
A Guide to Pregnancy
CONGRATULATIONS ON YOUR PREGNANCY



CONGRATULATIONS ON YOUR PREGNANCY

We appreciate that you have chosen us to share this exciting time.
Pregnancy is a very unique time in life, as you and your body will go through incredible changes with the growth of your baby. Every woman experiences pregnancy differently, so there is no “right” or “wrong” way to feel. We have compiled some information in this booklet that may be quite helpful to you. Please take time to read it and write down questions or concerns that we can discuss during your prenatal visits. The more information and support you have, the more you will be able to enjoy your pregnancy. Please do not hesitate to call if you have concerns between your scheduled office visits. We are here to help make your pregnancy as special as it can be!
Our office has obstetricians and nurse practitioners to care for you during your pregnancy and delivery. There is an obstetrician on call 24-hours a day, seven days a week. In the event that your obstetrician is not available at the time of delivery the “on call” obstetrician will be happy to assist in the delivery.
SPEARFISH WOMEN’S AND CHILDREN’S PROVIDERS







The day your baby is due is called the “estimated date of delivery,” or EDD. It is estimated on the fact that a normal pregnancy lasts about 280 days (or 40 weeks), counting from the first day of your last menstrual period. A normal range, however, is from as few as 259 days to as many as 294 days (37–42 weeks). Most women will go into labor 2 weeks before or after their EDD and only about 1 in 20 women will give birth on their exact due date. Your EDD is useful in tracking your baby's growth and your pregnancy's progress.
The 40 weeks of pregnancy are divided into three trimesters. These last about 12–13 weeks each (or about 3 months):
0-12 weeks (month 1-3)
13-27 weeks (month 4-6)
28-40 weeks (month 7-9)
First Visit Your first visit is usually scheduled 8 weeks from the first day of your last menstrual period. We will do a thorough review of your history and perform a physical exam. We will also perform a vaginal ultrasound to confirm your pregnancy dating and give you an accurate due date. We will draw a set of routine prenatal labs that includes your blood type, a complete blood count, as well as HIV, Hep B, syphilis and rubella screening.
16 weeks Your routine prenatal visits will include weight, blood pressure, urine testing and listening to your baby’s heartbeat. We will see you monthly until 28 weeks, then every 2 weeks until 36 weeks, and weekly until delivery. At these routine visits we will be obtaining additional screening as listed below.
16 weeks Prenatal visit and optional quad screen.
20 weeks Prenatal visit and ultrasound to evaluate your baby’s anatomy and growth.
25-28 weeks Prenatal visit and gestational diabetes screen. We will also check a blood count and perform an antibody screen to administer Rhogam if you are Rh negative.
30-36 weeks Prenatal visits increase to 2 weeks. We will perform a vaginal swab to test for Group B Strep at your 36 week visit.
36-40 weeks Prenatal visits increase to weekly.We will often check your cervix to evaluate cervical dilation.
40-42 weeks As long as you and your baby are doing well, we will continue your pregnancy 7-10 days beyond your due date. During this time period we may do additional testing (nonstress tests and ultrasounds to check amniotic fluid levels) to ensure that your baby is doing well. An induction of labor is usually scheduled between 41 and 42 weeks. This may vary depending on your cervical exam and personal history.
During pregnancy, you will have a blood test to find out your blood type (A, B, AB, O) and whether or not your blood has the Rhesus factor, or Rh factor. If your blood does have the factor, then it is Rh-positive and if it doesn’t, then your blood is Rh-negative.
When Does the Rh Factor Cause Problems?
The Rh factor causes problems when an Rh–negative mother’s blood comes in contact with a fetus’ Rh–positive blood. If this happens, the mother’s Rh–negative blood may produce antibodies that fight the Rh factor as if it were a harmful substance. During pregnancy, the woman and fetus do not share blood systems. However, a small amount of blood from the fetus can cross the placenta into the woman’s system. When this happens, a small number of pregnant women with Rh–negative blood who carry an Rh–positive fetus will react as if they were allergic to the fetus. These Rh–negative women make antibodies that attack the blood of the Rh–positive fetus. This causes anemia, which can lead to a serious illness, brain damage or even death of the fetus or newborn.

