




Minimally invasive gynecological surgery at Norton Women’s Care is for more than fibroids and endometriosis

ALSO IN THIS ISSUE
MEDS & PEDS DOCTOR AT CHI SAINT JOSEPH HEALTH
HIGH RISK FETAL-MATERNAL HEALTH AT UOFL HEALTH
MENOPAUSE TREATMENT AT WOMEN FIRST OF LOUISVILLE
REDUCING MATERNAL MORTALITIES AT NORTON HEALTHCARE
Breast cancer screening is the key in early detection and subsequent treatment of breast cancer. With the addition of cutting edge AI-driven imaging software, our 3D mammography provides a more comprehensive view of breast tissue, offering radiologists a clearer image and enabling them to detect abnormalities with higher accuracy. This advanced imaging technology enhances the chances of spotting tumors at their earliest stages. One in eight women will be diagnosed with breast cancer in their lifetime, but with early detection, the five-year survival rate is more than 80 percent!
Earlier Detection
Only mammogram to detect breast cancer 15 months earlier.
Fewer Call Backs
Reduces unnecessary call backs up to 40%.
More Accurate
Finds 41% more invasive cancers than traditional 2D Mammograms.
Screening Locations
Bardstown
Flaget Memorial Hospital
4305 New Shepherdsville Road
Bardstown, KY 40004
Berea
Saint Joseph Berea
Merle M. Davis Digital Mammography Suite 305 Estill Street
Berea, KY 40403
Lexington
CHI Saint Joseph Health — Breast Care Center
Saint Joseph East Medical Office Building 160 N. Eagle Creek Drive, Suites 101 & 104
Lexington, KY 40509
CHI Saint Joseph Health — Breast Care Center
CHI Saint Joseph Health Office Park 1401 Harrodsburg Road, Suite C-45
Lexington, KY 40504
London
Saint Joseph London 1001 Saint Joseph Lane London, KY 40741
Mount Sterling
Saint Joseph Mount Sterling 225 Falcon Drive
Mount Sterling, KY 40353
Nicholasville
Saint Joseph Jessamine
Sandra J. Adams Digital Mammography Suite 1250 Keene Road
Nicholasville, KY 40356






























































In A Moveable Feast, Ernest Hemingway wrote: “Write the truest sentence that you know.” I was thinking about those words while putting together the Women and Children’s Health issue of MD-Update. The truest sentence that I can write is that I am very concerned about the health of Kentucky’s children and the healthcare that is available to Kentucky women.
We have many caring, well-trained practicing pediatricians, obstetricians, gynecologists, and gynecologic surgeons in Kentucky. A few of them are profiled in this issue. What concerns me is the health of our children, as discussed by Dr. Steven Stack, Kentucky’s commissioner for public health. Dr. Stack says that 24.6% of Kentucky’s children, 0 to 17 years old, are considered obese and that percentage is increasing. “That’s a worrisome trend,” he states.
I am also concerned about the reproductive care that women in Kentucky have access to, particularly high-risk maternal-fetal health. I am also concerned about the care that Kentucky doctors are allowed to provide in high-risk maternal situations. In more than one conversation over this last year, doctors have told me that current laws prevent the best practices that they were taught and have practiced for years.
Some encouraging news on healthcare legislation from this year’s session is recapped by our friends at KMA. Representative Kim Moser (R-64) sponsored several healthcare bills. In a show of white coats, Kentucky doctors went to Frankfort during the sessions to meet and talk with legislators. Details on page 4.
The annual golf tournament presented by the Lexington Medical Society Foundation was May 29th. By all accounts it was successful. Over $30,000 was raised, which the Foundation will distribute to area healthcare organizations and medical student sponsorships. We had decent weather, which in Kentucky means sunny, cloudy, breezy, cool, and the chance of rain all in five hours.

The next issue of MD-Update will be in September. The MD-Update editorial calendar is on the preceeding page. Look for your specialty. I’m looking for some good stories. I’m sure you have one to tell. Give me a call or shoot me an email.

MD-UPDATE
MD-Update.com
Volume 14, number 3 ISSUE #152
EDITOR/PUBLISHER
Gil Dunn
gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda DeBord
CONTRIBUTORS:
Jan Anderson, PSYD, LPCC
Gui Cozzi
Amber Laflin, KMA
Cory Meadows, KMA
Lyndsey neese, MD
Scott neal, CPA, CFP
Eric Riley
CONTACT US:
ADVERTISING AND INTEGRATED
PHYSICIAN MARKETING: Gil Dunn gdunn@md-update.com
Mentelle Media, LLC 38 Mentelle Park Lexington KY 40502 (859) 309-0720 phone and fax
Standard class mail paid in Lebanon Junction, Ky. Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington KY 40502
MD-Update is peer reviewed for accuracy. However, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
Copyright 2024 Mentelle Media, LLC. All rights reserved. no part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Please contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter. Thank you.
Individual copies of MD-Update are available for $9.95.

Until next time, all the best, Gil
Dunn Editor/Publisher MD-Update

SEND YOUR LETTERS TO THE EDITOR TO: Gil Dunn,
gdunn@md-update.com, or 859.309.0720 phone and fax




Minimally invasive gynecological surgery at Norton Women’s Care is for more than fibroids and endometriosis


BY AMBER LAFLIN, DIRECTOR OF GOVERNANCE AND POLICY ANALYST AND CORY MEADOWS, KMA DEPUTY EXECUTIVE VICE PRESIDENT AND DIRECTOR OF ADVOCACY
FRANKFORT The 2024 General Assembly adjourned on Monday, April 15, concluding the 60-day “long” session which began on Tuesday, January 2. Initially slowpaced and marked by limited bill introduction, multiple committee cancellations, and minimal floor action, the session eventually settled into a rhythm punctuated by intermittent starts and stops. Despite a record-breaking 1,218 bills filed, lawmakers opted for a more measured approach than in recent years, passing only 214 bills, including 25 bills enacted over Governor Beshear’s vetoes.

Building on momentum from last year’s legislative session, KMA’s legislative priority for the 2024 session was prior authorization reform. Following an op-ed by KMA and nine specialty societies urging Kentucky lawmakers to act on prior authorization this session, Rep. Kim Moser introduced House Bill 317, legislation proposing to eliminate prior authorizations for physicians who have historically been approved for a specific medication, procedure, or service 90 percent of the time. Due to insurance company opposition, KMA entered negotiations with insurers and other stakeholders in an attempt to reach a compromise. Negotiations ultimately reached an impasse, and a deal could not be reached before the end of the session. Senate Bill 270, the KMA-supported prior authorization companion bill introduced by Sen. Jason Howell, also failed to be considered in the Senate. KMA is extremely disappointed by House Bill 317 and Senate Bill 270’s failure to pass. However, the Association is encouraged by the overwhelming bipartisan support the
measure received and remains optimistic that with continued advocacy from our members and the public, as well as collaboration with lawmakers, this critical legislation, which proposes to streamline the prior authorization process and ensure patients have timely access to care will soon be enacted.
Although the prior authorization bill did not pass, lawmakers acted on a wide range of healthcare measures with which KMA had significant involvement.
Maternal & Child Health: Rep. Kim Moser introduced House Bill 10 to support maternal and infant health and reduce the high mortality rate for mothers in Kentucky. Nicknamed the “Momnibus,” the measure requires most health plans to cover pregnancy, childbirth, and postpartum care along with in-home treatment for substance use disorder. It also calls on most plans to cover labor and delivery costs and all services and supplies related to breastfeeding. The legislation was ultimately attached to Senate Bill 74, a separate bill on maternal health sponsored by Sen.
Shelley Funke Frommeyer that, among other things, establishes the Kentucky Maternal Mortality Review Committee as a permanent entity under the state Department for Public Health. The amended bill cleared both chambers and was signed by the governor.
Healthcare Workforce
Protections: House Bill 194, a measure by Rep. Kim Moser to address workplace violence against healthcare providers, successfully passed both chambers. The legislation expands assault in the third degree to cover harm to healthcare providers in a health clinic, doctor’s office, dental office, long-term care facility, or a hospital or hospital-owned facility. Another workforce measure, House Bill 159, sponsored by Rep. Patrick Flannery, provides immunity for healthcare providers from criminal liability for inadvertent medical mistakes committed while providing healthcare services. However, providers can still be held liable in cases of gross negligence or wanton, willful, malicious, or intentional misconduct.
Cannabis: Introduced as a follow-up to last year’s Senate Bill 47 that allows Kentuckians access to cannabis for specific medical conditions starting in 2025, House Bill 829, sponsored by Rep. Jason Nemes, addresses medicinal cannabis use for K-12 students, allows public and private schools to opt out of the program and requires schools to establish policies if they choose to participate. Additionally, the bill allows local governments to apply fees and opt out of the program, prioritizes hemp businesses, clarifies state inspection powers, and ensures the program starts on time.
Vaping & e-Cigarettes: Another bill sparking a great deal of discussion was House Bill 11, sponsored by Rep. Rebecca Raymer, which

