A Cut Above
Lexington Clinic Orthopedic Surgeon Tharun Karthikeyan, MD, Embraces the Advantages of the ROSA Robot
ALSO IN THIS ISSUE

UofL HEALTH - CENTER FOR FOOT AND ANKLE EXCELLENCE
UK HEALTHCARE PHYSICAL MEDICINE & REHABILITATION HAS A NEW HOME
CHI SAINT JOSEPH HEALTH ORTHOPEDIST IN SMALL COMMUNITY SEES GENERATIONS OF PATIENTS
SPORTS HEALTH AND SHOULDER RECONSTRUCTIOIN PROGRAM AT NORTON HEALTHCARE
THE FUTURE FUND, SAVING FLOYDS FORK
ISSUE #147 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS VOLUME 13 • #4 • S EPTEM b E r 2023
Experience Matters.

When your quality of life has been affected by a bone or joint disorder, the orthopedic team at CHI Saint Joseph Medical Group is ready to get you back on your feet. With over 50 years of combined experience, our board-certified and fellowship-trained surgeons are passionate about their high standards of care.





Berea
305 Estill Street
Berea, KY 40403
P 606.864.0770
Bardstown
875 Pennsylvania Avenue
Bardstown, KY 40004

P 502.348.5685
Corbin
1 Trillium Way, Suite 306 Corbin, KY 40701
P 606.864.0770
Flemingsburg
101 JB Shannon Drive, Suites A & B Flemingsburg, KY 41041
P 606.209.0010
Lebanon
325 W. Walnut Street, Suite 300


Lebanon, KY 40033
P 502.348.5685
Lexington
211 Fountain Court, Suite 320
Lexington, KY 40509
P 859.264.9820
Orthopedics Team
London
148 London Mountain View Drive, Suite 4 London, KY 40741
P 606.864.0770
160 London Mountain View Drive London, KY 40741
P 606.864.0770
Mount Sterling
624 N. Maysville Road, Suite A Mount Sterling, KY 40353

P 859.497.4144
Somerset
118 Tradepark Drive, Suite B Somerset, KY 42503
P 606.416.5225
Winchester
1850 Bypass Road Winchester, KY 40391
P 859.737.5188
Collin Ball, DPM Patrice Beliveau, MD
Anup Chattha, MD
Vincent DePalma, DO
Adam Franson, DO Kevin Magone, MD
Jean-Maurice Page, MD James Rollins Jr., MD
Frank Taddeo, MD Jan Veloso, DPM
The board-certified physicians at CHI Saint Joseph Medical Group — Orthopedics are proud to offer comprehensive orthopedic care.
CHISaintJosephHealth.org
ISSUE #148 (October) – CANCER CARE





Hematology, Oncology, Plastic Surgery, Radiology, Radiation
ISSUE #149 (December) – IT’S ALL IN YOUR HEAD
ENT, Mental Health, Neurology, Neuroscience, Ophthalmology, Pain Medicine, Psychiatry 2024















ISSUE #150 (February) – HEART & LUNG HEALTH
Cardiology, Cardiothoracic Medicine, Cardiovascular Medicine, Pulmonology, Sleep Medicine, Vascular Medicine, Bariatric Surgery
ISSUE #151 (April) – INTERNAL SYSTEMS
Endocrinology, Gastroenterology, Geriatric Medicine, Internal Medicine, Integrative Medicine, Infectious Disease Medicine, Lifestyle Medicine, Nephrology, Urology
ISSUE #152 (June) – WOMEN & CHILDREN’S HEALTH
OB/GYN, Women’s Cardiology, Oncology, Urology, Pediatrics, Radiology





ISSUE #153 (September) – MUSCULOSKELETAL HEALTH















Orthopedics, Physical Medicine & Rehabilitation, Sports Medicine, PT/OT










ISSUE #154 (October) – CANCER CARE
Hematology, Oncology, Plastic Surgery, Radiology, Radiation










ISSUE #155 (December) – IT’S ALL IN YOUR HEAD
ENT, Mental Health, Neurology, Neuroscience, Ophthalmology, Pain Medicine, Psychiatry




Editorial topics and dates are subject to change

VOLUME 12 #4 EPTEM E 2022 World Class Hand Care Legendary practice Kleinert Kutz continues the training and legacy of its founders ALSO IN THIS ISSUE SPORTS MEDICINE AT UofL HEALTH & ATHLETICS TAKING THE PAIN OUT OF JOINT PAIN AT WELLWARD REGENERATIVE SPORTS MEDICINE AT CHI SAINT JOSEPH HEALTH NEW ORTHOPEDIC CENTER AT BAPTIST HEALTH LOUISVILLE VOLUME 12 #4 EPTEM E 2022 World Class Hand Care Legendary practice Kleinert Kutz continues the training and legacy of its founders ALSO IN THIS ISSUE SPORTS MEDICINE AT Uof HEALTH & ATHLETICS TAKING THE PAIN OUT OF JOINT PAIN AT WELLWARD REGENERATIVE SPORTS MEDICINE AT CHI SAINT JOSEPH HEALTH NEW ORTHOPEDIC CENTER AT BAPTIST HEALTH LOUISVILLE World Class Hand Care Legendary practice Kleinert Kutz continues the training and legacy of its founders ALSO IN THIS ISSUE SPORTS MEDICINE AT ofL HEALTH & ATHLETICS TAKING THE PAIN OUT OF JOINT PAIN AT WELLWARD REGENERATIVE SPORTS MEDICINE AT CHI SAINT JOSEPH HEALTH NEW ORTHOPEDIC CENTER AT BAPTIST HEALTH LOUISVILLE VOLUME 12 #4 EPTEM E 2022 World Class Hand Care Legendary practice Kleinert Kutz continues the training and legacy of its founders ALSO IN THIS ISSUE SPORTS MEDICINE AT UofL HEALTH & ATHLETICS TAKING THE PAIN OUT OF JOINT PAIN AT WELLWARD REGENERATIVE SPORTS MEDICINE AT CHI SAINT JOSEPH HEALTH NEW ORTHOPEDIC CENTER AT BAPTIST HEALTH LOUISVILLE VOLUME 12 #4 EPTEM E 2022 World Class Hand Care Legendary practice Kleinert Kutz continues the training and legacy of its founders ALSO IN THIS ISSUE SPORTS MEDICINE AT Uof HEALTH & ATHLETICS TAKING THE PAIN OUT OF JOINT PAIN AT WELLWARD REGENERATIVE SPORTS MEDICINE AT CHI SAINT JOSEPH HEALTH NEW ORTHOPEDIC CENTER AT BAPTIST HEALTH LOUISVILLE THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS 2023-24 Editorial Calendar Gil Dunn, Publisher • GDUNN@MD-UPDATE.COM • 859.309.0720 (direct) • 859.608.8454 (cell) Send press releases to gdunn@md-update.com To participate, please contact
2023
Welcome to the Orthopedics, PM&R and Sports Medicine Issue of MD-Update
LEXINGTON If you procrastinate, as I do frequently, I have good news for us. In this issue, beginning on page 29, our Mental Wellness expert, Dr. Jan Anderson, explains how and why we do it. Better yet, she has some great insights into how to “kick the procrastination habit.” Dr. Jan explains how we prefer the good feeling of the “escape” emotion of procrastination over the “dread” emotion of doing the task at hand.
Dr. Jan’s column echoed something Dr. Jim Rollins, orthopedic surgeon with CHI Saint Joseph Health in Mt. Sterling, told me. Many of his older patients have put off seeing him about a joint problem until surgery is needed. Most of our brains are wired, says Dr. Jan’s research, to choose the short-term pleasure over future pain.
It was founding father Ben Franklin who is quoted as saying, “Don’t put off until tomorrow what you can do today.” Mark Twain had his own version, “Never put off till tomorrow what you can do the day after tomorrow.”
A New Voice. A Familiar Name.
I am very pleased to welcome Stephen Henry, MD, former KY Lt. Governor, to MD-Update. Dr. Henry has been a community leader and advocate for sustainability and a healthy environment for years. In this issue, he puts forth a call to Kentucky physicians and all MD-Update readers to take up the challenge, responding to the AMA’s “new policy declaring climate change a public health crisis.”
Dr. Henry was a founding member of Future Fund, whose mission is to preserve riparian zones along Floyd’s Fork Creek in eastern Jefferson County. I invite you to read his Op-Ed column on page 10 and to answer his call. All movements start with one step.
Financial Déjá Vu and Medical Marijuana
I am always amazed by the wisdom and prescience of MD-Update Financial columnist Scott Neal. In this issue he discusses Saeculum, the Latin term for a long-lived life, and the four periods of that life as a metaphor for understanding history and our current economic situation. Our Legal columnist Sarah Charles Wright has written a detailed explanation of the new Kentucky laws regulating medicinal cannabis, aka medical marijuana.
Fall Sports
The end of baseball season and the beginning of football is the perfect time to meet some of Kentuckiana’s orthopedics, sports medicine, and PM&R doctors. That’s who we have for you in this issue. In mid-September, I’ll be traveling to Detroit to catch the playoff series of the USPBL with the Eastside Diamond Hoppers. Whatever team you’re cheering for, I hope you enjoy the experience.
Please look at the fall and 2024 lineup of MD-Update editorial topics on the preceding page. If you see your specialty, give me a call. I’m sure you have an interesting story to tell or an update on your medical practice to share. My door is open for your view on any topic that concerns healthcare in Kentucky.
Until next time, all the best, Gil Dunn Editor/Publisher MD-Update
MD-UPDATE MD-Update.com
Volume 13, Number 4
ISSUE #147
EDITOR/PUBLISHER
Gil Dunn
gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda Debord
CONTRIBUTORS:
Jan Anderson, PSYD, LPCC
Stephen Henry, MD, (ret) Fmr Lt. Gov.
Scott Neal, CPA, CFP
Adam Shewmaker, CPA, FHFMA

Sarah Charles Wright, Esq
CONTACT US:
ADVERTISING AND INTEGRATED
PHYSICIAN MARKETING: Gil Dunn gdunn@md-update.com

Mentelle Media, LLC

38 Mentelle Park Lexington KY 40502 (859) 309-0720 phone and fax
Standard class mail paid in Lebanon Junction, Ky. Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington KY 40502
MD-Update is peer reviewed for accuracy. However, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
Copyright 2023 Mentelle Media, LLC. All rights reserved. No part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Please contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter.
Thank you.
Individual copies of MD-Update are available for $9.95.
SEND
2 MD-UPDATE
YOUR LETTERS TO THE EDITOR TO: Gil Dunn, Publisher
gdunn@md-update.com, or 859.309.0720 phone and fax
LETTEr FrOM THE EDITOr/PUbLISHEr






ISSUE #147 3 ISSUE #147 10 OP/ED 18 PHYSICAL MEDICINE & REHABILITATION 20 ORTHOPEDICS/ SPORTS MEDICINE 24 ORTHOPEDICS 26 ORTHOPEDICS CONTENTS COVEr PHOTOGrAPHY bY PAUL MArTIN 12 A Cut Above Lexington Clinic Orthopedic Surgeon Tharun Karthikeyan, MD, Embraces the Advantages of the ROSA Robot 4 HEADLINES 5 ACCOUNTING 6 FINANCE 8 LEGAL 10 OP/ED SPECIAL SECTIONS: 18 PHYSICAL MEDICINE & REHABILITATION 20 ORTHOPEDICS/ SPORTS MEDICINE 24 ORTHOPEDICS 26 ORTHOPEDICS 28 MENTAL WELLNESS 30 NEWS FEATURED
UofL Health – Heart Hospital Recognized as “Great Heart Program”
 BY BECKER’S HOSPITAL REVIEW
BY BECKER’S HOSPITAL REVIEW
LOUISVILLE Becker’s Hospital Review has named UofL Health – Heart Hospital to its 2023 list of “Hospitals and health systems with great heart programs.”
The hospitals and health systems featured on the list are widely recognized for their outstanding heart care. The list commemorates programs that deliver quality outcomes, employ highly skilled team members and lead research in the heart care field.
“When it comes to everything heart, the Heart Hospital is a unique resource in the region,” says John Walsh, UofL Health – Heart Hospital CEO. “We are the area’s only academic hospital exclusively dedicated to comprehensive and innovative heart care. Recognition by Becker’s is another validation of our world-class team, their expertise, and our commitment to invest in your heart.”
UofL Health – Heart Hospital was opened

in 2022. Built on the world-renowned legacy of 40 medical heart firsts at Jewish Hospital, the Heart Hospital pulled together all heart services into one main location to heal, revive, protect, and even replace hearts. From the initial onset of cardiovascular symptoms to an emergent care and heart transplants, all occur at the Heart Hospital.
UofL Health – Heart Hospital has over 100 beds dedicated for heart patients. Rising 15 stories above downtown Louisville, with nearly 280,000 square feet, it provides leading-edge heart care on UofL Health’s academic medical campus. It includes six dedicated cardiac cath labs, two hybrid operating rooms, three electrophysiology labs, and three cardiac operating rooms collectively equipped for TAVR, Watchmen Flex and heart transplant procedures. More than 300 heart care professionals make up the Heart Hospital team, with preventative and follow up care extended to more than 30 locations across Kentucky and Indiana.
The Becker’s Hospital Review editorial team assessed rankings and awards from reputable organizations such as U.S. News & World Report, Healthgrades, Centers for Medicare and Medicaid Services (CMS), The Leapfrog Group and more.
4 MD-UPDATE
John Walsh, UofL Health –Heart Hospital CEO
PHOTOS PROVIDED BY UOFL HEALTH HEADLInES
UofL Health – Heart Hospital rises 15 stories above downtown Louisville
Five Keys to Effective Credentialing
BY ADAM SHEWMAKER, FHFMA, HEALTHCARE CONSULTING DIRECTOR

Credentialing can be burdensome, time-consuming and tedious. Details matter. Expertise and follow-up are critical to proper enrollment and protecting cash flow. In this article we provide five keys to effective credentialing.
1. Begin the Process Early
Some commercial insurance credentialing processes can take up to 120 days to complete. Start compiling all the necessary information as soon as you can to protect against potential delays and unpaid claims.
2. Attention to Details Matters
Because credentialing is intimately connected to cash flow, make sure all necessary information is complete and accurate. Missing or incomplete information will delay the process. Some of the most common errors or omissions may include:
Incomplete Provider Work History –Include current and all prior professional work history since graduating medical school. Work history must include MM/YYYY format on all start/end dates.
Malpractice Insurance – Include the current policy and up to 10 years policy history.


