


The Heart of the Matter
Interventional Cardiologists Say the Human Connection Is Most Important
ALSO IN THIS ISSUE
THE WOMEN’S HEART HEALTH PROGRAM AT UOFL HEALTH
ADVANCED CARDIAC IMAGING AT HARRISON MEMORIAL HOSPITAL, CYNTHIANA
TREATMENT OPTIONS FOR AFIB AT NORTON HEART & VASCULAR INSTITUTE
HYPERTENSION CLINIC GROWS AT BAPTIST HEALTH
ISSUE #150 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS VOLUME 14 • #1 • F E br UA ry/M A r C h 2024
LEXINGTON
Excellence is in our veins.
The first and only accredited Vein Center in Kentucky.
The Vein Center at Saint Joseph Hospital offers the highest level of vein care. Our providers specialize in the treatment of venous insufficiency (reflux) including thermal ablation and sclerotherapy of diseased veins. Vein procedures can eliminate chronic discomfort, swelling, inflammation, skin discoloration, and other symptoms associated with diseased superficial veins and varicose veins. These procedures are performed as an outpatient service at Saint Joseph Hospital.
Give us a call at 859.313.2698 or visit CHISaintJosephHealth.org/VeinCenter to learn more.

Vein Center
Saint Joseph Hospital
1 Saint Joseph Drive Lexington, KY 40504


 Steve Lin, MD
Medical Director
Nezar Falluji, MD
Hussam Hamdalla, MD
Sharat Koul, DO
Steve Lin, MD
Medical Director
Nezar Falluji, MD
Hussam Hamdalla, MD
Sharat Koul, DO

















































ISSUE #151 (April)
INTERNAL SYSTEMS





Dermatology, Endocrinology, Gastroenterology, Geriatric Medicine, Internal Medicine, Integrative Medicine, Infectious Disease Medicine, Lifestyle Medicine, Nephrology, Urology
ISSUE #152 (June)
WOMEN & CHILDREN’S HEALTH
OB/GYN, Women’s Cardiology, Oncology, Urology, Pediatrics, Radiology
ISSUE #153 (September)
MUSCULOSKELETAL HEALTH


Orthopedics, Physical Medicine & Rehabilitation, Sports Medicine, PT/OT






ISSUE #154 (October)
CANCER CARE
Hematology, Oncology, Plastic Surgery, Radiology, Radiation
ISSUE #155 (December)
IT’S ALL IN YOUR HEAD
ENT, Mental Health, Neurology, Neuroscience, Ophthalmology, Pain Medicine, Psychiatry
Editorial topics and dates are subject to change
THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS Editorial Calendar To participate, please contact Gil Dunn, Publisher GDUNN@MD-UPDATE.COM 859.309.0720 (direct) • 859.608.8454 (cell) Send press releases to gdunn@md-update.com
2024 ISSUE #146 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS VOLUME 13 • #3 • JULY 2023 Above and Beyond Endocrinologist Kupper Wintergerst, MD, and his team go the extra mile for their patients with diabetes ALSO IN THIS ISSUE UofL HEALTH - CENTER FOR WOMEN’S HEALTH EXPANDS CARE INTO COMMUNITIES LEGACY OB-GYN DOCTOR AT WOMEN FIRST OF LOUISVILLE REFLECTS AND LOOKS FORWARD CHI SAINT JOSEPH HEALTH PSYCHIATRIST SEES DISTURBING TRENDS IN ADOLESCENET MENTAL HEALTH PEDIATRIC ORTHOPEDIC SURGEON AT SHRINERS HOSPITAL - LEXINGTON ORAL HEALTH IS PART OF PRIMARY CARE ISSUE #147 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS A Cut Above Lexington Clinic Orthopedic Surgeon Tharun Karthikeyan, MD, Embraces the Advantages of the ROSA Robot ISSUE #148 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS VOLUME 13 • #5 • NOVEMBER 2023 Not Your Mother’s Breast Care Focusing on early detection and targeted care, the surgeons at Baptist Health Breast Surgery are ensuring patients receive the most innovative and individualized care available ALSO IN THIS ISSUE (CAR) T CLINICAL TRIALS AT UofL HEALTH - BROWN CARE CENTER 3D MAMMOGRAPHY IS WELL CARE AT WOMEN FIRST OF LOUISVILLE CHI SAINT JOSEPH HEALTH ONCOLOGY IN RURAL COUNTIES GLIOBLASTOMA RESEARCH & TRIALS AT NORTON CANCER INSTITUTE
Welcome to the Heart and Lung Issue of MD-Update
Heart disease remains a problem in Kentuckiana, but there’s improvement in diagnostics via cardiac imaging. As Yaz Daaboul, MD, cardiologist at Harrison Memorial Hospital in Cynthiana, told me, “Now we’re not only listening to heart valves, but we’re looking at them.”
Dr. Daaboul is new to Kentucky, coming here from Boston. The rural area appeals to him as he “becomes part of the community.” Get to know Dr. Daaboul starting on page 16.
Our cover story in this issue profiles Drs. Hussam Hamdalla and Sharat Koul, interventional cardiologists at CHI Saint Joseph Health. Building a human connection is the key to a positive doctor-patient relationship, they told me. Getting to know their patients’ personal stories helps them deliver the heart health care the patients are seeking. You can read more beginning on page 10.
I enjoyed talking with both Mrin Shetty, MD, at UofL Health Women’s Heart Health program and Kent Morris, MD, at the Norton Heart & Vascular Institute. Each of them related similar feelings of joy that they experience when their patients’ lives are improved by increased cardiovascular health. “It puts a spring in my step,” says Dr. Shetty. Dr. Morris wants his patients to “live life and enjoy it.”
Please get acquainted with Drs. Shetty and Morris and their work on pages 14 and 18.
Your Kentucky Medical Association and Medical Societies
MD-UPDATE
MD-Update.com
Volume 14, Number 1
ISSUE #150
EDITOR/PUBLISHER
Gil Dunn
gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda Debord
CONTRIBUTORS:
Megan Adkins, Esq.
Jan Anderson, PSyD, LPCC
Ashley boerrigter, MD
Afton Fairchild
Elizabeth Anderson-hoagland, ChFS, DPh, DPQI brandy Montgomery
Scott Neal, CPA, CFP
Emily Schott
CONTACT US:
ADVERTISING AND INTEGRATED
PHYSICIAN MARKETING:
Gil Dunn
gdunn@md-update.com

Dr. Tuyen Tran and Dr. Angela Dearinger of the Lexington Medical Society met with representative Daniel Fister (r)-56th during KMA’s Physician Day at the Capitol February 21, 2024.
It’s no secret that state legislatures across the country are trying to “practice medicine without a license.” Kentucky is not immune to the problem. The KMA represents physicians and their interests in Frankfort. As an example, in 2022 the KMA made lung cancer screening one of its top priorities and successfully advocated for the passage of House Bill 219, which established the Lung Cancer Screening program within the KY Department for Public Health. Funding for the program amounted to $1 million. Kentucky now ranks #2 in the nation for rates of lung cancer screening. Hooray for the KMA and its past president Dr. Neal Moser!
Clarification
In MD-Update #148, November 2023, there was a story on the PACE program administered by Bluegrass Care Navigators and Dr. James Borders. To clarify, the counties served by the PACE program run by Bluegrass Navigators are Anderson, Fayette, Franklin, Jessamine, and Woodford counties. Horizon PACE serves Barron, Clinton, Estill, Jackson, Laurel, Madison, McCreary, Pulaski, Rockcastle, Warren, and Wayne counties.
The 2024 MD-Update editorial calendar is on the preceeding page. When you see your specialty, give me a call. I’m sure you have a good story to tell.


Mentelle Media, LLC
38 Mentelle Park Lexington Ky 40502 (859) 309-0720 phone and fax
Standard
MD-Update
Ky 40502
Please

2 MD-UPDATE
class mail paid in Lebanon Junction, Ky. Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington
peer reviewed for accuracy. however, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
is
Mentelle Media, LLC. All rights reserved. No part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Copyright 2024
contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter. Thank you. Individual copies of MD-Update are available for $9.95. SEND YOUR LETTERS TO THE EDITOR TO: Gil Dunn, Publisher gdunn@md-update.com, or 859.309.0720 phone and fax Until next time, all the best, Gil Dunn Editor/Publisher MD-Update
LETTEr FrOM ThE EDITOr/PUbLIShEr





ISSUE #150 3 4 HEADLINES 6 ACCOUNTING 7 FINANCE 8 LEGAL 10 COVER STORY SPECIAL SECTION: CARDIOLOGY 14 CARDIAC IMAGING 16 CARDIAC IMAGING 18 ELECTROPHYSIOLOGY 20 HYPERTENSION 22 COMPLEMENTARY CARE 24 PUBLIC HEALTH 25 MENTAL WELLNESS 27 NEWS 32 EVENTS 16 CARDIAC IMAGING 14 CARDIAC IMAGING 20 HYPERTENSION 18 ELECTROPHYSIOLOGY CONTENTS ISSUE #150 10 The Heart of the Matter Interventional Cardiologists Say the Human Connection Is Most Important COVEr PhOTOGrAPhy by MArK MAhAN
Lung Cancer Screening Rate Hits New High
KMA’s “Breathe Better Kentucky” initiative helps state soar to #2 in nation in lung cancer screening rates
BY EMILY SCHOTT, DIRECTOR OF COMMUNICATIONS, KENTUCKY MEDICAL ASSOCIATION
Kentucky was recently ranked #2 in the nation for lung cancer screening rates by the American Lung Association in their 2023 State of Lung Cancer report. But what helped nudge the Commonwealth to the top of the list?
In the fall of 2021, then-Kentucky Medical Association (KMA) President Neal Moser, MD, kicked off his year of service with a mission: to improve the lung health of patients in a state where tobacco use and chronic lung diseases had chained Kentucky to the bottom of health rankings for years. Add to that the effects of the COVID-19 pandemic on lung health, and Moser was determined to find a way to help Kentuckians “breathe better.”
As a pulmonologist, Moser knew the combined impact of those issues would be an uphill battle. The KMA teamed up with its charitable arm, the Kentucky Foundation for Medical Care (KFMC), and the Anthem Foundation to put together a year-long campaign called “Breathe Better Kentucky” that encompassed public awareness, education for physicians, and advocacy in Frankfort to reach as many residents as possible and create the biggest impact.
“We wanted to take a multifaceted approach to this initiative. We knew Kentuckians were suffering from lung health issues, in great numbers, and the pandemic had only worsened our outcomes. By not only providing messaging to the public, but also education for our providers and advocating for important bills in the legislature, we were able to make real changes happen,” said Moser.
The centerpiece of the project was the sponsorship of a three-part series on Kentucky Educational Television (KET), Fighting to

Breathe, that examined the story of lung disease in Kentucky—the causes, the impact on those afflicted, and the exciting new developments in treatment and prevention. Hosts Renee Shaw and KMA member and Kentucky Health host Wayne Tuckson, MD, spoke with researchers, experts, advocates, and survivors who revealed eye-opening information that challenged basic assumptions about lung health. The program was also sponsored by the Foundation for a Healthy Kentucky.
Airing in the winter of 2022, the series received widespread praise and viewership of more than 50,000 during its premiere. It was re-aired more than twenty times throughout the season, and six segments from the series were also placed on PBS Learning Media, a free online repository providing curated materials for teachers K-12. More than one million teachers have access to this content.
It continues to remain available on KET.org.
In addition to the KET series, Breathe Better Kentucky tackled disparities by utilizing targeted social media and web advertisements in communities where lung health issues were more prevalent, public service announcements and radio advertisements, as well as messaging on streaming services. More than one million Kentuckians were reached through these efforts. A dedicated website, BreatheBetterKY.org, housed resources and important information as well.
The Kentucky Legislature and Your KMA
The KMA knows some of the most meaningful changes happen in and because of actions taken at the state capitol in Frankfort, so during the 2022 legislative session, KMA made lung cancer screening one of its top
4 MD-UPDATE PHOTS PROVIDED BY KMA
HEADLINES
In 2021, then Kentucky Medical Association (KMA) President Neal Moser, MD, speaks to the KY Crushed Stone Association (KCSA) on the harmful effects of dust on the lungs and the importance of lung screening for workers.

priorities, and successfully advocated for the passage of House Bill 219. Sponsored by Rep. Kimberly Moser, HB219 established the Lung Cancer Screening Program within the Kentucky Department of Public Health and the Lung Cancer Screening Advisory Committee. The program and advisory committee work collaboratively to increase lung cancer screening, reduce the state’s morbidity and mortality from lung cancer, reduce the cost associated with the treatment of lung cancer, and raise public awareness regarding the benefits of screening. Funding for the program in the amount of $1 million was included in the separate budget bill (House Bill 1) passed by lawmakers.
“We were thrilled with the passage of House Bill 219,” said Moser. “While getting legislation through that says, ‘this is a priority’ is always a win, getting the funding in place to actually make changes is when things really happen, so having that money earmarked in the state budget was huge.”
Finally, KMA set out to make lung health a priority for its member physicians as well. Through its “CME Guarantee” program, KMA produced two one-hour virtual education sessions that discussed improving outcomes, new technologies, eliminating health inequity, and lessons learned from the COVID-19 pandemic.
Success is a Team Effort
In November of 2023, the American Lung Association released its “State of Lung Cancer”
report, which revealed that Kentucky now ranks second in the nation for lung cancer screening rates, putting the Commonwealth among the best in the country in the category. It had previously ranked fourth.
“While we know that improvement is the result of the work of many, many people, I am pleased to think that our KMA played
even a small role in such an achievement,” said Moser.
“It’s gratifying to witness a project that we already felt was ‘successful’ continue to cultivate positive changes for our patients that are going to lead to thousands leading longer, healthier lives,” said current KMA President Michael Kuduk, MD. “We want to thank everyone who was involved, especially the KFMC, KET, the Anthem Foundation (now the Elevance Health Foundation), and all our physician members who worked tirelessly to get the word out and ensure their voices were heard.”
“There’s still work to be done in Kentucky, both in the areas of lung health and on other issues of course, but we couldn’t be more pleased with the results of the Breathe Better campaign and look forward to using it as a model for additional public health efforts in the future,” said Moser. “It’s clear that by working together, and amplifying the voices of physicians, we are able to achieve great things.”


