
























Social prescribing is a fairly new concept, but one all GPs should be familiar with. It’s often free for patients and can bring a wealth of benefits.
Andrea Downey | Managing Editor
YOU ASKED, WE DELIVERED: WE ARE NOW CPD VERIFIED


Complete the self-reflection and claim your CPD time, please scan here
The benefits of movement and exercise are well known, so is it about time it’s discussed as part of routine appointments?
Exercise has been linked to lower levels of obesity, reducing the risk of heart disease and diabetes, and improving mental health outcomes for conditions such as depression.
Yet statistics tell us that not enough Aussies are meeting exercise requirements. Alongside this, rates of loneliness are rising.
And just 18% report receiving a physical activity recommendation from their GP in the past year.
One solution to this is social prescribing – encouraging patients to exercise through joining running groups, walking groups or any other sports club.
Social prescribing is a fairly new concept, but one all GPs should be familiar with. It’s often free for patients and can bring a wealth of benefits.
I can personally attest to the benefits of exercise; it never fails to boost my mood, helps me sleep better and, in the interest of honesty, is beneficial to everyone around me as it helps me manage my stress levels.
So, this month I found our feature on how to prescribe exercise personal. It looks at what social prescribing is, how GPs can put it into practice and where they can refer patients.
SYNDICATION AND REPRODUCTION Contributors should be aware the publisher asserts the right to syndicate material appearing in Medical Forum on the mforum.com.au website. Contributors who wish to reproduce any material as it appears in Medical Forum must contact the publisher for copyright permission.
DISCLAIMER Medical Forum is published by Medforum Pty Ltd (Publisher) as an independent publication for health professionals in Western Australia. Neither the Publisher nor its personnel are medical practitioners, and do not give medical advice, treatment, cures or diagnoses. Nothing in Medical Forum is intended to be medical advice or a substitute for consulting a medical practitioner. You should seek immediate medical attention if you believe you may be suffering from a medical condition. The support of all advertisers, sponsors and contributors is welcome. To the maximum extent permitted by law, neither the Publisher nor any of its personnel will have any liability for the information or advice contained in Medical Forum. The statements or opinions expressed in the magazine reflect the views of the authors and do not represent the opinions, views or policies of Medical Forum or the Publisher. Readers should independently verify information or advice. Publication of an advertisement or clinical column does not imply endorsement by the Publisher or its contributors for the promoted product, service or treatment.
Advertisers are responsible for ensuring that advertisements comply with Commonwealth, State and Territory laws. It is the responsibility of the advertiser to ensure that advertisements comply with the Competition and Consumer Act 2010 (Cth) as amended. All advertisements are accepted for publication on the condition that the advertiser indemnifies the Publisher and its personnel against all actions, suits, claims, loss or damages resulting from anything published on behalf of the advertiser.
EDITORIAL POLICY This publication protects and maintains its editorial independence from all sponsors or advertisers. Medical Forum has no professional involvement with advertisers other than as publisher of promotional material. Medical Forum cannot and does not endorse any products.




48 Next of Kin: what to expect when caring for someone

Terracotta Warriors 53 Mandoon Estate – wines of regional character – Dr Craig Drummond MW

Our bumper round of competitions continues this month with plenty to choose from.
Win one of three copies of Next of Kin: What to expect when you’re expecting to care for a loved one
Or win one of 10 double passes to see two different films opening in October. If you’d prefer a glass of wine, we’ve got a doctor’s dozen to give away from Mandoon Estate.
See our lifestyle section for this month’s wine review and more details on our competitions.
PUBLISHERS
Alice Miles – Director Fonda Grapsas – Director
Tony Jones – Director tonyj@mforum.com.au
EDITORIAL TEAM
Managing Editor
Andrea Downey 0437 909 904 andrea@mforum.com.au
Clinical Editor
Dr Joe Kosterich 0417 998 697 joe@mforum.com.au
Graphic Design
Ryan Minchin ryan@mforum.com.au
ADVERTISING
Advertising Manager
Bryan Pettit 0439 866 336 bryan@mforum.com.au
Advertising Account Manager
Rita Murphy 08 9203 5222 rita@mforum.com.au
Clinical Services Directory
Alice Miles 08 9203 5222 alice@mforum.com.au
CONTACT MEDICAL FORUM
Suite 3/8 Howlett Street, North Perth WA 6006
Phone: 08 9203 5222 Fax: 08 6154 6488 Email: info@mforum.com.au www.mforum.com.au



















New updates to the Australian Asthma Handbook advise doctors to stop prescribing or advising treatment with as-needed shortacting beta2 agonists (SABA) alone to manage asthma in adults and adolescents.
Put together by the National Asthma Council Australia (NAC) the guidance now recommends anti-inflammatory reliever (AIR)-only therapy and maintenance-and-reliever therapy (MART) for adults and adolescents aged over 12.
Dr Brett Montgomery, Perth GP and member of the NAC Guidelines Committee told Medical Forum inhaled corticosteroids (ICS) were now indicated for all adults and adolescents with asthma.
“The last lot of guidelines said that there was a small number of people we could manage on short-acting beta agonists alone – people who had not had an exacerbation in the last year and only got their symptoms rarely. Many international guidelines have moved away from allowing that and we have followed suit in this new edition,” he said.
“Now, if you’re an adult or an adolescent who has asthma, we don’t think anyone should be managed on short beta agonists alone, instead we think everyone should have treatment that includes an inhaled corticosteroid. Our preferred starting approach will be to use a combination inhaler containing budesonideformoterol.”
The use of short-acting beta agonists alone for children was still an option, but the thresholds for the use of
More overseas trained doctors are heading to WA through a fasttracked program to boost the workforce, but there are concerns they are not getting the support they need.
New data from Ahpra show in the six months from 21 October 2024 to 30 April 2025 some 20 doctors recruited through the Expedited Specialist Pathway have identified WA as their preferred place of practice.
Of those, 19 were GPs and one was an anaesthetist. Further detail up to the end of August show the number of doctors registering to work in WA was 49.
But there were concerns about the level of support international medical graduates (IMGs) are receiving.

inhaled corticosteroid in children had changed slightly.
In terms of diagnosis, doctors should consider the use of fractional exhaled nitric oxide (FENO) testing in addition to spirometry as another way of proving a diagnosis.
“Nitric oxide is a chemical that is produced in our body when there’s inflammation. It’s important in blood vessels but can also be detected in tiny amounts in expired breath. If it’s above a certain threshold then we say that is also evidence of asthma” he said.
The new guidelines emphasised the importance of referral to appropriate specialists instead of increasing prescriptions or dosages.
“If asthma symptoms are still uncontrolled despite escalating therapy, we are wanting to emphasise the importance of referral to respiratory specialists to consider monoclonal antibody treatment,”
Dr Montgomery said.
The AMA wants to see more done to ensure IMGs practising in Australia can thrive. IMGs now make up 53% of Australia’s rural medical workforce and account for more than 50% of all GPs nationwide.
The AMA surveyed its members and published a report outlining the lived experiences of IMGs, the systemic barriers they encounter, and opportunities for reform.
AMA National President Dr Danielle McMullen said many reported feeling trapped in a complex and confusing registration process.
“Discrimination and anticompetitive practices only deepen their frustration and sense of exclusion, delaying their integration and eroding trust in the system itself,” Dr McMullen said.
“Qualified doctors are left feeling stuck, navigating a maze
of duplicate documentation, inconsistent requirements, and vague job descriptions at a time when Australia faces widespread medical workforce shortages that are only expected to worsen.”
To provide better support, the RACGP has launched fellowship to support overseas trained doctors when they arrive in Australia.
Vice President and WA Chair Dr Ramya Raman said: “These doctors are already working safely in our communities. By offering them fellowship, we can reduce professional isolation, strengthen their connection to Australian standards, and ensure they have access to ongoing education, mentorship, and resources.”
ADHD professionals are calling for a nationally consistent approach to diagnosing and prescribing for reforming care.
Professor Dave Coghill, President Australasian ADHD Professionals Association (AADPA), said with the first of WA’s specially trained GPs set to begin diagnosing and treating ADHD next year, now is the time for consistency.
It comes after a meeting between state and territory health ministers with their federal counterpart on September 12.
AADPA and others called on ministers to make prescribing rules consistent across Australia so specialist GPs, psychiatrists and paediatricians would be able to start, change, and continue ADHD medications by 30 June 2026.
However, no specific decisions were made at the meeting.
“Once WA and NSW actually implement their changes with GPs becoming more involved, then it’s going to be increasingly different between the states, so I think now is a good time to act when we’re just starting that journey,” Prof Coghill told Medical Forum
Chair of the RACGP WA ADHD Working Group Dr Sean Stevens said: “WA is one of the states and territories leading the way on reforming ADHD prescribing to empower GPs and help more patients get the care and treatment they need with less cost and fewer delays.
“The first WA GPs to independently diagnose and manage ADHD will start providing this care in early 2026, which is a huge step forward.”
For more news visit mforum.com.au and hit the ‘news’ tab
A new round of West Australian GPs were awarded a Fellowship of the RACGP last month.
Some 84 GPs were welcomed as fellows at a ceremony on September 19.
Fellowship of the RACGP recognises a doctor’s qualification and expertise as a specialist GP.
Achieving Fellowship represents the gold standard of general practice in Australia, typically following around 11 years of education, clinical training, rigorous assessment, and hands-on experience in primary care.
In addition to the newly recognised Fellows were three Rural Generalists – GPs who undertook additional rural skills training in fields vital to rural communities, such as emergency medicine and obstetrics.
RACGP Vice President and Western Australia Chair Dr Ramya Raman congratulated the GPs and said many have a strong track record and passion for helping patients in rural communities.
“It’s great news that 20 of the new Fellows are from rural areas and they have inspiring stories to tell,” she said.



“This includes Dr Megan Robertson, who completed the majority of her community GP training in regional Western Australia. She is motivated by a deep commitment to supporting rural and remote communities and embraced the challenges of remote general practice care.
“ Dr Charl Du Plessis who attained Rural Generalist Fellowship, has worked as a solo GP covering the entire Northern Goldfields area, including Leonara and Laverton, and ran outreach clinics to Cosmo Newberry, a remote Aboriginal community. When COVID-19 struck, he made the call to stay in the community to help patients in need.”
Ramsay Health Care are hosting a ‘Men’s health matters masterclass’ in November.
GPs can tick off their CPD and hear from specialists on male infertility, suicide and urological cancers.
Held on November 1 at Rendezvous Scarborough Hotel.
Visit www.joondalupprivate.com.au or email hensonw@ramsayhealth.com.au
Concept Fertility are hosting a GP Fertility Evening on November 5, covering PCOS, their donor program and fertility technology.
Hear from Concept’s new Medical Director Dr Sebastian Leathersich and enjoy a complimentary three-course dinner at Cooee Next Door.
Visit www.conceptfertility.com.au and head to their GPs section for more information
What if they told you
The Photon Counting CT machine at ChestRad requires ten times less radiation dose for lung cancer screening
All lung cancer screening bulk billed
1 Heismann, B Photon counting CT versus energy-integrating CT: A comparative evaluation Med Physics Dec 2024
Finding - Siemens Naeotom Alpha PCCT ten times more dose efficient for LCS than Siemens Definition Force
2. American Association of Physicists in Medicine Lung Cancer Screening CT Protocols V 6 0 November 2023
Finding - Siemens Definition Force four times more dose efficient for LCS than the next best CT machine

There is no doubt that movement is medicine, so how can doctors and allied health workers get on board when it comes to prescribing exercise to patients?
Not enough is known about the program set to replace the NDIS support currently provided to autistic children to know whether it will meet their needs, leading WA health professionals have said.
Federal Health and Disability Minister Mark Butler announced a new program called Thriving Kids will replace NDIS support, which will begin rolling out in mid-2026. He said the change was needed to keep the NDIS sustainable.
According to a government fact sheet, Thriving Kids will be delivered by scaling and building on existing mainstream and community services.
“This includes child and maternal health, GPs, playgroups, early childhood education and care and schools, as well as digital and phonebased supports.”
Dr Andrew Leech, GP and director of Garden Family Medical, sees many families with children who have autism and said the changes were causing anxiety.
“We’re hearing a lot of stress in families at the moment around the uncertainty of what’s going to happen, particularly the ones that are just starting the process,” he told Medical Forum
“These families need support, they are already exhausted and overwhelmed trying to navigate the system.”
He said without detail on what Thriving Kids will look like, it was also difficult to say what role GPs might play.
“Whatever happens, we GPs also need education and support on how to navigate this system and not be left out,” he said.
By Aleisha Orr

Professor Andrew Whitehouse said support services need to focus on empowering children in their everyday spaces.
“The NDIS does need to be reviewed or restructured because of a changing landscape with managing disability and how we deal with the increasing number of children needing support. We need to make it sustainable and accessible to everyone.”
The Kids Research Institute Australia deputy director Professor Andrew Whitehouse also acknowledged that the NDIS needed reform and does not necessarily support people with autism in the best way.
“The NDIS is geared towards providing support in clinical environments and that might be good for individuals with quite significant levels of disability, but with less severe disability needs the supports need to be in the community. That’s where the NDIS perhaps let kids and families down,” Professor Whitehouse told Medical Forum
But he said not enough was known about Thriving Kids to know if it would meet the individual needs of children with autism.
Concerns around whether health systems were geared up to cope with the changes were also raised.
Tenielle Williams, a registered psychologist at Kidd Clinic, said the proposal to move autism support outside of the NDIS represented a significant structural shift in how services were delivered and funded.
“At worst, families may be forced to disengage from established clinicians and restart therapeutic relationships with unfamiliar providers.
“More clinician time spent navigating bureaucracy rather than engaging in therapeutic work could lead to a destabilisation of the private sector workforce if clinicians lose NDIS-funded referrals, leading to workforce attrition at a time of already high demand.”
The Federal Government has committed $2 billion towards Thriving Kids and is hoping states and territories will match that to have the program fully implemented by mid-2027.
For more on this story visit www.mforum.com.au/features
Concept Fertility recently launched a new enhanced outpatient gynaecology service, and welcomed Medical Director
Dr Sebastian Leathersich.

Concept Fertility takes pride in its leading team of fertility specialists, gynaecologists, scientists and nurses, as well as its state-of-the-art laboratories and day hospital. Delivering the latest advances in fertility technology and women’s health, Concept’s priority is to ensure patients receive the highestlevel of quality care, whatever their treatment journey entails.
Since the start of this year Concept has seen exciting changes, with the appointment of a new Medical Director, Dr Sebastian Leathersich, and the addition of new services including Office Gynaecology with Dr Babak Shakeri.
is the highest level of fertility training available in Australia, held by only two other practising specialists in WA.
“My local and international experience and my advanced training in reproductive medicine give me the background and perspective to further build and develop Concept moving forward, providing comprehensive, compassionate and exceptional care to couples and individuals seeking fertility care,” Dr Leathersich said.

Leading this new era, Dr Leathersich brings a fresh perspective to Concept having recently returned from two years working in Spain. He is highly regarded for his clinical and academic experience, both locally and internationally, and his Certification in Reproductive Endocrinology and Infertility (CREI)
“We have a brilliant team at Concept, who are deeply committed to providing the highest standard of care and achieving the best possible outcomes for patients. From one of Australia’s top scientists, Scientific Director Dr Melanie Walls, PhD, to our team of highly experienced nurses, Concept is backed by some of the greatest talents in the field.”
Dr Leathersich is also experienced in fertility preservation and oncofertility, a vital service ensuring any person who is facing cancer treatment that might impact their fertility can receive counselling and be offered fertility preservation, when appropriate.
Dr Leathersich will see urgent fertility preservation cases within one to two business days, giving patients time to consider their options and proceed with treatment as quickly as possible.
He also specialises in male infertility and can provide advanced treatments and procedures to retrieve sperm, from medical management to surgical sperm retrieval, including microsurgical sperm extraction (microTESE). These treatments are only offered by a handful of specialists in Perth.
Gynaecologist
Dr Babak Shakeri joined the clinic earlier this year and recently introduced Office Gynaecology as a new service. Providing convenient treatment where women can be seen, assessed and treated quickly (often in a single visit or within one to two weeks), this service reduces the anxiety of long wait times and allows patients to get back to normal life, fast.