It’s also recommended to include the past 10 years malpractice claim history.
Hospital Privileges – Providers must have admitting privileges to an in-network hospital to participate with a health plan. If that doesn’t exist, then another in-network physician will need to supply in writing an admitting arrangement attesting that he/she will agree to admit any patients on the provider’s behalf. Also, a list where the covering physician has privileges will be needed.
Covering Colleagues – Providers are responsible for providing coverage for patients 24/7 and will need to disclose which colleagues may provide coverage during times of absence. This is particularly important for solo practitioners. Attestations – Fully answer all yes/no questions on each application and provide complete details for response when necessary.
3. Stay Current With CAQH
A current CAQH profile is an important part of some state Medicaid plans. Make certain that a provider’s CAQH profile is current with all personal details, attestations, and signed attestation page. An incomplete profile will cause delays in the process. CAQH must
be attested for insurance plans to be able to view it.
4. Include the Provider during the Process
Providers are responsible for completing the credentialing process for all the payers with which your organization participates. Although burdensome, it is critical that the provider assist throughout the process and provide all necessary credentialing data points.
5. Know Your Key Payers
Know which payers represent key revenue sources to your business so that you can prioritize credentialing processes accordingly. You can selectively schedule patients for your new provider based on which plans have been completed until the new provider is fully credentialed with all networks and plans.
Credentialing doesn’t have to be a burden. Contact us today to explore how Dean Dorton Healthcare Solutions can help simplify your credentialing.
Contact the author at 502.566.1054 or ashewmaker@ddafhealthcare.com
ISSUE #147 5
deandorton.com/healthcare Health system solutions and advisory services Medical billing and credentialing Finance and revenue cycle management Outsourced accounting, audit, and tax Risk management and compliance Technology and data analytics
ACCOUNTING
Empowering physicians to focus solely on the demands of their clinical practice
An Important Book Recommendation
BY SCOTT NEAL,
In the aftermath of the Great Recession of 2008, I recommended to our readers the bestselling book, The Fourth Turning: An American Prophecy by historians Neil Howe and William Strauss. In that book, the authors looked back over 500 years of history to explain a cycle theory that history moves in Saecula, Latin for a long-lived life of 80-100 years. According to this theory, within each Saeculum there are four periods, each lasting 20-25 years: a High (a period of confident expansion), an Awakening (a time of spiritual exploration and rebellion), an Unraveling (a period marked by individualism triumphing over crumbling institutions), and The Crisis (when society passes through a great and perilous gate in history). I liked the book because I could easily connect their theory with empirical evidence documented in history classes or that I could easily remember.
They opened the 1997 book with “America feels as though it is unraveling.” They marked the beginning of the Unraveling as 1984. It’s easy to criticize their theory as being overburdened with hindsight bias. But, as events unfolded between the book’s publication in 1997 and my reading in 2008, history revealed their predictions offered up in 1997 were eerily prescient.
I also connected with the book by the authors’ use of Jungian archetypes to describe the generations that are born during each turning. The baby boom generation, of which I am a part, is labeled Prophet; Gen X-ers, Nomads; Millennials, Heros; and those most recently born, Gen Z-ers, are labeled Artists. It is important to note that it is the much-maligned Millennials who will be the heroes on par with the Greatest Generation, the G.I.s who were in control at the culmination of the last crisis and got us through WWII. It is the change of control from one generation to the next that marks the turnings.
Mr. Howe has been quite busy (Mr. Strauss
died in 2021) and just this summer, published the follow-on book, The Fourth Turning Is Here: What the Seasons of History Tell Us about How and When This Crisis Will End. If I have piqued your interest, don’t worry. You don’t need to read both books to understand it. Just cut to the chase and read this one.
So why am I, a financial planner, telling you all this? It’s not because I think it to be the end-all, be-all statement on the state of the economy, financial markets, and political climate of today. Nor is it because the book has a clear prescription for how to deal with our current state. It’s because there is some risk that they are right. If so, it calls for us to be alert to the possibilities that confront us as the crisis reaches its climax that Howe calls Ekpyrosis, (nature’s fiery moment of death and discontinuity). “The Ekpyrosis refers specifically to the culminating years of the Crisis era, when public events move at maximum speed—completing the combustion of the old saeculum and making room for the birth of a new.” It’s important to remember that while the Fourth Turning is about crisis and calamity, I draw hope in the idea that it is then followed by a High and an Awakening.
So, how does Mr. Howe believe that this American Crisis will reach its climax? He gives himself plenty of wiggle room in citing how there could be anomalies this time around, but he asserts that it is likely to be resolved in the late 2020s or early 2030s in one of three ways: 1) a financial crash that is likely to be worldwide since we are now so interconnected; 2) Word War III among the superpowers, or 3) civil war in the U.S., as unthinkable as that is. Does the prospect of either of the last two make a financial crash more palatable? I

doubt it, but since this is a financial column, let’s stick with it.
If the current crisis period began in 2008, as Howe claims it did, we have witnessed three financial crashes since then: The Global Financial Crisis (fall of 2007 to 2009); the Pandemic Crash (late winter 2020); and a post-pandemic crash (winter of 2022). A follow-on recession was triggered by the first two. As you may recall, the U.S. led the world in an aggressive campaign of both fiscal and monetary stimulus, leading to easy money (i.e., primarily low or no interest loans). The stimulus worked and reduced the severity of the recessions and market crashes. However, it remains to be seen if we are going to dodge a recession this time around.
Since 2007, publicly held U.S. Government debt has tripled and, at this writing, stands at over 100% of GDP. The money supply grew by 300%. The Fed’s balance sheet grew by 1,000%. Additionally, credit card debt has now reached $1 Trillion dollars as of this month. All this is fueling inflation. According to Howe, “Chronic stimulus led to lowered savings, fed zombie firms, and suppressed business dynamism. Worse, it raised the risk of yet another crash by glutting Wall Street in order to feed Main Street. Worst of all, it ensured that the next crash — when it came — would be one that stimulus could no longer remedy.” So, what to do?
Last year in this space, I advised three steps that are, in light of the Fourth Turning, even more appropriate today: 1) De-risk as much as possible. 2) Set SMARTER goals. 3) Focus on cash flow (now and the future). I went into depth on each of these in 2022. If you need a copy of that article, let us know.
6 MD-UPDATE
Scott Neal is president of D. Scott Neal, Inc., a fee-only financial planning and investment advisory firm with offices in Lexington and Louisville. Correspond with him at scott@dsneal.com or by calling 1-800-344-9098.
CPA, CFP®
FiNANCE
“It feels like déjà vu all over again.” — Yogi Berra