ISSUE #150 5
The principal voice & resource for Central Kentucky physicians Physician Wellness Program 24/7 Medical Call Center Legislative advocacy in partnership with the Kentucky Medical Association Events and programing throughout the year LMS Dinner Social: March 21, 2024 –“The White Coat Investor” LEXINGTON MEDICAL SOCIETY Physicians taking care of the community since 1799 For more information visit lexingtondoctors.org or call (859) 278-0569 HEADLINES
In November of 2023, the American Lung Association released its “State of Lung Cancer” report, which revealed that Kentucky now ranks second in the nation for lung cancer screening rates.

2024 CPT and ICD-10-CM Changes for Fiscal Year 2024
BY BRANDY MONTGOMERY, HEALTHCARE CONSULTING MANAGER
Changes to CPT codes and ICD-10-CM codes for 2024 are coming. Thankfully, the changes for fiscal year 2024 are minimal compared to the extensive changes we’ve experienced over the last few years. There are 395 new, 13 revised, and 25 deleted ICD-10CM diagnosis codes for FY 2024. In addition, there are 153 new, 73 revised, and 102 deleted CPT codes for FY 2024.
CPT Changes
The 153 new CPT codes added for FY 2024 are codes in the Evaluation and Management section, several Surgery subsections (Musculoskeletal System, Respiratory System, Cardiovascular System, Urinary System, Female Genital System, Nervous System), the Radiology section, and Pathology and Laboratory.
The 102 deleted CPT codes were primarily pathology and laboratory codes, as well as Category III new technology codes.
The most extensive change implemented by CPT for FY 2024 was removing the time ranges from both the new and established office/ outpatient Evaluation and Management (E/M) codes and replacing them with a single total time amount, what had been the lower number of the range, which “must be met or exceeded.”
Even though the time range was replaced with a minimum time that must be met or exceeded, the activities that can be included in time-based coding/documentation have not changed from FY 2023, and they include:
• Preparing to see the patient (e.g., review of tests)
• Obtaining and/or reviewing separately obtained history
• Performing a medically appropriate examination and/or evaluation
• Counseling and educating the patient/ family/caregiver

• Ordering medications, tests, or procedures
• Referring and communicating with other healthcare professionals (when not separately reported)
• Documenting clinical information in the EHR or other health record
• Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver
• Care coordination (not separately reported)
ICD-10-CM Changes
The 395 new, 13 revised, and 25 deleted ICD-10-CM diagnosis codes affect 17 different chapters, with most of the changes occurring in the following 8 chapters: External Causes of Morbidity, Diseases of the Musculoskeletal System and Connective Tissue, Diseases of the Eye and Adnexa, Factors Influencing Health Status and Contact with Health Services, Diseases of the Nervous System, Diseases of the Eye and Adnexa and Congenital Malformations, Deformations and Chromosomal Abnormalities.
Brandy Montgomery can be reached at bmontgomery@deandorton.com
E/M Code Total time spent on date of the encounter (2023 guidelines) Total time spent on date of the encounter must meet or exceed (2024 guidelines) 99202 15-29 15 99203 30-44 30 99204 45-59 45 99205 60-74 60 99212 10-19 10 99213 20-29 20 99214 30-39 30 99215 40-54 40
Empowering physicians to focus solely on the demands of their clinical practice. Health system solutions & advisory services Medical billing & Finance & revenue cycle management Outsourced accounting, audit, & tax Risk management & compliance Technology & data analytics ACCOUNTING

Building Wealth Through Real Estate Investing
BY SCOTT NEAL, CPA, CFP®
Many years ago, a widowed client came in and said that she was faced with the dilemma of selling the family farm, worth about $1 million. She was hesitant to sell because the very low tax basis would produce a rather large capital gain tax burden upon the sale. I suggested that she consider doing a Section 1031 tax-free exchange into ten single family houses, each worth about $100,000. She looked at me and said, “Are you completely nuts? I am 85 years old.”
I explained to her that her age was why the strategy could work to her family’s advantage; her heirs would receive a step-up in basis upon her death. Furthermore, professional management could be obtained that would get her out of being a hands-on landlord. She ultimately went along with the idea.
Unlike many investment advisors, I have long been a fan of real estate investments, commercial as well as residential, to build wealth. This is because a) real estate tends to beat inflation over time, b) it carries favorable tax benefits, c) it is not correlated to the stock market or other financial assets, and d) it can effectively use debt to enhance return.
Navigating the complexities of real estate investing requires a solid understanding of the market, sound financial planning, and strategic decision making. We advocate having a solid team to assist. Here we will delve into the fundamentals of real estate investing, explore various strategies, and highlight key tips to help you succeed.
Tips for Success:
1. Conduct thorough market research. Before making any investment decision, it is essential to know local market trends, demographics, economic indicators, and regulatory issues. This is essential to mitigate risks and is often better left up to real estate professionals who are attuned with the local market.
2. Create a solid financial plan. It is imperative to establish clear investment goals, assess your own risk tolerance, and develop a budget that accounts for acquisition costs, ongoing expenses, allowances for vacancies, and the same sort of emergencies that can crop up in owning your own residence.
3. Build a reliable network of industry professionals, mentors, lenders, and potential partners. By cultivating relationships within the real estate community, investors can gain insights, identify opportunities, and expand their network.
4. Conduct due diligence. Before closing on a new purchase or even making an offer, investors should conduct thorough due diligence to assess the viability and potential risks associated with the investment. This may include property inspections, financial analyses, title searches, and legal review. Consider forming a limited liability company (LLC) or a series LLC if more than one property is to be owned (consult your legal counsel on that point.) Identifying potential pitfalls early on can help investors avoid costly mistakes.
5. Diversify the portfolio. All too often we see real estate investors hold just one property or multiple properties in close proximity to each other. Diversification is key to mitigating risk and maximizing returns in nearly all investments but rings especially true in real estate. Rather than focusing on one type of property, strategy, or location, consider diversifying your portfolio.
6. Utilize the tax code to maximum advantage. It is imperative to know the tax impact. Your preparer should be wellversed in the rules related to real estate, depreciation recapture, and passive income. If you can qualify to be an active investor, that is usually to your advantage.
When a client agrees to go along with our recommendation to explore real estate, we prepare a projection that runs from purchase to sale. We consider four potential sources of return: 1) cash-on-cash return from the net cash flow, 2) tax benefits, 3) appreciation, and 4) effects of leverage (debt). Each requires a separate calculation, but they all add up to total return.
Common Pitfalls to Avoid:
While real estate investing offers tremendous potential for wealth accumulation, it’s not without its challenges. Some common pitfalls to avoid include:
1. Taking on excessive to finance investments can ultimately strain cash flow, especially during economic downturns or periods of market volatility.
2. Ignoring market trends can lead to missed opportunities. The assessment of market trends does not end with purchase. Neighborhoods can change quickly.
3. Underestimating expenses can erode profitability and strain financial resources.
4. Successful real estate investing requires patience, discipline, and long-term perspective. Be patient and do your homework.
In Conclusion:
Real estate investing remains a compelling avenue for wealth creation. By understanding the fundamentals of investing, implementing sound strategies, and adhering to key principles, investors can unlock the full potential of a vehicle for wealth accumulation and enhanced financial freedom. Scott
Neal, CPA, CFP®
ISSUE #150 7
is
of D.
Neal,
a fee-only financial planning and investment advisory firm with offices in Lexington and Louisville. Reach out to him via email scott@dsneal.om or call 1-800-344-9098.
the President
Scott
Inc.,
FiNANCE


If you’re named in a medical negligence lawsuit, you’re in good company. According to the American Medical Association, one in three physicians will be sued for medical malpractice during their career. What now? The course of every medical negligence lawsuit is different, but here’s a general idea of what to expect:*
1. The Complaint/Answer
The plaintiff’s attorney will prepare a complaint and file it with the court system to initiate the lawsuit. In most cases, the plaintiff is the patient; if the patient is deceased, it will be the representative of the patient’s estate. The complaint details allegation(s) asserted against you and potentially against others (e.g., your medical group or other care providers), generally that you breached the applicable standard of care, thus causing injury to the plaintiff.
You’ll be notified of the suit through your practice’s risk manager, a representative from your medical group’s insurance company, or via certified mailing from the plaintiff’s attorney. If the latter occurs, it is important to alert your practice’s risk manager or your group’s insurance carrier immediately. Shortly thereafter, you’ll be contacted by an attorney hired to defend you. Your attorney will share and discuss the plaintiff’s complaint with you, then will file an answer on your behalf, which admits or denies each allegation.
2. Written Discovery
After the answer is filed, the written discovery process begins. The plaintiff’s attorney and your attorney will exchange written discovery requests. Requests consist of interrogatories (questions) and requests for production
A Phrase That Makes Every Physician’s Heart Skip a Beat: “You’ve Been
BY MEGAN ADKINS, ESQ., AND ASHLEY BOERRIGTER, MD
of documents from each party. Normally, the questions include asking about hospital affiliations, previous investigations of your medical license, if you have provided expert witness opinions throughout your career, as well as your education and training.
You’ll be contacted by your attorney to answer the plaintiff’s interrogatories without the plaintiff present. All communications you have with your attorney are protected under attorney-client privilege so long as no other persons are present.
3. Expert Witnesses
Your attorney will consult with expert witnesses to defend the medical treatment you provided. Expert witnesses are physicians who practice in your specialty and in similar clinical conditions; they will be compensated for their participation. For example, an interventional cardiologist in another state may provide an expert opinion on a case involving a death after STEMI. Different expert witnesses are hired by all parties to testify in support of their respective positions.
4. Deposition
After written discovery and consulting expert witnesses, the deposition stage occurs. Depositions are interviews conducted by parties’ attorneys of people with knowledge of the patient and/or the patient’s treatment. All questions are answered under oath. The interview recordings, both transcript and video, are eligible to be used in court.
Plaintiff Deposition Your attorney will ask the plaintiff any recollection they
Sued”

have of you, the medical treatment you provided, the patient’s medical condition before and after the treatment, and other relevant questions. You can choose whether or not to be present during this deposition..
Your Deposition You will have preparation meetings with your attorney prior to your deposition. The plaintiff attorney’s questions will generally focus on the scope of your practice and your specific treatment of the patient. Your attorney will also be present and intervene as needed.
Expert Witness Deposition(s) Expert witnesses testify regarding their opinion of the patient’s medical condition and whether the patient’s condition is related to the allegations in the lawsuit. All parties’ attorneys are present.
5. Mediation
Most judges order mediation (settlement conference) before trial. Mediation is generally conducted by an experienced attorney or retired judge. The mediator, plaintiff, plaintiff’s attorney, you, your attorney, and a representative from your insurance company meet in person to discuss potential settlement prior to trial. Your attorney will discuss the strengths of your defense and weaknesses of the plaintiff’s case. It usually lasts a full business day.
If the lawsuit is resolved at mediation, the plaintiff signs a document called a “Release and Settlement Agreement.” This document normally details that the lawsuit is being dismissed, you are not admitting liability for medical negligence,
8 MD-UPDATE
LEGAL

and the plaintiff is receiving a monetary sum. The agreement will also include various terms and conditions such as barring the patient from filing an additional lawsuit against you for the medical treatment at dispute in the current lawsuit.
6. Jury Trial
If the case is not resolved at mediation, it will proceed to trial. A medical negligence jury trial often takes place years after the lawsuit is filed; it lasts two to three weeks and requires your attendance every day. During the trial, both attorneys provide opening statements, then the plaintiff’s attorney
calls their witnesses. Your attorney then calls witnesses to rebut the plaintiff’s allegations and evidence. You will be able to testify, but this is not required; you and your attorney will decide prior to the trial. Lastly, both attorneys provide closing statements. Before deliberations, the jury is instructed to decide whether you breached the standard of care, and if so, the amount of damages to which the plaintiff is entitled. Kentucky Civil Rules require 9 of 12 total jurors to agree upon the verdict.
You may feel significant frustration and discouragement after being sued for medical
negligence. We encourage you not to be disheartened – being sued is common and not an indication of your medical ability. Take care of yourself emotionally during this time and reach out to your attorney as needed. The world needs you and the skillset you worked so hard to develop.
*This is not an exhaustive account for each event in medical negligence lawsuits.
Megan Adkins is an insurance and medical negligence defense attorney with Sturgill, Turner, Barker & Moloney, PLLC. She can be reached at 859. 255.8581.
Ashley Boerrigter, MD, is a board-certified OB/GYN and a maternal fetal medicine fellow at UK’s College of Medicine. This article is intended as a summary of state or federal law and does not constitute legal advice.