From the business of health care to compliance to litigation defense, Sturgill Turner’s experienced health care and medical negligence defense attorneys provide comprehensive legal services to health care providers, hospitals and managed care organizations across the Commonwealth.
Put our experience to work for you. Sturgill, Turner, Barker & Moloney, PLLC ♦ Lexington, Ky. ♦ 859.255.8581 ♦ STURGILLTURNER.COM

imposes fines on wholesalers and manufacturers who engage in the distribution of tobacco products that have not been granted authorization by the FDA. The bill also establishes escalating fines on retailers selling authorized
products to individuals under 21. Another anti-vaping bill, House Bill 142, introduced by Rep. Mark Hart, bans all tobacco, alternative nicotine, and vapor products in Kentucky public schools. It also requires school districts to adopt disciplinary procedures for students who violate the bans. KMA policy supports a ban on the use of electronic nicotine delivery systems in locations where tobacco use is prohibited and encourages education for the public, especially youth, on the dangers of using electronic nicotine delivery systems.
Kratom: Lawmakers also acted to regulate kratom, an herbal substance frequently sold online and in convenience stores. House Bill 293, sponsored by Rep. Kim Moser, prohibits sales to people under 21 and provides guidelines for manufacturing and labeling the product. KMA policy supports a complete ban on over-the-counter sales of kratom in Kentucky.
Greater Access to AEDs in Schools: Sponsored by Rep. Ruth Ann Palumbo, House Bill 169 updates current state law by mandating all Kentucky school buildings, including elementary schools, house a portable automat-
ed external defibrillator (AED) in a public, easily accessible spot. This builds upon 2023’s House Bill 331 ensuring AED presence in middle and high school buildings and at school events. Additionally, House Bill 1, the one-time spending and investment bill passed this session, designates $2.5 million to the Department of Education for AEDs in public schools. KMA policy calls for AED education and instruction as part of CPR training and supports the increased availability of AEDs in public spaces throughout the state.
Cancer Detection and Screening : Continuing the state’s efforts in recent years to increase access to cancer detection and screening initiatives, House Bill 52, by Rep. Deanna Frazier Gordon, requires health benefits plans to cover preventive cancer screenings and tests without any cost-sharing requirements. Likewise, House Bill 115, co-sponsored by Reps. Kim Moser and Lisa Wilner, eliminates copays and cost-sharing requirements for high-risk individuals who need follow up diagnostic imaging to rule out breast cancer.


BY ERIC RILEY, HEALTHCARE CONSULTING DIRECTOR AND GUI COZZI, CYBERSECURITY PRACTICE LEAD
Data privacy and security have never been more important in a digital age where information flows freely. Despite warnings as recently as 2023 to enhance and bolster cybersecurity defenses, ransomware attacks continue, resulting in significant operational impact to all sectors of healthcare.
Recently, two major healthcare providers, Kaiser Permanente and City of Hope, found themselves in the spotlight regarding data privacy concerns. Let’s delve into what transpired and how these organizations responded.
Kaiser Permanente apologized to its vast network of 13.4 million members after discovering that certain search information may have inadvertently been shared with external platforms, including Google and social media sites. The company attributed this data transmission to previous online technologies installed on its websites and apps. While the shared information did not include sensitive details like names or financial information, it did encompass IP addresses, usernames, indi-
cations of account activity, and health-related search terms.
Upon identifying the issue, Kaiser Permanente promptly removed the problematic technologies from its online platforms and assured members that there had been no reported instances of personal information misuse. Nevertheless, the organization took proactive measures by informing all affected members, both current and former, about the incident. Additionally, they expressed regret for the oversight and outlined steps, guided by experts, to prevent similar incidents in the future.
In a parallel scenario, City of Hope, another healthcare provider, faced a data breach affecting its members. The breach, which took place between September 19 and October 12, 2023, involved unauthorized access to a large amount of member information, ranging from email addresses to sensitive data like Social Security numbers and medical records.
City of Hope responded swiftly upon dis-

covering the breach, implementing mitigation measures and bolstering security protocols with the assistance of cybersecurity experts. Furthermore, they extended a gesture of goodwill to affected members by offering two years of free identity monitoring services. In tandem with this, they promptly notified relevant authorities, including law enforcement and regulatory bodies, and launched an internal investigation into the incident to ascertain its scope and impact.
Cybersecurity is an urgent issue in healthcare, but the risk is growing exponentially and it’s poised to keep rising with no signs of stopping. Consequently, the expansive landscape of healthcare creates additional vulnerabilities where data attackers can outpace your organization, disrupting patient care. What steps is your organization taking to prepare?
Contact Dean Dorton for expertise in healthcare, cybersecurity, and the dynamic place where they intersect. Contact Eric Riley at eriley@ddafhealthcare. com. Contact Gui Cozzi at gcozzi@ddaftech.com
Empowering physicians to focus solely on the demands of their clinical practice.


With the dramatic increase in the federal estate tax exemption in 2018, (now standing at $12.92 million) we have witnessed a decreased interest in doing effective estate planning. That’s too bad, because reducing or avoiding estate taxes is only one benefit of effective estate planning. Providing for and protecting assets for those you care about is a critical aspect of financial management, and often gets short shrift by busy professionals. The nature of medical practice, with its demanding schedules and high-stress environment, can make it difficult for physicians to find the time to focus on their personal financial affairs. However, estate planning is essential for ensuring that one’s assets are protected and distributed according to their wishes. It’s important to know that if you do not have an estate plan, the state has one for you.
Estate planning is the process of organizing and managing an individual’s assets in the event of death or incapacitation. It involves the creation of legal documents that outline the management and distribution of assets, the care of minor children, and healthcare directives. For physicians, who often have significant and complex financial portfolios, estate planning is particularly important.
A will is a legal document that specifies how a person’s assets should be distributed after their death. For physicians, a will ensures that their wishes regarding the distribution of their estate are honored. Without a will, the state’s intestacy laws will determine the distribution of assets, which may not align with your intentions. It is vitally important that the will be properly drafted by experienced legal counsel, preferably one who specializes in estate planning.
BY D. SCOTT NEAL, CPA, CFP
Trusts can be another critical component of estate planning. A trust is a fiduciary arrangement that allows a third party, or trustee, to hold and manage assets on behalf of beneficiaries. Trusts can be particularly beneficial for physicians because they can help manage and protect assets during the physician’s lifetime as well as postmortem. Trusts can also provide tax advantages and help avoid probate, a time-consuming and often expensive legal process.
A power of attorney (POA) is a legal document that grants a designated individual the authority to make financial and legal decisions on behalf of the physician. Physicians, given the high-risk nature of the profession and potential for unexpected medical events, should have a durable power of attorney in place. This ensures that their financial affairs are managed according to their wishes, even if they are unable to do so themselves. You can add “springing powers” to a POA that will trigger its use only if certain, pre-defined events occur.
Healthcare directives, including living wills and healthcare powers of attorney, are perhaps less essential components of an estate plan for someone in healthcare, but should still be considered. A living will outlines the maker’s preferences for medical treatment in the event he or she becomes unable to communicate their decisions for themselves. A healthcare power of attorney designates a trusted individual to make healthcare decisions on the maker’s behalf. These directives ensure that your medical preferences are respected, while also reducing the burden on family members during difficult times.
Physicians should regularly review and update
beneficiary designations on life insurance policies, retirement accounts, bank accounts, and other financial instruments. These designations take precedence over instructions in a will, so it is crucial to ensure they are current and reflect your wishes. Horror stories abound in the financial planning literature telling of significant sums being left to unintended beneficiaries because a designation was made years ago and never updated.
While the exemption for federal estate taxes is presently high, the increased level of exemption is scheduled to end in 2025. Congress will have to act to extend it. We see clients expend a lot of energy to reduce income taxes, but tax planning requires optimizing strategies to reduce estate, gift, and income taxes. This might include setting up trusts, making charitable donations, and utilizing lifetime gift exclusions.
Hopefully, you have been or will be able to accumulate rather significant assets over the course of your career. Proper estate planning ensures that these assets are protected and efficiently transferred to heirs, minimizing the impact of estate taxes and legal fees.
Sorry to remind you, but being at higher risk of malpractice lawsuits exacerbates the need for excellent legal documents. Estate planning can include asset protection strategies to shield personal assets from potential litigation. Establishing trusts and other legal structures can help protect a physician’s estate from creditors and legal claims, ensuring that their assets are preserved for their intended beneficiaries.

For physicians who own their practice, succession planning is a critical aspect of estate planning. Succession planning ensures that the medical practice continues to operate smoothly after the physician’s retirement, untimely death, or disability. This involves identifying and training a successor, outlining the terms of the practice’s transfer, and ensuring that the practice’s value is preserved for the physician’s estate and his or her dependents.
While not unique to physicians, many professionals often face complex family dynamics, such as blended families, dependent children, or family members with special needs. Effective estate planning can address these complexities by creating tailored solutions that provide for each family member according to unique needs. This might include setting up special needs trusts as well as ensuring adequate guardianship arrangements for minor and / special needs children or other dependents.
It is never too early to start estate planning. Everyone should begin planning as soon as they start their careers to ensure their assets are protected and their wishes are documented. Early planning also allows physicians to
take advantage of tax-saving strategies and accumulate wealth in a structured and efficient manner.
Estate planning can be complex, particularly for people with substantial and diverse assets. Consulting with estate planning attorneys, financial advisors, and tax professionals is crucial. These experts can provide tailored advice, ensure compliance with legal requirements, and help create a comprehensive and effective estate plan tailored to your unique circumstances, wishes, and needs.
Life circumstances change, and estate plans should be reviewed and updated regularly to reflect these changes. Physicians should certainly revisit their estate plans after major life events, such as marriage, divorce, the birth of a child, or significant changes in their financial situation. But a periodic review by a professional will make sure that you are taking care of changes in law and that the documents remain aligned with the current wishes and needs.
Open communication with family members about estate planning can prevent misunderstandings and conflicts. You should discuss your estate plans with your spouse, children, and other key family members to ensure that
everyone is aware of your wishes and understands the reasoning behind your decisions. This transparency can ease the execution of the estate plan and provide peace of mind for both the physician and loved ones.
Estate planning is a vital aspect of financial management for practicing physicians. It provides a structured approach to asset protection, tax minimization, and the provision for loved ones. Given your unique circumstances: high earning potential, risk of malpractice lawsuits, and the importance of retaining value in a medical practice for the benefit of colleagues and employees as well as heirs, there is a good chance you should prioritize estate planning as an integral part of your professional and personal life. By starting early, consulting with professionals, regularly updating plans, and communicating with family members, you can ensure that your estate is managed and distributed according to your wishes, and not merely that of the government. Besides that, your heirs will remember you more fondly if you leave them well prepared.
Scott Neal, CPA, CFP®, is the president of D. Scott Neal, Inc., a fee-only financial planning and investment advisory firm with offices in Lexington and Louisville. He has been serving physicians for over 40 years and can be reached at scott@dsneal.com or 1.800.344.9098.


