

Personal Health
2025 | A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content
“Smart stethoscopes and cheek swab tests promise faster heart condition diagnosis using AI and genetic insights.”
Dr Sonya Babu-Narayan, Clinical Director, British Heart Foundation Page 07

“In some parts of England, people can directly access enhanced primary eye care services at their local optical practices.”
Sarah Cant, Director of Policy and Strategy, The College of Optometrists Page 12

Women are less likely to receive help in a cardiac arrest
Time is critical during cardiac arrest, yet women remain less likely to receive CPR due to misplaced fears. These can be addressed through education and confidence.

WRITTEN BY Esther Kuku Director of Communications and Engagement, Resuscitation Council
When someone suffers a cardiac arrest, every second counts. Immediate CPR can more than double their chance of survival. A defibrillator, used within the first few minutes, can further raise the chances of survival. Yet, the problem is women are less likely to receive CPR or defibrillation in public than men — that needs to change.
Almost one in four people say they’d be less likely to help a woman than a man in cardiac arrest.
What’s holding people back from CPR?
According to a 2024 survey by St John Ambulance, almost one in four people say they’d be less likely to help a woman than a man in cardiac arrest. Common reasons include fear of causing harm, concern about inappropriate contact or
@Mediaplanet UK & IE
Project Manager: Matthew Kennedy matthew.kennedy@mediaplanet.com Business
being accused of touching someone inappropriately. Additionally, a review from the International Liaison Committee on Resuscitation (ILCOR) found growing evidence that concerns around exposing women’s chests or removing clothing to use a defibrillator may be stopping bystanders from stepping in. Modesty should never come before saving a life. In a cardiac arrest, hesitation driven by fear or doubt can cost precious time, and with it, a chance to survive.
Focus on the CPR facts
When someone needs CPR, the steps are the same for everyone, regardless of gender. You place the heel of one hand, with the other on top, in the centre of the chest and push hard and fast. If there is a defibrillator nearby, the ambulance service will tell you where to find it. The steps are simple — act fast, and don’t hesitate.
Building confidence is the solution
This isn’t about judgment; it’s about education. That’s why organisations like Resuscitation Council UK offer free, practical training that can give anyone the knowledge and confidence to help save a life. We believe a person’s chance of survival should never be determined by their gender.
Contact information: uk.info@mediaplanet.com or +44 (0) 203 642
Ollie Edmonds Strategic Sales Manager:
Junior Designer: Ellen Cahill Senior Content Manager: Angelica Hackett O’Toole | Paid Media Strategist: Jonni Asfaha Digital Lead: Henry Phillips | All images supplied by Getty Images, unless otherwise specified
Future-proofing the cardiology workforce with research training
Heart medicine relies heavily on research and innovation in bringing new treatments and life-saving procedures to patients with heart and circulatory diseases.

WRITTEN BY
Professor André Ng President, British Cardiovascular Society
In the UK, clinicians and academics have been at the forefront of international research. When I trained as a cardiologist, we were expected to take extra time to complete a research project and gain a higher degree before applying for a consultant post. This gave my colleagues and me skills that are difficult to achieve otherwise, including data analysis, scientific writing, the ability to appraise clinical evidence and the ability to communicate the findings effectively.
Balancing medical practice and research
Due to increasing emphasis on clinical and medical training and an expanded curriculum to cover a broad range of knowledge and skills, research training now seems to be under threat; trainees can finish training without completing a focused period of research. This risks the erosion of academic expertise amongst the clinical workforce and the ability to lead and deliver high-level clinical trials in future generations. We need to future-proof our workforce by equipping them with the necessary skills, so they are not only capable clinicians but also possess the critical mind and innovative perspectives necessary to ensure the delivery of excellent healthcare based on best evidence.
AI in cardiovascular care
Research training also has to incorporate AI, as there is good evidence that it can improve the quality and efficiency of cardiovascular care delivery in many areas. Good governance and ensuring the appropriate use of true and accurate data are vital so that the resulting technological tool provides effective and safe applications to improve patient care.
Clinicians of the next generation need to be involved now in AI development to shape and design the best use of these advances. The benefits of AI will support the new initiatives recently announced in the NHS 10-year Health Plan for England, targeting cardiovascular disease with a focus on prevention, early diagnosis and effective treatment.
Workforce plan for leadership
Underpinning the success of these initiatives will be a new workforce plan, which we hope will rebalance our training programmes, restoring the research elements so that the UK remains in a leading position in this vital field.
Anokhi Shah Managing Director: Ellie McGregor |
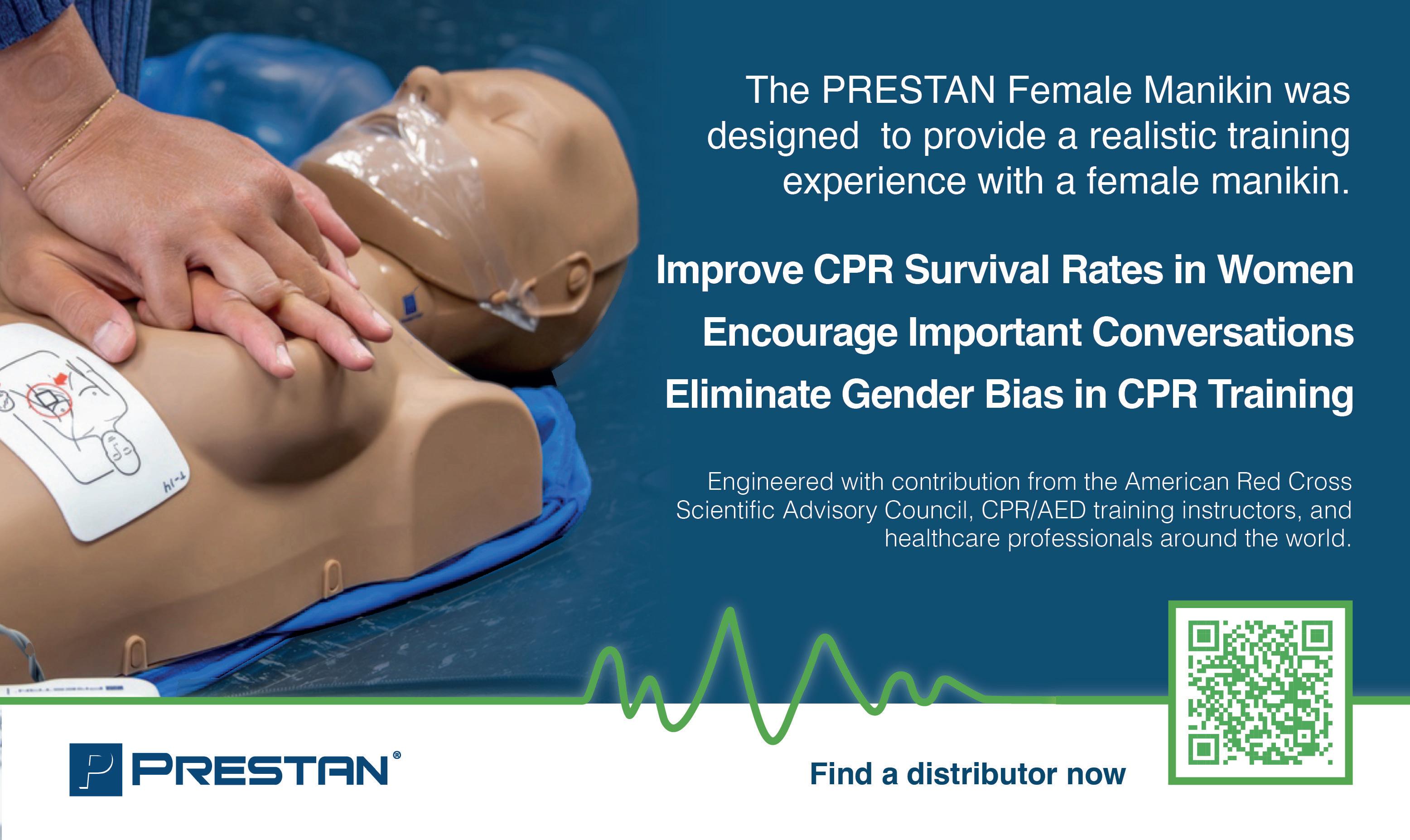
How gender-inclusive CPR training can save more women’s lives
Improve cardiopulmonary resuscitation (CPR) training with the right tools that can overcome gender barriers and enable life-saving CPR for women during cardiac emergencies.