ISSUE #150 9
YOU CARE FOR EVERYONE♦ WE TAKE CARE OF YOU♦ From the business of health care to compliance to litigation defense, Sturgill Turner’s experienced health care and medical negligence defense attorneys provide comprehensive legal services to health care providers, hospitals and managed care organizations across the Commonwealth. Put our experience to work for you. Sturgill, Turner, Barker & Moloney, PLLC ♦ Lexington, Ky. ♦ 859.255.8581 ♦ STURGILLTURNER.COM AT T ORNEY S KENTUCKY | TENNESSEE LEGAL

The Heart
Interventional
cardiologists say the human connection is most important
BY JIM KELSEY
LEXINGTON It’s fair to say that cardiologists understand a thing or two about connections. After all, the human circulatory system is a series of connections facilitating blood flow throughout the body. Heart valves and chambers, arteries and veins are all different components, each integral to the overall goal.
Interventional cardiologists Hussam Hamdalla, MD, and Sharat Koul, DO, both part of the team at CHI Saint Joseph Medical Group – Cardiology in Lexington, excel at diagnosing and repairing faulty cardiac function in their patients. But before all the high-level medical procedures and treatments take place, both say it is a completely different kind of connection that is often the key to achieving positive results for their patients.
“We have an excellent team, and the nice thing is we complement each other.”
— Hussam Hamdalla, MD, CHI Saint Joseph Cardiology Associates
“The majority of my time is in the office talking to patients,” says Hamdalla, who, like Koul, previously practiced at Ephraim McDowell Regional Medical Center in Danville, Kentucky. “When I see a patient, I like to understand their background, where they live, what their profession is, what their family is like, because it puts everything into context. It’s hard to simply listen to the complaint without understanding the context of the patient as a human being and what parts of their lifestyle, personal life, or their professional life could be driving some of these symptoms.”
“My philosophy is to function as an advisor to patients,” Koul adds. “My goal is to help them understand all their options and, in the
Hussam Hamdalla, MD, medical director of the cath lab, joined CHI Saint Joseph in 2023.
PHOTOS BY MARK MAHAN
of the Matter
end, work together to come up with a treatment plan that is aligned with their overall healthcare goals. I think the most important thing is to listen to your patients and understand what they really want in life.”
Connecting and Collaborating
You could call it a heart-to-heart talk about the heart. It’s about combining caring, compassion, and understanding with skill and expertise. By joining CHI Saint Joseph Health, both Koul and Hamdalla have had the opportunity to develop their particular skills and refine their specialties.
“We have an excellent team, and the nice thing is we complement each other,” says Hamdalla. “We each have our special kind of niche of things we do, and together between us and our cardiac surgeon, we provide a pretty comprehensive management for cardiac problems.”
“All of the physicians bring a specific expertise in terms of being able to home in on specific parts of cardiovascular treatment,” says Koul, who specializes in limb salvage and cardiovascular disease. “You’re able to hone your skills to specific areas because the field itself is too broad to be an expert at everything,”
Koul sees patients in area clinics in Danville, Lebanon, Lexington, and London three-tofour days a week. Then he spends at least one day in the lab, where he performs multi-hour wound procedures on complex leg patients.
“The care of the wound populations tends to be very much multidisciplinary in terms of care,” says Koul. “I work with one of the best wound specialists in the state on a regular basis and I work with a lot of excellent physicians who do a lot of wound work in general. These patients require a lot of care, and there are a number of different specialties that come together to provide optimized care.”
Sharat Koul, DO, sees patients at weekly clinics in Danville, Lebanon, Lexington, and London.
COvER STORY
Koul grew up in the Washington, D.C., metro area, attended the University of Virginia, and then went to medical school at Kirksville College of Osteopathic Medicine in Missouri. He did his residency at Cleveland Clinic and took a cardiology fellowship at Advocate Illinois Masonic Medical Center in Chicago, followed by an interventional fellowship at the University of Kentucky. After working briefly in Atlanta, he moved back to Kentucky in 2011.
Specializing in limb salvage and complex cardiovascular disease means that Koul sees extremely sick patients with a lot of comorbidities.
“They tend to have a lot of multisystem disease processes, which tend to roll into non-healing wounds and ulcers,” says Koul. “I’ve always found that patients’ connections with their hearts were somewhat disconnected. The heart is in your chest, and you don’t really know if your heart function is 50 percent or 30 percent. But I’ve found that patients have a deep attachment to their legs. Patients are very appreciative if you can help them walk and keep their legs because it’s literally part of their everyday life.”
The importance of the patient-physician connection also resonates with Hamdalla, who sees patients in the office at least three days per week.
“My ‘Why’ is to get up in the morning and see those patients that I have been taking care of for 10 years,” says Hamdalla. “I feel like I’m an integral part of their lives. I have patients who come to me to ask my advice for non-cardiac related problems. They will see a different specialist and they come to me and say, ‘This is what they recommended and I refuse to do anything until you tell me what your thoughts are.’ That’s a reflection of the deep trust and bond that I have with the majority of my patients.”
Originally from Jordan, Hamdalla first studied internal medicine at Brown Affiliated Hospital in Rhode Island, and then cardiology and interventional cardiology at the University of Kentucky. Now at CHI Saint Joseph Health, he is the medical director of the cath lab.
“One of the things that brought me to Saint Joseph Hospital is to be able to grow and take the next step in my life,” says Hamdalla. “One
“These patients require a lot of care, and there are a number of different specialties that come together to provide optimized care.”
— Sharat Koul, DO, CHI Saint Joseph Cardiology Associates
of the things that I have taken on here is tackling complex, chronically occluded lesions that require a special set of skills. Most cardiologists don’t have the experience or the desire to deal with such complex situations. That is one thing that I have taken on to be able to offer patients more options.”
Those options, Hamdalla is quick to point out, include more than just stents.
“Just because we can do it does not necessarily mean we have to do it,” Hamdalla says of stents. “We know that with lifestyle modification, exercise, and appropriate medicines to keep the blood pressure and heart rate well controlled, patients will do as well a majority of the time.”
Patient Population Is Changing
Both Koul and Hamdalla note that their patient populations are becoming increasingly younger, as unhealthy lifestyles become more prominent and troublesome.
“The national health system is going to have to change so that we focus more on prevention,” says Koul. “The cost to our communities is enormous from the standpoint of not only money but also loss of life and functionality of life.”
“The idea that atherosclerotic disease, especially in the heart, is a medical problem rather than a surgical or procedural problem is becoming much more evident,” adds Hamdalla. “Globally, we are going to focus more on prevention, as we should, rather than dealing with things when the milk has already been spilt.”
A positive change in the patient population, according to Hamdalla, is that patients are now more informed about their conditions and options for care.
“I joke with my patients that they have consulted Dr. Google, and I don’t say that in a derogatory way,” says Hamdalla. “It makes it better for the patient if they have done some homework to understand what we are talking about. They come in sometimes with very legitimate questions. The best patients are those who are involved and engaged in their own care.”
Different Presentations in Men and Women
That learning curve extends to physicians as well. Hamdalla points out that there is a better understanding that cardiovascular disorders plague both men and women, contrary to the once-held belief that men were the predominant victims of heart disease. The difference lies not in the frequency of cardiovascular disease, but in how it presents itself in men and women.
“We have learned to appreciate the challenges and the differences in the presentation between men and women in terms of the heart disease symptoms and how to manage them and work them up differently,” Hamdalla says.
While the treatment regimen might differ from patient to patient, Hamdalla stresses that the overall approach remains the same.
“I enjoy building up that long-term relationship with patients, walking through their journey dealing with the disease,” he says. “It is part of my job not to just put that stent in, but also to hold their hand and talk them through it so they can start resuming their lifestyle.”
Connecting information and care to understanding helps build the patient’s confidence, not only in the knowledge and skill of their physicians, but also in their own ability to regain control of their health. Ultimately, that is at the core of what Koul and Hamdalla want for their patients.
“We aspire to be the leaders in cardiac care in the area,” Hamdalla says. “We are working on building and being that place where everybody wants to get their cardiac care at CHI Saint Joseph Health.”
12 MD-UPDATE
COvER STORY
Save the Date

Saturday | May 18, 2024
Humankindness Gala
Lexington Griffin Gate Marriott Golf Resort & Spa
Please join us as we recognize our caregivers and their dedication to humankindness. Enjoy an evening with cocktails, dining, silent auction and entertainment by the Best Kept Secret Band. This year’s event will pay tribute to Jeff Murphy, former Vice President of Marketing and Communications, by recognizing his love of the arts.
Flaget Memorial Hospital Foundation
Saint Joseph Berea Foundation
Saint Joseph Hospital Foundation
Saint Joseph London Foundation
Saint Joseph Mount Sterling Foundation
BENEFITING
Knowledge Is Power
Through advanced multimodal cardiac imaging, Dr. Mrin Shetty can predict heart disease before it happens.
BY DONNA ISON

