

RESILIENCE
An innovative hip surgery helped Rayana Shoberg overcome pain and reclaim her mobility


“YOU CAN DO SOMETHING EVERY DAY OF THE YEAR IN THE BLACK HILLS. IT NEVER GETS BORING.”
- Ryan, RN
ICU Nurse




RA WELCOME FROM
Paulette Davidson
President and Chief Executive Officer, Monument Health
esiliency is a state of mind, it’s also a statement of physical determination or a firm commitment by an organization, like Monument Health, to be here for generations to come. Our goal is to see our patients through all of their peaks and valleys, victories and defeats; to stand with them as they experience tests

of fortitude and to weather those challenges together with them however we can.
In this issue we are proud to present you with inspiring stories of Resilience from Monument Health staff and patients all across the Black Hills and as far away as North Dakota.
Resilient Dermatologist Mary Logue, M.D., bridges the gap between rural communities and health care access for patients like young Wyatt Trout, who suffers from a rare skin condition. Rachelle White showed great long-term dedication so she could eventually undergo a gastric procedure that helped her to lose 175 pounds.
In the Summer 2021 issue you met 7-year-old Brady Thompson, who was born with an underdeveloped heart. Now 11 years old, a heart transplant has Brady back home on the ranch, where he belongs. In our cover story, Rayana Shoberg shows how tenacity isn’t just part of her character, it’s also the reason she was able to find a solution to her pain through surgery at our Hip Preservation Institute.
Finally, the Heart and Vascular Institute helped Pennington County Commissioner Ron Rossknecht push through cardiac rehab, and reach the summit of Black Elk peak.
Whether you are reading this issue in a comfortable chair at home, or in the midst of a challenge to your own resilience, I hope that you will find these stories as inspiring and moving as I do.


HEALTH
Managing Editor
Melissa Haught
Editor
Stephany Chalberg
Contributors
Wade Ellett
Colette Gannon
Kory Lanphear
Dani Sabrowski
Bob Slocum
Anna Whetham
Art Director
Stacy Brozik
Layout
Stacy Brozik
Terri Upward
Photographer
Kevin Eilbeck
©Monument

CONTENTS
FALL 2025
Where are they now: Brady Thompson
After a heart transplant and recovery requiring nearly a year away from home, Brady is back on the ranch. page 4
Patient Story: Reclaiming Her Life
It’s not a diet change; it’s a lifestyle change. How Rachelle White’s care team worked together to give her a new lease on life. page 8
My Space: Alexandra Brown
Curious how much planning goes into the hospital menus each day? Meet Alexandra Brown and learn about her passion for food. page 12
Ask the Expert: Cancer Genetics and Prevention
Jennifer Knowles, CNP, shares how family genetics can help you learn about risks for certain cancers. page 14
Patient Story: Closing the Gap
Mary Logue, M.D., Dermatologist, is passionate about improving access to care in rural communities. page 16
Foundation Feature: Paying It Forward for Peggy Don Behrens pays respect to his departed partner with a generous financial gift to Hospice House. page 20
Cover Story: Hip Hope
Hip surgery may not have been Rayana Shoberg’s ideal birthday gift. It was, however, a necessary one. page 22
Patient Story: From Heart Surgery to Black Elk Peak
Pennington County Commissioner Ron Rossknecht’s post-heart surgery goal: hike Black Elk Peak. page 26
Nurse Feature: All In the Family
Learn about the four members of the Stover family who work for Monument Health. page 28
Physician Spotlight:
Nicholas Czosnyka, M.D.
Get to know Dr. Czosnyka, General Surgeon at Spearfish Hospital and Clinic. page 30
APP Spotlight: Christine Duerksen, DNP, FNP-C, ENP-C Monument Health’s Director of APP Professional Practice plays many roles. page 32
My Space: Crystal Watters
Crystal puts your care into code. page 34
Introducing
Get to know the physicians who have recently joined Monument Health. page 36
Directory
Find a Monument Health provider near you. page 38
Crossword Puzzle
A challenging and entertaining stroll through this issue via a fun puzzle that you’re sure to enjoy. page 40
BRADY’S BACK
After a life changing year away, the talkative kid with a love of all things spicy is back on the ranch — right where he belongs.


Story by Wade Ellett
Photos by Kevin Eilbeck

In the Summer 2021 issue, we introduced you to Brady Thompson, an outgoing 7-year-old with a love for spicy food, living in Harding County, South Dakota — one of the most rural communities in the country. Brady was born with hypoplastic left heart syndrome, or HLHS, a condition in which the left side of his heart didn’t fully develop before birth, and can’t pump oxygenated blood throughout his body.
“His first surgery was when he was two days old,” said Terisa Thompson, Brady’s mom. “It was part of a three-surgery repair.” Brady’s next surgery was at six months, and the third came when he was about two and a half years old. Although these procedures helped reroute blood, they still don’t provide normal heart function.
Now 11 years old, a lot has changed for Buffalo’s smallest celebrity — most notably, his heart. On Nov. 6, 2023, Brady received a heart transplant at the University of Michigan’s C.S. Mott Children’s Hospital.
Crystal Page, the Physician Assistant at Buffalo Clinic who has cared for Brady for most of his life, can see a drastic change in her young patient. “He doesn’t have to be the boy with half a heart that can’t participate in any activity that overexerts him or could cause an injury,” she said. “He has energy, he gets to play like everyone else on the playground…he gets to be a kid.”
Brady echoes that sentiment himself. “I really like having more energy and getting to do more things,” he explained cheerfully, just after finishing a cookie. “It just feels good to move around!”
A Year Away from Home
A heart transplant is no small thing, and Brady and his parents had to stay in Michigan for a year for monitoring and post-transplant care. Although they made friends during their stay — it’s hard not to like Brady and the Thompsons — the whole family was relieved to return home.
“You know how it is in a small town: you know everybody and everybody knows you. And everybody around here knows Brady’s story,” said Terisa. “It was great coming back and seeing all the familiar faces. You come back and you just fit right back in.”
During the Thompsons’ absence, family, friends and neighbors helped take care of their land and cattle so that they could focus on Brady’s recovery. “That’s small-town life,” she said once more.

“Brady is doing so well! He looks like an entirely different kid. He’s pink, not dusky or blue. He has started growing again, too. You can just tell that he feels so much better. The Thompsons are a great family, and everybody is so happy to have them back! I think going through what they did has taught them to not take the little things in life for granted because they almost lost one of their own. They will always hold a special place in my heart, and I’m happy to call them all friends.”
CRYSTAL PAGE, PA-C, BUFFALO CLINIC
Brady’s heart transplant was made possible by an anonymous donor through the Gift of Life Donor Program, the largest organ procurement organization in the U.S.
Since 1988, the organization has worked with over 14,800 donors, helping to coordinate more than 41,140 organs transplanted. They are also dedicated to educating the public about the importance of organ donation, and encourage people to sign up for the donor registry.
For more information, visit donors1.org.

Brady will need to take anti-rejection medications for the rest of his life. Medications are nothing new for him, though. Crystal and her colleagues at Buffalo Clinic remain part of his ongoing care, which is going well. That is a relief to his entire family. “His mother looks more relaxed and less stressed, too. Each time a heart catheter after-transplant test for rejection came back negative, you could just feel the happiness in Terisa’s posts to update their followers,” Crystal explained. “The whole family looks so relieved and happy.”
For a ranching family whose land has been in the family for more than 100 years, Brady’s transplant is more than just a relief from worry for his parents; it’s reassurance that their son’s health and wellness will continue to improve in step with their way of life.
“I feel like I can do more out here than ever before,”
Brady said, enthusiastically.
His mom agreed. “Having him back here, healthy at home, it’s obvious to me that this is where he’s supposed to be.”
At 11 years old, Brady’s been through more than some people deal with in a lifetime. Through it all, he’s stayed the same enthusiastic, plucky kid. Even after a heart transplant, he’s still the same ol’ Brady…with one minor exception. After recovering from surgery, the Thompsons discovered that the kid once known for his love of all things spicy, who used to carry around his own bottle of hot sauce, now had an inexplicable hunger for cookies, candies and other sweet treats.
“I like to say that maybe my donor had a sweet tooth, and that’s why I like sweets now too!” Brady said with a chuckle.
Nationally Recognized for Excellence in Patient Safety & Quality of Care
Monument Health is nationally-recognized. Yet, our most meaningful accomplishment is consistently delivering high-quality care to our patients. And we will continue to strive to meet the needs of our communities and improve the health and wellbeing of everyone in the Black Hills region for generations to come.