A woman can produce antibodies any time the Rh–positive blood mixes with her blood, during:
• A miscarriage
• An induced abortion
• An ectopic pregnancy
• A blood transfusion
• Amniocentesis
How Can Problems With the Rh Factor Be Prevented?
• Chorionic villus sampling (CVS)
• Bleeding during pregnancy
Anemia can be prevented in the fetus if the Rh–negative woman has not yet made antibodies against the Rh factor. A simple blood test, can show if an Rh-negative woman has developed antibodies to Rh-positive blood. Rh immunoglobulin (RhIg, or Rhogam) is a blood product that can prevent an Rh–negative mother from responding to Rh–positive blood cells of the fetus when injected into one of the mother’s muscles. RhIg is not helpful if the mother has already made antibodies. RhIg is given around the 28th week of pregnancy and after delivery if the fetus is Rh-positive. Each pregnancy and delivery of an Rh–positive child requires repeat doses of RhIg.
Chromosomal defects (aneuploidy) are present in 1 in 150 live births, but the prevalence is much higher in early pregnancies because aneuploidy is the cause of many early pregnancy losses. Screening tests are easy to perform and DO NOT pose any risk to your fetus.
Quad Screen
• Most commonly recommended test at 16-22 weeks to detect an individual at risk of carrying a fetus with Down Syndrome, Trisomy 18 or a Neural Tube Defect
• Measures four different substances in your body – alpha-fetoprotein (AFP), estriol, human chorionic gonadotropin (HCG), and inhibin-A
• Detects Down Syndrome in 81% of the cases
• Detects 80% of neural tube defects
Cell-free DNA
• Best for women at high risk of aneuploidy (advanced maternal age, history of previous aneuploidy fetus, presence of fetal anomalies on ultrasound)
• Can be completed as early as 10 weeks into your pregnancy
• Evaluates small segments of DNA on fetal cells that have been released into maternal circulation
• Detects 99% of Down Syndrome fetuses and can also detect Trisomy 18, 13 and sex chromosome abnormalities

Carrier screening helps to identify reproductive couples at risk of having a baby with a specific genetic abnormality. Carrier screening is genetic testing performed on individuals who DO NOT display overt disease characteristics, but could have one variant allele in a gene that is only problematic if the reproductive partner also carries a variant allele. This testing is most beneficial if it is done prior to conception, but it is still very informative if it is done at any time during a pregnancy. Carrier screening only needs to be done ONCE in a person’s lifetime.
We currently recommend screening for Spinal Muscular Atrophy (SMA), Cystic Fibrosis (CF), and Fragile-X. If your screening is positive, then we will refer you to a genetic counselor and discuss prenatal diagnostic testing. Please let us know if you have any specific concerns due to your family history.
Spinal Muscular Atrophy
SMA is a disease of the spinal cord that leads to skeletal muscle atrophy and weakness. It is the leading cause of death in infants. Approximately 1 in 40-60 individuals are carriers of this mutation, and approximately 1 in 6,000-10,000 live births are affected by this condition. SMA is an autosomal recessive disease with complex genetics. If both parents are carriers of the mutation, it still may be difficult for a geneticist to predict the exact severity of disease in the unborn fetus.
Cystic Fibrosis
CF is a progressive multisystem disease that primarily affects the pulmonary, pancreatic and gastrointestinal systems. Approximately 1 in 2,500 individuals are affected by CF. The average life expectancy of an individual with CF is 42 years. CF is an autosomal recessive condition, so both parents would have to carry a mutation in order for an infant to have CF. To date there have been more than 1700 mutations detected, but carrier screening only tests for the most common mutations. If you have a family history of CF, then you may need DNA sequencing for the specific familial mutation.
Fragile X is the most common inherited form of intellectual disability and affects approximately 25% of individuals with autism or autism spectrum behaviors. Fragile X is an X-linked disorder with complex genetics, but only one reproductive partner needs to be a carrier to have an affected infant. Carrier screening detects individuals who may have a Fragile-X permutation. The permutation can become a full mutation through the normal process of egg/sperm/embryo development. Other times the offspring of an individual with a permutation will have infertility of Fragile-X associated ataxia/tremor syndrome.