LOUISVILLE Many women believe breast cancer is the leading cause of death amongst their gender. In actuality, heart disease claims nearly eight times the number of female lives yearly. According to Mrin Shetty, MD, an advanced multimodal imaging cardiologist and director of the Women’s Heart Health Program with UofL Health – Heart Hospital, “The truth is breast cancer kills about one in thirty women, but heart disease kills one in three women. And the main culprit is coronary artery disease.”
There are many other misconceptions that Shetty also encounters in her role. First, that heart disease presents itself the same in men and women. Shetty states, “Women are not small men. We may have the same disease process but present very differently. For example, a heart attack doesn’t always present with chest pain in women, it may manifest as progressive fatigue, lightheadedness, indigestion, nausea, vomiting. Historically, women’s symptoms have been brushed off and under-recognized, and I feel like we need to change that.”
Another fallacy that exists is that heart disease only affects older women; younger women in certain groups are also at high risk. These include patients during pregnancy and those undergoing chemotherapy for breast or some other cancer.
For Shetty, shedding light on these false beliefs and using advanced cardiac imaging techniques to predict disease are the first steps in the prevention of coronary artery disease and detection of infiltrative cardiomyopathies. “We need to give women the cardiovascular care that they deserve in a welcoming and safe environment where they feel that they are heard. And that is exactly what I’m trying to do with the Women’s Heart program,” Shetty says.
After growing up and attending medical school in Mumbai, India, Shetty moved to the U.S. to participate in externships with Massachusetts General Hospital in Boston and Mount Sinai in New York City. She then went on to complete an internal medicine residency at Saint Peter’s University Hospital - Rutgers Robert Wood Johnson Medical School in New Brunswick, New Jersey, where she served as chief resident. During her cardiology fellowship at the University of Chicago (NorthShore) program, Shetty filled the role of chief cardiology fellow. She then completed her formal education with advanced cardiac imaging training at Columbia University in New York. Following this training, Shetty came to the University of Louisville in 2023.
PHOTO BY JOHN LAIR
Advanced Multimodal Cardiac Imaging Is an Emerging Field
Multimodality imaging, a relatively new subspecialty within the broader field of cardiology, utilizes advanced imaging techniques, such as cardiac computed tomography (CCT), echocardiography, positron emission tomography (PET), cardiac magnetic resonance (CMR), and nuclear cardiology to view cardiac anatomy and function to assess risk and pathology.
In the past, patients may have been given a vague diagnosis of general heart failure or a thickened heart. Advanced imaging has changed that. Shetty explains, “Now, you can specifically find the cause of what is afflicting the heart muscle by looking at it in ways that we did not utilize in the past. We can detect atherosclerosis way before it becomes obstructive or symptomatic. In the right and motivated patient, they can take the steps necessary to never have that heart attack. And, to me, that is very exciting.”
Though still a niche within the field of cardiology, the value of multimodal imaging to offer greater insight into the cause and treatment of cardiovascular disease is undeniable for many types of patients, including high-risk individuals for whom screening
14 MD-UPDATE
Mrin Shetty, MD, is an advanced multimodal imaging cardiologist and the director of the Women’s Heart Health Program within UofL Health – Heart Hospital.
may prevent future incidence, persons with unspecified chest pain, and those with undiagnosed infiltrative cardiomyopathy.
Along with her other duties, Shetty participates in research, serves on committees for academic societies, and has written numerous papers, all to move the needle forward in terms of cardiovascular imaging. Shetty is also devoted to her role as an educator—both of future physicians and of patients. As an assistant professor of medicine at the UofL School of Medicine, Shetty is highly involved with the cardiology fellows as well as residents and medical students from internal medicine, family medicine, and even pharmacy.
Looking Forward to a Bright Future with UofL Health
The primary reasons Shetty and her husband, Dr. Yuvraj Chowdhury, who is an interventional cardiologist, chose UofL Health were the institution’s leadership, clear vision, and dedication to growth and excellence.
According to Shetty, “For early-career physicians, like my husband and me, you want to jump on the wagon when there’s excitement and a lot of positive energy going into building a program.”
In 2022, Kim Williams, MD, who is considered one of the grandfathers of cardiology, joined UofL Health as the chair of the department of medicine. Dinesh Kalra, MD, serves as the director of Advanced Cardiac Imaging, Lipid Clinic & Infiltrative Heart Disease Program. Shetty states, “For an advanced imager, like me, having Dr. Williams and Dr. Kalra as your mentors, that’s an opportunity you don’t pass up.”
Shetty is also enthusiastic about the impact the Women’s Heart Program can have throughout the state. “I think it is an exciting time. We have a dedicated team of cardiologists who are committed to the care of the female heart. We’re collaborating with different specialties—OB-GYN, oncology, rheumatology—to better serve those high-risk
patients who need dedicated cardiovascular care. We will be working on women-centered cardiac research and ensuring inclusivity in clinical trials and healthcare programs. Some people don’t expect to see that in their own local community, but we’re expanding our outreach and education.”
UofL Health’s cardiology department acknowledges the importance of health literacy. Through health fairs and community events, they hope to enlighten individuals to the fact that lifestyle plays a critical role in heart health.
The culmination of Shetty’s work is all in pursuit of one goal: allowing patients to live their best lives. Shetty says, “A lot of people just do not know how good their bodies can feel. Taking an individual with a body that is a vessel for suffering and pain and discomfort to one that becomes this instrument for vitality, I think that is a powerful thing. And having the ability to do that is what puts a spring in my step every day.”























ISSUE #150 15
CONTACT GIL DUNN (publisher/editor): 859.309.0720 859.608.8454 • gdunn@md-update.com ISSUE #146 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS VOLUME 13 #3 JULY 2023 LEGACY OB-GYN DOCTOR AT WOMEN FIRST OF LOUISVILLE REFLECTS AND LOOKS FORWARD CHI SAINT JOSEPH HEALTH PSYCHIATRIST SEES DISTURBING TRENDS IN ADOLESCENET MENTAL HEALTH PEDIATRIC ORTHOPEDIC SURGEON AT SHRINERS HOSPITAL LEXINGTON ORAL HEALTH IS PART OF PRIMARY CARE ISSUE #147 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS A Cut Above Lexington Clinic Orthopedic Surgeon Tharun Karthikeyan, MD, Embraces the Advantages of the ROSA Robot ALSO IN THIS ISSUE L HEALTH CENTER FOR FOOT AND ANKLE EXCELLENCE UK HEALTHCARE PHYSICAL MEDICINE REHABILITATION HAS A NEW HOME CHI SAINT JOSEPH HEALTH ORTHOPEDIST IN SMALL COMMUNITY SEES GENERATIONS OF PATIENTS SPORTS HEALTH AND SHOULDER RECONSTRUCTIOIN PROGRAM AT NORTON HEALTHCARE THE FUTURE FUND, SAVING FLOYDS FORK ISSUE #148 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS Not Your Mother’s Breast Care Focusing on early detection and targeted care, the surgeons at Baptist Health Breast Surgery are ensuring patients receive the most innovative and individualized care available ALSO IN THIS ISSUE (CAR) T CLINICAL TRIALS AT L HEALTH - BROWN CARE CENTER 3D MAMMOGRAPHY IS WELL CARE AT WOMEN FIRST LOUISVILLE CHI SAINT JOSEPH HEALTH ONCOLOGY IN RURAL COUNTIES GLIOBLASTOMA RESEARCH & TRIALS AT NORTON CANCER INSTITUTE .com OVER 150,000 visits! SPECIAL SECTION CARDIOLOgY – IMAgINg
Heart Care is Changing for the Better in Cynthiana
Harrison Memorial Hospital adds cardiac MRI
BY gIL DUNN
CYNTHIANA Harrison Memorial Hospital
(HMH), an independent, not-for-profit, community-based hospital in Cynthiana, Kentucky, has recently taken significant steps to increase and enhance cardiac care for its patients in Central Kentucky by investing in equipment and staff.
In July 2023, Yaz Daaboul, MD, joined the HMH medical staff to lead their Advanced Cardiac Imaging Program, and in October, the hospital upgraded the equipment for its MRI system to perform cardiac MRIs.
With the introduction of cardiac MRI, HMH now offers a complete spectrum of cardiac imaging services, including exercise and pharmacological nuclear cardiac stress imaging, transthoracic echocardiograms, transesophageal 3D echocardiograms, cardiac computed tomography angiography (CCTA), tilt table tests, short-term and long-term heart rhythm monitors, and electrocardiograms. These services, combined with interventional cardiology led by Matthew Shotwell, MD, make Harrison Memorial Hospital’s cardiac services truly comprehensive.
With cardiovascular MRI now available, cardiologists at HMH have enhanced ability
to treat patients with a range of heart conditions, including heart failure and cardiomyopathies, myocarditis, infiltrative disease, valvular heart disease, congenital heart disease, cardiac masses, and pericardial disease.
“The introduction of cardiac MRI is a tremendous addition to our cardiac services and reinforces our dedication to staying at the forefront of medical technology. It also ensures the best possible outcomes for our patients,” says Stephen Toadvine, MD, CEO of Harrison Memorial Hospital. “We remain dedicated to providing high-quality, patientcentered cardiac care for our community.”
Meet Yaz Daaboul, MD
Yaz Daaboul, MD, is board-certified in internal medicine, cardiovascular disease, structural and general echocardiography, and nuclear cardiology medicine. Daaboul obtained his Bachelor of Science in biology from the American University of Beirut, Lebanon, followed by his medical degree from Lebanese American University, Lebanon. He completed his internal medicine residency at Tufts Medical Center, Boston, where he also completed fellowships in cardiology and advanced cardiac imaging.

According to an HMH press release, Daaboul has authored more than 100 original research publications, abstracts, and book chapters, including in Topol’s Textbook of Interventional Cardiology, Braunwald’s Heart Disease companion textbook for Nuclear Cardiology and Multimodal Cardiovascular Imaging, and Springer’s textbook on Quality Measures. His research work has been cited 2000+ times.
He also serves as the medical director of the Imaging Core Lab at Baim Research Institute in Boston.
Meeting Unmet Needs
Daaboul enthusiastically speaks about his passion for excellence, “meeting unmet needs” when it comes to his education, his training, and his care for his patients. Lebanon, he says is a great country and provided him with a great medical education, but “Nothing compares with the opportunities and training in healthcare that is found in the U.S. We are constantly and extensively training to be the best doctors in the world. I wanted to be part of that,” he says.
Being the best version of himself included ten years at Tufts Medical Center, in a fast-paced urban environment, surrounded by

16 MD-UPDATE
SPECIAL SECTION CARDIOLOgY – IMAgINg

colleagues as determined as he was. When the opportunity was presented to him to lead his own program at Harrison Memorial Hospital in a rural setting, he took the challenge.
“I feel like I am finding my own way, meeting my needs to be the best doctor that I can be,” Daaboul says. “When you’re a doctor in a rural environment, you meet patients, not only in clinic, but also in the community. You’re not just a doctor in an office; you’re part of the community. It’s really refreshing; and it reminds me why I wanted to be a doctor in the first place — helping people.”
The magic of cardiology, says Daaboul, is that every day is different. “Literally, every hour of every day you don’t know what’s in the next room, who you’re going to meet, what condition they have, how you are going to help them get better.”
The diversity of cases is seen in Daaboul’s patient population, which can range from a young individual with congenital heart defects, to middle-aged individuals with sudden onset of symptoms or chronic heart disease, to older patients with advanced heart disease. He also sees some patients for preventative cardiac care. A typical week is clinic four days a week, Monday through Thursday, from 8 am to 3:30
pm, seeing, along with a team in the cardiology clinic, around 80 to 100 patients per day.
“We have an incredible team of nurses and staff who do all the heavy lifting,” says Daaboul. “It truly takes a village to see all the patients that we see in one day and to care for each of them in a patient-centered approach.”
Currently, the cardiology team at HMH has 15 team members, which includes two cardiologists and four advanced practice providers.
“Most importantly, we are an open clinic,” says Daaboul. “We are practically a walk-in clinic for people who are having symptoms of heart problems. We never turn someone away. Our scheduled 80 patients per day can easily turn into 100.”
Cardiac Care in Rural Kentucky
Cardiovascular disease is widespread in the Cynthiana community, says Daaboul. “Cardiac comorbidity is palpable and prevalent,” he says. “As a cardiologist, I have to adjust my threshold on what to look for in my patients for underlying causes, like smoking, obesity, diabetes — all of the common risk factors in the community. I also have to understand that in a rural community, many of my patients have not had longterm access to preventative healthcare, so many
symptoms were ignored, or not managed, until a bigger problem exists, and they finally come in to see me. That is a challenge.”
Bringing advanced cardiac imaging to his patients at HMH will be a gamechanger, says Daaboul. “Now, for instance, we’re not only listening to the heart valves, but we’re looking at them and scrutinizing the heart chambers and tissue characteristics as well. We’re growing our program, and it’s a manifestation of how much our patients trust us with their care, with their family’s care, and their extended families as well.”
One of the hallmarks of cardiac MRI is that it does not involve radiation exposure, making it a safe and effective diagnostic tool. “Patients can expect precise and detailed images of their heart’s chambers, valves, and muscles, facilitating accurate diagnoses and improving treatment plans,” says Daaboul.
HMH CEO Toadvine says that the volume of cardiac MRIs at HMH started at one or two per day and has been rapidly increasing since the installation.
Research and Clinical Trials
As medical director of the Imaging Core Lab at the Baim Research Institute, research remains one of Daaboul’s passions. One of his goals is to add Harrison and surrounding counties to the map of cardiovascular clinical trials. “Being part of the research that generates the guidelines and treatments in the cardiovascular field gives us the opportunity to tailor our treatments in a way we know for a fact our patients would benefit from,” says Daaboul.
“We are in active communications with research partners about making Harrison Memorial a site of clinical trials,” says Daaboul. There is precedent, he notes, such as the Framingham Heart Study, where, since 1948, researchers have conducted long-term cohort studies on arteriosclerotic cardiovascular disease, collecting data from three generations of residents in a small town in Massachusetts.
“If anything, Cynthiana and Harrison Memorial are great at pioneering things, and I won’t be surprised that, at some point in time, there will be a Cynthiana Heart Study,” says Daaboul.
ISSUE #150 17
PHOTO BY LEE THOMAS
SPECIAL SECTION CARDIOLOgY – IMAgINg
Yaz Daaboul, MD, joined the HMH medical staff to lead HMH’s Advanced Cardiac Imaging Program.
Making Sure the Beat Goes On
Norton Healthcare’s cardiovascular and surgical experts team up for advanced heart rhythm care
BY MENISA MARSHALL
LOUISVILLE World-class boxing champion
Sugar Ray Robinson once said, “Rhythm is everything. Everything starts with your heart, and if it’s not in rhythm, you’re in big trouble.”
Kent E. Morris, MD, MBA, who is board-certified in internal medicine, cardiology, and electrophysiology, can appreciate Robinson’s insights. Morris is associate director for Norton Heart & Vascular Institute and serves as medical director of electrophysiology.
EP, as it is known, assesses and treats conditions that affect the heart’s electrical system and activity. It uses radiofrequency ablation, pacemakers, and automatic implantable cardioverter defibrillators (AICDs) to fix hearts that are unable to maintain a healthy rhythm.
Morris explains that treating abnormal heart rhythm conditions generally falls within two broad areas. One is arrhythmia management, which includes atrial fibrillation or supraventricular tachycardia (SVT). The other involves implantable cardiac devices, such as pacemakers or defibrillators.
While SVT can present at any life stage, it often involves younger patients. Atrial fibrillation, commonly abbreviated as AFib, generally impacts older patients, but can occasionally affect those in their 30s or even their 20s.
Pacemakers are more commonly used among an older population. Implanted defibrillators — largely indicated for prevention of sudden cardiac death in patients with prior heart attack or cardiomyopathy — are used across all ages.
AFib, which can be paroxysmal (intermittent) or persistent (continuous), can be treated with medications or with ablation. During his years in practice, Morris has seen great progress in ablation procedures both in the technology as well as improvement in the outcomes. This progress has led to stronger recommendations for AF ablation in the clin-