RECLAIMING HER LIFE
Story by Wade Ellett
Photos by Kevin Eilbeck

Shedding 175
pounds helped improve
Rachelle White’s
health — and gave her a new lease on life.
According to the CDC, approximately 42% of adults in the U.S. are obese and another 31% are overweight. An estimated 100 million-plus Americans are actively trying to lose weight. Long-term success is rare: most dieters regain weight within five years.
In other words, the weight-loss struggle is real. More than 270,000 patients have bariatric procedures each year, and for them, the procedure isn’t just about losing weight — it’s about changing their lives. Just ask Rachelle White.
Rachelle is a busy woman. Born and raised in South Dakota, she went to college at Black Hills State University and got her master’s degree from National American University. Now she’s the Executive Vice President of the Black Hills Home Builders Association, has her own business — R. White Events — and is an active mother of three. She’s also one of the many people who has wrestled with weight loss.
“I have struggled with my weight for my entire life,” she said. “Even as a kid, I was a little heavy.” Throughout her teen years, and then 20s, she slowly gained weight and could never keep it off. During each pregnancy, she put on more weight and was never able to lose it again, despite her efforts.
“Each time I would do whatever diet was making the rounds at the time, lose 50 pounds, but then gain it all back, plus some,” she recalled. “And I got to a place after my boys were born, that I just needed to do something different.”
Rachelle had never seriously considered bariatric surgery before and was skeptical. However, a friend found success working with General Surgeon David Fromm, M.D., and Rachelle grew more interested. “After watching her journey for six months, and then talking to her about her experience, I was sold,” she said. “The very next thing I did was call Trish in the office and say, ‘I need a consultation.’”
Understanding Obesity
Tricia Hoffman, PA-C, is very familiar with Rachelle’s hesitance. “It’s unfortunate, but a lot of people don’t really understand bariatrics, or why some people struggle with weight loss,” she explained. “This isn’t about being lazy. These patients have tried everything. ‘Eat less, move more,’ doesn’t work for them. Obesity is a disease — genetic, hormonal, complex.”
The approach is different at Monument Health Bariatric and Metabolic Institute. Staff members like Tricia help to explain that while patients bear some responsibility for their weight, there are a number of factors that can make losing weight — and keeping it off — so challenging.
As Tricia — or “Trish,” as her patients call her — explained the science, the different factors at play and the possibilities for change, Rachelle’s perspective began to change. “I felt hope,” she said. “It was the first time in my life where I went into a doctor’s appointment and I wasn’t made to feel like being overweight was entirely my fault.”
The Monument Health Bariatric and Metabolic Institute provides a comprehensive, team-based approach to weight loss. They combine surgery with ongoing nutritional, mental health and lifestyle support. Their program features expert bariatric surgeons, advanced practice providers, dietitians and even a clinical psychiatrist. Both the Spearfish and Rapid City BMI programs have earned prestigious MBSAQIP accreditation, which ensures safe, high-quality bariatric care. With rigorous follow-ups — from post-op to annual lifetime care — and strong peer support, the center empowers patients like Rachelle to achieve lasting health, confidence and improved quality-of-life.
Scan the QR code below or visit monument.health/ bariatrics for more information.
“I tell people all the time — push the fear aside. Think about your future. Your confidence. The freedom you’ll have. This changes your life.”

That consultation was only the beginning. Contrary to what some might think, bariatric surgery isn’t a quick fix. Rachelle went through a six-month preparation process that involved multiple meetings with Trish, three visits with a dietitian and mandatory consultations with a psychiatrist.
“We’re one of the first centers in the country to fully integrate a clinical psychiatrist into our bariatric program to actively manage mental health and medications that can affect weight loss,” said Dr. Fromm. “We’re not just doing surgery. We’ve built a multidisciplinary clinic where dietitians, obesity medicine doctors, surgeons and our psychiatrist all work together under one roof.”
The Right Procedure for the Right Patient
The bariatric procedure that Dr. Fromm recommended was a biliopancreatic diversion with duodenal switch, or BPDDS. “This is a lesser-known surgery. It’s really effective for patients with a high BMI and significant weight-related health challenges,” he said. “And Rachelle was a perfect candidate and a great patient. She was more than just compliant — she was committed and ready for a real, long-term change.”
BPD-DS is a two-part surgery that includes a sleeve gastrectomy and a rerouting of the intestines to limit calorie and nutrient absorption. “People think it’s just about limiting your ability to eat,” Dr. Fromm explained. “It’s more than that; it’s about rewiring the body’s hunger signals and hormonal response. Patients tell me they’re just not hungry the way they used to be. That’s a huge win.”
A Purpose-Built Team
Dr. Fromm trained at the University of Iowa, which has a rich history when it comes to bariatrics. It was there, in 1966, that Edward E. Mason — often considered the grandfather of bariatrics in the U.S. — performed the first intentional gastric bypass for weight loss. “Whether you wanted to be involved in bariatric surgery or not, you learned a lot about these procedures when you studied there,” he reminisced.
Dr. Fromm was interested, and has been practicing bariatrics since 2009. In 2018, he came to Monument Health, seeing an opportunity to build a more comprehensive, multidisciplinary approach to bariatric care. “This clinic was built with purpose. When I joined Monument Health, it was a chance to grow something bigger, something better,” he said. “We’ve created a space where providers can literally walk down the hall to collaborate in real time. That makes a difference in patient care.”
That collaboration contributes significantly to the success of the program as a whole, but when it comes to losing weight and keeping it off, the responsibility still rests with the patient. “Surgery isn’t the right answer for every patient,” Dr. Fromm said. “They’ve got to be at the right point in their life, prepared to make what is essentially a lifelong
RACHELLE WHITE
“I have the best job in the world; I get to help patients transform their lives. In primary care, I was adding medications. Here, I can help people get rid of them and become the best version of themselves. And we’re not just sending them on their way — we’ll follow up with them forever, if they need us.”
TRICIA HOFFMAN, PA-C


commitment. Not everyone is ready for that yet.”
Trish confirmed that not every patient that schedules a consultation is ready for that kind of commitment. That’s one of the reasons for such a long, involved pre-surgical process. “We’re always looking for potential complications, and sometimes we need to slow down the process or hold off on surgery.”
Sometimes the team will work to address mental health issues first, or suggest alternative treatments including medication. “Even if surgery isn’t the best option for a patient right now, that doesn’t mean that we can’t help them. We’re just going to help in a different way,” she added.
From Start to Finish
Brianne Edwards, PA-C, has been working with Dr. Fromm for years. When he began building the bariatrics program at Monument Health, she was right there beside him helping to shape it. As it grew into the thriving practice that it is today, one thing stayed constant: the team sticks with patients for all of their journey.
“From the first consultation, to support after procedures, we’re with them the whole way,” said Brianne. “From start to finish.” That means that if someone needs help down the road, they’ve got help from the bariatrics team. “Even if it’s years later, we’re going to be part of the care. This isn’t a quick fix, and the patients are in it for the long haul. So are we,” she added.
Commitment, Community and Confidence
For bariatric surgery to be effective, patients have to commit. That’s exactly what Rachelle did. “I decided that if I was going to do this, I was going all in,” she said, matter-of-factly. She dedicated herself to the program, didn’t allow herself to cheat or bend the rules — of which there is a list that bariatric
patients are expected to follow — and came at the effort with an infectiously cheerful disposition.
To her, it was the people at the Bariatric and Metabolic Institute that made all the difference. “You walk in for your follow-ups and it’s like you’ve got a whole cheerleading team. They’re so supportive, and they remember you. You feel celebrated,” she said. The center also directs patients to a Facebook support group, and Rachelle became an active member. “It’s so powerful,” she said. “We’re posting about the things we never could have done before, offering support and just helping one another out. We’ve built a community.”
That community is lucky to have Rachelle, who is a cornerstone of the support group. “She had this funky spark — when she saw hope, she grabbed onto it and never let go. You could see her start to love herself again,” said Trish. “She’s open, honest and vulnerable in a way that inspires others. Not everyone’s willing to be that brave.”
A New Lease on Life
When she started this journey, Rachelle weighed 320 pounds. Now she weighs 145 pounds, and feels like she has a whole new lease on life. She’s more active, feels better and is more confident. “You have so much more energy and motivation to want to try things that you were scared to do before, or felt out of reach. This isn’t just life-changing, it’s life-saving.”
Behind the scenes, Rachelle’s success reflects not just her own effort, but the strength of the comprehensive, multidisciplinary care model at the Monument Health Bariatric and Metabolic Institute — including the bariatric surgeons, obesity medicine specialists, dietitians and the clinical psychiatrist, Kristen Butz, M.D. — that sets this program apart.
“Rachelle is the kind of patient that reminds you of how important our work is,” said Dr. Fromm. “It’s not just about the weight — we get to help people reclaim their lives.”
From l to r: Tricia Hoffman, PA-C; Brianne Edwards, PA-C; David Fromm, M.D.


FROM CLASSROOM TO KITCHEN
Alexandra Brown’s passion for teaching has opened new opportunities to bring hands-on nutrition education to community events.
Story by Stephany Chalberg
Photo by Kevin Eilbeck
Alexandra Brown is extremely busy. As Director of Food and Nutrition at Sturgis Hospital and Clinic and Director of the Teaching Kitchens, she spends part of her work days in menu meetings alongside Chef Kelsey Kerner. The two of them ensure the day’s hospital meals are on schedule. Alexandra then moves on to staff check-ins and scheduling, planning different upcoming Teaching Kitchen events, managing Sturgis Hospital’s Café 2140 and working on day-to-day operations of the Teaching Kitchen itself.
“I am incredibly lucky to have such an amazing team of rock stars,” Alexandra said. “They go above and beyond and make work fun. They are passionate about every task they work on, and it shows.”
Prior to taking this job, Alexandra worked in education
for 12 years, so perhaps it makes sense that she runs Monument Health’s event-based instructional nutrition initiative. “I still get the itch once in a while of being back in the classroom, but that all went away once I volunteered for my first teaching kitchen,” she said.
That was at the 2023 Black Hills Stock Show. After the event, Alexandra asked to continue to be a part of the Teaching Kitchen program. “After that conversation and a green light, we were off like a rocket,” she said. “We did four more within the first five months, and we continue to add new events to our regular events that we do every year.”
Each Teaching Kitchen is a bit different, depending on the event and the space. “Some events are presentations
I would love to be able to educate as many people as possible on healthy eating and healthy nutrition while continuing to build our Teaching Kitchen program.

where we show our audience how to make a certain item and provide nutritional facts about the ingredients. At other events, we make the recipe together with the audience,” she said.
“One of my favorite events was at the North Haines Volunteer Fire Department in Rapid City. We showed them how to prepare a healthy meal, provided recipe cards and had a wonderful presenter, Hollan Harper, D.O., Primary Care Sports Medicine Physician at Orthopedic & Specialty Hospital. Dr. Harper made an educational PowerPoint and answered the questions that our local heroes had.”
“I have a passion for working with our community,” Alexandra said. “I would love to be able to educate as many people as possible on healthy eating and healthy nutrition



while continuing to build our Teaching Kitchen program.”
Outside of her day job, Alexandra and her husband own BK Brown Kattle Company. Located in the Newell area, the ranch holds cattle, horses, chickens and a bunch of other critters. When they can sneak away, Alexandra and her husband enjoy taking their three farm dogs to the lake for camping and fishing. Alexandra also owns a small Western boutique that consists entirely of handmade products — from saddle blanket purses to jewelry, home décor, car air fresheners and much more — that she sells at vendor shows, when time allows. As if she doesn’t have enough going on, Alexandra is also working on getting a half-acre in-ground greenhouse. Her goal is to start a garden that can help feed her community, year-round.
ALEXANDRA BROWN, ON HER PASSION FOR WORKING WITH OUR COMMUNITY

ASK THE EXPERT:
CANCER GENETICS AND PREVENTION
Testing for your hereditary cancer risk is a powerful tool that can empower you to do early, or more frequent, screenings, and to have the knowledge to motivate lifestyle changes.