Cardiovascular disease remains a leading cause of death for women worldwide. Yet, only 44% of women recognise it as their greatest health threat.1 More troubling, women are significantly less likely to receive bystander CPR than men — 39% compared to 45%. This gap translates into lives lost; men’s odds of surviving a cardiac arrest are 23% higher.2
CPR training awareness and readiness

These numbers represent mothers, daughters, sisters and friends whose chances of survival are diminished not by the severity of their condition alone but by inaction or hesitation. Deepseated fears and misconceptions — such as anxiety about inappropriate contact, causing harm or lack of awareness — often prevent timely intervention. CPR training is not just about technique; it is about building the readiness to save a life when every second counts.
Gender-inclusive tools in CPR training
Female Manikin was developed to help close this gap. It offers a realistic representation that encourages discussion, dispels myths and builds familiarity. Ed Feil, PRESTAN VP of Global Sales and Marketing, says: “This female manikin furthers that mission by ensuring our training tools reflect the diversity of real-life situations.”
For decades, CPR manikins have largely been designed to represent male anatomy, which means trainees often lack experience in practising on a female form.
For decades, CPR manikins have largely been designed to represent male anatomy, which means trainees often lack experience in practising on a female form. This can subconsciously reinforce uncertainty, further widening the gap in real-world response rates.
This is why gender-inclusive tools are an essential part of advancing equality in emergency response. The PRESTAN

Ensuring people are prepared to respond By integrating such tools into training, educators can address the specific fears and biases that lead to hesitation, ensuring every student is prepared to respond to anyone in need.
Aubi Nemeth, Owner and Instructor of Sixth City CPR, adds: “As CPR instructors, part of our responsibility is ensuring our students are fully equipped to act without hesitation. Having a manikin with breasts is a vital step in removing the biases that have existed in CPR training for too long.”
When CPR training reflects the diversity of the people it aims to protect, we stand a greater chance of closing survival gaps and ensuring that lifesaving skills reach those who need them most.
References
1. American Heart Association. 2020. Heart disease awareness decline spotlights urgency to reach younger women and women of color.
2. American Heart Association. 2020. Women need CPR too.
Dr Aubi Nemeth, DNAP, CRNA
Owner and Instructor, Sixth City CPR
WRITTEN BY
Ed Feil
VP Global Sales and Marketing, PRESTAN
Personalised health guidance based on individual biomarkers promotes longevity
Health technology company uses metabolic signatures and predictive health biomarkers to enhance user longevity, delivering personalised recommendations tailored to each user’s individual health data.

The concept of longevity is rapidly transitioning from a niche of the wellness industry to a global public health priority. This transition comes in light of ongoing healthcare challenges, namely an ageing population and the persistent rise in rates of cardiovascular disease. Increasingly, research suggests that ageing is a modifiable process, rather than a simple biological event, shifting the focus from increasing your ‘lifespan’ to enhancing your ‘healthspan.’


“Longevity isn’t a fad; it is about adding years to your life and, more importantly, adding quality to those years,” explains Marius Ronnov, Co-Founder and CEO of Hume Health LLC. “Longevity is the compounding effect of good decisions which allow you to live a longer and better life.”
Why access to the right health data matters for longevity Longevity is no longer just luck of the draw; modern approaches emphasise the importance of prevention and tracking. Harnessing your health data has emerged as an important factor in supporting healthy ageing, building resilience and staying ahead of time. However, health data has long been disconnected, limiting the potential for meaningful change.
Data without context is like looking at your body in black and white. When combined and interpreted correctly, you can see it in full colour.
“The way people monitor their health today is fragmented. One app tracks calories, another tracks activity, and medical results live somewhere else, meaning the compounding value of that data is lost,” he explains. “By centralising and simplifying all of those pieces of data into clear and actionable insights, people can unlock the full potential of their health data to drive meaningful improvements.”
He aptly describes: “Data without context is like looking at your body in black and white. When combined and interpreted correctly, you can see it in full colour.”
Changing your ageing trajectory

