

FOCUS 2023
CHAIR MESSAGE
Building a Pipeline of Hope

4 8 12 14 18
MILESTONE
Patient Testing Begins for AMD Gene Therapy

RESEARCH
What’s Next in Glaucoma Innovation?

RESEARCH
Life After Death for the Human Eye

RESEARCH & CARE
Utah Lions Eye Bank Celebrates 50th Anniversary

PATIENT CARE
Family’s Eye Cancer Experience Inspires Children’s Book

Official Publication of the John A. Moran Eye Center, University of Utah Health
John A. Moran Eye Center
65 Mario Capecchi Drive
Salt Lake City, Utah 84132
801-581-2352
Co-Editors
Anna Cekola, Communications Editor
Elizabeth Neff, Director, PR, Communications, Marketing
External Relations Team/Contributors
Natalie Lam, Administrative Assistant
Tawnja S. Martin, Development Officer
Mia McCain, Marketing Manager
Brett Prettyman, Corporations and Foundations Development Editor
Heidi G. Reid, Director of Development
Lynn Ward, Executive Director, External Relations
C onsultants
Virginia Rainey, Writer/Editor
Catherine Reese Newton, Copy Editor
Graphic Design
Spatafore Design
Photography
Michael Schoenfeld, Major Portrait Photography
Todd Collins
Austen Diamond
James Gilman, CRA, FOPS
Matthew Hepworth
Kristan Jacobsen
Bryan W. Jones Laboratory
Laura Kinser
Scott Peterson
Cover Illustration
Russ Gray | Design & Illustration
Printing
Sun Print Solutions, West Valley City, Utah
A special thanks to the many hard-working Moran Eye Center employees, management, health care workers, physicians, patients, and researchers who generously contributed their time and talent to make this publication possible.
Research work highlighted in this publication was supported by an Unrestricted Research Grant from Research to Prevent Blindness, New York, New York, to the Department of Ophthalmology & Visual Sciences, University of Utah.
©️2023 John A. Moran Eye Center. All rights reserved. The Moran Eye Center does not assume responsibility for any representation therein, nor the quality or deliverability of the product itself. Reproductions of articles or photographs, in whole or in part, contained herein are prohibited without the publisher’s express written consent, unless otherwise stated.






What’s In Our Pipeline? Hope.

As physicians, we help our patients choose the best therapies, lifestyle changes, or surgeries to help their unique situation.
After all, what works for one person may underperform or not work for another—and now we know more about why. Each day scientists understand more about how genetics influence our risk for developing disease and the severity of the disease.
Over the past decade, it’s become clear a personalized medicine approach tailored to each person’s genetic makeup holds so much promise. Just one gene therapy might stave off a lifetime of struggles with medicines and procedures in the healthcare system.
At the John A. Moran Eye Center, we’re not just talking about it; we’re doing it. Gregory S. Hageman, PhD, is on the cusp of achieving a dream I share with him: defeating age-related macular degeneration.
Our first therapy for this blinding disease, developed by Moran’s Sharon Eccles Steele Center for Translational Medicine (SCTM), is being tested in humans. It will take time to get results, but boy, do we have hope.
Hope is, of course, irrevocably tied to innovation and change.
Visionaries like Dr. Hageman embrace it. He took a chance to study a disease the field had dubbed incurable and embraced the unorthodox as the SCTM developed a new way to speed drug development in academia.
This step for Dr. Hageman and his multidisciplinary team of experts is a testament to their approach.
We have five potential new AMD therapies in our drug pipeline and are beginning to tackle another frustrating, blinding disease: glaucoma.
Our Alan S. Crandall Center for Glaucoma Innovation, led by Iqbal “Ike” K. Ahmed, MD, FRCSC, is doing just that — raising hope. Alan would be so proud to see the impact it is poised to make.
At the forefront is a neuroprotective therapy developed by David Krizaj, PhD, and a team of multidisciplinary collaborators. And Dr. Ahmed continues to push the field forward with research on new surgical devices and approaches.
Have you ever heard of exosomes? They are a hot new research area, and our latest recruit to the Crandall Center, Fiona McDonnell, PhD, is excited to tap into their potential for new therapies and diagnostics.
The excitement doesn’t stop there, of course. In 2022, the Moran Eye Center ranked among the nation’s Top 10 eye centers. It is a remarkable honor that eye doctors around the country recognize the exceptional care we provide.
We could not have done any of this without the kind donors who have supported Moran throughout the years. Some have donated eye tissue upon death to our Utah Lions Eye Bank, which just celebrated its 50th anniversary. Others have lent their financial support to our institution, putting hard-earned money behind our efforts to create a brighter future for patients.

Randall J Olson, MD, and Gregory S. Hageman, PhD, are pictured shortly after they founded the Center for Translational Medicine (now the Sharon Eccles Steele Center for Translational Medicine) in 2009.
This year’s edition of FOCUS shares these stories and more. Many of you know I like to say we swing for the fences. We’ve taken some big swings, and they are heading straight out of the park.
Sincerely,

Randall J Olson, MD
Distinguished Professor and Chair, Department of Ophthalmology and Visual Sciences, University of Utah
The Cumming Presidential Endowed Chair CEO, John A. Moran Eye Center Director, University of Utah Vision Institute
2022-2023
TONI BLOOMBERG
La Jolla, California
WILLIAM “BILL” CHILD
Salt Lake City, Utah
THOMAS “TIM” DEE III
Salt Lake City, Utah
CHRISTENA HUNTSMAN
DURHAM
Salt Lake City, Utah
SPENCER F. ECCLES
Salt Lake City, Utah
CHRISTINE A. FAIRCLOUGH
Salt Lake City, Utah
WAYNE A. IMBRESCIA
John A. Moran Eye Center
CLAUDIA S. LUTTRELL
Salt Lake City, Utah
JOHN A. MORAN
Palm Beach, Florida
RANDALL J OLSON, MD
John A. Moran Eye Center
LYNN WARD
John A. Moran Eye Center
JOHN E. WARNOCK, PhD
Los Altos, California
NORM A. ZABRISKIE, MD
John A. Moran Eye Center
Patient Testing Begins for New AMD Therapy Developed at Moran
Patient testing is underway for a new therapy for agerelated macular degeneration (AMD) developed by the Moran Eye Center’s Sharon Eccles Steele Center for Translational Medicine (SCTM).
The treatment—a gene therapy delivered to the back of the eye—is the first of several precision medicine drugs developed by the SCTM to enter the FDA pipeline. It is tailored for individuals with the most prevalent form of AMD, caused by genetic mutations in the Complement Factor H gene (CFH) on Chromosome 1. The gene therapy delivers a modified version of CFH to the eye.
A Phase 1 clinical trial is assessing the drug’s safety in AMD patients who fit an appropriate genetic profile and have already lost their vision. A Texas woman became the first to receive the drug at a private practice in December 2022.
Physicians will give the therapy to nine patients during the Phase 1 trial. Once confident that the drug is safe, researchers will use larger groups of sighted patients in a Phase 2 trial to evaluate whether the treatment can slow or halt disease progression.
For SCTM Executive Director Gregory S. Hageman, PhD, this moment has been three decades in the making. Driven by a curious nature and inspired by a relative losing her sight to AMD, the then-marine biologist dove into what would become a lifelong passion for understanding—and treating—the disease.
His success could alter the course of history. While AMD is a leading cause of blindness for 1 in 5 Americans over age 70, there is no cure and few available treatments.
“When I decided to work on AMD, we knew practically nothing about its biology or clinical course, and many individuals told me I was wasting my time,” says Hageman. “Now I look back and think, ‘Wow, we’re actually going to give treatment a go.’ I have great confidence in the science, the unique genetic targeting behind our approach, and the SCTM’s extremely talented staff. I really believe this is going to work.”
ANATOMY OF A GENE THERAPY
Gene therapy is a personalized approach that could free patients from the burdens of ongoing treatment. But it was more of a dream than reality before technological advances allowed scientists to deliver genetic material into the cells of patients using harmless modified viruses.
To develop a gene therapy, SCTM researchers first needed a more complete understanding of the biology of AMD. Hageman’s methodical research over the past decades, which included conducting one of the largest ocular genetic studies, gave the world a new understanding of the role of genetics and biology in the development of AMD.
AMD-associated genes on chromosomes 1 and 10 account for approximately 90% of a person’s risk for developing AMD. A cluster of six genes on chromosome 1, which play critical roles in the immune system, directs one form; a pair of genes on chromosome 10, associated with maintaining ocular health as we age, causes a second. Importantly, Hageman’s team also discovered genetic variants on chromosome 1 that offer strong protection against developing AMD.
“We carry two copies of every gene, so if a person carries two copies of chromosome 1-associated protective genes, they’re highly protected and not likely to develop AMD,” explains Hageman. “If an individual carries two risk copies, they’re highly likely to develop AMD. Interestingly, if someone carries one protective gene and one risk gene, the risk of developing AMD is greatly diminished.”
Commercialized in conjunction with one of the SCTM's corporate partners, the lead product was designed to provide protection for individuals with one or more risk copies of CFH on chromosome 1.

T HE ROAD TO APPROVAL
FDA approval requires multiple phases of testing in humans. The Utah Retinal Reading Center (UREAD)—a component of the SCTM—will analyze images from all patients entered into the clinical trials worldwide. Using retinal imaging techniques, the SCTM has characterized AMD progression in specific genetic groups. Armed with the data, scientists and clinicians will use this information to evaluate the impact of the new gene therapy among the genetic groups.
Phase 1 patients are being divided into three groups. The first will receive the lowest dose of the drug and will be monitored for any complications, such as inflammation, for six months.
The dose will escalate to higher levels in the other two groups, which will also be closely monitored for adverse impacts.

P ATIENT AND DONOR SUPPORT
Although he’s not participating in the clinical trials, Moran patient Stephen Denkers and others like him have made this moment possible.
Denkers is one of thousands who have enrolled in an SCTM patient study to better understand the genetic inheritance within his family and to advance AMD research. He’s also a philanthropic donor to the program.
When his Moran physician explained there was nothing to stop AMD from stealing his sight, Denkers took comfort in thinking about a different future for his loved ones.
“I told him, ‘You may not be able to help me, but you can likely help my children, grandchildren, and so many others,’ ” says Denkers.
Since there are no animal models to research AMD, SCTM researchers chose early on to work with study participants and donated human eye tissue. The ongoing SCTM study Denkers enrolled in now has over 5,000 people with and without AMD or a family history of the disease. The study and the SCTM’s eye tissue repository of nearly 10,000 pairs of donor eyes made breakthroughs possible.
“Without people like Steve, quite simply, we wouldn’t have a drug in clinical trials,” says Hageman.
T HE END GAME
In 2022, the FDA approved four new gene therapies. This year another wave of approvals is anticipated for as many as 13 new gene therapies.
“Personalized medicine is the future, and Dr. Hageman is leading us into that future,” says Moran Eye Center CEO Randall J Olson, MD. “I couldn’t be more excited about this clinical trial because I know it’s based on meticulous work. There is no one who understands AMD at the level of Dr. Hageman and his team.”
Significant investments of time, finances, and resources that were made to understand the genetic underpinnings of AMD as the first step toward building a gene therapy have paid off. Researchers now also understand the genetic inheritances in different ethnic groups.
W hile the SCTM’s first new drug targets chromosome 1-directed AMD, the team is developing additional therapies to treat patients with chromosome 10-directed AMD.
For people like Denkers, it’s a pipeline of hope.
“I can only imagine where we will be 10 years from now,” said Denkers. “I can’t wait to see what this does for families and the world.”
BEHIND THE SCIENCE
The SCTM draws upon the collective strength of its interdisciplinary research team members. Their expertise has been vital to developing the lead product being tested. Key SCTM team leaders in this program are:
Monika Fleckenstein, MD, Clinical and Research Faculty
Jill Hageman, RN, Clinical Research Associate
Jin Liu, PhD, Research Scientist
B urt Richards, PhD, Director of Translational Vector Sciences
Steffen Schmitz-Valckenberg, MD, Clinical and Research Faculty, and Director, UREAD
B randi L. Williams, PhD, Director of Research and Science
Moussa A. Zouache, PhD, Research Faculty
STEP 1:
The SCTM therapy uses a vector, in this case a virus modified to be harmless, to deliver the protective gene.
HOW THE SCTM GENE THERAPY IS DESIGNED TO WORK
SCTM scientists have designed a gene therapy that adds a protective gene in the back of the eye to help slow tissue damage caused by AMD.
STEP 2:
Physicians will deliver the SCTM therapy through a single injection to the macula where AMD originates.
STEP 3:
The cells receiving the therapy serve as “factories” to make protective proteins. These proteins can then move throughout the eye to slow tissue damage.
Research for a new drug begins in the laboratory.
Vector with protective gene delivered to cells in the macula
Drugs undergo laboratory and animal testing to answer basic questions about safety.
and effective. The


What’s Next in Glaucoma Innovation?

