Volume 59 | No. 3 | September 2021
Time to introduce mentorship into surgical training programmes?
Surgery in South Africa – challenges and barriers
Editor Prof. J E J Krige
Deputy Editors Prof. E Panieri
Surgery in South Africa – the attitudes toward mentorship in facilitating general surgical training
Prof. S R Thomson
Emeritus Editors
Prof. C G Bremner
Surgical rib fixation as an alternative method of treatment for multiple rib fractures: an audit of results compared with traditional medical management

Prof. M R Q Davies
Prof. G J Oettlé
The spectrum of blunt abdominal trauma in Pietermaritzburg
The correlation between full moon and admission volume for penetrating injuries at a major trauma centre in South Africa
Manuscript Supervisor Sue Parkes, Department Medical School, York Tel. (011) 717-2080
E-mail: susan.parkes@wits.ac.za
An analysis of paediatric snakebites in north-eastern South Africa
An audit of patients clinically deemed as high risk for malignant breast pathology at the Helen Joseph Hospital Breast Clinic
The surgical burden of breast disease in KwaZulu-Natal province
Associate Editors J P Apffelstaedt, Stellenbosch
P C Bornman, UCT E Degiannis, Wits A Dhaffala, Transkei R S du Toit, Bloemfontein
D Kahn, UCT
An audit of patients presenting with clinically benign breast disease to the Helen Joseph Hospital Breast Imaging Unit
Clinicopathological spectrum of small bowel obstruction and management outcomes in adults – experience at a regional academic hospital complex
T E Madiba, Natal T Mokoena, Pretoria M D Smith, Wits M G Veller, Wits B Warren, Stellenbosch
The spectrum of abdominal wall desmoid fibromatosis and the outcomes of its surgical treatment
_____________
Published by the HEALTH & MEDICAL
A 7-year retrospective review of renal trauma in paediatric patients in Johannesburg
Editor-in-Chief Janet Seggie
Diabetes and lower extremity amputation – rehabilitation pathways and outcomes at a regional hospital
Factors affecting bacteriology of hand sepsis in South Africa
Cardiac tamponade following post-pericardiotomy syndrome

An inguinal hernia imposter
Deputy Editor Bridget Farham
Editorial Systems Manager Melissa Raemaekers
Scientific Editor
Ingrid Nye
The role of surgery in Conn’s syndrome – a case of refractory hypertension secondary to an aldosterone secreting adenoma
Biliary tract anatomical variance – the value of MRCP
Technical Editors
Emma Buchanan
Paula van der Bijl
Head of Publishing
Robert Arendse
Production
Bronlyne Granger
Art Director
Brent Meder
DTP,
Carl Sampson
&
Edward Macdonald
Head of Sales and Marketing
Diane Smith

Volume 52 | No. 4 | November 2014
Coordinator
Setting
Layout
Manager
Distribution
91 Developing a clinical model to predict the need for relaparotomy in severe intra-abdominal sepsis secondary to complicated appendicitis V Y Kong, S van der Linde, C Aldous, J J Handley, D L Clarke 96 Exposure to key surgical procedures during specialist general surgical training in South Africa 101 An audit of trauma-related mortality in a provincial capital in South Africa N B Moodley, C Aldous, D L Clarke 105 Propeller flaps for lower-limb trauma 108 Regional anaesthesia for cleft lip surgery in a developing world setting V Malherbe, A T Bosenberg, A K Lizarraga Lomeli, C Neser, C H Pienaar, A Madaree 111 Haemangiopericytoma/solitary fibrous tumour of the greater omentum J H R Becker, M Z Koto, O Y Matsevych, N M Bida 114 Largest recorded non-invasive true intrathoracic desmoid tumour G R Alexander 116 The mystical foot with pink mushrooms: Imaging of maduromycosis –a rarity in southern Africa G Jackson, N Khan 118 Isolated gallbladder perforation following blunt abdominal trauma S Cheddie, C G Manneh, N M Naidoo OBITUARY 120 Hamid Ismail Yakoob D Kahn
CONTENTS
ISSN 0038-2361
Official Journal of the Association of Surgeons of South Africa ORIGINAL, PEER-REVIEWED CLINICAL RESEARCH
Granisetron Fresenius 1 mg/ml (1 ml)

Granisetron Fresenius 1 mg/ml (3 ml)
Concentrate for solution for injection/infusion
INDICATIONS: For the prevention or treatment of nausea and vomiting induced by cytostatic therapy (chemotherapy and radiotherapy) and for the prevention and treatment of post-operative nausea and vomiting.1

Identifies Granisetron Fresenius1
For full prescribing information refer to professional information approved by the South African Health Products Regulatory Authority.
S4 GRANISETRON FRESENIUS 1 mg/ml (1 ml): 44/5.7.2/0671 S4 GRANISETRON FRESENIUs 1 mg/ml (3 ml): 44/5.7.2/0672


Reference: 1. Fresenius Kabi data on file.
Fresenius Kabi South Africa (Pty) Ltd, Reg. No.: 1998/006230/07 Stand 7, Growthpoint Business Park 162 Tonetti Street, Halfway House Extension 7, Midrand, Gauteng, 1685 PO Box 4156, Halfway House 1685 Tel: + 27 11 545 0000

Fax: + 27 11 545 0060
www.fresenius-kabi.co.za
IMA_13_3_2021_V1
Identifies the location of a small cut to help breaking/ opening the ampoule1
IN STOCK
EDITORIAL
74 Time to introduce mentorship into surgical training programmes? J Edge
GENERAL SURGERY SURVEYS
77 Surgery in South Africa – challenges and barriers
P Naidu, I Buccimazza
82 Surgery in South Africa – the attitudes toward mentorship in facilitating general surgical training
P Naidu, I Buccimazza
TRAUMA
86 Surgical rib fixation as an alternative method of treatment for multiple rib fractures: an audit of results compared with traditional medical management
BI Monzon, LM Fingleson, MS Moeng
90 The spectrum of blunt abdominal trauma in Pietermaritzburg
P Rhimes, S Moffatt, VY Kong, JL Bruce, MTD Smith, W Bekker, GL Laing, DL Clarke
94 The correlation between full moon and admission volume for penetrating injuries at a major trauma centre in South Africa
VY Kong, AA Keizer, MM Donovan, RD Weale, NS Rajaretnam, JL Bruce, A Elsabagh, DL Clarke
97 An analysis of paediatric snakebites in north-eastern South Africa
JJP Buitendag, S Variawa, D Wood, G Oosthuizen
BREAST DISEASE
102 An audit of patients clinically deemed as high risk for malignant breast pathology at the Helen Joseph Hospital Breast Clinic
H-M Brink, G Rubin, C-A Benn, S Lucas
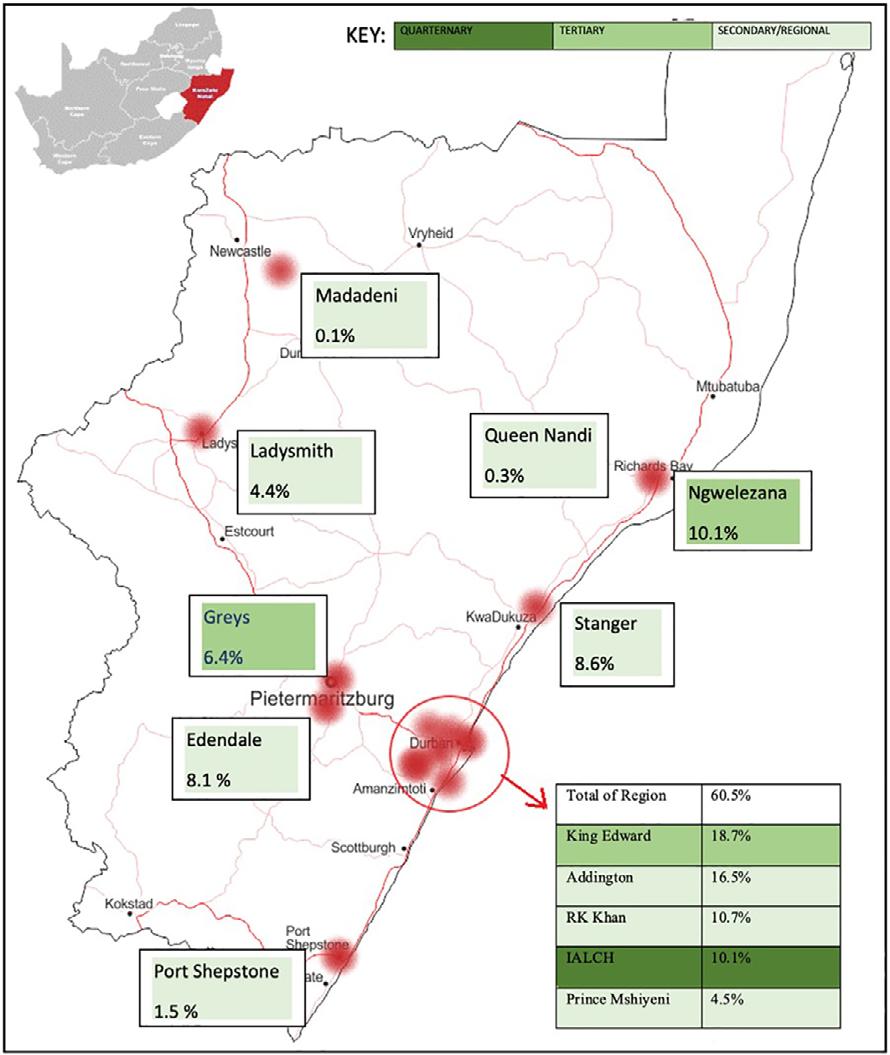
108 The surgical burden of breast disease in KwaZulu-Natal province
VU Ehlers, CF Kohler, E Lutge, A Tefera, DL Clarke, I Buccimazza
113 An audit of patients presenting with clinically benign breast disease to the Helen Joseph Hospital Breast Imaging Unit
NC Christofides, G Rubin, C-A Benn
GENERAL SURGERY
118 Clinicopathological spectrum of small bowel obstruction and management outcomes in adults – experience at a regional academic hospital complex
MR Mthethwa, C Aldous, TE Madiba
124 The spectrum of abdominal wall desmoid fibromatosis and the outcomes of its surgical treatment
I Bombil, L Ngobese
ARTICLES ONLINE
127 A 7-year retrospective review of renal trauma in paediatric patients in Johannesburg

NZ Mashavave, A Withers, T Gabler, V Lack, D Harrison, J Loveland
128 Diabetes and lower extremity amputation – rehabilitation pathways and outcomes at a regional hospital
P Manickum, SS Ramklass, TE Madiba
129 Factors affecting bacteriology of hand sepsis in South Africa
M van der Vyver, A Maderee
CASE REPORTS ONLINE
130 Cardiac tamponade following post-pericardiotomy syndrome
K Gandhi, JSK Reinders, PH Navsaria
130 An inguinal hernia imposter
RR Patel, S Tu, J Plaskett
131 The role of surgery in Conn’s syndrome – a case of refractory hypertension secondary to an aldosterone secreting adenoma
MD Carides, NT Sishuba, I Bombil, C Christofides
131 Biliary tract anatomical variance – the value of MRCP
C Ferreira, CB Noel
132 CPD
Editor Prof. S R Thomson
Deputy Editors
Dr I Buccimazza
Prof. E Panieri
Emeritus Editors
Prof. C G Bremner
Prof. M R Q Davies
Prof. G J Oettle
Prof. J E J Krige
Manuscript Supervisor
Susan Parkes (Secretariat), Association of Surgeons of South Africa
E-mail: susanparkes@mweb.co.za
Associate Editors
Prof. D Clarke
Dr T Hardcastle
Prof. E Jonas
Prof. P Navsaria
Prof. A J Nicol
Publisher
Medical and Pharmaceutical
Publications (Pty) Ltd. trading as
Production
Robyn Marais
Ina du Toit
Chandré Blignaut
Layout
Celeste Strydom
Sales
Asnath Masogo
Cell: 079 413 0119
E-mail: asnath@medpharm.co.za
Plagiarism is defined as the use of another’s work, words or ideas without attribution or permission. No manuscript which includes plagiarised material will be considered for publication in the SAJS. For more information on our plagiarism policy, please visit http://www.sajs.org.za
No.
September
Volume 59 |
3 |
2021 meeting expectations
https://doi.org/10.17159/2078-5151/2021/v59n3a3753
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]
http://creativecommons.org/licenses/by-nc-nd/4.0
Time to introduce mentorship into surgical training programmes?
J Edge
Division of Surgery, Stellenbosch University, South Africa
Corresponding author, email: dr@jennyedge.co.za
I didn’t realise it, but as a junior doctor working in New Zealand, I had the privilege of having my first mentor. She was an older woman, Dr Ira, a radiologist from Sri Lanka. At the time, I was working as the only female in the department of general surgery and battling with my male colleagues. After a particularly bruising incident, I went down to see her to complain. She gave me advice I have never forgotten. She introduced me to silence as a reply. It is a powerful weapon. You never regret what you haven’t said. It gives you space to contemplate the situation and eventually formulate a reply.
In 2020 the Association of Surgeons of South Africa (ASSA) sent out a questionnaire to all its members. The results have been published in two articles written by Naidu and Buccimazza and published in this edition of the SAJS. The first addresses challenges and barriers to pursuing a career in surgery in South Africa.1 The second article elucidates the attitudes toward mentorship among South African general surgeons.2 One hundred and twenty-nine respondents took part in the study overall. The majority (67%) were specialist surgeons and 18% registrars. Over half (53%) reported having suffered from burnout.1 Fiftyfour per cent reported not having a mentor, however, 80% felt mentorship is an important part of surgical training.2
The results of burnout are similar to those reported in other international studies. In a meta-analysis evaluating burnout amongst physicians in the USA, an estimated 67% reported having had symptoms.3 In 2019, the results from a questionnaire sent to all surgical trainees in the USA were published in NEJM.4 They asked about the incidence and source of abuse and discrimination, symptoms of burnout, and frequency of events. Ninety per cent experienced symptoms of burnout in the preceding year; 38.5% reported experiencing symptoms of burnout within the preceding week. There was an increased incidence of burnout amongst trainees who were subject to discrimination and harassment. Interestingly, the major source of most categories of abuse and discrimination was from patients and patients’ families.
As part of a quality improvement process in the Division of Surgery, Stellenbosch University, we conducted a similar anonymous survey in 2019 and 2020. Approximately 20 trainees responded. Specific questions about burnout were not asked but they were asked about incidents of discrimination and verbal abuse and their source. They also reported that the most common source of abuse and discrimination was from patients and their families. They were asked to indicate what the department could do to support them. The introduction of mentoring programmes was amongst the most popular options chosen.
The word mentor was first introduced by Homer in the 8th century in his epic poem the Odyssey. In the poem, Mentor was a friend of Odysseus. When Odysseus was called to war, he asked Mentor to take over the care of his son. And so, the concept of mentoring was formed. There are varied definitions of mentoring, and it can be applied in different ways. Naidu and Buccimazza describe the goal of a mentorship programme “to support and guide individuals through career and leadership development”.1 Programmes can be introduced on a one-to-one basis or can be run in groups. Many informal initiatives exist within surgical departments, however, the problem with having an informal structure is that extrovert registrars tend to benefit more than introverted registrars.
Whilst watching tennis, the surgeon Atul Gawande asked himself “If Rafael Nadal has a coach, how come lawyers and teachers and journalists don’t? Specifically, how come surgeons don’t”.5 Coaching is a self-directed process that is ongoing and facilitated by a trained instructor. Although there are identifiable goals, there are no measurable parameters. In that way, coaching and mentoring are similar.
Most surgical departments in South Africa are unlikely to be able to afford a formal coaching programme. However, why hasn’t there been widespread adoption of formal membership programmes within surgical training? There are many reasons cited. The most common objections are from the senior staff within the department. Generally, the people who would be mentors. I believe it is true to say that more attention is paid to the burnout rate among surgical trainees than to that among senior colleagues. There is a perception that adding a mentoring programme in a department adds to their work. Importantly, the study that was done by Naidu and Buccimazza demonstrates that senior surgeons recognise the importance of mentorship programmes and that they too experience burnout.
The fact we work in a resource-constrained setting with exceptionally high trauma volumes places extra burden on all surgeons. COVID-19 has diminished access to health care for our patients and there is a perception that we are all seeing surgical patients with more advanced disease. Although the survey done in our department was too small to claim a causal link to COVID-19, a higher percentage of trainees reported incidences of verbal abuse in 2020 compared to 2019.
There are many tools that can be used for educational purposes. Teaching, mentoring, and coaching are the most employed techniques worldwide. Ubuntu is an African concept that has been used to good effect in selected
74 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
038-2361
The
EDITORIAL
ISSN
© 2021
Author(s)
South African Journal of Surgery.
2021;59(3):74-76
BREAK OUT OF THE PAIN LIVE AGAIN. STILPANE
• Relief of short-term pain associated with anxiety and tension

• Effective in acute and post-operative pain treatment1


• Available in tablets (with caffeine) and capsules (without caffeine)
• Capsules are more suitable for CV or GI sensitive patients as it does not contain caffeine2,3

• Trusted, Affordable, Effective Relief1

CV: cardiovascular; GI: gastrointestinal References: 1. Outhoff K, Dippenaar JM, Nell M, et al. A randomised clinical trial comparing the analgesic and anxiolytic efficacy and tolerability of Stilpane® and Tramacet® after third molar extraction. SA J Anesthes Analg 2015; 21(2): 40-45. 2. Temple JL, Bernard C, Lipshultz SE, et al. The safety of ingested caffeine: A comperehensve review. Front Psych 8:80.doi: 10.3389/fpsyt.2017.00080. 3. Tavares C, Sakata RK. Caffeine in the treatment of pain. Revista Brasileira de Anestesiologia 2012; 62(3): 387-401. S5 STILPANE Tablets. Reg. No.: M/2.9/2. Each tablet contains paracetamol 320 mg, codeine phosphate 8 mg, caffeine anhydrous 32 mg, meprobamate 150 mg. S5 STILPANE Capsules. Ref. No.: B624 (Act 101/1965). Each capsule contains paracetamol 320 mg, codeine phosphate 8 mg, meprobamate 150 mg. For full prescribing information, refer to the professional information approved by the medicines regulatory authority (Tablets 11/1979, Capsules 03/1969). Trademarks are owned by or licensed to the Aspen Group of companies. © 2020 Aspen Group of companies or its licensor. All rights reserved. Marketed by Aspen Pharmacare for Pharmacare Limited. Co. Reg. No.: 1898/000252/06. Healthcare Park, Woodlands Drive, Woodmead, 2191. ZAR-CCM-07-20-00001 07/20. STEP OUT OF THE PAIN.
circumstances.6 The conventional modality utilised to train a surgeon is teaching with assessment by specialist exit exams. Teaching or training is a formal structured process whereby an individual learns specific skills. There is generally a curriculum that is followed and once the competence has been achieved, the process is complete. Atul Gawande looked for excellence in sport to form his opinion about the need for alternative education modalities that could be implemented to help the process of training a good rather than an ordinary surgeon.
Some of the barriers to choosing a surgical career in South Africa have been illustrated by this local questionnaire. If, as a profession, we are going to be able to continue recruiting bright medical trainees, train them and help them develop the resilience needed for a lasting career, we need to involve them in both identifying problems and working towards solutions. Group mentorship programmes are one way of achieving both: getting suggestions from the “shop floor” and being able to provide guidance and support.7 The survey carried out by ASSA is a move in the right direction.
One of the attributes of mentoring is that the mentee may choose their mentor. It may happen informally, as it did to me, and may or not be a person from an aligned profession. There is no doubt that my career path has been altered by the sage words from my mentor, Dr Ira. It behoves all of us in our profession to move on from simply being a teacher and to integrate the principles of mentoring and coaching into our daily surgical practice.
REFERENCES
1. Naidu P, Buccimazza I. Surgery in South Africa – challenges and barriers. S Afr J Surg. 2021;59(3):77-81. https://doi. org/10/17159/2078-5151/2021/v59n2a3391.
2. Naidu P, Buccimazza I. Surgery in South Africa – the attitudes toward mentorship in facilitating general surgical training. S Afr J Surg. 2021;59(3):82-85
3. Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians. A systematic review. JAMA. 2018;320(11):1131-50. https://doi.org/10.1001/jama.2018. 12777.
4. Hu Y-Y, Ellis RJ, Brock Hewitt D, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381(18):1741-52. https://doi.org/10.1056/ NEJMsa1903759.
5. The New Yorker 2013. Available from: https://www. newyorker.com/video/watch/atul-gawandedo-surgeons-needcoaches. Accessed 19 Jul 2021.
6. Clutterbuck DA, editor. Case studies of mentoring across the globe, part 1V. The SAGE Handbook of Mentoring. 1st ed. Chapter 31. SAGE.
7. Henry-Noel N, Bishop M, Gwede CK, Petkova E, Szumacher E. Mentorship in medicine and other health professions. J Cancer Educ. 2019;34(4):629-37. https://doi.org/10.1007/ s13187-018-136.
76 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
South African Journal of Surgery. 2021;59(3):77-81
https://doi.org/10.17159/2078-5151/2021/v59n3a3391
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]


