Emergency Department Technician, Kaylan Harrington has served her country since 2001. Now she’s helping homeless veterans in an unexpected way — donning an evening gown.


Emergency Department Technician, Kaylan Harrington has served her country since 2001. Now she’s helping homeless veterans in an unexpected way — donning an evening gown.



RAPID CITY:
Audiology & Ear, Nose and Throat
4940 5th Street, Rapid City, SD 57701 605-755-4100
SPEARFISH:
Audiology & Ear, Nose and Throat
Spearfish Clinic | 1445 North Avenue, Spearfish, SD 57783




605-644-4171
monument.health/ent
Jay W. White D.O., MS, HCA Rapid City Robert Burgess M.D. Rapid City Loren Jones M.D. Spearfish Jeanette Carlson CNP Spearfish Richard Bowen M.D. Rapid City


RAPID CITY:
Audiology & Ear, Nose and Throat
4940 5th Street, Rapid City, SD 57701 605-755-4100
SPEARFISH:
Audiology & Ear, Nose and Throat
Spearfish Clinic | 1445 North Avenue, Spearfish, SD 57783 605-644-4171
monument.health/audiology
Denise Byrd Au.D Spearfish Felicia Beltman Au.D Spearfish Merrill Hill Au.D. Rapid City President and Chief Executive Officer, Monument Health
President and Chief Executive Officer, Monument Health
Flipping through the pages of this issue of Monument Health Magazine, I think you’ll find that there is a consistent theme — service. The individuals featured in this issue have served others — their country, their community and their loved ones.
You’ll have an opportunity to get to know the brilliant woman on the cover, Kaylan Harrington, who served in the U.S. military for her entire adult life. She recently decided to help fight homelessness among veteran women by entering the Ms. Veteran America competition, and was named first runner up — all while attending nursing
school. We’re proud that she works for Monument Health.

Another story worth exploring is that of Ben Ericks, who came into this world with the tragic death of his biological mother. Ben could have grown up bitter and angry, but he didn’t. Instead he became a kind, generous man, who dotes on his wife and children and serves his country in the South Dakota National Guard.
Service comes in many forms, and in this issue you can also read about Deb Fredrich, one of our amazing volunteers. She has spent more than 10,000 hours helping individuals in hospice care, and she plans to do it, in her words, forever.

You’ll also meet James Woodhead, BSN, the Director of Nursing for the Custer Hospital and Clinic, and learn how important the community of Custer is to him in his role, and Don Wood, who struggled with a serious case of COVID-19, only to recover more fully than anyone could have expected.
We hope you enjoy these stories and more in this issue of Monument Health Magazine — it is a privilege to share them with you. As always, we welcome your feedback, story suggestions and questions about health care. Send your thoughts to us at magazine@monument.health.
Managing Editor
Melissa Haught
Editor
Stephany Chalberg
Senior Writers
Wade Ellett
David Scott
Contributors
Karlee Baumann
Jennessa Dempsey
Dawn Kocina
Ronda Neugebauer
Anna Whetham
Art Director
Stacy Brozik
Layout
Terri Upward
Photographer Bob Slocum
Social Media Manager
Breanne Brimm
Production courtesy of Rapid City Hospital
Volunteer Auxiliary
©Monument Health Magazine. All rights reserved. Reproduction of any part of this publication without the expressed consent of the publisher is prohibited. The information included in this publication is believed to be accurate at the time of publishing. Additional articles are available online at magazine.
monument.health Monument Health Magazine is a free, quarterly publication distributed throughout the Black Hills. Follow us on Facebook and Instagram for updates.
SPRING 2023
In Case You Missed It
This is our roundup of all the latest news and happenings throughout Monument Health. page 4
Awareness Months
Highlights of key health issues and medical staff. page 6
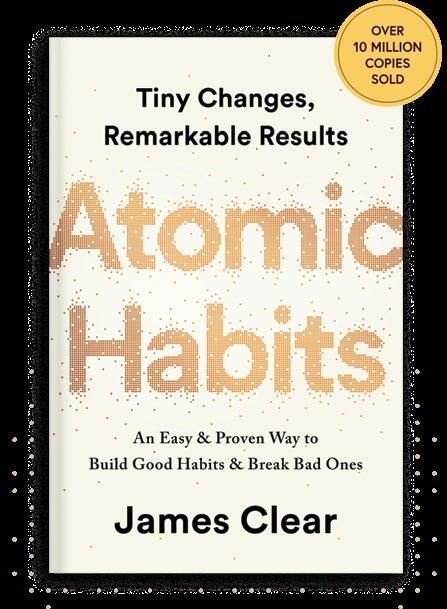
What I’m reading and listening to Monument Health caregivers share the books and podcasts they’re loving right now. page 7
My Space
Paige Whitacre is the manager of the communications center and security dispatch center. Her team acts as the nervous system of Monument Health, connecting the right people at the right time to avoid emergencies. page 9

Ask the Doc Sniffing and sneezing this time of year? You’re not alone. Ear, nose and throat physicians explain the difference between asthma and allergies, and how you can breathe a little easier this time of year. page 10
Volunteer Profiles
Donna Kluthe & Deb Fredrich pages 13 & 14
Finding his calling
James Woodhead, BSN, didn’t always know he wanted a career in health care, but found success in nursing. He has helped make Monument Health a great place to work as the Director of Nursing for the Custer Hospital and Clinic. page 16

Serving her country:
In combat boots or a crown Kaylan Harrington has served her country for her entire adult life. Now, this soldier is fighting homelessness among veteran women with an unexpected weapon — an evening gown. page 20
Leaving on a jet plane
With spring break and summer vacation plans on the horizon, a little preparation can go a long way to ensure your trip is worth writing home about. A clinical dietitian and pharmacist weigh in on the important steps to consider when traveling. page 25
The miracle of recovery
At one point, Don Wood didn’t know if he would regain his independence. With the help of a care team who wouldn’t give up, Don’s recovery is nothing short of a miracle. page 28
Becoming Ben
Ben Ericks came into this world with the death of his biological mother. His birth may have been tragic, but his life has been anything but, thanks to the love of his family. page 31
My Space
Monument Health creates a VIP experience for its patients coming to Rapid City Hospital. Danny Morris, Lead Valet, explains how this curbside service supports a positive experience. page 35

Physician Spotlight
Meet Derek Buck, M.D., D.C., an interventional and spine care specialist, physiatrist at Monument Health Orthopedic & Specialty Hospital. page 36
APP Spotlight
Meet Chris Barrozo, PA-C, a physician assistant at Monument Health Orthopedic & Specialty Hospital. page 37
Introducing
Get to know physicians who have recently joined Monument Health. page 38
Calendar
Upcoming events at Monument Health. page 39
Directory
Find a Monument Health provider near you. page 40
The Monument Health Heart and Vascular Institute’s Structural Heart Team completed its 500th transcatheter aortic valve replacement (TAVR) procedure on Oct. 25, 2022. TAVR is a minimally invasive heart procedure to replace a thickened aortic valve that cannot fully open.

The Structural Heart Team performed the first TAVR in Rapid City in 2014. This procedure was initially recommended for patients deemed too high-risk for surgery,
but it is now approved for all patients with symptomatic aortic stenosis, regardless of surgical risk. TAVR is the latest of Monument Health Structural Heart program’s efforts to use the most advanced transcatheter technologies.

Since 2013, the Structural Heart Team has implemented several treatments, including left atrial appendage occlusion and balloon mitral valvuloplasty (BMV) among others.
THE MONUMENT HEALTH HEART AND VASCULAR INSTITUTE WAS ONE OF ONLY 10 CENTERS IN THE UNITED STATES SELECTED FOR PARTICIPATION IN CLINICAL TRIALS TO EXPAND TAVR II.

Brad Haupt, Vice President of Supply Chain and Contract Management for Monument Health, received the 2022 Friend of Transit Award from the Dakota Transit Association. This award recognized his efforts working with Prairie Hills Transit providing affordable transportation for Monument Health patients and nursing home residents during the COVID-19 pandemic.
The Friend of Transit Award is given to an individual, business or agency from both North and South Dakota who has done an outstanding job in supporting transit in their communities or state. Nominees range from volunteers to state legislators and cannot be paid or employed by a transit entity. Haupt was nominated by Barb Cline, Executive Director of Prairie Hills Transit.
Monument Health expanded its use of robotic assisted technology in the operating room with the Intuitive Ion. The robotic platform allows pulmonologists to perform minimally invasive biopsies and gather tissue samples from areas that would be hard to reach or completely unreachable areas using a thin maneuverable catheter.