“One of the next things when it comes to surgery is augmented reality or AI.”
— Steven Radtke, MD

By LIZ CArey
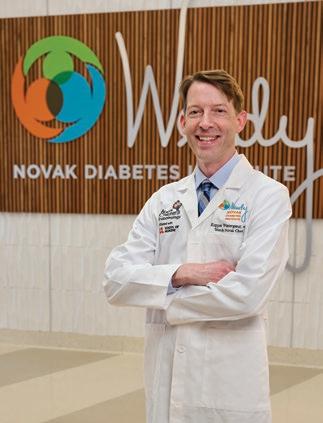
LOUISVILLE Advancements in minimally invasive gynecological surgery are changing the way patients and doctors perceive the procedure, say Jonathan Reinstine, MD, and Steven Radtke, MD.
Reinstine is the medical director at the Center of Excellence for Minimally Invasive Gynecology at Norton Women’s Care, where Radtke is a surgeon. Radtke is Reinstine’s successor, the two doctors say, and will ultimately take over the directorship.
Reinstine says that advances in the practice of minimally invasive gynecological surgery, or MIGS, are making the procedure more commonplace while expanding its use. Now applicable for more than just fibroids or endometriosis, the future of MIGS will help doctors treat more than just the gynecological aspects of pelvic pain.
Reinstine is a gynecologist with Associates in Obstetrics & Gynecology, part of Norton Women’s Care. After earning his medical degree from the University of Virginia in Charlottesville, he completed his residency at the University of Louisville where he is now a clinical professor in the school’s Department of Obstetrics, Gynecology and Women’s Health. He also serves as the associate director of fellowship in Minimally Invasive Gynecology.
Radtke earned his medical degree from Instituto Tecnológico y de Estudios Superiores de Monterrey, Mexico, and completed his OB/GYN residency at Southern Illinois University School of Medicine in Springfield. After completing his fellowship in MIGS at the University of Tennessee College of Medicine in Chattanooga, where he trained in advanced laparoscopic and robotic surgery, Radtke served as the chief of minimally invasive gynecological surgery at Texas Tech University Health and Sciences Center in El Paso before coming to Louisville and Norton Urogynecology Center.


Reinstine says “Over my 40 year career, MIGS has changed dramatically.”
“Back in the late 80s and early 90s, we were kind of winging it; we were creating it,” he says. “We didn’t have the instrumentation that we have now. Many of the surgical specialties
now embrace minimally invasive surgery for what it is. The instrumentation is fantastic.”
Patient knowledge of the procedure has also changed. Now, he says, patients with pelvic pain may go to their doctors and request a minimally invasive approach. “We have been able to utilize laparoscopic, hysteroscopic, or robotically-assisted procedures.”
“Robotics for gynecology was introduced in about 2004 after it was FDA approved,” says Reinstine. “It is only one of the options we have, but it can bring some components to the table on certain cases such as for cancer and advanced endometriosis.”
MIGS provides care for what is a growing problem, says Radtke.
“Prior to fellowship, I practiced general OB/ GYN for a couple years, and during that time I identified that resources were limited when it came to managing chronic pelvic pain conditions, which is a huge issue,” says Radtke.
In Radtke’s experience, endometriosis is the culprit in about 70% of patients experiencing pelvic pain. “This condition is way more than just a nuisance,” he says. “It can completely impair a patient’s quality of life. Even though there has been great progress in developing new medications to treat endometriosis, these are not always effective. Also, we see patients that want to address the problem without being committed to taking prescription meds indefinitely.
“When we proceed with surgery, the first thing we get is an answer. Inspecting the inner lining of the pelvis allows us to spot any abnormal areas suggestive of endometriosis and corroborate our suspicion as to the source of the patient’s pain. In the past, it was thought that endometriosis could be treated by superficially burning the lesions. Now we know that excising them is significantly more effective in terms of resolving the patient’s pain and decreasing the risk of recurrence. Furthermore, we often find implants on critical areas such
as the rectum, ureters, bladder, around major vessels, etc., which can’t be cauterized without injuring the underlying structure. This is where the specialty of MIGS comes in.”
MIGS practitioners are also trained to fully take advantage of new surgical technologies such as advanced laparoscopic instruments and robotic surgery.
“The mantra of the specialty is to solve a patient’s problem while minimizing the effect on surrounding tissues,” says Radtke. “For instance, markedly enlarged fibroid tumors that traditionally required a large abdominal incision to address can now be surgically managed via laparoscopy. This allows patients to return to normal life within a few days and markedly reduces long term risks such as infections, DVTs, hernias, scar tissue, etc. Most of our patients don’t even have to stay overnight in the hospital.”
Sometimes, Reinstine says, the results exceed expectations.
In one case, a patient who wanted to have children came to Reinstine with massively large fibroids. After extensive laparoscopic myomectomies, the patient did not get pregnant, he recalls. However, the patient opted to have a uterine artery embolization, a procedure not recommended for patients planning on getting pregnant.
After the procedure, while her symptoms improved, the patient experienced irregular periods. Reinstine says they discovered the patient was pregnant. After delivery through cesarean section, the doctor also discovered a fibroid inside of her uterus the size of the baby’s head.
After recovering from the cesarean section, she returned to Reinstine and asked for another fibroid embolization. Despite that procedure, the patient was able to get pregnant again and deliver another healthy baby.
“I think in a general sense for MIGS, patients are very relieved that a minimally invasive approach is possible for them. Thanks to recent advances, there is almost no situation where a problem cannot be solved via a minimally invasive technique,” says

“Sometimes the results exceed expectations.” - Jonathan Reinstine, MD
Radtke. “And I think that patients after surgery are very pleased, because the pain profile is so much better than what they expected. When we see them for their two-week postop check, most patients will tell us they only needed pain medications for one or two days.”
Reinstine said doctors’ attitudes about pelvic pain, and recognizing that female pelvic pain isn’t limited to gynecological issues, is an advancement for the field.
“So often it is assumed that pelvic pain is gynecological, but there can be so much more: gynecological, urogynecological, gastroenterological, musculoskeletal, and neurological,” he says. “What we’re doing now is evaluating all sources. This idea that women come back every one or two years to have a touch-up surgery for endometriosis is something we really need to get away from. We really can do a lot more than we used to and we have to consider multi-modal treatment plans to cover all bases.”
Both doctors said there needs to be a shift in patients’ view of pain as a symptom as well, and not just another aspect of life.
“I think most physicians are pretty good at knowing that pelvic pain is not normal,” says Radtke. “When we talk to patients, the main message is that pelvic pain that is interfering with their quality of life is not normal. Being incapacitated for seven to ten days out of the month during a menstrual cycle is not
normal. Luckily, there are options available to help with this.”
The future of MIGS, Reinstine says, lies in complex benign gynecology.
“One of the limitations for gynecologic surgeons is that we generally don’t operate on the bowel, and we generally don’t operate on the urinary tract. One of the reasons why the oncology surgeons will sometimes get tapped for benign cases is because they do operate on the urinary tract, and they do operate on the bowel,” he says. “At a national level, there’s a real push now for those of us in advanced benign gynecology to be able to do that. So complex benign gynecology, I think, will be the next phase of our fellowship, so that our trainees will be able, for example, to take care of rectal endometriosis. Or to be able to take care of invasive endometriosis into the bladder.”
The future will also be high-tech, Radtke says.
“One of the next things when it comes to surgery is augmented reality or AI. It’s not available yet, but it’s on the horizon,” Radtke says. “During laparoscopic or robotic surgery, the screen will have overlays that are assisting the surgeon, saying, ‘That area is highly suspicious for endometriosis,’ or ‘the appendix looks abnormal.’ It’ll basically be another set of virtual eyes to help surgeons not miss things.”
When there is innovation in MIGS, the surgeons at the Center of Excellence for Minimally Invasive Gynecology at Norton Women’s Care will be ready.

