by Hazlin Hassan
ost eye surgeons thrive under pressure. But what do you do when the unexpected nightmare scenarios suddenly occur during surgery? Well, as the Dutch may say, eye surgeons will certainly get that piglet washed! Which is another way of saying they will fix something, or get the job done.


Some of the most distinguished and experienced surgeons shared their experiences and tips on how to deal with the unexpected while conducting surgery, during the European
Z EISS O p ht hal m i c V i r tu al E x p e r i e n ce
E S C R S - E U R E T I N A S p o t l i g h t 2020
O c t o ber 1 – 4, 2020

Society of Cataract and Refractive Surgeons (ESCRS) Main Symposium on Saturday (Oct 4) at the virtual ESCRS 2020 congress.

“Every surgeon encounters complications. If you never have complications, you never operate,” said chairperson Professor David Spalton, former president of the ESCRS.
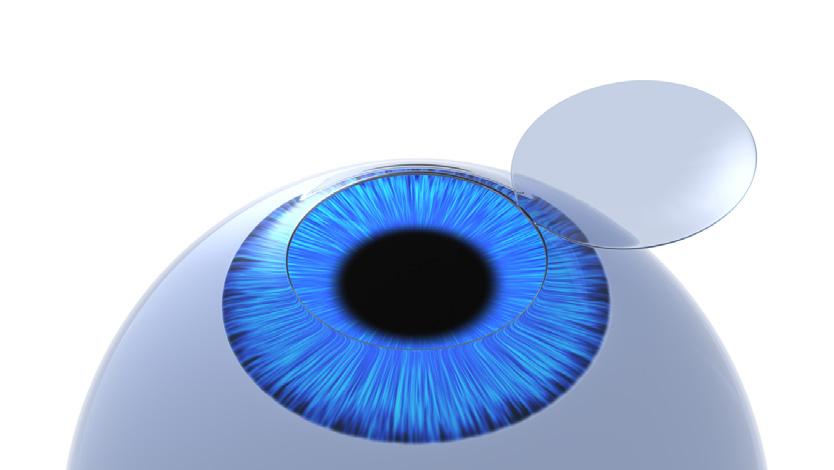
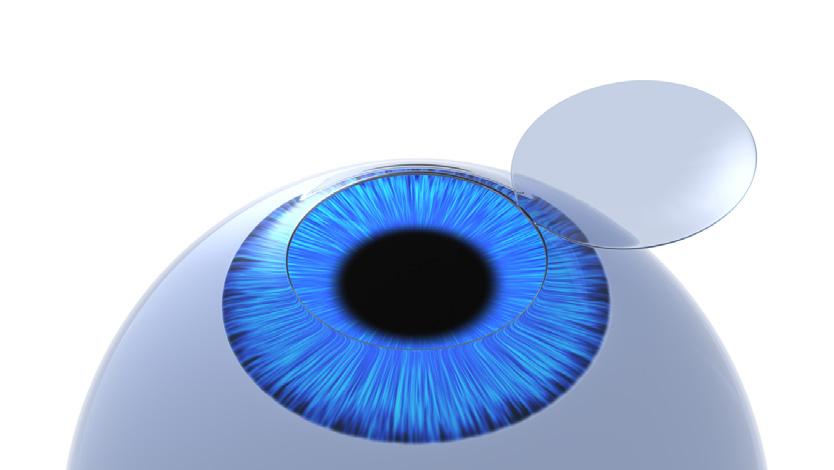
Having a shallow anterior chamber during phacoemulsification can be detrimental to the

Join
the unveiling of our all-new virtual showroom!
Join us for the virtual experience and learn more about the latest technologies in eyecare. We have an exciting program lined up, including the unveiling of our all-new virtual showroom!
Register here: www.zeiss.com/escrs-euretina-registration

o m /e sc r s - e u r et i n a - r e g is t r a t i o n
Register here:
CAKE AND PIE MAGAZINES’ DAILY CONGRESS NEWS ON THE ANTERIOR AND POSTERIOR SEGMENTS 04 | 10 | 20 cataract • anterior segment • kudos • enlightenment 3ISSUE posterior segment • innovation • enlightenment & M
Cont. on Page 3 >> J o i n u s f o r t h e v i r t u a l e x p e r i e n ce a n d l e a r n m o r e a b o u t t h e l a t e s t t e c h n o l o g i e s i n e y ec a r e We h a v e a n e x c i t i n g p r o gr a m l i n e d u p, i n c l u di n g t h e u n v e il i n g o f o u r a l l - n e w v i r t u a l s h o w r o o m ! R e g i s t e r he r e: ww w. z e i s s .c
ZEISS Ophthalmic Virtual Experience ESCRS-EURETINA Spotlight 2020 October 1 – 4, 2020
us for the virtual experience and learn more about the latest technologies in eyecare. We have an exciting program lined up, including
ZEISS Ophthalmic Virtual Experience ESCRS-EURETINA Spotlight 2020 October 1
4, 2020
–
Published by piemagazine.org cakemagazine.org Matt Young CEO & Publisher Robert Anderson Media Director Hannah Nguyen Production & Circulation Manager Gloria D. Gamat Chief Editor Brooke Herron Editor International Business Development Ruchi Mahajan Ranga Brandon Winkeler Writers Andrew Sweeney Hazlin Hassan Joanna Lee Olawale Salami Sam McCommon Tan Sher Lynn Maricel Salvador Graphic Designer Media MICE Pte. Ltd. 6001 Beach Road, #19-06 Golden Mile Tower, Singapore 199589 Tel: +65 8186 7677 | +1 302 261 5379 Email: enquiry@mediamice.com www.mediaMICE.com
What To Do When The Unexpected Happens Highlights from ESCRS Main Symposium
EURETINA 2020 Virtual Congress
Missed our EURETINA 2020 symposia? Watch the video recordings to hear our global experts talk about optimizing outcomes in patients with nAMD and DME.
Optimizing patient outcomes in nAMD: The key principles



Chair: Prof. Paolo Lanzetta
Hear from Dr. Michael Stewart, Dr. Nancy Holekamp, and Prof. Nicole Eter as they present the latest evidence and discuss hot topics in nAMD management.
Video recording
Vision in focus: Delivering optimized patient outcomes in DME in the real world





Chair: Prof. Ian Pearce


Listen to Prof. Jean-François Korobelnik, Dr. Varun Chaudhary, and Prof. Francine Behar-Cohen as they share expert guidance for optimizing management of patients with retinal vascular diseases.


