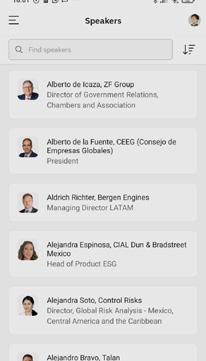
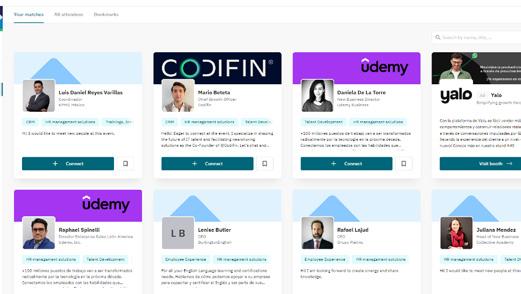
Matchmaking
Mexico’s leading B2B conference organizer uses a customized app to deliver an unparalleled experience
The MBE App delivered AI-powered intent-based matchmaking to Mexico Mexico Health Summit 2025 attendees MBE App Impact
165 participants
339 matchmaking communications
115 1:1 meetings conducted
27 speakers
14th Edition
click through rate during MHS
6 sponsors
10,407 visits to the conference website
direct pre-conference LinkedIn impressions
pre-conference click through rate
intentions
• Abeile Med
• Acceso en Salud
• Adium
• Alcon pharmaceutical Mexico
• Alandra Medical
• AMID
• AMIIF
• Anafarmex
• Apr HIFAC
• Area Industrial
• Art Tecnica
• Asesores Medico Biologicos SA de CV
• Asociación Healthtech
• Avanzia pharma
• AXA Mexico
• Baker McKenzie Mexico
• Baxter
• BBVA
• Becerril, Coca & Becerril
• Best Doctors
• Biocaps de México
• Bio- rad
• Biotech & rare Diseases Consultant
• B pL-Kedrion
• Bristol Myers Squibb México
• Brixton Venture Lab
• BuscaMed
• Business France
• Business Sweden
• Camara Italiana
• CAS
• CCE
• Centinel Biogen
• Central Media
• Centro Médico ABC
• Ceoderma
• CHG Meridian Mexico
• CleverClick 360
• clinicasdelhombre.com
• Co MED
• Cryoholdco
• CTr Scientific
• Deutsche pharma
• Diagnostikare
• Dlife
• Doctoralia Mexico
• Dubai Chamber
• DVA
• Edryx Healthcare
• Elek ta Medical
• Elery
• Embajada de Francia
• Ethical Nutrition
• Farcoyo.com
• Faes Farma
• Finsolar
• Freyr Life Sciences
• FQM
• Funsalud
• Gadmar SA de CV
• GE HealthCare Latin America
• Gecko Global Services
• G enomma Lab
• Gilead Sciences
• Glenmark pharmaceuticals
• Global Health Intelligence
• G rupo Somar
• Happy Clinic Ideas
• Healf
• Headline pr&Comms
• Helix Health
• Hike o n
• Holland House Mexico
• Hospitales Mac
• Hospitales puerta de Hierro
• ICAN LatAm
• IMSS
• INMEGEN
• Intramed
• International S o S México Emergency Services S de r L de CV
• Interpharm
• IQVIA
• Kerme
• Laboratorio Corne
• La Frutologia
• Leo pharmaceuticals
• Linet Group
• Lilly Latin America
• LLYC
• McCann Health SI
• Medical Center Tecámac
• Medikit
• Medisi America
• Medtronic
• Medu
• MeetingDoctors
• Milenium
• Molnlycke
• Monterrey Aerocluster
• M otion Corp
• Neolpharma
• N euraxpharm
• Newmont
• Ngrenta
• Novar tis Mexico
• NutriADN
• oCA Global
• o livares y Compañía, S.C.