Diagnostic and operative hysteroscopy
NovaSure® endometrial ablation for heavy menstrual bleeding
MyoSure® procedures for fibroids and polyps
Colposcopy, cervical biopsy, and LLETZ for abnormal screening results
Contraception counselling and insertion of long-acting reversible contraceptives
Pelvic pain and endometriosis management in selected cases
Fertility-preserving gynaecology that integrates closely with IVF treatment.
With experience in both public and private hospitals, Dr Shakeri has worked in complex surgical and routine gynaecology and has seen firsthand how valuable office-based care can be for patients.
“I started my career in obstetrics and gynaecology in Sydney, including training in advanced laparoscopic and minimally invasive gynaecology. Since 2019, I have been a consultant obstetrician and gynaecologist at Fiona Stanley and Fremantle Hospitals. I also attend office gynaecology clinics at Fremantle Hospital,” Dr Shakeri said.
“In the public system I regularly see women in distress, waiting for care that could be provided quickly in the right setting. Working in these clinics
has shown me how much patients value choice and efficiency. People want procedures done quickly and safely, with minimal disruption to their lives.
“At Concept, our aim is to meet this need by offering outpatient procedures within one to two weeks. By shifting suitable cases into the office setting, we not only help patients sooner but also reduce the strain on hospital operating theatres and inpatient beds,” says Dr Shakeri.
Office gynaecology, sometimes called ambulatory or procedural gynaecology, refers to procedures that are performed in a clinic instead of a hospital.
For complex and high-risk cases, inpatient surgery is essential,
however many other lower risk common procedures are considered safe and effective in an outpatient setting. Evidence also shows that outcomes are comparable, and, in many cases, patient satisfaction is higher.
“My patients benefit from a quick diagnosis and treatment, for example, a woman with heavy bleeding can have a consultation, a hysteroscopy, and even a treatment such as polyp removal or ablation within one to two weeks. Similarly, a woman with an abnormal cervical screening test can have a colposcopy and if required LLETZ within the same timeframe.”
Pain management is critical to making outpatient gynaecology successful. Depending on the patient and the procedure, there are a range of options used for pain management, this includes oral analgesics and anxiolytics, local anaesthetic gel and targeted local anaesthetic injections, methoxyflurane commonly known as the “green whistle” and for selected cases – light or deeper sedation.
With Dr Shakeri, Concept now offers a complete suite of outpatient gynaecology services where everything is coordinated by a single team, offering patients seamless continuity of care.
There is no doubt that movement is medicine, so how can doctors and allied health workers get on board when it comes to prescribing exercise to patients?
By Suzanne Harrison
Rachel Hutchinson experienced pain in her hips from a young age. It wasn’t until her mid-30s – when she and her family moved to Perth –that she was finally diagnosed with hip dysplasia.
“I was always very active, but I was unable to continue doing the things I loved due to my hips deteriorating so rapidly,” the now 41-year-old, mother-of-two said.
“Just walking a few hundred metres was very hard and I was on crutches.”
By the time of her diagnosis, arthritis had set in severely in both hips, and surgery was the only solution. Luckily her physiotherapist encouraged Pilates prior to the operation.
“Pilates was not something that had ever interested me, so it took
a bit of persuading. I had a lot of preconceived ideas and didn’t think I would get the same satisfaction that a gym workout or run provides.”
She decided to give reformer classes a go, which has low to no impact on the joints. She pushed herself as much as possible and worked hard to build muscle pre-and postsurgery.
“My recovery was quick. I began walking stairs the day after the surgery and after six weeks I was able to start working out and gradually build it up.”
While advice to start an exercise program is typical from a physiotherapist, it has become more commonplace among Australian GPs, under the banner term ‘social prescribing’.
This takes the concept of simply
suggesting more movement for patients a step further, so to speak, to actually prescribe things like exercise as a non-pharmaceutical treatment option.
The question is, what does this approach look like in daily practice? And should it be taught – or at least formally advised – to medical students and practitioners?
According to the Australian Journal of General Practice (AJGP) exercise prescription, while not traditionally part of the medical school curriculum or involved in many advanced post-graduate training programs, is rapidly becoming an essential skill in primary care.
“Its importance relates to exercise being an effective evidence-based intervention for osteoarthritis, back pain, tendinopathy, some
cancers, depression, diabetes and cardiovascular diseases,” according to the AJGP.
“Although referral to an exercisebased practitioner is a useful option, exercise prescription should become embedded as part of primary care medical practice because of its reported effectiveness and minimal side effects when appropriately implemented.”
In other words, just telling patients that ‘exercise is good for you’ is not enough.
The Australian Bureau of Statistics reports that in 2022 83% of adolescents aged 15–17 did not meet physical activity recommendations, 80% did not do enough musclestrengthening activities, and 37% of adults aged 18–64 did not meet physical activity recommendations.
In June last year, the Australian Institute of Health and Welfare reported that physical inactivity is the ninth leading preventable cause of ill health and premature death.
So, what does social prescribing for exercise look like in a medical setting?
RACGP National Chair Social Prescribing Special Interests Group
Dr Kuljit Singh is a strong proponent of a multi-faceted approach that utilises community programs.
Dr Singh told Medical Forum GPs play an increasingly important role when it comes to holistic health advocacy.
Patients at risk of heart disease, obesity, diabetes, mental health issues, musculoskeletal conditions, or social isolation and loneliness are candidates for prescribing more movement.
The concept of social prescribing is not new, but in our post-Covid world where loneliness has become an epidemic, group exercise can alleviate that isolation.
Dr Singh suggests that a question focusing on social isolation and loneliness be added to GP checklists for more proactive identification, and that link workers like community connectors or wellbeing officers are advocated to manage additional needs and provide more personalised support.
GPs can also emphasise the impact of social disconnection and often associated lack of physical activity using statistics and evidence.
“Social connection is as vital as physical activity for overall health; group exercise often feels more rewarding than solitary activity,” Dr Singh said.
“These community programs have shown benefits for patients including improved mental health, reduced pain and blood pressure, and increased wellbeing.”

She says a simple approach is for GPs to enhance communication so they can tailor recommendations to individual interests. For example, dance, or walking on the beach, as this increases engagement.
It is also helpful for practices to maintain a list of local free or lowcost activities which enables quick referrals during consultations, such as those on offer via local councils.
“You can provide written, printed, or digital prescriptions – including specific activity information – which boosts uptake more than verbal advice alone,” Dr Singh adds.
“And schedule follow-up appointments, which establishes accountability and sustains engagement.”
There has also been a shift from sportfocused exercise to inclusive, varied movement and social engagement options.
At her practice, Dr Singh said patients have been very open to exercise prescription and very grateful when they’ve tried it: “Any movement counts, not just formal fitness or sport.”
However, this advice needs to be complemented with additional information.
“Take the time to explain that it’s not just competitive sport, it’s movement. We’re not going to be running marathons; even just five minutes of movement a day, and then add in the social connection, and you’re killing two birds with one stone,” she said.
GP and RACGP WA Chair Ramya Raman is equally as enthusiastic about fostering a deeper, wholeperson approach to the patient-GP relationship.
When it comes to prescribing exercise, Dr Raman said the GP
role is to highlight, guide and offer continuing support.
She also agreed there is growing awareness and normalisation of social prescribing among GPs.
“The perception of exercise has shifted from being mainly about appearance or weight loss to being valued for its holistic health benefits, including reducing cholesterol, blood pressure, and improving mental health,” says Dr Raman.
“GPs can highlight that wide range of benefits, not only physical fitness but also improved mood, sleep, and energy levels.”
Patients often cite lack of time, fatigue, or the cost of activities as barriers to exercise. GPs can address these by suggesting flexible options and free or low-cost community programs.
A good example is joining a local Parkrun – which isn’t necessarily running, but simply walking and talking with friends – and tailored mat Pilates where there are after work sessions.
“There’s support for starting slow and building up. Walking is often promoted as the most accessible and beneficial form of exercise,” Dr Raman added.
Medical oncologist Kynan Feeney, Head of Department Oncology, Haematology and Palliative Care at SJOG Hospital Murdoch, explained there had been a paradigm shift when it comes to exercise recommendation attitudes.
He said advice for many injuries and conditions is now pro-movement.
“If a patient has back pain, rest is no longer the recommended strategy, it’s exercise. If you have cancer, the worst thing to do is rest to regain your strength, now we say you should exercise to make you stronger,” he told Medical Forum
“So, we’ve moved to really appreciating the importance of being active, and the deleterious effect of inactivity in general.”
He said the benefits of exercise span the whole spectrum of the human experience, from mind and body, pre-conception and pregnancy, early childhood through to older age, for prevention and treatment of a multitude of conditions. continued on Page
THE QUICK AND EASY WAY FOR GPs TO DIAGNOSE HEART RHYTHM ISSUES

D E V I C E
F I T T I N G
R E P O R T S
C O S T S
G P S U P P O R T

O l d , b u l k y H o l t e r m o n i t o r s a r e d i f f i c u l t t o
u s e a n d u n c o m f o r t a b l e f o r p a t i e n t s t o w e a r
P a t i e n t i s r e f e r r e d o f f - s i t e , h a v i n g t o b o o k a n d
t r a v e l f o r f i t t i n g w h i c h c a u s e s d e l a y s i n t e s t i n g
T y p i c a l l y r e p o r t e d b y g e n e r a l c a r d i o l o g i s t s , o f t e n
l a c k c l i n i c a l d e t a i l a n d r e t u r n e d i n d a y s o r w e e k s
O f t e n r e q u i r e s p a t i e n t s t o p a y o u t o f p o c k e t
e x p e n s e s l e a d i n g t h e m t o s k i p t e s t i n g
O n l y r e p o r t s H o l t e r , n o f u r t h e r s u p p o r t i s p r o v i d e d t o r e f e r r i n g G P s t o a s s i s t i n p a t i e n t c a r e

S m a l l l i g h t c u t t i n g e d g e H o l t e r m o n i t o r Q u i c k
a n d e a s y t o u s e , c o m f o r t a b l e f o r p a t i e n t s t o w e a r
P a t i e n t s a r e c o n v e n i e n t l y f i t t e d a t y o u r p r a c t i c e , a v o i d i n g t r a v e l a n d d e l a y s
D e t a i l e d c l i n i c a l r e p o r t s p r e p a r e d b y o u r t e a m o f
c a r d i a c e l e c t r o p h y s i o l o g i s t s r e t u r n e d i n h o u r s
1 0 0 % b u l k b i l l e d t e s t i n g w i t h o u t a n y a d d i t i o n a l
c o s t s f o r p r a c t i c e o r p a t i e n t s
C o m p r e h e n s i v e s u p p o r t p r o t o c o l s t o h e l p G P s
c o n f i d e n t l y a n d e f f i c i e n t l y m a n a g e p a t i e n t c a r e
w w w . C l o u d H o l t e r . c o m . a u




continued from Page 11
“In cancer care, the evidence is now incontrovertible – exercise is a form of cancer prevention and treatment.
“In multiple studies there is a straight-line relationship between the amount of exercise a person does to their cancer reduction.”
This includes any form of exercise from aerobic, to muscle strengthening, but also incidental day-to-day low activity like walking, meaning low or no-cost movement is hugely beneficial for all stages and ages.
“In patients who have had surgery and chemotherapy after a colon cancer diagnosis, regular vigorous exercise reduces the risk of cancer recurrence and overall death as much as chemotherapy, which is a very humbling realisation as to how important an intervention exercise can be,” Dr Feeney added.
“In prostate cancer patients, regular exercise – including weight bearing muscle building types of exercise – improves survival, quality of life and mitigates many side effects of cancer therapies, particularly the adverse muscle and metabolic effects of androgen deprivation therapy.”
While Dr Feeney highlights that GPs have a huge influence on their patients when it comes to lifestyle changes, doctors are time-poor with training geared more towards medical or surgical interventions, rather than motivational or structural interventions.
“We have to engage our colleagues in related disciplines, whether that be physiotherapists, exercise physiologists or personal trainers,” he said.
“Each patient’s needs might differ and the doctor should be able to identify the most appropriate next steps for them.”
Dr Feeney said exercise should be prescribed to “almost everyone” unless they have an eating disorder or a specific diagnosis in which an exercise program may be counterproductive.
With the facts crystal clear when

Rachel Hutchinson trained as a Pilates instructor after being prescribed sessions to help recover from her hip replacement.
it comes to exercise and health benefits, there is also a push to integrate social prescribing and movement guidance into medical and allied health training.
“Some associations and patient advocacy groups are working to include related curricula at universities. There are initial discussions with James Cook University, Bond University, and the observing of existing UK models,” Dr Singh said.
She strongly supports a move to official social prescribing-related education.
“We absolutely need to start at the grassroots levels, and we have been in touch with the Australian Medical Association trying to get it implemented into various universities. In the UK, it’s already commonplace,” she said.
“It needs to start in medical school, but also anyone in the allied health field.”
Dr Singh adds that GPs should sdvocate for the addition of social isolation and loneliness screening to GP checklists and chronic disease management plans, and support further education and integration of social prescribing concepts in medical and allied health training programs.
“Please bring social prescription into your tool box, and remember social isolation and lack of physical activity is now one of the leading risk factors for most of our chronic diseases.”
Dr Raman reminds GPs to consider what will work best for the patient and remember that pushing patients into intimidating settings, such as large gyms, may not be the best solution.
Instead, opt for non-threatening, supportive environments, such as encouraging habit-building by setting 28-day challenges to foster routine.
“The focus is on enjoyment rather than punishment – choosing activities patients will look forward to encourages sustainability,” she said.
For Rachel, being advised to start Pilates not only helped her recover better before and after surgery, but she loved it so much she has now trained to become a Pilates instructor.
“Pilates was a real gamechanger and having seen how much it had helped me, it inspired me to study and become an instructor to help others in similar positions. I am now preparing for hip number two to be replaced.”
Down syndrome was first identified more than six decades ago, but gaps in care continue to persist. Now, new Perth research has paved the way for developing a gold standard model of care.

By Aleisha Orr
In medical terms Down syndrome (DS) is not new, the underlying chromosomal cause was identified more than 65 years ago and there has been an understanding of it since it was first formally described in the 1860s.
However, for a WA study into the most common chromosomal abnormality in humans, researchers decided to take a step back.
With input from clinicians, it sought to identify patient and carer priorities for research and clinical care of children with DS in Australia.
Interestingly, the top priority identified also calls for what might be considered a further step back in order to reconsider the bigger picture when it comes to caring for those with the disability.
Individuals with DS and their carers ranked developing a gold standard model of care, including screening health checks, as the most important consideration in terms of future research.
Such a framework does not currently exist, but this project is giving those involved an opportunity to consider what it could look like.
Anaesthetist Professor Britta Regli-von Ungern-Sternberg was the lead author of the research, which was published in the Archives of Childhood Disease
She said while doctors could consider treatments and come up with a plan for a patient, which in theory may be sound, “the acceptability of any treatments or investigations to parents is critical”.

Prof Regli-von Ungern-Sternberg often sees patients with DS who require surgeries due to associated conditions. In paediatrics, the field she works in, parents also have to be on board.
“For optimal outcomes, we need our care to be acceptable, not just to the doctors and the other clinicians but to the parents, the carers and the children, it will work best when all the stakeholders agree it is really worthwhile,” she said.
In addition to UWA and Perth Children’s Hospital where Prof Regli-von Ungern-Sternberg is the Chair of Paediatric Anaesthesia and Director of the Institute for Paediatric Perioperative Excellence, the collaborative study involved The Kids Research Institute Australia and advocacy group Down Syndrome WA (DSWA).
When DSWA Chief Executive Cassie Hughes was asked what a gold standard health care model would be for those with DS, she said it was the remainder of the priorities being done well, in addition to improved continuity of care and understanding of DS among health professionals.