http://creativecommons.org/licenses/by-nc-nd/4.0
Surgery in South Africa – challenges and barriers
P Naidu,1 I Buccimazza2
1 Department of Surgery, Faculty of Medicine and Health Sciences, University of Cape Town, South Africa
2 Department of Surgery, Faculty of Health Sciences, University of KwaZulu-Natal, South Africa
Corresponding author, email: pnaidu2012@gmail.com
Background: Sustaining a surgical career can be challenging and there are numerous barriers to pursuing a career in surgery. These barriers and challenges are well reported in international literature, but there is a lack of knowledge on how this affects surgeons in South Africa. This study aimed to determine the barriers and challenges that South African surgeons face in their training and careers.
Methods: A 15-item questionnaire was designed and distributed via the Research Electronic Database Capturing software from 1 February–3 April 2020. Data were analysed in Stata 15 SE. All responses were anonymised.
Results: One hundred and twenty-nine participants responded to the questionnaire, 33 (26%) of whom were female. The majority were specialist surgeons (n = 87; 71%). One hundred and eleven participants (90%) reported they did not regret pursuing surgery. Barriers to pursuing surgery included limited personal time (n = 98; 76%), heavy surgical workload (n = 92; 71%), and difficulty taking leave of absence (n = 64; 50%), limited postgraduate training (n = 34; 26%), and verbal discouragement (n = 22; 17%). Challenges included difficulty maintaining work-life balance (n = 74; 56%), racial discrimination (n = 29; 23%) and gender discrimination (n = 15; 12%). Fifty-three per cent of participants experienced burnout.
Conclusion: Despite high career satisfaction, South African surgeons face numerous barriers to pursuing and challenges in sustaining a career in surgery and often experience burnout. These barriers and challenges disproportionately affect female surgeons and can be mitigated through formalised mentorship programmes, flexible work schedules, funding for postgraduate training, and training in diversity and discrimination.
Keywords: surgery, training, challenges, barriers
Appendix 1 available online: http://sajs.redbricklibrary.com/index.php/sajs/article/view/3391
Introduction
A career in surgery, while rewarding, is known to be highly competitive and demanding.1,2 The surgical work environment is challenging and fraught with mistreatment, which presents barriers to pursuing and difficulty in sustaining a surgical career.2
Reported challenges in the surgical workplace include discrimination on the basis of gender, race, pregnancy or childcare status; verbal, emotional, and physical abuse; sexual harassment; duty-hour violations; and genderbased salary discrepancies.3 These challenges perpetuate emotional and physical exhaustion and often deter medical students and junior doctors from pursuing a career in surgery.4 Overwhelming time commitments, lack of worklife balance, and disruption of personal life have all been cited as reasons for burnout, a common phenomenon among surgeons and surgical trainees.3,5 Nearly half the surgical resident workforce in the United States of America (USA) has reported burnout and one in 20 have reported suicidal ideation as a result of these workplace challenges.3,6,7 In sub-Saharan Africa, the demand on a surgical career is substantial owing to the high burden of surgical disease and lack of providers.8,9 These challenges may adversely affect the well-being of both patient and provider.10 In addition to
burnout, surgeons often neglect their physical, spiritual and emotional health, and fail to seek medical attention following occupational injuries.10,11 Among female surgeons, higher rates of pregnancy complications and infertility have been reported.12
A surgical career can be particularly challenging for women who have to balance work schedules with pregnancy and motherhood, and work in a traditionally male-dominated field which can sometimes be hostile and unaccommodating.13 Female surgeons experience greater discrimination than their male counterparts, have greater barriers to pursuing a surgical career, and fewer opportunities for career advancement, particularly with respect to academia.13,14
While challenges such as long work hours and poor worklife balance are common across both genders, South African female surgeons face unique challenges. In a study by Roodt, one-third of participants, mostly male surgeons, felt that an increased number of female surgeons complicated or disrupted the departmental routine and the majority perceived males to be better suited to a career in surgery than females.4 Apart from this single-centre study in the Western Cape, there is a paucity of literature on the challenges of a surgical career among South African surgeons and trainees.
77 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
ISSN 038-2361
SURGERY SURVEY
© 2021 The Author(s) GENERAL
The primary objective of this study was to evaluate the challenges of and barriers to pursuing a career in surgery amongst all surgical cadres throughout South Africa. A secondary objective was to establish whether some of these challenges and barriers are unique to female surgeons.
Methods
A 15-item questionnaire was designed on the Research Electronic Database Capture platform and included questions on both barriers to pursuing a career in surgery and challenges of a surgical career (as detailed in Appendix 1). The questions in the survey were informed by questions asked in previous studies, however, the survey was not a validated questionnaire or tool. Both male and female participants were asked questions on barriers and challenges, including questions on discrimination. The survey was circulated electronically to qualified general surgeons who are members of the Association of Surgeons of South Africa (ASSA) and/or Surgicom, and general surgical trainees/ medical officers through the various heads of surgical departments. Respondents could access the survey from 1 February–3 April 2020. Data were analysed in Stata 15 SE. All responses were anonymised and no identifying data were analysed. The ASSA committee approved the questionnaire for dissemination to its members. Ethical approval for this study was obtained (information removed for blinding). Descriptive analyses were performed as proportions, means and medians. Measures of association were performed
using chi-squared tests. A p-value < 0.05 was considered statistically significant.
A specialist surgeon was defined as any surgeon who had qualified with a specialist degree in any surgical specialty and was currently employed as a consultant.
78 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Definitions
Characteristics n (%) Gender Male 96 (74%) Female 33 (26%) Age 20–29 8 (6%) 30–39 36 (28%) 40–49 25 (19%) > 50 60 (47%) Marital status Married 94 (73%) Single 14 (11%) Non-marital relationship 10 (8%) Divorced 10 (8%) Other 1 (1%) Training/practice location Western Cape 42 (33%) Gauteng 41 (32%) KwaZulu-Natal 24 (19%) Free State 8 (6%) North West 5 (4%) Eastern Cape 3 (2%) Limpopo 3 (2%) Northern Cape 2 (2%) Mpumalanga 1 (1%)
Table I: Demographic characteristics of respondents (n = 129)
Position Specialist surgeon 87 (71%) Registrar 23 (19%) Fellow 8 (7%) Medical officer in surgery 5 (4%) Number of years in practice (median; IQR) 18 (10–28) Sub-specialty No 76 (66%) Yes 39 (34%) Type of subspecialty Colorectal 9 (23%) Gastroenterology 7 (18%) Breast and endocrine 5 (13%) Hepatobiliary 4 (10%) Trauma 3 (8%) Vascular 3 (8%) Bariatrics 1 (3%) Paediatric surgery 1 (3%) Transplant 1 (3%) Not specified 5 (11%) Type of post Full-time public 53 (43%) Full-time private practice 40 (33%) Part-time public with RWOPs 8 (7%) Full-time private with public sessions 7 (6%) Part-time public 4 (3%) Employed abroad 2 (2%) Limited private practice 2 (2%) Other (retired/supernumerary/lecturer) 7 (14%) Reason for choosing surgery as a career *participants were allowed to selected multiple options Technical aspect 69 (53%) Acute element of surgery 66 (51%) Inspired by role model 49 (38%) Academic competitiveness 18 (14%) Prestige 8 (6%) Family pressure 2 (2%) Other 13 (10%) Regret choice to pursue surgery? No 111 (90%) Yes 12 (10%)
Table II: Surgical career characteristics of respondents (n = 129)
Results
One hundred and twenty-nine participants responded to the survey, 33 (26%) of whom were female and 60 (47%) were over the age of 50 years (Table I). The majority of respondents (84%) were from the Western Cape, Gauteng, and KwaZulu-Natal. Specialist surgeons accounted for 71% of the responses (n = 87) and the median number of years in practice was 18 (IQR 10–28) (Table II). Most respondents were in full-time public practice (n = 53; 43%). The desire to pursue a surgical career was informed by a variety of reasons: technical aspect of surgery (n = 69; 53%), acute element of surgery (n = 66; 51%), inspired by a role model (n = 49; 38%), academic competitiveness (n = 18; 14%), prestige of surgery (n = 8; 6%), or family pressure (n = 2; 2%).
Many candidates perceived the demands of surgery, including a lack of personal time (76%), heavy workload associated with surgery (71%), and difficulty taking leave of absence (50%), as potential barriers to a surgical career (Table III). More than half of the participants reported a lack of personal time to spend with family or for outside interests. Specific barriers to training included limited opportunities for postgraduate training (26%) and the cost of training (9%), as well as verbal discouragement (17%) and a lack of mentorship (11%).
Unique challenges of a surgical career related to a lack of a work-life balance (57%), with 53% of participants reporting burnout. Specialist surgeons were more likely to experience burnout than any other position, although not statistically significant (p = 0.06). Other challenges related to a hostile work environment, including negative experiences with colleagues and discrimination and abuse of varying forms (Table IV). More participants reported negative experiences with male colleagues than with female colleagues (p = 0.02). In addition to challenges, candidates also suggested aspects that would facilitate surgical training, including formalised mentorship programmes (49%), scholarships or funding to pursue postgraduate surgical training (47%), and more flexible work schedules (36%) (Table IV).
Discrimination
Both males and females were asked to report if they believed gender discrimination was a challenge in their surgical career; gender discrimination was reported as a challenge among 15 out of 33 females (45%) and zero out of 96 males (0%). Females were more likely than males to pursue surgery if inspired by a role model (p = 0.007) or due to family pressure (p = 0.015). With respect to barriers to pursuing a surgical career, 45% of females (n = 15) reported gender discrimination and were more likely than males to experience verbal discouragement (p < 0.001). Females more than males reported limited time to have a child (p = 0.002). Additionally, females were also more likely to report sexual harassment than males (p < 0.001). Female surgeons reported unique challenges including having to impersonate male qualities to toughen up (n = 11; 33%), not being treated equally to their male colleagues (n = 15; 45%), and a hostile culture toward females (n = 9; 27%).
Other forms of discrimination and abuse included racial discrimination (n = 29; 23%), physical abuse (n = 15; 12%), and sexual harassment (n = 7; 5%).
There were statistically significant differences in challenges reported by males compared with females
(Table IV). While these challenges were reported by both males and females, female participants were more likely to report gender discrimination (p < 0.001), sexual harassment (p < 0.001), impersonating male colleagues to toughen up, not being treated equally to male colleagues (p < 0.001), and a hostile culture toward females (p < 0.001).
79 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Table III: Barriers to pursuing a career in surgery (n = 129) Limited personal time 98 (76%) To spend time with family 83 (64%) For outside interests 70 (54%) To date/marry 19 (15%) To have a child 13 (10%) Surgical workload 92 (71%) Difficulty taking leave of absence 64 (50%) Limited postgraduate training 34 (26%) Verbal discouragement 22 (17%) Discouragement by male colleague 15 (68%) Discouragement by female colleague 7 (32%) Family aspirations 11 (9%) Gender-based 11 (9%) Age 3 (2%) Other 6% Cost of training 11 (9%) Lack of mentors 14 (11%) Other (race/lack of experience/work environment) 10 (8%) Table IV: Challenges of a career in surgery (n = 129) Challenge Difficult work-life balance 74 (57%) Burnout 68 (53%) Negative experience with colleagues 47 (36%) Racial discrimination 29 (23%) Gender discrimination 15 (12%) Physical abuse 15 (12%) Sexual harassment 7 (5%) Impersonating male colleagues to toughen up 11/33 (33%) Not treated equally to male colleagues 15/33 (45%) Hostile culture toward females 9/33 (27%) No challenges 9 (7%) Negative experience with Both 26 (57%) Male colleague 18 (39%) Female colleague 2 (4%) Facilitation of surgical training Mentorship programme 76 (59%) Postgraduate surgical training scholarships 61 (47%) Part-time surgical training programmes 46 (36%) Other (flexible training programmes, appropriate cover of maternity leave, better working hours) 17 (13%)
The 12 candidates (10%) who regretted their career choice did not face more gender discrimination (p = 0.154) or racial discrimination (p = 0.903) than those who did not regret their career choice.
Discussion
Our study highlights that substantial challenges and barriers exist within surgical training in South Africa. Burnout was reported among more than half of the participants. Challenges related to the demanding nature of a surgical career, heavy workloads and long hours, having limited personal time, and the lack of a work-life balance were most commonly reported. These challenges can further be exacerbated by bullying in the surgical environment which has previously been documented and defined as persistent negative behaviour or aggression, and is often experienced more by women.15,16 In our study, 17% of participants were verbally discouraged from pursuing a career in surgery, mostly by male colleagues and 36% of participants reported a negative experience, both of which can be considered as bullying. This form of mistreatment can be mitigated through training focused on professionalism.
In addition to bullying, other forms of discrimination were reported by our participants and can make sustaining a career in surgery difficult. Nearly one-quarter of participants experienced racial discrimination and 12% reported gender discrimination, forms of mistreatment also reported in international literature.15,17 Challenges and barriers were reported by both genders, but some were unique to and more common among females; for example, the need to emulate masculine qualities and a hostile culture toward females. Five per cent of participants experienced sexual harassment, and while this is lower than international literature,15 women reported sexual harassment more than men. Nearly half the female respondents reported gender-based discrimination and not being treated equally to their male colleagues. Additionally, female surgeons found having a child to be more challenging than males. The survey did not capture other forms of discrimination, such as religious or ethnic discrimination. These would be important to explore in more detail in future studies.
Despite these challenges, 90% of participants were satisfied with and did not regret their career choice. This is consistent with findings from previous studies.1,5,18 Some of the reported benefits of a surgical career in our study included job satisfaction, making a difference, and financial stability. While this study did not report the proportion of surgeons who wished to leave surgical practice, previous US-based studies have shown that despite high career satisfaction, one in four surgeons were considering leaving surgery on the basis of work-schedule demands and limited personal time.1
In comparison to a study published in the USA among residents, fewer South African residents reported gender discrimination (31.9% in the US versus 21.7% in our South African study), fewer reported physical, verbal and emotional abuse (30.3% in the US versus 17.4% in our South African study), yet more residents in South Africa reported burnout (60.9%) in comparison to USA residents (38.5%).3 Similarly, in internal medicine, a study conducted by the American College of Physicians reported that 51.3% of female physicians reported gender discrimination, which is higher than that reported among our female cohort.19 In a study evaluating perceptions among residents in obstetrics
and gynaecology, 40.6% of women and 2.9% of men reported gender discrimination, in comparison to our South African study in which 45% of female participants and 0% of male participants experienced gender discrimination.20 The challenges described in this study are not new or unique to South Africa or to the field of surgery; they are a global phenomenon and often disproportionately affect female surgeons.1,5 However, mitigating these challenges and barriers requires context-relevant local solutions. In South Africa, this could necessitate the restructuring of surgical training, including: i) a formalised mentorship programme; ii) programmatic changes that facilitate surgical training, such as scholarship opportunities for postgraduate training and part-time or more flexible work schedules; and iii) specific training in awareness of discrimination and accepting diversity in the discipline, particularly with respect to the mistreatment and challenges experienced by female surgeons.
Mentorship in surgery is gaining traction globally.21 Formalised mentorship programmes have been reported to aid job satisfaction and retention, facilitate career development, increase opportunities to engage in academia with respect to research and education, and improve technical skills and confidence.21,22 The goal of mentorship is to support and guide individuals through career and leadership development. The role of a mentor in career development can be substantial, allowing for expansion of professional network and providing a new personal or clinical perspective. Mentorship could be beneficial with regards to providing advice on how to achieve a work-life balance, or how to deal with or report discrimination. With a shortage of experienced faculty, the advent of online learning platforms and technology has proven to be useful in linking mentors and mentees.23,24 Exemplary role models who encourage diversity and inclusivity are crucial in changing the current hostile culture and biases in surgery. Previous studies have shown that medical students considering a career in surgery are more likely to be influenced by a positive role model than those who do not have such an influence.25 In our study, women were more likely to be inspired by a positive role model to pursue a career in surgery than men. Furthermore, access to career and academic opportunities were important motivators for choosing a career in surgery.26-28 Mentors can play an important role in career development, both in the academic and clinical settings. One-quarter of participants expressed there were limited opportunities for postgraduate training. More than half reported that mentorship programmes would facilitate surgical training. Further studies are required to address the value of mentorship and how this can be leveraged to create a more sustainable, inclusive, and safe environment for surgeons and surgical trainees, especially for women in surgery.
A study in the USA found that male surgeons were significantly less likely to encourage female medical students to pursue a career in surgery.1 In our study, females were more likely to experience verbal discouragement compared to their male colleagues, and this was cited as a barrier to pursuing a surgical career. This overt and implicit discouragement needs to be addressed if we are going to increase diversity and opportunities for minority groups, such as females, in the field of surgery.1,2 In recent years, there has been an increasing number of female medical students, with some medical schools reporting a female majority.29 If we continue to foster an environment that is
80 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
hostile toward women in surgery, we will perpetuate the shortage of surgeons that currently exists.2,8
Furthermore, our study reported statistically significant differences in the challenges reported by males compared with females. Female participants were more likely to report gender discrimination, sexual harassment, impersonating male colleagues to toughen up, being treated unfairly compared with male colleagues, and a hostile culture towards female surgeons.
Professor Boffard, a world-renowned trauma surgeon and a past president of the International Society of Surgery, has been pioneering the way forward for female surgeons, being one of the first to recognise the need for and to implement part-time surgical training. These flexible work schedules are designed to “make surgery more attractive, particularly to women, who now consist of 60% of all medical graduates but only 5% of surgeons”.29 However, in Johannesburg, more than half the surgeons are female and creating an environment that fosters gender equity is essential.29 More flexible work schedules will not only benefit female surgeons, but male surgeons too. The majority of our participants were male, and the majority reported that the surgical workload was a challenge to sustaining a career in surgery. Furthermore, more than half the participants reported burnout. The Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) Trial, conducted in the USA, has paved the way for the discussion on flexible work schedules in international literature, reporting that more flexible work schedules can decrease the notoriously high surgical workload, and assist in greater job satisfaction and career retention.30,31
South African surgical training lacks postgraduate programmes, mostly pertaining to fellowship opportunities. One-quarter of participants identified this as a challenge and nearly half reported a need for these programmes to facilitate surgical training. Postgraduate research fellowship grants and scholarships are available but limited, however not nearly as scarce as clinical fellowships.26-28 The ASSA Trust plans to source private funding to support fellowship posts. There is further opportunity to engage corporates, societies, and other organisations to fund postgraduate surgical fellowships, thereby encouraging continued learning in the field of surgery.
While our study focused mostly on gender discrimination, there is an opportunity to incorporate the value of diversity and the meaning of professionalism into formalised training curricula and to create a platform for both trainee and faculty surgeons to express their opinions, concerns, and suggestions about discrimination in the surgical workplace. By building intentional platforms for engagement into training, we will not only create awareness about any form of discrimination, but also help to decrease the biases in surgery. Non-technical skills are becoming increasingly important in surgical training and have been shown to facilitate cultural diversity and improved surgical outcomes.32,33 These existing platforms could be expanded to include training on the value of other types of diversity, including gender, ethnic and racial diversity.
Study limitations
This study was limited by its methodological design. The questionnaire was limiting, providing only quantitative answers. A mixed-methodology study design would have provided even more valuable and substantial information regarding the challenges of and barriers to a surgical career
in South Africa. Additionally, this study was limited by the poor response rate, meaning that results are not necessarily generalisable to the entire South African surgical community. Despite these challenges, this study provides initial insight into the existing barriers to and challenges of a surgical career in South Africa. However, future studies should address the limitations discussed in this study.
Conclusion
This study highlights the numerous barriers to and challenges of surgical career in South Africa. More than half the South African surgeons who participated in this study experienced burnout. While barriers to pursuing and challenges in sustaining a surgical career are reported by both male and female surgeons, some inordinately affect females. Despite these challenges, career satisfaction was reported to be high among the overwhelming majority of surgeons. Encouraging sustainability of a surgical career requires addressing the barriers and challenges that exist. Potential solutions include formalised mentorship programmes, facilitating surgical training through postgraduate funding and flexible work schedules, and integrated training on discrimination and diversity. With increasing interest in medicine among females, the gender profile of medical school and postgraduate surgical training is changing. To address the shortage of surgeons, surgical work environments and training programmes need to adapt to reduce burnout and encourage inclusivity and diversity, especially among females.
Acknowledgement
We extend our gratitude to the steering committee of ASSA who enhanced the survey by their input, the ASSA secretariat for circulating it widely to the target audiences, and to all those who completed the survey.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Disclaimer
This survey was initiated by and conducted under the auspices of the Association of Surgeons of South Africa (ASSA).
Ethical approval
Ethical approval for this study was obtained from the University of KwaZulu-Natal Biomedical Research Ethics Committee (protocol number: BREC/00002259/2020).
ORCID


P Naidu https://orcid.org/0000-0002-1112-9606
I Buccimazza https://orcid.org/0000-0002-5399-3101
REFERENCES
1. Mahoney S, Strassle P, Schroen AT, et al. Survey of the US surgeon workforce – practice characteristics, job satisfaction, and reasons for leaving surgery. J Am Coll Surg. 2020 Mar;230(3):283-93. https://doi.org/10.1016/j. jamcollsurg.2019.12.003
Full list of references available on request.
81 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
South African Journal of Surgery. 2021;59(3):82-85
https://doi.org/10.17159/2078-5151/2021/v59n3a3597
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]


http://creativecommons.org/licenses/by-nc-nd/4.0
©
ISSN 038-2361
Surgery in South Africa – the attitudes toward mentorship in facilitating general surgical training
P Naidu,1 I Buccimazza2
1 Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
2 Department of Surgery, Inkosi Albert Luthuli Hospital, KwaZulu-Natal Department of Health, South Africa
Corresponding author, email: pnaidu2012@gmail.com
Background: There are many barriers to pursuing a surgical career in South Africa, some of which are unique to females. Mentorship has been proposed as a solution to mitigate these barriers. The value of mentorship has not been formally assessed among South African general surgeons and trainees.
Methods: The study was part of a larger study designed to assess barriers to pursuing a career in surgery, including the value of mentorship. A 15-item questionnaire was designed and distributed via the Research Electronic Database Capture from 1 February 2020–3 April 2020. Data were analysed using Stata 15 SE. All responses were anonymised.
Results: One hundred and twenty-nine (13.5%) of 955 potential participants responded to the survey of which 26% (33/129) were female. Sixty-seven per cent of respondents were specialist surgeons (87/129). Seventy per cent (90/129) of participants reported having a role model in surgery, however, 66% (86/129) reported they had no mentor in surgery. 107/129 (83%) participants reported the importance of mentorship. The need for a formalised mentorship programme to facilitate surgical training was recorded by 60% (78/129) of participants, while 18% (23/129) reported the need for a mentorship group specifically for females.
Conclusion: Eighty-three per cent of participants reported the importance of mentorship however two-thirds lacked a mentor. Most participants advocated for a mentorship group to facilitate surgical training. Establishing formalised mentorship programmes could mitigate the barriers to pursuing a surgical career.
Keywords: surgery, training, barriers, mentorship
Appendix 1 available online: http://sajs.redbricklibrary.com/index.php/sajs/article/view/3597
Introduction
Surgery is a highly competitive specialty and a particularly challenging learning environment.1 Barriers to pursuing a career in surgery include heavy workload, poor worklife balance, verbal discouragement, and limited options for postgraduate surgical training. These barriers can lead to low interest to pursue a surgical career choice. Challenges identified in the surgical workplace include, among others, verbal, physical and emotional abuse, long working hours, and lack of time for commitments outside of surgery.1,2 Challenges in the surgical workplace have led to burnout, physical and emotional exhaustion, and even attrition of surgeons. Some of these challenges are unique to female surgeons, such as limited time to plan a family and gender discrimination in the workplace.3 There is an increasing number of female doctors in medicine, yet a disproportionately low number of women in surgery. In South Africa, 60% of medical students are female, however, only five per cent are surgeons.4 The under-representation of women in surgery is evident at all levels including in academic and leadership positions.5,6
Mentorship has been gaining traction in the field of surgery and can be an important way to mitigate challenges
of and barriers to pursuing a surgical career. Mentorship has been defined as a “two-way relationship and type of human development in which one individual invests personal knowledge, energy and time in order to help another individual grow and develop and improve to become the best and most successful they can be.”7 Mentors can be important facilitators of the entrance of young doctors, particularly female doctors, into the field of surgery.8 Mentors can also play an important role in a mentee’s career satisfaction and development, particularly in academia, and aid in the retention of surgeons.9
While evaluation of mentorship in surgery has been increasingly reported in the literature from high-income countries, such as the United States, there is a paucity of literature on the value or perceptions of mentorship in lowand middle-income settings, such as South Africa.1,9
The primary objective of this survey was to determine the value of mentorship among South African general surgeons. The secondary objectives of this study were to determine the proportion of participants that felt a formalised mentorship programme for surgical trainees in general and women in particular was needed.
82 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
2021 The Author(s) GENERAL SURGERY SURVEY
Methods
This was a cross-sectional survey conducted using a 15item questionnaire (Appendix 1) which was designed and distributed via the Research Electronic Database Capture (REDCap) software (version 8.1.13, Vanderbilt University). The survey was developed by both authors, the senior author being a surgical sub-specialist, and included questions on challenges and barriers to pursuing a career in surgery, as well as the attitudes and perceptions of mentorship in facilitating surgical training. These questions were adapted from previously published studies.1-3,9 Questions on the value of mentorship were single-answer choice questions except for the question on methods to facilitate surgical training, where participants were allowed to select multiple answers. The questions on the value of mentorship were analysed using Stata 15 SE. The survey was circulated to qualified general surgeons who are members of the Association of Surgeons South Africa (ASSA) or Surgicom, as well as to general surgical trainees through their heads of department. The survey was conducted over a two-month period from 1 February 2020 to 3 April 2020. All responses were anonymous, and no identifying data were included. Descriptive analysis of the data was performed using measures of dispersion (means and median).
Results
One hundred and twenty-nine (13.5%) out of 955 general surgeons and trainees approached to participate, responded to the survey. Seventy-four per cent (96/129) were male and 47% (60/129) were older than 50 years of age (Table I). Sixty-seven per cent (87/129) of participants were consultant surgeons with a median of 18 years (IQR 10–28) post-fellowship experience. Twenty-three (18%) of the participants were registrars in surgical training and the median number of years in training was two years (IQR 1–3).
Fifty-three per cent of participants (69/129) reported having a role model in their lives and 70% (90/129) reported the presence of a role model in surgery (Table II). This role
model in surgery was a senior colleague in 60% (78/129) of cases.
Fifty-four per cent (70/129) did not have a mentor; of these 61% (43/70) felt they lacked mentorship and would have liked to have had a mentor for their career development. Eighty-four per cent (36/43) of the mentees had a male mentor and 68% (29/43) had two or more mentors. Fortyfour per cent (57/129) reported having a mentee with 56% (32/57) having both male and female mentees.
Eighty-three per cent of the participants (107/129) reported that they felt it was important to have a mentor (Table III).
83 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Characteristics Gender n = 129 Male 96 (74%) Female 33 (26%) Age n = 129 20–29 8 (6%) 30–39 36 (28%) 40–49 25 (19%) > 50 60 (47%) Position n = 129 Consultant 87 (67%) Fellow 8 (6%) Medical officer in surgery 5 (4%) Registrar 23 (18%) Unspecified 6 (5%) Median number of years post-fellowship (IQR) 18 (10–28) Median years in registrar training (IQR) 2 (1–3)
Table I: Demographic characteristics
Male (n = 96) Female (n = 33) n = 129 Presence of a role model in life Yes 55 14 69 (53%) No 31 13 44 (34%) No response 10 6 16 (13%) Presence of role model in surgery Yes 65 25 90 (70%) No 21 2 23 (18%) No response 10 6 16 (12%) Who is your role model Senior colleague 62 16 78 (60%) Other (family member/none) 18 5 23 (18%) Peer 6 6 12 (9%) No response 10 6 16 (13%) Presence of a mentor Yes 28 15 43 (33%) No 58 12 70 (54%) No response 10 6 16 (12%) Gender of mentor n = 43 Male 26 10 36 (84%) Female 0 2 2 (5%) Both 2 3 5 (12%) Number of mentors per respondent n = 43 1 11 3 14 (32%) 2 9 8 17 (40%) 3 or more 8 4 12 (28%) Presence of a mentee n = 129 Yes 42 15 57 (44%) No 44 12 56 (43%) No response 10 6 16 (13%) Gender of mentee n = 57 Male 16 3 19 (33%) Female 2 4 6 (11%) Both 24 8 32 (56%)
Table II: Presence of role models and mentors
Table III: The value of mentorship as reported by participants
differences.8 While mentorship has often been regarded as a casual relationship, recent literature argues that mentorship should be cultivated in surgical programmes as this is an important method of teaching both technical and nontechnical skills.8,12 Formalised mentorship programmes are becoming increasingly important globally for their ability to address mentor time constraints, increase confidence and interest in surgical careers among medical students,13 and increase satisfaction of the mentorship environment among surgical trainees.11 A recent study in the United Kingdom reported that 83% of participants (surgeons in various surgical specialties) were willing to undergo formal mentorship training to increase the number of qualified mentors and improve effective mentorship.14 However, formalised mentorship programmes require involvement of the surgical department and the academic institution to ensure success.9
Numerous organisations, including the College of Surgeons of East, Central, and Southern Africa, have established formalised mentorship groups specifically for female surgeons in all specialties.15 These dedicated groups for women in surgery have helped to improve retention of female surgeons in the field by increasing academic and leadership opportunities and providing support for challenges that are unique to female surgeons.15,16 A 2017 study reported that same-sex mentorship was preferred among females and could positively influence career choice and address barriers to pursuing surgery, advocating for the development of national mentorship programmes in the United States.17 Our study showed that 45% of female participants had a mentor, and an overwhelming majority (84%) of mentors were male, which could be explained by the male-dominated nature of surgery in South Africa but also suggests a lack of female mentors.
The need for a formal mentorship group for all surgeons was recommended by 60% (78/129) of the participants, whereas 18% (23/129) reported the need for a group to specifically support female surgeons; 16 out of the 23 (70%) respondents were female.
Discussion
Our survey shows that South African general surgeons and trainees perceive the need for mentorship in surgery. Eightythree per cent of participants regarded the presence of a mentor as important, yet two-thirds did not have a mentor in surgery. Sixty per cent of participants reported that a mentorship programme would facilitate surgical training and a similar amount further reported the need for a formalised mentorship group for all surgeons.
Mentors can play a role in aiding retention of surgeons and increasing career satisfaction by creating a supportive environment that cultivates learning, advice on how to mitigate stress and decrease barriers to pursuing surgical careers, particularly for female doctors.10 Surgical trainees in orthopaedics who had mentors reported significantly higher job satisfaction and career development than those without mentors.11 There are several barriers to effective mentorship which include time constraints, generational and cultural differences, scarcity of qualified mentors and gender
Nearly two-thirds of participants in the current study reported the need for a mentorship group for all surgeons and 70% of female respondents reported the need for a dedicated group to support female surgeons. Despite this, there is no published data as to whether South African academic institutions have formal mentorship programmes in general or for females specifically and if they are effective. Even in institutions that have established these programmes, there is no data on their effectiveness. We believe it should be a priority to establish formalised mentorship programmes in surgical training programmes whilst at the same time devising metrics to assess their value.
It is recognised that there are several inherent limitations and challenges associated with surveys. There was a relatively low response rate, and the study sample was not representative of all regions and academic institutions in South Africa despite constant communication and reminders to encourage survey completion. Being embedded in a larger questionnaire meant that for simplicity of completion mostly single-answer responses were used. As a result, we were unable to do a more qualitative assessment of some responses; for example, reasons why respondents felt it is important to have a mentor or what aspects the respondents felt they lacked in their training that could be improved by being mentored.
Despite these limitations, over 80% of the South African general surgeons and surgical trainees who participated in
84 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Conclusion
Male Female Total Important to have a mentor? n = 129 Yes 82 25 107 (83%) No 3 2 5 (4%) Missing 11 6 17 (13%) Perceived lack of mentorship (if no mentor) n = 70 Yes 30 13 43 (61%) No 14 13 27 (39%) Facilitation of surgical training n = 129 Mentorship programme 57 19 76 (59%) Postgraduate surgical training scholarships 50 11 61 (47%) Part-time surgical training programmes 36 10 46 (36%) Other (flexible training programmes, appropriate cover of maternity leave, part-time post graduate training, better working hours) 15 2 17 (13%) Is there a need for a mentorship group for all surgeons? n = 129 Yes 56 22 78 (60%) No 6 4 10 (8%) Unsure 34 7 41 (32%) Is there a need for a group to support female surgeons? n = 129 Yes 7 16 23 (18%) No 20 7 27 (21%) Unsure 50 3 53 (41%) Missing 18 8 26 (20%)
the study valued mentorship and 60% felt there was a need for a formal mentorship programme to facilitate surgical training.
Conflict of interest
The authors declare no conflict of interest.
Funding source
No funding was required.
Disclaimer
This survey was initiated by and conducted under the auspices of the Association of Surgeons of South Africa (ASSA).
Ethical approval
Ethical approval for this study was obtained from the University of KwaZulu-Natal Biomedical Research Ethics Committee (protocol number: BREC/00002259/2020).
ORCID


P Naidu https://orcid.org/0000-0002-1112-9606
I Buccimazza https://orcid.org/0000-0002-5399-3101
REFERENCES
1. Mahoney ST, Strassle PD, Schroen AT, et al. Survey of the US surgeon workforce – practice characteristics, job satisfaction, and reasons for leaving surgery. J Am Coll Surg. 2020;230(3):283-93.e1.
2. Hu Y-Y, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381(18):1741-52.
3. Roodt L. Female general surgeons – current status, perceptions and challenges in South Africa. A pilot study at a single academic complex. University of Cape Town; 2016.
4. Boffard K. SA trauma expert to head world body. S Afr Med J. 2010;100:144-5.
5. Cochran A, Elder WB, Crandall M, et al. Barriers to advancement in academic surgery – views of senior residents and early career faculty. Am J Surg. 2013;206(5):661-6.
6. Cochran A, Hauschild T, Elder WB, et al. Perceived genderbased barriers to careers in academic surgery. Am J Surg. 2013;206(2):263-8.
7. Flaherty J. Coaching – evoking excellence in others. 2nd ed. Development and Learning in Organizations. Taylor & Francis Ltd; 2006.
8. Entezami P, Franzblau LE, Chung KC. Mentorship in surgical training – a systematic review. Hand. 2012;7(1):30-6.
9. Kibbe MR, Pellegrini CA, Townsend CM, Helenowski IB, Patti MG. Characterisation of mentorship programmes in departments of surgery in the United States. JAMA Surg. 2016;151(10):900-6.
10. Welch JL, Jimenez HL, Walthall J, Allen SE. The women in emergency medicine mentoring programme – an innovative approach to mentoring. J Grad Med Educ. 2012;4(3):362.
11. Flint JH, Jahangir AA, Browner BD, Mehta S. The value of mentorship in orthopaedic surgery resident education – the residents’ perspective. JBJS. 2009;91(4):1017-22.
12. Holt GR. Idealised mentoring and role modeling in facial plastic and reconstructive surgery training. Arch Facial Plast Surg. 2008;10(6):421-6.
13. Drolet BC, Sangisetty S, Mulvaney PM, Ryder BA, Cioffi WG. A mentorship-based preclinical elective increases exposure, confidence, and interest in surgery. Am J Surg. 2014;207(2):179-86.
14. Sinclair P, Fitzgerald J, Hornby S, Shalhoub J. Mentorship in surgical training – current status and a needs assessment for future mentoring programmes in surgery. World J Surg. 2015;39(2):303-13.
15. McCarthy MC. The Association of Women Surgeons – a historical perspective 1981 to 1992. Arch Surg. 1993;128(6):633-6.
16. Odera A, Tierney S, Mangaoang D, Mugwe R, Sanfey H. Women in surgery Africa and research. Lancet. 2019;393(10186):2120.
17. Faucett EA, McCrary HC, Milinic T, et al. The role of samesex mentorship and organisational support in encouraging women to pursue surgery. Am J Surg. 2017;214(4):640-4.
85 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
https://doi.org/10.17159/2078-5151/2021/v59n3a3463
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]



http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361
Surgical rib fixation as an alternative method of treatment for multiple rib fractures: an audit of results compared with traditional medical management
BI Monzon,1 LM Fingleson,2 MS Moeng3
1 Trauma Unit, Steve Biko Academic Hospital, University of Pretoria, South Africa
2 Sunninghill Hospital Acute Care and Major Injuries Unit, South Africa
3 Trauma Unit, Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, South Africa
Corresponding author, email: bignaciomonzon@gmail.com
Background: Rib fractures are a common cause of morbidity and chronic pain, delaying return to normal activities. Reports suggest that surgical fixation improves acute and long-term outcomes.
Method: A single centre retrospective review of multiple rib fractures, comparing the outcomes of cases managed using surgical fixation with cases managed only with best medical therapy (BMT) over 2 years.
Results: Thirty-five patients with rib fractures were admitted over the study period. The most common causes of rib fractures were motorcycle crashes (34.2%) and falls (31.4%). Fourteen patients had surgery. There were no differences between the two groups regarding the number of fractured ribs, injury severity score (ISS), ICU or hospital length of stay. The median numeric pain visual analogue scale (VAS) on admission was eight points for non-ventilated patients. In the surgical group the median VAS significantly fell to a median of 2 points in the first 24 hours after surgery (p = 0.04). Only two out of 25 major complications were directly attributable to the surgery for rib fixation. Patients managed without surgery needed significantly longer time to return to normal activities compared to those who had surgery (median 7 weeks versus 3 weeks, p = 0.03).
Conclusions: Our preliminary results suggest that rib fixation should be considered a treatment alternative in patients with multiple rib fractures.
Keywords: rib fractures, surgical fixation, flail chest, trauma
Introduction
Rib fractures are common and causations are multifactorial; they are a recognised marker for severity of injury and a significant cause of in-hospital morbidity, chronic pain, and delays in return to normal activities.1-3 The number of ribs fractured, presence of flail segment, patient age, associated lung trauma and extra thoracic injuries, especially traumatic brain injury are predictors of outcome.1-10
The current standard of care for rib fractures is nonoperative and is based on several key components. These include appropriate oxygenation, management of respiratory failure with mechanical ventilation, lung re-expansion techniques, appropriate management of pain, removal of secretions and aggressive chest physiotherapy.1-10
Unfortunately, non-operative management addresses only the pathophysiological component of this problem, while the mechanical and anatomical problems (actual fractures) are usually overlooked and treated with options that are not designed to facilitate bone consolidation.
The impact of rib fractures on prolonged disability is usually greater than traditionally expected; chronic pain is considered to be present in 22% of cases (could be as high as
59%) and some form of disability in 53% of cases 6 months after injury.10-22
Attempts to provide rigidity to the chest wall in the event of fractures is not a new proposition, multiple techniques have been used along the years to achieve stability with variable success.
Efforts to advance the surgical fixation of flail chest and multiple rib fractures to the level of standard of care have not met the expectations or received the approval of many surgeons, mostly due to lack of appropriate evidence and familiarity with the procedures.11
Evidence in favour of surgical stabilisation of rib fractures has been limited by the quality of the studies as with other trauma related issues,11-20 however, the accumulated evidence both from randomised clinical trials and from the systematic reviews and metanalysis consistently favours rib fixation over medical management.1,12-26
This mounting experience points to significant advantages such as the reduced incidence of pneumonia and respiratory failure, shorter ventilation time, shorter ICU and hospital stay with minimal complications as well as faster return to productive life, all of which result in improved quality adjusted life-years and costs.1,12-26
86 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
© 2021 The Author(s) TRAUMA
Journal
South African
of Surgery. 2021;59(3):86-89
At our institution, all patients with rib fractures were admitted to a trauma ICU ward and offered the standard of care as per protocol of the unit, including intravenous analgesia; oxygen, nebulised bronchodilators as needed, mechanical ventilation when indicated, management of associated injuries and active physiotherapy. A computed tomography scan (CT) of the chest was obtained and three-dimensional (3-D) volume reconstructions performed to evaluate the thoracic skeleton and assess indication for surgery.
As per unit protocol, a follow-up visit was scheduled at two weeks interval after discharge in all cases to clinically assess pain level, physical and pulmonary functionality and obtain chest radiographies to exclude residual pulmonary problems and in the surgical cases to evaluate the fracture site and implant complications. Once the patients re-incorporated to normal activities, they were considered discharged and advised to return for consultation if a problem or concern arose.
Only patients who have three or more rib fractures, or a flail chest with severe pain, as assessed by numeric visual analogue scale (VAS) higher than 6 points, fracture displacement, pulmonary contusion or inability to tolerate physiotherapy are considered for fixation at our institution.
The aim of study was to compare outcomes between subjects with multiple ribs fractures who received surgical rib fixation, and those who only received best medical therapy (BMT).
Method
Retrospective study from 1 July 2015 to 31 August 2017 (a 25-month period).
Inclusion criteria
All trauma patients presenting with multiple fractured ribs at a level 2 private trauma centre in Johannesburg.
Exclusion criteria
Subjects < 18 years of age, incomplete clinical data, associated severe traumatic brain injury (GCS < 8), major spinal injuries, those with predominantly posterior fractures not amenable to surgical options, and those who have mild symptoms and are able to participate fully in physiotherapy care.
Data collected
The following information was extracted from clinical notes and entered on a Microsoft Excel Spreadsheet (Microsoft Corp, Redmond, WA): Demographic data (age and sex), mechanism of injury, patterns and number of rib fractures, associated injuries noted, physiological factors (revised trauma score, injury severity score, new injury severity score, probability of survival), medical treatment offered, surgical treatment offered, time to surgery, ICU length of stay, hospital length of stay, in-hospital mortality, procedure related complications, time to return to work or normal activities, pain assessment on admission, after surgery and during outpatient review, and radiological findings during outpatient review.
The surgical procedure to fix the ribs was performed using a muscle sparing thoracic incision (Figure 1). The ribs were stabilised using titanium plates and screws (RibFix BluTM, Zimmer Biomet, Jacksonville, USA); an effort was always made to provide stability for all accessible fractures.