Ion provides a planned path based on a patient’s CT scan, allowing physicians to target specific areas of a patient’s lungs. The robot also allows tracking for providers when multiple biopsies are attempted. It was designed to integrate with the existing technology already present in Monument Health’s operating rooms, allowing for higher precision and reducing the risk patients face during procedures.
Lung cancer is the third most common cancer behind breast cancer and skin cancer, and it is responsible for more deaths in the United States than any other form of cancer. Most lung cancer is found in adults 65 years of age or older, but factors such as a history of smoking or vaping can increase a person’s risk.
The COLA Laboratory Excellence Award was given to laboratories at Monument Health Orthopedic & Specialty Hospital and Monument Health Rapid City Urgent Care, Jackson Boulevard. Accreditation is given to laboratories that apply the highest standards of quality in day-to-day operations, demonstrate continued accuracy in the performance of proficiency
testing and pass a rigorous on-site laboratory survey. The Excellence Award is presented to only 11 percent of surveyed labs.
COLA is a leading national laboratory accreditor, whose program and standards enable clinical laboratories and staff to meet U.S. Clinical Laboratory Improvement Amendments (CLIA) and other regulatory requirements.
In April, we observe Occupational Therapy Month. At Monument Health, our occupational therapists play a vital role in improving the lives of our patients by helping them rehabilitate after an illness or injury. The occupational therapy team works closely with physical therapy and speech therapy to help patients learn, or re-learn, vital life skills like activities of daily living, home safety and energy conservation, among many others.
MAY IS WOMEN’S HEALTH MONTH
and a time to recognize the demands women face every day. There is no better time to empower and encourage women to make their health a priority. In May, we look at the benefits of living a healthy lifestyle and the ways managing women’s health care needs benefit women at every stage of their lives. This can mean scheduling necessary screenings and check-ups, living a more active and balanced lifestyle or checking in on mental health needs.
JUNE IS MEN’S HEALTH MONTH
and a time to recognize and address men’s physical and mental health care needs.
According to the CDC, 13 percent of men 18 years of age and over are in fair to poor health. It is important for men to understand their individual risks and health care needs at every stage of life. Men should take the time to schedule any screenings they need and make sure they are living an active and balanced lifestyle.
In May, we recognize Mental Health Awareness Month and work to break the stigma surrounding mental health. More than half of Americans will be diagnosed with a mental illness or disorder in their lifetime. One in five will struggle with mental illness this year. Mental illness can affect anyone and has a wide variety of causes and symptoms. Many conditions fall under the umbrella of mental illness, including anxiety, depression, substance abuse, PTSD and more. Battling mental illness is nothing to be ashamed of, and neither is seeking professional help. It’s okay to not be okay. Help is out there, and anyone experiencing a mental health emergency can call or text 988 to reach the suicide and crisis lifeline.
MAY 6-12, 2023
Nurses Week is celebrated May 6-12. During this week, we recognize and celebrate the critical role nurses have in providing high-quality patient-centered care. Nurses can be found performing a wide variety of tasks in every specialty across the health care industry.
A career in nursing starts with heart, and nurses use their wide range of knowledge to help people feel better during some of their most difficult times. Nurses across Monument Health have been recognized for their excellence through national awards like the DAISY Award, as well as locally through the STAR Awards. From our clinics to our specialty hospitals, our nurses work tirelessly to ensure patients’ health and well-being.
In May the sun is out longer, the weather warms up and people spend more time outside. This makes it the perfect time to recognize Skin Cancer Awareness Month. Skin cancer is the most common cancer in the United States. It is important to protect your skin all year. When working or playing outside wear sunscreen, long clothes, a brimmed hat and sunglasses that block UVA and UVB radiation.

Monument Health physicians and caregivers share what books and podcasts they’re enjoying.

Small changes are lasting changes — those small changes become habits that, according to author James Clear, are key to success. Atomic Habits is a comprehensive and practical guide on how to create good habits, break bad ones and get one percent better every day, all by making small changes.
 by Bessel
by Bessel
van
der Kolk, M.D.Bessel van der Kolk, M.D., uses scientific advances and modern research to explain the effects that trauma has on the body and the brain. In The Body Keeps the Score, van der Kolk shows how these effects can compromise the capacity for pleasure, self-control and trust. He also explores what readers can do to overcome the effects of trauma, including yoga, neurofeedback, meditation and sports, in order to activate the brain’s neuroplasticity.
Co-hosts Jamie Rathjen and Teresa Kenney want to be a voice of hope for women across the world. Their mission, in their own words, “is to inspire a new generation of women who are educated and informed about the gift and beauty of the feminine design.” The emphasis of this podcast is a holistic approach to women’s health care, providing resources for women to understand their own bodies and become geniuses when it comes to their hormones.
The Hidden Brain explores the thoughts and patterns that shape our behavior and decisions even when we don’t know that they’re there. Host Shankar Vedantam blends science and storytelling to dive into how we think and navigate the questions that lie at the heart of our complex and changing world.
Hosts Forrest Hanson and his father, clinical psychologist Dr. Rick Hanson, are joined by world-class experts to explore well-being, and how we can use practical science to feel, live and be better. Psychology, science and contemplative conversations are at the heart of this podcast, with an emphasis on how the listener can develop greater inner strength, overcome adversity and get the most out of life.

The Communications Center is a 24/7, 365-day operation and plays a crucial role in keeping everyone connected and informed of emergency situations.
The Communications Center caregivers answer around 33,000 calls per month — this includes about 4,600 emergency calls. Emergencies include paging physicians and caregivers if a patient is having an emergency, when critical tests results are ready, if security is needed or if there is a natural disaster. The Communications Center responds to emergency situations to ensure they are communicated to the proper teams, such as a Rapid Response or Fire.
I am privileged to partner with caregivers and providers from all specialties across our system to help communicate any emergencies and work through any process improvement opportunities. My teams are part of Safety Services, which means when an emergency call comes in, all other calls go on hold.


To provide support to our community, patients and caregivers through compassion. Our willingness to relieve the suffering of others builds trust with each other and our community. We do that by listening and taking appropriate action to get them the help needed. Most people who call the hospital are looking for help; my goal is to live up to that basic expectation.
My Passion
My passion is being prepared for emergency situations and knowing our hospitals are prepared. I love the partnership between so many departments to help support their communication needs when it’s most important. I enjoy being part of something with such a huge impact, yet totally behind the scenes. The heart of everything we do is for the people
In 1984, the Asthma and Allergy Foundation of America declared May National Asthma and Allergy Awareness Month. Otolaryngologists V. Richard Bowen, M.D., and Loren Jones, M.D., answer some common questions about asthma and allergies.


What is asthma?
Loren Jones, M.D.: Asthma is an inflammatory disease in the lungs that impacts the small airways or bronchioles. Inflammation of these airways causes them to narrow. It can also cause spasms of smooth muscle in the walls of these airways, which squeezes them and narrows them further. This can cause acute asthma attack symptoms like shortness of breath, cough and wheezing.
What are allergies?
V. Richard Bowen, M.D.: In people with allergies, the immune system identifies allergens — like pollen or certain foods — as dangerous, even though they’re not actually harmful. The result is inflammation of the skin, the sinuses, airways or digestive system. For some people this leads to minor irritation, but for others it can cause life-threatening responses.

How common are asthma and allergies?
Bowen: They are fairly common. Allergic rhinitis, or inflammation of the nose, affects 10 to 30 percent of the population. Some estimates suggest that asthma affects 300 million people worldwide. Roughly 80 percent of asthmatics also suffer from allergies.
Can allergies affect asthma?
Jones: Allergies can certainly affect asthmatics. The linings of the nose, throat, sinuses and lungs are all the same type of mucus membrane tissue and are largely susceptible to similar problems. In the same way that allergens can trigger the immune system to produce inflamed nasal tissues, they can also affect the airways of the lungs. In fact, some medications are used to treat both allergies and asthma.
Do men and women have different rates of asthma?

Bowen: Childhood asthma is more common in boys than girls — by a 3-2 ratio. However, this changes as we age: there are more women than men with asthma as adults, with eight women with asthma for every two men.
What is the most common type of allergy?
Jones: The most common type of allergy is pollen. This can be from trees, weeds and grasses. Allergic reactions to pollen are often referred to as hay fever. Other common triggers include pet dander, molds, dust mites and cockroaches — fortunately we don’t have to deal with cockroaches much in our area. The most common food allergies depend upon age. In children, milk, eggs and peanuts are the most common. In adults, the most common food allergen is shellfish.
Is there anything about western South Dakota that makes allergies and asthma more of a concern?
Bowen: The most problematic allergens, like pollen, are those that travel the furthest in the wind. That means individuals with allergies or asthma may have a problem in windy areas like western South Dakota.
Can allergies develop at any age?
Bowen: Allergies may develop at any age, but it’s most likely through the teens and early 20s. Infant allergies are usually food related or manifest in skin conditions such as eczema. When allergies first occur later in life, it is often because a person is exposed to allergens when their immune system function is compromised — such as when they’re sick or pregnant — or when they are exposed to new allergens.
Are people more likely to have multiple allergies or just one?
Jones: Yes, if you have one allergy, it is more likely you will have others. It’s unusual to test positive to only one allergen, although not unheard of. Since allergies are a function of a misguided immune response, the fact you have one allergy indicates that the immune system may be more likely to develop allergies to other things.
Do allergies ever go away?
Bowen: The good news is, yes, the older we get the less severe allergy symptoms become. Unfortunately, this may not occur until after age 60 for many people. However, for most folks, allergies greatly improve with test-specific allergy shots, or an under-the-tongue therapy. We recommend four to five years of therapy, that may give eight to 10 years — or more — of symptom relief.