While the condition, which occurs as a result of having an extra copy of chromosome 21 in each cell, is a developmental and intellectual disability that is also known by some characteristic physical features, individuals with the syndrome are at higher risk of other health problems.
Paediatrician Dr Ellen Taylor is the co-director of the medical division at PCH. Her interest in the condition led her to set up a clinic for children with complex medical issues associated with DS at the hospital.
While the clinic is focused on early interventions, it is only accessible to those considered medically complex and Dr Taylor said it can only take those most at risk.
“About 50% will have a cardiac issue, they're at higher risk of autoimmune disease, so many of them will develop celiac disease or thyroid disease or diabetes,” Dr Taylor said.

“Many of them get skin conditions like vitiligo or alopecia, many have respiratory disease, and that can be from a number of different multi-factorial reasons.
“They can also have cardiac disease, which can make any respiratory disease more complex, and they can also have just inherent lung disease, like infections that linger.”
In addition, she said those with DS tend to have large tongues, big tonsils and what might she described as ‘floppy airways’, which often led to snoring and sleep issues.
It is envisioned that a gold standard model of care would include targeted routine screenings.
In other countries there is a set schedule of screenings that are meant to take place at different ages.
Prof Regli-von Ungern-Sternberg said in some places outside of Australia the checks were done automatically, meaning patients don't have to be on a list, they are called to have checks at a certain age.
She said these include tests for hearing, neck instability, obstructive sleep apnoea, respiratory function and relevant immune diseases that they are at a higher risk of.
“Depending on their results it will be determined when their next check up will be.
“We don’t at the moment have, for our children with Down syndrome, such a clearly structured pathway,” Prof Regli-von UngernSternberg said.
She said some of these checkups could be done by GPs, while some would need to be done by specialists, but the important thing would be that there needs to be “good information flow between the primary care physician, specialists
continued on Page 16
continued from Page 15
and families so that everyone is always on the same page”.
Taking more of a preventative approach rather than a reactive one would allow health practitioners and patients to be one step ahead, she added, meaning treatment and early intervention could take place instead of waiting for major symptoms to arise.
Ms Hughes said sleep issues, which were discussed widely during inperson meetings with parents as part of the study, were one of the problems that early intervention could be especially useful for.
Nikki Schwagermann, a mother and carer of a young person with DS who runs the family support team within DSWA, told Medical Forum that sleep issues sometimes first arose
as what appeared to be behavioural problems, so ruling them in or out early on could be useful.
“Sometimes we look at trying to treat a behavioural concern, or a developmental delay, and in fact, it could be related to sleep,” she said.
A framework to work from Dr Aine Sommerfield, Clinical Research Manager in the anaesthesia and pain management research team at PCH, said input from those with lived experience of navigating the health system alongside those with DS had shown the current approach was ad hoc and depended on how informed an individual’s doctor was.

getting the best care they can get,” she said.
“A better system would provide a plan or a model of care to be followed.”
Ms Schwagermann said continuity of care was an issue that parents often raised with DSWA.

“There needs to be a coordinated referral pathway and feedback pathway, where the GP becomes the hub of that information,” she said.
“These kids might go to a speech pathologist, or they'll go to a paediatrician or a podiatrist, but it doesn't all come back to one central location and that's really challenging for our families.”
Ms Hughes said GPs have an important role to play in the health of those with DS.

“You really want to have a system where all the children are
Developing a gold standard model of care for those with DS, including screening health checks, was identified by research informed by 215 patients and carers, as well as 191 clinicians.
To identify a list of the top 10 priorities patients and carers have for clinical care and research for children with the genetic condition, surveys were created for clinicians, patients and carers to provide up to three suggestions of topics.
Once each of these was collated, the researchers classified the suggestions into broad themes, removed out-of-scope ideas and combined similar ideas.
In the early stages there were 565 ideas raised.
From there further surveys were conducted, one for patients and carers and one for clinicians, who were asked to select the 10 most important research ideas overall.
The results were compiled in a list for each for the two groups, ranking the most highlighted priority areas.
Nine parents of children with DS took part in a consensus meeting with four researchers to consider the ranked research ideas and come up with a final top 10.
These were:
“For many of our members, there's
1. Developing a gold standard model of care or best practice care, including screening health checks and spanning primary and secondary care
2. Sleep quality including obstructive sleep apnoea, snoring, breathing problems and circadian rhythm
3. Investigating acute care problems including acute infections such as sepsis
4. Improving respiratory health and management of chronic lung disease, rhinitis and sinusitis
5. Perioperative risk stratification and optimisation including safer anaesthesia, preoperative fasting and opioid sensitivity
6. Diagnosis and treatment of autoimmune diseases, immune response including response to vaccines
7. Diagnosis, management and treatment of ADHD/ ASD plus mental health issues for children with DS or Trisomy 21
8. Pain assessment tools and the management of pain and anxiety
9. Neck issues, including atlantoaxial instability development and screening
10. Coping and resilience tools for medical interactions.
actually no need to be going and seeing paediatricians and lots of specialists, but GPs don't have enough knowledge or experience a lot of the time, so then our families don't feel confident with them,” she said.
“A GP, and this is no fault of their own, sees thousands of patients, is schooled in hundreds of different conditions, and we can’t realistically expect them to have previously seen a child or person with DS.
“We get phone calls or emails at least once or twice a week from someone in the community saying, ‘Can you recommend a really good GP that works well with people with DS and knows about DS?’.
“Ideally, it would be amazing if across Perth's metro area there were 10 GP services that were very focused on people with DS, they'd have a captive audience.”
At the same time, Ms Schwagermann said behaviours, development delays or symptoms were often put down to an individual’s DS without giving enough consideration as to whether that was actually the case.
She hopes some sort of framework

that included a description of what DS is and is not would reduce this diagnostic overshadowing.
Dr Sommerfield said those involved in the research would be working on how to move forward in creating a gold standard model of care. She said there was still findings GPs could take from this research.
“Something GPs may want to look at would be around considering
sleep issues in patients with DS and not waiting for parents to raise problems.”
She said taking on that knowledge was important because sleep quality affects so much around development, language skills and schooling.
ED: DSWA asks anyone within the medical profession with an interest in providing care for people with DS to reach out to them.
PBCI is a comprehensive Breast Cancer Centre, located at Hollywood Consulting Centre, Nedlands. The team of specialists of specialist breast surgeons, medical oncologists, experienced breast physicians and a genetic counsellor, provide streamlined and evidenced-based care for women and men diagnosed with early or advanced breast cancer.
Patients have access to same-day consultation with an experienced Breast Physician, breast imaging, and diagnostic biopsy, with ongoing surveillance available for those at familial high risk
Our model of care includes the support of specialised Breast Care Nurses and clinical psychologists, ensuring comprehensive care throughout their breast cancer journey.

Through clinical trials, we provide patients with the benefit of access to international drug treatment trials and patient-focused research. Our research informs and underpins the treatment we provide to our patients.

The word challenge can’t be used enough in Dr Leigh Sheppard’s life, but it also sits alongside the words success and kick-ass.
By Ara Jansen
Dr Leigh Sheppard had already made it through high school and medical school before she was diagnosed with OCD and several other neurodevelopmental disorders.
That meant she had already established solid ways to live, cope and move through her life, with other people not really noticing she was different.
Like many things in her life which have not been easy, going to medical school was the response to a challenge posed by a loved one. She’s smart, driven, twice exceptional (gifted and neurodivergent) and not one to back down from someone questioning her ability to succeed.
In high school Leigh didn’t know what she wanted to do but she did know she wanted to be good at it and wanted to be helpful. She didn’t know what that looked like, so she did a broad undergraduate degree in science.
That challenge over whether she could do it? She graduated from medicine at Notre Dame in 2015.
“I remember at the end of medical school feeling a relief that I had finished and that I was always going to have that as a back-up qualification to secure my future. A lot of my OCD is around security, safety and abandonment,” she said.
“When I started work, I discovered I really enjoyed critical care medicine, specifically emergency medicine. I also struggled because of the increasing impact of my then undiagnosed conditions making it more and more difficult to work in that environment. It was a very difficult thing to negotiate because something I loved doing wasn’t necessarily the best for me in the long run.
“I remember being terrified at my first emergency rotation, but it was an amazing team and I loved it. When I started to have more difficulties in terms of my mental health, I kept making adjustments to see if it was possible.
“Then I considered working less hours or changing to a different job. But I realised this type of medicine wasn’t going to be possible for me. It was before my diagnosis, and I was doing everything possible to help myself.”
Leigh realised she needed to protect her health. She was especially cognisant of this because one of her friends, who had similar struggles, made different decisions and didn’t make it out of medicine alive. Part of Leigh’s syndromerelated trauma is due to several suicides in her life.

She chose to take a career break in 2023 because her symptoms had become too debilitating. For a period of time, she became almost bedbound. She says it felt like an extreme version of the game where the floor is lava but, for her, touching anything sent her catastrophising.
Because she managed her symptoms on her own for such a long time, it was hard to ask for help, but also people didn’t necessarily see her as needing any.
“That is very distressing. When I am asking for help, I have run out of ways to help myself. With therapy, I’m also getting better at advocating for my needs.”
Married to an award-winning marine scientist, Leigh and James have been together for 15 years.
Leigh realised she needed to protect her health. She was especially cognisant of this because one of her friends, who had similar struggles, made different decisions and didn’t make it out of medicine alive.
Leigh shares her husband’s love for all things marine, so they spend a lot of time near and in the water, whether it’s locally or overseas. They also like to hike.
James is Leigh’s biggest champion and the sun to her sometimescloudy day. Never far behind are the pair’s two German shepherds, Indi and Toby. They don’t have children, but Leigh’s niece and nephew receive very good gifts.
“My husband is so happy, and he has remained like that over a long period of time. I’m a bit negative and grumpy at baseline and his baseline is positive. He’s been instrumental in my adult life. Without him I don’t think I would have been where I am now. He’s an amazing human.
“We were lucky to have met each other. I remember looking at him and thinking ‘what a unicorn, how amazing’. It’s so good to know someone has your back.”
Leigh is a lover of Pilates and goes to classes three times a week. And she regularly weeds the lawn for a neighbour while getting her podcast fix.
It wasn’t until 2022 that Leigh was officially diagnosed with OCD, continued on

Ask: Establishment of a Carer Card in WA
What a WA Carer Card would mean for carers:



Recognition
Financial relief
Identification



Promote wellbeing
Align with other states

Community awareness
“You are one, know one or will be one.”
Scan to sign the petition or email your local MP.


continued from Page 19
ADHD, autism and associated trauma. Up to that point she had been very proactive in trying to discover what was going on.
She’d already had decades of managing herself, her life and how she moved through the world and related to others.
“I think I made it work for the people around me a lot more than it worked for me. It has definitely been a process of unravelling everything.
“The reason my diagnosis was so delayed was because the majority of my compulsions were internal. An example at university meant that if I wrote something and wasn’t sure I understood it, that meant re-reading the whole section again, not just that one part. I wasn’t slow but I spent a lot more time doing things.
“I never missed deadlines, but in order to make these, I had to put in way more hours. I worked through an incredible volume, it’s quite extraordinary. I’m working really hard to pare that back. I recognise that my normal is not someone else’s normal. I’m trying to rewire so I have more fun time and more down time. I’m much better at that now.”

Being diagnosed was a very difficult time, with so many issues and trauma being interconnected in Leigh’s head.
“There’s a really strong connection with trauma and the development of OCD. At the time of my diagnosis, I was navigating something traumatic – I was assaulted at work and felt unsupported in managing it.
“A few weeks after that I started compulsively washing my hands and couldn’t stop. I didn’t know when I was going to stop or how I was going to stop. And I felt the urge to not stop. It was so frustrating and scary. That was the first observable thing, because of how I had to mask so much to fit in.
“I’d been seeing a psych for years and that’s when it clicked. They thought all the things that were bothering me were generalised

anxiety. I don’t think I can explain how challenging it all is because it feels like my normal. It’s like doing a physical and intellectual challenge at the same time.”
When Leigh first received her diagnosis, she was devastated. People around her questioned whether she was fit be a doctor with OCD.
Could someone going through the recovery process and still be experiencing intense symptoms help someone else through their process?
“I took that as a challenge. People said it was a waste when I left emergency medicine. Why can’t I be an advocate for other people with OCD while struggling with symptoms? Yes, my drive to get through that was a tiny little bit rage fuelled.”
Currently Leigh has found a sweet working spot as a locum doctor for a private contracting company. She can make her own hours, gets to work in various situations and the diversity suits her.
With six months left of her GP fellowship training, she has put it on hold as a way to lighten the load for a little while, doing what’s best and honouring her values.
From occupational medicine to health checks, Leigh is really enjoying this way of working and says she might never have
found this if her OCD and her own advocacy hadn’t led her here.
“Trips away for work are good therapy – going to an airport is OCD city with all the things you have to touch. Every night I’m not in my own bed I’m a little bit uncomfortable because of my OCD but I know that discomfort is good for me. OCD is very nuanced.”
Wanting to help make the road a little less rough and isolating for others, in 2023 Leigh founded a not-for-profit. OCD WA’s mission is to build a supportive community and create psychologically safe and inclusive spaces to enhance the health and wellbeing of those with OCD and related disorders. An important part of the group is peer support, social events and advocacy alongside sharing resources, education and training.
The group is celebrating several October events with OCD Awareness Week from October 12-18, the Perth OCD Walk in Kings Park (October 19) and their annual fundraising exhibition Creative Connections from October 21 to November 2 at Terrace Greenhouse in South Fremantle.

The COVID pandemic saw in a number of restrictions to protect the health of West Australians, but has that created an ‘immunity gap’ among children?
By Aleisha Orr
In 2020 as the world was in the grips of the COVID pandemic, the state government at the time made the decision to lockdown WA’s borders to keep the virus out and protect the public’s health.
While it meant that WA fared far better that other states and countries, a Perth paediatrician has suggested the measures have led to an immunity gap responsible for a rise in young children being hospitalised with respiratory viruses.
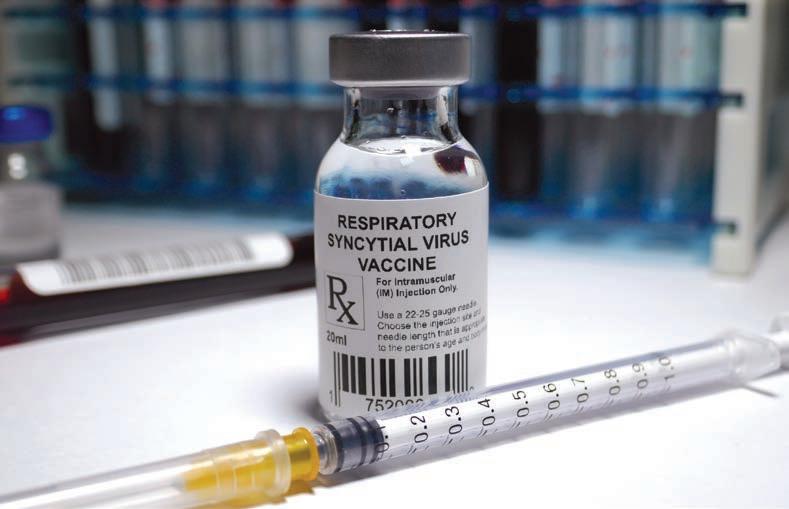
Professor Peter Richmond , head of paediatrics at the UWA School of Medicine and Head of the Vaccine Trials Group at The Kids Research Institute, told Medical Forum measures such as social distancing had inadvertently created a vacuum of immunity in young children.
Professor Richmond, who is also a consultant paediatric immunologist and head of the Department of Immunology at Perth Children’s Hospital (PCH), said nonpharmacological interventions such as border closures, mask-wearing, and social distancing drastically reduced the circulation of common respiratory viruses such as influenza and respiratory syncytial virus (RSV) in WA.
While this was beneficial at the time, it meant that a generation of young children, specifically those born during and just before the pandemic, did not get the typical exposure to these pathogens that other children got.