Fractures in ribs one, two, three, ten, eleven and twelve or fractures less than 3 cm from the costo-vertebral or sternocostal joints were not fixed. The flail segments were either bridged with a long plate spanning the two fractures or using two individual plates.
Data analysis
Descriptive statistics were used to summarise the data. Statistical difference between comparable groups was assessed using Student’s t-test for continuous variables, p < 0.05 was considered to be statistically significant.
Results
During the study period, 35 patients were admitted with a diagnosis of rib fractures alone or as part of polytrauma. The patients were mostly males with a median age of 44 years (range 16–68) (Table I).
The most common causes for rib fractures in our series were motorcycle crashes (34.2%) and falls (31.4%), closely followed by motor vehicle collisions. More than
87 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Figure 1: A typical example of multiple rib fractures and three plated fractures
sixty per cent of the cases were considered severe trauma (ISS > 16), the median ISS was 21 (4–75). For the patients treated with BMT, the median ISS was 24 (4–75) versus ISS 21 (16–75) for those offered surgery (Table 2).
There was no major difference regarding affected side (15 right – 19 left), and only one patient had bilateral fractures.
Seventy-seven per cent (77.1%) of the patients had three or more fractures (median 6; range 3–7) including nine flail chests (25.7%). The most common associated injuries were pulmonary contusion in 27 cases (77.1%), followed by haemopneumothorax in 24 cases (68.5%). Other associated injuries included clavicular fracture, upper and lower limb fractures, ruptured spleen and mild TBI, among others.
Numeric visual pain scale (VAS) assessments were administered to all conscious patients; overall the median VAS pain on admission for non-ventilated patients was 8 points (range 6–10), operated patients who were not ventilated demonstrated significant immediate postoperative reduction of the pain scales to a median of 2 out of 10 (range 1–4) (Figure 2).
Twelve of the fourteen patients (85.7%) had the surgery performed in the first seven days following injury (median 4 days, range 2–14).
Twenty-five major complications were recorded, 13 in the surgery group and 12 in the BMT group. The most common complication was pneumonia in 23% of cases (4 in each group); other complications included cardiovascular failure, severe sepsis and acute kidney injury requiring renal replacement therapy. Complications related to the ORIF procedure were recorded in only 2 of 14 patients operated (Table 3).
ICU and hospital stay were similar for patients operated or managed with BMT (6.5 and 8.5 days, respectively). The median time to return to normal productive life was 3 weeks for the surgical patients (ranging between 2–16 weeks) versus 7 weeks for the BMT group (range 3–52 weeks) (Table 4).
Discussion
The idea of stabilising fractured ribs to reduce pain, complications and facilitate healing is not new. In 1926, Jones3 first described the application of traction to the sternum to treat flail chest. Others soon followed with a myriad of different methods including traction, direct wiring of ribs and metal implants, unfortunately, surgical stabilisation did not become the standard of care, as mechanical ventilation was considered satisfactory for the treatment of the associated pulmonary contusion and to provide stability to the chest wall.3,5,6
Over the years, multiple publications have demonstrated a clear reduction in the need for opioid analgesia, incidence of pneumonia, shorter ventilation times and ICU stay and generally, a better outcome when surgery was offered over BMT.1,2,5,6,10,12-30 Unfortunately, in South Africa, not all patients have access to all of the BMT strategies, including options in advanced pain management.
Our series showed similar results between the two groups regarding ISS, number of fractures, pain VAS on admission, ICU and hospital length of stay and complications; the
88 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Surgery Best medical Pneumonia 4 4 Cardiovascular failure 1 2 Severe sepsis 2 1 Acute kidney injury (RRT) 1 2 Retained haemothorax 1 1 Chest wound seroma/hematoma 2Other 2 2 Total 13 12 (*) Some patients had
RRT
renal replacement therapy
IV: Time to return to normal activities Weeks Surgery Best medical 3 or less 8 4 to 6 3 10 7 or more 3 11 Average 5.3 9.3 Median (Range) 3 (2–18)* 7 (4–36) (*) Student’s t-test p = 0.003 p = 0.04* 12 10 8 6 4 2 0 Pain VAS Medical Surgical Post op
(*) Student’s t-test
2:
(VAS)
Table III: Complications (*)
more than one complication recorded
–
Table
Case by case pain VAS
Figure
Pain: numeric visual analogue scales
Gender Surgery Best medical Females 4 7 Males 10 14 Median age (Range) 43.5 years (34–68) 45 years (16–68) Table II: Injury severity score (ISS) Severity of injury (ISS) All Surgery Best medical Moderate (1–15) 2 2 Severe (16–25) 21 10 11 Very severe (26–40) 5 1 4 Critical (41–75) 7 3 4 Median (Range) 21 (4–75) 21 (16–75) 24 (4–75) (p > 0.05)
Table I: Demographic information
main difference observed was the time necessary to return to normal activities (median 7 weeks for medical therapy versus 3 weeks for surgical cases [p = 0.03]) and an obvious reduction of pain VAS in the postoperative period (p = 0.04).
Despite the clear advantage of mechanical ventilation to treat the respiratory failure associated with multiple rib fractures, the use of positive end-expiratory pressure (PEEP) does not achieve complete stability of the thoracic skeleton, which impacts the consolidation of the fracture site. Adequate analgesia, chest physiotherapy and early skeletal (rib) fixation seems to prevent complications, as stated in several recent studies.1,2,13,15-17,19,21
Study limitations
A single centre study with a small sample size having potential selection bias and lack of power. The retrospective nature opens it up to the usual limitations of such studies. The pain VAS is subjective and results may not be accurate.
Conclusion
There were no significant immediate differences between the ICU length of stay and complications in the BMT group and the surgical group. The postoperative pain VAS was significantly reduced in the surgical group. There was also a significant trend to earlier return to normal activities in the surgical group.
Based on the results of our study and the available evidence, we conclude that rib fixation should be offered to all patients that fit the criteria for surgery.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval was obtained from the University of the Witwatersrand Human Research Ethics Committee M180559.
ORCID



BI Monzon https://orcid.org/0000-0002-3543-6352
LM Fingleson https://orcid.org/0000-0002-9474-3520
MS Moeng https://orcid.org/0000-0001-7459-3388
REFERENCES
1. Witt CE, Bulger EM. Comprehensive approach to the management of the patient with multiple rib fractures: a review and introduction of a bundled rib fracture management protocol. Trauma Surg Acute Care Open. 2017;2:e000064. https://doi.org/10.1136/tsaco-2016-000064.
2. Kocher GJ, Al-Hourani M, Minervini F. Surgical fixation of rib fractures: how I do it. J Vis Surg. 2020;6:16. https://doi. org/10.21037/jovs.2019/11/04
3. Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma 1994;37(6):975-9.
4. Flagel BT, Luchette FA, Reed RL, et al. Half-a-dozen ribs: the break point for mortality. Surgery. 2005;138:717-23.
5. Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilisation or internal pneumatic stabilisation? A prospective randomised
study of management of severe flail chest patients. J Trauma. 2002;52(4):727-32.
6. Dehghan N, De Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:462-8.
7. Bulger E, Arneson MA, Mock CN, Jurkovic GJ. Rib fractures in the elderly. J Trauma. 2000;48(6):1040-6; discussion 10467.
8. Fabricant L, Ham B, Mullins R, Mayberry J. Prolonged pain and disability are common after rib fractures. Am J Surg. 2013;205(5):511-5.
9. Gordy S, Fabricant L, Ham B, Mullins R, Mayberry J. The contribution of rib fractures to chronic pain and disability. Am J Surg. 2014:207(5):659-62; discussion in 662-3.
10. Harrington DT, Philips B, Machan J, et al. Factors associated with survival following blunt chest trauma in older patients: results from a large regional trauma cooperative. Arch Surg. 2010;145(5):432-7.
11. Pressley CM, Fry WR, Philp AS, Berry SD, Smith RS. Predicting outcome of patients with chest wall injury. Am J Surg. 2012;204(6):910-3.
12. Leinicke JA, Elmore L, Freeman BD, Colditz GA. Operative management of rib fractures in the setting of flail chest: a systematic review and meta-analysis. Ann Surg. 2013;258(6). https://doi.org/10.1097/SLA.0b013e3182895bb.
13. Granetzny A, El-Aal MA, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. evaluation of the pulmonary status. Interac Cardiovasc Thorac Surg. 2005;4:583-7. https://doi.org/10.1510/icvts.2005.111807.
14. Richardson JD, Franklin GA, Heffley S, Seligson D. Operative fixation of chest wall fractures: an underused procedure? Am Surg. 2007;73:591-7.
15. Marasco SF, Davies AR, Cooper J, et al. Prospective randomised controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg. 2013;216(5):924-32. https://doi.org/.1016/jamcollsurg.2012.12.024.
16. Cataneo AJM, Cataneo DC, De Oliveira FHS, et al. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev. 2015;29(7):CD009919. https://doi. org/10.1002/14651858.CD009919.pub2
17. Cheng MJ. Surgical stabilisation of traumatic flail chest is superior to conservative management. Clin Res Prac. 2019;5(2):eP1948. https://doi.org/10.22237/crp/1568851320.
18. Slobogean GP, MacPherson CA, Pelletier A, Hameed SM. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg. 2013;216:302-11.
19. Swart E, Laratta J, Slobogean G, Mehta S. Operative treatment of rib fractures in flail chest injuries: a meta-analysis and cost effectiveness analysis. J Orthop Trauma. 2017;31(2):64-70(7). https://doi.org/10.1097/BOT.0000000000000750.
20. Pieracci FM, Lin Y, Rodil M, Snyder M. A prospective, controlled clinical evaluation of surgical stabilisation of severe rib fractures. J Trauma Acute Care Surg. 2016;80(2):187-94.
21. Katsoakis G, Hasenboehler EA, Strib EW, et al. Open reduction and internal fixation of rib fractures. Eastern Association for the Surgery of Trauma Practice Management Guideline. J Trauma. 2017;82(3):618-26.
22. Schulte K, Whitaker D, Attia R. In patients with acute flail chest does surgical rib fixation improve outcomes in terms of morbidity and mortality? Interact Cardiovasc Thorac Surg. 2016;23(2):314-9.
Full list of references available on request.
89 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
South African Journal of Surgery. 2021;59(3):90-93
https://doi.org/10.17159/2078-5151/2021/v59n3a3476
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]








http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN
The spectrum of blunt abdominal trauma in Pietermaritzburg
1 Critical Care Directorate, Nottingham University Hospitals, United Kingdom
2 Emergency Department, University Hospital Coventry, United Kingdom
3 Department of Surgery, University of the Witwatersrand, South Africa
4 Department of Surgery, University of KwaZulu-Natal, South Africa
Corresponding author, email: victorywkong@yahoo.com
Background: This study reviews the Pietermaritzburg Metropolitan Trauma Service (PMTS) experience with the management of blunt abdominal trauma (BAT).
Methods: A retrospective review of the hybrid electronic medical registry (HEMR) between December 2012 and September 2019 was conducted. All patients admitted following BAT were included.
Results: During the study period, 1 123 BAT patients were managed by the PMTS. The mean age was 29.19 years (SD 14.03). Of these admissions, 73.6% were male. The most common mechanism was road traffic crashes (RTCs) – 435 motor vehicle collisions (MVCs) and 250 pedestrian vehicle collisions (PVCs). There were 186 assaults, 118 falls, 62 community assaults, 22 accidents related to agriculture, construction or industry, 11 sporting injuries, nine animal injuries, seven patients injured by falling objects, five injured by trains, two hangings, one burn-related fall and two other causes. The mechanism of injury was unknown in 22 cases. There were 445 abdominal CT scans and 270 whole body CT scans. Surgical management was required for 395 patients. There were 259 index laparotomies and 176 repeat laparotomies. Four patients underwent selective arterial embolisation. Laparoscopy was undertaken in ten, and subsequently converted to laparotomy in five. There were 106 orthopaedic operations. Hospital stay ranged from 0–155 days (median stay three days). ICU admission was required in 24.9% of patients. The mortality rate was 7.5%.
Conclusion: BAT is common in South Africa. Whilst the vast majority of patients require non-operative treatment, a welldefined subset require a laparotomy. Imaging is central to the management of patients with BAT.
Keywords: blunt abdominal trauma, hybrid electronic medical registry
Introduction
Internationally, trauma is a leading cause of death in those less than 45 years old.1 In South Africa, despite a quarter of a century of relative political stability, trauma remains a major problem that places a huge burden on an already overstretched healthcare system.2 What makes the high burden of trauma in South Africa even more egregious is the high level of interpersonal violence which includes both blunt assault and frequently the use of firearms or bladed weapons.3 Much of the trauma oeuvre from South Africa over the last half-century has focused on penetrating trauma.4-9 However, a significant amount of trauma in South Africa is caused by blunt mechanisms. Common mechanisms for blunt trauma are road traffic injuries and non-penetrating violence.10 Road traffic injuries are a major cause of death in South Africa with the mortality rate being 2.7 times that of the global mean.11 Assaults with fists, and blunt weapons are also common. Blunt abdominal injury can be particularly challenging for a number of reasons. The abdomen contains a large number of viscera and multiple organ injury is common.10 The mechanisms of injury in blunt abdominal trauma (BAT) often result in concurrent non-abdominal injury which may also need urgent intervention. Clinical examination is not diagnostically reliable12 and the use of
US scanning13 and CT scanning14 are important diagnostic tools. This study reviews the Pietermaritzburg Metropolitan Trauma Service (PMTS) experience of suspected BAT and describes the spectrum and investigation, management of BAT in our setting.
Clinical settings
The hybrid electronic medical registry (HEMR) is a registry of patients admitted to the PMTS. The PMTS provides definitive trauma care to Pietermaritzburg, the capital of KwaZulu-Natal province, and is a trauma centre which acts as a referral centre for 19 rural hospitals. The ethical approval to maintain the HEMR is granted by the University of KwaZulu-Natal’s Biomedical Research Ethics Committee (BE221/13 and BE207/09).
The study
A retrospective review of the HEMR between December 2012 and September 2019 was conducted. All patients with suspected BAT on admission were included. Only patients treated at Grey’s Hospital, Pietermaritzburg, were included in this study, patients who were transferred from Edendale Hospital for CT scanning were excluded. Patient characteristics were reported alongside mechanism of injury,
90 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
038-2361
The Author(s) TRAUMA
© 2021
P Rhimes,1 S Moffatt,2 VY Kong,3,4 JL Bruce,4 MTD Smith,4 W Bekker,4 GL Laing,4 DL Clarke3,4
imaging requirements, management (including surgical intervention) and mortality.
Patient characteristics
During the study period, 1 123 patients were admitted with suspected BAT and were managed by the PMTS. The mean age of these patients was 29.19 years (SD 14.03). Of these admissions 73.6% (n = 827) were male, 24.8% (n = 279) were female and in 1.5% (n = 17) of cases, the sex was not clear from the HEMR. The median ISS was 14. Patient characteristics are displayed in Table I and presenting physiology is displayed in Table II.
related to agriculture, construction or industry, 11 sporting injuries, nine animal injuries, seven patients injured by falling objects, five injured by trains, two hangings, one burn-related fall and two other causes. The mechanism of injury was unknown in 22 cases.
Imaging
There were 445 abdominal CT scans and 270 whole body CT scans. Imaging is summarised in Table III.
Mechanism of injury
The most common mechanism was road traffic crashes (RTCs) which accounted for 61% (n = 685) of all cases. Of these, 435 were motor vehicle collisions (MVCs) and 250 were pedestrian vehicle collision (PVCs). There were 186 assaults, 118 falls, 62 community assaults, 22 accidents
Management
The majority of patients (64.8%) did not need surgical intervention. The remaining 395 patients required some form of surgical intervention, including orthopaedic surgery (n = 106) and other non-abdominal surgery (n = 129). There were 259 index laparotomies, of which 50.2% were conducted without prior abdominal CT. There were a total of 176 repeat laparotomies with several patients undergoing multiple repeat laparotomies. At index laparotomy, sple-
91 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Table I: Patient characteristics Total (n) 1 123 Mean age (years) 29.19 Range of age (years) 0.5–85 Median age (years) 28 Sex Male 827, Female 279, unknown 17 Injury to hospital mean time 1 day 13 hours 27 minutes Injury to hospital range 27 minutes – 118 days 1 hour 21 minutes Injury to hospital median time 14 hours 13 minutes Injury to hospital SD 6 days 7 hours 55 minutes Table II: Presenting physiology Mean HR (BPM) 98.65 HR range (BPM) 18–197 Median HR (BPM) 96 Mean SBP (mmHg) 121.22 SBP range (mmHg) 47–237 Median SBP (mmHg) 120 Mean lactate (mmol/L) 2.77 Lactate range (mmol/L) 0.3–17 Median lactate (mmol/L) 1.8 Mean pH 7.37 pH range 6.87–7.63 Median pH 7.39 Mean BE (mmol/L) -2.62 BE range (mmol/L) -27.6–15.8 Median BE (mmol/L) -2 Mean HCO3- (mmol/L) 22.33 HCO3- range (mmol/L) 5.3–40.9 Median HCO3- (mmol/L) 22.8 Mean Hb (g/dL) 11.62 Hb range (g/dL) 4.1–22.8 Median Hb (g/dL) 11.65
CXR 576 AXR 223 CT abdomen 445 Whole body CT 270 CT thorax 144 CT pelvis 174 CT angio 49 Contrast meal/swallow 9 Cystogram 79 US abdomen 49 US pelvis 3 US thorax 1 FAST scan 7
Table III: Imaging performed
Small bowel resection/repair Splenectomy Bladder repair Abdominal packing Diaphragm repair Stoma formation Pancreatectomy Pelvic packing Mesenteric repair Nephrectomy Large bowel repair Hepatic repair/suture Gastric repair Other 70 60 50 40 30 20 10 0 Interventions at index laparotomy
Figure 1: Interventions at index laparotomy
nectomy, small bowel repair, bladder repair and hepatic packing were the most common interventions. Common interventions at laparotomy or repeat laparotomy are shown in Figure 1 and Figure 2. Two patients underwent selective embolisation for splenic injury, one for hepatic injury and one for a renal injury. Laparoscopy was undertaken in ten cases, and subsequently converted to laparotomy in five cases. Hospital stay ranged from 0–155 days with the median stay being three days. ICU admission was required in 24.9% (n = 280) of patients. The mortality rate was 7.5% (n = 84).
Discussion
Our series demonstrates two main mechanisms of BAT in our region. The first is related to RTC and the second to interpersonal violence in the form of assaults by individuals and mobs. These two mechanisms accounted for 83% of the injuries described in this study. A coordinated nationwide multi-faceted strategy to reduce the high rate of road traffic related trauma is long overdue. Such a strategy will require political will and general buy-in from all stakeholders as it will require a major change in the culture of road usage.11 The experience with the total societal mobilisation around HIV/AIDS15 and more recently with the response to the COVID-19 pandemic16 suggests that it is possible to achieve the same with trauma in general and road traffic collisions in particular. Reducing the high rates of interpersonal trauma may be more difficult to achieve.
The management of BAT relies heavily on imaging. In the United Kingdom, it is rare for a case of BAT to proceed to surgery without first undergoing a CT scan.17 In our series, the rate is not as high. This difference is likely due to the disparity in injury severity and scanner availability between the two regions. It is difficult to rely on clinical examination to assess patients with injuries to multiple body regions.12 The use of sonar in the form of focused abdominal sonar for trauma (FAST) is increasingly common.18 We have still not fully developed this modality at our institution and there were only seven documented FAST scans in our
series. CT remains the gold standard in assessing BAT;19 it is very sensitive in the detection of free fluid and it is able to diagnose solid organ injury and grade almost all solid organ injuries. FAST scan is increasingly used to identify the presence of intra-abdominal fluid. As such, FAST remains an excellent modality for ruling in abdominal injury but is poor in grading the severity of the injury and must usually be followed by a CT if a non-operative approach is to be followed.13
Hollow visceral disruption cannot be treated nonoperatively and the commonest indication for laparotomy was a small bowel injury. Blunt small bowel injury has been well described from our unit and is still associated with delay in recognition and morbidity.10,20 Duodenal injury and bladder disruption were also common indications for laparotomy.21 Solid visceral injuries, especially hepatic, splenic and renal are amenable to non-operative management (NOM) provided the patient remains in a state of haemodynamic stability. CT imaging helps grade these injuries and direct therapy. Selective embolisation, endo-urological intervention and laparoscopy are adjuncts which increase the scope of NOM in these injuries.22,23 The low number of embolisations in our series again reflects our institutions inability to deliver this intervention. Pancreatic trauma is insidious and associated with delayed recognition. Complete ductal disruption should mandate an operation. If the disruption is at the neck of the pancreas, distal pancreatectomy or pancreatico-gastrostomy are potential solutions. If the injury involves the pancreatic head and duodenum, then the initial operative approach is to control soiling and provide drainage. Once the patient is stabilised, these injuries usually require a formal pancreaticduodenectomy.
Surgical management is complex and there is a high rate of repeat operation. This is frequently secondary to the use of damage control procedures. Once the patient’s physiology has been restored, definitive surgery can be undertaken, packs removed and open abdomens closed. Multiple, repeat laparotomies may be required to deal with ongoing intraabdominal sepsis. There is a high rate of non-abdominal operations in these patients and this reflects the fact that blunt torso trauma is truly polytrauma involving multiple body regions. The high rate of ICU admission and the high mortality rate reflect the severity of the polytrauma.
Conclusion
BAT is a common problem in South Africa. Whilst the vast majority of patients require non-operative treatment, a welldefined subset require a laparotomy. Imaging is central to the management of patients with BAT. Management is complex and associated with significant morbidity and mortality.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The ethical approval to maintain the HEMR is granted by the University of KwaZulu-Natal’s Biomedical Research Ethics Committee (BE221/13 and BE207/09).
92 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Small bowel repair/resection Stoma formation Hemicolectomy Bladder repair Feeding jejunostomy Ureterostomy Liver packing Large bowel repair Pancreactomy Splenectomy Other 10 9 8 7 6 5 4 3 2 1 0 Interventions at re-laparotomy
Figure 2: Interventions at re-laparotomy
ORCID








P Rhimes https://orcid.org/0000-0002-9689-3688
S Moffatt https://orcid.org/0000-0002-7649-4970
VY Kong https://orcid.org/0000-0003-2291-2572
JL Bruce https://orcid.org/0000-0001-8666-4104
MTD Smith https://orcid.org/0000-0002-6954-153X
W Bekker https://orcid.org/0000-0003-0695-5994
GL Laing https://orcid.org/0000-0001-8075-0386
DL Clarke https://orcid.org/0000-0002-8467-1455
REFERENCES
1. Institute of Medicine (US) Committee on Injury Prevention and Control. Reducing the burden of injury: advancing prevention and treatment. Washington: National Academies Press; 1999. https://doi.org/10.17226/6321.
2. Lutge E, Moodley N, Tefera A, et al. A hospital based surveillance system to assess the burden of trauma in KwaZulu-Natal Province South Africa. Injury. 2016;47:13540. https://doi.org/10.1016/j.injury.2015.08.020.
3. Seedat M, Van Niekerk A, Jewkes R, et al. Violence and injuries in South Africa: prioritising an agenda for prevention. Lancet. 2009;374:1011-22. https://doi.org/10.1016/S01406736(09)60948.
4. Stein A, Schnier G. Penetrating stab wounds of the chest. S Afr Med J. 1965;39:548-53.
5. Khumalo-Mugabi L, Moffatt S, Bekker W, et al. Penetrating trauma in children and adolescents in Pietermaritzburg. South African J Surg. 2020;58:33-6. https://doi.org/10.17159/20785151/2020/V58N1A3017.
6. Koto MZ, Matsevych OY, Motilall SR. The role of laparoscopy in penetrating abdominal trauma: our initial experience. J Laparoendosc Adv Surg Tech. 2015;25:730-6. https://doi. org/10.1089/lap.2015.0042.
7. Demetriades D, Rabinowitz B, Sofianos C, et al. The management of penetrating injuries of the back. A prospective study of 230 patients. Ann Surg. 1988;207:72-4. https://doi. org/10.1097/00000658-198801000-00014.
8. Kong VY, Oosthuizen GV, Clarke DL. The spectrum of injuries resulting from posterior abdominal stab wounds: a South African experience. Ann R Coll Surg Engl. 2015;97:269-73. https://doi.org/10.1308/003588415X14181254789204.
9. Chamisa I. Civilian abdominal gunshot wounds in Durban, South Africa: a prospective study of 78 cases. Ann R Coll Surg Engl. 2008;90:581-6. https://doi. org/10.1308/003588408X301118.
10. Bekker W, Kong VY, Laing GL, et al. The spectrum and outcome of blunt trauma related enteric hollow visceral injury. Ann R Coll Surg Engl. 2018;100:290-4. https://doi. org/10.1308/rcsann.2018.0013.
11. Wesson HKH, Boikhutso N, Hyder AA, et al. Informing road traffic intervention choices in South Africa: the role of economic evaluations. Glob Health Action. 2016;9. https:// doi.org/10.3402/gha.v9.30728.
12. Jansen JO, Yule SR, Loudon MA. Investigation of blunt abdominal trauma. BMJ. 2008;336:938-42. https://doi. org/10.1136/bmj.39534.686192.80.
13. Stengel D, Leisterer J, Ferrada P, et al. Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev. 2018;12:CD012669. https://doi.org/10.1002/14651858. CD012669.pub2.
14. O’Neill SB, Hamid S, Nicolaou S, et al. Changes in approach to solid organ injury: what the radiologist needs to know. Can Assoc Radiol J. 2020;10:352-61. https://doi. org/10.1177/0846537120908069.
15. The Joint United Nations Programme on HIV/AIDS. New modelling research shows partial progress in South Africa’s response to HIV; 2019. Available from: https://www. unaids.org/en/resources/presscentre/featurestories/2019/ june/20190628_south-africa-modelling. Accessed 1 Sep 2020.
16. Morris D, Rogers M, Kissmer N, et al. Impact of lockdown measures implemented during the Covid-19 pandemic on the burden of trauma presentations to a regional emergency department in Kwa-Zulu Natal, South Africa. African J Emerg Med. 2020 Dec;10(4):193-6. https://doi.org/10.1016/j. afjem.2020.06.005.
17. Pande R, Saratzis A, Winter Beatty J, et al. Contemporary characteristics of blunt abdominal trauma in a regional series from the UK. Ann R Coll Surg Engl. 2017;99:82-7. https:// doi.org/10.1308/rcsann.2016.0223.
18. Boulanger BR, Kearney PA, Brenneman FD, et al. Utilization of FAST (focused assessment with sonography for trauma) in 1999: Results of a survey of North American trauma centers. Am Surg. 2000;66:1049-55.
19. Bekker W, Smith MTD, Kong VY, et al. Isolated free fluid on computed tomography for blunt abdominal trauma – a South African experience. Ann R Coll Surg Engl. 2019;101:552-7. https://doi.org/10.1308/rcsann.2019.0078.
20. Bekker W, Hernandez MC, Zielinski MD, et al. Defining an intra-operative blunt mesenteric injury grading system and its use as a tool for surgical-decision making. Injury. 2019;50:2732. https://doi.org/10.1016/j.injury.2018.08.014.
21. Weale RD, Kong VY, Bekker W, et al. Primary repair of duodenal injuries: a retrospective cohort study from a major trauma centre in South Africa. Scand J Surg. 2019;108:280-4. https://doi.org/10.1177/1457496918822620.
22. Hildebrand DR, Ben-Sassi A, Ross NP, et al. Modern management of splenic trauma. BMJ. 2014;348:g1864-70. https://doi.org/10.1136/bmj.g1864.
23. Armstrong RA, Macallister A, Walton B, et al. Successful non-operative management of haemodynamically unstable traumatic splenic injuries: 4-year case series in a UK major trauma centre. Eur J Trauma Emerg Surg. 2019;45:933-8. https://doi.org/10.1007/s00068-018-0975-y.
93 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
https://doi.org/10.17159/2078-5151/2021/v59n3a3528
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]