JENNIFER KNOWLES
NFP-BC, Cancer Genetics and Prevention Clinic at the Cancer Care Institute, Rapid City Hospital
How does cancer develop, and what role do our genes play?
Cancer develops when changes called mutations occur in the genes that control how our cells grow and divide. Most cancers happen by chance, though some families carry inherited genetic changes that increase the likelihood of developing cancer. Knowing whether you carry one of these changes can be a powerful step toward protecting your health and the health of your loved ones.
What are hereditary cancer syndromes?
About 5–10% of all cancers are linked to inherited genetic mutations that are passed from one generation to the next. These are called hereditary cancer syndromes. People with these conditions face a higher lifetime risk of developing certain cancers, and often at younger ages than usually expected. For example, BRCA1 (BReast CAncer) and BRCA2 mutations are well-known for raising the risk of breast, ovarian, prostate and pancreatic cancers. Lynch syndrome is associated with a higher likelihood of colon, uterine, ovarian and other cancers. Li-Fraumeni syndrome, though rare, can be linked to multiple cancers including sarcomas, brain tumors and leukemia.
Who should consider genetic testing?
Anyone can choose to undergo genetic testing if they want to be proactive about understanding their cancer risk and overall health. Testing can be especially important if there are certain patterns in your family, such as multiple relatives with the same or related types of cancer, cancer diagnosed at unusually young ages, more than one type of cancer in the same person or rare cancers like male breast cancer. Even without a strong family history, many people pursue testing simply to gain clarity and peace of mind.
Why does genetic testing matter?
Genetic testing is more than just a lab result — it’s a tool for taking control. It can guide earlier or more frequent screenings, empower you with knowledge to make proactive lifestyle changes and provide useful information for family members who may also face increased risk. In short, it turns uncertainty into actionable information.
What happens if someone tests positive for a genetic mutation?
A positive result doesn’t mean cancer is inevitable. Instead, it allows you to take important steps with the support of your health care team. Depending on the mutation, your care may include earlier or more frequent screenings to detect cancer at its earliest stages, preventive medications or surgeries to reduce risk, and lifestyle changes such as improving diet, increasing exercise or quitting smoking. Another important step is sharing the results with relatives, who may also benefit from testing and proactive care.
How can a genetic provider help?
Although the process of genetic testing and interpreting results can feel overwhelming, genetic providers are there to guide you. They are trained professionals who help explain what your results mean, assess risks and support you in making informed choices for yourself and your family.
What is the main takeaway?
Genetic testing doesn’t predict the future. However, it can provide valuable insight into your health story. By understanding your genetic risk, you can work with your health care team to take proactive steps that put you in control. If cancer runs in your family — or if you simply want to be proactive about your health — consider starting a conversation with your doctor or a genetic provider. The knowledge you gain today could change your future, and your family’s, for the better.


To learn more about the Cancer Genetics and Prevention Clinic, scan the QR code.
CLOSING

THE GAP
The distance between reliable health care and rural patients is growing. When your child suffers from a rare health condition, you do whatever it takes to close that gap. Of course, it helps to have a passionate Physician like Dermatologist Mary Logue, M.D., in your corner.
Story by Kory Lanphear
Photos by Bob Slocum
Rural American families have always lived slightly removed from the services that many of us take for granted: entertainment, groceries, sometimes even fuel for vehicles. For Mark Trout and Victoria Klingbeil-Trout, life in Mohall, North Dakota, comes with a certain number of sacrifices; having to travel 45 minutes to Minot for medical care, for example. One thing they never expected to have to travel even further for, though, was reliable health care for one of their young sons, 3-year-old Wyatt.
Wyatt was born in Minot, North Dakota. He was three weeks premature. “It was kind of a traumatic delivery experience,” said Mark, Wyatt’s dad and a self-employed farmer and campus pastor. “He just looked a little bit different. He had what they called a collodion membrane over his entire body, which is kind of like a cellophane wrap over his skin.”
As Mark and his wife, Victoria, would be told later, the collodion membrane indicated a rare genetic disorder called lamellar ichthyosis, an incurable, lifetime condition that causes patches of dry skin to form scales all over the body.
The on-call pediatrician whisked tiny Wyatt to the NICU and placed him in an incubator. The high humidity inside helped the membrane to peel off without causing more pain and discomfort than necessary.
“Because ichthyosis is such a rare disorder, it wasn't something that a lot of the staff had ever dealt with,” Mark said.
Luckily, at the time, the Minot hospital had on its staff Mary Logue, M.D., a Dermatologist who specializes in pediatric patients and now practices at Monument Health Dermatology in Spearfish.
“Thankfully, the pediatrician reached out to me. I was able to identify his skin condition based on photos and provide immediate reassurance and advise on medical care recommendations,” Dr. Logue said. “Both as a medical student and a resident, I’ve seen around a half dozen cases of lamellar ichthyosis or related skin conditions. Pediatric dermatologists, which are few, and mostly localized to major cities, tend to be the most comfortable at identifying and treating this condition.”
Wyatt’s condition causes itchiness and discomfort at minimum. If his skin gets too dry it cracks and bleeds. Scales can form on his head and combine with his hair, which occasionally creates open wounds. These sores make him more susceptible to staph infection than the average person.
“Dr. Logue is really good at educating you and giving you the confidence you need to be able to care for a child that has a special skin type,” said Victoria. “I went home knowing that if something were to happen, I had someone to call who I could trust, and that it's going to be okay. That's so important.”
The RADS Solution
Ever since she was a young girl, Dr. Logue has held a soft
“I went home knowing that if something were to happen, I had someone to call who I could trust, and that it’s going to be okay. That’s so important.”
VICTORIA KLINGBEIL-TROUT, ON THE CARE THEY RECEIVED FROM DR. MARY LOGUE
spot for rural communities. She was born and raised just outside of Decatur, Illinois, “the Soybean Capital of the World.” She has been disheartened to see her hometown slowly shrink, along with other, similar rural cities in the U.S. As these areas lose population, they lose important services, particularly specialized health care.
“I completed my dermatology residency at the University of New Mexico, where I served a massive rural area including Navajo and Pueblo tribal nations. It was unacceptable to me that these communities were facing such a devastating lack of access to high quality dermatologic care,” said Dr. Logue “This issue is very personal to me. So, I founded a nonprofit called Rural Access to Dermatology (RAD) Society. It’s a ‘boots on the ground’ initiative bringing together my rural colleagues to improve access to care in rural communities across the country. I have patients from South Dakota, North Dakota, Montana and Wyoming and I’m honored to be part of their journey to healthier skin.”
It is important for Wyatt to be appropriately managed by an expert. So when Dr. Logue made the difficult decision to relocate from Minot to Spearfish and begin working for Monument Health, Mark and Victoria faced a gap in care.
“A lot of rural clinics don't think that you need to have dermatology,” said Victoria. “Your primary care doctor can treat some things; other things get misdiagnosed and kids are going years of being mistreated, causing issues. I’m seeing it with my co-workers and friends in the area. It’s just sad to see that we’re not getting access to those doctors.”
Mark and Victoria were so confident in Dr. Logue’s care of Wyatt that when she made the move to Spearfish, they stuck with Dr. Logue, despite the long distance. “It doesn’t feel like a sacrifice to drive seven hours to get good treatment, because we know Dr. Logue is an amazing doctor who goes above and beyond for her patients,” Mark said.

A Supportive Community
In addition to treating Wyatt, Dr. Logue put Mark and Victoria in touch with organizations that help parents of children suffering from conditions like Wyatt’s. They now belong to a community of other families that travel to gatherings across the U.S.
The support has been life changing, according to Mark.

“We apply an ointment to Wyatt’s skin twice a day. It helps to keep it moisturized and protected from infection. One jar costs about $20 and we go through about one jar a week. A patient advocacy organization supplies us with a case every three months,” he said.
Still, there is much care required for Wyatt on a daily basis. Special preparation and constant attention is necessary for Wyatt to experience a normal childhood. Mark and Victoria, though, are prepared. “Wyatt’s sweat glands are blocked so he can’t perspire properly. He overheats pretty easily,” said Victoria. “We use cooling rags, ice packs and spray bottles. We have a bunch of tips that we give daycare providers on how to help him play outside and what signs to notice in making sure he’s getting enough fluids.”
As for Dr. Logue, her mission extends beyond practicing great pediatric dermatology and advocating for rural health care. “I was a teacher before I went into medicine. I am really passionate about spending time in schools, volunteering, teaching kids about everything from the beautiful tones of our skin to our awesome birthmarks to different conditions,” she said. “It’s a really great way to get ahead of social stigma issues around skin conditions; just to normalize it and educate.”
Dr. Logue, in her own way, is not just closing a rural health care gap, she’s perhaps closing a people gap, too.

The Family Medicine Residency (FMR) Clinic in Rapid City is staffed by resident doctors who specialize in family medicine. Working closely with experienced family medicine physicians, an in-house laboratory and imaging services, it is a one-stop shop for your health care needs.
The FMR Clinic has same-day appointments and assists in scheduling consultations with specialty physicians should you need them. Family Medicine Residents also provide continuity of care, seeing their patients in the hospital setting, should you ever be admitted.
FMR also offers outpatient counseling services, a Community Closet and Food Pantry on site. We strive to meet the needs of the whole patient.
FMR accepts most insurance, including Medicare.
“ “
My first visit to this clinic and I am please with the choice I made to come here. The staff are very pleasant and helpful. The young resident I saw was very nice and accommodating to my needs. I would highly recommend this clinic. These young doctors have all the current knowledge on health care. How could you go wrong?
Family Medicine Residency Clinic 502 East Monroe St., Rapid City
PAYING IT FORWARD
Peggy FOR
After the love of his life passed on, Don Behrens paid tribute to her legacy with generous contributions to Monument Health Foundation and the Home+ Hospice Program.

