

COMPASSION
Going the extra mile for the best care in the world
ADVANCED VASCULAR CARE: THE VEIN CLINIC

Restore Your Leg Health at Our Premier Vein Clinic
Are painful, swollen legs or debilitating varicose veins affecting you? Don’t let vascular issues impact your daily activities and well-being any longer. Experience life-changing results at our premier vein clinic.

Bhaskar Purushottam, M.D., FACC, FSCAI, FSVMB

Alexander Schabauer, M.D., FSVMB, FACC

Moinuddin Syed, M.D.
Our vein clinic offers:
• 28 years of complex vascular care emphasizing the highest quality outcomes
• Care from physicians who have completed a dedicated vascular fellowship in venous disease from Mayo Clinic and Mount Sinai
• Comprehensive vascular evaluations and personalized treatment plans
• Advanced, minimally invasive treatments for venous insufficiency
• Expert care from experienced, board-certified vascular specialists
• Fast, virtually painless procedures for varicose veins, spider veins and chronic venous skin problems
• Rapid outpatient recovery and minimal downtime
• Enhanced mobility, comfort and overall quality of life
Schedule your consultation and take your first step towards pain relief.
Vein Clinic
THE HEART TEAM
At Monument Health, you’ll find western South Dakota’s largest group of cardiovascular specialists offering diagnostics, research and accredited labs. Our state-of-the-art facility includes surgical suites, catheterization labs, an electrophysiology device lab and a hybrid suite with advanced imaging equipment.
Our board-certified specialists collaborate with skilled nurses and providers to deliver the right care at the right time. Experience the full spectrum of heart and vascular care at Monument Health.

Amid Bitar, M.D. Cardiovascular Medicine

Ethan Levine, D.O., FHRS Electrophysiology

Michael D’Urso, M.D., FACC
Cardiovascular Medicine, Interventional Cardiology

Charan Mungara, M.D. Cardiothoracic Surgery, Vascular Surgery
















Alexander Schabauer, M.D., FSVMB, FACC
Cardiovascular Medicine




John Heilman III, M.D., FACC
Cardiovascular Medicine

Rajesh Pradhan, M.D. FACC
Cardiovascular Medicine


Luis Hernandez, M.D. Advanced Heart Failure

Bhaskar Purushottam, M.D., FACC, FSCAI, FSVMB
Cardiovascular Medicine, Interventional Cardiology

Moinuddin Syed, M.D. Cardiovascular Medicine
Joseph Tuma, M.D. FACC, FSCAI
Cardiovascular Medicine, Interventional Cardiology









Stephen Wasemiller, M.D. Cardiovascular Medicine





Jessica Tvedt CNP
Whitney Stull PA-C (Spearfish)
Lizanne Laird CNP Megan Hullinger CNP Kyle Larson FNP
Samantha Speed DNP
Diane Schabauer CNP
Becky Sharp CNP
Melanie White CNP Meghann Warnke CNP
Mikayla Crocker CNP
Evelyn Provell CNP
S. Martin Digler PA-C
Emily Horning PA-C
Rebecca Bierle CNP
Jessica Albers PA-C
Audrey Bickerdyke DNP
Cassie Brandsted CNP
Matthew Gross CNP
Kimberly Hayden PA-C
Jordan Hoffman PA-C
Nick Hollenbeck DNP
Lauren Tuma CNP
Claudia Smith CNP
Kelly Brandsted CNP
Jennifer Franke CNP
Arok Thon PA-C
Timothy Sedlak PA-C

TA WELCOME FROM
Paulette Davidson
President and Chief Executive Officer, Monument Health
he days may be getting shorter and the air a bit cooler but the drive to move forward never seems to go away. It’s the uplifting stories of our patients, physicians and caregivers that keep us going.

In this issue, I hope you’ll notice that central theme of returning, full-circle, throughout the magazine.
In our cover story, Ralph Kruse returned home to the Black Hills for surgery after a serious heart episode he experienced while abroad. Ralph and his wife Sandy chose to travel thousands of miles to be at Monument Health. That choice also allowed Ralph to recover at home.
You’ll also read a story about reunion and closure, something that can be rare in an Intensive Care Unit. Dillon Robbins and his parents returned to Rapid City Hospital to meet – and thank –physicians and nurses for saving his life, on the one-year anniversary of his life-threatening injury.
You will get to know a competitive athlete getting back to the sport he loves. Pat Baumann’s passion for endurance running was put on hold until a shoulder surgery got him back in the race.
Rounding out the issue is the story of June Kilby’s ankle replacement. June’s on-the-go lifestyle hit a snag when her ankle pain started keeping her from getting things done. But getting her ankle replaced at Spearfish Hospital made all the difference in the world.
As always, I thank you for taking the time to read these stories. Here at Monument Health, we like to say “It starts with heart.” My hope is that these stories that came from our hearts will find their way into yours.


Managing Editor
Melissa Haught
Editor
Stephany Chalberg
Contributors
Colette Gannon
Michelle Pawelski
Kory Lanphear
Stephen Simpson
Bob Slocum
Anna Whetham
Art Director
Stacy Brozik
Layout
Stacy Brozik
Terri Upward
Photographer
Bob Slocum


CONTENTS
FALL 2024
In case you missed it
Our roundup of all the latest news and happenings throughout Monument Health. page 4
Where are they now:
Laura Brunmaier, Ph.D.
Issue 8 cover story Laura Brunmaier, Ph,D., gives an update on her research and work, including an exciting new collaboration with NASA. page 6
My space: Anna Whetham
The work of Monument
Health’s Community Relations Specialist is motivated by a very personal – and meaningful –experience. page 8
Feature:
Farther than ever
Pat Baumann, a competitive athlete, faces down his toughest feat of endurance yet – injury. page 12
Ask the doc: Esperanza “Hope” Argenziano, M.D., Rheumatologist
Autoimmune disorders are as common as they are difficult to diagnose.
Dr. Hope aims to bring some clarity to these mystifying illnesses. page 16
Feature:
Guardians of the community
Find out how infectious disease is an important and growing specialty that requires multi-disciplined medical mastery. page 18
Feature:
Intensive Care Nurses
When a former patient returns to express gratitude, a pair of ICU nurses are granted a rare sense of closure. page 20
Cover story:
The heart of care
Ralph and Sandy Kruse were in the midst of another year of idyllic snowbirding vida en México, when a serious heart emergency landed them in a desperate, life-or-death situation. page 24
Nurse Feature:
Megan Winter, RN
Adaptability and connection with patients helps Megan Winter find her sweet spot as a Dermatology Nurse. page 28
Physician spotlight:
Michael Huot, M.D.,
Anesthesiologist
Dr. Huot elaborates on his long history, varied roles and surprising social media success at Rapid City Hospital. page 30
APP Spotlight:
Heart and Vascular Institute
Gaining the trust of patients is crucial, so the HVI Advanced Practice Providers use a team-based approach. page 32
Patient Story:
June Kilby and Colin Zdenek, DPM, FACFAS
An ailing ankle was starting to keep June Kilby from doing her job. A novel solution got her off the recliner and back on her feet. page 34
Introducing
Get to know physicians who have recently joined Monument Health. page 36
Directory
Find a Monument Health provider near you. page 38
Crossword Puzzle
An amazing and entertaining stroll through this issue via a fun puzzle that you’re sure to enjoy. page 40
Calendar
Upcoming events at Monument Health. page 41