http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361
© 2021 The Author(s)
The correlation between full moon and admission volume for penetrating injuries at a major trauma centre in South Africa
1 Department of Surgery, University of the Witwatersrand, South Africa
2 Department of Surgery, University of KwaZulu-Natal, South Africa
3 Department of Surgery, Alrijne Hospital, The Netherlands
4 Department of Surgery, Stanford University School of Medicine, United States of America
5 Department of Surgery, North West Deanery, United Kingdom
6 Department of Surgery, Waikato Hospital, New Zealand
7 Department of Surgery, Flinders Medical Centre, Australia
Corresponding author, email: victorywkong@yahoo.com
Background: The possible effect of full moon on admission volume of trauma centres is a well-mentioned phenomenon that has been perpetuated worldwide. We aimed to review the correlation between full moon and admission volume and to interrogate any possible relationship on admission for penetrating trauma.
Methods: A retrospective study from 2012 to 2018 at Pietermaritzburg Metropolitan Trauma Service (PMTS), South Africa.
Results: A total of 8 722 patients were admitted. Eighty-three per cent (7 242/8 722) were male and the mean age was 29 years. The total number of days during the study period was 1 953, 66 of which were ‘full moon’ (FM) days and 1 887 were ‘non-full moon’ (NFM) days. There was no significant difference between gender or age distribution. The mean number of admissions per day on FM days compared with NFM days was not significant (4.1 vs 4.5, p = 0.583). A total of 3 332 patients with penetrating trauma were admitted. This constituted 42% (113/271) of admission on FM days and 38% (3 219) on NFM days, which is not statistically significant (p = 0.229). Subgroup analysis did not demonstrate any significant difference between the number of stab wounds – 28% (77/113) vs 25% (2 124/3 219) – or gunshot wounds – 13% (16/113) vs 12% (990/3 219) – between FM and NFM days.
Conclusion: The correlation between full moon and trauma admission is unfound in our setting. The perpetuating notion that ‘it must be full moon tonight’ is likely to be an urban myth with no scientific evidence for such a claim.
Keywords: emergency medicine, trauma, epidemiology, full moon, lunar cycle
Introduction
Trauma in South Africa has been aptly described as a ‘malignant epidemic’ and represents a significant burden on the limited resources for all trauma centres throughout the country.1 Worldwide, there appears to be a common notion in many emergency departments (ED) that the effect of the full moon is somehow correlated to admission volume and busyness of the centre.2 The effect of lunar cycles on human behaviour was thought to be related to alteration of biological rhythm.3 Numerous theories have been postulated, including gravitational pull of the moon that may affect the function of the pineal gland. These were thought to alter human behaviour that includes disinhibition, increased aggression and self-destructive behaviour.3-5 For decades, the exact relationship between lunar phases and human behaviour has remained somewhat controversial and confusing, as numerous studies have attempted to correlate these with mixed results.2 Several studies from the United States in the 1990s consistently demonstrated that lunar phase has no effect on trauma and emergency admissions.2,6,7 Although the expression that ‘it must be full moon tonight’ is mostly made in jest, it remains one of the common urban
myths and is a widely held folklore in ED.2,3 In a survey published by Danzl in 1987 using the modified belief in lunar effects (BILE) scale, 80% of ED nurses and 64% of the ED physicians believe that the moon affects patients.7 Of these nurses, 92% find lunar shifts particularly stressful and indicated lunar pay differentials were warranted.7
At the primary author’s (VYK) institution (PMTS), there appears to be persistent conviction, in particular for admissions related to penetrating trauma from interpersonal violence, that the volume may be related to the full moon. Importantly, this phenomenon has never been studied in South Africa. This study was designed to review the correlation between full moon and admission volume and to interrogate any possible relationship on admission for penetrating trauma presented to a major trauma centre in a developing world setting.
Materials and methods
Clinical setting
This was a retrospective study conducted at the Pietermaritzburg Metropolitan Trauma Service (PMTS),
94 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
TRAUMA
African Journal of Surgery.
South
2021;59(3):94-96
VY Kong,1,2 AA Keizer,3 MM Donovan,4 RD Weale,5 NS Rajaretnam,6 JL Bruce,2 A Elsabagh,7 DL Clarke1,2
Pietermaritzburg, South Africa. The PMTS is one of the largest academic trauma centres in western KwaZulu-Natal (KZN) province and is one of the main teaching hospitals affiliated to Nelson Mandela School of Medicine at the University of KwaZulu-Natal (UKZN). Our trauma centre is headed by a full-time professor of surgery (DLC) and has three other full-time faculties, all of whom are fellowship trained subspecialists in trauma surgery. It provides undergraduate, postgraduate specialist and subspecialist fellowship training in trauma surgery for both local and international doctors regulated by the College of Surgeons of South Africa (CSSA). The PMTS provides definitive and tertiary level trauma care that covers a total catchment population of over 4.5 million. Due to the extremely high incidence of interpersonal violence, gang related and other criminal activities rampant throughout the province, penetrating trauma is exceedingly common and comprises a significant workload at our trauma centre.
The study
A retrospective review was undertaken using our electronic regional trauma registry, known as the hybrid electronic medical record (HEMR), which was first established in 2012. This is a comprehensive regional trauma data bank that contains the detailed admission and hospital clinical record of every trauma patient who was treated at our institution. The establishment of HEMR has been described elsewhere in the literature. All patients admitted to PMTS over the five-year period December 2012 – December 2018 were reviewed. The date and time of admission for each patient was analysed. The lunar phase of each admission date was interrogated based on the lunar data from the Johannesburg Observatory. Each admission date was classified as either ‘full moon date’ (FM) or ‘non-full moon date’ (NFM). The basic demographics were reviewed, including gender and age. A further review was conducted based on the different mechanisms of injury.
Statistical analysis
Statistical analysis was performed using the chi-square test for categorical variables and two-sided Fisher’s exact test for expected cell count less than five. Independent t-test and Mann–Whitney U test were used for continuous variables. For normally distributed data, the mean and standard deviation (SD) were calculated. For not normally distributed
data, the median and interquartile range (IQR) were reported. A value of p < 0.05 was considered statistically significant. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS®, Version 22, IBM Corporation, Armonk, New York).
Results
Overview
During the five-year study period, a total of 8 722 cases were admitted to PMTS. Eighty-three per cent (7 242/8 722) were male and the mean age was 29 years. The total number of days during the study period was 1 953, 66 of which were FM days and 1 887 were NFM days. There was no significant difference between the gender and the mean age of those who were admitted on FM days or NFM days. The mean number of admissions per day on FM days compared with NFM days was not significant (4.1 vs 4.5, p = 0.583) (Table I).
Full moon vs non-full moon days
A total of 3 332 cases of penetrating trauma were admitted during the study period. This constituted 42% (113/271) of admission on FM days and 38% (3 219) on NFM days, which was not statistically significant (p = 0.229). Subgroup analysis did not demonstrate any significant difference between the number of stab wounds – 28% (77/113) vs 25% (2 124/3 219) – or gunshot wounds – 13% (16/113) vs 12% (990/3 219) – between FM and NFM days (Table II).
Discussion
The perception of full moon correlating to admission volume in ED has long been recognised worldwide.2,6,7 There have been numerous studies interrogating the relationship between lunar phase and human behaviour.2,6,7 These include a wide range of phenomena such as homicide, suicide, violent crime and road traffic accidents.6-9 This remains somewhat controversial due to the different methodologies, definitions, and the lack of control of confounding variables in many studies.6-8 In a study by Calver et al., it was noted that violent and acute behavioural disturbance manifested more commonly during the full moon.9 However, in a large retrospective study of 1 444 cases by Coates et al. at a level one trauma centre in Pittsburgh, no correlation was noted.6 In particular, there was no significant difference between
95 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Full moon days Non-full moon days p-value Total days 66 1 887Total trauma admissions 271 8 451Mean trauma admissions per day 4.106 4.478 0.583 Demographics Female 49 (18.1%) 1 431 (16.9%) 0.62 Male 222 (81.9%) 7 020 (83.1%) 0.679 Mean age (SD) 29.29 (14.66) 29.59 (14.48) 0.738 Mean ISS (SD) 11.33 (7.78) 10.08 (8.68) 0.041 ICU admissions 32 (11.8%) 849 (10.0%) 0.34 Mean ICU stay (SD) 3.53 (5.08) 3.93 (6.32) 0.699 Mortality 12 (4.4%) 384 (4.5%) 0.822
Table I
Table II
* – Other subtypes are not shown on this analysis due to very small sample size
FM and NFM days regarding violent trauma admissions (assaults, gunshot wounds, and stab wounds). While the notion of full moon correlating to the admission volume is regarded by some as merely one of the many folklores in ED, a study by Danzl demonstrated that 80% of ED nurses and 64% of the ED physicians believe that the moon affects patients. Furthermore, a differential pay rise was considered warranted by 92% of ED nurses due to the perceived increase in workload and stress level.7
South Africa has a notorious international reputation for the level of civilian violence that is described as one of the highest outside countries not at war.10 This 'malignant epidemic' consumes significant resources of the overburdened and chronically underfunded health system.1,9,11 Understanding the potential factors that may influence the workload does have direct implications for resource planning. Milford et al. from Groote Schuur Hospital, Cape Town, noted correlations between temporal factors and weather variables on motor vehicle collisions and interpersonal violence.13 Other studies from South Africa reported a difference in the number of emergency department visits for traumatic injury in relation to major sporting events.13-15
Surprisingly, the phenomenon of full moon has never been studied in South Africa. To our knowledge, this was the first and only study from South Africa that also focuses exclusively on trauma admissions in relation to lunar cycle. Although not formally interrogated in this study, at the author’s institution (PMTS) there appears to be a pervasive notion that such correlations exist, and informal discussion on differential pay has frequently been raised. We have demonstrated that there was no correlation between the full moon and total admission volume. Neither does full moon have any effect on admission volume for penetrating trauma.
Conclusion
The correlation between the full moon and trauma admission volume is unfounded in our setting. The perpetuating notion that ‘it must be full moon tonight’ is likely to be an urban myth with no scientific evidence for such a claim. Further studies from other centres within South Africa may provide a more comprehensive view.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval for the maintenance of our registry and for this study was formally approved by the Biomedical Research Ethics Committee of the University of KwaZuluNatal (Reference number: BCA 207/09 and BCA 221/13).
ORCID








VY Kong https://orcid.org/0000-0003-2291-2572
AA Keizer https://orcid.org/0000-0001-9902-3023
MM Donovan https://orcid.org/0000-0003-3908-9076
RD Weale https://orcid.org/0000-0001-9296-527X
NS Rajaretnam https://orcid.org/0000-0001-9809-6896
JL Bruce https://orcid.org/0000-0001-8666-4104
A Elsabagh https://orcid.org/0000-0001-9887-8476
DL Clarke https://orcid.org/0000-0002-8467-1455
REFERENCES
1. Muckart DJ. Trauma, the malignant epidemic. S Afr Med J. 1991 Jan 19;79(2):93-5. Available from: https://www.ncbi. nlm.nih.gov/pubmed/1989097.
2. Thompson DA, Adams SL. The full moon and ED patient volumes: unearthing a myth. Am J Emerg Med. 1996 Mar; 14(2):161-4. Available from: https://www.ncbi.nlm.nih.gov/ pubmed/8924138
3. Lieber AL. Human aggression and the lunar synodic cycle. J Clin Psychiatry. 1978 May;39(5):385-92. Available from: https://pubmed.ncbi.nlm.nih.gov/641019/
4. Templer DI, Veleber DM, Bronner RK. Geophysical variables and behaviour: VI. Lunar phase and accident injuries – a difference between night and day. Percept Mot Skills. 1982 Aug;55(1):280-2.
5. Lebowski K. Why do we still believe in ‘lunacy’ during a full moon? Discover Magazine [Internet]. 2019. Available from: https://www.discovermagazine.com/mind/why-do-we-stillbelieve-in-lunacy-during-a-full-moon Accessed 11 Feb 2021.
6. Coates W, Jehle D, Cottington E. Trauma and the full moon: a waning theory. Ann Emerg Med. 1989 Jul;18(7):763-5. Available from: https://www.ncbi.nlm.nih.gov/pubmed/2735 596.
7. Danzl DF. Lunacy. J Emerg Med. 1987;5(2):91-5. Available from: https://www.ncbi.nlm.nih.gov/pubmed/3584923
Full list of references available on request.
96 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Trauma mechanism Full moon days Non-full moon days p-value Blunt trauma 153 (56.5%) 4 874 (57.7%) 0.69 Penetrating trauma 113 (41.7%) 3 219 (38.1%) 0.229 Blunt trauma subtypes* Assault 54 (19.9%) 1 622 (19.2%) 0.763 Road traffic accidents 66 (24.4%) 2 166 (25.6%) 0.636 Accidental fall 10 (3.7%) 352 (4.2%) 0.722 Penetrating trauma subtypes* Stab wounds 77 (28.4%) 2 124 (25.1%) 0.221 Gun shots 36 (13.3%) 990 (11.7%) 0.43
South African Journal of Surgery. 2021;59(3):97-101
https://doi.org/10.17159/2078-5151/2021/v59n3a3500
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]




http://creativecommons.org/licenses/by-nc-nd/4.0
An analysis of paediatric snakebites in north-eastern South Africa
JJP Buitendag,1 S Variawa,2 D Wood,3 G Oosthuizen4
1 Department of Surgery, Tygerberg Hospital, Stellenbosch University, South Africa
2 Department of Surgery, Khayelitsha District Hospital, Stellenbosch University, South Africa
3 Department of Emergency Medicine, Queens Hospital BHRUT, Queen Mary University London, United Kingdom
4 Department of Surgery, Ngwelezana Hospital, University of KwaZulu-Natal, South Africa
Corresponding author, email: johan_buitendag@yahoo.com
Background: Snakebites are an underappreciated health concern in middle- and lower-income countries. The lack of national data vastly impacts funding for this health crisis, as well as strategies for treatment and prevention. Children are particularly vulnerable to snakebite and data in this group is limited.
Methods: This study included paediatric patients, aged 13 years old or younger, admitted to Ngwelezana Tertiary Hospital, Department of Surgery with a snakebite or snakebite related complication, from 1 September 2008 to 31 December 2013. Data captured included demographics, time of presentation, syndromic symptoms, blood results and patient management.
Results: A total of 274 patients were included in this study. The median age at presentation was 8 years, with approximately 70% of the patients aged between 6 and 13 years, with a male predominance (56%). The median time of presentation after sustaining a snakebite was 7 hours (interquartile range 4–13 hours). The majority of patients (71%) presented with cytotoxic manifestations. A total of 53 patients received antivenom of whom 25% suffered adverse reactions. Fifty-six patients underwent one or more procedures on their affected limbs. Three patients required admission to the intensive care unit; all were part of the cytotoxic group and received antivenom. There were no recorded mortalities.
Conclusion: The majority of snakebites are cytotoxic in nature. One-fifth of the paediatric population require antivenom and one-fifth require a surgical procedure post envenomation. Adverse effects post antivenom use are common but manageable. Prevention programmes are needed to help reduce this burden of disease and a nationwide snakebite registry is long overdue.
Keywords: paediatric, snakebite, antivenom
Introduction
Snakebites are an underappreciated health concern in lowerand middle-income countries (LMICs).1 Global data on snakebites are region-specific and very limited regarding number of admissions, morbidity and mortality rates. The lack of data vastly impacts funding for this health crisis, as well as strategies for treatment and prevention.2 Current data suggests that Asia carries the highest burden of disease with approximately 15 400–57 600 deaths per annum, while sub-Saharan Africa estimates are at 3 500–32 100 deaths per annum.3 These estimates are based on hospital records and surveys from the affected regions.
Snakebite occurrence is reported more regularly in developed countries, however, lower-income countries are more commonly affected by snakebites therefore posing difficulties in analysis of epidemiological data.4 The North American Snakebite Registry was established in 2013 and records data collected prospectively across 10 states in the United States of America.5 Whilst this registry is dependent on accurate reporting, data collected has already provided beneficial information regarding directed public education, as well as further insight into the clinical manifestations of different snake species aiding treating physicians in management.5
There is data that suggests the number of snakebite cases in sub-Saharan Africa is as high as 100 000–500 000 per annum.6 A meta-analysis has recently showcased that it is difficult to determine the exact burden of disease in this region.7 It is reported that the highest incidence of snakebites in Southern Africa is in rural KwaZulu-Natal with an annual incidence of 28–96.5 per 100 000.8-10 Another study estimated that the number of cases per year is between 1 193–2 357.9
In the last five decades, multiple studies on snakebites have reported similar findings on seasonal preference, demographics and mortality rates, which reiterates the fact that little progress has been made regarding treatment and prevention strategies for this underappreciated health concern.8-10
The majority of potentially lethal snakebites in Southern Africa is due to cytotoxic envenomation from puff adders and the Mozambique spitting cobra.11 Due to the fact that snakebites and their outcomes are infrequently reported in Southern Africa, the mortality of 0.08–2.67 per 100 000 is based on small studies.12 Children are more likely to be envenomated following a snakebite and suffer more severe presentations. This may often lead to a higher proportion of children receiving antivenom.13 The data on paediatric snakebites is scarce. Campbell et al. from Arkansas
97 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
038-2361
2021 The Author(s) TRAUMA
ISSN
©
Children’s Hospital and the University of Arkansas for Medical Sciences, published a paper with 114 cases of paediatric snakebites.14 Aktar et al. included 151 paediatric snakebites in a study performed by Dicle University in Turkey.15 Here we present the largest paediatric snakebite case series published, to our knowledge.
Methods
Ngwelezana Hospital is a 554-bed hospital, designated as a tertiary hospital for the northern part of the province of KwaZulu-Natal. The hospital receives referrals from 18 hospitals for secondary and tertiary care. The emergency department sees approximately 3 500 patients annually.
Sampling
The patient population were all patients attending the emergency department at Ngwelezana Tertiary Hospital with snakebite from 1 September 2008 to 31 December 2013. The sample population included all patients aged 13 years old or younger who presented with snakebite during the specified period. As per national standard, the definition of a paediatric patient is considered as anyone below the age of 14 years.16 Patients were recruited consecutively and all patients in the study sample were included.
Patient selection and management procedure
Following admission, the condition of each snakebite patient was monitored from the time of admission to discharge by the surgical team. The diagnosis was made through a two-stage process. Firstly, if the patient identified the snake, brought it along to the hospital or visible fang marks were present, they were considered as having a suspected snakebite.
Secondly, suspected snakebite cases were further confirmed based on clinical symptoms on presentation such as local swelling, bleeding, or neurological symptoms. This system of syndromic assessment for snakebite is used to categorise envenomations and guide treatment. If the abovementioned criteria were not met, the patient was excluded from the study. Patients who developed significant swelling, bleeding or neurological symptoms were administered antivenom as per department protocol (Table I). Patients who required surgical intervention for skin necrosis had a procedure done in the operating theatre
only once the inflammation had settled. The affected soft tissue damage was usually clearly demarcated after 3 to 5 days. Patients with significant limb swelling and suspected compartment syndrome were acted on without delay.
Data
The demographic and clinical data of the patient was captured on a case report form and entered onto a secured database (Excel 2002). Data fields included patient demographics, time of bite to presentation, syndromic clinical symptoms, blood results, patient management and outcome. Ethical permission for the study was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (Ref. No.: BE034/14).
Statistical analysis
Descriptive statistics were initially done to describe the basic features of the data at hand and to indicate the dispersion of the data. These descriptive methods were also used to indicate the skewness and kurtosis of the data. In cases where outliers were evident, rank and percentile tests were
Table I: Protocol for antivenom administration
1. Indication correct – clinical severity, risk (SRS), pre-surgery
2. Consent from patient or guardian
3. Transfer patient to resuscitation area
4. Full monitoring
5. 2 x IV lines (large bore) appropriate for age
• 1 x Crystalloid for resuscitation
• 1 x Antivenom
6. Premedication
• Adrenaline IM
• 0.3–0.5 mg in adults
• 0.01 mg/kg (1:1 000) or 0.1 ml/kg (1:10 000) in children
• Expect tachycardia, monitor for dysrhythmias
• Fluid bolus 20 ml/kg
7. Antivenom initial dose
• 5 vials polyvalent for painful progressive swelling (repeat as required)
• 10 vials polyvalent for neurotoxic progressive weakness
• 2 vials monovalent Boomslang in bleeding
• Dilute in 200 ml normal saline and infuse over 20–30 minutes. (test dose not required)
8. Repeat doses of antivenom prn
9. Dr to closely monitor patient
10. Patients to be counselled re: Serum (type III reaction) sickness
98 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
18 16 14 12 10 8 6 4 2 0 Figure 1: Paediatric
monthly incidence Paediatric snakebite incidence Sep 08 Dec 08 Mar 09 Jun 09 Sep 09 Dec 09 Mar 10 Jun 10 Sep 10 Dec 10 Mar 11 Jun 11 Sep 11 Dec 11 Mar 12 Jun 12 Sep 12 Dec 12 Mar 13 Jun 13 Sep 13 Dec 13
snakebite
done to measure the true dispersion. Descriptive analysis was also used in aid of trend analysis of the historic data to make meaningful inferences. Mortality rate, age and sex are commonly measured with this method.
Continuous variables were compared using unpaired t-test, and categorical variables using chi-squared analysis. Chi-squared test compared the type of envenomation and subsequent treatment and reactions. Chi-squared analysis was also used to assess other categorical variables between groups.
Results
Demographics
Over a 5-year period from 1 September 2008 to 31 December 2013, a total of 274 children aged 13 years or younger presented with a snakebite. The median age at presentation was 8 years, with approximately 70% of the patients aged 6–13 years. Forty-four per cent of patients were female and 56% male. The majority of the patients were from the immediate area with 24% of patients referred from surrounding facilities. The peak incidence occurred over the warmer months, which are usually December–February (Figure 1).
Time after bite
The median time of presentation to Ngwelezana Hospital after sustaining a snakebite was 7 hours with an IQR of 4–13 hours. The earliest presentation was after 30 minutes and latest after 79 hours.
Syndromic distribution
The vast majority of patients (71%) presented with cytotoxic manifestations, 2% haemotoxic and 1% neurotoxic, while 26% of patients displayed no features in keeping with any of the latter categories and are unclassified in the data. Four patients presented with signs of both cytotoxic and haemotoxic manifestations and one patient with cytotoxic and neurotoxic manifestations. Patients with mixed envenomation were classified according to the predominant syndrome present.
Blood results
For the total patient sample, the median white cell count (x 109/L) was 10.0, haemoglobin (g/dL) 11.8, platelets (x 109/L) 308, INR (international normalised ratio) 1.12, urea (mmol/L) 3.3 and creatinine (umol/L) 43 (Table II). In the cytotoxic group, the median white cell count was 10.45 (± 6.3), haemoglobin 11.7 (± 2.1), platelets 301 (± 146), INR 1.13 (± 0.3), urea 3.3 (± 1.6) and creatinine 42 (± 18). In the haemotoxic group, the median white cell count was 14.0 (± 5.3), haemoglobin 7.8 (± 3.8), platelets 324 (± 163), INR 3.82 (± 4.0), urea 2.4 (± 3.4) and creatinine 28 (± 56). In the neurotoxic group, the median white cell count was 15.9 (± 2.6), haemoglobin 8.45 (± 3.1), platelets 142 (± 122), INR 1.28 (± 0), urea 3.8 (± 1.8) and creatinine 39 (± 9). Six patients suffered an acute kidney injury (AKI) according to the Kidney Disease - Improving Global Outcomes (KDIGO) classification system (creatinine ≥ 1.5x upper limit of normal) of which five were classified as cytotoxic and the patient with the most severe AKI was classified as haemotoxic. Two patients with an AKI received antivenom, however, both did not develop signs of anaphylactic shock. None of the patients with an AKI developed compartment syndrome or required limb amputation.
Management
A total of 53 out of 274 patients (19%) received antivenom of which 45 were categorised as cytotoxic, six were haemotoxic and two were neurotoxic. On average, six vials of antivenom were administered. Antivenom was administered to 23% of patients with cytotoxic presentations and 100% of patients with haemotoxic and neurotoxic presentations respectively. Of the total number of patients who received antivenom, 25% suffered adverse reactions. Six patients developed allergic reactions of which one patient progressed to anaphylaxis and seven patients developed anaphylaxis. Allergic reactions were considered as mild skin manifestations, e.g., skin rash or urticaria without systemic involvement. Anaphylactic reactions were considered as a drop in blood pressure from baseline, central nervous system deterioration, impalpable radial pulse, signs of airway obstruction and haemodynamic instability, with or without skin manifestations. All patients with hypersensitivity reactions received vasopressor support in the form of adrenaline infusion as well as intravenous fluid administration. One patient subsequently developed
99 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Admission bloods overview WCC (x10⁹/L) Hb (g/dL) Platelets (x10⁹/L) INR Urea (mmol/L) Creatinine (umol/L) Min 1.38 5.40 13.00 0.90 0.9 15 Q1 7.93 10.60 237.00 1.04 2.5 34 Q2 10.00 11.80 308.00 1.12 3.3 43 Q3 13.85 12.80 379.00 1.28 4.0 53 Max 26.10 15.70 987.00 7.10 41.0 688 Mean 11.17 11.59 319.56 1.30 3.8 48 Median 10.00 11.80 308.00 1.12 3.3 43 Range 24.72 10.30 974.00 6.20 40.1 673 IQR 5.93 2.20 142.00 0.24 1.5 19 Std dev 4.62 1.73 139.90 0.69 3.86 48 WCC – white cell count, Hb – haemoglobin, INR – international normalised ratio
Table II: Admission bloods overview
cardiovascular collapse and required cardiopulmonary resuscitation with return of spontaneous circulation. There was no correlation noted between age and the development of hypersensitivity reactions.
Outcome
A total of 56 patients underwent one or more procedures on their affected limbs; 32 patients had a split skin graft, 54 were debrided, two had a fasciotomy and five had belowknee amputations. The cytotoxic group accounted for the majority of procedures performed (Table III). The median time of presentation after bite for the five patients who required amputations was 10 hours (range 18.5 hours). Four of the five patients received antivenom and were below the age of 5 with a median age of 3 years. All patients who required lower limb amputation presented with progressive tissue necrosis and none developed compartment syndrome. Delay in presentation, and therefore antivenom administration, was considered as the most significant contributing factor for the need for limb amputation. Three patients aged 2, 9 and 13 required admission to the ICU of which all were part of the cytotoxic group and received antivenom. Only one of these patients suffered an adverse drug reaction (anaphylaxis), which was treated, and subsequently underwent a debridement and split skin graft of the affected limb. There was no correlation between age and admission to ICU. There were no recorded mortalities during this period.
Discussion
To date, this is the largest series of paediatric snakebites that we are aware of. Studies have shown that children under the age of 15 years are more vulnerable to sustaining snake bites due to inherent curiosity, lack of caution as well as walking barefoot.17 In rural areas, older children are often also involved in outdoor agricultural responsibilities.15,18 Wood et al. reported that children under 12 years were an independent risk factor for the severity of snakebites.19 A study by Campbell et al. in the United States of America reported on a series consisting of 114 cases and the lessons they learned.14 They reported a mean age of 7.3 years and males being more affected at 60%; Arkanas et al. reported similar findings with a mean age of ± 10 years. Kshirsagar et al. also reported a male predominance (60.49%) with a mean age of 9.2 years in males and 8.6 years in females in rural India.20 Our data is in keeping with this trend with a mean age of 7.7 years
and males accounting for 56% of cases. Interestingly they reported only 6% of patients requiring antivenom and only a single case had an anaphylactic reaction.12 In our series, 19% of patients required antivenom and eight had an anaphylactic reaction. Two of their patients required fasciotomies whereas in our data set, with significantly more patients, we also reported two fasciotomies.12 This might stem from our more liberal use of antivenom. In a study performed in a tertiary setting in Texas, United States, antivenom administration was more liberal (34%) with only one (2%) hypersensitivity reaction recorded. Of the 151 patients included in the study, only four (2.6%) required surgical intervention.21 The antivenom most commonly administered in their setting was CroFab, specific to crotaline species, which has been shown to have a low rate of hypersensitivity reactions.21,22
The data on snakebites in Southern Africa is predominantly from the KwaZulu-Natal region and its draining hospitals.6-8,11 There are five main clinical syndromes of snake envenomation recognised in South Africa as described by Müller et al.:
• Marked local pain and progressive swelling associated with prominent cytotoxic skin changes with coagulable blood.
• Progressive paralysis (neurotoxicity), with negligible or minor local swelling.
• Incoagulable blood, with negligible to mild local swelling.
• Moderate to marked local swelling, associated with neurotoxicity.
• Mild to moderate swelling, with negligible or absent systemic symptoms.12
Since there is overlapping of these syndromes, in our data series, we categorised our patients into cytotoxic, haemotoxic, neurotoxic and unclassified.
Wood et al. reported that 98% of their admissions in adults were due to cytotoxic envenomation.11 They reported four cases of haemotoxicity and five cases of neurotoxicity that were admitted.13 In our series 71% presented with cytotoxic manifestations, 2% haemotoxic and 1% neurotoxic, while 26% of patients displayed no features in keeping with any of the latter categories. The similarities to the study conducted by Wood et al. is evident. They also reported that 1/3 (33%) snakebites will have no envenomation symptoms whereas our data series had 26% patients with no symptoms of envenomation.
According to a study conducted in north-eastern Nigeria, the risk of mortality secondary to envenomation increases by 1% for every 1-hour delay between the time of the bite and presentation to medical personnel.23 Kshirsagar et al. reported a mortality rate of 1.85% in a study evaluating paediatric snakebites in rural areas of Maharashtra, India. All patients who demised presented to the hospital > 8 hours after the time of the bite.20 Transport limitations, presentation to traditional healers prior to seeking conventional medical treatment and increasing distance from healthcare facilities may play a role in delayed presentation.18,24 In our study, the median time of presentation to the hospital after the time of the bite was 7 hours with an IQR of 9 hours compared to 1.5 hours in an urban area in Taiwan.25 This may be attributed to the fact that many of the patients in our study come from surrounding rural areas that do not have access to transport which may contribute to the delayed presentation. This may
100 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Cytotoxic Procedure n (%) Split skin graft 28 (10) Debridement 48 (18) Fasciotomy 1 (0.4) Amputation 5 (0.8) Haemotoxic Split skin graft 3 (1.1) Debridement 3 (1.1) Fasciotomy 1 (0.4) Neurotoxic Debridement 2 (0.7)
Table III: Procedures performed for children with snakebites
increase the risk for severe envenomation and therefore mortality.
In our study, the INR median was 1.13 (± 0.3) in the cytotoxic group, 3.82 (± 4) in the haemotoxic group and 1.28 (± 0) in the neurotoxic group. The median INR is significantly higher in the haemotoxic group as expected; however, due to the low number of haemotoxic (6) and neurotoxic (2) patients it is difficult to draw a definitive conclusion. The median haemoglobin was also significantly lower (< 11 g/dL) in the haemotoxic group followed by the neurotoxic group. This finding is in keeping with the results reported by Hernandez et al.26 The median white cell count was highest within the neurotoxic group. Of note is that there was a low rate (2.2%) of acute kidney injury in our study. These occurred mostly within the cytotoxic group and one within the haemotoxic group. In comparison to a study conducted amongst adults in India, the rate of AKI was significantly higher (21.1%). Similarly, the predominating syndromes associated were cytotoxic and haemotoxic.27
Isbister et al. reported a study in which antivenom was most administered due to presence of coagulopathy followed by non-specific manifestations and neurotoxicity. In this study, 25% of patients who received antivenom suffered from hypersensitivity reactions, of which 44% were classified as anaphylaxis.28 In comparison to our study, of the 53 patients who received antivenom, 45 suffered cytotoxic envenomation equating to 23% of all patients with cytotoxic envenomation as compared to 100% of haemotoxic and neurotoxic patients who received antivenom. In comparison to the study conducted by Isbister et al., hypersensitivity reactions were noted in 23% of our patients who received antivenom, of which 62% were classified as anaphylaxis.
Hernandez et al. reported a study analysing the surgical considerations in paediatric snake bites conducted at Pietermaritzburg Metropolitan Trauma Service.26 This study included 72 patients below the age of 18 years of which a total of nine patients (12.5%) received antivenom and two subsequently developed anaphylaxis and were admitted to ICU. In total, ten patients (14%) were admitted to ICU of which seven were classified as cytotoxic (11% of all cytotoxic admissions), one neurotoxic (20% of neurotoxic admissions) and two haemotoxic (50% of haemotoxic admissions).26 In comparison to our study in a similar setting, 19% of patients received antivenom and a total of three patients (1.1%) required ICU admission for further monitoring following the administration of antivenom due to severe envenomation of which only one patient developed anaphylaxis and required surgical intervention to the affected limb. All three patients suffered from cytotoxic envenomation.
Hernandez et al. reported 5.5% of patients requiring subsequent debridement compared to 20% of the patients included in our study.26 Seven per cent of patients had a split skin graft at their facility compared to 11% at Ngwelezana Hospital. They also report 18 fasciotomies (25%) done as compared to two fasciotomies performed at Ngwelezana Hospital (0.7%).17 This may be explained by the higher number of patients who received antivenom at Ngwelezana Hospital as well as less delay in presentation. This is supported by the median time of presentation after injury at Pietermaritzburg of 20 hours compared to 7 hours at Ngwelezana Hospital.26 Only one amputation was reported at Pietermaritzburg (1.4% incidence) compared to five amputations performed at Ngwelezana Hospital
(1.8% incidence).26 There was an increase in median time of presentation after bite of 10 hours in the group of patients who had amputations compared to the overall sample population. Interestingly, four of the five patients who underwent amputations were below the age of 5. Severe envenomation is more likely in children due to their smaller body mass and this can explain the need for amputation in these very young children. Amputations pose a detrimental impact on the psychological and physical well-being of children. The ongoing growth within the residual limb and abnormal residual stump shape also poses an additional challenge with prosthetic rehabilitation.29 Approximately 89% of procedures performed at Ngwelezana Hospital were for patients with cytotoxic envenomation, including all five amputations.
In a study comparing snakebites between the paediatric and adult populations, Tekin et al. reported a mortality rate of 0.8% amongst children.30 There were no recorded mortalities in our study. This may be an indicator of effectiveness of our current management principles.
Conclusion
Paediatric snakebites are a significant burden on the health system of Southern Africa. Most snakebites in paediatric patients are cytotoxic in nature. As much as one-fifth (20%) of the paediatric population may require antivenom as well as a surgical procedure post envenomation. Adverse effects post antivenom use are common but manageable without risk of major morbidity or mortality. Snakebites in this population subgroup should be deemed as severe and extreme caution should be exercised when administering antivenom.
Prevention programmes are needed to help reduce this burden of disease and a nationwide snakebite registry is long overdue.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval for the study was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (Ref. No.: BE034/14).
ORCID