Story by Kory Lanphear | Photo by Kevin Eilbeck

Grief is powerful. The pain of losing a loved one sticks with you for a long time. Or, if we are so unfortunate ourselves as to face an end-of-life-diagnosis, we may even grieve for our own lives and what little time we have left.
However, grief is not what Don Behrens’s beloved partner, Margaret “Peggy” Lee Bowser, fell to when she was diagnosed with terminal bladder cancer in 2023. Instead, she faced her end with inspiring energy and, when that was no longer possible, in contented comfort surrounded by care and respect at Monument Health Home+ Hospice House.
Don, a former funeral business and storage facilities owner-operator, and Peggy had known each other for a long time before their relationship evolved. “Prior to having cancer, Peggy was still very active,” said Don. “We would go skydiving, hiking. We did a lot of off-roading. We’ve been upside down in a Jeep. We've been overseas to Europe — Germany. We hiked to the Leaning Tower of Pisa. Her thought on life was that if you stay active and you have your mind working, you'll always be young, and she always was.”
In the late summer of 2023, Peggy fell ill. She went to the Emergency Department at Rapid City Hospital, and physicians there ran tests that revealed terminal bladder cancer.
There were no treatment options, yet Peggy and Don sought further opinions. “We spoke to other physicians in different places, like Phoenix. And everybody that looked at the records said, ‘We’re not going to be able to help you.’”
On the advice of doctors, Peggy and Don arranged hospice care at Monument Health Home+ Hospice for when Peggy inevitably began to deteriorate.
Then, the two of them embarked on a series of bucket list trips to see as many United States locations as possible — too many places to remember, according to Don. One of those trips brought them to Portland, Oregon. “She told me that there was a doctor she wanted to see,” said Don.
Unbeknownst to Don, Peggy had booked herself a consultation with an end-of-life organization called Death with Dignity. Their purpose is to assist and advocate during the end of life journey for those with terminal illnesses.
At the time, Peggy was not sick enough to meet Death with Dignity’s requirements for their service. She did, however, sign up so that when the time came, Don would charter a plane from Rapid City back to Oregon. “You stay overnight in Portland, and the next morning they have what they call ‘the cocktail’ ready to go. Then you come in and you drink it,” Don said. “And that’s the end.”
Maybe it was an impulse born out of Peggy’s adventurous spirit, or maybe she didn’t want to put Don through watching her suffer; whatever the reason, Don insisted Peggy did not turn to Death with Dignity out of fearfulness. “Peggy had no fear,” he said. “Once we’d explored all the option and knew there's nothing we could do, she realized this is what’s going to happen.”
Peggy and Don returned to their life and stayed in touch with Death with Dignity. Peggy’s health took the expected turn, and she was admitted to Hospice House. “When we entered hospice care, it was like you were part of the family. The staff was phenomenal. It was an easy process,” said Don. “We ate all of our meals together, which was nice. We could sit there and visit. You were just at ease, because you knew there was good care.”
Still, Don assumed that Death with Dignity was what Peggy wanted. “In the last week, as her health started to slide, I asked her if she still wanted to go to Portland. And she said, ‘I like it here. The people are good to me. I’m staying put.’ She was so comfortable and well treated. It was her choice.”
Don was at Peggy’s side during her final hours on February 9, 2024. They had been together for 25 years.
“In the funeral business, I’ve buried countless people. You think you’re numb to it. Peggy was the biggest loss I’ve ever had. I’ve lost family and friends, but nothing’s hit me like this, and it shocked me,” said Don. “We had a great run, we really did. So I try to concentrate on that.”
After Peggy’s passing, Don gave a financial gift to Hospice House through Monument Health Foundation in Peggy’s name. Peggy had asked Don to make the donations after she was gone. “She was very impressed with the care. We wanted to pay that forward and keep it going for others,” Don said. “The whole hospice program is phenomenal. When you have a choice to get on a plane and be done in short order, and you choose to stay — that tells you a lot.”
“Don and Peggy’s story is a powerful reminder of how meaningful care can leave a lasting impact,” said Karlee Baumann, MBA-HCM, Development Officer, Monument Health Foundation. “Their decision to give back was a heartfelt expression of gratitude — an enduring way to honor the kind of care that we all deserve in our final moments.”
Don continues to stop by Hospice House just to say hello and chat with staff and volunteers, with whom he has made bonds that help him cope. Recently he was there to pay tribute to Peggy’s memory with the addition of a Memorial Stone adorned with her name to the Memorial Tree, which resides in the Hospice House Great Room. There, her name will remain alongside the names of other departed loved ones who also benefited from the gentle grace of hospice care.

To donate in honor of someone who received exemplary end-of-life care, scan the QR code or go to monument.health/memorialgiving.
HIP HOPE
Many young people who suffer from hip pain stop physical activities altogether. The Hip Preservation Institute finds solutions to help patients rediscover pain-free movement.


Story by Kory Lanphear
Photo by Kevin Eilbeck

Seventeen-year-old Rayana Shoberg is not the type of person to wait around for something she wants. When she decided to start working and earning her own money, she didn’t just get an after-school or summer job, she graduated high school two years early after acquiring her diploma through an online program, and then started a career in health care.
As impatient and ambitious as she is, when she was 13, lingering pain in her hips slowed her down. So, Rayana sought medical help. “Doctors and nurses told me that I just had growing pains,” she said. “I had doctor appointments where they would do MRIs and X-rays. I went through years and multiple different kinds of physical therapy, but nothing improved.”
A lifelong dancer and active athlete in cross country, basketball and softball, Rayana felt she had no choice but to give up dancing. By the time she was 16, Rayana was still in pain and growing frustrated. She hadn’t given up hope, though, and with the help of her parents, kept pushing for answers. “That’s when Dr. Milligan came in, and he realized that I have hip dysplasia in both hips and there was a chance of it becoming arthritis later in my life.”
After some initial treatment and physical therapy to judge the responsiveness of Rayana’s hips to nonsurgical solutions, Kenneth Milligan, M.D., Orthopedic Surgeon at the Hip Preservation Institute, suggested that Rayana undergo a periacetabular osteotomy (PAO) surgery.
The PAO procedure is a highly specialized hip surgery that is typically only available to patients in large metropolitan areas such as Denver and Minneapolis — and sometimes not even then. Its rarity is due to the training and expertise required to perform the procedure. It is also a relatively recent innovation — there just aren’t that many surgeons trained to perform PAOs yet.
In a PAO, the surgeon makes a small incision over the hip and uses live X-ray to help make several cuts in the pelvis allowing the hip socket to be rotated in a better position. This results in better stability of the hip and less pain.
The Shoulders of Giants
At his own practice, Pediatric Orthopedic Surgeon Eric Krohn, D.O., frequently encounters patients with hip dysplasia, many of them much younger than Rayana. Because of Dr. Milligan’s training in PAO procedures and his sole focus on hips, and Dr. Krohn’s experience diagnosing and monitoring hip deformities in young patients, the two began discussing how to help patients with hip pain who may encounter the same kind of frustrations as Rayana. The lack of accuracy in diagnoses, as Dr. Krohn pointed out, is not the fault of primary care providers or other physicians.
“They literally just don’t know what to look for because it’s not even on their radar,” he said.
“As recently as 10 years ago, specialists were still improving and refining the PAO technique,” Dr. Milligan said. “I had the benefit of watching them go through that learning curve. As a result, I’m able to avoid a lot of the mistakes of the early surgeons just because I got to train with the original pioneers of this surgery.”
“You can see so far because you stand on the shoulders of giants,” added Dr. Krohn.
The solution for Drs. Milligan and Krohn was to join their talents with Orthopedic and Sports Medicine Physicians, a General Surgeon and Physical Therapists at Monument Health Orthopedic & Specialty Hospital in forming the Hip Preservation Institute (HPI), which launched this past May.
MONUMENT HEALTH
HIP PRESERVATION INSTITUTE







TO LEARN MORE, scan the QR code or visit monument.health/ hippreservation
Breanna Connett, M.D. Eric Krohn. D.O.
Abbie Metzler, D.O. Kenneth Milligan, M.D.
Codi Grable, PT, CLT Quinn McCoy, PT
Ryan Steever, PT

The goal is to diagnose and treat hip problems early enough to prevent long-term complications like arthritis and delay total hip replacement surgery until old age. This way, patients can expect to live a full, active life without worry about discomfort, pain or further damage.
Catching hip dysplasia in young patients affords HPI the privilege of offering the full complement of treatments from the beginning. If physical therapy and rehabilitation exercises prove ineffective, surgical options are considered. One of those solutions is the PAO procedure.
Early intervention is so important because in order for the PAO surgery to be most effective, it needs to be performed on patients who are physically mature enough to be nearly finished growing. However, they also must have sustained as little cartilage damage as possible. Damage tends to compound as hips age. It is also irreversible.
Drs. Milligan and Krohn prefer not to focus on a specific ideal age for a patient to undergo a PAO. However, they say it’s generally in the 12- to 35-year-old range and varies on a case by case basis. “Really the idea of this surgery is to get people back to sports, to activities. We do the surgery on professional athletes, so we try to minimize any extra soft tissue disruption or muscle disruption and allow for the fastest recovery possible,” said Dr. Milligan.
The worst-case scenario for the HPI is that a young patient experiences hip pain which goes untreated for
too long. “We’re really focusing on trying to educate the public that if your kid has hip pain, and you go and you see your pediatrician or an orthopedist and they say it’s just growing pains, you should get a second opinion,” said Dr. Milligan. “Come have us take a look at it, because this is a fairly new field and that provider may not have had this particular training. Plus, in our specialty, we also follow special imaging protocols and have technology that allow us to make these diagnoses.”
A Birthday Procedure
Rayana’s PAO surgery was scheduled for late 2024 and just happened to be the day after she turned 17. “I’m not going to be able to go out and do what I enjoy anymore if I don’t get the surgery done,” she remembered thinking. “I’ve seen my grandma go through hip replacements later in life on both of her hips. She is 70 years old and can barely walk. Hopefully doing this surgery now would solve some of those future issues for me.”
The PAO took six hours to complete, and five months to heal. It was a trying time for Rayana; she made it through with help from her family and her boyfriend, and a physical therapy routine designed to get her hip back to full weight bearing as soon as possible.
In a follow-up appointment, Dr. Milligan determined that Rayana’s gait had improved. She decided to return to work. “I had put in an application for Nurse Aide at Rapid City Hospital in August of 2024 but couldn’t interview because of my upcoming surgery,” Rayana said. “They asked me to contact them when I was ready to return to work, which is what I did. There was an open Junior Clinical Assistant position at the Heart and Vascular Institute. I started March 10th.”
Rayana is now employed at the very organization that provided her hip treatment. “I want to be able to accomplish my dreams at a young age. You don’t find very many 20-yearolds that are nurses,” she said.
Her new job also provided a road test of sorts for the results of the PAO. “Before the surgery, if I worked a full day I’d be almost limping because I was hurting so bad. After the surgery, I could work an eight-hour day just fine. Later this summer, I will start my medical assistant program, then eventually go to nursing school. I’m really glad that I did the surgery.”
Whether or not Rayana goes back to have a PAO on the left side depends on her recovery, though she said it’s pretty likely that she will, despite her reluctance to spend another five months healing.
“A lot of people tell me that they’re having hip problems, too. And my advice is: if you feel it, get it checked out now. A $200 bill is better than having a $90,000 hip replacement surgery later in life,” she said.
Rayana is done waiting around. She’s ready to move on. And, thanks to HPI, she can do so pain free.
KENNETH MILLIGAN, M.D.
ERIC KROHN, D.O.