LOCATIONS: Monument Health Sports Performance Institute and O’Harra Stadium on the South Dakota Mines Campus
COST:
$199 Camp + Combine

$149 Camp (July 10-July 27 only) + Combine $99 Combine only (25% discount for members)
DAYS/TIMES:
Tuesdays, Wednesdays & Thursdays: 6 - 7:15 p.m.
Saturdays: 10 - 11 a.m.
Camp participants can work out at the Monument Health Sports Performance Institute during business hours

CAMP: JUNE 12-JUNE 30
• Focuses on movement skills integration
• Speed, agility and sport-specific movements
CAMP: JULY 10-JULY 27

• Focus on developing strength and power
• Get your athlete real college weight room experience

COMBINE: JULY 28
Tests include:
• Vertical jump
• Broad jump
• 10-yd + 40-yd dash
• 20-yd shuttle
• 3 cone drill
• 60-yd shuttle
• Bench press with velocitybased training technology
 REGGIE OVERTON Performance Specialist
CHRIS HATHAWAY Performance Coach CARL WISE Performance Specialist FAITH WILSON Performance Specialist KYLE TAYLOR Performance Coach
REGGIE OVERTON Performance Specialist
CHRIS HATHAWAY Performance Coach CARL WISE Performance Specialist FAITH WILSON Performance Specialist KYLE TAYLOR Performance Coach
Donna Kluthe began volunteering at the Rapid City Hospital gift shop in the 90s, but it wasn’t until 2012 that she found her way to wayfinding.


Where do you volunteer, and what are your duties?
My main duty is to escort patients to different areas of the hospital. Some of the areas are MRI, surgery waiting room, Respiratory Therapy and Heart and Vascular. We deliver flowers to the patient rooms. Many of the visitors who come in do not know how to get to patient rooms, and we escort them to the elevator, the ICU or to pediatrics and obstetrics, among other areas.
Why do you volunteer?
Because I am retired and enjoy keeping busy. I like helping people, and it enriches my life. People are very thankful for what we do. What is your favorite part of volunteering?
I enjoy talking with people and making them feel welcome and comfortable when they come in for an appointment or as a visitor. I work with great people who I would never have met outside of volunteering.
Would you recommend volunteering to others?
I tell people that it is a good way to give back to the community and it is a fulfilling, enjoyable experience.
Why is Monument Health a good place to volunteer?
I think volunteers benefit from Monument Health in knowing we are doing something to help someone else. We receive nice perks, like coffee, lunch and coupons from the gift shop for our birthdays. Also, a benefit for me is that I try to walk at least 10,000 steps a day. I can almost get that many during a 4-hour shift, which is why I am always eager to escort patients and visitors wherever they need to go. The busier we are, the more I like it!
Donna Kluthe
Volunteer, Rapid City Hospital
For more information about volunteering or to learn how to get involved, visit monument.health/volunteer or call Volunteer Services at 605-755-8980.
Deb Fredrich wasn’t sure she wanted to be a hospice volunteer, but gently rocking a 2-month-old infant — ill with brain cancer — changed her forever. More than three decades later, she’s still touching lives as a Monument Health volunteer.

When Deb Fredrich first began to investigate hospice care, she just wanted to understand it. Perhaps she was looking to heal a piece of herself and didn’t intend to get wrapped up in it. When she reached out to her local hospice care center, hoping to understand more about death and dying, they offered some educational opportunities which proved more consequential than she first imagined. Eventually, she was asked if she would consider volunteering in the home to work with patients and their families.

“At first I didn’t want to volunteer in hospice, because I knew I couldn’t keep people from dying,” Deb said. “Then I was told they wanted me to visit a baby.”
One leap of faith later, she found herself entering a stranger’s home to visit the child. Her trepidation in the unfamiliar situation melted away once the little one was in her arms.
“This baby was two months old, and I began to visit the family every third day,” she said. “The child was dying of brain cancer, and I asked what I should do. They said, ‘just hold him.’ They just wanted him to be held. It just totally pulled me in. It was totally a God thing, otherwise I would have never volunteered.”
A former Monument Health Auxiliary president, Deb recently received her recognition pin for 10,000 volunteer hours. Along the way, Deb has picked up much more than mere acquaintances and incidental memories. Some of the bonds formed along the way have endured and new friends have become like family. Deb says her time with patients isn’t always somber, in fact it’s often quite the opposite.

“I’ve met so many good people. That’s the fun part. With hospice care, I’m not helping them die, I’m helping them live. There is a patient I have now, we just make each other laugh the entire time.”
Often, in-home hospice patients have family by their side, who may receive a break when help arrives. Hospice care in the home is something many in the position desire, but it can be taxing on the family.
“It’s someone else to visit with, someone else to lend a hand. You’re there for the caretakers, too … the husband or the sibling, because they are there all day.”
Aside from providing a reprieve to those sitting vigil for the patient, Deb said a third party from outside the family can sometimes lift spirits or ease tension by precluding the stigmas around death and hospice.
“A lot of times when you’re dying, people don’t know what to do or what to say. People can get lonely. It’s not about fixing it; it’s about not shying away from it. They may want someone to cry with, or laugh with, but it’s just about empathy. My sister died at age 9 when she was home so in a way, I think that’s where it started, because at that time people were there for us. One patient’s husband asked me, ‘why do you do this?’ And I said, ‘well, somebody did it for me.’”
Although she has worked in the home and also at Monument Health’s Hospice House, Deb has volunteered in other areas.
“I started there and then I volunteered in one of the areas where we connect doctors with the families of patients who are in surgery. In that role, you do a lot of listening. You’re part of the support system. I did that for a few years and now I’m going to the gift shop once per week. The gift shop really is like a ministry in a way. People just want to talk. Everyone has a story and wants their story to be heard.”
Ten thousand hours is a long time to spend doing anything, but to spend it in service to others is a unique undertaking. Ten thousand hours is a long time to spend doing anything, but to spend it in service to others is a unique undertaking. It’s often said that 10,000 hours is the amount of time needed to master a skill. If so, Deb has truly mastered the art of compassion. She said her experience over the years has been ultimately uplifting and restorative.
“I’ll probably do this forever,” she said. “Gratitude is a big one. We’re grateful. My family has been so blessed and it’s nice to give back. I feel like we make a difference but mostly they make a difference in me. It has helped me to listen more attentively. Each situation is different, and I don’t want to have an agenda. I go in hoping to provide whatever they need. One family had a sick baby and the mother was also home with two preschoolers. I ended up being godmother to the family’s next child, and I first came into their home as a stranger. It’s not really me, it’s the Holy Spirit, it’s God working through me.”
Deb Fredrich has amassed 10,000 hours volunteering at Monument Health in various roles, but primarily as an in-home hospice worker. She is also a former president of the Volunteer Auxiliary. The ornament she holds was a gift meant to represent all the lives she has touched in her volunteer career.
GETTING INVOLVED - Volunteers play a vital role in providing a caring experience for our patients and families. If you have a passion for helping others, consider becoming a volunteer. “I always tell people they are part of a legacy of volunteers,” said Konnie Sorenson, Volunteer Services Manager for Rapid City Hospital. “Even before Rapid City Hospital was formed, there was a precedent for community members coming together to aid those in need. We’ve got some awesome people who volunteer with us and keep that tradition alive.” For more information about volunteering or to learn how to get involved, visit monument.health/volunteer or call Volunteer Services at 605-755-8980.
James Woodhead, BSN, Director of Nursing in Custer, went to college in Arizona on a basketball scholarship. He didn’t start school knowing he wanted to be in nursing, but two years into his education he realized he wanted to work in emergency care.
 Written by David Scott Photos by Bob Slocum
Written by David Scott Photos by Bob Slocum
“I made the decision to stop playing basketball and tried to focus on what I was going to do for a career,” he said. “I started volunteering in an emergency room (ER) and got an up-close introduction to nursing. Once I made my decision, I finished my prerequisites and applied to nursing school and got in.” With that, he began his career in nursing.
From his time volunteering, James knew he wanted to work in an emergency room.
“The intensity of the ER is what drew me to it. There is always something different coming through the door. It’s always changing, and it keeps you on your toes,” James said. “You have to be ready for anything, and that really drew me to it. I wanted to be a nurse first, but I knew I wanted to work in the ER. You get to save lives on a daily basis.”
After graduation, James worked at two different health care organizations in Arizona: Banner Health and Tenet Healthcare. He said both felt too big for him. James wanted to work somewhere patients were treated like people — ideally small-town medicine, but with the skills and expertise found in metropolitan hospitals. “I was looking for an organization that was not quite as large, but still had their stuff together. I wanted to work for a system that was smaller, but still established.”
James was on the lookout for a health care system that he fit into, and South Dakota was on the short list. James said, “My wife and I wanted to be in the Black Hills area. We were open to anywhere from Spearfish all the way down to Hot Springs. I had been keeping my eyes open for an opening here for probably a year-and-a-half, but I was really picky.” He had family in the area and was drawn by the beauty of the hills, but he was also looking for the right hospital to make his home.
It only took one interview with Monument Health Custer Hospital for James to know this is where he wanted to expand his career and create a life. “There truly is a family atmosphere. You get to know most of your patients on a personal level, you see them around town, there’s a high level of accountability among everyone here. Everyone truly goes above and beyond to make it a better place for both the patient and for the people who come to work here.”
The community of Custer and Monument Health leadership have invested in the health of the Southern Hills community — that impact was evident to James. Monument Health and the City of Custer partnered to build the $22 million hospital and clinic, which opened in May 2018. It includes
inpatient rooms, clinic care, physical therapy, urgent care services, an emergency department and a healing garden.
“It was clear to see how far along the Custer Hospital was. I could see the dedication to providing the best care to their community. Custer has a lot of resources and an organizational structure that you don’t expect to see in a lot of other critical access hospitals. It strikes the balance between that small town atmosphere with the level of care that comes with a bigger hospital,” James said.
Advice for the next generation of nurses James has found success in the health care field, and his leadership has helped Monument Health become a great place to work. He said one of the keys to success in nursing is being open to feedback. “Always be open to whatever feedback someone is giving you. Even if you’ve heard the same thing several times before, just listen to what that person is saying,” James said. “It builds trust, and they could always give you new information or present it in a new light.”
“You have to be ready for anything, and that really drew me to it. I wanted to be a nurse first, but I knew I wanted to work in the ER. You get to save lives on a daily basis.”
JAMES, ON CHOOSING THE EMERGENCY ROOM AS HIS FOCUS
He also stressed that nursing students shouldn’t get too buried in books. “Really listen to your instructors, especially when you’re in your clinicals, and be more aware of your surroundings.” He stressed that while there is good information in written materials, real-world nursing is dynamic, and instructors will have insights on how to solve problems.
James also said it’s important to work on your people skills because nursing is very people-centered. “You either have to be a people person or be willing to work on and build that skill,” he said.
James emphasized the importance of work-life balance in nursing. “It’s a high-stress career. There’s a lot of pressure put on everybody’s shoulders to get a lot done in a small amount of time. I cannot stress enough, people in the profession need to find balance in their lives. If they don’t take care of themselves, they’re not going to do a good job taking care of other people.”