The First Month (1-5 weeks): ½ inch, less than 1 ounce
• The fertilized egg attaches to the lining of the uterus. Some of these cells will grow into a baby. Other cells will form the placenta.
• Arms and legs begin to form.
• The brain and spinal cord begin to form.
• The heart and lungs begin to develop. The heart begins to beat near the end of this month.
The Second Month (6-10 weeks): 1 inch, less than 1 ounce
• Eyelids form, but remain closed.
• The inner ear begins to develop.
• Bones appear.
• Ankles, wrists, fingers and toes form.
• The genitals begin to develop.
• By the end of the month, all major organs and body systems have begun to develop.
The Third Month (11-14 weeks): 3½ inches, just more than 1 ounce
• Twenty buds for future teeth appear.
• All internal parts are formed, but are not fully developed.
• Fingers and toes continue to grow. Soft nails begin to form.
• Bones and muscles begin to grow.
• The intestines begin to form.
• The backbone is soft and can flex.
• The skin is almost transparent.
• The hands are more developed than the feet.
• The arms are longer than the legs.
The Fourth Month (15-18 weeks): 6–7 inches, 5 ounces
• Eyebrows, eyelashes and fingernails form.
• Arms and legs can flex.
• External sex organs are formed.
• Skin is wrinkled; the body is covered with a waxy coating (vernix) and fine hair (lanugo).
• The placenta is fully formed.
• The outer ear begins to develop.
• The fetus can swallow and hear.
• The neck is formed.
• Kidneys are functioning and begin to produce urine.
The Fifth Month (19-22 weeks): 10 inches, ½–1 pound
• The sucking reflex develops. If the hand floats to the mouth, the fetus may suck his or her thumb.
• He or she is more active. You may be able to feel him or her move.
• The fetus sleeps and wakes regularly.
• Nails grow to the tips of the fingers.
• Gallbladder begins producing bile, which is needed to digest nutrients.
• In girls, the eggs have formed in the ovaries.
• In boys, the testicles begin to descend from the abdomen into the scrotum.
The Sixth Month (23-26 weeks): 12 inches, 1–1½ pounds
• Real hair begins to grow.
• The brain is rapidly developing.
• The eyes begin to open.
• Finger and toe prints can be seen.
• The lungs are fully formed, but not fully mature.
The Seventh Month (27-30 weeks): 14 inches, 2–2 1/2 pounds
• The eyes can open and close and sense changes in light.
• Lanugo begins to disappear.
• The fetus kicks and stretches.
• The fetus can make grasping motions and responds to sound.
The Eighth Month (31-34 weeks): 18 inches, 5 pounds
• With major development complete, the fetus gains weight very quickly.
• Bones harden, but the skull remains soft and flexible for delivery.
• The different regions of the brain are forming.
• Taste buds develop and the fetus can taste sweet and sour.
• The fetus may now hiccup.
The Ninth Month (35-40 weeks): 20 inches, 6–9 pounds
• The fetus usually turns into a head-down position for birth.
• The skin is less wrinkled.
• The lungs mature and are ready to function on their own.
• Sleeping patterns develop.
• The fetus will gain about 1/2 pound per week this month.
The First Trimester
• Your period stops.
• Your breasts may become larger and more tender.
• Your nipples may stick out more.
• You may need to urinate more often.
• You may feel very tired.
• You may feel nauseated and even vomit.
• You may crave certain foods or lose your appetite.
• You may have heartburn or indigestion.
• You may be constipated.
• You may gain or lose a few pounds.
The Second Trimester
• Your appetite increases and nausea and fatigue may ease.
• Your abdomen begins to expand. By the end of this trimester, the top of your uterus will be near your rib cage.
• The skin on your abdomen and breasts stretches and may feel tight and itchy. You may see stretch marks.
• Your abdomen may ache on one side or the other, as the ligaments that support your uterus are stretched.
• A dark line, the linea nigra, may appear down the middle of your stomach from your navel to your pubic hair.
• You may get brown patches (chloasma, or the “mask of pregnancy”) on your face.
• Your areolas, the darker skin around your nipples, may darken.
• Your feet and ankles may swell.
• You may feel your uterus in your lower abdomen.
The Third Trimester
• You can feel the baby's movements strongly.
• You may be short of breath.
• You need to urinate more often as the baby drops and puts extra pressure on your bladder.
• Colostrum – a yellow, watery pre–milk – may leak from your nipples.
• Your navel may stick out.
• You may have contractions (abdominal tightening or pain). These can signal false or real labor.

Every diet should include proteins, carbohydrates, vitamins, minerals and fat. You should try to eat a variety of foods from all the basic food groups. If you do, chances are good that you and your baby are getting the right amounts of nutrients. However, during pregnancy, it is recommended that you consume higher amounts of the nutrients listed in the table below. Thus, we recommend a daily prenatal vitamin.
It is also important to be mindful of how much you eat. If you are a normal weight before pregnancy, you need only an average of 300 extra calories per day to fuel your baby's growth and keep you healthy during pregnancy — the amount in a glass of skim milk and half a sandwich. During your third trimester you will need about 400 extra calories per day.
Nutrient (Dietary Reference Intake (DRI) for pregnant women)
Calcium (1,000 milligrams)
Iron (27 milligrams)
Vitamin A (770 milligrams)
Vitamin C (85 milligrams)
Vitamin D (200 international units; some experts recommend 400 IU during pregnancy)
Vitamin B6 (1.9 milligrams)
Why You and Your Baby Need It
Helps build strong bones and teeth
Helps your red blood cells deliver oxygen to your baby.
Forms healthy skin and helps eyesight. Helps with bone growth.
Promotes health gums, teeth and bones. Helps your body absorb iron.
Helps build your baby’s bones and teeth.
Helps form red blood cells. Helps body use protein, fat and carbohydrates.
Vitamin B12 (2.6 micrograms) Maintains nervous system. Needed to form red blood cells.
Folate (400 micrograms)
Needed to produce blood and protein. Helps some enzymes function. Reduces the risk of neural tube defects.
Best Sources
Milk, cheese, yogurt, sardines
Lean red meat, dried beans and peas, iron-fortified cereals, prune juice
Carrots; dark, leafy greens; sweet potatoes
Citrus fruit, broccoli, tomatoes, strawberries
Sunlight exposure; vitamin D fortified milk, fatty fish such as salmon
Beef, liver, pork, ham, whole-grain cereals, bananas
Liver, meat, fish, poultry, milk (found only in animal foods – vegetarians who do not eat any animal foods should take a supplement)
Green, leafy vegetables; liver; orange juice; legumes and nuts
It depends on your pre-pregnancy weight and measurement of your body mass index (see the table below). If you are obese or overweight, you are at an increased risk for several pregnancy-related problems. These problems include gestational diabetes, high blood pressure, preeclampsia, and cesarean delivery. Thus we recommend a modest weight gain if your BMI is greater than 30 and a modest weight loss if your BMI is 40 or greater. The weight loss should not be drastic, should be individualized for each woman, and should be done only under a health care provider's close supervision.