ical guidelines. His team has treated many patients who have done well for decades after the procedure.
“I always hesitate to say we can cure AFib, but I think in some patients we’re able to do that,” Morris says.
The earlier heart disease is diagnosed, the better patients’ outcomes tend to be, and this is especially true for Afib, says Morris. He cautions however this may not apply for older patients with multiple comorbid factors, especially if those factors are not well controlled.
Game-Changing Technologies and Multidisciplinary Care
Morris describes interventional electrophysiology as a relatively new field. The first external pacemaker was invented around 1960. Implantable pacemakers soon followed. The first ablations occurred in the 1990s.
When he began practicing 14 years ago, AFib ablation could be a day-long procedure that often involved an overnight hospital stay. Today, it generally takes two to three hours, and most patients are home the same day.
“We can now make 3D electro-anatomic maps very quickly with 5-to-10,000 data
points that represent both the anatomy and electrical signals inside the heart,” says Morris.
Norton Heart & Vascular Institute is committed to innovation. In 2016 it was the first program in the Louisville area to complete a minimally-invasive WATCHMAN™ procedure. WATCHMAN devices help reduce stroke risks for patients with non-valvular AFib. They offer an alternative treatment for patients who cannot use blood thinners long term.
In 2021 the WATCHMAN FLX, which Morris considers easier and safer to use, was introduced. Fast-forward to January 2024 and Morris’ team completed its five hundredth WATCHMAN procedure, the first in Louisville to implant this many.
Morris applauds hardware and computing advancements for helping specialists achieve outcomes that were hard to imagine 10 or 15 years ago. Yet, he is quick to credit excellent multidisciplinary team work for much of the EP clinic’s overall effectiveness.
“We have nurse practitioners, physician’s assistants, nurse navigators, device nurses, device technicians, as well as amazing support staff,” says Morris. “It takes all of us to care for our patients.”
Common — and Surprising — AFib Causes and Culprits
AFib is a complex disease process. It can be related to genetics as well as modifiable risk factors such as hypertension, diabetes, obesity, alcohol use, and sleep apnea.
Full, accurate histories for patients are crucial since numerous classes of medications can potentially cause AFib. Various prescription and over-the-counter medications — including common cold treatments — have the potential to stimulate the heart and cause AFib.
A number of other factors can contribute to Afib. Patients are often surprised to learn sleep apnea, especially if it’s untreated, is a significant AFib risk factor. Individuals with
18 MD-UPDATE
SPECIAL SECTION CARDIOLOgY – ELECTROPHYSIOLOgY
Kent E. Morris, MD, is associate director for Norton Heart & Vascular Institute and serves as medical director of electrophysiology. PHOTOS
BY JAMIE RHODES

sleep apnea may complain of sleepiness or snoring, but they don’t connect their apnea to Afib symptoms such as a pounding heart or overall lack of energy.
Most sleep apnea patients are prescribed a CPAP machine to wear while sleeping, yet some people struggle with the equipment or decide for various reasons not to use it. Morris stresses it’s crucial to use CPAP equipment consistently as prescribed. Credible studies and literature conclude that successful treatment of Afib for patients with sleep apnea is unlikely unless the apnea is treated.
“If you have an ablation and you don’t treat your sleep apnea, the long-term success rates are almost as bad as if you never had an ablation,” says Morris. “If you have sleep apnea, you treat it, and you get an ablation, then your success rates are about as good as people that don’t have sleep apnea.”
When Morris sees new patients, he stresses that medications and technology can help them a lot, but they must also do their part to control their AFib. He lets them know credible data support the importance of controlling
their blood pressure, weight, diabetes, and glycemic levels and limiting their alcohol use.
“Atrial fibrillation is quite a varied disease. Depending on a number of factors, we have a very good chance of curing some people,” says Morris. “For others, it’s more a chronic disease we strive to manage over time.”
A Simple Aim: Live Life and Enjoy It!
Morris, who grew up in southern Illinois, was drawn to science at an early age. He enjoyed working with people and found opportunities throughout high school and undergraduate studies that led him to focus on medicine.
During his studies at Southern Illinois University School of Medicine, the future doctor was drawn to physiology-based and conceptual fields. He soon developed a special interest in cardiology.
While doing his fellowship at St. Vincent Heart Center in Indiana, Morris became friends with a student from Louisville. His friend connected him with a private cardiol-
ogy practice that hired him in 2010. A year later Norton Healthcare purchased the practice, which would become Norton Heart & Vascular Institute.
Morris strives to provide high-quality, compassionate, patient-centered care. Seeing the profound impact heart rhythm disorders make on people’s lives gives him a special appreciation for the trust his patients put in him and his colleagues.
It is gratifying, he says, to see patients come in for follow-up and report they are living full, happy, productive lives. Many patients say they no longer fear simple activities that might have once caused their hearts to “jump out of rhythm.”
“It can be a bit bittersweet,” says Morris. “On one hand your patients may no longer need you quite as much, yet it’s fantastic to see they are essentially cured of a heart rhythm disorder.”
Ultimately, Morris’ message to patients, and others as well, is simple: “We’re here if you ever need us, but go out and live life and enjoy it!”
ISSUE #150 19
SPECIAL SECTION CARDIOLOgY – ELECTROPHYSIOLOgY
Kent E. Morris, MD, describes the placement of the WATCHMAN device in the left atrium of the heart.
Nurse Practitioner
Becomes First Advanced Practice Clinician with Certification in Hypertension
Baptist Health Medical Group Cardiology began a certified hypertension program for patients with treatment-resistant hypertension
BY GIL DUNN
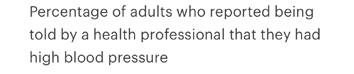
LEXINGTON A CDC report from the Behavioral Risk Factor Surveillance System in 2021 said that almost 40% of Kentuckians reported that they had high blood pressure. The national average in the U.S. is 32.4%. The same study said that the state with the highest percentage of individuals reporting with high blood pressure was Mississippi, with 43.9%. The state with the lowest population with high blood pressure was Colorado, with 26%.
Treating patients with refractory, or treatment-resistant, hypertension has been the goal of Kristy Salley, APRN, CVNP-BC, CHC, since she received advanced training as a certified hypertension clinician in 2021.
Salley recently obtained additional training and education through the American Board of Cardiovascular Medicine and is now a board-certified cardiovascular nurse practitioner, CVNP-BC, in addition to being a certified hypertension clinician (CHC). The CVNP-BC training was “more acutely focused on cardiovascular health than my previous APRN training, including “more in-depth interpretations of electrocardiograms,” she says.
Salley was the first nurse practitioner in Kentucky to achieve the certification in hypertension from the American Hypertension Specialist Certification Program. She continues to be the only nurse practitioner in Kentucky to hold this achievement. She has been a cardiology nurse practitioner for eight years, having received her nursing degree and APRN certification at Eastern Kentucky University. On her own initiative, she researched the steps necessary to pass the certification test.
Baptist Health Medical Group Cardiology and Salley began the specialized in-office hypertension program in May 2021. Obstacles with COVID-19 restrictions initially affected patient flow. Salley says the practice used telehealth visits effectively and has seen a full return


20 MD-UPDATE
SPECIAL SECTION CARDIOLOGY – HYPERTENSION
Kristy Salley, APRN, CVNP-BC, CHC, with Baptist Health Medical Group Cardiology, is a certified hypertension clinician and nurse practitioner.
“My goal and personal philosophy are to provide safe, holistic, patientcentered care to the best of my abilities and to treat each patient with respect, dignity, and empathy.”
— Kristy Salley, APRN, CVNP-BC, CHC
of in-office visits as COVID-19 infection rates have declined.
Individualized Patient Care
The patient population that Salley believes can most benefit from her care are patients with refractory hypertension who are on multiple anti-hypertensive medications with comorbidities such as coronary artery disease, diabetes mellitus, chronic kidney disease, obesity,
and peripheral vascular disease. She says she often rules out patients for secondary causes of hypertension such as renal artery stenosis, hyperaldosteronism, or pheochromocytoma.
“With my certification, I provide expertise in the management of refractory hypertension with consideration of concomitant medical conditions. I follow and work closely with my patients to improve their blood pressure and overall health outcomes. I obtained my certification in hypertension so I could better serve our population of patients in Kentucky,” says Salley.
Hypertension is known as “the silent killer” because it is frequently undetected until a cardiac event. Refractory hypertension is the most challenging. Uncontrolled hypertension can lead to serious complications such as heart attacks, strokes, and organ damage. Salley states that she saw the need for Kentuckians to have a skilled health care provider with additional training specific in hypertension. For this reason, she chose to pursue this avenue to help the community.

“My goal and personal philosophy are to provide safe, holistic, patient-centered care to the best of my abilities and to treat each patient with respect, dignity, and empathy,” says Salley.
There’s a Mobile App for That
Since 2021, the hypertension program with Baptist Health Medical Group Cardiology has seen consistent growth. With an increase in patient volume, more clinic days have been added to accommodate patients struggling with resistant hypertension. “Hypertension is a major cardiovascular risk factor and is especially prevalent in Kentucky,” says Salley. The clinic has enabled her to help many patients obtain normalized blood pressure readings, even for those with resistant hypertension on multiple anti-hypertensive medications with other comorbidities.
A grant funded by the American Heart Association for hypertension was awarded to Baptist Health Paducah in late 2023, aimed at improving hypertension monitoring and management. The grant has enabled the implementation of a comprehensive program that includes staff training, the provision of blood pressure devices, and the introduction of the MyChart Care Companion app. Baptist Health Medical Group Cardiology is the first cardiology practice to benefit from the grant by utilizing the new app. The app connects to the patient’s MyChart account and provides several features, including tracking blood pressure more effectively and providing guidance on a healthy diet, weight loss, and stress management. This functionality is designed to target adults age 18+ with hypertension, hypertensive cardiovascular disease without heart failure, chronic kidney disease, secondary hypertension, and abnormal blood pressure readings without diagnosis, allowing the patient to participate more actively in their care and to communicate more with their provider to improve cardiovascular health.