• o ntario’s Trade & Investment o ffice in M exico City
• page Executive
• pascual Asesoría en Farmacias
• pepsiCo
• philips Mexico Commercial
• pharma GBC
• plenna
• polar Salud
• prixz
• prp
• prosperia
• revista Lideres Mexicanos
• rGA reinsurance Company
• robert Walters
• rofina - Siegfried
• roemmers
• Salumedic
• Sanofi
• Seima
• Sentinel Biogen
• Servicios M edicos BMG
• Siegfried
• Signufarma
• Siemens Healthineers Mexico, Central America and the Caribbean
• Skye Group
• Sociedad Mexicana de Salud pública
• Sofía
• Sofía Salud
• Solistica
• Soluciones en Liderazgo Farmacéutico
• Stryker
• Stendhal
• Tand
• Tequilera de Arandas
• Theranomics
• Thermo Fisher Scientific
• Tindala, Salud Mental y Emocional Ejecutiva
• Trade and Commerce Council of India and Mexico
• Tuteur Group
• TV Azteca
• UDEM
• U CIN Médica
• Universidad panamericana
• Ve por Más
• Vantive
• Viatris
• Weber Shandwick
• WelbeCare
• Worldwide Clinical Trials
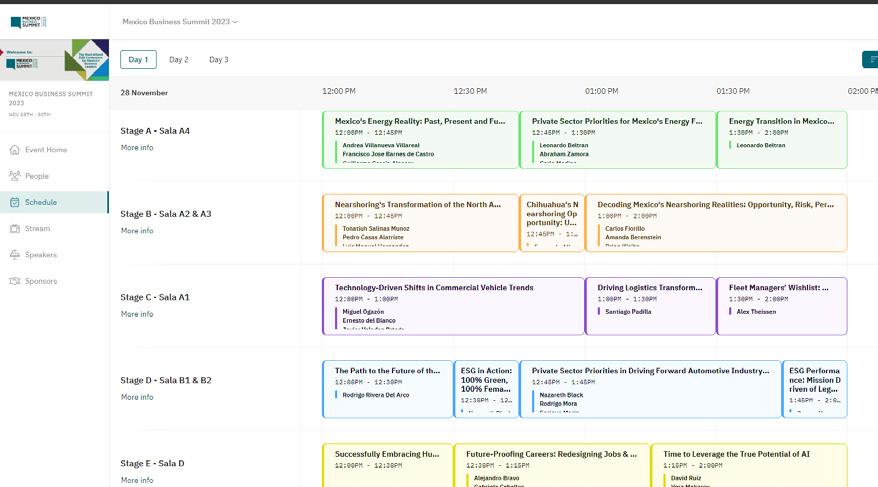
WEDNESDAY, SE PTEMBER 10
09:00 AI IN HEALTH: CHALLENGES AND OPPORTUNITIES FOR ITS INCORPORATION IN MEXICO
Speaker: Héctor Valle, FunSalud
09:30 THE ACCESS EQUATION: INNOVATION DRIVING HEALTHCARE REACH
Moderator: Héctor Valle, FunSalud
Panelists: Karla Alcazar, Lilly Latin America
David Sánchez, AXA Mexico
Jaen Velázquez, Siemens Healthineers Mexico, Central America and the Caribbean
10:15 EMPOWERING HOSPITALS THROUGH TECH, AI
Moderator: Marcelo Cruz, Clinicasdelhombre.com
Panelists: Gustavo García, Skye Group
Elisa Hierro, Meeting Doctors
Omar Silerio, Hospitales puerta de Hierro
12:15 PERSONALIZED MEDICINE IN MEXICO: HARNESSING GENETICS FOR IMPROVED HEALTHCARE
Moderator: Alejandro Gaviño, Mexican Association of Human Genetics
Panelists: Jorge Meléndez, INMEGEN
Luis Alberto Vélez, Theranomics
Gustavo Rodríguez, NutriADN
13:00 USER-CENTRIC INNOVATION: DESIGNING TECHNOLOGY FOR BETTER HEALTHCARE OUTCOMES
Speaker: Ana Riquelme, AMID
Rafael López, Diagnostikare
Carlos Loyo, GE Healthcare Latin America
Gizela Sosa, Sofía
Nicolás Vega, INTrAMED
15:00 HANDS ON, NOT LEFT BEHIND: PREPARING HEALTHCARE TALENT FOR AI-POWERED PRACTICE
Moderator: Carla Calderón, Baker McKenzie Mexico
Panelists: Mauricio Peón, Medu
Manuel Ferrero, page Executive
Héctor Orellana, Medtronic
15:45 FROM PIPELINE TO PREVENTION: HOW PHARMA IS RESHAPING CHRONIC DISEASE CARE
Moderator: Gustavo Alcocer, oLIVArES
Panelists: Arturo de la Rosa, Gilead Sciences
Gabriela Allard, Mexican Association of Diabetes
Miguel Freire, Novartis Mexico
Emily Morris, Sanofi
16:30 CONNECTING HEALTH: DIGITAL INTEGRATION FOR A HEALTHIER MEXICO
Speaker: Patrick Devlyn, CCE
19:00 END OF MEXICO HEALTH SUMMIT 2025
AI IN HEALTH: CHALLENGES, OPPORTUNITIES IT BRINGS TO MEXICO
Mexico’s healthcare system is at a critical juncture, as the combination of underinvestment, population aging, and rising chronic diseases has created a complex environment that stands to affect millions. These circumstances make it urgent to address long-standing structural challenges, which could be done by leveraging new technologies such as AI to improve access, efficiency, and equity.
