CANNABIS CLINICAL OUTCOMES RESEARCH CONFERENCE
May 30-31, 2024
Orlando, FL

May 30-31, 2024
Orlando, FL
At a Glance
Keynote Speakers
Session Moderators and Speakers
Top Abstracts Speakers
ABSTRACTS 23
Oral Presentations of Top Abstracts
Basic Science and Translational
Clinical Research, Population Health, and Health Behavior
EXHIBITORS 77 ABOUT 77
On behalf of the Consortium for Medical Marijuana Clinical Outcomes Research’s Scientific Program and Planning Committees, we welcome you to our 4th annual conference: Cannabis Clinical Outcomes Research Conference (CCORC), held in Orlando, FL on May 30th – 31st, 2024.
Our past conferences have offered an engaging hybrid venue gathering researchers, clinicians, policymakers, trainees, and other community stakeholders to explore our understanding of the health effects of medical marijuana. We eagerly anticipate another enriching experience this year built upon the momentum of our previous meetings.
One of the most exciting parts of CCORC 2024 is the opportunity to network, socialize, and get involved with cannabis clinical outcomes research. We hope that you will leave this conference having expanded your knowledge surrounding cannabis research and made new connections that may spark future collaborations.
We welcome you to CCORC 2024!
Sincerely,


Almut G. Winterstein, RPh, PhD, FISPE Director
Consortium for Medical Marijuana Clinical Outcomes Research
Robert L. Cook, MD, MPH
Associate Director
Consortium for Medical Marijuana Clinical Outcomes Research
Time (EDT) Session Description
9:00-9:20am
Day 1 Welcome Address Δ
Dr. Almut Winterstein
Consortium for Medical Marijuana Clinical Outcomes
Research
University of Florida
CCORC 2024 Agenda Overview Δ
9:20-9:30am
9:30-10:45am
Dr. Amie Goodin
Consortium for Medical Marijuana Clinical Outcomes
Research
University of Florida
Keynote: Cannabis, Endocannabinoids and PTSD* Δ
Introduction: Dr. Yan Wang, University of Florida
Dr. Matthew Hill
Hotchkiss Brain Institute
University of Calgary
10:45-11:00am Exhibitor Hall | Coffee Break
Presentations of Top Abstracts:
Cannabis, Women’s Health, and Gender
Moderator: Dr. Sari Paikoff, Florida Gulf Coast University
Anuradha Ramdas
University of Miami
11:00-12:00pm
Jocelyn Mueller
University of Central Florida
Melanie Zamora
University of Miami
Dr. Donald Porchia
University of Florida
MAY 30TH, 2024
Time (EDT) Session Description
12:00-1:00pm Lunch
Keynote: Using Laboratory Science to Inform Clinical Decision Making and Patient Safety in Medicinal Cannabis* Δ
1:00-2:15pm
Introduction: Dr. Md Mahmudul Hasan, University of Florida
Dr. Ryan Vandrey
Behavioral Pharmacology Research Unit
Johns Hopkins University
2:15-3:30pm Poster Session 1 | Exhibitor Hall | Coffee Break
Medical Marijuana & Me (M³): Cross-sectional and longitudinal survey findings from Florida medical marijuana patients
3:30-4:15pm
4:15-5:15pm
Dr. Yan Wang | Dr. Robert Cook | Sebastian Jugl
Juan Perez | Sophie Maloney
University of Florida
Presentations of Top Abstracts: Cannabis Use Patterns and Risk Perceptions in Selected Population
Moderator: Dr. Ellen Louise Terry, University of Florida
Alexandria Cashman
University of Miami
Dr. Armiel Suriaga
Florida Atlantic University
Dr. Naueen Chaudhry
University of Florida
Jacob Ross
University of California San Diego
5:15-6:30pm
Poster Session 2 | Exhibitor Hall | Networking Reception
Time (EDT) Session Description
8:00-8:15am
8:15-9:30am
Day 2 Welcome Address Δ
Dr. Robert Cook
Consortium for Medical Marijuana Clinical Outcomes
Research
University of Florida
Keynote: Cannabis Use Disorder* Δ
Introduction: Dr. Robert Cook, University of Florida
Dr. Margaret Haney
Irving Medical Center
Columbia University
Presentations of Top Abstracts: Cannabis as a Therapeutic and Novel Delivery Mechanisms
Moderator: Dr. Varan Govind, University of Miami
Dr. Mandip Sachdeva
9:30-10:30am
Florida A&M University
John Stauffer
University of Florida
Christopher Broxson
University of Florida
Dr. Niall Murphy
University of Florida
Time (EDT) Session Description
10:30-10:45am Exhibitor Hall | Coffee Break
10:45-11:30am
The Medical Marijuana Clinical Outcomes Repository (MEMORY): Overview of Florida medical marijuana dispensing data and preliminary results
Dr. Almut Winterstein | Sebastian Jugl | Priyanka Kulkarni
Darla Khouri University of Florida
11:30-12:00pm Closing and Awards Ceremony Δ
12:00-1:00pm Board Meeting and Lunch (Invitation Only)
* May be eligible for CME and CPE credits. Please check ccorc.mmjoutcomes. org/continuing-education-credit/ for details. The University of Florida College of Medicine designates this live activity for a maximum of 3.75 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. The University of Florida College of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. The University of Florida is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. This program has been approved by the Accreditation for Pharmacy Education for 3.75 hours of continuing pharmacy education credit.
Professor, Hotchkiss Brain Institute, University of Calgary
Dr. Matthew Hill is a Professor in the Departments of Cell Biology and Anatomy and Psychiatry at the Hotchkiss Brain Institute at the University of Calgary, the inaugural Chair of the Mental Health Initiative in Stress and Trauma and the Deputy Director of the Mathison Centre for Mental Health Research and Education. Dr. Hill is the Executive Director for the Canadian Consortium for the Investigation of Cannabinoids and both the Past President of the International Cannabinoid Research Society and the past Chair of the Neurobiology of Stress Conference. Dr. Hill’s research has demonstrated that the brain produces “endocannabinoids” (the brains own version of molecules like THC from cannabis) in response to stress to help us recover appropriately, and has found that chronic stress compromises how the “endocannabinoid” system functions, identifying this system as target for both the pathophysiology and treatment of stress related mood and anxiety disorders.
Research Focus: Behavior, Brain Development, Endocrinology, Mental Health, Neuroplasticity

Professor, Behavioral Pharmacology Research Unit, Johns Hopkins University
Dr. Ryan Vandrey is an experimental psychologist with degrees from the University of Delaware (BA) and University of Vermont (PhD). He is currently a Professor at the Johns Hopkins University Behavioral Pharmacology Research Unit (BPRU). Dr. Vandrey’s research focuses primarily on the impact of route of administration, dose, and chemical composition of cannabis products on resultant drug effects and pharmacokinetics. In addition, Dr. Vandrey has been involved with a broad range of studies related to the risks and
benefits of medicinal cannabis use, cannabis drug interactions, the effects of cannabis use on sleep, cannabis withdrawal and the treatment of Cannabis Use Disorder, cannabis product testing, and developing measures of cannabis use behavior.
Research Focus: Impact route of administration, dose, chemical composition of cannabis products on resultant drug effects and pharmacokinetics

Professor, Irving Medical Center, Columbia University
Dr. Margaret (Meg) Haney is a Professor of Neurobiology (in Psychiatry) at the Columbia University Irving Medical Center. As the Director of the Cannabis Research Laboratory and Co Director of the Substance Use Research Center, Dr. Haney is internationally recognized for her expertise in human laboratory studies of cannabis and cannabinoids. Her interest is both in conducting placebo controlled studies testing the efficacy of treatment medications for Cannabis Use Disorder and in testing the potential therapeutic effects of cannabis and cannabinoids.
Research Focus: Human laboratory models of cannabis and cocaine use disorders and the assessment of novel pharmacologic and immunologic approaches to treat these disorders

Presenter: Medical Marijuana & Me (M³): Crosssectional and longitudinal survey findings from Florida medical marijuana patients
Moderator: Cannabis Use Disorder
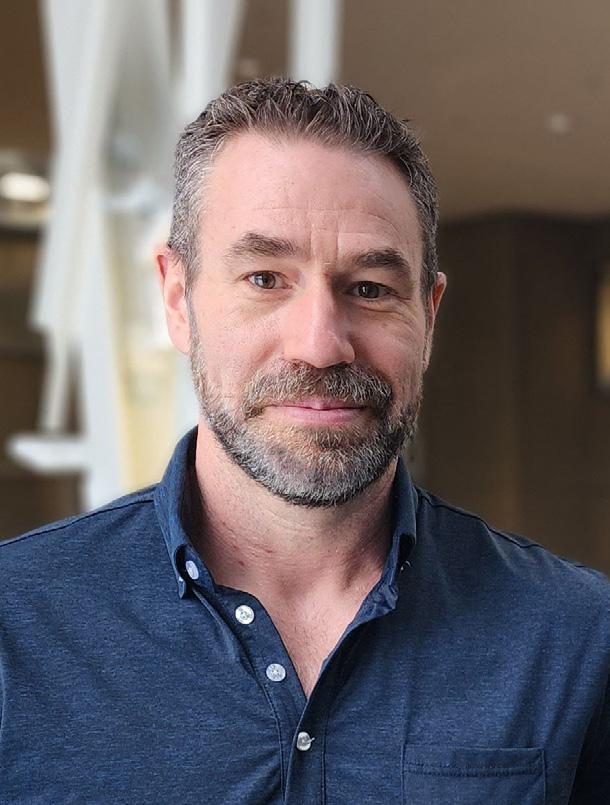
Professor, Department of Epidemiology and College of Medicine, University of Florida
Director, Southern HIV and Alcohol Research Consortium
Associate Director, Consortium for Medical Marijuana Clinical Outcomes Research
Over the past 20 years, Dr. Cook’s research has focused on strategies to improve health outcomes related to HIV and sexually transmitted diseases. He is the Director of the Southern HIV Alcohol Research Consortium (SHARC), which supports collaborative research and training related to alcohol and HIV infection across the state of Florida. Dr. Cook is also the co-lead of the “medical marijuana and me” cohort study and a co-investigator on several other research projects examining health outcomes of cannabis use.
Research Focus: HIV, sexually transmitted diseases, alcohol, cannabis, effects

Assistant Professor, Department of Pharmaceutical Outcomes & Policy, College of Pharmacy, University of Florida
Assistant Director, Consortium for Medical Marijuana Clinical Outcomes Research
Dr. Goodin is an Assistant Professor within the Department of Pharmaceutical Outcomes and Policy (POP) and the Center for Drug Evaluation and Safety (CoDES). She is the lead for the Pharmaceutical Health Services Research track within POP’s graduate program as well as the assistant director for Evidence within the Consortium for Medical Marijuana Clinical Outcomes Research. Currently, her research projects incorporate mixed-method approaches to assess the impact of policy changes related to treatment access and utilization for Substance Use Disorders, particularly among persons enrolled in Medicaid and pregnant women.
Research focus: Assessing the impact of controlled substance policies and improving policy-driven access for Substance Use Disorder treatments

Moderator: Presentations of Top Abstracts: Cannabis as a Therapeutic and Novel Delivery Mechanisms
Professor, Department of Radiology, Miller School of Medicine, University of Miami
Dr. Govind is a Professor of Radiology, University of Miami Miller School of Medicine, Miami, Florida. After obtaining Ph. D. in chemistry on the topic of NMR Spectroscopy and Imaging in biological systems, he joined Professor Andrew Maudsley’s research group as a postdoctoral fellow at the University of California, San Francisco (UCSF). In 2002, he took a faculty position in the Department of Radiology, University of Miami. He has become a tenured Professor in 2020 and continuing in the same department. He has been the principal investigator, or a multi-PI of several NIH- and other-funded studies.
Research Focus: Neuroimaging with specific focus on MR spectroscopy and diffusion tensor imaging, MR spectral characterization of tissue metabolites in in vivo and ex vivo, spectral simulations, MRS pulse sequence development, optimization of MRS sequence parameters for metabolites

Moderator: Using Laboratory Science to Inform Clinical Decision Making and Patient Safety in Medicinal Cannabis
Assistant Professor, Department of Pharmaceutical Outcomes and Policy, Department of Information Systems and Operations Management, University of Florida Assistant Director, Consortium of Medical Marijuana Clinical Outcomes Research
Dr. Hasan is an assistant professor in the Department of Pharmaceutical Outcomes and Policy with a joint appointment in the Department of Information Systems and Operations Management at the University of Florida. He is also the Assistant Director and Faculty Lead of the Medical Marijuana Research Repository (MEMORY) for the Florida state-funded Consortium for Medical Marijuana Clinical Outcomes Research. Prior to joining the UF, Dr. Hasan worked as an ORISE Postdoctoral Fellow of Drug Safety and Artificial Intelligence Methods in the Center for Drug Evaluation and Research at FDA. Dr. Hasan has completed PhD and worked as a postdoctoral research scientist at the Decision Analytics Lab at Northeastern University.
Research Focus: Substance use, mental health disorder, opioid related adverse health outcomes, and chronic diseases

Presenter: Medical Marijuana & Me (M³): Crosssectional and longitudinal survey findings from Florida medical marijuana patients
Presenter: The Medical Marijuana Clinical Outcomes Repository (MEMORY): Overview of Florida medical marijuana dispensing data and preliminary results
PhD Student, Pharmaceutical Outcomes & Policy, College of Pharmacy, University of Florida Research Assistant, Consortium for Medical Marijuana Clinical Outcomes Research
Sebastian Jugl is a trained pharmacist, fifth-year PhD student in the Department of Pharmaceutical Outcomes and Policy at the University of Florida, and a research assistant at the Consortium for Medical Marijuana Clinical Outcomes Research. His research employs epidemiological methods and artificial intelligence to develop algorithms for identifying outcomes and exposures real-world data, assessing the safety and effectiveness of medical cannabis and hormonal contraceptives, as well as evaluating substance use policies and programs, including Florida’s medical cannabis program. Sebastian has been recognized with the Emerging Leader Award from the International Society for Pharmacoepidemiology in 2023.
Research Focus: Comparative effectiveness, drug safety, and health services research within the clinical area of women’s health and oncology, focusing on hormonal contraceptives and medical cannabis as pharmacological intervention

Presenter: The Medical Marijuana Clinical Outcomes Repository (MEMORY): Overview of Florida medical marijuana dispensing data and preliminary results
PharmD Candidate, College of Pharmacy, University of Florida
Darla Khouri is a current PharmD candidate at the University of Florida. With an interest in pharmacology and public health she has immersed herself in research opportunities, including work with projects investigating teratogenicity, along with medical marijuana research during pharmacy school. Post graduation plans are to pursue a PGY1 pharmacy residency, with an interest in infectious disease pharmacy and ambulatory care.
Research Focus: The safety and efficacy of medical marijuana use in broad patient populations

Presenter: The Medical Marijuana Clinical Outcomes Repository (MEMORY): Overview of Florida medical marijuana dispensing data and preliminary results
PhD Student, Pharmaceutical Outcomes & Policy, College of Pharmacy, University of Florida Research Assistant, Consortium for Medical Marijuana Clinical Outcomes Research
Priyanka Kulkarni, MPH is a 2nd year PhD student at the Department of Pharmaceutical Outcomes and Policy and a Research Assistant working at the Consortium for Medical Marijuana Clinical Outcomes Research. She is a registered pharmacist from India, and currently, her research focuses on using pharmacoepidemiologic methods to investigate safety, effectiveness and utilization patterns of drugs among pregnant individuals and individuals with chronic illnesses.
Research focus: Using pharmacoepidemiologic methods to assess utilization patterns of drugs and the impact of policy interventions

Presenter: Medical Marijuana & Me (M³): Crosssectional and longitudinal survey findings from Florida medical marijuana patients
Research Coordinator I, Consortium for Medical Marijuana Clinical Outcomes Research, University of Florida
Sophie Maloney serves primarily as the Research Coordinator for the Clinical Core in the Consortium for Medical Marijuana Clinical Outcomes Research. She is also a Research Assistant for the Southern HIV & Alcohol Research Consortium. She completed her bachelor’s degree in Sociology from the University of Florida in 2021 and most recently graduated from Florida International University with a Master of Public Health.
Research Focus: Medical Marijuana, Regulatory Affairs

Moderator: Presentations of Top Abstracts: Cannabis, Women’s Health, and Gender
Professor, Department of Chemistry & Physics, Florida Gulf Coast University
Dr. Sari J. Paikoff received her PhD from UC Berkeley in Chemistry and Post-Doc at Duke Cancer Center. Her research focused on biomedical chemistry which a focus on small molecule drug development. She previously worked as a scientific program manager for the United states Government. Currently she teaches at Florida Gulf Coast University. Her classes included Organic chemistry, General, Organic and Biological Chemistry as well Chemistry and Physics for Nurse Anesthesia. Her current research interests are on scholarship of teaching and learning as well as the chemistry of medicinal plants.
Research focus: Bio-organic and medicinal chemistry, analysis of natural products, the development of sustainable process for manufacturing Shea Butter

Presenter: Medical Marijuana & Me (M³): Crosssectional and longitudinal survey findings from Florida medical marijuana patients
PhD Student, Department of Epidemiology, University of Florida
Juan is a Colombian MD, epidemiologist, and bioethicist with over 12 years of experience in clinical research. Throughout his career, he has been actively involved in conducting multicentric clinical trials, collaborating with the Ministry of Health and the Pharmaceutical Industry to increase knowledge on neglected diseases. In addition, he has served as a research synthesis specialist for different National Clinical Guidelines, including COVID-19, HIV, hypertension, and asthma. He is interested in consolidating his medical research training by pursuing a doctoral program in epidemiology at the University of Florida.
Research focus: Health disparities, clinical trials, medical cannabis

Moderator: Presentations of Top Abstracts: Cannabis Use Patterns and Risk Perceptions in Selected Population
Assistant Professor, College of Nursing, University of Florida
Ellen Terry, Ph.D., graduated from University of Texas at Arlington with a Bachelor of Arts (Honors) in Psychology in 2008. She completed both her Masters of Arts in 2010 and Ph.D. in 2015 in Clinical Psychology, from the University of Tulsa. Dr. Terry completed an NIA-funded T32 post-doctoral research fellowship at the University of Florida, with training focus on pain and aging. In 2024, she completed an NINDS-funded K22 career development award. Dr. Terry is a Principal Investigator of an NIA-funded multi-site R01 study. Dr. Terry is an Assistant Professor in the College of Nursing at the University of Florida.
Research focus: As a pain scientist, Dr. Terry uses evidence-based cognitive and behavioral techniques to successfully teach patients to manage their pain by identifying and changing negative thoughts about pain thereby enhancing positive emotions to directly reduce pain-related suffering. In addition, Dr. Terry is pursuing a highly innovative line of investigation that exploits neuroimaging techniques and machine learning approaches to investigate the neurobiological mechanisms underlying how cognitive and emotional factors influence pain in older adults.