“I would also recommend finding the right place for you,” James added. “You will grow and flourish when you find where you belong. That’s what Custer has done for me. There’s no place better, as far as I’m concerned.”
“The city partnered with Monument Health to build the $22 million hospital and clinic. Custer Hospital is beautiful, but more importantly, it provides an incredible amount of services for a community this size,” said James. “We’re proud of everything we have to offer, from physical therapy and an emergency department that could compete with those in much larger communities, to our healing garden and the amazing physicians and caregivers that work and live here.”

The community of Custer is proud of its hospital, and rightly so.
LOOKING TO PURSUE OR ADVANCE YOUR CAREER IN CHILD CARE?

FULL TIME POSITIONS AVAILABLE IN RAPID CITY
• Entry-level positions
• Eligible positions for 16-17 year olds
• Supervisory positions (advanced certification required)
monument.health/careers
Veterans make up roughly 11 percent of the country’s homeless population.

Homelessness is a serious problem among America’s veteran population. Veterans make up roughly 11 percent of the country’s homeless population. Around 60,000 veterans can be found sleeping on the streets on any given night, and women make up the fastest-growing group among the homeless veteran population.
“There are a lot of reasons why this number is growing,” said Kaylan Harrington, an Emergency Department Technician at Monument Health Rapid City Hospital. “A lot of women veterans are not utilizing VA health care right now either. Many think they don’t deserve it. Others had a terrible experience in the military and they kind of want to separate themselves from that.”

Kaylan is no stranger to military service. She served for 21 years, starting in the Air Force then crossing over to the Army as an officer. She has been deployed six times, with four tours to Iraq and Afghanistan. She now serves in the South Dakota National Guard and attends nursing school at SDSU.
“I have kind of an unusual resume,” she said with a smile, describing the many jobs she’s done in the military. In her most recent tours to Afghanistan, she worked with female engagement teams, who interact with Afghan women — it’s taboo for Afghan women to interact with men who aren’t direct members of their family. She also worked as a prison interrogator in Iraq and as an intelligence analyst. In other words, Kaylan is a legitimate, certified badass. She’s got a quick wit, a sharply intelligent mind, a can-do attitude and a beautiful,
IS A TOUGH BATTLE. ONE OF THE MOST EFFECTIVE — ALBEIT UNEXPECTED — WEAPONS IN THIS FIGHT MIGHT JUST BE AN EVENING GOWN.
friendly smile. For all those reasons, it’s no surprise that she was also the first runner-up in the 2022 Ms. Veteran America competition.

“I’ve been really humbled by all of this. I’m kind of a tomboy, a T-shirt and jeans kind of girl, and I thought this was something that I couldn’t do,” she said warmly. “But I know women who have competed and won, and I was so inspired by what they were able to do, the money they raised for women veterans and the representation that they brought forward on the national stage. I decided this is the year to do it, and South Dakota is a great state to represent. We take care of our veterans, and I would love to see this attitude and the care and compassion that we have in this state become the norm.”
The Ms. Veteran America competition was created in 2011 by Final Salute Inc., an organization with the mission to provide homeless women veterans and their children with safe and suitable housing. The competition supports the organization’s mission in two ways: all proceeds from the event are used to provide housing, and the event itself serves as a platform to build awareness. Fundraising is part of the competition itself. “All the girls worked their butts off for six months to a year to raise funds for the organization, and then all of the ticket sales were added to that,” Kaylan explained. “We raised over $700,000 for Final Salute.” Additionally, the winner and runners-up serve on an advocacy
“The women that I met are just unbelievable. There were doctors and lawyers right next to tank commanders and machine gunners,” Kaylan said. “There’s just a wide array of very educated, very humble, incredibly strong women.”
KAYLAN, ON MEETING WOMEN COMPETING IN THE MS. VETERAN AMERICA COMPETITION
To learn more about Final Salute Inc., and how the organization helps women veterans, visit finalsaluteinc.org.

board to continue building awareness of the challenges faced by women veterans.
“I’m very honored to be part of this. I’m humbled. The women that I met are just unbelievable. There were doctors and lawyers right next to tank commanders and machine gunners,” Kaylan said. “There’s just a wide array of very educated, very humble, incredibly strong women.”
Kaylan said her experience in the military has been positive, but she’s aware that hasn’t been the case for every woman who has served. “A lot of women have had very bad experiences, and that contributes to the problems and troubles they experience after they leave the military,” she said. “Women deal with combat differently, they experience PTSD differently. Sexual trauma is a huge issue in the military right now, and the VA was behind the curve when it came to providing resources catering to female veterans that were homeless.”
A lot of homeless women veterans are also single mothers, which presents additional challenges.
Final Salute, Inc. has programs designed specifically to help women veterans in need. The following programs helped thousands of women veterans across the country.
H.O.M.E.
The H.O.M.E. program helps women veterans integrate into their local communities and provides transitional housing and additional support with food, clothing, transportation, on-site case management, employment support and other essential support services to homeless women veterans and their children.
S.A.F.E.
The S.A.F.E. program is designed to help prevent homelessness by helping to ease financial burdens women veterans may experience. This includes emergency financial support for rent and utilities, but just as importantly it provides financial education resources.
Next Uniform
As women military personnel and veterans transition to the civilian workforce, the Next Uniform program provides professional business attire, dress shoes, makeovers and even image consulting and professional headshots to help women veterans find meaningful work after their military career.
Kaylan said, “Many shelters may not be safe for children, and male children that are teenagers may be separated from their mom and placed on a side of the shelter just for men, so many of these individuals avoid the traditional shelters.”
Jathe “Jas” Boothe founded Final Salute, Inc., because she discovered there simply weren’t existing programs to help female veterans with children. In 2005, while Jas was in the Army Reserves, she had to deal with a devastating cancer diagnosis only one month after losing everything she owned to Hurricane Katrina. That experience was eye-opening for her, and was ultimately what led her to start Final Salute, Inc. Since then, the organization has helped more than 7,000 women veterans and their children.
Kaylan, as first runner-up, joined second runner-up Ann Lutz, and winner Liliana “Joie” Byrd, as part of an advocacy board that will continue working to bring attention to the problems faced by women veterans, especially homelessness. “One thing that we’ve done is the Bataan Memorial Death March on March 17,” she said. This 26.2 mile march through the desert at White Sands Missile Range in New Mexico is an annual commemoration of the Bataan Death March attended by many survivors, veterans and supporters from across the globe. The trio wore their military uniforms, as well as their crowns and sashes, and raised money and awareness for Final Salute during the March.
“It’s the first time the Ms. Veteran America court has done something like that,” Kaylan said. “So we made a little bit of history, which felt great since it was also Women’s History Month.” Marching through the desert did nothing to deter Kaylan’s excitement for bringing awareness to the plight of homeless female veterans. “I’m excited for everything that we’re planning.”
Final Salute’s mission inspired Kaylan to step out of her comfort zone and onto the stage to compete for Ms. Veteran America, but there was an added bonus. “To bring national attention to this problem