Some of the biggest leaps researchers at the Alan S. Crandall Center for Glaucoma Innovation are taking come in small packages. Scientists are vetting new surgical devices so small they require a microscope to view. They are building molecules for the center’s first glaucoma drug. And they are studying how exosomes—the smallest portion of all nanoparticles released by human cells—might be used to treat or detect glaucoma.
The Crandall Center fosters success in the science of small by encouraging large, interdisciplinary teams to share disease models and test new ways of treating glaucoma together.
Researchers and physicians alike are looking toward a future when they can use a simple blood test to diagnose glaucoma and provide treatments that prevent vision loss.
“When you’re doing this kind of science, it really does take a village,” says Crandall Center Associate Director David Krizaj, PhD. “We are recruiting highly accomplished glaucoma researchers from across the country to turbocharge our output, and we are funding new research paradigms. All the puzzle pieces that need to come together for that future are assembled at the University of Utah.”
A NEW DRUG
Krizaj has spent the better part of his career tunneling deep into a narrow topic.
Glaucoma is not a well-understood disease, and it has taken Krizaj more than a decade to understand exactly how a muscular tissue in the eye known as the trabecular meshwork senses and regulates the eye’s internal fluid pressure. This mechanism is key to understanding glaucoma, a potentially blinding disease characterized by high fluid pressure. This elevated pressure kills the cells that make up the eye’s optic nerve, which is responsible for sending information from our eyes to our brain to create vision.
Now, Krizaj is using his knowledge to develop a potential new therapy, a one-two punch that stands to be the Crandall Center’s first blockbuster medication. Lab tests have shown his approach successfully lowers pressure; however, the jaw-dropping novelty of the treatment is its potential ability to also prevent optic nerve cells from dying —a function known as neuroprotection.
There are no neuroprotective drugs on the market for glaucoma, and one that could deliver such treatment would revolutionize care.
W hile universities have traditionally looked to big pharma to translate their discoveries into drugs, Moran has been changing that paradigm. Its Sharon Eccles Steele Center for Translational Medicine (SCTM) establishes partnerships
At left: Trabecular meshwork cells, which play a critical role regulating intraocular pressure. To better understand how the cells function, researchers use fluorescent stains to mark their proteins.

among philanthropists, industry, and academic scientists to speed up drug development. Krizaj points to the SCTM model when describing how interdisciplinary collaboration and private funding will take his discovery from bench to bedside.
Krizaj needed the help of other researchers—chemists and pharmacologists—and private investor funding to complete his work. The research team includes scientists at the University of Utah who are experts in synthetic and medicinal chemistry, organic and bioorganic chemistry, and pharmacology and toxicology.
“Different fields have different priorities, standards, and expectations,” says Krizaj. “That means you have to learn and respect where other people are coming from and then negotiate to find common ground. You have to merge visions of what a successful treatment is.”
The team is in the final stretch of experiments using disease models and next will apply to the FDA for permission to begin testing in humans.

NEW DEVICES
Until the past decade, glaucoma patients had the choice of taking several costly prescription eye drops daily for life or undergoing invasive surgeries with high complication rates and long recovery times.
Championed by Crandall Center Director and worldrenowned surgeon Iqbal “Ike” K. Ahmed, MD, FRCSC, micro-invasive glaucoma surgery (MIGS) changed all of that. MIGS places microscopic devices smaller than 1 mm inside the eye to drain fluid and lower pressure, and it is becoming the cornerstone of modern glaucoma care. Ahmed leads the field in designing and testing new MIGS devices.
Among the devices he’s studying at the Crandall Center are a new laser for glaucoma surgery and an adjustable MIGS device that can be customized for each patient. So-called “cold,” or excimer, lasers generate power from light in the ultraviolet range, and ophthalmologists already use them for procedures such as LASIK. Now, glaucoma surgeons might use the ELIOS excimer laser to create microscopic openings in the trabecular meshwork.
These holes would allow more fluid to drain out of the eye, reducing pressure.
“Currently, we use instruments and devices to remove parts of the drainage channel in a rudimentary way,” explains Ahmed. “An excimer laser is a more precise way to do that with less tissue damage. So much of glaucoma surgery is based on how the eye heals, so anything that can reduce the amount of tissue trauma is potentially better for patients.”
Ahmed is also testing a unique new MIGS device by Myra Vision. The device allows a surgeon to adjust fluid outflow at any point after surgery.
“One of the problems we have with glaucoma devices is that they are set with just a standard flow for all patients, and for some that might be too low, for others too high,” explains Ahmed. “This implant allows us to use a laser to open or close valves to determine how much flow we want at any given time for any given patient. This allows us to really customize the amount of drainage we have to each patient to reach the right target pressure.”
NEW RECRUIT
Born in Ireland, Fiona McDonnell, PhD, joined the Crandall Center in 2022 by way of Duke Eye Center. She specializes in one of the most exciting new areas of glaucoma research—nanoparticles released by all cells in the human body called exosomes. They have several potential applications in new therapies or diagnostic tests.
Studying exosomes, which are 20-150 nanometers in size, requires specialized expertise and equipment—not to mention patience, as she must painstakingly separate them from other cells. Funded by the National Eye Institute, McDonnell is trying to find exosomes specific to the trabecular meshwork—something that could one day help develop a simple blood test for glaucoma. She will also study whether introducing healthy exosomes to damaged cells can repair them.
“If so, a new treatment might be as easy as taking exosomes from a healthy donor or from another part of the body that is not diseased and introducing them into the eye,” explains McDonnell. “It’s similar to stem cell therapy in that you’re using the patient’s own cells.”
Exosomes are already used as carriers to introduce drugs into other parts of the human body. Now, McDonnell wants to see if they can deliver glaucoma therapies to the back of the eye.

COLLABORATIONS AHEAD
Microscopic imaging of exosomes, the subject of glaucoma research in the McDonnell Laboratory.
SCTM Executive Director Gregory S. Hageman, PhD, has changed the world’s understanding of age-related macular degeneration (AMD), a blinding disease impacting adults 55 and over. He and his team clarified the genetics and pathology of the disease. Now he’s testing his team’s first therapy in humans.
Hageman has noticed a potential connection between AMD and glaucoma. Genetic variants on chromosome 1 that increase a person’s risk for developing AMD also appear to increase a person’s risk for developing glaucoma. He’ll explore the finding as head of the Crandall Center’s Translational Research Initiative.
“W hile the SCTM approach was first used to study AMD, we are now excited to focus on glaucoma,” says Hageman. “There is so much work to do, and we have an amazing team of experts to do it.”

Life after Death for the Human Eye: Vision Scientists Revive LightSensing Cells in Organ Donor Eyes
Moran Eye Center scientist Frans Vinberg, PhD, grew up in Finland with the darkness of Arctic winters and the contrast of its midnight sun.
As a scientist, he’s made a career out of studying how the eye’s retina processes the contrasts between light and dark. His innovative approach stands to transform brain and vision research.
In 2022, Vinberg made headlines when he and colleagues revived light-sensing neuron cells in organ donor eyes and restored communication between them. Published in the prestigious journal Nature, their work provides a road map for how the field can begin using functioning human eye cells for research and drug development.
“The scientific community can now study human vision in ways that aren’t possible with animal models,” says Vinberg.
Fatima Abbas, PhD, lead author of the study, conducted experiments in the dark as she exposed donor eye tissue to different kinds of light and recorded photoreceptor responses.

T HE STORY OF A NEURON
Billions of neurons in our central nervous system transmit sensory information as electrical signals; specialized neurons known as photoreceptors sense light in the eye.
Vinberg’s research used the retina as a model of the central nervous system to investigate precisely how neurons die— and new methods to revive them.
It was a painstaking process requiring years of experimentation conducted in a dark room to record cell responses to different light stimuli. Fatima Abbas, PhD, lead author of the published study and then a postdoctoral fellow in the Vinberg Lab, performed most of the experiments.
“We were able to wake up photoreceptor cells in the human macula, which is the part of the retina responsible for our central vision and our ability to see fine detail and color,” explains Abbas. “In eyes obtained up to five hours after an organ donor’s death, these cells responded to bright light, colored lights, and even very dim flashes of light.”
W hile initial experiments revived the photoreceptors, the cells appeared to have lost their ability to communicate with other cells in the retina. The team identified oxygen deprivation as the critical factor leading to this loss of communication. They procured organ donor eyes in under 20 minutes from death to overcome the challenge.
Vinberg, who has a PhD in biomedical engineering, designed a special transportation unit to restore oxygenation and other nutrients to the organ donor eyes. Vinberg also built a device to stimulate the retina and measure the electrical activity of its cells. With this approach, the team restored an electrical signal seen in living eyes, the “b-wave.” It was the first b-wave recording from the central retina of postmortem human eyes.
“We were able to make the retinal cells talk to each other, the way they do in the living eye to mediate human vision,” says Vinberg.
To some, Vinberg’s approach might border on the macabre. But its benefits are clear.
Scientists can use the process demonstrated by the team to study other neuronal tissues in the central nervous system to develop potential new therapies for neurodegenerative

Frans Vinberg, PhD.
diseases, including blinding retinal diseases.
The method can reduce research costs when compared to nonhuman primate research. It also reduces dependence on animal models that don’t always apply to humans. Mice, for example, are often used for research, but they lack a macula, a critical structure in the back of the human eye involved in central vision.
“We hope this will motivate organ donor societies, organ donors, and eye banks by helping them understand the exciting new possibilities this type of research offers,” says Vinberg.
Authors of the study were Abbas, Silke Becker, PhD, Bryan W.Jones, PhD, and Vinberg of the University of Utah; Ludovic S. Mure, PhD, and Satchidananda Panda, PhD, of The Salk Institute for Biological Studies; and Anne Hanneken, MD, of Scripps Research.
WHAT’S NEXT?
Working with the Utah Lions Eye Bank, Vinberg is refining techniques to revive donor eye tissue recovered within one hour after death. This would extend the time window for harvesting functioning retinal tissue for research.

LEARN MORE
Scan to view a video about the Vinberg Lab research breakthrough.
Utah Lions Eye Bank Celebrates 50 Years of Giving the Gift of Sight
The Moran Eye Center’s nonprofit Utah Lions Eye Bank (ULEB) recently celebrated 50 years of working with eye tissue donors and their families to provide corneal tissue for sight-restoring transplants and eye disease research.
Donor families, transplant recipients, and ophthalmologists gathered at the ULEB in September 2022 for a celebration featuring educational tours, food trucks, and games.
“The celebration allowed us to extend our personal thanks to families of tissue donors who have provided hope to thousands of people and share our state-of-the-art facility and process,” says ULEB Director Chris Hanna. “Our coordinators work 24/7 to provide sensitive, timely service, so it was a great opportunity to give people an inside view of what we do.”

ULEB donors give the gift of sight in two ways:
Tissue donation for cornea transplants. This common and effective procedure restores vision for people with certain corneal diseases, such as keratoconus, or damage to the cornea from injury or infection.
Tissue donation of healthy and diseased eyes for research. ULEB supplies eye tissue to world-class researchers developing innovative treatments for various blinding eye diseases, such as age-related macular degeneration (AMD). Research on human tissue allows scientists—including those developing AMD therapies at Moran’s Sharon Eccles Steele Center for Translational Medicine (SCTM)—to investigate disease progression, genetics, and potential new therapies.
The ULEB serves Utah and Idaho as well as patients domestically and internationally. Since Lions Clubs International members founded the ULEB in 1972, it has provided more than 20,000 grafts of corneal tissue to restore vision.
A GRATEFUL PATIENT HONORS HER PHYSICIAN
By the time Janice Evans met Moran’s Mark Mifflin, MD, in 2013, she had a long history of eye problems.
Doctors diagnosed Evans with keratoconus, a potentially blinding corneal disease, at age 11. Now 70, she has had four cornea transplants (three of them in her right eye).
Keratoconus affects one in every 2,000 Americans and is the most common reason for a cornea transplant. The disease causes the cornea, the clear, dome-shaped window in front of the eye, to slowly thin and develop a cone shape over time. Because the cornea focuses light into the eye, the condition causes light rays to go out of focus, blurring and distorting vision. It makes daily activities, such as reading or driving, difficult.
“Keratoconus requires patients to be adaptive and resilient,” explains Mifflin. “It often starts in the late teens or early 20s, but symptoms slowly progress over 10 to 20 years. We can often correct a patient’s vision with glasses or special contact lenses, and the cornea will stabilize. Still, in about 10% to 20% of people, the cornea will eventually become too scarred or will not tolerate a contact lens. If either of these problems occur, we may need to do a transplant.”

A LONG & WINDING ROAD TO GOOD VISION
Evans’ keratoconus diagnosis did not come as a surprise. Her father and half of her siblings also have some form of the condition.
Evans could not see with eyeglasses and has worn some form of rigid contact lenses for nearly 60 years. Before her diagnosis, Evans loved playing softball and basketball. She had to stop playing sports as her sight deteriorated.
She worked editing news film during college and later as a broadcast news producer at KSL-TV News in Salt Lake City. By age 21, fuzzy vision in her right eye made reading impossible, and she had her first cornea transplant.
Six years later, she needed a cornea transplant in her left eye and had to turn down an offer to work for CBS News. However, the network waited for her eye to heal and hired her as a producer in the Chicago bureau. She then worked in the Washington, D.C., bureau before returning to KSL.
Cornea transplants can fail for various reasons, including rejection of the donor cornea or other complications. By 2009, Evans had a second cornea transplant in her right eye. By 2013, she needed a third and final one in that eye.
“I liked Dr. Mifflin right away,” she says. “Since it was my third time with that eye, I asked him, ‘How many at-bats do I get?’ He was so kind and direct. Without missing a
beat, he told me he has one patient who’s had six. I felt confident with him; he really eased my anxiety. You’re awake when they do the surgery, so I could tell he was a solid leader working with a great team.”
Mifflin has helped Evans manage her vision since that time. When the National Keratoconus Foundation (NKCF) solicited nominations for 2022 honors, Evans drew on her recent years of experience and deep gratitude to nominate Mifflin. Her story led the NKCF to name him its 2022 Top Doc.
Today, Evans wears rigid scleral contact lenses, lives independently, can drive, and enjoys cooking and reading.
As director of Moran’s Cornea and Refractive Division, chief of surgical services, and associate medical director of the ULEB, Mifflin has a unique perspective on the importance of corneal tissue donation.
“We could not restore sight to patients like Janice without tissue donated through the eye bank,” he says. “This is a life-changing surgery for patients with corneal diseases that span almost all decades of their life. I have greatly appreciated my long association with patients, families, and with the donors who make it possible to keep on trying and, in most cases, succeeding.”
WW2 'CANDY BOMBER' DONATES EYES FOR RESEARCH
Not all tissue donated to ULEB is used to restore vision. Tissue donated for research can have an equally significant impact for future patients.
Recently deceased, Colonel Gail S. Halvorsen donated his eyes to the ULEB. The Utahn lived by the principles described by family members as “service before self, attitude, gratitude, and that little things add up to big things.”
Better known as “The Candy Bomber,” Halvorsen played a vital role as a pilot in World War II’s Berlin Airlift, supplying food and other crucial supplies to civilians on the ground in West Berlin. One day, after he shared a few sticks of gum with a group of local children and saw the
joy they took in that small offering, he made it his mission to add packets of gum and chocolate to his airdrops. The idea soon took on a life of its own, bringing comfort to thousands of children.
That spirit of giving back lives on through the corneas Halvorsen donated to research upon his passing at age 101 in 2022.
“W hatever a donor’s age and the quality of their vision, each and every donation to research makes a difference in our efforts to translate scientific discoveries into treatments for blinding eye diseases,” says Gregory S. Hageman, PhD, executive director of Moran’s SCTM.