“Particularly preschool children, those in daycares or attending kindergarten, who are usually getting exposed to a lot of other children and generally getting exposed to viruses fairly frequently,” he said.
“When you're exposed to viruses, we mount an immune response to that particular strain of the virus, but also we generate a degree of cross-protective immunity to multiple strains of that particular virus.
“You're actually slightly less likely to pick up another virus immediately after you've just had one virus.”
The pandemic essentially put a pause on this natural process, leaving some children with a less-prepared immune system.
In the years following the height of the pandemic, as restrictions eased and viruses began to circulate again, there was a rebound in cases.
“There was definitely a reduction in the number of preschool children with viral-induced wheezing illnesses,” Professor Richmond said. "Things like RSV and influenza, for instance, really just disappeared for a period of time and then recurred.
"When those viruses start circulating again, you don't have a
A total of 1808 cases of RSV were detected in WA across the entire population in 2019. In 2020 the state recorded just one case. WA experienced one of its worst flu seasons on record in 2019 with 23,210 cases recorded, but that dropped to 1200 in 2020 and 36 in 2021.
In 2021, with the state border closed for the entire year and social distancing rules in place, 486 cases of RSV were recorded and 36 cases of influenza.
In 2022, when pandemic restrictions began to ease, WA recorded 11,629 cases of RSV, followed by 10,488 in 2023 and 9,246 in 2024.
The number of flu cases in 2022 also shot up to 14,004 in 2022, then 21,032 in 2023 and 17,022 in 2024.
So far this year WA has recorded more cases of RSV than it did last year, and more than 27,000 cases of influenza – an increase of more than 10,000 on 2024’s tally.
lot of protective immunity against that particular virus.”
Viral-induced wheezing
Professor Richmond said admission rates for respiratory viruses at Perth Children’s Hospital decreased during the height of the pandemic before spiking at more than 2000 in 2023.
“We did have a period of rebound where there were more cases of those viral infections occurring, causing children to end up in the emergency department or in hospital,” he said.
“But what I think was interesting is that this had an overall impact on viral-induced wheezing.”
Viral-induced wheezing is a common condition in young children, often triggered by respiratory viruses.
In Australia such wheezing is generally referred to as bronchiolitis in those under 12 months of age and is considered viral-induced wheezing for those from one to five years. It is then referred to as asthma beyond that age.
"The main difference is that young children don't respond to ventilation, so it's a useful clinical cut off to say at over 12 months old you can try some Ventolin to see if it helps,” Professor Richmond said.
“The physiology is also slightly different in that it's affecting a slightly different part of the lungs.
continued on Page 25

*Based on data from the WA notifiable infectious disease dashboard as of September 25 2025
An advocate for men’s health, Dr Tom Shannon likes to set a good example for his patients and encourage self-care for the prevention of illness.
Urologist and prostate cancer surgeon Dr Tom Shannon aims to be in his patient’s lives for the shortest time possible.
“I love the fact that I can be important to a patient for a very short period of time. The goal is not to need me and to get on with their lives, free of cancer, which is such a privilege to be part of. Our team makes a difference,” he says.
Tom has been a urologist for more than 25 years, specialising in prostate cancer diagnosis and treatment. He still loves his profession as much today, if not more than when he started.
From a young age Tom knew he wanted to be a doctor, even though it wasn’t something that was in his family. Fascinated with the human body, he was drawn to books about how the body worked.
Tom was also very clear he was going to be a physician during medical school, but exposure to some great surgical bosses in early years changed his view. As a young intern at Hollywood Hospital he had his own theatre list, developing a love for surgery.
“Hollywood was a great place to be a junior doctor. I had a great boss who gave true one-on-one mentoring. I learnt so much. When I finished my internship, I just started studying for surgery. I was really interested in cardiothoracics but after a year realised it wasn’t for

A/Prof Shannon is a graduate of the University of WA. He completed his Fellowship in Urology in 1999 and completed post-fellowship training in the UK and the US focusing on minimally invasive surgery and prostate brachytherapy. He was a pioneer of minimally invasive urological surgery in WA and is a leader in the development of prostate MRI. He is a strong advocate for men’s health and has been a board member of the Prostate Cancer Foundation of Australia (WA) for over 10 years.
me. I was sent to do urology for a rotation and remember complaining loudly. I was given great advice –the only way to know if I liked it was to approach it like I would be doing that job every day for the rest of my career.
Among other accomplishments, in 2004 Tom operated in WA with the pioneering French surgeon Professor Claude Abbou for the first demonstration of a laparoscopic radical prostatectomy. To date, the urologist has cared for more than 10,000 men and performed more than 3,000 open, laparoscopic and robotic surgeries.
A big advocate of self-care and the prevention of illness, Tom actively advocates for men’s health and prostate cancer. He has been involved with the Prostate Cancer Foundation of Australia since inception and holds an adjunct associate professor role with Edith Cowan University in exercise medicine.
With around 26,400 cases diagnosed in 2024, prostate cancer is estimated to account for 28% of the cancers to be diagnosed in
males for the year. Because prostate cancer survival rates are high, Tom says it’s a rewarding field to be working in.
He says there’s still work to do to bring equality to early detection. There’s excellent data showing the benefits of Prostate-Specific Antigen (PSA) testing and new Australian guidelines advocate men start testing at 40 and at regular intervals after, depending on personal risk. Tom argues that we could achieve significant gains with simple, but uniform changes.
“The goal is to find significant cancers early and cure them. Cures are achieved by complete surgical resection, which is a challenge, because you get one chance to do it really well. There are minimal margins for the cancer. To cure and retain continence and sexual function, you must be precise. The trifecta is the goal. Cure avoids needing testosterone suppression, which can be devastating.”
continued from Page 23
Bronchiolitis in young children is a much more severe viral infection of the lower airways, whereas viral wheezing is more in the middle and upper airways of their lungs,” he said.
While Dr Richmond said hospitalisation rates for children with respiratory viruses in 2024 had been similar to pre-pandemic levels, he warned that avoiding serious viral illnesses and the associated wheezing was still of importance.
While many children outgrow it, a severe early-life infection with a virus like RSV can increase the likelihood of developing recurrent wheezing episodes later on.
Vaccines key
Dr Richmond said immunisations were a tool to fill in the immunity gap as they offer “almost similar level of immunity depending on the match of that vaccine and the strain that's circulating”.
But immunisation rates against influenza in children under five are about half of what they were prepandemic and rates of vaccine hesitancy across WA were rising.
"In 2018, 2019, 2020, we had pretty reasonable coverage, sort of 40%, but that decreased in recent years to more like 20%,” Professor Richmond said.
Latest immunisation data show that between March and September 2025 42,370 children under five were vaccinated against the flu – a rate of approximately 26%.
Whooping cough has also seen a resurgence of more cases than expected. While cases of whooping cough are cyclic in nature, Professor Richmond said, the current spike in cases is larger than expected, again due to the immunity gap.
WA has recorded more whooping cough cases in the first nine months of this year than in the entirety of 2024. In 2024 some 1314 cases were recorded, compared to less than 100 in 2021, 2022 and 2023 while pandemic restrictions were still being eased.
More RSV cases have also been recorded this year compared to last with a total of 10,901 recorded by
September, compared to 9246 in all of 2024.
The National Immunisation Handbook recommends RSV vaccination for pregnant women, all people over 75 years of age, and anyone over 60 who is Aboriginal or Torres Strait Islander or who has medical risk factors for severe RSV disease.
WA has been seen as a trailblazer in RSV vaccinations, becoming the first state to offer free RSV vaccinations to infants in 2024 and continuing the program in 2025. Government figures suggest around 22,000 babies were protected during the 2024 RSV season resulting in a 57% reduction in hospitalisations.
Professor Richmond said there were positive signs in regard to uptake of new RSV immunisations, such as maternal vaccination and infant immunisation, which he described as encouraging.
He said researchers were working on developing next-generation vaccines that could offer protection against a combination of viruses, including RSV, influenza, and human metapneumovirus to provide more comprehensive protection. However, these were still a while away.
While WA was now in a period that is normalising to a pre-pandemic viral landscape, Professor Richmond said for a generation of children their immune systems were still playing catch-up. He urged GPs to remind
parents of the importance of getting their young children immunised.
Beyond vaccination, public health measures and parental vigilance remain key and GPs have a role to play in educating parents.
“It's really important for parents to be aware of both the things that they can do to prevent their children getting unwell with respiratory viruses, and part of that is not going to daycare when your child is sick.”
He said it was also important that parents were properly informed about how to deal with wheezing.
“We do find that children who have not been treated properly end up with a more severe admission with wheezing when they could have been treated with a preventer inhaler.
"It’s important that we educate parents about how to use bronchodilators such as Ventolin, using a spacer and having an action plan so they know when and how many puffs to give according to the child's age, which for kids under six, is usually six puffs.
“When they need to come and see the GP, and they may need additional treatments, such as steroids or having frequent symptoms, they might need a preventer.”
Expanded pharmacy prescribing powers will enhance primary care and collaboration with GPs, writes pharmacist Natalie Willis.
Western Australian community pharmacists will be able to diagnose, treat and prescribe appropriate Schedule 4 medicines for a broad range of conditions through the State Government’s Enhanced Access Community Pharmacy Pilot (EACPP).
An initial cohort of pharmacists commenced training in September, with the expectation that they will be delivering EACPP services towards the end of 2026.
The pilot is not without precedence. In countries with comparable economies and health systems such as Canada, the United Kingdom and New Zealand, pharmacists are already authorised to prescribe and dispense for conditions included in the pilot.
High levels of patient access, safety and satisfaction are a feature of these.
These same patient benefits are recorded across those Australian jurisdictions who have already authorised expanded pharmacist scope of practice services.
Queensland pharmacists treated 10,270 women through a statewide Urinary Tract Infection Pharmacy Pilot between June 2020 and September 2022. Patients reported being very satisfied (92.6%) with the service.
Similarly, a review of the initial 12 months of the Victorian Community Pharmacist Statewide Pilot recorded a patient satisfaction rating of 97%.
In each instance participating pharmacists were found to follow the treatment protocols and, where required, referred appropriately.
Broader health system benefits have also been recorded. South Australia recorded a 21% drop in related presentations to their metropolitan hospitals following the introduction


of their community pharmacy Urinary Tract Infection Program, when compared to the same MarchJuly period of the previous year.
So, rather than compromising patient safety and wellbeing, pharmacy scope of practice pilots continue to demonstrate that trained and authorised pharmacists provide safe and effective treatment to patients and are increasing patients’ access to timely primary healthcare services.
delivery
Increasing patients’ access to primary health care services should be a shared goal. As should be utilising the primary healthcare workforce to its full extent.
There should be no wrong door when it comes to patients accessing timely primary care.
Simply put, the WA pilot, and other similar services across Australia, are not about replacing, removing or restricting access to GPs, rather they are complimenting the services which are available.
On average patients visit their pharmacy 18 times a year, so the pharmacist is well placed to build strong relationships and have an intimate knowledge of medical history.
Patient service delivery in the EACPP will be strictly aligned with the Australian Therapeutic Guidelines and established protocols.
These ensure national harmonisation of services as they are the basis for pharmacist scope of practice across Australia and have been reviewed by key stakeholders, including medical and
On average patients visit their
18 times a year, so the pharmacist is well placed to build strong relationships and have an intimate knowledge of medical history.
pharmacy peak bodies and patient representatives.
They feature clear criteria for patient inclusion and exclusion, and for referral pathways to a GP or emergency care facility.
Pharmacist training, to a nationally consistent curriculum, is accredited by the Australian Pharmacy Council in accordance with the Accreditation Standards for Pharmacist Prescriber education programs, at an Australian Qualifications Framework level 8 (Graduate Certificate), comprising prescribing and clinical practice elements that build on a pharmacist’s core competencies.
assurance
To ensure that confidential conversations and clinical

examinations can be conducted appropriately, prescribing services under the pilot will occur in a WA Department of Health endorsed consultation room that will be audited within the Quality Care Pharmacy Program.
Pharmacists participating in the pilot will be required to document each consultation and to communicate this with the patient’s regular GP or medical centre, where the patient provides their consent.
In due course these consultations will form part of the patient’s My Health Record for access by all members of the patient’s healthcare team.

It is my firm belief that better utilisation of the expertise of the pharmacy sector to perform
certain treatments under designed protocols and guidelines, linked to clinical recording requirements and, when required, referral pathways, will introduce a huge capacity into the primary health care system.
There are currently over 130 prescribing pharmacists in Queensland and, overwhelmingly, they have assured me that their experience has involved good collaboration, communication and engagement with local GPs and medical centres.
This communication has built a level of confidence where GPs have started referring patients to prescribing pharmacists to treat acute conditions.
ED: Natalie Willis is the Vice President and National Councillor of the Pharmacy Guild of Australia’s WA branch.
(08) 9382 2388 conceptfertility.com.au marketing@conceptfertility.com.au







Two years ago, I had to make an impossible choice: delay an essential surgery that would protect my long-term health or proceed and risk not having anyone to care for my children during my recovery.
The surgery was a hysterectomy. Despite how routine the procedure might be on paper, the reality for me was far from standard.
I’m the primary caregiver and mother of two young children. My eldest lives with a complex disability and requires daily, handson support. The surgery would leave me physically incapacitated and unable to fulfil my role as a parent and carer for up to 12 weeks.
As the person who holds together all routines, therapies, and emotional scaffolding in our home, I had to plan for my absence the way a CEO might prepare to exit their company.
And I did. I built schedules, I coordinated an NDIS support worker, I arranged informal care from family, I put everything in place.
But, as often happens in life and the public health system, my surgery was bumped, pushed to a period that overlapped with school holidays and clashed with my family’s availability. The care plan I’d carefully built collapsed in a matter of days.
Monique Power was put in an impossible position when her potentially life-saving surgery was postponed. This is what she wants the health system to understand.
I called the hospital and explained the situation. What I needed was not complex, just someone to step into my shoes as a parent and carer to get the kids to school, prepare meals, manage routines, administer medications and be available to support my children with the dayto-day.
But the response I received, from a series of services, made one thing clear: the system was never designed with people like me in mind.
The hospital told me I could access their Hospital in the Home program; a post-op recovery service that sends support to patients recovering at home. But it was focused solely on me, not the family I care for, not the complex, daily realities of parenting a child with disability. I was passed on to external services such as in-home care providers, disability support organisations, third-party agencies. Everyone was kind, but none were equipped.
The responses were variations on a recurring theme: “We support the carer... not the caring role.”
Eventually, I tried Wanslea, my local NDIS Early Childhood partner, who I know offered an in-home childcare
service. It sounded promising at first, until I learned their processing time was five weeks minimum.
They weren’t sure they had any staff adequately trained to meet the complex needs of my daughter. They could only provide support for my eldest child, not both children, and there was no guarantee they’d be able to staff it at all.
When I pressed for options, their final offer came cold and matter of fact: “You can relinquish your children into foster care while you recover.”
I broke. I remember asking, because I couldn’t quite believe what I’d just heard: “You’re telling me my only option is to put my kids into foster care?”
There are moments as a carer when even your own body becomes an afterthought. We schedule our health around others and we ignore symptoms until they become nonnegotiable.
When the time comes to prioritise our own medical needs, the system often doesn’t allow us to, not without risking everything.
After pursuing all the known avenues of support, I had three options:
1. Postpone a medically essential, potentially life-saving surgery to remove high grade near-cancer cells from my body
2. Go through with it and send my children into foster care
3. Have the surgery and risk bleeding out trying to parent through my recovery.
The only reason those weren’t my only options was because of Carers WA which provided emergency funding to cover the cost of a livein support worker.
The NDIS wouldn’t fund the full coverage required, the hospital couldn’t.
This isn’t just my story, it’s the story of every carer who’s had to undergo surgery, or chemotherapy, or a hospital stay while raising a child with high support needs.
These are people whose work isn’t visible, who aren’t recognised as workers, but whose absence causes entire support ecosystems to collapse. A carer's role doesn’t stop for recovery, there is no such thing as time off.