Can I continue my vegetarian diet?
Yes. Plan your meals with care to ensure you get the nutrients you and your baby need. Be sure you are getting enough protein. You will probably need to take supplements, especially iron, vitamin B12 and vitamin D.
Can I eat fish?
You should avoid eating shark, swordfish, king mackerel or tilefish during pregnancy because they contain high levels of mercury that can be harmful to your developing baby.
However, fish and shellfish are good sources of protein, omega-3 fatty acids and other nutrients in pregnancy. You can enjoy common types of fish that are low in mercury, such as shrimp, canned light tuna (not albacore, which has a higher mercury content), salmon, pollock and catfish. You can safely eat up to 12 ounces (about two meals) of these fish per week while you are pregnant.
What is Listeriosis and how do I avoid it?
Listeriosis is an illness caused by bacteria that can occur in unpasteurized milk and soft cheese and prepared and uncooked meats, poultry and shellfish. It can be particularly harmful to pregnant women and their babies.
To prevent listeriosis, wash all fresh fruits and vegetables before using them. While you are pregnant, do not eat the following foods:
• Unpasteurized milk or soft cheeses
• Raw or undercooked meat, poultry or shellfish
• Prepared meats, such as hot dogs or deli meats, unless they are heated until steaming hot
Always be sure to wash your hands and any utensils, countertops or cutting boards that have been in contact with uncooked meats.
Can I drink caffeine?
Moderate caffeine intake (200 milligrams a day—the amount in approximately two 8-ounce cups of brewed coffee) does not appear to lead to miscarriage or preterm birth. It is not clear whether caffeine increases the risk of having a low birth weight baby. It may be a good idea to limit your caffeine intake during pregnancy for other reasons. Excess caffeine can interfere with sleep and contribute to nausea and light-headedness. It also can increase urination and lead to dehydration.
We encourage you to be active during your pregnancy. Walking, jogging, yoga and swimming are all excellent ways to stay fit and healthy during this time. Try to avoid activities where you can fall and hit your abdomen, i.e. biking, water skiing, horseback riding, skiing/snowboarding, contact sports.
Old guidelines recommended keeping your heart rate below 140 beats/minute. This can be difficult to determine and isn’t accurate for everyone, so use these rules instead:
• Exercise to a level at which you can carry on a simple conversation
• Drink plenty of fluids
• Avoid hot and humid conditions
• Be aware of the warning signs:
- Vaginal bleeding
- Dizziness or feeling faint
- Increased shortness of breath
- Chest pain
- Headache
- Muscle weakness
- Calf pain or swelling
- Uterine contractions
- Decreased fetal movement
- Fluid leaking from the vagina
Your ability to exercise will likely change during pregnancy. Please let us know if you are in a rigorous training program currently.
Unless we advise you otherwise, it is safe and healthy for you to continue to work until you deliver. Please consider the guidelines below:
• Take frequent breaks
• Elevate legs periodically
• Empty your bladder every 2 hours
• Stop if you’re short of breath
• Get extra rest on the weekends
• Use caution around heavy equipment
• Wear support hose if you have swelling
AVOID …
• Exhaustion
• Extreme heat
• Smoking areas/ noxious odors and fumes
• Lifting or pushing more than 20lbs
• Climbing ladders
• Trauma to abdomen
• Prolonged standing or walking
Be around cats?
Avoid changing the kitty litter to decrease your risk of toxoplasmosis exposure, but you do not need to stay away from your cat during pregnancy.
Garden?
Please wear gloves while gardening as your yard is likely a litter box for the neighborhood.
Color my hair?
It is considered safe to color your hair during pregnancy.
Use a hot tub?
Avoid hot tub, steam rooms and other related activities that would consistently elevate your core body temperature. Taking a bath is safe because the water will cool down.
Get a massage?
Massages are an excellent way to relax and help with some of the aches and pains that accompany a normal pregnancy. Just ask your masseuse if he/she has experience with pregnancy massage prior to setting up your appointment. Enjoy!
Use mosquito repellant?
Continue to use as needed, DEET related products.
Have nail treatments?
Getting acrylic nails or other nail services is fine during pregnancy.
Have sexual relations?
Sexual relations, including intercourse, are considered safe during all stages of pregnancy unless we have instructed you otherwise. Spotting and cramping are common symptoms 24 hours after intercourse.
Use sunscreen?
Please continue to use sunscreen to protect yourself from skin damage.
Travel?
Car travel should be limited to 6 hours per day with 10 minute breaks to stretch your legs every 2 hours. Please be sure to ALWAYS wear your lap belt across your hipbones/under your abdomen and your shoulder belt snug between your breasts. Travel by airplane is considered safe until approximately 34 weeks. Be sure to wear your lap belt and ambulate hourly. International travel, cruises, etc are generally not recommended after the 2nd trimester (>24 weeks). While traveling, please keep in mind that if you or your baby’s health changes and need to receive medical care wherever you are, it may not be the same care you would receive with us. Also, remember that any travel plans may need to be changed or cancelled if the health of you or your baby changes and your doctor advises against it.
This is reported in 70% of pregnant patients and can be attributed to the laxity in your muscles, tendons and joints as well as the weight from your growing uterus. You can ease this discomfort by avoiding excessive weight gain, using proper lifting/bending techniques (use your legs/bend at the knees), wearing comfortable shoes (avoid high heels), using a heating pad on the low setting for short periods of time (don’t place directly on your abdomen), or trying a warm bath. You may also consider physical therapy, massage or chiropractic care.
Constipation
This is caused by a change in your hormones, the weight of your uterus and the iron in your prenatal vitamin. Constipation can be prevented by drinking plenty of water, being sure there is adequate roughage and fiber in your diet and staying active. You can also use Metamucil, Citrucel, FiberCon, and/or Colace. Magnesium at bedtime can also be helpful.
Heartburn
This is caused by the relaxation of muscles in your esophagus and the upward displacement and compression of your stomach from your growing uterus. Try eating small, frequent meals and avoid lying flat immediately after eating. You can use antacids and over the counter proton pump inhibitors such as Prilosec.
Hemorrhoids
These are swollen veins around your rectum that may itch or cause pain with bowel movements or sitting. They are caused by excessive straining during bowel movements and the compression of pelvic veins as your uterus grows. Also review the medication list for treatment of hemorrhoids on page 18.
Headaches
Headaches are common in pregnancy; you may try a combination of Extra Strength Tylenol with caffeine and 400mg of magnesium. Other remedies to try are cold packs or massage. If symptoms persist, contact your provider.
Insomnia
Sleeping may become difficult, especially in your later months. This is due to the hormonal alterations in your natural sleep cycles. You can try warm baths before bed, massage and relaxation techniques such as yoga or meditation. Another option is Magnesium 200-400mg at bedtime. It is also safe to take Benadryl or Tylenol PM.
“Morning Sickness”
Despite its name, morning sickness can occur at any time of day. It is usually experienced during the first trimester and improves in the second trimester. It may be helpful to eat 5-6 small, bland meals throughout the day. You can also try some of the medications listed in “Safe Medications During Pregnancy.” Occasionally you may need prescription strength medications.
Brown areas on your face and abdomen are normal. As are elevated red spots on your face, neck and arms. The palms of your hands may become red. These changes are a result of hormonal alterations and will fade (may not disappear) after the delivery of your baby.
These can occur on your breasts, hips and abdomen, and are often genetic. The marks are red or purplish initially and fade into silvery streaks after pregnancy, but will not fade away completely. There is nothing that can prevent stretch marks, however creams, cocoa butter and calamine lotion may relieve the irritation and burning associated with them.
The tendency to develop these is inherited. They are caused by the compression of the large veins in your legs from the weight of your growing uterus. This creates pressure in the veins and they may become dilated and painful. Elevating your legs whenever possible and wearing support hose can alleviate symptoms. Exercise can also be helpful.