We’re proud to have been named the No. 1 Children’s Hospital in Kentucky and among the best nationwide in six pediatric specialties: Cardiology and Heart Surgery, Diabetes and Endocrinology, Neurology and Neurosurgery, Orthopedics, Pulmonology and Urology.
Norton Children’s remains committed to expanding access to pediatric health care throughout the region with three campuses, six regional outpatient centers, satellite locations and over 500 pediatric primary and specialty providers.
To make a referral to a Norton Children’s provider, call (502) 559-7337 (PEDS) or visit NortonEpicLink.com.
The certified experts at Women First Louisville are empowering females to thrive during menopause and beyond.
BY DONNA ISON
LOUISVILLE Previously, menopause was with politics and religion as a topic not fit for polite discussion. Even though every woman who reached midlife will contend with menopause, it remained a taboo topic. Fortunately, with the rise of online information and emergence of organizations like The Menopause Society, women are reaching new levels of awareness and access.
The Menopause Society, formerly known as The North American Menopause Society, was founded in 1989. It provides resources for healthcare providers and the public offering certification to individuals, identifying them as trusted experts in the menopause space. Kelli Miller, MD, OB/GYN, and Audrey Fenwick, PA-C, of Women First of Louisville are both Menopause Society Certified Practitioners (MSCP). They are using their expertise to dispel the myths surrounding menopause and to provide leading-edge education and the latest treatment options.
Miller completed her undergraduate education in biology and chemistry, and then her medical degree and training in obstetrics and gynecology at the University of Louisville. In 2002, she joined Women First. Miller’s primary passions are menopause medicine, hormonal wellness, and pelvic floor disorders including incontinence and prolapse.
Miller saw menopause care as an unmet need in the community of women she served. “In our medical and residency training, most training is about pregnancy, puberty, contraception. We get very little education in menopause care, despite the fact that we spend 40% of our lives in the menopause age range. I wanted to get more education to better inform my patients,” she says.
Fenwick shared this sentiment: “Menopause and sexual health are two areas in which women were not being heard, and solutions were not being presented and I wanted to go into that field.” To become part of the solution, Fenwick entered the Master of Science in Physician Assistant Practice at Rosalind Franklin University of Medicine and Science in North Chicago, Illinois. She worked at both the Northwestern Medicine Center for Sexual Medicine and Menopause and the Center for Complex Gynecology before entering her current position with Women First, where she focuses on menopause management and sexual health.
MYTH 1 Menopause just means hot flashes. Though hot flashes and night sweats are the most publicized symptoms, there are a host of other complaints that accompany menopause, including sleep disturbance, brain fog, fatigue, joint pain, weight gain, lower libido, vaginal dryness, heightened anxiety, and worsening depression. According to Miller, “Loss of estrogen affects pretty much every body organ system. And in 15% of women, the symptoms persist for all their life and not just a year.”
MYTH 2 Menopausal women must simply suffer in silence.
“For years and years—generations and generations—menopause went untreated or undertreated. Women stopped asking for help,” says Fenwick. Many women, and some primary providers, see the symptoms of menopause as a normal part of aging to be endured without complaint. According to Fenwick, “Women tell themselves, ‘I can just muscle through it and take what’s thrown at me.’ But we know that hot flashes and night sweats, alone, raise
our cardiovascular risk. This is something that needs to be treated. Quality of life doesn’t have to be compromised.”
Miller adds, “As I entered perimenopause, and now menopause, I didn’t feel there was a lot of information out there. We were told to just suffer in silence through the changes. There was not a lot of awareness about treatment; so I wanted to educate myself on the options and the science and data.”
MYTH 3 Hormone replacement therapy is dangerous.
This myth started with a 2002 study, referred to as the Women’s Health Initiative. Miller states, “A large study was published in 2002 that did a great disservice to women, because it showed an increased risk of breast cancer, heart attacks, blood clots, and strokes in women on hormone therapy. This caused a lot of media attention, outrage, and fear, which caused many women to stop taking hormone therapy and prescribers to stop prescribing it. It’s taken 20 years to get follow-up data from that study to refute those findings.”
The 2002 study utilized patients approximately 65 years old, which is much older than the typical menopausal age, and administered conjugated equine estrogens and a synthetic progestin (Provera), though both are less commonly used now, having been replaced by bioidentical hormone therapy, often using transdermal rather than oral estradiol to mitigate blood clot and stroke risk.
In their 2017 Hormone Therapy Position Statement, based on recommendations of an advisory panel of clinicians and researchers, The Menopause Society reported that, for vasomotor symptoms (VMS) and the genitourinary syndrome of menopause, hormone therapy is still the most effective treatment.1 In addition, there are actual health benefits


for women who adhere to hormone therapy. Fenwick points out, “It can reduce colon cancer risk, dementia risk, heart disease, and osteoporosis. Estrogen also reduces our breast cancer risk.”
Miller, Fenwick, and the other practitioners at Women First—a distinctly all-female practice—are committed to addressing these misconceptions and providing the most comprehensive and innovative obstetric, and gynecology care to females in every stage of life. This often starts with an in-depth conversation. Fenwick states, “When they first come in for their appointment, I try to learn about them, personally and professionally. Much of my time is really spent getting to know the patient and, specifically, learning about their goals for the appointment.”
These discussions should ideally start well before the onset of menopause. According to Miller,
“The average age of menopause is 51, but I like to start in the 40s, or even 30s, discussing hormone health and the decline of our ovarian hormones, how we feel with that decline, and talking through the bodily changes, physical and emotional and mental, that go along with that decline.”
Fenwick adds, “It’s very important to me to create an environment where shared decision-making is key and we talk about all the treatment options that are available. I try to be very fair and balanced. I lay out all the options that have been FDA-approved and things that may be used off-label. We discuss the risks and benefits of each of them. Then, the patient is able to make an informed decision on their treatment.”
In the past years, thanks to dedicated menopause experts, accurate articles, and the media no longer avoiding the topic, menopause has become much more widely discussed, leading to the sharing of invaluable information with the ultimate goal of women living their best lives well beyond fifty.
States Fenwick, “I went into this to make women feel heard, to educate women, and really maximize quality and quantity of life. Two thirds of our lives are spent in perimenopause and menopause, and I really want to help people to maximize that quality.”
In closing, Miller echoes, “I’m here to educate women that they’re not alone. They should communicate and find a provider that is supportive. They can get in the best shape of their life—body, mind, and spirit—by embracing the transition…because it is a fantastic transition. The 50s are probably the best time of my life, honestly.”

Because our patients deserve the best care at all stages in life.
At Women First, menopausal care is an essential part of what we do. That’s why we have two nationally certified menopause practitioners (NCMPs)
Dr. Kelli Miller and Audrey Fenwick, PA-C, focus on hormonal wellness with patients, delivering individualized care plans to help manage symptoms throughout each phase of menopause.
If you have patients struggling with menopause, refer to Women First for personalized care.


In addition to caring for patients, Tiffany Tonismae, MD, FACOG, is an assistant professor in the Department of Obstetrics, Gynecology and Women’s Health with the University of Louisville School of Medicine.
BY JIM KELSEY
LOUISVILLE Tiffany Tonismae, MD, FACOG, joined UofL Physicians – OB/GYN & Women’s Health on May 31, 2023. Though her time at UofL Health has only been a few months longer than a pregnancy, it is already safe to say that she has delivered in her new role. Tonismae is a maternal-fetal medicine and high-risk obstetrician specializing in high-risk pregnancies along with her partner Edward Miller, MD.
“There’s only two of us, but we have nurses, medical assistants, general OB/GYNs, and 24 residents that are all working as a team to provide care for not just Louisville, but the state of Kentucky and southern Indiana,” says Tonismae, who is also an assistant professor in the Department of Obstetrics, Gynecology and Women’s Health with the University of Louisville School of Medicine.
Tonismae grew up in South Carolina and was inspired by a local physician at an early
age to pursue a medical career. She earned a bachelor’s bachelor’s degree from Wofford College, then attended the University of South Carolina School of Medicine. She did her internship and residency in obstetrics and gynecology at Virginia Tech Carilion; then she completed a maternal-fetal medicine fellowship at Indiana University School of Medicine.
Tonismae continued her career at Johns Hopkins All Children’s Hospital in Saint Petersburg, Florida, for four years. Over time, she came to realize that she missed the teaching component of her work and looked for other opportunities. With some friends and family in Louisville, she found UofL Health to be a logical fit.
“I just fell in love with the setup and structure,” she says. “I spend a lot of time with students, with residents, teaching every single day, but I also still get a moment to have some private time with patients. It’s the best of both worlds.”
Due to the extremely serious nature of the care Tonismae provides, patients have many questions along with fears and anxieties. Tonismae says patients usually are referred to her because there is something abnormal on the ultrasound, something wrong with the fetus, or the mother has a medical condition that creates higher risk. She also does preconception visits with women who are at a high risk for complications and want to optimize their health before they get pregnant.
“There’s a lot of anxiety when people come to see me because there’s usually something going on,” says Tonismae. “My first step is to try to make people feel comfortable. I always start with making sure they know why they are there to see me. I want to make sure that what their OB is concerned about is the same thing they are concerned about.”
Sharing duties with Miller, Tonismae is on call every other week, covering the hospital consults and doing the rounds in the morning, followed by any scheduled deliveries or procedures. The afternoons are usually spent in the clinic.
Tonismae performs cesarean sections, cervical cerclages, high-risk deliveries, breech babiesdeliveries, and hysterectomies. Her patients present with a wide range of potentially serious issues, including hypertension, history of transplants, history of trauma such as gunshot wounds during pregnancy, thyroid disorders, advanced maternal age, and obesity.
Mental health has also become a more prevalent factor in high-risk pregnancies. Accordingly, Tonismae sees patients with anxiety, bipolar disorder, depression, and PTSD.
“We are finally getting the message out there that it’s OK to not be OK, but you have to be willing to talk about it and seek help for it,” says Tonismae.
Along with increased mental health awareness, other advancements in maternal healthcare include the use of technology such as ultrasound and MRI. Tonismae says that, when ultrasounds are limited, an MRI can reveal vital information, such as specific anat-
When it comes to banking for physicians, we’re just what the doctor ordered.
Republic Bank specializes in personal and private practice banking solutions for physicians.
Lexington
Patricia Morgeson (859) 519-3369
NMLS ID # 827418
Louisville
Gary Spence (502) 588-1595
NMLS ID # 1087080