Australia’s systems are siloed. Healthcare supports the patient, disability services support the individual with the diagnosis, carer organisations support emotional load, but no system supports the caregiving function itself.
It’s time to stop treating this gap like a glitch, it’s a policy failure and it’s costing families their health, their safety, and their stability.
This National Carers Week (October 12-18) we need more than

gratitude, we need integration. We need emergency coverage for carers undergoing major medical procedures, we need funding systems that recognise that a carer’s temporary absence is not a break, it’s a crisis in waiting.
Caring for others should never mean sacrificing your own right to be cared for.
At Perth Radiological Clinic your musculoskeletal investigations are reported locally by Perth’s largest team of musculoskeletal and spinal radiology experts.
• Our team specialise in providing expert imaging and pain injection services across the board, expediting treatment pathways with precise diagnostic insights.
• We offer MRI appointments in the evenings and on weekends for your patients’ convenience.
Stay tuned for the opening of our first regional branch PRC Bunbury – Open February 2026
Doctor Priority Line For urgent bookings and enquiries 9599 3929
Medicare Mental Health Centres offer free and confidential mental health support in communities across Perth for people aged 18 and over.
Walk-in support is available, or patients can book an appointment for counselling.
No Medicare card or referral needed.

Medicare Mental Health




Some 80% of us live in metropolitan Perth and, based on Medical Board numbers, the doctor-to-patient ratio is around one per 20. Of course, this ratio will be far higher in rural areas.
Recently a patient I had not seen at my practice before attended an appointment and asked about transferring her file across.
The practice she usually attended had one-by-one lost doctors to retirement or illness, to the point where only one remained. She had become worried about how long the practice would remain open.
This is not an unusual story – in fact, it is an increasingly common story in WA.
As of December 31 2024, the state’s population was over three million – an increase of 300,000 since the 2021 census. Some 80% of us live in metropolitan Perth and, based on Medical Board numbers of around 15,000 doctors, the doctor-to-patient ratio is around one per 20.
Of course, this ratio will be far higher in rural areas.
We also know that, just like the population in general, the medical workforce is ageing – the average age in some disciplines is in the mid to upper 50s.
The WA Health Workforce Strategy 2024 found 19% of specialists would be reaching retirement age in the next 10 years.
An effectively static medical workforce, coupled with a growing and ageing population, was always a recipe for the current situation and it affects all medical specialties.
We see this in wait times for private specialists, general practice and public hospitals. The saddest part is that this was all predictable – the demographic cliff in medical practice was predicted more than 20 years ago.
It’s a cliché that three into two won’t go. An increasing population and struggling medical workforce have produced the inevitable result, and the patient suffers.
This leads me to two questions: Will anyone in government take responsibility? Will anything be done to rectify it?

Complete your CPD with Medical Forum
Sign up to our Wednesday clinical newsletter to get the latest updates from your local specialists.
Scan the QR code to subscribe
By Dr Casey Whife, Sport & Exercise Physician
We’ve told patients to be active since dial-up internet. Australia’s adult guidelines landed in 1991, yet in 2022 only 22.4% met the recommended combined aerobic and strength targets.
In the same year just 18% of adults reported receiving a GP physical activity recommendation in the past year.
Somewhere between evidence and everyday practice, the message evaporates, and so do the years of healthy life.
If exercise were a drug, it would be PBS-listed with lifetime repeats. Cardiorespiratory fitness is among the most powerful, modifiable predictors of survival we have.
Studies show that moving from an ‘elite’ to ‘low’ fitness carried a fivefold higher risk of death.
Strength matters, too. Lower grip strength predicts higher all-cause, cardiovascular, respiratory and some cancer mortality.
Just 30-60 minutes per week of muscle-strengthening activity is associated with a 10-20% lower allcause and major non-communicable disease mortality. Recent publications suggest that power (strength at speed) may be at least as prognostic as strength.
No single pharmacologic class matches that breadth.
We’re past the “exercise is good for you” trope. Exercise prevents and treats disease.
In depression, prospective cohorts show protective effects even below guideline volumes. For treatment, a 2024 BMJ network meta-analysis of 218 trials found moderate symptom reductions comparable to psychotherapy and pharmacotherapy.
The effects were larger at higher intensities, and activities such as walking or jogging, yoga and strength training performed well. In those with impaired glucose


If exercise were a drug, it would be PBS-listed with lifetime repeats
tolerance, the Diabetes Prevention Program (DDP) multicomponent lifestyle arm – diet, more than 150 minutes of exercise per week, weight loss – cut diabetes incidence by 58% compared to 31% using metformin over three years.
In hypertensive adults, structured exercise lowers systolic BP by ~9mmHg, which performs similarly to a single first-line antihypertensive.
Then there is the CHALLENGE trial. After adjuvant chemotherapy for stage III/high-risk stage II colon cancer, the CHALLENGE trial’s structured exercise program improved survival relative to healtheducation with a five-year diseasefree survival of 80.3% vs 73.9% and an eight-year overall survival 90.3% vs 83.2%.
Across Australia’s nine National Health Priority Areas, an umbrella review found that exercise consistently had a positive effect
in either prevention or treatment, making it a uniquely broad and effective intervention alongside usual care.
For most asymptomatic, lowmoderate risk adults beginning lightmoderate intensity activity, routine ECG screening isn’t recommended. The message is: start now, progress sensibly.
Screening and cardiology input may be required in individuals with symptoms, a known disease, or vigorous/competitive plans.
However, for most people, brisk walking, light cycling, and basic strength training tend not to necessitate a stress test beforehand.
Make exercise vital
We record vital signs at every visit. We measure BP, lipids and HbA1c because they change risk profile and management.
Exercise and fitness are no different. Two simple steps to implement are:
Add the Physical Activity Vital Sign (PAVS): two simple questions that flag under-active patients and create accountability at follow-up:
1. Days per week of moderatevigorous exercise
2. Minutes per exercise session
PAVS = Q1 x Q2 = total minutes per week of physical activity
Track CRF annually: CRF independently predicts mortality and CVD events and should be included as a vital sign. Formal testing is available, but if not warranted, using validated nonexercise equations such as the NTNU Fitness Calculator can estimate VO2peak.
As for any script, the specifics matter. The FITT principle (Frequency, Intensity, Time, Type) is a valuable approach to progressing towards the World Health Organization exercise targets.
Tailor the starting dose; the deconditioned aren’t knocking 150 minutes out of the park on week one. Loop in exercise physiologists, physiotherapists and sport and

exercise physicians when needed.
Write a dose, not a pep-talk: “Let’s start with 10-minute walks after main meals and two short body weight strength sessions this week; we’ll add interval work next month.”
Then book the review. Make exercise the drug you’d never forget to renew, because its breadth, value and safety are hard to match.
If exercise were a drug, we’d put it in the water. Short of that, let’s make it a vital sign and a standing prescription in general practice. First, do no harm, second, prescribe exercise.
EOSedge is a precise, low dose imaging system that delivers full body images covering the full set of musculoskeletal and orthopaedic exams.
• Imaging complete in 20 seconds
• Full body images in standing position
• 24 hour repor t turnaround
• True 1:1 scale
Refer your patients now for lower dose imaging and bet ter visualisation for diagnostic or surgical planning and post operative assessment
• Low dose radiation
• Walk ins welcome
• All request forms accepted
• All scans are bulk billed

By Devesh Ramesh Sheth , Compounding Pharmacist
In the world of modern medicine where pharmaceutical giants churn out millions of identical pills, there's a quieter, more personal branch of pharmacy practice –sterile compounding.
It doesn’t make headlines but in hospitals, clinics, and specialised pharmacies across Australia, sterile compounding is saving lives, filling therapeutic gaps, and driving innovation.
Sterile compounding is the preparation of custom medications in a clean, controlled environment. Typically administered by injection, infusion, or into the eyes, they bypass the body’s natural defences, making sterility critical.
Compounded sterile preparations (CSPs) are made to meet the specific needs of a single patient. They might involve tailoring doses, removing allergens, combining multiple medications, or creating otherwise unavailable formulations.
Pharmacy compounding has existed since the earliest days of medicine, but sterile compounding in Australia didn’t gain attention until hospitals began preparing IV infusions and chemotherapy doses in-house during the mid-20th century.
By the 1990s, the risks of contamination and variability prompted increased scrutiny. The publication of sterile compounding guidelines in 2017 and their mandatory enforcement in 2018 marked a watershed moment.
Today it's a clinical science, performed under strict environmental controls with rigorous documentation and quality assurance.
Hospitals and ICUs: Compounded IV antibiotics, analgesics, and nutritional formulations (TPN) are staples in critical care units. Many hospital pharmacies compound medications daily to accommodate specific dosing, paediatric patients, or shortages.


Cancer care: Cytotoxic medications used in chemotherapy are often compounded to exact specifications for each patient. These high-risk preparations require advanced safety equipment and trained personnel.
Ophthalmology: Eye drops for conditions like severe infections or post-surgical care often require preservative-free or tailored concentrations, which compounding makes possible.
Paediatrics: Children require doses and formulations that aren't commercially available. Sterile compounding fills that gap by creating child-appropriate liquid injections or infusions.
Palliative care: End-of-life treatments often demand flexible dosing, alternative delivery routes, or combination therapies that sterile compounding can uniquely provide.
Biologic and personalised medicines: With the rise of personalised healthcare, there's growing interest in biologic compounding – tailoring treatments using hormones, peptides, and other complex molecules. Though regulatory hurdles are higher, the potential is vast for rare disease
treatment and regenerative therapies.
Advanced delivery systems: Compounded eye injections, longacting intrathecal infusions, and micro-dosed injectable implants are pushing sterile compounding into new territory, offering more precise drug delivery with fewer side effects.
Telehealth and remote access: Pharmacies can prepare and courier medications for patients in rural and regional areas, supported by remote clinician prescribing and digital consultation.
Automation and AI: New compounding robots, barcode verification systems, and AIpowered cleanroom monitoring are transforming how sterile products are prepared. These technologies improve accuracy, reduce contamination risk, and allow pharmacists to focus more on clinical roles.
Environmental and hazardous drug safety: With new containment systems like Closed System Transfer Devices and negative pressure isolators, pharmacies are better equipped to handle hazardous drugs like chemotherapy agents, improving worker safety.
Sterile compounding is providing precision therapies for patients when no off-the-shelf option exists
Critically ill infants, cancer patients, and remote rural communities and hospitals can benefit from what sterile compounding offers
Going forwards, sterile compounding will remain a vital partner in care.
With the precise and personal nature of compounding, the collaboration between the prescribing doctor and the compounding pharmacist is crucial.
Compounding sterile preparations is often a joint decision to meet a specific patient need. This teamwork adds an important layer to the narrative.
For example, for a paediatric patient requiring a medication dose far smaller than any commercially
available vial, sterile compounding allows preparation of a precise, safe dose.
From a doctor's perspective, risk and quality control are the most critical elements. There must be stringent testing that compounded sterile preparations undergo to ensure sterility, potency, and apyrogenicity.
The pharmacist is responsible for the entire process, including formula verification, calculations, ingredient traceability, and the final product release.
A pharmacist's world is full of specific processes and controls on this. ISO classifications, for example ISO Class 5 for critical areas, and the use of laminar airflow workstations provides important technical detail and highlights the rigor of the process.
Rigorous in-house and external reviews and quality assurance steps are required. This includes regular personnel competency testing, real-time status monitoring, end-product validation testing for sterility, apyrogenicity and potency, as well as regular environmental
monitoring to ensure the cleanroom is contamination-free.
Despite its importance, sterile compounding isn’t without challenges. High overhead costs for cleanrooms, extensive training, and compliance with evolving regulations make it a demanding field.
Recent controversies such as the unregulated compounding of weight loss injectables during national shortages have prompted regulators to draw clearer boundaries between pharmacy-level compounding and large-scale manufacturing.
The October 2024 ban on compounded GLP-1 agonists such as semaglutide was a strong reminder of the sector’s responsibility to prioritise patient safety and professional integrity.
Nevertheless, with clearer guidelines, smarter technology, and growing demand for personalised therapies, sterile compounding is poised for a transformative future.
Author competing interests - nil

Delivered in collaboration with Western Cardiology, our Acute Cardiac Service provides a direct referral pathway for privately insured patients presenting with acute cardiac conditions, including:
• Chest pain
• Cardiac arrhythmia (such as bradycardia)
• Presyncope/syncope
• Suspected heart failure
• Pacemaker/cardiac device issues
Eligible patients who meet admission criteria are admitted directly to our CCU.
By referring suitable patients to the service, you can ensure they receive efficient, comprehensive cardiac care in the comfort of a private environment.

By Dr Johan Mostert, Orthopaedic Surgeon, Subiaco
Frozen shoulder – adhesive capsulitis – is common in middle age, and more common in women than men.
The most common causes of nontraumatic shoulder pain in this age group are rotator cuff impingement and tears, including AC joint pain and biceps pathology; frozen shoulder; referred pain from the neck; shoulder joint arthritis; and brachial neuritis.
The key feature of frozen shoulder is the insidious onset of pain over weeks and months, often referred to as the ‘freezing’ phase. This is followed by a ‘frozen’ phase characterised by stiffness (loss of range of motion), lasting many months or even two-to-three-years.
There may be a ‘thawing’ phase in many patients where range slowly improves but often does not return to normal in the absence of treatment. Patients frequently find this condition deeply unpleasant as they cannot position the arm comfortably in the early phase.
Pain is described as a very deep ache in the shoulder. In the frozen phase, the loss of motion makes everyday activities very challenging.
Pathology and subtypes
There are several subtypes of frozen shoulder.
1. In most patients there is no obvious cause
2. There is a clear association with diabetes, especially type 1 diabetes, and in these patients the stiffness is often more severe and more likely to recur after surgery, but possibly resolves spontaneously given time
3. Calcific tendinopathy of the rotator cuff often presents as frozen shoulder
4. Frozen shoulder post immobilisation for fracture
5. Associated with cardiac events or even pacemaker insertion and post hemiplegic stroke
The key feature at arthroscopy is that the capsule is inflamed. A large percentage of the idiopathic