Video recording
“Join us as we examine the latest evidence from clinical trials and realworld practice to address key challenges in retinal disease management and ensure we are optimizing outcomes for our patients.”
Prof. Paolo Lanzetta
Additionally, we warmly welcome you to the Bayer Networking Lounge, which will provide you with an opportunity to connect with experts in the treatment of retinal diseases.
Learn more about Bayer Ophthalmology by visiting our online channels:

04 Oct 2020 | Issue #3 2 &
DME, diabetic macular edema; nAMD, neovascular age-related macular degeneration. The summary of product characteristics (SPC) of aflibercept solution for injection as approved by the European Commission can be found here BAYER and the Bayer Cross are registered trademarks of Bayer. © Bayer AG 2020. All rights reserved. Bayer (South East Asia) Pte Ltd, 2 Tanjong Katong Road Paya Lebar Quarter 3 #07-01, Singapore 437161. September 2020 | PP-PF-OPHT-ALL-0047-1 | PP-EYL-SG-0185-1 (09/20)
corneal endothelium. But the anterior chamber can become shallow when there is high pressure within the lens itself, said Dr. Miguel A. Teus, from Hospital Universitario Principe de Asturias, Spain.
consultant ophthalmologist and board member of the ESCRS and chairman of the Association of Ophthalmologists. His tips to help minimize problems: “Recognize trouble early. This may seem like a truism but it is true,” he said. “Get over the denial that the PC really has gone. Do not let the eye decompress as this will allow vitreous to prolapse,” he advised.
to deal with this,” shared Dr. Packard.
Refractive surprises, or any postoperative refractive errors not anticipated by the ophthalmologist or the patient, are the primary reasons for dissatisfaction after premium lens surgery, said Professor Nic Reus, from Amphia Hospital in Breda, The Netherlands.
“Don’t panic,” he advised. Perhaps easier said than done.
But first, analyze the refractive surprise. Perform manifest refraction, slit lamp examination, check the implanted versus intended intraocular lens (IOL) power, check the biometry used for calculations, and whether it is the correct patient! Retake measurements (biometry, corneal topography) and make sure the refraction is stable, around 6 weeks or more.
Options for treating the refractive surprise include correcting with spectacles or contact lenses, rotation of a toric IOL to reduce astigmatism, laser vision correction or IOL exchange, especially for larger refractive errors and hyperopic errors. However, Prof. Reus cautions that any surgical correction may exacerbate ocular surface disease. Is the patient, the doctor, or are both unhappy with the refractive outcome? He is of the opinion that it is better to treat the patient, not the refractive error.
The best way to deal with this is to aspirate the liquefied cortex to reduce the pressure within the lens.
This may also occur during hydrodissection. There is a risk of posterior capsule rupture.
This is easy to prevent by washing the OVD from the lens surface. It is also easy to solve by pressing the nucleus backwards.
Conclusions: “Check the intraocular pressure (IOP) intraoperatively,” he said, adding that anticipating a problem is always the best solution!
What do you do when the posterior capsule has ruptured? This was the scenario presented by Richard Packard,
Fill the eye with dispersive ophthalmic visco-surgical devices (OVD) before removing the phaco probe. Once things are stable, decide if you need to carry out an anterior vitrectomy, and decide if you are going to do it through corneal or pars plana incisions.
Once the eye is filled with dispersive OVD, make sure there is a second paracentesis for bimanual vitrectomy or create a pars plana opening with 23G trocar. Check that the phaco machine settings are on the highest cut rate with moderate flow rate and vacuum and low bottle height. Place an irrigation handpiece in the eye followed by the vitrector probe.
“In summary, have a strategy. Do not allow the eye to decompress. Avoid vitreous base traction - surprising little can cause peripheral breaks. But if you feel you cannot cope, there is no shame in asking for help. If the nucleus is at risk, remember VR surgeons are trained
“Offer apologies to the patient. Explain what the reason is for the remaining refractive error. Wait until the error has stabilised. Explain the various options, the pros and cons of treating the refractive surprise, any spectacle dependency, and risks of complications,” he advised.
In conclusion: Managing expectations before surgery is of the utmost importance. With a refractive surprise, carefully check manifest refraction, meticulously perform ophthalmic examination, retake biometry and corneal topography, and wait around 6 weeks before any intervention.
“Discuss the pros and cons of the various options with the patient. In most patients, a refractive surprise can be managed with excellent results,” Prof. Reus said.

3 CAKE and PIE magazines’ Daily Congress News on the Anterior and Posterior Segments
>> Cont. from Page 1
“Every surgeon encounters complications. If you never have complications, you never operate,”
— Prof. David Spalton