Golden Guitars Gala sets fundraising record for Children’s Miracle Network
The third Golden Guitars Gala, a Monument Health Foundation fundraiser for Children’s Miracle Network, broke records on June 8, 2024, by raising more than $478,600, setting a Foundation record for the largest amount raised at a single event. During the gala’s live auction, the topselling guitar, signed by Chris Stapleton auctioned for an impressive $37,000.
The Golden Guitars Gala, attended by more than 250 people, featured live music by Kory and the Fireflies, information about the impact of CMN in our region and a live auction featuring 18 celebrity guitars, plus one surprise celebrity guitar signed by Def Leppard.
Monument Health donation supports Spearfish High School Athletics
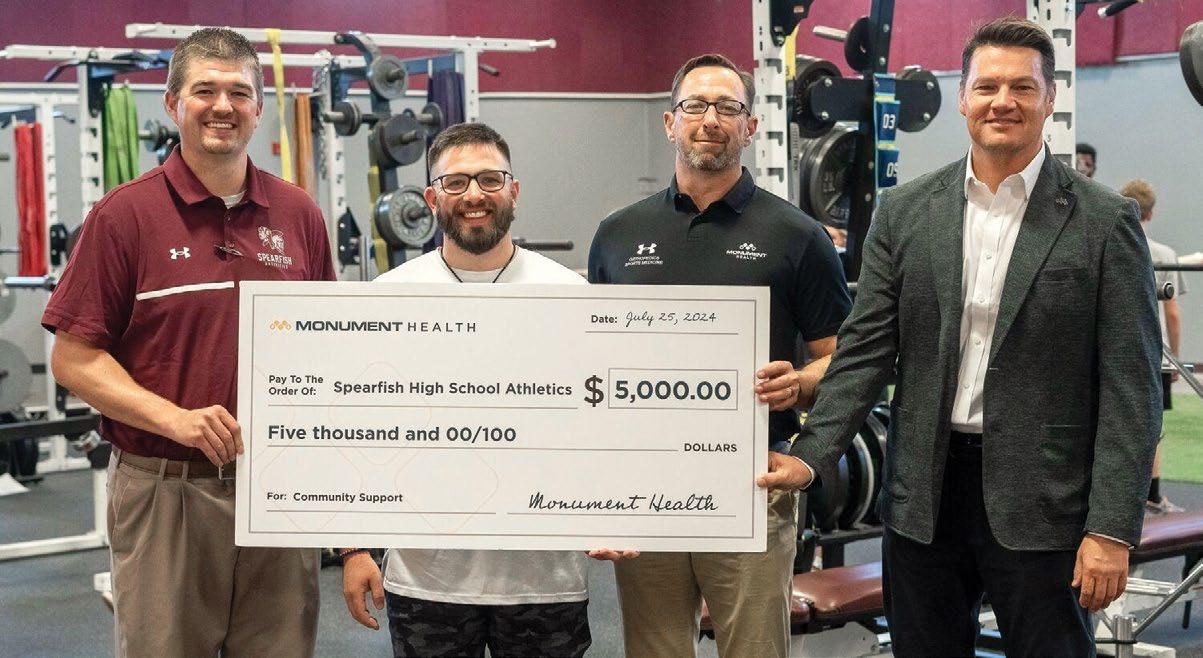
Monument Health Orthopedics & Sports Medicine team continues to partner with, and support, Spearfish High School Athletics through providing athletic training and strength and conditioning personnel and programming.
In addition to strength and conditioning programming throughout the school year, the summer 2024 program provided over 200 student-athletes an opportunity to join the summer SHS Performance Camp under the guidance of Eric Santure, CSCS, Monument Health Performance Coach, emphasizing improving overall athletic performance while decreasing injuries.
Thomas Worsley, President of Monument Health Spearfish Hospital and the Hills Markets, along with Eric and Justin Feeser, Monument Health Manager of Sports Medicine and Rehabilitation, Northern Hills presented a $5,000 check to Dalton Wademan, Spearfish High School Activities Director, to continue to improve the strength and conditioning equipment and facilities available to SHS student-athletes.
Monument Health is nationally recognized for its commitment to providing high-quality stroke care
Monument Health Rapid City Hospital has received the American Heart Association’s Get With The Guidelines® - Stroke GoldPlus quality achievement award for its commitment to ensuring stroke patients receive the most appropriate treatment according to nationally recognized, research-based guidelines, ultimately leading to more lives saved and reduced disability.
Monument Health also received the American Heart Association’s Target: Type 2 Diabetes™ Honor Roll award. Target: Type 2 Diabetes aims to ensure patients with Type 2 diabetes, who might be at higher risk for complications, receive the most up-to-date, evidencebased care when hospitalized due to stroke.

Monument Health breaks ground on Box Elder Urgent Care and Clinic

Monument Health began construction on one of two new locations planned for the Rapid City area. The first new location will be located on a 2.15-acre parcel of land near Liberty Plaza in Box Elder. The clinic will provide urgent care services and primary care services. Another clinic will open in Rapid Valley near Elk Vale Road and Highway 44 in fall 2025.
These additions will bring the total number of Monument Health urgent care centers in the Rapid City area to four, complementing the existing locations at Jackson Boulevard and Lacrosse Street.
West River Anesthesiology Consultants joins Monument Health to expand pain management services
To better serve the needs of patients in the Black Hills region, Monument Health expanded its pain management services with the addition of the West River Anesthesiology Consultants.
On July 1, 2024, five physicians and three certified nurse practitioners joined Derek Buck, M.D. in the Pain Management Clinic at the Orthopedic and Specialty Hospital on 1635 Caregiver Circle in Rapid City.
West River Anesthesiology Consultants has been providing pain management services in the Rapid City area for over 25 years. Their team of highly trained anesthesiologists and nurse practitioners have a wealth of experience in treating a wide range of conditions.
“We are thrilled to welcome West River Anesthesiology to Monument Health,” said Michael Huot, M.D., Medical Director of Monument Health’s Pain Management Clinic.
“Their expertise in pain management will be a valuable addition to our team and will allow us to continue to provide high-quality care for our patients, close to home.”

MICHAEL HUOT, M.D. Medical Director, Monument Health Pain Management Clinic

We first introduced you to Laura in Issue 8 of Health Magazine. At the time, her research project centered around engineering substances found naturally in the human body to create new blood vessels.


LAURA BRUNMAIER BUILDS A FOUNDATION FOR NEW DISCOVERIES
To paraphrase 1980s one-hit wonder Matthew Wilder, nothing is going to break the stride of Laura Brunmaier, and there is no slowing down the South Dakota Mines Ph.D. research assistant.
Story by Michelle Pawelski
Photos by Bob Slocum

“If I don’t have a problem that needs to be solved, I get bored. Engineering works well for that. We are not just exploring something for the love of science; we are trying to find problems and come up with solutions,” Laura said.
And that is precisely what she has been doing since leaving a successful career in 2016 and returning to academia.
In May, Laura defended her Ph.D. dissertation on establishing the foundation for developing a tissue engineering vascular graft – research she has spent the past five years working on with Dr. Travis Walker, associate professor in the Karen M. Swindler Department of Chemical and Biological Engineering.
Simultaneously, she contributed to the National Institute of Health (NIH) proposal to create a new tissue engineering and cell culture laboratory with soft matter characterization on the Mines’ campus. And a day before her dissertation defense, Laura received $100,000 for a NASA R3 grant proposal she submitted with the university’s physics department. The proposal looks at the effects of low-dose ionizing radiation on inflammasome development in endothelial cells.
“I have a new project now,” Laura said just days after presenting her dissertation.
Laura will spend the next year working on NASA research while waiting for NIH funding to build the new lab, providing space to expand her research and develop a usable biomaterial vascular graft. The Mines lab will be a part of the South Dakota Biomedical Research Infrastructure Network (SD BRIN), led by the University of South Dakota and its Sanford School of Medicine. The goal of SD BRIN is to develop human resources and research talent in the areas of biomedical sciences and bioinformatics.
Laura has spent several years laying the foundation for a vascular graft that is made of biological material that’s already in the human body. She was awarded a $20,000 grant from the National Institute for Occupational Safety
“We are not just exploring something for the love of science; we are trying to find problems and come up with solutions.”
and Health and then a $40,000 grant from the Alternatives Research and Development Foundation to develop a media for cells that was chemically defined and had no animal constituents.
“All these projects set a foundation for us to build a vascular graft so we can start to understand what inflammation looks like in endothelial cells, which are really important to the longevity of any vascular transplant,” she said.
Laura hopes to hear about the NIH funding sometime in early 2025.
“I think we will have really good traction in the next two to four years,” she said. “We are just waiting for the money to come in and for this lab to get built, but we have a strong set of intuition on how to handle these materials and what we need to do now.”
Laura’s current focus is on her NASA research and building the lab, which she said will be her “new baby.” However, she believes there is a lot of opportunity for growth in the world of biomedical engineering in Western South Dakota and plans to be at the forefront of that growth.
“The university is emphasizing entrepreneurship, which I think is great because there are a lot of smart people here that come up with some great ideas, and some of those ideas have led to good businesses in the area,” she said. “It would be great to see more biotech in this area, and it would be awesome if I could help with that.”
LAURA BRUNMAIER, ON ENGINEERING


COMMUNITY STRONG
Story by Kory Lanphear
Photos by Bob Slocum
As a Community Relations Specialist and former Miss South Dakota, Anna Whetham has a passion for bringing groups together. Her awareness of community needs and a harrowing medical experience provided a serendipitous backdrop to bring her unique skill set to Monument Health.
Every day is different for Anna Whetham.
As Community Relations Specialist in Strategic Marketing and Communications, Anna brings Monument Health and the people it serves together, which means acting as a point of contact between organizations both internal and external.
“Community Relations focuses on a couple key areas: through sponsorship, community health education and engagement with our caregivers,” she said. Sometimes that means organizing and facilitating free health screenings at existing events, such as Lakota Nation Invitational, and sometimes that means organizing and putting on Monument Health sponsored gatherings like Special Rodeo.
“That’s a unique opportunity that I have: I get to work with a lot of different people. I get to work with leaders, I get to work with nurses and physicians, I get to work with all different types of departments. It’s a firsthand glimpse of the work that people are doing inside our facilities and outside our facilities. I get that well-rounded view of how everything is connected.”
The work is a calling, not only because of Anna’s enthusiasm for community engagement and her prior experience in a very public role as a Miss South Dakota 2011, but also due to a scary episode that was both life changing and also life affirming.
Several years ago, Anna, expecting her first child, experienced pregnancy complications that required hospitalization at Rapid City Hospital. She was diagnosed with a preeclamptic complication called HELLP syndrome (Hemolysis, Elevated Liver enzymes and Low Platelets), which is a dangerous blood and liver condition that can threaten the life of both mother and baby.
“Things got really intense, really fast. Essentially, the pregnancy became toxic to my body, and my body was starting to shut down,” she said. Anna’s daughter
“The power of presence is a big piece of what we’re doing. And it helps with trust, but also with trying to help our community have better access to health care at the end of the day.”
ANNA WHETHAM, COMMUNITY RELATIONS SPECIALIST
was born premature at 27 weeks gestation and weighed a mere 1 pound, 15 ounces. An extended stay in the neonatal intensive care unit (NICU) followed.
Anna and her daughter have since fully recovered and are completely healthy. The experience, though, had a profound influence on Anna. “Ever since that happened, there was just a piece of my heart that was still connected to the hospital, and to how health care plays such an important role in our lives, even in ways we may not understand until we need it.”
Later, when she was presented with the prospect of working for Monument Health, Anna saw it as a chance to not only give back, but to help shape and strengthen the organization’s outreach in the area. Her efforts have borne fruit, too. “This past fiscal year, we did 18,664 health screenings at 91 different events/locations. From the sponsorship standpoint, we gave out over a half-million dollars to 188 different community organizations.”
IN FISCAL YEAR 2024:
18,664 HEALTH SCREENINGS AT
91 DIFFERENT EVENTS/ LOCATIONS
OVER A HALF-MILLION DOLLARS DONATED TO 188 DIFFERENT COMMUNITY ORGANIZATIONS