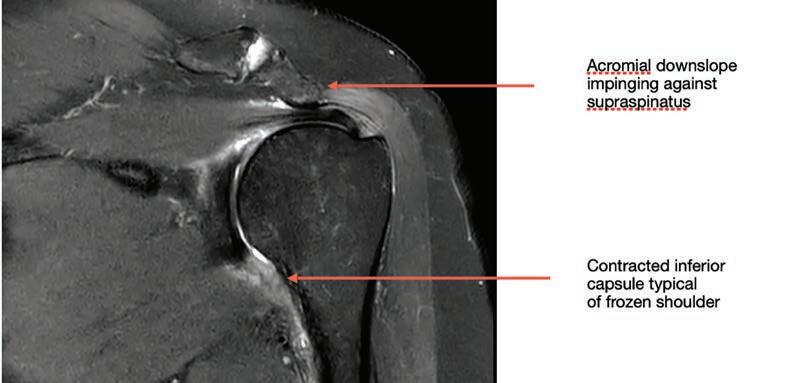

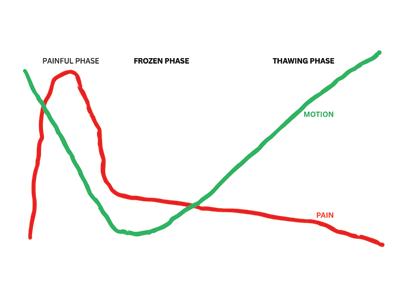
group have significant rotator cuff tendinosis and impingement evident on history and MRI and arthroscopic examination.
The key clinical features are deepseated shoulder pain followed by stiffness.
In a patient whose shoulder is sore, determining whether the shoulder is stiff can be challenging. The important steps are to stand behind the patient, gently support the affected forearm and with the other hand gently hold their scapula.
By assessing range slowly and gently we can minimise pain and by holding the scapula we can isolate true shoulder (glenohumeral) movement by eliminating scapulothoracic movement.
We can then truly assess passive
glenohumeral range, in particular ER and abduction. Frozen shoulder results in restricted abduction and ER, whereas rotator cuff disease does not.
Patients should be examined for wasting or scapular winging, which suggest pain from brachial neuritis – these patients will usually not have stiffness. Rotator cuff pathology can be very painful but usually does not result in stiffness.
Key investigations are plain radiographs and ultrasound, or MRI where feasible. Ultrasound should be combined with plain XR to exclude arthropathy or neoplasia, which can also cause deep-seated pain
The most important therapeutic step is steroid injection into the shoulder (glenohumeral) joint to switch off the inflammatory reaction in the capsule.
This can be done under CT or US
1 Frozen shoulder is common in middle age. Often there is no obvious cause.
2 Many patients get better over time, but it can take years.
3 Key pathological feature is capsular contracture and synovitis.
4 Key clinical feature is loss of range (passive glenohumeral range)
5 A plain x-ray should always be requested with ultrasound, where feasible MRI is best.
6 Most useful treatment is steroid injection into the shoulder joint, followed by physiotherapy when pain settles.
7 Many patients require manipulation under anaesthetic to restore range of motion.
8 A large percentage of patients also have pathology that can be remedied arthroscopically.
guidance and is best performed by radiologists who are performing this procedure on a regular basis.
Patients typically report significant improvement in pain level within two to four weeks. Once pain abates, patients can commence on a range of motion programme with a physiotherapist.
It is reasonable to wait 6-12 weeks to ascertain whether patients are improving.
It is worth noting that steroid injection is much more predictable than hydrodilatation. Many patients find that pain becomes more tolerable after the injection, but they cannot achieve a functional range of motion.
Surgical intervention should be considered in this group, and for patients with calcific tendinopathy and those with features of subacromial impingement on history or MRI.
Under anaesthesia, the surgeon stabilises the scapula and gently manipulates the shoulder with palpable release of the contracted inferior and anterior capsule. Patients often find the immediate restoration of range of motion tremendously satisfying.
Arthroscopic release of the contracted capsule can be performed when more significant stiffness is present.
If the diagnosis is unclear, early referral is advisable. When the diagnosis has been clearly established but no improvement has occurred after 6-12 weeks patients should also be referred.
Many patients require manipulation under anaesthetic to restore range of motion, typically this gives rapid improvement. A large percentage of patients also have pathology that can be remedied arthroscopically, such as rotator cuff impingement and calcific tendinopathy.
Author competing interests – nil





By Dr Helen Douglas, Dr Suzanne Rea & Dr Anna Goodwin-Walters, Specialist Plastic and Burns Surgeons, West Leederville
Any full-thickness skin injury will leave a scar, but why do some wounds heal quickly and well, and others leave an obvious scar?
Some factors are intrinsic to our bodies and less amenable to amelioration. Other factors are extrinsic, like lifestyle and can be optimised to influence healing and scarring.
Leaving a scar
There are several factors that can influence wound healing and scarring:
Age: young skin produces more collagen and a larger inflammatory response, meaning younger people heal quicker but scar worse.
This is important if you are the parent of a child considering scar revision, as surgery may be best left until older, however ablative CO2 laser can improve scars at any age.
Skin type: in general, darkerskinned individuals form worse scars than those with lighter skin, however pale South-East Asian skin

frequently forms problematic scars.
The answer probably lies in hereditary genetics, but we have yet to fully delineate scar genetic pathways or treatment targets.
Nutrition: low levels of protein, vitamins and minerals can affect wound healing and scars. Vitamin C, A and E are required to make and cross-link collagen and stabilise membranes whilst zinc, copper and selenium are all important enzyme co-factors.
Vitamin D has been shown to have a complex but vital role in several types of scar formation and immunity.
Medications: immune modulating drugs, such as steroids, will delay healing and can increase risks of poorer scarring.
However, some anti-inflammatory medications have been observed to reduce scar collagen and improve scars. The relationship is complex, and any medication changes must be made with full understanding of implications and risks.

Wound factors: infection, tension or shear can disrupt collagen bonds, delay healing and subsequently produce scars with excess collagen (hypertrophic) or stretched scars.
Prompt identification and treatment of any issues is key to optimising healing and preventing problematic scars.
Smoking/vaping: aside from being a bad idea in general, it also delays wound healing by reducing oxygen transport to the skin and nicotine constricts blood vessels and reduces blood flow to the wound.
Prevention or cure?
With elective surgery it may be possible to optimise intrinsic and extrinsic factors for wound healing and scarring, but this isn’t possible in trauma or emergency situations. So, once we have a wound, how can we support it from the earliest stages to prevent a poor scar?
Suture removal
Remove sutures in a timely fashion


Key messages
Factors affecting wound healing and scarring are complex and interlinked
Some of these factors can be improved prior to surgery, but effective post-injury or post-operative wound care is important for all healing and scars
Early, targeted multi-modal scar treatments with scar therapy and CO2 laser can improve long-term scar outcomes.
to prevent unsightly dots either side of the scar, where the skin has started to heal around the stitch. The better the blood supply, the quicker the healing and the faster the sutures can be removed.
This is roughly 5-7 days for the face, 7-10 days in upper limbs and trunk and 10-14 days in lower limbs.
Massage and moisturiser
Once a wound is stable and dry, gentle massage and moisturiser can be applied to hydrate and improve sensitivity.
This is best performed with a water-based moisturiser at first to prevent spots in the freshly healed area and ten minutes twice a day can help flatten scars and prevent adhesions.
Silicone
Silicone has been shown to hydrate and improve scars in the early postinjury period. This can be in the form of gels – especially for faces –or sheets – useful to apply at night – and can apply light pressure to the wound, assisting with flattening and reducing itch.
Sun protection
Scars can burn easily, change pigment and become more obvious and should be protected with SPF50+ sunscreen for at least the 18-month maturation period of the scar.
Compression garments
For certain scars, such as burns and weight loss surgery, compression garments can help reduce the scar blood flow, keeping it flatter and paler.
They can assist lymphatic fluid drainage and make the scarred area feel more comfortable. These
garments can be as simple as a Tubigrip or as sophisticated as a custom-made suit.
Early CO2 laser
Modern powerful ablative CO2 lasers can be used as early as six-weeks post-injury to treat scars which are thick and red or show early signs of becoming problematic.
The laser vaporises thin columns of scar tissue and leaves undamaged adjacent skin to allow healing within two days. This minimises risks while allowing laser energy to remodel deeper scar collagen and has been shown to improve long-term scar outcomes.
There are some risks of problematic scarring we can improve and some we can’t. Early expert wound and scar care is key to a good scar outcome.
Author competing interests – nil
By Dr Dinusha Chandratilleke, Immunologist/Allergist, Wembley
Allergic rhinitis (AR) is a common often under-recognised condition affecting up to 20% of Australians that can significantly impact quality of life, sleep, school and work performance.
Typical management includes allergen avoidance, oral antihistamines, combined corticosteroid/antihistamine nasal sprays and antihistamine eye drops.
Allergen immunotherapy (AIT), also known as desensitisation, offers an additional treatment option with difficult to control disease.
AIT involves administering increasing doses of a specific allergen, like grass pollens or dust mite, to a patient to induce tolerance. Unlike antihistamines or corticosteroids that only control symptoms, immunotherapy aims to ‘reprogram’ the immune response to reduce/stop reactivity to the specific allergen.
The two approaches are subcutaneous immunotherapy (SCIT) or sublingual immunotherapy (SLIT, with drops/tablets). They have similar efficacy and a standard treatment course is three years.
Figure 1 outlines pros and cons of each approach. In Australia, SCIT remains the most popular option, but SLIT is becoming more prevalent.
Protocols vary depending on the specific product, but for SCIT the up-dosing phase (i.e. from zero to maintenance) is typically weekly for 4-12 weeks, followed by monthly maintenance injections for the remainder of the course.
SLIT up dosing can be as short as a few days, with maintenance consisting of daily dosing of drops/ tablets.
In Australia the most common allergens used in immunotherapy are grass pollens, house dust mite and animal dander (cat/dog), with tree pollens, weed and mould less common.
How does it work?
In short, this is still under


Pros
Cons
• Less expensive
• Less frequent dosing (monthly)
• Slightly delayed dose has minimal impact on efficacy.
• More inconvenient (all injections administered by GP or allergist)
• Local swelling can be severe
• Slightly higher risk of systemic reactions (anaphylaxis).
investigation. The principle is around shifting the immune response from a pro-allergic Th2 response to a regulatory Th1 response.
Proposed mechanisms include induction of T-regulatory cells that secrete suppressive cytokines (IL-10 and TGF-β) and increasing IgG4 blocking antibodies, which result in reduced mast cell and basophil reactivity.
Ultimately the aim is to achieve a long-lasting reduction in allergic symptoms. Most patients start to notice improvement in their symptoms within 6-12 months.
When to refer
Clinical indications include allergic rhinitis, allergic conjunctivitis, or allergic asthma.
Indications for an allergy referral include uncontrolled symptoms despite antihistamines/nasal
• More convenient (can be done at home)
• Low risk of systemic reactions
• Tablets/drops are easily transported.
• More frequent dosing (daily)
• More expensive
• Missed doses have a significant impact on efficacy
• Local reactions (mouth itch) can be irritating.
corticosteroids, significant impact on quality of life, for example sleep disturbances, time off school/work, and desire for long-term symptom relief rather than continuous medication use
Evidence is weaker in eczema. There is no evidence for desensitisation for chronic skin itch or urticaria.
GPs play a crucial role in managing allergic rhinitis and overseeing immunotherapy through identification of patients with possible allergic rhinitis/ rhinoconjunctivitis.
• Initial investigations: specific IgE (RAST) testing to grass/tree/ dust/animal dander to confirm aeroallergy
• Initiating treatment: allergen minimisation, antihistamines/ nasal corticosteroids
AIT ‘reprograms’ the immune response, reduces reactivity to specific allergens and is the closest thing to a cure for aeroallergy
Main clinical indications are allergic rhinitis, allergic conjunctivitis and allergic asthma
Consider AIT in patients not responding to standard medical therapy, with significant impact on QOL.
• Referring patients with difficult to control disease
• Counselling patients, providing an overview of AIT – benefits, time commitment (three years)
Typically, the first dose of SCIT is given by the allergist, before requesting the GP’s assistance with ongoing up dosing/maintenance.
Give deep subcutaneous injections (posteriorly over triceps). The risk of systemic reaction is low, but 30 minutes observation required
to exclude anaphylaxis, even if stable on maintenance.
Resuscitation equipment (IM adrenaline, oxygen) must be available. Advise no exercise for two hours after each injection. Withhold AIT if patient has a fever, wheeze, or symptomatic asthma.
Contact the consultant immunologist/allergist if any concerns or reactions
Case 1: Immunotherapy is suitable
Sarah is a 34-year-old woman with longstanding perennial rhinitis, sinus congestion and watery/itchy eyes. Specific IgE testing showed she was positive to dust (23.10 kU/L), negative to grass/tree/animal.
No significant improvement with allergen minimisation strategies or nasal sprays.
Referred to an immunologist, skin prick testing positive to house dust mite only. Commenced on SCIT to D.pteronyssinus (50%) / D.farinae (50%) mix.
Mild local reactions are treated with Cetirizine 10mg given 30 minutes before each injection.
Within 12 months, Sarah has noticed a significant improvement in her symptoms, QOL questionnaire dropping from 48 to 17. AIT will continue for three years.
2: Immunotherapy is not suitable
John is a 45-year-old man with a history of childhood eczema, but skin symptoms on his hands and feet have worsened over last 12 months.
Topical corticosteroids are partially effective. He requested allergy testing to find the cause of his eczema: specific IgE was positive to grass (28.1 kU/L) and dust (17.3 kU/L), with a high total IgE (1242). No nasal/sinus symptoms or asthma. In this case, immunotherapy is not routine practice for the treatment of eczema, as the mechanism of disease is not IgE based.
There could be a role for allergen minimisation strategies, but he will benefit more from a thorough topical corticosteroid plan, consideration of systemic immunosuppression, or biologics (if satisfying PBS criteria).
Author competing interests – nil
Mr Saud Hamza
Specialising in:
Oncoplastic Breast Surgery including breast reconstruction and rotation flaps
Breast reduction and mastopexy (nipple lifting)

Removal of breast implants and mastopexy Thyroid Surgery.
Practicing Location: Mandurah & Murdoch
Operating Locations:
St John of God Murdoch, Murdoch Peel Health Campus, Mandurah Hollywood Private Hospital, Nedlands
The Mount Hospital, Perth
Email: info@saudhamza.com.au
Healthlink EDI: mrhamzas

Dr Wei Ling Ooi
Specialising in:
Oncoplastic Breast Surgery including breast reconstruction and rotation flaps
Breast reduction and mastopexy (nipple lifting)

Removal of breast implants and mastopexy.
Practicing Location: Murdoch
Operating Locations: St John of God Subiaco, Subiaco
Email: secretarydrooi@gmail.com
Healthlink EDI: wlingooi
Dr Kai Hellberg
Specialising in:
Gallbladder Surgery
Hernia Surgery
Endoscopic Services with Gastroscopy & Colonoscopy

Haemorrhoid treatments and other benign procto-rectal conditions
Ingrown Nail Surgery
All Skin and Soft Tissue Procedures.
Practicing Location: Mandurah & Murdoch
Operating Locations:
St John of God Murdoch, Murdoch Peel Health Campus, Mandurah
Email: murdochrooms44@gmail.com
Healthlink EDI: hellberg
Postal Address | Suite 44, Level 2, Murdoch Clinic, 100 Murdoch Drive, Murdoch WA 6150 Appointment Bookings | Phone: (08) 6148 0540 Fax: 9332 9425
www.perthsurgeons.com.au
By Dr Laurence Webber, General Surgeon, Mt Lawley
The vast majority of mesh hernia repairs in Australia are still performed using mesh made from polyester or polypropylene – synthetic plastics invented more than 50 years ago.
While the durability of mesh hernia repairs is well documented, we know less about what happens to these products in the body over time.
Recent concerns regarding microplastics and the recent class actions over the outcomes of transvaginal pelvic mesh have placed renewed emphasis on alternatives to permanent synthetic surgical prostheses.
Due to these concerns, many patients now explicitly seek alternatives to permanent mesh and, fortunately, hernia mesh manufacturers now produce a variety of absorbable products both biological and synthetic in nature. These meshes typically are either absorbed or broken down by the body over time and can be a manmade synthetic product or an animal-based mesh, often made from bovine or porcine collagen.
New materials
An example is poly4hydroxybutyrate (P4HB), a fully absorbable, monofilament scaffold that typically resorbs within 12-18 months. During this absorption time, the tissue ingrowth into the mesh gradually transfers load to newly formed functional tissue.
By around one year, patient tissue remodelling often shows greater than threefold the strength of the native abdominal wall, providing durable repair after mesh disappearance.
P4HB maintains strength in the presence of bacteria and integrates rapidly, with abundant collagen formation at 52 weeks documented in preclinical and clinical studies.
Long-term follow up of major hernia repairs using these P4HB meshes have shown equivalent or better results than some permanent meshes. This mesh has now been