“If we do not incorporate new technologies, the challenge will become unsustainable. The world is moving toward digitalization. In healthcare, this means telemedicine and technologies that can serve remote areas of the country where specialists do not go”
Héctor Valle Executive President | FunSalud
system is fragmented and complex. IMSSBienestar adds even more complexity,” Valle says. Access disparities are stark: while residents of Mexico City or Guadalajara have relatively easier access, citizens in Morelia or Veracruz face significant barriers. “We do not have enough doctors; we do not have them in the right specialties; and we do not have them in the right places,” he adds.
“We are among the countries that invest the least in healthcare, and our life expectancy is not good. While Japan and Spain continue to advance, Mexico faces a much greater challenge,” says Héctor Valle, Executive president, FunSalud.
This underinvestment affects human resources, medical equipment, and hospital infrastructure. For example, the majority of endocrinologists are concentrated in Mexico City, Jalisco, and Nuevo Leon, leaving states such as Campeche, Tabasco, and Guerrero with fewer than six specialists each, says Valle. Hospital beds per capita remain far below oECD standards, and projected shortages by 2030 could become severe. “Mexico has one hospital bed for a large number of inhabitants, and by 2030 the shortage will be enormous. A single bed costs 1 million dollars; there is simply not enough budget to cover the need,” he adds.
Challenges extend beyond infrastructure. Chronic and cardiometabolic diseases and violence exacerbate the pressure on an already fragmented system. “our healthcare
Amid these challenges, technology offers significant opportunities. Valle highlighted the transformative potential of AI, telemedicine, genomics, and robotics. “AI can become a co-pilot for physicians: with patient data, it can help build clinical records and make use of unstructured information,” he says. remote consultations, virtual reality training, IoT-enabled monitoring, and 3D printing of medical devices can all accelerate care delivery and address geographic inequities. public-private partnerships, digital-first care models, and preventive interventions are central to these efforts.
Valle stresses the importance of systemic and collaborative approaches. “We must invest in both the public and private sectors, incorporating new technologies to reduce gaps and achieve greater equity,” he adds. Initiatives with international organizations such as the World Bank are underway to strengthen Mexico’s system and prepare for future pandemics.
Toward a New Healthcare Framework
Looking ahead, the focus is on leveraging technology to close access gaps and improve efficiency. By incorporating AI and digital tools, Mexico can implement models of care that are more preventive, data-driven, and patient-centered. public-private collaboration and increased investment are essential to scale these innovations effectively. “If we do not incorporate new technologies, the challenge will become unsustainable. The world is moving toward digitalization. In healthcare, this means telemedicine and technologies that
can serve remote areas of the country where specialists do not go,” says Valle.
The path forward requires both urgency and vision. By combining strategic investment,
innovation, and systemic reform, Mexico has the opportunity to redefine healthcare delivery, reduce inequities, and ensure a more resilient and sustainable system for the decades to come.
THE ACCESS EQUATION: INNOVATION DRIVING HEALTH CARE REACH
Mexico’s population is being burdened by underspending the healthcare system, which strains the finances of individuals. With high out-of-pocket expenses and uneven access across the country, innovation and collaboration are increasingly seen as key to bridging gaps in coverage and quality of care.
“There is innovation in Mexico, but equitable access remains a challenge. Innovation must be directed and adapted to meet the needs of patients,” says Jaen Velázquez, Director of Strategy and Business Development, Siemens Healthineers.
Healthcare in Mexico continues to carry a heavy financial burden for households. out-ofpocket costs in Mexico are more than double the oECD average. Between 2018 and 2024, out-of-pocket health spending rose 41.4%, with average quarterly household expenses increasing from MX$1,135 (US$60.79) to MX$1,605 (US$85.99), reports INEGI.
According to the Mexican Association of Insurance Institutions (AMIS), many families are now spending more than one month of their income on medical care, averaging over MX$9,500 (US$507). This financial pressure is compounded by low government spending, as Mexico invests only 5.4% of its GD p in healthcare, well below the oECD average of
9.2%. These challenges highlight the urgent need for public-private collaboration that expands access and strengthens healthcare delivery nationwide.
“Next year’s health budget appears likely to remain very challenging,” says Héctor Valle, president, FUNSALUD.