2 18 November 2022 | Issue #1 SHOW DAILY by DIGITAL MARKETING + ADVERTISING + VIDEO PRODUCTION + MEDICAL WRITING + EVENTS Request our 2023 Media Kit Now! Write enquiry@mediamice.com for a copy HQ Office: 6001 Beach Road, #09-09 Golden Mile Tower, Singapore 199589 Phone: +65 8186 7677 Satellite Office: 2 Nuoc Man 2 Street, Da Nang City, Vietnam 50506 Phone: +84 868 063 773 E-mail: enquiry@mediamice.com Web: www.mediamice.com
Biomarkers From Inflammation to Infections and Neurodegenerative Diseases
by Tan Sher Lynn
Experts discussed the role of biomarkers in the detection of various diseases.
Inflammation is a key mechanism of dry eye disease (DED) and plays an important part in the vicious circle of dry eye, according to Dr. Elisabeth Messmer from Germany. It can also be present in other ocular surface disease such as allergy. Good thing is, inflammation decreases with positive therapeutic response.
“Inflammation can be clinically evident, such as in conjunctival hyperemia and blepharitis. But very often, inflammation in DED is subclinical and we need to test for inflammatory markers in the tear film as direct evidence of inflammation, or hyperosmolarity of the tear film as indirect evidence of inflammation. The American Society of Cataract & Refractive Surgeons (ASCRS) recommend tear film osmolarity MMP-9 testing in the tear film as essential screening test before cataract surgery and refractive surgery. MMP-9 is stimulated by desiccating stress, hyperosmolarity, estrogen and pro-inflammatory cytokines leading to a cycle of escalating inflammation. A number of bedside tests are available, including the Inflammadry®, Tearlab®
and I-Pen®, which are helpful to identify patients with significant ocular surface inflammation and autoimmune disease,” she said.
Speaking on the detection of viral infection, Dr. Marc Labetoulle from the South-Paris University, France, said that it is very difficult to determine the cause of keratitis on a clinical setting, as the condition can be due to amoeba, fungi, bacteria and viruses. Hence, biomarkers are needed to improve the reliability of diagnosis. Conventional diagnostic methods like virus in cultured cells, immunofluorescence, immunochemistry and in situ hybridization are timeconsuming, poorly reproducible and not cost-effective. As such, gene amplification becomes the method of choice.
With 100% sensibility and 67.9% specificity, PCR has been shown to be more efficient than conventional techniques. However, the efficacy of PCR may be affected by few factors, including the time of transportation to the lab, the quality of the DNA/RNA extracted, the choice of primers, and the fact that some eye drops may inhibit the Taq polymerase reaction. “In summary, sampling should be made in case of presumed viral
keratitis, if there is atypical pattern (observed via slit lamp examination), atypical medical history or resistance to treatment. A good sampling is an early sampling. And all these require real collaboration with the microbiologist,” Dr. Labetoulle said.

Looking beyond the eye, Dr. Marlies Gijs from the University Eye Clinic Maastricht, The Netherlands, said that as the eye and the brain share many neuro and vascular similarity, the eye may offer insights into the diagnosis of neurodegenerative disease which comprises over 100 types of diseases that are progressive, largely incurable and ultimately terminal, such as Alzheimer’s disease, Parkinson’s disease and amyotrophic lateral sclerosis (ALS). Neurodegenerative disease is caused by the degeneration of neurons in the central nervous system (CNS), resulting in a decline in cognitive and/or physical abilities.
“Current treatment options are very limited. They can only modestly slow disease progression and cannot stop or reverse it,” shared Dr. Gijs. Hence, a timely and accurate diagnosis is important as treatment needs to start at the preclinical stages of the disease. Since neurodegenerative diseases are associated with various vision problems, presence of neuropathological hallmarks can be detected through (retinal) imaging, histological analysis (postmortem retina) and (tear) fluid analysis.
“Yet they have not yet been implemented in the diagnostic pipeline of neurodegenerative diseases due to various factors including the heterogeneity of the disease, numerous comorbidities, need for imaging instruments, inconclusive results, as well as moderate sensitivity and specificity. When looking into tear fluid levels, studies with large sample size are definitely needed for threshold determination,” she added.
5 CAKE and PIE magazines’ Daily Congress News on the Anterior and Posterior Segments
“Current treatment options are very limited. They can only modestly slow disease progression and cannot stop or reverse it,”
— Dr. Marlies Gijs
Insights into AMD New Findings and Novel Treatment Approaches