And yet, there is always more work to be done. “The power of presence is a big piece of what we’re doing. And it helps with trust, but also with trying to help our community have better access to health care at the end of the day.”
In her free time, Anna stays as close to her family as possible. “Family is very, very important to me, especially because there was a time that we had to look at potentially, you know, saying goodbye. And so it has put an even bigger emphasis on making sure that I am being as present as I can.”
She and her husband Josh, also raise horses as a hobby, so perhaps it’s no surprise that the project in which Anna is most heavily involved is Monument Health’s Special Rodeo. “That was a unique opportunity that was brought to us that Monument Health decided to take on because of the importance of celebrating and embracing diversity and lifting up those in our area that have disabilities,” said Anna.
Even though the connection of Special Rodeo to a traditional rodeo is spiritual – the participants interact only with tame therapy animals –it speaks to the necessary creativity for what is central to the challenge of Anna’s endeavor: how to help those beyond the walls of the hospitals.
“How can we, with the resources that we have, make an impact? How can we best use those resources in a way that is continuing to change people’s lives?,” she said. “Sometimes that impact may not even have a health specific component to it. It might be lifting people up, encouraging them and developing a positive spirit out in our community, which goes a long way.”








FARTHER THAN EVER
Story and Photos by Bob Slocum
Pat Baumann
is no stranger to a challenge. As an avid endurance runner, formidable circumstances are kind of his thing.
Last year Pat found himself dealing with an unfortunate, unforeseen obstacle when he suffered a major shoulder injury during a race. Now, with the help of Monument Health’s orthopedic and physical therapy experts, he’s back on the trail and pushing himself farther than ever.
“What I love about endurance running is that it’s demanding. It’s like a wall you have to overcome,” Pat said. “When you start out running you hit a wall, and you can’t go any further. So you slam yourself into that wall again and again until you can make it another 100 yards; a little further and a little further. Over time, you’re now going many miles.”
The grit and mental outlook to overcome obstacles that endurance running cultivates was needed throughout Pat’s injury and recovery. He called on that perspective over the course of a year to receive surgical intervention, rehab his shoulder and resume his active lifestyle.
“I feel so blessed about what I can do with this arm and shoulder now,” Pat said. “I can lift it up and have a full range of motion. There was a time I couldn’t imagine getting back to this point after my injury.”
The Fall
It happened about halfway through the Bighorn Mountain Trail Run, an 18-mile extreme mountain endurance event set in some rugged, remote Wyoming terrain. Rain the previous night had made the primitive deer trail slick and muddy in the low spots but that wasn’t stopping the racers from attacking the course; Pat included.
Pat lost traction in the mud while descending a steep slope and felt his feet fly out from under him. “I was taking a risk,” Pat said. “I was just screaming down the mountain going full speed and pretty soon I was in the air.”
As he braced for a rough landing, Pat stuck out his left arm and came down with the full weight of his body on his elbow. The impact jarred his humerus bone from the shoulder, tearing his rotator cuff. In extreme agony and covered in mud, Pat had a moment to assess his circumstance.
“I knew I had to try and get up and finish, because it’s so remote out there that I didn’t want to have someone come in on horseback or have LifeFlight sent in,” Pat said.
Rising to his feet, Pat started off and fell again. This time, the impact forced the bone completely out of the joint, causing even more damage.
“Oh, man, talk about pain,” Pat said. “On a 1-10 scale, the pain was an 11 in that moment.” Pat received assistance from a fellow runner who stopped to check on him.
“I just asked her to pray for me,” Pat said. “She prayed and laid hands on me gently and as we prayed the bone popped into place and the pain came to a manageable level.”
There were 9 miles to go at that point, but Pat held his arm close to his body and made it to the finish.
The Comeback
Pat sought treatment at his hometown Monument Health Custer Hospital, where he began working with the physical therapy staff, including Kevin Sobolik, DPT, CSCS. Kevin, who is the supervisor of rehabilitation services at Custer Hospital, set a goal for Pat to achieve some healing standards before he could be a candidate for surgical repair to the shoulder.
“We put in a lot of hard work and used a lot of creativity

Pat with Joseph Humpherys, D.O. (L) and Kevin Sobolik, DPT, CSCS (R).
To watch a video about Pat’s story, scan the QR code below.


with Pat to try and make sure we were sparking muscles to return like they’re supposed to,” Kevin said. “At the same time, we were watching the boundary to not overdo things. We worked that balance for quite awhile. Certainly there is still more work to do moving forward to heal and improve his shoulder.”
The importance of starting the shoulder to heal from the traumatic tissue damage was emphasized by Joseph L. Humpherys, D.O., FAAOS.
“One of the side effects of doing a surgery on the shoulder is the shoulder getting tight and stiff. So if you go into surgery tight and stiff you come out 10 times stiffer. For Pat, we had to do a lot of pre-physical work to get that range of motion back before he was ready to actually have a surgery,” said Dr. Humpherys, a fellowship trained sports medicine and orthopedic surgeon.
Rotator cuff repairs are a common procedure for Dr. Humpherys, who typically performs three to four such surgeries per week. What made Pat’s case unique,
The Century Club: a Lifelong Pursuit
Recently cleared for full activity, Pat has a full range of motion in his shoulder and can do all the things he enjoys. That includes keeping up with his 20-plus grand and great-grandchildren, as well as getting back out on the running trail. Pat’s passion for running was sparked by his mother, who was an early influence and his top supporter in his own running goals.
“She would run around the block and I would follow her and just really enjoy it,” Pat said. “I ran my first marathon at 14, and I remember Mom in her ’55 Chevy driving ahead of me every few miles, making sure I was doing alright.”
Pat continued to pursue distance running throughout high school then college, and all the way through retirement.
One year removed from his accident, Pat once again competed in the Bighorn Mountain Race and dominated the course. Then, Pat set his sights on an even bigger goal: a 100-mile ultramarathon. In August 2024 Pat completed the Lean Horse Ultra, making it 100 miles on foot in 29 hours.
“I believed I was going to finish the 100 miles and if I didn’t finish, it wasn’t going to be because of my shoulder,” Pat said. “The shoulder did what it was supposed to do. I feel so blessed and can’t say enough about Dr. Humpherys and Kevin. Their care and professionalism has really helped me though all this.”
he said, was the emphasis on repairing the muscle so that Pat could eventually regain normal function.
“We didn’t know if we could repair the muscle initially, so we had contingencies in the surgery to recreate a muscle that’s not repairable,” Dr. Humpherys said. “We had to release a lot of different things and shift the muscles around a little bit. We were able to get his shoulder back where it belongs, and now Pat’s motion and strength is in a great place.”
Once the surgery was complete, there was still plenty for Pat to do in physical therapy. He has continued to see Kevin at Custer Hospital, as well as Dr. Humpherys, who regularly holds clinics there to better serve Southern Hills orthopedic patients.
“We have a super solid group of therapists here who all have a close relationship with our primary physicians,” Kevin said. “The ability to communicate with them and with Dr. Humpherys directly on a face-to-face basis makes a big difference for our patients.”




ASK THE DOC: AUTOIMMUNE DISORDER EXPLAINED

ESPERANZA “HOPE” ARGENZIANO, M.D., RHEUMATOLOGIST
Dr. Argenziano, (or “Dr. Hope” as she is sometimes known) is a board-certified rheumatologist at Monument Health Rapid City Clinic, Flormann Street.
She is a U.S. Air Force veteran who herself suffers from an autoimmune disease called lupus. Her illness cut short her promising military career, but Dr. Argenziano used her experience with lupus to transition to health care so that she could help others who experience autoimmune conditions.
One in 15 people in the United States is afflicted with some sort of an autoimmune disorder. An autoimmune disease is a noncommunicable condition that occurs when the internal self-defense mechanism is triggered to attack cells or tissues within its own body. There are over 100 acknowledged autoimmune disorders, and the symptoms can range from skin lesions, to bowel inflammation to joint pain. Why the body attacks itself in this way is unknown.
Tune into your health with Monument Health’s Doc Talk, a weekly podcast. Listen at monument.health/podcast.
1 IN 15 PEOPLE IN THE UNITED STATES
IS AFFLICTED WITH SOME SORT OF AN AUTOIMMUNE DISORDER.
What is a rheumatologist?
A rheumatologist is a physician who has undergone internal medicine training initially and is board-certified in internal medicine, then goes on to a rheumatology fellowship for 2 to 3 years where they are mainly treating rheumatology patients. Rheumatologists see patients who need evaluation for diseases such as lupus and lupus-like diseases as well as vasculitis, rheumatoid arthritis, spondyloarthritis and other inflammatory arthritides, such as gout.
What are some common autoimmune conditions?
The most common autoimmune conditions seen by a rheumatologist include rheumatoid arthritis, psoriatic arthritis, gout, lupus, Sjögren syndrome, vasculitis and scleroderma. There are multiple other autoimmune diseases that are not treated by a rheumatologist, which include multiple sclerosis, Crohn’s disease and ulcerative colitis, skin psoriasis, Graves’ disease and Hashimoto’s thyroiditis.
Are these harder to diagnose or treat?
Rheumatologic conditions can be difficult to diagnose, especially in the early stages. In the early stages of disease, a patient may not have all of the symptoms or all of the positive blood testing to make a clear cut diagnosis. Rheumatologic
To learn more about Dr. Argenziano and listen to her podcast, scan the QR code below.

conditions can also be difficult to treat as the same medication does not work for every patient with this specific condition. It may take 2–3 trials of medications before a patient’s symptoms are improved. Our goal of treatment is to get them to low disease activity or remission.
What are common misconceptions of autoimmune conditions?
One misconception is that autoimmune diseases can be cured. Unfortunately, there is no cure for most autoimmune conditions. Another misconception is that patients can get treated for specific conditions and then stop their medications. In fact, most patients with a rheumatologic condition often require treatment throughout their lifetime.
What advances are you seeing in your field that will help patients?
We continue to see advances in medications for rheumatologic diseases. New treatments for rheumatoid arthritis, vasculitis and lupus are constantly being researched. Rheumatology researchers also are continuing to find more advanced ways of diagnosing patients early and also trying to discover ways of testing the patient to see what therapy will work best for them.