JJP Buitendag https://orcid.org/0000-0001-7169-129X
S Variawa https://orcid.org/0000-0001-7672-1259
D Wood https://orcid.org/0000-0002-3151-5651
G Oosthuizen https://orcid.org/0000-0002-6936-5716
REFERENCES
1. Gutiérrez JM. Improving antivenom availability and accessibility: science, technology, and beyond. Toxicon. 2012;60(4):676-87. https://doi.org/10.1016/j.toxicon.2012.02. 008.
2. Kasturiratne A, Wickremasinghe AR, De Silva N, et al. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Full list of references available on request.
101 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
https://doi.org/10.17159/2078-5151/2021/v59n3a3474
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]




http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361
An audit of patients clinically deemed as high risk for malignant breast pathology at the Helen Joseph Hospital Breast Clinic
H-M
Brink,1 G Rubin,2 C-A Benn,3 S Lucas4
1 Department of Diagnostic Radiology, University of the Witwatersrand, South Africa
2 Department of Radiology, Helen Joseph Hospital, South Africa
3 Breast Surgical Unit, Helen Joseph Hospital, South Africa
4 Department of Radiology, Chris Hani Baragwanath Academic Hospital, South Africa
Corresponding author, email: heilabrink@gmail.com
Background: The Helen Joseph Hospital Breast Clinic has implemented a clinical triage system for patients presenting with a variety of breast concerns. The goal of this system is to expedite the process from initial presentation to radiological assessment of patients with suspected breast malignancy or breast abscess in a resource limited setting. The objective was to assess the clinical, imaging and histological diagnoses of breast disease in these patients with malignancy and sepsis. Methods: A retrospective audit of patients clinically deemed high risk for malignant breast pathology referred to the breast imaging unit (BIU) in 2018. Patients were triaged based on strict clinical criteria: presence of a breast mass with or without lymph nodes or a breast abscess. Patients that were subsequently referred for mammography/ultrasound were identified using the patient files in the BIU. Results were recorded on Microsoft Excel and analysed using SAS version 9.2.
Results: Three hundred and twenty-five patients were included in this study. Eighty-seven (26.8%) were diagnosed with breast cancer and 236 (72.6%) with benign disease. The most common presenting complaint was a palpable mass (n = 227; 69.9%). Ninety-five per cent of patients characterised as BI-RADS 5 had malignant disease. 55.8% of malignancies diagnosed on ultrasound had locally advanced disease. The most common histological diagnosis of malignancy was invasive ductal carcinoma (n = 67, 77%). The most commonly diagnosed benign disease was breast abscess (n = 42, 17.8%).
Conclusion: BI-RADS findings correspond to similar studies, however, a large number of benign breast disease was diagnosed. This may indicate heightened clinical awareness of breast cancer diagnosis and early detection. A significant percentage of malignancies presented as locally advanced. Except for a lower number of invasive lobular carcinoma, the histological spectrum of malignant disease is similar to comparative studies.
Keywords: malignant breast pathology, high risk patient, Helen Joseph Hospital Breast Clinic
Introduction
The Helen Joseph Hospital Breast Clinic has implemented a clinical triage system for patients who present at the breast clinic. This is an open access clinic where any patient with a breast concern is seen. Patients are triaged into three groups according to strict clinical criteria: high-, intermediate-, and low-risk cases.
Low risk includes patients with no clinical suspicion of breast disease – asymptomatic patients presenting for screening. Intermediate risk includes patients with unilateral breast pain, a breast mass deemed clinically benign, nonspontaneous nipple discharge, or palpable lymph nodes but no breast involvement.
High risk includes any patient with a breast mass that has a clinical suspicion of malignancy, with or without palpable axillary lymph nodes, or an acute breast collection/abscess. Even though patient age is not part of the triage protocol, patients with increased age are deemed more likely to have
malignant breast disease and are more often referred in this high-risk category. This is at the referring clinician’s discretion. These patients are referred to the Helen Joseph Breast Imaging Unit (BIU) for urgent imaging and, if necessary, intervention within seven days from presentation. The goal of this triage system is to expedite the process from initial presentation to diagnosis and the timeous management for any patient with a suspicion of breast malignancy. It also aims to decrease the patient burden on the BIU in a resource limited setting and it standardises the referral criteria for clinicians across varying levels of experience. Breast abscesses and other acute breast collections are added to this group as they require urgent intervention.
The aim of this study was to conduct an audit to assess the spectrum of breast disease clinically deemed high risk for malignant breast pathology, their clinical and imaging features, and their final histological diagnosis.
102 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
BREAST DISEASE
© 2021 The Author(s)
Journal
Surgery.
South African
of
2021;59(3):102-107
Context
Even though the incidence of breast cancer in Africa is low in comparison to other countries, the related morbidity and mortality is as high, or even higher, than developed countries.1
A recent Ghanaian study reviewed 330 histologically proven breast cancer patients. The peak incidence of diagnosis of breast cancer was in the age group of 40–49 years.2 This is in keeping with multiple other studies done in sub-Saharan Africa,3-5 which showed that patients in this region present at the pre- and perimenopausal stage, versus high-income countries where the majority of patients present postmenopausal.6,7 The different presenting complaints that were subsequently diagnosed as histologically confirmed breast malignancy were also noted. The most common presenting complaint was a breast lump (75.2%).2
Invasive ductal carcinoma (IDC) was the most common histological subtype identified (82.1%). This is in keeping with the trend elsewhere in Africa, Europe and worldwide.8
The Breast Imaging-Reporting and Data System (BIRADS) system of reporting for breast disease aims to standardise mammography and ultrasound reports.9 An American study done in 2018, which focused on a majority African American demographic, studied the correlation between the mammographic BI-RADS category compared to the histological diagnosis. Breast cancer was diagnosed in 0.03% of patients with a BI-RADS grade of 1–3, 29% of patients reported as BI-RADS 4, and 89.7% of patients reported as BI-RADS 5.10
No previous research has been done to assess this population’s specific burden of disease, highlighting the need for the study in this context.
Objective
The primary objective was to analyse the spectrum of imaging findings of the patients clinically deemed as high risk for malignant breast pathology at the Helen Joseph BIU. The secondary objective was to document the associated clinical and relevant laboratory findings.
Materials and methods
Research paradigm
A retrospective audit of imaging findings of patients clinically deemed high risk and for immediate breast imaging.
The patients who were referred to the Helen Joseph BIU from 1 January to 30 June 2018 and who were clinically deemed as high risk for malignant breast pathology and seen at the Helen Joseph Hospital BIU were considered. Patients with illegible records or missing imaging findings were excluded.
Files and records at the Helen Joseph Hospital BIU were accessed. The National Health Laboratory Services (NHLS) online database was accessed in order to obtain the relevant histology/HIV/MC&S results.
The data was collected using a pre-formulated data collection sheet and entered into a Microsoft Excel spreadsheet. Each patient was allocated a study number and only this number was linked to the patient’s personal identifiable information.
A triage book is kept at the Helen Joseph Hospital BIU which contains the names and hospital numbers of each
patient who is booked at the imaging unit as well as their triage status.
Each patient has a corresponding file that contains their imaging request form, imaging report, history questionnaire and a biopsy information sheet.
The triage book was used to identify the patients seen and triaged as high risk from 1–30 June 2018. The corresponding mammography files were then accessed to obtain their demographics, clinical history, imaging findings and histology results. This unit’s practise is that every patient should receive a mammogram, except in the following cases: patients who are younger than 35 years of age start with ultrasound imaging and only if deemed necessary and appropriate are then referred for mammography; patients with painful or ulcerative breast pathology where mammography would cause too much discomfort for the patient; and patients who are physically unable to be positioned for mammography, for instance, bed-ridden patients.
The patient’s HIV status was documented either from the request form, the history questionnaire or the NHLS online database. If no results were found for a 6-month window period prior to the patient’s clinic date, the patient was determined as HIV “unknown”.
Data analysis and statistics
Data was captured electronically in Microsoft Excel. Further analysis was done using SAS Version 9.2. Descriptive statistics namely frequencies and percentages were calculated for categorical data. Means and standard deviations or medians and percentiles were calculated for numerical data. The Shapiro–Wilk test was used to investigate if numerical data followed a normal distribution. A significance level p-value of 0.05 was used.
Results
Seven hundred and sixty patients were identified as high risk from the triage book, however several patient files were not found. The large number of missing patient files could be due to a variety of factors: if patients presented for followup appointments subsequent to their initial booking date, they were given a new file number which made the tracing of these patients’ information difficult. A large number of patients also defaulted on their appointment dates, and some files were erroneously labelled as high risk, but were, in fact, patients presenting for annual screening – these patients were also excluded. Three hundred and thirty-four (334) patients with imaging were identified during the study period and nine of these patients were excluded from the study due to indecipherable imaging reports. The total number thus included was 325.
Demographics and presenting complaints
Table I depicts the patient demographics. Added are their presenting complaints and type of imaging obtained. Percentages of benign versus malignant disease are given. Two patients were not confirmed to have either malignant or benign disease as there was no histology for correlation, but these patients were suspected to have malignant disease based on their imaging features. These patients are added in the ‘unknown’ column.
The majority of patients were female (96.6%). All male patients were diagnosed with benign disease. The most common presenting complaint was a palpable mass for
103 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
both benign and malignant disease. The median age of malignancies was 57, which was higher than for benign disease of 41.
Imaging findings
Tables II and III demonstrate the different imaging findings on mammography and ultrasound with comparison between malignant and benign disease. Of the patients who had masses present on mammography, 58.6% were malignant. This accounted for 78.2% of the total number of malignancies. All of the patients who had malignant masses on mammography (54/87 of malignancies) also presented with identifiable masses on ultrasound. 86/87 of malignancies had masses on ultrasound. The one patient with biopsy proven malignancy who did not have an identifiable mass on ultrasound presented with suspicious microcalcifications on mammography and no mass.
Spiculation was the most common border characteristic of the malignant masses (30.9%) on mammography. Forty (40) (52.6%) of malignancies on mammography had suspicious microcalcifications.
In Table III, we can see that 86 (51.5%) of masses seen on ultrasound proved to be malignant.
Only 65 out of these 86 patients with malignant masses had a size documented on ultrasound, of which 49 (75.3%) were larger than 2 cm and 12 (18.5%) larger than 5 cm. Thus, 61 out of 65 (93.8%) of presenting masses were larger than 2 cm. The majority of poorly circumscribed masses identified on ultrasound were malignant (88.2%).
Axillary adenopathy was present on ultrasound in 57 of the 86 (66.2%) patients presenting with malignancy. Of these 57 patients, 48 had malignant infiltration of their ipsilateral axillary nodes on ultrasound. Thus, 55.8% of patients presenting with breast carcinoma had ipsilateral malignant axillary nodal involvement. Of note is that most patients with malignant lymphadenopathy (35/48; 72.9%)
104 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Malignant Benign Unknown Total (% of total patients) Sex Male 0 11 (100%) 0 11 (3.4%) Female 87 (27.7%) 225 (71.7%) 2 (0.6%) 314 (96.6%) Age (median) Median = 46 57 41 54 HIV status Negative 32 (23.7%) 102 (75.6%) 1 (0.7%) 135 (41.5%) Positive 7 (13.5%) 45 (86.5%) 0 52 (16%) Unknown 48 (34.8%) 89 (64.5%) 1 (0.7%) 138 (42.5%) Presenting complaint Palpable mass 80 (35.3%) 146 (64.3%) 1 (0.4%) 227 (69.9%) Nipple discharge 1 (10%) 9 (90%) 0 10 (3.1%) Lump in armpit 1 (11.1%) 8 (88.9%) 0 9 (2.8%) Breast pain 5 (7.9%) 58 (92.1%) 0 63 (19.6%) Breast erythema 0 2 (100%) 0 2 (0.6%) Skin thickening 0 1 (100%) 0 1 (0.3%) Metastatic disease 0 5 (83.3%) 1 (16.7%) 6 (1.9%) Breast cancer in remission 0 5 (100%) 0 5 (1.5%) Other 0 2 (100%) 0 2 (0.6%) Type of imaging Mammography 76 (35.7%) 136 (63.9%) 1 (0.5%) 213 (65.5%) Ultrasound 87 (26.8%) 236 (72.6%) 2 (0.6%) 325 (100%) Malignant Benign Unknown Number of patients BI-RADS 1 2 3 4 5 6 140 120 100 80 60 40 20 0 0 0 0 0 0 0 0 0 1 2 2 9 25 40 38 77 125 0
Table I: Patient demographics
IDC DCIS Papillary Phylloides Lymphoma ILC Mucinous Histological type Number of patients n = 67.77% n = 8, 9.2% n = 5, 5.7% n = 2, 2.3% n = 2, 2.3% n = 2, 2.3% n = 1, 1.1% 0 10 20 30 40 50 60 70 Figure 2:
spectrum of malignant disease
Figure 1: BI-RADS imaging findings
Histological
Table II: Imaging findings on mammography
presented with multiple suspicious ipsilateral axillary lymph nodes.
Figure 1 compares the BI-RADS imaging findings with malignant versus benign disease. Ninety-five per cent of breast lesions that were assessed as BI-RADS 5 proved to be malignant. The two patients with BI-RADS category 5 imaging and reportedly benign histology had suboptimal biopsy results with no representative histology of the lesion.
Spectrum of disease
Figure 2 depicts the histological spectrum of malignant disease. IDC formed the majority of the malignancies (77%). The most commonly diagnosed benign breast disease was breast abscesses (n = 42, 17.8%) followed by normal imaging
findings (n = 35, 14.8%) and fibroadenomas (n = 29, 12.3%). Of the 42 diagnosed breast abscesses, 19 (45.3%) patients were HIV negative, six (14.3%) patients were HIV positive, and 17 (40.5%) patients had unknown HIV status.
Discussion
The Helen Joseph Hospital Breast Clinic has a triaging system allowing for timeous breast imaging referral and management of patients with suspected breast cancer. This aims to standardise the referral criteria for any clinician examining a patient with a breast concern. We initially expected to see a large majority of malignancies in this study, however, the majority proved to have benign disease. This is likely due to a high concern and awareness of the early
105 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Mass present Malignant Benign Total 68 (58.6%) 48 (41.4%) 116 Number of masses 1 50 (60.2%) 33 (39.8%) 83 2 7 (63.6%) 4 (36.4%) 11 3 1 (100%) 0 1 > 3 9 (50%) 9 (50%) 18 Mass size < 20 mm 4 (57.1%) 3 (42.9%) 7 20–50 mm 10 (83.3%) 2 (16.7%) 12 > 50 mm 5 (83.3%) 1 (16.7%) 6 Mass shape Round 2 (14.3%) 12 (85.7%) 14 Oval 0 1 (100%) 1 Irregular 3 (100%) 0 3 Breast density a 16 (32%) 34 (68%) 50 b 20 (37.7%) 33 (62.3%) 53 c 11 (25.6%) 32 (74.4%) 43 d 2 (25%) 6 (75%) 8 Calcifications No suspicious 24 (22.6%) 82 (77.4%) 106 Suspicious 40 (93%) 3 (7%) 43 Benign 4 (8.3%) 44 (91.7%) 48 None 1 (25%) 3 (75%) 4 Borders Circumscribed 6 (17.7%) 28 (82.3%) 34 Obscured 5 (71.4%) 2 (28.6%) 7 Microlobulated 14 (87.5%) 2 (12.5%) 16 Indistinct 14 (82.4%) 3 (17.6%) 17 Spiculated 21 (95.5%) 1 (4.5%) 22 Architectural distortion Yes 33 (66%) 17 (34%) 50 No 11 (10.4%) 95 (89.6%) 106 Associated features Trabecular thickening 1 (50%) 1 (50%) 2 Skin thickening 46 (68.7%) 21 (31.3%) 67 Intramammary nodes Yes 2 (22.22%) 7 (77.78%) 9 No 74 (36.5%) 129 (63.5%) 203 Axillary nodes Yes 22 (81.5%) 5 (18.5%) 27 No 54 (29.2%) 131 (70.8%) 185
Table III: Imaging findings on ultrasound
diagnostic value of breast cancer as well as an indication of the spectrum of clinical experience in an academic teaching hospital. There is also a large number of patients suspected of having a breast abscess attending the breast clinic, and these are referred for imaging and immediate management.
The majority of patients included in the study were females (n = 314, 96.6%). Only 11 males were included, of which 100% were diagnosed with benign disease. Global and local trends show that male breast cancer comprises less than 1% of diagnosed breast malignancies.11,12 The lower rate in this study may be due to the low number of male patients who were seen during the study period.
The median age of patients diagnosed with breast malignancy was 57, with the largest number of patients presenting
between 60–69. Interestingly, this is out of keeping with findings in several other sub-Saharan African studies where the peak incidence of breast cancer was in pre- and perimenopausal patients.3-5 This appears more in keeping with peak incidences in high income countries6,7 where women were of post-menopausal age.
The most common presenting complaint was a breast lump. This included 69.9% of all patients and 92% of malignancies. This is in keeping with a recent study done in Kumasi, Ghana, in which they showed that of 330 patients with histologically proven malignancies, 75.2% presented with breast lump.2
The majority of patients with breast malignancy had a mass present on ultrasound and mammography. It is worth noting
106 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Mass present Malignant Benign Total 86 (51.5%) 81 (48.5%) 167 Mass size < 20 mm 16 (28.6%) 40 (71.4%) 56 20–50 mm 37 (61.7%) 23 (38.3%) 60 > 50 mm 12 (75%) 4 (25%) 16 Number of masses 1 62 (53%) 55 (47%) 117 2 10 (62.5%) 6 (37.5%) 16 3 3 (60%) 2 (40%) 5 > 3 9 (36%) 16 (64%) 25 Margin Circumscribed 8 (14.8%) 46 (85.2%) 54 Not circumscribed 60 (88.2%) 8 (11.8%) 68 Echo pattern Anechoic 0 1 (100%) 1 Hyperechoic 4 (25%) 12 (75%) 16 Complex cystic/solid 3 (42.9%) 4 (57.1%) 7 Hypoechoic 44 (57.1%) 33 (42.9%) 77 Isoechoic 0 2 (100%) 2 Heterogenous 5 (55.6%) 4 (44.4%) 9 Posterior features None 0 2 (100%) 2 Enhancement 0 6 (100%) 6 Shadowing 15 (83.3%) 3 (16.7%) 18 Combined 2 (100%) 0 2 Vascularity Yes 1 (100%) 0 1 No 4 (80%) 1 (20%) 5 Collection Yes 1 (2.3%) 42 (97.7%) 43 No 84 (30.6%) 191 (69.4%) 275 Calcifications Yes 9 (69.2%) 4 (30.8%) 13 No 2 (11.1%) 16 (88.9%) 18 Architectural distortion Yes 2 (50%) 2 (50%) 4 No 1 (5.9%) 16 (94.1%) 17 Oedematous Yes 6 (20%) 24 (80%) 30 No 3 (27.3%) 8 (72.7%) 11 Axillary LN Yes 57 (70.4%) 24 (29.6%) 81 No 30 (12.5%) 210 (87.5%) 240
that of the 65 malignant masses measured on ultrasound, 49 (75.3%) were greater than 2 cm. Metastatic nodes were seen on ultrasound in 48/86 (55.8%) of malignancies and 35 (40.7%) had multiple ipsilateral metastatic nodes. This would indicate that at least 55.8% of malignancies diagnosed on ultrasound had locally advanced disease based on imaging features.
Ninety-five per cent of patients characterised as BIRADS 5, and 20.8% of patients characterised as BI-RADS 4 proved to have malignant disease. This is in keeping with an American study that was done in 2018 which focused on a majority African American demographic. The study compared the correlation between the mammographic BIRADS category given in reports versus the final histological diagnosis. It was found that 29% of patients reported as BI-RADS 4 and 89.7% of patients reported as BI-RADS 5 were diagnosed with malignancy.10 This also corresponds to another recent Ghanaian study, where out of 54 histologically proven malignancies, 85.2% of patients had findings in keeping with BI-RADS 4 and 5.13 IDC (67, 77%) comprised the majority of diagnosed breast malignancies, followed by ductal carcinoma in situ DCIS (8, 9.2%). This is in keeping with the previously mentioned study done in Kumasi, Ghana where the different histological types of breast cancer were given.2 Out of 340 patients, 82.1% proved to have IDC. Another study done in the Central African Republic in 2018 also showed IDC to be the most common tumour at 64.9%, followed by invasive lobular breast cancer (ILC) (9.8%).14 ILC constituted only 2.3% of patients in our study, which was lower than in the above comparison studies.
Breast abscesses were the most common benign condition. This was expected as these patients are referred for immediate intervention. A large number of patients presented with lactational breast abscesses. A recent Zambian study found that HIV infection was a significant risk factor for developing lactational breast abscesses.15 In our study, only 14.3% of the total number of breast abscesses were known to be HIV positive. This could be due to a large number of the patients (40.5%) presenting as HIV unknown. The second most common finding was normal imaging. This highlights the difficulties faced in assessing breast disease if clinical examination alone is used.
Study limitations
A large number of patients had unknown HIV status due to difficulty in tracing results.
The majority of benign breast disease results are not biopsy proven, as BI-RADS 1–3 diagnoses commonly do not require biopsy according to the BI-RADS management guidelines. Some imaging occult malignancies may have been missed.
Self-identified race was not available from the patient files at the BIU – this limits the appropriate comparison to patient groups in comparison studies.
Another limiting factor is the low number of biopsyproven malignant disease. This could partly be due to the large number of missing files from the initially identified number of high-risk patients.
Future applications
It was interesting to note that all of the masses that were seen mammographically were also identified on ultrasound. This
would be valuable for a further study considering ultrasound as a possible screening tool for clinically suspicious masses in resource limited settings.
There were several missing files from the initially identified study sample. A large percentage of this is due to the filing system in the department as new file numbers are given to follow-up patients. This can be further assessed to possibly keep original file numbers regardless of the number of visits to aid future research in this department. Many patients also defaulted on their mammography appointments. Patients should be counselled regarding the importance of followup appointments at the initial clinical assessment. A large number of imaging reports did not comment on the relevant BI-RADS imaging categories. This can be highlighted and encouraged in mammography training. This is a study of a single centre breast unit triage system. Subsequent studies, with comparison to other triage systems, are needed and may highlight changes that should be implemented. This triage system does, however, significantly decrease the burden of the radiology department in a resource limited setting and can be considered for implementation in other centres.
Conclusion
This is an index study of a breast clinic triaging system. BIRADS imaging findings largely correspond to other similar studies, however, a large number of benign breast disease was diagnosed in this study. This requires ongoing evaluation of the triaging system, but highlights that clinical evaluation of breast disease requires imaging and biopsy. Clinical presentation of breast malignancy at our centre corresponds to other comparative studies with the majority of patients presenting with palpable breast masses. A large number of our patients presented with locally advanced breast malignancy based on imaging. The histological spectrum of malignant breast disease is similar to the available literature, however, we saw a lower number of ILC. A large number of imaging reports did not report on the relevant BI-RADS imaging categories. This should be further encouraged during mammography training.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The study was approved by the Human Research Ethics Committee of the University of the Witwatersrand, approval number M190675.
ORCID




H-M Brink https://orcid.org/0000-0002-8359-6393
G Rubin https://orcid.org/0000-0001-8435-3521
C-A Benn https://orcid.org/0000-0002-4777-4316
S Lucas https://orcid.org/0000-0002-0378-183X
REFERENCES
1. Forouzanfar MH, Foreman KJ, Delossantos AM, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378(9801):1461-84.
Full list of references available on request.
107 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
South African Journal of Surgery. 2021;59(3):108-112 https://doi.org/10.17159/2078-5151/2021/v59n3a3364
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0] http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361