Ms. Veteran America isn’t a traditional pageant — that’s why Final Salute, Inc., and the contestants prefer to call it a competition. The winner and runners-up are selected based upon a point system in which contestants are scored during a series of interviews by female military members of prominent standing. Contestants answer questions on significant women in military history, current events and policies that affect women in the military, homelessness or veterans. Contestants are also scored on advocacy and talent.
is incredibly important, and I’m proud to be part of it. But it also has been a great reminder that women do incredible things in different ways, and you can do more than one,” she said with a smile. “You can be a badass in the military and still want to put on a dress and a nice pair of heels once in a while. One doesn’t have to overshadow the other.”
“This year, the talent portion was a lip sync battle,” said Kaylan with a laugh. “I lip synced Prince’s ‘Let’s Go Crazy’ — I love him, he makes me so happy, and I got really into it. There was a full costume, and I bedazzled my Guitar Hero guitar. I won best talent for the competition.” Kaylan also won most donations, raising $11,000 in South Dakota, all of which will be used to benefit homeless women veterans.
The final day is the evening gown event and the pushup competition. In addition to the judges’ scores, Ms. Veteran America and Final Salute, Inc., leadership also consider contestant activity, interaction and participation.
“I ended up having a lot of fun during the competition, and I’m proud of the work we’re doing to help homeless women veterans,” Kaylan said. “It’s a big problem, but I’m proud to be part of a group that is working on solutions.”
ALL YOUR BAGS ARE PACKED, BUT ARE YOU READY TO GO? HERE’S HOW YOU CAN MAKE SURE YOU STAY HEALTHY DURING YOUR NEXT TRIP.

 Written by Wade Ellett
Written by Wade Ellett

Taking a trip, whether a weeklong vacation or just a weekend getaway, is a great way to decompress, refresh and celebrate. But anyone who has had a trip go awry because of health issues can tell you that a dream vacation can become a nightmare when you don’t feel well. Whether it’s food poisoning, allergies or misplaced medication, health issues can derail any trip. Luckily, there are ways to make sure that your travels are smooth sailing.
Eating can be a big part of travel. Whether you enjoy fine dining or food trucks, it’s important to enjoy what you eat while on vacation. “I often advise my patients not to worry about losing weight while on vacation,” said Rachel Van Den Top, Clinical Dietitian. “I think your
mind should be focused on the exciting things you’ll be doing, new places you’ll see and the yummy foods to try rather than the number on the scale during vacation.”

Rachel also warns travelers to be on the lookout for what she calls, “travel tummy.” That can be anything from inconvenient abdominal discomfort or more serious travelers’ diarrhea. “This can be a result of a difference in climate, different sanitary practices or simply the stress from travel. If you know you’re going to an area where the tap water is contaminated, it is especially important to plan ahead and have bottled water available. You also will want to avoid drinks with ice in them, as the ice may be made from the contaminated water,” Rachel explained. Researching beforehand can help you learn if an area has water that you should avoid or if you need to be vigilant about unsanitary food practices. This will help you avoid travel tummy as well as more serious conditions such as hepatitis A or typhoid, or illnesses caused by bacteria, parasites and viruses.
Travelers should also be on guard against dehydration, which can pose serious risks. Even in areas where water may be contaminated, it’s important to stay well-hydrated, especially in warm climates. “Do your best to have a water bottle on you at all times or bottled water nearby. You can set a timer on your phone to remind you at a certain time of the day to catch up on water intake,” suggested Rachel. “Since you will be eating different food than you are used to, and in a different routine, it is important to drink adequate water to keep your bowel movements regular.” In areas where water may be contaminated, you will want to drink bottled water or use a water purification method.

These suggestions can help you avoid getting ill on your trip, but what if you have medication that you need to continue taking during your travels? Pharmacist Stephanie Magbuhat, PharmD, suggested having all prescription medications ready well before your departure date. “The most important piece of advice I can offer is to plan ahead,” said Stephanie. “Long before your travel date approaches, call your preferred pharmacy and make sure you have refills on all your medications, and confirm you will have enough to get you through the entirety of your trip, as well as a little extra to account for any flight or weather delays.” Most insurance companies will allow at least one vacation override per medication per calendar year if the refill dates don’t quite line up. “Just call your pharmacy with your specific travel dates, and they will happily call your insurance company if needed,” added Stephanie.

Although airlines strive to make sure everyone’s checked baggage arrives where it should be on time, everyone knows someone who has lost luggage — keep your medications in your personal item or in your carry-on luggage to prevent any issue with lost baggage. Medications should be kept in their original, labeled containers from the pharmacy. Remember to pack a cooler for medications that have to be kept cold, like insulin.
If you forget to get your medications filled prior to departure, or your medicine is lost or damaged, contact a pharmacy in your travel area.

“Typically, when traveling within the United States, most prescription medications can be transferred over the phone to a pharmacy of your choosing. Special rules and restrictions do apply, especially for controlled or DEA scheduled medications, that may make this process more complicated. Be mindful, higher copayments may also occur when filling at an out-of-network pharmacy,” said Stephanie.

It’s not uncommon to throw routine out the window when traveling, but remember that medications must be taken as prescribed. “Remember which medications need to be taken with food and which need to be taken on an empty stomach. Be mindful that some medications shouldn't be mixed with alcohol,” said Stephanie. “If you are traveling across multiple time zones, or fear you can't replicate your normal routine, feel free to call your pharmacist for specific recommendations.”
If traveling internationally, you will need to take additional steps to prepare. Some foreign countries may have additional travel requirements, such as required or recommended vaccines or medications for protection against common pathogens. Some prescription medications may not be available, or may even be illegal, in some countries. “To be sure the medications you are traveling with are permitted, and you have all the correct documentation, you should always check with the embassy or consulate in that county prior to departure, especially if traveling abroad with DEA scheduled medications,” advised Stephanie. For specific guidelines, the CDC’s website is a reliable source of information, or ask your primary care provider for guidance. Depending on your destination, you may not have access to the same over-the-counter medications that you do at home. It may be worthwhile to pack your own, especially if you have seasonal allergies, a sensitive stomach or are prone to headaches.


Stephanie suggested, “In addition to basic first aid supplies, your travel kit should also include medications for the following ailments: diarrhea, heartburn, allergies, motion sickness, pain and fever relief, constipation


and insect bites. If you are interested in specific recommendations, contact your pharmacist for a personalized list geared toward your destination and in accordance with your prescription medications to assure there are no conflicting drug interactions.”
If you’re flying into a different time zone, you may also experience jet lag, which is a temporary sleep problem caused by your body’s circadian rhythms — or internal clock — not adjusting to your new destination as quickly as you travel. Symptoms include daytime fatigue, upset stomach, difficulty staying alert and a general unwell feeling. The farther your trip takes you, the more severe your symptoms may be. While there is no single, surefire way to prevent jet lag, there are steps you can take to reduce the likelihood of experiencing it or reduce your symptoms. You can start by getting plenty of rest before your trip, since starting your trip already sleep deprived will make symptoms worse. Try to sleep on the plane if it is night where you’re going but try to stay awake if it’s daytime at your destination. You can also try to gradually adjust your schedule before you leave — if your trip will take you east, go to bed an hour earlier each night a few days before you depart. If flying west, reverse it and go to bed one hour later. Once you reach your destination, keep your routine with the local time, including when you go to bed and get up, as well as when you eat your meals. Staying hydrated can also help counter the symptoms of jet lag.
Whether you’re traveling around the globe, across the country or just down the road, your getaway should make you feel awesome, not awful. Taking these steps can help you ensure that you don’t get a case of travel tummy, suffer from too much jet lag or just wish you were back home.

When long-haul trucker Don Wood got sick while on the road to Colorado in December 2021, he couldn’t anticipate the hardships and challenges that were ahead of him. When he left his home in Spearfish, he was perfectly healthy. By the time he returned, however, he was sick, and it was quickly getting serious.
“I left on Monday to make my deliveries to lumber yards in Colorado and Wyoming, and by the time I got back that Saturday, I wasn’t feeling well at all,” he said. As soon as he got home that day his wife, Patty Wood, helped get him to the hospital to be tested for COVID-19. “I got tested and sure enough it was COVID-19,” Don said, “When that came back, they hospitalized me right away.”
From there, things went from bad to worse for Don, as he developed some of the most severe complications from COVID-19. Just four days after Christmas, he went into cardiac arrest. “He was in Spearfish hospital for the first couple weeks, then he coded, so they sent him to Rapid City,” said Patty. At Rapid City Hospital, he was taken to the ICU and placed on a ventilator. He was there for five-and-a-half weeks.
During the height of the pandemic, the mortality rate for COVID-19 patients on ventilators was between 50 and 97 percent. Don was fighting for his life, and the odds were against him. Even if he did survive, his doctors were concerned about
potential long term brain damage.
“His neurologist ordered an EEG. There was very little brain activity, but I saw some. It wasn’t nothing,” Patty said. “So, after talking with the doctor, she recommended we wait a few more days and do another EEG. We just weren’t ready to give up on him.” That time was enough for Don to wake up. “I know a lot of people don’t believe in miracles, but we do. We got seven miracles, and Don waking up was a big one.”
Difficult decisions
Don moved between nine hospitals and clinics in nearly as many months. Either to receive more specialized care or because there weren’t enough beds due to the pandemic.
He was airlifted to Scottsbluff, Neb., where his health began to turn around, even though things looked grim when he arrived. The receiving physician had to perform a bronchoscopy. His lungs were so full of fluid that doctors didn’t have high hopes of recovery. “The person who does the life flights came to visit me. He didn’t think I was going to make it when I came in, and he ended up giving me his cap. He said he was rooting for me.” Don pointed to the red baseball cap he was wearing and continued, “I call it my $51,000 cap!”
It was in Scottsbluff where they were finally able to get Don back on solid food. “When I went into the hospital, I weighed 230 pounds. When I finally woke up and they took me off the ventilators, I had lost 100 pounds,” he said.
After he stabilized and was able to eat again, the hospital was ready to discharge him. “I was in a wheelchair. I was so weak, and I couldn’t walk. They said there wasn’t anything more they could do for me, and they were discharging me.”
It was recommended that Don be placed in an assisted living facility. For the Woods, that was completely out of the question. "We said no,” Patty said. “He didn't want to be in a nursing home, and I didn’t want him there either. He wouldn't have been happy that way.” They decided to try physical therapy. This eventually brought Don back home to Spearfish, where he started physical therapy at Monument Health. “That was when we really started to notice a difference,” Patty said, “We came here, and Don was in a wheelchair, and 14 months later he was walking.”