Colonel Gail S.

A longtime partnership with the ULEB has helped the SCTM develop the world’s largest donor eye tissue repository dedicated to research, with 10,000 pairs of eyes available for scientists to compare healthy and diseased tissue. As a result, the SCTM has made groundbreaking discoveries related to AMD—a common blinding disease among Americans age 55 and older.
The number of Americans with AMD is expected to grow to 40 million by 2050.
Since there are no animal models to study AMD, scientists work with donated human ocular tissue to research the biology of the disease.
“Without donations to research, we would not have made such rapid progress toward a gene therapy we have in clinical trials to treat a prevalent form of AMD,” Hageman says. “Colonel Halvorsen did incredible things with his life. He gave and gave, and then when he passed away, he gave once again. We could not be more honored that he chose to donate to the ULEB and SCTM.”
Says Halvorsen’s daughter Denise Williams: “My father focused on helping others during his life, and he saw eye tissue donation as another way to continue to do that, even in death.”

From Daisy to Mina —New Book Helps Families Dealing with a Rare Eye Cancer

Daisy Callister was just 16 months old when her parents noticed a peculiar white spot in her right eye. Days later, they sat in a hospital waiting room while surgeons removed Daisy’s eye—full of cancer.
Daisy, now a spirited 9-year-old, lives a happy life with her parents and two siblings as a survivor of retinoblastoma, a rare cancer that usually affects children under the age of 5.
The family’s journey—from the first realization that something was wrong until Daisy became comfortable with her prosthetic eye—was at times heartbreaking and difficult to navigate. Along the way, they found comfort in hearing stories of other young children forced down the same path.
So they decided to pay the experience forward to help other families facing similar circumstances.
The result is a children’s book based on Daisy’s journey titled Mina and Her New Eye.
Written by Lisa Ord, PhD, LSCW, director of the Moran Eye Center’s Patient Support Program, the story follows a young mouse named Mina who encounters a similar diagnosis and outcome to Daisy’s.
The Daisy Callister Fund, created by Daisy’s grandparents through the family’s Edward J. Callister Foundation, donated funds for the project, part of a retinoblastoma education and support campaign across the Salt Lake Valley.
Retinoblastoma, a cancer that develops in the eye’s lightsensitive retina, affects about 300 U.S. children annually. With current treatments, the survival rate is greater than 95%. Early detection and intervention—as was the case with Daisy—are essential to prevent the cancer from spreading.
“Having a resource like this book is super important, not only for the child but also for the parents and siblings grieving for the loss their loved one is experiencing,” Ord says.
Ord decided that original plans to focus on patients with actual photos might be a little too real for children and their families.
“Using animals as the characters takes it one step away from the person involved,” Ord says. “It’s not quite as scary; they can view it from a distance, so to speak, but

they still understand it is the process they will be experiencing themselves. It helps them know what to expect.”
Holly Nielsen, an award-winning illustrator, brought Mina—and other characters like Dr. Badger, Dr. Bunnywhite, and Mr. Hedge, the prosthetic eye-maker— to life.
In the book, Grandpa Mouse takes a photo and notices a white glow in Mina’s eye and shows it to Mama Mouse, who promptly takes her young daughter to the eye doctor. This is often how cases of retinoblastoma are discovered.
Michelle and John Callister kept noticing something different about their daughter’s right eye and started investigating. Eventually, they determined they were seeing a flash of white in Daisy’s pupil.
They called John’s parents, who advised them to contact the Moran Eye Center immediately.
The following days, weeks, and months were a whirlwind for the Callisters. Somewhere in the blur, they received a book called My Fake Eye. When family members created the fund in honor of brave little Daisy, they wanted to create a new, updated book.

Specialists known as ocularists custom-make prosthetic eyes for each patient to provide a natural appearance. (Courtesy Richard T. Caruso, Eye Prosthetics of Utah)
Ord consulted many specialists while writing the book, and Hailey Haffey, PhD, a medical storytelling expert at the University of Utah School of Medicine, provided editing support.
Sprinkled throughout the pages are questions for young patients to consider. They provide a safe way to discuss difficult issues with children and allow them to express their feelings.
How do you feel about your surgery?
W hat do you want to do to be happy while you get ready for your new eye?
W hat do you want to do to be happy when you have your new eye?
“The Callister family was so generous to take their experience and want to help make a difference for others who will be going through the same thing,” says Ord.
ABOUT MORAN’S PATIENT SUPPORT PROGRAM
The nationally recognized Patient Support Program at the Moran Eye Center offers a variety of professionally moderated support groups and vision rehabilitation services to help patients of all ages, families, and caregivers find ways to understand, accept, and move past the limitations of vision loss. For more information, visit moraneye.link/patient-support.

MINA AND HER NEW EYE Scan to download a PDF of the book.
Changing Lives through the Art of Specialty Contact Lenses

Beyond a range of everyday vision-correcting options in rigid and soft contact lenses, the Moran Eye Center provides patients with access to new generations of specialty contacts for challenging or rare eye issues.
Brandi Lavoie is one of those patients. She came to Moran with achromatopsia — a rare condition marked by the partial or total absence of color vision.
“This inherited retinal condition leads to reduced visual acuity, severe loss of color discrimination, day blindness, and extreme light sensitivity,” explains Dix Pettey, OD, Lavoie’s contact lens specialist.
Lavoie has lived with achromatopsia since she was an infant and could not open her eyes outside. She got by with tinted glasses for most of her childhood.
“In my early teen years, lens options advanced, and my doctor found special contacts that could work for my situation,” Lavoie says. “After trying lots of tints and colors, he found a solution. I started using one pair for day and one for night. When I moved to southern Utah for college, I worried I wouldn’t find a contact lens specialist, so I flew home for appointments. Since I’m legally blind without my lenses, it was scary to contemplate a change.”
After college, Lavoie started as an associate director of student philanthropy and engagement at the University of Utah. She decided to give Moran a try.
“It turns out I didn’t need to worry about switching doctors,” she says. “Everyone at Moran had full knowledge of my condition. They have my lenses hand-painted in Colorado, and they’re great.”
Pettey employs tinted and painted contact lenses for various eye conditions, including aniridia (partial or complete loss of the iris), double vision, migraine, and heterochromia (different-colored eyes in the same person).
“Thanks to advances in contact lens technology, we can add specialized tints to soft contacts to help with light sensitivity, improve patient comfort, and allow them to function at their very best,” says Pettey.
Brandi Lavoie uses one pair of special hand-painted contact lenses for day and one for night to help manage a rare condition affecting color vision.

SCLERAL CONTACT LENSES
Barbara Wesley relies on sharp vision to create her finely detailed glass art pieces. She credits special scleral contact lenses, along with the “kindness and caring” of Moran’s David Meyer, OD, with improving her personal and professional life.
Wesley has keratoconus, which causes the cornea (the clear part of the eye) to become thin and develop a conelike bulge. This results in distorted vision and sensitivity to light and glare.
“In the early stages of keratoconus, you can often improve vision with glasses or soft contact lenses,” explains Meyer, Moran’s director of contact lenses. “But as it progresses, you need special contact lenses to maintain the best vision possible.”
Wesley received her keratoconus diagnosis around age 20.
“By the time I was 40, my vision had really gotten bad,” Wesley says. “I saw double, and everything was blurry. That’s when I was fortunate enough to get a cornea transplant from Dr. Randall Olson at Moran. It changed my life. I remember driving home from the university, and I saw an airplane lower its landing gear and trees on the mountains—it was amazing, and I am forever grateful.”
For several years, Wesley wore gas-permeable lenses, which are hard contact lenses that allow more oxygen to reach the eye than soft options. However, the lenses are small and tend to fall out. They were uncomfortable if any dust or debris came in contact with them.
“Those lenses just didn’t work for me,” Wesley recalls. “I missed seeing the Grand Canyon for the first time because dust was blowing everywhere, and I couldn’t get out of the car because I knew it would blow right into my eyes.”
W hen Meyer met Wesley in 2014, he knew she was a perfect candidate for scleral lenses.
“They’re made specifically for irregular corneas and are much larger than rigid lenses, so they rest on the entire white part of the eye,” says Meyer. “They do a great job of sealing around the eye.”
Another advantage of scleral lenses is that a chamber of fluid forms between the cornea and the back of the contact lens. Because of this, one of the nicknames for a scleral lens is a “liquid bandage.”
“My husband says the lenses changed his life, too,” says Wesley. “Instead of looking for lost contacts and sitting in the car to avoid dust, we enjoy spending time outdoors.”
Survey Identifies Diabetic Retinopathy Screening and Care as Top Outreach Eye Care Need

“ARCHES provides a roadmap for a coordinated, statewide response to providing eye care where it’s needed most.”
Craig J. Chaya, MD, medical director of Moran's Global Outreach DivisionW here is Utah succeeding, and where is it falling short in providing eye care to the state’s most underserved groups?
A recent survey of eye care providers and stakeholders identified screening and care for diabetes-related vision loss as the most urgent need for residents on the Navajo Nation, people experiencing homelessness, former refugees, and underinsured or uninsured Utahns. Vision screenings for children and access to eyeglasses closely followed.
The insights are part of the ongoing Utah Assessment and Review of Community Health Eye Care Study (ARCHES), launched in 2020 by a team of Moran Eye Center and University of Utah health care professionals.
W hile Moran’s Global Outreach Division provides donorfunded charitable care for thousands of Utahns each year at clinics around the state and on the Navajo Nation, the need for care outpaces capacity. Outreach Division Medical Director Craig J. Chaya, MD, University of Utah Division of Public Health Associate Professor Sharon Talboys, PhD, and Moran resident Sean Collon, MD, spearheaded the study to address the challenge by bringing more voices and providers to the table.
“Preserving vision is an investment in our communities that allows our neighbors to fully participate in society, find or hold jobs, care for their loved ones, and engage in school,” says Chaya.
T OP PRIORITIES AND BARRIERS TO EYE CARE
With 61 responses from ophthalmologists, optometrists, and vision health stakeholders, the survey results mirrored the state’s geographic population distribution. Respondents named screening and care for diabetic retinopathy their top priority for underserved residents.
Diabetic retinopathy causes irreversible vision loss as it changes the blood vessels in the retina in the back of the eye. It is the most common diabetic eye disease and a leading cause of blindness in American adults, but many patients skip screenings and treatment due to care costs. Only one survey respondent reported more than 50% of their underserved diabetic patients were up to date on their annual eye screening—a necessary sight-saving precaution. In 2021, Moran’s Global Outreach Division launched a monthly Hope in Sight Retina Clinic as a first step to address the dire need for ongoing monitoring and care, including laser treatments and injections.

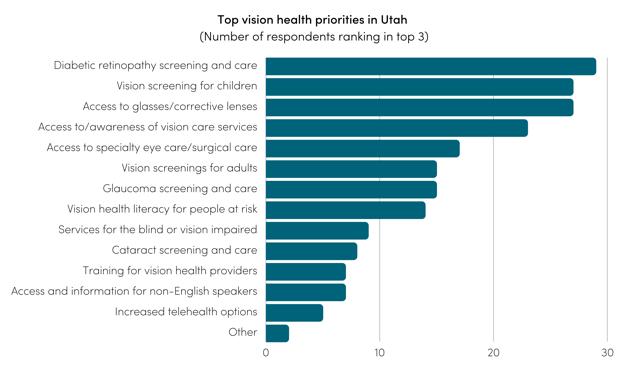
T OP OUTREACH VISION HEALTH PRIORITIES
missing work and lack of transportation were the second most significant barriers, closely followed by a lack of awareness about eye disease and knowledge about resources.
Nearly 85% of survey respondents reported their institution is equipped to serve uninsured patients, non-English speakers, and people with disabilities. Fifty percent of ophthalmologists and 23% of optometrists reported having a funding stream for uninsured patients’ care. Yet, many commented that one of the most significant limiting factors in underserved groups receiving eye care was the lack of patient awareness about how or where they could receive care, coupled with a limited understanding of why they need to receive such care.
“The need for better collaboration among providers and communicating with patients are key takeaways,” says Collon.
Talboys says the findings “will help us advance a public health model for vision care in Utah, where screenings, health education, and linking people to needed services become an integral part of the overall approach.”
N EXT STEPS
➢ Create a referral network that connects primary care community clinics across the state with charitable eye care resources.
➢ Use teleophthalmology to screen diabetic patients for diabetic retinopathy at their local primary care clinics.
➢ Conduct community focus groups and interviews to refine the list of vision care needs and priorities.
➢ Distribute educational materials to patients that explain the basics of eye diseases, eye care and safety, and the need for regular dilated eye exams.
➢ Create research projects to address care priorities.
Navajo Nation Study: Cataracts, Unmet Need for Eyeglasses Are Top Two Causes of Blindness