ISSUE #147 7 Lace up your shoes for a good cause. October 14, 2023 rain or shine Race Start: 9 a.m. Registration Begins: 7:30 a.m. Location R.J. Corman Railroad Group Headquarters 101 R.J. Corman Drive • Nicholasville, KY 40356 Online Registration Presented by All proceeds will benefit the Yes, Mamm! Yes, Cerv! programs, providing free mammography and cervical cancer screenings, diagnostic testing, and program support to underinsured and uninsured patients across Kentucky. Register to run or walk by scanning this QR code or by finding the registration page at this link: RunSignUp.com/Race/Info/KY/Nicholasville/YesMamm5KatRJCorman Republic Bank & Trust Company Loan Originator ID #402606 Here are just a few of the medical banking solutions we offer: • Special Home Loan Programs Reduced closing costs* and exclusive financing options for medical residents and physicians. • Business Banking for Private Practices This includes lines of credit and equipment financing. • Treasury Management Business on-site deposit and remote deposit capture, as well as lockboxes. • Online Banking & Mobile Deposit** Because your time is too important to spend on a trip to the bank. * You must have opened or open your primary checking account to receive promotional closing costs. Your primary checking account must be maintained and in active status for the term of the Loan or a $500 fee may be assessed. Please ask us about the Promotional Closing Cost Program Participation Agreement for more details.**Message and data rates may apply from your carrier. Usage and qualification restrictions apply. Republic Bank specializes in personal and private practice banking solutions for physicians. CALL US TODAY Lexington Emily Miller (859) 266-3724 NMLS ID # 419242 Gary Spence (502) 588-1595 NMLS ID # 1087080 Louisville When it comes to banking for physicians, we’re just what the doctor ordered.
Medical Marijuana in Kentucky
What do healthcare providers need to know?
 BY SARAH CHARLES WRIGHT
BY SARAH CHARLES WRIGHT
Possessing marijuana in Kentucky is a Class B misdemeanor punishable by up to 45 days in jail. Two significant events in the last ten months, however, have minimized the likelihood of prosecution for individuals possessing marijuana for medicinal use. On November 15, 2022, following the Kentucky Legislature’s failure in 2020 and again in 2022 to pass a medical marijuana bill, Governor Beshear signed Executive Order 2022-798 granting a full and complete pardon to anyone who after that date is accused of possessing “medicinal cannabis” under certain conditions.1
This past spring, the Legislature enacted medicinal cannabis legislation, which has been codified in KRS Chapter 218B. However, only eleven of the twenty-nine separate sections of Chapter 218B are currently in effect. The other eighteen sections don’t become effective until January 2025. Importantly, they include the sections that will statutorily shield patients from criminal prosecution and administrative action for possession and use of “medicinal cannabis,” and afford them civil rights and other protections related to employment and parental custody. They also include the sections that establish the registration process for patients to obtain a medicinal cannabis “registry ID card,” which patients must have to legally buy and use medicinal cannabis. The procedures for doctors and advanced practice registered nurses (APRNs) to be deemed “medicinal cannabis practitioners” by their licensure boards are not due to be issued until next July.
In the meantime, Executive Order 2022798 remains in effect. This article discusses what practitioners can do now to help patients with specific medical conditions obtain medicinal cannabis, and what they will be able and required to do starting January 2025.
1 The terms “medical marijuana” and “medicinal cannabis” are interchangeable, and simply refer to marijuana used for medicinal purposes. See KRS §§ 218A.010(28) and KRS 218B.010(15).
Practitioners should refer to Chapter 218B for the requirements for establishing a medicinal cannabis business in Kentucky.
Executive Order 2022-798
To be clear, the Governor’s Executive Order does not “legalize” the prescribing of medicinal cannabis in Kentucky, nor does Chapter 218B. Marijuana is not approved by the FDA for medical use and remains an illegal drug under federal law. The Executive Order does, however, allow doctors to recommend its use to patients with certain medical conditions and eliminates the fear of criminal prosecution for possessing medicinal cannabis in Kentucky through the end of 2024 provided the following requirements are met:
• The individual must have legally purchased the medicinal cannabis in another state and have written proof of the location and date of purchase to show the cannabis was lawfully obtained.
• The individual cannot possess more cannabis than legally allowed by the jurisdiction where they bought it, and in any case, not more than eight ounces.
• The individual or their caregiver has a written certification from a Kentucky licensed physician or osteopath in good standing with the Kentucky Board of Medical Licensure (KBML) or the licensure board in the patient’s state of residence showing they have one of the qualifying medical conditions – cancer, ALS, epilepsy, intractable seizures, Parkinson’s disease, multiple sclerosis, sickle cell anemia, PTSD, cachexia or wasting syndrome, neuropathies, severe arthritis, hepatitis C, fibromyalgia, intractable pain, muscular dystrophy, HIV, AIDS, glaucoma, or a terminal illness.
• The certification includes: (i) the person’s name, date of birth, address, and telephone number; (ii) the certifying provider’s name, license number, address, and telephone
number; (iii) the provider’s statement that he/she has a bona fide provider-patient relationship with the individual and in his/ her professional opinion, the patient has one of the listed conditions; and (iv) the provider’s dated signature.2
In short, through December 2024, Kentucky physicians and osteopaths (but not APRNs) may only issue written certifications to patients to obtain medicinal cannabis in a jurisdiction outside Kentucky where it is currently legal.
KRS Chapter 218B Registry ID Card
Beginning in 2025, patients must have a CHFS issued medicinal cannabis registry ID card to legally obtain and use medicinal cannabis in Kentucky.3 Patients must submit an approved application to CHFS together with a written certification issued in the last ninety days from a “medicinal cannabis practitioner” that the patient has a qualifying medical condition and may benefit from using medicinal cannabis.4 Patients with a criminal record of a disqualifying offense cannot be registered cardholders.5 The patient must pledge in the application not to “divert” medicinal cannabis to anyone not allowed to possess it under Chapter 218B. Once issued, a registry card is good for one year. The CHFS registry of cardholders will be confidential and exempt from the Kentucky Open Records Act.
2 Per the Executive Order, the written certification does not constitute a prescription for medical cannabis as it is still illegal in Kentucky to prescribe it.
3 This includes patients with a valid out-of-state registry ID card and supporting documentation, and designated caregivers of qualified patients, and parents/legal guardians of qualified patients under 18.
4 KRS § 218B.050(6)(c) states that to apply for registry ID card, a certification is only valid for sixty days but can be renewed up to three times. However, KRS § 218B.055(6)(b) states that to apply for or renew registration, the certification must have been issued within the last ninety days. Hopefully, CHFS will issue regulations clarifying when a certification is stale and won’t be accepted.
5 Disqualifying offenses include conviction of a felony that classifies them as a violent offender, or of a felony violation of state or federal controlled substance law.
8 MD-UPDATE
LEGAL
YOU CARE FOR EVERYONE
WE TAKE CARE OF YOU
Qualifying Medical Conditions
The list of qualifying medical conditions in Chapter 218B is shorter than the list in Executive Order 2022-798 but allows for the Kentucky Center for Cannabis at the University of Kentucky to add to the list as research on the use of medicinal cannabis to treat various conditions develops. For now, the list includes any type of cancer; chronic, severe, intractable or debilitating pain; epilepsy or other intractable seizure disorder; multiple sclerosis, muscle spasms/spasticity; chronic nausea/cyclical vomiting syndrome resistant to conventional medical treatment, and PTSD.
Becoming a Medicinal Cannabis Practitioner
Beginning January 1, 2025, only “medicinal cannabis practitioners” can lawfully issue the written certification qualified patients in Kentucky must have to apply for a registry ID card. Kentucky physicians, osteopaths, and APRNs authorized to prescribe controlled substances under KRS 314.042, may apply to their licensure board for authorization to be medicinal cannabis practitioner. The KBML and Kentucky Board of Nursing (KBN) are
to issue regulations outlining the authorization process by July 2024. Authorizations will not be given to practitioners with an ownership or investment interest in or compensation agreement with a cannabis business licensed under Chapter 218B. Once authorized, medicinal cannabis practitioners must register as such with the Kentucky All Schedule Prescription Electronic Reporting (KASPER) system before issuing medicinal cannabis certifications.6
Written Certification Requirements
Medicinal cannabis practitioners will be required to have an established bona fide practitioner-patient relationship with the patient in order to issue a medicinal cannabis certification. The practitioner must physically examine the patient, diagnose or confirm the patient has been diagnosed with a qualifying medical condition, and consult with the patient about possible risks and side effects of using medicinal cannabis given their condition.7 The practitioner will also be required to
6 KRS §§ 218A.202.
obtain a KASPER report on the patient covering the preceding twelve months.8 The practitioner must then certify in writing to all of the above and that they believe the patient could receive therapeutic or palliative benefit from using medicinal cannabis. The practitioner will be obligated to enter each certification issued in KASPER within twenty-four hours.9
While practitioners and patients will need to meet multiple requirements to obtain medicinal cannabis under Chapter 218B, it is hoped that making this form of treatment legally available for patients with serious medical conditions and terminal illness will improve their quality of life and provide a safer alternative to addictive opioids.
Sarah Charles Wright is a corporate and healthcare law attorney with Sturgill, Turner, Barker & Moloney, PLLC. She can be reached at swright@sturgillturner.com or (859) 255-8581. This article is intended to be a summary of state or federal law and does not constitute legal advice.

8 KRS
9 KRS §§ 218B.050(6) and 218A.202(4).
ISSUE #147 9
7 Certifying minors as qualified patients additionally requires custodial parent or legal guardian informed written consent.
§ 218__ states that CHFS will work with the KBML and KBN to develop educational programming for practitioners regarding the purpose and use of KASPER to monitor patients seeking certification.
♦
♦
From the business of health care to compliance to litigation defense, Sturgill Turner’s experienced health care attorneys provide comprehensive legal services to health care providers, hospitals and managed care organizations across the Commonwealth.
Sturgill, Turner,
PLLC ♦ Lexington, Ky. ♦ 859.255.8581 ♦ STURGILLTURNER.COM AT T ORNEY S KENTUCK Y
LEGAL
Put our experience to work for you.
Barker & Moloney,
| TENNESSEE
Physicians, Our Patients and The Environment

How we serve and are connected
BY STEPHEN L. HENRY, MD, (RET.) FMR LT. GOVERNOR 1995-2003
LOUISVILLE Thirty years ago, the efforts to preserve the Floyds Fork watershed sparked a massive conservation movement in Jefferson County. This movement largely began with members of the medical community recognizing that the quality of our environment had a direct impact on the quality of our health. Together with the help of a wellknown community leader and philanthropist, Mary Bingham, I gathered the support of my colleagues and created the Future Fund, Inc. Mrs. Bingham, wife of Barry Bingham, Sr. who owned WHAS Radio and TV as well as the Courier Journal newspaper equally recognized the need to preserve our land and our health. These voices and partnerships helped to create a system that has today saved over 6,500 acres of conservation space, agricultural land and what many know today in part as the Parklands of Floyds Fork. But it all began with the recognition that health and environment go hand in hand.
I was raised in Western Kentucky and attended Western Kentucky University (WKU), a regional area rich with agriculture and land. After completing my undergraduate degree, I arrived as a medical school student at the University of Louisville School of Medicine, a region rich in concrete. After expressing dismay over the lack of green space on campus, my classmates quickly introduced me to the local Olmstead Parks; Cherokee/ Seneca and its 800 plus acres of green space. I was amazed at how well the parks were integrated into urban areas, rendering the concrete city landscape seemingly nonexistent. The parks became our mental and physical refuge from the daily grind of medical school internship and residency. However, we saw a need for more green space especially as urban
sprawl was beginning to threaten our more rural areas in the county.

A significant number of our medical school class remained at UofL for internships and, in my case, I stayed, specifically for orthopedic residency. Together, with a handful of my classmates, Ed Tillett (Orthopedics), Ken Hodge (ENT), David Easley (Psychiatry), Janet Day (OB/GYN), and Russ Williams (General Surgery), who was also the medical society president, we began advocating for additional park space in the outer boundaries of Louisville. We saw the need for a second generation of Olmsteadian parks. With their support and encouragement, I was convinced that one of the only ways to make this happen was to involve myself in the process of government and run for one of three commissioner seats in county government. My platform was based on a vision for future city planning which called for a new generation of parks and green space on the perimeter of Louisville. I ultimately won and became the A District Commissioner for Jefferson County. Out of the gate I wanted to set an example about the need to take ownership over our environmen-
tal issues at home and immediately converted my car to a natural gas flex fuel vehicle to highlight the importance of clean air. We went on to establish the Clean Fuels Coalition and then started the process of protecting the Floyds Fork watershed. Having served as the president of the Tyler Park Association and understanding the impact of parks on our health I was motivated by my fellow physicians and colleagues, who also grew up near Cherokee Park, to advocate for restrictions to developments near the Floyds Fork watershed. Needing an additional ally, I called upon David Jones, healthcare executive and co-founder of Humana. Both of us agreed on the need for future green space to promote health lifestyles, exercise, clean water, and clean air. Major contributions from Humana assisted in additional land purchases that have helped to make the Future Fund the largest nonprofit landowner in Jefferson County. By the end of 1994, the Jefferson County Fiscal Court passed a comprehensive protection zone along 80% of the southern course of Floyd’s Fork Creek. The plan or Design Review Overlay (DRO) was designed to limit development along the riparian zones along the 31 miles of Floyds Fork Creek in eastern Jefferson County. The plan provided set back of residential development to limit run-off of fertilizer and roadway pollutants. Riparian zones provide a natural filtration of such pollutants. The DRO further restricted filling of the floodplain to allow for development close to the creek. With the protection of the DRO, the Floyds Fork, Inc. purchased thousands of acres of flood plain over the next 25 years. A decade later, David Jones and his son Dan would lead another equally important mission to establish the Parklands of Floyd’s Fork with a significant component of the greenway being comprised of land from the Future Fund, Inc. Together, we had a reason to cel-
10 MD-UPDATE
OP/ED
Stephen L. Henry, MD, (ret.)
ebrate and expect that future generations of government would remember and recognize the positive impact these conservation movements had made on our community.
Government, however, has had a very short memory. Unfortunately, significant development under Mayor Fisher’s administration through the office of Planning & Development has threatened years of envi-
ronmental progress by allowing high density development in the flood plain and within yards of Floyds Fork.


It seems that once again, our medical community is needed to remind government about the impact of clean air and water on the health and well-being of our community and its people. As physicians must continue to advocate for our patients, fellow citizens
and even ourselves. If we want and expect a sustainable environment that promotes sustainable health, we must participate in discussions which influence the outcome for future generations.
Personally, my own physician challenges me to exercise more to raise my HDL and moderate my triglycerides and cholesterol. He also advocates for a healthier high fiber diet with fewer calories to lower my blood glucose and A1C levels. He recommends drinking no less than 2.5 liters a day to promote healthy renal function, and I completely agree with all of his recommendations. However, I also must consider the environmental effects on my lungs and heart when I run or bike in our parks. Louisville routinely reports air quality index levels above the World Health Organization’s (WHO) air quality standards. While medicine can play a substantial part in keeping us healthy, our environment also has its role…whether it will be a positive or negative one is up to us.
In June of 2022 the AMA adopted a new policy declaring climate change a public health crisis. In fact, AMA board member Ilse Levin stated, “Taking action now won’t reverse all of the harm done, but it will help prevent further damage to our own planet and our patient’s health and well-being.”
Clearly, physicians as a whole have ignored the obvious threat to our patient’s health by ignoring the quality of our environment but it’s not too late to join us. Together, we can continue to impact our local community by saving Floyds Fork one acre at a time. For more information, please visit www.savingfloydsfork.org or call Future Fund, Inc at 502.376.1967.
ISSUE #147 11
OP/ED
Floyds Fork Conservancy Greenway Project (Parcels outlined reflect land acquired to protect Floyds Fork Waterway)
“A knee replacement depends highly on the accuracy of those measurements. The robot also allows us to make minor adjustments virtually, before we make any actual cuts.”