Presenter: Medical Marijuana & Me (M³): Crosssectional and longitudinal survey findings from Florida medical marijuana patients
Moderator: Cannabis, Endocannabinoids and PTSD
Assistant Professor, Department of Epidemiology, University of Florida
Assistant Director - Clinical Core, Consortium for Medical Marijuana Clinical Outcomes Research
Yan Wang is an Assistant Professor of Epidemiology at the University of Florida (UF). She current leads or co-leads several National Institutes of Health (NIH) funded projects that utilize advanced technologies and methods (e.g., wearable sensors, ecological momentary assessment/EMA) to improve the understanding of epidemiology, etiology, and intervention of substance use (e.g., alcohol, medical marijuana).
Research focus: Leveraging advanced methodology and new technology (e.g., wearable sensor) to improve health behavior monitoring and intervention, especially cannabis and alcohol use

Presenter: The Medical Marijuana Clinical Outcomes Repository (MEMORY): Overview of Florida medical marijuana dispensing data and preliminary results
Distinguished Professor, Department of Pharmaceutical Outcomes & Policy, University of Florida Director, Center for Drug Evaluation and Safety (CoDES) Director, Consortium for Medical Marijuana Clinical Outcomes Research
Almut Winterstein has been a fixture within the University of Florida’s College of Pharmacy since 2000, serving as principal investigator on more than 25 extramurally funded grants and contracts and publishing more than 400 manuscripts and conference abstracts. As an expert in drug safety, she chaired the FDA’s Drug Safety and Risk Management Advisory Committee from 2012-2018. Recognizing her contributions in the field, Dr. Winterstein became a fellow of the International Society of Pharmacoepidemiology in 2013, where she currently serves as president. In 2022 she was inducted into the Academy of Science, Engineering, and Medicine of Florida.
Research focus: Post-marketing evaluation of drugs in pediatrics and perinatal care, infectious disease and psychiatry and the evaluation and improvement of quality surrounding medication use using real-world data

Abstract: Anti-fibrotic Effects of Cannabidiol are Diminished When Fibrotic Scar Formation is Active: Implications for Patients with Inflammatory Bowel Disease
Senior Biological Scientist, Gastroenterology, Hepatology & Nutrition, University of Florida
Christopher Broxson is a senior biological scientist in the laboratory of Dr. Ellen M. Zimmermann at the University of Florida. He earned a Bachelor of Science in microbiology in 1995 and a Bachelor of Arts in chemistry in 1996 at Florida Atlantic University in Boca Raton, FL. Upon completing his undergraduate degrees, he accepted a position as a junior chemist in the Materials Science & Engineering department at the University of Florida. In 1997 he transitioned to a senior biological scientist position and joined Dr. Zimmermann’s team in 2013 where he studies inflammatory bowel disease and fibrosis to this day.
Research focus: Inflammatory bowel disease, Crohn’s disease, ulcerative colitis, fibrosis, cannabinoids

Abstract: Prevalence of Mental Health Conditions and Symptoms Among Emerging Adult Cannabis Consumers Compared to NonConsumers: Preliminary Results from the Herbal Heart Study
Research Volunteer, Herbal Heart Study, University of Miami
Alexandria Cashman is a recent graduate of the BSPH program at the University of Miami School of Nursing and Health Studies. She has expanded upon her interests in public health, gastrointestinal disease, and psychiatric conditions as a research volunteer in Dr. Denise Vidot’s Herbal Heart Study. She recently presented her senior thesis on a community-health intervention to bridge the gap between cannabis as a complementary form of medicine for individuals with IBD. With a persistent interest and focus on the medical implications of cannabis, Alexandria is thrilled to present on cannabis use and mental health at CCORC.
Research focus: Mental health symptoms, including heightened sensitivity, stress, irritability, racing thoughts, and mood swings among cannabis consumers and nonconsumers.

Abstract: Patterns and Perceptions of Marijuana use for Symptom Control in Inflammatory Bowel Disease Patients
Assistant Professor, Gastroenterology, University of Florida
Dr. Chaudhry is academic faculty for Celiac and Inflammatory Bowel Diseases (IBD) at the University of Florida, and has a strong focus in clinical and translational research in the field. She completed her medical education at King Edward Medical College, Lahore Pakistan. She then trained at Brookdale University Hospital and Medical Centre, Brooklyn and University of Florida, Gainesville in Internal Medicine and Gastroenterology respectively. Prior to her clinical gastroenterology fellowship, she trained in basic science as a post-doctoral fellow in IBD as well as clinical research methodology as part of her MS degree at UF.
Research focus: I have a focus in health outcomes research in IBD. In my collaboration with the UF Department of Pharmaceutical Outcomes and Policy, I explore health outcomes using big data such as the IBM Marketscan claims database, Medicare and Medicaid databases. Our work focuses on multiple aspects of outcomes in patients with IBD, including risk of cardiovascular disease, patterns of biologic use, infections, epidemiology studies, and health care burden of the college aged transitional population.

Abstract: Effects of cannabis expectancies upon current anxiety and depressive symptoms among women with post-traumatic stress disorder
Research Coordinator, University of California San Diego Research Assistant, University of Central Florida
Jocelyn received her Master’s in Applied Psychology from the University of New Orleans. She has been a research assistant for Dr. Karina Villalba and the Women’s Global Health Research Lab at the University of Central Florida since August 2021. Throughout her education, she has contributed to various research projects including the Biological and Environmental Risk for Affective Disorders Lab which investigates how parent-child relationships effect a child’s risk for developing depression, and the Crescent City Substance Use Lab which focuses on COVID’s impact of isolation on substance use. Jocelyn is employed as a research coordinator for Behavioral Genetics Sibling Study at the University of California San Diego.
Research focus: Sex differences within alcohol and substance use, women’s health, and sex education

Abstract: Pharmacological interactions between cannabidiol and oxycodone in the brain
Associate Research Professor, Department of Orthodontics, College of Dentistry, University of Florida
Dr. Murphy is an associate research professor at the University of Florida (UF), where he performs research at the intersection of neuroscience, psychology and pain. With a diverse background, including tenures at UCLA, RIKEN Japan, and as an executive in the French pharmaceutical industry, he brings a wealth of international experience to his work covering preclinical and clinical research.
Research focus: Interactions between pain and reward systems, with a particular focus on how these dynamics manifest in the context of aging, neurodegeneration and addiction

Abstract: Gender differences in correlations of self-reported marijuana use with a creatininenormalized urine biomarker among persons with HIV
Manager and Analyst II, Research Design and Data Coordinating Center (RDDC), Department of Biostatistics, University of Florida
Dr. Porchia received a MS in mathematics, a MS and a PhD in modeling and simulation as well as a graduate certificate in data mining from the University of Central Florida (UCF). He joined the department of biostatistics at the University of Florida in 2023, affiliated with the RDDC. He is currently working on the analyses for several studies involving alcohol, cannabis, HIV, and gut microbiome. Before joining UF, he was an associate lecturer in the department of mathematics at UCF.
Research focus: His research interests include applying machine learning, artificial intelligence and biostatistics in epidemiology and public health especially involving HIV, alcohol, and cannabis.

Abstract: Cannabis Use During Pregnancy: Trimester-Specific Insights into Cannabinoid Preferences – Results from COVID-19 Cannabis Mom Study
Research Assistant, School of Nursing and Health Studies, University of Miami NIH International Research Fellow, University of Miami & University of the West Indies
Anuradha is a recent Master of Public Health graduate from the University of Miami Miller School of Medicine. She is a research assistant for the Denise C. Vidot Global Cannabis and Psychedelics Laboratory and an NIH research fellow at the University of Miami and the University of the West Indies. Anuradha is passionate about women’s health and global health. She looks forward to seeing how her research efforts will contribute to eliminating gaps in health equity while creating healthier communities worldwide.
Research focus: Women’s health, reproductive health, global health, minority health, health disparities, & mental health

Abstract: Posttraumatic Stress Disorder Symptoms are Associated with Impaired Mnemonic Pattern Separation but Paradoxically Improved Pattern Separation with Comorbid Heavy Cannabis Use
Research Coordinator, Anesthesiology Department, UC San Diego Health Clinical Research Assistant, VA San Diego Healthcare System
Jacob Ross is a graduate student at UC San Diego currently pursuing a master’s degree in biology. A US Navy veteran himself, Jacob is looking to pursue a PhD in clinical psychology and to build a career in both clinical practice and continuing to engage in research addressing the neural mechanisms of trauma and novel therapeutic strategies for conditions affecting veterans. When he’s not in the MRI suite or research clinic, Jacob is involved in opioid overdose prevention efforts in the local San Diego community.
Reseach focus: PTSD, trauma, veterans, cannabis, non-pharmacological & adjunctive pain interventions, clinical trials

Abstract: Oral Delivery of Cannabinoids using Milk Exosomes and their delivery to Breast Tumors: Pharmacokinetic and Pharmacodynamic Investigations
Professor and Section Leader – Pharmaceutics, College of Pharmacy and Pharmaceutical Sciences, Florida A&M University
Dr. Sachdeva got his M.Sc. and Ph.D. of Biopharmaceutics from Dalhousie University, Canada, in 1986 and 1989, respectively. He then worked with SynPhar laboratories in Edmonton, Canada, as a Group Leader, Drug Targeting, during 1989-93, and then moved to academia as an Assistant Professor, Pharmaceutics, at Florida A&M University in 1993 and got promoted to Full Professor in 2002. He has guided 28 Ph.D.’s, 31 Post-Doctorates, and scores of postgraduate and undergraduate students. He has been Editor-in-Chief for CRC Critical Reviews in Therapeutic Drug Carrier Systems (current impact factor of 4.89), since 2007. To his credit he has around 185 original publications, one edited book and 10 book chapters and several Conference Proceedings papers, with Google H-index of 53.
Research focus: Cancer drug delivery (breast and lung cancer), 3D-printing of tumor cells and human cornea, topical and transdermal delivery

Abstract: Sublingually-administered CBD is safe and effective in reducing symptoms associated with strenuous exercise
PhD Student, University of Florida Research Coordinator, Sports Medicine & Human Performance Research Laboratory
John Stauffer is the Research Coordinator at the Sports Medicine & Human Performance Research Laboratory at The University of Florida. In 2021, John received his bachelor’s degree in Health, Exercise and Sports Studies from Denison University. In 2023, John received his Master of Science in Applied Physiology and Kinesiology at the University of Florida. He is now working toward his PhD in Sports Medicine at the University of Florida. He is currently involved with clinical research, observing pain management and modulation through drug and technology mechanisms.
Research focus: Cannabis use, alcohol use, anxiety, depression, childhood abuse, intimate partner violence

Abstract: What are the odds of dying from drug intoxication among cannabis users who also used opioids, kratom, and alcohol?
Assistant Professor, Christine E. Lynn College of Nursing, Florida Atlantic University
Dr. Armiel Suriaga is an assistant professor at Florida Atlantic University. The National Institute on Drug Abuse Diversity Scholars Network selected him as a scholar in 2023. He is also a Master of Public Health in Epidemiology scholar at Harvard University T.H. Chan School of Public Health. Dr. Suriaga completed his Ph.D. at FAU in 2021, receiving several awards, including the Daisy Award, excellence in leadership, scholarship, and service awards. He was also a faculty scholar of the American Association of Colleges of Nursing and Johnson and Johnson in 2018 and 2019. He has presented his scholarly work at regional, national, and international conferences. His innovative research on cannabis was featured in several media outlets in the U.S., such as Sun Sentinel, Denver7News, Pain News Network, Health Leaders Media, Hemp Gazette, and SWISSINFO.CH., as well as some Spanish news outlets.
Research focus: Substance use, misuse, and abuse, particularly opioids, kratom, and cannabinoids