Conducting the first large-scale eye study of its kind on the Navajo Nation, Moran Eye Center researchers determined cataracts and the unmet need for eyeglasses are the top causes of blindness for the country’s largest Native American tribe.
Publishing in Vision, the researchers examined records from the first visits of 2,251 patients to Moran physicians on the Navajo Nation between 2013 and 2021. Among first-time patients without eyeglasses, 20.67% had mild visual impairment, 9.71% had moderate to severe impairment, and 3.13% were blind. Cataracts, a clouding of the eye’s lens that occurs with aging, were the most common cause of blindness, affecting 40% of these patients. The unmet need for eyeglasses was the second most common cause at 33%. The study additionally found 17.71% of diabetic patients had diabetic retinopathy, a potentially blinding complication of diabetes.
“Until now, no large-scale study of distance and near vision impairment has been conducted on the Navajo Nation,” says Craig J. Chaya, MD, medical director of Moran’s Global Outreach Division and a study author.
“We believe data is the first step toward long-term resolution of eye care health inequities for tribes in the United States. We will use this data to inform our continued efforts on the Navajo Nation.”
Moran’s Global Outreach Division has partnered with Utah Navajo Health Services to provide eye care and sight-restoring cataract surgeries on the Navajo Nation since 2013. While the study was limited to Moran patients, it gives key insights into eye care needs on the Nation, which encompasses portions of Utah, Arizona, and New Mexico and is home to an estimated 173,000 people. Many residents live remotely without adequate access to eye care. They may also experience high rates of sun exposure and have little access to nutritious food, contributing to the development of cataracts and diabetes.
The published study is “Patterns of Blindness on the Navajo Nation: A 9-Year Study,” authored by Ryan T. Wallace, MD; Michael Murri, MD; Lori McCoy; Esteban Peralta; Jeff Pettey, MD, MBA; and Chaya.
Patients from a September 2022 clinic at Navajo Mountain High School, including a mother and daughter at right, are pictured outside the campus before their exams. More than 100 adults and 30 children received exams and eyeglasses or updated prescriptions at the clinic, one of several hosted by the outreach team in 2022. Patients with more intensive needs, like retina and glaucoma issues, were scheduled for surgeries or follow-up procedures

930+
Comprehensive Eye Exams for Adults
Local Outreach Overview 2022
410+
Comprehensive Eye Exams for Children
280+
Adult Glasses
210+
Pediatric Glasses
135+
Cataract and Other Eye Surgeries for Adults and Children
Sofiia, a nurse who settled in Utah recently from Ukraine, received a free eye exam and new eyeglasses as part of the Hope in Sight Outreach Clinic at the Midvalley Health Center in October 2022. She was among 68 Utahns who are former refugees to receive comprehensive eye exams, eyeglasses, and surgery referrals if needed at the clinic.







distributing about 80 pairs of glasses to students.
Support for Promising Young Physician-Scientists
The Achievement Rewards for College Scientists (ARCS) Foundation of Utah has selected two incoming Moran Eye Center residents to receive its 2023-2024 research scholarships. This year, ARCS will award $15,000 each to the two incoming Moran residents to pursue research during residency with the hope they will choose careers that continue their scientific investigations. Moran matches the award for the following two years of residency, providing a total of $45,000.
George Sánchez, MD, will receive the Might Family Foundation Award in memory of Bertrand T. Might; and Erica N. Woertz, MD, PhD, will receive the Mark and Kathie Miller Award in honor of Moran CEO Randall J Olson, MD.
Sánchez earned his medical degree at Dartmouth Medical School. His honors included receiving the Arthur Naitove Surgical Scholar Award, given to one graduating medical student with the greatest potential for making a significant contribution to the field of surgery.
At Dartmouth, Sánchez conducted research in a variety of topics, including the role of anti-vascular endothelial growth factor therapy injections to treat age-related macular degeneration.
Sánchez, who grew up in Hialeah, Florida, as the son of Cuban immigrants, is passionate about providing care to underserved and Spanish-speaking communities. At Moran, he looks forward to continuing his research and providing high-quality, cutting-edge patient care.
Woertz earned her medical degree and doctorate at the Medical College of Wisconsin (MCW). Her dissertation on the visual system in human albinism —completed under the direction of Joseph Carroll, PhD, through the Dennis P. Han, MD Advanced Ocular Imaging Program— earned a top MCW prize. She has co-authored numerous peer-reviewed journal articles and contributed to work presented at prestigious vision and neuroscience conferences. Her extensive training included a visiting student research rotation at Moran under the mentorship of Paul S. Bernstein, MD, PhD. During this rotation, she continued to study human albinism using fluorescence lifetime imaging ophthalmoscopy, an advanced imaging technique designed to characterize pigments in the retina.
During her residency training, she plans to further her research into the connection between retinal pigment, retinal cellular structure, visual acuity, and genetic variability in human albinism.

From left: ARCS Foundation Utah President Sue Dintelman; Moran CEO Randall J Olson, MD; ARCS Scholar
Erica N. Woertz, MD, PhD; ARCS Scholar
George Sánchez, MD; Moran Vice Chair of Education Jeff Pettey, MD, MBA; and ARCS Foundation Utah Vice President for Scholar Outreach Anne Erickson.
New Ophthalmic Hospitalist Position Combines Teaching Moments with Enhanced Patient Care

As the Moran Eye Center’s first ophthalmic hospitalist, Theresa Long, MD, is breaking new ground in resident education and patient care.
One of only a handful of specialists in the emerging ophthalmic hospitalist field, Long recently completed her residency and a tailor-made anterior segment and ophthalmic hospitalist fellowship at Moran.
In her new role, she conducts inpatient and emergency room consults at University of Utah hospitals and supervises Moran’s consulting residents as they make training rounds. She also provides clinical care and performs surgeries at the Moran Eye Center.
“Theresa is passionate about education, and she’s an advocate for change,” says Jeff Pettey, MD, MBA, Moran’s vice chair of education. “As she runs the hospital eye service, our residents gain mentored experience with complex, vision-threatening issues from a highly trained expert. Our hospital patients are admitted with everything from eye socket fractures to strokes in the eye that require specialized care. Residents follow these patients throughout their hospital stay, armed with in-depth knowledge about their conditions. It’s a win-win for hospital patients and trainees.”
Long will continue to expand her educational role as a lecturer and member of Moran’s resident admissions committee and academic administration.
“I’m excited to work with trainees in hospital settings. This will allow them to learn to assess and manage clinically complex patients experiencing a range of conditions,” says Long. “Every moment of our time on the consult service leads to incredible teaching opportunities.”
Long’s own path, Pettey says, offers a perfect example of the individual approach Moran’s nationally ranked education program takes with trainees.
“We work with them to identify strengths and find ways to invest in their success,” he says. “During Theresa’s residency, she blossomed with some unique skills and strengths, making her the ideal candidate to mentor and pioneer our hospital service.”
Associate Program Director of Education Rachel Simpson, MD, adds: “Theresa is highly contemplative—the type of person who devotes time to think things through and figure out how to ensure we do the best job possible. Her skill set lends itself well to this type of medicine.”
Moran offers one of the nation’s top educational programs, providing excellent didactic training and extensive surgical experience. The latest Ophthalmology Times survey of chairpersons and residency program directors at eye centers across the country ranked Moran No. 9 for Best Residency Program. A 2022 survey by physician website Doximity placed Moran’s residency program at No. 5 in the U.S. and No. 1 in the West.


FOR 4 SPOTS IN 2023
340+ MORAN-TRAINED OPHTHALMOLOGISTS
PRACTICING in 45 U.S. states, the District of Columbia, Puerto Rico, and 2 countries
FELLOWSHIP PROGRAM 2022-2023









IN A TYPICAL THREE-YEAR period, one Moran resident, on average, performs about 740 SURGERIES & PROCEDURES.
300 MORE THAN ARE CATARACT SURGERIES
86 IS THE NATIONAL REQUIREMENT
57 PRESENTATIONS
39 PUBLICATIONS BY MORAN TRAINEES IN 2022 AND CURRICULUM DETAILS
Scan for more information about our Education Program.
















2022-2023 OPHTHALMIC PATHOLOGY/RESEARCH FELLOWS 2022-2023





Endowed Chair Marks a Lifetime of Care, Friendship, and Support
John Cumming has seen firsthand how the Moran Eye Center helps people with vision issues and gives them hope.
Cumming’s struggle to keep his eyesight started in his early teens after being shot in the eye by a BB gun. The injury damaged his pupil and impacted his vision in certain light conditions. His father, Ian, turned to Moran CEO Randall J Olson, MD, for help.
“I had been seen by a lot of folks,” says John Cumming, founder and chairman of Powdr, a Park City-based ski and adventure lifestyle company. “Their answer was, ‘That is just the way it is going to be’ or ‘You are just lucky you can see.’ My dad got me an appointment with Dr. Olson, and that all changed.”
L IFETIME OF CARE
Olson remembers that first visit with Cumming—then a young teen feeling socially conscious about his eye looking like a “cat eye” thanks to his injured pupil.
More concerning was the vision loss Cumming experienced—a dangerous issue for an athletic and active young man.
Olson performed surgery on the injured eye, repairing the damaged pupil by removing scar tissue and stitching up a tear.
“It was pretty avant-garde back then to go in and suture that torn area and make sure it was totally free to create the new pupil,” Olson says. “The re-formed pupil and surgery have held to this day.”
Olson and Cumming’s relationship has spanned more than 30 years and more surgeries than Cumming wants to remember. Over time, it turned into much more than purely medical.
For those reasons, John and his brother, David, decided to establish the new Cumming Presidential Endowed Chair to honor Olson.
“Looking at life through broken eyes is not something I’ve enjoyed, but having a partner to guide me through it has been a gift,” Cumming says.
“Dr. Olson has been a tether of optimism for me. Everything he says is thoughtful, empathetic, and responsible. Even when he has news I don’t want to deal with, it is always delivered with a warm, positive, enthusiastic, and can-do spirit.”
G IVING BACK, SUPPORTING A PASSION
In addition to the initial eye injury in his teens, Cumming has dealt with one eye problem after another, including cataracts, floaters, retinal detachment, optic neuritis due to multiple sclerosis, and a macular hole.
In appreciation of the ongoing care, the Cumming Foundation created the endowed chair for Olson. Once Olson retires, the title will change to The Randall J Olson, MD, Presidential Endowed Chair to honor his legacy.
“This endowment is extremely important, and it is going to be used for critical needs I have from time to time,” Olson says. “It makes a huge difference when there is a flexible fund for the department chair to utilize when a pressing need arises. This is just the latest evidence of the Cummings’ generosity for giving.”

Ian Cumming, who passed away in 2018, was known as a corporate titan who quietly supported causes to help under-served communities. He played an important role on a committee helping to create venues for the 2002 Winter Olympics and made many local philanthropic donations. John Cumming has carried on the tradition. Cumming says funding the endowment is “tiny” compared to what he and so many others have gained from Olson and the Moran Eye Center.
“The reality through all of it is that I can see,” Cumming says. "Moran’s efforts have helped so many, many hundreds of thousands of people across the world. For that, we are very grateful. I hope, in some incremental way, it will help maintain the momentum Randy has created at Moran. When you are confronted with not being able to see, it is terrifying. Having help in resolving those issues in a rational, thoughtful way is a gift beyond description.”
“Looking at life through broken eyes is not something I’ve enjoyed, but having a partner to guide me through it has been a gift. Dr. Olson has been a tether of optimism for me. Everything he says is thoughtful, empathetic, and responsible. Even when he has news I don’t want to deal with, it is always delivered with a warm, positive, enthusiastic, and can-do spirit.”
JOHN CUMMING
WHAT IS AN ENDOWMENT?
An endowment is a gift to the university where the principal — the original value of the gift — is invested and not spent directly. Only a portion of the interest accrued on the endowment is distributed to support a program or need. The remainder is reinvested and augments the principal, so the endowment can grow and keep pace with inflation. Endowments last in perpetuity and support distinctive programs, scholarships, research, professorships, buildings — per the donor’s wishes — for generations to come.
Moran Names Two New Endowed Chair Holders
John E. and Marva M. Warnock Presidential Endowed Chair

Craig J. Chaya, MD, medical director of Moran’s Global Outreach Division, has been named as the Warnock Presidential Endowed Chair. Moran CEO Randall J Olson, MD, nominated Chaya to fill the endowed position left vacant with the death of Alan S. Crandall, MD. The Warnock Presidential Endowed Chair agreement requires an ophthalmologist with a passion for outreach work who shares Moran’s commitment to fighting preventable blindness worldwide. Chaya received training in international ophthalmology as a Himalayan Cataract Project/Freedom Foundation Fellow in Kathmandu and Hetauda, Nepal, and volunteered with Crandall on many outreach trips locally and internationally.
“There are overwhelming unmet vision care needs in the world,” Chaya says. “Technology and innovation will allow us to reach more people with visual impairment than ever before. I am grateful for the unwavering commitment of the Warnock family, and I am honored to be leading our Moran outreach initiatives.”
Dr. Ezekiel R. and Edna Wattis Dumke Endowed Chair
Jeff Pettey, MD, MBA, Moran’s vice chair of Education, has been named the inaugural holder of the Dumke Endowed Chair for Global Outreach in the John A. Moran Eye Center.
The Dr. Ezekiel R. and Edna Wattis Dumke Foundation established the endowed chair to promote excellence in teaching, research, and leadership in global outreach.
Pettey has long been a part of Moran’s outreach team locally and internationally and has lectured worldwide on ophthalmic education and outreach.
With support from the endowed position, Pettey will continue efforts to expand access to eye care throughout Utah and the Navajo Nation.
“I’m honored to be the recipient of this generous gift from the Dumke family,” Pettey says. “The endowment supercharges the Moran Eye Center’s global education mission and will expand training, collaboration, and capacity building. The Dumke family’s rich legacy will live on through the gift of sight throughout the world.”