Advil | Pepto-Bismol | Ibuprofen | Actifed | Motrin | Aleve
Follow the directions on the box and use only when needed.
Bug bites/rash/itch/cuts:
• Bacitracin
• Benadryl Cream or Spray
• Caladryl Lotion
• Hydrocortisone cream
• Neosporin
• Oatmeal Bath
• Polysoporin
Constipation:
• Citracel
• Docusate Sodium (Colace)
• Fibercon
• Metamucil
• Milk of Magnesia (MOM)
• Miralax
• Suppository or Enema
Diarrhea:
(Only use after 12 weeks of pregnancy for no more than 24 hours)
• Kaopectate
• Immodium AD
Gas:
• Gas-X
• Mylanta Gas
• Mylicon
Headaches and Aches/Pain:
• Acetaminophen (Tylenol)
• Magnesium 400mg
Heartburn/GI upset:
• Maalox
• Mylanta
• Omeprazole (Prilosec)
• Pepcid
• Rolaids
• Tums
Hemorrhoids:
• Anusol HC
• Preparation H
• Tucks Pads
Insomnia:
• Benadryl
• Melatonin
• Tylenol PM
• Unisom
Nausea:
• Acupuncture
• Ginger capsules 250mg every 6-8 hours
• Ginger extract powder 1 gram/day
• Sea Band
• Unisom/doxylamine 1/2 tablet at bedtime, if no improvement, add 1/2 tablet in the morning
• Vitamin B6 25-50mg every 8 hours
Nasal Congestion/ Cough/Cold/Allergies:
• Afrin Nasal Spray (use only 3 days)
• Chloraseptic Spray
• Diphenhydramine (Benadryl)
• Loratadine (Claritin)
• Mucinex
• Ocean Mist Nasal Spray
• Robitussin or Robitussin DM
• Sudafed (do not take if hypertensive)
• Triaminic DM
• Tylenol Cold
• Vicks Cough Syrup
Sore Throat:
• Cepacol
• Cepastat Lozenges
• Chloraseptic Spray
Yeast Infections:
• Clotrimazole
• Lotrimin
• Miconazole
• Monistat
Your physicians at Monument Health Spearfish Clinic, North Avenue can be reached 24 hours a day. During business hours please call our office at 605-644-4170. If you need assistance after hours, please call Labor & Delivery at 605-644-4048.
Pregnancy Warning Signs
• Decreased fetal movement (see section below on Fetal Kick Movements)
- Your baby should have an established pattern of daily activity starting around 28 weeks of gestation. During your baby’s normal active time you should be able to count fetal kick movements. This can be done by going to a quiet place in your home or office without distractions. Once you start to feel movements, start timing. You should feel four kicks, rolls, jabs, etc in one hour. Notify us immediately if you become concerned or aware of lack of movement during your baby’s usual active time.
• Any vaginal bleeding
• Leaking of fluid vaginally
• Fever >100.5, especially associated with abdominal pain
• Persistent and severe headache that is not relieved with Tylenol
• Blurred vision
• Sudden weight gain or loss
• Significant decrease in urine output
• Swelling or puffiness, especially in the hands, face and around the eyes
• Severe or sharp abdominal pain with or without nausea and vomiting