 by Tan Sher Lynn
by Tan Sher Lynn
Dr. Caroline Klaver from the Erasmus MC Rotterdam, The Netherlands, offered new insights into retinal disease derived from the EyeRisk study. A total of data of 53,000 subjects from 20 European eye epidemiology studies encompassing genotype, phenotype environmental risk factors and blood biomarkers were used, followed by the development of a genotype assay for age related macular degeneration (AMD) and subsequent works. “EyeRisk created a large AMD genetic epidemiology database, developed a genotype pipeline for AMD, provided evidence that AMD is due to at least three pathways, identified metabolic biomarkers for AMD, showed a role of CFH in lowering oxidation and identified genetic
clusters for GA patients. The next steps are: to use genetics and the lessons learnt from systems biology to guide the development and application of personalized intervention,” shared Dr. Claver.
Presenting on the impact of AIbased biomarker detection in optical coherence tomography (OCT) scans, Dr. Adnan Tufail from the Moorfields Eye Hospital, United Kingdom, said that AI biomarker detection is rapidly evolving, with roles in population studies (AMD, nAMD, OCT-A), and in the future can be deployed to guide treatment and response to treatment. “This will massively accelerate our understanding of clinical trials and novel biomarkers in precision medicine,” he said.
Meanwhile, Dr. Robyn Guymer from Australia talked about the approaches to slow progression of intermediate AMD, which include lifestyle changes, AREDS formulation, supplements and statin.
According to Dr. Guymer, due to concerns about thermal laser causing regression of drusen and choroidal neovascularization (CNV), the use of thermal laser to slow AMD progression was shelved. New laser modalities, such as the nanosecond laser (2RT) has been developed to selectively target the retinal pigment epithelium (RPE) and reduce collateral thermal damage to the neuro retina.
The LEAD study, a 36-month, randomized, sham-controlled trial of subthreshold 2RT nanosecond laser,
shows that there was no significant difference in the overall progression rate to late AMD between those receiving laser or sham treatment. However, 2RT may have a role in slowing progression for intermediate AMD without coexistent RPD. “There seems to be a dearth of RCT in early stages of AMD. Now that we have potentially new ways of classifying early AMD severity and progression using multimodal imaging, it is hoped that there will be a large increase in clinical trial activity investigating novel interventions for early-stage AMD before vision-threatening complications appear,” she said.
According to Dr. Jordi Mones from the Institut de la Màcula, Spain, novel therapeutic approaches for neovascular AMD include intravitreal drugs such as brolucizumab (approved), faricimab (in phase 3, ongoing) and KSI 301 (in phase 2b/3, ongoing); intraocular devices such as the port delivery system; and gene therapy like the RGX 314 (to initiate phase 2), a novel AAV8 vector to subretinally deliver an anti-VEGF Fab, as well as ADVM-022 where phase 1 trials show a substantial reduction in antiVEGF treatments following a single IVT injection. “Long-lasting drugs is a reality. Now, our objective is not just to provide short-term benefits to patients, but to try to provide vision for them for 10 years or more,” he said.
Talking about improving adherence and outcomes in AMD therapy via home monitoring, Prof. Anat Loewenstein from the Tel Aviv Medical Centre, Israel, said that the information generated by tele-connected OCT in patients’ homes has the potential to support current retinal disease management and future evolution in monitoring patterns, drug selection and dosing, as well as patient outcomes. “Home OCT testing gives new insights in retinal fluid dynamics. A clinical trial was conducted with the patient self-operated Notal Vision OCT on an elderly AMD patient population. Eighty-eight percent (88%) and 93% of eyes were successfully self-imaged by patients on the Notal OCT V2.5 and V3, respectively. Patient feedback on device usability was consistently positive and the device meets the requirement of successful patient self-imaging,” she concluded.
04 Oct 2020 | Issue #3 6 &
Optimizing Real World Outcomes in DME
 by Brooke Herron
by Brooke Herron
We all know that clinical trial results don’t always translate to the same outcomes in the real world. Of course, this is due to a variety of factors outside strict study controls — there are issues of compliance, cost and treatment burden for physicians to contend with. Therefore, this important topic was covered during the virtual EURETINA 2020 in a Bayersponsored symposium called Vision in Focus: Delivering Optimized Patient Outcomes in DME in the Real World, chaired by Prof. Ian Pearce (United Kingdom).
International guidelines for treatment
“We all see patients in our daily practice that come into our office with retinal vascular disease — and I think our patients expect that they will respond quickly to treatment… they want to see an increase in vision soon after their first treatment. They want to maximize and maintain those vision gains over a long period of time with a minimal number of treatments,” began Dr. Varun Chaudhary (Canada).
Patients don’t care what their vision is at week 52 or 104 — they care about what their vision is every single day, he continued. To assess this, Dr. Chaudhary says physicians need to look at the area under the curve (AUC).
“AUC analyses suggest that in patients with a baseline VA of <69 letters, vision gains with aflibercept are superior [to ranibizumab and bevacizumab] over two years,” he said. In these patients, international guidelines also suggest
using aflibercept over other anti-VEGF agents.
This is according to EURETINA guidelines, which says aflibercept is the drug of choice in patients with BCVA of <69 letters. “Guidelines from across the globe, including Asia, Canada and Germany are in line with the EURETINA guidelines,” noted Dr. Chaudhary.
From clinical trials to the real world
Following the presentations, Prof. Pearce helpfully summarized the main points and facilitated further discussion.
Prof. Jean-François Korobelnik’s (France) talk on Early intensive and proactive long-term treatment: delivering on the promise of RCT-like outcomes in the real world showed how “randomized clinical trial-like (RCT) vision gains can be achieved in clinical practice with early intensive treatment, including the use of five initial monthly loading doses and proactive extended dosing, while reducing treatment burden in subsequent years.”
In her presentation, Prof. Francine Behar-Cohen (France) discussed All in the action: multi-targeting three underlying pathways, which concluded that “aflibercept is the only antiVEGF approved in countries throughout the world that blocks all VEGFR-1 ligands (including VEGF and PGF), inhibiting three pathways in the pathogenesis and progression of retinal vascular disease: vascular permeability, edema and inflammation.”
Further, Prof. Pearce noted that while patients with DME need repeated appointments, diabetics are often not the easiest group to get into the office each month. Thus, he asked the panel: “How do you get them into your practice?”
According to Prof. Korobelnik: “We try our best to explain to the patient how important it is to comply.” Usually patients are motivated, and don’t want to lose any vision gains, he said, adding that they take time at the beginning to really explain this to patients.
Dr. Chaudhary added to this and emphasized the importance of the loading dose and the ultimate hope to reduce injection frequency over time. “We try to get patients to appreciate that early, intense treatment has disease modifying effects… meaning fewer treatments over the long-term. I think that really resonates with patients.”
Another important thing to communicate with patients is establishing that what is achieved in five months is going to be the threshold for the best vision achieved, he shared.
Prof. Pearce notes this is inspired by Protocol T, where patients receive treatment until there is no improvement. “After we get to the level, we can step off the gas a little,” he concluded.
7 CAKE and PIE magazines’ Daily Congress News on the Anterior and Posterior Segments
Behind the Masquerade

Unmasking Uveitis and Endophthalmitis
by Brooke Herron
While acute endophthalmitis is often associated with infectives, like bacteria or fungi, low grade infections can also occur postoperatively or from trauma — and in some cases, endophthalmitis can masquerade as uveitis. Therefore, the disease mechanisms, diagnosis and treatment of both sight-threatening conditions were discussed by experts on the second day of the virtual EURETINA 2020 congress in a session chaired by Drs. Jose Garcia Arumí (Spain) and Jan Van Meurs (The Netherlands).
It’s an emergency: Viral retinitis
Viral retinitis is a major infective entity and remains an absolute emergency situation in uveitis, began Dr. Bahram Bodaghi (France). “Herpes agents are the most frequently involved, but there are also some emerging diseases. There is a high rate of complications and unfortunately, a poor visual outcome,” he shared.
The main entity is acute retinal necrosis (ARN), which is a rare disease — with an incidence rate of 0.63 per million,