used in thousands of hernia repair cases around the world.
Other alternatives to this product include porcine and bovine biological meshes.
These are typically very fast absorbing meshes and are suitable for special circumstances in complex hernia repair and abdominal wall reconstruction.
Some meshes now even come as a composite of absorbable and nonabsorbable fibres to facilitate leaving as little permanent implant in the body as possible.
The upshot of all these offerings is that we can now choose a mesh implant to meet patient requirements, expectations and preferences with shared decision making discussing the pros and cons of permanent synthetic mesh,
Most hernia mesh repairs use plastics developed 50 years ago Today there are multiple options available
Patients can make an informed decision in consultation with their surgeon.
biologics, and absorbable P4HB mesh.
Given the legal memory of inadequate risk disclosure in mesh litigation, transparency and documentation are essential and, in ideal circumstances, the patient and clinician make the decision together about what prosthesis will be used in each surgical situation.
These mesh products are all listed on the prostheses list, meaning no increased out-of-pocket costs to insured patients and many are stocked on-shelf or are easily accessed in most private hospitals.
In summary, there are now plenty of mesh choices on the market, and with proper patient education a satisfactory product can be found for each case.
Author competing interests – nil
By Dr Mark Hurworth , Orthopaedic Surgeon, Murdoch
Patients who engage actively in their care generally achieve superior outcomes compared to those who adopt a passive stance.
Passivity – whether encouraged by compensation systems, chronic pain frameworks, or overreliance on pharmaceutical solutions –undermines outcomes.
In my practice, particularly in elective orthopaedic surgery, successful results rely heavily on patient engagement.
Procedures such as knee replacement, atraumatic rotator cuff repair, and spinal surgery not only demand strict adherence to preand post-operative regimens but evoke the moral question of whether surgery should proceed unless the patient has exhausted reasonable non-operative treatments.
Such treatments typically include physiotherapy and structured exercise, but until recently these have been difficult to quantify objectively.
My current research interests focus on using technology to refine this process in three ways:
1. Improving measurement, moving beyond patient-reported outcomes to objective data
2. Using exercise as a measurable treatment, standardising non-op, pre-op and post-op treatment
3. Expanding remote care, allowing patients to undertake treatment within their own homes while still generating meaningful clinical data.
These efforts aim not only to improve outcomes but also to reinforce agency, making patients active partners in their care rather than passive recipients.
Exercise as a prescription
Exercise provides a unique therapeutic model precisely because it demands engagement. It activates the musculoskeletal system – arguably the body’s largest organ – and in doing so stimulates an intricate range of biological processes.
Exercise embodies agency, requiring active patient participation and delivering benefits that surpass those of many medications
A pharmaceutical agent that could simultaneously reduce cardiovascular risk, prevent diabetes, strengthen bone, preserve cognition, alleviate depression, and extend life with negligible adverse effects would be universally prescribed
In modern healthcare, agency expressed through structured exercise may be the most powerful prescription available.
Cardiovascular function improves, metabolism is enhanced, and neurochemical changes elevate mood and cognition.
Evidence consistently demonstrates that exercise is as effective as pharmacological interventions in multiple domains. A systematic review found exercise interventions comparable to medications for the secondary prevention of coronary heart disease, rehabilitation after stroke, and prevention of diabetes.
Another trial reported that structured exercise can be as effective as antidepressants for major depression. Unlike pharmaceuticals, exercise impacts nearly every organ system simultaneously and produces improvements in sleep, energy, and resilience.
Medications often carry significant side effects including possible addiction. Exercise, when performed appropriately, carries minimal risk and enhances self-efficacy.
Patients assume responsibility for their progress, develop discipline, and build a stronger connection with their own bodies. This sense of control generates a positive feedback loop that reinforces both physical and psychological health.

Exercise offers preventive benefits that no single drug can match. The World Health Organization identifies physical inactivity as the fourth leading cause of global mortality.
Regular physical activity reduces cardiovascular risk by up to 35%, type 2 diabetes by 50%, and certain cancers by approximately 20%. It also delays cognitive decline, with strong evidence showing reduced incidence of dementia in physically active older adults.
From an economic perspective, exercise is cost-effective. Many interventions such as walking, resistance training and stretching require no equipment.
Even when costs exist, such as gym memberships, they are modest compared with the long-term financial burden of pharmaceutical management for chronic disease.
This argument is not intended to dismiss pharmacological treatments, they remain essential for many conditions, particularly genetic disorders, acute infections, or advanced illnesses.
However, lifestyle interventions such as exercise should not be regarded as optional adjuncts but as primary therapeutic strategies.
Encouragingly, some healthcare systems now include exercise prescriptions, reflecting a gradual shift toward recognising movement as medicine.
In orthopaedic practice, this principle is especially important. Compliance with prehabilitation and rehabilitation directly influences surgical success.
Patients engaging in structured exercise before surgery not only experience improved outcomes but also embody the principle of agency, demonstrating commitment to their own recovery.
Author competing interests – nil
By Dr Sheldon Moniz, Orthopaedic Surgeon, Murdoch
Hand and wrist injuries are frequently encountered in primary care and a sound understanding of diagnosis and early management is essential to facilitate appropriate referrals and optimise patient outcomes.
The functional complexity of the hand arises from its structural architecture: the rigid proximal transverse arch, the mobile distal transverse arch, and the longitudinal arch.
Together, these provide the mechanical foundation for both power (hook, spherical) and precision (tip-to-tip, lateral) grips.
The coordinated action of flexor and extensor tendons enables fine motor function. Disruption due to trauma or degeneration may lead to profound functional impairment and underscores the importance of early recognition and intervention.
Presentations in primary
Fingertip and nailbed injuries
These are common and require careful assessment to preserve function and appearance. Management should consider three key elements: sensation, structural durability, and bone integrity.
While some cases may require surgical repair – particularly where there is nailbed laceration, subungual hematoma, or distal phalanx fracture – initial GP management should prioritise wound irrigation, dressing, tetanus prophylaxis, and prompt referral.
Most injuries can be definitively managed in emergency under a digital (ring) block with appropriate local anaesthesia and minor surgical intervention.
Bites and lacerations
Bites (human or animal) carry a high risk of infection. Empirical antibiotics (e.g., amoxicillinclavulanate), tetanus status and blood borne virus exposure risk should be assessed.
Radiographs are essential to rule




out fractures or foreign bodies. Early splinting and referral are advised.
Mallet finger
Caused by extensor tendon disruption at the distal phalanx, resulting in loss of active fingertip extension.
Initial treatment involves continuous splinting in extension for 8-12

weeks. Patient education and hand therapy follow-up are key.
Trigger finger (A1 Pulley Stenosis)
Common in diabetes, rheumatoid and hypothyroidism. Presents with painful locking or clicking of the finger.
Suspected infection, such as septic tenosynovitis, constitutes a surgical emergency requiring urgent ED referral.
Key messages
Hand and wrist injuries are prevalent in primary care and often underestimated
A systematic approach, early diagnosis, and appropriate management – including timely referral – are essential to prevent complications and preserve function
Practical knowledge on these conditions ensures a critical role in patient recovery and continuity of care.
Volar plate injuries and finger dislocations
These frequently involve the PIP joint. After assessing for instability and deformity, immobilise (typically at 30° flexion) and arrange referral as needed based on severity and associated fracture.
Dupuytren’s contracture

surgery is indicated for functional impairment.
Carpal Tunnel Syndrome (CTS)
Presents with nocturnal paraesthesia, weakness and thenar atrophy. Initial management includes splinting and nerve gliding exercises.
Refractory cases may warrant nerve conduction studies and surgical referral. An X-ray is often helpful to exclude thumb arthritis which may cause similar symptoms.
Fractures and dislocations
Distal radius fractures: Among the most common. Evaluate for articular involvement and postreduction deformity. Reimaging post-immobilisation is essential.
Phalangeal and metacarpal fractures: Assess for displacement, rotation, and joint involvement. Stable injuries may be managed with buddy strapping or splints; refer if unstable or intra-articular.
Thumb injuries
UCL injury (Skier’s Thumb): Suspect with forced abduction injuries; instability warrants referral.
with splinting and analgesia; consider surgical input if function is significantly affected.
Tendon ruptures
FDP (Jersey Finger): Inability to flex the DIP joint post-trauma. Surgical management is typically required.
EPL rupture: Often post distal radius fracture or rheumatoid arthritis. Presents with inability to extend the thumb.
Key management principals
Make a thorough assessment: Mechanism of injury, functional impact and a detailed examination (deformity, range of motion, tenderness) are fundamental.
Imaging: Always start with plain radiographs – PA, lateral, oblique views – in traumatic presentations.
Initial management: Includes correct splinting, analgesia, wound care and avoiding delays in referral.
Referral criteria: Suspected tendon ruptures, joint instability, displaced fractures and infections should prompt early specialist involvement.
Basal thumb osteoarthritis: Common in older adults. Begin Complete the self-reflection and claim your CPD time, please scan here
Author competing interests – nil
Exercise to improve outcomes
Hand and wrist injuries
Preventing problematic scars
Compounding medicine
Down syndrome care
Aeroallergen immunotherapy
Advancements in mesh
hernia repairs
Prescribing exercise as medicine
Frozen shoulder
Immunity impacts of COVID restrictions
Exercise and patient care
Lung cancer screening
Online first
Advanced care in general practice
Chronic disease management rebates
Diagnostic and Interventional Radiologist

What is your area of practice?
MH: I am a consultant diagnostic and interventional radiologist based in Claremont since 2010. I am in full time private practice and workload is a mixture of Medicare, private, DVA and WC/MVIT.
Where did you train?
MH: I graduated from the University of Auckland medical school in 1998. I then moved to Perth as a resident medical officer and then emergency department registrar in 2000.
I returned to NZ in 2002 to commence radiology training with an emphasis on interventional radiology. I completed my radiology training in 2006. My first-year consultant role was in Auckland, however I wished to return to Perth and relocated permanently in 2008.
What procedural services do you offer?
MH: I provide MSK interventional radiology services including spinal and peripheral radiofrequency ablation (RFA), wide array of cortisone injections/blocks, Morton’s neuroma ablation, hyaluronic injections and orthobiologic procedures including PRP and autologous tenocyte implantation.
How is your service different?
MH: I am passionate about raising awareness of radiology interventions that can improve patient outcomes with minimally invasive treatments which have increased rapidly in recent years.
I note current issues facing patients with chronic spinal/ MSK pain – excessive waiting periods; treatments being performed as inpatient GA/sedation procedures when they could be outpatient procedures; and excessive cortisone administrations which can be mitigated by appropriate use of RFA, PRP, and hyaluronic acid.
Most health practitioners are aware of CT guided RFA for spinal conditions, however there is a growing interest in using RFA for osteoarthritis of hips, knees, shoulders, and peripheral nerve pain conditions.
I am passionate about raising awareness of radiology interventions that can improve patient outcomes with minimally invasive treatments which have increased rapidly in recent years.



What happens inside our cells when we exercise? While the benefits of physical activity for cardiovascular, metabolic, and musculoskeletal health are well established, how mechanical forces influence cellular function have remained elusive.
A recent scientific study led by WA researchers and published in Science Advances identifies a previously unrecognised pathway that explains how cells physically sense exercise and convert mechanical forces into metabolic responses.
This breakthrough not only helps us understand why both inactivity and excessive loading to our body can damage tissues but also offers potential pharmacological intervention on exercise to improve the benefits of physical activities.
Historically, subcellular mechanobiology has focused on the cytoskeleton and nucleus as the primary structures responsible for sensing and transmitting mechanical cues.
However, the role of the endomembrane system, another extensive intracellular network, has been largely overlooked.
This study demonstrates that membrane tension in the endoplasmic reticulum (ER) functions as a novel cellular language for expressing mechanical stress, reshaping established paradigms and offering new insight into how cells interpret mechanical cues at the organelle level.
The research uncovers a new mechanotransduction mechanism in which mechanical strain applied to the plasma membrane (PM) is relayed directly to the ER via physical tethers at PM-ER membrane contact sites (MCSs).
These structures act as physical 'bridges' that transmit force into the endomembrane system, independently of the cytoskeleton.
As a result, mechanical loading alters ER membrane tension, which modulates ER-mitochondria interactions and affects
mitochondrial respiration and overall energy metabolism.
This force-sensitive axis serves as a cellular decision-maker, determining whether mechanical input promotes energy production or activates stress pathways.
Using a custom-designed bioreactor system, organelle-targeted membrane tension probes and fluorescence lifetime imaging microscopy (FLIM), the researchers dynamically measured subcellular membrane tension in live cells.
The results were striking. Moderate, physiological strain increased ER tension, enhanced ER-mitochondria coupling, and boosted cellular energetics.
In contrast, excessive strain disrupted these interactions, inducing ER stress, mitochondrial dysfunction, and impaired energy output. This provides a clear cellular explanation for why both underuse and overuse of tissues such as tendons and ligaments can lead to degeneration.
One of the study’s most significant findings is the identification of ER membrane tension as a potential biophysical indicator of cellular mechanical stress.
Unlike traditional biomarkers that rely on indirect or invasive measures, ER tension can be monitored in real time in live cells. This discovery may pave the way for early diagnosis and monitoring of mechanically induced pathologies, such as tendinopathy, muscle atrophy, and fibrosis.


These findings help explain, at the cellular level, how physical activity influences tissue health and why there is a 'sweet spot' for mechanical loading.
Clinically, this could inform personalised exercise prescriptions tailored to deliver optimal mechanical strain during rehabilitation, recovery, or athletic training.
It also opens avenues for mechanomodulatory therapies, where drugs or gene-based interventions target organelle tethers to simulate beneficial strain in sedentary or immobilised patients.
Notably, the pathway identified here provides a biochemical means not just of mimicking, but of actively modulating mechanical input. By targeting PM-ER tethering structures, it becomes possible to dampen force transmission and protect cells from damage in overloaded environments.
For example, partial inhibition of this pathway could reduce straininduced cellular stress in elite athletes or workers in physically demanding roles, preserving longterm tissue integrity.
This study bridges the gap between exercise physiology and cellular biology, offering a molecular blueprint for how mechanical force influences metabolism.
It reframes physical activity not only as a systemic health booster but also as a mechanical nutrient, an input that cells are equipped to detect, process, and respond to with remarkable precision.
Understanding this new organellebased language of force may lead to the next generation of interventions. Whether through exercise, pharmacological intervention, or molecular diagnostics, this work lays the foundation for more nuanced and targeted strategies to enhance musculoskeletal and metabolic health.
Author competing interests –the authors were involved in the study.
Journalist Casey Beros cared for her dad until his death two years ago. She decided to share what she’d learnt in a new book called Next of Kin.