Results often available within 24-48 hours.

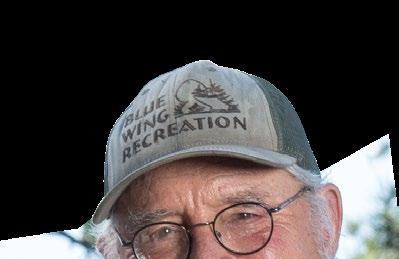

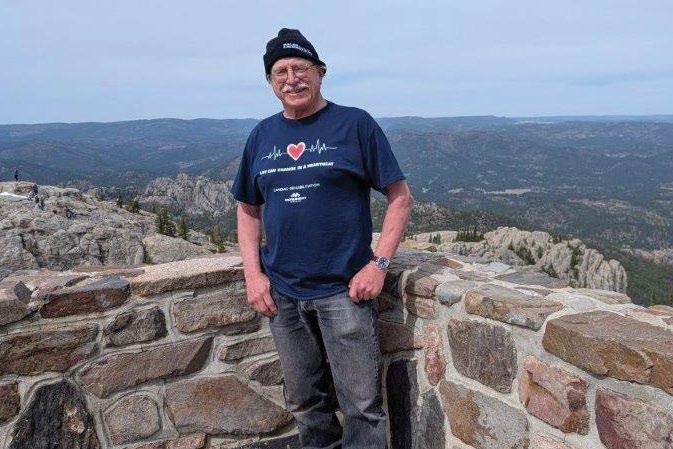
FROM HEART SURGERY TO BLACK ELK PEAK
Thanks to heart surgery at Monument Health Heart and Vascular Institute, Pennington County Commissioner Ron Rossknecht can reach new heights, literally.
Story by Colette Gannon |
by Kevin Eilbeck
After heart surgery, most patients aim to regain their strength, return to daily routines and reclaim a sense of normalcy. Pennington County Commissioner Ron Rossknecht had something bigger in mind: the summit of Black Elk Peak. Four months after undergoing heart surgery at Heart and Vascular Institute, Ron reached South Dakota’s highest point: 7,242 feet in the air, and a world away from the operating room where his journey began.
Photo

A lifelong South Dakotan who grew up in North Rapid City, Ron, 73, has built a life grounded in hard work and a connection to his community. He’s practical and deliberate, the kind of person who takes time to weigh his options and make informed decisions. That mindset carried over when, during what he thought would be a routine checkup, he learned something new about his heart health.
With a history of hereditary heart murmur, it didn’t come as a surprise when a routine appointment to refill a medication turned into an EKG and then an appointment with Charan Mungara, M.D., Cardiothoracic Surgeon at Heart and Vascular Institute (HVI) in Rapid City. What was surprising was the news that Ron needed surgery to replace a heart valve and repair an aneurysm.
After speaking with several physicians, Ron and his partner, Sue, had a choice to make: get the surgery at home in Rapid City at HVI, or go to Mayo Clinic in Rochester, Minnesota.
Before deciding, Ron wanted to talk with someone who had undergone a similar procedure at Monument Health. Dr. Mungara connected him with a previous patient. That conversation gave Ron the clarity he needed. He chose to move forward with the heart team at HVI.
Ron had his valve replacement and aneurysm repair on Dec. 12, 2024. Just five days later, he joined a five-hour Pennington County Commission meeting via Zoom.
“I wasn’t there in person, but I put my suit on and sat on Zoom for five hours. I never missed a meeting because of the surgery, which I was pretty impressed by,” said Ron.
While in recovery, Ron was approached by HVI staff about joining their Cardiac Rehabilitation Program.
Cardiac rehab programs are medically supervised programs that are designed to improve cardiovascular health for patients following surgeries and heart attacks. They typically include exercise training and lifestyle education to improve heart health. At Monument Health, patients graduate from their cardiac rehab programs after 36 sessions, which equates to three months in the program at a rate of three times per week.
“I was teetering about whether or not I wanted to do it,” said Ron. “I was hesitant because I would have to commit to three times a week, but after my introductory lesson, I really liked it. We’d talk to each other at the round table and watch each other graduate. It was heartwarming.”
Ron started slowly, using the elliptical for his first few sessions. After those first sessions, he decided to try the treadmill, at which point Ron was asked if he had a goal. He decided his goal would be to walk two miles in less than 40 minutes.
“Some people can probably do that easily, but when you’re coming out of heart surgery, it’s a different story,”
“ ”
You don’t have to go to Denver or Mayo for heart surgery. You can get that same quality of care — and better — right here at home in Rapid City at Monument Heath.
RON ROSSKNECHT, ON RECEIVING HIGH-QUALITY CARE, CLOSE TO HOME
said Ron. “I won’t regret one minute that I was able to do that at the rehab.”
On April 4, 2025, after finishing his final treadmill walk and weight training routine, Ron’s peers gathered at their round table to celebrate as Ron graduated from the program and received his navy blue T-shirt with the words, “life can change in a heartbeat.”
“We always had to wear a white T-shirt with a pocket for our heart monitors,” said Ron. “When you complete all 36 sessions, you get the blue shirt. That was kind of a big deal.”
That blue T-shirt wasn’t the end of Ron’s journey. Early in his recovery, Ron had made another goal: to hike Black Elk Peak.
On April 12, exactly four months after surgery, Ron and Sue completed the climb together. Wearing his Monument Health cardiac rehab T-shirt, Ron proudly stood at the summit of Black Elk Peak.
Reflecting on his experience, Ron hopes others in western South Dakota understand that they do not need to travel far for expert heart care.
“You don’t have to go to Denver or Mayo for heart surgery. You can get that same quality of care — and better — right here at home in Rapid City at Monument Health,” said Ron. “I want our community to be aware of the quality and experience that Monument Health offers and how thankful I am to all of the staff involved in my procedure and recovery.”

ALL IN THE

Story by Colette Gannon
Photos by Kevin Eilbeck
In the Black Hills, nearly everyone knows someone who works at Monument Health. For the Stover family, that connection runs deeper. Denise, Brooke, Brad and Julia don’t just share a bond through family, they also share a commitment to serving others through their work in health care.
At many organizations, four immediate family members working at the same company would be rare. However, it’s fairly common at Monument Health, the largest private employer in Western South Dakota. Monument Health employs more than 5,600 people across its five hospitals and over 40 medical clinics and specialty centers.
In the Fall 2023 issue we featured Lito and Lucita Casilang and their daughter Sandra Gruenig, a family originally from the Philippines who all work at Rapid City Hospital. Their passion for patient care rang loudly, and the same can be said for the Stover family.
Denise’s Story
The family’s passion for patient care begins with Denise Stover. Currently the Director of Healthcare Informatics, Denise started her career 35 years ago as a licensed practical nurse in an outpatient clinic.
After 11 years of outpatient care, Denise transitioned to an inpatient role at Monument Health Rapid City Hospital, recalling the early years of her husband bringing the kids to the hospital to have dinner with her on her breaks.
Reflecting on her transition from nursing to IT, Denise said, “I would have never guessed that my career would have taken the path that it did. I’ve been at Monument Health this long because I could make changes when I needed to for my family. There has always been a spot for me, and I could always find advancement.”
FAMILY
Following in their Mother’s Footsteps
One of those children brought to the hospital to eat dinner with her mom was Brooke Hochstetter, LPN, the eldest of Denise’s children. Inspired by her mother’s nursing career, Brooke received her licensed practical nursing degree during COVID-19 and currently works in the procedure room and clinic at Heart and Vascular Institute vein clinic. She also recently applied to further her education and become a registered nurse.
With previous experience at a dermatology clinic, Brooke started considering Monument Health as an employer after learning about the tuition reimbursement offered, the overall benefits package and the supportive team environment.
New to her position, Brooke has come to appreciate the teamwork on her floor and the willingness of colleagues to teach her.
Next comes Brad Stover, LPN, younger brother to Brooke and youngest son to Denise. Currently a licensed practical nurse at Orthopedic & Specialty Hospital, Brad was inspired to go into health care through his own lived experiences.
“A competitive bicycle racer in my youth, I was an orthopedic patient all my life, and I was just really fascinated with orthopedics,” said Brad. “I like to see progress with our patients and see them heal and get better.”
Brad also appreciates the opportunities available at Monument Health, saying he feels his skills improve each day while making a difference. He also feels confident that Monument Health will always have a place for him, even when he is ready to move into another type of nursing or position.
“There are very few organizations in the area that offer so much variety,” said Brad. “You can still have your title as a nurse, and you can go to so many different departments and do a different style of nursing.”
A Nurse with a Calling
Finally, we have Julia Stover, RN, the final feature of the Stover Monument Health family unit. Married to Brad, Julia currently works at Cancer Care Institute as an Infusion Registered Nurse.
From Rapid City, Julia went to school in Sioux Falls before starting her career. She chose to move back to Rapid City after meeting Brad, getting a job at the Cancer Care Institute.
“I feel a great sense of purpose with my job,” said Julia. “I see people on the worst days of their lives, and I am proud that I can help make them feel better. I am also excited to be currently enrolled in a nurse practitioner program.”
Caregivers at Monument Health are woven into the fabric of our communities. They are neighbors, friends and family — sometimes all three.
When Patients Are Family
And just as much as Monument Health caregivers are like family, so are patients—sometimes literally.
When Denise’s mom—Brooke and Brad’s grandmother— had cancer, the family was relieved to know the quality of care she would be receiving at Cancer Care Institute.
“My mom has had three different bouts of cancer, and all three times she has gone to the Cancer Care Institute for care,” said Denise. “To know Julia is a part of that team is amazing. It is a wonderful feeling to see my family take part in bringing that to our community.”
Family, Community and Care
To the Stover family, working at Monument Health means providing care for community members as if they were family.
“At the end of the day, we’re always here for you,” said Denise. “The door is always open. You always have access to high-quality care, close to home, and I think that is such an important part of our community.”