To learn more about Infectious Disease at Monument Health, scan the QR code or visit monument.health/infectiousdisease.
GUARDIANS OF THE COMMUNITY
Infectious disease is a medical specialty that touches nearly every aspect of health care. Discover why Monument Health is choosing to expand the capacities of this vital department.
Story by Stephen Simpson Photos by Bob Slocum
Sandeep Sohal, M.D., grew up in Toronto and was fascinated as a child any time his parents took him to see a physician. “When we were sick, a doctor would prescribe antibiotics, and it was really cool because you can fix something pretty quick — it was almost like magic,” he said.
As he got older, Dr. Sohal was naturally drawn to biology and eventually attended medical school in the Caribbean. He did clinical rotations in Detroit, completed his residency in internal medicine in Brooklyn, and then went back to Detroit to complete his fellowship in infectious diseases.
Dr. Sohal’s fellowship took place during the COVID-19 pandemic. “I think that time really showed me that infectious diseases are everywhere,” he said. “And that out of nowhere, your reality can change.” The pandemic, though challenging, served to galvanize Dr. Sohal’s resolve to help people through this field of medicine. “From that point I really knew I wanted to be on the frontlines, in the trenches, fighting infectious diseases.”
What is an Infectious Disease Specialist?
The pandemic has shined a spotlight on this medical specialty in recent years. “It was kind of amazing because it totally changed everything — literally overnight,” said Dr. Sohal. “I don’t know of any profession that has changed so much so quickly.”
Interest in this field of medicine has certainly grown in recent years, however, infectious disease experts have always played a vital role in the health care of communities throughout the world. But what is this specialty all about?
“I like to explain it as a field where we try to fix something, first of all,” explained Dr. Sohal. Infectious disease’s propensity to cure the conditions it’s treating sets it apart from other medical specialties. “Conditions like diabetes and blood pressure require chronic treatment; you can’t technically cure those conditions, but you can work to prevent complications.”
Infectious disease as a specialty represents some significant overlap in medical skills. “It’s a convergence,” said Dr. Sohal. “Things like medicine, surgery, pharmacy and also antibiotics. We have to wear different hats.” When pinpointing an infectious disease, these specialists use their vast medical knowledge to do some detective work to ensure that their recommended treatment is as precisely effective as possible. “Is it bacteria? Is it a virus? Is it not infectious? We really have to dig deeper. And sometimes there’s information that maybe no one else knows that we have to dig up through a very detailed history.”
When explaining what this field of medicine is like, Dr. Sohal likes to reference the TV show “House,” starring Hugh Laurie. “In that show, Dr. House is an infectious disease physician. So I tell people this field of medicine is kind of like that show — maybe just less witty and fewer jokes.”
Impact on the Community
The topic of infectious diseases is paramount to the discussion around public health. One issue that Dr. Sohal and others keep at the forefront of their minds regarding public health is drug resistance. “We can prevent our hospital and the local area


from getting more drug-resistant organisms,” Dr. Sohal said. “And that’s a big part of our job, too — thinking about which antibiotic we’re using from a community perspective. We want to be able to narrow antibiotic use down to specific drugs for specific infections and do that for just the right number of days.”
Dr. Sohal reported that these intentional efforts around antibiotic use in the Black Hills region have supported above-average results compared to other geographical areas in the country.
A Growing Team
Monument Health recently announced that the infectious disease team will be expanding. “We’re very appreciative to Monument Health for seeing the value of infectious disease and expanding the team,” said Dr. Sohal. “We’re very happy to welcome three new providers this year. Andrea Calderon, M.D., William Greene, D.O. and Nicholas Goodhope, M.D.”
This increased capacity of Monument Health’s infectious disease specialists will continue to ensure that patients are receiving the best care possible. According to Dr. Sohal, all medical specialties benefit from a strong presence of infectious disease specialists. “Studies have shown that the presence of an infectious disease physician results in improved outcomes and care for patients. And if you think about it,” he said, “that makes sense. There’s usually some component of an infectious process or at least a concern of one. Many times we can help stop antibiotics quicker or determine just the right antibiotic to use. Since our recent hire of three new infectious disease physicians, we hope to expand our practice in the Black Hills to match the growth of the community and continue to provide the best care and outcomes possible for our patients. I’m excited to see how things will progress in the next few years.”


TOUCH AND GO
As first contact caregivers, Intensive Care Unit nurses rarely get the opportunity to find out how their patients ultimately fare. When Dillon Robbins, a grateful patient, returns to thank the caregivers, they each get to experience a rare feeling — closure.
Story by Kory Lanphear
Photos by Stephany Chalberg
Dillon Robbins enters the Surgical Intensive Care Unit at Monument Health Rapid City Hospital and sees features and faces that are utterly unfamiliar, despite the fact that he spent nearly a month within its walls. He spots a nurse who initially registers a dim recollection of the young man standing before him. After a moment, the nurse, Adam Drake, RN, fully recognizes Dillon as one of his former patients. For his part, Dillon is only just now meeting someone whom he had only heard about, seeing a face he has thus far only been able to imagine.
It is an emotional moment, and long overdue, but a rare occurrence. Dillon has returned to the intensive care unit where he was treated for a traumatic brain injury he suffered one night in the early spring of 2023. Now, exactly one year later, Dillon is in the midst of recovery, with a renewed purpose in his life. It begins with demonstrating his gratitude to the ICU Caregivers at Rapid City Hospital.
On April 15, 2023, Dillon, then a 19-year-old student at South Dakota Mines, fell down a set of stairs at a fraternity party. After being rushed to Rapid City Hospital, he was treated in the Emergency Department and taken directly into surgery. Dillon had suffered a diffuse axonal injury, which is when a whiplash motion causes shearing of the white matter of the brain, leaving microscopic damage –or worse. His brain had shifted 1.5 centimeters to the right, and physicians performed a craniectomy, which is a procedure that removes part of the skull. “To alleviate the pressure so the brain has somewhere to go,” said Bryce Winters, RN, Adam’s colleague and another of Dillon’s caregivers. Dillon’s injury was so severe that he flatlined more than once.
After the surgery, Dillon was intubated and comatose for 22 days. Suffering from paralysis, his care was fraught with complications: from a staph infection in the lungs to two bouts of pneumonia and experiencing a phenomenon of frenetic, spiking brain activity, called neurostorming.
Adam and Bryce kept tabs on Dillon and also made a connection with his parents, Matt and Karen, sympathizing with their distress at Dillon’s unsettled condition. The bond the ICU physicians and caregivers developed with Dillon’s family is rare only in that there is seldom a chance for such relationships to develop, so transitory is the nature of Adam and Bryce’s work. “In our unit, they are critically sick,” Adam said. “A lot of times, you may not see them all the way through their care.”
Bryce and Adam are accustomed to taking comfort in the small improvements of their patients. One of the best things that can happen is when a patient is transferred out of the ICU to a different unit, a development that usually signifies improvement. The downside is that, because they are not involved in a patient’s continuing care, ICU staff rarely find out what happens to patients after their transfer. “We work three days a week. So then maybe you come back the next week and they’re gone,” Adam said.

The prognosis for patients with brain injuries can vary. Day in and day out, the caregivers can never really know what to expect. But it seemed like everyone was aware of what was going on with the patient in Room 250. For Adam, seeing what Dillon’s parents were experiencing hit really close to home. “I’m potentially trying to be a dad. And I was thinking about my future children and sharing memories together with them.
So then I’m like, ‘I really hope this kid can recover so they can share those memories or make more memories.’”

Dillon (middle) thank nurses Adam Drake, RN, (L) and Blake Wright, RN, (R) one year after an accident nearly took his life.
Adam Drake, RN, (L) and Bryce Winters, RN, (R).