– Tharun Karthikeyan, MD
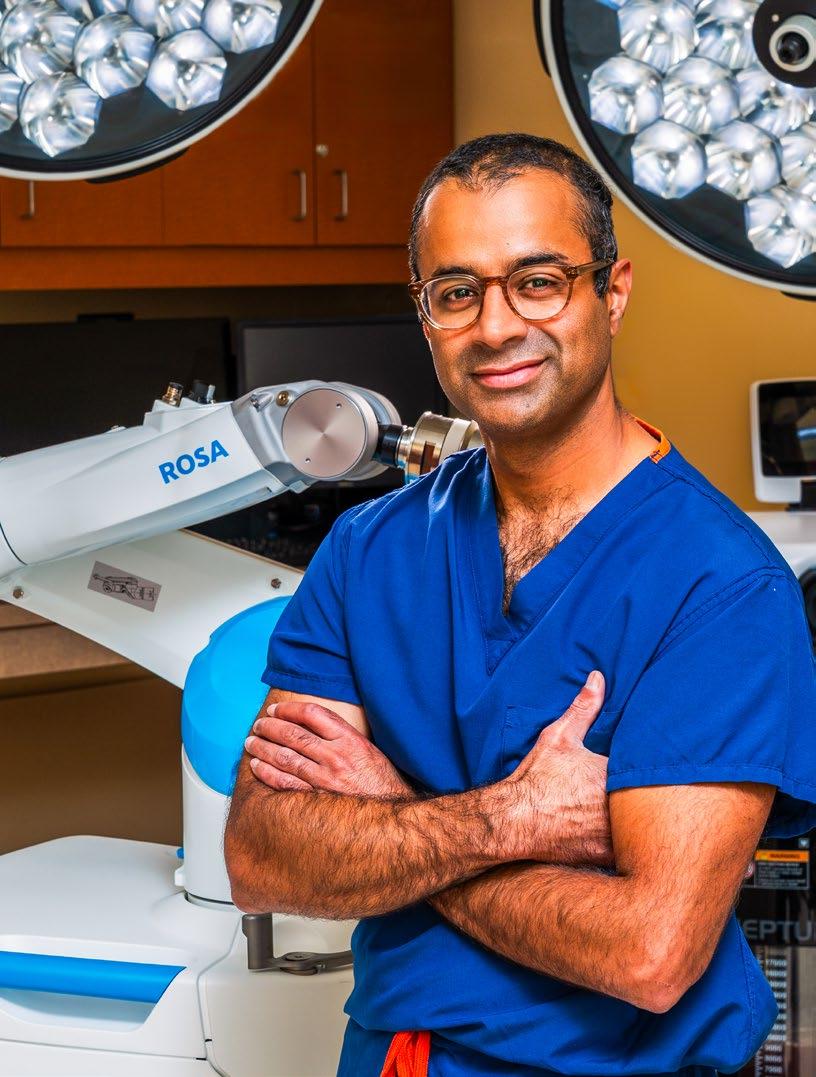
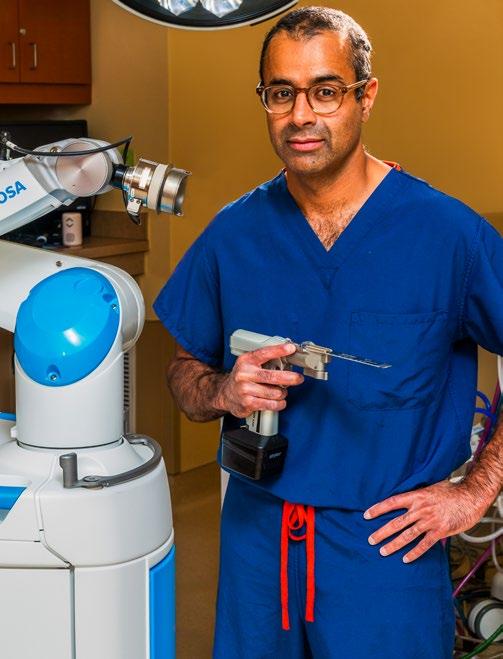
A Cut Above Lexington Clinic Orthopedic Surgeon Tharun Karthikeyan, MD, embraces the advantages of the ROSA robot
 BY JIM KELSEY
BY JIM KELSEY
LEXINGTON A master craftsman not only possesses remarkable skills, but also knows what tools to use, when to use them, and why. The skill comes in utilizing the tool to its full capacity.
Orthopedic surgeon Tharun Karthikeyan, MD, has made a career of using his keen eyes and steady hands to perform delicate knee and hip replacement surgeries. It is fair to say he has mastered the craft. A native of West Virginia, he graduated from James Madison University. He continued to study his profession of choice, honing his skills at the University of Pittsburgh School of Medicine, where he also completed an orthopedic surgery residency and a trauma fellowship. He completed a total joint fellowship at OrthoCarolina Hip and Knee Institute in Charlotte, North Carolina. In 2012, he brought his talents to Lexington Clinic’s department of orthopedics and sports medicine, specializing in joint replacement.
For the ensuing decade, the techniques that Karthikeyan used to perform hip and knee replacements remained largely unchanged. He consulted with patients and their families before surgery, explaining the marginal risks, recovery process, and likely outcomes. He carefully planned every surgery with his team, mapping out the processes, becoming more precise and more efficient. He and his surgical team had virtually perfected the procedures and were overwhelmingly successful in helping the majority of their patients have positive outcomes. But despite all the training, skill, and practice, there was still room for improvement. That improvement came with the addition of a new team member who goes by the name of ROSA®, the Robotic Surgical Assistant, manufactured by Zimmer Biomet.
“I was hesitant at first because knee replacement was my bread and butter,” admits Karthikeyan, who also serves on the Board
of Directors of Lexington Clinic and is the Director of Hip and Knee Surgery at Saint Joseph Hospital. “We were efficient and had good outcomes with patients. It didn’t feel like we had a problem to fix. But the reality is, that while a knee replacement is a very good and reliable operation, there are still about 10 to 20 percent of total knee replacement patients that don’t really love their knee replacement. Robotics is going to be the technology that unlocks the secret of how to bring that dissatisfaction rate down.”
Lexington Clinic began exploring the possibility of robotics for knee replacement in 2022, evaluating the leading robots on the market before choosing ROSA. Karthikeyan and his team acquired ROSA in January 2023 and, after training, performed their first procedure using ROSA in early February. Now, Karthikeyan uses it multiple times per week.
“Anyone who is a candidate for a knee replacement is a candidate for a robotic knee replacement,” he says. “We use the robot for almost every knee replacement.”
Physician and Patient Education
Today, there are only two ROSAs in use in Kentucky. As an educational consultant for Zimmer Biomet, Karthikeyan provides surgeon-to-surgeon education on the use of ROSA robotic technology. Surgeons from Kentucky, West Virginia, and Indiana have come to Lexington Clinic Surgery Center to observe Karthikeyan and his team perform total knee replacements.
“Those are some of my favorite days,” says Karthikeyan, who was the first surgeon in Lexington to employ this robotic surgical system for knee replacement. “It’s exciting to share the technology and to answer questions.”
Karthikeyan performs surgeries on Mondays, Wednesdays, and Fridays. Approximately 55 percent of those surgeries are knee replacements, with the other 45 percent hip replacements. He sees patients in the office on Tuesdays and Thursdays. The average age of his joint replacement patients is 63 years old and evenly split between men and women.
During the patient consultation, Karthikeyan encourages patients to try nonsurgical options if they have not already done so. He explains what a knee replacement is, using a model as a visual aid, and discusses recovery time and the importance of physical therapy.
“There are often misconceptions about what a joint replacement looks like,” says Karthikeyan. “For knee replacements, people get the idea that the bone is just lopped off here and lopped off there and it’s just a big piece of metal. But we actually keep the bone and just cut off the arthritic ends and essentially cap them. Another common misconception is the longevity of the implants. People think that
ISSUE #147 13 PHOTOS BY PAUL MARTIN AND PROVIDED BY LEXINGTON CLINIC
COVER STORY
Lexington Clinic acquired the ROSA® by Zimmer Biomet in January 2023. Now, Karthikeyan uses it multiple times per week.
their hip or knee replacement is only going to last 10 or 15 years, but we can get 30 to 40 years or longer out of the modern materials.”
With less than a year of experience utilizing ROSA, Karthikeyan and his team already have become experts in the process. They can perform the robotic knee replacement in about an hour, which is essentially the same amount of time as needed for the conventional total knee replacement surgery.
Regardless of the robot’s capabilities, the success of every surgery still relies on the skillful work of Karthikeyan and his team. ROSA is a tool that hasn’t replaced them but has enhanced what they are able to do.
“We have a team that is very well versed in these operations,” Karthikeyan says. “Many times, I don’t have to say a word. They know what the next step is and I just hold my hand out and the instrument is there. There is no single one of us who could do this on our own. Everyone understands that their role is critical and that, ultimately, we all work for the patient.”
Investment Begets Better Outcomes
Putting the patient first is what led to the decision to purchase ROSA in the first place. While it is too early to get an accurate picture of the long-term advantages of a knee replacement using the robot, other benefits are already apparent.
“Even a very high-volume, experienced total knee surgeon is going to have a margin of error in terms of estimations of angles, thicknesses, or distances. The robot is more accurate in estimating those variables,” says
Karthikeyan. “A knee replacement depends highly on the accuracy of those measurements. The robot also allows us to make minor adjustments virtually, before we make any actual cuts to see how that will affect the overall behavior of the knee in terms of range of motion. So we can make minor adjustments and test them in real time before we ever make a cut. That’s not something we can do with traditional instrumentation.”
Also in the future, at least for Karthikeyan, is the use of the robot for hip replacements.
In the meantime, the master craftsman will continue to fine tune his skills with ROSA and the knee replacement procedures. Once a skeptic, he is now a firm believer in the benefits of the robot for his patients, his team, and even himself.
“The benefit for the patient, we think, will be an earlier recovery and a longer lasting more natural feeling knee replacement,” he says. “The benefit to me is that I can feel more confident in the knee replacement that I just executed for that patient.”

14 MD-UPDATE
PHOTOS BY PAUL MARTIN AND PROVIDED BY LEXINGTON CLINIC
“For knee replacements, people get the idea that the bone is just lopped off here and there, but we keep the bone and just cut off the arthritic ends and essentially cap them.” - Tharun Karthikeyan, MD
COVER STORY
“Anyone who is a candidate for a knee replacement is a candidate for a robotic knee replacement,”- Tharun Karthikeyan, MD, orthopedic surgeon, Lexington Clinic Department of Orthopedics and Sports Medicine
Your Trusted Lung Transplant Partner
The Lung Transplant Program at world-renowned UofL Health – Trager Transplant Center offers the highest level of expertise in lung transplant and advanced lung disease. With more than 360 lung transplants completed since 1991, we are home to lifesaving “firsts” in the region, including Kentucky’s first double-lung transplant and the state’s first dual heart-lung transplant.
As a global leader in ground-breaking research, innovation and education, patients receive cutting-edge advancements and less invasive treatments that save lives and improve quality of life. We are leading experts in advanced organ diseases and organ failure, specializing in:
n Advanced Lung Disease
n Single and Double-lung Transplant
n Multi-organ Transplants – including lung, to treat several advanced diseases simultaneously
With every referral, our interdisciplinary team partners with you to navigate a plan for the best possible outcomes. Together, we can offer hope to patients and their families.
To explore our best-in-class care, visit UofLHealth.org For Heart/Lung, call 502-587-4384
Matthew Fox, MD Lung Transplant Surgical Director

THAT’S THE POWER OF U

700 Bob-O-Link Drive, Lexington | 859.258.8575 | lexingtonclinic.com/sports Below L-R: Tharun Karthikeyan, MD David Dome, MD James Gardiner, MD Benjamin “Bo” Schneider, MD Stephen Umansky, MD Peter Hester, MD W. Jeffrey Grantham, MD Brandon Devers, MD
ORTHOPEDICS Your Orthopedic Pros!

Lexington Clinic Orthopedics – Sports Medicine has served Central Kentucky for over 40 years. Our fellowship-trained physicians treat a variety of orthopedic conditions and injuries, utilizing cutting-edge surgical procedures and non-surgical techniques to ensure the best patient outcomes.
From evaluation, imaging and therapy management to surgical treatments, you can count on your #orthopros to help keep you moving.
Some of the specialty services offered include the evaluation and treatment of:
• Fractures & Dislocations
• Hand, Wrist & Finger conditions
• Hip, Knee and Ankle conditions
• Osteoarthritis
• Shoulder & Elbow conditions
• Sports-related Injuries
• Sprains & Strains
• Work-related Injuries
As well as:
• Convenient Physical Therapy Services
• OrthoGo Walk-In Clinic M-F 7:30 a.m. – 7:00 p.m.
• Overhead Throwing Program
• Sports Injury Prevention Programs
LEXINGTON CLINIC
Making a Difference
UK HealthCare’s Physical Medicine and Rehabilitation Department expands into new facility, adding faculty, staff, and patients
BY GIL DUNN
LEXINGTON Like the mythical baseball field in the movie, Field of Dreams, an Iowa cornfield transformed into hallowed ground for dishonored and forgotten legendary baseball players, the new UK HealthCare outpatient Physical Medicine & Rehabilitation (PM&R) clinic at Cardinal Hill Rehabilitation Hospital on Versailles Road in Lexington has patients coming to it from all over Kentucky in mass numbers, seeking rehabilitation and independence. To paraphrase a famous line from the movie, “If you build it, and they will come.”
The UK HealthCare Department of PM&R had been spread over two locations, the Good Samaritan Hospital on the UK HealthCare campus, and a smaller space at Cardinal Hill. In 2015, Encompass Health, an inpatient acute care provider, purchased the Cardinal Hill location from Easter Seals. UK PM&R remained as a tenant. Through negotiations, the decision was made for UK to lease all the outpatient physician clinic and therapy space from Encompass. Thus began a multi-year remodeling and upgrade project which consolidated all the UK outpatient PM&R services into one location.
Meet the Chairperson
Susan McDowell, MD, chair of the UK