NICHOLAS CZOSNYKA, M.D.
GENERAL SURGEON, MONUMENT HEALTH
SPEARFISH HOSPITAL AND CLINIC
Photo by Kevin Eilbeck
My Role
I am one of three full-time general surgeons in Spearfish. My practice is broad. It focuses on taking calls to address emergencies such as appendicitis, cholecystitis and diverticulitis. I also do elective care such as hernia repairs, varicose vein treatments and endoscopy. I have a special interest in treating breast cancer and work closely with the medical and radiation oncology teams and Plastic Surgery in Rapid City to deliver comprehensive breast cancer care, with the surgical portion of treatment able to be performed at the Spearfish Hospital. Every day looks a bit different than the last, and that is one of the things I love about general surgery. Typically, I have one and a half scheduled days in the operating room, two days doing endoscopy, and the rest of the week is for visiting patients in the clinic.
My Goals
Most importantly, my goal is to take care of my patients with effective and safe surgery. I want people to feel like they can trust a recommendation I give for surgery and also understand their diagnosis completely when they walk out of my clinic. To accomplish that, I work to stay up to date on surgical best practice guidelines and always try to remember that there might be a better or different way to explain things that could make my message more clear.
My Passion
There are many parts of my profession that I love, but I am particularly passionate about helping my patients understand the why behind the recommendations I make. As a surgeon, I love to operate, because it is the nuts and bolts part of patient care that makes the difference in people’s lives, but I also really like talking to patients before and after surgery, helping to answer their questions and make sure they understand what to expect before and after surgery.
I also am very fortunate to have a loving family and strong community here in Spearfish. We are active in our local church. I love listening to and playing music, particularly different styles of guitar music and I recently became passionate about home renovation projects.
My Team
There is a great team of nurses and tech that help in countless different ways; in the Clinic, OR, Endoscopy and the hospital. A surgeon can’t do it alone, and the foundation of support all around me is what makes the days flow so smoothly. I work with Kayla Hatten, CNP, directly. She is the nurse practitioner that works alongside me in the clinic and the OR. She does a great job seeing patients for all general surgery needs that I treat.
“There are many parts of my profession that I love, but I am particularly passionate about helping my patients understand the why behind the recommendations I make.”
NICHOLAS CZOSNYKA, M.D.

Want to learn more about Dr. Czosnyka? Scan the QR code for more information.

CHRISTINE A. DUERKSEN, DNP, FNP-C, ENP-C
Director of APP Professional Practice, Doctor of Nursing Practice, Certified Family & Emergency Nurse Practitioner, Monument Health & Lead-Deadwood Hospital
Photo by Kevin Eilbeck

Since starting at Monument Health in November 2022, Christine Duerksen has come to serve in a dual capacity.
As Emergency Nurse Practitioner in the Lead-Deadwood Emergency Department, Christine is also the system-wide Director of APP Professional Practice, a leadership role that involves partnering with the Chief Medical Officer and Chief Nursing Officer to support, develop and guide advanced practice providers (APPs) throughout the health system.
Christine is also an Associate Professor for Mount Marty University’s Family Nurse Practitioner Program, where she educates and mentors the next generation of nurse practitioners.
“My schedule is dynamic and varied,” she said. “On clinical days, I provide comprehensive emergency care in a fast-paced, rural setting. Our Emergency Department varies in volume from day to day, depending on the many events in Deadwood.”
In her administrative role, Christine’s days are filled with meetings, systemlevel planning and committee work. She also leads initiatives that strengthen provider expertise and improve patient satisfaction.
Christine’s mission is to improve the development and visibility of APPs within Monument Health by ensuring that they are empowered, well-supported and equipped to deliver
high-quality, evidence-based care.
“As a lifelong learner and educator, I am committed to staying at the forefront of clinical practice and sharing that knowledge with students, colleagues and interdisciplinary team members,” she said.
“I find purpose in mentoring, fostering interdisciplinary collaboration, and shaping a culture that prioritizes clinical excellence and provider well-being. I wake up and am eager to arrive at work to care for the people of the Black Hills, because I love what I do.”
Christine said she feels privileged to work with the dedicated and highly skilled team in Lead-Deadwood because of their commitment to excellence, teamwork and mutual respect. “I greatly value my role as director and look forward to the continued growth and future opportunities for APPs at Monument Health.”
Outside of work, Christine enjoys strength training, biking, canvas painting, baking, hunting, fishing and spending quality time with her family. Taking time to recharge through these activities helps her stay grounded, focused and effective in her job.
PROVIDING COMPREHENSIVE CARE
Advanced Practice
Providers (APPs) play a vital role in your health journey as essential members of your comprehensive care team. Serving as physician assistants (PAs), nurse practitioners (NPs) or Certified Registered Nurse Anesthetists (CRNAs) these highly skilled professionals work closely with physicians to ensure you receive seamless, personalized care. APPs serve in a number of roles within a health care system and enhance the patient experience by broadening the scope of your health care team. This means you can expect APPs to assess, diagnose, and treat illnesses and injuries, prescribe medications, order and interpret tests and formulate treatment plans while working closely with physicians to provide coordinated care. APPs contribute to a diverse and wellrounded care team, often specializing in areas like family medicine, surgery, oncology, cardiology, emergency medicine and more.
CRYSTAL WATTERS
CODER II, HEALTH INFORMATION MANAGEMENT

Behind every medical procedure is a complex coding process. Crystal Watters’ expertise ensures accurate documentation that helps patients and providers navigate insurance requirements.
Story by Kory Lanphear
Photo by Kevin Eilbeck
When you are treated at a hospital, you are probably not thinking much about how the costs of your care are tracked. However, your arrival triggers a complicated process in which every treatment you receive, every medication you are given, is notated by nurses and physicians and then must be transcribed into a numerical code that will be used for billing.
That’s where Crystal Watters, Coder II for Health Information Management, comes in.
“Each procedure and each diagnosis that a patient receives has a code that goes on the claim to the insurance company,” Crystal said. “Coding is about getting the correct information for patients to get their claims and services paid. A Coder puts what the physicians and providers do into a language that the insurance companies can understand.”
A 10-year veteran of Monument Health, Crystal codes for all of General Surgery and Trauma Surgery across the organization. She spends a lot of time interpreting and clarifying physician notes.
“Insurance things are hard enough as


Our Patient Financial Service Advocates are dedicated to supporting patients in navigating the financial aspects of their health care journey. From assisting with insurance claims to offering flexible payment options and financial assistance, we work to ensure patients have the resources and support they need to manage their health care expenses with confidence.
For more information scan the QR code:


“My providers are awesome. They’re so supportive of me, and they just help me learn and be a better coder. Their clinical brain and my coder brain don’t always say the same thing and in that case we work together to translate their words into a code that fits.”
CRYSTAL WATTERS
it is, so we want to input the correct information and get reimbursement for the organization. We don’t want to have that burden for our patients. We also need to be in federal compliance,” she said.
Crystal and her fellow Coders once relied on reference books to find the right codes. The books, which she called “big and cumbersome” are still in use today, though most coding is now done using software. “There's a lot in my head, but there’s a lot of things that you just can’t memorize. So we start with an electronic dictionary, where you put in the first few words of the procedure or diagnosis, then drill down to the most specific procedure or diagnosis.”
Originally from Iowa, Crystal moved to Spearfish from Wheatland, Wyoming, where she started out posting payments at a clinic while working as a dental assistant. She was ultimately approached about taking on the role of Billing and Coding Manager for the clinic. Unfamiliar with the duties of the job, she simply learned as she went. “When I moved here, I had been on that Coder path and that’s what I wanted to do,” she said.
In addition to her duties at Monument Health, Crystal is the President of the local chapter of American Academy of Professional Coders, an organization for fellow Coders to get education, share information and network. “I presented for the national conference in Orlando this year on bariatric surgery/obesity medicine, which is rapidly evolving with the growing impact of weight loss drugs,” Crystal said.
“My presentation was called ‘The Skinny on Bariatric Surgery and Medical Weight Loss Management.’ After that, somebody at the Obesity Medicine Association asked me to speak at their conference at the end of April at National Harbor in Washington, D.C. Looking at the speaker list and seeing Ph.D.s and M.D.s, was intimidating. Then I remembered that even though they are experts in their part of this, I’m an expert in my part. It was a really great experience.”
Crystal has since presented to the American Academy of Pediatrics and will present this November to the American Society for Metabolic and Bariatric Surgery in Louisville, Kentucky.
The thing Crystal likes most about her job is interacting with physicians and collaborating with them to clarify their documentation. “My providers are awesome. They're so supportive of me, and they just help me learn and be a better coder. Their clinical brain and my coder brain don’t always say the same thing and in that case we work together to translate their words into a code that fits.”
In her spare time, Crystal loves to go to indoor climbing gyms and attend concerts. Her favorite venue is Red Rocks in Colorado, where she’s seen artists like Nine Inch Nails, Tom Petty and Soundgarden.
Welcome our newest physicians
CARDIOTHORACIC & VASCULAR SURGERY

Tomasso Cambiaghi, m.d., is a fellowship-trained Cardiothoracic/Vascular Surgeon at Heart and Vascular Institute. Dr. Cambiaghi trained for a fellowship in Cardiothoracic Surgery at Houston Methodist Hospital and completed residency in Integrated Vascular Surgery at McGovern Medical School in Houston.
COLON & RECTAL SURGERY

Steven Donahue, m.d., is the first fellowship-trained colorectal surgeon to join Monument Health and the only one practicing in Rapid City. He practices with the Monument Health General Surgery group at Rapid City Hospital.
ENDOCRINOLOGY

Natasha Rayan, m.d., is a fellowshiptrained Endocrinologist at Rapid City Clinic, Flormann Street. Dr. Rayan trained for an Endocrinology, Diabetes and Metabolism Fellowship at Ohio State University Wexner Medical Center in Columbus.
FAMILY MEDICINE

Max Bunchek, m.d., faccws, is a Family Medicine Physician at Flormann Clinic in Rapid City. A Fellow of American College of Clinical Wound Specialists, Dr. Bunchek completed Residency at Medical College of Wisconsin via Wisconsin Northern & Central Graduate Medical Education through the Fox Valley Family Medicine Residency Program in Appleton, WI.