Dillon was in the Intensive Care Unit for a total of 22 days. It was not a sure thing that he would completely recover, if at all. It was unclear if he would ever be able to care for himself, no less walk, ever again. The concern on the unit between physicians and nurses on multiple shifts was evident as even the most minor of milestones were tracked. “Once he started making improvements enough to where he could understand us and interact somewhat, you could tell that he had a drive that would push him farther than most. He had a lot to work through, and he knew that. And he wasn’t gonna give up,” said Bryce.
Dillon’s parents were with him on the day of his one
“You don’t always get that thanks,” he said. “I think the epitome of what you seek after you become a nurse is that feeling of, ‘Wow, we helped save this guy’s life. I made a difference.’”
BRYCE WINTERS, RN
year reunion with the caregivers who saved his life, just as they were there for the entirety of his stay in the ICU. Their familiarity with the layout of the hospital corridors speaks to their dedication to seeing through their son’s care, whatever his ultimate fate. The many hours and days they spent worrying were a mere blink for Dillon, however, as his memory from that time is mostly gone.
Even though the caring touch is fleeting, its healing spirit lingers and stays with Dillon wherever he may go in his life. And Dillon carries with him the knowledge that the collective actions of Bryce, Adam and all of the physicians and caregivers to treat him were crucial to his survival and ultimate recovery. In fact, Dillon was so profoundly affected by his experience at Monument Health that he has refocused his career aspirations, changing his college major from engineering to occupational therapy.
Later, Dillon, Matt and Karen meet Bryce, RN on his day off at a local lunch spot. Of all the physicians and nurses to touch Dillon’s life, Bryce was the closest to the Robbins family, having requested specifically to be assigned to Dillon’s room while he was in the ICU. He has stayed in contact with the family and shared in the joys and triumphs of Dillon’s continuing recovery. He feels honored by Dillon’s gratitude. “You don’t always get that thanks,” he said. “I think the epitome of what you seek after you become a nurse is that feeling of, ‘Wow, we helped save this guy’s life. I made a difference.’ You know? And that is very fulfilling.”
(L to R:) Karen Robbins, Lalith Uragoda, M.D., Dillon Robbins and Matt Robbins reunite on the one-year anniversary of Dillon’s accident.
COMING SOON
NEW URGENT CARE LOCATIONS



To meet the growing health care needs of the Box Elder and Rapid Valley communities, Monument Health is opening two new urgent care locations.
Monument Health also plans on building a medical campus on the corner of E. Mall Dr. and E. North St., with phase one focusing on emergency services.


THE HEART OF CARE
Monument Health physicians and caregivers are committed to delivering high-quality care that makes a difference in our communities. That’s why when a nurse at the Heart and Vascular Institute went the extra mile to ensure a patient facing a critical medical situation in Mexico could receive life-saving care at home, it made a lasting impression.
Story by Colette Gannon Photos by Bob Slocum
When Shelley Paris, RN, a patient care coordinator at Monument Health Heart and Vascular Institute, received a pleading call from Sandy Kruse, whose husband, Ralph, was experiencing a cardiovascular incident in Mexico, she did what her passion for nursing has always led her to do: be there for her patients.
Ever since she began her career as a nurse 25 years ago, Shelley has believed that developing strong connections with patients is one of the most important aspects of her job.
“I’m very protective of my patients,” said Shelley. “That’s why I hand out business cards with the direct line to my desk to each of them. I think it’s important that they talk to me and not somebody that doesn’t know anything about them,” she said.
Shelley didn’t know that when she handed a card to Sandy and her husband Ralph Kruse, she would later become a key player in saving his life.
A health crisis abroad
It was December of 2023. Enjoying retirement, Hill City residents and high school sweethearts, Ralph and Sandy were spending a winter at their vacation home north of Puerto Vallarta, Mexico, as they had done for the past 20 years.
Though generally healthy, Ralph had been diagnosed in 2016 with aortic valve disease, and underwent open heart surgery that same year to have a tissue valve replaced. “Generally, these valves tend to last anywhere between 10 to 15 years,” explained Rajesh Pradhan, M.D., FACC, who has been seeing Ralph as a patient. “But it’s hard to predict who gets that amount of time.”
Just weeks after the couple arrived in Mexico, Ralph started experiencing symptoms that indicated something might be wrong. He noticed the symptoms worsening as his neighbors cut and burned green brush in the lot in front of the couple’s house.
“The smoke came into our house so thick that I could hardly breathe,” explained Ralph.
After a bad night of sleep and a trip to the local doctor for a nebulizer treatment, it became clear that something was, in fact, seriously wrong.
“By the end of that afternoon, I asked Sandy to take me to the emergency clinic,” recalled Ralph. “They ran an X-ray on me and immediately shoved me in an ambulance and sent me to the Punta Mita Hospital in Mexico. For the next five or six days,

I don’t remember much of anything.”
The race for a bed
Met with the news that her husband’s heart and kidneys were failing, Sandy watched as Ralph was placed on a ventilator while the medical team at Punta Mita Hospital worked to clear an infection that had developed in his lungs.


Scan the QR code to watch a video interview with Ralph Kruse about his experience.
"We’ve been married for 52 years, and glad to be sitting here and looking at 53," said Ralph.



With 80% failure in one lung and 60% in the other, Ralph remained on the ventilator for six days. Meanwhile, an echocardiogram revealed that his aortic heart valve was failing.
Following this discovery, the cardiologist got the Kruse couple together, advising them to try to get Ralph back to the United States for a transcatheter aortic valve replacement (TAVR), which the hospital in Mexico was not equipped to do.
“I got on the phone right away. The doctors had told us they thought we should try to get back within 72 hours,” said Sandy. “We were checking in Dallas, Houston, San Antonio, Phoenix and Tucson, and couldn’t find a


hospital that would accept him. I was thinking, ‘Where are we going to go? We don’t know where we’re going.’”
After four days of desperately searching for an open hospital bed, Sandy remembered the business card she was given, took a chance, and called Shelley Paris, RN, at the Monument Health Heart and Vascular Institute.
“I remember answering the phone, and I could hear the desperation in her voice,” said Shelley. “I’ve always been a patient advocate. So, when a patient calls needing something, it’s never been in my vocabulary to say, ‘That’s not my job.’”
Guided by this dedication to patient advocacy, Shelley worked with Dr. Pradhan and caregivers at Monument
“I’ve always been a patient advocate. So, when a patient calls needing something, it’s never been in my vocabulary to say, ‘That’s not my job.’”
SHELLEY PARIS, RN, ON THE COORDINATION OF RALPH’S CARE
Ralph with his caregivers at Punta Mita Hospital in Mexico. Ralph’s arrival in Rapid City via air ambulance.
“We’re so fortunate to have Monument Health here, and to have the Heart and Vascular Institute. We can stay right here in the Black Hills for the best care in the world.”

Health to find an open bed, allowing the couple to come back to Rapid City.
The Kruses were finally coming home.
The journey home
After nearly three weeks at the Punta Mita hospital, the Kruses were met with an air ambulance and Sandy watched as Ralph was carried onto the plane before she boarded for their journey to Rapid City Hospital.
“It’s where I wanted to go in the first place,” Sandy said. “I didn’t want to go to Dallas, Houston or one of those other places.”
“By the time we got to the hospital, they were prepared and waiting for us,” she remembers. “They even had a person on staff that spoke Spanish to coordinate with the hospital in Mexico, and the nurses in Rapid City had the room ready.”
While the medical care team worked to stabilize Ralph,
Dr. Pradhan and Joseph Tuma, M.D., FACC, FSCAI, scheduled the TAVR procedure he needed.
“He had the TAVR, and everything went great. By Wednesday, Jan. 24, he was discharged after 33 total days at both hospitals. Just getting back here saved his life,” said Sandy.
Exceptional care, lasting impact
Today, Ralph is doing well with a clean bill of health.
“We’re so fortunate to have Monument Health here, and to have the Heart and Vascular Institute,” said Ralph. “We can stay right here in the Black Hills for the best care in the world.”
As for Shelley, the Kruses credit her for being the catalyst that helped to save Ralph’s life.
“We had a follow up with them, and when I went out, Sandy jumped up and hugged me,” recalled Shelley. “Tears were in my eyes, and Ralph said, ‘You’re our angel.’ I’m just a nurse, but Ralph called me an angel.”
RALPH KRUSE


THE SWEET SPOT
Megan Winter, RN, discovers her ideal role at Monument Health through helping patients.
Story by Stephen Simpson
Photo by Riley Winter
There’s a reason that when someone discovers a place of thriving it’s called a sweet spot. That place in life is where passion meets service. Finding it comes from trial and error, but once a person lands there — well, it’s sweet. Megan Winter, RN, is a portrait of uncovering that place in life.
A nurse with Monument Health Dermatology in Rapid City, Megan felt a deep desire to use her life to serve those around her. “I always knew I wanted to help people,” she said, “specifically in the medical field. And in nursing, you really get to make an impact on your patients. That’s always been really important to me.”
Megan is excited for the opportunity to make a difference in the lives of people in her hometown. She was born and raised in Rapid City, attended Central High School and graduated in 2015. She earned her bachelor’s degree in nursing from the University of South Dakota in May of 2020, so Megan started her nursing career in a crucial time in health care. “I joined the nursing field in the midst of the COVID-19 pandemic,” she said, “so that was definitely a learning curve.” This tumultuous time in medicine was a challenge for Megan and other caregivers, but it also galvanized her call to serve people.
Expressing yourself
Today, Megan is a wife and a mother. Her daughter turned 1 this year. “She keeps me pretty busy,” she shared. Megan and her family love spending time outside, enjoying their beautiful Black Hills surroundings. “We try to stay pretty active,” she said. Her family also expresses themselves through cooking.
Megan also finds joy in fashion. “When I’m not in scrubs, then I try to express myself with fashion, and I think it’s a fun way to express who you are as a person, and it makes you feel good about yourself.”
Knowing the truth of your passion is vital when searching for your sweet spot in life. Megan is attuned to her heart of service. She is also in touch with her life outside of work. So, with a few adjustments, Megan was able to transform her nursing career from a fulfilling and challenging job to a calling.
Finding your sweet spot
One of the reasons that Megan originally chose to pursue nursing as a career was for its adaptability. “There’s always job stability, and there’s so many different ways you can use your degree,” she said. “There's teaching, if you want to go that way. There’s different specialties to pursue. You can also go into research. These options always made me feel comfortable because I knew that I didn’t have to be stuck in one area of nursing if I ever wanted to change my focus.”
Megan started as a nurse in the progressive care unit. “I was there for almost a year, and then I decided it was time for a change,” Megan recounted. “I wanted something with a more balanced schedule, so I was drawn to the dermatology clinic.”