“Each reading from the app is patient specific in real time. For those patients who are less tech-savvy, there’s a telephone helpline to walk patients through the process,” says Salley.
For more information, or patient referral, contact 859.277.5887.
ISSUE #150 21
PHOTO PROVIDED BY BAPTIST HEALTH LEXINGTON Bring them to us. For nearly 30 years, we’ve helped hundreds of clients solve their biggest money concerns. Stop worrying, and start living life on a path towards financial freedom and security. Thinking clearly about money. Caring deeply about you. FEE-ONLY FINANCIAL PLANNING LEXINGTON | LOUISVILLE 800.344.9098 | DSNEAL.COM What financial concerns keep you awake at night? See how we think about money dscottneal.com
SPECIAL SECTION CARDIOLOGY – HYPERTENSION
A Century of Commitment to the Fight Against Heart Disease and Stroke
100 Survivors Project launches to celebrate centennial milestone, kick off American Heart Month
BY AFTON FAIRCHILD MARKETING COMMUNICATIONS DIRECTOR KENTUCKY AMERICAN HEART ASSOCIATION
KENTUCKY To celebrate its 100th birthday and in honor of American Heart Month and National Wear Red Day in February, the American Heart Association in Kentucky launched the 100 Survivors Project, which celebrates individuals from across the Commonwealth who have battled heart disease and stroke-related conditions. Throughout its Centennial year, the Association will feature local survivors’ stories on its social media platforms, at events to honor their journeys and spread awareness about heart and brain health.
“As we close out our first 100 years and begin the next, our work remains as important as ever, and no one better represents the work of the American Heart Association than survivors of heart disease and stroke,” says Andrea Ooten, executive director in Central and Eastern Kentucky. “In addition to showcasing the real faces behind the statistics, we know that sharing the impactful stories of these resilient survivors will provide hope and inspiration to others facing similar battles.”
A celebration of a century of profound impact on heart health and well-being, 2024 also marks the start of the organization’s Bold Hearts celebration. In addition to telling the stories of survivors whose journeys have been fueled by their own bold hearts, the Association’s second century of mission-critical work now begins and the organization will continue its steadfast commitment to making the bold moves needed for new paths of scientific discovery, eradicating barriers to health equity and advocating for policies that give every


Kentuckian the opportunity for a longer, healthier life.
Celebrating 100 Years
The American Heart Association was founded by six cardiologists on June 10, 1924, but the distinguished achievements of the organization for the past century are the result of the passion of more than 40 million volunteers, supporters, employees, and more than $5 billion invested in scientific research. But there is still work to be done. According to the Kentucky Office of Vital Statistics, heart disease and stroke remain the No. 1 and No. 5 leading causes of death in Kentucky.
“Our relentless pursuit will continue until heart disease and stroke are the stories of our past, and not of our future,” says Ashley Sokoler, executive director of the American Heart Association in Kentuckiana and Western Kentucky. “We also know we can’t create a world of equitable health and well-being alone, which is why volunteers, donors and advocates play such an important part in accelerating our lifesaving work.”
The American Heart Association’s Centennial is a celebration of the lifesaving achievements that exemplify a shared vision for a bold new century that will exponentially advance heart and brain health. The Association shares a commitment to bettering the health of all citizens with like-minded community leaders and organizations, who are relentless in their efforts to eliminate heart disease and stroke in the new century.
To learn more about the Association’s 100th birthday or how to participate in the 100 Survivors Project, visit www.heart.org/kentucky or contact Afton Fairchild at afton.fairchild@heart.org for more information.
22 MD-UPDATE
Rep. Kimberly Moser, co-sponsor of House Bill 331, with local youth advocates, Alexis Loveless of Louisville and Max Thompson of Georgetown, both of whom are heart survivors.
COMPLEMENTARY CARE
Yolana Wakefield-Wilson, Community CPR Manager with the American Heart Association, provides a Hands-Only CPR demonstration to Sen. Shelley Funke Frommeyer.





100 SURVIVORS FOR 100 YEARS
















Improving Provider Engagement in Lung Cancer Screening Awareness
Physician encouragement to get screened and quit smoking is essential and effective
BY ELIZABETH ANDERSON-HOAGLAND, CHFS, DPH, DPQI
FRANKFORT Lung cancer is the leading cause of cancer death in Kentucky, despite being the third most common type of cancer. Over 4,500 mothers, fathers, sisters, brothers, sons, and daughters are diagnosed with lung cancer each year. Cigarette smoking remains the top cause of lung cancer, with eight in ten cases tied directly to the patient’s own cigarette use.1 However, it’s important to note that radon exposure (a colorless, odorless gas that is naturally found in some types of rock), occupational exposure, and exposure to secondhand smoke are also risk factors and can multiply one’s risk.
In the past, lung cancer was a death sentence, but with modern medical technology and medications, lung cancer can be treated if caught at an early enough stage. Six in ten adults will be alive five years after diagnosis if lung cancer is caught at a localized stage.2 If cancer is caught early, patients will not only live longer but also have a higher quality of life. Unfortunately, only 24 percent of cancers are caught at a localized stage. This is why screening is so important.
Increasing Lung Cancer Screening
Current recommendations for an annual low-dose CT scan are for those who:
• Are 50 to 80 years old (or 50-77 through Medicare);
• Have a 20-pack-year smoking history;
• Currently smoke or have quit within the past 15 years.3
Low-dose CT scans are quick and painless and involve no needles or dyes. For those who meet the screening criteria, an annual lowdose CT scan is covered by insurance with no co-pay to the patient.
1 What Are the Risk Factors for Lung Cancer? U.S. Centers for Disease Control and Prevention.
2 American Lung Association. State of Lung Cancer Report 2022: Kentucky.
3 U.S. Preventive Services Task Force. Lung Cancer: Screening. U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality.
However, only one in ten eligible Kentuckians are being screened for lung cancer.4 By comparison, over 70 percent of eligible women have received mammograms and 74 percent of eligible Kentuckians have received colonoscopies or equivalent colon cancer screening. Why is there such a huge discrepancy in screening rates between cancers?
There are a few reasons why lung cancer screening rates lag behind that of other cancers:
1. A change to guidelines in 2021;
2. Stigma around smoking and cigarette use;
3. Lack of established protocols in health care settings.5
The U.S. Preventive Services Task Force re-examined the evidence for lung cancer screening and found benefit for lowering the age of screening from 55 to 50. This important change means millions more Americans are eligible for screening that were not previously able to access the testing. Changes to screening protocols can take time to filter to primary care providers, who have a busy case load with more work to be done than hours in a day. One of the stated goals of the state Lung Cancer Screening Program is to provide outreach and education to healthcare providers to make sure everyone is familiar with the new guidelines.
In 2024 it is widely established that smoking has adverse health consequences and remains the leading cause of death and disability in Kentucky and the United States. Unfortunately, common language about smoking calls it a habit, rather than, more accurately, a nicotine addiction, and people who smoke blame themselves for being unable to quit, rather than blaming commercial tobacco companies that deliberately engineered cigarettes to be more addictive. That self-blame can manifest as
4 American Lung Association.
5
defensiveness when patients are asked standard questions by providers about tobacco use history. As addiction is a chronic, relapsing disease, health care providers can also grow weary of asking the same tobacco questions over and over again, as there is the belief that people will “just quit when they want to.” We know, however, that half of all people who quit smoking do so because their doctor recommended it. Health care provider recommendations absolutely make a difference.
Health care clinics and offices can and should develop policies and procedures about lung cancer screening to increase screening rates.6 Teams should get together to discuss what makes the most sense in their patient flow, but some recommendations follow. First, every single patient should be asked about tobacco use at every visit. This reduces the likelihood that tobacco users feel singled out as it is a standard question, reduces likelihood of missing a tobacco user who has potentially just started using or relapsed recently, or simply forgetting in the hustle and bustle of the day. Clinic staff should make sure they are aware of current lung cancer screening guidelines, as well as the benefits and risks of lung cancer screening, so they are able to help patients make the decision whether screening is right for them. Since time is at a premium during patient visits, having hard copy materials such as brochures and fact sheets can both act as a prompt for providers and patients, and as an educational resource for patients.
If interested in downloadable fact sheets and posters about lung cancer screening, please email LungCancer@ky.gov for pdfs.
24 MD-UPDATE
et al. An assessment of primary care and pulmonary provider perspectives on lung cancer screening. Annals of the American Thoracic Society.
Trippette M,
Vol. 15; 1. September 21, 2017.
Elizabeth Anderson-Hoagland is health promotion supervisor in the Kentucky Department for Public Health, Division of Prevention and Quality Improvement
PUBLIC HEALTH
6 McDowell S. New lung cancer screening guidelines increase eligibility. American Cancer Society.

Are You Craving Connection?
Start sharing your feelings... and be smart about it
BY JAN ANDERSON, PSYD, LPCC
CLIENT Yeah, things are good with us. We’re crazy busy, doing all kinds of stuff… It’s just that I miss the closeness we used to have. It’s like we’re two ships passing in the day. We’re friendly and we wave, but it’s all in passing. It sounds strange, but I’m actually kind of lonely, even when we’re together…
DR. JAN Have you said anything to your partner about how you’ve been feeling?
CLIENT Well, no. It sounds kind of silly, right? What do I say? Hey, I’m happy, I love you… and I’m lonely.
DR. JAN That’s actually a good start.
CLIENT Really?
DR. JAN Definitely. What do you get from a steady diet of superficial connections? Low-level loneliness. You’re noticing it and sharing it in an attempt to repair the disconnect and feel closer again. Humans are programmed to need to know we belong, especially to our partners. You get that affirmation through a felt sense of connection. When the connection feels weak or missing, it’s not silly to be concerned. It’s being protective of the bond between you and your partner.
CLIENT Let me guess. It’s about the “v” word, right?
DR. JAN (chuckling): Ah yes, vulnerability. Vulnerability comes with being human, but that doesn’t mean you have to like it. Who likes realizing you’re somewhat exposed and at risk of being rejected or hurt? No wonder you play it conservatively. Rather than say something, you don’t. Rather than ask for something, you don’t. There’s just one problem…
CLIENT Conflict avoidance?
DR. JAN Conflict avoidance feels great in the moment. In the long run, it may cost you the connection you crave. The moment you start hiding your feelings is the moment you start losing your connection.
Hide Your Feelings; Lose Your Connection
CLIENT So I’ve got to tell her I’m feeling lonely? Face the fear and do it anyway?
DR. JAN Actually, no. What I have in mind doesn’t involve force, willpower, or mind games to make sharing your feelings with your partner easier. Because those tactics don’t work.
CLIENT So what does work? You just took the only cards I know how to play off the table!
DR. JAN Start by focusing on the hidden obstacle: What may be holding you back is beating yourself up for feeling vulnerable in the first place. The inner critic attack may be more of an obstacle than fear of your partner’s reaction.
CLIENT (pausing): What do you mean?
DR. JAN Right when you’re feeling your most vulnerable — missing the closeness and connection with your partner and worrying
about what to do about it — your inner critic gets in your face and shames you for feeling vulnerable. You’re being silly! What’s wrong with you? No wonder we resist feeling our vulnerability.
An inner critic attack can be debilitating. That shame spiral can completely shut you down or send you spinning out of control. You’ll either say nothing at all or you’ll say the wrong thing.
CLIENT Yeah, I know the feeling.
DR. JAN The problem isn’t feeling vulnerable. The problem is how you react to feeling vulnerable: How do you get your inner critic to let up so you can tell your partner that you miss the closeness you had and work on fixing it?
CLIENT Exactly. So how do you shut it up? Ignore it? Shout it down?
DR. JAN Here’s a little secret about dealing with an inner critic. Underneath all that nastiness and meanness is something you’d never expect: High Anxiety.
An inner critic’s job is to help you avoid rejection, hurt, humiliation, and all the other forms of harm we humans can inflict on each other. In the process of desperately trying to protect you from getting hurt, your inner critic can freak out and become quite abusive.
CLIENT Wait, you’re telling me that in the process of trying to protect me, my inner critic abuses me?
DR. JAN Weird, huh? It’s actually like a protective parent who’s trying to help you but gets anxious, and it comes out sideways as anger. Like a parent who yells at their kid when the kid wanders off in a store: Don’t you ever do that again! What doesn’t get expressed is the vulnerability underneath: When I couldn’t find you, I panicked. Or a parent who tries to scare their kid into social skills: Nobody is going to like you if
ISSUE #150 25
MENtAL WELLNESS
you keep pushing and shoving! Or a parent who tries to scare their kid into motivation: If you don’t keep up, you’re going to get left behind! What doesn’t get expressed is the vulnerability underneath: I’m worried about you fitting in and making it in the world.
CLIENT I can relate to that.
DR. JAN It’s like the inner critic has been handed a set of rules designed to help you survive and thrive in the world. Its job is to beat up on you when you get out of line and break one of these rules. So you don’t screw up your life.
Your Inner Critic Doesn’t Make the Rules.
CLIENT So where did the rules come from?
DR. JAN Great question. As a little kid, you have to figure out how to fit in and make a place for yourself in your family. In other words, you have to figure out the rules, the do’s and don’ts, in your particular family situation. Human beings are very adaptive, so we quickly internalize the rules, and they operate on autopilot. Now you don’t even have to think about it.
This makes you very efficient, but now you don’t know what’s going on in your own mind. At different points in your life, it can be useful to reexamine how your mind works, the internal rules in place, and how well those rules are serving you now. You may want to install some updates so you get better results.
CLIENT My brain could definitely use some rewiring. Can that actually be done? How do you even start?
DR. JAN: You start by looking under the hood to see what’s operating on default. For example, here are some typical internal rules operating in what neuroscientists call your default mode network:
NEVER BE: Weak! Fake! Lazy! Pushy! Selfish! Manipulative!? Needy! Bossy! Entitled! Emotional!
ALWAYS BE: First. Nice. Authentic. Caring. Busy. Transparent. Objective. Responsible. The best.
Do any of these internal rules resonate for you?
CLIENT (laughing): I check all of the above!
DR. JAN Let’s take a closer look and do some prioritizing. I’ve created a tool to make it quick and easy.
Dr. Jan’s Inner Critic Quiz
Directions: Using the examples above and adding your own, answer each of the following three questions. Next, rank your answers in priority order.
1. The three worst possible things someone could say to describe me are:
2. Three things I do to avoid doing or feeling are:
3. Three things I dislike most in other people:
Make the Mental Shift. The Emotional Connection Will Follow.
CLIENT So how does the information from this tool help make it easier to talk to my partner?
DR. JAN Let this tool, and everything else we’ve talked about, help you become more aware of when you’re shutting yourself down. Notice your inner critic’s self-talk and acknowledge how shutting you down is an attempt to help you in the moment. Next, identify what it is your inner critic is most concerned about. What is it trying to protect you from happening in the moment? Acknowledge and appreciate that concern. Finally, acknowledge what it’s costing you in the long run. Going through this process creates a subtle shift from an either/or mindset to a both/ and mindset. Either/or thinking forces you to choose between two simplistic extremes when both feel wrong. Either/or thinking tends to make you overreact or underreact.
CLIENT Like I either lose it and say too much or I zip it and don’t say anything at all?
DR. JAN Right. The beauty of both/and thinking is that it looks for a way to accommodate both options. In the process, you end up with a superior third option, one that’s better suited to complex human interactions.
CLIENT So how would it work in my situation?
DR. JAN Let’s look at a quick example of how a shift in your thinking can make it easier
to connect.
Either/or thinking limits you to two simplistic extremes: EITHER I can express my true feelings OR I can avoid making my partner mad or hurting their feelings.
Both/and thinking looks for a way to accommodate BOTH positions in a win/ win way: How can I be honest and express my true feelings AND reduce the risk of getting hurt or hurting my partner in the process?
CLIENT I see what you mean. You’re right; it‘s a higher level of thinking and it sounds challenging. It also sounds on target.
DR. JAN I’m a big fan of both/and thinking. I’m blown away by how it changes how your mind works and how you relate to the people closest to you. But don’t take my word for it. Try it for yourself.
Both/and thinking is an effective way to express conflicting emotions, resolve interpersonal conflict, and build relationships. If you’re interested in learning more, please get in touch with me for a complimentary consultation.