Thomas L. Heaton, d.o., is a Family Medicine Physician at Flormann Clinic in Rapid City. A graduate of Monument Health Rapid City Hospital Family Medicine Residency.

Joshua Larson, m.d., is a board-certified Family Medicine Physician at the new Box Elder Clinic. Dr. Larson completed his residency at Lincoln Family Medicine Residency Program in Lincoln, NE.


Gaddiel Rios, m.d., is a Family Medicine Physician at the new MED360 by Monument Health Clinic in Rapid City.
Jeffrey Stephens, m.d., ph.d, is a Family Medicine Physician joining seven other family medicine physicians at Custer Clinic. He completed his residency through Wray Rural Training Track with North Colorado Family Medicine.

Blake Wadsworth, d.o., is a Family Medicine Physician at the new Rapid Valley Clinic. Dr. Wadsworth completed his residency at the Rapid City Hospital Family Medicine Residency Program.
GASTROENTEROLOGY

Emuejevoke Okoh, m.d., is a fellowshiptrained Interventional Gastroenterologist at Rapid City Hospital. Dr. Okoh trained for an Advanced Endoscopy Fellowship at the University of Texas Health Science Center of San Antonio, and a Gastroenterology Fellowship at Brooke Army Medical Center at Fort Sam Houston in Texas.
GYNECOLOGIC ONCOLOGY

Keely Ulmer, m.d., is a fellowship-trained Gynecologic Oncologist at the Cancer Care Institute in Rapid City Hospital. In addition to being a Gynecologic Oncology fellow, Dr. Ulmer was also Administrative Chief Resident and a Resident Physician in Obstetrics & Gynecology at University of Iowa Hospitals and Clinics in Iowa City.
HOSPITAL MEDICINE

Tyler Maxey, d.o., is a Hospitalist at Rapid City Hospital. Dr. Maxey completed his residency in Internal Medicine at the University of Missouri Health Care in Columbia, MO.


Gurpreet Singh, m.d., is a Hospitalist at Rapid City Hospital. Dr. Singh completed his residency in Internal Medicine at Jamaica Hospital Medical Centre in Queens, NY.
Amanda Sturgill d.o., is a Pediatric Hospitalist at Rapid City Hospital Children’s. She completed her residency in pediatrics at HCA Florida Palms West Pediatric Residency.
INTERNAL MEDICINE, OUTPATIENT

Kathyayini Tappeta, m.d., is an Internal Medicine Physician at Rapid City Clinic, Flormann Street. Dr. Tappeta completed her residency at Florida Atlantic University in Boca Raton, FL.
NEUROLOGY

Alireza Shirizian, m.d., is a Neurologist at Neurology and Rehabilitation in Rapid City. Dr. Shirizian completed his fellowship at the University of Chicago.
OBSTETRICS & GYNECOLOGY

Michael Growney, m.d., is a fellowship trained OB/GYN at Spearfish Clinic, North Avenue. Dr. Growney spent 17 years practicing as an OB/GYN at Women’s Health Center in Pueblo, CO where he was the President and Chief of Staff.
ORTHOPEDIC SURGERY - SPEARFISH

Jake Enos, m d., is a fellowship-trained Orthopedic Surgeon in Spearfish. Dr. Enos completed his fellowship at the University of Wisconsin Hospitals and Clinics in Madison, WI.
PSYCHIATRY

Chaston Ellis, d.o., is Psychiatrist at the Behavioral Health Center in Rapid City. Dr. Ellis completed his residency at the University of Utah School of Medicine in Pocatello, ID.
PULMONARY & CRITICAL CARE

Bryton E. Perman, m.d., is a fellowshiptrained Internist in Pulmonary Critical Care at Rapid City Hospital. Dr. Perman trained for a Pulmonary and Critical Care Medicine Fellowship at University of Missouri School of Medicine in Columbia.

Daniel O. Pfeifle, m d., is a fellowshiptrained Internist in Pulmonary Critical Care at Rapid City Hospital. Dr. Pfeifle trained for a Pulmonary/Critical Care Medicine Fellowship at Indiana University School of Medicine, Indianapolis.

Anuj Shivalingaiah, m.d., is a fellowship-trained Intensivist in Pulmonary Critical Care at Rapid City Hospital. Dr. Shivalingaiah trained for Fellowship in Pulmonary and Critical Care Medicine at The Brooklyn Hospital Center in New York City.
SLEEP MEDICINE & NEUROLOGY

