raised will directly support our helpline services, including the free-to-call Helpline and Home Dialysis Peer Support Service, as well as our ongoing campaign work.
We would like to thank all of our Best Foot Forward fundraisers, reaching this milestone would not have been possible without you. Each step, each pound, and each supportive message means everything to us.
As we celebrate this success, we look forward to building on this momentum for the year ahead. Thank you once again to all our supporters — you have truly made a difference.

Magda

“This challenge is a great excuse for us to get out and about whilst raising vital funds for such a wonderful charity.”
Maz and little Jack


"I have been suffering from chronic kidney disease for the last 24 years and was fortunate enough to have a transplant in 2020. This challenge means a lot to me and the other kidney patients (70,951) in the UK."
Ranji Uthayashanker
Friday 25th and Saturday 26th October Radisson Blu Hotel, East Midlands Airport
STANDARD PRICES
Friday Evening 2-Course Supper Dialysis/Transplant patient* FREE
Friday Evening 2-Course Supper
Friday Bed and Breakfast
Saturday Day Delegate (event only) (includes entry to the event, tea/coffee breaks, full buffet lunch)
Saturday 3-Course Evening Dinner
Saturday Bed and Breakfast
Saturday Special Package (includes Saturday day delegate, plus 3-course evening dinner and Saturday bed and breakfast)
* Please delete as appropriate
1st Delegate Details
Title: First Name(s):
Surname:
Address:
£16.00
Single £89.00
Double/Twin*£99.00
£55.00
£30.00
Single £89.00
Double/Twin*£99.00
Single £140.00
Double/Twin*£190.00
My donation to the work of the NKF £
Total £
Postcode:
Tel: Email:
I am a member of KPA
Special Requirements (subject to availability) please TICK as appropriate
FULLY DISABLED IMMOBILE VEGETARIAN
OTHER (Please state)
2nd Delegate Details
Title: First Name(s):
Surname:
Address:
Tel:
Postcode:
Email:
I am a member of KPA
Special Requirements (subject to availability) please TICK as appropriate
FULLY DISABLED IMMOBILE VEGETARIAN
OTHER (Please state)
Please be advised that photographs may be taken at the event for promotional and documentation purposes. If you do not wish to have your photo taken, please inform a member of the staff or the photographer present. Please send the booking form with a cheque made payable to NKF and return to: NKF, The Point, Coach Road, Shireoaks, Worksop, Notts, S81 8BW. You can also book online at www.kidney.org.uk or by calling 01909 544999.
Any event booking cancellation must be confirmed in writing. The NKF is unable to offer refunds on bookings cancelled after 12th September 2024 and recommends cancellation insurance is purchased.