Expanding Access to Healthcare
Inequality, insufficient resources, and persistent public health issues continue to restrict coverage. However, the private sector can play a crucial role in expanding access, and its level of engagement will determine whether health systems remain reactive or evolve into resilient ones, according to the World Economic Forum. Its contributions can take many forms, acting as a funder, implementer, or innovator. Funding is particularly relevant in contexts with limited public budgets, such as Mexico.
In Mexico, public-private partnerships (ppp) have emerged as an important mechanism for advancing healthcare innovation. These collaborations not only enable the development of new products and services but also promote innovative approaches to organizational management and processes.
Different private sector stakeholders keep working to continue raising the level of care in Mexico. For example, Lilly Latin America has many years of experience in diabetes and is entering the field of obesity. The company is exploring alternative methods of administering GLp-1 medications beyond injectables, with the goal of achieving scalable production to reach a wider population, explains Karla Alcazar, president and General Manager, Lilly Latin America.
“There is innovation in Mexico, but equitable access remains a challenge. Innovation must be directed and adapted to meet the needs of patients”
Jaen Velázquez
Director
of Strategy and Business Development | Siemens Healthineers
“There is significant opportunity for publicprivate partnerships. We work to mobilize patients as early as possible to prevent them from reaching the healthcare system with high costs and to ensure they still have the possibility of being cured,” says Alcazar.
Insurance companies are also stepping up. “ o ur challenge is to create products that complement the system and support patients from the moment of diagnosis,” says David Sánchez, Director of Health Claims, AXA Mexico.
However, the private sector’s efforts alone are not sufficient as for medical innovation to reach patients, collaboration among all stakeholders in the healthcare ecosystem is essential, reports AMIIF.
The private sector is introducing a range of initiatives. Alcázar highlights the need for an ambitious continuing medical education plan to standardize knowledge, especially among primary care physicians. Meanwhile, Velázquez suggests launching pilot projects focused on Mexico’s most prevalent diseases to evaluate potential savings, always guided by data. Also, Sánchez stresses the importance of designing products that complement the public system, while promoting public policies for cost transparency and regulations to prevent malpractice.
“We need to find the spark that will allow us to transform the healthcare system,” says Valle.
EMPOWERING MEDIUM-SIZED HOSPITALS THROUG H TECH, AI
Medium-sized hospitals in Mexico must grapple with limited resources, growing chronic disease burdens, and uneven access to quality care. While AI could help to address these problems, its success depends on structured data, clear processes, and a focus on patient outcomes, warn industry leaders.
“AI is a term that is everywhere right now, and it will change the healthcare system,” says Marcelo Cruz, Co-CEo, Clinicasdelhombre. com. “But we must ground it in practical applications that expand access and reduce costs.”
regional pressures, including the expected doubling of the global population aged 60 and above by 2050, rising chronic disease prevalence, and projected healthcare worker shortages, are creating an urgent need for scalable and sustainable solutions that improve patient outcomes and operational performance. Furthermore, Mexico has only 2.4 doctors per 1,000 inhabitants — below the oECD average of 3.5 — and over half of the population lacks consistent access to medical services.
Technology can help. AI-enabled analytics can help to address these gaps by optimizing resource allocation and supporting preventive care initiatives, while EHrs facilitate real-time clinical decision-making and population-level health management. Digital tools, when integrated with value-based care models, provide actionable insights for hospitals to shift from service-volume-driven approaches to patient-outcome-focused strategies.
While AI adoption is growing, many AI projects fail without proper foundations. “There is a big myth around AI. Globally, 70% of projects have failed. To make it work, hospitals must first have structured data, defined processes, and an improved patient journey. only then can AI be implemented,” says Gustavo García, Chairman, Skye Group. He also explains that investment in AI is not a one-time expense but an ongoing effort.
The challenge in incorporating these technologies lies in agility and well-distributed funding, says omar Silerio, Director General, Hospitales puerta de Hierro. It is “fundamental
to have a Capex for medical equipment and for technology; it is fundamental to have them well allocated,” says Silerio. He also urges hospitals to move beyond transactional relationships with patients to a commitment that provides value to all parties.
“There is a big myth around AI. Globally, 70% of projects have failed. To make it work, hospitals must first have structured data, defined processes, and an improved patient journey. Only then can AI be implemented”
Gustavo García Chairman | Skye Group
prescriptions, pose significant challenges. According to García, the industry needs to look toward Mexican companies before reaching for expensive international solutions.
“Many Mexican healthtech companies have both the technology and the information. They must experiment with AI to see where it fits each clinic or hospital’s needs. Believe me, in Mexico, we will develop health technologies that can compete globally,” says García.