Abstract: Cannabis Consumption and Problems in the Family: Differences Across Gender, Ethnicity, and U.S. Nativity Among Young Adult Cannabis Consumers - Preliminary Insights from the Herbal Heart Study
Undergraduate student, University of Miami
Melanie is a psychology major on the pre-medical track at the University of Miami. She is a first-generation student. She loves to read, travel, and spend quality time with her loved ones.
Research focus: Cannabis usage and its correlation with cardiovascular health
Anuradha Ramdas
University of Miami
Co-authors: Amrit Baral1, Ranya Marrakchi El Fellah1, Bria-Necole Diggs1, Cynthia Lebron1, Sarah E Messiah2, Denise C Vidot1
1University of Miami, 2University of Texas
Background: Increased rates of cannabis use during pregnancy emphasize the need for further research on the effects of cannabis and cannabinoids to safeguard maternal and fetal health. While research on this topic is emerging, there is a crucial gap in the pattern of cannabinoid preferences and cannabis use during pregnancy by trimester. This study aims to provide trimester-specific insights into cannabinoid use patterns among pregnant individuals.
Methods: This analysis draws data from the COVID-19 Cannabis Mom Study, a cross-sectional investigation into cannabis use during pregnancy and breastfeeding. Informed consent and data collection were facilitated through REDCap. Participants utilized an electronic survey link to self-report their cannabinoid usage, patterns, and behaviors during pregnancy. Descriptive statistics, implemented via SAS Analytics, were employed to compute and present information on cannabis use and dominant cannabinoids consumed across trimesters during the participant’s current pregnancy.
Results: In the total sample (N=252, mean age 31.2 years (SD=6.0).), 32.1% (n=81) reported currently being pregnant. Within this group, the majority were in their second trimester (43.2%), followed by third (35.8%) and first trimester (21.0%). Of those currently pregnant, 95.1% reported cannabis use before pregnancy, and 90.1% continued during pregnancy. Among pregnant individuals that repor ted THC as the dominant cannabinoid consumed, the highest prevalence of use was in the third trimester (42.5%) compared to 23.4% in the first trimester and 34.0% in the second trimester. CBD-THC ratio dominant cannabinoid was most prevalent during the second trimester (47.6%) compared to 23.8% in the first trimester and 28.6% in the third trimester. Most (85.7%) of those unsure of the dominant cannabinoid used during pregnancy were in their second trimester compared to 14.3% in the first trimester and 0.0% in the third (overall p=0.10).
Conclusion: Results revealed that most pregnant individuals, particularly those in their second or third trimester, were utilizing cannabis to alleviate pregnancy-related symptoms during the COVID-19 pandemic. Additionally, the findings showed a difference in cannabinoid dominance by trimester. These findings underscore the need for trimester-tailored interventions and education for pregnant individuals and healthcare providers that address potential risks and benefits associated with cannabis use during each trimester of pregnancy.
Jocelyn Mueller
University of Central Florida
Co-authors: Karina Villalba1, Jamia Sapp1, Robert Cook2, Christa Cook1, Dinender Singla1, Amie Newins1, Jennifer Attonito3
1University of Central Florida, 2University of Florida, 3Florida Atlantic University
Background: This study sought to identify whether expectancies regarding the effects of cannabis to suppress anxiety and depression mediate the connection between historical cannabis use and current reported levels of anxiety and depression among women with and without PTSD.
Methods: Data was analyzed from 300 women who reported via online survey any historical use of cannabis and scored ≥1 on the PTSD-4 scale. Dependent variables were current levels of anxiety and depression. Mediating variables were positive versus negative cannabis expectancies. T-tests assessed whether variables differed between PTSD-positive and -negative women. Ordinary least squares (OLS) mediation models tested cannabis expectancies for anxiety and depression as a mediator between historical cannabis use (dichotomized at <3 years and 3+ years of use) and current anxiety and depression levels among PTSD-positive women.
Results: Of participants, 57% screened positive for PTSD. Differences were observed in anxiety (p = 0.001) and depression (p = 0.001) levels between positive and negative PTSD groups; no sociodemographic differences existed between groups. Participants who used cannabis for 3+ years had higher positive cannabis expectancies and lower levels of current anxiety. The mediation model for depression was significant (indirect effect = 0.35, SE = 0.16, 95% CI = 0.070 to 0.709) among PTSD-positive women. The indirect effect of positive cannabis use expectancies in the anxiety model was significant (indirect effect = 0.26, SE = 0.13, 95% CI = 0.028 to 0.543) among PTSD-positive women. The depression model was partially mediated while the anxiety model was fully mediated.
Conclusion: Findings show that positive cannabis expectancies contributed to the relationship between historical cannabis use and current lower levels of depression and anxiety, suggesting a psychological component to the effects of cannabis on the mental health of women with PTSD.
Melanie Zamora University of Miami
Co-authors: Amrit Baral1, Bria-Necole A Diggs1, Ranya Marrakchi El Fellah1, Sarah Messiah2, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1 1University of Miami, 2University of Texas, 3Florida International University
Background: Cannabis usage amongst the family circle generates inquiry whether it displays a negative impact towards domestic interactions; accompanied by the distribution of problems arising from its anticipated utilization. This study aims to examine family dynamics among cannabis consumers with respect to social determinants of health (gender, ethnicity, and US nativity.
Methods: This analysis utilized data from the ongoing Herbal Heart Study Cohort (n=150), which explores the impact of cannabinoids and different cannabis consumption methods on subclinical cardiovascular risk among young adults aged 18-35 in South Florida. Cannabis use was self-reported and confirmed through rapid urine drug screening. As part of the Marijuana Problem Scale (MPS) questionnaire, participants were queried about potential family issues arising from cannabis consumption, with response options ranging from “no problem” to “minor problem” and “serious problem.” For the purpose of this analysis, responses were coded into a binary variable, simplifying to “Yes” if any problem was reported and “No” otherwise. Participants self-reported US nativity (US-born vs Foreign-born) and ethnicity as Hispanic/Latino or non-Hispanic. Descriptive statistics were employed for prevalence, and significance tests were conducted using Chi-squared tests with SAS Analytics.
Results: Among the total cannabis consumers (n=76), 57.9% were female, with a mean age of 25.0 years; 55.3% identified as Hispanic/Latino, and 75.0% were born in the US. Overall, 25.3% of the sample reported cannabis-related family problems. There was no significant difference in current age (p=0.2698) as well as age of cannabis use initiation (p=0.7181) between cannabis users repor ting family problems and those who did not. However, a notable disparity emerged between Hispanics and non-Hispanics, with 38.1% of Hispanics repor ting problems compared to 8.8% of non-Hispanics (p=0.0034). Sex differences were not significant (p=0.9370). Interestingly, a higher percentage of foreign-born young adults reported family problems caused by cannabis compared to US-born individuals (47.4% vs. 17.5%, p=0.0093).
Conclusion: The results highlight a relationship between the Hispanic community, family, and cannabis consumption. Ethnicity emerged as a significant factor, sparking interest in its relationship with cannabis usage. Further exploration is needed to understand how cannabis consumption impacts familial relationships negatively, underscoring the need for additional research in this domain.
Dr. Donald Porchia
University of Florida
Co-authors: Yancheng Li, Michael Truver, Bruce Goldberger, Eric C Porges, Yan Wang, Samuel Wu, Robert L Cook University of Florida
Background: Cannabis use is common among persons with HIV (PWH). However, accurately quantifying cannabis consumption and its components such as THC has been a long-standing challenge due to the variety of cannabis products available, variability in smoking and other consumption behaviors, as well as the reliability and validity of self-reported cannabis measures. Further, the relationship between a timeline follow back (TLFB) and cannabis metabolites/biomarkers in older PWH has been less explored. We sought to determine the correlation between the selfreported quantity of cannabis use in grams per day (overall and flower-specific) with a creatinine-normalized urine biomarker (THC-COOH). We also explored whether the correlations differed by gender at birth, and whether the correlations would improve if we used the self-reported potency to weight the quantity of cannabis consumed.
Method: Data were collected from 2018-2022 from participants in the MAPLE study, a longitudinal study examining health effects of cannabis among persons with HIV in Florida. This analysis included data from 253 PWH (mean age 49, 41% Female, 16% White, 68% Black, and 13% Hispanic) who used cannabis products. The quantity of daily cannabis use over the past 30 days was collected by a trained interviewer using a self-reported, calendar-based TLFB and pictures to help estimate grams of flower. Using these findings, cannabis quantity was summarized as grams of flower per day and converted to a standardized 15% THC flower grams per day since most flower was obtained from non-dispensary sources. Urine THC-COOH, a biomarker for THC, was determined by mass spectroscopy from 103 samples. Spearman correlation coefficients were used to compare creatinine-normalized THC-COOH levels with grams and potency-adjusted grams per day both overall and flower-specific as stratified by gender.
Results: Among the 103 PWH with THC-COOH results, grams and potency-adjusted grams per day both overall and flower-specific were all significantly associated with THC-COOH urine biomarkers (r = 0.43-0.45, p < 0.01). When stratified by gender at birth, the correlations showed a stronger relationship for males (r = 0.54-0.58, p < 0.01) than for females (r=0.27-0.32, p=0.08-0.21).
Conclusions: TLFB is a valid instrument to measure self-reported marijuana use. However, the association between self-reported consumption of cannabis with urine THC-COOH biomarkers is stronger in males than in females. It is worth noting that our population consisted of older adults living with a chronic condition, HIV, so further investigation may be needed to explore the association between self-reported cannabis consumption and urine biomarkers among females.
Alexandria Cashman University of Miami
Co-authors: Amrit Baral1, Bria-Necole A Diggs1, Ranya Marrakchi El Fellah1, Sarah E Messiah2, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1 1University of Miami, 2University of Texas, 3Florida International University
Background: As cannabis legalization, normalization, and its use expands, the incidence rates of mental health conditions and symptoms in young adults, a population with a relatively higher prevalence of cannabis use, has been on rise. Understanding the mental health implications of cannabis consumption in the younger population is crucial as this milestone is critical for brain development and emotional regulation. The study aims to shed light on the varied manifestations of mental health symptoms, including heightened sensitivity, stress, irritability, racing thoughts, and mood swings among cannabis consumers and non-consumers.
Methods: The data analyzed are from an ongoing Herbal Heart Study cohort of young adults aged 18-35, to examine the impacts of cannabinoids and diverse cannabis consumption methods on subclinical cardiovascular risk. Cannabis use was selfreported and further confirmed by rapid urine drug screening during enrollment. Participants underwent a comprehensive mental health review using standardized measures, reporting any experienced mental health-related conditions or symptoms within the preceding 30 days. Prevalence of the conditions and/or symptoms were compared between cannabis users (CUs) and non-users (NUs). Descriptive statistics were computed and Chi-squared/Fisher’s exact tests where appropriate were conducted using SAS Analytics with a two-tailed alpha set to 0.05.
Results: In the overall sample of 150 young adults, mean age was 26.4 years (SD=4.5), 66.7% were female, 51.3% Hispanic/Latino and 50.7% cannabis users. 20% reported experiencing depression, with a significant difference noted between CUs at 30.3% and NUs at 9.5% (p<0.01). Anxiety was reported by 35.3% of the sample, predominantly among CUs (48.7%) compared to NUs (21.6%, p<.001). While 14.7% reported excessive worries overall, no significant difference was found between CUs and NUs (p=0.188). Significant differences in sensitivity were observed between CUs and NUs (15.8% vs 4.0%, p=0.017). Stress was reported by 42.7% of young adults overall, with no significant difference in prevalence between the two groups (p=0.602). Irritability was more prevalent among CUs (26.3% vs 8.1%, p<.01). Additionally, racing thoughts were reported by 21.0% of CUs compared to 5.4% of NUs (p < .01), and mood swings were noted in 14.5% of CUs versus 4.0% of NUs (p=0.028).
Conclusion: Notably, higher prevalence of depression, anxiety, irritability, racing thoughts, and mood swings were observed among cannabis users than non users, highlighting the need for targeted interventions addressing the mental health implications of cannabis consumption in this demographic.
What are the odds of dying from drug intoxication among cannabis users who also used opioids, kratom, and alcohol?
Dr. Armiel Suriaga
Florida Atlantic University
Co-authors: Oliver Grundmann2, Lenny Chiang-Hanisko1, Raquel Panos1, Sebastian Kuzak1
1Florida Atlantic University, 2University of Florida
Background: Drug-related overdose or intoxication is a serious public health issue that has claimed the lives of more than one million people since 1999. The National Institute on Drug Abuse (2023) reported a steady increase in drug-involved overdose death rates from opioids, stimulants, benzodiazepines, and antidepressants. Opioids contributed to nearly 70% (70,601 out of 106,000 deaths) of these deaths in the United States in 2021 alone. However, the association of cannabis use with drugrelated intoxication (DI) is seldom reported.
Objective: Our study aimed to report our preliminary findings on the association of cannabis use with DI, leading to a fatality.
Methods: We used de-identified data from the Florida Department of Law Enforcement from 2020 to 2021. Analyses included descriptive statistics and regression modeling with Stata 17. We restricted our analysis to the association of cannabis use with DI among those who also used alcohol, opioids, and kratom. The presence of mitragynine in biological fluids commonly identifies kratom use. We dichotomized DI (yes/no) as the cause of death as determined by the medical examiners through autopsy and toxicology results.
Results: Our results indicated that 2,888 out of 7,287 decedents with cannabis use died from DI. Among decedents with cannabis use, the mean age was 38.34 (SD= 14.8) and ranged from 0-94 years. Males are more affected (n=5,830 or 80.01%), white (n=4,973 or 68.3%), and those in the 25-34 age group (n=2,037 or 28%), followed by the 35-44 age group (n=1,596 or 22%). Among cannabis users, 5,304 (72.8%) used two or more substances; 87 used kratom, 3,113 used opioids, and 2140 used alcohol. In the intercept model, the odds of dying from DI increased by .63 times compared to the odds of dying among non-cannabis users. After controlling for confounders (age, gender, ethnicity, opioid, alcohol, and kratom), the odds of dying from DI among those who used cannabis was .60 (OR=.60, [95% CI .59, .68]), p=<0.001. Among those who also used opioids, the odds of dying from DI increased (OR=15.92, [95% CI 14.97, 16.93]), p=<0.001; mitragynine, (OR=5.06, [95% CI, 3.77, 6.80]), p=<0.001. No significant result with alcohol (OR=.95, [95% CI .89, 1.01]), p=0.103. Limitations of the study included no data on cannabis doses and frequencies, cannabis source, and indications of use.
Conclusion: This result has clinical implications among those who co-use cannabis with opioids and kratom, which necessitates innovative harm reduction strategies and education dissemination for public safety, particularly young adult users.
Dr. Naueen Chaudhry University of Florida
Co-authors: Karen Yung, Hanzhi Gao, Chelsea Salmon, S Devi Rampertab, Angela Pham, Ludmila B De Faria, Ellen M Zimmermann University of Florida
Introduction: Inflammatory bowel disease (IBD) patients sometimes use marijuana for disease-related symptoms. Data regarding use and impact of marijuana in this population is lacking. Our study explores patterns of marijuana use, underlying symptom response, and beliefs about marijuana in patients with IBD.
Methods: Anonymous survey comprising 39 questions on demographics, disease features, patterns of marijuana use, disease symptoms, quality of life, and true/ false statements about marijuana was administered via REDCap to 108 participants recruited from University of Florida (UF) IBD clinic. Summary statistics stratified by diagnosis, hospitalization, other complications, marijuana usage, and outcomes were examined. As appropriate, Wilcoxon-Mann-Whitney tests and Kruskal-Wallis Rank Sum tests were used for continuous variables, and Pearson’s Chi-squared tests and Fisher’s exact tests were used for categorical variables. Logistic regressions were used to investigate patterns of marijuana use, hospitalization, and bowel surgery. Proportional odds logistic regression was used to investigate patterns of marijuana use and improvement in symptoms.
Results: The participants were 51(47.2%) male, 56(51.9%) female,1 unreported gender. Age distribution was 17-25 yrs(13.9%), 26-45 yrs(50%), 46-65 yrs(26.9%) and >65 yrs(9.3%). The majority (61.9%) reported medical marijuana use. However, younger age (p=0.007), and duration of IBD diagnosis5 years (OR 21.94, CI [2.91, 250.18], p=0.0059) and marijuana use 1 or more times weekly (OR 11.13, CI [1.78, 97.69], p=0.0163. Marijuana users with a history of hospitalization for IBD had higher odds of having depression/anxiety (OR 14.3, CI [2.34,143.2] p=0.009) and diarrhea symptoms (OR 13.3, CI [2.2,128.9] p=0.01). Additional results attached in Figures 1 and 2.
Conclusion: Marijuana can be helpful for symptom control, improving quality of life, and limiting opioid use in IBD patients. Patients demonstrate good insight about its role in the management of their disease. Our findings are limited due to sample size and possible positive response bias since participants were current marijuana users.
Jacob Ross
University of California San Diego
Co-authors: Bruna Cuccurazzu1, Cindy Napan1, Dean T Acheson1,2, Dewleen G Baker1,2, Victoria B Risbrough1,2, Daniel M Stout1,2
1University of California San Diego, 2VA San Diego Healthcare System
Background: Posttraumatic stress disorder (PTSD) is associated with impaired ability to use contextual cues to regulate emotional responses. Contextual learning is a hippocampus-dependent process that underlies the ability to differentiate novel cues from previously learned but similar stimuli. Heavy cannabis use is highly prevalent in individuals with PTSD. With the advent of recreational and medicinal cannabis availability, the impact of heavy cannabis use in individuals with PTSD on contextual learning mechanisms is poorly understood.
Objective: To test the hypothesis that heavy cannabis use would be associated with significant disruptions in hippocampal-dependent memory in individuals with PTSD symptoms using the Mnemonic Similarity Task (MST).
Methods: To investigate the relationship between heavy cannabis use and PTSD on pattern separation ability, data from two independent samples with the same inclusion criteria were combined. Adult participants (n = 123; 31 female) with and without heavy cannabis use and with a range of PTSD symptoms completed the mnemonic similarity task to assay mnemonic pattern separation ability, and selfreport measures of PTSD severity (PCL-5), depression symptoms (BDI-II), and cannabis use (CDDR) were collected.
Results: In the no cannabis use group, increasing PTSD symptom severity was associated with lower mnemonic pattern separation performance (p=.005). In contrast, in heavy cannabis users, increasing levels of PTSD symptom severity was associated with greater pattern separation performance (p=.032), but after including depression symptoms (BDI-II) as a covariate, this relationship was no longer significant (p=.96). Secondary analyses indicated that at low levels of PTSD symptom severity, heavy cannabis use is associated with lower pattern separation ability compared to those without heavy cannabis use; we also show preliminary evidence that this pattern is stronger in women than in men.
Conclusions: These results provide evidence that heavy cannabis use may have a detrimental impact on contextual learning ability but may spare this ability in individuals with elevated PTSD symptoms. Future work should include collection of hormonal assays and measures of both endogenous and exogenous cannabinoid levels to examine their interacting contributions on hippocampal-dependent mnemonic processes.
Dr. Mandip Sachdeva Florida A&M University
Several studies have shown that cannabinoids possess anticancer activities including cell migration inhibition, anti-proliferation, apoptosis and anti-angiogenesis against various cancers including breast, skin, lung, prostate and glioblastomas. However, cannabinoids such as CBD have poor bioavailability (13-19%) when taken orally due to their first pass metabolism, high lipophilicity (log P values of > 5) and low aqueous solubility (2–10 μg/ml in water). Milk exosomes have shown promise as novel therapeutic possibilities for the treatment of several illnesses, including cancer. Human, bovine, porcine, horse, yak, sheep, and goat are among the species from which exosomes have been isolated. Exosomes derived from these milk sources have been reported to have anti-inflammatory, antioxidant, anticancer and antimicrobial properties. Camel milk and its components have been reported to possess anticancer activity against a range of cancer diseases. We explored the potential of Camel milk derived exosomes (CMDE) to enhance the bioavailability of CBD. CMDE, isolated and purified through differential ultracentrifugation, showed it to be a promising carrier due to their high yield and economical scalability compared to other sources. Our in-vitro cytotoxicity studies demonstrated the anticancer potential of CMDE against DOX resistant MDA-MD-231 and RM resistant MDAMB-468 cell lines. In-vitro permeability studies using MDCK cells demonstrated the ability of CMDE to traverse tight junctions, while high drug loading and entrapment efficiency contributed to improved overall bioavailability of CBD. Specifically, our in-vivo pharmacokinetic study (PK) in SD rats revealed a significant enhancement in bioavailability for the CBD-CMDE compared to the control group. Furthermore, PK studies showed enhanced bioavailability of CBD from CBD-CMDE with AUC(0-24h) of 1350.56±187.50 ng/mL*h as compared to CBD control formulation with AUC(024h) of 351.95±39.10ng/mL*h. Further CMDE containing Vybrant DiO when given to tumor bearing animals by the oral route was found localized in tumors which further supports our Pk observations. Overall, CMDE can be used to enhance the oral absorption of poorly bioavailable APIs making it a noteworthy contribution to the field.
John Stauffer University of Florida
Co-authors:
Paul A Borsa, Joshua A Crow, Mark D Bishop, Robert L Cook University of Florida
Context: Current research has shown evidence that phyto-cannabinoids may have a promising therapeutic potential in a variety of physical ailments, and cannabidiol (CBD) is of particular interest due to its positive safety profile, non-intoxicating effects, and widespread capabilities in a number of musculoskeletal diseases. Very little is known about CBD and how it functions in the body from both an efficacy and mechanistic perspective, especially in humans. Our objective was to investigate the therapeutic impact of a controlled short-term trial of CBD use for reducing symptomatic response and facilitating recovery following induced muscle injury.
Methods: A double-blind, randomized, two-arm study design was used with participants randomly assigned to either an active CBD dose group or a placebo control group. Participants completed a 15-day study trial which included baseline testing, intervention (CBD/placebo dosing regimen), and follow-up assessments. Participants self-administered the investigational product (CBD or placebo) under the tongue (sublingual) twice daily for 15 days. Daily dosage of CBD was 67mg. An experimental injury protocol for the quadriceps muscle group on day 10 induced pain and functional disability in otherwise healthy men (n=9) and women (n=20) [age: 20.1 yrs, weight: 64.2±8.5kg, height: 169±5.3cm]. Follow-up measurements occurred on days 11 through day 15 (24 to 96-hours post-exercise).
Results: There were no reports from participants of side effects or treatmentemergent adverse events from consuming the CBD or placebo (Pla). This indicates that the product was safe to use and well tolerated by the participants. The design was statistically underpowered (p-values > 0.05), but trends were observed for reduced symptomatic response and improved recovery. Symptoms and functional deficits were most pronounced 24 to 48 hrs. post-exercise and were least pronounced by day 5. Pain was reported using a numerical rating scale (0 – 100) with 0 indicating ‘no pain’ and 100 indicating ‘worst pain imaginable’. A trend was observed for CBD users to report less pain at rest (PAR) and movement-evoked pain (MEP) after exercise especially at 48-hrs post-exercise [PAR (CBD = 52/100 v. Pla 63/100)] and [MEP (CBD = 23/100 v. Pla 38/100)]. The CBD group also reported that they were more functional (CBD = 68/100 than placebo (61/100) at day 2 postexercise.
Conclusions: CBD administered sublingually demonstrated a favorable safety profile and showed promise in reducing symptoms associated with strenuous exercise. Clinical studies using larger sample sizes are needed to confirm the reported trends in controlling pain and function post-exercise.
Christopher Broxson University of Florida
Co-authors:
Ellen M Zimmermann, University of Florida
Background: Inflammatory bowel disease (IBD) is divided into two subcategories known as ulcerative colitis (UC) and Crohn’s disease (CD), of which CD is qualifying medical condition for medical cannabis use. Chronically recuring IBD flares can cause serious medical complications due to a buildup of collagen-rich fibrotic scar tissue in the intestine. In models of skin, liver, and airway fibrosis, the cannabis component cannabidiol (CBD) has antifibrotic therapeutic potential.
Objective: Here, we seek to understand the influence of CBD on human intestinal myofibroblasts (hIMF), the primary cell responsible for fibrotic scarring, to better understand the implications for IBD patients.
Methods: Cultured hIMFs were exposed to 1µM CBD for 4hr before (-4hr), simultaneous to (0hr), or 4hr after (+4hr) fibrotic stimulation using 5ng/ml transforming growth factor beta-1 (TGF) for 20hr to mimic the pro-fibrotic environment of human disease. To interrogate the peroxisome proliferator-activated receptor gamma (PPARG) pathway, 10µM of the PPARG antagonist T0070907 was administered 1hr prior to CBD treatment and TGF-stimulation. Gene expression was measured by qPCR and secreted collagen protein was analyzed by ELISA. Statistical analysis was done using 1 way ANOVA with Sídak’s multiple comparisons correction.
Results: As expected, TGF-stimulation increased pro-fibrotic gene expression compared to vehicle-treated controls (COL1A1 p<0.0001; SERPINH1 p=0.0002; ACTA2 p<0.0001; CCN2 p=0.007). Compared to cells only stimulated with TGF, cells pre-treated with -4h CBD had significantly lower fibrotic gene expression (COL1A1 p0.05). Compared to vehicle-treated cells, cells exposed to only CBD at any time point increased expression of PPARG (-4hr CBD p<0.001; 0hr CBD p=0.003, +4hr CBD p<0.0001). However, compared to TGF-stimulated cells, only the -4hr CBD with TGF increased PPARG mRNA (p=0.001) and decreased COL1A1 protein secretion (p=0.04). Time-course experiments revealed TGF to be a potent, quick-acting, and long-lasting suppressor of PPARG gene expression implicating the PPARG nuclear receptor as a possible CBD effector pathway. Surprisingly, the PPARG blocker failed to block the effects of CBD.
Conclusions: Pretreatment with CBD effectively reduced collagen gene and protein expression and thus had clear anti-fibrotic effects. However, in the presence of TGF, a common mediator of scar formation, the effects of CBD were abrogated. Therefore, the timing of CBD treatment is critical to its actions and may limit its potential efficacy an anti-fibrotic for IBD patients and beyond.
Dr. Niall Murphy
University of Florida
Co-authors: Ariana C Brice-Tutt, Alexandria S Senetra, Tyler Serres, Abhishek Gour, Marcelo Febo, Adriaan W Bruijnzeel, Wendi Malphurs, Azin Behnood-Rod, Cassidy Kramer, Robert M Caudle, Barry Setlow, Abhisheak Sharma, and John K Neubert University of Florida
Background: We previously showed that co-administering cannabidiol (CBD) potentiates the analgesic actions of the opioid oxycodone in a rat model. In contrast, CBD does not potentiate the rewarding actions of oxycodone in the absence of pain. CBD also has little effect on behavioral sensitization to oxycodone. Given the apparent contrasting effects of CBD on oxycodone’s analgesic and rewarding properties, we sought to elucidate peripheral and central sites at which CBD and oxycodone may interact.
Objective: Determine pharmacokinetic interactions between CBD and oxycodone in the plasma and brain, and the impact of co-administration on brain neurochemistry.