By Ara Jansen
As a writer you’re often told to write what you know. That was never more relevant than to health journalist Casey Beros and her latest book Next of Kin - it’s about what to expect when you’re expecting to care for someone you love.
The Perth-born journalist felt the pull home from Sydney when her dad was diagnosed with mesothelioma and given six months to live. Casey, her husband and two kids moved back across the country so she could spend previous time with and care for her dad.
What started as six months turned into two years, before her father passed away in 2023.
This double-sided experience –both incredibly joyful and painful –led her to write Next of Kin, a highly accessible and practical guide around looking after someone who is dying, sitting side-by-side with an honest, generous and moving recount of her own journey.
Casey echoes her father’s thoughts calling life a glorious tragedy –the death of her father but the opportunity to spend intensive time with him.
With her journalist hat never far, Casey had the foresight to record many conversations with her dad
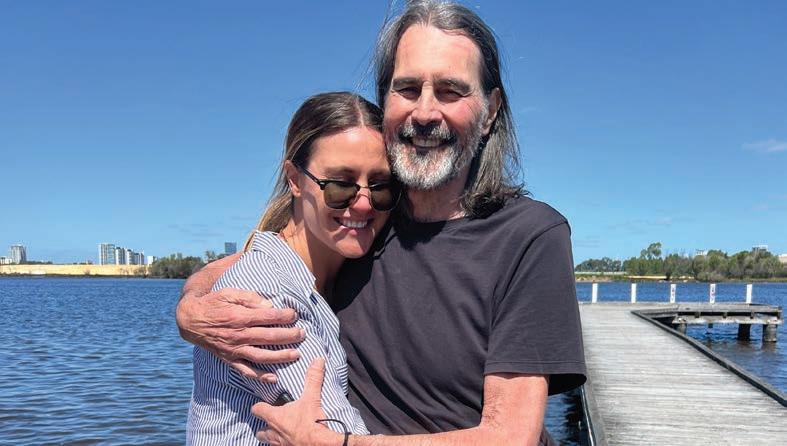
and take copious notes about what they were both going through.
She has written the book she wished she had at the beginning of her care journey, covering medical, physical, legal, financial and emotional care.
“I’m encouraging people to read this before they need it,” said Casey. “For the people who are in it, or have recently been through it, this is an ‘I see you’.
“My dad was my person. He was my soul mate in a lot of ways. There’s now a gap in my life that can’t be filled by anyone else. The way he
got me has not been replaced. I chose to look after him and would choose it one hundred times over.”
Casey said coming back to Perth to be with her dad did not feel so much like a duty, but a compulsion, even though she didn’t really know where it came from.
“I never remember having the conversation about coming to Perth. We had been in Sydney for 15 years. COVID kind of forced our hand as I was working for myself and my husband was working remotely as a teacher.”
Casey went from not seeing her

“I chose not to live with hope of a miracle. The truth is that you are going to lose them at some point. The gift of a prognosis is that someone has started a clock and put it on the wall. In this case the clock was wrong, and I got two-and-a-half years.”

dad much to seeing him every day, with their connection and emotions on steroids knowing their time together was finite.
While rationally knowing she would lose him, Casey took the opportunity to have many deep conversations about life but also about how we and the system could do better in this space.
“I chose not to live with hope of a miracle. The truth is that you are going to lose them at some point. The gift of a prognosis is that someone has started a clock and put it on the wall. In this case the clock was wrong, and I got twoand-a-half years.
“I really leant into every day being with him. We went on holidays, had second breakfasts. We didn’t dawdle because you always think you have more time. I still don’t have any regrets that I leant in so hard and left nothing on the table.
“It was a willing investment, but I don’t recommend it. People who read the book will be able to relate to being able to see what you did on the other side.
“I’m young and able-bodied and

otherwise fit and healthy, I can do this. But I did wave the white flag a few times, which I needed to do way sooner. If you had said while I was in the trenches ‘you can find five minutes’ I would have quite liked to have punched you in the face.”
The author said now she lets the grief come when it does, which is allowing her to move forward. That’s not to say grief doesn’t still hit Casey. Something seemingly unrelated – like picking up a yoghurt in the supermarket – can suddenly bring on waves of grief.

“What an insane privilege to be able to do that for him. A lot of people wouldn’t be able to move a family of four across the country to do something like this.
“My family and friends really stepped up and helped my family stay alive. They dropped us meals, checked in, picked the kids up from school.”
Next of Kin is available online. Medical Forum has three copies of the book to giveaway, see our competitions for how to enter.
While creating the Terracotta Warriors: Legacy of the First Emperor was an incredible experience for one of its designers, it’s also proving a huge hit with visitors to the WA Museum Boola Bardip.
By Ara Jansen

For Dan Schoknecht it was a trip of a lifetime. Travelling to China to help pick the artefacts which would make up an international-first exhibition.
More than a year later, the Terracotta Warriors: Legacy of the First Emperor is open at the WA Museum Boola Bardip and running into summer.

“We had nothing – the exhibition started as an idea and a partnership with the Shaanxi Cultural Heritage Promotion Centre,” said Dan, the senior exhibition coordinator.
The museum team went to China in November 2023 where they negotiated to bring more than 225 Chinese artefacts to Perth for an exhibition they created and designed in partnership with the centre and Emperor Qinshihuang’s Mausoleum Site Museum.
With some of the items never before seen in Australia and nearly half having never left China, the exhibition consists of 10 terracotta figures including, eight warriors, a seated attendant and a horse.
It’s the largest number of warriors allowed out of China at one time loaned to one institution.
The objects and artefacts range from kitchenware to rare gold ornaments and adornments, a bronze swan, jade pieces and jewellery, and even some terracotta pigs and piglets excavated from a tomb. These are Dan’s personal favourites. For visitors, there a model piglet to touch.
“We wanted variety in the objects but we also wanted them to tell a story,” says Dan. “We created a narrative around the objects which would take people on a journey. We made sure it was a unique assemblage of objects, displayed in a unique way. It’s a particularly large assembly, larger than would normally be put together.”
Known the world over, the chance discovery of the Terracotta Warriors near Xi’an in 1974 remains one of the most significant archaeological finds of all time. Buried for more than 2000 years,

the life-sized warriors were created to guard China’s First Emperor, Qin Shihuang, in the afterlife and became a legendary army frozen in time. The exhibition focuses on the extraordinary world of Emperor Qin Shihuang, exploring his life, legacy and afterlife.
Terracotta Warriors invites visitors to step into the Qin dynasty through never-before-seen immersive digital experiences and cutting-edge multimedia, bringing this ancient civilisation to life.
The exhibition explores the emperor’s vast tomb, rare artefacts and the ongoing archaeological
discoveries that continue to reshape our understanding of early China.
“The warriors are the most wellknown of these artefacts and they only let you have 10 at a time,” Dan adds.
“Visiting the sites was awe inspiring and we were privileged to meet people who have been working with some of these artefacts all their lives.”
A rich program of events supports the exhibition, including large-scale external projections, behind-thescenes tours, talks, school visits and interactive experiences.
This includes a Friday mahjong club, activity zone, family Sundays, yum cha, screen printing, adventures in archaeology, music, quiet mornings and Chinese arts over tea.
The Terracotta Warriors runs to 22 February 2026. Tickets from WA Museum Boola Bardip and includes a season pass option to visit the exhibition as often as you like.

We’ve got more to give away this month from books to movie tickets and wine.
Win one of three copies of Next of Kin: What to expect when you’re expecting to care for a loved one
We also have three double passes to the Terracotta Warriors: Legacy of the First Empire exhibition to give away.
If a trip to the movies is more your scene, win one of 10 double passes to see The Travellers in cinemas from October 9.
Or win one of 10 double passes to see After the Hunt starring Ayo Edebiri, Andrew Garfield and Julia Roberts, in cinemas from October 16.
If you fancy some premium wine, we’ve got a doctor’s dozen to give away from Mandoon Estate. See over the page for details.
To enter, use the QR code on this page or go to mforum.com.au and hit the competitions tab.




















































































Our podcasts bring you the latest updates and key insights into new treatment options available.
Join our clinical editor Dr Joe Kosterich in conversation with WA specialists to learn more about developments to improve patient outcomes. Our podcasts are now CPD verified. Look for the CPD logo to complete your self-reflection and claim your time.
Learn more about:
Aortic stenosis: managing low-risk patients with Dr Gerald Yong
Rethinking radiation oncology with A/Prof Yvonne Zissiadis & Celia Byatt
Holistic management of osteoarthritis with Dr Arash Taheri
Lung Cancer Screening with Prof Fraser Brims
How to approach acute and chronic knee pain with Dr Jean Louis Papineau
Listen on your favourite podcast platform – scan the QR code to follow us!

Located at Caversham in the Swan Valley, this historic vineyard was purchased by the Erceg family in 2008 with no time wasted before the winery was established and their first vintage in 2010.
It was delivered by winemaker Ryan Sudono who has had notable success with their Mandoon Estate wines in Australian wine shows.
The name Mandoon is Noongar for “place of many trees” and was chosen to pay respect to the original custodians of the land.
Their commitment to saving and preserving old vines is impressive. We often underestimate our Swan Valley in comparison to wines from more southern regions, but this site having vines dating back to 1895 has been revitalised and is creating wonderful wines that the Valley does so well –Chenin Blanc, Verdelho, Grenache and Shiraz.

Mandoon 2024 ‘Wild Bunch’ Chenin Blanc, Swan Valley, RRP $34
From vines planted in 1972 this wine displays typical varietal tropical fruit aromas with complex oaky characters coming through. Flavours of green apple and Nashi pear. Slightly taut and austere in its youth, a reflection of Chenin’s acidity and structural integrity which will give it up to 20 years aging. A terrific wine which will uphold the valleys reputation for aged Chenin Blanc.
Mandoon 2023 Old Vine Grenache, WA, RRP $34
From old bush vines dry grown and low yielding, which gives great concentration of flavour. Great varietal definition here, a radiant beetroot red colour, fragrant, lightly perfumed with rose petal and spice. For me this wine is for current drinking.
Mandoon 2022 Old Vine Shiraz, WA, RRP $34
Based on 1955 Swan Valley vines, this wine is a youthful crimson-purple colour with a spicy nose of blackcurrant and black pepper. Rich, round and supple flavours of black cherry and satsuma plum. A complete wine with a 10-12 year future.
Mandoon 2016 Reserve Sparkling, Margaret River, RRP $42
As a Champagne tragic I am hard to please with other sparkling wines, but I must admit this wine is very good. Made in the traditional method with Chardonnay from their cooler climate Karridale vineyard. A fine, concentrated and persistent bead immediately suggests a wine of quality.

Review by Dr Craig Drummond Master of
Mandoon 2021 Reserve Chardonnay, Margaret River, RRP $59
An excellent Chardonnay that shows the generosity of Margaret River with the cool climate touch of the southerly Karridale sub-region. Intense aromas, nice integration of pristine fruit, stone fruits and cashew from oak. Great current drinking with six to eight years ahead.
Mandoon 2021 Cabernet Sauvignon, Margaret River, RRP $36
A big Cab with a long future. Spicy, blackberry and cinnamon on the nose, and a cigar box ‘Bordeaux type’ oaky aroma. Flavours big and long of blackcurrant, green capsicum and menthol. Tannins fine, dusty and gripping with a firm acid finish. Very youthful with a 15-20 year future.
Mandoon 2024 Block 1985 Verdelho, Swan Valley RRP $34
A signature Swan Valley Verdelho and my favourite wine of this tasting. Appearance is deceptive, a light lemon almost water white, but certainly drinks like great wine. The fruity aromas leap from the glass with overt tropical pineapple and lime cordial, beautiful fruit salad with a tangy citrus after taste. A delightful wine, simple yet profound and another good wine to lay down in the cellar.

CONTACT
Cherie:
P: 08 9387 5000
E: offi ce@wfmp.com.au
Scan QR code for more details
FULL/PART-TIME VRGP
• Long Established
• Accredited/Teaching Practice
• GP Owned
• Well-Equipped Treatment Room
• Full-time RN support.

CONTACT
Practice Manager: P: 08 6165 2444
E: reception@comogp.com.au
Scan QR code for to email

BURSWOOD
CONTACT
Dr Ang:
P: 08 9472 9306
E: info@thewalkingp.com.au
Scan QR code for more details
• 75% of gross billings
• Accredited mixed-billing clinic
• Perfect for new VR GP’s
• Full/Part-time options.

CONTACT
Practice Manager Folu: P: 0435 800 320

CHURCHLANDS
CONTACT
Practice Manager:
Seeking a GP who can work regular full time or part time hours
• No after hours consulting
• Remuneration is negotiable.
• Well equipped treatment room.
• Pathology adjacent.
• Privately owned/Mixed billing.
• Friendly registered nurses and experienced administration support.
E: practicemanager@herdsmanmedical.com.au
Scan QR code for more details

BENNETT SPRINGS
CONTACT
Jasmine Brierty:
P: 0457 905 538
VR GP OPPORTUNITY
• Mixed Billing
• Waiting patient base
• Greater nursing support for CDM and procedures
• Division of Sonic Healthcare.
E: Jasmine.Brierty@ipn.com.au
Scan QR code for more details

JINDALEE
CONTACT
Jasmine Brierty:
P: 0457 905 538
Jindalee Medical Centre
Full or Part-time GP
• Flexible arrangement to suit lifestyle
• Private billing Mon-Fri practice
• On site pathology
• DPA approved location
• 12 consult rooms, treatment & procedure rooms.
E: Jasmine.Brierty@ipn.com.au
Scan QR code for more details
Opening for VR GP - F/time or P/time Full Private List Available
Unique opportunity to join our family orientated practice in one of Perth’s fastest-growing suburbs.
• FRACGP essential
• Up to 70% private billings
• Enjoy working for a doctor-owned, non-corporate, well support, and accredited practice.
FULL OR PART-TIME VR GP
• Busy mixed billing general practice
• Well established patient base
• Flexible working hours
• Nursing support
• Positive team environment
E: pmanager@parkwoodmc.com.au
Scan QR code for more details
Bunbury Family Doctors is owned by a local GP with a passion for patient-focused medicine. We foster a collaborative team environment with strong admin and clinical support. We believe happy doctors make healthier communities. You will be supported by our friendly administration team, nurses and onsite pathology.
We are a small independent clinic, accredited by RACGP, focusing on excellent patient care and GP wellbeing.
Enjoy working in a new purposebuilt general practice located in a prime position in South Bunbury. The clinic is close to specialists, pharmacies, pathology and radiology clinics. Bunbury Family Doctors is ideally located only a short drive to Perth or you can explore all that is on offer in the south-west region from wineries, beautiful beaches or scenic nature trails.
Private billing, strong admin support, full books and a 5-day roster – a place where GPs can do what they love and practice high-quality medicine whilst still maintaining a work/life balance.
CONTACT
Dr Brendan O’Dea:
P: 08 9778 5800
E: brendan@bunburyfamilydocors.com.au
W: www.bunburyfamilydoctors.com.au
Scan QR code for more details

Complete the self-reflection and claim your CPD time, please scan here YOU ASKED, WE DELIVERED: WE ARE NOW CPD VERIFIED



The ECU Health Service is seeking expressions of interest from vocationally registered general practitioners
15% service fee
Mixed billing
Free, reserved parking
Full time registered nurse support
Exceptional administrative support team
Best Practice Premier (Spectra)
Flexibility of four to six sessions per week.
Monday to Friday, 8.30am – 4.30pm.
No weekends or after-hours.
Located within the Wellbeing Precinct on the ECU Joondalup Campus, our AGPAL accredited, purpose-built general practice is on the same floor as the free student psychological services, the Living Room (a peer led support and guidance service), with a coffee shop and free reserved GP parking close by.



The ECU Health Service assists students, staff and the university community with their health care needs. The primary function of the service is to provide our students with accessible and affordable health care for the duration of their studies.
Students are charged the rebate fee or bulk billed, and staff and other patients are charged private commercial rates.
Applications are now open from candidates who have either Permanent Residency or Australian citizenship, unrestricted Medical Board of Australia registration and no Provider Number restrictions.
Please contact Laura Harnett – Practice Manager on telephone 0479 188 513 / 08 6304 5618 or email practicemanager@ecu.edu.au.




at 162 Cambridge St West Leederville (directly opposite SJOG Subiaco).
2 large fully fitted consults rooms (including sink and treatment bed) available and seperate treatment room available.
Each consult room $250 per half day session (includes use of waiting room and kitchen area). Reception/Admin support available for an additional fee. CONSULTING
For further information regarding availability or to arrange inspection please contact: reception@oswa.com.au/ (08) 9332 0066
Fully fitted including sink Includes use of waiting area, staffroom/kitchen
$250 per half day session
Reception/patient check-in support available for additional fee.
For further information or to arrange inspection please contact: admin@wocwexford.com.au















Partner with Australia’s largest independent practitioner network and experience freedom over your billings, appointment types, and clinic care.
Explore our WA GP vacancies






At Humphrey Homes, every home we design and build begins with listening. We take the time to understand your vision, your lifestyle and your budget - then shape that insight into thoughtful spaces that are beautifully crafted. By seamlessly integrating architecture, interior design and construction, we make creating your forever home harmonious, effortless and deeply personal.
To start the conversation, call Dean Humphrey on 9284 5444.
“Humphrey Homes delivered not just a house but a sanctuary that perfectly suits our family’s needs and lifestyle. We would not hesitate to work with them again and wholeheartedly recommend their services to others who value excellence, transparency, reliability, and a truly client-centric approach.”
- Angela and Amit, City Beach