Research shows that the ‘trajectory of ageing’ is a dynamic process, one that can be influenced by behavioural choices and lifestyle interventions. By analysing daily metabolic biomarkers alongside periodic body composition measures, new technology can help reveal both positive trends and early risk signals.
“One of the most powerful predictors we can now track is cardiovascular recovery, which shows how quickly the heart returns to baseline after stress,” continues Ronnov. “Alongside this, we can measure body composition over time, helping people maintain and build muscle mass while reducing harmful fat. By layering these different metrics with metabolic metrics, we are making health both measurable and actionable.”
By converting these signals into specific guidance on sleep, recovery and activity, health technology has the ability to help people connect daily behaviour with long-term outcomes and ageing.
Metabolic signatures and predictive analytics
Metabolic signatures refer to patterns in your body’s metabolism which provide a comprehensive blueprint of your metabolic health. Insights from metabolic signatures are now being used to uncover potential future health risks and guide personalised interventions.
“We take signals from biometrics, interpret them and translate that into insights and recommendations based on each person’s individual goals,” explains Ronnov. “Instead of just providing one snapshot in time, we are able to provide people with an understanding of their overall wellbeing and potential future health risks.”
Created on the principle that people should have ownership of their health outcomes, Ronnov’s novel and sophisticated approach to utilising metabolic signatures and predictive health markers is making metabolic health visible and actionable for consumers.
Building on the above, Hume Health introduces two core metrics: Metabolic Capacity, which reflects the body’s ability to perform and recover on a daily basis, and Metabolic Momentum. Metabolic Momentum provides a way to visualise the trajectory of ageing. Rather than treating health as a fixed state, people can see whether they’re trending upward, plateauing or declining.
Observed over time, these signals illustrate how incremental changes in recovery, sleep and body composition accumulate into meaningful shifts in long-term health.
INTERVIEW WITH Marius Ronnov Co-Founder and CEO, Hume Health
INTERVIEW WITH Dr Sharifah Halimah Jaafar, MD Medical Advisor to Hume Health
WRITTEN BY Bethany Cooper

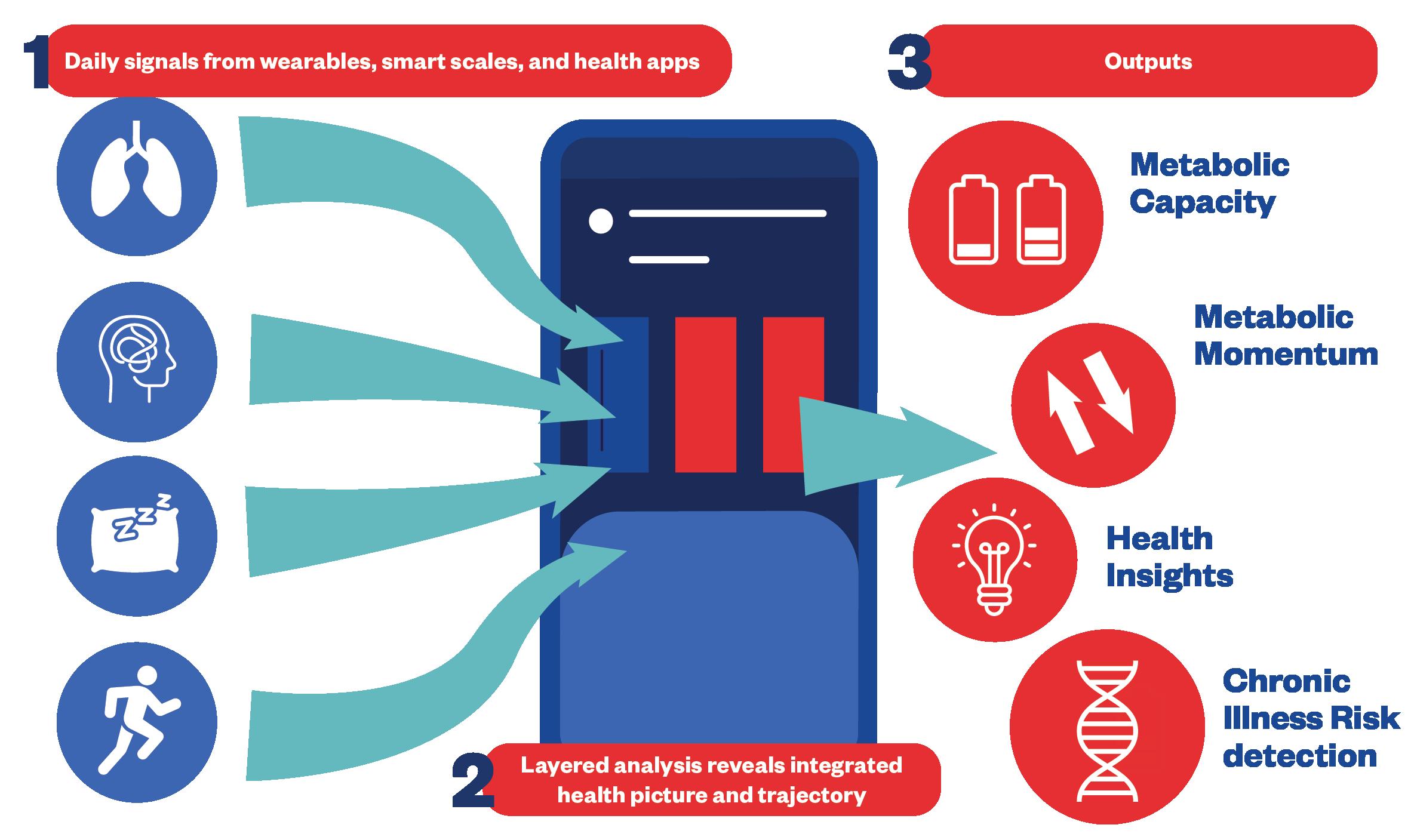
Guiding you from morning to evening
Each day, Hume users receive recommendations for balancing recovery and exertion in line with current Metabolic Capacity, a daily threshold informed by recent performance and recovery trends. As simple as taking a short walk, prioritising hydration or going to bed 20 minutes earlier, behavioural recommendations are built to fit naturally into your routine and evolve with you day by day.
Every week, your health score and metabolic momentum aggregate your progress, giving a clear picture of your overall health and trajectory beyond natural day-to-day variability.
Senior Consultant Dr Sharifah Halimah Jaafar explains: “The most valuable insights come from how health markers change together over time. By tracking body composition, cardiovascular recovery and metabolic health as a whole, we can spot early signs of how a person is ageing. Recognising these shifts and linking them to small changes in sleep, nutrition or activity can lower the risk of chronic disease, build resilience and extend years of good health.”
The science behind behaviour change
Clinical terminology can often feel inaccessible, something Ronnov himself experienced after having a stroke in his late 20s. “People typically come to us because they want to change something specific — be it their weight, their health or help with managing a chronic condition,” he says.
“We use plain language, clear visuals and easy-tounderstand scores, showing the whole picture and actionable steps towards their personal goals. People are able to make gradual improvements and notice meaningful benefits in their daily lives.”
He continues: “Knowledge alone doesn’t change behaviour. That’s why we have built our technology around the concept of behavioural science, with an easy-to-use interface. We use microhabits and impact loops that fit seamlessly into everyday life.”
Real-world impact
With a substantial user base of over 3 million people, Hume Health has built a community of users who are in it for the long haul, motivated through the tangible reward of milestones achieved and measurable health progress. “Our technology shows you progress before you even notice it, whether it’s steadier energy, better sleep or improved recovery,” explains Ronnov. Personalised health means no two experiences are identical, but many users see changes within weeks, with further measurable and compounded
improvements appearing throughout ongoing use.
“Prevention is more powerful than reaction, and small daily decisions compound into a longer, healthier life,” says Ronnov. Early changes often include cardiovascular recovery, meaning how quickly your heart returns to baseline after stress — one of the strongest predictors of long-term healthspan.
Many users see that curve shortening, meaning their body is bouncing back faster, with more overall resilience. Within six weeks, most users begin to show measurable improvements in body composition, muscle mass and fat reduction. By six months, more than 80% of active users have demonstrated improvements in markers associated with physiological ageing, meaning stronger cardiovascular health, better metabolic flexibility and a younger physiological age than when they started their journey.
Based on first party platform data; individual results may vary.
A metabolic health ecosystem
At the centre of Hume’s system is the app. Inputs are aggregated from a user’s devices, including Hume’s own BodyPod and Band — precise body composition readings and continuous monitoring of cardiovascular, respiratory, sleep and activity signals.
The software unifies these signals into a single health profile, smoothing out inconsistencies and applying AI trained on longevity and behavioural science.
Individualised metrics include Metabolic Capacity for daily guidance on recovery and exertion, alongside Metabolic Momentum for tracking longer-term trajectories.
Hume’s Chronic Illness Risk Detection provides a wellness insight that flags deviations associated with cardiovascular strain, inflammatory triggers and immune system shifts that may be signs of long-term health risks. Individual patterns in behaviour and physiological response inform personalised and actionable recommendations designed to compound into sustained health improvements.
The ecosystem transforms fragmented information into clear, actionable insights — helping make healthy ageing both measurable and accessible.
“We want to be at the centre of the conversation for longevity, not solely focused on extreme interventions or healthcare professional involvement, but reminding everyday people that they can take control of their health and wellbeing,” concludes Ronnov. “We are giving people a platform to access data-driven health guidance, empowering them to be better — for themselves and their families.”
DISCLAIMER:
Hume Health provides general wellness recommendations and is not intended to diagnose, treat, cure, or prevent any disease. Individual results may vary. Users should consult a healthcare professional before making significant changes to their health routines.
Know your pulse to know your heart rhythm — it could save your life
Over 1.6 million people in the UK are diagnosed with atrial fibrillation (AF). Another 500,000 have yet to be diagnosed. Living with AF increases your risk of stroke.