HealthCare Department of Physical Medicine & Rehabilitation recalls that PM&R became her specialty and life’s work by research and discovery. In her third year of medical school, she was searching for a specialty and was concerned that “nothing was lighting my passion, my fire,” she says. Then she came upon a description of PM&R in the back pages of a specialty resource volume. It interested her enough to take an elective rotation in PM&R in her fourth year of medical school.
“After two days in my rotation in physical medicine, I knew I had found my place. I could work with people, fixing things for them, improving their quality of life and develop long-term relationships using my skills, knowledge, and technology,” says McDowell.
“I found my ‘Why,’” she says, “because I can have a positive impact on every patient’s life that I touch in my work as a physician, using everything I’ve learned and my ability to interact with other specialists to benefit patients. Doing whatever is necessary. Taking a challenging situation and finding a way to bring value to a patient’s life, for them to be independent. For them to find social, mental, and physical daily health and wellness in everything they do.”
McDowell grew up in Augusta, Georgia, the youngest of six children. In high school she played softball and basketball. Her mother was a nurse. She received her BS in chemistry from Augusta College of Georgia and her medical degree from the Medical College
18 MD-UPDATE
Susan McDowell, MD, chair of the UK HealthCare Department of Physical Medicine & Rehabilitation
SPECIAL SECTION PHYSICAL MEDICINE & REHABILITATION
PHOTOGRAPHY BY GIL DUNN
of Georgia. She completed her residency in PM&R at the University of Kentucky. She is board-certified in PM&R with a subspecialty certificate in spinal cord injury medicine. She provides inpatient and outpatient care for adults and children.
McDowell joined the UK faculty in 1994, directed the residency program from 1996 through 2001, and became chairperson for the Department of PM&R in 2013. Now she leads a department with 19 doctors, a practice manager, a nurse manager, plus two RNs, three medical assistants, seven administration staff, and a clinical social worker at a newly remodeled facility.
In addition to her clinical and administrative department work she is on faculty and professor of PM&R at the UK College of Medicine. She also serves as a consultant at the Lexington Shriner’s Medical Center for Children where she participates on a multidisciplinary movement disorders team.
PM&R: A Broad Mission with a Long-term Focus
According to the description on its website, which McDowell crafted, UK Physical Medicine & Rehabilitation helps patients who have severe neurological or musculoskeletal impairments. The goal is “to restore each patient to their highest possible level of medical, psychological, social, and vocational function. A multidisciplinary team approach is used in all aspects of care.”
Areas of specialties include arthritis, back pain, stroke, brain injury, congenital neuromuscular, sports injuries, musculoskeletal disorders, electromyography, neuromuscular disorders, spasticity management, spinal cord injury, and management of amputees.
McDowell says that the decision to take the PM&R outpatient physician clinic to Cardinal Hill was made to allow more space for care of the rehabilitation patient. The move doubled the space to provide patient care, assured all clinic rooms were fully accessible, pulled all teaching faculty into one location to facilitate medical student and resident education and allows more opportunities to do meaningful research work. The process started in the winter of 2020 and was completed in June 2022.
“We really closed the loop on providing a wide range of rehabilitation care and services within one location,” say McDowell, adding that now inpatient care individuals can transition to outpatient care in the same physical location.
The numbers bear out the wisdom and forecasting of the expansion and consolidation.
Combined physician clinic visits for Cardinal Hill and Good Samaritan were 8,442 in 2020, 9,028 in 2021, and 9,956 in 2022. In fiscal year 2023, the new facility had 11,931 visits. In the first six months of calendar year 2023, the outpatient therapy visits have already topped 14,000.
“We’re already at year three of our projections after the first year,” McDowell states. “We believed the need was present, but we’re still a little surprised. It affirms what we thought the need was going to be.”
Growing a Department to Fill the Need
What’s driving the growth of PM&R? Multiple factors are the reason, says McDowell. Certainly, the new and increased space allows for more patients. The extra space has given room for adding new faculty and staff. New faculty translates into more specialized services, a wider breadth of care, and more research.
Faculty members and their areas of interest include:
• Nicholas D. Annichiarico, DO, UK HealthCare Medical Director of inpatient rehabilitation services
• Samuel H. Byron, DO, osteopathic manual manipulation
• Derek S. Dixon, DO, musculoskeletal and neurologic rehabilitation
• Nicholas C. Elwert, DO, medical director of stroke rehabilitation
• Lauren E. Fulks, MD, pediatric rehabilitation
• Emily D. Hogancamp, MD, pediatric and neurologic rehabilitation
• Cecil T. Hollen, DO, musculoskeletal care
• Justin Huber, MD, stroke rehabilitation research
• Jamie L. Key, DO, brain injury rehabilitation, residency program director
• Brock H. Marrs, MD, interventional pain
• Robert B. Nickerson, MD, electrodiagnostic medicine
• Michael C. Parrott, DO, musculoskeletal care
• Dwan R. Perry, DO, musculoskeletal care, sports medicine
• Stephen T. Porter, MD, brain injury rehabilitation
• Randal E. Schleenbaker, MD, general rehabilitation
• Sara Shahid Salles, DO, spinal cord injury medicine, movement disorders management
• Nancy J. Stiles, MD, inpatient rehabilitation
• Nathanial J. Thomas, DO, musculoskeletal care, amputee care
• Celysse M. van Zyl, DO, osteopathic manual manipulation
McDowell says her department has a fine balance of senior leadership with “new recruits who have the mindset and skills we value. They’re willing to step up and be accountable to our patients and everyone in our department. We look at our department like a family.”
Technology Aids Recovery
Increased staff is just one of the factors driving growth. Another is new technology, which McDowell and her team embrace. Ultrasound diagnostic technology has dramatically advanced PM&R, says McDowell. Electronic nerve testing and muscle response are the new standards for diagnosing loss of function or pain. Spinal cord stimulation, which can revive nerve pathways, can lead to recovery of movement to pre-trauma levels.
Physical and occupational therapy equipment and techniques have also advanced exponentially. PTs and OTs at UK’s Cardinal Hill facility use the ZeroG Gait and Balance System, which uses harnesses similar to the ones used in mountain climbing attached to the bodyweight support system, allowing stroke and brain injury patients an opportunity to walk as part of the recovery process. Aquatherapy can
ISSUE #147 19
SPECIAL SECTION PHYSICAL MEDICINE & REHABILITATION
also be effective. There is a large therapy pool at Cardinal Hill, which McDowell says is used for patients relearning to walk and is effective in management of musculoskeletal rehabilitation. The post-concussion and vestibular rehabilitation programs also use state-of-the-art technology for achieving the best outcomes.
The new generation of electric wheelchairs can be like buying a new car, says McDowell. “What accessories do you want it to have?” she says. “A battery-powered wheelchair can give real independence to a person who cannot move themselves.”
According to McDowell “tech-assistant technology” uses computers programmed to speak for a nonverbal patient. The computer can speak for the verbally disabled person with preprogrammed sentences, such as “I’d like a drink of water,” by using a motion as simple as a slight movement of the head or pointing to an icon on the computer screen.
“Technological advancements are ripe for helping individuals with disabilities become
self-sufficient,” says McDowell. “What we non-disabled people take as a convenience such as an iPad, an iPhone, or Alexa, can be modified for use for the disabled population.”
“The disabled population is relatively small, so the return on investment for new products is limited. So, we adapt existing technology for our use in treating the disabled,” she concludes.
The Role of the Physiatrist. Making a Difference.
McDowell acknowledges that PM&R is sometimes under-appreciated by other physicians and the general public, but not the disabled population. There haven’t been many TV shows or movies about physiatrists. She wants referring physicians to know that PM&R physicians can improve outcomes for musculoskeletal and neurologically impaired patients through non-surgical interventions.
“What we do is exam the patient, diagnose the problems, develop a rehabilitation plan,
put the plan in motion, and then follow up for progress and adjust or modify the plan as needed. Getting someone back to normal, or as pre-injury normal as possible. Meeting them where they’re at, from crawler to walker.”
Reflecting on her career, McDowell says that little by little she came to believe that she could make a difference as she acquired the knowledge of her specialty and learned leadership. She recalls seeing her mother give her all for her family when times were tough. She learned early in life about personal responsibility, accountability, self-discipline, and giving back through family, academics, athletics, and community.
“I learned resiliency, not giving up, realizing that sometimes it takes longer than you want it to. Not getting a ‘Yes’ on the first try. We embrace that in our department. We teach it, we live it and breathe it. We’ve come a long way. There’s more work to do and we’ll get there.”

20 MD-UPDATE
SPECIAL SECTION PHYSICAL MEDICINE & REHABILITATION
“I learned resiliency, not giving up, realizing that sometimes it takes longer than you want it to. We embrace that in our department. We look at our department like a family. ”- Susan McDowell, MD PHOTOGRAPHY BY GIL DUNN
Game-Changing Orthopedic and Sports Health Care
Norton Healthcare program aims for exceptional holistic care
BY MENISA MARSHALL
LOUISVILLE A new care approach is emerging in sports medicine and Ryan J. Krupp, MD, is happy to see it reflect game-changing elements of orthopedic care. Krupp is an orthopedic surgeon with Norton Orthopedic Institute, as well as executive medical director of Orthopedics and Sports Health and Shoulder Reconstruction for Norton Healthcare
“The focus is shifting from traditional injury treatment to the overall health and well-being of athletes,” says Krupp. “This holistic approach recognizes athletes are complex individuals who require comprehensive care.”
Krupp explains that across multiple targeted programs and services, Norton Healthcare works to deliver first-rate orthopedic and related care that goes beyond sports alone.
It is about meeting the overall care needs of patients who may run the gamut from weekend warriors to Silver Sneakers members, to high level athletes.
“This is for anybody. The level someone operates at doesn’t matter,” he says. “Our goal is to treat every person as an individual, and help every patient maintain their best level of health and optimal performance.”
Comprehensive, Innovative Care
Within the broad areas of orthopedics and sports health, various Norton Healthcare departments and teams strive to deliver exceptional care across various parameters.
Patients range in age from adolescence to their 90s, which makes for a diverse range of clinical presentations. Conditions that Krupp and the rest of the shoulder team treats run
the gamut from shoulder instability or dislocations in younger patients to proximal humerus fractures among older patients. The practice’s arthroscopic work involves many rotator cuff and labral repairs along with a variety of other interventions.

The team, which also includes Justin Givens, MD, Joshua J. Christensen, MD, Nyagon G. Duany, MD, and Chad E. Smith, MD, treats “teens and tweens,” but their care sometimes calls for coordination with other departments and care teams. For example, a case involving a 12-year-old might ultimately be referred to a pediatric orthopedic surgeon. Conversely, one of his pediatric orthopedic colleagues might refer a 16-year-old with an extensive labral tear.
“There’s a lot of care overlap, and we work together to provide the best care and outcomes possible for every patient,” says Krupp.
ISSUE #147 21
SPECIAL SECTION ORTHOPEDICS/SPORTS MEDICINE
Ryan J. Krupp, MD, performs surgery at Norton Brownsboro Hospital. PHOTOS BY JAMIE RHODES/ NORTON
HEALTHCARE
Early Love of Sports Sparks “Fixer’s” Medical Career
In his leadership role within the shoulder surgery realm, one key thing Krupp likes about his work is helping people enjoy their lives and get the most from their experiences at any age. He says, “Keeping people mobile and active really resonates with me.”
A look at Krupp’s background leaves little doubt as to what drew him to orthopedic and sports medicine. He is proud to come from a “working class” family and enjoyed playing multiple sports in high school.
In high school, he suffered an open tibia fracture while playing basketball. He was impressed by the surgical procedures that he underwent, including placement of an intramedullary nail. Undergoing surgery and the follow up physical therapy and rehab struck him as important work that helps athletes and others recover from serious injuries.
Interacting with surgeons, physical therapists, and other caregivers resonated with the young patient who saw himself as “a fixer.” The physician-in-the making had always liked analyzing things, finding answers, and developing action plans.