Methods: Male and female Sprague Dawley rats were allocated to one of three treatment groups: CBD (10 mg/kg), oxycodone (0.56 mg/kg), or CBD plus oxycodone (10 and 0.56 mg/kg respectively). Rats received daily intraperitoneal administration of drugs for two weeks. Blood samples were taken periodically. Brains were extracted after the final drug administration. Tissue punches of the periaqueductal gray, nucleus accumbens and anterior cingulate cortex were collected from 100 micrometer frozen sections. Plasma and brain tissue were analyzed using mass spectrometry for CBD, oxycodone, their metabolites, and a panel of neurochemicals including monoamines and acetylcholine.
Results: Co-administration of CBD with oxycodone generally potentiated plasma and brain levels of oxycodone, and impeded oxycodone’s metabolism. In contrast, CBD metabolism appeared to be slightly accelerated by the presence of oxycodone. Rats given oxycodone alone generally had the largest positive difference in brain neurochemical content, particularly serotonin. In contrast rats given CBD plus oxycodone generally exhibited similar brain neurochemical content as rats given CBD alone. These results suggest that CBD co-administration might attenuate the neurochemical effects of oxycodone.
Conclusions: The apparent paradox of CBD’s ability to potentiate oxycodone analgesia without potentiating oxycodone’s rewarding effects cannot be explained by a generalized potentiation of oxycodone bioavailability. Our findings suggest that CBD co-administration might normalize the impact of oxycodone on brain neurochemical activity, thus providing an explanation for why CBD does not impact the rewarding actions of oxycodone; however, the sites at which CBD potentiates the analgesic actions of oxycodone remains undetermined.
Mounika Aare Florida A&M University
Co-authors: Breana Boirie, Jassy Lazarte, Aakash Nathani, Mandip Singh Florida A&M University
Objective: The objective of this study was to evaluate the effect of combinations of various cannabinoids and terpenes against drug-resistant lung and breast cancers.
Methods: Several cannabinoids including cannabichromene (CBC), cannabidiolic acid, cannabidivarin, cannabinol, cannabigerol and terpenes; β-caryophyllene (BC), bisabolol, myrcene, linalool, limonene, geraniol, nerolidol, α-pinene, α-terpineol, and γ-terpinene were screened for their anticancer activity against doxorubicinresistant (DOX-RT) MDA-MB-231 breast cancer, and osimertinib-resistant H1975 (with EGFR, T790M, L858R mutations) and PDX lung cancer cell lines (with EFGR, L858R mutations) using 2D cytotoxicity and 3D spheroids assays. Combination index (CI) values of cannabinoids with BC were evaluated using compusyn software. Other assays such as colony formation, wound healing, apoptotic assay, and cell-cycle analysis by flow cytometry were done to investigate the possible mechanisms underlying the synergism of the combinations investigated. In-vivo
studies were conducted to further test the efficacy of combinations. Briefly, 5 million DOX-RT MDA-MB-231 cells were injected subcutaneously into the right flank region of BALB/c nude mice. The animals were treated after the tumor volume reached 180 – 200 mm3. The animals were administered CBC (15mg/kg, i.p.), BC (100mg/kg, i.p.), and CBC+BC thrice a week for two weeks. Western blotting and qPCR was done to understand the molecular mechanisms.
Results: It was observed that CBC, CBDA with BC over a concentration range of 0.3-10µM has shown strong synergism with CI values of 0.1-0.4 whereas other combinations of CBG+BC, CBDV+BC, and CBN+BC have shown synergism at low concentrations but strong antagonism at high concentrations (5, 10µM). CBC+BC was the most potent combination among the in-vitro studies, and hence, was further evaluated in in-vivo tumor xenografts. The tumor volume in the combination group was reduced two-fold relative to individual treatments (p<0.001) and fourfold relative to control (p<0.0001). Western blot analysis of tumor xenografts revealed downregulation of apoptotic markers: PARP (p<0.0001), mTOR (p<0.001), pAMPK (p<0.001), surviving (p<0.0001); autophagy markers, LC3 (p<0.001) and Glypican 5 (p<0.0001); and migration markers, vimentin (p<0.0001) and integrin (p<0.0001). Immune checkpoint proteins PD-L1 (p<0.0001) and PD-1 (p<0.0001) were also downregulated by combination treatment. Few of these markers like PD-L1, PARP, mTOR were further confirmed by qPCR and found to be significantly downregulated as well. CBC was found to induce apoptosis and autophagy considerably more potently than BC; whereas BC inhibited cancer cell migration which explains the synergism of CBC+BC.
Conclusion: The results obtained
emphasizes that the combination of CBC and BC can successfully overcome doxorubicin resistance in TNBC.
Breana Boirie Florida A&M University
Co-authors:
Mandip Sachdeva, Florida A&M University
Background: Pancreatic ductal adenocarcinoma (PDAC) has the fourth highest mortality rate amongst all cancer types. Gemcitabine is the standard treatment for PDAC however resistance to this drug does occur over time. Cannabinoids have been proven to have anti-cancer properties since cannabinoid receptors are well overexpressed in pancreatic cancer.
Objective: The objective of this study was to test the efficacy of combination of cannabinoids against pancreatic cancers.
Methods: Several cannabinoids such as cannabichromene (CBC), cannabidiol (CBD), cannabigerol (CBG), cannabinol (CBN), cannabidivarin (CBDV) were screened for their anticancer activity against MIAPACA 2 Wild Type (WT) and PANC1 Wild Type (WT). Combinations of selected cannabinoids were evaluated to determine the most potent combination. Combination Index (CI) values were calculated for the tested combinations using compusyn software. Furthermore, the cannabinoids were also tested in 3D Spheroids using magnetic nanoshuttles against MIAPACA 2 WT cells.
Results: The IC50 values of cannabinoids were found to be in the range of 4-10 μM with CBC and CBD
being the most potent cannabinoids. CBC IC50 values were found to be 5.4±0.2 μM and 4.87±0.4 μM against MIAPACA and PANC1 cell lines respectively whereas IC50 values of CBD were found to be 4.32±0.22 μM and 5.09±0.1M. CBC+CBD combination was the most potent of all the tested combinations. The IC50 value of CBC+CBD reduced by approximately 3.5 folds. Moreover, the CI value of CBC+CBD was 1) at low concentrations. As expected, the IC 50 values of cannabinoids increased when screened against 3D spheroids. The development of Gemcitabine resistant MIAPACA 2 and PAN 1 cell lines are ongoing. The mechanism underlying the synergism of CBC+CBD was anticipated to be associated with PD-L1-NF-KB pathway and will be investigated in the future.
Conclusion: CBC+CBD combination was found to be the most effective combination in treating pancreatic cancer.
Mayilvanan Chinnaiyan University of Oklahoma
Co-authors: Daniel Brobst, Geraldine Chissoe, Balaji Sadhasivam, Vengatesh Ganapathy, Lurdes Queimado University of Oklahoma
Introduction: Cannabis and tobacco rank among the most widely used drugs globally. Tobacco use has decreased in the past decade, but use of electronic cigarettes (e-cig) has increased steeply in US among youth and combustible tobacco smokers. The prevalence of cannabis use and co-use with tobacco products has increased steeply. Smoked cannabis is the most common form of
use among cannabis users. Combusted cannabis results in a significant buildup of harmful substances in the oral cavity and cannabis use has been shown to increase the progression of oropharyngeal cancer. Some cannabinoids have been identified as anti-inflammatory agents; while others are approved for use in palliative care. However, health implications of smoking cannabis and its co-use with tobacco products use remain uncertain. There is a need to understand the effects of cannabis use and co-use with tobacco and e-cigarettes on oral inflammation.
Aim: To characterize the oral inflammatory patterns among cannabis smokers, tobacco smokers, and e-cig users.
Methods: Upon ethical approval, participants were recruited through a secure online survey platform. Following self-reporting and biochemical confirmation, participants were categorized into four groups: Non-users (NU), exclusive cannabis smokers (CAN), exclusive e-cigarette users (EC), and combustible tobacco users (TOB). Saliva samples were collected to evaluate 37 markers of inflammation using an ELISA based assay (Bio-Plex Pro, Bio-Rad). Data was analyzed by ANOVA and independent t-tests.
Results: Data from 45 participants is currently complete: 8 (NU), 11 (CAN), 10 (EC), and 16 (TOB). Compared to non-users, 7 key pro-inflammatory markers were increased in cannabis smokers (e.g., TNFSF-13, GP130, and IL-6a) and 6 were increased in tobacco smokers (e.g., IFN-g, IL-2, and IL-35). Pro-inflammatory markers also increase in e-cig users, but the increase didn’t reach significance. Compared to non-users there was no significant decrease in inflammatory markers in cannabis, tobacco, or e-cig users. In this relatively small series, the patterns of
inflammation varied significantly among the 4 groups. Data for a larger series is currently being analyzed and will be presented.
Conclusion: Our initial findings indicate distinct oral inflammatory patterns among cannabis smokers, combustible tobacco, and e-cig users. Chronic inflammation is recognized as a significant health risk factor, with a critical role in cancer development. Further research is urgent to better elucidate the implications of the varied inflammation patterns observed across different products use.
Grant support: TSET Health Research Promotion Center and NIH/NCI (R01CA242168, Queimado). Dr. Queimado holds a Presbyterian Health Foundation Endowed Chair in Otorhinolaryngology.
Martina Compagno Florida State University
Co-authors: Claudia Silver1, Kari Basso2 , Amber Berstein1, Caroline Bishop1, Aidan Carley1, Joshua Cazorla1, Jenna Claydon1, Alexis Cox1, Ashleigh Crane1, Chloe Crispy1, Emma Curley1, Tyla Dolezel1, Ezabelle Franck1, Camilla May1, Alejandro Navarez1, Frank Pacheco1, Olivia Turner1, and Debra Ann Fadool1 1Florida State University, 2University of Florida
Objective: Anxiety-like and memory behaviors were examined in adult mice following gestational exposure to cannabidiol (CBD), the non-psychoactive ingredient of cannabis.
Methods: Primiparous dams were orally administered 100 mg/kg CBD or ethanol vehicle mixed in strawberry jam. Dams and pups were assessed for health outcomes. At 3 months of age, offspring were metabolically profiled using a comprehensive laboratory animal monitoring system (CLAMS) and challenged via glucose tolerance testing. Adult offspring were behaviorally phenotyped using the buried marble, light-dark box (LDB), elevated-plus maze (EPM), and object memory recognition.
Results: CBD was detected in maternal plasma using GC-MS 10-min post consumption (34.2 + 1.7 ng/ul), peaked within 30 min (371.0 + 34.0 ng/ul), and below our detection limit by 4 hours (< 10 ng/ul). Fetal exposure to CBD significantly decreased survival of the pups; 38% of CBD-treated pups died before weaning age (23 days) whereas only 8% of jam-treated pups died prior to weaning. Cross-fostering a CBD-treated pup to a drug-free dam allowed survival rates similar to that of jam-treated pups. We did not observe changes in litter size, maternal body weight or pup birth weight (postnatal day 0, P0) between CBD- vs. jam-treated animals, however, by postnatal day 10 and 21, CBD-exposed male mice weighed significantly less, which could be rescued by cross-fostering to a drug-free dam. Perinatal exposure to CBD increased meal size and caloric intake for adult male offspring in the dark cycle (1w ANOVA, p<0.05), while early postnatal CBD exposure decreased fasting glucose, but had no effect on glucose clearance. Adult female offspring showed increased drink size if exposed to CBD during early postnatal development, independent of light cycle. In utero exposure caused mice of both sexes to bury more marbles (1w ANOVA, p≤0.05), and females, not males, lost this behavior if they were cross-fostered to control dams. In
utero exposure decreased time spent in the light compartment of an LDB apparatus when females were raised to adults. In utero exposure decreased performance of male mice in the 24hour object recognition test (p=0.0123). Adult female mice spent less time in the closed arms of the EPM if exposed to CBD in utero and this was unchanged with cross-fostering to a drug-free dam.
Conclusion: The use of CBD during pregnancy in mice affects pup survival, and later, OCD-like, anxiety-like, and longterm memory as an adult. Perinatal CBD exposure affects adult meal size, caloric intake, drink size, and fasting glucose.
Lisa Eckel Florida State University
Co-authors: Savoya Joyner, Florida State University
Objective: Elevated peripheral markers of inflammation and impaired cannabinoid signaling have been reported in patients with anorexia nervosa (AN). Because the endocannabinoid system modulates immune function, food intake, and energy expenditure, all of which are dysregulated in AN, it represents an important therapeutic target. Despite this, few studies have examined whether cannabinoids can attenuate AN symptoms. Here, we examined whether Δ⁹-tetrahydrocannabinol (THC) attenuates hypophagia, hyperactivity, weight loss, and inflammation in a preclinical animal model of activity-based anorexia (ABA).
Methods: ABA was induced in female rats by combining food restriction (2h access to food/day) with free access
to running wheels (RWs). Rats were removed from the paradigm after losing 22% of their baseline body weight or 7 days, whichever occurred first. Rats in the ABA-THC group received daily injections of vehicle (1 mL/kg, i.p.) until they had lost 10-12% of their baseline body weight (by day 3) and then received daily injections of THC (1 mg/kg, i.p.). Control rats received daily injections of vehicle. At the end of the study, rats were perfused and brain tissue was processed for Iba1 immunoreactivity to quantify microglial expression (a measure of central inflammation) in brain areas that control energy balance.
Results: ABA-induced weight loss was attenuated by THC treatment, with ABA-THC rats losing about 12% less weight than ABA-VEH rats. This reduction in weight loss in ABA-THC rats was mediated by a selective decrease in energy expenditure, with ABATHC rats displaying a 50% decrease in RW activity relative to ABA-VEH rats (day 4-7 average: 4477 ± 766 vs. 9810 ± 594 revolutions, p < 0.05). Preliminary findings suggest that THC attenuated the number of Iba-1 positive neurons in the arcuate nucleus of the hypothalamus.
Conclusion: Daily THC treatment was effective in attenuating weight loss in rats with ABA. Ongoing work will determine whether this action of THC is mediated, at least in part, by decreasing neuroinflammation in brain areas that regulate energy balance.
Bassma Eltanameli University of Florida
Co-authors: Sulafa Al Sahlawi, Brian Cicali, Rodrigo Cristofoletti University of Florida
Introduction: Patients using medical marijuana often take other medications, increasing their risk of drug-drug interactions (DDIs). In vitro, cannabidiol (CBD) and its active metabolite 7-Hydroxycannabidiol (7-OH- CBD) were found to precipitate several CYPmediated metabolic DDIs via reversible and time-dependent inhibition (TDI). We aim to leverage available in vitro and in vivo data to predict the magnitude of CBD-induced metabolic DDIs using a forward stepwise, model-based approach recommended by the FDA guidance.
Methods: The basic model was applied to predict the potential of DDIs precipitated by CBD and 7-OHCBD. R1 and R1, gut were used to address reversible inhibition in the liver and intestine, respectively, while R2 was used to address TDI. Enzymes showing potential risks for DDIs were further investigated using the static mechanistic model. DDIs were classified as weak (AUCR < 2), moderate (2 ≤ AUCR < 5), or severe (AUCR ≥ 5) as per the FDA criteria. Subsequently, a Physiological-Based Pharmacokinetic (PBPK) model for CBD and 7-OH-CBD was developed and validated using the Simcyp™ Simulator (v.22) and was used to predict available clinical DDI studies.
Results: CBD and, to a lesser extent, 7-OH-CBD had the potential to precipitate DDIs with all major CYP enzymes when evaluated using the basic model. The static mechanistic model showed that CBD and 7-OH-CBD could lead to severe DDIs with drugs metabolized by CYPs 2C19, 3A, and moderate DDIs with drugs metabolized by CYPs 2C9 and 1A2. The PBPK model successfully predicted CBD and 7-OHCBD systemic exposure in healthy
adults following intravenous and oral administration. Predicted plasma concentrations were within the 95% confidence interval of the observed values, and the PBPK model was further validated using additional datasets. All predicted pharmacokinetics parameters were within two-fold of the observed values. The PBPK model predicted clinical DDIs after fitting the in vitro ki values to recapitulate observed DDIs. CBD increased omeprazole AUCR by 211% after single administration and caffeine AUCR by 85% after multiple administration. CBD did not significantly inhibit all other tested enzymes.
Conclusion: Although CBD showed an inhibitory effect on major CYP enzymes in vitro, it was not clinically evident, except for CYP2C19. CBD administration did not significantly inhibit other CYP enzymes (AUCR < 2). The validated PBPK model for CBD will be extended to simulate the DDI potential with clobazam and stiripentol and real-world scenarios, including the impact of age, food consumption, and liver and kidney function on the magnitude of DDIs.
Alexandria Senetra Florida State University
Co-authors: Samantha L Penman1, Panayotis K Thanos1, Christopher R McCurdy2, Abhisheak Sharma2
1University of New York at Buffalo, 2University of Florida
Background: The endocannabinoid (eCB) system is comprised of endogenous cannabinoids, anandamide (AEA) and 2-arachidonoyl glycerol (2-
AG), their respective metabolic enzymes, fatty-acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL), and the cannabinoid type-1 (CB1) and type-2 (CB2) receptors (Lu et al, 2016). The eCB has been identified as an important neuromodulatory system responsible for many physiological functions, such as pain, neuroprotection, cognitive function, and motor activity (Zou et al, 2018).
Objective: To develop a sensitive bioanalytical method to obtain baseline levels of anandamide and 2-AG in the brain of C57BL/6 mice and stabilize further metabolism of 2-AG during sample processing and storage.
Methods: A bioanalytical method to quantify baseline levels of AEA and 2-AG in mouse brain homogenates, was developed using a Waters Acquity I-Class ultra performanceliquid chromatography coupled with a Xevo TQ-XS triple quadrupole mass spectrometer (UPLC-MS/MS). Whole mouse brains were harvested, flashfrozen, and stored at -80˚C until analysis. Samples were thawed on ice and homogenized at a ratio of 1:3 (mg/ μL) with 50 mM Tris Buffer + 50 nM NF1819 (pH-7.4±0.1).
Results: Charcoal-stripped plasma was used as a surrogate matrix to ensure complete removal of endogenous AEA and 2-AG. A range of 1-250 ng/mL was found to be linear for AEA and 2-AG, with a correlation value of >0.99 using a 1/x2 weighing factor. Patel et al. stated that degradation of 2-AG after collection of brain sample decreases, while AEA appeared unchanged during sample preparation. Thus, we used 50 mM Tris buffer with 50 nM NF1819 (MAGL inhibitor), to help prevent the metabolism of 2-AG while processing brain samples. Concentration ranges of AEA in whole mouse brains were found to be 30.8-45.8 ng/g in males and 35.9-53.5 ng/g in females. The
2-AG concentration ranges in male and female mouse brains were 695.3-2344.2 and 709.5-1957.7 ng/g, respectively. There were no significant sex differences observed between baseline levels of AEA or 2-AG in mice.
Conclusions: This sensitive and selective bioanalytical method was successfully applied for the quantification of AEA and 2-AG brain levels in male and female C57BL/6 mice and could be used to understand the effect of different treatments on baseline endocannabinoid levels. By utilizing the MAGL inhibitor during sample processing, we were able to prevent the degradation of 2-AG and achieve a linearity range required for the quantification of endogenous endocannabinoids in whole mouse brains.
Gabriel Spandau
University of Florida
Co-authors: Jamie Loizzo1, Nicole Stedman1, James Bunch1, Brian Pearson2
1University of Florida, 2Oregon State University
Background: The expansion of medical cannabis usage in the United States highlights the increasing importance of understanding patient perceptions and educational needs regarding these programs and products. In a recent investigation of a medical cannabis social media channel, our research team
identified a prevalent concern among Florida’s medical cannabis patients regarding potential contaminants in their products. This concern is underscored by reports of various contaminants in a range of medical cannabis products available in Florida. Drawing from this preliminary social media analysis, and incorporating insights from studies on trust in social media and medication, we have designed and piloted a survey instrument.
Objectives: RO1: Determine medical cannabis patient concern over contaminated medical cannabis products. RO2: Describe medical cannabis patient perception and experience of contaminated medical cannabis products. RO3: Determine medical cannabis patient trust and perception of current medical cannabis program regulation. RO4: Determine medical cannabis patient knowledge of potential medical cannabis contaminants.
Methods: The survey instrument was developed by the Principal Investigator (PI) and the research team, drawing on insights from prior research conducted by our team and studies on trust in social media and medications. The PI distributed the survey to 22 medical cannabis patients and a panel of five experts with different research backgrounds related to cannabis, alcohol, public health, and policy. Following the completion and review of the survey, participants provided detailed feedback, which was subsequently analyzed by the PI to refine the survey items. Adjustments were made to the wording of questions, response options, and the inclusion of specific concepts and questions based on this feedback.
Results: The pilot testing indicated that the flow of questions was generally logical, with minor adjustments needed.
The survey effectively addressed the main constructs of interest, although there was a recognized need to enhance the sections probing knowledge of potential contaminants and clarify certain response options.
Conclusion: Incorporating feedback from the pilot study and adhering to the research scope, we believe the revised survey instrument will effectively capture the targeted constructs. This tool is expected to provide valuable insights for medical cannabis researchers and inform considerations for the Florida medical cannabis program’s regulatory practices.
Kimia Zandbiglari University of Florida
Co-authors: Shobhan Kumar, Sebastian Jugl, Masoud Rouhizadeh
University of Florida
Background: Cannabis use for medical and recreational purposes has significantly increased recently. Yet, structured electronic health records (EHR) often lack detailed information on usage patterns, including mode, frequency, and co-use with other substances, necessitating analysis of unstructured clinical notes. Understanding these use details can improve healthcare delivery and public policy amid growing cannabis access and acceptance.
Objective: This study seeks to uncover detailed cannabis use patterns through natural language processing (NLP) analysis of free-text EHR notes,
focusing on mode of administration, usage frequency, and co-use with other substances.
Methods: We analyzed 1162 sentences from the clinical notes of 500 unique patients, with a positive cannabis use status, seen at the University of Florida Health system within a 60-day timeframe per patient from their first visit in the health system. The notes were searched using the Cannabis Use Lexicon (CULx) that our group previously developed to identify textual mentions of cannabis use. We manually reviewed the extracted sentences to categorize cannabis use mentions across several axes, including: mode of cannabis administration (‘By Mouth’, ‘Smoking/ Vaping’, ‘Topical’, ‘Unknown’); frequency of use (‘Unknown’, ‘Daily’, ‘Weekly’, ‘Occasionally’); and co-use with other substances (‘Alcohol’, ‘Illicit Drugs’, ‘Opioids/Opiates’, ‘Other Medications’ including selected other prescribed or OTC medications, ‘Tobacco/Nicotine’, ‘Unknown’). To accurately classify these categories from the sentences, we trained and applied several NLP models, including BERT, RoBERTa, Clinical BERT, Decision Trees, and Logistic Regression. Performance was assessed via accuracy, sensitivity, and positive predictive value (PPV).
Results: Of the 500 patients, 39.4% had documented cannabis use modes, 44.2% frequency, and 34% co-use with substances. Smoking/vaping and daily use were most common, with notable tobacco/nicotine and alcohol co-use. The NLP classifiers, achieving up to 93% accuracy, 94% PPV, and 93% sensitivity, closely matched human annotation in detecting cannabis use patterns. RoBERTa excelled in use methods and co-use identification, with over 93% PPV and sensitivity, especially for co-use (95% PPV, 94% sensitivity). ClinicalBERT was most accurate in frequency identification, with 89% PPV and 90%
sensitivity.
Conclusions: Our manual annotation revealed frequent mentions of detailed cannabis use patterns reported in unstructured EHR notes. We successfully developed a preliminary NLP system to automatically replicate expert manual categorization of these details. Our work provides a strong foundation for recognizing and categorizing these patterns within EHRs to ultimately facilitate research into cannabis use trends within unstructured EHR notes.
Qingchen Zhang
University of Florida
Co-authors: Philip W Melchert, Barry Setlow, Christopher R McCurdy, John S Markowitz
University of Florida
Background: In the state of Florida, smoked cannabis flower is the primary form of medical cannabis (MC) dispensed for various qualifying conditions. MC is recommended for conditions including cancer, epilepsy, glaucoma, HIV/AIDS, post-traumatic stress disorder (PTSD), amyotrophic lateral sclerosis (ALS), and others. Given its common usage, concerns exist regarding potential drug-drug interactions (DDIs) when conventional medications including pulmonary therapeutics are used concurrently with MC.
Objective: This study aimed to collect and characterize cannabis smoke condensate (CSC) from combusted
cannabis and assess the influence of the in vitro inhibitory effects on the drug-metabolizing enzymes (DMEs) carboxylesterase 1 (CES1) and six cytochrome P450 enzymes (CYP) 2C8, 2C9, 2C19, 2D6, 2B6, and 2E1 expressed in human lung S9 (HluS9).
Methods: Standardized cannabis cigarettes sourced from the NIH National Institute of Drug Abuse Supply Program (NIDA) were combusted in an enclosed smoke exposure system. The generated smoke was routed through an ultra-cold condenser, allowing for the collection of CSC. The CSC was analyzed for the presence of eight major CBs and metabolites via LC-MS/ MS. In vitro enzyme inhibition studies were conducted using human lung S9 to evaluate the potential inhibitory effect of CSC on CES1, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2B6, and CYP2E1.
Results: A total of 5.0 ± 1.5 mg per cigarette of CSC was collected, which contained 0.02 ± 0.01% cannabidiol (CBD), 0.94 ± 0.44% cannabinol (CBN), 6.46 ± 3.76% Δ9-tetrahydrocannabinol (THC), and 0.14 ± 0.07% cannabigerol (CBG) of the total condensate. In vitro enzyme kinetics studies revealed that to CES1 in HluS9, the inhibition mechanism of CSC was reversible mixed-type complete inhibition, with an inhibition constant (Ki) of 0.12 ± 0.08 μM using THC as the index compound. CYP1A2 and CYP3A showed activities in Hlus9. The half-maximal inhibitory concentration (IC50) of CSC for CYP3A inhibition was determined to be 17.85 μM with THC as the index compound.
Conclusions: CSC exhibited strong inhibition of CES1 and mild inhibitory effects on CYP3A activity. Further investigations are warranted to elucidate the inhibition mechanisms and assess the inhibitory effects on other active CYPs in HluS9.
Anurag Aka
University of Miami
Co-authors: Amrit Baral1, Yash Agrawal1, Ranya Marrakchi El Fellah1, Bria-Necole A Diggs1, Sarah Messiah2, Joseph De Santis1, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1 1University of Miami, 2University of Texas, 3Florida International University
Background: Many individuals, especially young adults aged 18-35 years, seek to utilize substances including cannabis as a means of self-treatment and coping. Understanding the complex interplay between mental health disorders and adverse childhood outcomes (ACEs) is critical for effective intervention and support strategies. Therefore, our study aims are to explore the association between cannabis use and mental health outcomes among those who have experienced ACEs.
Methods: Data comes from an ongoing Herbal Heart Study cohort investigating
the effects of cannabinoids and various routes of cannabis consumption on subclinical cardiovascular risk among 18-35 years old young adults in South Florida. Anxiety and depression were assessed by the Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) respectively. ACEs were assessed via the 11-item ACEs questionnaire. Correlation analysis was performed using Pearson’s correlation coefficient in R (v4.2.2) to estimate the correlation of anxiety and depression with total ACEs overall and among cannabis consumers (CB+), and non-consumers (CB-).
Results: Of the total study participants (N=150) [mean age: 24.6y (SD=4.5)], 66.7% were female, 51.3% identified as Hispanic, and 50.7% were CB+. In the overall sample, there was a moderately positive correlation between anxiety (r=0.30, p<0.001) and depression (r=0.31, p<0.001) with ACEs. For CB+, a weak positive correlation (r=0.23, p=0.04) was observed between anxiety and ACE scores, suggesting a proportional increase in anxiety with higher ACEs scores. Similarly, CB- exhibited a moderate positive correlation (r=0.31, p<0.01) between total anxiety and ACE scores, indicating a stronger relationship compared to CB+. A notably stronger positive correlation (r=0.42, p<0.001 was identified between total depression and ACE scores among CB+, suggesting a more pronounced impact on depression in this group.
Conclusion: Results showed a proportional increase in anxiety with higher adverse childhood experiences among CB+ and CB-. However, CB+ had a strong positive correlation between depression and ACEs, while CB- had no statistically significant correlation. Further research could explore the underlying reasons for the differences in the correlation between anxiety/ depression and ACEs among CB+