Awards & Honors
NATIONAL RANKINGS
We feel honored and humbled each year to receive recognition as one of the nation’s top academic ophthalmology centers. In 2022, our rankings soared, and we are excited to share the news.
The Moran Eye Center rose to No. 10 in the U.S. News and World Report magazine’s 2022-2023 Best Hospitals for Ophthalmology ranking. The magazine bases its rankings on voting results asking ophthalmologists nationwide where they would send their patients with the most complex eye conditions.
The 2022 Ophthalmology Times magazine survey of eye center chairpersons and residency program directors ranked the Moran Eye Center as No. 10 in Clinical Care. The survey also placed the Moran Eye Center as a leading institution in its other polled categories:
No. 9 Best Residency Program
No. 12 Best Research Program
No. 12 Best Overall Program
In a third recent survey, Doximity’s Residency Navigator ranked Moran’s residency program at No. 5 nationwide and No. 1 in the West. A social networking website for physicians, Doximity conducts an annual survey to determine rankings used by medical school graduates evaluating high-quality training programs. Moran selects just four residency applicants from a pool of more than 700 annually.
POWER LIST
Iqbal “Ike” K. Ahmed, MD, FRCSC, a physician and director of the Alan S. Crandall Center for Glaucoma Innovation, is the second most influential person in ophthalmology worldwide, according to The Ophthalmologist magazine power list. Widely recognized as one of the world’s top surgeons for complex eye conditions, Ahmed is also renowned for his innovative surgical devices for treating diseases, including glaucoma and surgical complications.
A lso, in 2022, Ahmed received the Charles Kelman Medal from the Brazilian Association of Cataract and Refractive Surgery (BRASCRS). As part of the honor, he delivered an address—“IOL Fixation Beyond the Capsular Bag”—during the BRASCRS 2022 convention in Salvador, Brazil.

Awards & Honors

Liliana Werner, MD, PhD, a celebrated researcher focusing on artificial intraocular lenses (IOLs), broke ground as the first woman selected for the American Academy of Ophthalmology’s (AAO) Charles D. Kelman Award and Lecture in 2022. One of the most coveted awarded lectures in ophthalmology, the honor recognizes outstanding achievements in improving cataract surgery through education or innovation.
Werner presented her “25 Years Evaluating New IOL Technologies and Complications” lecture at AAO’s annual meeting in Chicago. She is the fourth Moran faculty member to receive the Kelman Award.
The year brought several additional honors for Werner.
“The Dead Bag Syndrome,” a video produced by Werner and a stellar team of collaborators, continues to receive accolades, including 2022 honors as “Best of Show” at AAO; “Best of the Best” (Cataract Complications) at the American Society of Cataract and Refractive Surgery; the Michael Blumenthal Award at the European Society of Cataract and Refractive Surgery (ESCRS) Video Festival; and first prize in the category of Complications in Cataract and Refractive Surgery from the Brazilian Association of Cataract and Refractive Surgery.
The International Society of Refractive Surgery (ISRS), a partner of the AAO, selected Werner as a 2022 recipient of the Presidential Recognition Award. The award honors her contribution to the field of refractive surgery and the ISRS. Co-director of the world-renowned Intermountain Ocular Research Center, Werner joined Moran in 2002. She and her team vet new IOL technologies worldwide and conduct critical research on related complications. Their work has established foundational knowledge regarding interactions between ocular tissues and IOL design, materials, and surface modifications.
Werner has authored more than 360 peer-reviewed publications and book chapters, co-edited three books, and received numerous awards in international meetings for scientific presentations, videos, and posters. In 2020, she became the first woman and the first Latina to hold the position of U.S. Associate Editor for the Journal of Cataract & Refractive Surgery
She serves as Moran’s inaugural vice-chair for Equity, Diversity, and Inclusion.
Awards & Honors

Paul Bernstein, MD, PhD, a physician-scientist and Moran’s vice-chair for clinical and basic science research, received the Best Investigator of the Year award at the annual Brain and Ocular Nutrition (BON) Conference in Cambridge, United Kingdom.
The award recognizes Bernstein’s remarkable contributions to the field of ocular nutrition, including his work as a principal investigator on the benchmark Age-Related Eye Disease Study 2 (AREDS2), which followed up on an earlier AREDS study to zero in on the effects of certain antioxidants and eye health. As part of the award, he presented a lecture titled: “The role of carotenoids and very-long-chain polyunsaturated fatty acids in retinal health and disease throughout the lifespan.”
BON brings together global experts in brain and ocular nutrition to share research findings on the role of nutrition and lifestyle for the eye and brain and discuss ideas relating to the role of nutrition in human health, function, and well-being.
Amy Lin, MD, a cornea specialist and researcher, received an Achievement Award from the American Academy of Ophthalmology (AAO).
The Achievement Award program recognizes members for their contributions to the AAO, its scientific and educational programs, and the field of ophthalmology.


Brian Stagg, MD, MS, a glaucoma specialist and researcher, earned a David L. Epstein Clinician-Scientist Research Award from the Chandler Grant Glaucoma Society.
He received a $10,000 grant for his project, predictive modeling to provide personalized recommendations for testing frequency for glaucoma patients.
The reward honors David L. Epstein, MD, widely considered one of the most influential leaders in the world of glaucoma and research into the disease over the past 40 years.

Scholars Honors
The Utah Health Equity Leadership & Mentoring (U-HELM) program selected Moran’s Afua Oteng Asare, OD, PhD, as one of 12 scholars for 2022-23.
Launched at the University of Utah School of Medicine in 2018, U-HELM provides mentoring and leadership development opportunities to scholars from underrepresented populations in the health sciences or involved in health equity research and practice.
Asare also has been accepted into the University of Utah Vice President’s Clinical and Translational Research Scholars Program, which is designed to offer intensive mentorship and support to early-stage faculty members engaged in clinical and translational research. The goal is to help these faculty transition into the role of accomplished, funded principal investigators.
Awards & Honors

Promoting Equity, Diversity, and Inclusion in Healthcare
Moran hosted its inaugural Diversity Day Robert H. Hales, MD, Memorial Endowed Lectureship in April 2022.
The event aimed to “recognize and honor the diversity around us all,” according to Liliana Werner, MD, PhD, vice-chair for Equity, Diversity, and Inclusion (EDI). Speakers and participants emphasized the need for more diversity in ophthalmology, why it matters, and how the entire community can work to address the many issues involved.
Featured speaker Terri L. Young, MD, MBA, FARVO, FAOS, chair of the Department of Ophthalmology and Visual Sciences at the University of Wisconsin, presented “Mentoring and Sponsoring Social Identity and Building an Inclusive Environment.”
Abdulkhaliq Barbaar, MSW, MBA, former director of Moran’s Global Outreach Division who is now director of Health, Equity, Diversity, and Inclusion at the University of Utah, presented “Voices of New Americans.”
He detailed the challenges of the refugee and resettlement process and how it affects medical care, something he experienced firsthand. The endowment that supported the event honors the late Robert H. Hales, a prominent Utah ophthalmologist and local medical community leader known for his love of teaching and mentorship.
Moran’s EDI program marked another milestone in 2022, welcoming the first recipient of a new scholarship for medical students who demonstrate a commitment to increasing opportunities for underrepresented minorities within the field of ophthalmology.
Medical student Ruby Garcia, University of Nevada, Reno, spent four weeks at Moran working with clinical and research mentors. The fellowship included direct patient care experiences covering a broad range of ophthalmic specialties.

CELEBRATING GIFTS OF SIGHT
Moran CEO Randall J Olson, MD, welcomed donors to celebrate a newly updated donor wall displaying 1,421 names in December 2022.
“You are making it possible for us to carry out our mission that ‘no person with a blinding condition, eye disease, or visual impairment should be without hope, understanding, and treatment,’” Olson told generous donors who gathered in the Moran atrium where the wall is on display.
Donations to Moran support many causes, including breakthrough research that enables physicians and researchers to take on the challenges of glaucoma, age-related macular degeneration, and other blinding diseases and transform their findings into clinical care.
Donors also make it possible for people in underserved communities in Utah and worldwide to have sight-restoring surgeries and care that changes lives.



 From left, Ira Rubinfeld, Randall J Olson, MD, Harald Olafsson, OD, and Ranae Olafsson.
Kerry and David Carlson.
Moran CEO Randall J Olson, MD, addresses donors at the wall celebration.
From left, Ira Rubinfeld, Randall J Olson, MD, Harald Olafsson, OD, and Ranae Olafsson.
Kerry and David Carlson.
Moran CEO Randall J Olson, MD, addresses donors at the wall celebration.

Highlights
Translational Research Day
Moran’s annual Translational Research Day welcomed Nicole Fram, MD, director and managing partner of Advanced Vision Care and clinical instructor of Ophthalmology at the Stein Eye Institute, UCLA, as its keynote speaker.
Her lecture, “How Complications Become Your Lessons,” looked at how the interaction of bench research and clinical experience solves clinical dilemmas.
The annual conference, co-chaired by Bryan W. Jones, PhD, and Leah Owen, MD, PhD, included presentations from six Moran faculty members on a variety of ophthalmic research topics.
Global Ophthalmology Summit
With the mission of improving eye health and eliminating vision loss through public health advocacy and global ophthalmology education and research collaborations, the American Academy of Ophthalmology held its first Global Ophthalmology Summit in Park City, Utah, in August 2022.
The summit, which brought all ophthalmology subspecialties and interested eye care professionals to the table, included networking events based on geography and focus areas, cutting-edge surgical simulation technology, and an in-depth look at the current state of vision impairment and its causes worldwide.

The event grew from a global ophthalmology fellows retreat Moran hosted in 2020.

Interventional Glaucoma Consortium
The Interventional Glaucoma Consortium, an expansion of the Interventional Glaucoma Congress (IGC), brought together the top thought leaders in the interventional glaucoma field at the Moran Eye Center and Grand America Hotel in Salt Lake City in 2022.
The event included a dedicated program for glaucoma fellows in partnership with Moran. Consortium chairs, including Moran’s Ike Ahmed, MD, FRCSC, and Rachel Simpson, MD, curated the program.
The IGC’s think tank approach encouraged the select group to exchange innovative ideas and education that “promotes a proactive, not reactive, approach to patient care.”
Moran Vice Chair of Education Jeff Pettey, MD, MBA, co-hosts a session at the Global Ophthalmology Summit 2022 with California cataract expert David Chang, MD (shown on video screen). From left, Bryan W. Jones, PhD, Nicole Fram, MD, and Leah Owen, MD, PhD. Moran’s Ike Ahmed, MD, FRCSC, and Rachel Simpson, MD, participate in an IGC session.


Iqbal
Professor
SPECIALTIES
• Glaucoma
• Complex Cataract Surgery
• Lens Implant Complications

Associate Professor
SPECIALTIES
• Comprehensive Ophthalmology
• Cataract Surgery
• Refractive Surgery


Adjunct Associate Professor; Associate Editor of morancore.utah.edu
SPECIALTY
• Glaucoma
Associate Professor
SPECIALTIES
• Neuro-Ophthalmology
• Oculoplastics and Facial Plastic Surgery
CEO of the John A. Moran Eye Center
Randall J Olson, MD
Distinguished Professor and Chair, Department of Ophthalmology and Visual Sciences
The Cumming Presidential Endowed Chair
Director, University of Utah Vision Institute
SPECIALTIES
• Cataract Services
• External Eye Diseases


Craig J.
Professor; Val A. and Edith D. Green Presidential Endowed Chair
SPECIALTIES
• Vitreoretinal Diseases and Surgery
• Retinal Biochemistry
• Macular and Retinal Degeneration

Kathleen B. Digre, MD
Distinguished Professor of Neurology and Ophthalmology; Chair of Clinical Ophthalmology
Resource for Education (Moran CORE) Committee
SPECIALTY
• Neuro-Ophthalmology
Associate Professor; Warnock Presidential Endowed Chair; Medical Director, Moran Global Outreach Division
SPECIALTIES
• Cataract Surgery
• Glaucoma
• Anterior Segment Surgery

David C. Dries, MD
Associate Professor
SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus
• Complicated Adult and Child Strabismus
• Craniofacial Disorders


Professor
SPECIALTIES
• Treatment and Management of AMD
• Degenerative Retinal Diseases

Professor SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus
Meet Our Physicians

Assistant Professor; Director of Ocular Oncology
SPECIALTIES
• Vitreoretinal Diseases and Surgery
• Ocular Oncology

Assistant Professor SPECIALTIES
• Adult and Pediatric Retina Conditions and Surgery


Professor
SPECIALTIES
• Cataract Services
• Neuro-Ophthalmology
• Comprehensive Ophthalmology
Scan for a video playlist to learn more about the care our physicians provide.
Assistant Professor SPECIALTIES
• Uveitis and Ocular Immunology
• Comprehensive Ophthalmology
• Cataract Surgery


Associate Professor; Vice-Chair Faculty Affairs
SPECIALTIES
• Retinal Diseases and Surgery
• Macular, Retinal Degeneration

Associate Professor; Medical Director of Utah Lions Eye Bank
SPECIALTIES
• Corneal Transplantation
• Cataract Surgery
• Vision Correction Surgery (LASIK, PRK, Phakic IOLs)
• Ocular Surface Disease
Associate Professor; Director of Medical Student Education for the Department of Ophthalmology; Editor of morancore.utah.edu
SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus

Assistant Professor SPECIALTIES
• Cataract Surgery
• Comprehensive Ophthalmology
• Ophthalmic Hospitalist Services
Meet Our Physicians

Scan for a video playlist to learn more about the care our physicians provide.