per year. In these patients, Dr. Bodaghi says it’s important to focus on the rate of ocular atrophy despite therapeutic management.
“The diagnosis is based on PCR (polymerase chain reaction), and more and more, we are using real-time PCR for its rapidity, high sensitivity and quantification,” he continued. In these cases, treatment is emergent with intravenous acyclovir, followed by oral valacyclovir. He further discussed treatment in more severe cases.
In cases of ARN that do not respond to intravitreal or systemic treatment, Dr. Van Meurs asked
Dr. Bodaghi if he would consider vitrectomy to decrease the viral load. He responded: “We should insist on the medical therapy first, and then vitrectomy might be proposed in very severe instances when you have a pseudo-endophthalmitis case of ARN. But I’m not in favor of vitrectomy to all patients with ARN when they arrive because in those cases we have a high rate of secondary retinal detachment.”
In summary, he said that ARN is an
absolute emergency — it’s sightthreatening, despite appropriate treatment and host immune status.
Don’t wait to treat
In cases of endophthalmitis, Dr. Van Meurs had a short, but sweet, message as his presentation’s name: Earlier antibiotic treatment is the most feasible step to improve treatment of endophthalmitis.
Remember the choice of antibiotics is no issue, and treatment should move forward — and clearly, early administration of antibiotics is more feasible than early vitrectomy, he shared. “What we like to do is inject first, and then do diagnostics later.”
He says in the near future, intravitreal antibiotics will be injected immediately… ideally by the referring doctor not to lose any time.
Surgical treatment of endophthalmitis
Endophthalmitis is a devastating complication of intraocular surgery, said Dr. Arumí. “The b-scan is a good way to evaluate the severity of the disease, and intraocular antibiotics remain the mainstay of treatment in non-aggressive cases.

“Vitrectomy is the best approach in aggressive cases: fungal, traumatic, chronic and in secondary complications,” he explained. “Time is crucial, and with early treatment, we can obtain a good postoperative BCVA.”
In these cases, pars plana vitrectomy (PPV) removes bacteria and their toxins, clearing the ocular media, and thus, allowing for a more rapid visual recovery.
Following his presentation, he commented further during the expert panel: “I think that vitrectomy is quite aggressive surgery; if the solution is with intravitreal, then I think it’s better to wait,” said Dr. Arumí.
“The problem with PRN, is that after some time, you can have a retinal detachment due to the necrosis and the traction that the vitreous exerts over the retina. In those cases you have to perform the vitrectomy,” he concluded.
04 Oct 2020 | Issue #3 8 &
Of UNICORNs and OCT-A Parameters

Highlights from the Imaging Symposium
by Olawale Salami
On the menu: The OCTA word salad, with a side of other metrics
“On top of this, different device software does not offer the same set of measurements or parameters, and when they do, they often use disparate nomenclature to compare similar parameters,” she said.
Furthermore, Dr. Munk emphasized that there is an urgent need to ensure that clinicians and researchers measure the same structures and use the same language to characterize them.
Finding the UNICORN: Expert consensus on OCTA nomenclature in exudative AMD
Dr. Marion Munk from Bern, Switzerland, highlighted an essential requirement for a universal understanding of optical coherence tomography-angiography (OCT-A) findings. “There is a need to rely on standardized terms in the literature in daily practice and clinical trials to ensure uniformity in communication,” said Dr. Munk. For example, in OCT, when we use the term ‘central macular thickness’, we all know that we are referring to mean thickness of the central 1 mm of the Retina, she noted.
“Besides, we need to consider that the parameters we assess are well defined and reliable, and represent surrogates of patient outcomes, so the question is: are these requirements met in OCT parameters,” Dr. Munk asked her the audience during her presentation.
“Not only do we have to deal with artifacts in this imaging modality, but there are also different segmentation algorithms in different OCT models,” she noted.
According to Dr. Munk, there is a massive variety of abbreviations, parameters, and terms used interchangeably in daily clinics and trial literature. Furthermore, it remains unclear which of these parameters represents the most relevant surrogate markers.
“Therefore, we brought together a team of experts in retinal vascular diseases to tackle this problem, and conducted a comprehensive literature search of all terms used in reporting OCTA findings in retinal vascular diseases. Next, based on the review, we developed a standardization survey completed by experts and members from EURETINA, the Retinal Society, and the Japanese Retina and Vitreous society,” she shared.
In conclusion, Dr. Munk stated that after there rounds of review and feedback of responses, we are preparing a manuscript which will be discussed during a consensus meeting.
The UNICORN project (an acronym for Unified Expert Commentary On OCTA in Neovascular AMD) was conceived to address the lack of consistency in the nomenclature and quantitative metrics in OCT, introduced Dr. Usha Chakravarthy. “There has been a rapidity in the proliferation of terms to describe lesions in many diseases. Notably, the use of different imaging instruments on similar nAMD lesions can lead to differences in OCTA findings’ interpretation,” she noted.
Reporting on the current status of the project, Dr. Chakravarthy highlighted that to date, a semi systematic review of descriptive and quantitative metrics in nAMD have been completed. “In addition, with a collaborative grant with Dr. Nadia Waheed, we have worked with our trainees to construct a dictionary of terms and definitions from published sources. We have also identified the most consistent features of nAMD for a unified nomenclature and created a repository that will act as a publicly available reference,” she shared.
Explaining the methodology, Dr. Chakravarthy stated that 11 experts graded 23 image sets and answered questions. “We then utilized mixedeffects logistic regression models to test agreement,” she explained.
Concluding her presentation, Dr. Chakravarthy said: The first UNICORN report has been submitted to the journal Ophthalmology for peer review. The next steps include a more robust evaluation, consisting of a more extensive set of images, pre and post-test training, and provision for users to alter image segmentation. We are also planning a full systematic review of OCTA in nAMD.”
9 CAKE and PIE magazines’ Daily Congress News on the Anterior and Posterior Segments
“The use of different imaging instruments on similar nAMD lesions can lead to differences in OCTA findings’ interpretation.”
— Dr. Usha Chakravarthy
“There is an urgent need to ensure that clinicians and researchers measure the same structures and use the same language to characterize them.”
— Dr. Marion Munk
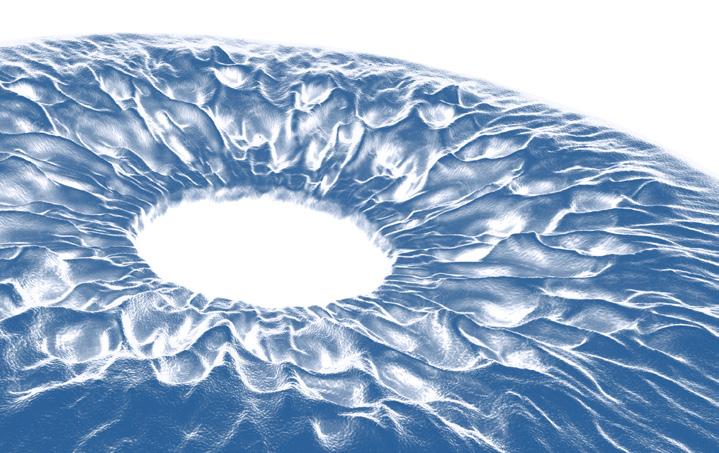
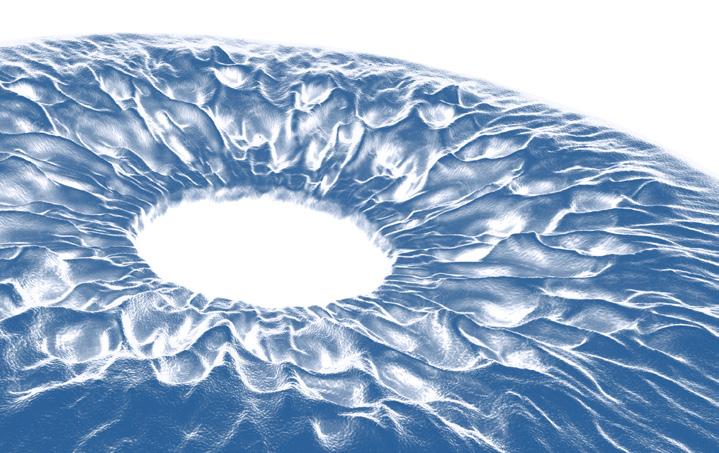
Corneal Intrastromal Femtosecond Refractive and Therapeutic Surgery
Highlights from the Clinical Research Symposium
by Olawale Salami
Novel treatments for keratoconus: Are we there yet?
Would it be possible to treat keratoconus by enhancing and regenerating the corneal stroma with minimally invasive surgical procedures? Dr. Jorge Alio and his team have opened new frontiers in the search for new keratoconus treatments.
In his presentation at the virtual ESCRS 2020 congress, Dr. Jorge Alio said: “We aimed to find an alternative to the classical corneal transplantation to regenerate the corneal stroma.”