and CB-. Additionally, interventions tailored to address mental health needs of individuals with ACEs could be developed.
Shannon Antoine-Hardy Florida A&M University
Co-authors: Joseph Telfair, Kelly Sullivan, Mase William
Georgia
Southern University
It is estimated that 3.4 million people in the United States have epilepsy. Epilepsy is the fourth most common neurological disorder which can lead to poor quality of life, developmental delays, injury, or premature death. There are roughly 28 FDA approved antiepileptic drugs (AEDs) to treat seizures and despite the availability of these AEDs, 30 to 40% of the patients remain resistant to drug treatment. Evidence from anecdotal reports and small clinical trials have reported numerous therapeutic benefits of medical cannabis (MC). Because more individuals with epilepsy are seeking alternative medical treatment, it is essential to understand the social and contextual factors that influence their decision-making. Individuals’ beliefs about AEDs may influence their intention towards the acquisition or dissent of MC. Therefore, the purpose of this study was to investigate predictors that affect individuals’ intention to adopt cannabis for therapeutic purpose (CTP), explore
perceived barriers to CTP, as well as assess individuals’ beliefs about their personal need for anti-epileptic drugs.
Methods: This study employed a concurrent nested-triangulation study design. Semi-structured interviews and Beliefs about Medicine- Epilepsy Specific (BMQ-E) questionnaire was used to gather data on salient beliefs about CTP and AED medication. The participants were recruited through the Epilepsy Foundation of Georgia and included both men and women, aged 18 years and older with a clinical diagnosis of epilepsy. Thematic analysis was utilized to identify themes and MAXQDA was used to code transcriptions. Data were analyzed using descriptive statistics for the BMQ-E questionnaire.
Results: The most frequently mentioned positive outcomes of using CTP included seizure reduction, fewer side effects, and improved mental/emotional state. Negative stigma, dependency, and fear of job loss were the most frequently mentioned negative outcomes.
Discussion: The results of this study were limited to the participants who were enrolled; therefore, the beliefs about CTP and AEDs were less likely to be representative to the general population of adults with epilepsy. This elicitation study was intended to provide groundwork for future studies that examine the political, contextual, and public health implications for CTP use among those with severe chronic conditions.
Amrit Baral
University of Miami
Co-authors: Yash Agrawal1, Anurag Aka1, Sarah Messiah2, Joseph De Santis1, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: In contemporary health research, the exploration of mindfulness practices and cannabis science is expanding. With growing interest in mindfulness and increasing prevalence of cannabis use in this demographic, this study aims to investigate associations between mindfulness and quality of life among young adult cannabis users, providing valuable insights into their holistic experiences.
Methods: Data is a subsample of cannabis users (n=76) from the baseline visit of the ongoing Herbal Heart Study cohort (N=150), studying the impact of cannabinoids and cannabis consumption routes on subclinical cardiovascular risk among young adults (18-35 years), residing in South Florida. The validated Five Facet Mindfulness Questionnaire (FFMQ-15) was administered to measure mindfulness with regards to thoughts, experiences, actions, and daily life. The overall scores of all five subscales were calculated based on standardized instruction. Quality of life (QOL) was assessed using the 26-item World Health Organization Quality of Life questionnaire (WHOQOLBREF), comprising four domains: physical health, psychological wellbeing, social relations, and environment. Total scores within each domain were transformed to a 0–100 scale, aligning with WHOQOL-100 standards for comparison. Two items gauged participants’ overall perceptions of QOL and their health. Total QOL scores and
scores across domains were compared between those practicing and not practicing mindfulness using Mann–Whitney U tests.
Results: Of the 76 cannabis users, 57.9% were female, mean age 25.0 years (SD=4.3), and 63.2% reported practicing mindfulness. Significant differences in the total median QOL scores were observed between individuals who reported practicing mindfulness and those who did not (95.0 vs 87.5, U=879.0, Z=-2.1385, p=0.036). Specifically, respondents engaged in mindfulness practices had higher median scores in the psychological well-being (66.7 vs 54.2, U=842.0, Z=-2.5470, p=0.013) and social relations (75.0 vs 66.7, U=890.0, Z=2.0370, p=0.041) domains. Conversely, no significant differences were found between mindfulness practitioners and non-practitioners in the physical health (Z=-1.7255, p=0.089) and environment (Z=-1.3556, p=0.179) domains. Notably, those incorporating mindfulness practices exhibited a lower median score for their overall perception of QOL and general health (5 vs 4, U=1281.5, Z=2.2268, p=0.026).
Conclusion: Findings highlight the complex interplay between mindfulness practices, cannabis use, and quality of life domains within cannabis consumers. Further research and nuanced interpretation of these relationships and their impact on young adult health.
Elayna Bassuk University of Miami
Co-authors:
Amrit Baral, Denise C Vidot University of Miami
Background: Cannabidiol (CBD) is one of the primary cannabinoids in the cannabis plant that has been reported to have benefits such as pain management, anti-inflammation, and an anxiolytic agent. Evidence suggests increased prevalence of CBD use as a palliative and/or adjunct therapy among cancer patients globally. Yet, there is a lack of literature on the prevalence and perceived benefits of CBD among cancer patients at various stages of cancer treatment.
Methods: Data utilized in this analysis is from the National Cancer Institutefunded study titled “A Multidisciplinary Approach to Assess Frequency, Patterns, and Reasons for Cannabis Use among Sociodemographic Diverse Cancer Patients’’. Cannabis use, cancer status, and perceived benefits were self-reported via a survey administered in REDCap to patients within Sylvester Comprehensive Cancer Center. Survey was administered in English and Spanish. Descriptive statistics were calculated to estimate the proportions of CBD use and its perceived benefits, using SAS Analytics.
Results: Of the total cancer patients (N=495) [mean age:45.9 years (SD=15.1)], 51.8% were male, 39.4% were Hispanic/LatinX, and 63.1% consumed cannabis in the past 30 days [current cannabis users (CCUs)]. Cancer treatment status among CCUs were 15.5% newly diagnosed, 43.8% under treatment, 35.4% completed therapy/following up, and 5.3% were not receiving treatment at time of survey. Among CCUs, 13.7% reported CBD as their dominant cannabinoid. Within this group, the majority were
undergoing treatment (45.2%), followed by those who finished treatment/ follow-up (41.9%), those not receiving treatment (9.7%), and newly diagnosed patients (3.2%). Perceived benefits of cannabis use among CBD users were pain management (72.4%), relief from stress, anxiety, or depression (17.3%), managing nausea and vomiting (3.5%), improved sleep (3.4%), and relief from neuropathy (3.4%).
Conclusions: Majority of CBD-dominant CCUs reported pain management as a perceived benefit which highlights the analgesic property of CBD in cancer care. Results also indicate CBD was reported to alleviate mental health symptoms as well as other symptoms potentially arising as side-effects of cancer treatment. These insights underscore the multifaceted role of CBD in cancer patients’ lives and warrant further exploration into personalized healthcare approaches in oncology settings to improve cancer patients’ experiences, treatment, prognosis, and quality of life.
Naueen Chaudhry University of Florida
Co-authors: Karen Yung, Chelsea Salmon, S Devi Rampertab, Angela Pham, Ellen M Zimmermann, Ludmila Barbosa De Faria University of Florida
Introduction: Inflammatory bowel disease (IBD) patients often use marijuana for disease-related symptoms. Since legalization in some states, the college-aged population has
shown the greatest increase in its use. Our study explores attitudes towards marijuana among college students with IBD.
Methods: Anonymous survey comprising 39 questions on demographics, disease features, patterns of marijuana use, disease symptoms, quality of life, and true/false statements about marijuana was administered via REDCap to 108 participants recruited from University of Florida (UF) IBD clinic. Responses of college students were compared to the older cohort. Two 60-minute focus groups were conducted via Zoom with 8 participating college students. An interview guide of was shared with participants in advance. Interviews were transcribed for analysis. Compiled data was analyzed by the groundedtheory approach to identify any unique themes that arose from the collected data. Focus group transcripts were independently open-coded by 2 authors prior to categorizing the codes and identifying common emergent themes.
Results: Of 108 survey participants,18 were college students. Medical vs recreational marijuana was more predominant among both college students (8 [44.4%]) and the older>25 yrs cohort (57, [65.5%]). College students reported a greater ratio of medical vs recreational marijuana when using combination patterns of medical/recreational therapies (p=0.0184), and greater hesitancy when considering to start using marijuana (p=0.0451) compared to older>25 yrs. Eleven themes emerged from focus group discussions (Table 3: themes, descriptions and representative quotes). Participants reported ability to avoid opioids and additional pharmaceuticals for symptom management with marijuana use, especially nausea, abdominal pain and poor appetite. It was helpful in navigating mental health challenges such as anxiety and
college stress, without impacting their social interactions. Overall, students demonstrated cautious use patterns and good understanding of different formulary effects. They acknowledged challenges such as binge eating, and managing timing of academic and extra-curricular activities to prevent suboptimal performance associated with their marijuana use. Since recreational marijuana illegal in Florida, they voiced concerns about legal repercussions.
Conclusion: Our findings provide valuable insight into the attitudes of college students with IBD towards marijuana use for symptom management and reveal an understanding of its impact on college students’ mental and physical health, social life, relationships, and academic needs. The healthcare and academic aspects of marijuana use in this population warrant further investigation. Our findings are limited due to sample size and possible positive response bias since participants were current marijuana users.
Abigail Cherenfant University of Miami
Co-authors: Amrit Baral1, Renessa S Williams1, Ranya Marrakchi El Fellah1, Sarah Messiah2, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: Within the exponentially increasing interest in cannabis research,
there exists a recognized diversity gap within the field, concerning the underrepresentation of Black, indigenous, and people of color (BIPOC) communities in the literature. This study attempts to narrow this gap by examining cannabis use routes among young adult Black populations in South Florida. Such exploration is vital for a more comprehensive understanding of cannabis-related behaviors and underscores the importance of considering race-ethnicity in understanding cannabis consumption patterns.
Methods: The data analyzed in this study comprises a subset of cannabis users from the ongoing Herbal Heart Study cohort, examining the impact of cannabinoids and methods of cannabis consumption on subclinical cardiovascular risk among individuals aged 18-35 in South Florida. Participants’ race-ethnicity was categorized as non-Hispanic Whites (NHW), non-Hispanic African Americans/Blacks (AA), Hispanic/ Latino, and others. Cannabis use was self-reported and confirmed through a rapid urine drug screening test. Descriptive statistics and Fisher’s exact tests were employed using SAS Analytics.
Results: Among total cannabis users (N=76), 57.9% were female, with a mean age of 25.0 years (SD=4.3). Hispanic/ Latino constituted 51.3% of the sample, followed by AA (19.7%), and NHW (18.4%). The majority of participants used vapes (35.5%), followed by joint (34.2%), and blunt use (30.3%). A significant difference in cannabis consumption methods by race-ethnicity was observed (p=0.02). AA (40.0%) were more likely to report blunt use compared to Hispanic/Latino (25.6%) and NHW (14.3%). Similarly, AA (53.3%) were more likely to be joint users compared to Hispanic/Latino (31.0%) and NHW
(28.6%). In contrast, only 6.6% of AA, compared to 57.1% of NHW and 43.6% of Hispanic/Latino, reported using vapes.
Conclusion: This study highlights the significant race/ethnic disparities in cannabis consumption methods among young adult populations in South Florida, emphasizing the prevalence of blunt and joint usage over vapes. Blunt use has been associated with an increased likelihood of cannabis dependence, nicotine dependence, as well as myriad other risk factors (e.g., perceptions of decreased risk) compared to other methods of cannabis administration. As a result, this may contribute to cardiovascular disease risk. Moving forward, targeted interventions and public health campaigns should consider these patterns in consumption routes to analyze cannabis-relative behaviors effectively among BIPOC communities.
Justine Clement University of Miami
Co-authors: Bria-Necole Diggs1, Amrit Baral1, Cynthia Lebron1, Sarah E Messiah2, Denise C Vidot1 1University of Miami, 2University of Texas
Background: Cannabis use among pregnant and breastfeeding individuals has become a topic of increasing concern, particularly with the recent increases in acceptance and legalization. Understanding factors influencing cannabis use during
breastfeeding is crucial for developing appropriate public health interventions and clinical guidelines. Thus, this study aimed to explore the reasons for cannabis use during breastfeeding across different race/ethnic groups, shedding light on potential disparities to inform culturally competent guidance.
Methods: Cross-sectional data from the COVID-19 Cannabis Mom Study (N=221) was analyzed. Informed consent and data collection were conducted anonymously via a REDCap electronic survey link. Participants self-reported their cannabis usage and reasons for use during pregnancy and breastfeeding. Ethnicity was categorized as Hispanic/Latino, Non-Hispanic White (NHW), and Non-Hispanic Other (NHO) -inclusive of African Americans/ non-Hispanic Blacks, Asians, and Native American/Alaskan Natives, Pacific Islander due to smaller sample sizes. Chi-Square/Fisher’s Exact tests examined reasons for cannabis use by race/ethnic group.
Results: The overall sample (N=221) was 64.1% NHW, 16.6% Hispanic/Latino, and 65.4% currently pregnant (22.7% in the first trimester, 44.0% second trimester, and 33.3% third trimester). The majority (94.7%) reported consuming cannabis before being pregnant and 89.3% reported currently consuming cannabis while pregnant. There were no statistically significant differences by race/ethnicity in the proportions of those consuming cannabis during pregnancy to relieve nausea, stress, anxiety, pain, or for fun or to relax. There was a difference in reason for use by ethnicity in self-reported relief of vomiting (NHW: 59.2%, NHO: 46.6%, Hispanic/Latino: 28.6%; p=0.05) and to relieve symptoms of a chronic condition (NHW: 4.1%, NHO:13.3%, Hispanic/ Latino: 28.5%; p=0.03).
Conclusions: Findings show that most
pre-pregnancy cannabis users continue use during pregnancy, and reasons for use varies by race/ethnicity. More Hispanics/Latinos consume cannabis during pregnancy to relieve symptoms of a chronic condition versus NHW and NHO while NHO had a higher prevalence of cannabis use to relieve vomiting compared to Hispanics/Latinos. These findings underscore differential reasons for cannabis use during pregnancy by ethnicity as a premise for culturally inclusive public health education and harm-reduction interventions and pregnancy health provider education.
Juan Cuesta University of Miami
Co-authors: Bria-Necole A. Diggs1, Amrit Baral1, Domenick Maglione1, Ranya Marrakchi El Fellah1, Michelle Weiner2 , Shari Kaplan3, Denise C Vidot1 1University of Miami, 2Nova Southeastern University, 3Cannected Wellness
Background: Terpenes, naturally occurring volatile compounds in plants, contribute to the aroma, flavor, and colors of cannabis. Research suggests that terpenes may enhance therapeutic potency of cannabis as part of the entourage effect. Cannabis industries often use terpenes for strain differentiation, yet their role in flavor and medicinal effects remains elusive to many consumers. This study aims to estimate the prevalence of cannabis consumers by age considering terpene content when purchasing cannabis for medical purposes.
Methods: Data are from the Cannabis Users and Terpenes Study, an anonymous electronically administered
survey via REDCap designed to collect self-reported data on cannabis consumption patterns, reasons for use, and consideration of terpene content in their cannabis. Descriptive statistics and chi-square tests were conducted using SAS Analytics with a two-tailed alpha set to 0.05. A post-hoc analysis compared terpene consideration and age group category determined by the distribution of sample.
Results: Of total respondents (N= 2,599), mean age was 31.1 years (SD=14.3). More than half consumed cannabis for medicinal purposes (63.2%, N=1288), of which 55.8% purchased with a medical card while 44.2% selfmedicated without a medical card. Almost half of participants (41.8%) did not consider the terpenes content when purchasing cannabis products, compared to 36.0% that did and 22.2% considered sometimes only. A significant association was found between age and considering terpenes when purchasing cannabis (p=0.01). There was a difference by age group in consideration of terpenes during cannabis purchase (44.2% of 18-to35-year-olds, 42.3% of 36-to-52-yearolds, 37.5% of 53-to-69-year-olds, and 46.7% of respondents over 70 years of age). Among respondents considering terpene content when purchasing cannabis, 78.9% use terpenes for flavor, 67.8% for medical benefits, 70.4% to enhance their high, and 61.5% for a more natural high.
Conclusions: Participants over 35 years of age tend to factor terpenes into their cannabis purchases more often. Notably, a larger proportion of cannabis consumers used terpenes for their flavor and to enhance their high. Future research and age-appropriate education is required to address the needs of cannabis consumers regarding terpenes and their health advantages.
Robert Dvorak
University of Central Florida
Co-authors: Daniel Paulson, Michael Dunn, Madison Maynard University of Central Florida
Background: Older adults are at an elevated risk of medical complications due to polypharmacy. Increasingly, older adults are turning to Medical Cannabis (MC) to address medical issues. However, there is little evidence of MC efficacy on event-level symptoms in older adults. Further, it is unclear if therapeutic effects increase problematic use patterns.
Objective: (1) To examine the momentary associations between MC and clusters of physical and psychiatric symptoms at the daily level. (2) To examine if the effects of MC on symptom clusters are associated with problematic and/or pathological use patterns.
Methods: A sample of older adults (n = 106) were recruited through social media. Participants had medical conditions approved for treatment using MC. Once enrolled, participants received text messages to complete six daily assessments of symptoms for 15 days.
Results: Participants provided 5,156 momentary assessments across 1,106 cannabis use days. Trajectories of symptoms were examined across the day leading up to, and following, use
initiation. On use days, there was a decline in all symptoms following use. This was most robust for subjective pain and weaker for negative affect, trauma symptoms, and nausea. Negative affect, pain, and nausea evinced momentary negative reinforcement associations with subjective cannabis intoxication. Negative reinforcement parameters were subsequently associated with adverse cannabis use outcomes. The decline in post-use trauma symptoms and the momentary negative reinforcement effect for negative affect were both associated with cannabis use disorder symptoms. The momentary negative reinforcement effect for pain and nausea were associated with higher cannabis use problems, but not use disorder symptoms.
Conclusions: These data suggest that MC may be effective in reducing common symptom clusters. However, the negative reinforcing effect may complicate the therapeutic nature, increasing cannabis use disorder symptoms among those with higher reinforcement for psychiatric symptoms and increasing cannabis use problems (though not use disorder symptoms) among those with higher reinforcement for physical symptoms. Identifying behavioral interventions to maximize benefits while minimizing costs may increase the efficacy and safety of MC as an effective therapy in older adults.
Hu University of Miami
Co-authors: Juan Pablo de Rivero Vaccari1, Yan Wang2, Cristiane Takita1 , Isildinha M Reis1, Alexandra McMahon1 1University of Miami, 2University of Florida
Background: Breast cancer is the most frequently diagnosed cancer and the second leading cause of cancer death in American women. Some breast cancer patients use Medical Marijuana (MMJ) to manage treatment-related symptoms. Although MMJ is generally considered safe and well-tolerated in cancer patients, there are potential adverse effects and conflicting reports on its interactions with cancer therapies and their impact on clinical outcomes. Therefore, we propose a prospective cohort study of a diverse breast cancer population (50% minorities) to assess the impact of MMJ on clinical outcomes and QOL.
Objective: The objectives are to (i) Assess the impact of MMJ on clinical outcomes and QOL in breast cancer patients after adjusting for age, race/ethnicity, tumor stage, and subtypes; (ii) Evaluate the relationship between inflammasome/inflammatory biomarkers and the biological effects of MMJ on clinical outcomes of breast cancer; (iii) Investigate potential interactions between MMJ properties (i.e., THC/CBD ratio, dose, and type) and cancer treatments on clinical outcomes.
Methods: We proposed to enroll 60 breast cancer patients who plan to initiate MMJ and collect data on patient and tumor characteristics, treatments, clinical outcomes, and adverse reactions to obtain a comprehensive understanding of the usage and effects of MMJ. We will collect subjective and objective data through combined in-person visits and technology-
based assessments. In two proof-ofconcept pilot studies, we evaluated inflammasome biomarkers in predicting radiotherapy (RT)-related clinical outcomes and the effects of MMJ on chronic pain.
Results: In the first pilot study of 63 breast cancer patients, we showed that RT-induced skin toxicity is significantly higher in patients with higher mean levels of inflammasome markers including caspase-1 (p=0.023), IL-18 (p=0.04), and hsCRP (p=0.028). Patients with post-RT pain 4+ have higher mean levels of ASC (p=0.017), IL-6 (p=0.022), and hsCRP (p=0.002). In addition, patients who died presented higher mean levels of caspase 1 (p=0.043), IL-6 (p=0.03), and hsCRP (p=0.005). A higher percentage of patients with a 4+ pain score had worse but not significant 5-year Progression Free Survival (52.2% vs. 38.5%) and Overall Survival (39.1 vs. 20.5). We will also present preliminary data from the second ongoing pilot study evaluating whether inflammasome activation mediates the effects of MMJ on chronic pain.
Conclusions: Inflammasome activation and inflammation contribute to RTrelated skin toxicity, pain, and worse overall survival. Therefore, inhibiting inflammasome activation with MMJ has the potential to improve breast cancer QOL and clinical outcomes.
Exploring the relationship between previous cannabis experience and pain among a population of current medical cannabis users in Florida
Simone Jackson University of Florida
Co-authors: Sophie Maloney, Juan Perez, Abigail Gracy, Anne Gracy, Elena Kalina, Emmely Pavila University of Florida
Background: Florida has one of the largest medical cannabis (MC) programs in the United States, with over 870,000 current qualified users in 2023. Pain is not specifically listed as an approved qualifying medical condition for receiving a MC card in Florida, however, 30% of certified users nationally report pain as a reason for medical cannabis use. Despite an increase in medical cannabis use for pain-related outcomes, little is known about the degree of pain relief among those having used cannabis for long periods. To address this research gap, we explored the relationship between previous cannabis experience and selfreported pain among current MC users.
Objective: Describe sociodemographic characteristics and self-reported pain among MC users with varying cannabis use experience. Identify potential associations between previous cannabis experience and both self-reported pain and sociodemographic characteristics.
Methods: A secondary data analysis was conducted using data collected from the cross-sectional arm of the Medical Marijuana & Me (M3) study. Using a bivariate analysis, we compared sociodemographic characteristics and self-reported pain intensity (Brief Pain Index; BPI) between categories of cannabis experience (5 years of use). We performed a multinomial logistic regression to address potential confounders.
Results: In total, 629 MC users (median age 45 (IQR 35-58), 86% White, 63% female, 83% attended college, 58% employed) completed the survey. Most
respondents had more than 5 years of previous cannabis experience (54%), followed by 1-5 years (34%), and less than 1 year (12%). Age, sex at birth, education, and employment status were not statistically different across the groups. MC users who identified as White were more likely to report 5 years (86%) of experience (p=0.046). Respondents across all categories of previous cannabis experience reported similar worst pain intensity BPI scores within the past 24 hours (mean 7.7, SD=1.7). A multinominal logistic regression model showed no associations of sociodemographic characteristics and self-reported pain with previous cannabis use experience.
Conclusions: We found that most respondents had more than 5 years of previous cannabis experience, but there was no statistically significant relationship between experience and self-reported pain. Future research should longitudinally assess pain to explore how specific use patterns impact pain among medical cannabis users.
Isabella Jimenez University of Miami
Co-authors: Bria-Necole Diggs1, Amrit Baral1, Marlene Camacho-Rivera2 , Jessica Islam3, Sarah E. Messiah4 , Denise C Vidot1
1University of Miami, 2Moffit Cancer Center, 3SUNY Downstate Health Sciences University, 4University of Texas
Background: Cannabis has been documented to display analgesic properties and literature suggests its efficacy as a natural alternative to pharmaceutical painkillers in alleviating chronic pain arising from health conditions. Additionally, prior studies reported a surge in cannabis use during the early stages of COVID-19 to manage symptoms of anxiety. While the use of cannabis to manage chronic pain and mental health symptoms during the early stage of COVID-19 have been documented by previous research, there remains a gap in knowledge regarding the cannabis use patterns among patients living with chronic pain during later stages of the COVID-19 pandemic.
Methods: The data utilized in this analysis are from the COVID-19 Cannabis Health Study, a global crosssectional study that collected selfreported data on cannabis use, chronic health conditions, and COVID-19 using REDCap survey. This study includes data collected from March 2020 to March 2023. Descriptive statistics were employed using SAS Analytics with a two-tailed alpha set to 0.05.
Results: Of the total respondents (N=2,816) 94.5% consumed cannabis within the past year and 28.4% reported living with chronic pain. Among those with chronic pain, 50.1% were male and 84.7% were Non-Hispanic White. Of those living with chronic pain, 99.0% consumed cannabis within the past year and 60.9% consumed for both recreational/adult and medicinal purposes (compared to 5.7% medicinal only and 30.8% recreational/adult only). Before COVID-19 was declared a pandemic, participants reported a higher prevalence of pipe/bowl cannabis consumption compared to any other route (i.e. blunt, joint, edible, etc.); however, after COVID-19 was declared a pandemic the most common route consumed switched to edible use.