MD

Mark D.
Professor; Director, Cornea and Refractive Division; Chief, Surgical Services; Associate Medical Director, Utah Lions Eye Bank; Director, Cornea Fellowship Program
SPECIALTIES
• Corneal Transplantation
• Cataract Surgery
• Vision Correction Surgery (LASIK, PRK, Phakic IOLs)

Assistant Professor
SPECIALTIES
• Cataract Surgery
• Medical and Surgical Glaucoma
• Comprehensive Ophthalmology
Professor; Director of the Ophthalmic Pathology Laboratory
SPECIALTIES
• Cataract Services
• Ophthalmic Pathology
• Comprehensive Ophthalmology

Associate Professor
SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus


Associate Professor; Dumke Endowed Chair for Global Outreach; Vice Chair, Education; Residency Program Director
SPECIALTIES
• Anterior Segment and Complex Cataract Surgery
• Comprehensive Ophthalmology
Adjunct Associate Professor SPECIALTY
• Comprehensive Ophthalmology
Associate Professor; Division Chief of Oculoplastic and Reconstructive Surgery
SPECIALTIES
• Oculoplastic and Facial Plastic Surgery
• Pediatric Eyelid, Eye Socket, Tear Duct Abnormalities

Professor
SPECIALTIES
• Oculoplastic and Facial Plastic Surgery

Steffen Schmitz-Valckenberg, MD
Professor; Jon M. Huntsman Presidential Chair at the University of Utah
SPECIALTY
• Macular and Vitreoretinal Diseases and Surgery

Assistant Professor; Chair of Visual Electrophysiology
SPECIALTIES
• Neuro-Ophthalmology
• Visual Electrophysiology



Assistant Professor; Associate Program Director of Education
SPECIALTIES
• Glaucoma
• Cataract Surgery
• Anterior Segment Surgery

Adjunct Associate Professor SPECIALTY
• Comprehensive Ophthalmology



Professor; Director of Moran’s Uveitis Division
SPECIALTIES
• Uveitis and Ocular Immunology
• Vitreoretinal Diseases
Professor; Chief of NeuroOphthalmology; Vice-Chair of Quality and Value
SPECIALTY
• Neuro-Ophthalmology

Professor; Director of Vitreoretinal Diseases and
• Retinal Diseases and Surgery
Assistant Professor
SPECIALTIES
• Glaucoma
• Comprehensive Ophthalmology
• Cataract Services
• Geriatric Ophthalmology

Assistant Professor
SPECIALTIES
• Neuro-Ophthalmology
• Pediatric Ophthalmology
• Adult and Child Strabismus


Adjunct Associate Professor; Resident Research Director SPECIALTY
• Glaucoma
Associate Professor; Chief of the Division of Pediatric Ophthalmology
SPECIALTIES
• Pediatric Ophthalmology
• Adult Strabismus
Meet Our Physicians

Scan for a video playlist to learn more about the care our physicians provide.


Professor; Vice Chair and Medical Director of Clinical Services; Executive Director of Clinical Operations
SPECIALTIES
• Glaucoma Services
Associate Professor
SPECIALTIES
• Corneal Transplantation
• Cataract Surgery
• Vision Correction Surgery (LASIK, PRK, Phakic IOLs)
OTHER SPECIALTIES

G.
Medical Director of Anesthesia Services at Moran
SPECIALTY
• General Anesthesiology

Robert M. Christiansen, MD, FACS
Patient Support Program Specialist
SPECIALTY
• Vision Rehabilitation


Director, Ophthalmic Ultrasound Department
SPECIALTY
• Ophthalmic Ultrasound
Director, Patient Support Program SPECIALTIES
• Psychosocial and Functional Issues Related to Vision Loss

Deepika Bagga, OD, provides a full range of optometry services, with special interest in contact lenses and dry eye management.
John A. Moran Eye Center Midvalley Health Center

Brandon J. Dahl, OD, FAAO, specializes in comprehensive optometry, pediatrics, disease management with special emphasis on anterior segment disease, and contact lenses.
Farmington Health Center

David Meyer, OD, FAAO, is the Director of Contact Lens Services, specializing in fitting lenses for keratoconus, postsurgical corneas, pediatrics, irregular or high astigmatism, and eye trauma. He also provides comprehensive eye care for glasses and soft contacts.
John A. Moran Eye Center Midvalley Health Center

Shandi M. Beckwith, OD, provides a full range of optometry services for adults and children, with special interests in myopia management and contact lenses.
Farmington Health Center
Redwood Health Center
South Jordan Health Center

Timothy L. Gibbons, OD, is the Director of the Optometry Division, specializing in comprehensive eye care with special interest in contact lenses, pediatrics, and glaucoma.
Redwood Health Center Stansbury Health Center

Spencer D. Mortensen, OD, FAAO, specializes in contact lenses, sports vision, and general optometry.
Midvalley Health Center

Robert H. Corry, OD, provides a full range of optometry services for adults and children, with a special interest in ocular pathology, contact lenses, and dry eye management.
South Jordan Health Center

Gabriel A. Hulewsky, OD, provides comprehensive optometry services, with special interest in contact lenses, dry eye management, and sports vision.
Midvalley Health Center Parkway Health Center

Edward R. Nicholls, OD, provides comprehensive eye care services, with special interest in contacts, ocular pathology, myopia control, pediatrics, and those with special needs.
Westridge Health Center

Ryan Coyle, OD, provides a full range of optometry services, with an emphasis on primary care, contact lenses, and the diagnosis and treatment of ocular diseases.
Redstone Health Center

Mark A. McKay, OD, specializes in full scope optometric care, including adult and pediatric care, contact lenses, and anterior segment eye disease.
John A. Moran Eye Center Redwood Health Center

Dix H. Pettey, OD, MS, specializes in fitting contact lenses for keratoconus, pediatrics, postsurgical, and eyes with severe or irregular astigmatism. He also provides comprehensive eye care for glasses and soft contacts.
John A. Moran Eye Center Midvalley Health Center
MORAN EYE CENTER Research Team

Iqbal “Ike” K. Ahmed, MD, FRCSC
Professor; Director, Alan S. Crandall Center for Glaucoma Innovation
SPECIALTIES
Glaucoma, Cataract, and Lens
Implant Surgical Therapeutics; Novel Device and Surgical Technique Development

Research Assistant Professor
SPECIALTIES
Retinal Electrophysiology; Retinal Degenerative Diseases; Diabetic Retinopathy; Photoreceptor Physiology

Research Associate Professor (Emerita)
SPECIALTY
Retinal Cell and Molecular Biology

Professor; Mary H. Boesche
Endowed Professor of Ophthalmology and Visual Sciences
SPECIALTIES
Visual Cerebral Cortex Structure and Function; Development of Novel Technologies

Paul S. Bernstein, MD, PhD
Professor and Vice-Chair for Clinical and Basic Science
Research; Val A. and Edith D. Green Presidential Endowed Chair
SPECIALTIES
Nutritional Biochemistry; Macular and Inherited Retinal Degeneration; Fluorescence Lifetime Imaging Ophthalmoscopy

John A. Moran Presidential Endowed Chair; Executive Director, Sharon Eccles Steele Center for Translational Medicine
SPECIALTIES
Genetics and Assessment of Pathways Involved in AMD Etiology; AMD Target Identification and Therapeutic Development

Research Assistant Professor SPECIALTIES
Pediatric Vision Health; Health Services and Systems Research; Health Equity and Disparities; Cost Effectiveness Analysis; Implementation Science

Research Professor (Emeritus) SPECIALTY Electrophysiology

Professor; Ralph and Mary Tuck Presidential Endowed Chair
SPECIALTIES
Membrane Protein Transport in Photoreceptors for Inherited Retinal Disease; Photoreceptor Biochemistry; Molecular Cell Biology

Professor
SPECIALTIES
AMD, Degenerative Retinal Diseases; High-Resolution Imaging; Identification of Prognostic Biomarkers for Disease Progression; Validation of Clinical Endpoints for Interventional Trials

Assistant Professor SPECIALTIES
Vitreous; Collagen; Extracellular Matrix; Aging; Protein Aggregation

Associate Professor; Direc tor, Marclab for Connectomics
SPECIALTIES
Retinal Degeneration Disorders; Retinal Neurotransmission and Neurocircuitry; Metabolomics
MORAN EYE CENTER Research Team 2022-2023

Professor
SPECIALTIES
Photophobia (abnormal light sensitivity); Migraine: its effects on visual quality of life; Ischemic Optic Neuropathy

Professor; Co-Director, Intermountain Ocular Research Center
SPECIALTIES
Ocular Pathology; Comprehensive Ophthalmology; Intraocular Lens Research; Postoperative Inflammation

Professor (Emeritus); Distinguished Professor of Bioengineering, University of Utah; Doctor Honoris Causa, Universidad Miguel Hernandez de Elche, Spain
SPECIALTIES
Artificial Vision/Neural Prosthetics

Helga E. T. Kolb, PhD
Professor (Emerita); Doctor Honoris Causa, Universidad Miguel Hernandez de Elche, Spain; Editor, webvision.med.utah.edu
SPECIALTY Retinal Anatomy

Distinguished Professor (Emeritus) SPECIALTIES
Retinal Neurotransmission and Networks; Retinal Degenerations; Metabolomics

Associate Professor SPECIALTIES
Cognitive Neuroscience; Prefrontal Modulation of the Visual Cortex


Professor and Deputy Director of Research; John Frederick Carter Endowed Professor of Ophthalmology and Visual Sciences
SPECIALTIES
Glaucoma and Intraocular Pressure Regulation; Photoreceptor Signaling; Calcium Regulation in Neuropathological Disorders

Assistant Professor SPECIALTIES
Glaucoma; Conventional Outflow Physiology; Exosomes; Biomedical Engineering Microfluidics

Associate Professor SPECIALTIES
Translational Analysis of Genetic and Molecular Disease Pathophysiology for Blinding Diseases, Including ROP, Strabismus, and Amblyopia; AMD
Research Assistant Professor
SPECIALTIES
Biochemistry and Biophysics of Macular Carotenoids; Mouse Models of Retinal Disease; Raman Imaging of Nutrients in the Retina

Research Assistant Professor; Assistant Professor, Electrical and Computer Engineering
SPECIALTIES
Computational Neuroscience; Neural Mechanisms of Visuospatial Perception

Associate Professor; Dumke Endowed Chair for Global Outreach
SPECIALTIES
Phacoemulsification Platform Efficacy and Efficiency; Ophthalmology Training Methods and Outcomes
BUILDING BRIDGES FROM RESEARCH TO PATIENT CARE

Steffen Schmitz-Valckenberg, MD
Professor; Jon M. Huntsman
Presidential Chair; Director, Utah
Retinal Reading Center, uread.org
SPECIALTIES
AMD; Retinal Imaging; Structural-Functional Correlation

Liliana Werner, MD, PhD
Professor; Co-Director, Intermountain Ocular Research Center; Vice-Chair for Equity, Diversity, and Inclusion
SPECIALTIES
Ocular Biodevices Research; Different Intraocular Lens Designs; Materials and Surface Modifications; Interactions between Ocular Implants and Ocular Tissues

Brian C. Stagg, MD
Assistant Professor
SPECIALTIES
Clinical Decision Support in Glaucoma; Personalized Medicine; Health Informatics; Population Health

Jun Yang, PhD
Professor
SPECIALTIES
Pathogenetic Mechanisms of Retinal Degeneration; Cell Biology of Photoreceptors

Ning Tian, PhD
Professor; Adjunct Professor, Neurobiology
SPECIALTIES
Retinal Neurobiology; Synaptic Plasticity

Research Assistant Professor
SPECIALTIES
Retinal Degeneration Diseases; Neuroscience; Gene Therapy

Frans Vinberg, PhD
Assistant Professor
SPECIALTIES
Retinal Neurobiology; Bioengineering; Mechanisms of Light Signaling and Plasticity in the Retina; Retinal Disease

Moussa A. Zouache, PhD
Research Assistant Professor
SPECIALTIES
AMD; Genetics of Eye Disease; Computational Biology; Engineering Ophthalmology; Drug Development