Differences Between False Labor and True Labor
Timing of Contractions
Change with movement
Strength of contractions
Often are irregular and do not get closer together (called Braxton Hicks contractions)
Contractions may stop when you walk or rest, or may even stop with a change of position
Usually weak and do not get much stronger (may be strong and then weaken)
Pain of contractions Usually felt only in the front
Come at regular intervals and, as time goes on, get closer together. Each lasts about 30-70 seconds.
Contractions continue, despite movement
Steadily increase in strength
Usually start in the back and move to the front


• Toiletries: toothbrush, toothpaste, shampoo, conditioner, body wash/soap, lotion, brush/comb, deodorant, etc. …
• Nursing bra and pads if nursing, or sports bra/support bra if not
• Going home outfit with comfy shoes (feet may be swollen)
• Camera
• Optional Items:
- Socks, slippers, robe, pajamas for post-partum
- Underwear 4-5 pairs (hospital supplies disposable mesh underwear)
- Pads if you prefer a specific brand (hospital will supply)
- Electronic devices with chargers
- Snacks for support partner
• Going home outfit
• Rear-facing car seat
• Optional Items:
- Bottles/formula if there is a certain brand you prefer and are bottle feeding. (The hospital will supply Similac pre-made bottles and nipples.)
- Diapers/wipes if you prefer a specific brand (hospital supplies Pampers)
- Baby wash and lotion (hospital supplies Johnson & Johnson)
- Receiving blankets/blankets
- Sleepers (hospital will provide infant gowns for stay)
Many women worry that receiving pain relief during labor will somehow make the experience less "natural." The fact is, no two labors are the same, and no two women have the same amount of pain. Some women need little or no pain relief, and others find that pain relief gives them better control over their labor and delivery.
Some methods you can try to ease the discomfort you may feel during labor:
• Utilitze the relaxation and breathing techniques taught in your childbirth class
• Have your pregnancy support person firmly press on your lower back
• Take a warm shower or bath, if safe for you and your baby
• Place an ice pack on your back
• Use a tennis ball for massage
• Rest in between contractions and take slow, deep breaths
• If you become warm or perspire, soothe yourself with cool, moist cloths
On the Labor and Delivery unit, we will also have a CRNA work with you to pick the best method of pain relief for you.
Systemic Analgesics
These are medications that can be given as an injection into a muscle or vein. They work on your whole nervous system, but will not cause you to lose consciousness. The side effects include nausea, drowsiness and difficulty concentrating. Systemic analgesics are not given right before delivery because they may slow the baby's reflexes and breathing at birth.
Epidural Analgesia
Sometimes called an epidural block, causes some loss of feeling in the lower areas of your body, yet you remain awake and alert. An epidural block may be given soon after your contractions start, or later as your labor progresses. An epidural block is given in the lower back into a small area (the epidural space) below the spinal cord. You will be asked to sit or lie on your side with your back curved outward and to stay this way until the procedure is completed. Your skin will be cleaned and numbed with a local anesthesia injection. The epidural needle will be placed, a small tube (catheter) will be inserted through it, and the needle is then withdrawn. Medication will then be given through the catheter and pain relief will begin within 10–20 minutes. You can move when it's done, but you will not be allowed to walk around.
General Anesthesia
General anesthetics are medications that put you to sleep (make you lose consciousness) and are generally reserved for emergency cesarean sections.
Breast milk is nature's perfect baby food. Your milk has just the right nutrients, in just the right amounts, to nourish your baby fully. It also helps your baby's mind and body grow. Breastfeeding (also called nursing) is a good choice for both the baby and the mother.
Why Breastfeeding is Good for Your Baby
• The colostrum – a yellow, watery pre-milk – that your breasts make for the first few days after birth helps your newborn's digestive system grow and function.
• Breast milk has antibodies that help your baby's immune system fight off sickness. Babies who are breastfed also have a lower risk of asthma, obesity, allergies and colic.