Since COVID-19 has been declared a pandemic, 51.4% of chronic pain patients had no change in their cannabis dosage, while 39.8% increased their dose.
Conclusion: The study concluded that there was a change from pipe/bowl usage as the most common route prior to COVID-19 to edible usage post-COVID-19 in the study sample. Almost 40% of people with chronic pain increased their overall cannabis dosage during the COVID-19 pandemic. The data presented notable findings to address the gap in literature regarding use of cannabis by chronic pain patients during COVID-19. Given that the COVID-19 pandemic affected public health on a large scale, future research examining how cannabis use among patients with other chronic conditions was affected by COVID-19 is crucial.
Ethan Kumar University of Miami
Co-authors: Amrit Baral1, Ranya Marrakchi El Fellah1, Bria-Necole A Diggs1, Sarah Messiah2, Raul Gonzalez3 , Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: With a global rise in cannabis use and evolving societal norms surrounding its legalization, there is a growing need to understand how cannabis consumption is associated
with lifestyle choices. Dietary preferences, fasting, and exercise practices play a crucial role in shaping the overall health of an individual. While existing literature has reported the impact of cannabis on various health aspects, the prevalence and nature of these behaviors among cannabis users compared to non-users remain poorly understood. This study aims to provide valuable insights in 18-35-year-olds, a population with a relatively higher prevalence of cannabis use.
Methods: This analysis drew data from the initial assessment of the ongoing Herbal Heart Study cohort, investigating the impact of cannabinoids and cannabis delivery methods on subclinical cardiovascular risk in a population of healthy young adults (18-35 years) in South Florida. Participants self-reported their dietary preferences and weight control behaviors. Descriptive statistics and Chisquared tests/Fisher’s exact test where applicable, were employed for analysis using SAS analytics.
Results: In a sample of 150 participants (mean age: 24.6 years, SD: 4.5), 66.7% were female, 51.3% Hispanic/Latino, and 50.7% reported cannabis use. The majority (78.0%) were omnivores/did not have any dietary restrictions. Only 6.7% were vegetarians, 4.7% pescatarian, 2.7% vegan, and 8.0% other. 53.0% of omnivores were cannabis users. Conversely, among pescatarians, 57.1% were non-users. Among vegetarians, 60.0% were non-users. Dietary preferences showed no significant differences between cannabis users and non-users (p=0.892). Notably, 26.7% of cannabis users, compared to 5.4% of non-users (p<.001), reported fasting/ refraining from eating for weight or shape control in the past three months. Additionally, 20.0% of cannabis users, in contrast to 5.4% of non-users (p < .01), engaged in “driven” or “compulsive”;
exercise for weight/shape control or burn fat or calories in the same period.
Conclusion: This study highlights a complex interplay between cannabis use and lifestyle factors among young adults, showing no significant dietary differences but a pronounced disparity in weight control practices between users and non-users. Cannabis users more frequently resort to fasting and compulsive exercise, pointing towards a behavioral pattern that may heighten cardiovascular risk. These preliminary findings underscore the importance of further research into how cannabis use influences lifestyle choices and cardiovascular health, aiming to inform strategies for this growing demographic.
Liva
LaMontagne University of Florida
Co-authors: Hanzhi Gao, Linda B Cottler, Roger B Fillingim, John B Williamson, Vijaya Seegulam, Yan Wang, Catalina Lopez-Quintero University of Florida
Background: Sleep is vital for overall health, yet over a quarter of Americans report insufficient sleep. With increasing cannabis legalization, people may turn to it to improve sleep, especially when coping with pain. Among patients who use medical cannabis, more than half may also use non-medical cannabis recreationally. However, findings on how cannabis affects sleep are mixed. The All of Us program allows objective sleep assessment via Fitbit wearables, supplemented by self-reports of
cannabis use and pain.
Objective: We examined how participants’ past-3-month cannabis use related to concurrent Fitbit sleep measurements and pain, controlling for sociodemographic factors.
Methods: The study included 3794 participants with Fitbit sleep data with a median age of 49.60 [IQR: 34.58, 63.04], 70.6% female, 87% White, and 59.3% had income > $75.000. Of these, 759 (20%) reported past-3-month cannabis use. We selected past-7-day pain intensity and sleep data recorded within the 3-month period before the date of reporting past-3-month cannabis use (yes/ no). Using robust SEM regression analyses in R, we separately regressed average minutes of nightly total sleep and sleep latency (total time in bed – total time asleep) on cannabis use, pain, and sociodemographic factors (age, gender, race, income, relationship status).
Results: Based on Chi-square tests, participants who used cannabis in the past 3 months disproportionally had lower income, higher pain intensity, were younger, and Black/ African American compared to non-users. Based on multivariate regression analysis, participants who used cannabis in the past 3 months compared to non-users had 2.7 minutes longer sleep latency during that time, all other variables held constant. Overall pain intensity among participants was low (<5 on a 10-point scale), and a unit-increase in pain was associated with a 1.46-minute decrease in average nightly total sleep and a 0.51-minute increase in sleep latency, all other variables held constant. Each year-increase in age was associated with 0.79-minute decrease in total sleep. Black/African American participants had 42.39 minutes less total sleep than White participants, independently of cannabis use (all p values < 0.05).
Conclusions: Our findings among the relatively high-SES Fitbit users in the All of Us program suggest that cannabis use may be concurrently associated with taking longer to fall asleep. Our study also aligns with previous reports of shorter sleep durations among Black/ African Americans compared to Whites. More research is needed on the interaction effects between sociodemographic factors and cannabis use on pain and sleep outcomes.
Liva LaMontagne University of Florida
Co-authors: Catalina Lopez-Quintero, Yancheng Li, Roger B Fillingim, John B Williamson, Kimberly Sibille, Zhigang Li, Robert L Cook, Yan Wang University of Florida
Background: More than 70% of chronic pain patients report sleep disturbances. Older adults are increasingly seeking medical cannabis (MC) to relieve chronic pain and improve sleep. The relationships between self-report measures of sleep quality and objective time asleep are weak, suggesting they might have different relationships with intentions to start MC.
Objective: The goals of this study are to evaluate the relationships between sleep and intentions to start medical cannabis at baseline. We examine the associations of self-reported sleep quality and Fitbit-measured sleep with intentions to start MC.
Methods: Our analysis included baseline data from 96 participants in the Study on medical Marijuana and Its Long-term Effects (SMILE), 48 planning to start MC treatment, 48 – not; 81 (84%) White, 65 (67%) female, median (IQR) age = 66 (57,70.25). At intake participants reported whether they planned to start MC (yes/ no), rated past-30-day sleep quality (1 -very bad; 4 - very good) and started wearing Fitbit Charge 4s. We averaged total time asleep over the first week. We regressed sleep measures on MC intentions, controlling for pain intensity, opioid use, and sociodemographic factors (age, gender, race, income, relationship status) with robust SEM regressions in R.
Results: Based on Mann-Whitney U-tests, there were no differences in self-reported sleep quality by MC intention groups. Participants intending to start MC had less sleep, Mdn (IQR) = 6.83 (5.41, 7.16) than participants who did not, Mdn (IQR) = 7 (6.18, 7.56) hours. Based on multivariate regression analysis, subjective sleep quality was not associated with intentions to start MC. First-week Fitbit average total sleep time was negatively associated with intentions to start MC (B = -61.46, p = 0.014) with interested participants sleeping over an hour less on average. Subjective sleep quality was also negatively associated with pain intensity (B = - 0.02, p = 0.000) and positivelywith opioid use (B = 0.67, p = 0.000) and age (B = 0.02, p = 0.009, all p-values FDR-adjusted for multiple testing).
Conclusions: As hypothesized, our initial findings indicate that getting less sleep on average may be associated with higher interest in MC treatment. Our findings also align with an established body of work showing a concurrent negative relationship between pain and self-reported sleep quality. A future research direction is to better understand the prospective effects
of MC treatment and opioid use on subjective and objective sleep measures among older adults with chronic pain.
Catalina Lopez-Quintero University of Florida
Co-authors: Krishna Vaddiparti, Elizabeth Castañeda, Liva LaMontagne, Juan Guillermo Perez-Carreño, Lina M Velilla-Jimenez
University of Florida
Background: Previous studies have explored the prevalence and factors contributing to the development of cannabis use disorders (CUD) among cannabis users. However, less is known about the medical reasons associated with meeting criteria for a CUD and its severity. This study aims to examine whether the reasons for using cannabis as a medicine varied across CUD status among a sample of young Hispanic/ Latino adults who use cannabis.
Methods: We analyzed data from 165 Hispanic/Latino young adults (Mean age = 21.4 [SD = 0.11]; 49.4% female) recruited in South Florida. Participants indicated whether they met criteria for a cannabis use disorder in the past 12-months based on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (categorized as: No CUD, Mild CUD, Moderate/Severe CUD).
Participants also reported the reasons for which they used cannabis as a medicine, including: (i) reducing pain, (ii) improving sleep, (iii) increase appetite,
(iv) reduce nausea, (v) improve mood, and (vi) reduce anxiety. Associations between CUD status and reasons of cannabis use were explored using multinomial regressions, while adjusting for socio-economic factors (e.g., age, sex, years of education). Associations are expressed as relative risk ratios (RRR) and their corresponding 95% confidence intervals (95% C.I.).
Results: In this sample of cannabis users, 47.3% did not meet criteria for a CUD, while 30.9% met criteria for a mild CUD, and 21.8% met criteria for a moderate to severe CUD. The most common reason cited for using cannabis as medicine was to reduce anxiety (70.9%), followed by improving sleep (64.2%), increase appetite (44.9%), reduce pain (38.2%), improve mood (33.5%) and reduce nausea (25.5%). Multinomial regression models showed that relative to those who did not used cannabis to improve sleep, individuals who used cannabis to improve their sleep had a higher expected risk of meeting the criteria for mild CUD compared to not meeting the criteria for CUD (IRR=3.6, 95% C.I.=1.4, 9.2).
Conclusions: Our results extend prior research by documenting a relationship between CUD status and use of cannabis as a medicine to improve sleep. Future longitudinal studies should explore the temporality of this association to clarify the role of sleep as a potential etiological mechanism in the development of CUD.
Dina Marrakchi El Fellah University of Miami
Co-authors: Bria-Necole Diggs1, Amrit Baral1, Ranya Marrakchi El Fellah1 , Jessica Islam3, Marlene CamachoRivera2, Sarah E Messiah4, Denise C Vidot1
1University of Miami, 2Moffit Cancer Center, 3SUNY Downstate Health Sciences University, 4University of Texas
Background: In tandem with the surge in the prevalence of anxiety amid COVID-19 pandemic, exploration and research of alternative and naturalistic treatments as anxiolytics has been burgeoning. Psilocybin, a fungi-based psychedelic substance, has shown potential in reducing anxiety levels; however, its co-use with cannabis is under-documented. This analysis aims to explore the prevalence of anxiety and patterns of psilocybin use among cannabis consumers at times of public health crisis, such as during the COVID-19 pandemic.
Methods: The global COVID-19 Cannabis Health Study (N=2,816) is a multi-site cross-sectional study conducted via a REDCap electronic survey. Cannabis and psilocybin use were self-reported. Anxiety was assessed using the Generalized Anxiety Disorder (GAD-7) and standardized cut-offs were applied to categorize the levels of anxiety as minimal, mild, moderate, or severe. Data included in this study are from March of 2020 to March of 2023. Descriptive statistics were employed and ChiSquare/Fisher’s exact tests were conducted using SAS Analytics with two-tailed alpha set to 0.05.
Results: Of the overall sample, 95.5% consumed cannabis in the past year and 25.0% consumed psilocybin. Among the cannabis consumers, 52.8% were males,
74.4% Non-Hispanic White, and 26.1% consumed psilocybin. The average GAD7 score among cannabis consumers was found to be 7.4 (SD=5.5) indicating mild anxiety. 40.6% of cannabis consumers who never consumed psilocybin had minimal anxiety. There was a significant difference in anxiety and changes in psilocybin use (p=0.04); 35.6% of cannabis consumers that have consumed psilocybin but had no change to their psilocybin use since COVID-19 was declared a pandemic were found to also have minimal anxiety. In contrast, of the cannabis consumers that decreased their psilocybin use, 32.3% were found to have mild anxiety. Among those with an increase in their psilocybin use, 26.0% were found to have mild anxiety and 26.0% were found to have moderate anxiety.
Conclusion: A considerable proportion of cannabis consumers experienced various levels of anxiety. Findings suggest an association between changes in psilocybin use patterns during the pandemic with varying anxiety levels. Given the increasing couse of psychedelics and cannabis along with growing research on their impact in mental health treatment, future studies are warranted to determine whether changes in use at times of public health crisis directly impacts anxiety levels or vice versa.
Ranya Marrakchi El Fellah University of Miami
Co-authors: Amrit Baral1, Bria-Necole A
Diggs1, Sarah Messiah2, Raul Gonzalez3 , Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: Prior studies have reported raised heart rate as an immediate physiological response to cannabis ingestion. Changes in heart rate typically correlates with blood pressure, depending on the dosage of cannabis use. Although evidence suggests that cannabis use may have these cardiovascular implications, findings are unclear and there is a dearth of knowledge regarding its effect on BP by routes of cannabis administration. Given the current popularity of various cannabis consumption methods, our analysis aims to explore the association of different routes of cannabis administration on blood pressure among young adult cannabis consumers.
Methods: The study utilized data from the baseline visit of the ongoing Herbal Heart Study cohort, which explores the impact of cannabinoids and various routes of cannabis administration on subclinical cardiovascular risk among young adults (18-35 years) in South Florida. Participants self-reported cannabis use, and use was further confirmed through rapid urine tests for drug screening. Blood pressure readings were obtained using a digital sphygmomanometer (blood pressure cuff), with three readings taken consecutively and the mean value of the readings was included in this analysis. Abnormal blood pressure was defined as systolic blood pressure ≥130 mm Hg or diastolic blood pressure ≥85 mm Hg. Descriptive statistics were employed to estimate the prevalence of abnormal blood pressure by different routes of cannabis administration: joint, blunt (wrapped in tobacco leaf), and vape.
Results: Among the total sample of
150 participants, the mean age was 24.6 years (SD=4.5), with 66.7% being female, 51.3% identifying as Hispanic/ Latino, and 50.7% reporting cannabis use. There was no significant difference in mean age between cannabis users and non-users (p=0.254). Within the cannabis user group, 30.3% used blunts, 34.2% used joints, and 35.5% used vape. Abnormal blood pressure was observed in 14.7% of the total sample, with 63.6% of those cases occurring among cannabis users. Among cannabis users with abnormal blood pressure, the majority were blunt users (31.8%), followed by vape users (22.7%) and joint users (9.1%).
Conclusion: The findings indicated a higher prevalence of abnormal blood pressure among cannabis users, with variations observed based on the method of consumption. Further investigation is necessary to uncover potential causal relationships. Overall, future research is required on the method of consumption to gain a deeper understanding of the potential implications for subclinical cardiovascular risk associated with cannabis.
Hamza
Masoud University of Miami
Co-authors: Amrit Baral1, Ranya Marrakchi El Fellah1, Bria-Necole A Diggs1, Sarah Messiah2, Raul Gonzalez3 ,
Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: With the increasing prevalence of cannabis use among young adults, various strains and potencies have become readily available. Studying the potential impacts of different forms of cannabis consumption on memory is a critical public health priority. This research provides valuable insights for policymakers, enabling them to develop evidence-informed regulations for cannabis legislation at the state level.
Methods: Data are from cannabis consumers from an ongoing Herbal Heart Study Cohort, studying the effects of cannabis, cannabinoids, and routes of cannabis consumption on subclinical cardiovascular risk among young adults (18-35 years old) residing in South Florida. Participants self-reported the strains and potency of cannabis they consume the most. As a part of the Marijuana Problem Scale (MPS) questionnaire, participants were queried about memory loss as a perceived problem caused by cannabis consumption, with response options: “no problem” to “minor problem” and “serious problem.” For this analysis, responses were coded into a binary variable: “Yes” if any problem was reported and “No” otherwise. Descriptive statistics and Chi-squared/Fisher’s exact test where appropriate were employed using SAS Analytics.
Results: Out of 76 cannabis users, 57.9% were female, with a mean age of 25.0 years (SD=4.3). Hispanics/Latinos constituted 51.3% of the sample, followed by African Americans (19.7%), and Non-Hispanic Whites (18.4%). The majority of participants indicated hybrid (42.1%) as their usual strain of cannabis use, followed by indica (30.3%), sativa
(18.4%), and 9.2% were uncertain about their usual strain. A larger proportion reported predominantly consuming high-potency cannabis (64.5%), followed by regular to mid-grade potency (25.0%), with the remaining 10.0% uncertain about the potency they mostly consume. Concerning self-reported memory loss as a problem caused by cannabis 43.4% reported having such a problem. Breaking down memory loss by cannabis strain mostly used, 34.8% of indica users, sativa (64.3%), and hybrid (37.5%) reported memory loss. Among those who reported memory loss, the majority were high potency cannabis users (81.8%) followed by those who were unsure of the potency (12.1%), and regular-mid grade users (6.1%, p=0.0025).
Conclusions: Findings suggest an association between cannabis strains, potency, and self-reported memory loss among young adults, with sativa users demonstrating the highest prevalence, followed by hybrid and indica users. Further exploration is needed to research the details and mechanisms of these findings.
Morgan McLaurin University of Miami
Co-authors: Bria-Necole A Diggs1, Amrit Baral1, Ranya Marrakchi El Fellah1, Cynthia Lebron1, Sarah Messiah2, Denise C Vidot1
1University of Miami, 2University of Texas
Background: The increasing prevalence of cannabis use among breastfeeding
individuals underscores the necessity for a better understanding of the specific cannabinoids consumed, including tetrahydrocannabinol (THC) and cannabidiol (CBD), during this important time period. Given that THC and CBD can be passed from mother to infant through breast milk and their effects on neurodevelopmental processes have been documented, our analysis aims to describe the prevalence of these cannabinoids in breastfeeding individuals.
Methods: Data are from the COVID-19 Cannabis Mom Study (N=221), a crosssectional study utilizing REDCap for consenting and survey distribution. The study collected self-reported information on cannabinoid use and breastfeeding history. Descriptive statistics and Chi-squared/Fisher’s exact tests examined patterns of cannabinoid use by route of consumption and reason for use.
Results: Among the participants currently breastfeeding (N=78), mean age was 31.0 years (SD=5.3), 62.8% were Non-Hispanic White, 18.0% Hispanic, 87.2% born in the United States, and 2.6% currently pregnant. The majority (92.3%) reported currently consuming cannabis while breastfeeding, of which 34.7% reported an increased change in their cannabis use while breastfeeding. Most (79.5%) reported cannabis use for medical reasons while breastfeeding. Regarding the self-reported dominant cannabinoid in the cannabis consumed by respondents currently breastfeeding, 52.7% reported THC dominant, 37.8% reported a THC and CBD ratio, while none (0.0%) reported CBD as their dominant cannabinoid. There was a difference in dominant cannabinoid by report of cannabis use for medical reasons (p=0.047). Specifically, among those consuming cannabis for medical reasons while breastfeeding, 51.6%
reported THC dominant, 41.9% THC and CBD ratio, 3.2% CBD, and 3.2% did not know the dominant cannabinoid in the cannabis consumed. Among those breastfeeding using cannabis for nonmedical reasons, 58.3% reported THC dominant, 16.7% THC and CBD ratio, 0.0% CBD, and 25.0% were unsure of the dominant cannabinoid in their cannabis.
Conclusions: Findings here showed a high prevalence of cannabis use while breastfeeding and significant differences between dominant cannabinoid and self-reported medical cannabis use status while breastfeeding. Only 3.2% of medical cannabis consumers reported the use of CBD dominant cannabis. Considering the differential effects of cannabinoids on receptors of the endocannabinoid system, these findings highlight the necessity for cannabinoid-specific education for those planning to and currently breastfeeding. Further research on the short and long-term impact each cannabinoid has on mother and breast-fed babies, for healthcare providers and mothers to make more informed decisions regarding cannabis use during breastfeeding.
Maria Carmenza Mejia Florida Atlantic University
Co-authors: Panagiota Kitsantas, Charles Hennekens, Allison Ferris Florida Atlantic University
Background: This study explored
admissions for cannabis use disorder (CUD) among pregnant women in publicly funded treatment facilities in the United States (US) from 2000 to 2021.
Methods: Data from the Treatment Episode Data Set-Admissions (TEDS-A) included 33,729 admissions of pregnant women with CUD. We calculated absolute as well as relative changes overall as well as by race/ethnicity, age and co-substance use.
Results: CUD-involved admissions among pregnant women increased 2.7-fold from 2.3% in 2000 to 6.2% in 2009. They steadily decreased to 4.3% in 2014 but reached a peak of 6.7% in 2018 and subsequently declined to 3.0% in 2021. Significant racial/ethnic disparities were noted, with higher rates in 2021 among White (48.8%) and Black (32.5%) non-Hispanic relative to Hispanic (9.6%). Although a decrease in CUD-involved admissions was observed among White women between 2010 (52.2%) and 2018 (45.4%), a significant increase was noted since then with a peak in 2020 at 51.2%. Since 2014 there was an increase in CUD related admissions among pregnant Black non-Hispanic women (29.6%) with a major increase in 2018/2019 (36.1%) and a 1.2-fold increase since 2014. Although CUD admissions were more prevalent between the ages of 2129 years old, a notable decline was observed between 2018 (62.1%) and 2021 (57.2%). A significant increase of 2.3-fold was observed in CUD admissions in women of at least 30 years of age between 2010 (12.2%) and 2021 (28.1%). CUD admissions in pregnant women deceased in those ≤20 years old with a notable increase in 2021(19.2%) which fell to 14.7% in 2021. Most co-substance use in CUD related admissions peaked in 2018 and declined since 2019 with the exception of inhalants which spiked in 2020.
Narcotics, stimulants, depressants, and hallucinogens were the most prevalent co-substances among CUD admissions in pregnant women, particularly between 2017 and 2021. Overall, we observed a steady increase of narcotics from 2000 to 2017 and a decrease since then, while hallucinogens, inhalants and stimulants varied considerably from year-to-year in CUD-related admissions.
Conclusion: The data revealed significant changes in CUD admissions among pregnant women over two decades, with variations across different racial/ethnic groups and age categories. These findings suggest the necessity for tailored intervention strategies and continuous adaptation of treatment services for pregnant women with CUD in US publicly funded facilities. Future analytic studies are recommended to test the hypotheses generated by these descriptive data and address the complex needs of this population.
Zully Moreno University of Miami
Co-authors: Amrit Baral1, Ranya Marrakchi El Fellah1, Bria-Necole
A Diggs1, Sarah E Messiah2, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: Cannabis is often cited as a potential alternative or an adjunct for managing symptoms of physical and mental chronic medical conditions. While existing literature
reports extensive physiological effects of cannabis use, an understanding of its impact on subjective well-being such as the quality of life (QoL) is still lacking. This study seeks to bridge this gap by assessing various domains of QoL among young adults, a population that has been reported to have a higher prevalence of cannabis consumption using various methods. We further compared the differences with their non consumer counterparts.
Methods: The data is from the initial assessment of participants in the ongoing Herbal Heart Study cohort that investigates the effect of cannabinoids on subclinical cardiovascular risk among young adults (18-35) in South Florida. QoL was assessed through the 26-item World Health Organization Quality of Life questionnaire (WHOQOLBREF), categorized into four domains: physical health, psychological wellbeing, social relations, and environment. The mean scores within each domain were utilized to compute domain scores, aligned with WHOQOL-100 standards, and subsequently transformed to a 0–100 scale. Two items gauged participants’ overall perceptions of QoL and health. To compare QoL scores based on cannabis use status and administration routes, the Mann–Whitney U test and Kruskal–Wallis were applied as appropriate, using SAS Analytics.
Results: Of the total young adults (N=150), the mean age was 24.6 years (SD=4.5), with 66.7% being female, 51.3% identifying as Hispanic/Latino, and 50.7% reporting cannabis use. Among cannabis users, 30.3% were blunt users, 34.2% joint, and 35.5% vape (35.5%). The total QoL score did not show a significant difference between cannabis users and non-users (Z=1.5494, p=0.12). The median scores for overall QoL and general health were not significantly different between the
two groups (P=0.49) and by routes of cannabis administration among users (p=0.36). Similarly, there was no statistically significant difference in median scores across all four domains when comparing cannabis users to non-users. However, within the group of cannabis users, a significant difference emerged in the median score for psychological well-being by routes of cannabis consumption:[ joint (75.0), blunt (62.5), and vape (58.3), Kruskal Wallis X2= 10.234, df=2, p<.01)].