“We must be clear about the pillars: healthcare staff, patients, and then technology. Each is independent, but together they drive efficiency, reduce time, and lower costs,” says Elisa Hierro, Medical Director, MeetingDoctors. Hierro explains that technology can help to center care around patients, enabling easier access to information and preventive services. “For physicians, AI is useful to make processes more efficient, as long as it is a complement and not a substitute,” she adds.
Despite the potential benefits, mediumsized hospitals encounter multiple barriers to implementing digital solutions. Budgetary constraints, limited infrastructure, workforce shortages, and regulatory ambiguities, such as the partial recognition of digital
Cultural expectations among physicians and patients, along with skepticism toward digital tools, further complicate adoption. Successful implementation requires multi-stakeholder collaboration involving technology providers, government agencies, and academic institutions. Strategies to overcome these challenges include incremental digital integration, staff training, patient education programs, and robust regulatory frameworks to provide clarity on telemedicine and digital health compliance.
“To continue to innovate, we must change our mindset to focus on the objective of giving better prognoses to patients. That is the benefit, and budgets must be adjusted to implement technology accordingly,” says Silerio.
Hierro adds that strategy and education are essential for scaling. “You must have a clear strategy, implement only what is necessary, and complement it with training for all staff. It depends on the niche, but it is also about losing the fear of trying something new.”
PERSONALIZED MEDICINE: HARNESSING GENETICS FOR IMP ROVED CARE
Mexico stands at a pivotal moment in its healthcare evolution, with personalized medicine — also known as precision medicine — emerging as a transformative approach. By tailoring treatments to the genetic, molecular, and contextual characteristics of individual patients, this strategy has the potential to improve outcomes, reduce adverse effects, and optimize resource allocation. However, widespread adoption remains limited due to financial, regulatory, and infrastructure challenges.
“In recent decades, medicine has undergone significant transformations due to advances in genetics and biogenetics,” says Alejandro Gaviño, president, Mexican Association of Human Genetics. He adds that personalized medicine presents an innovative approach, aligning genetic, environmental, and contextual solutions to address high-prevalence diseases such as cancer, cardiovascular conditions, and diabetes.
Yet, healthcare in Mexico faces persistent financial pressures. Households shoulder much of the cost, as out-of-pocket expenses more than double the oECD average. These expenses also rose 41.4% between 2018 and 2024, according to INEGI. This dynamic underscores the challenge of ensuring equitable access to new technologies, including personalized medicine, which can
transform care delivery but also carries the risk of widening inequalities.
The global genomics market is projected to grow from an estimated US$44.21 billion in 2025 to more than US$175 billion by 2034, driven by sequencing technologies and AI integration. In Mexico, the market was valued at about US$480 million in 2023 and could exceed US$1.4 billion by 2030, supported by growth in precision oncology diagnostics and consumer genomics, says Jorge Meléndez, Director General, INMEGEN. He adds that ongoing efforts aim to develop platforms that integrate Mexican innovation and facilitate genomic diagnostics. These efforts include the sequencing Mexican patients and prenatal/pediatric screening to enable early diagnosis and prevent complications.
Institutions such as Hospital Universitario UANL, Centro Médico ABC, and Hospital Ángeles are already applying personalized immunotherapy treatments, setting a precedent for wider adoption. Meléndez also highlights the need to expand genetics specialist programs and strengthen bioinformatics capabilities to ensure the proper interpretation of genomic studies.
Tumor analysis, for example, enables the study and treatment of various types of cancer, says Luis Alberto Vélez, CEo and Founder, Theranomics. “Collaborations with private insurers have demonstrated tangible benefits: at least 30% of patients receiving molecularguided treatments show significantly improved overall survival,” he says. Vélez adds that the same genetic approaches applied to cancer can be adapted to manage chronic diseases, especially given Mexico’s rapidly aging population and low birth rates. He says that proactive and personalized medicine should become standard across both public and private sectors, and that multidisciplinary approaches must start from the first patient visit, particularly for rare and complex diseases.
“ p ersonalized and precision medicine can prevent up to 80% of the most common diseases through healthy lifestyle interventions,” says Gustavo rodríguez, CEo and Founder, NutriADN. In oncogenetics and prenatal medicine, timely diagnosis is essential, but prenatal testing is performed in less than 1% of Mexico’s population, compared to 40%–50% in the European Union, he adds.