© 2021 The Author(s)
The surgical burden of breast disease in KwaZulu-Natal province
VU Ehlers,1 CF Kohler,1 E Lutge,2,3 A Tefera,2 DL Clarke,1,4 I Buccimazza5
1 Department of Surgery, Pietermaritzburg Metropolitan Hospital Complex, KwaZulu-Natal Department of Health, South Africa
2 Epidemiology Unit, KwaZulu-Natal Department of Health, South Africa
3 School of Nursing and Public Health, University of KwaZulu-Natal, South Africa
4 Department of Surgery, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, South Africa
5 Department of Surgery, Inkosi Albert Luthuli Hospital, KwaZulu-Natal Department of Health, South Africa
Corresponding author, email: ehlers.vincent@gmail.com
Background: The current surgical workload assessments in KwaZulu-Natal (KZN) are inadequate to inform strategies to improve surgical services. Breast diseases have a well-defined spectrum and surgical treatment options, analysis of which could guide health policy in the field. This project aimed to quantify and analyse the operative workload for breast pathology in KZN.
Method: A retrospective review of breast-related operations conducted at public sector hospitals in KwaZulu-Natal province between 1 July and 31 December 2015 was undertaken. Data was collected from theatre operative registers and manually categorised as follows: sepsis, benign pathology, malignant pathology, and by hospital, according to geographic location, and complexity of care to determine factors to improve the service for breast care in the province.
Results: In the 6-month study period, 13 282 general surgical procedures were performed of which 776 (5.8%) were breast-related operations. There were 372 (47.9%) operations for breast sepsis, 140 (18%) for benign breast lesions, 17 (2.2%) for cosmetic indications and 27 (3.5%) for diagnostic procedures. There were 223 (28.7%) procedures for nonbenign disease: 21 (2.6%) wide local excisions (WLE), 203 (26.2%) mastectomies of which 161 (72.2%) mastectomies had an axillary lymph node dissection and 26 (11.7%) were performed as onco-plastic procedures. Hospitals in the Durban and Pietermaritzburg metropolitan areas performed 75% of the breast-related procedures. The majority (69.6%) of sepsis-related procedures were performed at secondary/regional facilities, while 58.3% of non-benign breast surgeries were performed at tertiary and quaternary centres.
Conclusion: Breast sepsis accounts for almost 50% of the surgery and is mainly dealt with at hospitals above district level. One-third of breast surgery in KZN province is for non-benign disease. There is a paucity of breast-conserving surgery. Elucidation of these observations can guide improvement in the provincial breast care service.
Keywords: breast surgery, breast pathology, breast cancer, general surgery
Introduction
Low- and middle-income countries (LMICs), specifically in sub-Saharan Africa, have a deficit in health services and systems’ research. The lack of evidence results in difficulties in creating surgical plans and research agendas, while further increasing the risk of services being inefficient or ineffective.1,2 South Africa faces a complex mix of surgical disease, which includes emergency surgery, trauma, benign surgical conditions and surgical oncology. There are also a number of long-term trends which impact the management of this burden.3,4 These include the increasing degree of surgical sub-specialisation within what was once considered “general surgery” as well as the need for multidisciplinary teams of surgeons, oncologists, radiologists and pathologists to appropriately coordinate the treatment of surgical oncology.5 These trends have directly impacted the management of breast pathology, which itself covers a spectrum of conditions ranging from benign to malignant. The assessment of breast disease is difficult as malignant conditions need to be identified and this may require access to sophisticated imaging and diagnostic services. In addition,
malignant disease requires treatment algorithms involving access to advanced oncological therapeutic services. Some benign conditions may also require ongoing access to these advanced services. This makes planning for breast services complex, and for these reasons it is imperative that reliable data regarding the burden of breast pathology be captured to facilitate planning. In light of the above, this paper focuses on surgery for breast-related conditions and aims to quantify the operative workload for breast related pathology in the province of KwaZulu-Natal (KZN) over a six-month period, and to grade the type of procedures according to complexity, indication and geographical distribution. It is hoped that this data may provide evidence to support the ongoing development of breast care services in the province.
Clinical setting
KZN province is situated on the eastern seaboard of South Africa and has an area of 94 361 km2 and a population of just over 10 million people. It has a densely inhabited coastal area around the port city of Durban as well as a number of other urban conurbations namely Pietermaritzburg, in the
108 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
BREAST DISEASE
midlands, the Ladysmith/Newcastle area in the north west and a large port at Richards Bay, two hours north of Durban. However, about half of the population is rural and lives in districts with high poverty and inequality indices. There are 37 district hospitals, 12 regional hospitals, three tertiary hospitals and a single central quaternary centre in the province. Only two dedicated Breast Units exist in the province: one in Durban at Inkosi Albert Luthuli Central Hospital and the other at Grey’s Hospital in Pietermaritzburg. The units offer a full spectrum of diagnostic and surgical breast services. In patients with breast cancer, weekly multidisciplinary team meetings determine the sequence and type of multimodal treatment. Advanced oncoplastic surgery techniques are available for all patients requiring breast-conserving surgery or mastectomy with immediate reconstruction. The Breast Units are largely ambulatory diagnostic services which assess the full spectrum of breast pathology. The exception is puerperal breast sepsis that is seen at emergency departments and treated by general surgeons across the province.
It is recommended that breast cancer surgery be centralised, while breast sepsis and some benign lumpectomies can be performed by surgical departments throughout the province.
Methods
This is a retrospective review of operations for breast pathology that were conducted at all regional, tertiary and a single quaternary hospital in the public sector of KZN province for the period 1 July–31 December 2015. Data was collected from operating theatre registers for this period. The variables collected included: the district in which the hospital is placed, the name of the operation, the date of the operation and the indication or outcome of operation if available. The data was entered into an Excel database and manually categorised by the primary authors. For the purpose of this review, all procedures involving the term ‘breast’ were included and subsequently categorised for analysis under the following categories: breast-related sepsis, benign mass removal, diagnostic procedures, treatment of nonbenign breast disease and level of facility.
Statistics
The data were quantitatively analysed and reported using non-parametric descriptive statistics. To gain an overview of the spectrum of disease and proportion of major subgroups within the sample, the frequency distribution of categories was reflected using percentages.
109 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Name of hospital Level Total breastrelated procedures (n = 776) Breast sepsis procedures (n = 372) Non-benign surgical interventions (n = 223) Benign breast procedures (n = 140) Cosmetic procedures (n = 15) Diagnostic procedures (n = 16) Inkosi Albert Luthuli Quaternary 78 (10.1%) 1 (0.3%) 49 (22%) 13 (9.3%) 10 (66.7%) 2 (12.5%) King Edward Tertiary 145 (18.7%) 61 (16.4%) 31 (13.9%) 47 (33.6%) 2 (13.3%) 5 (31.3%) Ngwelezane Tertiary 78 (10.1%) 48 (12.9%) 12 (5.4%) 13 (9.3%) 1 (6.2%) Grey’s Tertiary 50 (6.4%) 3 (0.8%) 38 (17%) 6 (4.3%) 2 (13.3%) 0 Addington Regional/ Secondary 128 (16.5%) 82 (22%) 40 (17.9%) 4 (2.9%) 0 0 RK Khan Regional/ Secondary 83 (10.7%) 43 (11.6%) 15 (6.7%) 21 (15%) 0 3 (18.8%) Stanger Regional/ Secondary 67 (8.6%) 59 (15.9%) 1 (0.4%) 5 (3.6%) 1 (6.7%) 1 (6.2%) Edendale Regional/ Secondary 63 (8.1%) 28 (7.5%) 24 (10.8%) 11 (7.9%) 0 0 Prince Mshiyeni Regional/ Secondary 35 (4.5%) 18 (4.8%) 4 (1.8%) 10 (7.1%) 0 3 (18.8%) Ladysmith Regional/ Secondary 34 (4.4%) 20 (5.4%) 9 (4%) 5 (3.6%) 0 0 Port Shepstone Regional/ Secondary 12 (1.5%) 6 (1.6%) 0 5 (3.6%) 0 1 (6.2%) Queen Nandi Regional/ Secondary 2 (0.3%) 2 0.5%) 0 0 0 0 Madadeni Regional/ Secondary 1 (0.1%) 1 (0.3%) 0 0 0 0 Mohatma Gandhi Regional/ Secondary 0 0 0 0 0 0 Newcastle Regional/ Secondary 0 0 0 0 0 0 St Aidens Regional/ Secondary 0 0 0 0 0 0 Total 776 372 233 140 15 16
Table I: The distribution of breast surgery across KwaZulu-Natal quaternary, tertiary and regional hospitals
Results
During the six-month study period, 13 282 general surgical procedures were performed in KZN province. Seven hundred and seventy-six (5.8%) were for breast-related procedures. Table I summarises the indications for breast surgery in the province.
Geographic and hospital distribution
The majority of operations related to breast pathology were concentrated around the major cities of Durban, Pietermaritzburg and Richard’s Bay. Five facilities in the greater Durban region contributed 60.5% of breast-related
procedures, followed by 14.5% from the two facilities in Pietermaritzburg, and 10.4% from the two facilities near Richard’s Bay. Three regional hospitals did not perform any breast operations during the study period. Quaternary and tertiary hospitals performed the majority (58.3%) of nonbenign breast surgeries, while the secondary institutions performed the majority (69.6%) of sepsis-related operations.
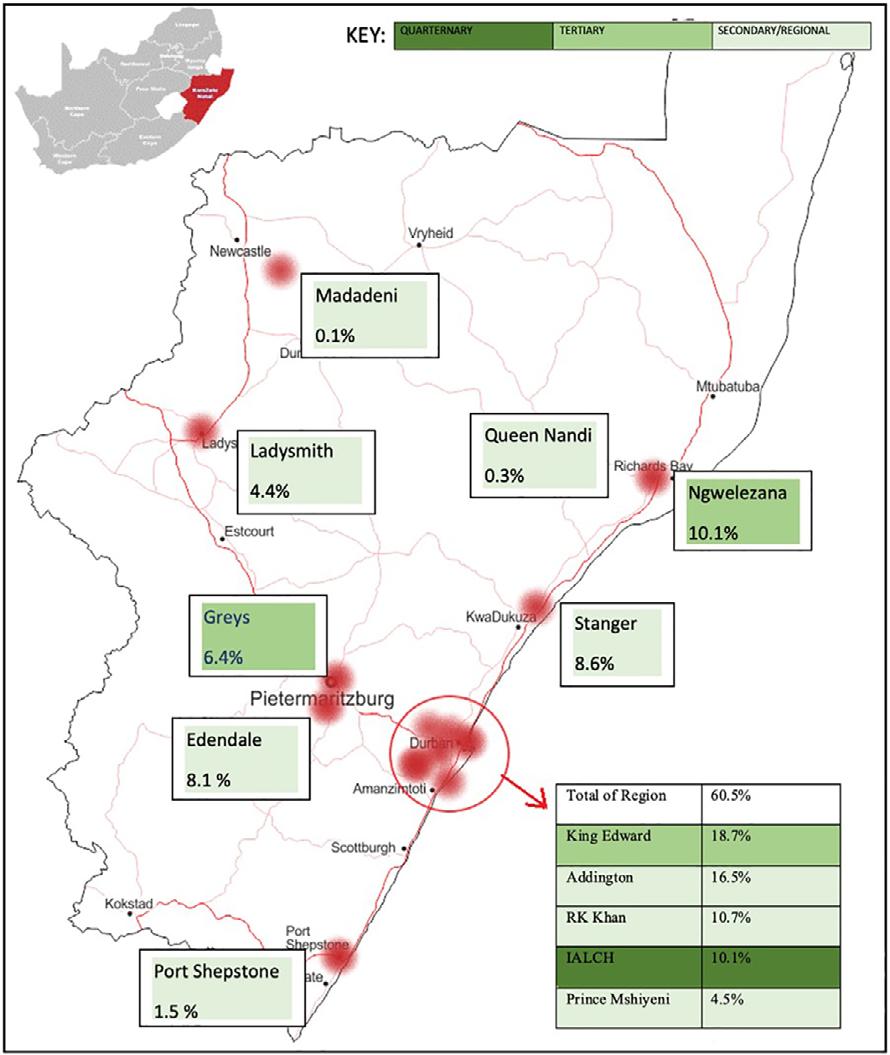
Figure 1 is a map showing the distribution of all breast related surgeries across the province.
Breast sepsis (n = 372)
Three hundred and seventy-two (47.9%) operative procedures were performed for breast sepsis, of which 359
Image adapted from: https://d-maps.com/carte.php?num_car=89567&lang=en
110 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Figure 1: A map of KZN indicating the total breast procedures performed at each of the participating regional, tertiary and quaternary hospitals in the province
(46.3%) were incision and drainage of breast abscesses, nine (1.2%) debridement of wounds on the breast and four (0.5%) carbuncle excisions.
Benign breast pathology (n = 140)
There were 140 (18%) procedures for benign breast lesions. These were subdivided into: 49 (6.3%) fibroadenomas, 73 (9.4%) lumpectomies of unspecified mass, a single phyllodes tumour and 17 (2.2%) other miscellaneous benign procedures, such as duct excisions, cyst and skin nodule excisions.
Non-benign breast disease (n = 223)
Two hundred and twenty-three (28.7%) operations were for non-benign disease. There were 20 (2.6%) wide local excision (WLE). A single WLE included an axillary lymph node dissection (ALND). Mastectomies contributed the remaining 203 (26.2%) procedures, of which 161 (72.2%) included an ALND. In five (2.2%) mastectomies, a sentinel lymph node biopsy (SLNB) was also performed. Twentyfour (3.1%) oncoplastic surgery procedures associated with mastectomies or breast-conserving surgeries were performed. These included contralateral reductions and symmetry adjustments.
Of the 203 mastectomies, 180 (88.7%) were unilateral, 18 (8.9%) bilateral and in five cases this was unspecified. Table II shows the total number of mastectomies, including those with lymph node dissections and SLNB.
Cosmetic procedures (n = 15)
There were 15 (1.9%) purely cosmetic procedures, including breast reduction and removal of accessory breast tissue. The indications for the latter breast reductions were not recorded in the available data.
Diagnostic procedures (n = 27)
There were 27 (3.5%) procedures undertaken for diagnostic purposes. Of these, 16 (2.1%) were performed in isolation
and included excisional biopsies, incisional biopsies and two SLNB. The remaining 11 diagnostic procedures were performed in conjunction with non-benign therapeutic and septic procedures; this accounts for the overlap of procedure numbers within the dataset.
Discussion
There is a significant burden of breast-related pathology requiring surgical treatment in KZN. This burden comprises roughly six per cent of the total general surgical procedures within the province. Attempts to streamline the process of care for breast pathology and to develop referral algorithms are warranted.6
A third of all breast-related procedures were for malignant disease. There are 33 mastectomies for cancer each month, suggesting an annual load of just over 400 mastectomies for cancer in the province. Mastectomy is performed at most regional and all tertiary centres in the province. This is appropriate as the technical aspects of the operation can be standardised and the operation can be performed safely without recourse to advanced anaesthetic and ICU care. Of note is the high rate of mastectomy as opposed to that of WLE and the relatively low rate of SLNB. This suggests that most of the breast cancer being treated is advanced and as such is not suitable for breast-conserving surgery. The late presentation of disease is in keeping with other studies in sub-Saharan Africa. The delays in diagnosis reflect both poor health-seeking behaviour in the patient population and the inadequacies of the primary healthcare system for early diagnosis and appropriate referral.7-9 This may reflect the lack of essential skills to examine masses and perform diagnostic procedures at the district levels, which impedes appropriate and early referrals. What must be understood is that each patient undergoing a mastectomy requires multidisciplinary management involving chemotherapy and radiotherapy. This care cannot be delivered at each regional centre and this care needs to be centralised. In this regard, the management of breast cancer differs to that of other complex cancers in that the operation can be decentralised but the adjuvant and
111 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Name of hospital Level of facility Total non-benign procedures (n = 223) Mastectomies with axillary clearance (n = 161) Isolated mastectomies performed (n = 37) Mastectomies with SLNB (n = 5) Wide local excisions (n = 20) Inkosi Albert Luthuli Quaternary 49 (22%) 30 (18.6%) 14 (37.8%) 4 (80%) 1 Grey’s Tertiary 38 (17%) 33 (20.5%) 4 (10.9%) 1 (20%) 0 King Edward Tertiary 31 (13.9%) 22 (13.7%) 3 (8.1%) 0 6 Ngwelezane Tertiary 12 (5.4%) 8 (5%) 3 (8.1%) 0 1 Addington Regional/ Secondary 40 (17.9%) 30 (18.6%) 7 (18.9%) 0 3 Edendale Regional/ Secondary 24 (10.8%) 21 (13%) 3 (8.1%) 0 0 RK Khan Regional/ Secondary 15 (6.7%) 7 (4.3%) 0 0 8 Ladysmith Regional/ Secondary 9 (4%) 8 (5%) 1 (2.7%) 0 0 Prince Mshiyeni Regional/ Secondary 4 (1.8%) 2 (1.3%) 2 (5.4%) 0 0 Stanger Regional/ Secondary 1 (0.4%) 0 0 0 1
Table II: Operations for non-benign breast pathology across KZN hospitals July–December 2015
neoadjuvant care cannot. Complex gastrointestinal cancer surgery needs to be centralised in terms of both the operation and the adjuvant and neoadjuvant care.10 KZN province has tertiary centres that are capable of performing the complex surgical procedures, however, the resources to provide the adjuvant and neoadjuvant care are not as widely available. Future planning around the delivery of care for breast disease needs to take this into consideration.
The substantial burden of breast sepsis requiring surgery may well reflect inadequate primary care services, as breast sepsis should ideally be detected early and managed with aspiration and antibiotics rather than surgery.11,12 Previous analysis from this same macro-data set has shown that most soft tissue sepsis is managed at regional and tertiary institutions rather than district hospitals. This suggests that district hospitals are not providing the expected level of surgical care and that this workload is being transferred to higher levels of care.13,14
Study limitations
The major limitation to this study is the lack of detail of the recorded data. The data were extracted from the operative logbooks and therefore lack supporting clinical data apart from the name of the operation. The diagnostic procedures are likely to be underrepresented in the data set due to a large proportion of diagnostic procedures being performed as a minor procedure outside of a theatre operating room. This same limitation may exist for septic procedures where simple abscess incision and drainage are frequently done outside of the operating theatre.
Conclusion
There is a significant load of breast pathology requiring surgical care in KZN province, of which just under one third is for non-benign disease and nearly half is secondary to breast sepsis. Improving data collection and standardising operative records amongst facilities will allow for the development of evidence-based strategies to meet the surgical workload of the province. Skills development programmes for the management of breast sepsis are warranted at district level facilities to avoid over-burdening regional and tertiary facilities. The ongoing development and strengthening of breast-related sub-specialist services is warranted to appropriately manage the entire spectrum of breast pathology.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
The study was approved by the Biomedical Research Committee of the University of KwaZulu-Natal (reference: BE528/16) and by the KZN Health Research and Knowledge Management Unit (reference: KZ_2016RP21_975).
ORCID






VU Ehlers https://orcid.org/0000-0002-3027-1712
CF Kohler https://orcid.org/0000-0001-5159-9971
E Lutge https://orcid.org/0000-0003-0272-0100
A Tefera https://orcid.org/0000-0003-1036-2796
DL Clarke https://orcid.org/0000-0002-8467-1455
I Buccimazza https://orcid.org/0000-0002-5399-3101
REFERENCES
1. Katz MG, Price RR, Nunez JM. Local research catalyses National Surgical Planning comment on “Global Surgery - informing national strategies for scaling up surgery in sub-Saharan Africa”. Int J Health Policy Manag. 2018;7(11):1058‐60. https://doi.org/10.15171/ijhpm.2018.78.
2. Gajewski J, Bijlmakers L, Brugha R. Global surgery –informing national strategies for scaling up surgery in subSaharan Africa. Int J Health Policy Manag. 2018;7(6):481-4. https://doi.org/10.15171/ ijhpm.2018.27.
3. Dell AJ, Kahn D. Surgical resources in South Africa: an international comparison and deficit calculation. World J Surg. 2018;42:541-8.
4. Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569-624.
5. Licitra L, Keilholz U, Tahara M, et al. Evaluation of the benefit and use of multidisciplinary teams in the treatment of head and neck cancer. Oral Oncol. 2016;59:73-9. https://doi. org/10.1016/j.oraloncology.2016.06.002
6. Pace LE, Shulman LN. Breast cancer in sub-Saharan Africa: challenges and opportunities to reduce mortality. Oncologist. 2016;21(6):739‐44. https://doi.org/10.1634/theon cologist.2015-0429
7. Ohene-Yeboah M, Adjei E. Breast cancer in Kumasi, Ghana. Ghana Med J. 2012;46(1):8‐13.
8. Rayne S, Lince-Deroche N, Hendrickson C, et al. Characterising breast conditions at an open-access breast clinic in South Africa – a model that is more than cancer care for a resource-limited setting. BMC Health Serv Res. 2017;17(1):63. https://doi.org/10.1186/s12913-016-1959-4.
9. Rayne S, Schnippel K, Kruger D, Benn CA, Firnhaber C. Delay to diagnosis and breast cancer stage in an urban South African breast clinic. S Afr Med J. 2019;109(3):159-63. https://doi.org/10.7196/SAMJ.2019.v109i3.13283.
10. Loots E, Ramdial PK, Sartorius B, Mulder CM, Clarke DL. Malignant and pre-malignant oesophageal pathology in a South African teaching hospital. S Afr J Surg. 2018;56(1):214. https://doi.org/10.17159/2078-5151/2018/v56n1a2076.
11. Dixon JM, Khan LR. Treatment of breast infection. BMJ. 2011;342:d396. https://doi.org/10.1136/bmj.d396.
12. Scott-Conner CE, Schorr SJ. The diagnosis and management of breast problems during pregnancy and lactation. Am J Surg. 1995;170:401-5. https://doi.org/10.1016/S00029610(99)80313-4
13. Ehlers V, Kohler C, Di Rago N, et al. Soft tissue sepsis places a massive burden on regional and tertiary surgical services in KZN Province South Africa. World J Surg. 2020;44:2526-32. https://doi.org/10.1007/s00268-020-05510-5.
14. Tefera A, Lutge E, Clarke DL. Bellwether operations in KwaZulu-Natal Province, South Africa, are performed at regional and tertiary rather than district hospitals. S Afr Med J. 2020;110(5):374-6. https://doi.org/10.7196/SAMJ.2020. v110i5.14218
112 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
South African
https://doi.org/10.17159/2078-5151/2021/v59n3a3477
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]



http://creativecommons.org/licenses/by-nc-nd/4.0
©
ISSN 038-2361
An audit of patients presenting with clinically benign breast disease to the Helen Joseph Hospital Breast Imaging Unit
NC Christofides,1 G Rubin,2 C-A Benn3
1 Department of Diagnostic Radiology, University of the Witwatersrand, South Africa
2 Department of Radiology, Helen Joseph Hospital, South Africa
3 Breast Surgical Unit, Helen Joseph Hospital, South Africa
Corresponding author, email: nicc1988@gmail.com
Background: Benign breast pathology is a common presenting complaint, and its assessment is important to characterise not to miss malignant pathology. At Helen Joseph Hospital (HJH), patients are triaged at the breast clinic according to the clinical suspicion of benign versus malignant disease. The patients are assigned a colour label based on their clinical presentation. This triage system affects waiting times between clinical examination and mammography appointments. This study aims to assess the association between clinical examination and the radiological and pathological findings of disorders deemed clinically benign, and to ascertain the spectrum of benign breast disorders encountered at HJH.
Method: A retrospective study of imaging results of patients at HJH presenting as clinically benign breast disorders from January to June 2018 was conducted. Assessed Breast Imaging-Reporting and Data System (BI-RADS) score was noted and if core biopsies were performed, their results and patient demographics were documented.
Results: Of the 1 263 clinically benign patients presenting from January to June 2018, the radiological assessment was: BI-RADS 1: 158 (12.5%), BI-RADS 2: 685 (54.2%), BI-RADS 3: 292 (23.1%), BI-RADS 4a: 54 (4.3%), BI-RADS 4b: 29 (2.3 %), BI-RADS 4c: 21 (1.7%), BI-RADS 5: 24 (1.9%). There were 133 biopsies (including eight BI-RADS 3 patients), with 46 (3.6%) confirmed malignancies. The combined specificity of mammography and ultrasound was 65.52% (54.56–75.39%) and combined sensitivity 91.30% (79.21–97.58%)
Conclusion: There is a vast spectrum of benign conditions presenting in this population group with only 3.6% confirmed malignancies, confirming an accurate triage system utilised at the breast clinic. Radiological imaging is highly sensitive but less specific, emphasising the triad of clinical, radiological and histological assessment as the gold standard with regard to diagnosis of breast disease.
Keywords: clinically benign breast disease, breast imaging unit, Helen Joseph Hospital
Introduction
Benign breast pathology is a common presenting complaint, with benign diseases more common than malignancies in young women.1 In North America, benign breast disorders account for 90% of breast complaints presenting to hospitals.2 The majority of patients presenting with breast complaints are found to have benign breast disorders, as seen in both developing and developed countries.1,3 Benign breast disorders have various modes of presentation and comprise multiple entities.4 These disorders require adequate diagnosis and monitoring to identify a mis-assessment of malignant pathology and to review for the small increased risk of breast cancer development associated with some benign pathology.5 Benign breast disease, such as phyllodes tumour, can carry an increased risk of progression to malignant phyllodes tumours.5
In order to correctly diagnose these conditions, triple assessment is utilised with the radiological correlation forming an integral part of benign breast disorder diagnosis and monitoring.6 Since breast cancer is the most common cancer in female patients, the diagnosis of a benign breast disorder is a relief to most patients.7,8 It is therefore important
to classify the percentage of patients presenting with these conditions and to ascertain the spectrum of benign disorders seen in our community. Triple (clinical, radiological and pathological) assessment is the gold standard in order to achieve a definitive diagnosis.6
Breast Imaging-Reporting and Data System (BI-RADS) is the radiological classification system used for breast imaging to help standardise breast imaging reporting.9 It is also useful in aiding adequate communication of findings to both radiologists and clinicians alike, as well as providing a method to monitor outcomes of patients.9 The BI-RADS classification system and the risk of malignancy is noted in Table I.
At the Helen Joseph Hospital (HJH), patients are triaged at the breast clinic according to a clinical suspicion of benign versus malignant breast disease. The patients are assigned a colour label based on their clinical presentation. Patients who present with a clinical suspicion of an abscess, or high suspicion for cancer are triaged as red (deemed high risk clinically and requiring imaging as soon as possible). Those who present with breast pain or breast asymmetry but with no mass, or any non-suspicious mass, milky/infected nipple
113 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
2021 The Author(s) BREAST DISEASE
Journal of Surgery. 2021;59(3):113-117
discharge, or palpable axillary lymph nodes with no definite palpable breast pathology are triaged as yellow. This triage system affects waiting times between clinical examination and mammography appointments. An assessment was performed of patients triaged as yellow (clinically benign) who received a date for their imaging studies within 6–8 weeks of their clinical examination. Thus, the sensitivity of our triage system as well as radiological and histological correlation is vital to patient management.
This study aims to assess the association between clinical examination and the radiological and pathological findings of disorders deemed clinically benign and to ascertain the spectrum of benign breast disorders encountered at HJH.
Methods
This was a retrospective study of mammographic, sonographic and histological (where available) results of all patients group (irrespective of age or gender) presenting to HJH breast unit with clinically benign breast disorders from January to June 2018. This included all patients who were classified as benign by the HJH breast unit, based on certain clinical features: breast pain, breast asymmetry, milky or yellow nipple discharge, possibility of palpable lymph nodes with nothing palpable in the breast, palpable mass with no suspicion for cancer. All reports that were illegible or lost were excluded.
The mammogram and ultrasound reports were collected and from them, BI-RADS scores, core biopsy reports and the demographics were collated on a data sheet.
The frequency of all BI-RADS classifications found was calculated.
All patients who received a biopsy were documented and the results correlated with their clinical and imaging results. Histology results were accessed from the National Health Laboratory Service (NHLS) for all patients who underwent a biopsy. An anonymised database (on Excel) based on demographics, BI-RADS score and histology results was collected and documented.
The study is reliable as it is an audit on the department, based on the radiological reports in a unit with a dedicated breast imaging specialist and thus is repeatable.
The study is valid as all lesions classified as BI-RADS > 4 receive biopsies (gold standard as per BI-RADS) and thus the diagnoses had histological correlation.
Descriptive statics (percentages and frequencies) were calculated for categorical data.
Pearson’s chi-squared test to determine the association between radiological and histological findings was performed. The sensitivity and specificity were calculated. Prior to the commencement of this study, ethical clearance was obtained; certificate number M191172.
Results
There were a total of 1 263 patients with a wide variety of ages, and 34 male and 1 229 female patients. Table II demonstrates the demographics of the patients included in the study.
114 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
ACR BI-RADS Atlas
Assessment Management Likelihood of malignancy BI-RADS 0: Incomplete –
imaging. Recall patient BI-RADS 1: Negative Routine screening 0% BI-RADS 2: Benign Routine screening 0% BI-RADS 3: Probably benign Short interval follow-up (6 months) > 0% but < 2% BI-RADS 4: 4a: Low suspicion 4b: Moderate suspicion 4c: High suspicion Biopsy > 2% but < 10% > 10% but < 50% > 50% but < 95% BI-RADS 5: Highly suspicious Biopsy > 95% BI-RADS 6: Known
Surgical management
Table I: Concordance between BI-RADS assessment categories and management recommendations
5th Edition10
needs additional
biopsy proven malignancy
Demographics Number of patients BI-RADS 1 BI-RADS 2 BI-RADS 3 BI-RADS 4 BI-RADS 5 Age groups < 20 65 15 24 25 1 0 21–30 166 38 56 63 9 0 31–40 176 29 68 54 22 3 41–50 263 28 145 53 31 6 51–60 238 19 152 45 18 4 61–70 243 21 166 35 16 5 71–80 99 7 65 17 6 4 > 80 13 1 9 0 1 2 Gender Males 34 1 2 30 0 1 Females 1 229 157 683 262 104 23 Total number of patients involved in the study 1 263 158 685 292 104 24
Table II: Demographics of study patients and their distribution within BI-RADS classification
BI-RADS 2 BI-RADS 3 BI-RADS 4 BI-RADS 5 BI-RADS category per age group
In Figure 1, the percentage of patients per age group within each of the BI-RADS categories is shown.
Of the clinically benign patients presenting from January to June 2018 the spectrum of imaging findings was as follows:
BI-RADS 1: 158 (12.5%), BI-RADS 2: 685 (54.2%), BIRADS 3: 292 (23.1%), BI-RADS 4a: 54 (4.3%), BI-RADS 4b: 29 (2.3 %), BI-RADS 4c: 21 (1.7%), BI-RADS 5: 24 (1.9%).
In Table III, the BI-RADS category of every patient who underwent biopsy is recorded and their results are supplied. These results are expressed as a percentage of the total sample number, with only 3.6% of all patients classified as clinically benign representing malignant disease.
The eight BI-RADS 3 patients who underwent biopsy were to either confirm diagnosis, such as in the case of a giant fibroadenoma or at the request of the patient and all eight were confirmed histologically to be benign.
There were also three patients within the BI-RADS 4 and 5 categories who did not undergo biopsy. The reasons were multifocal: patient refusal, patient too unstable or clinically unwell to undergo biopsy or no stock of biopsy needles (these patients were subsequently rebooked).
115 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
BI-RADS Biopsy result Total Malignant Benign 3 0 8 8 4a 4 49 53 4b 5 24 29 4c 16 5 21 5 21 1 22 Total 46 87 133 Percentage of total patient number 3.6% 6.9% 10.5%
Table III: Patients that underwent biopsy, their results and BI-RADS group as well as the percentage representation in terms of the total number of patients
Types Number of patients Benign Fibroadenoma 24 Fibrocystic breast disease 21 Benign breast tissue 20 Fat necrosis 9 Epidermal inclusion cyst 2 Sclerosing adenosis 2 Benign intraductal papilloma 2 Usual ductal hyperplasia 2 Periductal inflammation 1 Lactational changes 1 Mycobacterial infection 1 Previous abscess cavity 1 Acute mastitis 1 Malignant Invasive carcinoma no specific type 32 Ductal carcinoma in situ (DCIS) 8 Malignant phyllodes 2 Lymphoma 2 Mucinous carcinoma 1 Papillary carcinoma 1
1 < 20 20–30 31–40 41–50 51–60 61–70 71–80 > 80
1.2% 1.9% 3.0% 2.3% 2.2% 1.5% 3.6% 1.4% 1.7% 2.8% 1.3% 0.4% 0.6% 1.3% 0.5% 0.3% 0.1% 0.7% 0.0% 0.1% 0.2% 0.3% 4.2% 2.5% 11.5% 12.0% 13.1% 5.1% 0.5% 5.4% 4.3% 1.7% 4.4% 5.0% 0.7% 2.0% 0.1% 0.0% 0.0% 0.2%
Table IV: Biopsy results found within the sample of patients
BI-RADS
Figure 1: Graph showing the percentage of patients per BI-RADS category divided into age groups
Figure
study
a – mammogram (RCC) and b – ultrasound views of a biopsy confirmed fibroadenoma; c – mammogram (RMLO) of a patient with an oil cyst; d – mammogram (RMLO) and e – ultrasound views of fat necrosis post mild trauma to the breast; f – mammogram (RCC) of a patient with biopsy confirmed malignant phyllodes; g –mammogram (RCC) of a patient with biopsy confirmed mucinous carcinoma of the breast; h – mammogram (RCC) of a patient with biopsy confirmed B-cell lymphoma of the breast; i – mammogram (RMLO) and j – ultrasound of a patient with a biopsy confirmed invasive carcinoma; k – mammogram (RCC) of a patient with biopsy confirmed DCIS
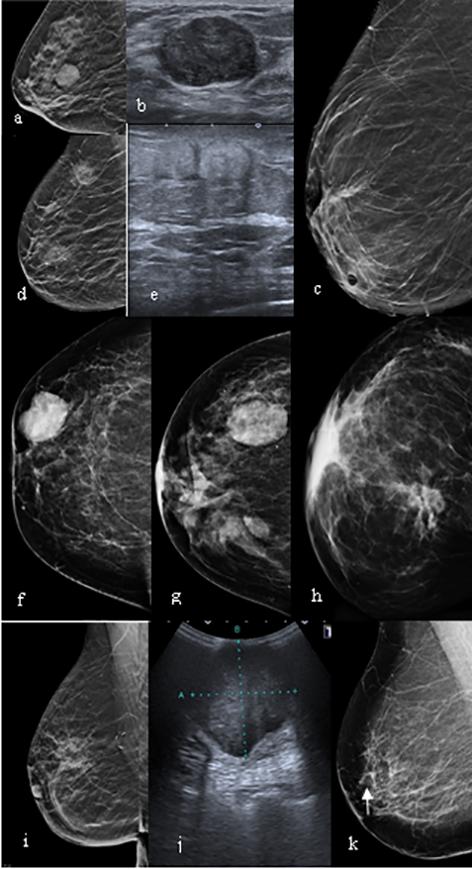
An assessment of all biopsies was performed, their results and the patients’ distribution among the BI-RADS categories (Table III) documented. From these results, a chi-squared value of 77.307 with a p-value of < 0.00001 was obtained. This indicates a statistically significant correlation between the radiological findings and the corresponding histological results.
Table IV depicts the spectrum of disease found amongst all the study participants that underwent biopsy. The majority of the patients depicted displayed benign histology in keeping with the clinical findings.
The imaging spectrum of disease within the study population is illustrated in Figure 2.
Discussion
Our results demonstrate a wide distribution of ages amongst all the clinically benign patients presenting at an open access breast clinic. The majority of patients were between the ages of 40 and 70, however, in more developed countries, most patients presenting with benign breast diseases are between the ages of 30 and 50 years.11 This may be related to better access to health care and earlier detection in these more developed countries.
Most of the patients within this clinically benign population fell within the benign or probably benign BI-RADS categories with 1 135 (89.9%) out of a total of 1 263 between BI-RADS 1, 2 and 3. This is in keeping with the literature as clinical examination alone has a sensitivity of 54%, while its specificity is 94%, and as such, some suspicious lesions may be mis-diagnosed as benign pathology.12
There were 128 (10.1%) patients within this clinically benign group who were radiologically suspicious (BIRADS 4–5). This is higher than expected as per the literature. After a single step triage system (as in our case), 52% of patients with malignancies were given non-urgent dates. Subsequently, after a second stage triage, only 4% of patients with malignancies were given non-urgent dates.13
A total of 133 biopsies were performed (some performed on BI-RADS 3 patients for confirmation of diagnosis or at the patient’s request). Three of the radiologically suspicious patients did not undergo biopsy due to refusal, inadequate clinical status, or lack of stock of biopsy needles.
Of the 133 patients who underwent biopsies, only 46 were confirmed to have malignancies, representing 3.6% of the total sample (1 263) patients. This is comparable with international triage systems as it is expected that 4% of patients with breast cancer will be triaged as semi-urgent (or yellow labelled as in our case).13
This emphasises that clinical examination is a good screening modality, but cannot be used as a stand-alone investigation in our country or globally.12
From Table IV, one can see that the majority of malignancies were found to be invasive carcinoma of no specific type (69.6% of all malignancies found) with the next most common malignancy being ductal carcinoma in situ (DCIS) (17.4%). This is in keeping with the literature as invasive ductal carcinoma is recognised as the most common subtype of breast cancer.14
Some other malignant lesions seen were malignant phyllodes, lymphoma and mucinous breast carcinoma – lesions which can mimic benign disease clinically as well as on imaging. They present as well-defined masses clinically and well-circumscribed masses on both mammogram and ultrasound. It is in these cases that histology becomes very important.
With regards to the benign diseases found on biopsy, Table IV shows that the most common findings were fibroadenomas (27.6% of all benign diseases found) which is in keeping with the literature (found in 25% of women),11 with fibrocystic breast disease (24.1%) and benign breast tissue (23%) being the next most common diagnoses.
From the above results, one can conclude that radiological assessment alone has a high sensitivity of 91.30% (79.21–97.58%), however, the specificity in our institution is lower
116 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
2: The imaging spectrum of disease seen in this
population;
at 65.52% (54.56–75.39%). According to the literature, however, the sensitivity should be 99% with a specificity of 95.2%,15 thus there is room for improvement, and this further emphasises the need for the gold standard of therapy which is the triple assessment.
This study was limited by the population group sampled; this may not be representative of the full population of our country as it represents only a small subset based on the catchment area of HJH.
Conclusion
A vast array of BI-RADS categories were found within this population clinically assessed as presenting with benign disease with a radiological correlation of the majority (89.9%) being benign. Only 3.6% of the total sample were confirmed radiologically and histologically as malignant disease, which is in keeping with international standards.
Radiological imaging alone is highly sensitive but less specific when compared with the histological findings, emphasising that the triad of clinical, radiological and histological assessment is indeed necessary with regards to breast imaging and clinical diagnosis. Of note is the useful application of a triage system at a clinical level to streamline referral for imaging in a resource-limited health care setting.
Acknowledgements
The study was conducted and completed at the University of the Witwatersrand. Our thanks go to the staff at the Breast Imaging Unit at Helen Joseph Hospital for allowing us access to patient records and imaging. And to our families and friends for their support and advice.
Conflict of interest
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Funding source
None.
Ethical approval
Ethical clearance has been approved by Human Research Ethical Committee (Medical) Wits. Ethical Clearance Certificate No. M191172.
ORCID