MORAN EYE CENTER ADJUNCT RESEARCH TEAM
INTERNAL University of Utah
Paul Bressloff, PhD
Brittany Coats, PhD
Karen Curtin, PhD, MStat
Michael Deans, PhD
Jungkyu Kim, PhD
Kristen Kwan, PhD
Jon Rainier, PhD
Jason Shepherd, PhD
Monica Vetter, PhD
Catherine Bowes Rickman, PhD
Carter Cornwall, PhD
Margaret DeAngelis, PhD
Adam Dubis, PhD
Eugene de Juan, MD
Eduardo Fernandez, MD, PhD
Anne Fung, MD
Werner Gellermann, PhD
Mary Elizabeth Hartnett, MD
Wen Fan Hu, MD, PhD
Ariana Levin, MD
Li Jiang, MD, PhD
Tiarnan Keenan, MD, PhD
Anat Loewenstein, MD
Philip Luthert, MBBS, FRCP, FRCPath, FRCOphth
Jordi Monés, MD, PhD
Debra Schaumberg, ScD, OD, MPH
Omer Trivizki, MD
Larry A. Wheeler, PhD
Barry Willardson, PhD
Lloyd Williams, MD, PhD
ADJUNCT VOLUNTEER OPHTHALMOLOGISTS 2022-2023
Adjunct volunteer faculty collaborate on research projects, participate in clinical studies, attend teaching opportunities, and assist on our outreach medical missions.
Jason Ahee, MD St. George, Utah
Arwa Alsamarae, MD Santa Rosa, California
Lisa Arbisser, MD Sarasota, Florida
Nicholas Behunin, MD St. George, Utah
John Berdahl, MD Sioux Falls, South Dakota
Ashlie Bernhisel, MD Merced, California
Ronnie Bhola, MBBS St. Augustine, Trinidad
Kristin O. Bretz, MD Salt Lake City, Utah
Eric Brinton, MD Salt Lake City, Utah
Gregory Brinton, MD Murray, Utah
Michael Burrow, MD Salt Lake City, Utah
Joseph Chen, MD Ventura, California
Robert J. Cionni, MD Salt Lake City, Utah
Richard P. Corey, MD Salt Lake City, Utah
David A. Crandall, MD West Bloomfield, Michigan
Sonya Dhar, MD New York, New York
Jane Durcan, MD Salt Lake City, Utah
Jayson David Edwards, MD St. George, Utah
David Faber, MD Salt Lake City, Utah
Sophia Fang, MD Tigard, Oregon
William J. Fishkind, MD Tucson, Arizona
Roger C. Furlong, MD Butte, Montana
Mitchell J. Goff, MD Salt Lake City, Utah
Reeta Gurung, MD Kathmandu, Nepal
Anna Gushchin, MD Hines, Illinois
Arezu Haghighi, MD Ventura, California
Tara Hahn, MD Houston, Texas
Bradley Hansen, MD Idaho Falls, Idaho
Matheson A. Harris, MD Salt Lake City, Utah
James G. Howard, MD Murray, Utah
Todd Jackson, MD Las Vegas, Nevada
Zachary Joos, MD Renton, Washington
Khizer Khaderi, MD Sacramento, California
Victoria Knudsen, MD Murray, Utah
Elliott Kulakowski, MD Park City, Utah
Robert C. Kwun, MD Murray, Utah
David P. Lewis, MD Brigham City, Utah
Jay J. Meyer, MD Auckland, New Zealand
Majid Moshirfar, MD Draper, Utah
Valliammai Muthappan, MD Sewickley, Pennsylvania
William Myers, MD Chicago, Illinois
Anastasia Neufeld, MD Vancouver, British Columbia, Canada
Tom Oberg, MD Salt Lake City, Utah
Hreem Patel, MD Stickley, Illinois
Rachel Patel, MD Sacramento, California
David B. Petersen, MD Salt Lake City, Utah
Marcos Reyes, MD St. George, Utah
Trent Richards, MD Layton, Utah
Christopher Ricks, MD Provo, Utah
Sanduk Ruit, MD Kathmandu, Nepal
Derek J. Sakata, MD Salt Lake City, Utah
Joshua Schliesser, MD St. George, Utah
Loren S. Seery, MD Kennewick, Washington
D. Snow Slade, MD St. George, Utah
Robert E. Smith, MD West Valley City, Utah
R. Doyle Stulting, MD, PhD Atlanta, Georgia
Russell Swan, MD Sioux Falls, South Dakota
Scott O. Sykes, MD Ogden, Utah
Geoff Tabin, MD Palo Alto, California
Robert L. Treft, MD Layton, Utah
James Tweeten, MD Boise, Idaho
Albert Ungricht, MD Salt Lake City, Utah
Jeremy Valentine, MD Provo, Utah
Aaron N. Waite, MD Lehi, Utah
Gary Wallace, MD Idaho Falls, Idaho
Matthew S. Ward, MD Provo, Utah
Charles H. Weber, MD Oregon City, Oregon
Eric Weinlander, MD Madison, Wisconsin
Robert C. Welch, MD Twin Falls, Idaho
John Welling, MD Medford, Oregon
Brice J. Williams, MD, PhD Ogden, Utah
Darcy Wolsey, MD, MPH Salt Lake City, Utah
Gilbert C. Wong, MD West Jordan, Utah
DonRaphael Wynn, MD Boise, Idaho
Zachary J. Zavodni, MD Salt Lake City, Utah
JOHN A. MORAN EYE CENTER
Donor Report
The following individuals and organizations contributed to the Moran Eye Center from January 1, 2022-December 31, 2022.
DONORS
gifts of $1,000,000 and above
Dick and Timmy Burton Foundation
The Cumming Foundation
Olson-Huntsman Vision Foundation
Perceive Biotherapeutics
gifts of $100,000 and above
The Lawrence T. and Janet T. Dee Foundation
Melvin J. Harwood
Judelson Family Foundation
Gabe L. Newell
Ruth and Randall Olson, MD
Research to Prevent Blindness
Sharon Steele-McGee
gifts of $50,000 and above
Val A. Browning Foundation
Thomas and Candace Dee Family Foundation
Thomas H. and Carolyn L. Fey Family Foundation
William B. Hale*
Kenneth L. Russell, DDS*
James W. and Jeanne J. Welch
JOHN A. MORAN EYE CENTER Donor
gifts of $25,000 and above
Bill and Barbara Chrisman
Stephen G. and Susan E. Denkers Family Foundation
Willard L. Eccles Charitable Foundation
William and Fern England Foundation
Grandeur Peak Global Advisors, LLC
Thomas R. and Susan C. Hodgson
Kemmerer Family Foundation
James M. and Alison Luckman
The Mark and Kathie Miller Foundation
The June Morris and Frendt Family Foundation
Dave and Donna Newberry
Edward H. Skinner
Lisa and Bill Wirthlin
gifts of $10,000 and above
Anonymous
American Society of Cataract and Refractive Surgery
ARCS Foundation, Utah Chapter
William and Sara Barrett
David L. and Kerry Ellen Carlson
Julie T. Crandall
Linda Mara Damiano
Teri and Dean Flanders Foundation
Cecelia H. Foxley, PhD
Doug, Miranda, and Elke Freeman
R. Craig and Gloria H. Hansen
Margaret D. Hicks
Stephen and Lynda Jacobsen Foundation
G. Frank and Pamela M. Joklik
Klintworth Family Foundation
Donald A. and Susan P. Lewon
John and Irene Martin
Thomas O. and Diane J. Might
The Olch Family Trust
Thomas C. Praggastis and Michelle Dumke Praggastis
Richard and Carmen Rogers
Shiebler Family Foundation
Sidra Tree Foundation
James M. Steele and Linda Wolcott-Steele
Dean T. Terry
Utah Lions Foundation
Theodore Waddell and Lynn H. Campion
Terry L. Wright
gifts of $5,000 and above
Anonymous
Association for Research in Vision and Ophthalmology
Fred and Linda Babcock
David Bernolfo
Rodney H. & Carolyn Hansen Brady Foundation
Coon Family Foundation
Errol P. EerNisse and Sonja Chesley EerNisse
Christine A. and Fred W. Fairclough
Joan B. Firmage
Rick Frerichs and Jean Zancanella
Elaine Gordon
Drue B. Huish
Daniel C. and Barbara Hurlbutt
John C. Jarman
Kay W. Lipman
Suzelle and William McCullough
Charles H. McLeskey, MD, and Nanci S. McLeskey, DNP
Karl and Joan M. Mosch
Pegah N. and Majid Moshirfar, MD
Robert N. Owens and Brenda B. Harding
JOHN A. MORAN EYE CENTER Donor
Frank C. and Alice K. Puleo
Zoe and Lon Richardson Jr.
Steven R. and Debra K. Rowley
Susan O. Taylor
John Cramer Terrill
Albert T. Vitale, MD, and Patricia A. Vitale, MD
Warde Foundation
James R. and Linda R. Wilson
Wolf Eye Center, Alaska
gifts of $1,000 and above
Anonymous
Daniel and Laura Alter
Curtis and Susan Anderson
David G. and Marie P. Anderson
Ronald I. Apfelbaum, MD, and Kathleen A. Murray, MD
Eugene W. Banks
Bonnie Barry
William F. and Victoria F. Bennion
Joseph Edward Bernolfo III
Ann P. Bernstein and Paul S. Bernstein, MD, PhD
Michael and Patricia Brill
Irene G. Casper and Ruth A. Morey
Glenn D. Clapp and Kara E. Clapp, PhD
William Clifford, MD, and Jean Clifford, JD
The Honorable Suzanne B. Conlon
Lisa Z. and David A. Crandall, MD
Tony and Joyce Crandall
Eileen Crawford and Alan Jones
Ronald W. Crouch and Elizabeth A. Nielson
William R. and Phyllis S. Crowley
Robert W. and Carol N. Culver
Jim and Susan C. Deacon
Kevin W. Deesing
Jane Durcan, MD and John Hoffman, MD
Henry W. and Leslie M. Eskuche Foundation
Carlton Fenzl, MD
Jack M. and Marianne Ferraro
John H. and Carol W. Firmage
Claire Freedman
Ardis and Luther L. Fry, MD
Eric Fry, MD
James R. and Barbara Gaddis
Carolyn S. and Robert O. Hoffman, MD
Julia and Clair Hopkins Jr., DDS
Jerry S. and Claudia F. Howells
Theodore M. and Charlotte G. Jacobsen
Jim S. and Jeanne N. Jardine
Donald Johnson
Kamas Valley Lions Club
Rick and Beth Kent
Judd P. and Lori R. King
Julia J. Kleinschmidt, PhD
Mel and Wendy S. Lavitt
Frank and Barbara Layden
S. Whitfield and Christina Lee
The Robert B. Lence Family
Paul and Ruth Lyon Family Foundation
Juan E. and Esther R. Medina
Vicki Bettilyon Merchant
Van B. and Maude E. Norman
Ruth L. Novak
Josephine C. and Merrill C. Oaks, MD
JOHN A. MORAN EYE CENTER Donor
Suzanne E. Oelman
Ranae and Harald E. Olafsson, OD
Nancy and Randy Parker
Bonnie D. and James L. Parkin, MD
Dinesh and Kalpana Patel Foundation
Gretchen and Jeff Pettey, MD, MBA
David P. and Suzanne J. Razor
Ronald Reaveley Family
Lynette E. and Daniel Reichert
Helene H. Richer
Edward N. Robinson
Gary W. Rodgers and Chris Filtz
Derek Sakata, MD, and Cindy Sumarauw, DDS
Joseph and Maurine Schumann
Stephen and Marji Bailey Sofro
Howard S. Spurrier, DDS
Stephen D. and Sonnie S. Swindle
Lary J. and Judy W. Talbot
David B. Theobald
Daniel M. Thomas
Douglas Unger
Cynthia A. and Gary W. Wallace, MD
Judith E. A. Warner, MD
Elizabeth B. Wilder
John C. and Carlene A. Williams
Jean A. and Harry C. Wong, MD
gifts of $100 and above
Anonymous
Hans G. Ahrens
Michael Alessandro
Anne D. Alexander
Jeffrey Allen and Gail Gidney
Carol A. and James A. Anderson, PhD
Milton M. and Emily Dianne Anderson
Barry J. and Cathy F. Angstman
Amir and Lisa B. Arbisser, MD
John B. and Neena D. Ashton
R. Larry and Alicia H. Ashton
Katherine Ashworth
Pamela J. Atkinson
Ekhlas Attia
Robert K. Avery and C. Frances Gillmor
Margaret D. and Bryce G. Barker, MD
Merlene Barlow
Thomas Bath
Margo Bathelt
Jan L. and F. Robert Bayle
David W. Becker Jr., MD, JD
Helen Begelman
John E. Bendixen
Janis S. and Richard Y. Bennion III
Ronni and Richard Bergman
Ken and Arlene Berrett
John P. Berry and William Alban
Sheila M. Bilbrey
Margaret N. and Peter W. Billings
Bonnie Blanchard
Arlyn R. and Norma Bodily
Sheri A. and O'Dell M. Bodily
Gary and Herlinda B. Bowen
Alan S. Bradbury
Richard T. and Sharon Bretzing
Michael H. and Patty P. Brimley
Joan M. and Steven M. Brinton
Merle Y. Broadbent
Jane and Lyman R. Brothers III
Marlise P. and Tim W. Brough
JOHN A. MORAN EYE CENTER
Lewis J. Brown
Reid H. Brown
Rosie Brown
Susan J. Brown
David C. Burke
Terri A. Burton
Miriam C. Bushnell
Robin C. Campbell JD, and Marion R. Riley
Randall C. Carlisle
Shirley A. and John K. Carmack
Keith Carson
Donald A. Cathcart
Patrick Reed and Angela Cattelan Reed
Jean Chang
Kirstin M. Chavez
Michelle and Craig Chaya, MD
Qing Chong
Phil W. and Susan D. Clinger
Sherman W. and Susan Clow
John Cofer
Marian Connelly-Jones
Sandra Lee Corp
Kathryn and Denny Cortez
Margaret A. Cragin-Masarone
Paul B. and Tonita M. Crookston
Charles H. Culp
Carl Dennison
Paul Dent
Carolyn Bartlett Deru
T. Jerald and Carol D. Diana
Cameron B. and Rachel M. Diehl
Marilyn E. Domenick
Anita J. and John Drew
James R. and Janet Dunn
Lois M. Dutson
Peter M. and Bonnie H. Edwards
Maureen C. Ellis
Jessie Embry
Eugene F. and Joan R. Erbin
Dennis D. and Carma B. Ewing
The Eye Institute of Utah
Fred Farmer
Rebecca Felix
Daniel S. and Carri Fergusson
Theresa Ferraro
The Firmage Group
Carole E. Fishburn
Leslie and Jon R. Fishburn, MD
Barbara D. Fitzpatrick
Linda T. Flanders
Diane R. Florez
Robert D. Folker
Norine W. Foote
Stanley and Janice T. Foutz
Elaine T. and Frank W. Fox, PhD
Michelle and Todd France
Linda L. Francis
Brian L. and B. J. Fullmer
D. Jay Gamble
Gregory and Jannis Gardner
K. Gary and Linda S. Garff
William A. and Claudia M. Gislason
Zella F. Gledhill Family Trust
John C. and Beth B. Goebel
Joni L. and Kurt Goodfellow
Robert M. Graham
Kay B. Greene
Penelope and Gary M. Grikscheit, PhD
JOHN A. MORAN EYE CENTER Donor Report
Bernard I. Grosser, MD, and Karen J. McArthur
Sivaraman Guruswamy and Vasantha Sivaraman
Margaret L. Haas
Vicky Hall
Ronald C. Hamblen
Gary Hammer
Kristine H. Hammond
Gloria J. and Jim Hannon
Heather B. Hansen
Gareld D. and Betty Jo Hanson
Joan M. and Francis V. Hanson, PhD
Timothy R. and Gloria T. Jean Hanson
Brad D. Hardy, JD, and Jolie A. Coleman
Douglas Hattery
James V. and Gail Hawkins
Susan D. Heath
Vanessa Hendricks
John R. Herman
Nicole L. Herman
Deon T. Hilger
Brad Hobbs, MD
Forest and Pamela Holmes
Barbara Horwitz
Nate Hughes
Samuel T. and Sandra A. Hunter
Thelma P. Iker
Albert Imesch
Clare E. Jackson
Stanley C. and Lana J. Jardine
Roy and Eileen G. Jenkins
Jensen Charitable Foundation
Linda H. and Leland D. Jensen
Norman S. and Gail R. Jensen
Billie Jo and Curt Jones
Jenna Jones
Ryan C. and Jaime Lynn Jones
W. Stanley Jones and M. Gay Taylor-Jones
Mary M. Katsanevas
Brad, Tracey, Sam, Jonah, and Zev Katz
Joette M. and Kurt Katzer
Robyn Carter Keller
Richard A. and Kathleen O. Kennedy
Paul and Geraldine Kilpatrick
Cornelia Kincanon
Douglas Koch, MD and Marcia Murphey
Steve Kornet
Barbara Brittain Korous
David Krajeski and Carol Kotler
Paul Kriedeman and Sarah Werner-Kriedeman
Marilyn and Bob Kukachka
Roger O. and Sue Ladle
Kate Lahey and Michael J. Lahey, MD
Nelson V. Laird
Loris Largo-Rhodes
Jean M. Larsen, PhD
Julie and Darrell R. Larsen Jr.
Christopher G. Latour and Sally M. Patrick, MLS
Harriet T. Lawrence
Lawrence J. and Wendy Foster Leigh
Amy Lin, MD
Darlene Lindley
Judy and Stephen W. Lindsey
Lindsey and Jon Little
JOHN A. MORAN EYE CENTER
Christopher and Susan E. Lockwood
Richard M. and Susan N. Lockwood
Samuel D. and Carol Loftin
Nancy T. Lombardo
Elizabeth Ann Love
Anita L. Lumadue
Dorothy Burton Lyon
Joseph A. and Kim K. Machara
David J. and Vicki W. Mackay
Neil N. and Sandra A. Malamud
Peter Mandros
Glenna Marshall
Collette Marthia
Tawnja Stout Martin
David Matheson
Kurt Matzen
Willard Z. Maughan, MD and Rona Lee W. Maughan, PhD
Bill and Sue Mautz
Mayfield Lions Club
Gary and Suzanne F. McCloskey
James P. and Karen L. McCormick
Lori L. McCoy
Marcie and Wade McEntire
Kevin J. and Pamela McLaughlin
Marvin A. and Renee B. Melville
Suzanne H. Mihalopoulos
Patricia L. Milazzo and Robert E. Briggs
Zella Fae Millard
Ann Marguarite and Kenneth G. Miller
Cory and Christine Mills
Betsy J. Minden
Bruce I. Miya
Casey E., Daysha, and Elle Moore
Edward B. Moreton
Mary and Tony V. Morgan, MD
Paula F. and Michael V. Morris
Moschetti Family
Gary and Lisa Mulcock
Margaret K. Mumford
Linda Myers
Ron and Anna M. Naylor
Barbara and Charles Neal
Marilyn H. Neilson
Sylvia C. Newton
Jeanette Nice
Deanna Nielsen
Brent T. Nilsen
Van B. and Maude E. Norman
Joan J. Odd
Sandra C. and Jim O'Hearn
Stephen L. and Barbara F. Olsen
Lisa Oransoff
Lisa M. Ord, PhD
Kami Page
Brent Palfreyman
Jill and Karl Palmer
Dennis L. and Anne J. Parker
Sangita Patel
Sarah Patrick
Carol and Andrew Pendleton
Bruno E. Perri
Elaine Peterson
Lynn and Gary G. Peterson, PhD
Nedra A. Peterson
George J. and Cynthia Strike Petrow
Jax Hayes and Kathryn H. Pettey
Tamara Phillips
JOHN A. MORAN EYE CENTER
Warren S. Phillips
Howard and Sharon Poch
Herbert H. and Dana D. Pollock
Donald R. and Joyce M. Polster
Jeanniene Turner Posey
Wayne L. and Loretta Pralle
Brent Price
John and Marcia Price Family Foundation
John R. Prokos and Melinda R. Baas
Kenneth M. Pugh
Diana L. Ramirez
V. Raman and Elizabeth Rao
W.E.* and Harriet R. Rasmussen
Elaine and Edgar Redman
Joan Reese
Jeffery A. and Heidi G. Reid
Burt T. Richards, PhD
Mary and Arnold Richer Jr.
Suzanne Rodriguez
Tonya Rogers
Gerald Rolfe
Francis X. and Georgina N. Rossbach
Michael A. Rudick, PhD and Lani Poulson
Alene M. and Leonard H. Russon
Melanie A. and John M. Sacco
J. Stanley and Patricia Schoenfeld
Susan B. Schulman
Richard and Jill Sheinberg
Becky Shiflett
David K. and Patricia L. Sias
Robert and Jan Silberling
Susan M. Skankey
Joanne C. Slotnik and Stephen Trimble
Vicki A. Slotte
Richard and Jenny M. Smartt
Brad J. Smith
Rosanne Smith
Laura J. Springhetti
Lynn H. Stevens and Nedra Wright Stevens
Ron V. and Barbara R. Stevens
Ruth C. and Michael Stevens, MD
Barbara F. and Gerald B. Stringfellow, PhD
The Surgi Care Center Of Utah
Tom and Marsha Swegle
William R. Tanner
R. Burke Teichert
Louis V. and Carole D. Tervort
Mary E. Thompson
Toni Thompson
Ning Tian, PhD and Ping Wang
Candy Turnbull
V. Randall and Susan F. Turpin
Stephen and Ingrid Tyler
John C. and Linda E. Van Dyke
Joseph S. and Margaret P. Viland
Theresa Vonier
Verdon R. and Laurene S. Walker
Everett Lee Ward
Matt J. and Lynn W. Ward
Garda L. Wardle
William J. and Gail C. Wariner
Peter C. and Susan Weaver
Bart and Marlene Wheelwright
Gordon C. and Barbara W. Whiting
Pauline Wiessner, PhD
Joleen S. Willey
JOHN A. MORAN EYE CENTER
Janet C. and H. James Williams, MD
Stephen P. and Nancy Z. Williams
Kurt and Chris Wimberg
Darcy H. Wolsey, MD, Brandon A. Wolsey, MD
Holly C. Wolsey and Tim Soper
Hope Worner
Heather Wozab
Henry C. Wurts and Elaine Ellis
Bette and Kenneth Yanni
Linda Yates
IN HONOR OF
Those in whose honor gifts were made to the Moran Eye Center from January 1, 2022-December 31, 2022.
William R. Barlow Jr., MD
David Bernolfo
Paul S. Bernstein, MD, PhD
Scott Bradbury
Doreen S. Bromfield
Craig J. Chaya, MD
Susan C. Chortkoff, MD
Joseph D' Agnillo
LaVerne A. Diehl
Kathleen B. Digre, MD
David C. Dries, MD
Abagail Durrant
Christine A. Fairclough
Fred W. Fairclough
Roger C. Furlong, MD
Eric D. Hansen, MD
Mary Elizabeth Hartnett, MD
Joseph L. Hatch, MD
Robert O. Hoffman, MD
Eileen Hwang, MD, PhD
Rachael Jacoby, MD
Griffin J. Jardine, MD
Gracie Jones
Jaime Jones
Amy Kalivas
Bradley J. Katz, MD, PhD
David Kimball, DO
Marissa B. Larochelle, MD
Amy Lin, MD
Maureen K. Lundergan, MD
Sharon Lyons
Nick Mamalis, MD
Allie M. Mecham
David A. Meyer, OD
Mark D. Mifflin, MD
Christine Mills
Majid Moshirfar, MD
Austin Nakatsuka, MD
Randall J Olson, MD
Bhupendra Patel, MD
Jeff Pettey, MD, MBA
Charles Pieper
Ashley Polski, MD
Sheila Sconiers
Akbar Shakoor, MD
Rachel G. Simpson, MD
Lois J. Spiegel
Kim Y. Taylor, MD
Colleen Thomas
Albert T. Vitale, MD
Judith E. A. Warner, MD
Miriam Wilhelm
Darcy H. Wolsey, MD
Norm A. Zabriskie, MD
JOHN A. MORAN EYE CENTER
IN MEMORY OF
Those in whose memory gifts were made to the Moran Eye Center from January 1, 2022-December 31, 2022.
Martha S. Ahrens
Margaret L. Bath
Barnie P. Bobbitt
Colleen H. Bowman
Rourke H. Bowman
Robert Brace
Lauren Elyse Bradley
Steven E. Brady, MD
William J. Buhl
Dorothy B. Burton
Richard O. Christiansen
Patricia H. Cofer
Kathleen C. Coon
Bianca Coppa
Ruth H. Craig
Alan S. Crandall, MD
Mary C. Cravens
Jack F. DeMann
Yuriko Dennison
Wayne E. Egan
Sylvia Farmer
Richard A. Fay
James W. Firmage
John Firmage, Jr.
Bruce R. Fishburn, MD
Marian B. Flandro
Zora Foote
Lynda S. Gamble
Chris Georgelas
Alona Taylor Hill
Joyce Hill
Norman C. Jensen
Paul D. Keller Jr.
Yoshie K. Kishimoto
Wm. M. Kleinschmidt
Ryan Link
Bud G. Mahas
Lois Maxwell
Ilene C. McKenna
Harvey Dee Mecham, PhD
Jay A. Meservy, JD
Jean Holt Miller
Steven J. Nichols
Verlan R. Nielsen
Marilyn Oransoff
Julie C. Palfreyman
Roy Garland Pedigo
Darcy Peterson
Darlene M. Phillips
Darlene Prokos
Marion Raish
Svetlana Stojsic
Amelia L. Stone
Graig Taylor
Randall S. Taylor
James Ward Thompson
Richard "Dick" Tomlin
Richard M. Walker
Curtis Wilde
Donald M. Willey
William A. Worner
JOHN A. MORAN EYE CENTER
PLANNED GIFTS
Those who have planned gifts in place to the Moran Eye Center as of December 31, 2022.
Anonymous
JoAnne Ambrose
Neal R. Anderson
David R. and Karen S. Bachman
Bonnie Barry
David Bernolfo
Elmen D. Bloedel
Toni F. Bloomberg
Irene G. Casper and Ruth A. Morey
Donald A. Cathcart Jr.
Richard and Susan Coe
Thomas D. and Candace C. Dee
Carol M. Fay
Dan G. Forman, DVM
Elaine T. and Frank W. Fox, PhD
Bernard I. Grosser, MD, and
Karen J. McArthur
Cliff Hammer
Joseph L. Hatch, MD
Jerry S. and Claudia F. Howells
Curtis C. and Lynne P. Kennedy
Tim and Wendy A. Lacy
Ted Albert McKay
Charles H. McLeskey, MD, and Nanci S. McLeskey, DNP
John A. Moran
Ruth and Randall Olson, MD
Sylvia Prahl-Brodbeck
Linda Stauss Rankin, PhD
Don B. Reddish
Ken and Holly Reynolds
Janet M. Schaap
Edward H. Skinner
Daniel Soulia
Sharon Steele-McGee
Susan O. Taylor
Alice G. Telford
Mary E. Thompson
Haru Toimoto
The Moran Eye Center is grateful for the contributions made to support our mission and goals. We have made every effort to ensure that this January 1, 2022-December 31, 2022, Donor Report is as accurate as possible. Should you find an error or wish to change your listing, please contact us at 801-585-9700.
*Deceased
Best Hospitals for Ophthalmology
No. 10 Nationwide