Mohamadmostafa Jahansouz, m.d., dabph, is a fellowship-trained Neurologist and Sleep Medicine Physician at Monument Health Neuroscience Center in Rapid City. Dr. Jahansouz completed a two year postdoctoral research fellowship in neurology at Harvard Medical School, followed by a neurology residency at Tulane University School of Medicine in New Orleans.
We’re near you
ASSISTED LIVING
Monument Health
Assisted Living
432 North 10th Street Custer, SD 57730
605-673-5588
AUDIOLOGY
Monument Health
Rapid City Clinic 4150 5th Street Rapid City, SD 57701
605-755-5700
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
BARIATRICS
Monument Health
Bariatric and Metabolic Institute
1445 North Avenue Spearfish, SD 57783
605-644-4170
Monument Health
Bariatric and Metabolic Institute
353 Fairmont Boulevard Rapid City, SD 57701
605-755-5700
BEHAVIORAL HEALTH
Monument Health
Behavioral Health Center 915 Mountain View Road Rapid City, SD 57702
605-755-7200
Monument Health Family Medicine
Residency Clinic 502 East Monroe Street Rapid City, SD 57701
605-755-4060
Monument Health
Lead-Deadwood Clinic 71 Charles Street Deadwood, SD 57732
605-717-6431
Monument Health Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
Monument Health
Sturgis Clinic
2140 Junction Avenue Sturgis, SD 57785
605-720-2600
CANCER CARE
Monument Health Cancer Care Institute 353 Fairmont Boulevard Rapid City, SD 57701
605-755-2300
CARE CENTER
Monument Health Sturgis Care Center 949 Harmon Street Sturgis, SD 57785
605-720-2400
DIABETES
Monument Health Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
DIALYSIS
Monument Health Dialysis Center 425 N Cambell Street, Suite 200 Rapid City, SD 57701
605-755-6950
Monument Health Dialysis Center
132 Yankee Street Spearfish, SD 57783
605-722-8110
DERMATOLOGY
Monument Health Gillette Clinic
620 W Four-J Court
Gillette, WY 82716
307-682-1204
Monument Health
Rapid City Clinic 4150 5th Street
Rapid City, SD 57701
605-755-5700
Monument Health
Dermatology
550 East Colorado Boulevard Spearfish, SD 57783
605-717-8860
EAR, NOSE & THROAT
Monument Health
Rapid City Clinic 4150 5th Street
Rapid City, SD 57701
605-755-5700
Monument Health
Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
ENDOCRINOLOGY
Monument Health
Rapid City Clinic
640 Flormann Street
Rapid City, SD 57701
605-755-3300
GASTROENTEROLOGY
Monument Health
Rapid City Hospital
353 Fairmont Boulevard Rapid City, SD 57701
605-755-5700
GENERAL SURGERY
Monument Health
Rapid City Hospital
353 Fairmont Boulevard Rapid City, SD 57701
605-755-1000
Monument Health
Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
HEART & VASCULAR
Monument Health Gillette Clinic
620 W Four-J Court Gillette, WY 82716
307-682-1204
Monument Health Heart and Vascular Institute
353 Fairmont Boulevard Rapid City, SD 57701
605-755-4300
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
HOSPITALS
Monument Health Custer Hospital 1220 Montgomery Street Custer, SD 57730
605-673-9400
Monument Health
Lead-Deadwood Hospital 61 Charles Street Deadwood, SD 57732
605-717-6000
Monument Health
Rapid City Hospital
353 Fairmont Boulevard
Rapid City, SD 57701
605-755-1000
Monument Health Spearfish Hospital 1440 N Main Street Spearfish, SD 57783
605-644-4000
Monument Health
Sturgis Hospital
2140 Junction Avenue Sturgis, SD 57785
605-720-2400
HOME MEDICAL EQUIPMENT STORES
Monument Health Home+
Home Medical Equipment 1635 Caregiver Circle Rapid City, SD 57702
605-755-6150
Monument Health Home+
Home Medical Equipment 1800 N Haines Avenue Rapid City, SD 57701
605-755-9000
Monument Health Home+
Home Medical Equipment
911 East Colorado Boulevard Spearfish, SD 57783
605-717-8930
HOSPICE CARE
Monument Health Home+
Home Health & Hospice
224 Elk Street Rapid City, SD 57701
605-755-7710
Monument Health Home+
Home Health & Hospice 931 East Colorado Boulevard Spearfish, SD 57783
605-644-4444
Monument Health Home+
Hospice House 224 Elk Street Rapid City, SD 57701
605-755-7710
IMAGING SERVICES
Monument Health Rapid City Clinic 640 Flormann Street Rapid City, SD 57701 605-755-3300
Monument Health Custer Hospital 1220 Montgomery Street Custer, SD 57730 605-673-9400
Monument Health
Lead-Deadwood Hospital 61 Charles Street Deadwood, SD 57732 605-717-6000
Monument Health
Rapid City Hospital 353 Fairmont Boulevard Rapid City, SD 57701 605-755-1000
Monument Health Spearfish Hospital 1440 N Main Street Spearfish, SD 57783
605-644-4000
Monument Health Sturgis Hospital 2140 Junction Avenue Sturgis, SD 57785 605-720-2400
Monument Health
Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
Monument Health
Orthopedic & Specialty Hospital 1635 Caregiver Circle Rapid City, SD 57702 605-755-6100
Monument Health
Orthopedic and Sports Medicine 2479 East Colorado Boulevard Spearfish, SD 57783
605-644-4460
INFECTIOUS DISEASE
Monument Health
Rapid City Clinic
640 Flormann Street
Rapid City, SD 57701
605-755-3300
INFUSION SERVICES
Monument Health Infusion Services
2880 5th Street
Rapid City, SD 57701 605-755-7700
LAB SERVICES
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701 605-755-3300
Monument Health
Custer Hospital 1220 Montgomery Street Custer, SD 57730 605-673-9400
Monument Health
Lead-Deadwood Hospital
61 Charles Street Deadwood, SD 57732
605-717-6000
Monument Health
Rapid City Hospital
353 Fairmont Boulevard Rapid City, SD 57701
605-755-1000
Monument Health
Spearfish Hospital 1440 N Main Street Spearfish, SD 57783
605-644-4000
Monument Health
Sturgis Hospital
2140 Junction Avenue Sturgis, SD 57785
605-720-2400
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
LIFESTYLE MEDICINE
Monument Health
Rapid City Clinic
640 Flormann Street Rapid City, SD 57701
605-755-3300
NEPHROLOGY
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
NEUROLOGY
Monument Health
Neuroscience Center
677 Cathedral Drive Rapid City, SD 57701
605-755-5000
NEUROPSYCHOLOGY
Monument Health
Neuroscience Center 677 Cathedral Drive Rapid City, SD 57701
605-755-5000
NEUROSURGERY
Monument Health
Neuroscience Center
677 Cathedral Drive Rapid City, SD 57701
605-755-5000
OB/GYN
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
OCCUPATIONAL MEDICINE
Monument Health
Box Elder Clinic
375 Berky Drive Box Elder, SD 57719
605-755-2273
Monument Health
Rapid City Clinic, Mount Rushmore Road
6015 Mount Rushmore Road Rapid City, SD 57701
605-755-2273
Monument Health Rapid Valley Clinic
2526 Elderberry Boulevard Rapid City, SD 57703
605-755-2273
Monument Health
Rapid City Urgent Care
1303 N Lacrosse Street Rapid City, SD 57701
605-755-2273
Monument Health
Rapid City Urgent Care 2116 Jackson Boulevard Rapid City, SD 57702
605-755-2273
ORTHOPEDICS
Monument Health Gillette Clinic 620 W Four-J Court Gillette, WY 82716
307-682-1204
Monument Health
Orthopedic & Specialty Hospital 1635 Caregiver Circle Rapid City, SD 57702
605-755-6100
Monument Health
Orthopedic and Sports Medicine 2479 East Colorado Boulevard Spearfish, SD 57783
605-644-4460
PHARMACIES
Monument Health Home+ Pharmacy
353 Fairmont Boulevard Rapid City, SD 57701
605-755-8184
Monument Health Home+
Pharmacy 1420 North 10th Street, Suite 1 Spearfish, SD 57783
605-717-8741
Monument Health Home+ Specialty Pharmacy
725 Meade St. Rapid City, SD 57701
605-755-3065
PLASTIC SURGERY
Monument Health Rapid City Clinic 4150 5th Street Rapid City, SD 57701
605-755-5700
PODIATRY
Monument Health
Orthopedic & Specialty Hospital 1635 Caregiver Circle Rapid City, SD 57702
605-755-6100
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
PRIMARY CARE CLINICS
Monument Health Belle Fourche Clinic 2200 13th Avenue Belle Fourche, SD 57717
605-723-8970
Monument Health Box Elder Clinic 375 Berky Drive Box Elder, SD 57719
605-755-2273
Monument Health Buffalo Clinic
209 Ramsland Street Buffalo, SD 57720
605-375-3744
Monument Health
Custer Clinic 1220 Montgomery Street Custer, SD 57730
605-673-9400
Monument Health
Family Medicine
Residency Clinic 502 East Monroe Street Rapid City, SD 57701
605-755-4060
Monument Health Hill City Clinic
238 Elm Street Hill City, SD 57745
605-574-4470
Monument Health
Hot Springs Clinic 1100 Highway 71 South, Suite 101
Hot Springs, SD 57747
605-745-8050
Monument Health
Lead-Deadwood Clinic 71 Charles Street Deadwood, SD 57732
605-717-6431
Monument Health
Rapid City Clinic
640 Flormann Street Rapid City, SD 57701
605-755-3300
Monument Health
Rapid Valley Clinic 2526 Elderberry Boulevard Rapid City, SD 57703
605-755-2273
Monument Health
Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
Monument Health
Sturgis Clinic 2140 Junction Avenue Sturgis, SD 57785
605-720-2600
Monument Health
Wall Clinic 112 7th Avenue Wall, SD 57790
605-279-2149
PULMONOLOGY
Monument Health
Rapid City Clinic
640 Flormann Street Rapid City, SD 57701
605-755-3300
RHEUMATOLOGY
Monument Health
Rapid City Clinic
640 Flormann Street Rapid City, SD 57701
605-755-3300
SAME-DAY APPOINTMENTS
Monument Health
Custer Clinic
1220 Montgomery Street Custer, SD 57730
605-673-9400
Monument Health
Lead-Deadwood Clinic 71 Charles Street Deadwood, SD 57732
605-717-6431
Monument Health
Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
Monument Health Sturgis Clinic 2140 Junction Avenue
Sturgis, SD 57785
605-720-2600
SLEEP CENTERS
Monument Health
Rapid City Clinic 2929 5th Street
Rapid City, SD 57701
605-755-4000
Monument Health
Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
SURGERY CENTERS
Same Day Surgery Center 651 Cathedral Drive Rapid City, SD 57701
Monument Health
Surgery Center 1316 North 10th Street Spearfish, SD 57783
605-642-3113
THERAPIES –PT, OT, SPEECH
Monument Health
Inpatient Rehabilitation Center
1050 Fairmont Boulevard, Suite A100 Rapid City, SD 57701
605-755-1230
Monument Health
Rehabilitation 2200 13th Avenue Belle Fourche, SD 57717
605-723-8961
Monument Health
Rehabilitation 1220 Montgomery Street Custer, SD 57730
605-673-9400
Monument Health
Rehabilitation 61 Charles Street Deadwood, SD 57732
605-717-6000
Monument Health
Rehabilitation 2140 Junction Avenue Sturgis, SD 57785 605-720-2400
Monument Health
Rehabilitation 2449 East Colorado Boulevard Spearfish, SD 57783
605-644-4370
Monument Health
Orthopedic & Specialty Hospital 1635 Caregiver Circle
Rapid City, SD 57701 605-755-6100
TRAVEL MEDICINE
Monument Health
Rapid City Clinic 640 Flormann Street
Rapid City, SD 57701 605-755-3300
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783 605-717-8595
URGENT CARE CLINICS
Monument Health Box Elder Urgent Care 375 Berky Drive Box Elder, SD 57719 605-755-2273
Monument Health
Rapid City Urgent Care 1303 N Lacrosse Street Rapid City, SD 57701 605-755-2273
Monument Health
Rapid City Urgent Care 2116 Jackson Boulevard Rapid City, SD 57702 605-755-2273
Monument Health
Rapid Valley Urgent Care 2526 Elderberry Boulevard
Rapid City, SD 57703
605-755-2273
Monument Health
Sturgis Urgent Care Services
2140 Junction Avenue Sturgis, SD 57785
605-720-2600
UROLOGY
Monument Health
Rapid City Clinic
2805 5th Street
Rapid City, SD 57701
605-755-5700
WOUND & OSTOMY CARE
Monument Health
Rapid City Clinic
2929 5th Street
Rapid City, SD 57701
605-755-1309
Monument Health
Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
ISSUE 19, FALL 2025 // RESILIENCE
11. Rayana Shoberg accepted a position as what type of assistant for the Heart and Vascular Institute?
12. Alexandra Brown wants to start a ___________ that can help feed her community.
DOWN
2. Brady Thompson said “I like sweets now.” He thinks his heart donor might have had a __________ __________!
3. In which department does Christine Duerksen, APP, work at the LeadDeadwood Hospital and Clinic?
4. The condition that Brady Thompson was born with is called ___________________ left heart syndrome (HLHS).
7. Bariatric surgery is a ______________ commitment.
8. Jennifer Knowles, NFP-BC, is bringing awareness about Cancer Genetics and ___________ at the Cancer Care Institute.
10. A __________, like Crystal Watters, puts what the physicians and providers do into a language that the insurance companies understand.
ACROSS
1. To pay tribute to the memory of the late Peggy Lee Bowser, the Home+ Hospice House put a ___________ _______ on the Memorial Tree.
5. What summit did Commissioner Ron Rossknecht hike?
6. In which North Dakota city do Mark, Victoria and Wyatt Trout live?
9. How many family members in the Stover family work throughout Monument Health?


+ Botox Cosmetic Injections
+ Chemical Peels - Skin Resurfacing
+ CoolSculpting
+ Dermabrasion
+ Facial Fillers
For more information, visit monument.health/plasticsurgery
HUNTER R. MOYER, M.D.
OLGA SCHUTH, M.D. Plastic Surgery
MONUMENT HEALTH
PLASTIC SURGERY
4150 5th Street | Rapid City 605-755-6000