Matt Weigel, Physical Therapist, and Meagan Stephens, Occupational Therapist, at Monument Health Rehabilitation in Spearfish were part of Don’s recovery team. Matt said when Don came in he wasn’t sure what to expect. “COVID-19 was a new thing and people in Don’s position often wouldn’t survive to start physical therapy. We didn’t have a ton of data.”
Matt started with small, attainable goals. Don was on six liters of oxygen a day, and Matt didn’t want to push him too far, too fast. “We would just do exercises lying down, then a couple standing exercises,” Matt said. “Eventually, we were able to use some of the leg machines. After that, we started to see Don walking a little bit, but not a ton.”
“I know a lot of people don’t believe in miracles, but we do. We got seven miracles, and Don waking up was a big one.”
DON’S WIFE, PATTY, ON HIS RECOVERY
Don’s lungs were particularly concerning. COVID-19 had done a lot of damage, and there was a lot of scarring. Matt said, “He was on quite a lot of oxygen when he came in. His lungs aren’t ever going to be how they were before he got sick, but I didn’t expect to see anywhere near as much recovery as we did.”
After Don’s physical therapy, Meagan would take over for his occupational therapy. Like physical therapy, occupational therapy went slowly. “We were on a separate schedule because he could not tolerate two therapies in a row, so PT and OT were always on separate days,” she said. “If we were back-to-back, therapy wouldn’t have been as effective.”
While Matt focused on Don’s strength, mobility and endurance, Meagan helped Don learn how to do everyday tasks to help make him more independent. “Patty was helping Don with 90 percent of his active daily living tasks. Things like helping him get dressed, getting in

“We are very skilled, and there is a lot of training that goes into physical and occupational therapy, but it’s still a collaboration with our patients. No one wants to be in therapy but Don was determined. He showed up every day and did the work. Putting in that time and seeing his successes was really rewarding. It was one of those cases that reminded me why I chose the work I did.”
Matt Weigel, Physical Therapist Spearfish Physical Therapy
and out of the bathroom, showering — all the small things we take for granted,” said Meagan. “We wondered if we would ever get him back to that full independence. Could we get him to the point where he was able to tie his shoes without getting exhausted? By October we had him doing all those things for himself.”
From small successes to big wins Don was hitting his goals, and the focus shifted from seeing the most he could hope to do, to seeing how far he could go. “We started with these very basic goals, like standing up from furniture, or having him walk across a room on his own,” Matt remembered. “And Don was putting in the work and hitting all of these goals. These were just basic things a person needs to do every day, but they seemed lofty at first.”
As Don started to achieve these goals Matt said more things suddenly seemed possible. “I started to ask questions like, ‘Can you make yourself lunch or walk to the mailbox?’ ‘Can we actually get outside with oxygen?’ ‘Can you get down the stairs?’ It opened up my eyes. We’d talk about what he wanted to accomplish, and we kept going and broke past what we thought was the top limit.”
Don remembered a very special milestone he was able to reach. “I had whiskey and my coffee that I wanted to be able to reach. It was really high up, and I just wanted
to be able to stand tall and balance on my own to get it. I was able to finally reach up there and get my whiskey, my coffee and my filters on my own.”
Meagan remembered setting that goal. “We were going to get the whiskey behind the coffee. It’s funny but that's a lot of what occupational therapy looks like, getting back those little things we do every day.” She and Matt worked as a team to reach their goals, often checking in with each other to see what milestones Don was able to achieve. Another major achievement sticks out in Meagan’s mind. “I'll never forget the day when I saw their car pull up and Don stepped out of the driver's seat and grabbed his oxygen. I ran to Matt, and said, ‘Don just drove here!’ He walked in so proud.”
Patty looks back at that time now and remembers the support she had from her family, the work Matt and Meagan put into bringing some normalcy back into their lives and her husband’s strength. “You know, it's funny, he had the right attitude, and he worked so hard at it. He really wanted to get better, and he was used to being a normal person. It was hard for him to lose that, so he worked hard to get it back.”
Meagan agreed and said that it can be a hard battle. “When that independence is taken away from you, it can be frustrating and tiresome. To be able to retrain your body, to regain that strength is a huge victory.”
On Aug. 23, 1988, Melody Rindahl was murdered by her husband, Randy. She was a victim of domestic abuse, but to those that knew and loved her, she was so much more. She was a beloved sister, a singer with a beautiful voice and a devoted friend. She was also a mother, despite the fact that her son had not yet been born.
When paramedics arrived on the scene, they found seven-and-a-half months pregnant Melody,


Though he may have been born of tragic circumstances, Ben Ericks has had a great life. If you were to ask him what kept him from being a victim of that tragedy his answer would be simple — family.by Wade Ellett Photos by Bob Slocum
Ben’s mom, Patsy Ericks, recalled a conversation she had with Dr. Theissen, who delivered Ben as a premature infant via C-section.
“Ben was about seven and I saw Dr. Theissen in the grocery store. He didn’t remember me at first, and then I told him my sister was Melody, and that I met him when he delivered her baby. He immediately started crying in the store and told me, ‘the call that I made to your parents was the most difficult thing I did in my entire career.’ Seven years after the event and that was his reaction,” Patsy said. “A decade later he came to the house when Ben was getting ready to go to basic training. It was really special to us that he did that.”
not breathing and without a pulse. They knew in that instant she wouldn’t survive. And while this might sound like the end of a story, it’s actually the beginning. Because though Melody’s life was ending, the most important thing in her world would live on — her son.
His journey certainly didn’t start in a positive way. His biological mother was kept alive by CPR until the paramedics could get her to the hospital. There, she was sustained by a life-support system until he could be delivered by emergency cesarean section. Despite the quick action of the paramedics on the scene, he had suffered oxygen deprivation and there were concerns about his health.
Because he was premature and due to the traumatic nature of his birth, he had to stay in an incubator, and twice required CPR. The outlook wasn’t great — there was a very real chance that he would never be able to walk or talk.
Loni Bedard, CNP, cared for Ben while he was in the NICU. Despite 39 years at Rapid City Hospital, she’s never seen another case like this. “I can still remember seeing him lying on the radiant warmer,” she recalled. “Just a fragile, preterm baby who needed so much support in the NICU to survive. He was a miracle baby.”