Despite technological advances, barriers remain significant. Sequencing costs, bioinformatics interpretation, and specialized expertise requirements can make genomic testing prohibitively expensive. “Access and coverage considerations are critical. Catastrophic diseases require dedicated funds for unprotected patients, and molecular diagnostics can cost millions per patient per year,” says Vélez. regulatory agencies such as CoFEprIS and the FDA must balance speed of approval with patient safety, particularly for rare diseases, he adds.
Further intervention may be necessary to increase access. “Distributive justice in public healthcare is complex; expert panels and decentralized services are needed to maximize social impact,” says Meléndez. Collaborative approaches between government and private sector players can be critical to overcoming bureaucratic and regulatory barriers, maximizing the impact of innovation.
Mexico could have a bright future in precision medicine. With growing institutional support, technological platforms, and regulatory improvements, the country has the potential to become a regional hub for genomics and personalized care, particularly in oncology and chronic disease management. By integrating genetics into everyday medical practice, from preventive interventions to targeted therapies, Mexico can transition from reactive healthcare to proactive, personalized care, ensuring better outcomes and more efficient use of resources, say experts.
DESIGNING TECHNOLOGY FOR BETTER HEALTHCAR E OUTCOMES
Mexico faces a growing burden caused by chronic diseases and an aging population. To face it, the healthcare sector must focus on deploying user-centric innovation that prioritizes the needs of patients and health professionals, say experts. But for technology to be successful, it must be aligned with clinical objectives and the broader health ecosystem from the outset.
“Focusing on the user, primarily the physician, is key to maximizing the impact of healthcare innovations,” says Nicolás Vega, Head in Mexico, INTrAMED.
“It is essential that this technology remains usercentered, ensuring ease of use. Both academic institutions and medical professionals must be prepared to fully leverage its technological capabilities”
Carlos Loyo Commercial Director of Image Products | GE HealthCare
Despite the promise of technology, technology adoption in Mexico is limited by several challenges, including resistance to change among staff, budgetary constraints, and the complexity of integrating new systems with legacy infrastructure. “Mexico’s large, fragmented healthcare system, coupled with diverse population experiences, presents unique challenges for technology adoption,” says Ana riquelme, Executive Director, AMID.
Ensuring interoperability between platforms, safeguarding sensitive patient data, and training personnel to effectively use these tools requires careful planning. Successful implementation often depends on a phased approach, combining pilot programs with continuous monitoring and feedback. Hospitals must also develop clear protocols for data management and cybersecurity, while fostering a culture of collaboration between IT teams and clinical staff. partnerships with technology providers and local health authorities can further support integration and scale-up.
Furthermore, technology should serve as a tool to solve clinical problems rather than an end in itself, says rafael López, Founder, Diagnostikare. “Systematic involvement of patients and health professionals is crucial,” he adds, underscoring the need for continuous feedback loops in product design. López also highlights the necessity of a comprehensive evaluation framework for health technologies, citing the European Union as a benchmark. Trust, quality, and adoption are essential for successful implementation, while the Mexican market would benefit from a more mature regulatory framework.
To achieve this, both doctors and patients must be central to innovation. “It is essential that this technology remains user-centered, ensuring ease of use. Both academic institutions and medical professionals must
be prepared to fully leverage its technological capabilities,” says Carlos Loyo, Commercial Director of Image products, GE HealthCare.
Systemic thinking is also key to product development, says Gizela Sosa, Vice president of product, Sofía, noting that observation and careful analysis of the healthcare environment are critical for meaningful innovation. “When a new proposal or innovation is introduced, it must meet the needs of patients, achieve cost savings, and deliver clinical outcomes,” says Sosa. She also stresses the importance of international references and continuous knowledge sharing to improve solutions.
“Innovation extends beyond technology generation and requires focus on medical education, clinical collaboration, and prevention,” says Vega. He highlights the need for strategic information sharing and stronger alliances across the healthcare community to ensure technology reaches its full potential.
Experts agree that user-centric innovation in Mexico must balance accessibility, usability, and trust, while fostering collaboration across the healthcare ecosystem. Aligning technology with clinical objectives and strategic partnerships is crucial to improving healthcare outcomes nationwide.
PREPARING HEALTHCARE TALENT FOR AN AI-POWERE D PRACTICE
While Mexico’s medical schools graduate thousands every year, the country does not have enough doctors to meet the needs of its population. This shortage of skilled healthcare professionals leads to longer wait times, delayed treatments, and higher costs, eventually overburdening systems. Filling the gap in medical professionals requires a new approach. While AI has been touted as a tool to support clinical practices, it could also play a role in enhancing medical education, experts say.