Without a diagnosis, you are at high risk of an AF-related stroke, which is often fatal. Yet, how many people realise that it is as important to know that your heart is in rhythm as it is to know your heart rate?
The sooner you detect and seek a diagnosis, the greater the chance of receiving anticoagulation therapy to reduce the risk
of AF-related stroke .
AF-related stroke
A deadly cause of stroke is atrial fibrillation – the most common irregular heart rhythm disorder (arrhythmia). AF is so simple to detect. A manual pulse check or use of the latest apps on your watch or mobile phone can detect

Lan irregular heart rhythm. The sooner you detect and seek a diagnosis, the greater the chance of receiving anticoagulation therapy to reduce the risk of AF-related stroke.
Pulse field ablation
It is also important to be aware of and access the latest treatment options. Most recently, NICE have approved Pulse Field Ablation (PFA), which, in studies, has proven to have the greatest success rates for people with an early diagnosis following the onset of AF and speedy PFA treatment. PFA can be performed under local sedation, takes less time than regular ablation techniques, and for many, they can return home the same day. Less time in hospital saves costs to the NHS. Importantly, early treatment with PFA has shown that for many, their hearts are restored to a normal rhythm, and they can lead active lives once again without the fear of AF-related stroke, heart failure and other side effects of AF.
Know Your Pulse to Know Your Heart Rhythm – it could save your life. www.knowyourpulse.org www.afa-international.org www.heartrhythmalliance.org
Photon-counting CT scanners are revolutionising heart diagnostics
The latest computed tomography (CT) scanning technology offers cutting-edge diagnostics to heart patients, allowing doctors to see tiny moving structures in vivid high-resolution.
ondon’s Royal Brompton Hospital, part of Guy’s and St Thomas’ NHS Foundation Trust, is the UK’s largest specialist heart and lung centre and consistently takes a pioneering approach to medical technology. It’s why Dr Thomas Semple wanted to work there.
As a consultant radiologist at the hospital for the last seven years, he has expertise in imaging of heart and lung conditions from newborns to adults. “The hospital has been an early adopter of cutting-edge cardiac technology for longer than I’ve been in medicine,” he says. “For instance, it’s been using state-of-the-art cardiac CT scanners since the 1990s.”
Pioneering photon-counting CT scanners
A cardiac CT scan is an imaging test that creates high-resolution images of coronary arteries and other heart structures. Scans are non-invasive, safe, quick and can be done on an outpatient basis. Recently, Royal Brompton’s scanning capabilities took a quantum leap forward with the introduction of Siemens’ NAEOTOM Alpha CT scanner — the only one of its kind in London, based at 79 Wimpole Street Consulting Rooms and Diagnostic Centre, and the first in private practice in the UK.
As the world’s first commercially available photon-counting CT scanner, it creates extraordinarily high-resolution images in a fraction of
a second, allowing experts to analyse the heart and coronary arteries in vivid detail at a low radiation dose.
Detailed images reduce the need for additional testing
“Even with high-end conventional CT scanners, it can be difficult to see small vessels through small coronary stents or around heavily calcified coronary disease,” says Dr Semple. “None of that is an issue with our photon-counting scanner. It’s been likened to moving from a traditional Polaroid camera to a modern digital single-lens reflex camera.”
As the hospitals’ clinicians can more confidently diagnose with a single scan, this new technology reduces the need for additional testing. “It allows us to more confidently determine what is a significant disease that needs treating,” says Dr Semple. “With the right scan done by the right team at the right time, it’s likely to be the only test needed to guide decisions” and can be used in many other areas of medicine too.
A revolutionary change in health imaging For Dr Semple, it’s an exciting development — and proof that Royal Brompton remains at the forefront of heart health for people of all ages. “We were already pushing the boundaries with conventional scanners,” he says. “This new technology will allow us to go even further.”