“I always knew I wanted to help people, specifically in the medical field. And in nursing, you really get to make an impact on your patients.”
MEGAN WINTER, ON CHOOSING HER CAREER IN NURSING
Serving others
The sweet spot — that place where going to work is fun and fulfilling: that’s what dermatology is for Megan. “I’m so grateful to work alongside such amazing health care professionals. Our team is very close, and we all support one another. We help each other to grow each and every day,” she said.
Dermatology is an opportunity for Megan to flex her care muscles and help people optimize their health. “We do a lot of patient education and love to include patients in their care, which is very important,” she shared.
Megan enjoys connecting with patients, and she’s had the joy of forging some meaningful relationships. “I’ve been with Dermatology now for a little over three years,” she said. “We get to see patients on such a regular basis. There’s a couple who come in every four to six months for their routine skin exams, and they always remember a little bit about me — things about my family, my husband and they’d always ask what was new. I really enjoy catching up with them and I really appreciate that they remember those things about me.”
The variety that comes with working as a dermatology nurse is thrilling for Megan. “Dermatology is pretty unique because we don’t just do regular clinics. We also do outpatient surgery.” These surgeries are a special chance for Megan and her fellow caregivers at the Dermatology Clinic to offer some special care to patients.
“Surgery days are my favorite,” she said. “We really get to be hands-on in patient care. There are some cases where patients are in our clinic for Mohs surgery for over four hours.” Some of these surgeries involve skin cancers, which can be a rattling experience for patients. “We get to comfort them,” Megan said. And for Megan and others who have found their sweet spot, providing that kind of fulfilling care is a gift to the world.
Michael Huot, M.D.
Chief of Staff, Monument Health
Director of Pain Management, Monument Health
Anesthesiologist, Monument Health


Scan the QR code to learn more about Dr. Huot.
My Role

“I also want to continue to advance a health care culture that is not only medically excellent, but also compassionate and kind.”
I am a Rapid City local and I started part-time as a transporter at Monument Health in 1999 through college until 2003. I did rotations here as a medical student from 2005-2007. After residency in New York, I returned in 2011 and have worked here ever since. As an anesthesiologist, I provide perioperative (mid-surgery) care to some of the most complex cases in the area. As Director of Pain Medicine, I facilitate high-quality pain treatment through a multimodal, patient-focused approach. I am also Chief of Staff, so I sit on the hospital Board of Directors and work to assist our medical staff in providing excellent quality care.
My Goal
I am active in increasing quality in our organization, from helping to write bylaws, to being credentials chair for 5 years, to now being Chief of Staff. We have elevated from a 1-star hospital to 3 stars and I believe we can continue to improve on this journey toward excellence. My professional goals are to continue excellent anesthesia care and to expand our Pain Management Clinic to better serve outlying communities. I also want to continue to advance a health care culture that is not only medically excellent, but also compassionate and kind.
My Passion
One of my passions is helping chronic pain patients in our community. These patients live in pain and it is a terrible disease to have. Every day we help patients get their life back.
I’m a Clinical Associate Professor and I am passionate about teaching future physicians how to deliver excellent compassionate care that focuses on treating the whole patient.
My Life
I have been married for 25 years. I have three kids and one grandchild. I love to spend time with my family. My three kids, in-laws and other siblings all live in the same neighborhood. There are more than 30 Huots within a half-mile of one another!
My wife and I recently purchased a sailboat and I am eager to get back out onto the water. We also love camping in our 1977 Volkswagen camper bus, taking care of our bees and gardening in our greenhouse. I am also an avid cyclist. If it has wheels and pedals, I enjoy it!
I am very active on TikTok. I currently have 87,000 followers and 18 million video views. It gives me a platform to encourage others in so many ways!
MICHAEL HUOT, M.D, ON HIS PROFESSIONAL GOALS

A TEAM APPROACH
Story by Stephen Simpson Photos by Bob Slocum
Roger DeRaad, NP
Matt Gross, CNP
Kim Hayden, PA-C
Advanced Practice Providers demonstrate that patients at Monument Health benefit from a team approach to care.
There’s an old cliche that states that the word “team” stands for “together, everyone achieves more.” This statement might be overused, but its message rings true in many aspects of life. At Monument Health, teamwork is at the foundation of patient care. This optimized model is perhaps most evident when considering the vital role of an Advanced Practice Provider, or APP, also called a mid-level practitioner, plays in collaborating with physician and patients.
“Of course patients all want to visit with the physician who opened up their chest to save their life. But in cardiology, it takes a team of people,” explained Roger DeRaad, NP, the very first APP hired at the Heart and Vascular Institute (HVI). “When a person first sees a middle-level practitioner, many people might think, ‘How is this person different from a doctor? Or how do you fit in?’ I think the best answer is that we are part of the bigger team.”
A Strong Background in Health Care
APPs and physicians play two distinct but very connected roles in care. Physicians are the experts in their fields at Monument Health. APPs are well-trained providers who direct changes in medication, changes in the plan of care, and order further testing to further the care a patient is receiving. There is a tremendous amount of communication and collaboration between the physician and the APP to ensure the patient is receiving the best possible treatment.
Matt Gross, CNP, elaborated on his role at HVI, “We have backgrounds in preventive medicine. We have backgrounds and training in knowing how to help patients navigate lifestyle choices that can help prevent a second or third event from happening.” Treating the entirety of a person and working to prevent future conditions is nearly impossible outside of the context of a team. That’s why caregivers like APPs are so crucial.
Patient Education
One of the most impactful ways APPs help to make a difference in the long-term health of patients is through education. Kim Hayden, PA-C, shared that patient
LOCALLY GROWN
Both Kim and Matt were born and raised in Rapid City. Matt was even born at the Rapid City Hospital. He said, “It’s an honor to be trusted with the care of fellow community members. It’s been really cool taking care of several people who have helped me as I’ve grown up.”
education is key to her and other APPs’ roles; education is also a passion of hers. “The most satisfaction I find in my role is from educating patients and from making patient contact,” she said. “Helping patients understand potentially complex medical issues and translating that in a way that is digestible for them is one of the things that APPs really excel at.”
Heart and Vascular Institute Team APPs really shine in a context like Monument Health’s Heart and Vascular Institute to the immense benefit of their patients. “Heart and Vascular is a very, very strong team,” Matt said. “Our group of nearly 30 APPs has been very stable; a lot of us have been here a long time and we’ve accrued a lot of knowledge together.”
When a patient is visited by an APP at Monument Health, they can feel assured in that strength and stability of the care team. These advanced providers are proud to take patient connection a step further and make a difference in their patients’ lives. “I have complete confidence in each and every APP on this team,” Kim shared. “We are a solid group – every caregiver here is top notch.”
Matt and Roger perhaps paid their team the ultimate compliment: “If I ever needed open heart surgery and I was out of the area, I would travel back here to get it done,” Matt said.
Roger added, “As I approach 65, I’m becoming more interested in what health care in our community is like. And I can confidently say that I trust our caregivers, which is a great place to be.”

JUNE’S BLOOM: A RENEWAL IN FAITH
Story by Kory Lanphear
The tiny town of Faith, South Dakota, is perhaps best known as the location of the discovery of the most complete Tyrannosaurus Rex skeleton yet found, nicknamed Sue. But there is still one tough, old bird who is bound and determined not to end up as just another fossil.
June Kilby is well aware of the benefits of a restoration. After all, in her spare time she renovates and flips trailer homes in Faith. The 78 year old prefers to stay busy and she’s always on her feet, even when it meant ignoring debilitating pain in her ankle.

“Well, I actually retired three times. It lasted about six weeks. I didn’t like it,” June said. So, she unretired and taught school for three years, then moved on to road construction. Finally, June settled on a full-time job as a waitress and bartender. “And that’s what I still do today.”
Fusion refusal
Just a short six months ago, the pain in June’s ankle was starting to take its toll on her ability to stay active. “My ankle has had a lot of trauma. It was broken once, and I was born with kind of a goofy joint. I reached a point where it was just, ‘Oh my goodness. I need to have somebody look at this.’”
June scheduled a consultation with podiatrist Colin Zdenek, DPM, FACFAS, one of the newer physicians at Monument Health Spearfish Clinic. With extensive training from his Silicon Valley Reconstructive Foot
Photos by Bob Slocum
and Ankle Fellowship, Dr. Zdenek’s surgical expertise covers a wide range of foot and ankle deformities, including chronic ankle instability, tendon injuries, flatfoot and high arched reconstructive surgery, bunion and hammertoe correction, and the list goes on.
Upon examining June, Dr. Zdenek discovered that she had developed chronic ankle arthritis, which was likely exacerbated by the previous injury to her ankle. “She had a difficult time getting through her shift on a daily basis. She was unable to perform her usual activities without pain or discomfort,” Dr. Zdenek said.
June could either slow down and learn to live with the pain, or undergo surgery to alleviate her suffering once and for all.
Dr. Zdenek proposed two surgical options: an ankle fusion — a surgical procedure where bones are compressed together to reduce inflammation and pain — or a total ankle replacement, also called an arthroplasty. June elected to undergo the total ankle replacement, because an ankle fusion would have meant an extensive recovery time with no activity. For June, that meant there would be a lot of sitting around, which would have been unbearable.
Dr. Zdenek agreed with June’s decision: “Total ankle replacements are a great alternative to an ankle fusion because patients can begin weight bearing at a much earlier date.”
A burning desire
In an ankle arthroplasty, damaged organic parts of the ankle are replaced with inorganic material like plastic, steel or even ceramics. Dr. Zdenek obtained a threedimensional CT scan of June’s ankle, which was then sent to engineers so they could create a cutting guide system