Here are just a few of the medical banking solutions we offer:
• Special Home Loan Programs
Reduced closing costs* and exclusive financing options for Medical Residents and Physicians employed at participating programs**.
• Business Banking for Private Practices
This includes lines of credit and equipment financing.
• Treasury Management Business on-site deposit and remote deposit capture, as well as lockboxes.
• Online Banking & Mobile Deposit**
Because your time is too important to spend on a trip to the bank.
*Reduced closing costs is defined as $500 lender credit towards closing costs. To be eligible for the reduced closing costs applicants must have opened or open a primary checking account with Republic Bank and use this account on a regular basis until the Loan is paid in full and closed. To qualify as “Primary” checking account, the Account must be opened with a minimum of $50.00 and used on a “regular” basis. The term “regular” is defined by the following activity requirements: Minimum of one credit or deposit into the account per month through direct deposit or at any of Republic’s banking centers or ATMs; and establishing a recurring direct deposit within thirty (30) days of account opening if Borrower is employed at the time of the Loan closing or within thirty (30) days of Borrower’s employment start date, whichever may occur first; and Making five (5) or more payments or debits per month through the Account (this requirement may be met through ATM withdrawal, debit card usage, ACH or checks); and Borrower’s regular Loan payment must be withdrawn from the Account, in accordance with all terms set forth in the Authorization Agreement for Direct Deposits. For more detail, please ask about the Promotional Closing Cost Program Participation Agreement.
** To be eligible for the reduced closing costs Medical Residents and Physicians must have executed employment contract with one of the following programs: University of Louisville, University of Kentucky, University of Cincinnati, University of South Florida, Vanderbilt University, St. Elizabeth Medical Center, Children’s Hospital Cincinnati, Hospital Corporation of America, St. Thomas Hospital, Tri-Health Inc., Baycare Medical Group, The Christ Hospital Network.
omy of the brain and how the placenta interacts with the uterine wall. Another significant advancement is genetic testing.
“Thirty years ago, the only option to get answers beforehand was to do an invasive procedure that put you at risk of losing the pregnancy,” says Tonismae. “Now I can send the mom to get some blood drawn and I can give her some pretty good specifics about her risk of having abnormalities with the pregnancy. That has made people a lot more comfortable and has made genetic screening more available for every patient in pregnancy.”
While helpful, the results of these screenings aren’t always good. The conversations aren’t always easy. The decisions can be even harder, particularly in the modern political climate.
“When I first started here, we had a patient whose blood screening tests showed an abnormality in the baby’s chromosomes,” says Tonismae. “An ultrasound showed multiple abnormalities. She had an invasive screening test to prove what we suspected. Because of that test we were able to get consults from other subspecialists before she delivered. We
were able to talk about delivery in a way where she would get closure because, unfortunately, this baby was not going to survive. A lot of our conversations were geared toward what were her goals for delivery and what she wanted it to look like for her child.”
Tonismae continues, “One of the things she said to me was, ‘I want to be able to hold my child while my child is still living and I want to do everything I can to make my child comfortable.’ We were able to have specialists available at delivery and have everything scheduled. She had other children at home, so we were able get pictures, get mementos, record baby’s heartbeat, get her pictures for her family to have afterwards. If we didn’t know all of this beforehand, that baby probably would have been swiftly swept away to the NICU and mom may not have had a chance to really see the baby before the baby passed.”
Even on the hardest of days, Tonismae tries to help her patients find a silver lining.
“When it’s bad news, the patient’s first
emotions are always fear, anger, and sadness,” says Tonismae. “When you see them come back, you watch those emotions evolve. They are not afraid, because they have a better understanding. They may still be sad, but they are happy with the plan. They may still be angry, but a lot of them have turned that anger around into helping other people in their same situation. My favorite thing is when somebody comes in, gets bad news, and when I see them postpartum, they tell me that they joined a support group and they shared their story. They helped somebody else in their same situation. That’s what is going to make it a better world. We are not just here for ourselves. We are here for everybody who comes after us.”

BY GIL DUNN
LEXINGTON For Alexander Hernandez, MD, faith, family, and fate all played a role in his journey to become a “Meds and Peds” family practice provider at CHI Saint Joseph Health - Primary Care in Lexington, Kentucky. His faith is the backbone of his patient care approach, being open to discussing his patients’ spiritual health as well as their physical conditions. He met his wife, Alyson, through their church. His father was a doctor, and Hernandez recalls following him doing hospital rounds in Miami as a young boy,
albeit without much youthful enthusiasm. He would rather have been playing baseball.
Hernandez, an internal medicine and pediatrics physician, grew up in Florida and completed his undergraduate education at the University of Central Florida, earning a BS in molecular biology and microbiology.
Hernandez credits his father, along with his seventh-grade science teacher, for sparking his early interest in science and medicine.
“I was fascinated with how the human organs work in the body, the way the heart works, the way the gut works,” says Hernandez. “The more I studied, the more I realized that
I’d be able to use that knowledge for good and help people. Now it’s all about getting to know my patients on a level where I can build the type of relationship with them where they never feel as if they’re being ignored.”
He came to Kentucky after attending Loyola University Chicago – Stritch School of Medicine, where he also earned his Master of Science in medical physiology. After matching for his residency program at UK in 2022, Hernandez said he fell in love with the people of Kentucky, and the community holds a special place in his heart because it’s also where he met his wife.

His UK residency gave Hernandez the serendipitous opportunity to work in a community outreach program hosted by CHI Saint Joseph Health, which led to being offered a position in primary care with the multi-pronged task of developing a “Med & Peds” practice that welcomed the Central Kentucky Hispanic population because Hernandez is fluently bilingual.
As someone who has been a camp counselor and worked on mission trips, Hernandez says he knew he wanted to work with kids. But his focus on becoming a “med-ped” was to make sure that the relationship didn’t end when his pediatric patients turned 18. They can still turn to him as a primary care doctor. Because he speaks both Spanish and English, Hernandez says he hopes to connect with people who often face hurdles in obtaining healthcare.
In May 2015, as a 1Y medical student, Alexander Hernandez and a classmate worked at a makeshift clinic in Guatemala in a building where the students addressed general health concerns of the local population and provided some resources.

It is Hernandez’s intention to build a multigenerational family practice, from infancy through adolescence and adulthood. By caring for the different generations, Hernandez believes he will be able to more fully understand and treat the entire family’s health concerns. “Knowing the medical history and health conditions of parents or grandparents will give me insights into the health of the children,” he says. Diet, lifestyle, habits, both good and bad, possible inherited conditions, and family dynamics all play a role in the health of a family. “I want my patients to know that I’m someone they can trust, that I have their best interests as my priority,” he says.
Having been in practice for a little over a year, Hernandez has watched his patient population steadily take shape: 70 percent adults and 30 percent pediatrics with about 20 percent of his patients being Hispanic. His adult patients present with typical problems of diabetes, COPD, hypertension, and gout. His pediatric patients can start as early as two weeks old and run through 18 years old. Some aspect of childhood obesity is frequently present, and Hernandez is quick to point out that “body shaming” in overweight children is a problem he addresses with understanding and compassion. “We encourage small, but important changes in their eating habits, eating more fruits and vegetables, limiting soda and sugar-filled drinks, getting more active,” he says. Some of Hernandez’s Hispanic patients are bilingual, some speak only Spanish. “When my Hispanic patients learn that I can speak their native language, a bright light goes on in their faces. They are so relieved that they’ve found someone who can understand them easily, not condensed or translated by a family member. Some of them want to give me a hug, they’re so happy,” says Hernandez. “We start our doctor–patient relationship with a basis of trust built on common language and cultural understanding.”
Going on medical mission trips to Panama in high school and Guatemala as a medical student was inspiring and informative for Hernandez. The experiences confirmed his intentions to be a caregiver and showed him first-hand the differences in healthcare found in the United States and Latin America. He recalls that on one of his mission trips that applying a simple medication and treatment for head lice in children was a significant act of care.
Another challenging aspect of healthcare for the newly arrived, Hispanic-speaking patients is how completely different the structure of healthcare systems are in the U.S. from Latin America. “Clinics in some parts of Latin America are much more informal,” says Hernandez. “In Cuba, for instance, it’s sometimes one large room with a doctor sitting at his desk and a row of chairs. Everyone sits in line, waiting their turn to talk to the doctor. In other areas of Latin America, such as in Mexico, clinics are informal compared to here, and patients may have their provider’s contact information readily available to text or call, but patients still have their privacy respected in clinics. Family medicine in Latin America is sometimes really just one big family event,” says Hernandez.
While some Latin American countries like Mexico have more advanced healthcare and access to specialists and medications, some countries like Cuba, says Hernandez, are less
advanced and more restricted. He notes that he is seeing an increase in his Cuban patient population. Word seems to be spreading that there’s a Spanish-speaking doctor in town. “I tell all of my Hispanic patients to tell their family, friends, and coworkers that we’re here for them,” says Hernandez.
Primary care is similar to ER care, says Hernandez, in that he feels that he is on the front line. “I want to be the doctor who keeps people healthy and out of the hospital. But if a hospital stay is needed, to provide the medical history of their care for my hospitalist colleagues,” he says.
Hernandez says, “My philosophy with my patients ties into my faith. I want any patient that comes to me to understand that they are loved and cared for, and I am always here for them. Sometimes the process of receiving treatment can feel like it’s taking a long time, but I hope to communicate with my patients, in the best way that I can, to help them get through whatever it is they’re facing, reminding them of God’s mercy even in the most difficult of times, which is often when I see my patients.”
CHI Saint Joseph Health is a faithbased healthcare system, founded in 1877 by the Catholic Sisters of Charity of Nazareth in Kentucky, with a mission to provide compassionate care to the poor and underserved. It seems like a good fit for Alexander Hernandez.