“We hypothesized that autologous, adipocyte-derived adult stem cells
 — Dr Jorge Alio
— Dr Jorge Alio
(ADASC) injected into the stromal pocket of the patient with keratoconus, in isolation or on acellular corneal laminas,
can transform into keratocytes. These cells do not generate inflammatory responses and could be suitable for the treatment of keratoconus,” Dr. Alio explained.
“We have studied the evolution of these cells as well as the evolution of implanted acellular or decellularized laminas in vivo, using confocal microscopy,” he said.
Dr. Alio presented results of an early phase clinical study: “We conducted a 3-arm, randomized trial in patients with advanced keratoconus, in which 5 patients per group received either autologous implantation of ADASC, ( group 1), decellularized human corneal stroma( group 2) or ADASC + decellularized human corneal stroma( group 3). The primary outcome measure was the safety of our interventions.”
“Overall, our results show that the transplantation of ADASC and decellularized human corneal stroma into the human cornea are safe, induced no inflammatory responses and represent the future of keratoconus treatment,” shared Dr. Alio, summarizing the results.
“We have demonstrated that ADASC

04 Oct 2020 | Issue #3 10 &
“Taken together, our results show that the corneal transplantation of ADASC and decellularized human corneal stroma are safe, induced no inflammatory responses and represent the future of keratoconus treatment.”
cells survive in vivo in the human corneal stroma. Our early results have demonstrated modest improvements in visual parameters. However, more longitudinal studies are needed to confirm these results in larger patient populations,” he added further.
Why bioengineered stromal lenticules?
tissue, we have been working on collagen-based, bioengineered tissue,” added Dr. Lagali.
Starting with a fundamental building block of medical-grade porcine collagen, it is then cross-linked to increase transparency and mechanical strength. Then, the size, thickness, and swelling can be customized. “We have shown positive results in rabbit and pig models, which were the basis for our first human trials,” Dr. Lagali shared. “We found good improvements in visual acuity in the first 10 eyes implanted with the bioengineered lenses in humans, which was sustained up to 3 months followup,” he added.
Active bioengineered implants represent the next frontier on additional functions of bioengineered implants, noted Dr. Lagali. “This is because we can load these implants with active substances during fabrication, which can then be released slowly to elicit desired

therapeutic effects. We have currently loaded collagen implants with recombinant nerve growth factor (rNGF), and the slow release curve demonstrates that after 2 months, about 25% of the rNGF had been released,” he shared.
The widespread use of human donor lenticules for additive keratoplasty will, in the future, result in a higher incidence of stromal rejection,” said Dr. Neil Lagali.