• The protein and fat in breast milk are better used by the baby's body than the protein and fat in formula.
• Babies who are breastfed have less gas, fewer feeding problems and often less constipation than those given formulas.
• Breastfed babies have a lower risk of sudden infant death syndrome (SIDS).
Why Breastfeeding is Good for You
• It is convenient – the baby's food is always available and at the right temperature.
• Breastfeeding releases the hormone oxytocin, which makes the uterus contract and helps it return to its normal size more quickly. This also reduces bleeding after delivery.
• It may decrease your risk of some forms of cancer and other illnesses.
• It may help you lose pounds gained during pregnancy faster than you would if you were bottle-feeding.
• It is cheaper than bottle-feeding.
• It creates a special bond between you and your baby.
Your breasts initially produce colostrum, but within a few days they will be engorged (full and tender) with milk. Your suckling infant will then be able to trigger the “let down” reflex. During this, you may feel a pins-and-needle sensation. The first milk that flows out of your breasts is watery and sweet to quench your baby’s thirst and provide sugar, protein, mineral, and fluid. As the feeding goes on, the milk becomes thick and creamy and provides the nutrients your baby needs to grow. Try to breastfeed without supplementation the first 6 months of your baby’s life. You can breastfeed longer if both you and your baby are willing. Any amount of breastfeeding, even a few days, is good for the baby.
Remind your nurse during labor that you plan to breastfeed, so she can help you get started right after delivery. You should try to nurse the first hour after birth as this is the time your newborn is most alert. When you and your baby are ready to begin nursing, find a good position (see example image on the next page). Cup your breast in your hand and stroke your baby’s lower lip with your nipple. The baby will open his or her mouth wide. Quickly center your nipple in the baby’s mouth and bring your baby to your breast – not your breast to your baby.
Check the Baby’s Technique
If the baby is not latched on well, start over. To break the suction, insert a clean finger between your breast and your baby’s gums. When you hear a soft pop, pull your nipple out of the baby’s mouth.
Do Not Watch the Clock
Let your baby set his or her own nursing pattern. Many newborns nurse for 10-15 minutes on each breast.
Nurse on Demand
When babies are hungry, they will nuzzle against your breast, make sucking motions, or put their hands to their mouths. Crying is a late sign of hunger. You may nurse very often (8-12 times in 24 hours) in the baby’s first weeks of life.
Switch Sides
When your baby empties one breast, offer the other. You do not have to nurse at both breasts in one feeding. At the next feeding, offer the other breast first.
Cradle hold. Sit up straight and cradle your baby in the crook of your arm. The baby’s body should be turned toward you and his or her belly should be against yours. Support the baby’s head in the bend of your elbow so that he or she is facing your breast.
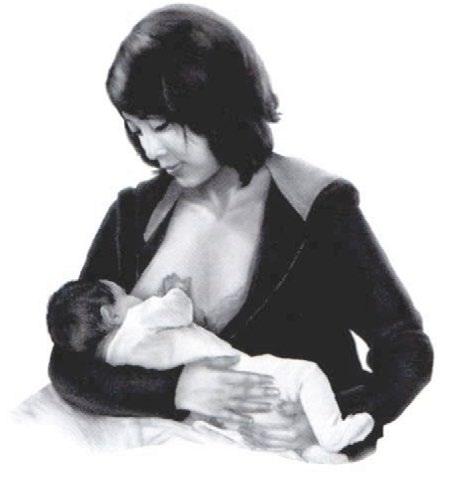
Cross cradle hold. As in the cradle hold, nuzzle your baby’s belly against yours. Hold him or her with the other arm. This way, the baby’s bottom rests in the crook of your arm and your hand supports the baby’s head and neck. This position gives you more control of the baby’s head. You may need to support the baby’s head with pillows. This position is useful for a newborn who is having trouble getting the hang of nursing.
MORE HELPFUL HINTS
Side-lying position. Lie on your side and nestle your baby next to you. Place your fingers beneath your breast and lift it up to help your baby reach your nipple. This position is good for night feedings. It is also good for women who had a cesarean delivery because it keeps the baby’s weight off the incision.

Football hold. Tuck your baby under your arm like a football. Sit the baby up at your side, level with your waist, so he or she is facing you. Support the baby’s back with your upper arm and hold his or her head level with your breast. This hold is good for nursing twins and for women who had cesearean births.

• With any position, make sure the baby’s whole body (not just his face) is turned toward you.
• Use pillows or folded blankets to place the baby at the level of your breast.
• You may want to prop your feet on a stool to raise your knees and help bring your baby closer to your breast.