859.629.7245
LOUISVILLE Kentucky’s most recent Maternal Mortality Review reports alarming statistics about pregnancy-related deaths. Nearly 90% of these deaths are preventable, and substance use is linked to death in more than 50% of cases. In more urban areas, pregnancy-related deaths of Black women are more frequent than deaths of white women. In Kentucky, many women have hypertension or it is acquired during pregnancy or the postpartum period, causing significant morbidity. These statistics should be a call to action for all healthcare workers caring for women of childbearing age.
At Norton Healthcare, we are using innovative programs to respond to many maternal mortality issues. We have chosen to tackle this challenge using a comprehensive approach to patient-centered care. Highlights of our current efforts include improving care for pregnant patients with hypertension or those at risk for preeclampsia; implementing a doula program for underserved patients; continuing our Maternal Opiate and Substance Treatment (MOST) Program; and increasing our work in health equity.
BY LYNDSEY D. NEESE, MD, MMM, CPE, FACOG

Healthcare Foundation, Norton Children’s Hospital Foundation from donors such as Aetna Better Health of Kentucky and Edie Nixon. Our doulas are trained professionals who provide physical and emotional support before, during, and immediately after childbirth. Their patient focus is on populations considered underserved. This kind of intervention is evidence-based, with a broad range of positive outcomes, including but not limited to shorter labor, increased satisfaction with the birthing process, and reduced cesarean section rates.
In 2023, we began a cardio-obstetrics program that offers integrative care by cardiologists, maternal-fetal medicine physicians, and obstetricians for patients with heart disease and hypertension. Last year, we added a virtual hospital program for postpartum patients with hypertension.
One of the largest preventable causes of maternal mortality is hypertension, which accounts for 16% of maternal deaths in the United States. In addition to increasing the risk for preeclampsia, eclampsia, and stroke during pregnancy, many patients also deliver preterm due to these complications. We also know that having preeclampsia increases the likelihood of developing heart disease, diabetes, renal disease, and hypertension — all of which are rampant in Kentucky.
In 2021, we began a comprehensive program for hypertension and preeclampsia prevention. The program involves providers and patients receiving education on the benefits of low-dose aspirin to prevent preeclampsia. The previous year, we collected our prescribing rate for low-dose aspirin therapy for our patients. After education, we have seen a fourfold increase in the prescribing rate.
The program also includes using doulas to support prenatal care for our underserved patients with hypertension to encourage follow-up care and decrease barriers to care. Patients receiving support from doulas had a decrease in preeclampsia rates and an increase in postpartum follow-up visits.
The doula program provides another level of care thanks to donations through the Norton
We know that more than 50% of maternal deaths in Kentucky are attributed to substance use disorder. Many schools of thought exist on how to address it, but we know that patients with substance use disorder can thrive with help and support. By offering medical stabilization and outpatient treatment through the Norton MOST Program, in less than 10 years we have helped more than 1,400 patients and their families on the road to recovery. These are patients who have unique needs, and many other treatment programs do not care for pregnant patients.
A survey conducted by Norton Healthcare assessed healthcare needs in West Louisville — a nine-neighborhood community where 65,000 residents are mostly African American. The survey revealed that 36% of respondents
“We must recognize and find solutions to the fact that Black women experience higher maternal mortality rates in Kentucky.” — Lyndsey Neese, MD
felt they had difficulty finding a specialist. Of those, 46.9% said they were looking for women’s healthcare. Transportation, childcare, and office hours were all issues.
We must recognize and find solutions to the fact that Black women experience higher maternal mortality rates in Kentucky. A new women’s health office will offer services at Norton West Louisville Hospital and is scheduled to open this fall. At this location, women’s healthcare providers will offer outpatient gynecological care, outpatient gynecological surgery, prenatal care, and ultrasounds. We believe that
this increased access to care will improve maternal outcomes for our community.
The Louisville Metro Public Health and Wellness health equity data website states that “one major root cause of infant mortality, preterm birth, and low birth weight is the access and availability to adequate healthcare and health insurance, specifically for preventative, prenatal and/or other maternal health related services.”
If we are going to make a difference, we must recognize that even our locations matter. I am proud to be part of an organization that sees this as important. The goal: provide life-enhancing programs and services to one of Kentucky’s most underserved communities.
Norton West Louisville Hospital is under construction on the Norton Healthcare Goodwill Opportunity Campus at 28th Street and Broadway in Louisville. This unique concept was born out of a partnership between
Goodwill Industries of Kentucky and Norton Healthcare to offer social services with various community partners as well as health care in a single location.
The vision includes women’s services as well as adult and pediatric primary care, cardiology, orthopedics, diabetes care, and behavioral health services. The hospital will feature a 24/7 emergency department; inpatient treatment; operating rooms; imaging services, including X-ray, CT, and MRI; and a retail pharmacy.
By offering greater access to prenatal, postpartum, and overall women’s care, we hope that we can contribute to the success of families and improve health moving into the future. Our community depends on it.
Lyndsey D. Neese, MD, MMM, CPE, FACOG, is an OB/ GYN with Norton OB/GYN Associates. She also serves as medical director of quality for women’s services for Norton Healthcare. Her passion is providing safe, equitable care for all women. Dr. Neese is the American College of Obstetricians and Gynecologists Kentucky section vice chair and OB leader for the Kentucky Perinatal Quality Collaborative.






















Editor’s introduction: Long-term health for the people of Kentucky must include addressing the health needs of Kentucky’s children. We asked Steven J. Stack, MD, MBA, commissioner for public health and chief medical officer for the Commonwealth of Kentucky for the past four years, to share his thoughts and describe what the Department of Public Health is doing for Kentucky’s children.
MDU On the scale of health problems in Kentucky, where do you put addressing childhood obesity?
STACK Childhood obesity is a serious challenge in Kentucky. In terms of negative longterm impact on the health of Kentuckians, increased future burden of disease, and escalating healthcare costs, it ranks high as a population-level concern.
MDU Please describe childhood obesity in Kentucky. How is it defined?
STACK Body mass index, or BMI, describes a person’s weight adjusted for their height. The formula is weight in kilograms divided by the square of their height in meters.
Data tables show BMI percentiles based on sex and age-specific cohorts. There are two terms commonly used to describe the high side of the BMI gradation — overweight and obese.
1. Overweight is between the 85th to 95th percentile.
2. Obese is 95th percentile or greater.
MDU What trends have been found by measuring childhood obesity in Kentucky in the last 10-20 years?
STACK While the rate of overweight children has stayed relatively stable, the rate of obese children has increased over this time period. More specifically, 19.3% of Kentucky children age 0–17 were obese in the 2016–2017 school year. In 2021–2022, the most recent year of data, 24.6% of Kentucky children 0–17 years old were obese. That’s a worrisome trend.
MDU Can you talk about it by regions as well as statewide? Are there differences?
STACK The available data is obtained mostly from the Youth Behavioral Risk Survey
(YBRS), a self-reported survey of middle and high school students. The study provides invaluable information, but there are limitations to the geographical detail it provides.
Even at the state level, though, the data shows Kentucky children are not faring as well as the rest of the nation. Kentucky’s childhood obesity rate of 24.6% is markedly higher than the national average of 18.1% and is second only to West Virginia at 24.8%. Said differently, Kentucky children have the second highest rate of obesity in the nation when compared to all other states.
MDU What are the most problematic, stubborn, and fundamental causes of childhood obesity in Kentucky?
STACK Our dietary and physical activity environment is fundamentally different than it was 100 years ago. We now have abundant access to calorie-dense, nutrient-poor food coupled with machines and technology that make our daily routines less physically
demanding. Increased calories plus decreased physical activity means increased obesity.
MDU What policies, procedures, and actions can the Kentucky Department for Public Health perform to reduce childhood obesity in Kentucky?
STACK For the Kentucky population overall, surveys have found that 31% of Kentuckians did not engage in any non-work exercise in the prior 30 days; 45% ate fruit less than once per day; and 20% ate a vegetable less than once per day. Add to this the frequent intake of processed foods and snacks along with sugary sodas and beverages, and we have a recipe for obesity and declining health.
It is essential that we find ways to change our lived environments and daily routines in a couple simple to say, but devilishly difficult to do, ways:
• Increase physical activity to at least three to four days of moderate physical activity (i.e., walking) for 30–45 minutes.
• Eat at least two fresh fruits or vegetables every day.
There are certainly many other things we could do, but I think it is most important that we start with things that are achievable and sustainable. If we lay a solid foundation of improved habits, we can later build on that foundation.
Additionally, Kentucky is one of 17 states to have received a State Physical Activity and Nutrition (SPAN) grant from the CDC to address obesity. This program is pursuing five focus areas:
• Creating community bike/walk plans to increase active transportation.
• Providing guidelines to increase fresh produce and reduce processed, high sodium, high fat, and high sugar foods offered in food pantries, cafeterias, parks, and recreational settings, etc.
• Promoting food prescription and voucher programs.
• Training for early childhood educators to improve nutrition standards, reduce digital screen time, and increase physical activity.
• Promoting newborn breastfeeding.
MDU Where is Kentucky in pediatric vaccination rates nationally in comparison to recent years?
STACK Kentucky’s kindergarten age children lag behind both the national and many of our border state averages for routine immunizations. For the 2022–23 school year, Kentucky kindergarten age children had a roughly 90% vaccination rate for MMR, varicella, and DTaP; by comparison, the national average for these is about 93% and the rates in Tennessee, Virginia, and West Virginia are generally 95% or higher. To keep our children safe from vaccine preventable illnesses, it is important that we get these rates higher.
On a good note, however, we are making improvement. In 2021–22, Kentucky’s kindergarten age vaccination rates for MMR, varicella, and DTaP were less than 87%, so we have had a 3% or greater absolute
improvement in just one year. It will take sustained effort, though, to maintain and further improve these rates.
Unfortunately, we are a victim to our own success. Generally high vaccination rates have made many of these diseases uncommon or even rare. As vaccination rates have decreased in recent years, however, we have seen measles, for example, appearing with increasing frequency in communities with particularly low immunization rates. This translates into young and medically vulnerable children at higher risk for serious illness that could result in long-term harm.
Our partners in immunization outreach are:
- Foundation For A Healthy Kentucky
- Kentucky Association Of Health Plans
- Kentucky Chapter Of American Academy Of Pediatrics
- KY Department Of Education
- KY High School Athletics Association
- KY Hospital Association
- KY Medical Association
- KY Nurses Association
- KY Pharmacist’s Association
- KY Primary Care Association
- KY Voices For Health
- High Five For Health
MDU What are the other major health problems that Kentuckians face that the Department for Public Health is addressing?
STACK Reducing smoking rates, helping people living with substance use disorder reduce their risks of harm, and striving to eliminate overdose deaths.