According to Dr. Lagali, bioengineered lenticular tissue is well defined and follows standardized lenticule production, with customized thickness options. “It is also easy to control tissue characteristics and avoid rejection. Bioengineered tissue can provide additional functions that human tissue cannot,” he explained.
The first approach is the decellularization of human tissue, noted Dr. Lagali. “This, however, still requires a source of human donor corneal tissue. Human clinical data is limited, and a recent meta-analysis of deep anterior lamellar keratoplasty in patients with keratoconus showed stromal rejection rates of 3-24%,” he shared.
“As an alternative to the use of human
Laboratory made bioengineered stroma can provide unlimited tissue for refractive and therapeutic purposes.
11 CAKE and PIE magazines’ Daily Congress News on the Anterior and Posterior Segments
“Laboratory made bioengineered stroma can provide unlimited tissue for refractive and therapeutic purposes.”
— Dr. Neil Lagali
“As an alternative to the use of human tissue, we have been working on collagen-based, bioengineered tissue,”
— Dr. Neil Lagali
“We have studied the evolution of these cells as well as the evolution of implanted acellular or decellularized laminas in vivo, using confocal microscopy,”
— Dr Jorge Alio
How many behind-the-scenes photos would it take to make that one perfect “Virtual Amsterdam” shot? Let us count the ways... and search “PIE and CAKE Magazines” on YouTube to see our latest videos from ESCRS and EURETINA Virtual. Or Just click HERE.
Diagnosing and Treating Retinal Vascular Diseases
by Hazlin Hassan
Retinal vascular disorders are a range of eye diseases that affect the blood vessels in the eye. They are linked to vascular diseases, such as high blood pressure, high cholesterol and diabetes – conditions that cause atherosclerosis, or a thickening of the artery walls.
Retinal vascular diseases can have severe consequences for those affected by the condition, including vision loss. Diagnosing and treating them can be complex.
Among some of the topics discussed during a session at the virtual EURETINA 2020 congress on Saturday (Oct 3) included the management of macular edema in vein occlusion, the surgical management of resistant cases
of vein occlusion, and whether an optical coherence tomography angiography (OCT-A) is essential in cases of vein occlusion.
The GENEVA trial has shown that more than 65% of the maximal reduction of central retinal thickness that can be obtained during the first three months after therapy is already present 24 hours after treatment, said Paolo Lanzetta, MD, from University of Udine, Italy.
In the 6-month analysis, each 1-month increase in ME duration was associated with a significantly lower likelihood of achieving a best corrected visual acuity (BCVA) improvement of 15 letters or more.
“This suggests that prompt treatment for


retinal vein occlusion is associated with improved functional outcomes,” said Dr. Lanzetta.
In a study comparing ranibizumab (Novartis 2010) versus the dexamethasone implant (Allergan 2009), ranibizumab was associated with a greater increase in BCVA (mean difference 9.13) compared to dexamethasone. There was no significant difference at 3 months.
A combination therapy with simultaneous administration of aflibercept and dexamethasone was effective in resolving macular edema, despite the absence of visual improvement.
Earlier combined treatment in the course of the disease might lead to better functional outcomes, he noted.
When it came to the comparative efficacy of anti-VEGFs, he said there were no statistically significant differences in any outcome among anti-VEGF drugs.
In a study involving conbercept versus ranibizumab, there were no significant differences found in the improvements of BCVA and adverse events between the two groups. However, there were significant differences between conbercept and ranibizumab treatment in terms of central macular thickness (CMT) favoring conbercept.
The current evidence suggests that intravitreal pharmacotherapy is effective in ameliorating vision function in RVOME patients, Dr. Lanzetta said. “The treatment armamentarium is expanding. Early treatment provides better results.

04 Oct 2020 | Issue #3 12 &
“The treatment armamentarium is expanding. Early treatment provides better results. When choosing a dexamethasone implant, consider the employment of an as-needed retreatment protocol with monthly follow-up,”
— Dr. Paolo Lanzetta
When choosing a dexamethasone implant, consider the employment of an asneeded re-treatment protocol with monthly follow-up,” he concluded.
While pharmacological therapy remains the first-line treatment for macular edema, pars plana vitrectomy (PPV) may be beneficial in cases of vitreoretinal traction or persistent macular edema resistant to medical treatment, said Dr. Jose Garcia Arumi, from University Hospital Vall d’Hebron, Spain.
In cases of traditional macular edema, early release of traction may contribute to the resolution of the macular edema.
In a study of 26 patients with central retinal vein occlusion (CRVO) and macular edema (ME) who underwent vitrectomy, the visual and macular thickness improved at 6 months. A high vitreous VEGF level was associated with greater improvement of macular edema.

“The role of PPV in diffuse or nontractional macular edema remains controversial. Vitrectomy with ILM peeling may achieve visual improvement
and may be a good option for certain cases. The effects may last for years with minimal additional treatments,” he said in ending his presentation.
Is the OCT-A essential in vein occlusion? This was the question raised by Francesco Bandello, MD, from University Vita-Salute, Ospedale San Raffaele, Milan, Italy. RVO is the second most common retinal vascular disorder and 16 million people are affected in one or both eyes worldwide.
Before the advent of OCTA, fluorescein angiography (FA) was used to detect ischemic areas, tortuous vessels, microaneurysms, and collateral vessels.
“Yes, microvascular changes in RVO are all readily visible with OCTA. It is better than FA and OCT for microvascular changes and cystoid spaces,” he opined.
But there are still limitations. It is unable to view peripheral vascular perfusion due to a limited field of view. OCTA is also prone to artifacts, shadowing of edema, and inaccuracy of segmentation.
Virtualcariously*


adverb

When you put yourself in someone else’s virtual shoes, instead of having the physical experience yourself. Example: We’re all living through ESCRS & Euretina virtualcariously.

Vitreous VEGF level may be correlated with the visual prognosis and changes of macular edema in CRVO patients after vitrectomy.

13 CAKE and PIE magazines’ Daily Congress News on the Anterior and Posterior Segments
“The role of PPV in diffuse or non-tractional macular edema remains controversial. Vitrectomy with ILM peeling may achieve visual improvement and may be a good option for certain cases. The effects may last for years with minimal additional treatments.”
— Dr. Jose Garcia Arumi
*New virtual conference definitions, by Media MICE
20/20 in
3. Take posterior corneal astigmatism into account: “Whether you use standard mathematical models or total corneal measurements, please remember never to use both — you are going to correct the same problem twice, and you are going to get it wrong.”
4. Be alert for unusual corneas: “Keratoconus or post-refractive eyes might present with an unusual ratio between anterior and posterior corneas, however standard mathematical models are not designed to account for that.”
The L e n s
by Brooke Herron
Thanks to the COVID-19 pandemic, this year has left our vision for the future a bit cloudy, to say the least. However, while things like travel, in-person meetings and the ability to even leave the house have stalled — ophthalmic innovation has continued. Therefore, 20/20 in 2020: The Lens, was a main symposium during the 38th Congress of the ESCRS, with discussion on getting to emmetropia, correcting astigmatism, assessing progress in IOL accommodation, and more.