“Orthopedics really appeals to me and my personality,” he says. “I’ve always liked being able to define problems and find solutions for them.”
Krupp and his brother were the first members of their extended family to attend college. Krupp briefly participated in the football program at the University of Dayton. He loved the experience but was attending the Ohio school on an academic scholarship and decided his chemical engineering and pre-med courses had to come first. He holds a degree in chemical engineering but knew early in his education
and work journeys that sports and medicine were in his blood. “It’s something I’ll always enjoy,” he says.
The love of sports is a Krupp family trait. Both his son and daughter are competitive athletes. “It’s a lot of fun that we enjoy together as a family,” says Krupp, who sees his personal experience with athletics as an advantage in his work. It helps him understand the impact of training or muscle overuse. It allows him to relate with patients, sometimes including their parents, and treat them more effectively.
After college, Krupp worked briefly as a chemical engineer and in pharmaceutical sales before starting medical school at the University of Louisville. He completed an orthopedics residency at UofL followed by a sports medicine and shoulder reconstruction fellowship at the Steadman Hawkins Clinic of the Carolinas. Krupp joined Norton Orthopedics in 2008.
Aside from providing direct patient care, Krupp plays a key role in the business side of his practice. He also carves out time for clinical research. Research is critically important to the ever-changing treatment of orthopedic injuries — something in which the team, and Krupp especially, is involved.
“I’m involved with companies developing the next generation of implants and procedures we use for surgery,” he says. “I even do some
PHOTOS BY JAMIE RHODES/ NORTON HEALTHCARE
work on projects looking at robotics, artificial intelligence and those types of things.”
Through his practice, Krupp sees a wide spectrum of shoulder issues among patients from their teens to their golden years. Among different age groups common problems can range from instability to dislocations to proximal humerus fractures.
Krupp does a significant amount of arthroscopic work, plus open surgeries as needed for rotator cuff or labral repairs. He also performs many total and reverse shoulder replacements as well as a variety of additional arthroscopic and open surgeries, which can include proximal humerus fractures, clavicle fractures, acromioclavicular joint separations, and various other instability operations.
“We’re really a tertiary referral center, so we get a lot of difficult cases sent in from outside,” says Krupp.
Despite a busy practice schedule, Krupp and his colleagues provide coverage for community programs and events. Over the past 15 years they have covered everything from high school and college sports to Iron Man competitions.
Team’s Newest Member Specializes in Advanced Shoulder, Elbow Care
Justin Givens, MD, is excited to join Norton Healthcare’s Orthopedic Institute. As the team’s newest member, he welcomes opportunities to provide patients with advanced, innovative shoulder and elbow care.
Givens grew up in southcentral Kentucky and graduated from Lindsey Wilson College with a surgical residency at the University of Louisville. He completed a shoulder and elbow fellowship at the Florida Orthopedic Institute, and recently completed a special sports fellowship that involved extra training.
22 MD-UPDATE
Ryan J. Krupp, MD, Nyagon G. Duany, MD, and Justin Givens, MD, are three members of the shoulder surgery team at Norton Orthopedic Institute.
SPECIAL SECTION ORTHOPEDICS/SPORTS MEDICINE
Shoulder to shoulder with the best in joint care.
Justin Givens, M.D., is joining the Norton Orthopedic Institute team and bringing an innovative approach to shoulder and elbow care. To make a referral, visit NortonEpicLink.com or call (888) 4-U-NORTON (486-6786).

He expects to treat many young patients for shoulder problems or dislocations related to trauma, sports injuries or overuse. Givens is one of only a few specialists in Kentucky able to perform pyrocarbon hemiarthroplasty, an innovative partial humeral replacement technique for those with intact rotator cuffs.

The FDA only recently approved this procedure for use in the US. Its use in Europe has shown promising results that help patients avoid full shoulder replacement and stay active with fewer restrictions on what they can lift.
Among his cohort of older patients, Givens treats injuries related to rotator cuff tears or arthritis. He sees hardworking people who have endured years of pain because they were told nothing could be done for them. “I’m not saying we have an answer for every problem, but we have a lot of options in our toolbox,” he says.
For example, Givens cites allograft reconstruction as an innovative procedure that can allow replacements in the setting of severe bone loss and deformity when there were previously no answers for this issue.
Muscle transfers, another relatively new development, are proving to be game-changers for treating shoulder pain and loss of function. The procedure involves moving a working muscle or tendon to replace one that is non-functioning. Most of the muscle transfers the Norton Orthopedic Institute team performs involve rerouting part of a patient’s trapezius muscle to function in a new way.
Platelet-rich plasma injections are another useful tool to help patients suffering from “borderline injuries.” For instance, a patient might have a partial cuff tear or a painful shoulder that does not call for full reconstructive surgery. PRP injections are a non-operative option that can help relieve pain and stimulate healing.
Subscapularis-sparing surgery is another innovative procedure Norton Orthopedic Institute experts can offer candidates for shoulder replacement. It allows surgical reconstruction of the shoulder while leaving the muscles of the rotator cuff intact. Givens is well versed in this procedure, which typically involves a shorter healing time than traditional shoulder replacement techniques.
“Our experience doing subcap-sparing surgery makes us one of only a few places in the
country doing this procedure,” says Givens. “It allows the patient to be out of a sling in a couple of days instead of spending weeks in a sling waiting for your rotator cuff to heal.”
Striving for Exceptional Individualized Care
Emerging technologies continue to play a crucial role in the impressive work Krupp, Givens, and the rest of the team does to provide patients with their best possible outcomes. Both physicians see the value of having a wide portfolio of options available to meet their patients’ individual care needs.
“You might say we’re always looking for a better mouse trap,” Krupp says with a laugh.
Both Krupp and Givens agree this is an exciting time to look at different ways to add technology like robotics or artificial intelligence
to their work. They continue to see great promise in today’s emerging technologies and better processes like the improved longevity of today’s shoulder replacements. Due to improved coatings and other advances, modern-day implants may be able to last well beyond 15 to 20 years. They also promote stronger bone-growth bonds.
“Our aim is always to provide the best individualized care we can to every patient,” says Krupp. “We strive to treat every patient the way we want our own families to be treated.”
Ultimately, the doctors and their teams work from the concept that exceptional care is built on meeting each patient’s unique needs using the right individualized approaches, resources, and tools. It is important, Krupp points out, to avoid the well-known adage that warns if the only tool you have is a hammer it is tempting to treat everything as if it were a nail.
24 MD-UPDATE
HEALTHCARE SPECIAL SECTION ORTHOPEDICS/SPORTS MEDICINE
Chad E. Smith, MD, and Joshua J. Christensen, MD, are also members of the shoulder surgery team at Norton Orthopedic Institute.
PHOTOS BY JAMIE RHODES/NORTON
Orthopedist Jim Rollins, MD, Is What Every Town Needs
Years of practice in the same town means generations come to see the CHI Saint Joseph Health orthopedist
BY TIM CORKRAN
MOUNT STERLING Most small towns have a family physician, the doctor who treats generations of patients, attends the local high school events, and advocates for the health of the population. Mount Sterling is lucky to have its own local orthopedist. Jim Rollins, MD, has been a Montgomery County fixture for over 20 years, just as likely to be spotted on the football sidelines as in his pew at church. His practice, as part of CHI Saint Joseph Medical Group - Orthopedics, has him healing bone and joint injuries and performing joint replacements, just the way he had envisioned it during medical school; helping the same families year after year, caring for young athletes, along with folks drawn in from the wider region.
Rollins grew up in central Ohio and owes his profession to a football injury. As a high schooler, the orthopedist who treated his back served as an inspiration and a motivator. Instead of his college plan for architectural engineering, Rollins migrated to medicine, with that same orthopedist remaining a mentor through those years. After getting his medical degree from the Medical School of Ohio, now the University of Toledo, Rollins had a residency mentor whose style of practice was to be emulated. Orthopedist Anthony Frogameni, MD, impressed Rollins with how he integrated into his community and how he worked with patients. This style guided Rollins in the creation of his Mount Sterling practice.
Rollins and his wife, along with their two sons, arrived in the area in the late 1990s to be nearer to her family. He soon had his practice up and running and within a few years, his pattern
was set. Local people with joint wear and tear or work or sports related injuries comprised the bulk of his patients, along with plenty of folks from further east and southeastern Ohio. For a time, he was interested in hand surgery and foot and ankle injuries, but he has migrated to joint replacement as his surgical focus.
Local Concerns, Local Involvement
Rollins’ patient population ranges from 10–90, and like most Kentucky physicians, his practice is informed by the common health concerns of the Commonwealth’s population. Obesity, diabetes, and generational sense of autonomy, so common in his patient
population, concern him because of the added impact to common joint maladies. He tries to work with his patients to reduce these risk factors, and he will not perform surgery on patients whose BMI exceeds 40.
Rollins rues the independence of some of his eastern Kentucky neighbors, noting that many with minor joint injuries could avoid later surgery if they saw him sooner. He always tries conservative measures first — medical interventions, physical therapy, injections, lubrication, arthroscopy, to name a few — but some patients won’t come to him until it is too late for these things, and joint replacement is the only option.
Rollins says his practice has a family atmosphere to it. He notes that people in his region often come into their appointment with 4–5 different family members, and he is seeing a second generation of patients. Multiple times he has treated the children of people he treated a few decades ago. “With over 22 years there,” he says, “I have developed a pretty good relationship with my patients. Now I am seeing the children of some of my patients.” Rollins is also a fixture on the Montgomery County football team sidelines, having served as the home game physician for over 20 years. He enjoys being part of the student experience and providing the immediate care that may prevent later extensive joint damage.
Rollins knows many of his patients well. Often people he has treated for minor issues return years later for joint replacements. “I get to see the full range: some of my patients had arthroscopic surgery years ago, then as they get older, they are getting a joint replaced.” And they clearly value this familiarity. He notes that

ISSUE #147 25
“People come by the house all the time saying ‘I need to see you, can you get me in?’” – Jim Rollins, MD
PHOTOGRAPHY BY GIL DUNN
SPECIAL SECTION ORTHOPEDICS
“I have developed a pretty good relationship with my patients. Now I am seeing the children of some of my patients.”
“People come by the house all the time saying, ‘I need to see you — can you get me in?’”
Evolving Needs and Evolving Practice


Rollins has watched his sports medicine work evolve over the years with the increase of competitive activities. He has always seen a lot of young athletes, but now the population has two distinct characteristics. He sees more young women than he used to, as so many girls now participate in competitive cheerleading and contact sports. In addition, he sees more stress injuries that come with the longer, more intense seasons many athletes are involved with. The chance to play a sport year-round at the competitive level brings damage that the three-sport athlete rarely risked.
Rollins always wants better for his patients, as any neighbor would. His preference for a conservative approach with early intervention is an example of this. His work to counsel his patients on their general health is another. He cites common variables to treatment and

recovery, such as depression and anxiety; these hinder healing in his patients and he speaks to them about it.
Technology has improved his practice over the years. He currently uses a computer navigation program during surgery and notes that post-operative management is easier with this. “Our instrumentation comes from years of designs — and we are getting better at tracking patients because of the technology,” he says. He is currently working to get robotic surgery as an option for the Mount Sterling office, noting “It has been proven to reduce
patient pain and recovery time — it makes a difference.” He would like his patients to have access to robotic surgery because “There are fewer variables — it just does not miss.”
Rollins’ philosophy of care is simple. He says, “I treat my patients like how I would want to be treated — and I tell them what I would want a member of my family to be told.” He prefers they come to him sooner rather than later, but respects their independent nature. His faith helps this, as he believes that “God is the greatest healer, and there are times when he can do the healing, not me.”
Without an orthopedist like Jim Rollins, Mount Sterling and Montgomery County would be a lesser place. Active student athletes, farmers and laborers, and an aging population of former blue-collar workers means joint injuries abound, and having an orthopedist who is accessible and integrated to the community lessens the impact of these things. Rollins would not want it any other way, concluding, “My phone number is out there, so I get called a lot. It’s kind of a small community.”
26 MD-UPDATE
Bring them to us. For nearly 30 years, we’ve helped hundreds of clients solve their biggest money concerns. Stop worrying, and start living life on a path towards financial freedom and security. Thinking clearly about money. Caring deeply about you. FEE-ONLY FINANCIAL PLANNING LEXINGTON | LOUISVILLE 800.344.9098 | DSNEAL.COM What financial concerns keep you awake at night? See how we think about money dscottneal.com CHI Saint Joseph Health – Orthopedics For patient referral, contact: 624 North Maysville Road, Suite A Mount Sterling, KY 40353 859.497.4144 Patient
SPECIAL SECTION ORTHOPEDICS
care is a team sport at CHI Saint Joseph Health Orthopedics - Mt Sterling.
Helping Patients Put Their Best Foot Forward
BY DONNA ISON
LOUISVILLE Orthopedic surgeon Victor Anciano, MD, has started his career at UofL Health – UofL Physicians on the right foot. Along with the UofL Health – Mary & Elizabeth Hospital team, Anciano and fellow orthopedic surgeon Todd Hockenbury, MD, helped lead the effort to garner approval for UofL Health as a Foot and Ankle Center of Excellence, which is quite an accomplishment. To earn this accreditation, a facility must be assessed by a national center of excellence organization, which evaluates and scores every aspect of care – from preoperative clinic evaluation to the anesthesia workup, to surgery and postoperative plans, including physical therapy and nutrition counseling. Surgeons, physicians, nurses, and staff from each of these teams worked together to secure the coveted status for the center, located within Mary & Elizabeth Hospital.
Originally from Caracas, Venezuela, Anciano came to the United States at the age of seventeen. After receiving a BA from Earlham College in Richmond, Indiana, he went to medical school at Harvard Medical School in Boston, Massachusetts. A residency in orthopedics at the University of Virginia, Charlottesville and a foot and ankle fellow ship with OrthoCarolina in Charlotte, North Carolina, followed.
At UofL Health, Anciano is not only an orthopedic surgeon but part of the physician team for UofL Cardinal Athletics and was recently appointed associate program director for the UofL orthopedic residency. He is also a gratis clinical professor for both the orthopedic residency and podiatry residency at UofL Health. He finds the ever-changing nature of the specialty particularly exciting. “I think of all the fields in orthopedics, foot and ankle is the one that still has the most unknowns. That’s very attractive to me because there’s a lot of research to be done and knowledge to explore. There’s a lot left to understand; it’s a very complex region of the body,” says Anciano.
One recent development is the shift toward
made from sustainably caught Icelandic cod, seem to possess an antibiotic component in addition to providing a collagen matrix that promotes faster healing.
Anciano has also been pioneering fixation of certain fractures and joint fusions with non-metal screws. This is a newer technology that allows for the hardware to be incorporated within the bone resulting in fixation of the fracture/joint and no metal left behind after some time.
Along with championing the center, Anciano and Hockenbury, just launched an orthopedic foot and ankle fellowship. Anciano finds his new role as an instructor particularly