When you are pregnant, your body stores extra nutrients and fat to prepare you for breastfeeding. Once your baby is born, you need more food and nutrients than normal to provide fuel for milk production. When you are nursing:
• Eat a well-balanced diet. During breastfeeding you need about 500 calories a day more than you did before you became pregnant or about 2,500 calories a day for most women.
• Make sure you get 1,000 mg of calcium a day. Your health care provider may suggest that you keep taking a daily vitamin.
• Avoid foods that bother the baby. If your baby acts fussy or gets a rash, diarrhea, or congestion after nursing, let your baby's doctor know. This can signal a food allergy.
• Drink at least eight glasses of liquid a day.
For the first few weeks, check for these signals to tell if your baby is well-nourished:
• My baby nurses often. A newborn should nurse at least 8-12 times in 24 hours (every 2 hours or so). Your baby may spend about 10-15 minutes on each breast.
• My baby is drowsy and content after nursing.
• My breasts feel full and firm before feedings. After, they are less full and feel softer.
• My baby wets at least 6 diapers a day. His or her urine should be nearly clear. During the first month, your baby should have at least 3 bowel movements a day. The stool should be soft and yellow.
• My newborn baby is gaining weight. Most newborns lose a little weight at first. After 2 weeks, most babies are back up to their birth weight. Newborns should gain weight after the first week.
If you are worried that your baby is not getting enough milk, tell the pediatrician right away and have the baby's weight checked.
Having a baby is a joyous time for most women. But 70-80% of new mothers have the postpartum blues or “baby blues” and feel sad, afraid, angry or anxious after childbirth. They may cry for no clear reason, have trouble sleeping, eating, and making choices and almost always question whether she can handle caring for a baby. These feelings may come and go in the first few days after childbirth, but often go away within a week or so without treatment. Postpartum depression is a more serious condition that affects approximately 10% of women. It most commonly starts 1–3 weeks after delivery. Women with postpartum depression need treatment with counseling and sometimes medication.
When to suspect postpartum depression
A new mother may be developing – or already have – postpartum depression if experiencing any of the following signs or symptoms:
• The “baby blues” do not start to fade after about 1 week.
• Strong feelings of depression and anger come 1–2 months after childbirth.
• Feelings of sadness, doubt, guilt or helplessness seem to increase each week and get in the way of normal functions.
• She is not able to care for herself or her baby.
• She has trouble doing tasks at home or on the job.
• Her appetite changes.
• Things that used to bring her pleasure no longer do.
• Concern and worry about the baby are too intense, or interest in the baby is lacking.
• Anxiety or panic attacks occur.
• She fears harming the baby.
• She has thoughts of self-harm or suicide.
A new mother experiencing any of these signs should visit with her obstetrician or provider immediately.
What you can do
• Get plenty of rest. Do not try to do it all. Try to nap when the baby naps.
• Ask for help from family and friends, especially if you have other children. Have your partner help with feedings at night.
• Take special care of yourself. Shower and dress each day, and get out of the house. Get a baby sitter or take the baby with you. Go for a walk, meet with a friend, and talk with other new mothers.
• Tell your partner or a friend how you feel. Often just talking things out with someone you trust can provide relief.
• Call us if your feelings do not improve or if you feel hopeless. Tell us if you are afraid you might neglect or hurt your baby.
Episiotomy care
You will be taught “peri-care” prior to leaving the hospital. This will include using a squirt bottle to cleanse your perineum (area between the vagina and anus) after toilet use. You will also be able to use ice packs and witch hazel pads to soothe your perineum. A warm, plain water sitz bath, three times a day, whether or not you are still bleeding can also be soothing to uncomfortable stitches or hemorrhoids.
Contraception
There are several methods of contraception available and we will discuss these fully at your first postpartum visit. It is important to know that nursing your baby does not protect you from getting pregnant.
Exercise
You are encouraged to walk and get out of the house as often as possible/desired after delivery; however you should avoid strenuous exercise until after your postpartum visit (at least 6 weeks).
Menstruation
Your first menstrual cycle after delivery tends to be heavy and contain clots. It may start, stop and start again. You can expect to menstruate for the first time 4 – 8 weeks after your delivery if you do not nurse your baby. However, if you nurse your baby, menses may be delayed for an indeterminate amount of time. Don’t worry; menses will not interfere with nursing.
Postpartum Intercourse
We advise you to wait at least 6 weeks before resuming intercourse. If you have had an episiotomy, intercourse may cause some discomfort initially.
Your initial postpartum visit
Unless you had problems during your pregnancy and/ or delivery, you should arrange for a follow-up exam no later than 6 weeks after your baby’s birth. You will have a general physical exam, including a thorough pelvic exam. We will also discuss contraception.


BOOKS:
• Pregnancy, Birth and Breastfeeding: What to Expect When You’re Expecting, Heidi Murkoff
• The Pregnancy Bible, Joanne Stone, Keith Eddleman
• The Mother of All Pregnancy Books, Ann Douglas
• The Pregnancy Book, The Birth Book, The Breastfeeding Book, The Baby Book, William and Martha Sears
• The Nursing Mother’s Companion, Kathleen Huggins
• New Mothers Guide to Breastfeeding, American Academy of Pediatrics
FOR FUN:
Belly Laughs, Jenny McCarthy
Maybe Baby, Lori Leibovich
My Boys Can Swim: The Official Guys Guide to Pregnancy, Ian Davis
WEBSITES: www.americanpregnancy.org – pregnancy www.llli.org – breastfeeding www.aap.org – pediatrics www.healthychildren.org – pediatrics