Conclusion: Although no significant difference in the overall QoL was observed between two groups, a significant difference in psychological well-being among cannabis consumers by methods of use highlights the importance of examining specific QoL dimensions in understanding the impact of cannabis use on holistic well-being among cannabis habitual users.
Anne-Barbara Ocejo University of
Miami
Co-authors: Amrit Baral, Denise C Vidot University of Miami
Background: The evolving landscape of cannabis research in oncology along with the surge in availability of diverse cannabis products has generated increased interest in its use among cancer patients for various medical
and non-medical reasons. This growing utilization underscores the need for a comprehensive understanding of usage patterns, cannabinoid dominance, and the demographic factors shaping consumption. This study addresses the critical gap in literature on cannabinoid preference, specifically Delta-8tetrahydrocannabinol (THC) and Delta-9THC by ethnicity among cancer patients in different stages of their cancer treatment.
Methods: This analysis utilized data from a cross-sectional study of adult cancer patients seen at a National Cancer Institute (NCI)-designated comprehensive cancer center in the last 5 years to assess cannabis use patterns, source, and reasons for use. Descriptive statistics were computed to estimate the self-reported proportions of Delta-8 and Delta-9 THC as dominant cannabinoid in cancer patients’ cannabis by ethnicity and cancer treatment status. Chi-squared/ Fisher’s exact tests where appropriate were conducted to compare dominant cannabinoid proportions.
Results: Of the overall sample (N=495) [mean age 45.9 years (SD=15.1)], 63.1% were current cannabis users, 51.8% were male, and 39.4% were Hispanic/ LatinX. Cancer treatment statuses for current cannabis users included 15.5% newly diagnosed, 43.8% under treatment, 35.4% completed therapy and following up, and 5.3% not receiving treatment. Among current cannabis users, 16.8% reported Delta-8-THC as their dominant cannabinoid, while only 9.7% indicated Delta-9-THC as their primary cannabinoid in their cannabis. 29.8% of Delta-8-THC users and 36.7% of Delta-9-THC users were Hispanic. The majority of Delta-8-THC users were undergoing treatment (52.6%), followed by those who completed treatment/ in follow-up (42.1%), with only 3.2% being newly diagnosed or not receiving
treatment. Delta-9-THC users showed no newly diagnosed cases (0.0%), with the majority under treatment (72.7%), followed by those in follow-up (22.7%), and not receiving treatment (4.5%). There was a significant age-related difference in Delta-9-THC usage among current cannabis users: 3.2% among 2039 years old, 12.7% among 40-59 years old, and 16.7% among ≥60 years old (p=0.02).
Conclusion: Among the 63.1% of current cannabis users, the study reveals Delta8-THC as the dominant cannabinoid for 16.8% of users surpassing Delta-9THC at 9.7%. The prevalence of Delta8-THC underscores the importance of comprehending cannabis utilization among cancer patients and the necessity for personalized treatment. Overall, this study provides valuable educational insight for clinicians, researchers, and policymakers in the ongoing discussion surrounding cannabis use in cancer care.
Juan Perez University of Florida
Co-authors: Sophie A Maloney, Hanzhi Gao, Ruba Sajdeya, Gabriel A Spandau, Yan Wang, Robert L Cook, Catalina Lopez-Quintero University of Florida
Background: Longitudinal studies have found attrition to surveys up to 30%. The overall retention rate will typically continue decreasing over time and change according to the survey modality (mail, phone, online, social media). Some studies report that incentives, such as $10 gift cards increase retention to follow-up. Additionally,
cannabis cessation, reported in 16.3% of current or former cannabis users, can be associated with attrition. However, associations between participant’s characteristics with loss to follow-up status remain underreported and poorly understood.
Objectives: This study aims to describe retention rates in a cannabis longitudinal study and characterize the population lost to follow-up in terms of sociodemographics, reasons for cannabis use, and cannabis use patterns.
Methods: The Medical Marijuana and Me study (M3) study included a longitudinal survey to characterize a population of new medical marijuana users in Florida. Follow-up methods included mail, email reminders, and phone calls (3 maximum attempts per participant). The study offered a $20 card plus a $10-$20 bonus for completing the follow-up survey on time. We described retention rates among participants according to the top three reasons for use. Using bivariate analysis we compared sociodemographics, standardized self-reported measures (Generalized Anxiety Disorder-7 scale; Patient Health Questionnaire Depression scale, and Cannabis Use Disorder Test-Revised: CUDIT-R), and cannabis use patterns between participants lost to follow-up at 3-month and those completing the 3-month follow-up visit.
Results: Among 602 participants at baseline, 239 (39.7%) were lost to follow-up in the 3-month visit (median age: 37 years; ICR: 26 years). Depression was the reason for use with higher loss to follow-up (41.9%), followed by anxiety (40.4%), and chronic pain (37.6%). Between the lost to follow-up group and the group completing the 3-month visit, being female (55.2% vs. 65.6%, respectively), having a college degree or higher (65.4% vs. 78.2%),
having private health insurance (44.8% vs. 53.7%) were different (p<0.05).
Anxiety and depression status, main reason for cannabis use, type of product used, and cannabis experience were not associated with loss to follow-up. Conversely, having a normal CUDIT-R and using cannabis for medical purposes were associated with a complete follow-up (p<0.005).
Conclusions: In the M3 study, some characteristics informed the likelihood of being non-adherent to the study visits. This information will help researchers adjust sample size calculation and target specific subpopulations to increase study participation and reduce selection bias. Further research will help in understanding adherence to study procedures in cannabis research across the United States.
Vanessa Quinn University of Florida
Co-authors: Amie Goodin, Jungjun Bae University of Florida
Background: Cannabis has been proposed as a potential therapeutic or as therapeutic adjuvant for a variety of physical and mental health conditions, including anxiety. However, there are inconclusive findings regarding safety and effectiveness of cannabis as a treatment for anxiety disorders or symptoms of anxiety. Substitution of prescription benzodiazepines with cannabis to relieve anxiety has been reported in small cohort studies; however, there is limited data
regarding factors associated with concurrent cannabis and prescription benzodiazepine use.
Objectives: Our objective is to examine factors associated with concurrent medical cannabis and prescription benzodiazepine use in people with anxiety.
Methods: Recruitment strategies for this cross-sectional survey were convenience sampling from May 2022 through May 2023 of adult medical cannabis users from Florida clinics. The survey included items from validated instruments to assess mental and physical health status and cannabis use behaviors, along with questions about medication use. We examine sociodemographic factors and cannabis use behaviors in respondents that reported diagnoses of anxiety. Factors include: age, race/ethnicity, sex at birth, veteran status, health insurance status, age at first cannabis use, and cannabis use frequency. A logistic regression model estimated the relationship between sociodemographic factors and cannabis use behaviors associated with concurrent prescription benzodiazepine use relative to no benzodiazepine use. Results were calculated with robust standard errors and reported with 95% Confidence Intervals.
Results: There were 632 total respondents and 451 respondents had anxiety diagnoses (71% of all respondents). Among those with anxiety, mean age at first cannabis use was 20 years (SD=10) and mean current age was 44 years (SD=13). The majority (88%) reported using cannabis “4 or more times per week.” Concurrent prescription benzodiazepines were reported by 151 (33%) of those with anxiety. Current age was the only sociodemographic factor significantly associated with concurrent benzodiazepine use (OR=1.02; 95%
CI 1.00-1.03), where each additional year of age suggested a 2% increase in likelihood of concurrent prescription benzodiazepine use. No other sociodemographic factors nor cannabis use behaviors (e.g., age at first use and frequency of use) were significantly associated with concurrent prescription benzodiazepine use; however, few respondents indicated infrequent cannabis use.
Conclusions: Prescription benzodiazepine use was prevalent among this convenience sample of cannabis users with anxiety. Older adults were more likely to have concurrent prescription benzodiazepine and cannabis use than younger adults with anxiety, indicating that safety communications could be tailored to this population. Findings may not be generalizable due to the sampling strategy.
Carter Reeves University of Utah
Co-authors: A. Taylor Kelley1,2, Lirit Franks1, Michael A Incze1, Adam J Gordon1,2, Gerald Cochran1,2 1University of Utah, 2VA Salt Lake City Healthcare System
Objective: To identify reliance on different sources of medical cannabis information among participants in a state medical cannabis program and the impact of source reliance on illicit cannabis used medicinally.
Background: Medical cannabis (MC) is
now used by nearly 4 million individuals across the US, making access to accurate MC information imperative to ensure safe MC use practices and optimize outcomes for this population. Understanding which sources of MC information individuals rely upon most, as well as the impact of this information on illicit medical cannabis use, could therefore be valuable in helping state MC programs maximize benefits for MC users and reduce possible harms from illicit cannabis used medicinally.
Methods: Design and Participants: In this exploratory analysis of baseline data from a prospective cohort study, we analyzed survey results from adult patients newly enrolled (<6 months) in Utah’s MC program. Assessments: Participants self-reported their reliance on different sources of MC information (where participants receive their information), whether they accessed illicit medical cannabis and motivations for doing so. Analysis: We analyzed demographics using descriptive statistics. Differences in reliance on sources of MC information were analyzed using Wilcoxon rank-sum tests. We used binominal logistic regression to determine associations between MC information source reliance and illicit medical cannabis use, controlling for other drivers of illicit medical cannabis use (ensuring adequate supply and cost.)
Results: The sample included 211 MC program participants (mean age 39.3, SD=0.81, 56.6% female, 84.4% white, 11.3% Hispanic/Latinx, 19.1% rural). Of the participants, 11.8% reported current use of illicit medical cannabis. Participants were most likely to report reliance on information from dispensary pharmacists (54.9%), followed by card-issuing health care providers (44.7%), friends/peers (39.9%), and the internet (29.8%), which all had significantly higher levels of reliance
than the Utah MC program’s resources (17.9%, P’s<0.01). In binomial regression analysis, when the majority of participants’ information came from the Utah MC program resources, the odds of using illicit medical cannabis decreased (AOR=0.02, p0.05).
Conclusion: Despite the low percentage of individuals relying upon Utah’s MC program, this source of information may be effective in attenuating medicinal use of illicit cannabis. Future research is needed to determine what type of information disseminated through Utah’s MC program was most impactful to reduce illicit medical cannabis use.
Teddy Salan University of Miami
Co-authors: Christian Camargo1, Suresh Pallikkuth1, Yan Wang2, Varan Govind1 1University of Miami, 2University of Florida
Background: Among various mechanisms implicated in the etiology of Alzheimer’s disease (AD), neuroinflammation, oxidative stress, and disruption of the endocannabinoid (ECS) system, play key roles in the disease onset and progression. Numerous human and animal model in vivo studies have demonstrated the potential of cannabis-based products in modulating these processes, specifically cannabidiol (CBD), due to its anti-inflammatory, anti-oxidative, ECS modulatory, and neuroprotective
properties. However, it is unclear how many studies have used neuro-imaging techniques to examine the effects of CBD on the above processes in the brains of AD patients in vivo.
Objective: To perform a systematic literature review to summarize the impact of CBD treatment in the brains of AD patients using neuroimaging methods.
Methods: PubMed literature search containing the terms “Alzheimer’s disease”, combined with “cannabidiol”, “cannabinoid”, “cannabis”, or “marijuana” and with “MRI” or “PET” was performed.
Results: The literature search identified 32 articles. None of these articles investigated marijuana or its products or their effects on the brains of patients with AD. Therefore, to the best of our knowledge, there are no published studies that investigated the effects of CBD in the brains of patients with AD using brain imaging methods (i.e., MRI and PET). However, there are two brain MRI and three PET studies that evaluated the effects of CBD on AD-relevant brain structures (e.g., hippocampus) and function in healthy human subjects or animal models. MRI: One study using arterial spin labeling MRI showed that CBD increased cerebral blood flow in healthy subjects and associated with improved reaction time and working memory, particularly in the hippocampus and other brain structures affected by AD. Another study using structural MRI showed that CBD treatment in cannabis consumers restored the hippocampal structure, as evidence of the differential effect of CBD compared to other cannabis compounds. PET: Three studies evaluated the use of cannabinoids in AD animal models; one showed that CBD improved fluorodeoxyglucose metabolism and memory, and two studies showed that synthetic
cannabinoids (WIN-55-212-2 and JWH133) reduced TNF-α expression and β-amyloid levels.
Conclusions: Despite CBD showing promising results in restoring hippocampal structure and function and reducing neuroinflammation in the brains of healthy subjects, evidencebased knowledge on the effects of CBD on the brains of AD patients using advanced in vivo MRI techniques is still lacking. Future studies should focus on filling this knowledge gap and gather comprehensive brain imaging data in AD patients who are taking cannabis products.
Teddy Salan University of Miami
Co-authors: Flavia M Nelson1, Ramon Flores Gonzalez1, Suresh Pallikkuth1, Yan Wang2, Varan Govind1
1University of Miami, 2University of Florida
Background: Multiple sclerosis (MS) is an auto-immune disorder that disrupts neural communication in the central nervous system (CNS). People with multiple sclerosis (pwMS) consume cannabis-based products for alleviating symptoms such as spasticity, pain, and sleep difficulties. Multiple studies and clinical trials have demonstrated the
benefits of Δ9-tetrahydrocannabinol (THC) for relieving these symptoms in PWMS. However, less attention has been given to cannabidiol (CBD) which, unlike the psychoactive THC, provides several benefits due to its anti-inflammatory, anti-oxidative, and neuroprotective properties making it a strong add-on therapeutic option for better clinical management of MS.
Objective: Perform a systemic literature review to summarize the effects of CBD and other cannabis products on the CNS in PWMS, identified using neuroimaging methods.
Methods: A PubMed literature search containing the terms “multiple sclerosis” combined with “cannabidiol”, “cannabinoid”, “cannabis”, or “marijuana” and with “MRI” or “PET” was performed.
Results: The literature search resulted in 9 articles related to the use of THC or CBD and MRI changes in pwMS, eight of those used MRI and one used PET imaging. MRI: Five articles examined cognitive changes in pwMS who smoked cannabis, showing cognitive deficits correlating with tissue volume reduction on structural MRI and less efficient activation on functional MRI. One of these studies showed recovery in some cognitive functions after 28day cannabis abstinence. Two articles examined pwMS treated with nabiximols (THC:CBD), showing reduced spasticity and changes in brain functional connectivity, but no microstructural improvements based on diffusion MRI. One article from the CUPID study found that dronabinol (THC) had no effect on brain lesion volumes in pwMS. PET: A single PET study showed differential effects of THC and CBD on brain metabolism in pwMS, those taking THC showed hypermetabolism of cerebral fluorodeoxyglucose while those taking CBD had hypometabolism. To the best of our knowledge, this is the only
study investigating the effect of CBD, without THC, on the brain. Furthermore, no advanced MRI techniques, such as MR spectroscopy, diffusion kurtosis imaging, and neuromelanin MRI, and no cannabinoid-receptor specific PET ligands were used in prior articles.
Conclusion: Despite MS being a qualifying condition for receiving medical marijuana, evidencebased knowledge on the effects of cannabinoids, in particular CBD, on neuroinflammation and neuronal function the CNS in pwMS is still lacking. Comprehensive brain imaging studies using advanced MRI techniques are warranted for evaluating neuro-inflammation, neuro-immune activation, neuronal function, and neurotransmitters in pwMS who are taking cannabis products.
Cataryna Senra University of Miami
Co-authors: Amrit Baral1, Bria-Necole
A Diggs1, Ranya Marrakchi El Fellah1, Sarah E Messiah2, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: The COVID-19 pandemic impacted health and societal norms globally, prompting widespread changes in behaviors including social distancing, virus testing practices, and vaccine uptake. Evidence showed that there
was a surge in cannabis consumption during the pandemic especially among the younger population. Yet, there is a dearth in literature reporting COVID-19 associated behaviors among young adults by cannabis consumption status. Therefore, this analysis examines COVID-19 history among young adult (18-35-year-olds) cannabis consumers and non-consumers in South Florida.
Methods: Data are from the ongoing Herbal Heart Study, examining the effect of cannabinoids and cannabis administration routes on subclinical cardiovascular risk among healthy young adults in South Florida. COVID-19 history responses were self-reported via the COVID-19 Cannabis Health Questionnaire via PhenX toolkit. Descriptive statistics and Chi-squared/ Fisher’s exact tests, where applicable, analyzed COVID-19 history in cannabis users (CUs) and non-users (NUs).
Results: Of 150 study participants, mean age was 24.6 years (SD=4.5), 66.7% were female, 51.3% Hispanic/ Latino, and 50.7% reported cannabis use. A large proportion of the sample (70.9%) reported exposure to someone with COVID-19, with CUs constituting the majority. About half (49.3%) of the sample lived or stayed with individuals experiencing COVID-19 symptoms or tested positive, of which 54.2% were CUs. Access to COVID-19 testing was high (98.0%) in the overall sample. A considerable proportion (97.3%) had undergone COVID-19 testing since the pandemic declaration. Notably, 58.6% of respondents testing positive for COVID-19 were CUs. Fear of transmitting the virus to someone else reported by 51.3% of NUs and 34.7% of CUs (p=0.040). A notable proportion (27.5%) expressed fear of being diagnosed with COVID-19: 41.5% were CUs. Since COVID-19 was declared a pandemic, 83.9% of the sample reported isolating themselves and of these 52.0%
were NUs. While a majority received the COVID-19 vaccine (81.1%), the proportion differed significantly between CUs and NUs (72.0% vs 90.4%, p<.01). Furthermore, a higher percentage of non-users (75.4%) received the booster shot compared to cannabis users (54.9%, p=0.022). Among recipients experiencing side effects, 59.0% were non-users.
Conclusion: Findings revealed that CUs had higher prevalence of selfreported exposure to the virus and lower engagement in preventive measures, such as self-isolation. Notably, disparities in vaccine uptake and booster shot receipt highlight the need for tailored public health interventions to address the unique challenges and perceptions within the CU population during the ongoing pandemic.
Thomas Snooks Dalhousie University
Co-authors: Phil Tibbo2, Pablo RomeroSanchiz3, Sarah DeGrace1, Haley Bernusky4, Sean Barrett1, Sherry Stewart1 1Dalhousie University, 2Nova Scotia Health Authority, 3University of Sussex, 4University of York
Over the past 20 years, levels of Δ9-tetrahydrocannabinol (THC) in cannabis have significantly increased while levels of cannabidiol (CBD) have increased much less in comparison. Cannabis with higher THC potency (commonly assessed via THC:CBD
ratio) may increase the risk for cannabis dependence and exacerbate anxiety. However, few studies of cannabis potency effects on cannabis dependence and anxiety have examined gender moderation. Additionally, there are issues with how cannabis potency is calculated via THC:CBD ratio that may contribute to inconsistencies in the literature. To address these concerns, N = 199 (55.8% women) recent cannabis users (>1g in the past month) with trauma histories and whose biological sex and gender identity were congruent – a group at high risk for anxiety and cannabis dependence – completed an online survey including a measure of self-reported THC and CBD levels in participants’ typically-used cannabis products. Cannabis potency was measured by THC:CBD ratio (THC%/ CBD%) and by relative THC proportion (THC%/[THC%+CBD%]). The Cannabis Use Disorder Identification Test-Revised (CUDIT-R) and Generalized Anxiety Disorder-7 (GAD-7) assessed cannabis dependence and anxiety, respectively. Consistent with previous research, cannabis potency was significantly, positively correlated with cannabis dependence, p = .002, and anxiety levels, p = .020, but only when assessed via THC proportion and not THC:CBD ratio. Additionally, women reported significantly higher anxiety levels and THC:CBD ratios than men. However, no significant gender differences were found in the relationships of either potency measure with any of the outcome variables. Results are consistent with a convergence of previously reported gender differences in cannabis dependence among recent cannabis users. Findings also point to the importance of considering relative THC proportion as a superior predictor of adverse cannabis outcomes than THC:CBD ratio in both men and women.
Renessa
Williams University of Miami
Co-authors: Ella Remund1, Ellen Almirol1, Yen-Tyng Chen2, Adam Carrico3, Jade Pagkas-Bather1, Denise Vidot4, Justin Knox5, John Schneider1, Dustin T Duncan6
1University of Chicago, 2Rutgers University, 3Florida International University, 4University of Miami, 5Columbia University, 6New York University
Introduction: Black gay, bisexual, and other sexual and gender minorities (SGM) must contend not only with racial minority stress (e.g., racerelated housing and job discrimination, racism within and outside the LGBTQ+ community), but with sexual minority stress as well (e.g., sexual minorityrelated discrimination, SM-related violence, homophobia). According to the Sexual and Gender Minority (SGM) Health Disparities Research Framework, multilevel stress encompasses individual (e.g., socioeconomic status demographics), interpersonal (e.g., discrimination), community (e.g., safe spaces) and structural (e.g., neighborhood conditions) factors that may further contribute to health inequities in the Black SGM community. There is evidence to suggest cannabis use is linked to stress, therefore, assessing multi-level stressors may yield novel insights into the broader
determinants of health that contribute to cannabis use.
Methods: Cross-sectional data from a Chicago-based cohort of Black men and Black transgender women aged 16-35 years were collected from October 2022 to February 2023 (N=553). Correlates were chosen based on the SGM framework, in which participants selfreported multilevel stressors including age, gender, income, employment, mental health, discrimination, violence, incarceration, neighborhood access and safety. Further, the Cannabis Use Disorders Identification Test (CUDIT-R) identified non-hazardous use, hazardous use, and possible cannabis use disorder based on established cutoffs. Bivariate analyses and regression models were used to examine the correlates associated with cannabis use.
Results: Among our sample of cannabis users (N=489, 88%), 62% were older than 27 years, 83% were cis-gender male, 59% were gay, and 55% were living with HIV. Among those who reported symptoms of possible cannabis use disorder (n=250, 51%), approximately 56% had experienced intimate partner violence (IPV), 37% had anxiety symptoms, and 44% were incarcerated, which was proportionally higher than those who reported hazardous or nonhazardous use. Compared to those with non-hazardous use, those with possible use disorder had a significantly greater likelihood of reporting individual-level stress including anxiety symptoms (OR 2.27, 95% CI 1.24, 4.10, p<0.01) and microaggressions (OR 1.66, 95% CI 1.00, 2.75, p=0.05). Those with possible cannabis use disorder were also significantly more likely to experience IPV (OR 1.88, 95% CI 1.12, 3.15, p=0.02) compared to non-hazardous users, an interpersonal stressor. No significant differences were observed between participants with or without hazardous cannabis use.
Conclusion: Findings suggest multiple levels of stress are associated with cannabis use. Future research should consider how mental health, discrimination, and violence mediate cannabis usage to mitigate stress and improve health among Black SGM, a population underrepresented in health research.
Maxwell Wray University of Miami
Co-authors: Amrit Baral1, Bria-Necole
A Diggs1, Ranya Marrakchi El Fellah1, Sarah E Messiah2, Raul Gonzalez3, Barry Hurwitz1, Claudia Martinez1, Denise C Vidot1
1University of Miami, 2University of Texas, 3Florida International University
Background: Research suggests that men and women experience anxiety and depressive disorders at different rates and are affected by cannabis differently. There is also some concern that cannabis use has negative impacts on the mental health of young adults who may use cannabis to alleviate symptoms of anxiety and depression. However, the relationship between sex, age, and cannabis use on mental health is unclear. This study assesses if there are sex-based and aged-based differences in anxiety and depression among cannabis consumers (CB+) and non-consumers (CB-).
Methods: Data were utilized from the ongoing Herbal Heart Study which investigates the relationship between cannabis use and subclinical cardiovascular risk. The Beck Anxiety Inventory (BAI) and the Beck Depression Inventory (BDI) were administered. BAI and BDI are 21 question surveys that respectively classify anxiety and depressive symptoms experienced during the preceding week as either minimal, mild, moderate, or severe. First, BAI and BDI scores were compared among CB+ and CB- in the overall sample and then stratified by sex with t-tests and Mann-Whitney tests. This analysis was repeated to compare scores among Hispanic and non Hispanic participants, and among participants aged 18-26 and 27-35. Lastly, Chi-Square tests of independence and Fisher tests were used to see if cannabis use was related to severity of BAI and BDI scores.
Results: Among 150 participants [mean age: 24.6y (SD=4.49)], 66.7% were female, 51.3% were Hispanic/Latino, and 50.7% were CB+. In the overall sample, CB+ had significantly higher BAI scores than CB- (p=0.03), and participants aged 18-26 had significantly higher BDI scores than those aged 27-35 (p=0.018). No significant differences were found for BDI score between CB+ and CB- in the overall sample (p=0.15) or for BAI and BDI scores between Hispanic and non Hispanic participants. Sex stratification revealed that male CB+ had significantly higher BAI and BDI scores than CB- (p=0.015 and p=0.003, respectively) and female CB+ aged 1826 had significantly higher BDI scores than female CB+ aged 27-35 (p=.04). Lastly, cannabis use was not associated with severity of BAI and BDI scores.
Conclusion: Sex and age based differences were found in this cohort of cannabis consumers and nonconsumers. Additional research is
needed to evaluate the relationship between sex, age, and cannabis use, alongside implementing an intervention to lower depressive and anxiety symptoms among male cannabis users and young adults.