UofL Health’s new Foot and Ankle Center of Excellence will provide the latest innovations in orthopedic diagnosis, treatment, and aftercare to the region.
Victor Anciano and fellow orthopedic surgeon Todd Hockenbury, MD, helped lead the effort to garner approval for UofL Health as a Foot and Ankle Center of Excellence
SPECIAL SECTION ORTHOPEDICS
PHOTO BY UOFL HEALTH
rewarding. He says, “Residents are constantly motivated and keep you young. They ask questions, make you keep up with the literature, and I appreciate that. The hunger of the mind is infectious.”
From Athletes to Arthropathy
Anciano’s week entails two operating days and three clinic days. Mondays are reserved for inpatient operations and Fridays for outpatient procedures. His three clinic days take place at three different locations: UofL Health – Mary & Elizabeth Hospital, Medical Center East, and Medical Center South. During this time, he cares for patients of all ages — from children with injuries to geriatrics with deteriorating joints. Anciano sees a wide range of pathology including acute injuries, chronic deformities, arthritis, bunions, diabetic foot problems, ankle replacements, and more.
With each patient, Anciano strives to gain a full understanding of their life prior to and their expectations after surgery. He states, “Everyone who comes in has a goal in life. Understanding patients and where they want to be with their day-to-day activities, sports, and social interests helps a lot to drive care.”
Customizing Care for Athletes
Care for athletes varies greatly depending on their level of play, commitment to the sport, and their future plans. For example, a high school athlete who competes primarily for the camaraderie and enjoyment and only wants to make it successfully to the end of their senior season may merit less aggressive treatment than a college athlete who has every intention of making a career from their sport.
Communication is key in formulating a surgical plan, and the discussion focuses on the future, with Anciano asking, “What are your long-term goals as an athlete?” He then decides how to best get them ready for the next game, the next season, and, in some cases, the next decade of competition. The answer may be surgery coupled with optimizing lifestyle choices and physical therapy.
Anciano is proud of the sports medicine
team that has been built at UofL Health. Each of UofL’s sports teams has access to a full range of medical care from the sports medicine team, orthopedic team, and athletic trainers. At the Cardinal Station clinic, orthopedics shares a space with sports medicine and family medicine, making it easier to have an open dialogue. According to Anciano, “UofL Health fosters an environment where it’s very easy to approach each other, which at the end of the day is the best for the patient, because whenever there’s lack of communication between providers, that’s when things can end up falling through the cracks.”

With weekend warriors, the conversation is more about everyday quality of life and what activities they need to be able to accomplish to feel fulfilled. “It comes in different flavors … to get back to running a weekend marathon, walks with the dogs, or family time. Whenever these injuries get in the way, then that’s the conversations we have — how to make them and their life better,” says Anciano.
Orthopedic Dangers of Diabetes
Diabetic patients, along with individuals with other systemic diseases, are perhaps the most complex sector of Anciano’s patient population. Anciano believes one of the biggest misconceptions among non-orthopedists is that all foot and ankle pain originates in the foot and ankle. He points out that there are many conditions, including diabetes, cardiac and lung diseases, and lumbar radiculopathy that can cause edema, pain, or neuropathy in the foot. Therefore, it is often the orthopedic surgeon’s mission to get to the real root of the problem. Anciano says, “The challenge comes in understanding that it’s not just looking at
the foot, but making sure the patient has the care they need for the other things that are going on in their life and with their health.”
One of the most serious situations with diabetic patients is Charcot arthropathy. This advanced neuropathy leads to a loss of sensation that results in foot injuries and deformities that, left untreated, can lead to amputation. Diabetics who undergo a high-level amputation have approximately a 50% five-year mortality rate. Therefore, patient education, alongside Charcot reconstructive surgery, is crucial. Anciano stresses to these individuals that lifestyle changes and treatment compliance can mean the difference between losing a limb or not.
In closing, Anciano acknowledges that though foot and ankle surgeons are not normally in the business of saving lives, they do save the quality of life for their patients. In Anciano’s words, “We (foot and ankle surgeons) very rarely deal with life and death issues, but we do save quality of life, and I think it’s very important for people to have that … to be happy, to be healthy.”
28 MD-UPDATE
Disclaimer: Victor Anciano, MD, holds a consulting agreement with Medline.
Fellow UofL Health orthopedic surgeon Logan Mast, MD, with Victor Anciano, MD, and “Louie the Cardinal” at Fenway Park in Boston.
FUN FACT: Dr. Anciano says that If Barbie paid a visit to him with foot complaints, she would likely be diagnosed with metatarsalgia, equinus deformity with a mild cavus, and webbed toes and be treated with an Achilles lengthening procedure and a cavus foot reconstruction.
SPECIAL SECTION ORTHOPEDICS
PHOTO BY SCOTTY PERRY
The Secret to Kicking the Procrastination Habit: Stop Beating Yourself Up and Do This Instead
BY JAN ANDERSON, PSYD, LPCC

My husband: “Want to get lunch?”
Me: “I can’t. My deadline for the article on procrastination is due tomorrow to MD-Update magazine.”
My husband (laughing): “I can see why you were asked to write about that. You procrastinate like a pro.”
I can understand my husband’s reaction. He’s more what organizational psychologist Adam Grant calls a “precrastinator,” someone who wakes up with a compulsive need to get things done as soon as possible, even if the deadline is six months away.
My husband and I have a running argument about how late I actually was for our first in-person date years ago. I’m sure I wasn’t more than ten minutes late, but he swears that he’d put on his jacket and was getting ready to leave because he thought he’d been stood up.
Me: Here’s why I’m writing an article on procrastination: It’s a sign that I’ve broken up with my perfectionism! I don’t have to be
perfect to share what I’m learning as a “recovering” procrastinator, right? As they say in rehab, “Relapse is part of recovery.”
My husband: Keep going to your meetings.
Procrastination has a bad reputation. It can give you one, too.
But is true? Take my two-question procrastination quiz to find out.
Question #1: Procrastinating, the act of unnecessarily putting off decisions or actions, means you are:
a. Lazy.
b. Careless.
c. Disorganized.
d. Unprofessional.
e. All of the above.
Answer: None of the above. You wouldn’t keep procrastinating if you weren’t getting something out of it. (That’s why stupid is not one of the choices above.)
You are using procrastination to help you escape the negative emotions that are triggered by things you need to get done.
Question #2: Is procrastination a problem with time management and willpower?
Answer: No. Procrastination is a way to manage unpleasant emotions. Procrastination uses a powerful emotion-focused coping strategy — avoidance — to feel better in the present moment. Future moment be damned.
Our Brains Are HabitMaking Machines
One of the great things about your brain is that it is very efficient at forming habits. Once routine or mundane tasks become habits, they can run on autopilot and free up your grey matter to focus on other important stuff.
But there is a flip slide. Bad habits, like procrastination, go on autopilot, too.
Those unpleasant emotions flying under your radar (restlessness, boredom, anxiety, worry, etc.) can instantly and automatically, without your awareness or permission, trigger
a procrastination habit behavior, like:
• Checking your news feed
• Catching up on your email
• Snacking
• Surfing the internet
• Going on social media
• Watching television or YouTube videos
• Doing easier tasks or chores, like cleaning or organizing
• Doing some other “productive” task rather than the project or task at hand
How Your Brain Can Get Stuck in a Procrastination Habit Loop
According to neuroscientist and addiction psychiatrist, Jud Brewer, the discomfort of uncertainty affects your brain the same way an empty stomach rumbles with discomfort when you’re hungry.
When your stomach is empty, the discomfort alerts you to go get some food. If your stomach is really empty, you want to get food fast. Any food.
In a similar way, when you’re feeling the discomfort of a difficult task with an uncertain outcome, your brain knows that a little hit of certainty will make you feel better fast. Handy digital “certainty snacks” are at your fingertips. All you have to do is start scrolling.
Before you know it, this efficient way of quickly dismissing unpleasant feelings associated with unpleasant tasks goes on autopilot. Now you’re reaching for handy “procrastination bites” without even thinking about it.
The immediate problem (unease, anxiety, uncertainty) is solved ... temporarily. But the real problem (the looming deadline) is not. Now you feel even worse.
Here’s the crazy part: The worse you feel, the more likely you are to start the whole habit loop again. Remember how procrastination is about trying to get rid of unpleasant emotions?
ISSUE #147 29
MENtAL WELLNESS
Welcome to a habit loop that seriously sucks.
To Work with Your Mind, You Have to Understand How It Works
When you feel stressed at the prospect of an unpleasant task, your survival brain (the amygdala) responds by secreting chemicals that shut down your thinking brain (your prefrontal cortex). That leaves you with survival brain options only — fight, flight, freeze, or appease. When you find yourself acting impulsively, you’re probably in survival brain mode.
So how do you get your thinking brain back online?
Procrastination is a problem with emotional regulation, remember? So the first place to start is, well, with your emotions.
Don’t worry. Whether you’re someone completely dissociated from your feelings, constantly overwhelmed by them, or swinging wildly from one extreme to the other, there’s hope for you.
How do I know this? As a recovering procrastinator (I’m a lifetime member), I stumbled upon Dr. Jud’s groundbreaking research on habit change. It’s been shown to be effective with heavy-hitters like smoking, overeating, anxiety, and worry. My results so far are promising.
How to Hack into Your Brain’s Autopilot
Don’t get upset with your brain for going on autopilot and taking you on detour after detour.
The problem is not that there’s something wrong with your brain or its wiring.
The problem is that your brain’s autopilot is operating on outdated, incomplete information.
It’s time to hack into your brain’s autopilot programming; install some updates and add in some real-time input.
Start with a simple formula (an abbreviated form of Dr. Jud’s habit change process) to break down one of your own procrastina-
tion habit loops: When I do ______, I get _______. It costs me _______.
Here’s an example:
When I: Put off finishing the current chapter in my book by doing something else “productive.”
I get: Brief relief from feeling lost and confused about how to organize the concepts in this chapter.
It costs me: An inner critic attack for another other delay in getting the book finished and into the hands of people who could benefit from it.
Remember the crazy part? Because now I feel even worse; I’m at risk of reentering the habit loop and starting another spin cycle of procrastination.
Remember how procrastination uses a powerful emotion-focused coping strategy — avoidance — to feel better in the present moment?
Fortunately, there’s an antidote to avoidance.
Curiosity Is Your Superpower in Your Quest to Quell Procrastination.
Because curiosity intrinsically feels good, it can have an undoing effect on those unpleasant emotions that triggered you in the first place. Curiosity also has the capability to increase your distress tolerance. This ability to self-regulate can help shut down procrastination or help you ward off an inner critic attack when you do screw up.
The next time you realize you’re in a procrastination habit loop, try a bold, counterintuitive move:
Instead of trying to avoid, ignore, or overpower the bad feelings, tap into your natural curiosity and turn toward the unpleasant emotions as you answer the questions below. You don’t have to be brave. Just be curious. As author James Stephens wrote, “Curiosity will conquer fear even more than bravery will.”
1. What’s it like?
Example: What’s it like to make no progress in getting your book done? It feels awful. I’m so mad at myself. It’s a helpless feeling.
Hint: Tap into your sensory experience (for example, This doesn’t feel good is a more powerful motivator for behavior change than simply thinking I should/shouldn’t do this.)
2. What do you tell yourself?
Example: My publisher is going to be so frustrated with me and disappointed. He’s probably going to give up on me.
3. What are you getting from this now?
How about later?
Now: Right now, I get the illusion that I can scare myself into getting this done.
Later: Then I freeze up and get nothing done. And have another inner critic attack.
4. Is there a better way to handle this?
The feel-good chemicals generated by curiosity will help you seek out and experiment with different behaviors that may work better. Dr. Jud calls this process looking for the BBO (the bigger, better offer). Is there a better way to handle this? What can I try that may produce better results?
Example: Want to try something radically different? Procrastination researcher Timothy Pychyl found that self-forgiveness when you procrastinate was related to less procrastination in the future. Pychyl concluded that “This finding reflects the power of forgiveness to move us from an avoidance motivation to an approach motivation.”
As you explore and experiment with different behaviors, your orbitofrontal cortex (OFC) will fire up and do what it’s uniquely designed to do: compare the relative reward value of various behaviors, determine which ones are most rewarding, and shuffle them to the top of your greatest hits list.
And try savoring the good feelings associated with any wins and success experiences. (Yes, that’s radical, too. Do it anyway.) It will help your OFC reinforce the new habit behavior. You won’t need to resort to force, shame, or scare tactics in order to get things done.
I’ve shared here a very abbreviated version of Dr. Jud Brewer’s habit-change process. If you want to do a deeper dive, please contact me!
30 MD-UPDATE
MENtAL WELLNESS
Physician Named Baptist Health Louisville President
LOUISVILLE In July, Jonathan A. Velez, MD, became president of Baptist Health Louisville taking over for Larry Gray, who retired after a 40-year career with Baptist Health.