NC Christofides https://orcid.org/0000-0003-3522-6643
G Rubin https://orcid.org/0000-0001-8435-3521
C-A Benn https://orcid.org/0000-0002-4777-4316
REFERENCES
1. Edge J. Benign breast conditions in young women. CME. 2010;28(11):500-2.
2. Marchant DJ. Benign breast disease. Obstet Gynecol Clin North Am. 2002;29(1):1-20.
3. Vorobiof DA, Sitas F, Vorobiof G. Breast cancer incidence in South Africa. J Clin Oncol. 2001;19(18):125-7.
4. Rungruang B, Kelley JL. Benign breast diseases: epidemiology, evaluation, and management. Clin Obstet Gynecol. 2011;54(1):110-24.
5. Dyrstad SW, Yan Y, Fowler AM, Colditz GA. Breast cancer risk associated with benign breast disease: systematic review and meta-analysis. Breast Cancer Res Treat. 2015;149(3):56975.
6. Mansel RE, Webster D, Sweetland H, et al. Hughes, Mansel & Webster's. benign disorders of the breast. 3rd ed. Saunders (Ltd); 2009.
7. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
8. 2014 National Cancer Registry Tables [Internet]. National Health Laboratroy Service. 2014. Available from: http://www. nicd.ac.za/centres/national-cancer-registry/. Accessed 31 Oct 2019.
9. Lee J. Practical and illustrated summary of updated BI-RADS for ultrasonography. Ultrasonography. 2017;36(1):71-81.
10. D’Orsi C, Sickles EA, Mendelson EB, Morris EA. Breast imaging reporting and data system: ACR BI-RADS breast imaging atlas. 5th ed. American College of Radiology; 2013.
11. Stachs A, Stubert J, Reimer T, Hartmann S. Benign breast disease in women. Dtsch Arztebl Int. 2019;116(33-34):56574.
12. Jatoi I. Screening clinical breast examination. Surg Clin North Am. 2003;83(4):789-801.
13. Hung WK, Chan SW, Suen DT, et al. Triaging referral to a specialist breast clinic. ANZ J Surg. 2006;76(5):310-2.
14. Sharma GN, Dave R, Sanadya J, Sharma P, Sharma KK. Various types and management of breast cancer: an overview. J Adv Pharm Technol Res. 2010;1(2):109-26.
15. Karim MO, Khan KA, Khan AJ, et al. Triple assessment of breast lump: should we perform core biopsy for every patient? Cureus. 2020;12(3):e7479.
117 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
South African Journal of Surgery. 2021;59(3):118-123
https://doi.org/10.17159/2078-5151/2021/v59n3a3243
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]



http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361
© 2021 The Author(s)
Clinicopathological spectrum of small bowel obstruction and management outcomes in adults – experience at a regional academic hospital complex
MR Mthethwa,1 C Aldous,2 TE Madiba3
1 Department of Surgery, Nelson R Mandela School of Medicine, Pietermaritzburg Hospitals Complex, University of KwaZulu-Natal, South Africa
2 School of Health Science, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, South Africa
3 Department of Surgery, Colorectal Unit, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, South Africa
Corresponding author, email: musamthethwa70@gmail.com
Presented at the Meeting of the Surgical Research Society of Southern Africa in Bloemfontein, South Africa on 25–26 June 2015.
Background: Delay in operative management of small bowel obstruction (SBO) results in increased morbidity and mortality. The objective was to evaluate clinical presentation and treatment outcome of SBO.
Method: Prospective cohort study between 2013–2014. Adult patients presenting with SBO were included. Demographics, clinical details, investigations, operative findings, in-hospital progress and outcomes were documented.
Results: There were 156 patients (median age 37 [IQR 27–54 years]) with early (44) and delayed (112) presentation. M:F ratio was 1.4:1. Common causes of obstruction were adhesions (94; 60.3%) and hernias (31; 19.9%). Non-operative management was feasible in 59 patients (37.3%) with a success rate of 71.2%. Nonviable bowel was present in 45.1% (early 31%, delayed 50%; p = 0.078). Sixty-one patients (54%) underwent bowel resection; nine patients (20.5%) in the early presentation group and 52 (46.4%) in the delayed group (p = 0.003). Thirty-one patients needed ICU admission (early 5, delayed 26; p = 0.091). The delayed group had longer ICU stay (p = 0.018) and longer hospital stay (p < 0.001). There were more complications (p = 0.084) and re-laparotomies (p = 0.156) in the delayed group. Eight patients died (5.1%).
Conclusion: The main causes of SBO were adhesions and hernias. Late presentation was associated with higher resection rate, higher critical care admission and longer hospital stay.
Keywords: small bowel obstruction, adhesive bowel obstruction, acute abdomen
Introduction
The diagnosis of intestinal obstruction is based on clinical and radiological evaluation and can be categorised as complete or partial.1-3 The former requires operative management and the latter should initially be managed non-operatively, especially when the most probable causes are adhesions or abdominal tuberculosis.1,3-5 Provided that the patient does not have peritonitis, the fluid shifts and electrolyte derangements caused by the proximal bowel dilatation can be corrected, and spontaneous resolution of the obstruction monitored clinically.4,6,7 These principles apply to both high-income countries (HICs) and low- and middle-income countries (LMICs).8-10 There is variation in the aetiology of small bowel obstruction (SBO) with adhesions from previous operations being a predominant aetiology in HICs, and hernias and tuberculosis remaining as the main causes in LMICs and countries with poorly resourced healthcare systems.9-13 Delay in reaching health care facilities is a variable that affects the system’s ability to provide surgical intervention and is most marked in the poorly resourced
health care settings.7,13-15 Late presentation and undue delay in operative intervention for SBO may result in bowel ischaemia and increased need for resection with the resultant risk of complications.4,16,17 As an upper middle-income country with many rural communities,18 South Africa is well placed to investigate SBO and establish if the global trends seen in the international literature are evident in our setting. We, therefore, decided to undertake a study on SBO in our catchment area; the aim was to evaluate the aetiology and clinical patterns of SBO, reasons and patterns of delay to definitive surgical management, and the impact of delay on outcomes in our region.
Methods
The study was conducted at the Pietermaritzburg Academic Hospitals, namely Edendale and Grey's hospitals. Pietermaritzburg is the capital city of the KwaZulu-Natal (KZN) province, The two hospitals provide a full 24hour surgical service and serve the local community of the Pietermaritzburg metropole, as well as various district
118 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
GENERAL SURGERY
hospitals within the western region of the KZN province, which comprises a population of 3.5 million people.19
A prospective, cohort, observational study was conducted between 1 August 2013 and 31 July 2014. Patients older than 12 years, with an admission diagnosis or operative findings of SBO were identified. Those misdiagnosed, and those with colonic or functional SBO were excluded. Data captured included demographics, clinical presentation, physical findings, investigation results, aetiology of obstruction and management. Late presentation was defined as symptoms for more than two days prior to presentation. Patients were categorised into two groups, namely those receiving operative management (OM) group and those receiving nonoperative management (NOM) group. Patients in the NOM group were managed by keeping the patient nil by mouth, inserting a nasogastric tube (NGT) for decompression, intravenous fluid, electrolyte correction and close clinical monitoring. Patients suitable for NOM were given 100 ml Gastrografin orally on admission or during the first 24 hours of admission to document bowel patency using abdominal radiographs.
The success of NOM was documented at the first passage of stools. Failure of NOM was recorded when an indication for operative intervention was identified by persistent symptoms (persistent vomiting, high NGT output, persistent abdominal pain and tenderness), clinical deterioration (tachycardia, worsening abdominal pain and tenderness) or confirmation of complete SBO on a Gastrografin radiographic study or on abdominal CT scan. OM was offered to patients with complete SBO, those with peritonism and severe SIRS with metabolic acidosis, and for failed NOM. Operative findings were recorded, including the obstructing pathology and the presence or absence of a nonviable bowel segment. Operative intervention and mode of abdominal closure were also recorded. Postoperative complications, postoperative critical care admission, and relaparotomy rate were recorded, as were the lengths of ICU and hospital stay (LOS). Follow-up was until the patient’s discharge from hospital or death.
Statistics
Descriptive statistics were applied to the data. The chisquared test was used for categorical data and the independent t-test for continuous variables. Continuous data for hospital and ICU stay were expressed as mean and standard error of the mean (Mean [SEM]); the rest of the continuous data were expressed as the median and interquartile range
(IQR). A p-value of < 0.05 was considered statistically significant.
Results
One hundred and fifty-six patients were enrolled in the study of whom 91 (58%) were male (M:F ratio 1.4:1). The median age was 37 (IQR 27–54) years. There were 125 referrals: 94 (60%) from district hospitals, 22 (14%) from clinics, five (3%) from other hospital departments and four (3%) by local general practitioners. Thirty-one patients (20%) were selfreferred from within the Pietermaritzburg metropole.
The main cause of SBO was adhesions from previous operations in 94 patients (60.3%), followed by hernias in 31 patients (19.9%). Other causes are detailed in Table I. Forty-four patients presented early and 112 were delayed. Of the 112 delayed presenters, 103 patients (66%) presented late to our hospital, and a further nine were delayed within the hospital (6%). The median delay was 4 (IQR 2–6) days. Reasons for the delay are shown in Table II. The most common reasons were inappropriate health-seeking behaviour (60; 53.6%) and delayed referral (52; 46.4%). District hospitals were the major point of delay, contributing
119 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Adhesive
Prior operations n Per cent Trauma laparotomy 40 25.6 Appendicectomy 26 16.7 Obstetrics/gynaecology 15 9.6 Gastrointestinal 13 8.3 Non-adhesive group (62 [39.7%]) Pathology n Per cent Inguinal hernia 12 7.7 Incisional hernia 9 5.8 Umbilical hernia 8 5.1 Epigastric hernia 2 1.3 Tumour/stricture1 14 9 TB abdomen 8 5.2 Inflammatory mass2 6 3.8 Ileo-sigmoid knot 2 1.3 Small bowel volvulus 1 0.6
Table I: Aetiology of small bowel obstruction in 156 patients
group (94 [60.3%])
1 Primary tumour (7), secondary tumour (7)
2 Appendix mass (3), tubo-ovarian mass (3)
Behavioural pattern Reason for delay* n Per cent Delayed first presentation n = 50 (44.6%) Did not seek medical help 22 19.6 Used alternate/herbal medicine 15 13.4 Self-medication (OTC) 13 11.6 Delayed referral n = 62 (55.4%) Base hospital 28 25.0 Clinic 20 17.9 General practitioner 5 4.5 Definitive hospital1 9 8.0 OTC – over-the-counter medicine *Delay – Some patients had more than one point of delay: delay in base + GP practice (3); delay in base + clinic (3); delay in GP practice + clinic (1); delay in base + definitive hospital (2) 1Reason for delay at definitive hospital – Incorrect diagnosis/management (5); admitted to wrong specialty (4)
Table II: Patterns of delay in surgical management among 112 patients with small bowel obstruction
to delay in 28 patients. Some of the late presenting patients had more than one point of delay.
Clinical presentations varied, with typical symptomatology of SBO observed in 135 patients (86.5%). Complete obstruction was observed in 94 patients (60.3%). Other positive findings were tachycardia 68 (43.6%), fever 38 (24.4%), leucocytosis 80 (51.3%), peritonism 38 (24.4%), and persistent tenderness 19 (12.2%). All patients underwent plain abdominal X-ray. Sixty patients (38.5%) were given oral Gastrografin with serial follow-through radiographs of whom six (3.8%) needed an abdominal CT scan to finalise management decision. Fourteen (9.0%) and four (2.5%) patients respectively underwent only abdominal CT scan and ultrasound scan. Blood gas assessment showed normal blood gas (54; 34.6%), metabolic alkalosis (78: 50%), and metabolic acidosis (24; 21.8%). Electrolytes were normal in 73 patients (46.8%), abnormal in 55 (35.3%) and 58 patients (37.2%) had renal impairment.
Fifty-nine patients (37.8%) were clinically suitable for NOM, of whom 22 and 37 were early and late presenters respectively. The median duration of NOM was 2 (IQR 2–4) days. NOM was successful in 42 of 59 patients (71.2%) and the other 17 failed NOM and required operative intervention. Thus, 114 patients were considered for surgical intervention, but one patient refused intervention and was excluded from the analysis and discharged back to their base hospital. As a consequence, 155 patients were available for analysis (early 44, delayed 111).
One hundred and thirteen patients were offered operative intervention: 96 patients (85%) at the outset and a further 17 patients (15%) who failed NOM. Of the 17 patients who failed NOM, seven patients (41%) needed bowel resection. Adhesiolysis was the most common intervention at laparotomy, carried out in 73 of 113 patients (64.6%). Adhesions were also observed in other obstructions due to hernias, tuberculosis (TB) abdomen or inflammatory mass
120 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Clavien–Dindo classification Complication Total n = 77* Early n = 16* Delay n = 61* p-value Grade I Surgical site infection 6 2 4 Prolonged ileus 20 4 16 Renal dysfunction 4 1 3 Hypocalcaemia 1 1 0 Thrombocytopenia 1 0 1 Hypoglycaemia 1 0 1 Sub-total 33 (43%) 8 (50%) 25 (41%) 0.520 Grade II High output ileostomy 1 0 1 Pneumonia 7 2 5 Catheter-related sepsis 2 0 2 Sub-total 10 (13%) 2 (12.5%) 8 (13%) 0.958 Grade III Enterocutaneous fistula 1 0 1 Ischaemic bowel 4 0 4 Peritonitis 2 0 2 Sub-total 7 (9%) 0 7 (12%) 0.148 Grade IV Anastomotic failure 5 1 4 Enterocutaneous fistula 1 0 1 ARDS 3 2 1 Septic shock 3 0 3 MODS 2 0 2 MI 1 0 1 Pneumonia 2 2 0 Sub-total 17 (22%) 5 (31.3%) 12 (20%) 0.337 Grade V Renal dysfunction 2 0 2 Pneumonia 1 0 1 Peritonitis 1 0 1 Ischaemic bowel 3 0 3 Pulmonary embolism 1 0 1 MI 1 1 0 MODS 1 0 1 Sub-total 10 (13%) 1 (6.3%) 9 (15%) 0.363
Table III: Observed morbidity in patients undergoing surgical intervention for small bowel obstruction stratified according to the Clavien–Dindo classification20
*Some patients had more than one complication; ARDS – acute respiratory distress syndrome, MODS – multi-organ dysfunction syndrome, MI – myocardial infarction
(such as appendicular and tubo-ovarian complex); however, they were not the primary cause of SBO.
Figure 1 shows different pathways and outcomes of patients presenting with SBO during this study. Nonviable bowel was seen in 51 of 113 patients (45%) undergoing laparotomy; nine (31%) from the early presentation group and 42 (50%) from the delayed group (p = 0.078). Bowel resection was undertaken in 61 of 113 patients (53.9%), including the seven of the 17 patients who failed NOM. Thus nine patients (20.5%) in the early presentation group and 52 (46.4%) in the delayed group underwent resection (p = 0.003). Other interventions were hernia repair (25) and appendicectomy (3). A stoma was deemed necessary in 12 patients undergoing bowel resection. Appendicectomy was performed in SBO due to appendix inflammatory mass. Fifteen patients required temporary abdominal closure (TAC) using Bogota bag.
Thirty-one patients required critical care admission (27.4%); five in the early group (11.4%) and 26 (23.4%) in the delayed group (p = 0.091). Three patients (7%) required relaparotomy in the early group as opposed to 20 (18%) in the delayed group (p = 0.156).
Fifty-five patients (35.3%) developed complications; 11 of 44 in the early group (25%) and 44 of 111 in the delayed group (37%). The 55 patients developed 77 complications (44 intra-abdominal and 33 extra-abdominal complications). Table III depicts different complications, according to the Clavien–Dindo classification system.20 Eleven out of 29 patients with early presentation (37.9%) developed 16 complications and 44 patients out of 84 patients with delayed presentation (52%) developed 61 complications (p = 0.084). The delayed group had more complex complication patterns. Seventeen patients had two complications each, and seven had three each. In addition, from the delayed presentation group, 12 and eight patients had an un-reversed stoma and
121 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Small bowel obstruction 156 Primary operative management 96 Non-operative management 59 Refused OM 1 Resection* 47 Resection* 4 7 0 0 1 0 0 Resection 7 Resection 3 Success 42 Failed, had surgery 17 No resection 42 Deaths 8 No resection 10 0
* for gangrene 50 45 40 35 30 25 20 15 10 0 Observed outcomes Aetiology of small bowel obstruction Adhesions (63) Hernias (29) Tumours (10) TB abdomen (6) Others (5) Ischaemia Dead bowel Resection ICU need Relaparotomy
Figure 1: Flowchart of outcomes of small bowel obstruction observed during the study
Figure 2: The graph shows the degree of bowel viability, need for critical care and reoperation related to aetiology
an open abdomen, respectively. Eight patients (5.1%) died, seven (6.3%) from the delayed group and one (2.3%) from the early presentation group (p = 0.442).
The causes of mortality were myocardial infarction (MI) (1), pulmonary embolism (1), multiple organ dysfunction (5), for the delayed group, and MI (1) for the early presentation group.
Figure 2 demonstrates the different aetiologies together with associated complications. Adhesions and hernias were the most common causes of obstruction and thus contributed to most of the complications.
The mean hospital stay was 8.7 (SEM 0.6) days; the mean hospital stay for the early group was 5.6 (SEM 0.6) days vs 9.9 (SEM 0.8) days for the delayed groups (p < 0.001). The mean ICU stay was 1.5 (SEM 0.4) days; the mean ICU stay for the early group was 0.5 (SEM 0.2) days as opposed to 1.9 (SEM 0.5) days for the delayed group (p = 0.018).
Discussion
The aetiology and pattern of SBO have been the topics of extensive research in various settings. It differs in LMICs which are poorly resourced from that in well-resourced HICs.1,3,5,11,12 Hernias are the leading cause of SBO in LMICs, whereas postoperative adhesions are the main cause in the HICs.10-13 The most common cause in this series was adhesions from previous operations, much as in the HICs. However, the common operations leading to adhesions were laparotomies for trauma followed by appendicectomy as opposed to other parts of the world where appendicectomy and colorectal operations are the main index operations leading to subsequent development of adhesive SBO.11 This is probably related to a higher incidence of trauma-related laparotomy in our setting.21 All types of hernias, namely congenital and acquired, were the second major cause at 19.9% which is higher than 10% in HICs1,5,12 and lower than 36% reported from other LMICs.11-13
Surgical candidates in this series had a variable clinical presentation. The majority of patients presented late, and there were different points of delay. Patient factors included lack of insight, thinking the abdominal symptoms would resolve in time, attempting self-medication or herbal medication. Factors related to the primary health caregivers included incorrect diagnosis, inappropriate management at primary health care levels, and multilevel consultations. Delay at the base hospital was the most frequent point of delay. Delays at the definitive hospitals were related to misdiagnosis and admission to the wrong speciality and further diagnostic imaging. In a study by Malangoni et al. of 366 patients, 222 were admitted to surgical service and 114 to medical service, operated patients admitted to surgical service had shorter preoperative (2.7 vs 6.3) days, p < 0.01 and overall LOS (17.9 vs 22.8) days, p < 0.0001.22 Multilevel consultation is another factor that increases the delay to definitive hospital and surgical intervention. In an emergency departmentbased study, of 355 advised admissions, 238 (67%) were delayed. The common reason for delay was multiple consultations with further investigations, p < 0.001 and file making process, p < 0.001.23 Incorrect diagnosis results in patients being sent back home and then re-consulting to the same point or elsewhere a day or so later, before they re-join the referral ladder. There is evidence to suggest that race may play a role in influencing delay in presentation for medical attention. A North American outcome comparison
study among different races discovered that Black patients had relatively longer delays irrespective of access to health care facility.8 Inter-hospital transfer was another cause of delay in this series. An Australian study by Limmer et al. demonstrated that inter-hospital transfer tends to delay surgical intervention and increases the length of hospital stay. Amongst the 910 adults patients in the study who underwent emergency abdominal surgery, 290 (31.9%) were transferred in from local district hospitals, had delayed surgical intervention (14.2h, p = 0.001), postoperative LOS 1.1 days (p = 0.001) and overall LOS 1.6 days (p < 0.001) – observed in all emergencies except peptic ulcer perforations.24 Other reasons for delay include the time since the onset of illness because of late presentation due to lack of health care facilities, lack of health awareness, ignorance and poverty.13,15 Late presentation and undue delay in operative intervention for SBO results in bowel ischaemia, increases the need for resection and the risk of complications.4,16,17
There was nonviable bowel in 45% of cases. Bowel resection was necessary in 54% of cases with the vast majority coming from the delayed group. Admittedly not all resections are necessarily due to late presentation but may be necessitated by the condition responsible for the obstruction, namely tumours or strictures.
Fifty-four per cent of patients underwent resection in this study, which is higher than the 36% (range 9–51%) reported in the literature.25,26 In a study by Meier et al., resection was necessary in 32.4% and there was a longer hospital stay for the OM group, and nine deaths (6.6%) were observed, all from the OM group.26 The complication rate for the whole group was 35% (25% and 37% for the early presentation and delayed presentation groups, respectively). These differences, however, did not reach statistical significance. A systematic review of nine studies by Thornblade et al. demonstrated an average mortality of 4% after surgery and 2% after NOM.25 The same review demonstrated a shorter hospital stay after NOM than after OM.25
This study demonstrates that delay in operative management of SBO is associated with a significantly increased rate of bowel resection, re-laparotomy rate and a longer LOS. There is also a trend that delay is also associated with higher ICU usage and longer ICU stay, and a high rate of complex morbidity and mortality. Other authors have confirmed that delay before intervention in SBO is associated with increased morbidity and mortality.8,10,16,25 Thornblade et al.25 reported lower resection rates in the early surgery group than in the delayed surgery group. SSI rates were similar and a longer average LOS for the delayed surgery group.25
NOM of SBO is acceptable in patients with a partial obstruction due to adhesions or abdominal tuberculosis in the absence of persistent tachycardia, fever, leucocytosis, metabolic acidosis, septic shock, persistent or progressive abdominal pain and tenderness, or peritonism.1,3,5,25 This involves keeping the patient nil by mouth, nasogastric tube insertion where necessary, initiation of anti-TB treatment in cases of abdominal TB,9 and regular clinical and radiological evaluations for improvement or deterioration.27,28 Oral feeds are introduced when symptoms and signs abate. In this study, 59 patients were candidates for NOM. The success rate following NOM was 72.4%, and there was no difference between early and delayed presenters. The role of NOM in patients with delayed presentation has not been described
122 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
in the literature. The observed success rates in the delayed group are said to be related to obstructive morphology, namely matted adhesions versus adhesive band.3,29 The average duration of NOM for this study was 3.15 days in this series. Although evidence for the optimal duration of NOM is absent, most authors suggest that NOM should not extend beyond 3–5 days for non-resolving SBO, even in the absence of clinical deterioration.3,5,16
Current management guidelines support the use of watersoluble contrast meal and follow-through as an adjunct to NOM.3,5,30 This improves time to bowel function recovery and reduces overall hospital stay.30 The dose is 50 to 150 ml given orally or via nasogastric tube, on admission or at 48 hours of unsuccessful NOM. The likelihood of treatment success is demonstrated by the presence of contrast at the ileocaecal junction as visualised on an erect abdominal X-ray.30 Failure of progress is diagnostic of complete obstruction and is an indication for operative intervention.1,3,5 In the current study, a Gastrografin meal and follow-through was given in 60 patients, and it influenced decision-making in 56 patients. The earlier the Gastrografin meal and follow-through is given, the sooner the diagnosis of complete SBO is made, thus avoiding further delays. The use of Gastrografin in this study was limited to differentiating partial from complete SBO. It is crucial that the patient is adequately hydrated before this investigation is undertaken.30
Current management guidelines recommend abdominal CT scan for all patients with suspected SBO to confirm SBO and assess the risk of small bowel ischaemia.1,3,5 Furthermore, abdominal CT scan has a value in patients posing a diagnostic dilemma and those with a history of malignancy, prior irradiation or those with possible abdominal TB.1,3 Abdominal CT is, however, of limited availability in resource-challenged settings, and, in this study, it was necessary for 20 patients where it was useful in defining the presence, cause, the site and degree of SBO. Most notably, the turnaround time for this investigation was long, a common issue in resource-limited settings. In patients who present with a possibility of undiagnosed underlying malignancy, it is advisable to perform this investigation in patients who respond to NOM even on an elective basis.28,31
Conclusion
The leading cause of SBO in adult patients in our region is adhesions from previous operations followed by hernias. Most patients present late and/or are delayed by the referral process. Delayed presentation was associated with higher resection rate, higher critical care admission and prolonged hospital stay. Morbidity and mortality rates were higher in the delayed groups although the difference in morbidity and mortality did not reach statistical significance. While NOM is appropriate in selected cases, proper clinical evaluation and use of further imaging modalities may be invaluable in deciding on the need for surgery. We encourage active preventive measures, including early repair of hernias, improved education for patients at risk and heightened awareness at primary health care level to ensure early diagnosis and early referral to centres with appropriate surgical facilities.
Acknowledgements
Dr Yoshan Moodley, University of KwaZulu-Natal, for statistical analysis.
Conflict of interest
All authors declare no conflict of interest.
Funding source
No funding was required.
Ethical approval
Ethical approval was obtained from the Biomedical Research Ethics Committee (BREC) of the University of KwaZuluNatal (REF: BE207/13). Informed consent was obtained from each participant, and confidentiality was maintained by using study codes as identifiers instead of names.
ORCID