Every day, the OMMU works to provide qualified patients, caregivers and physicians the information and resources they need to access Florida’s medical marijuana program.
The mission of the Medical Marijuana Education and Research Initiative is to educate and inform Florida’s diverse minority communities about medical marijuana and the potential consequence to health and well-being from recreational use.
The Consortium for Medical Marijuana Clinical Outcomes Research, founded by the state of Florida legislature, conducts, disseminates and supports research on the clinical effects of medical use of marijuana.
Composed of nine universities in the state of Florida, the Consor tium works to enhance the evidence on the safe and effective use of medical marijuana to inform clinical decision-making and guide policy.
Learn more at mmjoutcomes.org
Jennifer Attonito, PhD – Florida Atlantic University
Lisa Eckel, PhD – Florida State University
Raul Gonzalez Jr, PhD – Florida International University
Amie Goodin, PhD – University of Florida
Varan Govind, PhD – University of Miami
Jeevan Jyot, PhD – University of Florida
Sari Paikoff, PhD – Florida Gulf Coast University
Mandip Sachdeva, PhD – Florida A&M University
Rose Stiffin, PhD – Florida Memorial University
Ellen Terry, PhD – University of Florida
Almut Winterstein, PhD – University of Florida
Jennifer Attonito, PhD – Florida Atlantic University
Nicholas Cherup, PhD – University of Miami
Robert Cook, MD, MPH – University of Florida
Lisa Eckel, PhD – Florida State University
Amie Goodin, PhD, MPP – University of Florida
Varan Govind, PhD – University of Miami
Md Mahmudul Hasan, PhD – University of Florida
Sebastian Jugl, RPh, MS – University of Florida
Priyanka Kulkarni, MPH – University of Florida
Catalina Lopez-Quintero, PhD – University of Florida
Sari Paikoff, PhD – Florida Gulf Coast University
Juan Perez, MD, MSc – University of Florida
Linda Robayo, PhD – University of Miami
Mandip Sachdeva, PhD – Florida A&M University
Teddy Salan, PhD – University of Miami
Ellen Terry, PhD – University of Florida
Yan Wang, PhD – University of Florida
Almut Winterstein, RPh, PhD, FISPE – Director
Robert Cook, MD, MPH – Associate Director
Yan Wang, PhD – Assistant Director, Clinical Core
Amie Goodin, PhD, MPP – Assistant Director, Evidence
Md Mahmudul Hasan, PhD – Assistant Director, MEMORY
Jeevan Jyot, PhD, PMP – Assistant Director, Research Administration
William Anderson, PhD (Chair) – Florida International University
Martha Rosenthal, PhD (Vice Chair) – Florida Gulf Coast University
Christopher McCurdy, PhD – University of Florida
Peter Holland, MD – Florida Atlantic University
Eric Holmes, PhD – Florida State University
Max Orezzoli, PhD – Florida Memorial University
Jacqueline Sagen, PhD – University of Miami
Dinender Singla, PhD – University of Central Florida
Charles Weatherford, PhD – Florida A&M University
Amie Goodin, PhD & Almut Winterstein, PhD – Conference Co-Chairs
Jeevan Jyot, PhD, PMP – Coordination and Logistics
Allison Veliz, MA – Marketing and Communications
As the official journal of the Consortium, Medical Cannabis & Cannabinoids will publish the Consortium’s conference proceedings, guidelines, and position statements.
For CCORC 2024, selected abstracts will be published in the Medical Cannabis & Cannabinoids. Read more about Medical Cannabis and Cannabinoids by clicking the ad below.

On behalf of the Consortium for Medical Marijuana Clinical Outcomes Research’s Scientific Program and Planning Committees, we would like to express our gratitude to all involved in organizing and conducting CCORC 2024, including: keynote speakers, session members, board members, exhibitors, and volunteers. We thank, AV Matters, Studio D Meetings and Events, and the Office of Events at the University of Florida College of Pharmacy for technical support and event coordination. We hope to see you again at CCORC 2025!