INTERVIEW WITH Dr Thomas Semple Consultant Radiologist, Royal Brompton Hospital, part of Guy’s and St Thomas’ NHS Foundation Trust
WRITTEN BY
Trudie Lobban MBE Founder & CEO, Arrhythmia Alliance and AF Association
Paid for by Royal Brompton and Harefield
WRITTEN BY Tony Greenway

Testing for heart conditions in seconds
Cutting-edge technology promises faster diagnosis of heart conditions using smart stethoscopes and cheek swab tests to detect heart failure and arrhythmogenic cardiomyopathy (ACM) early.
Anew version of the humble stethoscope, first invented more than 200 years ago, can boost the diagnosis of heart problems, while a cheek swab can flag a heart condition in children. The findings, presented at the recent European Society of Cardiology Congress, were made possible by the support of the British Heart Foundation and thanks to the generosity of the public.
A test result in just 15 seconds with a smart stethoscope
People visiting their GP with symptoms like fatigue and breathlessness could benefit from a 15-second examination with a ‘smart’ stethoscope. Smart stethoscopes record sounds in the chest and the heart’s electrical activity, and then use artificial intelligence to analyse the readings.
Researchers at Imperial College London, led by Professor Nicholas Peters, found patients examined using a smart stethoscope were twice as likely to be diagnosed with heart failure, in a study involving more than 200 GP surgeries. The stethoscope also helped to detect atrial fibrillation and heart valve disease.
Patients with abnormal readings could more quickly be started on treatment and sent for heart tests to confirm if they have a heart condition. If smart stethoscopes can provide earlier diagnosis, that could mean fewer people finding out they have heart conditions for the first time after being rushed to A&E.
Painless cheek swabs take two minutes
A cheek swab test, being developed with BHF funding, could diagnose a dangerous heart condition in children earlier. ACM is responsible for more than 10% of sudden cardiac deaths in children.1 It involves abnormalities in proteins within the heart, which are mirrored in the lining of the cheeks.
Researchers at City St George’s, University of London, led by Dr Angeliki Asimaki, and Great Ormond Street Hospital, recruited 51 young people with a known genetic predisposition to ACM. Among 10 who went on to develop the heart condition, eight showed abnormalities in a cheek swab before changes appeared in other medical tests.
The swab test could identify children in the early stages of ACM who might need extra monitoring and treatment, while providing reassurance to other at-risk children and their families.
Reference: 1. Cohen, M and Atkins MB. 2022. Arrhythmogenic right ventricular cardiomyopathy in the pediatric population. Current opinion in cardiology vol. 37,1 (2022): 99-108. doi:10.1097/ HCO.0000000000000937.
Why TAVI could be the best option for aortic stenosis patients
After being diagnosed with a life-threatening heart condition, Thomas Farmer had a quick and painless procedure known as transcatheter aortic valve implantation (TAVI). According to him, the results have been nothing short of ‘incredible.’

Thomas says he found out about his heart problem by accident. It happened around two years ago when he visited A&E after a fall, and an examination picked up a heart murmur. “I was given an echocardiogram,” remembers Thomas, now 77.
Aortic stenosis diagnosis
After being referred to a cardiologist at Royal Stoke University Hospital for more tests, his aortic valve was shown to be severely calcified. This is known as aortic stenosis, which can restrict the flow of blood from the heart to the rest of the body. A common symptom of aortic stenosis is shortness of breath on exertion. Thomas, a retired builder, had spent his working life climbing up and down scaffolding without a second thought — but recently, he’d been getting out of breath walking up stairs. Now, it was clear why.
“I hadn’t heard of the condition before,” he says. “But I’m fairly laid back, so my question to the cardiologist was: ‘What shall we do now?’”
After the
TAVI procedure, he was given a check over, and the consultant discharged him that afternoon.
The benefits of a TAVI procedure
There were two options. Thomas could have open heart surgery to replace the valve or a procedure
called transcatheter aortic valve implantation (TAVI). While open heart surgery is a major operation, TAVI is much less invasive and involves the insertion of a new replacement valve into the heart using a small tube via the main blood vessel in the top of the leg. “It was suggested that TAVI would be the best, simplest option [for me]*,” says Thomas.
Thomas was awake throughout the procedure, which took around 90 minutes. “It was incredible,” he says.
“I was listening to the [cardiologists] talking about what they were doing and found it fascinating. I felt no pain whatsoever.” He’s also full of praise for the staff at Royal Stoke.
“They were all fantastic, from the porters to the assessment nurses to the [cardiologists],” he says.
Recovery and life after TAVI
After the TAVI procedure, he was given a check over, and the consultant discharged him that afternoon. Recuperation at home took a further 24 hours. Thomas has now planned a holiday with his partner. “I feel fine,” he says. “We had to cancel one holiday because of the operation, so we’ve rebooked, and we’re going to Tenerife. My advice to anyone in a similar situation is: ‘Go for it. Have TAVI.’”
*Disclaimer: Doctors should follow the latest national and international guidelines to select the most appropriate treatment for their patients.
WRITTEN BY
Dr Sonya BabuNarayan Consultant Cardiologist and Clinical Director, British Heart Foundation
INTERVIEW WITH Thomas Farmer Patient with aortic stenosis
WRITTEN BY Tony Greenway