The quest for emmetropia
When aiming for emmetropia, there are two essential requirements, said Dr. Giacomo Savini (Italy). These are updated instruments and formulas. “Now, in 2020 we have 16 IOL power formulas and 11 optical biometers.”
As far as the devices go, he says it’s not possible to say that one is better than another from a refractive point of view. This is because all manufacturers follow the measurements of the original IOL Master (Carl Zeiss Meditec, Jena, Germany) to be able to use the ULIB (User Group for Laser Interference Biometry) constants.
“My suggestion is to never over promise because we know that 15%, maybe 20%,

of eyes will have a prediction error higher than 0.50 D,” said Dr. Savini.
He says currently, his top formulas are Barrett II, EVO 2.0, Kane, Olsen (Phaco-Optics) and RBF. “The main problem is that it is difficult to optimize their constants without the authors’ support, as all of these formulas are unpublished,” he explained. “Without this constant optimization, this means they are not superior to traditional formulas.”
Correcting astigmatism
“Toric IOLs are gradually becoming the standard of care for [cataract patients with astigmatism], but their refractive results following implantation are not always predictable,” said Dr. Adi Abulafia (Israel). Therefore, he shared a list of seven tips for improving toric IOL outcomes.
1. Validate the data and look at the corneal topography: “Dry eyes should be treated preoperatively and remeasured since corneal measurements in these eyes can be unreliable.”
2. Use several measuring devices: “My advice, if possible, is to use at least three different devices for measurements.”
5. Account for corneal surgically induced astigmatism (SIA): “This is a controversial issue,” he said, noting that creating the ideal, personal SIA cornea calculation consists of several factors, including consistent location and would architecture and a measuring device with a high degree of accuracy and repeatability.
6. Optimize the toric IOL alignment: “It seems that computer-assisted marking has a small advantage over manual marking.”
7. Have a low threshold for toric IOL calculations: “Use your predicted post-op residual astigmatism as your reference.”
Restoring accommodation with IOLs: Have we made progress?

We currently don’t have any accommodative lenses that are worth being called accommodative lenses (A-IOLs), began Prof. Gerd Auffarth (Germany). On the different types he discussed, he said that dual optic systems might be better than single optic systems, although with minimal effect.
“Changing the curvature or refractive index — or a combination of those — could be really interesting . . . maybe combined with optoelectronic or mechatronic systems. We need something that is independent of the capsular bag and zonular fibers to make sure that we get what we predict. We’ll see what happens in the future,” he concluded.
04 Oct 2020 | Issue #3 14 &
AI at ESCRS & EURETINA 2020
Do AI Ophthalmologists Dream of Electric Corneas?
by Andrew Sweeney
Artificial Intelligence (AI) is one of the hottest topics in ophthalmology at present. The technology is now emerging from the pages of science fiction and is increasingly useful in the medical field. AI is becoming easier to use for clinicians and patients alike, and is now being deployed in a variety of ophthalmological segments.

Therefore it shouldn’t come as a surprise that the Clinical Research Symposium: Artificial Intelligence was one of the highlights on the second day at the virtual ESCRS & EURETINA 2020 congress. The two-hour long session, one of the longest at the conference, was dedicated to AI and its applicability to ophthalmology. Chaired by ESCRS president Prof. Dr. Rudy MMA Nuijts and Dr. Damien Gatinel, the Head of The Anterior and Refractive Surgery Department of The Rothschild Foundation in Paris, the symposium was a fascinating examination of AI technology.
The symposium was split into segments where several doctors presented their research into various forms of AI. These included surgical applications, using AI to search for rate pathologies affecting the eyes, and digital eye testing, and all the presentations are likely to be beneficial and insightful for any ophthalmologists. Each presentation
also included time for questions from both symposium participants and the audience.
Each of the presentations were of high quality and a particular highlight was Development of a Machine Learning Accessible EHR Suitable for Registry Studies by Dr. Bruce Allan. A consultant ophthalmic surgeon at Moorfields Eye Hospital, Dr. Allan spoke on the importance of correct data gathering and making AI work for you, not the other way around. It will likely prove highly beneficial for clinicians working in smaller sized facilities.
Another highlight was Artificial Intelligence for Classification of Corneal Dystrophies Including Fuchs’ Endothelial
Corneal Dystrophy. Presented by Dr. Jodhbir Mehta of the Singapore National Eye Center, the presentation was that rare combination of both highly informative and aesthetically appealing. Dr. Mehta included some fantastic images of the cornea in his presentation, some of the best we’ve seen thus far into the ESCRS/EURETINA joint congress, and his findings on the potential of AI in the corneal feed were sagacious and profound.
Throughout the presentations and the resulting discussion the main crux of the symposium remained the same. This was how can AI best be applied to ophthalmology in an easy to use manner for the patient and clinicians. This was a key point picked up on by Dr. Robert Wisse, an assistant professor at the University Medical Center Utrecht and head of the cornea, glaucoma and general ophthalmology unit.
Dr. Wisse spoke about demographic changes in Europe and the exponential rise in the number of elderly patients. He emphasized to the participants of the symposium that any AI solution adopted by ophthalmologists needs to be mindful of the less tech savvy like the elderly. Otherwise, AI technology will not prove to be an effective tool.
Indeed, Prof. Dr. Nuijts pointed to the example of his 86-year-old mother, and pointed out that while she’s able to use a tablet device, he feared other technology might be outside of her grasp. Discussion on the easy application of AI technology will no doubt continue. This will be facilitated by ongoing discussion about the application of telemedicine deriving the coronavirus pandemic, which has similar characteristics to the debate surrounding AI.
Is this how future ophthalmologists will look?

15 CAKE and PIE magazines’ Daily Congress News on the Anterior and Posterior Segments
CONTENT MARKETING + ADVERTISING + MEDICAL WRITING






6001 Beach Road, #19-06 Golden Mile Tower, Singapore 199589 magazine posterior segment innovation enlightenment




























 by Brooke Herron
by Brooke Herron