BY CLAIRE WEEKS, MS, KENTUCKY TOBACCO PREVENTION & CESSATION PROGRAM CESSATION ADMINISTRATOR
ELLEN CARTMELL,

FRANKFORT Providers play a critical role in helping Kentuckians quit tobacco products. That’s why the Kentucky Department for Public Health has released new tools providers can use to support patients on their quit journey. QuitLogix Education now offers on-demand trainings at no cost to providers to help them expand their tobacco-cessation knowledge base while earning CME, CNE, or CPE credits.
The training is meant for healthcare providers and social service agencies who want to help care for their patients during their tobacco dependence journey. Featured QuitLogix Education courses include:
• Medicaid and Quit Now Kentucky benefits for tobacco cessation
• Best practices for tobacco cessation using medication and behavioral support
• Special quitline programs for tobacco cessation
• Connecting the harms of tobacco use to chronic health conditions
• Tobacco cessation for behavioral health populations
• Vaping and e-cigarettes: What are they and how do they harm?
• Conversations for screening, responding to, and preventing vaping Modules range from 15 to 30 minutes, with stop-and-play functionality to fit into busy clinic schedules. Each module contains a short video with interactive features that help you immediately integrate content into practice. These modules include an excellent introduction to Quit Now Kentucky, the state’s tobacco quitline and give providers the most up-to-date information on how their patients can get free counseling and which health insurance providers cover cessation medications. Those who are interested
can review a summary of each module at quitlogixeducation.org/kentucky/.
The QuitLogix Education modules were designed by respiratory hospital National Jewish Health, which also operates Quit Now Kentucky. Quit Now Kentucky is available 24/7 at no cost to Kentucky residents of all ages. In addition to coaching, participants can receive free nicotine replacement therapy if they are uninsured, enrolled in Medicare or report a behavioral health diagnosis such as depression, PTSD, schizophrenia, or anxiety. Kentucky law requires all commercial and public health insurance providers to cover nicotine replacement therapy with no copay. As Medicare is a federal program, this law does not apply to Medicare’s coverage policies.
According to the 2020 U.S. Surgeon General’s Report on smoking cessation, a majority of cigarette smokers attempt to quit each year, but fewer than one in three use cessation medications or behavioral counseling to support their quit attempts. Medication and counseling are the two critical factors for success in quitting smoking. Cessation medication can more than double the chance of success and getting cessation counseling can do the same.
Quit Now Kentucky participants under the age of eighteen are directed to My Life, My Quit, which is staffed by coaches who are not only trained in nicotine addiction but also in child psychology. My Life, My Quit allows youth to receive customized help quitting vaping through text messages or online chat. Both Quit Now Kentucky and My Life, My Quit can be incorporated into electronic medical records systems to allow providers to refer patients to the quitline directly.
Quitting is “the single most important step a smoker can take to improve the length and
quality of their life,” according to the U.S. Surgeon General. The Surgeon General also concluded in 2020 that smoking cessation reduces the risk for all-cause mortality, cardiovascular disease, chronic obstructive pulmonary disease, adverse reproductive health outcomes and 12 types of cancer. Although considerable progress has been made in the U.S. in reducing smoking over the past half century, there is still work to be done.
While Kentucky has one of the highest smoking rates in the nation, the good news is that nearly nine in ten (88%) of Kentucky adults who smoke said they wanted to quit, according to the 2021 Kentucky Behavioral Risk Factor Survey. Kentucky providers play an important role in encouraging their patients to quit. When patients hear from their provider not just ‘smoking is bad for you,’ but also ‘I believe you can quit and I want to show you these things that can help,’ it can make all the difference in their motivation to seek help quitting.
National Jewish Health is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians and by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Provider approved by the California Board of Registered Nursing, Provider Number 12724.
If you have questions about the accreditation of this activity, please contact proed@njhealth.org or 303.398.1000. For more information about tobacco cessation or prevention resources in Kentucky, contact the Kentucky Tobacco Prevention & Cessation Program at the Kentucky Department for Public Health at Ky.TobaccoFree@ky.gov.
LEXINGTON An-Yu Chen, MD, was appointed to Team Kentucky’s board of physicians and advisors as part of the Cabinet for Health and Family Services. Chen is currently head of section at Lexington Clinic Gastroenterology and a member of the Lexington Clinic board of directors. Governor Andy Beshear appointed Chen in 2023, and he was confirmed by the Kentucky Senate on April 15, 2024, for a fouryear term.




LEXINGTON Sarah H. Min, MD, has joined Lexington Clinic in Rheumatology. She is board-certified in internal medicine and in rheumatology. She provides treatment for inflammatory rheumatic diseases such as rheumatoid arthritis, psoriatic arthritis, systemic lupus erythematosus, inflammatory muscle diseases, Sjogren’s syndrome, scleroderma, vasculitis, mixed connective tissue disease, gout, pseudogout, enteropathic arthritis, systemic autoinflammatory disease, sarcoid arthritis, osteoarthritis, and osteoporosis. Min’s office is located at 1221 South Broadway, Lexington, KY 40504. Lexington Clinic was founded in 1920 and is Central Kentucky’s oldest and largest group practice. With 300+ providers in 35+ specialties, Lexington Clinic has more than 34 locations and serves about 600,000 patients yearly throughout Central Kentucky.















BY JAN ANDERSON, PSYD, LPCC
I’m a concierge psychologist specializing in relationships, resilience, and success. I primarily work with executives and professionals, including couples and families, who want to feel better and function better at work and home.
Over the past ten years, I’ve experienced the emergence of an unexpected specialty—the estrangement of a parent and adult child—which now accounts for one-third of my practice.
For parents navigating low or no contact with an adult child, the instinct is to try to fix the rift immediately. The last thing estranged parents expect me to put on the table is the possibility of taking a step back.
There’s a good chance your kid may appreciate your backing off a bit. I’ve noticed that adult children often view this space as giving them room to focus on their most pressing developmental task: “adulting.” Just don’t expect your child to express this in a mature, emotionally intelligent, or considerate way. It’s usually pretty ugly.
Believe it or not, recognizing when to pause and respect your adult child’s need for space can be crucial for your emotional well-being and the potential healing of the relationship.
Most parents find it incredibly difficult to reduce contact or wait for the adult child to reach out. Creating more distance can feel counterintuitive when the ultimate goal is reconciliation. “If I back off, they will never come back!” is often an estranged parent’s first reaction.
If you’re an estranged parent and the fear of permanent loss is overwhelming, this article is for you. If you’re an estranged parent feeling guilt or shame about needing or wanting to take a step back, this article is for you.
Backing off doesn’t mean giving up. It’s a strategic pause. It’s about respecting your child’s need for space while still expressing love and readiness to reconnect when they are. In the meantime, don’t worry about spending every waking moment waiting anxiously or deep in depression. You’ve got important work to do, and you’ll now have time to do it.
Stepping back allows time and space for an estranged parent to develop three crucial emotional skills:
1. Emotional Regulation: Learning to manage your emotions better gives you the steadiness to handle potential future interactions with your adult child more effectively.
2. Distress Tolerance: Developing the skill of soothing emotional pain without acting
impulsively can improve your well-being and set a foundation for a renewed relationship with your adult child.
3. Self-Compassion: Don’t confuse self-compassion with being a wuss. Developing self-compassion will be your superpower. Tender self-compassion will fuel your emotional recovery and make you resilient. Cultivating what Dr. Kristin Neff calls “fierce self-compassion” will enable you to recognize and honor your limits and set boundaries.
• Space can be a smart strategic move. It respects your child’s wishes and at the same time gives them an opportunity to miss you.
• Space can be healing for both parties. Knowing that you have the option to take a step back can restore some sense of control, autonomy, and safety when you feel like you’re at the mercy of your adult child. In this way, stepping back can be therapeutic and ease an estranged parent’s suffering. Space gives your adult child the autonomy to handle their feelings independently, which can be crucial for their personal development.
• Space can help reset expectations: Space gives you time to adjust your expectations about the relationship’s future. As one parent said, “I could consider what kind of relationship is realistic, not just the one I idealize.”
I hope you’ve forgiven yourself if you have fallen prey to any or all of these common, natural, and very human reactions to being shunned by your adult child:

For nearly 30 years, we’ve helped hundreds of clients solve their biggest money concerns. Stop worrying, and start living life on a path towards financial freedom and security.
Thinking clearly about money. Caring deeply about you.
See how we think about money dscottneal.com

• A power play to force or threaten your adult child into submission.
• A passive-aggressive form of punishment or revenge.
• An attempt to get a reaction from your adult child. For example, a guilt trip or something dramatic, desperate, or impulsive.
You’ve probably found that these tactics tend not to work and likely leave you feeling worse (as if you thought that was possible). Even when force, threat, or manipulation work, they don’t really work because you don’t get what you want—a genuine emotional connection with your child.
So, how do you let your adult child know you’re always open to communication, but on their terms? How do you manage to be vulnerable enough to be open and emotionally available while maintaining enough personal boundaries to avoid being too vulnerable?
An excellent place to start is by shifting out of some common “thinking errors” that may be getting in your way:
Thinking Error #1: If I back off, it means I don’t care about my child. It means I’m abandoning them.
Mindset Shift: Frequently, adult children perceive your repeated attempts at connection as “violating my boundaries,” “not respecting my decisions,” or even “selfish” or “needy.” Adjust your self-talk to “Backing off does NOT mean that I’ve stopped loving my child. It means I’m doing something more aligned with my child’s needs now.”
Thinking Error #2: If I back off, it means I’m giving up. I should never give up. I must always keep trying.
Mindset Shift: Sometimes, giving up is an intelligent and adaptive move. When you give up doing A, it frees you up to try B, C, or D until you find something that works better. One parent described stepping back as “I’m not giving up. I’m trying something different.”
Thinking Error #3: I’m the parent. I should be strong. I should be able to figure this out and fix it.
Mindset Shift: Parents are actually pretty freaking vulnerable to our adult children. Our children have plenty of power to hurt us. It’s not only okay to seek support, comfort, and guidance, but it’s crucial to do so when you’ve been rejected by the last person you ever thought would reject you: your child.
Thinking Error #4: I’m the parent. I’m responsible for the strength of the family unit and the well-being of my family’s relationships.
Mindset Shift: “You’re the parent” does not mean that you should somehow be unaffected and unflappable when shunned and shamed by your adult child. So join the human race. Come on in. The water’s fine.
Thinking Error #5: No matter how my adult children treat me, they are my children, and I have to accept it.
Mindset Shift: Actually, you don’t have to take it. You are not superhuman and filled with a limitless capacity to absorb whatever treatment is inflicted on you by your adult child. Your inner child needs you, too. Let it be okay to set some limits and boundaries that protect, support, and validate your inner child’s needs and feelings. This does not mean your adult child doesn’t count. It means that you count, too.
If you need support and strategies to navigate this challenging path while holding space for possible future reconciliation, contact me at 502.426.1616 or LifeWise@ DrJanAnderson.com to schedule a complimentary telephone consultation or appointment. You don’t have to struggle with estrangement from your adult child alone.

LEXINGTON CHI Saint Joseph Health and CHI Saint Joseph Medical Group honored their 2024 Employee of the Year and Leader of the Year award recipients at the CHI Saint Joseph Health Foundations Humankindness Gala on Saturday, May 18, 2024.
THIS YEAR’S RECIPIENTS ARE:
CHI SAINT JOSEPH HEALTH CORPORATE


Employee of the Year:
Carlis Richards, market coordinator, Emergency Services, Berea
Leader of the Year:
Andre Fomby, market director, IT, Lexington
CHI SAINT JOSEPH MEDICAL GROUP




Physician of the Year
Derrick Williams, MD, Richmond
APP of the Year:
Chris Clark, Nicholasville
Employee of the Year: Andrew Roberts, Corbin
Leader of the Year: Jennifer Jones, Manchester


ADDITIONAL CHI SAINT JOSEPH HEALTH WINNERS INCLUDE:
Continuing Care Hospital - Ghassan Shakhashiro, MD, Physician of the Year, Lexington; Emily White, Employee of the Year, Winchester; Dawn Erb, Leader of the Year, Lexington
Flaget Memorial Hospital - Olivia Kelley, MD, Physician of the Year, Bloomfield; Janette Yingling, APP of the Year, Lexington; Barbara Hunter, Employee of the Year, Bloomfield; Brooke Daidsman, Leader of the Year, Bardstown
Saint Joseph East - Kevin Donahue, DO, Physician of the Year, Lexington; Heather Smith, APP of the Year, Lexington; Kathy Williams, Employee of the Year, Lexington; Jason (Jay) Elery, Leader of the Year, Lexington
Saint Joseph Hospital - Korey Brammell, DO, Physician of the Year, Huntington, W.Va.; Michael Farran, APP of the Year, Lexington; Dee Thompson, Employee of the Year, Lexington; Rachel Kennedy, Leader of the Year, Frankfort
Saint Joseph Jessamine - Erica Houp, Employee of the Year, Nicholasville; Patsy Harlow, Leader of the Year, Versailles
Saint Joseph London - Abdul Siddiqui, MD, Physician of the Year, London; Angel Patterson, APP of the Year, London; Loretta Philpot, Employee of the Year, London; Joshua Holland, Leader of the Year, London
Saint Joseph Berea - Asad Jadoon, MD, Physician of the Year, Richmond; Reida Sowden, APP of the Year, Richmond; Teresa Fightmaster, Employee of the Year, Richmond; Jackie Maynard, Leader of the Year, Berea
Saint Joseph Mount Sterling - Byram Ratliff, MD, Physician of the Year, Lexington; Sean Lawson, APP of the Year, Somerset; Vanessa Harris, Employee of the Year, Clay City; Kayla Isaacs, Leader of the Year, Richmond










Annual event raises money for local medical charities




LEXINGTON A generous presenting sponsorship contribution from Stockyard Bank & Trust coupled with hole sponsorships and 21 teams raised over $30,000 at the Lexington Medical Society Foundation’s 34th annual golf tournament on May 29th at the University Club in Lexington.
Physicians, medical community stakeholders, and financial partners answered the call. Under partly sunny skies and breezy conditions, players “scrambled” their way to the finish.
The winning team, from the law firm Sturgill Turner, of Scott Miller, Jay Phillips, Mike Scatena, and Temple Juett posted a handicapped scored of 47. The second place team, playing for UK Healthcare Jon Webb,



MD, Mike Shepherd, Glenn Stroud & Kevin Schuer with a score of 52. The third place team was Arvinda Padmanabhan, MD, Rusty Page, MD, Shawn Peterson, and Paul Ladd with a score of 54.
LMSF chair John Collins once again steered the Foundation’s major fundraiser to a successful outcome. LMSF donates funding grants to Central Kentucky healthcareoriented charities such as Baby Health Services, Bluegrass Council for the Blind, Radio Eye, Camp Horsin’ Around, Kidney Alliance of KY, Ronald McDonald House, Surgery on Sunday, Chrysalis House, and more.
More information on the Lexington Medical Society is at www.lexingtondoctors. org or 859.278.0569.













Keynote speaker describes how elite athletes navigate emotional disorders
LOUISVILLE The UofL Depression Center’s annual benefit event took place on Thursday, April 25, at the UofL Conference Center on the Shelby campus. The guests heard a presentation from Kevin Chapman, PhD, entitled “Emotion Regulation and the Modern Athlete: Balancing Process and Outcome.”

Chapman, founder and director of the Kentucky Center for Anxiety and Related Disorders, a former two-sport college athlete and a member of the Center College Athletic Hall of Fame, told the audience that “multiple studies indicate that elite athletes experience comparable rates of emotional disorders as the general population, but they have a greater risk of emotional disorder after suffering an injury in their sport.”
Also addressing the audience was Kara Winger, former USA world champion and 2008 Olympic track and field athlete. Winger competed in the javelin throw and in 2022 set a world record in the USA Outdoor Track and Field Championship. Winger discussed the process of healing and learning from injuries she suffered in her quest for an Olympic medal.




The UofL Depression Center provides treatment services and educates students, residents, and practicing physicians. More information is at 502.588.4450 and www. uol.edu/depression.


PHOTOS BY GIL

At UofL Health – Trager Transplant Center, we offer life-saving care backed by innovative research and academic expertise. Our revolutionary transplant specialists performed Kentucky’s first adult heart, pancreas, heart-lung and liver transplants. As leading experts in advanced organ diseases and organ failure, we specialize in:
n Advanced Heart Disease, Ventricular Assist Device & Heart Transplant
n End-stage Lung Disease, Single & Double Lung Transplant
n End-stage Liver Disease, Liver Transplant
n Advanced Kidney Failure, Kidney Transplant, including Living Donor Kidney Transplant
n Pancreas Transplant
Our world-class surgeons are part of an interdisciplinary approach, collaborating with specialized teams to provide the highest level of care. Our experts thoughtfully prepare patients through the entire transplant procedure, including the crucial post-transplant process. Whether patients have a specific disease or are awaiting a transplant, our dedicated team offers compassionate care, every step of the way.
It’s a referral that can be life-saving. That’s the Power of U.
Covered by most insurance (Medicare 50 - 77)
Quick and painless
No needles, IVs or dyes
Get screened every year to catch cancer early


Lung cancer can be treated if caught early!
“Kentucky has achieved notable success in a state with dismal lung cancer incidence, mortality, smoking rates and 5-year survival
We are now #2 in the country for lung cancer screening.”
Michael R. Gieske, MD Director of Lung Cancer Screening St Elizabeth Virtual Health Center
You are eligible for screening if:
20 15 50 You are 50 to 80 years old
You smoked a pack of cigarettes a day for 20 years
You currently smoke or quit within the past 15 years