“At first, we didn’t know if he was going to survive,” said Patsy Ericks, Melody’s oldest sister. “But he did much better than they
expected and he came home with us in 23 days.” The baby boy was named Benjamin Lee; the name Melody had picked out if her baby was a boy.
Patsy credits the physicians, nurses and other caregivers for Ben’s quick recovery.
“Dr. Thiessen delivered Ben, and Dr. Kovarik was the neonatologist that took care of him after birth,” she said. “And of course, the NICU nurses that looked after Ben were amazing too.”
This was long before the hospital would become part of the Monument Health system; at the time, it was Rapid City Regional Hospital. Obstetrician Hubert H. Theissen, M.D., and Neonatologist Stephen Kovarik, M.D., have both since retired. Many of the nurses who treated Melody and Ben have also retired.
Loni Bedard continues seeing patients as a certified nurse practitioner, and despite her tenure at Rapid City Hospital, she’s yet to have another case that has stuck with her like Ben’s. “I knew Patsy, Curt and their kids. We went to church together. Between the trauma, the severity of the situation and knowing the family, I had a lot of emotions. It’s not something I could ever forget.”
Despite the tumultuous beginning, Ben
“You don’t have to live in that environment.
I know it feels like there’s no other way, but if you’re in an abusive relationship, seek help. It takes courage to stand up and talk to somebody and admit you need help. That’s not something to be ashamed of,” Ben said. “Know that there are other people who have gone through what you’re going through. There are people who are still going through it and there are people that want to help.”
Almost 160,000 South Dakotans will be affected by domestic violence during their lifetime.
If you or someone you know is a victim of domestic abuse, help is available by calling 800-799-7233, by texting “START” to 88788 or by visiting thehotline.org.
grew up a happy, healthy boy. He started his life as a ward of the state, but Patsy and her husband Curt were quickly granted an interim guardianship over Ben, who they took home and raised as their own. Soon after, their guardianship was made more permanent, and one and a half years later they officially adopted him. “That was just a formality though.
Ben was already part of our family,” said Patsy, who became Ben’s adoptive mother.
Ben’s arrival in the Ericks family was unexpected, but he fit perfectly. The infant found himself in a home with three older sisters, Clarissa, Charity and Cameo. “I was four months old when Ben came to live with us, so I’ve never known anything different,” said Cameo Haugen. “There were a lot of times growing up that people assumed we were twins.”
Good families tend to find their own balance, their own equilibrium. It was no different for the Ericks family. Clarissa was 11 years old, and Charity was 6 when Ben joined the family. With 4-month-old Cameo a recent addition as well, the balance of the family shifted. “Us older girls — without ever really thinking about it — took on one of the babies,” said Charity Hathaway.
“Ben was my baby. Whenever he needed
something, it was me who got it for him. Looking back at the family pictures, I always had Ben in my lap or we were sitting next to each other, arms around one another. From day one, we had a very, very close connection and bond with each other. We still do.”
That closeness didn’t just affect their family life, it also had a profound effect on Charity’s career path. She knew at a young age that she wanted to work in health care so that she could help others in need. “I vividly remember the night that Ben’s mom was shot. I remember the policeman coming to our door. I remember our grandma coming over to stay with us,” she said. “It truly impacted the future of my life. I remember visiting Ben in the NICU and telling my mom, ‘I’m going to be a nurse someday because I want to take care of people that need me.’” Charity did just that, becoming a Registered Nurse and earning her BSN. Though she no longer lives in Rapid City, she worked at Monument Health for 17 years, with the majority of her career in Labor and Delivery.
Despite worries that lack of oxygen and blood flow perfusion could have lifelong debilitating effects, Ben was not only a healthy

child, but he grew into an athlete who played high school football and was even signed to play at the collegiate level. Instead he chose to serve his country, enlisting in the South Dakota National Guard, deploying to Afghanistan in 2013 for Operation Enduring Freedom, and to Cuba in 2022. “There was a lot of worry when I was a baby, but the only problem I’ve really had was a little asthma,” Ben said with a chuckle. “And what kid these days doesn’t have a little asthma growing up.”
Having never truly met his biological mother, Ben only knows Melody through the stories his mom, grandmother and sisters have shared with him. “I’ve lived a good life with a great family, and there is always — in the back of my mind — a question of what if that never happened? What would my life have been like if I had grown up in the shadow of that abusive relationship? I would have had a very different upbringing,” Ben explained, thoughtfully. “So I know my biological mom through their memories, and I know she loved me, but I’m grateful for my family that raised me.”
When talking about family, it’s clear how important the people in his life are to him.
“He’s probably the best husband and father anybody could ask for. He’s the complete opposite of his biological father,” said Cameo.
“He’s loving and caring, and dotes on his wife
and his children. He’s amazing.”
To Ben, Curt Ericks is his dad — his biological father simply provided genetics. He said, “I had a great role model growing up with my dad, and I think I strive to be like him, not the other guy. I think being a role model is very important, and I had the best. I just focus on being a good husband and role model to my boys.”
“I want them to see what a healthy marriage is and what it should be. I know I had that growing up with my family,” he added.
You can’t untangle the life of Ben Ericks from the murder of his biological mother. Patsy said, “This story became a huge part of our entire family. When something like that happens, everybody responds differently, and you never forget.” And while that’s true, Ben’s story isn’t a tragic one, even if that’s how it started. Instead, it’s the story of a kid who grew up in a good family — his family. He was a great brother, and grew into the kind of man any parent would be proud of; a good husband, a good father and a man who cares about the people around him.

“I think the story of my life can give a different perspective on what family is and how important it is,” Ben said. “Family isn’t just who your biological parents or siblings are. It’s the people that are there for you. The ones who love you.”

Melody’s experience is not a new one, and sadly, it isn’t the last of its kind.Her story, voice and memory are remembered and honored in a short film by Emmynominated Director, Jason Clemons. To watch Melody’s Story, scan the QR code below. Front row; Ben and Dr. Kovarik (retired). Back row; Lorie Hausmann, RN (retired), Loni Bedard, CNP, and Sandy Ashmore, RN (retired).
“Family isn’t just who your biological parents or siblings are. It’s the people that are there for you. The ones who love you.”
BEN ERICKS
For many, the valet is the first and last caregiver a patient will see during their visit to Rapid City Hospital. Their kindness and customer service can help set the tone for the patient visit. On an average month, Valet Services park and retrieve 2,800 cars and help welcome 2,100 patients — this includes assisting with wheelchairs when necessary.
While most people think of valet services only being available at high-end restaurants or hotels, Monument Health believes its patients are VIPs who deserve this curbside service.

My Role
I have been with Monument Health for 23 years, and my current role as Valet Supervisor is to help ensure patients’ cars are safely parked at Rapid City Hospital. Many patients tell us getting to and from their appointments would be much more challenging without this service. It’s especially helpful during the cold winter months.

My Goal
At the end of the day, if I can help a patient feel like a VIP, I have achieved my goal. I hope I can put a smile on everyone’s face who I come in contact with, and hopefully that will set a standard for the rest of their visit. My team and I are very dedicated to creating a positive experience for patients.
My Passion
At the end of the day, I feel good knowing I was part of caring for our patients and their families. Outside of work, I enjoy camping and taking our Jeep throughout the Black Hills. My wife and I just became first-time grandparents; I’m looking forward to this new adventure.

My role is to provide conservative treatment options to patients with back and neck pain. I also accurately diagnose painful spinal conditions and move the patient through a thorough treatment process. This begins with the least invasive options, and if the patient’s pain doesn’t improve then we determine if surgery is necessary. Ultimately, my role is to ensure a patient’s source of pain is accurately identified and treated.
My Goal
I bring the most current and minimally invasive treatment options for spinal pain to the Black Hills. Nobody wants pain and discomfort to limit what they can do, and I want to help patients get relief. Hopefully that allows them to return to activities and lifestyles that they enjoy. My goal is to help each patient live their best life and contribute to better spinal health throughout the region.


The most rewarding part of my job is seeing patients improve their quality of life and regain the ability to do the things they love. Outside of work, I’m passionate about my children — anything I do with them! We love exploring the Black Hills and spending time in the outdoors, kayaking, canoeing and camping. I am also very grateful for the friends I have made in the time that I have been here.
Advanced Practice Provider (APP) refers to physician assistants (PA-C), certified nurse practitioners (CNP) and certified registered nurse anesthetists (CRNA). Because of their advanced training, APPs can do many of the same things a physician does. Patients benefit from having both their physician and their APP working together on their care.
My Role
I work with a team of skilled professionals at the Monument Health Orthopedic & Specialty Hospital. We provide a variety of musculoskeletal care for our community. This involves evaluating patients with acute and chronic orthopedic concerns in our clinic, as well as assisting the surgeon in the operating room.
My Goal
My goal, and that of orthopedics, is to help patients improve or restore function so that they can get back to their normal routine. I try to understand patient expectations and use the tools of orthopedic medicine to help meet their needs as a provider. My goal for the next year is to continue to mentor new APPs in orthopedics to become better providers, which ultimately helps deliver high-quality care for our community.
My Passion
I have been involved with health care in a variety of capacities over the last 25 years, and orthopedic care has always given me joy. This is a field of medicine where I get to see patients typically improve the quality of their life. To be able to see a patient come back to the clinic after surgery and show me they can walk better or even lift their arm over their head when they couldn’t before makes me happy. Knowing that, as a physician assistant, I was able to help get the patient to that point of life satisfaction is my passion.
Physician Assistant, Monument Health Orthopedics & Specialty Hospital
A surgical APP, like Chris, often see patients before, during and after surgery. These visits provide the surgeon with additional patient information. This comprehensive care model ensures the patient is treated by a highly trained care team.


Julieta Munoz-Mejia, m.d., is a board-certified Critical Care Physician at Monument Health Rapid City Hospital.


Dr. Munoz-Mejia received her medical degree from the National Autonomous University of Honduras. She completed her residency in internal medicine at Loyola Medicine - MacNeal Hospital in Berwyn, Ill. and was the Chief Resident at Griffin Hospital in Derby, Conn. She completed her fellowship in Critical Care Medicine at Baylor College of Medicine. Dr. Munoz-Mejia is a member of the American Medical Association, American College of Physicians, Society of Critical Care Medicine (SCCM), American Thoracic Society (ATS) and American College of Chest Physicians. She is fluent in English and Spanish.
Javier Bogarin, m.d., fccp, is a board-certified Critical Care, Pulmonologist and Sleep Medicine Physician at Monument Health Rapid City Hospital. He completed medical school at the University of Rio de Janeiro in Brazil, his internal medicine residency at Rush Presbyterian –St. Luke’s Medical Center in Chicago and two fellowships in pulmonology at Rush Presbyterian – St. Luke’s Medical Center and the University of Miami – Jackson Memorial Hospital. Dr. Bogarin joins the Monument Health team after years of being a locum and working in private practice.
Christopher Robbins, m.d., ccd, is a Family Medicine Physician at Monument Health Flormann Clinic in Rapid City.