Pain management in the UK’s ageing population
With rising expectancy, older adults encounter more complex pain conditions, often compounded by multimorbidity and cognitive changes, demanding careful consideration of medicines, interventions, side effects and patient experiences.
The UK population aged 65 and over is projected to rise to 27% by 2072 (ONS, 2025), with increasing social and healthcare challenges. Chronic pain rises substantially in this population, often alongside multimorbidity (Bokerman et al, 2024). Many older adults face not only pain but also limitations in mobility, social participation and independence. Age-related changes, including slower information processing and sensory impairments, make pain assessment challenging (Schofield, 2018).
Non-drug interventions can benefit older people with chronic pain.
Pharmacological challenges in older adults
Managing pain in older adults is complex. Long-term use of common analgesics, such as paracetamol, are now being questioned (Ahmed, 2023). Pain relief and other medicines used for pain management must be prescribed cautiously; while opioids carry risks (confusion, falls and constipation), though addiction is less of a concern than in younger populations.
The principle ‘start low and go slow’ is key: alongside careful assessment, monitoring and the shortest possible duration for all medicines, especially for those with cognitive impairment. Recent initiatives, such as the NIHRfunded HOPE-AO project, aim to address the risks of analgesic overprescribing in older adults. Given these diverse needs of older adults, alternative interventions
are part of a comprehensive pain management strategy.
Non-pharmacological approaches
Non-drug interventions can benefit older people with chronic pain, including acupuncture, relaxation, exercise, music therapy, TENS, hydrotherapy and massage (Anderson et al, 2018). Technologybased self-management and peer support have gained traction, particularly since the Covid-19 pandemic (Reid et al, 2018). These approaches may not be suitable for individuals with cognitive impairment or those unable to engage.
Family members often play a key role in supporting engagement and monitoring responses. Patient and professional beliefs also influence outcomes, highlighting the need for continuous education in geriatric pain care.
Lived experience insights
At the heart of holistic pain management are patients’ experiences. Older adults in our current NIHR study share:
• Victoria says: “Long-term pain affects every part of my life, with once-simple tasks now draining more energy.”
• Ann feels dismissed when told, ‘It’s your age,’ believing proper advice could help her live fully.
• Carer Roger highlights the complexity of managing medications.
• Isabella worries about interactions, dizziness, fatigue and constipation from new prescriptions.
This highlights that effective pain management must remain personalised and person-centred, integrating research, clinical expertise and lived experience to meet the complex needs of older adults.
How complex regional pain syndrome exposes the chronic pain gap

Complex regional pain syndrome (CRPS) is a little-known chronic pain condition. Its story shows why patients need better recognition, support and change.
The agony of CRPS
CRPS is a rare but devastating chronic pain condition, often triggered by a minor injury, that causes excruciating, disproportionate limb pain far beyond what the initial harm should cause1. CRPS is widely considered one of the most painful conditions known2. Yet, it is often misdiagnosed or overlooked due to low awareness among health professionals. There is no quick fix, and even advanced treatments often only offer partial relief.
The chronic pain crisis
CRPS is one dramatic example of a broader crisis. Chronic pain affects an estimated 28 million people in the UK3 This widespread issue carries an economic burden, costing around £10 billion annually4. The human toll is alarming: 16% of people with chronic pain say their pain is so bad they sometimes want to die 5, and about a quarter have been forced to stop working because of it5
Yet, chronic pain remains under-recognised and underresourced, being only recently classified as a condition in its own right5. In addition to this, it still receives only a tiny fraction of research funding4. Meanwhile, pain services are overstretched with long waits and patchy access to care.
Uniting voices for change
Addressing this crisis requires advocacy and policy action. Pain UK, a national umbrella charity, unites over 40 organisations to amplify patients’ voices6. It raises awareness and pushes for better care and patient rights, and its mission is that no one living in pain should suffer in silence7
To that end, Pain UK has proposed a national Chronic Pain Charter — a pledge that health providers will ‘listen, believe, diagnose and treat’ people in pain7. Pain UK also urges the Government to recognise chronic pain as a disability, as well as improve access to benefits and workplace support7
As a society, we must no longer marginalise those living with chronic pain. Millions of people need us to believe them, support them and invest in solutions. By uniting voices and demanding action, from funding pain research to expanding specialist services, we can bring hope and a better quality of life to those affected by chronic pain.

WRITTEN BY
Dr Margaret Dunham Chair of the Pain in Older People Special Interest Group of the British Pain Society
WRITTEN BY Ashley I. Simpson Consultant Peripheral Nerve Surgeon, Trustee and Chair of the Clinical Advisory Board, Pain UK
Tackling the scourge of joint pain for the over-55s
Joint pain often strikes people just as they are seeking to remain active as they enter their older years.

Joint pain is a major issue within an ageing population and one that adds to the burden on an already overstretched health service in the UK. Its onset often comes among people aged 55 and upwards at a time when they still want to remain active into their later years by exercising and maintaining a good level of mobility.
However, pain in the back, shoulder, hips, knees and elbows can hinder this.
The Consumer Healthcare Association (PAGB) Self-Care Census 2024 indicated, for example, that 10% of all GP appointments relate to backache.
Joint pain interventions
There are over-the-counter solutions that can help people stay fit, healthy and mobile and reduce the need to see a doctor. Philip Lindsell, Flarin Holdings Managing Director, explains that living with persistent joint and muscular pain goes far beyond physical discomfort.
Reducing NHS pressures
According to Lindsell: “At Flarin, we believe that by helping to ease pain through our patented formulation, we can make a real difference — supporting people not just to manage their symptoms, but to stay active, reduce disruption to their daily lives, and live more fully.”
The analgesic Flarin is aimed at the 55+ market, as that demographic tends to suffer increasing levels of joint and muscular pain. However, he says market research, supported by anecdotal evidence, indicates that there are also significant numbers of younger users, such as those who are active in sport or suffer work-related pain.
Living with persistent joint and muscular pain goes far beyond physical discomfort.
“It can lead to an emotional burden, more GP and NHS visits, increased sick days at work and difficulties with everyday tasks,” he says. “For many, this can have a huge impact on quality of life and independence. Increased self-care can eliminate the need for a doctor visit, reducing pressure on the NHS and also saving patients’ time and enabling them to treat their pain more quickly.”