The 51-year-old Velez had served as chief operations and physician executive at Gulf Coast Medical Center in Ft. Myers, Florida.
“Dr. Velez’s has a wealth of experience in several key areas, including building relationships with medical staff, overseeing a robot-assisted surgery program, and adopting best practices to improve the quality of patient care, said Patrick Falvey, Baptist Health system chief operating officer.
“We look forward to working with Dr. Velez at Baptist Health Louisville, where we have several major projects including a heart
New Surgeon and Gastroenterologist Join Baptist Health Louisville
LOUISVILLE Katherine
surgery expansion with new cath labs, a 40-bed rehabilitation hospital in the East End and our Baptist Health Breckenridge healthplex set to open in July,” said Carl Thomas, hospital administrative board chair.
Velez began his healthcare career in Colorado Springs, Colorado spending 11 years as an emergency medicine physician. The University of Pennsylvania School of Medicine graduate received his bachelor’s degree in computer science.
While working in the ER, Velez took on administrative roles melding his information technology and medicine backgrounds. In 2007, he joined Memorial Health System in Colorado Springs as its chief medical information officer (CMIO). He left that posi-
tion in 2012 when he joined Hartford HealthCare Corporation in Connecticut, as VP and CMIO for the five-hospital system. There, he led the effort to implement the Epic electronic medical record. In 2015, he was promoted to VP of medical affairs. In 2017, he moved to Florida to join Lee Health’s Gulf Coast Medical Center.
New Physician Joins Baptist Health Medical Group in Elizabethtown and Bardstown
Yared, MD has joined the Baptist Health General Surgery team. Yared specializes in general surgery procedures, breast surgery, minimally invasive surgery, as well as gallbladder surgery and hernia repair.

Daniel specializes in the diagnosis and treatment of conditions affecting the esophagus, stomach, intestines, and colon. He received his medical degree from the University of Tennessee College of Medicine and completed an Internal Medicine residency and Gastroenterology fellowship at the University of Louisville.
Katherine Yared, MD

Yared has a certification in LGBT Health and Wellness Competency.
She trained at the University of Louisville School of Medicine, earning a Distinction in Medical Education honor. Yared completed her General Surgery residency at the University of Tennessee Medical Center.
New Gastroenterologist Joins Baptist Health
LOUISVILLE Harrison
Daniel, MD is joining Baptist Health Medical Group Gastroenterology, with practice locations in La Grange, Louisville, and Shelbyville.

Erin Drenkhahn, MD, Joins Baptist Health Medical Group in Lexington

LEXINGTON Erin Drenkhahn, MD, has joined the Baptist Health team to offer family care for life, seeing patients of all ages from newborns to seniors. Her services include preventive care, well visits, and care for chronic conditions, including diabetes and hypertension. Drenkhahn is board certified in family medicine and serves as the chairperson of outpatient medicine at Baptist Health.
erin Drenkahn, MD
Drenkhahn is a graduate of the Saint Louis University School of Medicine. She completed her Family and Community Medicine residency at the University of Kentucky Albert B. Chandler Hospital.
Jeffrey Austin, MD, has joined Baptist Health Medical Group General Surgery to offer compassionate, patient-centered care. Austin specializes in da Vinci® robotic surgery and minimally invasive laparoscopic and endoscopic surgical procedures involving the thyroid, parathyroid, gallbladder and colon, as well as abdominal hernia repair and more.
ELIZABETHTOWN
A native of Bowling Green, Kentucky, Austin earned his medical degree from the University of Louisville School of Medicine and completed his general surgery residency at Charleston Area Medical Center in Charleston, West Virginia. He has earned certification in da Vinci Xi™ robotic surgery as well as endoscopic and laparoscopic surgeries. In addition, he has completed the Advanced Surgical Skills for Exposure in Trauma course. He is a member of the American College of Surgeons and the American Medical Association.
SEND YOUR NEWS ITEMS TO MD-UPDATE > news@md-update.com News News SEND YOUR NEWS ITEMS TO MD-UPDATE > news@md-update.com PHOTOs PROVIDeD BY BAPTIsT HeALTH
Harrison Daniel, MD
Jeffrey Austin, MD
ISSUE #147 31
Jonathan A. Velez, MD
UofL Health and Lifepoint Rehabilitation Celebrate Opening of New Rehabilitation Hospital in Louisville

LOUISVILLE On July 19, 2023, UofL Health and Lifepoint Rehabilitation, a business unit of Lifepoint Health, celebrated the opening of Frazier Rehabilitation Hospital – Brownsboro, a 55,000-square-foot inpatient rehabilitation hospital now serving patients in eastern Louisville.
“Accessible and affordable healthcare is a right for every Kentuckian,” said Kentucky Lt. Governor Jacqueline Coleman in attendance. “The new Frazier Rehabilitation Hospital –Brownsboro will help patients recover and return home. I applaud UofL Health and Lifepoint Rehabilitation for their investment in Team Kentucky.”
With 40 beds, the new facility anticipates serving more than 1,200 patients each year, addressing a growing need for inpatient rehabilitation services throughout the region. Inpatient rehabilitation facilities offer patient-centered therapy programs designed to support those who have experienced a loss of function from an injury or illness through intensive, specialized treatment and recovery.
“UofL Health and Lifepoint Health are proud to share the common rehabilitation goal of helping each individual reach their fullest potential,” said Tom Miller, CEO of UofL Health. “This new hospital increases rehabilitation access in multiple ways. The location is convenient for the growing east end of Louisville, and it frees up essential space to further grow specialty programs only available downtown. I applaud Lifepoint for this joint
investment and we look forward to serving even more of our community.”

Frazier Rehabilitation Hospital –Brownsboro provides acute rehabilitation and recovery for patients who suffer from stroke, traumatic brain injury, spinal cord injury, complex neurological disorders, orthopedic conditions, multiple traumas, amputation, and other injuries or disorders. The facility includes all private rooms, a secured brain injury unit with private dining and therapy gym, a therapeutic exterior courtyard outfitted with activities and equipment to promote ambulation, large interdisciplinary therapy gyms and a transitional living apartment designed to support patients in preparing for activities of daily living.
“We are proud to partner with UofL Health as we expand access to care for inpatient
rehabilitation services in Louisville,” said Russ Bailey, President of Lifepoint Rehabilitation. “We strive in all that we do to help our patients recover as comprehensively as we can, so that they may return to their families and their daily lives as quickly as possible. We do this by bringing our industry-leading and evidence-driven framework for high-quality rehabilitation care. We’re excited to welcome patients to Frazier Rehabilitation Hospital – Brownsboro, and grateful to work alongside UofL Health as we advance our mission of making communities healthier.”
32 MD-UPDATE News
PHOTOs PROVIDeD BY BAPTIsT HeALTH
Frazier Rehabilitation Hospital - Brownsboro is located at 5000 Chamberlain Lane, near the intersection of I-71 and I-265 in the northeast area of Jefferson County. More information is at FrazierRehabBrownsboro.com.
Your Source for Graphic Design since 2003 GRAPHIC DESIGN • INTERACTIVE PUBLICATIONS • PROJECT MANAGEMENT and more... www.provationsgroup.com
Kentucky Lt. Governor Jacqueline Coleman and Karen Young, CeO, UofL Health Frazier Rehabilitation Hospital – Brownsboro cut the ribbon at the new rehabilitation facility with Matthew Adamkin, MD, medical director, extending a hand.


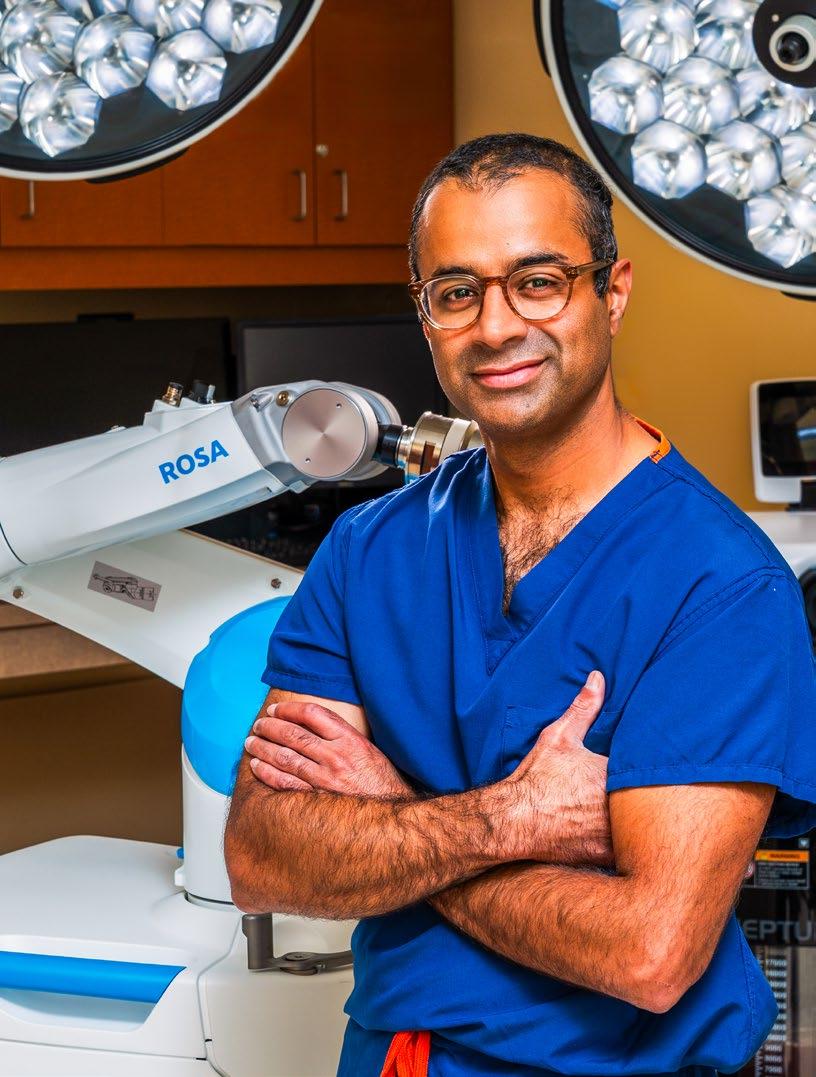



















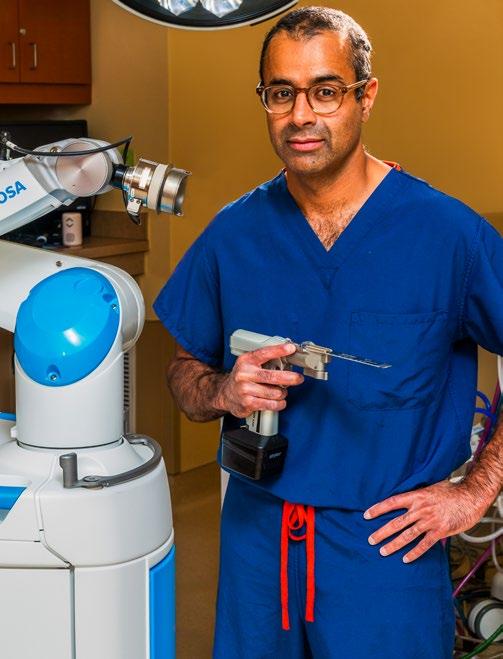






 BY BECKER’S HOSPITAL REVIEW
BY BECKER’S HOSPITAL REVIEW







 BY SARAH CHARLES WRIGHT
BY SARAH CHARLES WRIGHT






 BY JIM KELSEY
BY JIM KELSEY