Dr. Robbins completed his residency at the Rapid City Regional Hospital Family Medicine Residency Program and obtained his doctorate of medicine from the University of Texas Health Science Center at Houston Medical School in Lubbock, Texas. He is a patient-oriented family medicine physician who treats pediatrics, adolescents, adults and geriatrics. Dr. Robbins is also a clinically certified densitometrist. He is passionate about helping patients through a wide range of health and lifestyle issues and takes a hands-on approach to health care. When he’s not working with patients, Dr. Robbins enjoys being outdoors with his family.
Leslie VanDyne, m.d., is a general surgeon specializing in trauma care at Monument Health Rapid City Hospital. She received her medical degree from the University of South Dakota Sanford School of Medicine in Vermillion, S.D. She completed her Surgical Residency at Mount Carmel Health Systems in Columbus, Ohio, and her Trauma Critical Care Fellowship at MetroHealth Medical Center in Cleveland, Ohio. Dr. Van Dyne’s practice is focused primarily in the inpatient setting, working with acutely ill surgical patients. She has a passion for treating critically sick patients and received additional training for the treatment of ICU and complex trauma patients. Dr. Van Dyne approaches every patient as if they were one of her family members. She believes this mindset helps her to keep perspective on what is important. Outside of work, she and her husband enjoy exploring Rapid City and the Black Hills, as well as traveling to see new cities. She also collects houseplants and recharges by spending time with their blind dog, Boomer.
Eric Krohn, d.o., is a Pediatric Orthopedic Surgeon at Monument Health
Orthopedic & Specialty Hospital in Rapid City, S.D. He received his medical degree from Lake Erie College of Osteopathic Medicine in Erie, Pa., completed his residency at Good Samaritan Regional Medical Center in Corvallis, Ore. and a fellowship in pediatric orthopedics at the University of Michigan in Ann Arbor, Mich. He is a member of the American Academy of Orthopedic Surgeons, the American Osteopathic Academy of Orthopedic Surgeons and the Pediatric Orthopedic Society of North America. When he isn’t working, Dr. Krohn likes to fish, cycle, hike, camp, travel and study history. Dr. Krohn specializes in deformity correction, growth modulation and fracture care.
DIRECTORY // COMMUNITY
HOSPITALS
Custer Hospital
1220 Montgomery Street
Custer, SD 57730
605-673-9400
Lead-Deadwood Hospital
61 Charles Street
Deadwood, SD 57732
605-717-6000
Rapid City Hospital
353 Fairmont Boulevard
Rapid City, SD 57701
605-755-1000
Spearfish Hospital
1440 N. Main Street
Spearfish, SD 57783
605-644-4000
Sturgis Hospital
2140 Junction Avenue
Sturgis, SD 57785
605-720-2600
CLINICS
Belle Fourche Clinic
2200 13th Avenue
Belle Fourche, SD 57717
605-723-8970
Buffalo Clinic
209 Ramsland Street
Buffalo, SD 57720
605-375-3744
Custer Clinic
1220 Montgomery Street
Custer, SD 57730
605-673-9400
Family Medicine
Residency Clinic
502 East Monroe Street
Rapid City, SD 57701
605-755-4060
Family Health Education Services
930 N. 10th St
Spearfish, SD 57783
605-642-6337
Gillette Clinic
20 W Four-J Court
Gillette, WY 82716
307-682-1204
Hill City Clinic
238 Elm Street Hill City, SD 57745
605-574-4470
Hot Springs Clinic
1100 Highway 71 South, Suite 101
Hot Springs, SD 57747
605-745-8050
Lead-Deadwood Clinic
71 Charles Street
Deadwood, SD 57732
605-717-6431
Rapid City ClinicFlormann St.
640 Flormann Street
Rapid City, SD 57701
605-755-3300
Rapid City Clinic5th St.
2805 5th Street
Rapid City, SD 57701
605-755-5700
Spearfish ClinicNorth Ave.
1445 North Avenue
Spearfish, SD 57783
605-644-4170
Spearfish ClinicNorth 10th St.
1420 North 10th Street
Spearfish, SD 57783
605-717-8595
Sturgis Clinic
2140 Junction Avenue Sturgis, SD 57785
605-720-2400
Wall Clinic 112 7th Avenue
Wall, SD 57790
605-279-2149
URGENT CARE Custer
Urgent Care Services 1220 Montgomery Street
Custer, SD 57730
605-673-9400
Lead-Deadwood
Urgent Care Services 71 Charles Street
Deadwood, SD 57732
605-717-6431
OrthoExpress
Walk-in Clinic
1635 Caregiver Circle
Rapid City, SD 57702
605-755-6180
Rapid City Urgent Care
Jackson Blvd.
2116 Jackson Boulevard
Rapid City, SD 57702
605-755-2273
Please call your local clinic to schedule an appointment. Monument Health is also offering extended services through video and telephone visits with your provider.
Heart and Vascular Institute
353 Fairmont Boulevard
Rapid City, SD 57701
605-755-4300
Rapid City Urgent Care
Lacrosse St.
1303 N. Lacrosse Street
Rapid City, SD 57701
605-755-2273
Spearfish
Urgent Care Services
1420 North 10th Street
Spearfish, SD 57783
605-717-8595
Sturgis
Urgent Care Services
2140 Junction Avenue Sturgis, SD 57785
605-720-2600
SPECIALTY & SURGICAL CENTERS
Assisted Living
432 North 10th Street Custer, SD 57730
605-673-5588
Audiology & Ear, Nose and Throat
4940 5th Street Rapid City, SD 57701 605-755-4100
Behavioral Health Center
915 Mountain View Road Rapid City, SD 57702
605-755-7200
Care Center
949 Harmon Street Sturgis SD 57785
605-720-2400
Cancer Care Institute
353 Fairmont Boulevard Rapid City SD, 57701 605-755-2300
Dermatology
4150 5th Street Rapid City, SD 57701 605-755-5340
Dermatology
550 East Colorado Boulevard
Spearfish, SD 57783 605-717-8860
Dialysis Center
955 East North Street Rapid City, SD 57701
605-755-6950
Dialysis Center
132 Yankee Street
Spearfish SD 57783
605-722-8110
Home+ Home Health and Hospice
931 E Colorado Boulevard
Spearfish, SD 57783
605-644-4444
Home+ Home Health
224 Elk Street
Rapid City, SD 57701
605-755-7710
Home+ Home Medical Equipment
1800 N. Haines Avenue
Rapid City, SD 57701
605-755-9000
Home+ Home Medical Equipment
1635 Caregiver Circle, Rapid City, SD 57702
605-755-6150
Home+ Home Medical Equipment
911 East Colorado Boulevard
Spearfish, SD 57783
605-717-8930
Home+ Home Medical Equipment
2707 Lazelle Street
Sturgis, SD 57785
605-720-2676
Home+ Hospice House
224 Elk Street
Rapid City, SD 57701
605-755-7710
Home+ Infusion
224 Elk Street, Suite 100 Rapid City, SD 57701
605-755-1155
Home+ Pharmacy
353 Fairmont Boulevard
Rapid City, SD 57701
605-755-8184
Home+ Pharmacy
1420 North 10th Street, Suite 1
Spearfish, SD 57783
605-717-8741
Home+ Specialty Pharmacy
2006 Mount Rushmore Road, Suite 2
Rapid City, SD 57701
605-755-3065
Neuroscience Center
677 Cathedral Drive
Rapid City, SD 57701
605-755-5276
Orthopedic & Specialty Hospital
1635 Caregiver Circle
Rapid City, SD 57702 605-755-6100
Orthopedics and Sports Medicine 2449 East Colorado Boulevard
Spearfish, SD 57783 605-644-4460
Rehabilitation
2200 13th Avenue Belle Fourche, SD 57717 605-723-8961
Rehabilitation 220 Montgomery Street Custer, SD 57730
605-673-9470
Rehabilitation
61 Charles Street Deadwood, SD 57732 605-717-6370
Rehabilitation
2479 East Colorado Boulevard
Spearfish, SD 57783 605-644-4370
Rehabilitation
2140 Junction Avenue Sturgis, SD 57785
605-720-2570
Rehabilitation Center 1050 Fairmont Boulevard Rapid City, SD 57701 605-755-1230
Sleep Center 2929 5th Street Rapid City, SD 57701 605-755-4000
Sports Performance Institute powered by EXOS 1635 Caregiver Circle Rapid City, SD 57702
605-755-6683
Surgery Center 1316 North 10th Street
Spearfish, SD 57783
605-642-3113
Are you feeling hopeless, angry, tired or restless?
GET HELP NOW. CALL OR TEXT 988 for 24/7, free confidential support.