As AI transforms healthcare across the world, Mexico faces a critical challenge: bridging the gap between traditional medical education and the skills required for the
modern, technology-driven practice, says Carla Calderón, Head of the Health and Life Sciences practice, Baker McKenzie Mexico.
Healthcare education in Mexico exists within a complex ecosystem, where universities and clinical environments must balance patient care with the training of future professionals. However, despite these efforts, structural challenges persist within the country’s medical workforce. In 2023, the country had nearly 666,000 medical professionals, with about 17,500 new doctors and 12,500 specialists entering the field annually. Yet, only about 2.5 doctors per 1,000 inhabitants are actively practicing, placing Mexico in the lower quartile among oECD countries.
“With these tools, professionals will have a better foundation to enter the industry. We must take a multidisciplinary approach, including social work, nursing, and administration, so healthcare services have all the necessary perspectives. Just as algorithms are constantly trained, so must our professionals be”
Mauricio Peón Technology Director | Medu
for Healthcare and Life Sciences, p age Executive. “Aligning expectations is key to closing the gap. In medical school, students are not trained to manage a company, lead a team, or build a budget, yet those skills are increasingly necessary.”
Furthermore, the number of specialists being trained falls short of demand, says Héctor o rellana, Vice p resident for North Latin America, Medtronic. “We train between 1,800 and 2,000 physicians per year in some specialties, and it is probably not enough,” says o rellana. “There has to be a general alignment in education to truly improve people’s lives. We must constantly intervene to remain at the forefront and enhance the patient experience. Training has to happen within companies and hospitals.”
This limited availability of active practitioners and educators directly contributes to a shortage of skilled healthcare professionals, which has tangible consequences. p atient care is affected through longer wait times and delayed treatments, while marginalized communities face heightened disparities in access to quality care, reports Adecco. Hospitals incur higher costs due to reliance on temporary staff and overtime, and overburdened systems struggle to implement new technologies and innovate in care delivery.
“A recent graduate has to walk a tightrope without the safety net of real-world preparation,” says Manuel Ferrero, partner
AI offers a pathway to address these gaps. From enhancing diagnostics and preventive care to enabling remote surgeries, AI holds transformative potential. To realize this potential, healthcare professionals need early exposure to AI during their training and curricula must change to include digital health from the start, says Mauricio peón, Technology Director, Medu.
“There should be modules on AI, digital innovation, and simulations early in medical education,” says p eón. “With these tools, professionals will have a better foundation to enter the industry. We must take a multidisciplinary approach, including social work, nursing, and administration, so healthcare services have all the necessary perspectives. Just as algorithms are constantly trained, so must our professionals be.”
Mexico allocates a smaller percentage of GDp to health compared to oECD members, making collaboration between the private and public healthcare sectors essential, says Ferrero. “partnerships can be fostered through programs, but what is really needed is a public policy agenda that responds to people’s needs,” he adds.
paradoxically, new doctors also face limited opportunities, says peón. “In 2024, only 41% of graduates secured placements,” he adds. “We must train better-prepared physicians who can contribute real value to Mexican institutions. A wave of opportunities is coming with digital tools, but preparation will be decisive.”
“The real issue is not whether patients exist, but whether we are ready to treat them,” o rellana says. “Talent remains the cornerstone, and we must ensure tools are used ethically to develop better healthcare professionals.”
FROM PIPELINE TO PREVENTION: PHARMA RESHAPES CHRONIC DI SEASE CARE
Chronic diseases represent a significant health and economic challenge for Mexico’s healthcare system. Conditions such as diabetes, hypertension, cardiovascular disease, and mental health disorders affect millions of individuals and place substantial pressure on both public and private healthcare systems. Despite ongoing efforts, gaps remain in access, continuity of care, and effective disease management, and traditional pharmaceutical approaches focused solely on drug development are proving insufficient to address these complex, long-term challenges.
“personalization in the treatment of chronic diseases is the frontier we want to reach,” says Gustavo Alcocer, partner and Co-Chair Life Sciences Group, oLIVArES. But to do so, regulatory bottlenecks must be avoided to ensure innovations reach patients quickly.
“We need to leverage digitalization for regulatory dossiers in order to accelerate access to innovation,” he adds.
“Many patients abandon new medical devices because they do not find them sustainable or rewarding. We need to create materials in different languages and formats to reach communities on their own terms”
Gabriela Allard Vice President Latin America | Mexican Association of Diabetes
p harmaceutical companies in Mexico are adopting innovative solutions to tackle complex challenges. Mature medicines with proven efficacy are being strategically deployed to maintain continuity of care, particularly in underserved regions, through both government initiatives and private distribution networks. Meanwhile, emerging technologies — including AI, biomarker-driven research, and advanced drug discovery platforms — are accelerating the development of targeted therapies for chronic and complex conditions.