To learn more about Dr. Zdenek, scan the QR code.

specifically for June’s ankle.
“A 3D printed model is sent to my office so that June was able to visually see how the implant would be placed,” he said.
June was relieved that Dr. Zdenek made sure that she absolutely understood what the procedure was, why he was doing it and how he was to perform it. “And from somebody that doesn’t like a hole poked in them, that was so comforting to know that I wasn’t going to be held up, because we live in the country and I do a lot of country things. Can’t be tethered,” she said.
June said she hardly noticed any discomfort during the recovery because she was so accustomed to the pain from her former injuries. In fact, the hardest part was sitting still in her recliner. “I think I was in that chair for about two and a half months,” said June. She fantasized about ridding herself of the memory — and the recliner — via symbolic ceremony. “I’m burning it in the driveway and getting a new one!”
Recliner declining
Six months after the ankle replacement procedure, June credited Dr. Zdenek and the ankle arthroplasty for restoring her to her full activity levels. Her ankle has felt so good that she has started planning to build a greenhouse by hand from scrap pallets; a project which she said she never would have been able to undertake before the procedure.
As for the fate of June’s recliner, she may have to make other plans. “My husband won’t let me burn it in the driveway,” she said with a laugh. “He’s like, ‘Why don’t you just sit down and read a book?’”
Welcome our newest physicians

CARDIOLOGY
Moinuddin Syed, m.d., is a board-certified and fellowship-trained interventional cardiologist at the Heart and Vascular Institute. Dr. Syed completed his medical degree at Deccan College of Medical Science in Telangana, India and his residency in internal medicine at John H. Stroger, Jr. Hospital of Cook County in Chicago. He has completed fellowships in Cardiology at West Virginia University, Interventional Cardiology at Boston University and Vascular Diagnostic and Intervention at Mount Sinai Hospital in New York, N.Y. He is certified by the American Board of Internal Medicine Cardiovascular Disease, American Board of Internal Medicine, National Board of Echocardiography and the Certification Board of Nuclear Cardiology.

EMERGENCY MEDICINE
Justin Orren, d.o., is an Emergency Physician at Monument Health Spearfish Hospital. Dr. Orren pursued residency at Kansas City University’s Graduate Medical Education Consortium via Freeman Health in Joplin, Mo. Previously, Dr. Orren attained a doctorate at University of Pikeville - Kentucky College of Osteopathic Medicine and a Bachelor of Arts in Biology with Chemistry and Social Sciences minors at University of North Texas in Denton.

HOSPITAL MEDICINE
Julie Hoffmann-Janisch, d.o., is a Doctor of Osteopathy at Monument Health Rapid City Hospital. Trained at Western University of Health Science Pomona, Calif., Dr. Hoffmann-Janisch completed residency and internships in Internal Medicine at Maricopa Medical Center in Phoenix, Ariz. and obtained a Bachelor of Science in Sociology and a Bachelor of Arts in Chemistry, both from Arizona State University in Tempe. Dr. Hoffman-Janisch has also worked as a Locums Hospitalist in such diverse areas as Washington, Kansas and Missouri.

HOSPITAL MEDICINE
Jorge Aguilar, m.d., is a boardcertified Doctor of Internal Medicine at Monument Health Rapid City Hospital. Dr. Aguilar attended Medical School at Universidad Nacional Autónoma de Honduras in Tegucigalpa, Honduras, completed residency at Loyola Medicine-MacNeal Hospital in Berwyn, Ill., and was the Chief Resident of Internal Medicine, at Griffin Hospital in Derby, Conn. Dr. Aguilar has an Obesity Medicine Fellowship through Columbia University Vagelos College of Physicians and Surgeons in New York, N.Y.

INFECTIOUS DISEASE
Andrea Calderón, m.d., is a boardcertified Infectious Disease Specialist at Monument Health Rapid City Hospital. Dr. Calderón completed an Infectious Disease Fellowship at Cleveland Clinic Main Campus in Ohio, and Internal Medicine Residency at Cleveland Clinic Florida in Weston, Fla. Dr. Calderon attained a Bachelor of Science in Biology with a minor in Spanish at University of Texas at Arlington. She is fluent in Spanish.

OBESITY MEDICINE
Kyle Larson, d.o., is a boardcertified family medicine physician specializing in wellness medicine and weight management with the Obesity Medicine and Metabolic Surgery Clinic at Rapid City Hospital. Dr. Larson completed his medical degree at Rocky Vista University - College of Osteopathic Medicine in Parker, Co. and his family medicine residency at Monument Health’s Family Medicine Residency Program in Rapid City. Dr. Larson is also an Associate Clinical Professor at University of South Dakota’s Sanford School of Medicine.