26 MD-UPDATE
md-update.com YOUR RESOURCE FOR tHE BESt IN KENtUCKY HEALtHCARE MENtAL WELLNESS
Baptist Health Medical Group Welcomes New Doctors
ELIZABETHTOWN K. John Yun, MD, has joined Baptist Health Medical Group Ear, Nose & Throat. Yun specializes in treatment for sinus, thyroid, and parathyroid disorders; ear infections; hearing loss and disorders that affect balance; as well as plastic and reconstructive surgery of the head, face, and neck.
A native of South Korea, Yun moved with his parents to Missouri. He earned his medical degree from the University of Minnesota School of Medicine and completed an otolaryngology – head and neck surgery residency at West Virginia University Medical Center and West Virginia University Hospitals.
Yun has earned national certification for the American Board of Otolaryngology –Head and Neck Surgery. He is a fellow of the
American College of Surgeons, the American Academy of Facial Plastic and Reconstructive Surgery, and the American Academy of Otolaryngology – Head and Neck Surgery.
With more than 30 years of experience, he continuously seeks new and improved procedures and technologies to enhance patient outcomes. He has received the Honor Award from the American Academy of Otolaryngology – Head and Neck Surgery and the Excellence in Teaching award from the Kentucky College of Osteopathic Medicine.
Yun will be practicing at Baptist Health Medical Group Ear, Nose & Throat, located at 2411 Ring Road, Suite 105, in Elizabethtown.
ELIZABETHTOWN Rehan Khan, MD, has joined Baptist Health Medical Group Gastroenterology. Khan diagnoses and treats conditions affecting the esophagus, stomach, intestines, and colon. Some of his special interests include acute and chronic hepatitis, celiac disease, cirrhosis of the liver, colitis, inflammatory bowel disease, irritable bowel syndrome, peptic ulcer disease, gastroesophageal reflex disease (GERD), and dysphagia.
After earning his medical degree from Dow Medical College in his native Karachi, Pakistan, Khan completed an internal med-
icine residency at Lankenau Hospital in Wynnewood, Pennsylvania, followed by a gastroenterology, hepatology, and nutrition fellowship at University of Louisville School of Medicine.
Khan is a diplomate and board certified in gastroenterology and internal medicine by the American Board of Internal Medicine. He is a member of the American College of Gastroenterology, the American Gastroenterological Association, and the American Society of Gastrointestinal Endoscopy.
Khan will be practicing at Baptist Health Medical Group Gastroenterology, located at 2406 Ring Road in Elizabethtown.

27 MD-UPDATE SEND YOUR NEWS ITEMS TO MD-UPDATE > news@md-update.com News News
K. John Yun, MD
Your Source for Graphic Design since 2003 GRAPHIC DESIGN • INTERACTIVE PUBLICATIONS • PROJECT MANAGEMENT and more... www.provationsgroup.com PHOTOs PROVIDeD BY BAPTIsT HeALTH
Rehan Khan, MD
Physicians Join CHI Saint Joseph Medical Group
MOUNT STERLING Experienced provider
Ray Brenton Terrell, MD, has joined CHI Saint Joseph Medical Group – Urology in Mount Sterling. Terrell has 27 years of professional experience serving Mount Sterling, West Liberty, Winchester, Lexington, and Georgetown. He will be devoting all of his time and focus to providing care to patients in Mount Sterling and the region. His new office is at 227 Falcon Drive, Suite G-03.
Terrell chose the field of urology because it offered a unique blend of surgery and primary care. Throughout his years of practice, he has worked to dispel the misconception that urology is a specialty that primarily serves older men. The scope of urologic care is broad and encompasses men and women of all ages and demographics.
After earning his bachelor’s degree from Georgetown College, Terrell received his medical degree from the UK College of Medicine. He did his urologic residency at the University of Iowa Hospitals and Clinics before returning to Mount Sterling to practice. He is board certified by the American Board of Urology. Additionally, he is a member of the American Urologic Association and the Kentucky Urologic Association. Terrell has done research and published studies in the areas of prostate cancer and urothelial cancer. A specific area of interest is advanced diagnostics in the area of prostate cancer screening and detection.
“I could not be more excited and happy to return to my roots in Mount Sterling to continue to serve the wonderful people who have always been there for me,” says Terrell.



BARDSTOWN Sanjiv Mehta, MD, joined CHI Saint Joseph Medical Group – Orthopedic Surgery at Flaget Memorial Hospital. Mehta began his career in Greensburg and says returning to serve Nelson County “feels like a homecoming.”
Mehta has two physician parents who influenced his career path. “I knew in sixth grade I was going to be a doctor,” says Mehta. “I consider myself very blessed for finding my calling early in life.”
During an internship rotation in India, Mehta discovered his passion for the field of orthopedics. “I was seeing a patient who had a femur fracture, who was laying in front of me writhing in pain. I was able to repair his fracture, and the next day, when I saw him, he was eternally grateful, thanking me and telling me I was a blessing. Right then, I found my passion.”
Prior to beginning his professional career in Kentucky, Mehta earned his medical degree from the University of the Punjab in India and served as a visiting lecturer at the Prince of Wales Hospital in Hong Kong. In 1990, Mehta arrived in Louisville, where he accomplished two fellowships and an internship at the University of Louisville. For over two decades, Mehta has seen patients across Kentucky – beginning his career in the Bardstown area and most recently serving patients in Louisville.
“The community of Bardstown is where I started my orthopedic career,” says Mehta. “I’m looking forward to reconnecting with my patients – most of whom have been driving from Bardstown to Louisville to see me. I’m so appreciative of them, and I look forward to returning.”
LEXINGTON Damir Kusmic, MD, has joined CHI Saint Joseph Medical Group Gastroenterology. Kusmic brings a wealth of experience in internal medicine and a goal of providing exceptional care to the patients he serves daily.
Specializing in gastroenterology, a field he describes as “an internal medicine specialty,” Kusmic highlights the procedure-based nature of his work, with a specific interest in the biliary system and the pancreas. His patient care philosophy revolves around kindness, understanding, and diligent work.
Born in Bosnia, Kusmic moved to the US in 1996, growing up in Bowling Green and eventually pursuing medical education, including med school and fellowship. Fluent in Bosnian–Serbo–Croatian, Kusmic brings a multicultural perspective to his practice, enhancing his ability to connect with patients.
Kusmic is a graduate of Western Kentucky University in Bowling Green and received his medical degree from the UK College of Medicine. He completed his residency at Marshall University/Joan C. Edwards School of Medicine in Huntington, West Virginia, and a gastroenterology fellowship at East Tennessee State University Quillen College of Medicine in Johnson City, Tennessee.
Kusmic is particularly interested in endoscopic retrograde cholangiopancreatography (ERCP) because “It’s an intensive procedure, but it’s very satisfying in that it’s also therapeutic. When people have a bile duct obstruction, you can change the clinical picture and improve pain.”
28 MD-UPDATE News PHOTOs PROVIDeD BY CHI sAINT JOsePH HeALTH
Ray Brenton Terrell, MD
Damir Kusmic, MD
sanjiv Mehta, MD



Harrison Memorial Hospital Welcomes New Physicians
Michael Horn, MD, to Head Cancer Care at HMH
CYNTHIANA Harrison Memorial Hospital (HMH) announced the addition of Michael Horn, MD, to the medical staff. Horn brings more than two decades of medical expertise to his new role as the head of Cancer Care at HMH.
Horn earned his BS in biology from UK and his MD from the UK College of Medicine. Horn completed a residency in internal medicine, as well as a fellowship in hematology/ oncology at UK Chandler Medical Center. In 2009, he attained an MS in healthcare man-
agement from Harvard University School of Public Health, Boston.
Horn is board-certified by the American Board of Medical Oncology.
“Our hospital is truly fortunate to welcome Dr. Michael Horn to our team. His exceptional expertise in the fields of hematology and oncology with his genuine commitment to patient care, will undoubtedly enhance our ability to provide top-notch medical services to our community,” said Stephen Toadvine, MD, HMH CEO.
Ashley Blake, DO, Joins HMH Medical Staff
CYNTHIANA Ashley Blake, DO, has joined Derek Clarke, MD, and Jennifer Canan, DO, in providing full-service obstetrical and gynecologic care to female HMH patients. She will specialize in general gynecology care and full-service obstetrical care from pregnancy diagnosis to delivery and follow-up care.
“As a native of Cynthiana, Dr. Blake brings a deep understanding of the community’s needs and a passion for serving its residents,” said Stephen Toadvine, MD, HMH CEO. “Her strong ties to the area and her expertise in women’s health makes her a tremendous asset to the HMH medical team and community.”
Blake graduated from Harrison County High School in 2010. She obtained her BS in biology from Marshall University in Huntington, West Virginia, and her medical degree from the West Virginia School of Osteopathic Medicine in Lewisburg. She did her residency through the University of Kentucky at the Bowling Green, Kentucky, campus. She is member of the American College of Obstetrics & Gynecology.
In addition, Blake is a captain in the West Virginia National Guard. She is married to Matthew Blake, MD, an internal medicine physician.
HMH Awarded Five Stars in CMS Overall Hospital Quality Star Ratings for 2023
CYNTHIANA Harrison Memorial Hospital has been awarded the prestigious five-star rating in the CMS Overall Hospital Quality Star Ratings for 2023. HMH joins a group of only five hospitals in Kentucky to receive this honor.
The CMS assigns star ratings annually to hospitals across the country by selecting 46 of the hospital quality measures CMS publicly reports on Medicare.gov. Then CMS divides them into five measure groups: mortality, readmissions, safety of care, patient experience, and timely and effective care. These ratings serve as a
reflection of the hospital’s commitment to providing high-quality healthcare services and ensuring positive patient outcomes.
Stephen Toadvine, MD, the chief executive officer of HMH, expressed his gratitude and appreciation for the hard work and dedication of the hospital’s staff in achieving this significant milestone. “Receiving a five-star rating from CMS is a testament to our unwavering commitment to patient care and safety. It is an honor to be recognized among the top hospitals in the country. We owe this achievement to the exceptional efforts of our entire HMH team,” he says.
SEND YOUR NEWS ITEMS TO MD-UPDATE > news@md-update.com ISSUE #150 29 PHOTOs PROVIDeD BY HARRIsON MeMORIAL HOsPITAL
Michael Horn, MD
Ashley Blake, DO
Officers Announced for Lexington Clinic’s 2024 Board of Directors



LEXINGTON At Lexington Clinic’s annual Board of Directors meeting, the following officers were elected to serve for the year: president – Michael T. Cecil, MD; vicepresident – Tharun Karthikeyan, MD; secretary – Robby K. Hutchinson, MD; treasurer – An-Yu Chen, MD.
Other members of the board include Brandon Devers, MD, Jamil Farooqui, MD,
Paul Rooke.
“Lexington Clinic is committed to perfecting the patient experience. By using modern data analytics, best practice protocols, experience, and compassion, we aim to provide the highest quality care to the people of Central Kentucky,” said Cecil.
Lexington Clinic was founded in 1920 and is Central Kentucky’s oldest and largest group practice with 350+ providers in more than 30 different specialties, and over 25 locations, serving about 600,000 patients yearly throughout Central Kentucky.