MR Mthethwa https://orcid.org/0000-0002-5374-050X
C Aldous https://orcid.org/0000-0002-7199-9160
TE Madiba https://orcid.org/0000-0002-0155-9143
REFERENCES
1. Maung AA, Johnson DC, Piper GL, et al. Evaluation and management of small-bowel obstruction – an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S362-9. https:// doi.org/10.1097/TA.0b013e31827019de
2. Zielinski MD, Bannon MP. Current management of small bowel obstruction. Adv Surg. 2011;45:1-29. https://doi. org/10.1016/j.yasu.2011.03.017
3. Ten Broek RPG, Krielen P, Di Saverio S, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO) – 2017 update of the evidencebased guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018;13:24. https://doi.org/10.1186/s13017-018-0185-2.
4. Aldemir M, Yaǧnur Y, Taçyildir I. The predictive factors for the necessity of operative treatment in adhesive small bowel obstruction cases. Acta Chir. Belg. 2004;104:76-80. https:// doi.org/10.1080/00015458.2003.11681150
5. Rami Reddy SR, Cappell MS. A systematic review of the clinical presentation, diagnosis, and treatment of small bowel obstruction. Curr Gastroenterol Rep. 2017;19:28-42. https:// doi.org/10.1007/s11894-017-0566-9
6. Kumari N, Charokar K, Bharang K. Study of clinical presentation and management of intestinal obstruction and its evaluation with respect to morbidity and mortality. Int J Surg Orth. 2020;6:166-72. https://doi.org/10.17511/ijoso.2020.i03. 05
7. Shih SC, Jeng KS, Lin SC, et al. Adhesive small bowel obstruction – how long can patients tolerate conservative treatment? W J Gastroenterol. 2003;9:603-5. https://doi. org/10.3748/wjg.v9.i3.603.
8. Chiu AS, Jean RA, Davis KA, Pei KY. Impact of race on the surgical management of adhesive small bowel obstruction. J Am Coll Surg. 2018;226:968-76. https://doi.org/10.1016/j. jamcollsurg.2017.11.006
9. Chalya PL, Mchembe MD, Mshana SE, et al. Tuberculous bowel obstruction at a university teaching hospital in northwestern Tanzania – a surgical experience with Full list of references available on request.
123 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
https://doi.org/10.17159/2078-5151/2021/v59n3a3355
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]


http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN
The spectrum of abdominal wall desmoid fibromatosis and the outcomes of its surgical treatment
I Bombil,1 L Ngobese2
1Department of Surgery, Chris Hani Baragwanath Academic Hospital, South Africa
2Department of Anatomical pathology, University of the Witwatersrand, South Africa
Corresponding author, email: ifongobombil@gmail.com
Background: Desmoid fibromatosis (DF) arises in musculoaponeurotic structures, most commonly the rectus abdominis muscle. It is locally aggressive with no propensity for metastasis. The aim was to describe the spectrum of abdominal wall DF and its surgical treatment and outcome at a tertiary institution.
Methods: All abdominal wall DF resected from 2007 to 2019 were retrospectively analysed. The tumours had a fullthickness abdominal wall excision. The defect was reconstructed with biological implants covered by either skin edge undermining or split skin graft. Histological diagnosis was based on characteristic morphological and immunohistochemistry parameters. Parameters analysed were demographics, lesion size, procedure performed and outcomes.
Results: Eleven female patients with a median age of 29 years (range 21–61) presented with rapid growth over 6–24 months of anterior abdominal wall tumours with a median maximum resected diameter of 163 mm (range 63–200 mm). There was no specific complication related to the abdominal wall reconstruction. With a median follow-up of 5 years (range 1–11 years), all patients displayed an asymptomatic abdominal wall bulge (eventration). One patient has had a small recurrence currently being observed.
Conclusion: Striking features of DF tumours at Chris Hani Baragwanath Academic Hospital (CHBAH) were their location, rapid growth, female gender and large size. Biological implant without complex plastic surgery techniques result in good outcomes, though the rate of progression of eventration to hernia is unknown.
Keywords: desmoid fibromatosis, abdominal wall, biological implants
Introduction
Desmoid fibromatosis (DF) is one of the rare (5–6 cases/ million) malignancies of mesenchymal origin arising from musculoaponeurotic structures throughout the body but occurs most commonly in the rectus muscle of the anterior abdominal wall.1,2 It is a neoplastic proliferation of myofibroblast that often displays aggressive infiltrative growth with a tendency toward local recurrence but no propensity to metastasise.3
More than 80% of DF tumours are sporadic and in a small proportion (5–10%) of cases they are linked to familial adenomatosis polyposis (FAP) and Gardner syndrome.4 Sporadic tumours harbour somatic mutations in ß-catenin gene (CTNNB1), while FAP-associated tumours display germline mutations in adenomatosis polyposis coli (APC) gene.1,5 Both mutations though mutually exclusive in DF result in stabilisation and translocation of ß-catenin to tumour cell nuclei as demonstrated by ß-catenin immunohistochemistry nuclear positivity.3,5 The mutated ß-catenin is resistant to degradation and its accumulation acts as an oncoprotein.
The epidemiology of DF tumours is variable and displays a range of presentation in different age groups. In children, there is equal incidence in males and females with tumours frequently located at extra-abdominal sites. In young adults, there is a trend toward female predominance
and the usual site is the abdominal wall. In adults over 40 years and the elderly, there is equal gender distribution and tumours are seen equally at abdominal and extraabdominal sites.6 Abdominal DF tumours typically arise in young females of childbearing age and often occur during gestation or following childbirth.6 The presentation is either asymptomatic (incidentally found during imaging) or a slow growing, painless, deep-seated mass. In rare cases, patients present with a rapidly expanding mass which may reach a large size.1,3
There are few publications on DF tumours in South Africa and around the world.7-10
An international multi-institution study in seven European sarcoma reference centres reported on the beneficial role of low dose chemotherapy in FAP-related desmoid tumour.11 Despite radical excision, DF tumours are prone to recur –“Desmoid tumour don’t die”10 – and radiotherapy has been used to reduce the risk of recurrence. Locally, Sharma et al. at the Johannesburg General Hospital reported in 2006 that the mainstay of treatment is surgery with no obvious benefit from radiotherapy.12 Pickard et al. from Groote Schuur Hospital reported similar results in 2019, although they emphasised the role of primary radiotherapy on patients whose tumour was unresectable as it produced a partial response or stabilisation of the disease.13
124 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
038-2361
GENERAL SURGERY
© 2021 The Author(s)
South African Journal of Surgery.
2021;59(3):124-126
In this report, we reviewed patients with DF tumour treated at CHBAH and detail the clinical spectrum and present the results of surgical treatment.
Method
A retrospective analysis of 11 cases of DF tumours resected from January 2007 to December 2019 at CHBAH. Data were obtained from the theatre registry and patient files from the department of records. Parameters analysed were patient demographics, histological reports, the description of the procedure performed and outcome. Patients were treated with full-thickness resection of the anterior abdominal wall tumour from skin to peritoneum aiming for a clear radial margin of 2 cm and a complete resection (R0). Technical details of tumour resection and reconstruction method complications were recorded.
Results
Thirteen procedures were performed on 11 patients. All were female with a median of 29 years (range 21–61). The excision of the abdominal wall and reconstruction were performed in all patients. The patients’ characteristics and surgical management are depicted in Table I. There was no enterocutaneous fistula and all split skin grafts (SSG) were successful. Seven patients were available for follow-up with a median of 5 years (1–11 years) and revealed gradual weakening of the abdominal wall that was less pronounced in the group where Permacol™ and normal skin cover were used. No patient received adjuvant therapy.
Discussion
This study is in keeping with the literature where abdominal wall location is the most common tumour site in young adults.6 Although all patients are female, relationship with pregnancy was established in only one case where the tumour was noted a few months post-delivery. Another unusual finding in this study is the relatively rapid tumour growth (6–24 months) with nearly all patients presenting with very large tumours.
The international guidelines from the desmoid tumour working group recognise the role of low dose chemotherapy, radiotherapy and certain drugs (nonsteroidal antiinflammatory drugs (NSAIDs) and anti-oestrogen.1,11,12 The antihormonal alone or in combination with NSAIDs reported partial, stable disease and disease progression of 25%, 65% and 10% respectively. Tyrosine kinase inhibitors were also tried in selected patients with unresectable disease. The overall response rate was 6%. More than a third of patients required dose reduction whereas 10% discontinued the treatment due to side effects. The result from the international, multi-institutional retrospective analysis reported 54.1% of partial response, 40.55% of stable disease and disease progression in 5.4% of 37 patients treated from 2000 to 2018 with low dose methotrexate and vinca alkaloid (vinorelbine and or vinblastine).11
Although these therapies can be used on DF tumours at all locations, they are generally used in the context of advanced or rapidly progressive disease that is irresectable or would involve multi-organ resection. The recommendation from the joint global consensus-based guidelines approach for
125 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Table I: Age, tumour size, tumour location, lead time and reconstructive method Age (years) Size (mm) Lead time (months) Site Type of biological implant Skin cover Additional procedures Complex procedure: full-thickness abdominal wall excision + reconstruction with implant (inlay) + additional procedures + skin cover 23 200 x 190 x 100 12 LUQ & LLQ Permacol™ Immediate SS Ribs resection, diaphragm re-implantation and insertion of ICD 37 95 x 75 x 150 < 24 RUQ Permacol™ Immediate SS Ribs resection, diaphragm re-implantation and insertion of ICD 29* 260 x 160 x 80 6 Most of the anterior abdominal wall Strattice™ SSG 6 weeks later Shaving of the pubic rami and resection of the dome of the bladder Standard procedure: full-thickness abdominal wall excision + reconstruction with implant (inlay) + skin cover 27 150 x 120 24 LLQ Permacol™ Immediate SS Nil 33 63 x 60 x 58 < 24 RUQ Permacol™ Immediate SS Nil 21# 157 x 135 x 95 12 LUQ & LLQ Permacol™ Immediate SS Nil 46 150 x 135 x 84 12 RUQ Permacol™ Immediate SS Nil 26** 175 x 145 x 95 12 RUQ & RLQ Permacol™ Immediate SS Nil 31 170 x 145 x 100 12 Peri-umbilical Strattice™ SSG 6weeks later Nil 29 127 x 96 x 250 > 12 RUQ Strattice™ SSG 6 weeks later Nil 61 175 x 150 x 104 < 24 Mainly RLQ & RUQ XenMatrix™ SSG 6 weeks later Nil * – recurrence, # – re-excision for involved margin, ** – tumour noted few months after delivery RUQ – right upper quadrant, RLQ – right lower quadrant, LUQ – left upper quadrant, LLQ – left lower quadrant, SS – undermined surrounding skin, SSG – split skin graft, ICD – intercostal drain
adult and paediatric patients emphasised the role of active surveillance in certain cases, relegating surgery or medical treatment to second-line therapy. When the disease progressed during active surveillance, preference was given to surgery for abdominal wall desmoid tumour or to medical therapy for intra-abdominal and extremities tumour.1,9
In comparing surgery alone versus surgery combined with radiation, the feeling was that radiation did not contribute much but was fraught with the risk of radiation-induced sarcoma.1
In this study, we used biological implants as they are the safest option to place directly onto the bowel, and this is believed to provide regenerative repair.14-16 The nature of the biological implants makes them prone to biodegradability by host enzymatic activities (collagenase, protease). This can lead to loss of integrity of the implant and eventual abdominal wall eventration. Certain biologics (like Permacol™) are cross-linked and bioengineered to resist the catalytic activity of the enzyme with expected satisfactory outcomes, considering the complexity of the abdominal wall defect.17 Both Strattice™ and XenMatrix™ are non-crosslinked acellular dermal reconstructive tissue matrix derived from porcine collagen. These are believed to provide durable abdominal wall support through their regenerative repair, biocompatibility and easy incorporation into the recipient tissue. However, that expectation was not met in our study as progressive abdominal wall weakness was noted. We did not come across any study that describes reconstruction of the abdominal wall after full-thickness excision except for a case report that shows no eventration after a short follow-up of 6 months,15,18 but the literature from the repair of incisional hernia with biological implant reports findings similar to our study when a biological implant is used as a bridge.14,17,19 Interestingly, no patient developed enterocutaneous fistula due to the presence of the biological implants.13,20 Nevertheless, we need to recognise that the biological implants alone are not expected to fulfil the role of satisfactory long-term abdominal wall substitute for full-thickness abdominal wall loss. We believe that such expectation is unrealistic. Biological implants are commendable in this study because they simplify the management of large abdominal wall defect that would otherwise have required complex plastic surgery reconstruction that is not without significant morbidity. Complex plastic reconstruction techniques are inappropriate to use as the primary procedure due to the possibility of local recurrence and donor site disability.
Conclusion
All our DF patients were female and had anterior abdominal wall tumours that had full-thickness abdominal wall excision. The resultant full-thickness defect was bridged with biological implants with minimal periprocedural morbidity. The recurrence rate was low in the 60% in whom follow-up was obtained. The abdominal wall-bridged defect exhibited gradual eventration with time, and it is unclear if further, more complex reconstructive abdominal surgery will be required for these patients.
Conflict of interest
The authors declare no conflict of interest.
Funding source
None.
Ethical approval
Ethical approval was obtained from the human ethics committee of the university of the Witwatersrand and the research review board of CHBAH (M191119).
ORCID


I Bombil https://orcid.org/0000-0002-4819-0785
L Ngobese https://orcid.org/0000-0001-8379-793X
REFERENCES
1. Desmoid tumour working group. The management of desmoid tumours – a joint global consensus-based guideline approach for adult and paediatric patients. Eur J Cancer. 2020;127:96107. https://doi.org/10.1016/j.ejca.2019.11.013.
2. Xiao J, Mao J, Li B. Clinical characteristic and treatment of intra-abdominal aggressive fibromatosis – a retrospective study of 16 patients. Front Med (Lausanne). 2020;7:2. https:// doi.org/10.3389/fmed.2020.00002.
3. Fisher C, Thway K. Aggressive fibromatosis. Pathology. 2014;46(2):135-40.
4. Huss S, Nehles J, Binot E, et al. β-Catenin (CTNNB1) mutations and clinicopathological features of mesenteric desmoid-type fibromatosis – CTNNB1 mutations of mesenteric desmoids. Histopathology. 2013;62(2):294-304.
5. Rossi S, Laurino L, Dei Tos AP. Desmoid-type fibromatosis: from morphology to molecular genetics. Diagn Histopathol. 2008;14(11):546-51.
6. Fletcher C, Bridge J, Hogendoorn P, Pancras C, Mertens F. WHO Classification of tumours of soft tissue and bone. 4th ed (IARC WHO Classification of Tumours). Lyon: IARC Press; 2013. p.72-6.
7. Kasper B. Desmoid tumours: a perfect example for making progress in treatment management through international collaboration. ESMO Open. 2019;4:e000636. https://doi. org/10.1136/esmopen-2019-000636
8. Papazoglou A, Komporozos V. Diagnosis and treatment of sporadic and familial adenomatous polyposis (FAP) –associated desmoid tumours: literature review. Hellenic J Surg. 2018;90:299-307. https://doi.org/10.1007/s13126-0180494-7
9. Ganeshan DM, Amini B, Nikolaidis P, Assing M, Vikram R. Current update on desmoid fibromatosis. J Comput Assist Tomogr. 2019;43(1):29-38. https://doi.org/10.1097/ RCT.0000000000000790
10. Sifumba S, Thomson SR, Madaree A. Desmoids don’t die. SAMJ. 1993;83(7):536-7.
11. Napolitano A, Provenzano S, Colombo C, et al. Familial adenomatosis polyposis-related desmoid tumours treated with low-dose chemotherapy – results from an international, multiinstitutional, retrospective analysis. ESMO Open. 2020;5(1). https://doi.org/10.1136/esmoopen-2019-000604.
12. Sharma V, Chetty DN, Donde B, et al. Aggressive fibromatosis – impact of prognostic variables on management. S Afr J Surg. 2006;44(1):6-8, 10-11.
13. Pickard HDP, Jacob N, Malherbe F, et al. The management of desmoid tumours at Groote Schuur Hospital – a retrospective review of current practice. South African Journal of Oncology. 2019;3. https://doi.org/10.4102/sajo.v3i0.68.
14. Patel KM, Nahabedian MY, Albino F, Bhanot P. The use of porcine acellular dermal matrix in a bridge technique for complex abdominal wall reconstruction – an outcome analysis.
Full list of references available on request.
126 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
South African Journal of Surgery. 2021;59(3):127a-127d
https://doi.org/10.17159/2078-5151/2021/v59n3a3196
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0] http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361
© 2021
A 7-year retrospective review of renal trauma in paediatric patients in Johannesburg
NZ Mashavave, A Withers, T Gabler, V Lack, D Harrison, J Loveland
Department of Paediatric Surgery, Chris Hani Baragwanath Academic Hospital, University of the Witwatersrand, South Africa
Corresponding author, email: nzxaba@gmail.com
Background: South African data on paediatric patients with renal trauma that are usually managed conservatively is scarce. This study aimed to review a 7-year experience of paediatric renal trauma and management.
Methods: A retrospective review of all paediatric admissions with renal injury was conducted in the Department of Paediatric Surgery, University of the Witwatersrand, between 1 January 2012 and 31 December 2018. Data from medical records reviewed included patient age, gender, mechanism of injury, severity of injury, management and length of hospital stay.
Results: Thirty-one patients with renal injuries were identified, of which 30 had complete data. Of these cases, 26/30 (87%) sustained blunt renal injuries and 4/30 (13%) were penetrating. The median age at presentation was 6 years, and 60% were females. Three patients had isolated renal injuries, and 23 had concomitant injuries including hepatic (9), thoracic (8), splenic (5), head (4), facial (3) and ureteric (1). Twenty-three patients were managed non-operatively. Two required renal exploration with resultant nephrectomies and one haemodynamically unstable patient died preoperatively. Four patients required operative intervention for concomitant injuries with no renal exploration. Two patients required ureteric stenting. The median length of hospital stay was 7 days (Range: 4–11 days, IQR 7 days).
Conclusion: Renal injuries in haemodynamically stable patients should be managed non-operatively. A 93% renal preservation rate was achieved in this cohort of patients with nephrectomy performed only in haemodynamically unstable patients with Grade V injuries, in keeping with international norms.
Keywords: paediatric, renal injuries, conservative management, South Africa






127 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
The
SURGERY
Author(s) PAEDIATRIC
Read the full article online at http://sajs.redbricklibrary.com
of Surgery. 2021;59(3):128a-128g
https://doi.org/10.17159/2078-5151/2021/v59n3a3264
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0]



http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361
© 2021 The Author(s) GENERAL
Diabetes and lower extremity amputation –rehabilitation pathways and outcomes at a regional hospital
P Manickum,1 SS Ramklass,1 TE Madiba2
1 School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
2 Department of General Surgery, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
Corresponding author, email: prabashni1@gmail.com
Background: Lower extremity amputations (LEAs) are most frequently due to diabetes mellitus (DM), a disease on the rise. The objective of this study was to determine the prevalence and aetiology of LEAs at Addington Hospital from 2013 to 2017 and to explore the physiotherapy referral practices and outcomes.
Methods: Retrospective study carried out at Addington Hospital, Durban. Patients who underwent LEAs were filtered from theatre registers and the hospital Meditech database. Data collected included patients' demographic profile, diabetic status, level of amputation, limb orientation, physiotherapy referral status, and rehabilitation outcomes. Physiotherapy files were scanned for the attendance of referred patients. Study endpoints were prevalence, diabetes status, referral status, compliance and rehabilitation outcomes.
Results: From 2013 to 2017, 1 028 LEAs in 843 patients were identified with single amputations (697) and multiple amputations (146). The median age was 61 (IQR 52–68) years, and the M:F ratio was 1.3:1. A total of 574 (68.1%) patients had DM. Seven hundred and thirty-eight (71.8%) amputations were as a result of DM. The level of amputations was below-knee (479; 46.6%), toectomy (236; 23%), above-knee (196; 19%) and trans-metatarsal (117; 11.4%). Only 148 patients (17.6%) were referred for physiotherapy, of which 91 (61.5%) attended. Mobility in those who attended rehabilitation was with a walking frame (51; 56%), crutches (29; 31.9%), prosthesis and crutches (7; 7.7%), and wheelchair-bound (4; 4.4%).
Conclusion: Over half the amputations were associated with DM, which was also a risk factor for multiple amputations. Although referral and attendance for physiotherapy were very poor, mobility in those who attended was excellent, indicating a dire need to improve hospital referral pathways.
Keywords: prevalence, diabetes mellitus, lower extremity amputations, rehabilitation, physiotherapy
Read
128 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
SURGERY
Journal
South African
the full article online at http://sajs.redbricklibrary.com
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0] http://creativecommons.org/licenses/by-nc-nd/4.0
ISSN 038-2361


© 2021 The Author(s)
Factors affecting bacteriology of hand sepsis in South Africa
M van der Vyver, A Maderee
Department of Plastic and Reconstructive Surgery, Inkosi Albert Luthuli Central Hospital, South Africa
Corresponding author, email: marietavdv@gmail.com
Background: Hand sepsis is a common cause of morbidity. The study was conducted in the KwaZulu-Natal province of South Africa, investigating the bacteriological profile and aetiology of hand sepsis, aiming at optimising empiric antibiotic therapy.
Methods: This is a descriptive study of 120 patients who presented to the plastic surgery department of Inkosi Albert Luthuli Central Hospital with hand sepsis, from January 2017 to April 2019, that required surgical drainage. Data recorded included: aetiology of sepsis, underlying comorbidities, length of hospital stay, and outcome. A pus swab was taken during surgical drainage for microscopy, culture and sensitivity (MCS) analysis. The relationship between clinical factors and microbiological findings was analysed.
Results: The predominant bacterial strains cultured from infected patients, excluding methicillin-resistant Staphylococcus aureus, were Staphylococcus aureus (80.8%) and Streptococcus spp. (20.0%), mostly due to spontaneous onset infection (58.3%). Cultures of the more problematic Streptococcus spp. were more frequently associated in patients with diabetes mellitus (60.0%), penetrating trauma (41.9%), or blunt trauma (31.3%). The diabetes group in isolation had the longest median hospital stay of 8 (5–15) days, the most need for multiple procedures (60.0%), amputations (30.0%), and skin grafts (20.0%). The most effective antimicrobial drug particularly in mixed cultures was amoxicillin-clavulanic acid.
Conclusion: Staphylococcus aureus infection was the most common. Streptococcus spp. occurred more frequently in patients with traumatic injury and diabetes mellitus. The latter required further surgical procedures and an increased hospital stay. Amoxicillin-clavulanic acid is the preferred empiric antimicrobial agent.
Keywords: hand sepsis, bacteriology, optimising empiric antibiotic therapy
129 SAJS VOL. 59 NO. 3 SEPTEMBER 2021 South African Journal of Surgery
PLASTIC SURGERY
South African Journal of Surgery. 2021;59(3):129a-129e
https://doi.org/10.17159/2078-5151/2021/v9n3a3318
Read the full article online at http://sajs.redbricklibrary.com
South African Journal of Surgery. 2021;59(3):130a-130c
https://doi.org/10.17159/2078-5151/2021/v59n3a3410
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0] http://creativecommons.org/licenses/by-nc-nd/4.0
Cardiac tamponade following post-pericardiotomy syndrome
K Gandhi,1,2 JSK Reinders,1,3 PH Navsaria1
1 Trauma Centre, Department of Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
South African Journal of Surgery
ISSN 038-2361
© 2021
The Author(s)
CASE REPORT
2 Surgical Gastroenterology Unit (HPB), Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
3 Trauma Department, Groene Hart Hospital, Gouda, The Netherlands
Corresponding author, email: dr.karan.gandhi@gmail.com
Summary
Subxyphoid pericardial window (SPW) is performed as both a diagnostic and therapeutic intervention in patients presenting with a penetrating cardiac injury (PCI). Post-pericardiotomy syndrome (PPS) with cardiac tamponade has been reported after penetrating cardiac trauma1 and after transdiaphragmatic pericardial window.2 We describe the first PPS with acute tamponade, weeks after diagnostic SPW for a PCI.
Read the full article online at http://sajs.redbricklibrary.com
South African Journal of Surgery. 2021;59(3):130d-130e https://doi.org/10.17159/2078-5151/2021/v59n3a3490
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0] http://creativecommons.org/licenses/by-nc-nd/4.0
An inguinal hernia imposter
RR
1 Department of General Surgery, Groote Schuur Hospital, South Africa
2 Department of General Surgery, Victoria Hospital, South Africa
3 Department of Anatomical Pathology, Groote Schuur Hospital, South Africa
Corresponding author, email: ravin.patel.3@gmail.com
Summary
South African Journal of Surgery
ISSN 038-2361
© 2021 The Author(s)
CASE REPORT
This is a report of one of the many imposters of an irreducible inguinal hernia, a dermoid cyst. It is a rare entity that should be considered in the differential diagnosis of a groin lump when an atypical clinical presentation or groin examination occurs. Complete excision with histological evaluation remains the mainstay of surgical treatment.
Keywords: dermoid cyst, inguinal hernia, inguinal canal, incarcerated, hernia surgery





Read the full article online at http://sajs.redbricklibrary.com

130 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
Patel,1,2 S Tu,3 J Plaskett2
South African Journal of Surgery. 2021;59(3):131a-131c https://doi.org/10.17159/2078-5151/2021/v59n3a3609
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0] http://creativecommons.org/licenses/by-nc-nd/4.0
South African Journal of Surgery
ISSN 038-2361
© 2021 The Author(s)
CASE REPORT
The role of surgery in Conn’s syndrome –a case of refractory hypertension secondary to an aldosterone secreting adenoma
MD Carides,1 NT Sishuba,2 I Bombil,3 C Christofides3
1 Medical Outpatient Department, Bertha Gxowa Hospital, South Africa
2 Department of Surgery, Charlotte Maxeke Johannesburg Academic Hospital, South Africa
3 Department of Surgery, Chris Hani Baragwanath Academic Hospital, South Africa
Corresponding author, email: michaelac@live.co.za
Summary
Primary aldosteronism, eponymously known as Conn’s syndrome, has recently gained recognition as the most common cause of endocrine hypertension. Unilateral subtypes, such as aldosterone secreting adenomas, are managed surgically and are potentially curable. The background of refractory hypertension and hypokalaemia in a forty-year-old man raised suspicions of Conn’s syndrome which was localised to an aldosterone secreting adenoma in the right adrenal gland. The patient underwent a laparoscopic intraperitoneal right adrenalectomy which resulted in normalisation of his plasma aldosterone concentration as well as improved blood pressure control.
Read the full article online at http://sajs.redbricklibrary.com
South African Journal of Surgery. 2021;59(3):131d-131f
https://doi.org/10.17159/2078-5151/2021/v59n3a3544
Open Access article distributed under the terms of the Creative Commons License [CC BY-NC-ND 4.0] http://creativecommons.org/licenses/by-nc-nd/4.0
South African Journal of Surgery
ISSN 038-2361






© 2021 The Author(s) CASE REPORT
Biliary tract anatomical variance – the value of MRCP
C Ferreira,1 CB Noel2
1 Department of Surgery, Faculty of Health Sciences, University of the Free State, South Africa
2 Department of General and Hepatopancreaticobiliary Surgery, Universitas Academic Hospital, South Africa
Corresponding author, email: ferreirac4@ufs.ac.za
Summary
Duplication of the common bile duct (CBD) is a rare congenital anomaly of the bile ducts that should be diagnosed prior to surgery in order to optimise management and prevent complications. We report a case of a patient presenting with choledocholithiasis and type Va duplicated extrahepatic bile duct that was missed on ultrasonography. The atypical course prompted further imaging with magnetic resonance cholangiopancreatography (MRCP), which identified the aberrant bile duct and assisted in safe preoperative and operative management. This case highlights the importance of accurate pre-interventional imaging and agrees with the reclassification of duplications of the CBD.
Keywords: bile duct, extrahepatic, anomaly, duplicated, injury
Read the full article online at http://sajs.redbricklibrary.com
131 SAJS VOL. 59 NO. 3 SEPTEMBER 2021
SAJS CPD QUESTIONS
- Please submit online before 31 March 2022 -
The surgical burden of breast disease in KwaZulu-Natal province
1. Choose the incorrect answer: Regarding the surgical burden of breast disease
a. Low- and middle-income countries (LMICs), in sub-Saharan Africa, lack health services and systems’ research.
b. A number of long-term trends in South Africa, such as surgical sub-specialisation and multidisciplinary surgical oncology teams, have had minimal impact on the management of breast pathology.
c. There is a significant burden of breast-related pathology requiring surgical treatment in KZN, and comprises roughly 6% of the total general surgical procedures within the province.
d. The care of breast pathology needs to be streamlined, and the development of referral algorithms is warranted.
2. Choose the incorrect answer: Regarding the surgical management of benign and non-benign breast disease
a. One-third of breast surgery in KZN province is for nonbenign disease.
b. Mastectomy is the most common procedure for non-benign breast disease, and 70% of patients also have an axillary lymph node dissection (ALND).
c. Approximately 70% of sepsis-related breast procedures are performed at secondary/regional facilities, while about 60% of non-benign breast surgeries are performed at tertiary and quaternary centres.
d. Incision and drainage of breast abscesses comprise under 2% of procedures performed for breast sepsis.
An audit of patients clinically deemed as high risk for malignant breast pathology at the Helen Joseph Hospital
Breast Clinic
3. True or false: The Helen Joseph Hospital Breast Clinic triages patients presenting at the Breast Clinic into three groups according to strict clinical criteria: high-, intermediate-, and low-risk cases.
a. True
b. False
4. Choose the incorrect answer: Regarding patients presenting with benign breast disease
a. The majority of patients presenting with breast complaints are found to have benign breast disorders, as seen in both developing and developed countries.
b. Benign breast disorders have various modes of presentation and comprise multiple entities; thus, adequate diagnosis is required to avoid misassessment of malignant pathology.
c. Benign phyllodes tumour carries a minimal risk of progression to malignant phyllodes tumours.
d. Triple (clinical, radiological and pathological) assessment is the gold standard to achieve a definitive diagnosis of a breast complaint.
5. Choose the incorrect answer: Regarding patients presenting with benign breast disease
a. The age distribution amongst patients presenting with clinically benign breast disease at an open access breast clinic in Johannesburg is similar to that seen in developed countries.
b. Clinical examination alone has a sensitivity of 54%, while its specificity is 94%; thus, some suspicious lesions may be misdiagnosed as benign pathology.
c. About 4% of the total patient sample had a confirmed malignancy on biopsy, which is in keeping with international standards.
d. Some malignant lesions, such as malignant phyllodes, lymphoma and mucinous breast carcinoma, can mimic benign disease clinically and on imaging.
Subscribers and other recipients of SAJS visit our new CPD portal at www.mpconsulting.co.za
• Register with your email address as username and MP number with seven digits as your password and then click on the icon “Journal CPD”
• Scroll down until you get the correct journal. On the right hand side is an option “ACCESS”. This will allow you to answer the questions. If you still can not access please send your Name and MP number to cpd@medpharm.co.za in order to gain access to the questions.
• Once you click on this icon, there is an option below the title of the journal: Click to read this issue online

• Once you have completed the answers, go back to the top of the page next to the registration option. There is another icon “Find my CPD certificate” (You will have to answer the two questions regarding your internship and last CPD audit once you have completed a questionnaire and want to retrieve your certificate).
Medical Practice
• Please call MPC Helpdesk if you have any questions: 0861 111 335. MDB015/1329/08/2021
• If you click on that icon it will open your certificate which you can print or save on your system.
Volume 59 | No. 3 | September 2021
Consulting: Client Support Center: +27121117001 Office – Switchboard: +27121117000

WHAT MAKES OUR JOURNALS DIFFERENT? • Peer reviewed articles • 11 medical journals to choose from • Official journal at society related congresses • Official journal for the various related societies • All journals available digitally www.medpharm.co.za • Academic medical journals that reach YOUR target market • Privately owned company (Directors: Prof. Oppel Greeff & Pierre Marais) MEDICAL AND PHARMACEUTICAL JOURNAL PUBLISHER Black on white Reversed (White on black) Grey scale Main Logo (full colour) MEDPHARM PUBLICATIONS LOGO Colours: CMYK Red C: 0 M: 100 Y: 100 K: 0 CMYK Green C: 90 M: 0 Y: 70 K: 10 Web Red # ed1c24 Web Green # 009f73 Pantone Red Pantone Red 032 C Pantone Green Pantone 7724 C Fonts: Myriad Pro
WWW.MEDPHARM.CO.ZA
a
WHY WOULD YOU LOOK ANYWHERE ELSE?
A publications list of more than ten titles comprising of over fifty journal editions. With
reach of more than 40 000 healthcare workers countrywide.
Paracetamol Fresenius


10 mg/ml
Short-term treatment of mild to moderate pain and the shortterm treatment of fever when the oral route of administration is unsuitable1


CONVENIENT BUILT IN HANGER ON BOTTLE LABEL

1

Peel label from here

2
4
S3 PARACETAMOL FRESENIUS 10 mg/ml (100 ml): Each bottle contains 1 g of paracetamol. 45/2.7/1188. Reference: 1) Fresenius Kabi data on file. *As per the latest Department of Health (DOH) published price. For full prescribing information refer to Professional Information approved by the South African Health Products Regulatory Authority. Fresenius Kabi South Africa (Pty) Ltd, Reg. No.: 1998/006230/07. Stand 7, Growthpoint Business Park, 162 Tonetti Street, Halfway House, Extension 7, Midrand, Gauteng, 1685. PO Box 4156, Halfway House 1685 Tel:+ 27 11 545 0000 Fax: + 27 11 545 0060 www.fresenius-kabi.co.za Quality Hospital Care IN STOCK SEP per single unit R14,47* Exc. VAT IMA_18_5_2021_V1
3