Digital tools are playing a growing role in transforming chronic care, says Emily Morris, Head Latin America and General Manager p harma Mexico, Sanofi. She adds that AI is revolutionizing patient identification, enabling more precise and personalized treatments.
Digital health solutions can enable continuous monitoring, personalized treatment plans, and actionable insights that improve adherence and outcomes, but access remains a central issue. “When we look at what is happening in the world, there is a significant gap. What could happen in Mexico if these therapies were available?” says Miguel Freire, president, Novartis Mexico. He adds that prevention and primary interventions must be strengthened through publicprivate collaboration, especially for rural and vulnerable communities.
p atient behavior is a key determinant of outcomes. “The doctor can prescribe, but the result is in the hands of the patient. It has been proven that the simpler the treatment, the better the results,” says Arturo de la rosa, Vice president Latin America, Gilead Sciences. In Brazil, for example, preventive innovation led to a 5% drop in mortality from heart attacks in 2013, adds de la rosa.
For that reason, innovation must be paired with education and accessibility, says Gabriela Allard, p resident, Mexican Association of Diabetes. “Many patients abandon new medical devices because they do not find them sustainable or rewarding. We need to create materials in different languages and formats to reach communities on their own terms.” Furthermore, in Mexico, access to technology and therapies often remains a privilege rather than a standard, she adds.
Looking ahead, the trajectory of chronic disease care in Mexico points toward a fully integrated ecosystem that bridges therapeutic development with prevention and real-world impact. p harmaceutical companies are positioned to lead this transformation by scaling proven solutions: maintaining access to mature medicines, expanding the adoption of digital health tools, advancing precision drug discovery, and implementing preventive interventions at the population level.
The next generation of chronic disease care will likely be defined less by individual technologies and more by the healthcare ecosystem’s ability to deliver inclusive, effective, and sustainable innovation. “Consumers are increasingly empowered, sustainability-focused, and looking for personalization. If it only takes one click, even better,” says Alcocer.
MEXICO’S HEALTH SYSTEM FACES CHALLENGES, DIGITAL OPP ORTUNITIES
Mexico’s health system faces significant challenges, but new opportunities in digital integration, clinical research, and innovation could strengthen its ability to serve a growing population, according to p atrick Devlyn, president of the Health Commission, CCE.
“If we connect healthcare, we connect Mexico, and a healthier Mexico will undoubtedly be a stronger, more productive country, one that enables higher levels of well-being for its population,” says Devlyn.
Fragmentation remains one of the main challenges affecting the healthcare system, with separate structures such as IMSS, ISSSTE, INSABI, SEDENA, and SEMA r operating independently. This lack of coordination, combined with unequal access between urban and rural areas, limited interoperability across institutions, and a persistent digital divide, has hindered efficiency and patient care.
Despite the gaps, Mexico’s demographic and technological context offers potential. With a population of nearly 130 million people, including a relatively young segment rapidly adopting digital tools, the country is positioned to leverage health innovation, says Devlyn. private sector startups, multinational companies and academic institutions are contributing to an expanding healthcare ecosystem.
r ecent government initiatives, including steps toward regulating telehealth and electronic health records, signal growing interest in digital health. Lessons from the pandemic underscored the value of
integrated systems, with countries that connected health information platforms and worked closely with private partners achieving stronger responses and saving more lives, says Devlyn.
A digitally connected health system could allow patient information to move securely across facilities, reducing duplicate tests, speeding up diagnoses, lowering costs, enabling early prevention, and supporting better planning of public health policies.
Telemedicine and hybrid care models could expand access to isolated communities, while data analytics and AI could improve prevention and early diagnosis while guiding evidence-based public policy.
However, interoperability standards are necessary to ensure hospitals, pharmacies, laboratories, insurers and other actors can securely share information, says Devlyn.
Collaboration between the public and private sectors is essential, as neither has the resources to tackle the challenge alone, says Devlyn. But by combining regulatory authorities, telecom providers, pharmaceutical firms, private hospitals, startups, academia and civil society, Mexico could build a health system that is more resilient and equitable.
“Mexico has an opportunity to make a significant leap forward by leveraging existing private-sector technologies and connecting them with the public sector to benefit patients,” says Devlyn.
His call to action emphasizes investment in innovation, modern regulation, adoption of digital tools by healthcare professionals, and stronger partnerships. Connecting the country’s health system could ultimately strengthen Mexico’s economy, productivity, and social well-being.