JANUARY 17 | 12:00 -1:00 PM
COMMON & COMPLEX CASES IN INTERVENTIONAL PAIN
FEATURING DR. BRANDON GISH
LEXINGTON CLINIC INTERVENTIONAL PAIN MANAGEMENT
FEBRUARY 21 | 12:00 -1:00 PM
COMMON FOOT & ANKLE CONDITIONS, INITIATING
TREATMENT AND EMERGING TRENDS
FEATURING DR. BENJAMIN “BO” SCHNEIDER
LEXINGTON CLINIC ORTHOPEDICS - SPORTS MEDICINE
MARCH 20 | 12:00 -1:00 PM HYPERTENSION
FEATURING DR. LESLYE JONES

ZOOM LINK IS ONLY ACTIVE ON THE DATE/TIME OF THE CME PRESENTATION.
Use the QR Code at left to log-in to the Zoom sessions or visit https://kyma.org/education-cme/ to access the activities on the scheduled date/time.
This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the Kentucky Medical Association and Lexington Clinic. The Kentucky Medical Association is accredited by the ACCME to provide continuing medical education for physicians.
The Kentucky Medical Association designates this live activity for 1.0 AMA PRA Category 1 Credit.
Physicians should claim only the credit commensurate with the extent of their participation in the activity.
LEXINGTON CLINIC PRIMARY CARE - GEORGETOWN
APRIL 17 | 12:00 -1:00 PM
OBESITY TREATMENT & BEYOND: A REVIEW
OF USING GLP-1 AGONISTS FOR MAINTAINING WEIGHT LOSS
FEATURING DR. MARISA BELCASTRO
LEXINGTON CLINIC FAMILY MEDICINE, VETERANS PARK
MAY 15 | 12:00 -1:00 PM
SURGICAL VS. NONSURGICAL TREATMENT OF DEGENERATIVE ROTATOR CUFF TEARS
FEATURING DR. JAMES GARDINER
LEXINGTON CLINIC ORTHOPEDICS - SPORTS MEDICINE
JUNE 19 | 12:00 -1:00 PM
ULTRASOUND CAN ADVANCE CARE FOR COMMON MUSCULOSKELETAL, RHEUMATOLOGIC & NEUROLOGICAL CONDITIONS
FEATURING DR. THERESA WOLFE
LEXINGTON CLINIC PHYSICAL MEDICINE & REHABILTATON
JULY 17 | 12:00 -1:00 PM
CHOLELITHIASIS
FEATURING DR. M. DANIEL MILLER
LEXINGTON CLINIC GENERAL SURGERY
AUGUST 21 | 12:00 -1:00 PM
CANCER PREVENTION & EARLY DIAGNOSIS FOR KENTUCKY PROVIDERS
FEATURING DR. ROBERT SUMME, RADIATION ONCOLOGY MARKEY CANCER CENTER AT LEXINGTON CLINIC - RICHMOND
SEPTEMBER 18 | 12:00 -1:00 PM
IS SURGERY WORTH IT? THE LANCINATING TRUTH OF TRIGEMINAL NEURALGIA
FEATURING DR. ROBERT CHRISTOPHER SPEARS
LEXINGTON CLINIC NEUROSURGERY
OCTOBER 16 | 12:00 -1:00 PM
ADVANCES IN THE DIAGNOSIS & TREATMENT OF DIFFICULT-TO-TREAT & SEVERE ASTHMA
FEATURING DR. SHUYA WU
LEXINGTON CLINIC ALLERGY, ASTHMA AND IMMUNOLOGY
NOVEMBER 20 | 12:00 -1:00 PM
A FUNCTION BASED APPROACH TO THE EVALUATION OF SHOULDER PAIN - CASES & DEMONSTRATIONS
FEATURING DR. W. BEN KIBLER
LEXINGTON CLINIC ORTHOPEDICS - SPORTS MEDICINE

30 MD-UPDATE News
Kimberly Hudson, MD, Jordan Prendergast, MD, David Keilar, MD, Mr. Nick Rowe, and Mr.
PHOTOs PROVIDeD BY LeXINGTON CLINIC
Michael T. Cecil, MD
Tharun Karthikeyan, MD
Robby K. Hutchison, MD
An-Yu Chen, MD
Lexington Clinic and the Kentucky Medical Association have partnered up to o er online CME! NEW CME OFFERING FOR 2024
Kentucky’s leader in heart care

Easy access to exceptional heart care is more than just a matter of convenience. For those who need it most, it can be life-changing and lifesaving. At Norton Heart & Vascular Institute, thanks to our 100 specialty trained physicians and advanced practice providers, we offer 28 locations across Kentucky and Southern Indiana. And our subspecialty multidisciplinary programs — such as A-fib, Structural Heart, Advanced Heart Failure and Recovery, Cardio-obstetrics — enhance provider collaboration and patient satisfaction.
Because when it comes to heart and vascular care, we stop at nothing to get your patients the care they need.
To make an appointment or refer a patient, call (502) 446-6484 (NHVI) or visit NortonEpicLink.com.
Lexington Medical Society Installs New Officers
The meeting included the KMA General Assembly legislative update and preview









LEXINGTON The 2024 officers of the Lexington Medical Society (LMS) assumed their duties on January 30, 2024, at the annual Presidential Transition and KMA Update meeting at the Signature Club in Lexington.
Angela Dearinger, MD, MPH, FACP, FAAP, is the new LMS president. Hope Cottrill, MD, is president-elect, Tina Fawns, MD, is secretary/treasurer and Christine Ko, MD, is vice-president-elect. It is the first time that all of the LMS officers are females.
Dearinger is board-certified in internal medicine and pediatrics with a master’s degree in public health. She has been a faculty member at the UK College of Medicine since
2005. In her acceptance speech, she recalled that she was from Paintsville, Kentucky, a graduate of Transylvania University in Lexington, and received her medical degree from the UK College of Medicine.
It was during her residency that Dearinger says she realized that “academic medicine was the career path for me,” so she returned to Kentucky and the UK College of Medicine to teach medical students and residents.
She noted several influential mentors, Dr. Chipper Griffin, dean of the UK College of Medicine, Dr. F. Doughlas Scutchfield, who “taught public health before it was in the UK curriculum,” and Dr. Tuyen Tran, who
encouraged her to get involved in the LMS to “be part of the broader physician community.”
Cody Hunt, KMA health policy manager, gave an overview of the KY 2024 long session and noted healthcare bills such as the Omnibus Maternal Health Bill (HB10); AED & Sports Medicine (HB169); Criminal Liability for Health Care Providers (HB159); and Workplace Violence Against Healthcare Workers (HB194).
The next LMS dinner social meeting is scheduled for Thursday, March 21. The topic is “The White Coat Investor” and features speaker James Dahle, MD, a noted financial expert.
32 MD-UPDATE PHOTOS BY JOE OMIELAN
New LMS officers, Christine Ko, MD, vice-president elect, Angela Dearinger, MD, president, Hope Cottrill, MD, president-elect
Outgoing LMS President Lee Dossett, MD, presents the speaker’s gavel to President Dearinger
KMA President Patrick Padgett and Cody Hunt, KMA Health Policy Manager
James Borders, MD, director, PACE at Bluegrass Navigators, and Michael Lally, MD
Stephen Mooney, MD, Baptist Medical Group, and James Francis, MD, Nephrology Associates
Khalil Rahman, president, Nephrology Associates, past-president, Lexington Medical Society
Jesi Hale and David Dornbos, III, MD, UK neurosurgeon and new member of the Lexington Medical Society
Jacob Mitcham, Maddie Mitcham, UK 3Y medical student, and Marian Bensema, MD (ret)
Christine Ko, MD, David Bensema, MD, past-president LMS, and Hope Cottrill, MD, LMS president-elect
EvENTS

 MARK
MD Cardiothoracic Transplant Surgeon
MARK
MD Cardiothoracic Transplant Surgeon


Here, your heart is in the right place. Better patient outcomes start here, where hearts are in the right place. Welcome to UofL Health – Heart Hospital, an exciting chapter in the epic Jewish Hospital story. When you are searching for specialists to care for your patients, experience is key. With a history as one of the nation’s best hospitals for cardiology and heart surgery, this is home to over 40 medical heart firsts and is the area’s only Heart Hospital dedicated to comprehensive cardiovascular care. Our world-class network offers you a true partnership in the care of your patients. Here, patients with a wide spectrum of heart issues have exclusive access to a network of specialists that can heal, protect, revive, and even replace hearts. With every referral, we work hand in hand with our referring physicians to provide heart care that is truly life-changing for patients, and their families. Visit UofLHealth.org or call 502-587-4000.
SLAUGHTER,
Lung Cancer Screening is easy
Covered by most insurance (Medicare 50 - 77)
Quick and painless
No needles, IVs or dyes
Get screened every year to catch cancer early


Lung cancer can be treated if caught early!
“Kentucky has achieved notable success in a state with dismal lung cancer incidence, mortality, smoking rates and 5-year survival
We are now #2 in the country for lung cancer screening.”
Michael R. Gieske, MD Director of Lung Cancer Screening St Elizabeth Virtual Health Center
You are eligible for screening if:
50 You are 50 to 80 years old
20
15
You smoked a pack of cigarettes a day for 20 years
You currently smoke or quit within the past 15 years






 Steve Lin, MD
Medical Director
Nezar Falluji, MD
Hussam Hamdalla, MD
Sharat Koul, DO
Steve Lin, MD
Medical Director
Nezar Falluji, MD
Hussam Hamdalla, MD
Sharat Koul, DO








































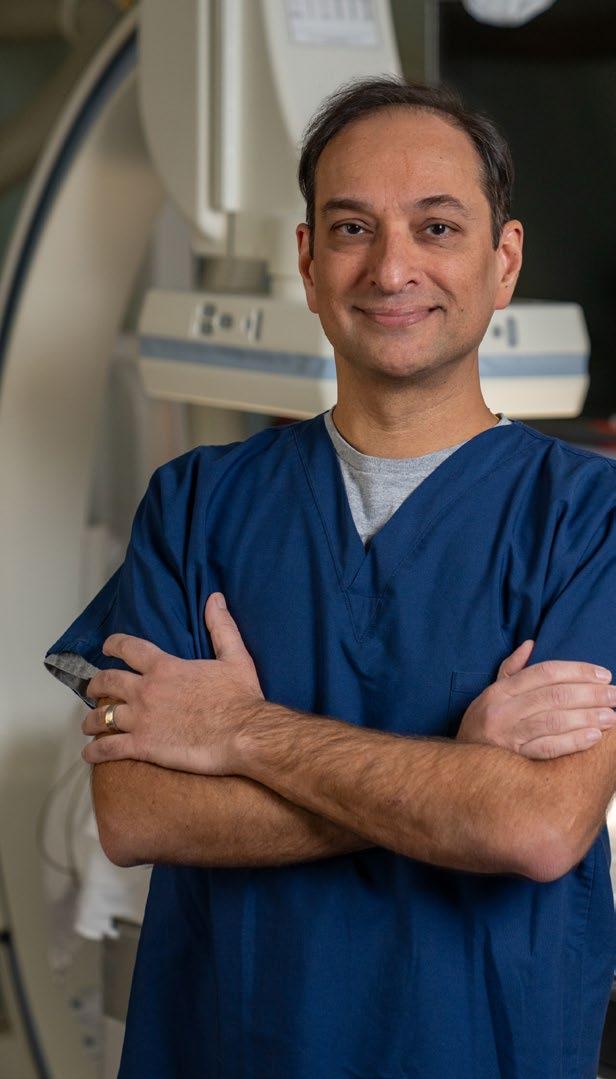














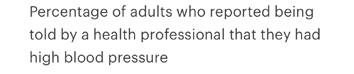



























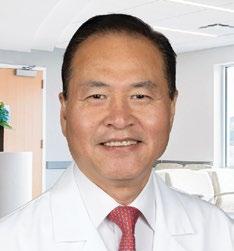























 MARK
MD Cardiothoracic Transplant Surgeon
MARK
MD Cardiothoracic Transplant Surgeon