Relief from pain and inflammation
Flarin is an oral painkiller, based on a lipid formulation of ibuprofen, which is absorbed in the small intestine and can be taken continuously for up to 10 days, with or without food and without consulting a doctor.
Lindsell says that in a clinical trial, it was shown to be as effective as twice the dose of standard ibuprofen and gives patients ‘powerful relief from pain and inflammation.’ Flarin is widely available in supermarkets, pharmacies and online.





POWERFUL RELIEF FROM JOINT PAIN & INFLAMMATION

INTERVIEW WITH Philip Lindsell Managing Director, Flarin Holdings
WRITTEN BY
Mark Nicholls
Stop waiting for failure: rethinking osteoporosis identification and care
Pilot shows that osteoporosis can be identified before a fracture, saving pain and suffering.
Osteoporosis, defined as low bone density, impacts one in three women and one in five men over 50.1 Sufferers risk broken bones from minor trips or falls, and for most, this is the first time they become aware of their condition. Many suffer multiple fractures before receiving a diagnosis and treatment, risking painful recoveries and a loss of independence.
Waiting for failure is failing patients
Medical journalist and osteoporosis sufferer, Dr Sarah Jarvis MBE, describes this as ‘waiting for failure’ — something that would be unthinkable for other conditions. We don’t wait for a heart attack before treating high blood pressure. Why wait for a broken hip before addressing fragile bones?
Things are beginning to change
Royal Cornwall Hospitals Trust is piloting DensityScan, a new tool which automatically assesses bone health during a routine X-ray.
The software, developed by North Eastbased IBEX Innovations and delivered through Agfa Radiology Solutions, is already having an impact. Osteoporosis Lead Penny Lewis commented: “Whatever the outcome, patients benefit, whether it’s reassurance that their bones are normal or early treatment and advice if they’re at risk. Either way, they get personalised care sooner.”
In a recent example, a patient was identified to be at a very high risk of fracture. The patient did not display any outward signs of osteoporosis and had not previously suffered a fracture. Lewis and the Fracture Liaison Service she leads were able to confirm the patient’s osteoporosis and begin a course of treatment to lower her risk of fracture.
Personalised, risk-based care
The Cornwall pilot shows how personalised medicine can improve osteoporosis care. Instead of reacting to a fracture, patients can be proactively assessed and offered earlier, tailored support. For some, this may be simple lifestyle changes. For more severe cases, Lewis notes: “New guidelines give us clear treatment options, and DensityScan allows us to spot the people who need them most, before they suffer the consequences of this silent disease.”
Reference:
1.https://www.osteoporosis.foundation/facts-statistics/epidemiologyof-osteoporosis-and-fragility-fractures#:~:text=Worldwide%2C%20 1%20in%203%20women,669%2D74.

Five steps to stronger bones at any age

Around 3.5 million people in the UK have osteoporosis,1 a condition that weakens bones and makes them more likely to break.
By the age of 50, one in two women and one in five men will experience a broken bone (also referred to as a fracture) because of osteoporosis.2 While the statistics sound daunting, there’s plenty we can do to protect our bones — at any age.
1. Know your risk of osteoporosis
The first step is awareness. Genetics play a role; if one of your parents has broken a hip, your chances of developing osteoporosis increase. Women are also at higher risk after menopause, when falling oestrogen levels accelerate bone loss.
Certain medications, including some forms of steroids, anti-epileptic medications and breast cancer treatments, can also contribute. To help, the Royal Osteoporosis Society (ROS) has a free online osteoporosis risk checker on their website that offers tailored advice and practical tips on looking after your bones.
A balanced diet is the foundation of bone health.
3. Eat for your bones
A balanced diet is the foundation of bone health. Calcium and vitamin D are vital, but so are a wide range of nutrients. Aim for a healthy, balanced diet with plenty of fruit and vegetables, carbohydrates, dairy or fortified alternatives and protein sources like meat, beans, fish and eggs. A varied plate supports bones as well as overall wellbeing.
4. Exercise smartly
Experts recommend at least two and a half hours of moderate-intensity aerobic activity every week. Weight-bearing with impact exercise (such as jogging or racket sports) is particularly important for preventing osteoporosis, combined with musclestrengthening activities like lifting weights or using resistance bands.
5. Choose bone-friendly habits
Smoking and heavy drinking both weaken bones and increase the risk of falls. Quitting smoking starts to restore bone health, and sticking to alcohol guidelines lowers your risk further. People with osteoporosis risk factors or a low calcium intake should also limit their caffeine consumption, since a high caffeine diet increases the amount of calcium you lose.
Strong bones are built over a lifetime, so it’s never too early — or too late — to take action.
References:
Paul Scott CEO,

2. Top up your vitamin D
Vitamin D helps your body absorb calcium, which keeps your bones strong. From April to September, 10 minutes of daily sun exposure is usually enough. Between the end of September and the start of April, most of us need a daily supplement of 10 micrograms (400 IU). Those with limited sun exposure should consider a vitamin D supplement year-round.

International Osteoporosis Foundation. 2019. Broken bones, broken lives: A roadmap to solve the fragility fracture crisis in the United Kingdom.
Regular eye checks detect diseases early and prevent sight loss
Regular eye tests can help prevent avoidable sight loss and detect serious health conditions like dementia, diabetes and heart disease — helping you live healthier for longer.