ORTHOPEDICS
Kenneth K. Milligan, m.d., specializes in adult reconstructive surgery and young adult hip preservation surgery. His clinical interests include the anterior approach to total hip replacement, personalized total knee replacement surgery using robotics, and revision hip and knee surgeries. Dr. Milligan graduated from the University of Colorado Medical School in 2016. During his time there, he also earned a master’s degree in Bioengineering with a focus on Orthopedic Biomechanics Modeling. Following medical school, Dr. Milligan completed an internship and residency at Yale University. He trained with some of the leading experts in Direct Anterior hip surgery. He served as a guest lecturer for the Yale Engineering Department and mentored students on their senior thesis engineering projects. Dr. Milligan furthered his expertise with a fellowship in Adult Reconstruction and Hip Preservation in Ottawa, Ontario, Canada, where he focused on complex and revision arthroplasty and outpatient total joint procedures. He also treated young adults with hip dysplasia, Femoral Acetabular Impingement (FAI), labral tears, and other hip conditions.
We’re near you
ASSISTED LIVING
Monument Health
Assisted Living
432 North 10th Street Custer, SD 57730
605-673-5588
AUDIOLOGY
Monument Health Rapid City Clinic 4150 5th Street Rapid City, SD 57701
605-755-5700
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
BARIATRICS
Monument Health
Gillette Clinic
620 W Four-J Court Gillette, WY 82716
307-682-1204
Monument Health
Bariatric and Metabolic Institute 1445 North Avenue Spearfish, SD 57783
605-644-4170
Monument Health
Bariatric and Metabolic Institute
353 Fairmont Boulevard Rapid City, SD 57701
605-755-5700
BEHAVIORAL HEALTH
Monument Health Behavioral Health Center 915 Mountain View Road Rapid City, SD 57702
605-755-7200
Monument Health Family Medicine
Residency Clinic
502 East Monroe Street Rapid City, SD 57701
605-755-4060
Monument Health
Lead-Deadwood Clinic 71 Charles Street Deadwood, SD 57732
605-717-6431
Monument Health Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
Monument Health
Sturgis Clinic 2140 Junction Avenue Sturgis, SD 57785
605-720-2600
CANCER CARE
Monument Health Cancer Care Institute
353 Fairmont Boulevard Rapid City, SD 57701
605-755-2300
CARE CENTER
Monument Health
Sturgis Care Center 949 Harmon Street Sturgis, SD 57785
605-720-2400
DIABETES
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
Monument Health
Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
DIALYSIS
Monument Health
Dialysis Center
425 N Cambell Street, Suite 200 Rapid City, SD 57701
605-755-6950
Monument Health Dialysis Center 132 Yankee Street Spearfish, SD 57783
605-722-8110
DERMATOLOGY
Monument Health Gillette Clinic 620 W Four-J Court Gillette, WY 82716
307-682-1204
Monument Health Rapid City Clinic 4150 5th Street Rapid City, SD 57701
605-755-5700
Monument Health
Dermatology
550 East Colorado Boulevard Spearfish, SD 57783
605-717-8860
EAR, NOSE & THROAT
Monument Health
Rapid City Clinic
4150 5th Street Rapid City, SD 57701
605-755-5700
Monument Health
Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
ENDOCRINOLOGY
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
GASTROENTOROLOGY
Monument Health
Rapid City Hospital
353 Fairmont Boulevard
Rapid City, SD 57701
605-755-5700
GENERAL SURGERY
Monument Health
Gillette Clinic
620 W Four-J Court
Gillette, WY 82716
307-682-1204
Monument Health
Rapid City Hospital
353 Fairmont Boulevard Rapid City, SD 57701
605-755-1000
Monument Health
Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
HEART & VASCULAR
Monument Health Gillette Clinic
620 W Four-J Court Gillette, WY 82716
307-682-1204
Monument Health Heart and Vascular Institute
353 Fairmont Boulevard Rapid City, SD 57701
605-755-4300
Monument Health
Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
HOSPITALS
Monument Health Custer Hospital 1220 Montgomery Street Custer, SD 57730
605-673-9400
Monument Health
Lead-Deadwood Hospital 61 Charles Street Deadwood, SD 57732
605-717-6000
Monument Health
Rapid City Hospital 353 Fairmont Boulevard Rapid City, SD 57701
605-755-1000
Monument Health Spearfish Hospital 1440 N Main Street Spearfish, SD 57783
605-644-4000
Monument Health Sturgis Hospital 2140 Junction Avenue Sturgis, SD 57785
605-720-2400
HOME MEDICAL EQUIPMENT STORES
Monument Health Home+
Home Medical Equipment 1635 Caregiver Circle Rapid City, SD 57702
605-755-6150
Monument Health Home+
Home Medical Equipment 1800 N Haines Avenue Rapid City, SD 57701
605-755-9000
Monument Health Home+
Home Medical Equipment 911 East Colorado Boulevard Spearfish, SD 57783
605-717-8930
HOSPICE CARE
Monument Health Home+
Home Health & Hospice 224 Elk Street
Rapid City, SD 57701
605-755-7710
Monument Health Home+
Home Health & Hospice 931 East Colorado Boulevard Spearfish, SD 57783 605-644-4444
Monument Health Home+ Hospice House 224 Elk Street Rapid City, SD 57701 605-755-7710
IMAGING SERVICES
Monument Health Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
Monument Health Custer Hospital 1220 Montgomery Street Custer, SD 57730 605-673-9400
Monument Health
Lead-Deadwood Hospital 61 Charles Street Deadwood, SD 57732 605-717-6000
Monument Health Rapid City Hospital
353 Fairmont Boulevard Rapid City, SD 57701 605-755-1000
Monument Health Spearfish Hospital 1440 N Main Street Spearfish, SD 57783 605-644-4000
Monument Health Sturgis Hospital 2140 Junction Avenue Sturgis, SD 57785 605-720-2400
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783 605-717-8595
Monument Health
Orthopedic & Specialty Hospital 1635 Caregiver Circle Rapid City, SD 57702 605-755-6100
Monument Health
Orthopedic and Sports Medicine 2479 East Colorado Boulevard Spearfish, SD 57783 605-644-4460
INFECTIOUS DISEASE
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701 605-755-3300
INFUSION SERVICES
Monument Health
Infusion Services 2880 5th Street Rapid City, SD 57701 605-755-7700
LAB SERVICES
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
Monument Health
Custer Hospital 1220 Montgomery Street Custer, SD 57730 605-673-9400
Monument Health Lead-Deadwood Hospital
61 Charles Street Deadwood, SD 57732
605-717-6000
Monument Health
Rapid City Hospital
353 Fairmont Boulevard Rapid City, SD 57701
605-755-1000
Monument Health
Spearfish Hospital 1440 N Main Street Spearfish, SD 57783
605-644-4000
Monument Health Sturgis Hospital
2140 Junction Avenue Sturgis, SD 57785
605-720-2400
Monument Health
Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
LIFESTYLE MEDICINE
Monument Health Rapid City Clinic
640 Flormann Street Rapid City, SD 57701
605-755-3300
NEPHROLOGY
Monument Health Rapid City Clinic
640 Flormann Street Rapid City, SD 57701
605-755-3300
NEUROLOGY
Monument Health
Neuroscience Center
677 Cathedral Drive Rapid City, SD 57701
605-755-5000
NEUROPSYCHOLOGY
Monument Health
Neuroscience Center 677 Cathedral Drive Rapid City, SD 57701
605-755-5000
NEUROSURGERY
Monument Health
Neuroscience Center
677 Cathedral Drive Rapid City, SD 57701
605-755-5000
OB/GYN
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
OCCUPATIONAL MEDICINE
Monument Health
Rapid City Urgent Care
1303 N Lacrosse Street Rapid City, SD 57701
605-755-2273
Monument Health
Rapid City Urgent Care 2116 Jackson Boulevard Rapid City, SD 57702
605-755-2273
ORTHOPEDICS
Monument Health Gillette Clinic
620 W Four-J Court Gillette, WY 82716 307-682-1204
Monument Health Orthopedic & Specialty Hospital 1635 Caregiver Circle Rapid City, SD 57702
605-755-6100
Monument Health Orthopedic and Sports Medicine 2479 East Colorado Boulevard Spearfish, SD 57783
605-644-4460
PHARMACIES
Monument Health Home+ Pharmacy
353 Fairmont Boulevard Rapid City, SD 57701
605-755-8184
Monument Health Home+ Pharmacy 1420 North 10th Street, Suite 1 Spearfish, SD 57783
605-717-8741
Monument Health Home+ Specialty Pharmacy
2006 Mount Rushmore Road, Suite 2 Rapid City, SD 57701
605-755-3065
PLASTIC SURGERY
Monument Health
Rapid City Clinic 4150 5th Street Rapid City, SD 57701 605-755-5700
PODIATRY
Monument Health Orthopedic & Specialty Hospital 1635 Caregiver Circle Rapid City, SD 57702
605-755-6100
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
PRIMARY CARE CLINICS
Monument Health Belle Fourche Clinic 2200 13th Avenue
Belle Fourche, SD 57717
605-723-8970
Monument Health Buffalo Clinic 209 Ramsland Street Buffalo, SD 57720
605-375-3744
Monument Health Custer Clinic 1220 Montgomery Street Custer, SD 57730
605-673-9400
Monument Health Family Medicine Residency Clinic 502 East Monroe Street Rapid City, SD 57701
605-755-4060
Monument Health Hill City Clinic 238 Elm Street Hill City, SD 57745
605-574-4470
Monument Health
Hot Springs Clinic 1100 Highway 71 South, Suite 101 Hot Springs, SD 57747
605-745-8050
Monument Health
Lead-Deadwood Clinic 71 Charles Street Deadwood, SD 57732 605-717-6431
Monument Health Rapid City Clinic 640 Flormann Street Rapid City, SD 57701 605-755-3300
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783
605-717-8595
Monument Health Sturgis Clinic 2140 Junction Avenue Sturgis, SD 57785
605-720-2600
Monument Health Wall Clinic 112 7th Avenue Wall, SD 57790
605-279-2149
PULMONOLOGY
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
RHEUMATOLOGY
Monument Health
Rapid City Clinic 640 Flormann Street Rapid City, SD 57701
605-755-3300
SLEEP CENTERS
Monument Health
Rapid City Clinic 2929 5th Street Rapid City, SD 57701
605-755-4000
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783
605-644-4170
SURGERY CENTER
Same Day Surgery Center 651 Cathedral Drive Rapid City, SD 57701
Monument Health Surgery Center 1316 North 10th Street Spearfish, SD 57783 605-642-3113
THERAPIES –PT, OT, SPEECH
Monument Health Inpatient Rehabilitation Center
1050 Fairmont Boulevard, Suite A100 Rapid City, SD 57701
605-755-1230
Monument Health
Rehabilitation 2200 13th Avenue Belle Fourche, SD 57717 605-723-8961
Monument Health
Rehabilitation 1220 Montgomery Street Custer, SD 57730 605-673-9400
Monument Health
Rehabilitation 61 Charles Street Deadwood, SD 57732
605-717-6000
Monument Health
Rehabilitation 2140 Junction Avenue Sturgis, SD 57785 605-720-2400
Monument Health
Rehabilitation 2449 East Colorado Boulevard Spearfish, SD 57783 605-644-4370
Monument Health
Orthopedic & Specialty Hospital 1635 Caregiver Circle Rapid City, SD 57701 605-755-6100
TRAVEL MEDICINE
Monument Health
Rapid City Clinic 640 Flormann Street
Rapid City, SD 57701 605-755-3300
Monument Health Spearfish Clinic 1420 North 10th Street Spearfish, SD 57783 605-717-8595
URGENT CARE CLINICS
Monument Health Rapid City Urgent Care 1303 N Lacrosse Street Rapid City, SD 57701 605-755-2273
Monument Health
Rapid City Urgent Care 2116 Jackson Boulevard Rapid City, SD 57702 605-755-2273
Monument Health
Lead-Deadwood Urgent Care Services 71 Charles Street Deadwood, SD 57732 605-717-6431
Monument Health Spearfish Urgent Care 1420 North 10th Street Spearfish, SD 57783 605-717-8595
Monument Health
Sturgis Urgent Care Services 2140 Junction Avenue Sturgis, SD 57785 605-720-2600
UROLOGY
Monument Health
Rapid City Clinic 2805 5th Street Rapid City, SD 57701 605-755-5700
WOUND & OSTOMY CARE
Monument Health
Rapid City Clinic 2929 5th Street Rapid City, SD 57701 605-755-1309
Monument Health Spearfish Clinic 1445 North Avenue Spearfish, SD 57783 605-644-4170
ISSUE 16, FALL 2024 // COMPASSION
DOWN
1. Megan Winter, RN started her nurse career in the ________________ care unit
2. Dillon Robbins suffered a diffuse ___________ injury
3. __________ “Valley” of Dr. Zdenek’s Reconstructive Foot and Ankle Fellowship
4. TAVR = trans________________ aortic valve replacement
6. ___________ of Pain Management, Dr. Michael Huot
9. The object of June Kilby’s “burning desire”
12. Monument Health Gold stroke award Get ______ ____ Guidelines
14. Karen M. ________________ Department of Chemical and Biological Engineering
15. Ralph and Sandy Kruse’s “Puerto” place of winter in Mexico
ACROSS
1. The “P” in Roger DeRaad, NP
5. Matthew ________________, 1980s one hit wonder
7. Sue, the skeleton of a Tyrannosaurus Rex, was discovered in this small town
8. In alphabetical order, the first names of Dillon Robbins’s ICU nurses
10. After summer, before winter
11. Dr. Huot’s recently purchased watercraft
13. Monument Health Heart and _________________ Institute
15. Aka the answer to 13 across
17. SD BRIN, South Dakota Research Infrastructure
18. Acronym for Anna Whetham’s syndrome diagnosis
19. Brunmaier’s unpunctuated education credentials
20. Aka “party” for Golden Guitars
21. A common autoimmune disorder
22. _________________ “Cuff” shoulder surgery
16. 100 mile ______ marathon
19. Joint ______, a common symptom of autoimmune disorders
October
October
October
October
October
November
December