B est Clinical Care Program No. 10 Nationwide
B est Residency Program No. 9 Nationwide
B est Research Program No. 12 Nationwide
B est Overall Program No. 12 Nationwide

Residency Education No. 5 Nationwide No. 1 in the West
University of Utah Health
Top 10 in the Vizient Quality and Accountability Ranking for the 13th Consecutive Year
No. 6 Ambulatory Care No. 7 Inpatient Care
JULY 1, 2021 — JUNE 30, 2022
Moran Eye Center at a Glance
SURGERIES PERFORMED: 7,999
•Cataract — 4,117
•Pediatric — 1,002
•Retina — 856
•Oculoplastic — 715
•Other — 695
•Glaucoma — 362
•Cornea — 252
PATIENT VISITS BY SPECIALTY
153,369


The John A. Moran Eye Center at the University of Utah is the largest ophthalmology clinical care and research facility in the Mountain West, with more than 60 faculty members, 10 satellite clinics, and 17 research laboratories and centers.
Physicians provide comprehensive care in all ophthalmic subspecialties, making Moran a major referral center for complex cases. Services include:
Cataracts
Cornea & External Eye Disease
Electrophysiology
Emergency Care
Glaucoma
LASIK and Vision Correction
Surgery
Neuro-Ophthalmology
Oculoplastic and Facial
Plastic Surgery
Ocular Oncology
Optometry
Patient Support Program for Patients with Vision Loss
Pediatric Ophthalmology
Pediatric Retina
Retinal Diseases
Strabismus
Ultrasound
Uveitis