Average life expectancy in the UK is 81 years. However, figures from the Office for National Statistics (ONS) reveal healthy life expectancy is just 62 years.1 Taking good care of your eyes could prevent ill health and help us all live well for longer. Your eyesight doesn’t just affect how you cope with dayto-day tasks like driving or reading the news; there’s a strong link between vision and your mental and physical health, too. In fact, as many as one in five dementia cases are directly linked to eyesight issues.2
Eye tests are essential health checks
Poor eyesight is not inevitable. As much as half of all sight loss is actually avoidable.3 Regular eye tests are essential check-ups for everyone. They do more than simply test visual acuity; they detect eye disease early, helping to prevent future avoidable sight loss, and can spot markers for a host of serious health conditions, including cardiovascular disease, stroke, diabetes, hypertension and dementia.
know a sight test can detect conditions such as heart disease or Alzheimer’s, and worryingly, fewer than half (48%) realise optometrists (opticians) can diagnose age-related macular degeneration — the UK’s leading cause of blindness.
Life-saving optometrist referrals
Following a sight test, optometrists can direct people to get the help they need for a wide range of illnesses. This could be a potential life-saver for the 400,000 adults in the UK estimated to be living with undiagnosed heart failure and 88,000 people living with undetected brain tumours.5
Following a sight test, optometrists can direct people to get the help they need for a wide range of illnesses.
Poor health literacy is a barrier to testing Yet, four in 10 of us fail to have our eyes checked regularly (once every two years).4 Lack of awareness about the role sight tests play in keeping us healthy is doubtless a driver for this low uptake.
Research conducted by Eye Health UK found just one in 10
Lifestyle matters
In addition to routine sight tests, adopting healthy lifestyle habits can also help keep your eyes healthy. This includes protecting your eyes from sun damage whenever UV levels rise to three or more, eating healthily and staying active. Limiting screen time and spending time outdoors are also important, especially for children.
References:
1. Office for National Statistics (ONS), released 12 December 2024, ONS website, statistical bulletin, Healthy life expectancy in England and Wales: between 2011 to 2013 and 2021 to 2023
2. https://jamanetwork.com/journals/jamaophthalmology
3. Deloitte Access Economics (2017) Incidence and risk of sight loss and blindness in the UK Royal National Institute of Blind People.
4. Eye Health UK.
5. Heart Failure estimate = British Society for Heart Failure 2024. Source for Brain Tumour estimate The Brain Tumour Charity.

Chronic pain remains under-recognised and under resourced, being only recently classified as a condition in its own right.
~Ashley I. Simpson, Consultant Peripheral Nerve Surgeon, Trustee and Chair of the Clinical Advisory Board, Pain UK
David Cartwright Chair, Eye Health UK
Magnification: potential key to independence for people with low vision
Eye care professionals can transform lives by introducing the power of magnification — restoring independence, confidence and connection.
For many older adults, conditions such as macular degeneration, diabetic retinopathy or glaucoma mean standard optical correction is no longer enough. At this stage, magnification — enlarging and enhancing what remains visible — can be lifechanging. Rather than attempting to ‘correct’ what the eye can no longer see, magnification works with existing vision to make the world clearer, sharper and more accessible.
The power of modern magnification
Today’s low-vision solutions go far beyond simple magnifying glasses. Digital magnifiers can enhance contrast, sharpen images and offer viewing modes tailored to the user’s comfort. Portable devices make it easy to read menus, price labels or timetables while out and about. Desktop systems provide crisp, high-contrast text for books, newspapers and mail, with adjustable zoom for effortless reading. For advanced vision loss, text-to-speech technology can instantly read aloud printed material — ensuring no information is out of reach.
Restoring daily independence Magnification supports much more than reading. It can make cooking safer, medication easier to manage, hobbies more enjoyable and even enable people to continue working. Distance cameras, for example, can bring the TV screen from across the room closer to the eye, making television viewing more comfortable. For caregivers, these tools offer peace of mind — knowing their loved one can keep enjoying daily routines and cherished hobbies without constant assistance. By matching the right device to the individual’s needs and lifestyle, eye care professionals and community partners can help restore not just sight, but self-confidence. Introducing these tools early — before frustration sets in — can preserve independence and quality of life.
Alan Davis, General Sales Manager, HumanWare, says: “Magnification is not just about making things bigger; it’s about giving people back the ability to engage fully with their lives. The right solution can turn frustration into confidence, and isolation into independence.”
Low-vision technology pioneers HumanWare has been pioneering low-vision technology for more than 35 years. Its range spans handheld magnifiers, advanced desktop systems and wearable solutions — all designed with input from users and clinicians. The mission: help people with vision loss see possibilities, not limitations.

Expanding community eye care as part of the 10 Year Health Plan for England

The Government’s 10 Year Health Plan for England rightly prioritises preventative, community-based care to improve patients’ outcomes and cut waiting times.
The College of Optometrists welcomes the Government’s 10 Year Health Plan. Ophthalmology is the NHS’s busiest outpatient specialty, with nearly 9 million appointments annually and long hospital wait lists that lead to unnecessary sight loss. Bringing more eye care earlier and closer to home is vital.
Role of optometrists in the community
Optometrists — eye care professionals who perform eye tests, prescribe glasses and diagnose and manage a variety of eye conditions — are well-placed to deliver the aims of the 10 Year Health Plan. High street optical practices often offer extended hours and weekend access in the heart of communities — already meeting the Government’s aims for neighbourhood health services.
To make the ambitions of the Government’s Health Plan a reality in England, enhanced community eye care services must be expanded.
In some parts of England, people can directly access enhanced primary eye care services at their local optical practices. These include urgent care for sudden (acute) eye conditions, pre and post-cataract care and glaucoma referral, filtering and management. These services support earlier intervention and avoid unnecessary GP and

hospital appointments.
Need for urgent eye care services
Evidence from evaluations of existing community-based urgent eye care schemes found that, up to 97% of acute eye cases are resolved by optometrists without hospital referral. Today, 70% of eye problems presenting to emergency departments could be managed in primary eye care.
However, despite their proven benefits, these urgent eye care services are not yet available across England. Even where services exist, public awareness that they can visit their optometrist for urgent care is limited.
England eye care must catch up
To make the ambitions of the Government’s Health Plan a reality in England, enhanced community eye care services must be expanded, funded and rolled out across every region. Scotland, Wales and Northern Ireland already have far greater availability of enhanced services within optical practices and much higher public awareness of the role of community optometrists. To achieve the same for England, commissioners need to recognise the pivotal role optometrists will play in achieving the Health Plan’s goals. They should build on this existing delivery of high-quality eye care closer to home — to reduce pressure on hospitals and avoid unnecessary sight loss.

